Похожие презентации:
dermatology ppt
1. KURSK STATE MEDICAL UNIVERSITY
Guidelines In Tropical DermatovenerologyFOR THE STUDENTS OF MEDICAL FACULTY
KURSK - 2024
2. CONTENTS:
1. Tropical diseases. Soft chancre.Venereallymphogranulomatosis. Donovanosis. Tropical
trepanematosis (pinta, bejel, yaws).
2. Aingum. African sleeping sickness (trypanosomiasis).
Dracunculiasis.
3. Tropical mycosis ( chromomycosis, blastomycosis,
sporotrichosis, actinomycosis, coccidioidomycosis ,
mycetoma).
4. Keloids. Disturbances of pigmentation ( vitiligo, melasma)
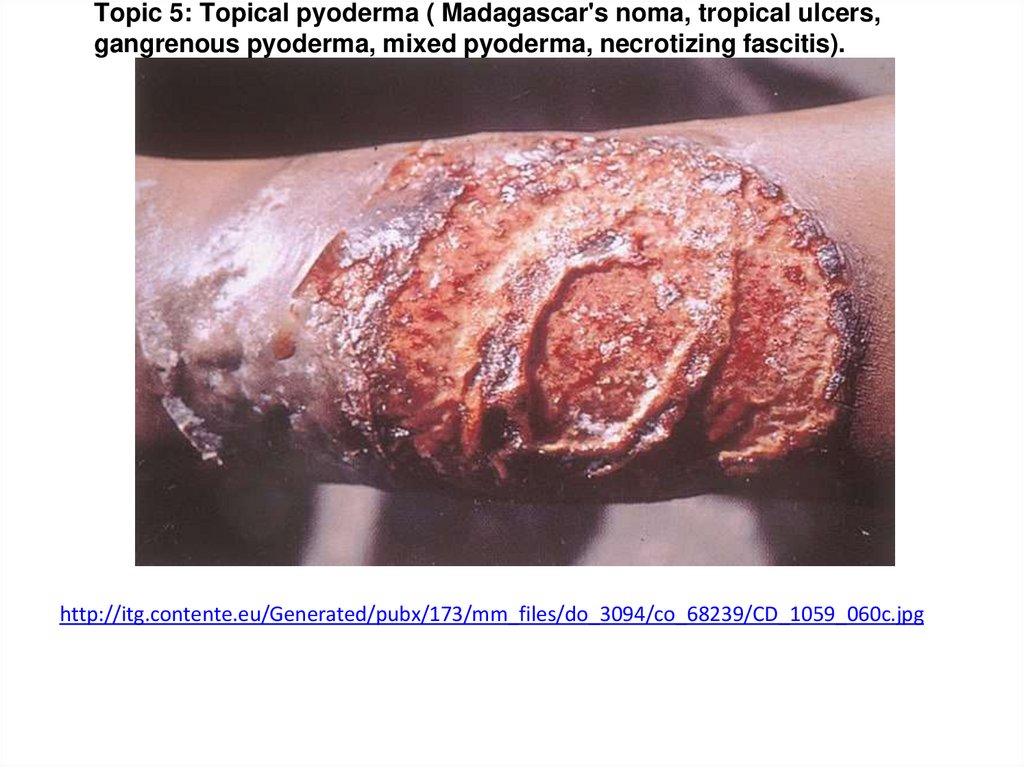
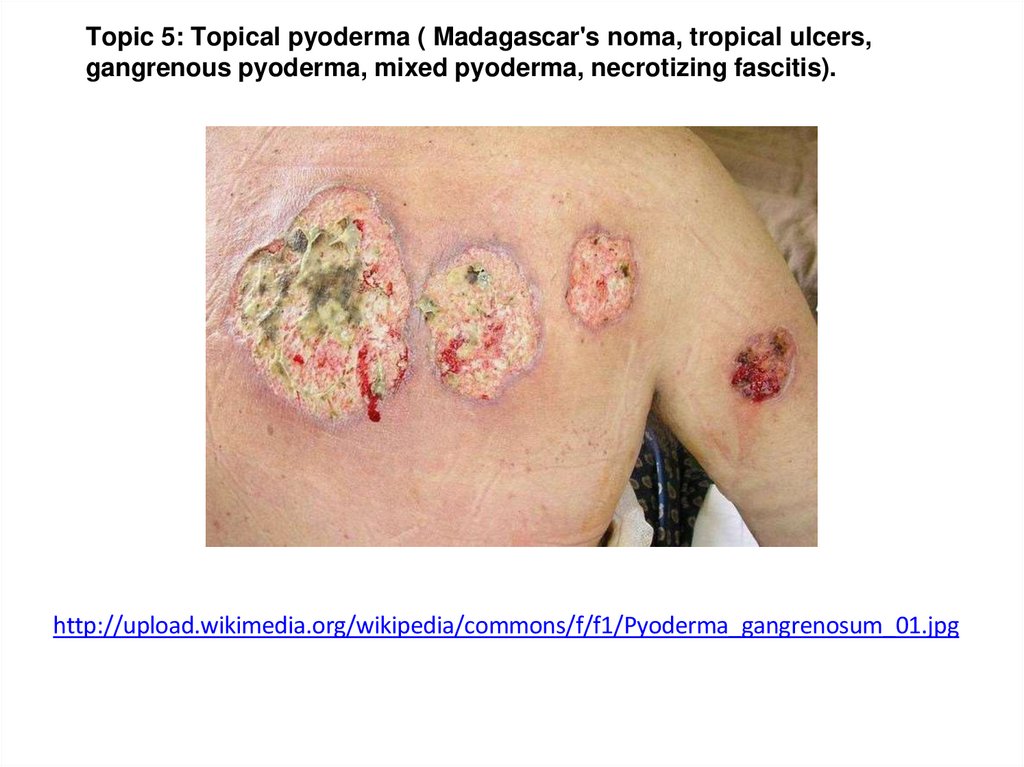
5. Topical pyoderma ( Madagascar's noma, tropical ulcers,
gangrenous pyoderma, mixed pyoderma, necrotizing
fasciitis).
3.
Topic 1: Tropical diseases. Soft chankre.Venereal lymphogranulomatosis.
Donovanosis. Tropical trepanematosis
(pinta, bejel, yaws).
4. Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis. Donovanosis. Tropical trepanematosis (pinta, bejel,
yaws).Aim for Self-Assessment
To classify different types of tropical diseases into group according to
geographical regions.
To identify the etiology and epidemiology of each tropical disease.
To identify and differentiate the pathogenesis(stage by stage) of each etiology
factor in the formation of corresponding tropical diseases in human body.
To determine associated factor such as physical factor, mechanical factor,
chemical factor, biological factor which can increase the risk of infected by
tropical disease.
To determine the primary diagnosis the tropical diseases based on their clinical
pictures.
To understand method of treatments and preventive measures of tropical
diseases.
Plan of study
Learn to classify various tropical diseases according geographical regions.
Learn etiology and way of transmission of each tropical disease.
Learn to differentiate tropical diseases according to clinical picture.
Learn to carry out the differential diagnosis for tropical diseases.
Learn on ways of transmission for risk of affection with these diseases.
Learn the way of prevention and treatment for each particular tropical disease.
5.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Summary
Tropical diseases are infections and conditions that either occur uniquely in
tropical and subtropical regions, widespread in the tropics and difficult to prevent or
control.
Donovanosis is caused by a bacterium called Klebsiella granulomatis. It can
be cured by antibiotics. It is usually found in people who have poor nutrition and live in
poor or underdeveloped communities. People with donovanosis usually notice one or
more fairly painless ulcers or nodules on the genitals, or around the anus or mouth.
Donovanosis is a sexually transmitted infection (STI). A very small proportion of people
may be infected through direct, nonsexual contact. There have been reports of the
infection being spread from mother to child during delivery, but this is very rare.
Donovanosis is contagious even when there are no noticeable symptoms.
Symptoms generally appear from 3 to 40 days after infection. Occasionally symptoms
may take as long as a year to develop. In Australia, the people who are most at risk of
catching donovanosis are : aboriginal people living in remote or marginalised
communities. People who have sex with someone from a country with high rates of
donovanosis.
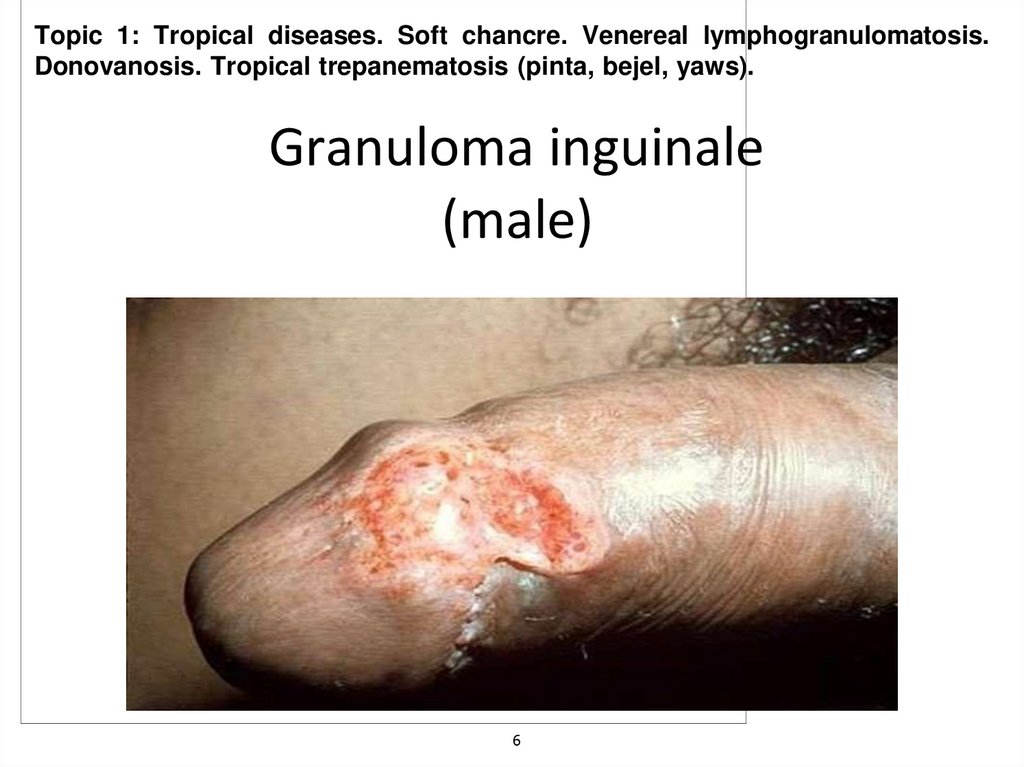
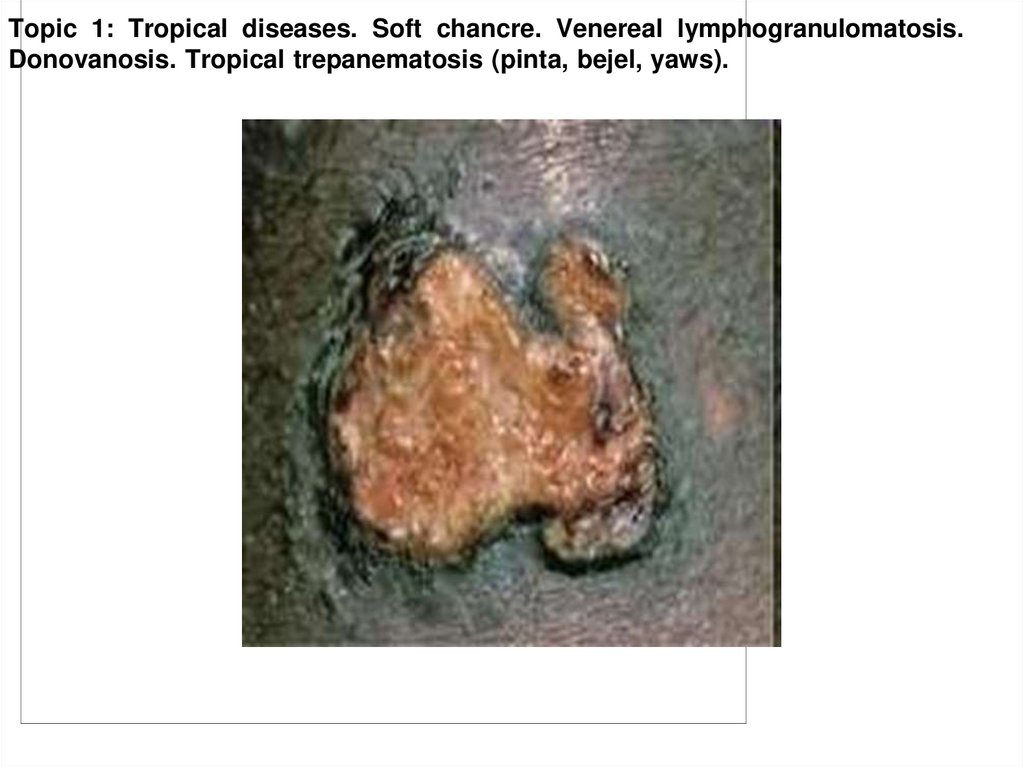
6. Granuloma inguinale (male)
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Granuloma inguinale
(male)
6
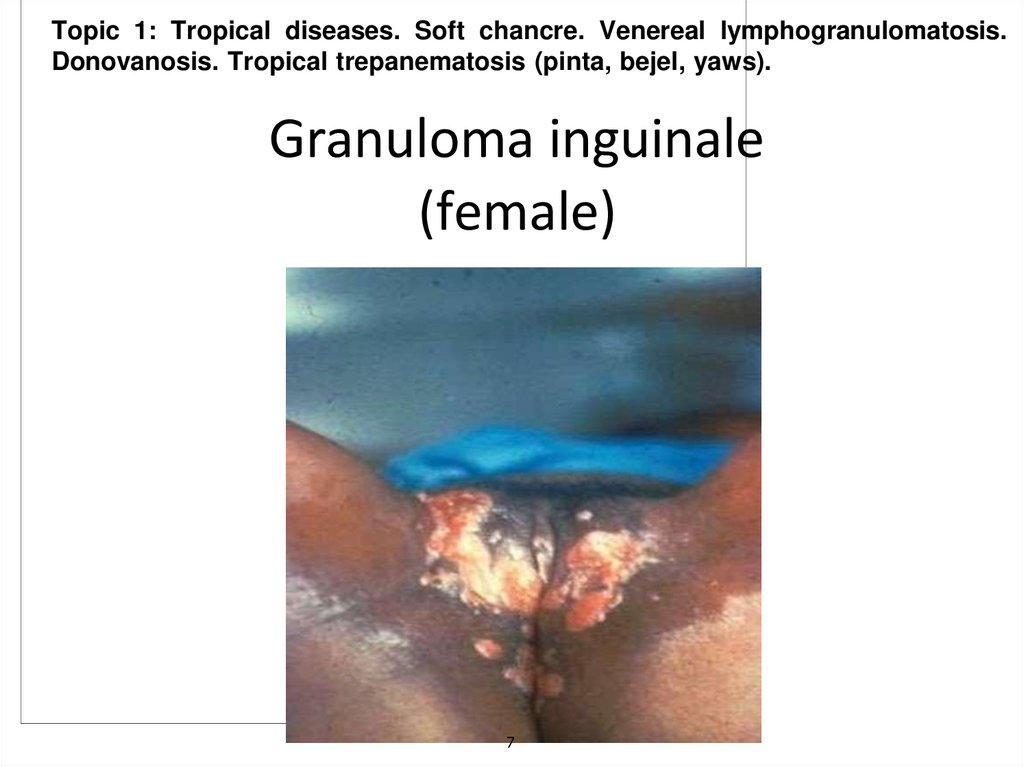
7. Granuloma inguinale (female)
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Granuloma inguinale
(female)
7
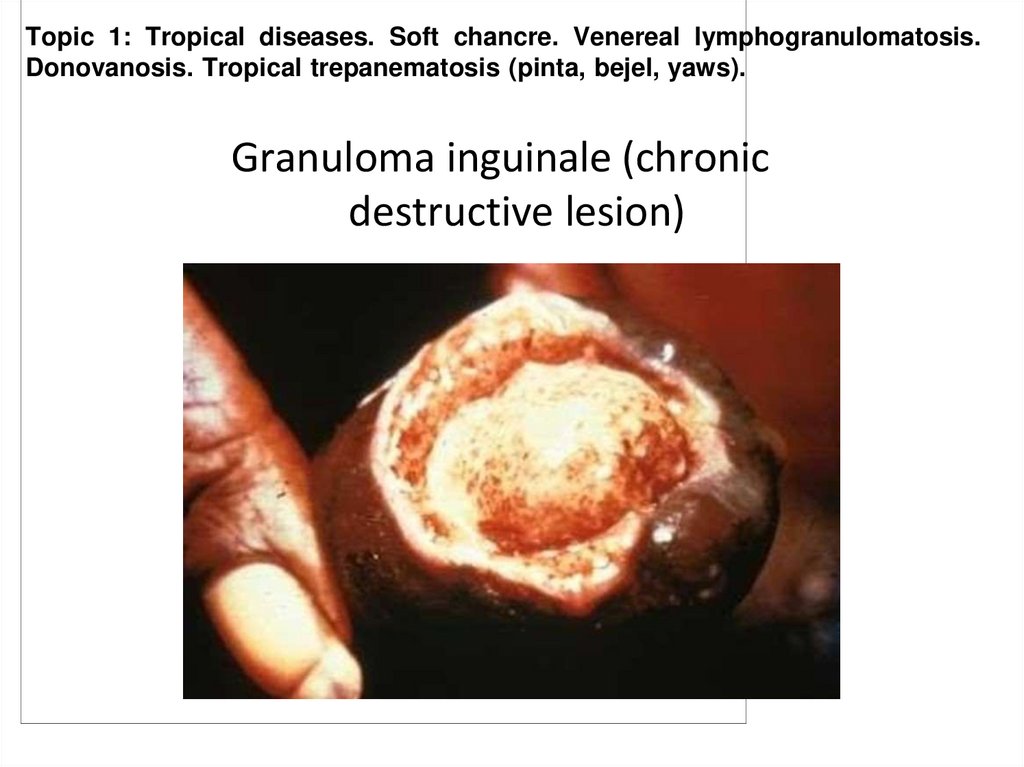
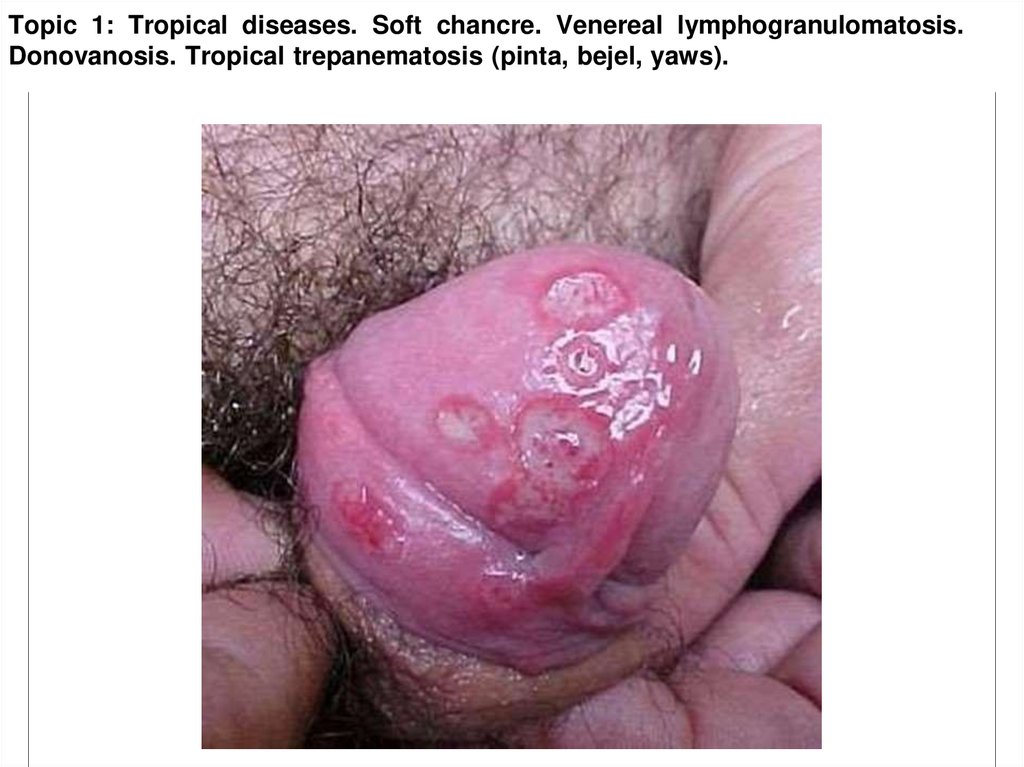
8. Granuloma inguinale (chronic destructive lesion)
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Granuloma inguinale (chronic
destructive lesion)
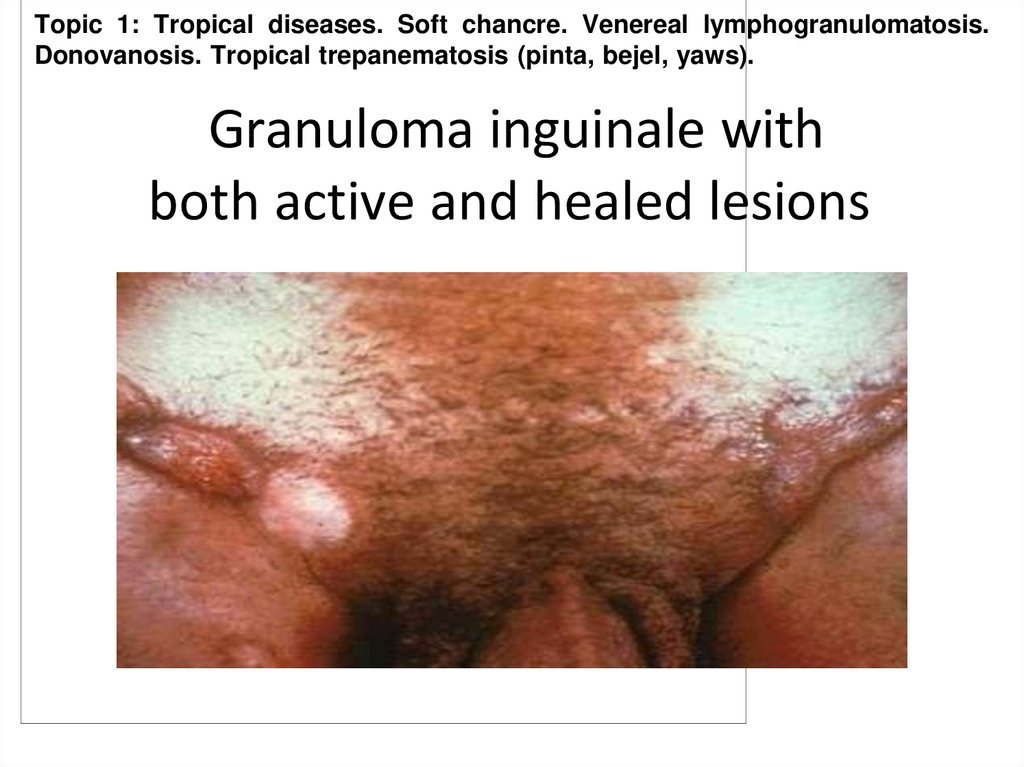
9. Granuloma inguinale with both active and healed lesions
