Похожие презентации:
Drug allergy: the mechanisms of development, symptoms, diagnostics, and treatment. Measures preventing the drug allergy
1.
Zaporizhian State Medical UniversityPharmacology Department
Lecture № 3
DRUG ALLERGY: the Mechanisms of Development,
Symptoms, Diagnostics, and Treatment.
Measures Preventing the Drug Allergy.
2.
Adverse Drug Reactions (ADRs) include all unintendedpharmacologic effects of a drug except:
● Therapeutic Failures,
● Intentional Overdosage,
● Abuse of the Drug, or
● Errors in Administration.
ADRs are categorized into:
Type A: predictable (75%) – dose dependent, related
to the known pharmacologic actions of the drug, and
occur in otherwise healthy individuals
Type B: unpredictable (25%) reactions - generally
dose independent, unrelated to the actions of
the drug, and occur
2
only in SUSCEPTIBLE INDIVIDUALS.
3.
Unpredictable reactions:● Drug Intolerance
● Drug Idiosyncrasy
● Drug Allergy
● Pseudoallergic Reactions.
Drug allergy is a non-predictable immunologically
mediated ADR to a pharmaceutical and/or
formulation agent in a sensitized person.
Drug allergy differs from drug toxicity in many ways:
● The lesion produced by allergy is lower in incidence
● It is unpredictable;
● Prior exposure to the drug may cause sensitization;
● The lesion is dose independent and rash, fever,
eosinophilia and blood dyscrasias can occur.
3
4.
A. Humoral Type:Type I (Anaphylactic) reactions - Immediate hypersensitivity
reactions are IgE mediated:
Urticaria, Itching, Subepidermal Necrolysis – Lyell's syndrome,
Angioedema, Asthma, Rhinitis, Anaphylactic Shock.
Type II (Cytolytic) reactions are mediated by IgG or IgM:
Blood Transfusion Reactions, Haemolytic Disease of Newborns,
Autoimmune Haemolytic Anemia, Thrombocytopenia, Agranulocytosis,
Aplastic Anaemia, Haemolysis, Organ Damage (the liver, kidney,
muscle), Systemic Lupus Erythematosus and Some Drug Reactions.
Type III (Retarded) reactions are mediated by circulating antibodies
(predominantly mopping antibody, IgG):
Serum sickness - symptoms develop within 7-10 days and include
Urticaria, Lymphadenopathy, Myalgia, Arthralgia, Fever,
Polyarthritis Nodosa, Stevens-Johnson syndrome.
Systemic lupus erythematosus is an autoimmune disorder that may be
induced by Hydralazine, Novocainamide, Isoniazid and other drugs.
5.
B. Cell Mediated:Type IV (Delayed hypersensitivity) reactions:
several hours or days after exposure to the antigenare cell-mediated through production of sensitized
T-lymphocytes carrying receptors for the antigen.
On contact with antigen these T cells produce
limphokines which attract granulocytes and generate
an inflammatory response, e.g., contact dermatitis,
some rashes, fever, photosensitization.
5
6.
The antigen reacts with reaginic IgE antibodies, boundto the surface of mast cells and basophils, leading
to their degranulation and liberation of histamine
and other mediators:
●Those that Vascular Permeability and contract
smooth muscles: Histamine, PAF, SRS-A, Bradykinin.
●Those that are chemotactic for or activate other
pro-inflammatory cells: Leukotriene B4,
Eosinophil and Neutrophil Chemotactic Factors.
●Those that modulate the release of other
mediators: Bradykinin, PAF, Prostaglandins.
●Those which cause termination of the immune
inflammatory response.
6
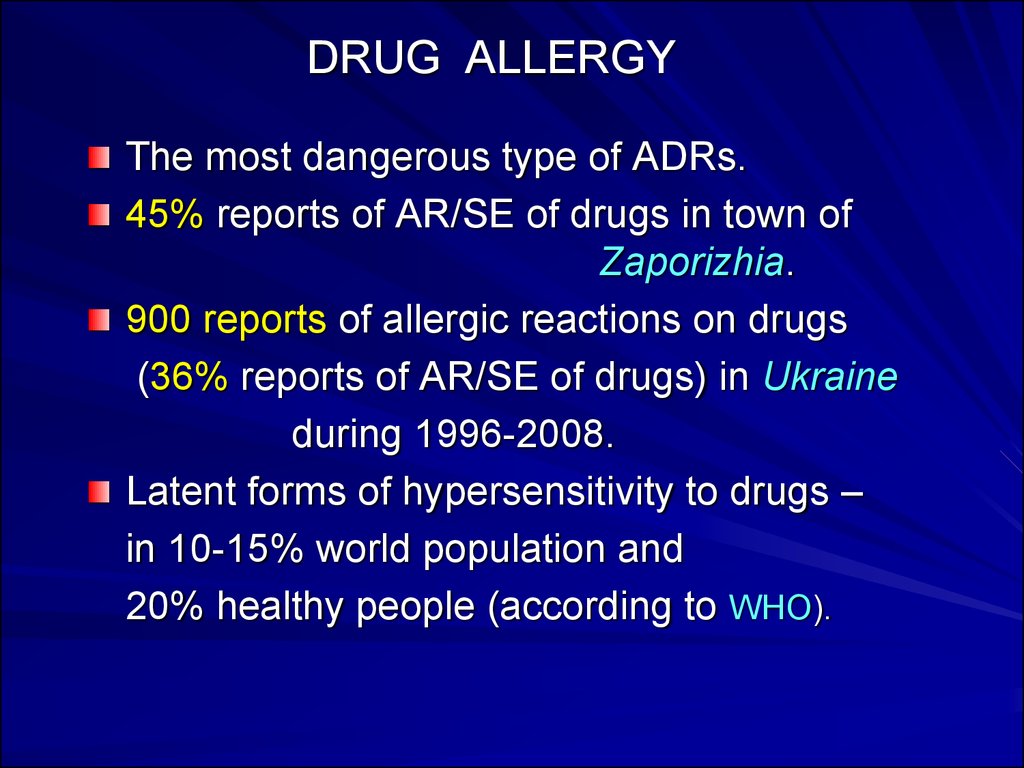
7. DRUG ALLERGY
The most dangerous type of ADRs.45% reports of AR/SE of drugs in town of
Zaporizhia.
