Infestations. Manifestations of arthropods diseases
1.
InfestationsArthropods cause skin diseases in a variety of ways:
- infestation: arthropods lived on the skin
-irritation: by bites or body fluids
-hypersensitivity: to bite or presence of
arthropod
2.
Manifestations of arthropods diseasesInsects:
Bees, wasps, ants---- stings\ bites.
Mosquitoes---bites.
Flies—myiasis.
Fleas—bites.
Bed bugs---bites.
Lice–-- infestation.
Buterflies----caterpillar dermatitis.
Beetles---paederous dermatitis.
Mites:
o Demodex folliculorum----rosacea.
o Sarcoptes scabiei---scabies.
House dust mites—role in AD and eczema.
Ticks:
tick bites, vectors of rickettsial infections and erythema migrans.
3.
Scabies-Scabies is a world wide problem, common in
underdeveloped countries with overcrowding; 300
million cases/year world wide, affecting all ages, races.
-Scabies is caused by sarcoptes scabeii , an 8-legged
mite.
-IP is 14 days (2-6 ws),but only 24 -48 hrs in subsequent
infection.
-The entire life cycle is 30 days within the epidermis.
-Female mite invades the st corneum-burrow-total 60 to
90 eggs, after 3 days- larvae, after 7 days-adult mite
4.
Clinical picture• Mode of infection:
-close personal contact
-indirect by clothing or bedding
-sexual contact
• Clinical features:
-Severe itching mainly at night.
-Lesions consist of burrows (grey,curved or S-shaped ridges 0.5-1
cm), vesicle or papule at the end of burrow, urticarial papules,
nodules, scratch marks,pustules and eczematous changes.
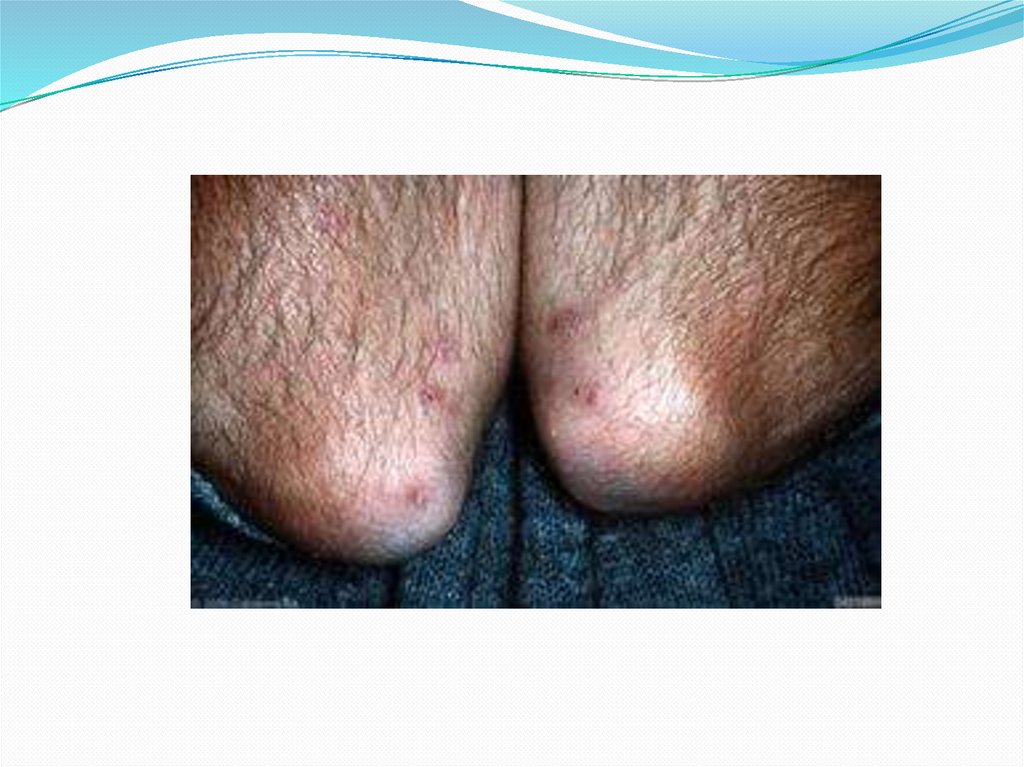
Sites:
-The mite prefers warm moist areas ( webs and sides of fingers,
wrists, forearms,cubital fossae,axillae, around nipples,buttocks,
periumbilicaly, genitalia and popliteal fossae.
5.
6.
7.
HP-The burrow containing the female mite is located
within the horny layer.
Diagnosis:
-burrows
-itching mainly at night
-more than one family member is affected
-demonstration of the mite, eggs and or feces
8.
Clinical varieties:1-Nodular scabies ( at genitalia).
2-Scabies in infants( atypical presentation and
distribution).
3-Norwegian scabies( crusted scabies): infestation with
large number of mites, up to million in mentals or
immunosuppresives.Characterises by subungual
hyperkeratosis,warty palms and soles, generalised
erythema and scaling, generalised LN and or
oesinophilia.
