Похожие презентации:
Health care systems and policy. (Chapter 9)
1. Chapter 9
Health Care Systems andPolicy
© 2006 Thomson-
2. Learning Objectives
• Describe factors affecting the cost anddelivery of health care.
• Explain why health promotion is a major
component of the rhetoric about health
care reform at the national level.
• Differentiate between traditional
systems of health care and managed
forms of health care.
© 2006 Thomson-
3. Learning Objectives
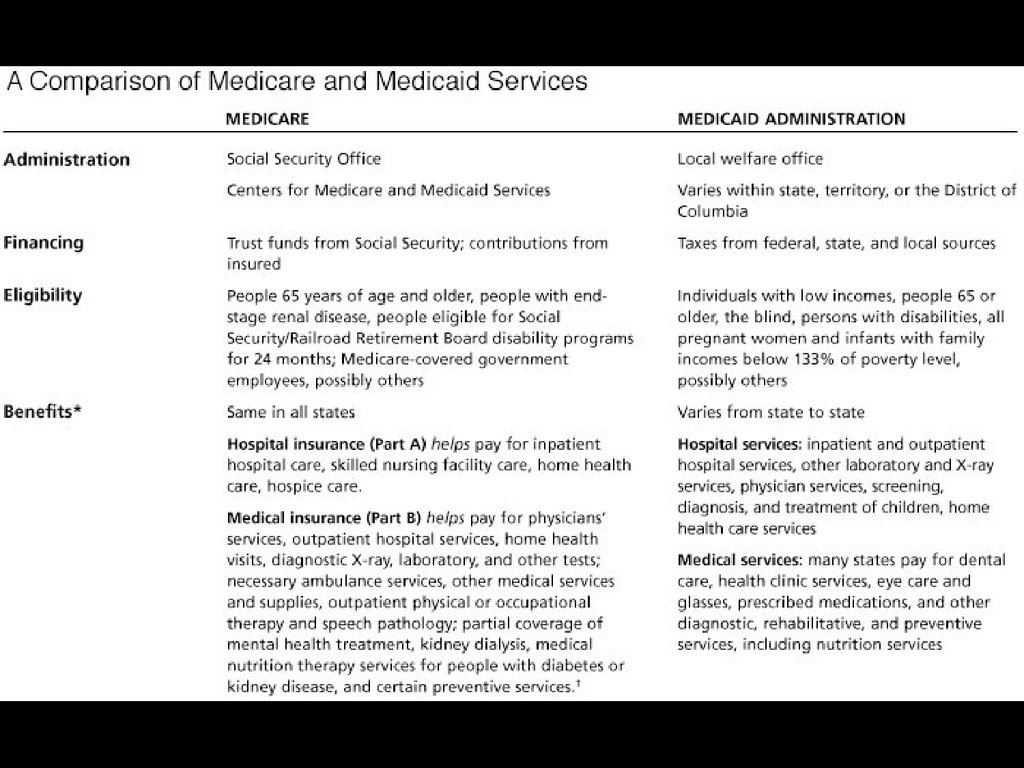
• Describe eligibility requirements for andservices provided to recipients of
Medicare and Medicaid.
• Identify consumer trends affecting
health care.
• State the value of using medical
nutrition therapy protocols to document
client outcomes in various health care
settings.
© 2006 Thomson-
4. Introduction
• In 2000, Americans spent morethan $1.2 trillion for health care
which represents over 13% of the
gross national product.
• This amount exceeds the average
amount spent by any other
industrialized country.
© 2006 Thomson-
5. Introduction
• Public policy is attempting to direct ourmedical system toward health promotion
although Medicaid and Medicare and other
major third-party payers offer limited
reimbursement for preventive procedures.
• Many studies show that early detection
and intervention, immunization, and
behavior change could significantly reduce
many of the leading causes of death and
disability.
© 2006 Thomson-
6. An Overview of the Health Care Industry
• Two general categories of healthinsurance in the United States:
– Private
• Traditional fee-for-service
• Group contract
– Public
• Medicare
• Medicaid
• State Children’s Health Insurance
Program
© 2006 Thomson-
7.