900 reports of allergic reactions on drugs
(36% reports of AR/SE of drugs) in Ukraine
during 1996-2008.
Latent forms of hypersensitivity to drugs –
in 10-15% world population and
20% healthy people (according to WHO).
8. Allergic Anamnesis Ignoring
Analgin, Aspirin, Ampicillin were administered inpatients with allergic anamnesis (sometimes with other
trade names).
Severe allergic reactions were observed –
Anaphylactic Shock, Quincke‘s edema, Toxic Dermatitis.
Allergic reacitons on Flemoxin and Grunamox in
patients with drug allergy to Amoxicillin
Allergic reacitons on Solpadein the active substance
of which is Paracetamole.
The main reason of manifestation – absence of
knowledge of numerous trade names of
Generic Drugs containing the Same Active Agents.
8
9.
The various subtypes of T lymphocytes(Cytotoxic, Helper and Suppressor) and their
responses constitute Cell Mediated Immunity (CMI).
They regulate Humoral Immunity, B lymphocyte function.
T-cells carrying CD4+ antigen are responsible for
the HELPER function and the delayed hypersensitivity.
Th1 cells enhance CMI but inhibit Humoral Immunity.
Th2 cells have the opposite effect.
T-cells carrying CD8+ antigen are mainly responsible
for the CYTOTOXIC and SUPPRESSOR functions.
9
10.
The spectrum of drug allergic reactions and syndromesIgE mediated
Cytotoxic
Immune Complex
Hypersensitivity
vasculitis
Pulmonary Drug
Hypersensitivity
Clinical Manifestations
Examples of Agents
Urticaria, angioedema, bronchospasm, β-Lactam Antibiotics,
anaphylaxis, TEN
Chemotherapeutics, NSAIDs
Hemolytic anemia, thrombocytopenia, Penicillin, Quinine,
Sulfonamides
granulocytopenia
Serum sickness
Penicillin, Infliximab,
Thymoglobulin
Cutaneous or Visceral Vasculitis
Hydralazine, Penicillamine,
Propylthiouracil
Pneumonitis, Fibrosis
Nitrofurantoin, Bleomycin,
Methotrexate
DRESS
Drug Rash, Fever, Eosinophilia,
Anticonvulsants,
hepatic dysfunction, lymphadenopathy Sulfonamides, Allopurinol
Cutaneous Druginduced Lupus
Erythematosus
Immunologic
Hepatitis
Erythematous / Scaly Plaques
Hepatitis, Cholestatic Jaundice
Hydrochlorothiazide,
Ca2+ channel blockers,
ACE inhibitors
Para-aminosalicylic Acid,
Sulfonamides,
Phenothiazines
DRESS: Drug Rash with Eosinophilia and Systemic Symptoms;
TEN - Toxic Epidermal Necrolysis
10
11.