4-Scabies in clean people.
9.
Treatment:A) General treatment:
-early diagnosis, isolation & treatment.
-a hot bath with a hard brush precede scabicide app. Overnight to the whole body
except the head.
-ex and treatment of contacts.
-boiling of cloths, bed linens, towels,etc
-may give second tr after 1-2 weeks.
B) Topical treatment
-permethrin (synthetic pyrethroid) 5% for adult and 2.5% for children (in lotion-one day).
-sulphur ointment 5-10% for 3-4 successive nights.
-benzyl benzoate 25% lotion for 3-5 successive days.
-crotamiton 10% cream--- weak antiscabitic.
-gamma benzene hexachloride 1% lotion-----CNS toxic
-malathion 0.5% lotion-----highly toxic-----C) Systemic treatment
-antihistamines.
-antibiotics for secondary infection.
-ivermectin 200ug/kg/day once, repeate after 2 weeks.
10.
Pediculosis capitis• It is a scalp infestation caused by pediculosis humans
capitis, 3-4 mm in length.
• life span= 30 days– total 300 eggs – 7 days to hatch to
nymphs that require 8-14 days to mature.
• outside the body survive for 2-7 days.
• nits are ova within chitinous cases attached to hair.
11.
Epidemiology:• more common among school children esp. girls 3:1
• the density of head louse is highest in occipital and
postauricular regions.
• mode of transmission: shared caps, brushes and
combs.
• head lice infestation crosses all economic and social
boundaries whereas body lice preferentially affects
the homeless.
12.
CP• itching
• scratching----excoriations—sec. infection—
occipital lymphadenitis
• rarely hypersensitivity rash (pediculid)
Diagnosis:
adult lice-rare
oval egg capsules (nits)-common
occ. Lymphadenitis, sec infection
13.
14.
Pediculosis corporiso is infestation of the pediculosis humans corporis lice
in the cloths or bed linens close to the body.
o the average number of louse is 10.
o the bite of the louce leads to red macule and
haemorrhagic spots.
o scratching---sec infection and pigmentation.
o body lice are major vectors of typhus, trench fever and
relapsing fever.
15.
Pediculosis pubis(phthiriasis pubis)crab lice rather than pubic lice as infestation may
involve other hairy areas e.g beard, eyelashes, thighs,
and axillae.
caused by phthirus pubis.
transmitted by :
-sexual contact
-use of underwears
-lavatory seats
severe itching or presence of small dark spots in the
underwears (excreta) are the the usual presentation.
16.
17.
Treatment:synthetic pyrethroids: permethrin 1% rinse hrs to overnight
Benzyl benzoate 25% emulsion over night.
gamma benzene hexachloride 1% lotion in minutes.
malathion 0.5% lotion in hrs.
ivermectin 1% topically or orally 250 ug \kg.
General measures:
- better to repeate after one week to kill newly hatched
larvae
-reomval of the remainig eggs with fine toothed comb
-treatment of the secondary infection
-boiling and ironing of cloths in ped. Corp
18.
Cutaneous leishmaniasisIs a chronic disease caused by the protozoan parasite
of the genus leishmania, family trypanosomatidae,
its transmitted by female sandfly of genus
phlebotomus.
It has a worldwide distribution, but endemic to
Mediterranean countries, central Asia and north Africa
19.
Classification:1-Old world CL:
L.major, L. tropica, L. infantum, L. aethiopica
2-New world CL:
L. mexicana, L. brazilliensis
Pathogenesis:
Leishmania organisms exist in two forms:
a) promastigote stage; a spindle-shaped organism
with a fine flagellum in the midgut of the sandfly
b) amastigote stage( L-D bodies); an ovoid shape with retracted flagellum
intracellulaly of the reticuloendothelial system in the host.
Reproduction is by binary fission.
Factors play a role in the parasite-human interactions:
-exposure
-parasite virulence
-host immunity(Th-1 resp)
20.