© 2006 Thomson-8. Private Insurance
• Approximately 70.2% ofAmericans have private insurance.
• Private insurance can be in the
form of traditional fee-for-service
insurance or group contract
insurance.
© 2006 Thomson-
9. Private Insurance
• Traditional Fee-for-Service Plans– Include a billing system in which the
provider charges a fee for each service
rendered.
– Critics of this plan claim that they
encourage physicians to provide more
services than necessary.
– Proponents prefer the greater flexibility and
unrestricted access to physicians, tests,
hospitals, and treatments.
© 2006 Thomson-
10. Private Insurance
• Group Contract Insurance– Managed-care systems, represented by health
maintenance organizations (HMOs) and
preferred provider organizations (PPOs), are
prepaid group practice plans that offer health
care services through groups of medical
practitioners.
– The goal of managed care is improved quality
of care with decreased cost.
– 91% of employees with health insurance were
enrolled in managed-care plans in 1999.
© 2006 Thomson-
11.
© 2006 Thomson-12. Private Insurance – Group Contract Insurance
• HMOs provide comprehensive servicesacross the continuum of care and they
make money by keeping people healthy.
• Prepaid group health plans emphasize
health promotion since they provide
health care services at a preset cost.
• By keeping people healthy, HMOs avoid
lengthy hospitalizations and costly
services.
© 2006 Thomson-
13. Private Insurance – Group Contract Insurance
• General HMO models:– Staff model
– Group model
– Network model
– Independent practice association
(IPA)
– Point-of-service (POS) plan
© 2006 Thomson-
14. Private Insurance – Group Contract Insurance
• In some HMOs, provider receives acapitation payment
– Capitation payment – A
predetermined fee paid per enrollee
per month to the provider
© 2006 Thomson-
15.
© 2006 Thomson-16. Public Insurance
• Medicare and Medicaid administered by the Centers forMedicare and Medicaid Services
(CMS)
• State Children’s Health Insurance
Program
© 2006 Thomson-
17.
© 2006 Thomson-18.
© 2006 Thomson-19. The Medicare Program
• Medicare is the largest health careinsurer in the U.S.
• It is designed to assist:
– People 65 and older
– People of any age with end-stage renal
disease
– People eligible for Social Security disability
payment programs for more than 2 years
– Qualified railroad retirement beneficiaries
and merchant seamen
© 2006 Thomson-
20. The Medicare Program
• Medicare consists of two separateparts:
– Hospital insurance (Part A)
– Medical insurance (Part B)
© 2006 Thomson-
21. The Medicare Program
• Medicare Part A– Provides hospital insurance benefits
that include up to 90 days of inpatient
care annually with a 20 percent
coinsurance fee.
– Hospital inpatient charges are
reimbursed according to prospective
payment system known as diagnosis
related groups (DRGs).
© 2006 Thomson-
22. The Medicare Program
• Medicare Part B– An optional insurance program financed
through premiums paid by enrollees and
contributions from federal funds.
– Enrolled Medicare Medical Nutrition Therapy
(MNT) providers are able to bill Medicare for
MNT services provided to beneficiaries with
type 1, type 2, and gestational diabetes,
nondialysis kidney disease, and post-kidney
transplants.
© 2006 Thomson-
23. The Medicare Program
• Coverage Gaps• Medicare Modernization Act
• Medicare Advantage Plan
© 2006 Thomson-
24. The Medicaid Program
• Medicaid is a joint state and federalprogram that provides assistance with
medical care for:
– Eligible, low-income persons
– Certain low-income pregnant women and
children
– The aged, blind, and people with disabilities
– Members of families with dependent
children in which one parent is absent,
incapacitated, or unemployed
© 2006 Thomson-
25. The Medicaid Program
• The individual states defineeligibility, benefits, and payment
schedules.
• Typically, one must meet three
criteria, including income,
categorical, and resource.
© 2006 Thomson-
26. The Medicaid Program
• Medicaid covers a variety of servicesand settings, including inpatient and
outpatient hospital services, physicians’
services, skilled nursing home and
home health services, and laboratory
and x-ray tests.
