Похожие презентации:
Acute intestinal infections. Dehydration. Principles of rehydration therapy
1.
Acute intestinal infections.Dehydration.
Principles of rehydration therapy
2.
General characteristic of infectious diseaseswith fecal-oral mechanism of transmission
- particular localization of the causative agent GIT
(small or large intestine, rectum, mesenterium)
- the movement of the agent with feces or vomiting mass
- penetrate in a susceptible organism in a special ways of transmission
(watery, alimentary, contact-household)
- various factors of transmission (foodstuff, water, hands, insects, toys,
soil)
- different localization of the causative agent in the intestine: in lumen of
intestine, intestinal epithelium, on the mucous membrane, in lymphatic
tissue of intestine
-causative agent can constantly be in intestine (cholera, dysentery, some
helminthic invasion) or temporarily,
- the ability to penetrate from the intestine to the blood and other tissue
(ascariasis, amebiasis, strongyloidiasis, trichinosis, echinococcosis)
3.
- The incidence of infectious diseases is higher:- in the warm and/or rainy periods
(in moderate climatic zones is more often registered during
a summer or autumn);
- in countries with low socio-economic level of development;
- among people of risk-groups:
- age - children and the elderly,
- chronic GIT-pathology - patients with
gastritis, duodenitis, peptic ulcer, cholecystitis;
- profession - sanitary workers, plumbers, teachers,
medical personal;
- occupation – fishermen, water-rescuers,
veterinarians, animal trainers
4.
Diarrhea- disorder of frequency, volume and consistency of stool
accompanied with abdominal pains.
Diseases with diarrhea syndrome are divided on 3 types:
Type A - proceeding without an inflammation of intestine
Type B - proceeding with an inflammation of intestine
Type C - caused by the short-term penetration of infectious agents through
mucous membrane of intestine without damage
5.
Type A-In the small intestine;
-disorder of water and electrolyte absorption;
-Mucous membrane of intestine is not involved
in the inflammation (at biopsy of intestine –
morphological changes are insignificant
or not find);
-General symptoms:
fever, malaise, anorexia - are moderate or absent;
-Typical symptoms:
1) pain in mesogastrium;
2) plentiful, watery stool, meteorism;
3) in coprocytogramm – leucocytes are not found;
-This type of diarrhea can be caused by:
- viruses ( Rotavirus, Parvovirus etc.);
- toxicogenic bacteria (V. cholerae, E.coli, S.aureus, B. cereus);
- parasites (Giardia intestinalis, Ascaris lumbricoides, Cestodes,
Ancylostoma duodenale, Strongyloides stercoralis, Trichinella
spiralis, Cryptosporidium parvum and etc.)
6.
Type B– large intestine is involved and affected;
- inflammation of intestinal wall;
- infectious agents are implanted in a mucous membrane
of the large intestine and damage it;
- General symptoms:
fever, malaise, anorexia - are moderate or severe;
- Typical symptoms (colitis):
- pain in hypogastrium, painful spasms of large intestine, tenesmus;
- in coprocytogramm – leucocytes, admixture of mucus and blood;
- stool is scanty, brown or pink
- This type of diarrhea is caused by:
- bacteria ( Shigellae, Salmonellae, S. V. Parahaemoliticus, Yersinia
enterocolitica, E. coli, Campylobacter jejuni, Clostridium difficile)
- parasites (E. histolytica, Balantidium coli, Schistosomae)
7.
Type C- caused by penetration of infectious agent in mucous membrane and
lymphatic tissue of intestine (usually small intestine) without damage.
- General symptomes:
-fever, chills, headache, malaise, disorded sleep;
- Typical symptomes:
-diarrhea or constipation, mesadenitis,
-roseola-spot rash, bradycardia,
-hepatosplenomegaly,
-leukopenia,
- in coprocytogramm: -macrophages
The classical examples - Salmonella typhi, more rare - Yersinia
enterocolitica, Campylobacter jejuni, Pseudomonas aeruginosa
8.
Factors contributing to the development of diarrhea- the reduced acidity of gasric juice;
- nonactive intestinal peristaltics;
- imbalance of intestinal microflora;
- insufficien level of coproantibodies;
Sometimes diarrhea can develop as nonspecific response of human
organism on the severe infection proceeding outside of the intestine (more
often - in newborns, but can be in adults, caused by Gram-negative
microflora).