Atopic allergy and targets for therapyAllergen
IgE synthesis
Mast cells Degranulation
Mediator Release
Local Anaphylaxis (ATOPY)
Avoid allergen
Desensitize
Stabilize Mast Cell Membrane
(Cromolyn, Ketotifen, Ephedrine)
Mediator Antagonists
(Antihistaminics, Anti-cytokines)
Late Phase Inhibitors
(Glucocorticoids, Indomethacin)
Nose
GIT
Lungs
Skin
(Hay, fever) (Pain, Diarrhea) (Asthma) (Eczema)
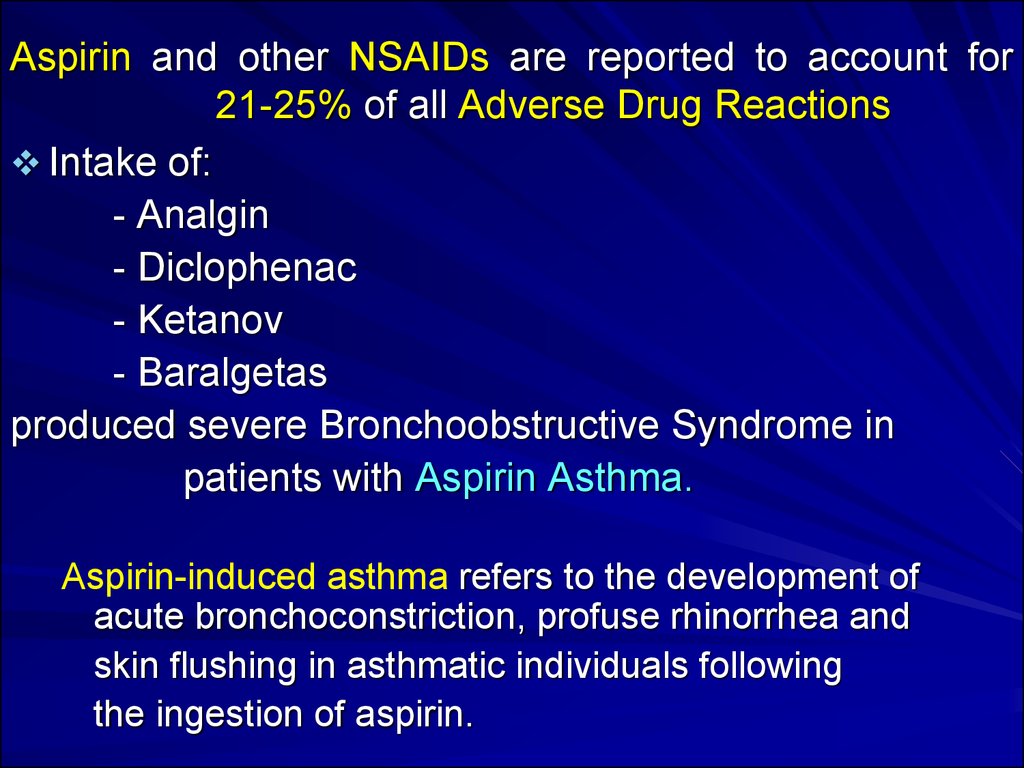
12. Aspirin and other NSAIDs are reported to account for 21-25% of all Adverse Drug Reactions
Intake of:- Analgin
- Diclophenac
- Ketanov
- Baralgetas
produced severe Bronchoobstructive Syndrome in
patients with Aspirin Asthma.
Aspirin-induced asthma refers to the development of
acute bronchoconstriction, profuse rhinorrhea and
skin flushing in asthmatic individuals following
the ingestion of aspirin.
13.
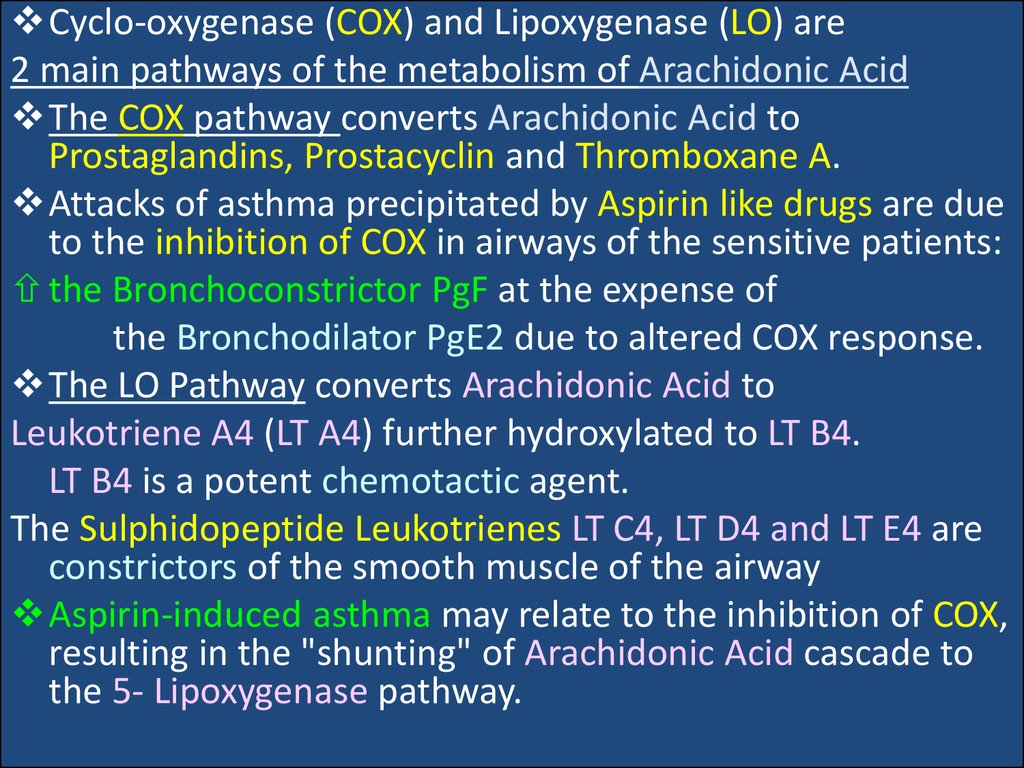
Cyclo-oxygenase (COX) and Lipoxygenase (LO) are2 main pathways of the metabolism of Arachidonic Acid
The COX pathway converts Arachidonic Acid to
Prostaglandins, Prostacyclin and Thromboxane A.