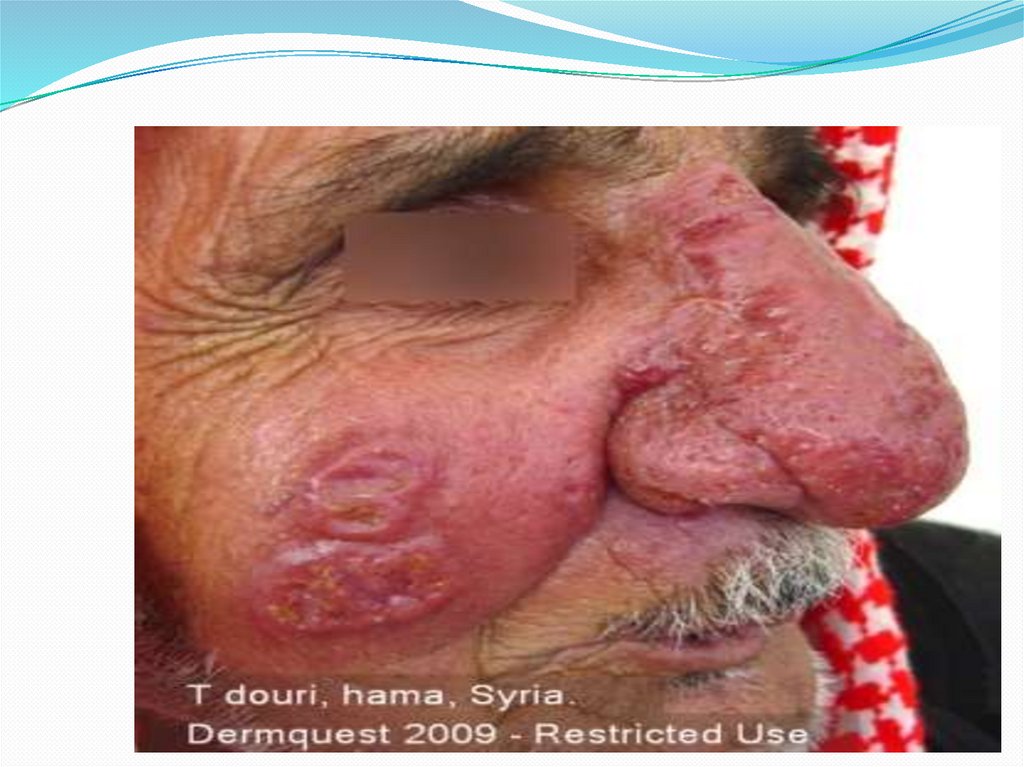
Clinical picture:There are many clinical features depending on the response of the host to
the parasite:
1) Acute cutaneous leishmaniasis (ACL):
-IP 2-8 w- starts as small painless edematous and erythematous
papule , usually solitary on exposed sites that may enlarge to nodule or
plaque or may ulcerate. The majority resolve spontaneously w scarring,
but may become chronic or disseminated. Two types are distinct:
a) the wet (rural form); L.major-rodents are reservoir-IP 1-4w-multiple
secondary nodules frequently seen around the lesion -healing in 2-6 m.
b) the dry (urban form); L.tropica-anthroponotic-IP more than 2 mlesions are more solitary, more inflammatory lasts longer 1-2 ys and
more difficult to treate.
21.
CP:2) Chronic leishmaniasis (chronic lupoid leishmaniasis):
The primary lesions last more than 2 ys. One or
several red non-ulcerated plaques are present
resembling lupus vulgaris.
3) Diffuse cutaneous leishmaniasis: is a chronic,
disseminated form most frequently associated with
L.aethiopica infection in the highlands of Ethiopia and
Kenya.
4)Post-kalazar dermal leishmaniasis. 1-5 ys postvisceral
leishmaniasis. Nodules centrofacially and/or
hypopigmented macules on the trunk.
22.
23.
24.
HP:Histopathology of ACL:
• Before ulceration; dermal infiltrate of macrophages filled
w leishmania-donovain bodies together w lymhoid and
plasma cells.
• With ulceration ; an influx of neutophils occurs.
• Later on reduction of organisms and macrophages, and a
granulomatous infiltrate contains epitheliod cells and giant
cells occur.
Histopathology of chronic leishmaniasis:
• Tuberculoid infiltrate as lupus vulgaris but devoid of
caseation necrosis. Few organisms may be seen.
25.
Diagnosis:History of exposure in endemic areas.
Chronic painless lesions.
Smear by Giemsa stain(50% +ve); macrophages w intracellular
amastigotes.
Biopsy---Hx & E, Giemsa (80% +ve).
Culture—demonstrates promastigotes.
Leishmanin (montnegro) test; 0.1 ml of promastigotes
suspension given intradermally, positive reaction appears 48-72
hrs as erythematous papule, used for persons not living in
endemic areas.
Serologic tests: indirect fluoresent antibody test and ELISA test
(lacks specificity).
PCR: to detect different species of leishmania.
26.
TreatmentWhy we treat leishmaniasis, considering 90% of the primary lesions of CL heal
spontaneously?
1)Medical treatment:
A) Parentral
a) Pentavalent antimonials:
-sodium stibogluconate ( pentostam); IV or IM ,20 mg\kg\day for 21 days for
multiple ressistant lesions. It inhibits phosphofructokinase of parasite.Side effects;
painful, anaphylactoid reaction, ECG changes, ,hemolytic anemia and hepatorenal
injury.
b) Amphotericin-B
c) Pentamidine
B) Oral
ketoconazol- itraconazol-rifampicin
C) Topical:
-treate secondary infection
-intralesional Sb injection; weekly
2)Non medical treatment;
-Cryotherapy; for early and localised few lesions
-Heat therapy; 50 C for 20 sec weekly
-Surgical excision
PREVENTION AND CONTROL:
Treat ps, DDT spraying, eradication of reservvoir animals, personal protective measures,
vaccination ..etc



 Литература
Литература