The reasons of noninfectious secretory diarrhea:
1. Exogenous: - after some medicine:
- purgatives
- antacids
- of diuretics, antiasthmatic, cholinergic, cardiac, thyroid, antimetabolitic
drugs
- prostaglandines
- toxins
- errors of a diet
- hypersensitivity of the intestine (without structural damage)
9.
2. EndogenousA.
B.
D.
E.
F.
G.
Congenital enzymopathy,
Na+diarrhea – absence of sodium (hydrogen in enterocytes)
The functional distresses of intestine
Colo-enteritis (ulcerous, ischemia, necrotization, hemorrhage )
Pellagra
Metabolic diseases - hyperthyroidism, insufficiency of adrenal
glands and pancreas
H. Allergy, purpura Schonlein- Henoch
10.
Clinical variants of diarrheaClinical criteria
Enteric
Colitic
(in small intestine) (in large intestine)
Stool
Frequency
More then 3 t/d
Consistency
watery and mushy
(porridge-like)
mushy (porridge-like)
Volume
plentiful
scanty
Color
yellow, orange, green,
transparent (depends
on the properties of
the pathogen)
brown, pink, red
Admixture
usually not, sometimes
mucus
often a lot of mucus
and blood like streaks
11.
Clinical variants of diarrheaClinical criteria
Enteric
(in small intestine)
Colitic
(in large intestine)
Pain
Localization
epigastric and
parumbilical area
hypogastrium, left iliac
region
Character
colics, spasms
cutting, cramping
pain, tenesmus
Example
Salmonellosis, cholera,
intestinal yersiniosis,
E. coli-infection
Shigellosis, amebiasis,
balantidiasis
12.
Criteria of degree of dehydration in choleraCriteria
I degree
II degree
III degree
Loss of body
mass
5%
8%
9% and more
Body
temperature
36,5-37,5ºC
36,5-37,0ºC
less 36,6ºC
Rate of stool
up to 15 times
20-25 times
more 25 times,
or absent
Frequency of
vomiting
till 10 times
10-20 times
More 20 times
or absent
13.
Criteria of degree of dehydration in choleraCriteria
I degree
II degree
III degree
Pulse rate
Normal
(80b/min)
80-120 b/min
More 120b/min
or week
Blood pressure
Normal
120/80-100/70
90/70-80/60
Less 80/60
70/40- 40/0
Daily diuresis
Normal
Olyguria
Anuria
Cyanosis
Absent or pale
skin
Acrocyanosis
Total cyanosis
Skin elasticity
and turgor
Normal
Decreased
Significantly
decreased
14.
Criteria of degree of dehydration in choleraCriteria
I degree
II degree
III degree
Muscle cramps
Absent
In 1-2 group of
muscles
Generalized
muscle cramps
Sonority of
voice
Weakened
Hoarseness
Aphonia
Thirst and
dryness of
mucous
membranes
Moderate or
absent
Expressed
The most severe
Ht
Up to 45%
Up to 65%
More 65%
Electrolyte
shifts in the
blood
Decrease
potassium (+)
Decrease
potassium (++)
and sodium (+)
Decrease
potassium
(++++)
sodium (+++)
15.
RehydrationPrimary
Replacement fluids
lost before
hospitalization
Compensatory
Recovery
of continuing
water and electrolyte
losses
during hospitalization
16.
Rules of primary rehydration1. Duration - 2-4 hours
(except for elderly, children, patients with chronic
pathology of the cardiovascular system, alimentary
cachexia: 6-8 hours);
To restore the balance of electrolytes, it is necessary to
determine the volume of the lost liquid (V);
To do this, you need to know the body weight (m) and the
degree of dehydration in percent (%)
2. To weigh the patient (body mass - m);
3. Regarding the existing clinical symptoms (see table) to
determine the degree of dehydration (according to WHO
classification) (%);
17.
4. The volume of the lost fluid is calculated by theformula:
m×%
V=
100%
5. To determine the method of introduction of fluid:
oral or parenteral:
- oral: 1-st and 2-nd degree of dehydration
without vomiting
V×1,5
1,5 - a constanta characterizes the ratio between
volume of fluid introduced in intestine and
absorbed into the blood
Oral solutions: rehydron, glucosolan, citroglucosolan;
18.