Attacks of asthma precipitated by Aspirin like drugs are due
to the inhibition of COX in airways of the sensitive patients:
the Bronchoconstrictor PgF at the expense of
the Bronchodilator PgE2 due to altered COX response.
The LO Pathway converts Arachidonic Acid to
Leukotriene A4 (LT A4) further hydroxylated to LT B4.
LT B4 is a potent chemotactic agent.
The Sulphidopeptide Leukotrienes LT C4, LT D4 and LT E4 are
constrictors of the smooth muscle of the airway
Aspirin-induced asthma may relate to the inhibition of COX,
resulting in the "shunting" of Arachidonic Acid cascade to
the 5- Lipoxygenase pathway.
14.
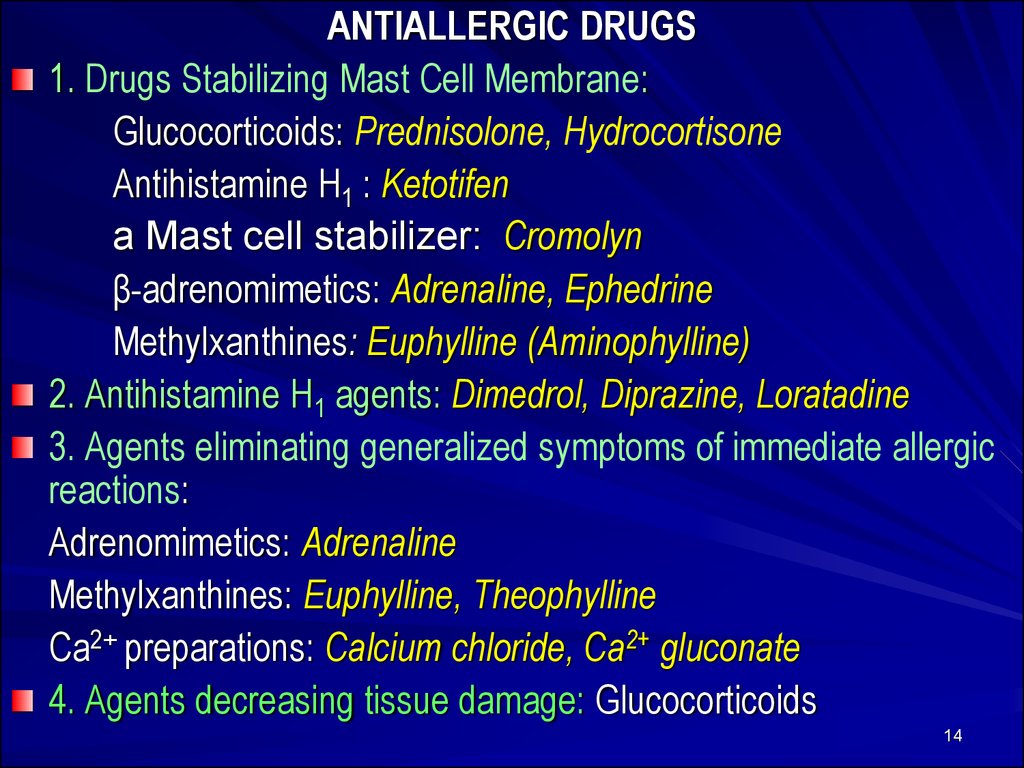
ANTIALLERGIC DRUGS1. Drugs Stabilizing Mast Cell Membrane:
Glucocorticoids: Prednisolone, Hydrocortisone
Antihistamine H1 : Ketotifen
a Mast cell stabilizer: Cromolyn
β-adrenomimetics: Adrenaline, Ephedrine
Methylxanthines: Euphylline (Aminophylline)
2. Antihistamine H1 agents: Dimedrol, Diprazine, Loratadine
3. Agents eliminating generalized symptoms of immediate allergic
reactions:
Adrenomimetics: Adrenaline
Methylxanthines: Euphylline, Theophylline
Ca2+ preparations: Calcium chloride, Ca2+ gluconate
4. Agents decreasing tissue damage: Glucocorticoids
14
15. GLUCOCORTICOIDS (GCs)
1. Short-acting: Hydrocortisone acetateCortisone
2. Intermediate-acting:
Prednisolone
Triamcinolone
3. Long-acting: Betametasone,
Dexametasone
OINTMENTS for local use - Fluorine-containing:
Synaflan, Flumethasone
AEROSOLS or POWDERS FOR INHALATIONS:
Beclometasone
Fluticasone
15
16.