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Granuloma inguinale with
both active and healed lesions
10. Venereal lymphogranulomatosis is a disease due to infection with Chlamydia trachomatis. It is also known as climatic bubo,
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Venereal lymphogranulomatosis is a disease due to infection
with Chlamydia trachomatis. It is also known as climatic bubo,
lymphopathia venereum, which is a chronic, sexually transmitted
infectious disease, most often found in hot climates.
Unlike genitourinary chlamydial infection which infects
squamo columnar epithelial cells, this disease is primarily an infection
of lymphatics and lymph nodes. Chlamydia trachomatis gains
entrance through breaks in the skin, or it can cross the epithelial cell
layer of mucous membranes. The organism travels from the site of
inoculation down the lymphatic channels to multiply within
mononuclear phagocytes of the lymph nodes it passes.
11.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Primary stage : the interval from the moment of infection
to the appearance of the first symptoms of the disease (the
incubation period) is ten to 25 days. Presence primary
lesion, in the form of a nodule, blister, or shallow skin
defect (erosion), arises at the site of penetration of the
virus. There are no subjective sensations. These
symptoms disappear spontaneously after a few days.
12.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Secondary stage : usually begins five to 30 days later and is
characterized by affection of the lymph nodes (mostoften,inguinal),
which enlarge, indurate, and fuse, forming painful tuberous tumors.
The skin over these turns a cyanotic red. Patients experience
elevated temperature, headaches, exhaustion, and pain in the joints.
Malacic foci develop and the skin over them becomes thin.Fistular
apertures appear, discharging a thick yellow-greenpus.The lymph
nodes gradually decrease in size and the fistular aperture scicatrize,
but neighboring lymph nodes become involved and new fistular
apertures form. The secondary stage of the disease lasts from two or
three months to several years. The scars formed sometimesleadto
considerable disturbances of lymph circulation andtothe development
of elephantiasis. When the inguinal lymph nodes are affected, lymph
circulation is disturbed in the gonads, perineum, and anal region.
13.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
14.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
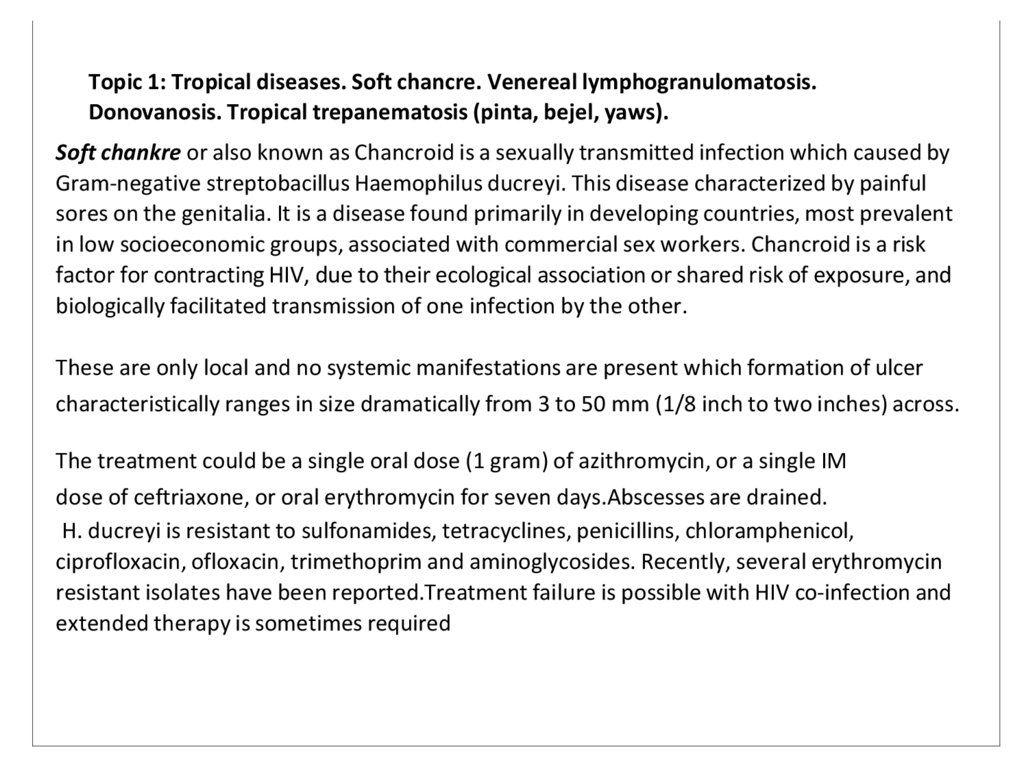
Soft chankre or also known as Chancroid is a sexually transmitted infection which caused by
Gram-negative streptobacillus Haemophilus ducreyi. This disease characterized by painful
sores on the genitalia. It is a disease found primarily in developing countries, most prevalent
in low socioeconomic groups, associated with commercial sex workers. Chancroid is a risk
factor for contracting HIV, due to their ecological association or shared risk of exposure, and
biologically facilitated transmission of one infection by the other.
These are only local and no systemic manifestations are present which formation of ulcer
characteristically ranges in size dramatically from 3 to 50 mm (1/8 inch to two inches) across.
The treatment could be a single oral dose (1 gram) of azithromycin, or a single IM
dose of ceftriaxone, or oral erythromycin for seven days.Abscesses are drained.
H. ducreyi is resistant to sulfonamides, tetracyclines, penicillins, chloramphenicol,
ciprofloxacin, ofloxacin, trimethoprim and aminoglycosides. Recently, several erythromycin
resistant isolates have been reported.Treatment failure is possible with HIV co-infection and
extended therapy is sometimes required
15.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
16.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
17.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
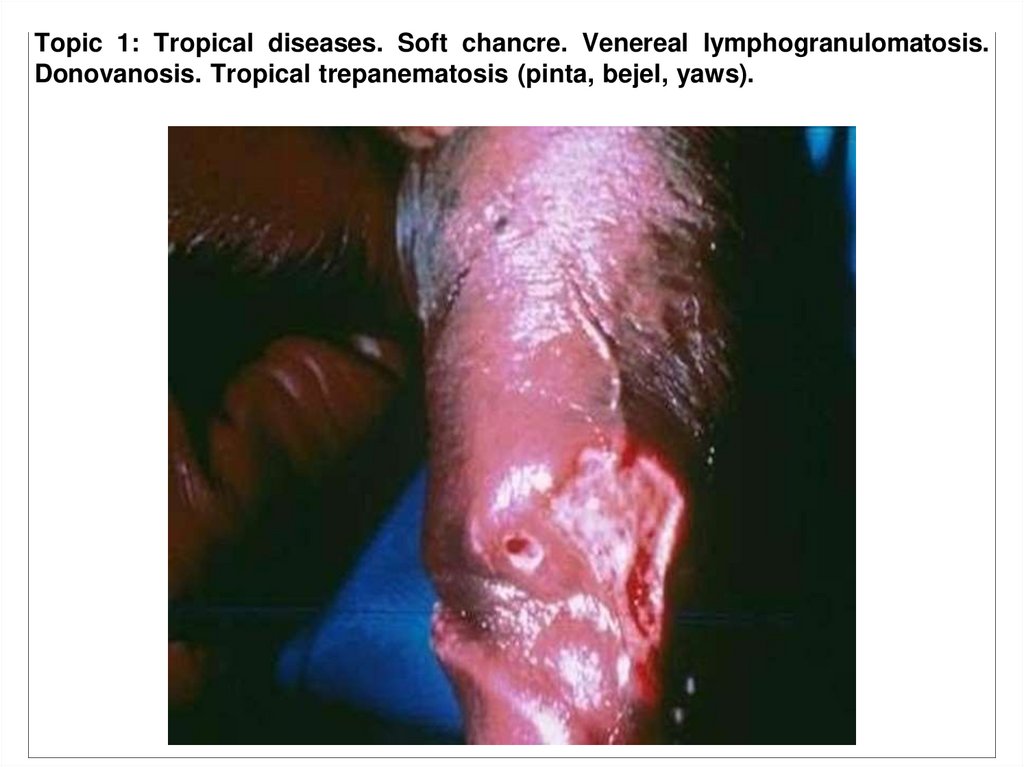
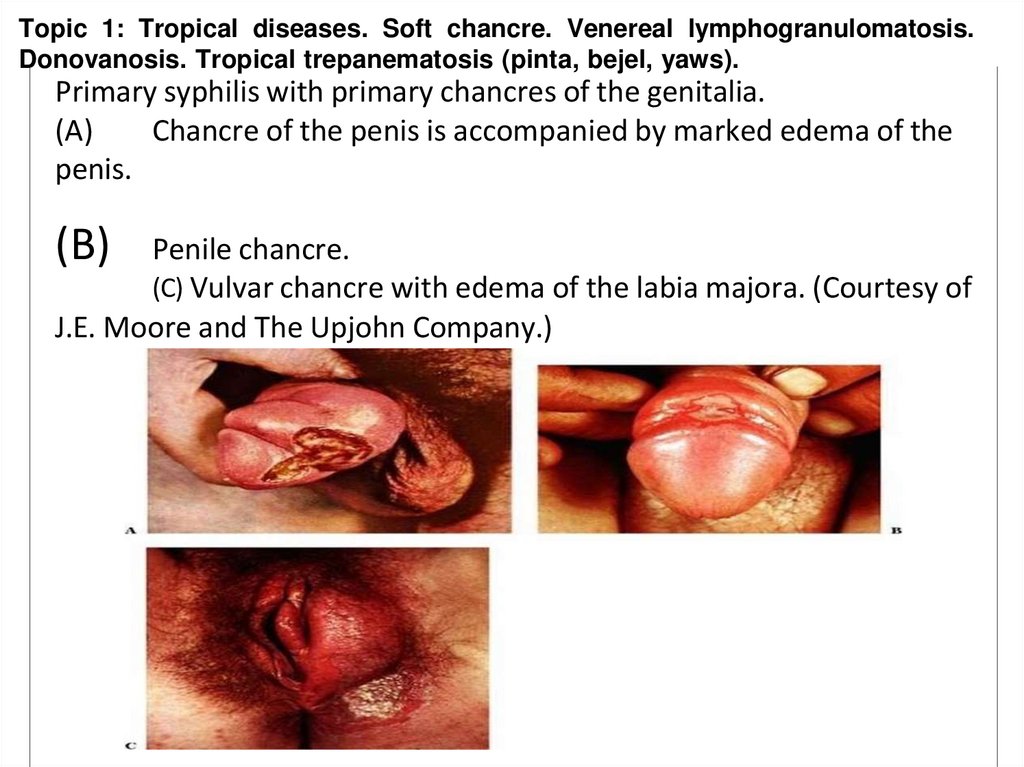
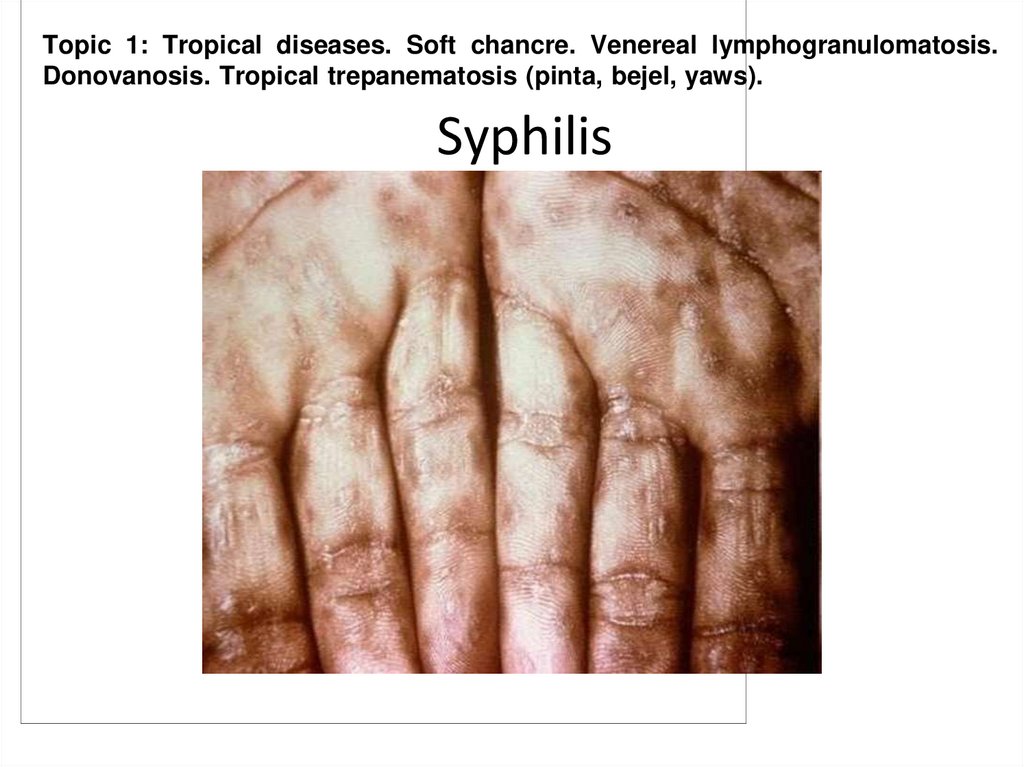
Primary syphilis with primary chancres of the genitalia.