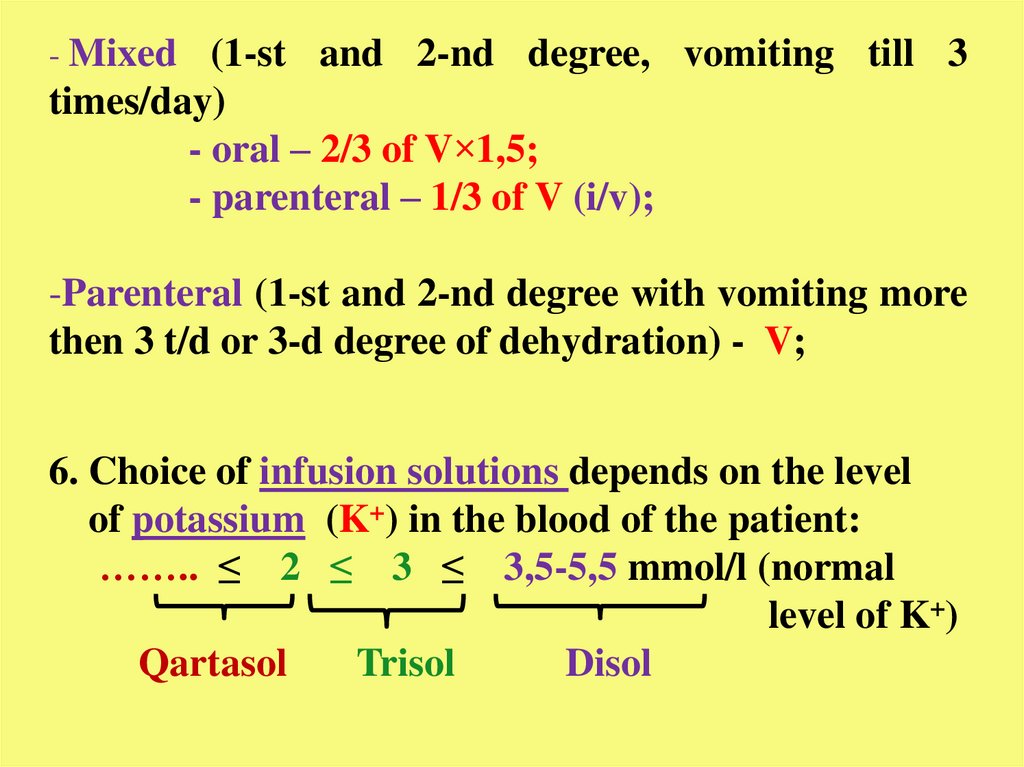
- Mixed (1-st and 2-nd degree, vomiting till 3times/day)
- oral – 2/3 of V×1,5;
- parenteral – 1/3 of V (i/v);
-Parenteral (1-st and 2-nd degree with vomiting more
then 3 t/d or 3-d degree of dehydration) - V;
6. Choice of infusion solutions depends on the level
of potassium (K+) in the blood of the patient:
…….. ≤ 2 ≤ 3 ≤ 3,5-5,5 mmol/l (normal
level of K+)
Qartasol
Trisol
Disol
19.
7. To determine the speed of intravenous infusion:1-st degree – 60-80 drops/min (usual);
2-nd degree – 100-120 drops/min;
3-d degree – by stream;
8. To stop i/v rehydration is possible, if there:
- no vomiting,
- constant, and normal pulse and blood pressure,
- daily diuresis exceeds the daily stool volume
in 1,5 times
20.
Salmonellosis- acute intestinal zoo-anthroponotic infection with fecal-
oral mechanism of transmission, described by a preferred
lesion of small intestine and development of severe
intoxication and diarrhea in the clinic.
ETIOLOGY:
- Family Enterobacteriaceae, genus Salmonella
-Includes 1 species, 7 subspecieses, 2300 serotypes
- Gram (-) motile rods without spors
- Has 4 antigenes: O – somatic antigene (lipopolysaccharid )
H- a flagellar antigene
K – a capsula antigene – facilitates infiltration
salmonella inside of enterocytes
Vi – virulence antigene
21.
-Produces: - enterotoxin – causes a diarrhea(activation a cAMP)
- cytotoxin - destroys the membrane of the cell,
disrupting the synthesis of proteins
- hyaluronidasum, neuraminidase,
R-plasmide (resistance)
-Releases: - endotoxin - (lipopolysaccharid the complex
cellular of a wall) causes a set of toxic
symptoms
-Grows well on usual mediums
-Stable in environment: - in water – 5 months
- in milk – 300 days
- at 18-24 dg C – 80 days
-Sensitive: - usual concentrations of desinfectants inactivate
in 30 min
- at boiling perish immediatly
22.