• To date, 36 state Medicaid programs
cover certain forms of nutrition services
provided by dietitians.
© 2006 Thomson-
27. The State Children’s Health Insurance Program
• The State Children’s Health InsuranceProgram (SCHIP) is the largest single
expansion of health insurance coverage
for children in more than 30 years.
• States have flexibility in targeting
eligible uninsured children.
• Many of the children served come from
working families with incomes too high
to qualify for Medicaid but too low to
afford private health insurance.
© 2006 Thomson-
28. SCHIP Enrollment, 1999-2003
© 2006 Thomson-29. The Uninsured
• The uninsured include the workingpoor and those who work for small
businesses.
• The employed uninsured number
15 million.
© 2006 Thomson-
30. The Uninsured
• The non-working uninsurednumber 9 million and include:
– The homeless
– Some deinstitutionalized mentally ill
patients
– Low-income people who do not
qualify for Medicaid
© 2006 Thomson-
31. % of U.S. Persons without Health Care Coverage, 2003
© 2006 Thomson-32. Demographic Trends and Health Care
• By the year 2030, the baby boomwill become a senior boom with 21
percent of the population over 65
years of age.
• Racial and geographical factors in
the population are also important
to the shape of the future.
© 2006 Thomson-
33.
© 2006 Thomson-34. The Need for Health Care Reform
• Health care reform refers to theefforts undertaken to ensure that
everyone in the U.S. has access to
quality health care at an affordable
price.
© 2006 Thomson-
35. The Need for Health Care Reform
• Some of the challenges of healthcare reform include:
– Making health care accessible to
everyone.
– Containing costs.
– Providing nursing home care to those
who need it.
– Ensuring that Medicare and Medicaid
can serve all who are eligible.
© 2006 Thomson-
36. The Need for Health Care Reform
• Cost, access, and quality areinterrelated and manipulating one has
an astounding impact on the others.
• Health care policy makers are studying
alternative models of delivery and
financing in hopes of applying other
nations’ successes to the U.S.
© 2006 Thomson-
37.
© 2006 Thomson-38. The High Cost of Health Care
• Health care inflation is wellestablished and the level of health
care activity is expected to grow as
a result of various factors
including:
– An aging population
– Increased demand
– Continuing advances in medicine
© 2006 Thomson-
39. National Health Expenditures (Billions of Dollars)
© 2006 Thomson-40. The High Cost of Health Care
• Major contributors to health careexpenditures in the U.S. are:
– The administrative cost of the
insurance process itself
– Professional liability costs
© 2006 Thomson-
41. The Nation’s Health Dollar, 2002
© 2006 Thomson-42. The High Cost of Health Care
• Efforts at Cost Containment– Efforts to curb soaring health care
costs cover a broad spectrum...
• from slowing hospital construction
• to reducing length of hospital stays, and
• increasing copayments and deductibles
for insured employees and Medicare
recipients.
© 2006 Thomson-
43. The High Cost of Health Care - Cost Containment
• One example of cost containmentis the prospective payment system
(PPS) that the federal government
implemented.
– The purpose of the PPS was to
change the behavior of health care
providers by changing incentives
under which care is provided and
reimbursed.
© 2006 Thomson-
44. The High Cost of Health Care - Cost Containment
• PPS (continued)– Prospective payment means knowing the
amount of payment in advance.
– PPS uses diagnosis related groups
(DRGs) as a basis for reimbursement.
– Patients are classified according to the
principal diagnosis, secondary diagnosis,
sex, age, and surgical procedures.
© 2006 Thomson-
45.
© 2006 Thomson-46. The High Cost of Health Care - Cost Containment
• PPS (continued)– There are 23 categories and a total of
490 DRGs.
– One consequence of PPS has been an
increased focus on outpatient
services.
© 2006 Thomson-
47. The High Cost of Health Care
• Equity and Access as Issues inHealth Care
– Public opinion polls in the U.S. reveal
that most people believe all citizens
are entitled to access to health care...