(A)
Chancre of the penis is accompanied by marked edema of the
penis.
(B)
Penile chancre.
(C) Vulvar chancre with edema of the labia majora. (Courtesy of
J.E. Moore and The Upjohn Company.)
18.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Treponematosis is a term used to collectively describe any of the diseases caused by the
bacterial species Treponema. There are three subspecies that would be discussed in this
lesson which cause the following diseases: Yaws (Treponema pallidum pertenue), Bejel
(Treponema pallidum endemicum), Pinta (Treponema carateum). Treponemal diseases are
distinguished on the basis of epidemiological characteristics and clinical manifestations.
They are at present indistinguishable by morphological, immunological or serological
methods.
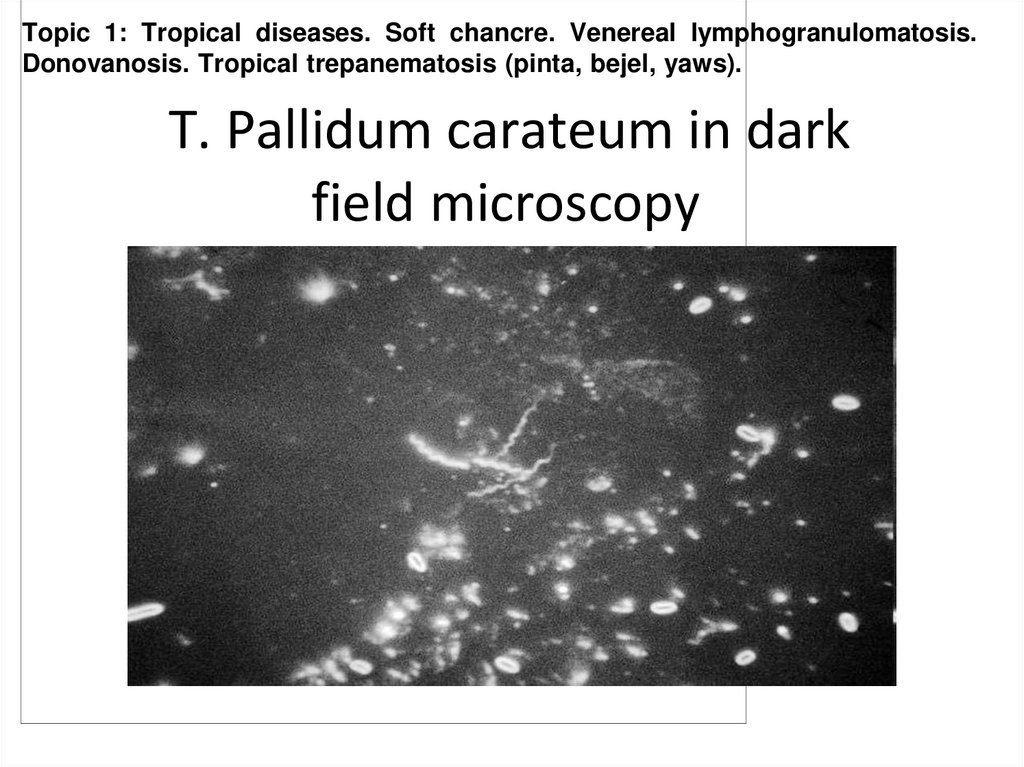
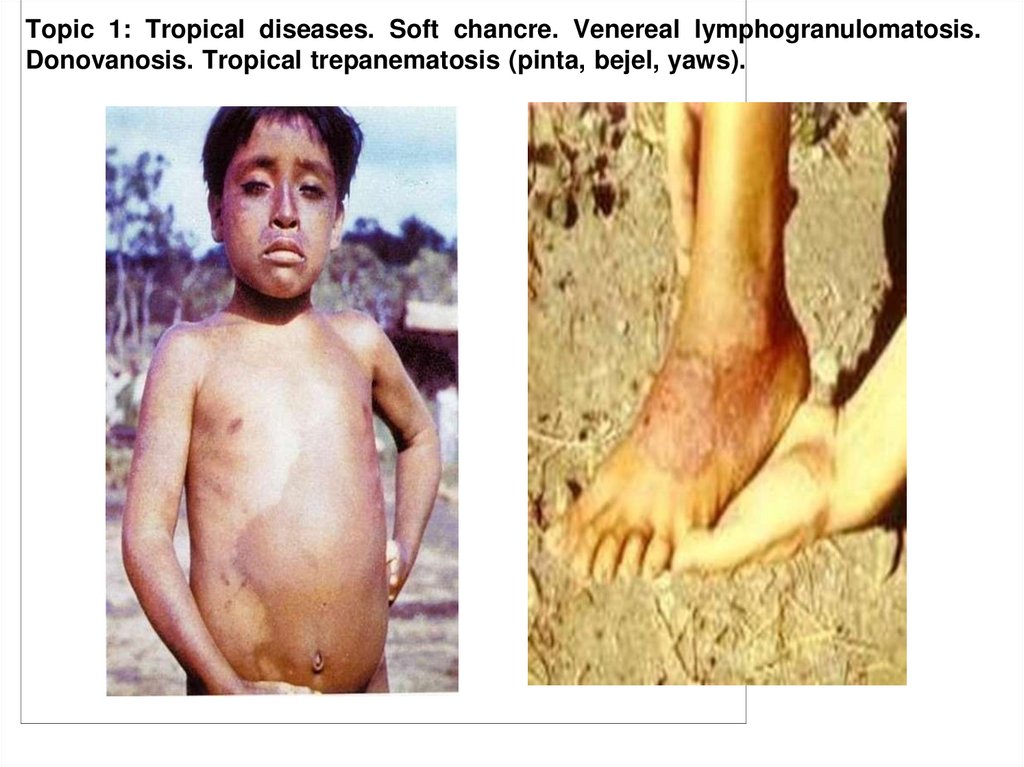
Yaws is a long-term (chronic) infection that mainly affects the skin, bones, and joints. This
disease is not sexually transmitted. Yaws mainly affects children in rural, warm, tropical areas,
such as the Caribbean Islands, Latin America, West Africa, India, and Southeast Asia.Yaws is
transmitted by direct contact with the skin sores of infected people.
About 2 - 4 weeks after infection, the person develops a sore called a "mother yaw" where
bacteria entered the skin. The sore is a growth that may be tan or reddish and looks like a
raspberry. It is usually painless but does cause itching.These sores may last for months. More
sores may appear shortly before or after the mother yaw heals as the person scratches or
spreads the bacteria from the mother yaw to uninfected skin. Eventually the skin sores heal.
19. T. Pallidum carateum in dark field microscopy
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
T. Pallidum carateum in dark
field microscopy
20. Primary lesions of Yaws
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
2
21. Syphilis
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
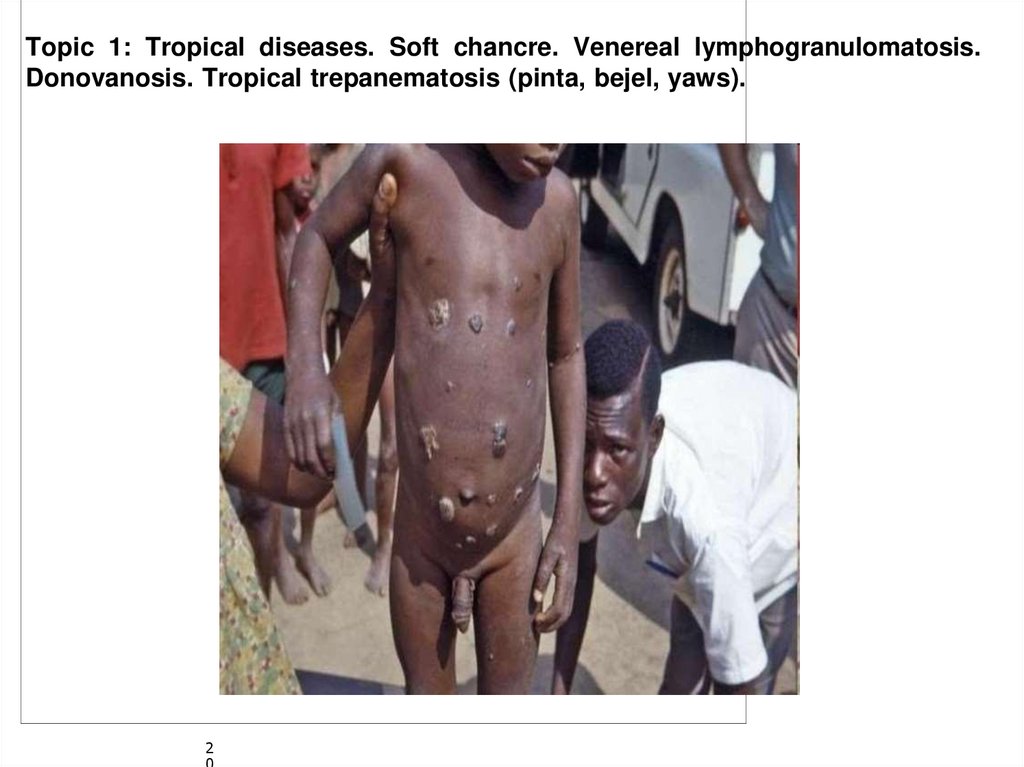
Syphilis
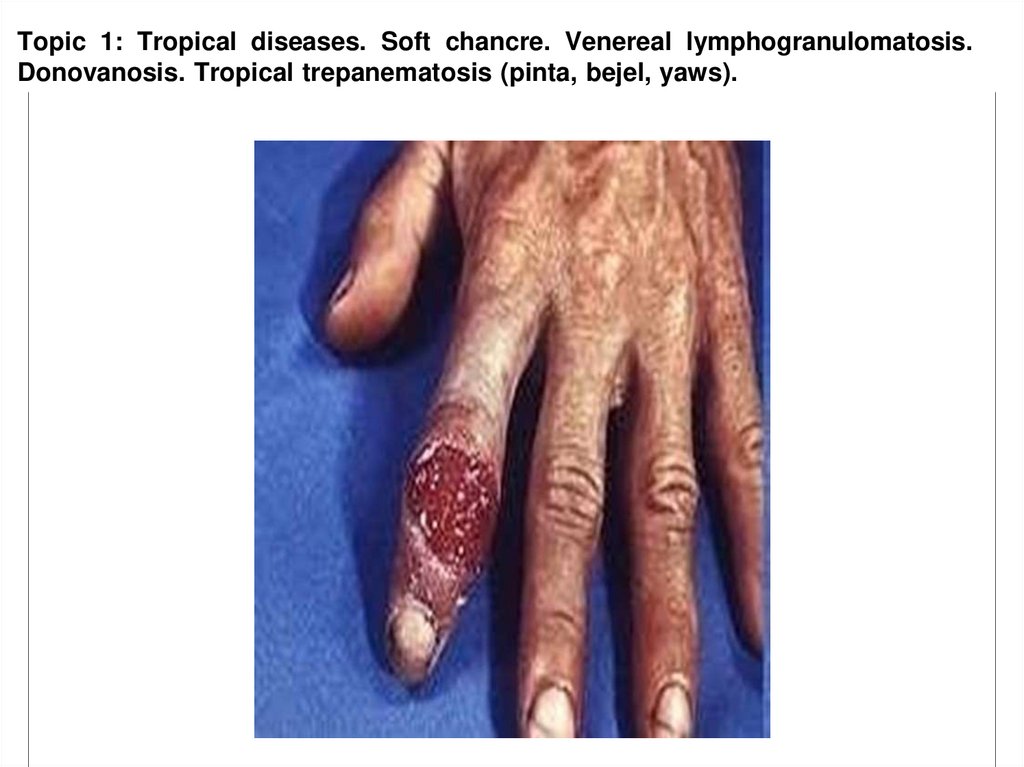
• Syphilis is a STI caused by the spirochete bacterium Treponema pallidum subspecies
pallidum.
• The primary route of transmission is through sexual contact; however, it may also be
transmitted from mother to fetus during pregnancy or at birth, resulting in congenital
syphilis.
• The signs and symptoms of syphilis vary depending in which of the four stages it
presents (primary, secondary, latent, and tertiary).
• The primary stage classically presents with a single chancre (a firm, painless, non-itchy
skin ulceration).
• Secondary syphilis with a diffuse rash which frequently involves the palms of the
hands and soles of the feet.
22.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
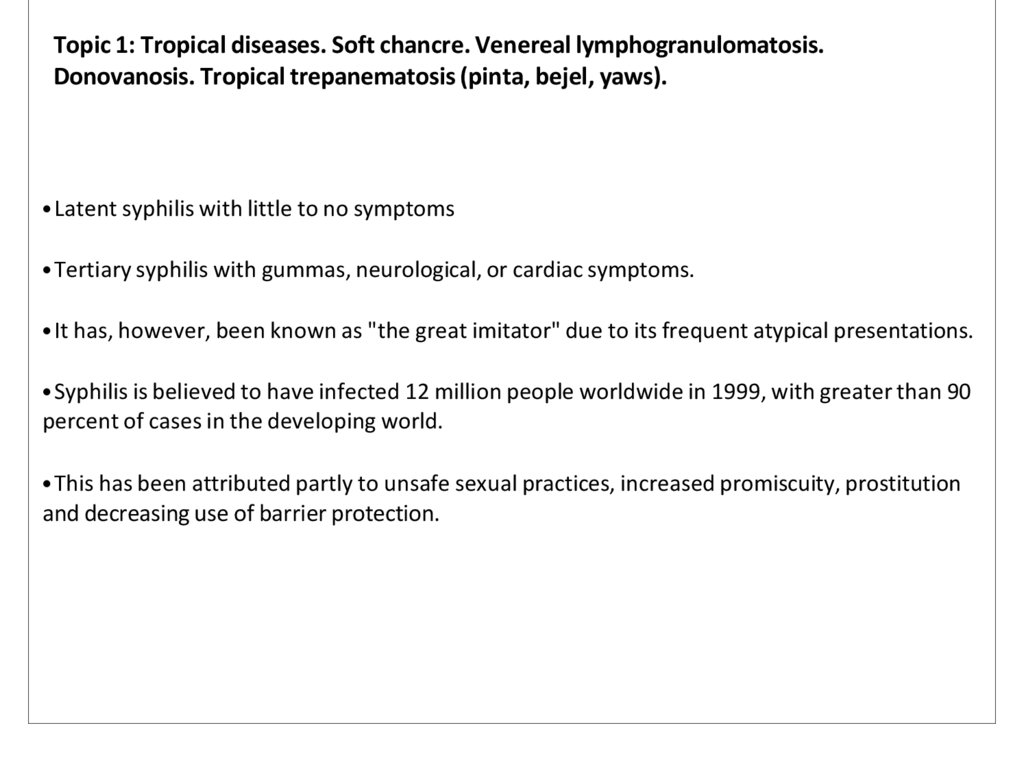
• Latent syphilis with little to no symptoms
• Tertiary syphilis with gummas, neurological, or cardiac symptoms.
• It has, however, been known as "the great imitator" due to its frequent atypical presentations.
• Syphilis is believed to have infected 12 million people worldwide in 1999, with greater than 90
percent of cases in the developing world.
• This has been attributed partly to unsafe sexual practices, increased promiscuity, prostitution
and decreasing use of barrier protection.