The factors of pathogenicity- Ability to endocellular parasitism
-K – antigene, promoting the infiltration
-R-plasmide – resistance to a/b
-Presence of aggressive enzymes
-Ability to cause a bacteriemia, sepsis
-Ability to reproduce in many bodies
-Ability to cause disbiosis
-Ability to derivate L-of the form
-Presence of toxins
23.
EPIDEMIOLOGY-Source of an infection – warm-blooded animals, swimming birds
- patient with manifested form of the disease
- carriers (especially chronic)
-Mechanism of transmission – fecal-oral
-Routs of transmission – alimentary, watery, contact
-Factors of transmission – foodstuffs (meat, lactic products, eggs, fish)
- contaminated water
- dust (at processing skins animal)
- contact with subjects of environment
-Risk groups – children till 2-5 years
- old people
- patient with chronic GIT-pathology
- immunocompromised patient
- Seasonal prevalence – summer-autumn
24.
PATHOGENY1. Penetration of S. through a mouth in stomach
2. Mass destruction with excretion endo- and exotoxin –
toxemia
3. Entering in small intestine, infiltration through
enterocytes, colony, reproduction, accumulation
4. Activation of cAMP, appearance of a secretory diarrhea
The destruction all S. at this stage causes only localized
form with subsequent recovery
5. Bacteriemia at gastrointestinal form is short-term, at
incompetence of immunity S. can penetrate into a blood,
causing hematosepses
25.
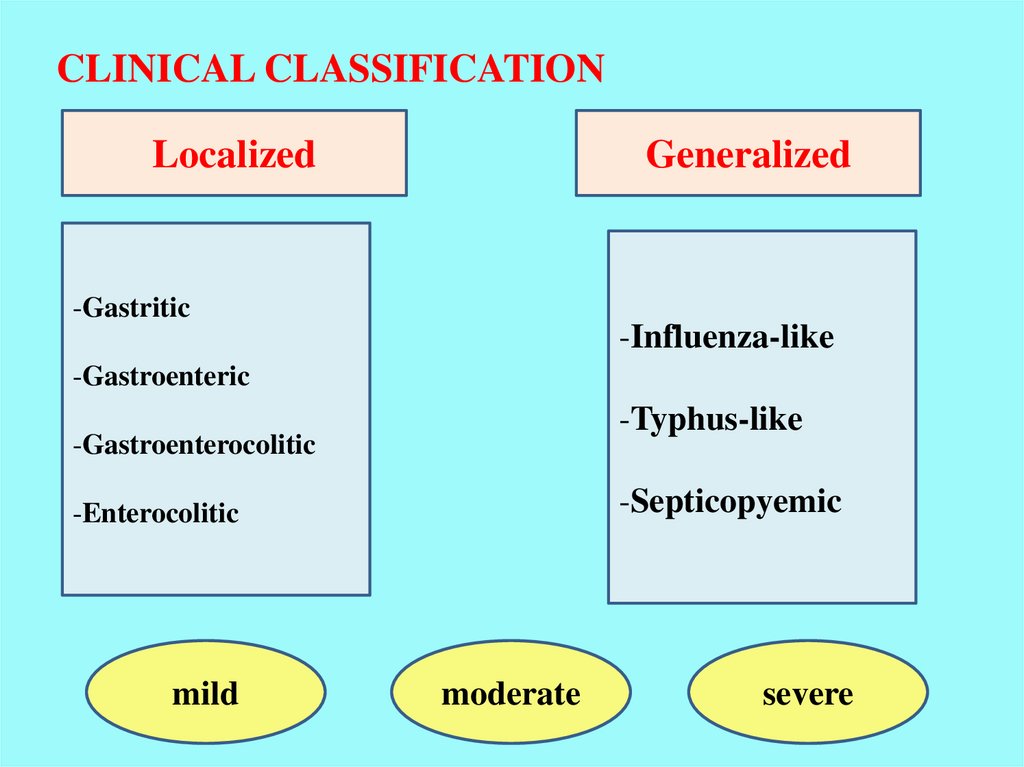
CLINICAL CLASSIFICATIONLocalized
Generalized
-Gastritic
-Influenza-like
-Gastroenteric
-Typhus-like
-Gastroenterocolitic
-Septicopyemic
-Enterocolitic
mild
moderate
severe
26.