Mechanism of Action of GlucocorticoidsSteroid hormones are lipid soluble and cross cell membranes
easily.
Once inside the cell, the hormone molecules bind with specific
receptor proteins.
The hormone–receptor complex enters the nucleus of the cell
where it activates Gene Expression –
nucleic acids (DNA and RNA) and
the Genetic Code to synthesize
new proteins.
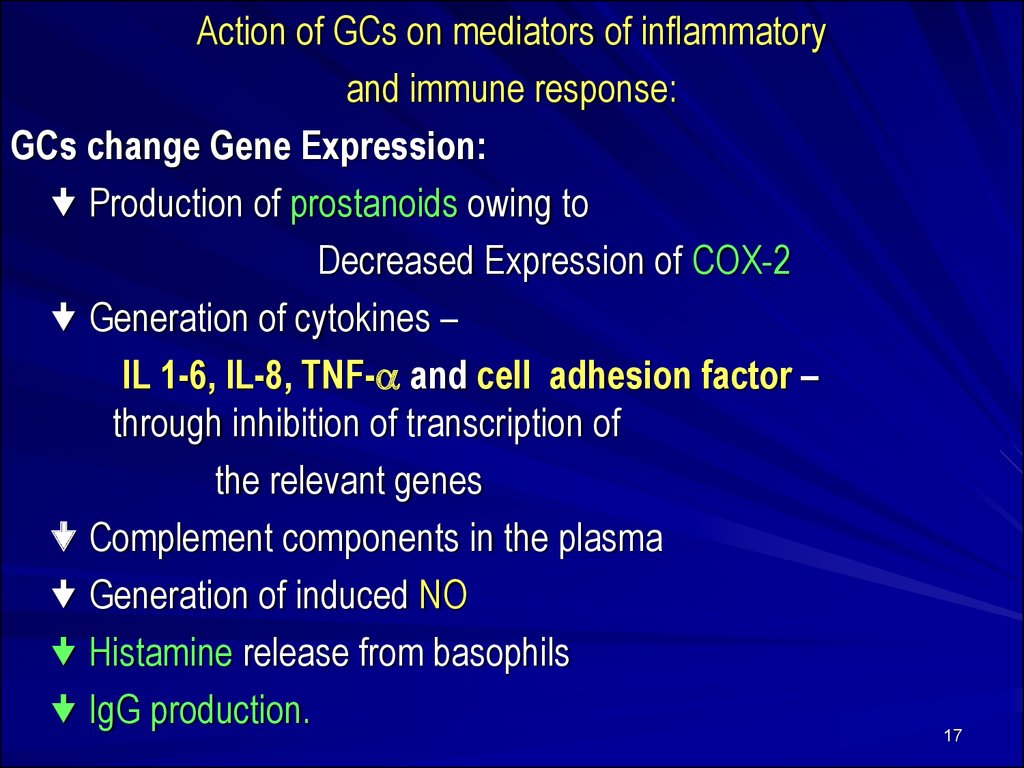
17.
Action of GCs on mediators of inflammatoryand immune response:
GCs change Gene Expression:
Production of prostanoids owing to
Decreased Expression of COX-2
Generation of cytokines –
IL 1-6, IL-8, TNF- and cell adhesion factor –
through inhibition of transcription of
the relevant genes
Complement components in the plasma
Generation of induced NO
Histamine release from basophils
IgG production.
17
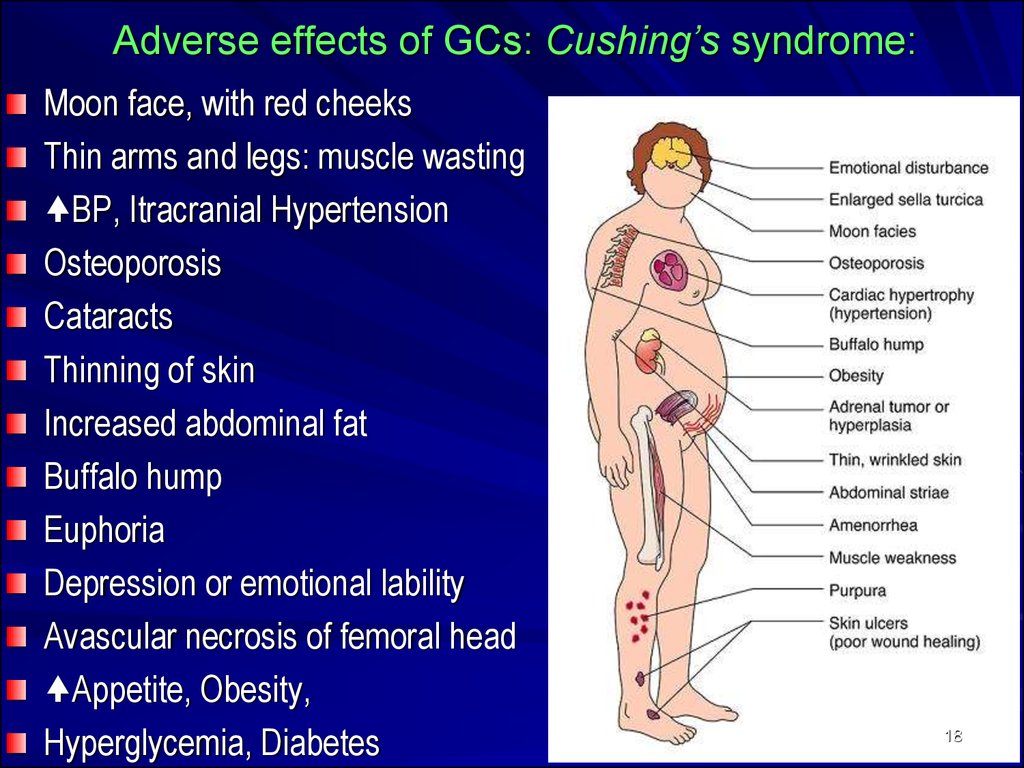
18. Adverse effects of GCs: Cushing’s syndrome:
Moon face, with red cheeksThin arms and legs: muscle wasting
BP, Itracranial Hypertension
Osteoporosis
Cataracts
Thinning of skin
Increased abdominal fat
Buffalo hump
Euphoria
Depression or emotional lability
Avascular necrosis of femoral head
Appetite, Obesity,
Hyperglycemia, Diabetes
18
19.
Cromolyn sodium (caps. 20 mg for inhalation) andNedocromil (aerosol: 2 mg/dose) stabilize mast cells and