23. Syphilis
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Syphilis
24.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
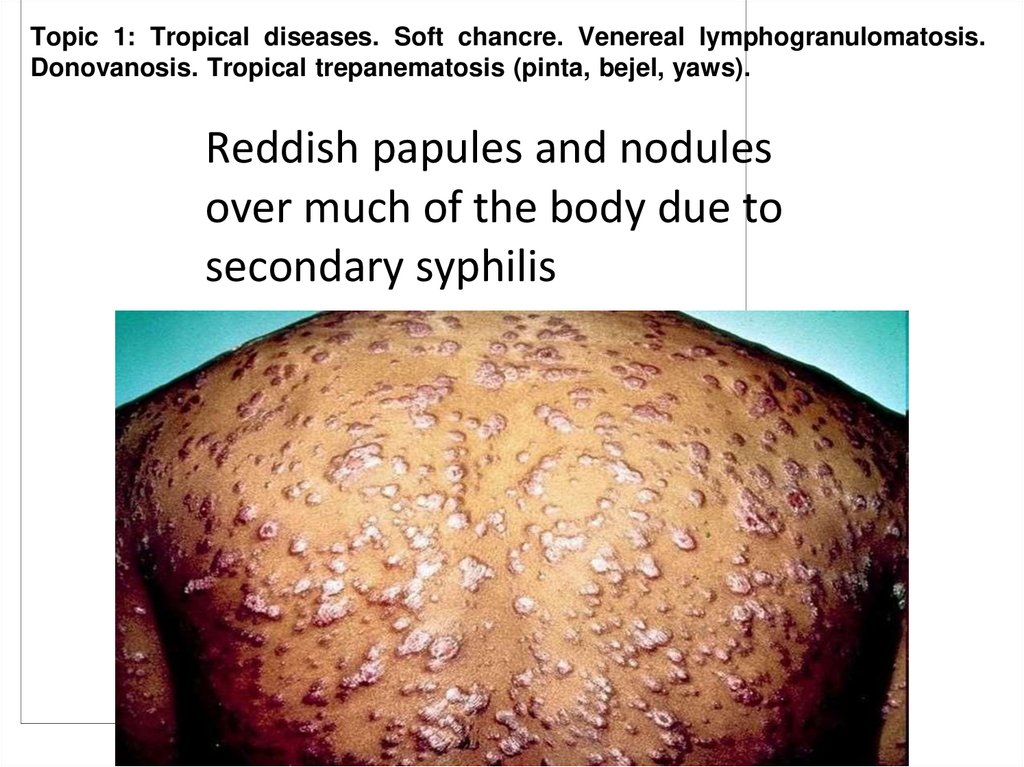
25. Reddish papules and nodules over much of the body due to secondary syphilis
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Reddish papules and nodules
over much of the body due to
secondary syphilis
26.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
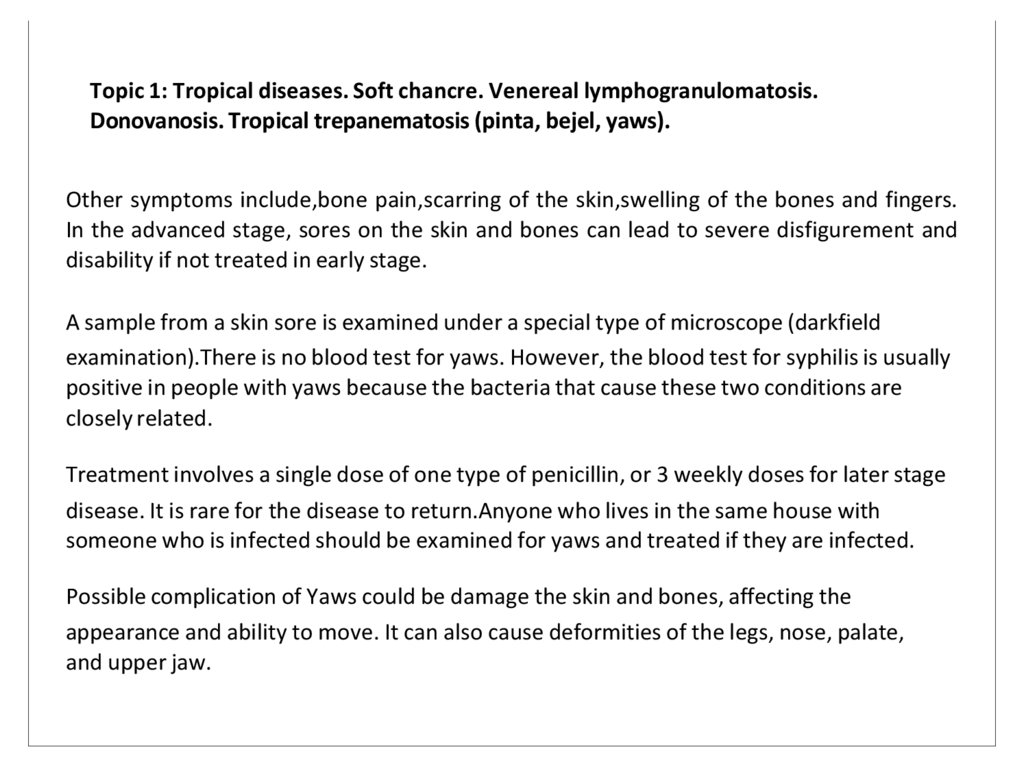
Other symptoms include,bone pain,scarring of the skin,swelling of the bones and fingers.
In the advanced stage, sores on the skin and bones can lead to severe disfigurement and
disability if not treated in early stage.
A sample from a skin sore is examined under a special type of microscope (darkfield
examination).There is no blood test for yaws. However, the blood test for syphilis is usually
positive in people with yaws because the bacteria that cause these two conditions are
closely related.
Treatment involves a single dose of one type of penicillin, or 3 weekly doses for later stage
disease. It is rare for the disease to return.Anyone who lives in the same house with
someone who is infected should be examined for yaws and treated if they are infected.
Possible complication of Yaws could be damage the skin and bones, affecting the
appearance and ability to move. It can also cause deformities of the legs, nose, palate,
and upper jaw.
27.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
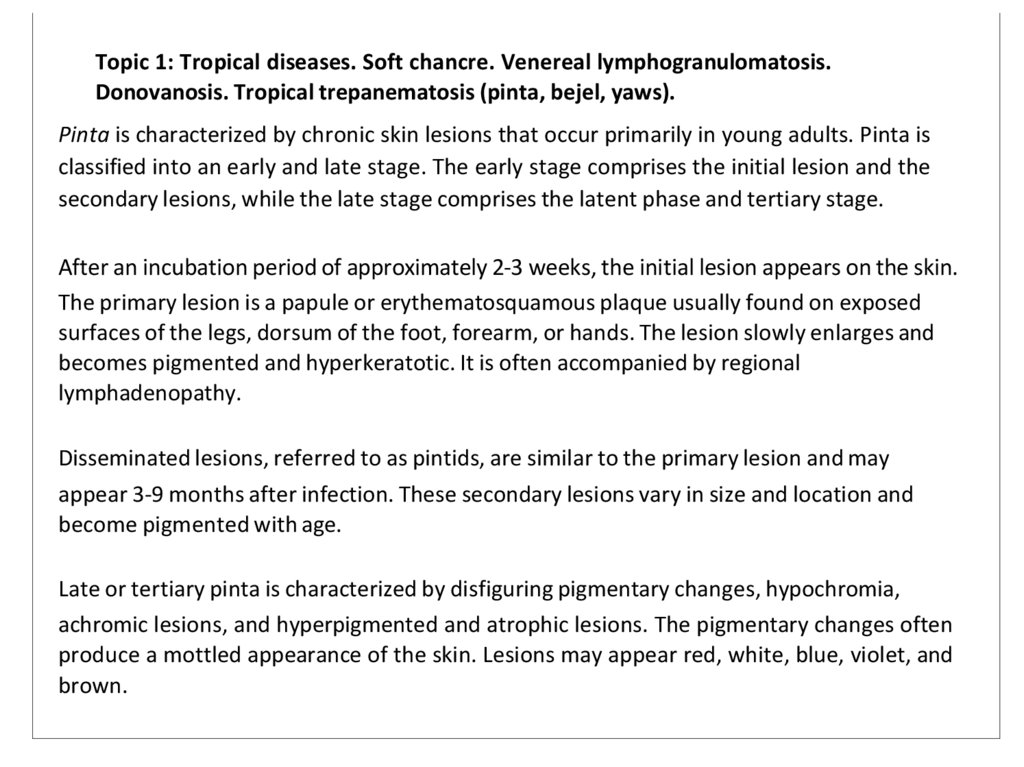
Pinta is characterized by chronic skin lesions that occur primarily in young adults. Pinta is
classified into an early and late stage. The early stage comprises the initial lesion and the
secondary lesions, while the late stage comprises the latent phase and tertiary stage.
After an incubation period of approximately 2-3 weeks, the initial lesion appears on the skin.
The primary lesion is a papule or erythematosquamous plaque usually found on exposed
surfaces of the legs, dorsum of the foot, forearm, or hands. The lesion slowly enlarges and
becomes pigmented and hyperkeratotic. It is often accompanied by regional
lymphadenopathy.
Disseminated lesions, referred to as pintids, are similar to the primary lesion and may
appear 3-9 months after infection. These secondary lesions vary in size and location and
become pigmented with age.
Late or tertiary pinta is characterized by disfiguring pigmentary changes, hypochromia,
achromic lesions, and hyperpigmented and atrophic lesions. The pigmentary changes often
produce a mottled appearance of the skin. Lesions may appear red, white, blue, violet, and
brown.
28. Pinta in different stages
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
29.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
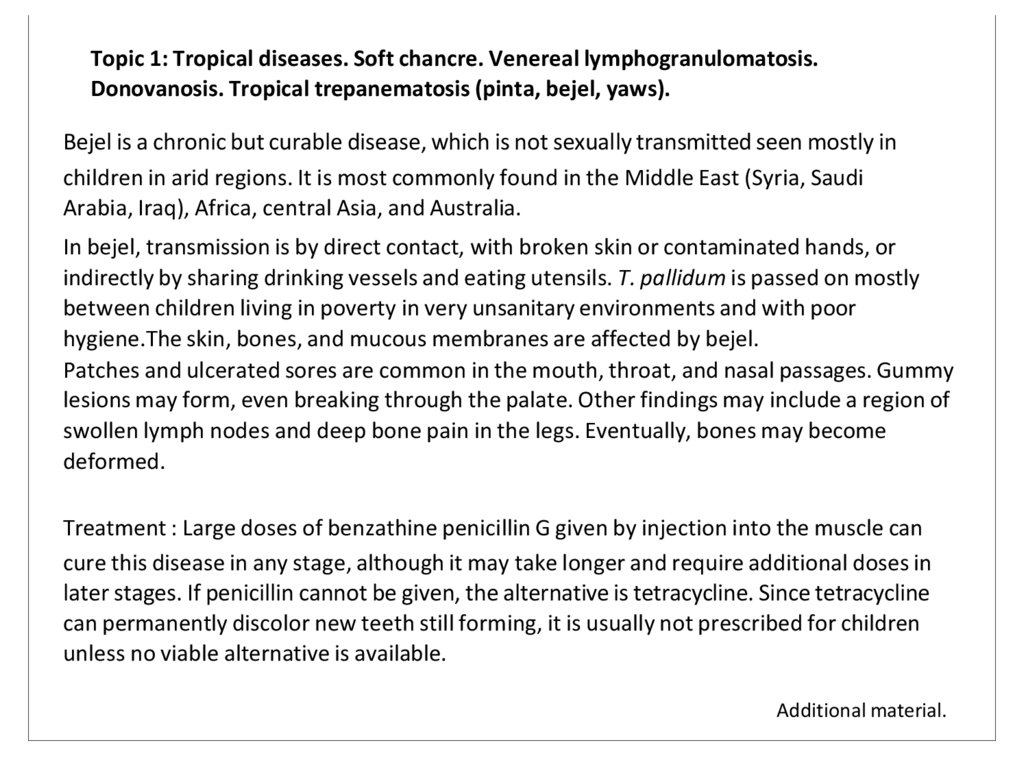
Bejel is a chronic but curable disease, which is not sexually transmitted seen mostly in
children in arid regions. It is most commonly found in the Middle East (Syria, Saudi
Arabia, Iraq), Africa, central Asia, and Australia.
In bejel, transmission is by direct contact, with broken skin or contaminated hands, or
indirectly by sharing drinking vessels and eating utensils. T. pallidum is passed on mostly
between children living in poverty in very unsanitary environments and with poor
hygiene.The skin, bones, and mucous membranes are affected by bejel.
Patches and ulcerated sores are common in the mouth, throat, and nasal passages. Gummy
lesions may form, even breaking through the palate. Other findings may include a region of
swollen lymph nodes and deep bone pain in the legs. Eventually, bones may become
deformed.
Treatment : Large doses of benzathine penicillin G given by injection into the muscle can
cure this disease in any stage, although it may take longer and require additional doses in
later stages. If penicillin cannot be given, the alternative is tetracycline. Since tetracycline
can permanently discolor new teeth still forming, it is usually not prescribed for children
unless no viable alternative is available.
Additional material.
30. Skin lesion in Bejel
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
31.
Question for Self Assessment.1.
Name different types of tropical diseases.
2.
Classify different types of tropical diseases in accordance to geographical regions.
3.
Define Donovanosis.
4.
Give classification of Donovanosis.
5.
What is the causative agent of Donovanosis ?
6.
What are the symptoms of Donovanosis ?
7.
What is the diagnosis of Donovanosis?
8.
What method of treatment that you know for Donovanosis ?
9.
What are the possible complications of Donovanosis?
10.
Name the preventive measures for Donovanosis?
11.
What is Lymphogranuloma venereum?
12.
Explain the pathophysiology of Lymphogranuloma venereum?
13.
Name three stages of Lymphogranuloma venereum.
14.
What is the causative agent of Lymphogranuloma venereum?
15.
What are the differential diagnosis for Lymphogranuloma venereum?
16.
What are the laboratory investigations that should be carry out for
Lymphogranuloma venereum?
32.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
17. What is Soft chankre ?
18. What method of treatment that you know for Lymphogranuloma venereum?
19. What is the characteristic of Soft chankre ?
20. Which group of people are more fond to be infected by Soft chankre ?
21. Which disease can be provoked by Soft chankre ?
22. What is the clinical manifestation for Soft chankre ?
23. What method of treatment that you know for Soft chankre ?
24. Define Trepanomatosis.
25. Give the clasification of Trepanomatosis in accordance of causative agent.
26. What is Yaws ?
27. Name method of transmission of Yaws.
28. What are the symptoms of Yaws ?
29. What are the methods of diagnosis that you know for Yaws ?
30. What are the method of treatment that you know for Yaws ?
31. What are the possible complications of Yaws ?
32. What is Pinta ?
33.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
34. Classify Pinta into stages of development of the disease.
35. Describe each stage of the disease.
36. What is Bejel ?
37. Name the methods of transmission of Bejel.
38. What are the clinical manifestations of Bejel ?
39. What are methods of treatment that you know for Bejel ?
34.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Test Question:
1.What is the cause of Donovanosis?
A)Caused by bacterium
C) Result of a genetic disorder
B) Caused by fungal infection
D) Triggered by poor nutrion
Answer:A
2.How many days symptoms of Donovanosis usually appear?
A)10-40 days
B) 25 days
C) 3-40 days
D) 15-20 days
Answer:C
3.How can Donovanosis transmitted?
Direct,nonsexual contact
B) Indirect,sexual contact
C) By contaminated water
Answer:A
35.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
4.What method of treatment for Donovanosis?
A)Amoxicillin
C) Metronidazole
B) Ciprofloxacin
D) Doxycycline
Answer:D
5.What is the causative organism of venereal lymphogranulomatosis?
A)Treponema pallidum
B) Neiserria gonorrheae
C) Chlamydia trachomatis
D) Haemophilus ducreyi
Answer:C
6.How many stages venereal lymphogranulomatosis have?
A)Two
C)Four
Answer:B
B)Three
D)One
36.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
7.What is the preferred antibiotic treatment for venereal lymphogranulomatosis?
A)Ciprofloxacin
B) Doxycycline
C) Amoxicillin
D) Metronidazole
Answer:B
8.Is it Yaws is a sexually transmitted?
A)Yes
Answer:B
9.How long incubation period for Pinta?
A)2-4 weeks
C) 2-3 weeks
B) No
B) A month
D) 7 days
Answer:C
10.What is the alternative treatment if penicillin cannot be given?
A)Chloramphenicol
B) Amoxicillin
C) Bisoprolol
D) Tetracycline
Answer:D
37.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Task 1: Soft Chancre (Chancroid)SituationA 28-year-old male presents with multiple
painful ulcers on the penis. The lesions have ragged edges, are covered with purulent
exudate, and are accompanied by tender inguinal lymphadenopathy.
Questions
1. What is the most likely diagnosis?
Soft Chancre (Chancroid).
2. What is the causative agent of this disease?
Haemophilus ducreyi
3. How is the disease transmitted?
Throughsexualcontact
4. What is the primary diagnostic test for this condition?
Gramstain of theulcer exudateshows “schooloffish”pattern(gram-negative
coccobacilli). Cultureon enrichedmedia isconfirmatory.
5. What is the recommended treatment?
Single-dose azithromycin (1gorally)or ceftriaxone(250 mgintramuscularly).
38.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Task 2: Venereal Lymphogranulomatosis (Lymphogranuloma Venereum)SituationA 30year-old man presents with a small, painless genital ulcer that healed spontaneously two
weeks ago. He now has painful inguinal swelling with “groove sign” (enlarged lymph
nodes above and below the inguinal ligament).
Questions
1. What is the most likely diagnosis?
Lymphogranuloma Venereum (LGV).
2. What is the causative organism?
Chlamydiatrachomatis (serovars L1, L2, L3).
3. What is the pathognomonic sign of this condition?
Groovesign (inguinal nodes divided by the inguinal ligament).
4. Which populations are most at risk?
Men who have sex with men (MSM), especially those with multiple sexual partners.
5. What is the treatment?
Doxycycline100mg orally twice daily for 21 days.
39.
Topic 1: Tropical diseases. Soft chancre. VenerealDonovanosis. Tropical trepanematosis (pinta, bejel, yaws).
lymphogranulomatosis.
Task 3: Donovanosis (Granuloma Inguinale)SituationA 35-year-old woman presents with
slowly progressing, painless genital ulcers that are beefy red in appearance, bleed easily
on touch, and have a rolled edge. There is no regional lymphadenopathy.
Questions
1. What is the likely diagnosis?
(Granuloma Inguinale).
2. What is the causative organism?
Klebsiellagranulomatis .
3. How is this disease diagnosed?
Visualization of Donovan bodies (intracellular safety pin-shaped organisms) on Wrightor
Giemsa-staineds mears from the lesion.
4. What are the complications of untreated Donovanosis?
Genital disfigurement, secondary bacterial infections, and strictures.
5. What is the treatment?
Azithromycin 1g orally weekly or 500mg daily for at least 3 weeks, until lesions heal.
40.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Task 4: Tropical Treponematosis (Pinta, Bejel, Yaws)SituationA 10-year-old child from a
rural tropical region presents with hypopigmented patches on the skin (involving the face
and arms) and hyperkeratotic nodules on the soles of the feet.
Questions
1. What are the three main forms of tropical treponematoses?
Pinta, Bejel, and Yaws.
2. What is the causative agent for Yaws?
Treponema pallidum subspecies pertenue.
3. How does Pinta differ from Yaws?
Pinta primarily causes skin discoloration and depigmented lesions, while Yaws begins with
papillomatous lesions and progresses to destructive bone and soft tissue damage.
4. What is the mode of transmission?
Non-sexual transmission via direct contact with infectious lesions.
5. What is the treatment for these conditions?
Single-dose benzathine penicillin G (1.2 million units intramuscularly for adults; 600,000
units for children).
41.
Topic 1: Tropical diseases. Soft chancre. Venereal lymphogranulomatosis.Donovanosis. Tropical trepanematosis (pinta, bejel, yaws).
Task 5: Differential Diagnosis Across ConditionsSituationA healthcare provider in a
tropical region encounters three patients with genital ulcers. One has painless ulcers
with Donovan bodies, the second has painful ulcers with ragged edges, and the third
initially had a small painless ulcer but now has swollen, tender lymph nodes.