THE SEVERITY OF SALMONELLOSISSYMPTOME
MILD
MODERATE
SEVERE
Duration the fever
1-2 days
3-6 days
7 and more
Height fever
Up to 38C
Up to 39 C
39 and more
Duration of
diarrhea
Up to 3 days
4-10 days
11 and more
The frequency of a Up to 5 t/d
stool
6-10 t/d
11 and more
The frequency of a 0-1 t/d
vomiting
2-4 t/d
5 and more
BP
norm
Up to 90
80 and lower
The pulse rate
Up to 100
Up to 120
120 and more
27.
LABORATORY INSPECTIONSPECIFIC TESTS (for confirmation):
1. Bacteriologic research:
material – feces, vomitive masses, gastric lavage (localized form)
- blood, urine, bile, liquor (generalized form)
medium – cholic broth, selenitic nutrition, bismuth-zinci sulfas
2. Serological test: - IHA test
- CF test
- ELISA
3. Immunofluorescence
4. Detection of antigenes S. in coprofiltrates (express-diagnosis)
NONSPESIFIC INVESTIGATION:
1. CBC- neutrophilia, eosinipenia, shift to the left, acceleration ESR
2. Urinalysis – signs of a set of symptoms “toxic kidney”
28.
TREATMENTSPESIFIC THERAPY
1. Not indicated for the localized forms
2. Antibiotics should be given the patient of risk-groups and at
generalized form :
- quinolones (ciprofloxacin 0,5g×2t/d; ofloxacin 0,4×2t/d)
- chloramphenicol 0,5×4t/d
- cephalosporins of 3-rd generation
- ampicillinum, amoxicillin,amikacinum
NONSPESIFIC THEAPY
1. Detoxication PO or IV (lavage stomach and intestine; enterosorbents,
plentiful drink
2. Rehydration PO or IV
3. Metabolites, angioprotectors
4. Ferment drugs
5. Biologic preparations
6. At TIS - glucocorticosteroids
29.
DISCHARGE FROM HOSPITAL ONLY ATCLINICAL CONVALESCENCE:
-1 negative bacteriological test of a feces in 2 days after ending
treatment
-Decree group 2 negative bacteriological testes with the
subsequent observation
3 month with monthly
bacteriological testing
30.
Cholera- Acute intestinal infectious disease with fecal-oral mechanism of
transmission, saproantroponosis, characterized by functional disorder
of enterocytes, development of dehydration and demineralization,
clinically manifested by severe diarrhea-syndrome.
It is the typical disease with a diarrhea of Type A.
Etiology
Vibrio cholerae is presented in 2 species:
- Vibrio cholerae biovar cholerae;
- Vibrio cholerae biovar El-Tor;
The new strain Bengal O139, causes diarrhea of people, but not
agglutinate with 01 group antiserum (it is resistant to streptomycin and
co-trimoxazole), now it belongs to the 3rd biotype.
31.
32.
Characteristics:-small Gram “—” comma-shaped rods (size 1.5 - 4 microns of length and
0.2 – 0.4 microns);
-mobile, have flagella (the most mobile between pathogenic infectious
agents);
-has no spores and capsules;
-facultative aerobes, gallophile;
-grows on the simple alkaline media with pH of 7.8-8.0;
Feature:
- thermostable endotoxin;
- thermolabile exotoxin – cholerogen – provides a development of
dehydration;
- factors of aggression:- neuraminidase, lipase, protease;
- H-antigen, O-antigen (serogroup O1 is divided into:
-Inaba, - Ogava,- Higoshima);
Resistance:
-high in water, humid environment (a few months), in food stuffs (2-5 days);
Sensitivity: - to the dryness, ultraviolet irradiation;
- disinfection, high temperature, boiling;
- antibiotics – tetracycline, ampicillin, chloramphenicol.
33.
Halofeels (optimal pH of nutrient medium from 7.8 to 8.0)- they are easily colouring by all aniline stains.
- well grow on the simple medium (1 % of peptonic water)
Stability in the external environment – survival rate:
- in sea water
- on subjects of use
- in fresh water
- in milk
- on vegetables
- in a fish and sea products
- in the freezer
-
- 10 - 60 days (Eltor)
- 3 - 7 days
- 7 - 18 days
- 7 - 14 days
- 1 - 10 days
- 2 - 14 days
21 days
34.