prevent the release of bronchoconstrictive and inflammatory
substances when mast cells are confronted with allergens
and other stimuli.
They stabilize the mast cell membrane and inhibit release of
the mediators of Type I allergic reaction, including: histamine
and Slow Reacting Substance of Anaphylaxis (SRS-A) from
sensitized must cells.
Pretreatment with cromolyn blocks allergen-induced and
exercise-induced bronchoconstriction by acting on
inflammatory cells such as eosinophils.
19
20.
Ketotifen (tab. 1 mg), a cromolyn analog, is an antihistaminic(H1) and mast cell stabilizer.
● It inhibits stimulation of immunogenic and inflammatory
cells (mast cells, macrophages, eosinophils, lymphocytes,
neutrophils) and mediator release.
● It is believed to inhibit airway inflammation induced by
platelet activating factor (PAF).
Ketotifen prevents bronchial asthma attacks.
● It also produces relief in patients with rhinitis, atopic
dermatitis, conjunctivitis, urticaria, food allergy, migraine
Adverse effects: sedation, dry mouth, dizziness, nausea,
weight gain.
21.
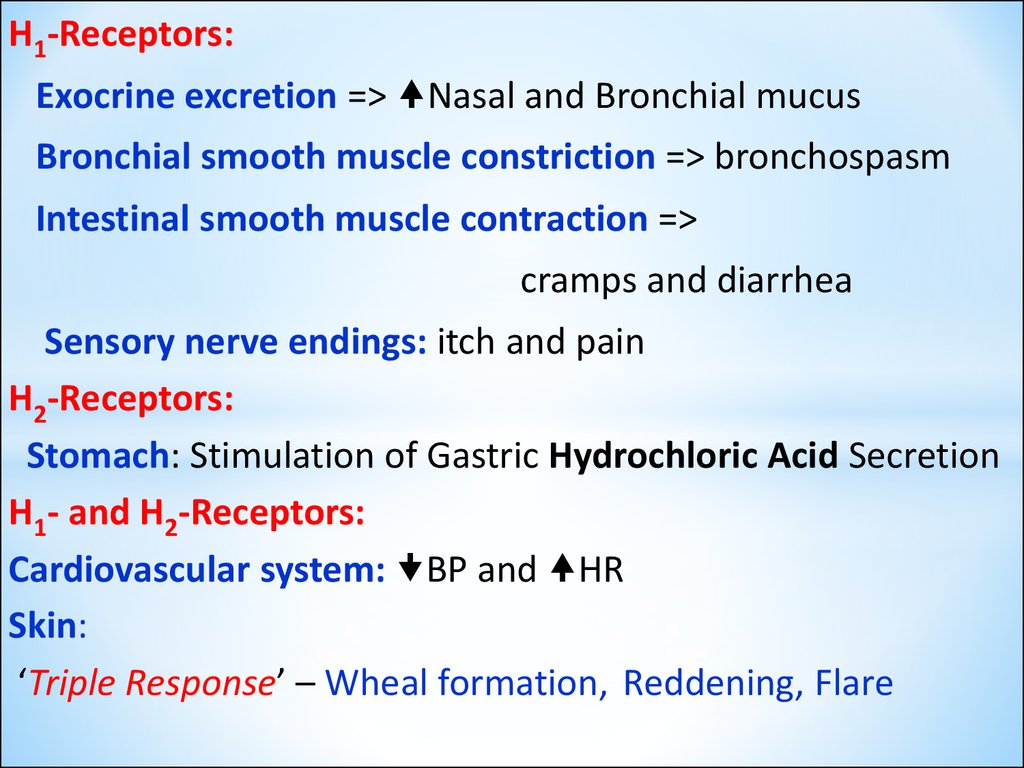
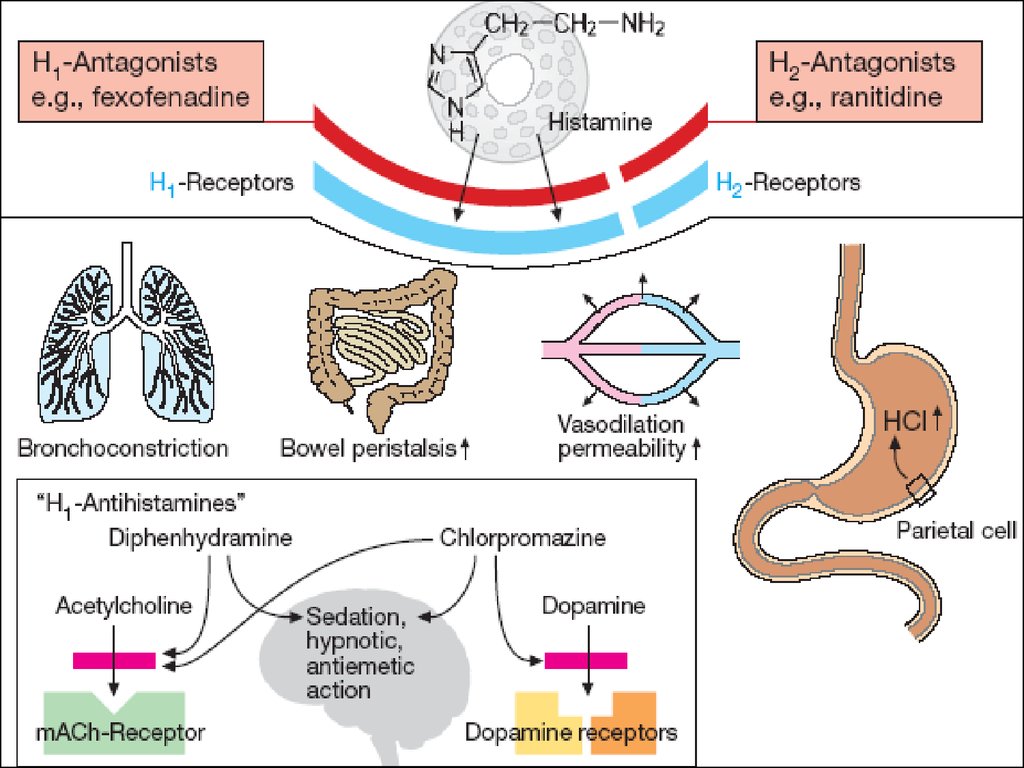
H1-Receptors:Exocrine excretion => Nasal and Bronchial mucus
Bronchial smooth muscle constriction => bronchospasm
Intestinal smooth muscle contraction =>
cramps and diarrhea
Sensory nerve endings: itch and pain