– but debate continues about the
acceptable level of health care and
what benefits should be included.
© 2006 Thomson-
48. The High Cost of Health Care – Equity and Access
• Racial and Ethnic Disparities inHealth
– A recent report released by DHHS
shows significant improvements in
the health of racial and ethnic
minorities but also indicates that
important disparities in health persist.
© 2006 Thomson-
49. Health Care Reform in the United States
• Almost all industrialized countriesexcept the U.S. have national health
care programs.
• In these systems, coverage is generally
universal and uniform and costs are
paid entirely from tax revenues or by
some combination of individual and
employer premiums and government
subsidization.
© 2006 Thomson-
50. Health Care Reform in the United States
• Health care reform in the U.S.raises a formidable list of issues
including:
– Overall cost containment
– Universal access
– Emphasis on prevention
– Reduction in administrative
superstructure and costs
© 2006 Thomson-
51. Health Care Reform in the United States
• While the government remainsundecided on what kind of health
care system is needed or how to
pay for it, health care reform is
evolving at an accelerating rate
without legislation.
© 2006 Thomson-
52. Nutrition as a Component of Health Care Reform
• Many believe that nutritionservices are the cornerstone of
cost-effective prevention and are
essential to halting the spiraling
cost of health care.
© 2006 Thomson-
53. Nutrition as a Component of Health Care Reform
• The American Dietetic Association(ADA) has urged that nutrition
services be included in any health
care reform legislation.
• Registered dietitians also need to
be recognized as the nutrition
experts of the health care team.
© 2006 Thomson-
54. Nutrition as a Component of Health Care Reform
• Cost-Effectiveness of NutritionServices
– ADA encourages all of its practitioners
to document the cost-effectiveness
of nutrition services.
– Cost-effectiveness studies compare
the costs of providing health care
against a desirable change in patient
health outcomes.
© 2006 Thomson-
55.
© 2006 Thomson-56. Nutrition as a Component of Health Care Reform
• Cost-Effectiveness (continued)– Effective nutrition therapy can produce
economic benefits as a result of altered food
habits and risk factors.
– Practice guidelines or protocols that clearly
specify appropriate care and acceptable
limits of care for each disease state or
condition are important to enhance the
quality, efficiency, and effectiveness of the
health care system.
© 2006 Thomson-
57. Nutrition as a Component of Health Care Reform
• Care delivered according to a protocolhas been linked with positive outcomes
for the client.
• Examples of outcomes include:
–
–
–
–
Measure of control (serum lipid profiles)
Quality of life
Dietary intake
Patient satisfaction
© 2006 Thomson-
58.
Measurable Outcomes ofNutrition Intervention
© 2006 Thomson-
59. Nutrition as a Component of Health Care Reform
• Developing standardized protocolsof care for nutrition intervention is
considered a must for achieving
payment for nutrition services and
expanding current levels of thirdparty reimbursement.
© 2006 Thomson-
60. Medical Nutrition Therapy and Medicare Reform
• The ADA believes thatreimbursement for nutrition
services through Medicare and
Medicaid is inadequate.
• ADA supports the inclusion of
medical nutrition therapy as a
covered benefit in all types of
health care delivery.
© 2006 Thomson-
61.
© 2006 Thomson-62. Medical Nutrition Therapy Providing Return on Investment
• Oxford Health Plan– Saved $10 for every $1 spent on nutrition
counseling for at-risk elderly patients
• The Lewin Group
– 8.6% reduction in hospital utilization for patients
with CVD
– 16.9% reduction in physician visits for patients
with CVD
– 9.5% reduction in hospital utilization for diabetes
patients
– 23.5% reduction in physician visits for diabetes
patients
© 2006 Thomson-
63. Medical Nutrition Therapy Providing Return on Investment
• University of California Irvine– Lipid drug eligibility was obviated in 34 of 67
subjects
– Estimated annual cost savings from the
avoidance of lipid medication was $60,652
• Pfizer Corporation
– Projected $728,772 annual savings from
reduced cardiac claims
• U.S. Department of Defense
– Saved $3.1 million the first year for CVD
patients
© 2006 Thomson-
64. Evaluating Nutrition Risk in Older Adults
• NSI DETERMINE Checklist - anutrition screening tool to help
identify warning signs of potential
nutrition problems.