EpidemiologySource: - vibrio-carrier (more dangerous in epidemiological – chronic form);
- patients with clinically manifested form (especially in the first 4-5 d);
- patients with obliterated form,
- convalescents (within 2-4 weeks).
In the first days of the disease the patient discharges about more then 1 million
of vibrios.
Mechanism of transsmition:
fecal-oral realized by:- watery way – is leading (drinking, bathing),
- alimentary (milk, rice),
- contact
Susceptibility: general and high, depends on the:
- season (active drinking, bathing, flies),
- age (elderly and children),
- persons with GIT-pathology ( hypoacid gastritis, anemia and
helminthiasis),
Immunity: resistant, specific, antitoxic
Morbidity: high (due to fast distribution) - 1 - 3 %.
35.
Due to the wide application ofpathogenic treatment
(rehydration), the mortality from
cholera has decreased
significantly;
But prognosis is always serious
at the dehydration of III-IV
degree.
Recently, the mortality rate
decreased from 6% to 1%.
36.
37.
38.
The factors of vibrio pathogenicity facilitating the process colonisation- flaggella - adds mobility to vibrioes;
- the mucinase - dilutes slime on a surface of enterocytes, facilitating fixation of
exotoxin on receptors (Gm1-ganglioside);
-hyaluronidase and neuraminidase – facilitate infiltration of exotoxin in
enterocytes;
- other toxic components (hemolysins for eltor etc.)
39.
PathogenesisScheme of the pathogenesis of cholera has the following steps:
1.
2.
3.
4.
5.
6.
Ingestion of Vibrio cholerae in the intestine, reproduction in an alkaline
environment and destruction, the release and accumulation of toxins,
including cholerogen;
Increased secretion of isotonic fluid:
a) cholerogen activates the cAMF on membranes of enterocytes,
increases a permeability of enterocyte membranes for sodium and
water;
b) blocks the sodium pump and reduces of resorption of
isotonic fluid;
Dehydration (in a severe form);
Haemoconcentration, slowing blood flow,
hypoxemia, hypoxia;
Metabolic acidosis with the accumulation
of toxic products;
Extrarenal urinary disorders up to anuria
in severe cases or extrarenal coma.
40.
PathomorfologyBiopsy of the small intestine:
- swelling of the basal layer of the mucosa and the endothelium of blood
vessels,
- structure of enterocytes is not violated,
- signs of functional hyperactivity – (enteritis ) are not developed;
At the autopsy:
- severe dehydration of all tissues, ischemia of mucosa in stomach, small
intestine and colon, it is swollen, with small hemorrhages,
- in all parenchymatous organs expressed dystrophic changes
41.
Clinical classificationAtypical
Typical
Subclinical
erased
Mild
“Dry”
Complicated
Moderate
Hemorrhagic
Gastric
Severe
Uncomplicated
Mixed
42.
1. Incubation - 2 - 3 days (from some hours to 5 days)2. Prodrome is not typical, but sometimes may be:
- feeling of anxiety, weakness,
- rumbling in abdomen, pain in chewing and
calf muscles,
- sweating, dizziness, cold extremities.
3. Climex –
1) In typical cases disease begins suddenly, more often at the night or
before morning with acute diarrhea but without abdominal pain and
tenesmus.
2) Stool quickly becomes watery and then resembles a rice water, loses its
odor and becomes the smell of raw fish or grated potatoes.
3) The patient feels:
- discomfort in epigastric and paraumbilical area,
- rumbling around the navel, murmurs in abdomen, feeling of
bloating,
- insuperable desire on defecation;
- after a few hours, sometimes a day, diarrhea accompanied with
repeated vomiting, sometimes a fountain, without nausea.
Vomit quickly becomes watery and resembles rice water.
43.
Profuse diarrhea, repeated vomiting lead to dehydration4) Intoxication (have endogenous character), weakness, thirst,
dryness of the mouth;
5) The skin becomes bluish, cold and loses its elasticity, turgor;
6) Tongue is dry, abdomen is retracted, painless, possible meteorism
(hypokalemia);
7) Voice becomes hoarse, breathing quickens (tachypnea);
8) Tachycardia and decreased blood pressure;
9) Reduced diuresis, convulsions of some groups of muscles;
10) Consciousness is not changed, patient indifferent, feels fear;
11) Body temperature remains normal;
12) CBC without significant changes;
Severity of the disease is determined by the degree of dehydration,
hemodynamic and metabolic disorders.