H2-Receptors:
Stomach: Stimulation of Gastric Hydrochloric Acid Secretion
H1- and H2-Receptors:
Cardiovascular system: BP and HR
Skin:
‘Triple Response’ – Wheal formation, Reddening, Flare
22.
2223.
H1-Receptor AntagonistsI GENERATION (SEDATIVE):
Dimedrol (Diphenhydramine)
Diprazine (Promethazine)
Suprastine (Chloropyramine)
Diazoline
Tavegyl (Clemastin)
II GENERATION (NON-SEDATIVE):
Loratadine (Claritin)
Terfenadine
Astemizole
Phencarol (Quifenadine)
III GENERATION (ACTIVE METABOLITES):
Telfast (Fexofenadine) 23
Zirtek (Cetirizine)
24.
Pharmacodynamics of antihistamine H1 blockersBlock the actions of histamine by reversible competitive
antagonism at the H1-receptor
Antagonist effects at other receptors:
M - Cholinoceptors
α1 - Adrenoreceptors
5-Hydrohytryptamine (5-HT) receptors
Diprazin Dimedrol Suprastin Diazolin
24
25.
Dimedrol (Diphenhydramine)-Tab 0.05 g, amp 1%-1 mlcompetes to H1 receptors on the smooth muscle of
the bronchi, GIT, uterus, and large blood vessels.
By binding to receptors, suppresses histamine-induced
allergic symptoms, even though it does not prevent its
release.
Central antimuscarinic actions is responsible for antivertigo,
antiemetic, and antidyskinetic action.
Clinical uses:
Allergy symptoms
Motion sickness
Parkinson’s disease
Nonproductive cough
Insomnia
25
26.