© 2006 Thomson-
65. Evaluating Nutrition Risk in Older Adults
• “Determine Your Nutritional Health”Checklist
– I have an illness or condition that made me
change the kind or amount of food I eat.
– I eat fewer than two meals each day.
– I eat few fruits or vegetables or milk
products.
– I have three or more alcoholic drinks almost
every day.
– I have tooth or mouth problems that make it
hard for me to eat.
© 2006 Thomson-
66. Evaluating Nutrition Risk in Older Adults
• “Determine Your Nutritional Health”Checklist (continued)
– I don’t always have enough money to buy the
food I need.
– I eat alone most of the time.
– I take three or more different prescribed or
over-the-counter medicines a day.
– Without wanting to do so, I have lost or
gained 10 pounds in the last 6 months.
– I am not always physically able to shop, cook,
and/or feed myself.
© 2006 Thomson-
67. Evaluating Nutrition Risk in Older Adults
• Campaign Long-Term NutritionRisk Reduction
– Demonstrates how nutrition screening
and case management can help lower
nutrition risk among frail, homebound
older adults.
© 2006 Thomson-
68. Evaluating Nutrition Risk in Older Adults
• Goals and Objectives– Improve the nutritional status of frail,
homebound older adults receiving home
services under the Medicaid Waiver Program
by:
• Nutritionally screening clients
• Providing home-based medical nutrition therapy
where indicated
• Using a coordinated case management approach
to determine need for further services
• Evaluating the effectiveness of home-based
medical nutrition therapy
© 2006 Thomson-
69. Evaluating Nutrition Risk in Older Adults
• Methodology– Older adults contacted to complete
"Nutrition Screening Checklist"
– Clients identified as “at risk” referred for for
an initial home visit and in-depth nutritional
assessment
– MNT care plan devised and carried out
– In-depth nutritional assessment repeated at
discharge
© 2006 Thomson-
70. Evaluating Nutrition Risk in Older Adults
• Results– Semiannual samplings of 20% of all
discharged patients
– 89% of clients surveyed lowered their
nutrition risk scores after receiving
home-based medical nutrition
therapy.
© 2006 Thomson-
71. On the Horizon: Changes in Health Care and Its Delivery
• The future offers much that ispositive for the profession of
dietetics.
• Yet to be achieved are the
effective provision and allocation
of resources, such as nutrition
services as part of preventive care.
© 2006 Thomson-
72. On the Horizon: Changes in Health Care and Its Delivery
• A coordinated strategy for health care,political will, and active collaboration of
both health care professionals and
consumers of health care services will
be required to achieve this goal.
• Health care reform for the U.S. is
certain, but the exact nature of the
reform will continue to evolve.
© 2006 Thomson-
73. Ethics and the Nutrition Professional
• What Is Ethics?– A philosophical discipline that attempts to
determine what is morally good and bad,
right and wrong
• Codes of Ethics
– The ADA published its first code of ethics in
1942
– Most recent code became effective in 1999
– ADA code applies to all ADA members and
credentialed practitioners
© 2006 Thomson-
74. Ethics and the Nutrition Professional
• Guiding Principles– Autonomy - respecting the individual’s
rights of self-determination, independence,
and privacy
– Beneficence - protecting clients from harm
and maximizing possible benefits
– Non-maleficence - the obligation not to
inflict harm intentionally
– Justice - striving for fairness in one’s
actions and equality in the allocation of
resources
© 2006 Thomson-
75. Ethics and the Nutrition Professional
• Health Promotion and Ethics• Ethical Decision Making
© 2006 Thomson-









































































 Медицина
Медицина Финансы
Финансы Право
Право