44.
Atypical forms:- Fulminant cholera (due to reproduction and accumulation of Vibrio in
the biliary tract, small intestine and penetration of its toxins in the blood in
high concentrations):
- sudden onset and rapid development of dehydration,
- fast development of hypovolemic shock,
- convulsions of all muscle groups,
- symptoms of encephalitis and coma;
- Dry cholera (cholera sicca) is very severe (“tragic”) form of the disease
with a malignant course:
- severe weakness,
- rapid development of collapse,
- dyspnea, convulsions,
- cyanosis, coma.
This form of the disease is rare, usually in malnourished patients.
- Obliterated cholera is characterized by unclear symptoms and mild
severity (often observed in the case of cholera El-Top).
45.
The basic clinical diagnostic symptoms of cholera:1.
2.
3.
4.
5.
6.
Classic tetrad - diarrhea, vomiting, dehydration (isotonic dehydration),
seizures,
Acute onset of illness with diarrhea and following vomiting
(without nausea, abdominal pain, tenesmus), vomit and feces in the
form of rice-water,
Subnormal or normal body temperature,
Acrocyanosis (total cyanosis), the symptoms of “cholera face”, “hands
of washerwoman”, cholera folds, “cholera glasses”,
Hoarse voice (aphonia), tachypnea,
Tachycardia, decreased blood pressure (collapse), oligoanuria.
46.
Specific diagnosis of cholera1) Bacteriological method – classical, main in laboratory diagnosis of
cholera. For bacteriological study using feces and vomit (10-20 ml) and
1% peptone water;
2) Serologic method –
- immobilized reaction (RI),
- microagglutination of Vibrio cholera by O-serum
(contrast microscopy) (result in a few minutes),
- reaction of immunofluorescence (results in 2 - 4 hours),
- RIHA, RN, ELISA.
Nonspesific diagnostic
1) CBC+Ht – relative leukocytosis, shift of formula to the left, increased ESR
and Ht, hemoconcentration;
2) Urinalysis - leukocyturia, proteinuria, microhematuria, admixture
47.
48.
TreathmentNonspecific therapy:
1.
2.
3.
4.
Rehydration – oral and parenteral;
The use of cardiac glycosides is contraindicated, due to increased
disturbance of microcirculation, assisting in the development of kidney
failure;
Diet №4, and in 3-4 days - with a predominance of foods that contain a
lot of potassium (e.g. potatoes);
Pro – and eubiotics, sorbents;
Specific therapy:
The principles of antibiotic therapy of cholera:
a) Administration of antibiotic after obtaining material for bacteriological
examination,
b) Continuity of the drug (including night hours),
c) Parenteral using of a/b till disappearance of vomiting, after that – in
oral form,
d) Determine susceptibility to antibiotics,
e) Treatment with antibiotics regardless of the degree of dehydration
should be at least 5 days.
49.
Woman undergoing treatment at a cholera unitin Lima, Peru
50.
Antibacterial therapy:- doxycyclin
- tetracyclinum
- biseptolum
- furazolidonum
- ciprofloxacin
0.1g × 2t/d PO
0.5g × 3t/d PO
960 mg × 3-4 t/d PO
0.1 – 0.15g × 4t/d PO
0.5g -1.0g × 2-3t/d PO
-quinolones and cephalosporins of 3-rd generation
Rules of discharging from the hospital:
Patients discharged from hospital after receiving negative results of
bacteriological examination, which is taking before discharge, 24-36h
after the treatment with antibiotics.
- complete convalescence;
+ 3 negative tests of a feces;
+ 1 negative test of bile;
51.
Prophylaxis:- personal hygiene;
- improvement of sanitary conditions of the external environment;
- use only of high-quality WATER;
-vaccination forms antibacterial and antitoxic immunity
(does not influence onspreading of cholera and consequently in the
present the time widly does not be used!);
-Persons who were in close contact with cholera patients need in
emmediate prevention.
For this purpose, use tetracycline in dose - 0,3g × 3 t/day for 4 days.
The dose for children is reduced in accordance with age.
52.
Don’t worry!Be happy!













































 Медицина
Медицина