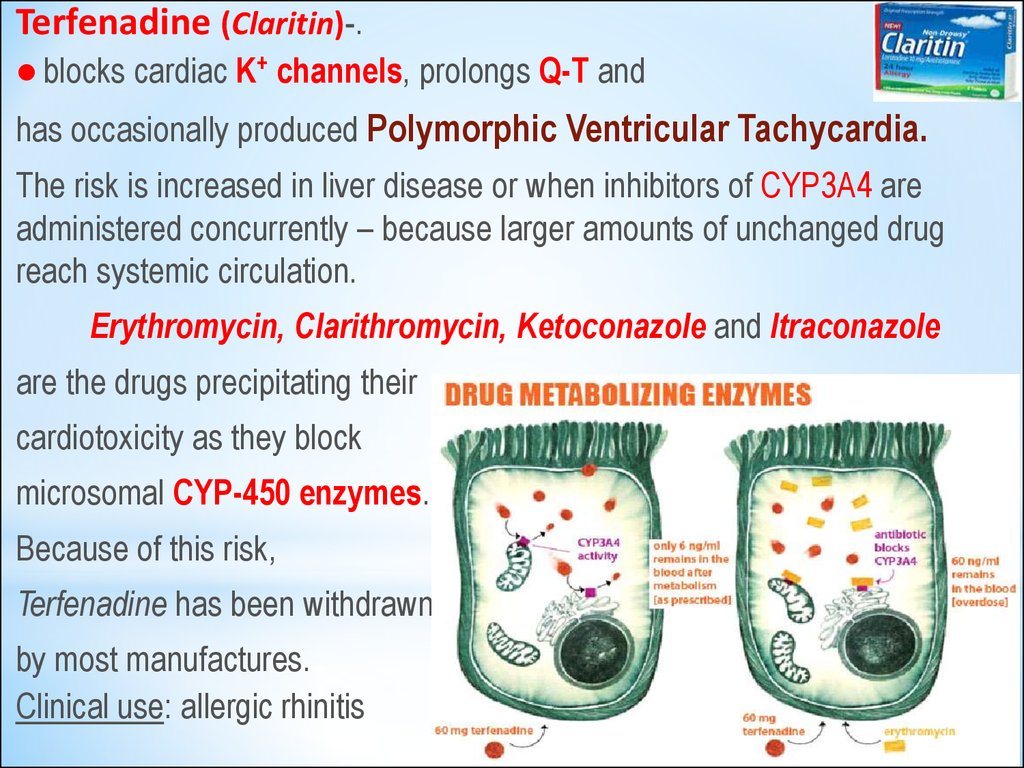
Terfenadine (Claritin)-.blocks cardiac K+ channels, prolongs Q-T and
has occasionally produced Polymorphic Ventricular Tachycardia.
The risk is increased in liver disease or when inhibitors of CYP3A4 are
administered concurrently – because larger amounts of unchanged drug
reach systemic circulation.
Erythromycin, Clarithromycin, Ketoconazole and Itraconazole
are the drugs precipitating their
cardiotoxicity as they block
microsomal CYP-450 enzymes.
Because of this risk,
Terfenadine has been withdrawn
by most manufactures.
Clinical use: allergic rhinitis
26
27.
Anaphylactic shockSympathomimetics:
Adrenaline h/ch - 0.1% sol.
0.3-0,5-1 ml in 2-3 ml of 0.9%
NCl solution SC in the region
of injection and around it,
SL or intratracheal instillation,
Mesaton 1% sol. 1-2 ml IV in
0.9% NaCl solution
Noradrenaline h/t 0.2% in
0.9% NCl solution IV infusion
Glucocorticoids:
Prednisolone 3% solution
30-90 mg and more IV
in 0.9% NCl solution
Cardiac
Glycosides:
Strophanthine
0.025% 1-2 ml IV in
0.9% NCl solution
Broncholytics:
Euphylline 2.4% sol.
3-5-10 ml IV
in 0.9% NaCl solution
Enzyme preparations:
Penicillinase
1000 000 UA in 2
ml of 0.9% NaCl solution in the
region of injection
Oxygen inhalation for
hypoxia control or
prevention
27
28.
Drugs used to treat Delayed Type Hypersensitivity Reactions:I. IMMUNOSUPRESSANTS - suppressing mainly
cell-mediated immunity:
1.Inhibitors of IL-2 production or action:
Cyclosporine (Sandimmune)
Tacrolimus
2.Inhibitors of cytokine gene expression:
Glucocorticoids: Prednisolone
3. Antitumor Cytotoxic Agents:
a) Alkylating agents: Cyclophosphan
b) Antimetabolites: Azathioprine, Mercaptopurine,
Methotrexate
4.Blockers of the T-cell surface molecules involved in signaling Monoclonal Antibodies: Basiliximab
and Daclizumab
28
29.
Drugs used to treatDelayed Type Hypersensitivity Reactions:
II. Drugs decreasing tissue damage –
1. Glucocorticoids
2. NSAIDs















 Медицина
Медицина