Questions
1. Which condition is associated with painful ulcers?
Soft chancre (chancroid).
2. Which condition is characterized by painless ulcers with Donovan bodies?
Donovanosis (Granuloma Inguinale).
3. Which condition progresses from a painless ulcer to painful lymphadenopathy?
Venereal Lymphogranulomatosis (Lymphogranuloma Venereum).
4. What test would differentiate Haemophilus ducreyi from other causes?
Gram stainor cultureofthe ulcerexudate.
5. What is the first-line treatment for these conditions?
Soft Chancre: Azithromycin orceftriaxone.
Donovanosis: Azithromycin.
LGV: Doxycycline.
42. Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
Dracunculiasis43. Introduction
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Introduction
• Definition:
• Dracunculiasis,also known as Guineaworm
disease, is a parasitic infection caused by
Dracunculus medinensis.
• Epidemiology:
• -Historically prevalent in Africa, Asia, and the
Middle East.
• -Cases now limited to a few regions due to
eradication efforts.
44. Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
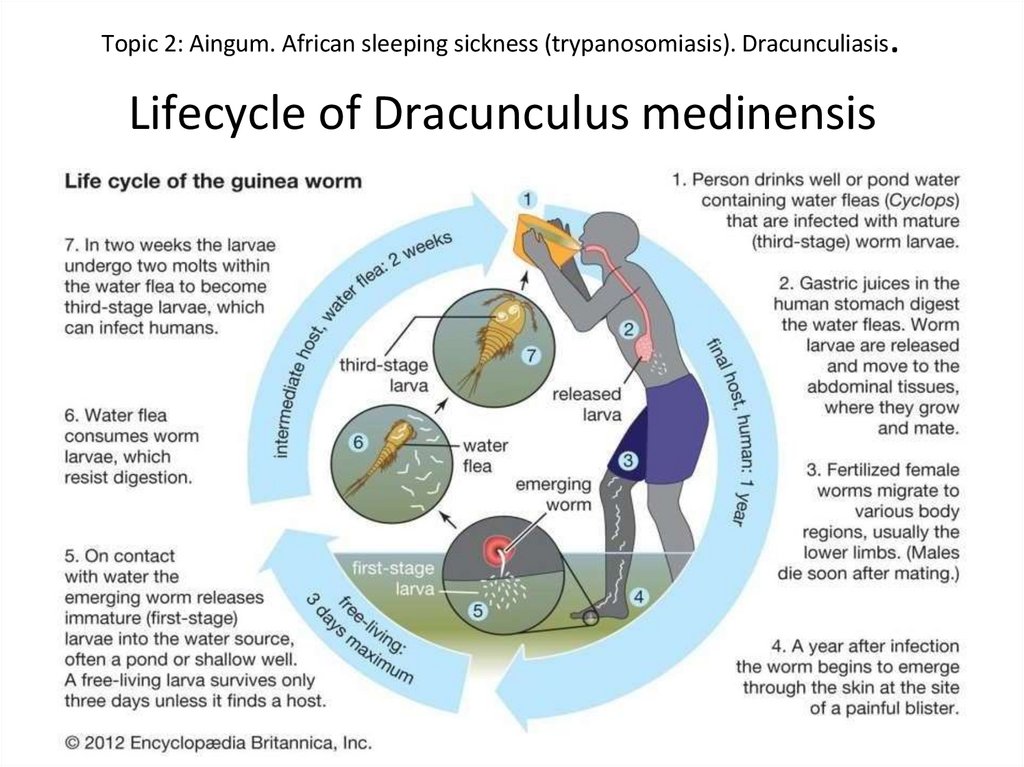
.Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
Lifecycle of Dracunculus medinensis
45. Clinical Manifestations
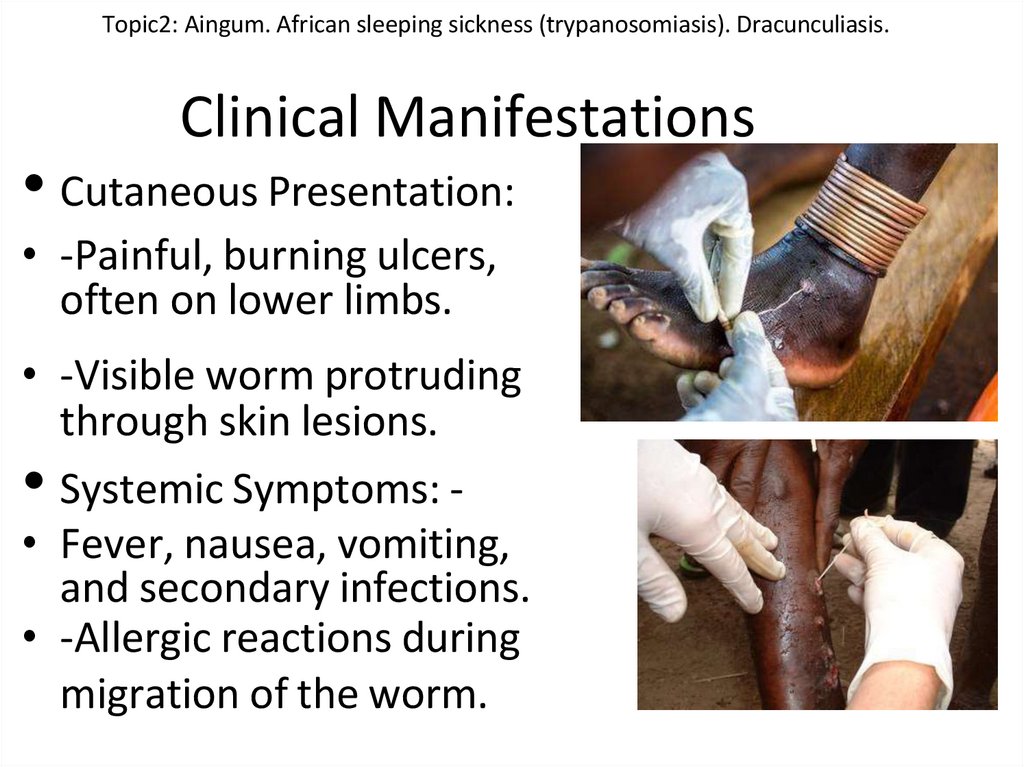
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Clinical Manifestations
• Cutaneous Presentation:
• -Painful, burning ulcers,
often on lower limbs.
• -Visible worm protruding
through skin lesions.
• Systemic Symptoms: • Fever, nausea, vomiting,
and secondary infections.
• -Allergic reactions during
migration of the worm.
46. Diagnosis
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Diagnosis
• Clinical Diagnosis:
• -Observation of emerging worm or ulcer.
• -Patient history of drinking contaminated
water.
• Differential Diagnosis:
• -Filariasis, abscesses, or other dermatological
parasitic infections.
47. Complications
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Complications
• Dermatological Complications:
• -Chronic ulcers.
• -Scarring and fibrosis.
• -Secondary bacterial infections.
• Systemic Issues:
• -Septicemia in untreated cases.
48. Treatment
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Treatment
• Mainstay Treatment:
• -Manual extraction of the worm (rolling it on a
stick).
• -Careful wound management to prevent
secondary infections.
• Supportive Therapy:
• -Analgesics andantibiotics.
• -Anti-inflammatory agents for symptomatic
relief.
49. Prevention
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Prevention
• Key Measures:
• -Providing clean drinking water (filtration and
chemical treatment).
• -Community health education.
• -Avoidance of contaminated water sources.
• Eradication Efforts:
• -The Carter Center's Guinea Worm
Eradication Program.
50. Role of Dermatovenerologists
Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Role of Dermatovenerologists
• -Recognizing cutaneous manifestations.
• -Differentiating dracunculiasis from similar
dermatological conditions.
• -Contributing to public health initiatives.
51. Conclusion
Topic 2: Aingum. African sleeping sickness (trypanosomiasis).Dracunculiasis.
Conclusion
• -Dracunculiasis is a preventable and
eradicable disease.
• - Dermatological expertise is essential in
diagnosis and management.
• -Collaborative efforts are key to achieving
global eradication.
52. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
Aim for Self-Assessment● To be able to differentiate ainhum with other disease which involved especially the
fifth toe.
● To be able to differentiate infection that is cause by bitten of different flies which
may cause African Sleeping Sickness. Able to distinguish the sign and symptom and
difference stages for early diagnosis and treatment.
● To be able to give the transmission , life cycle and incubation of the parasite
Dracunculus medinensis which cause the Dracunculiasis which also known as
guinea-worm disease.
53. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
Plan of StudyLearn about the differential diagnosis of ainhum with other disease, the causes, the
clinical appearance, sign and symptom of ainhum, and the proper treatment of
aingum according to stages before it become worsen.
● Learn the way of transmission, incubation period, the life cycle,the sign and
symptom that occur in different stages of African Sleeping Sickness, learn to
differentiate 1st stage ( heamolymphatic phase) and 2nd stage ( neurological phase),
and give the first line treatment according to different stage.
● Learn to way of transmission, incubation period, life cycle, sign and symptom of the
Dracunculiasis, and able to give treatment and prevention.
54. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
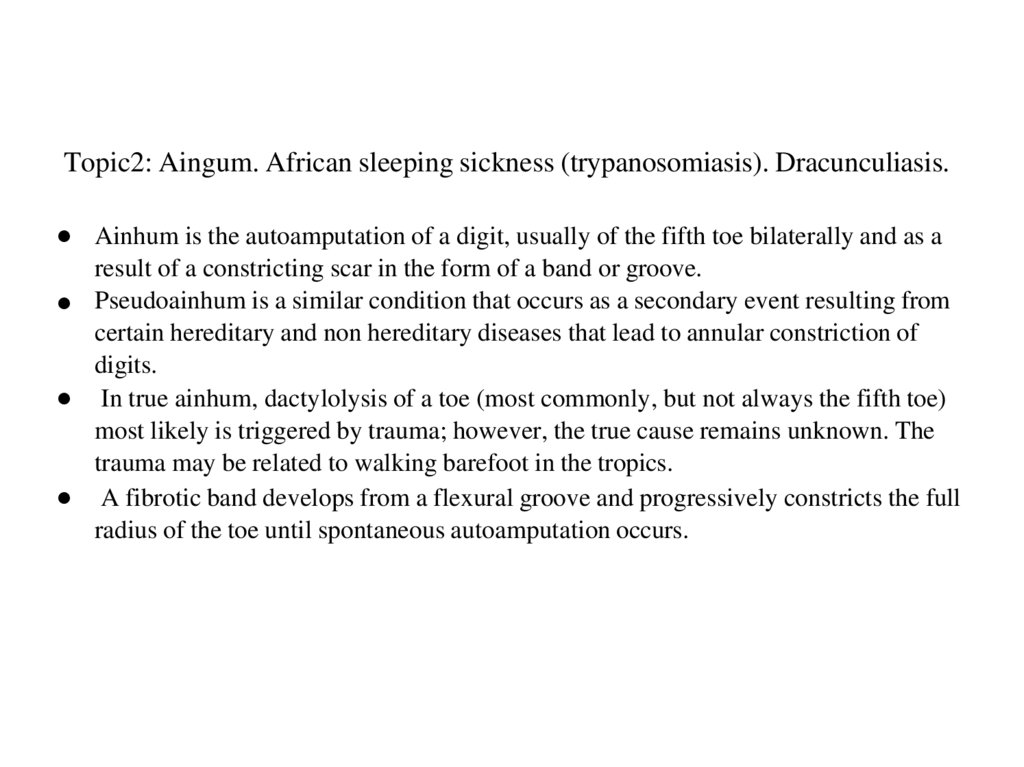
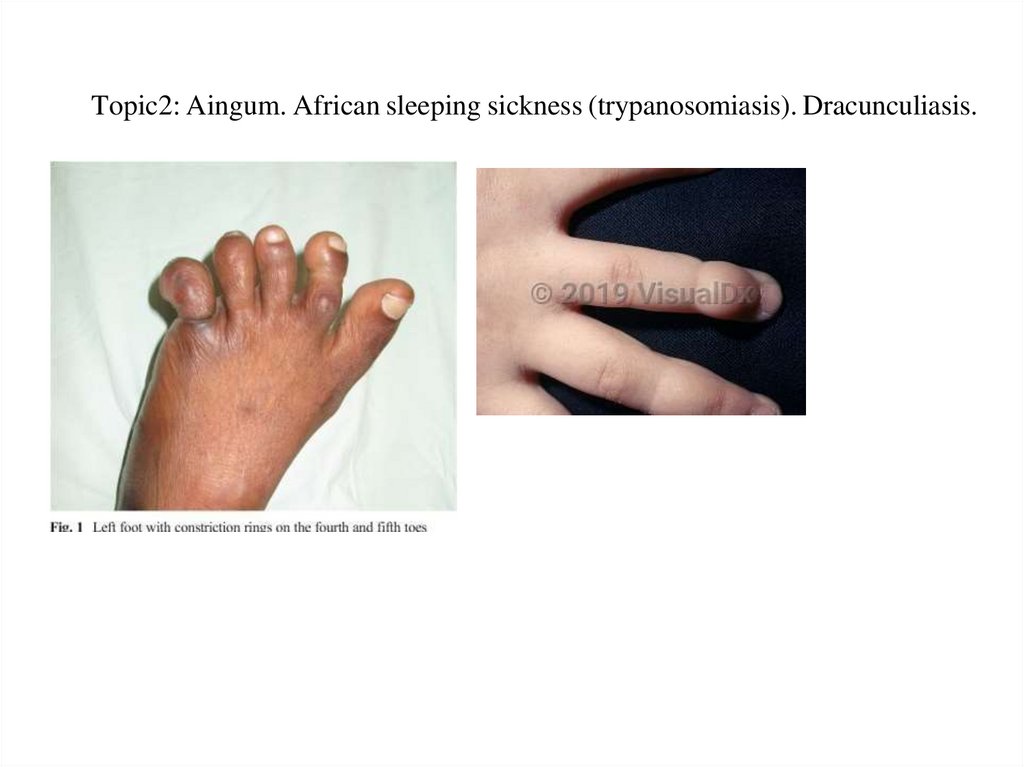
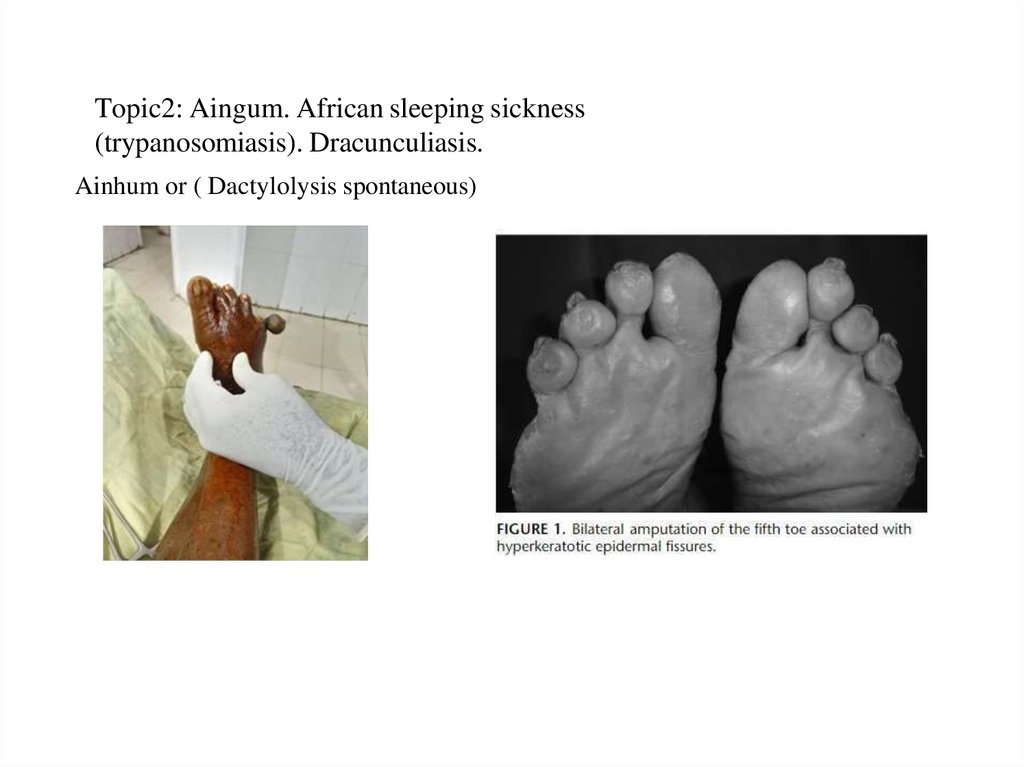
● Ainhum is the autoamputation of a digit, usually of the fifth toe bilaterally and as aresult of a constricting scar in the form of a band or groove.
● Pseudoainhum is a similar condition that occurs as a secondary event resulting from
certain hereditary and non hereditary diseases that lead to annular constriction of
digits.
● In true ainhum, dactylolysis of a toe (most commonly, but not always the fifth toe)
most likely is triggered by trauma; however, the true cause remains unknown. The
trauma may be related to walking barefoot in the tropics.
● A fibrotic band develops from a flexural groove and progressively constricts the full
radius of the toe until spontaneous autoamputation occurs.
55. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
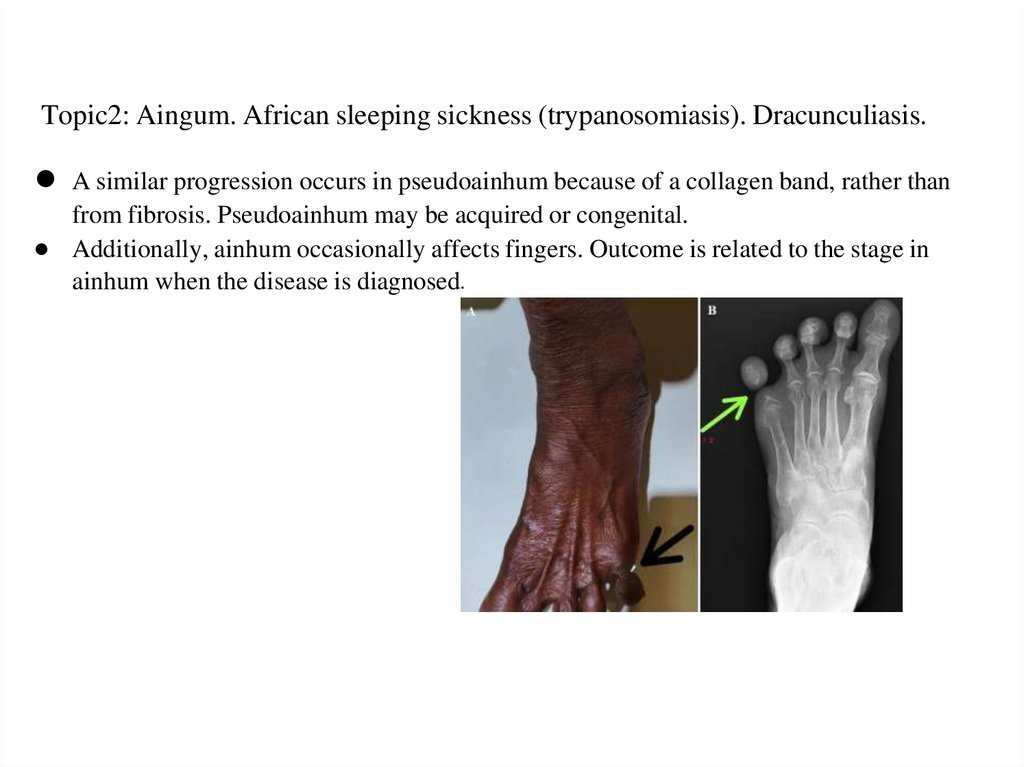
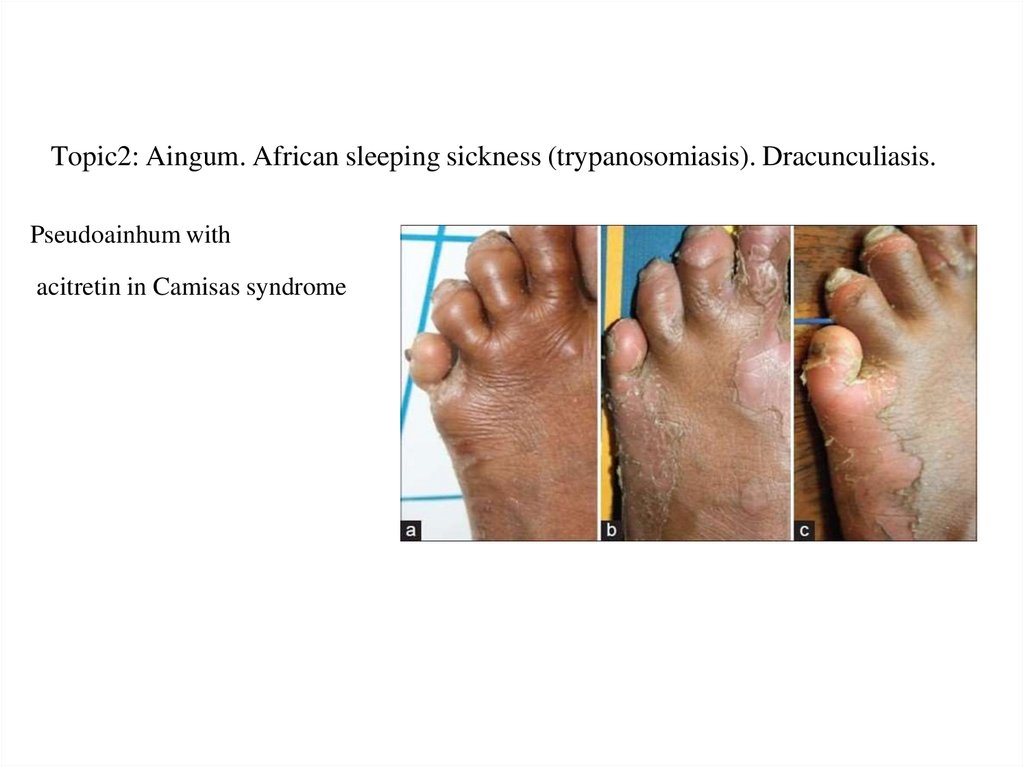
● A similar progression occurs in pseudoainhum because of a collagen band, rather thanfrom fibrosis. Pseudoainhum may be acquired or congenital.
● Additionally, ainhum occasionally affects fingers. Outcome is related to the stage in
ainhum when the disease is diagnosed.
56. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
57. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
Pseudoainhum withacitretin in Camisas syndrome
58. Topic2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.
Ainhum or ( Dactylolysis spontaneous)59. Topic 2 : Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
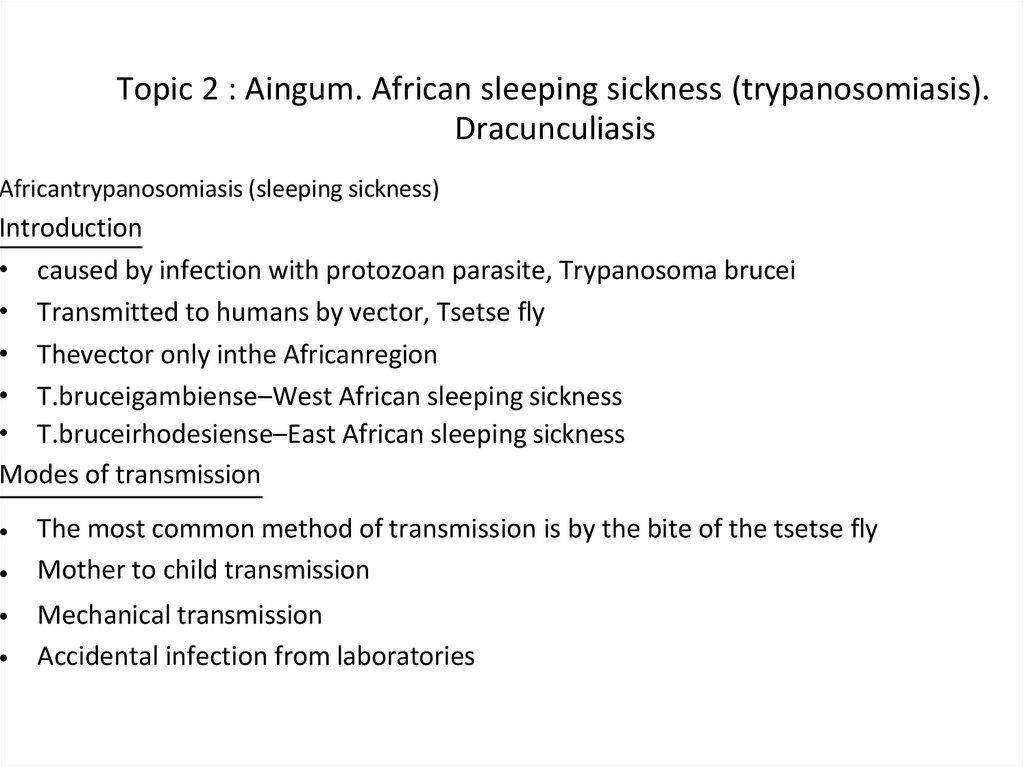
Africantrypanosomiasis (sleeping sickness)Introduction
• caused by infection with protozoan parasite, Trypanosoma brucei
• Transmitted to humans by vector, Tsetse fly
• Thevector only inthe Africanregion
• T.bruceigambiense–West African sleeping sickness
• T.bruceirhodesiense–East African sleeping sickness
Modes of transmission
The most common method of transmission is by the bite of the tsetse fly
Mother to child transmission
Mechanical transmission
Accidental infection from laboratories
60.
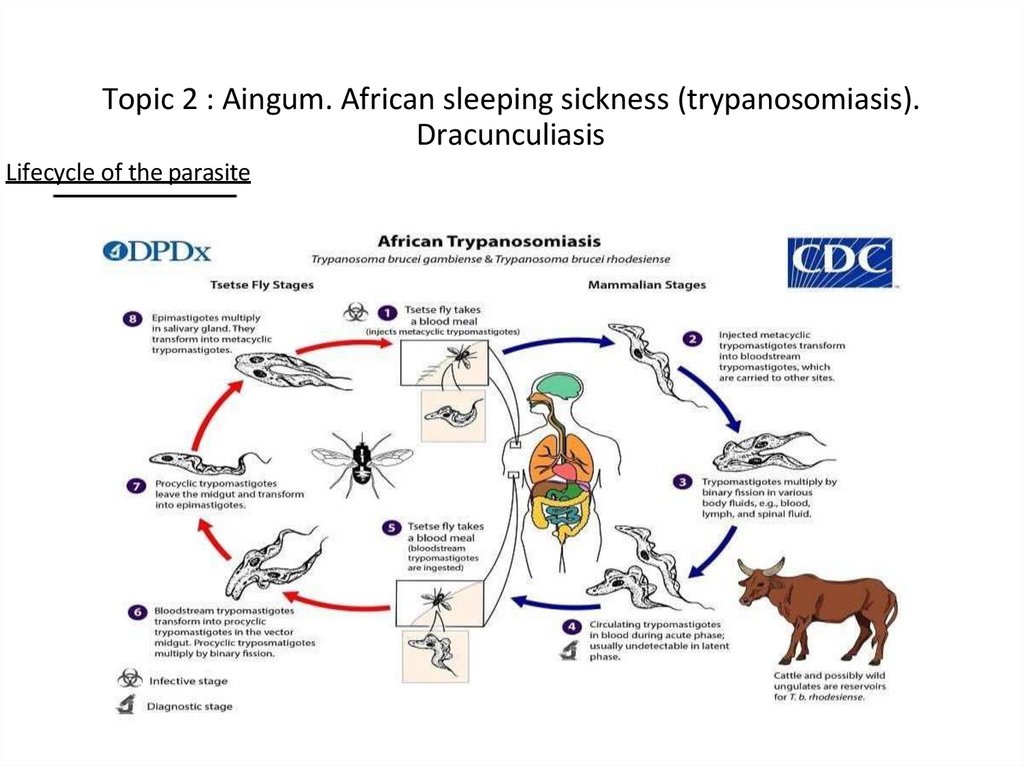
Topic 2 : Aingum. African sleeping sickness (trypanosomiasis).Dracunculiasis
Lifecycle of the parasite
61. Topic 2 : Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
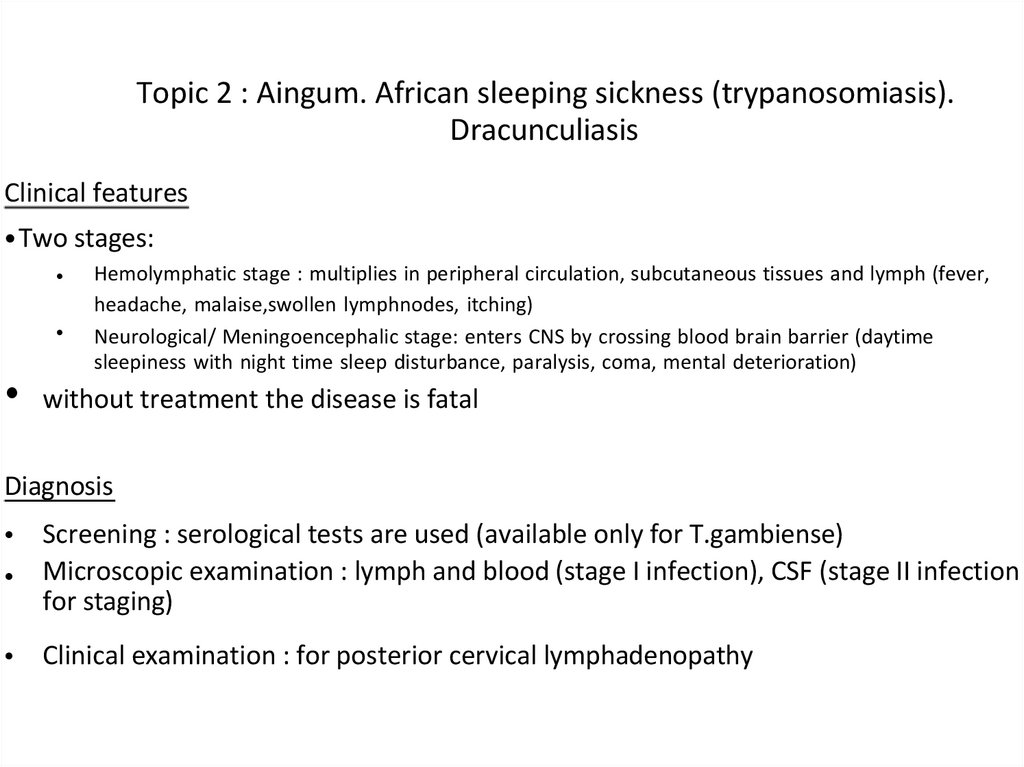
Clinical features• Two stages:
Hemolymphatic stage : multiplies in peripheral circulation, subcutaneous tissues and lymph (fever,
headache, malaise,swollen lymphnodes, itching)
Neurological/ Meningoencephalic stage: enters CNS by crossing blood brain barrier (daytime
sleepiness with night time sleep disturbance, paralysis, coma, mental deterioration)
• without treatment the disease is fatal
Diagnosis
• Screening : serological tests are used (available only for T.gambiense)
• Microscopic examination : lymph and blood (stage I infection), CSF (stage II infection &
for staging)
• Clinical examination : for posterior cervical lymphadenopathy
62. Topic 2 : Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
Treatment for stage IPentamidine
• Used against T.b.gambiense
• Generally well tolerated
Suramin
• Used against T.b.rhodesiense
• Causes urinary tract problems and allergic reaction
Treatment for stage II
• Melasoprolol
Used against both the species
Causes reactive encaphalophaty which can be fatal
eflornithine
• Effective against T.b.gambienseonly
• Treatment regimen is strict but less toxic than melarsoprolol
63. Topic 2 : Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
Control of African sleeping sickness• Control involves 2 strategies:
Control of the reservoir
By population screening and treatment of the disease in those who are having the disease
Control of the vector
Insecticides : DDT(25%) and Dieldrin(20%) are applied from aircraft
Clearing of vegetation
Genetic control through sterile male technique
Flytraps : blue coloured traps coated within secticides are used
Prevention
• Long sleeved shirts and medium-weight pants with neutral colors can be used
• Vehicle should be thoroughly inspected before entering area of resident
• Avoiding bushes
• Permethrin impregnated clothing and repellents can be used
64. Topic 2 : Aingum. African sleeping sickness (tryopanosomiasis). Dracunculiasis
Skin characteristicSwelling (Winterbottom’s
sign)
Rashes and skin ulcer
• Hyperpigmentation
• Edema
Itching
65. Topic 2 : Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis
Choose 1 correct answer.1) Which drug is commonly used to treat late-stage African trypanosomiasis involving the CNS
A) Quinine
B) Melarsoprol
C) Amphotericin B
D) Metronidazole
Correct answer : B
2) What is the primary treatment for ainhum?
A) Antibiotics
B) Surgical amputation of the affected toe
C) Topical corticosteroids
D) Physical therapy
Correct Answer: B
66.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis).Dracunculiasis.
3) Which of the following complications is more commonly associated with
East African trypanosomiasis?
A) Pruritus
B) Meningismus
C) Cardiac complications
D) Chronic lymphadenopathy
Correct answer: C
4) What is the most likely cause of death in untreated late-stage West African
trypanosomiasis?
A) Aspiration or seizures caused by CNS damage
B) Cardiac arrest
C) Respiratory failure due to pulmonary embolism
D) Severe anemia
Correct Answer: A
67.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.5) What are the key dermatological features of Dracunculiasis?
(Select all that apply)
1. Erythematouspapules withcentralcrusting.
2. Painfulskinulcerwith a visiblewormemerging.
3. Chronic ulceration with secondary bacterial infection.
4. Nodular skin lesions on the face.
Correct Answers: 2, 3
6) Which of the following strategies are effective in preventing Dracunculiasis?
(Select all that apply)
1. Filtering water witha fineclothorpipe filter.
2. Drinking only bottled waterinendemic regions.
3. Using temephosto kill infected copepods in water sources.
4.Vaccination against Dracunculusmedinensis.
Correct Answers: 1, 3
68.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.7) Which statements about the life cycle of Dracunculus medinensis are true?
(Selectall thatapply)
a) Humans become infected by drinking water containing infected copepods.
b) Adult worms migrate to subcutaneous tissue to release larvae.
c) Copepods release larvae into the bloodstream of humans.
d) The worm emerges through the skin to release larvae into water.
Correct Answers: a,b,d
8) Which diseases should be included in the differential diagnosis of Dracunculiasis?
(Select allthat apply)
1. Cutaneous larva migrans.
2. Filariasis.
3. Leishmaniasis.
4. Mycetoma.
Correct Answers: 1, 2, 4
69.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.9) What is ainhumprimarily characterized by?
A) A skin condition affecting the scalp
B) The progressive constriction of the toe, leading to amputation
C) A type of arthritis in the fingers
D) A viral infection causing lesions on the skin
Correct Answer: B
10) Which population is most commonly affected by ainhum?
A) Elderly individuals
B) People living in temperate climates
C) Individuals of African descent, particularly in rural areas
D)Childrenunder theageof10
Correct Answer: C
70.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.Clinical Task:
A 34-year-old man from a rural area in East Africa presents to your clinic with a one-month
history of intermittent fever, fatigue, and rash. Over the last week, he has developed worsening
headaches, confusion, and excessive daytime sleepiness. On examination, you note cervical
lymphadenopathy and a reduced level of consciousness. He mentions being bitten by several
flies during a recent trip near a river.
Questions:
1. What is the most likely diagnosis based on the patient’s presentation and history?
East African trypanosomiasis (Trypanosoma bruceirhodesiense).
2. What diagnostic test would confirmthis diagnosis?
Microscopic examination of a blood smear to detect trypanosomes or lumbar puncture to assess
cerebrospinal fluid (CSF) for trypanosomes in late-stage disease.
3. What are the key clinical features suggesting CNS involvement in this patient?
Confusion, excessive daytime sleepiness, headaches, and reduced level of
consciousness.
4. What is the recommended treatment for late-stage African trypanosomiasis?
Melarsoprol, as it crosses the blood-brain barrier and is effective in treating CNS involvement.
5. What complication should be monitored closely during treatment with
melarsoprol? Encephalopathic reaction, a serious and potentially fatal adverse
effect of melarsoprol.
71.
Topic 2: Aingum. African sleeping sickness (trypanosomiasis). Dracunculiasis.A 35-year-old male farmer from a rural area presents with a painful ulcer on his
lower leg. He describes a burning sensation in the lesion, which started10 days
ago. On examination, there is an inflamed ulcer with the tip of a whitish worm
visible at the base. He recalls drinking untreated pond water frequently in the
past year.
Questions:
1) What is the most likely diagnosis?
Diagnosis: Dracunculiasis(Guinea worm disease).
2) How would you manage this
patient? Management:
Slowly extract the worm using a stick or gauze.
Administer pain relief and antibiotics for secondary
infection. Advise preventive measures (clean water,
filtration).
72.
Topic 3: Tropical MycosesChromomycosis, Blastomycosis,
Sporotrichosis, Actinomycosis,
Coccidioidomycosis, Mycetoma
73. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Blastomycosis74.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
• Blastomycosis is a disease caused by the fungus
Blastomyces dermatitidis.
• The fungus lives in moist soil and in association with
decomposing organic matter such as wood and
leaves.
• Lung infection can occur after a person inhales
airborne, microscopic fungal
spores
from the
ra
t
environment; however, many people who inhale the
spores do not get sick.
• The symptoms of blastomycosis are similar to flu
symptoms, and the infection can sometimes become
serious if it is not treated.
75. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
RISK FACTOR•The disease usually affects people with weakened immune systems,
such as those with HIV or organ transplant recipients.
•Men are more likely to be affected than women.
•Lung infection may produce no symptoms, but when the infection
spreads, skin lesions or bone lesions may appear and the bladder,
kidney, prostate, and testes may be affected.
Symptoms:
Cough (may produce brown or bloody mucus)
Shortness of breath
Sweating
Fever
Fatigue
General discomfort, uneasiness, or ill-feeling (malaise)
Unintentional weight loss
Joint stiffness and joint pain
Muscle stiffness and pain
Rash
Skin lesions
Chest pain
76. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Findings• Physical: The physical examination may not reveal any abnormal findings. In the pneumonic form, findings
may be present that are associated with pneumonic consolidation (eg, dullness on percussion, bronchial
breath sounds, egophony, rales). Decreased or absent breath sounds suggest pleural effusion.
Occasionally, erythema nodosum may be observed in association with pulmonary blastomycosis.
• Skin lesions are more common on the face,neck,and extremities. Early in the disease course, the lesions
are sharply demarcated papules. Later, they expand to form ulcerated lesionwith small pustules at the
margins. Central healing and scar formation occur as the lesions grow larger. Some are verrucous, with
raised irregular borders; multiple lesions may appear simultaneously or in sequence.
• Lesions begin as papules or pustules or as subcutaneous nodules. Within a few weeks to months, the
primary lesions evolve into ulcers, with indurated dusky or violaceous granulomatous or verrucous
borders, or into vegetating plaques. Typically, the border is arciform or serpiginous, contains
numerous tiny pustules or microabscesses covered with crust, andrises abruptly from the normal
surrounding skin. Over a period of months to years, the lesions enlarge, eventually involving a
substantial portion of the face, for example, and produce severe disfigurement. As the lesions
enlarge, they heal centrally, with atrophic scar studded with telangiectasia.
• Although the vast majority of patients with cutaneous blastomycosis acquire it by dissemination
from a pulmonary focus, a few well-documented cases of primary cutaneous (inoculation)
blastomycosis have been described in laboratory workers. The skin lesions are described as
"chancriform" and are accompanied by nodular lymphangitis.
• Bone involvement rarely leads to a draining abscess. The involved joint may be tender and swollen.
77. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Other problems to be considered:Skin
Squamous cell carcinoma
Pyoderma gangrenosum
Keratoacanthoma
Tuberculosis verrucosa cutis
Halogenoderma
Lupus vulgaris
Blastomycosis like pyoderma
Chromoblastomycosis
Bone and joints
Metastatic carcinoma
Bacterial osteomyelitis
Brain
Brain neoplasm
78.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.hepatit.com/en/tag/blastomycosis-in-humans
79.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.onlinedermclinic.com/archive/blastomycosis
80.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.onlinedermclinic.com/archive/blastomycosis#!prettyPhoto
81. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
EXAMS AND TESTS, DIAGNOSISEXAMS AND TESTS
• History of living in an area where the fungus is commonly found
• Chest x-ray
• Tissue biopsy
• Skin biopsy
• Sputum culture and special stains
DIAGNOSIS
• The diagnosis is usually made by obtaining a body fluid specimen or biopsy of affected tissue
• and looking for the characteristic fungal forms in tissue under a microscope.
• A culture of body fluids or tissue from an affected site may also be performed.
• Blood tests to detect antibodies to the fungus can be done, but are not very accurate.
An antigen test, performed on a urine sample or serum sample, is also available.
82. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
TreatmentMedicines may not be needed for a blastomycosis infection that remains in the lungs, unless it
becomes severe.
When the disease is severe, or when it spreads outside of the lungs, the following medicines
(anti-fungals) may be prescribed:
1. Itraconazole
2. Fluconazole
3. Ketoconazole
Amphotericin B may be used for severe infections
You should follow-up regularly with your doctor to make sure the infection doesn't return.
PROGNOSIS
• Patients with minor skin sores (lesions) and relatively mild lung infections usually recover
• completely.
If the infection is not treated, it can become severe enough to cause death.
83. References
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
References
• http://www.cdc.gov/fungal/blastomycosis/
• http://www.onlinedermclinic.com/
• http://dermnetnz.org/fungal/blastomycosis.ht
ml
84. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
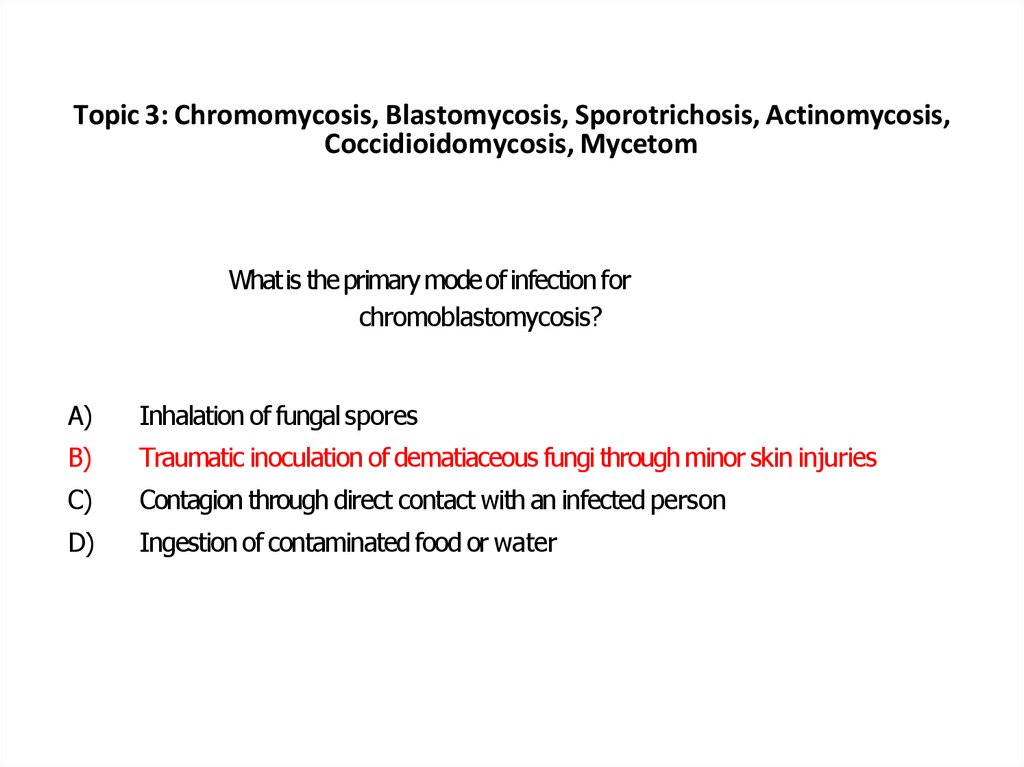
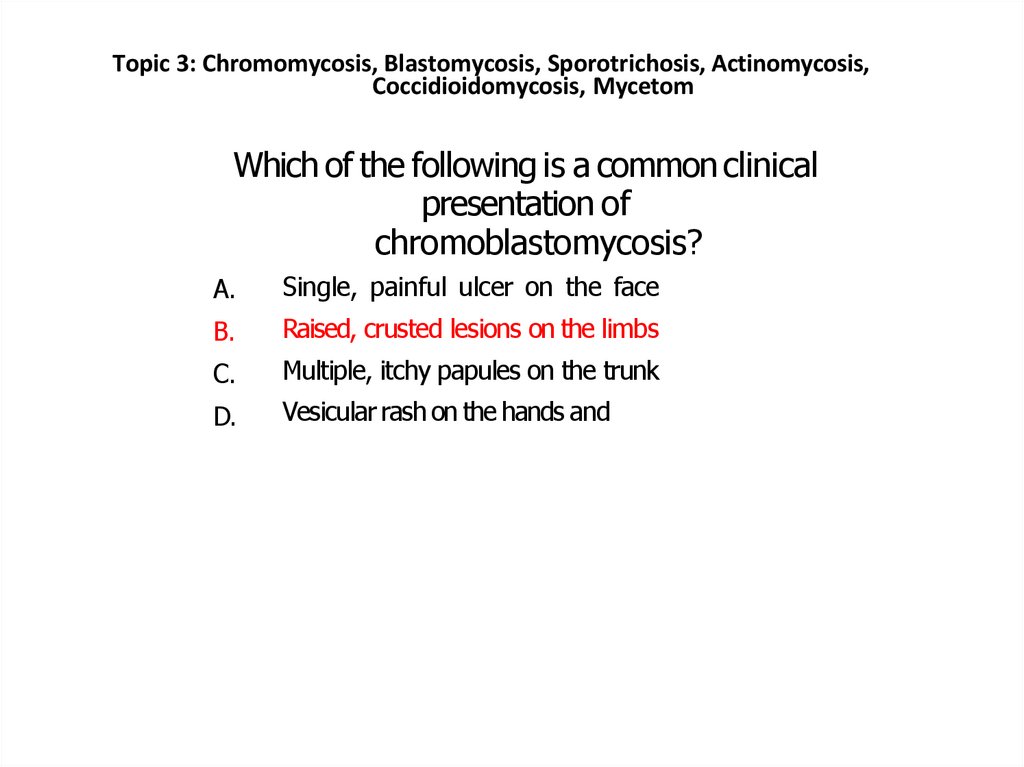
Chromomycosis85. Chromomycosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Chromomycosis
• Chromoblastomycosis (also known as
chromomycosis) is a chronic fungal infection in
whichthereare raisedcrustedlesions
affecting the skin and subcutaneous tissue. It
usually affects the limbs.
Chromoblastomycosis may be due to several
fungi found in soil, wood and decaying plant
material.
The organism is inoculated into the skin by a
minor injury, for example, a cut with a splinter
86. The most common names of the most common organisms are:
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
The most common names of the
most common organisms are:
• Hialophora verrucosa
• Fonsecaea pedrosi
• Fonsecaeacompacta
• Cladosporium carrionii
• Rhinocladiellaaquaspersa (Ramichloridium cerophilum)
87. Clinical feature of chromomycosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Clinical feature of chromomycosis
Chromoblastomycosis generally presents as a single lesion on an
exposed site such as the foot or hand.
It starts as a small firm red or grey bump.
It grows very slowly: only about 2mm per year.
Eventually a warty dry nodule or plaque develops.
There may be at least partial clearing with scarring in the centre
of the lesion.
The affected limb can enlarge generally (elephantiasis).
New lesions may develop in time as satellites around the first one
or the infection may be scratched into a new site.
It may cause no discomfort but is frequently very itchy.
Rarely,squamouscell carcinoma (SCC) develops within long
standing chromoblastomycosis.
88. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
The infection is sometimes confusedwithotherskinconditionssuchas:
Other fungal infections such as sporotrichosis
Bacterial infections such as atypical mycobacterium infection,
tuberculosis, leprosy and syphilis
Protozoal infections such as leishmaniasis
Squamous cellcarcinoma
Skin disorders such as psoriasis, discoid lupus
erythematosus.
89. Diagnosis and Test
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Diagnosis and Test
Microscopy and culture of scrapings or pus swabs suggest
the diagnosis. Histopathology of chromoblastomycosis may
show typical thick-walled dark-brown cells on skin biopsy
confirming the presence of a dematiaceous fungus. It is
dark coloured due to melanin in the walls of the organism.
Clusters of characteristic thick-walled brown 'sclerotic'
(hard) cells are seen on microscopy, after add of potassium
hydroxide (KOH).
• Culture at 25-30 degrees celsius grows olive-green to black
fungalcolonies afteroneor twoweeks. Namingthe
responsible fungus can be difficult. Phaeohyphomycosis is
thenamegiven toinfection causedby dematiaceous fungi.
90. Treatment
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Treatment
• Rarely, chromoblastomycosis resolves
spontaneously leaving a scar.
Treatment is difficult and prolonged. It may include:
• Itraconazole, posaconazole or voriconazole,
• possibly in combination with terbinafine;
• Flucytosine;
• Thiobendazole;
• Local heat;
• Cryotherapy;
Surgery to remove the affected tissue completely.
91.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.dermnetnz.org/c
ommon/image.php?path=/fu
ngal/img/chrobla.jpg
92.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.dermnetnz.org/common/image.php?path=/fungal/img/ch
roclo.jpg
93.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://dermaamin.com/site/atlas-of-dermatology/3-c/266chromoblastomycosis-.html
94.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://see.visualdx.com/diagnosis/chromoblastomycosis
95. References
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
References
• http://emedicine.medscape.com/article/1092
695-overview
• apps.who.int/medicinedocs/en/d/Jh2918e/6.3
.html
• http://www.dermnetnz.org/fungal/chromobla
stomycosis.html
• http://www.doctorfungus.org/mycoses/huma
n/other/chromoblastomycosis.php
96. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
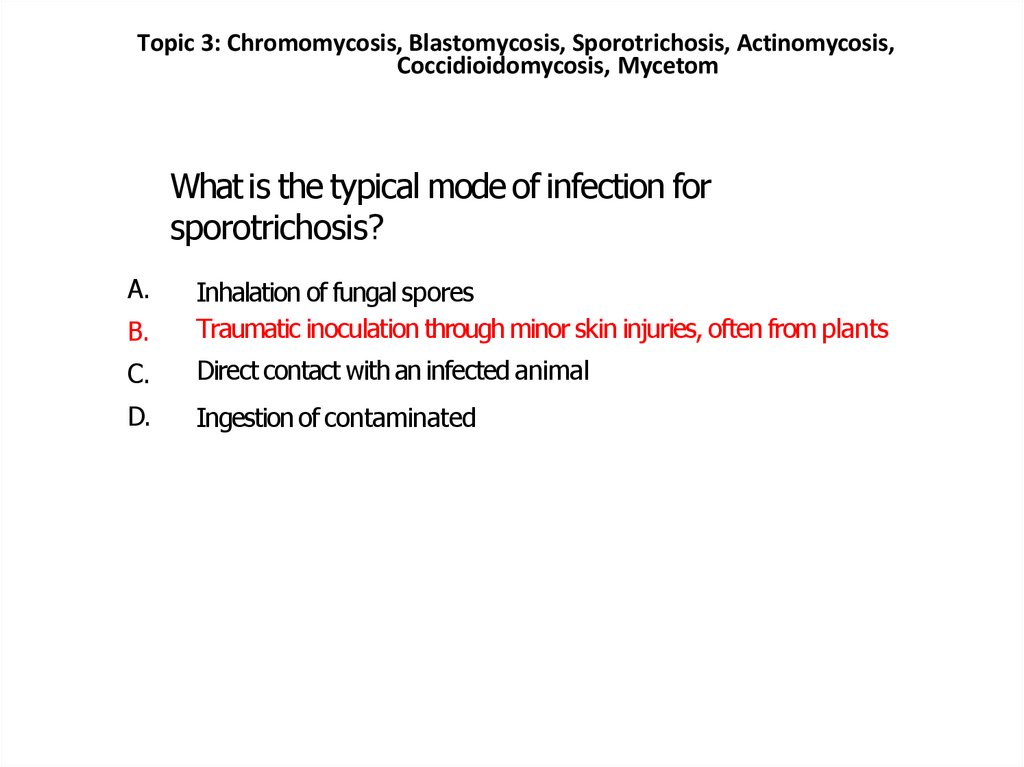
Sporotrichosis97. Sporotrichosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Sporotrichosis
• Sporotrichosis is a fungal infection of the skin
caused by the fungus Sporothrix schenckii,
which is found on decaying vegetation,
rosebushes, twigs, hay, sphagnum moss and
mulch-rich soil.
Because roses can spread the disease, it is one
of a few diseases referred to asrosethornorrose-gardeners' disease.
98. How does sporotrichosis arise?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
How does sporotrichosis arise?
• The most common route of infection with S schenckiiis
via the skin through small cuts, scratches or punctures
from thorns, barbs, pine needles or wires.
Sporotrichosis does not appear to be transmitted from
person to person but there are reported cases of
transmission from infected cats to humans. In very rare
cases, spore-laden dust can be inhaled or ingested and
in people with a weakened immune system cause
disseminated (widespread) sporotrichosis.
• People at risk of contracting sporotrichosis include
farmers, nursery workers, landscapers and gardeners.
Adult males are, by their occupation, most exposed to
the risk of infection.
99. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
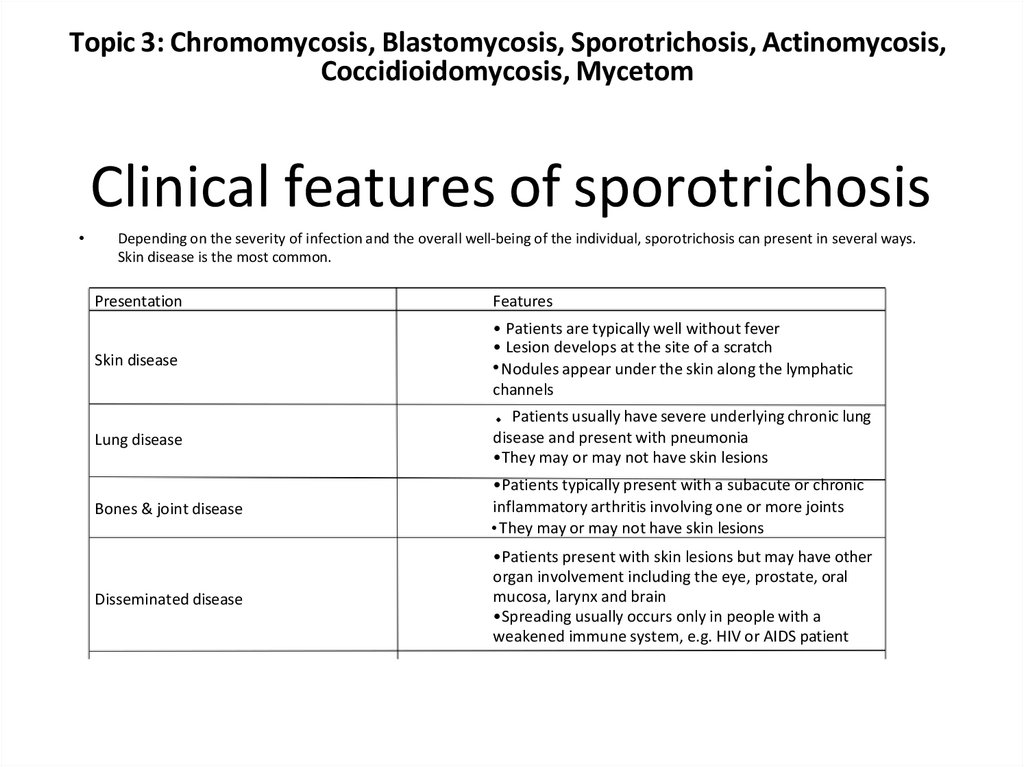
Clinical features of sporotrichosisDepending on the severity of infection and the overall well-being of the individual, sporotrichosis can present in several ways.
Skin disease is the most common.
Presentation
Features
Skin disease
• Patients are typically well without fever
• Lesion develops at the site of a scratch
• Nodules appear under the skin along the lymphatic
channels
Lung disease
Patients usually have severe underlying chronic lung
disease and present with pneumonia
•They may or may not have skin lesions
Bones & joint disease
•Patients typically present with a subacute or chronic
inflammatory arthritis involving one or more joints
• They may or may not have skin lesions
Disseminated disease
•Patients present with skin lesions but may have other
organ involvement including the eye, prostate, oral
mucosa, larynx and brain
•Spreading usually occurs only in people with a
weakened immune system, e.g. HIV or AIDS patient
100. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
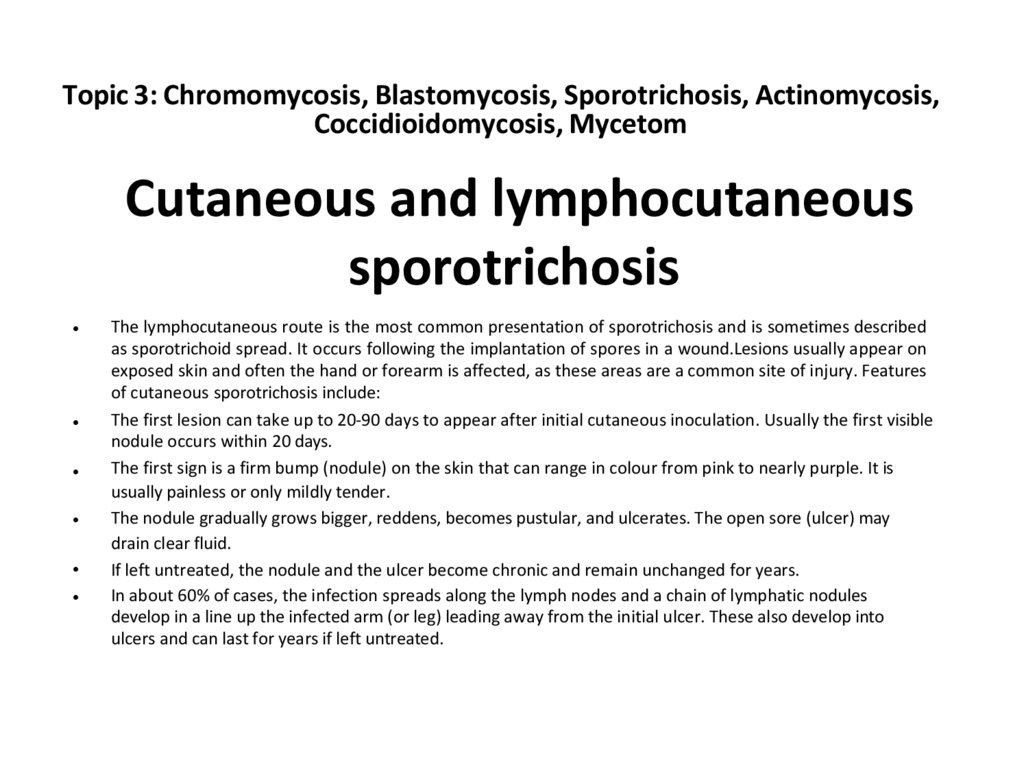
Cutaneous and lymphocutaneoussporotrichosis
The lymphocutaneous route is the most common presentation of sporotrichosis and is sometimes described
as sporotrichoid spread. It occurs following the implantation of spores in a wound.Lesions usually appear on
exposed skin and often the hand or forearm is affected, as these areas are a common site of injury. Features
of cutaneous sporotrichosis include:
The first lesion can take up to 20-90 days to appear after initial cutaneous inoculation. Usually the first visible
nodule occurs within 20 days.
The first sign is a firm bump (nodule) on the skin that can range in colour from pink to nearly purple. It is
usually painless or only mildly tender.
The nodule gradually grows bigger, reddens, becomes pustular, and ulcerates. The open sore (ulcer) may
drain clear fluid.
If left untreated, the nodule and the ulcer become chronic and remain unchanged for years.
In about 60% of cases, the infection spreads along the lymph nodes and a chain of lymphatic nodules
develop in a line up the infected arm (or leg) leading away from the initial ulcer. These also develop into
ulcers and can last for years if left untreated.
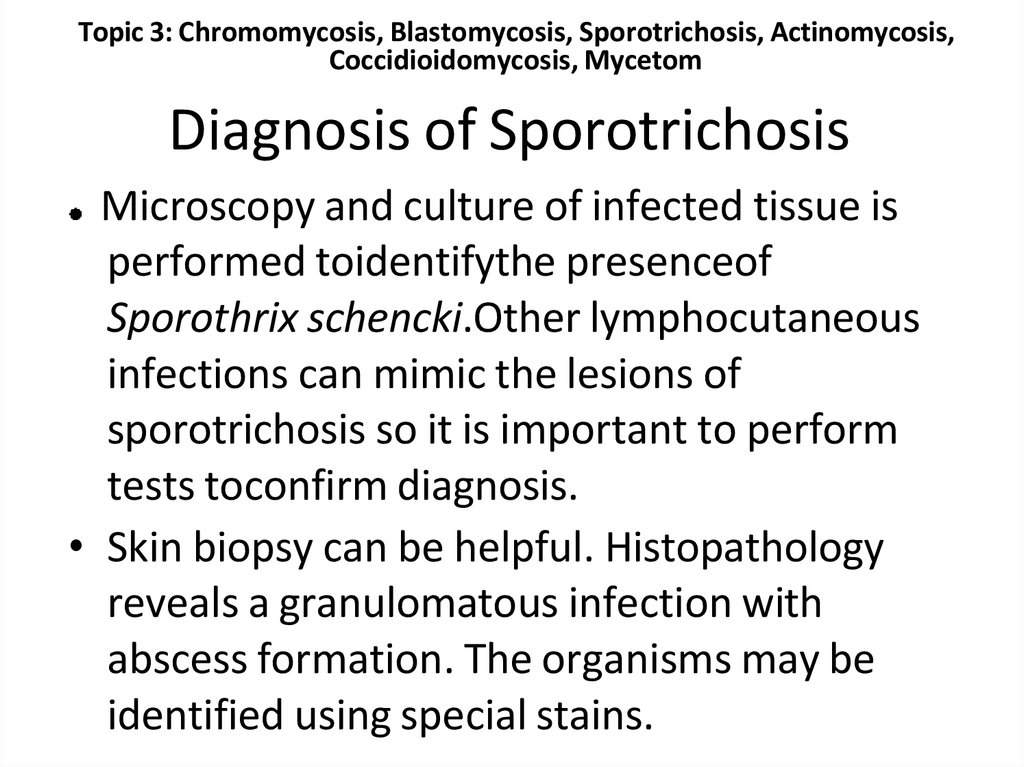
101. Diagnosis of Sporotrichosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Diagnosis of Sporotrichosis
Microscopy and culture of infected tissue is
performed toidentifythe presenceof
Sporothrix schencki.Other lymphocutaneous
infections can mimic the lesions of
sporotrichosis so it is important to perform
tests toconfirm diagnosis.
• Skin biopsy can be helpful. Histopathology
reveals a granulomatous infection with
abscess formation. The organisms may be
identified using special stains.
102. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
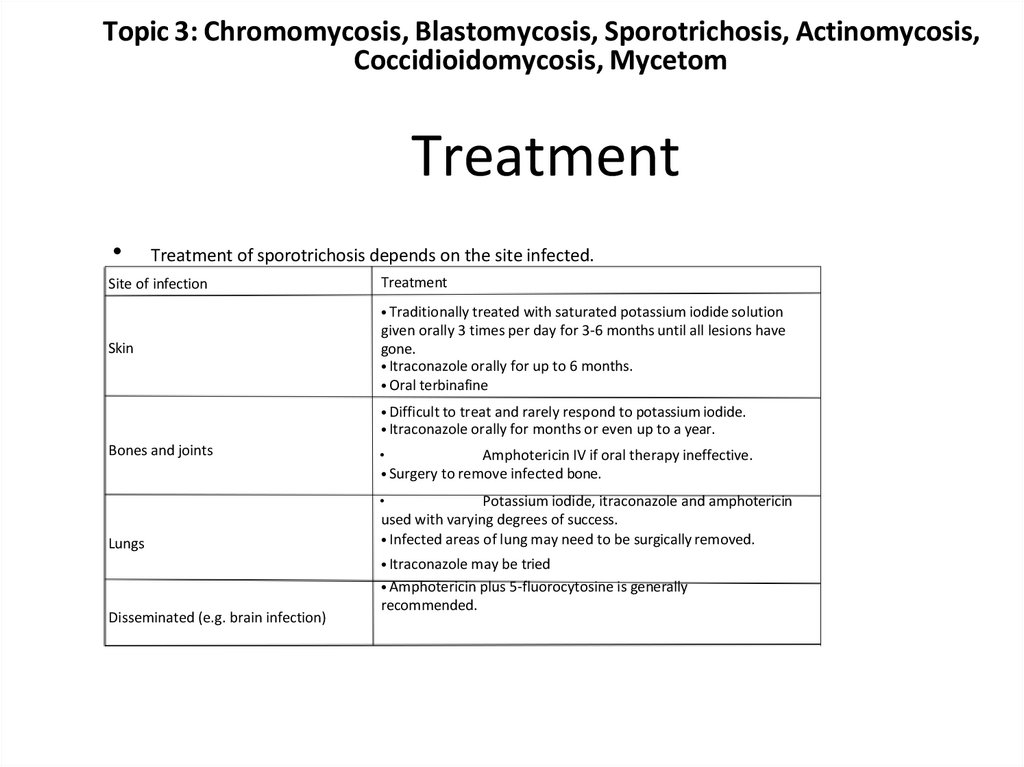
TreatmentTreatment of sporotrichosis depends on the site infected.
Site of infection
Treatment
• Traditionally treated with saturated potassium iodide solution
Skin
given orally 3 times per day for 3-6 months until all lesions have
gone.
• Itraconazole orally for up to 6 months.
• Oral terbinafine
• Difficult to treat and rarely respond to potassium iodide.
• Itraconazole orally for months or even up to a year.
Bones and joints
Amphotericin IV if oral therapy ineffective.
• Surgery to remove infected bone.
Lungs
Potassium iodide, itraconazole and amphotericin
used with varying degrees of success.
• Infected areas of lung may need to be surgically removed.
• Itraconazole may be tried
• Amphotericin plus 5-fluorocytosine is generally
Disseminated (e.g. brain infection)
recommended.
103.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Treatment of sporotrichosis can be prolonged but should continue until all lesions have resolved.
This may take months or years, and scars may remain at the original site of infection. However,
most people can expect a full recovery. Systemic or disseminated sporotrichosis is usually more
difficult to treat and in some cases life-threatening for people with weakened immune systems.
Patients should be advised of measures to take to prevent sporotrichosis. These include wearing
gloves, boots and clothing that covers the arms and legs when handling rose bushes, hay bales,
pine seedlings or other materials that may scratch or break the skin surface. It is also advisable to
avoid skin contact with sphagnum moss.
104.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.patienthelp.org/diseasesconditions/sporotrichosis.html
105.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.moavenandpartners.com/doctors/information_form/sporotric
hosis.shtml
106.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://dermaamin.com/site/atlas-of-dermatology/18-s/1162sporotrichosis-.html
107.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://dermaamin.com/site/atlas-of-dermatology/18-s/1162sporotrichosis-.html
108. References
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
References
• http://www.cdc.gov/fungal/sporotrichosis/
• http://dermnetnz.org /fungal/sporotrichosis.ht
ml
• http://www.doctorfungus.org/mycoses/huma
n/sporo/sporotrichosis.php
109. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Actinomycosis110. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
• Actinomycosis is a chronic (slowly progressive) infectioncaused by various bacterial species of the Actinomyces
genus, most commonly Actinomyces israelii.
Actinomyces are normal in habitants of the mouth,
gastrointestinal tract, and female genital tract, and do
not cause an infection unless there is a break in the skin
or mucosa. Actinomycesalso appear to require the
presence of other accompanying bacteria in order to
cause disease.
• The disease is characterised by the formation of
abscesses and draining sinu stracts (small tunnels which
open onto the surface of the skin or mucous membranes
and drain pus). The draining pus contains yellow granules
called sulphur granules (named from the colour of the
granules, not the content).
• Historically, actinomycosis was thought to be a fungal
disease because of the appearance of the bacteria and
the slowly progressive nature of the illness.
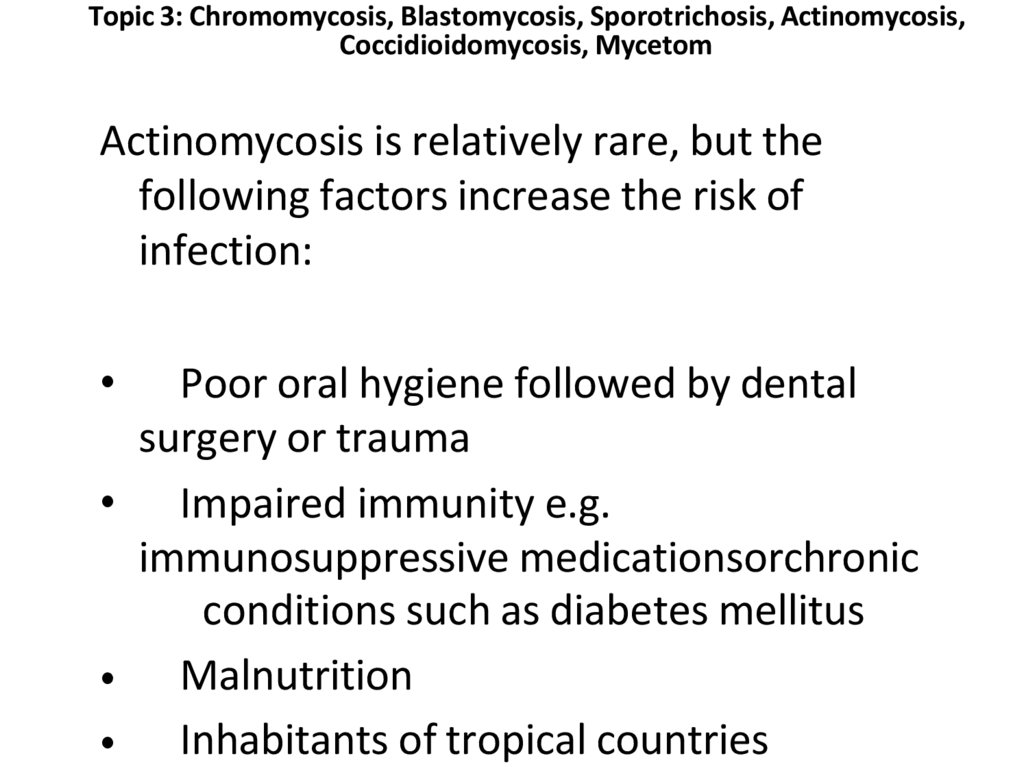
111. Actinomycosis is relatively rare, but the following factors increase the risk of infection:
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Actinomycosis is relatively rare, but the
following factors increase the risk of
infection:
Poor oral hygiene followed by dental
surgery or trauma
• Impaired immunity e.g.
immunosuppressive medicationsorchronic
conditions such as diabetes mellitus
• Malnutrition
• Inhabitants of tropical countries
112.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://escholarship.org/uc/item/53h0n68b/7.jpg
113.
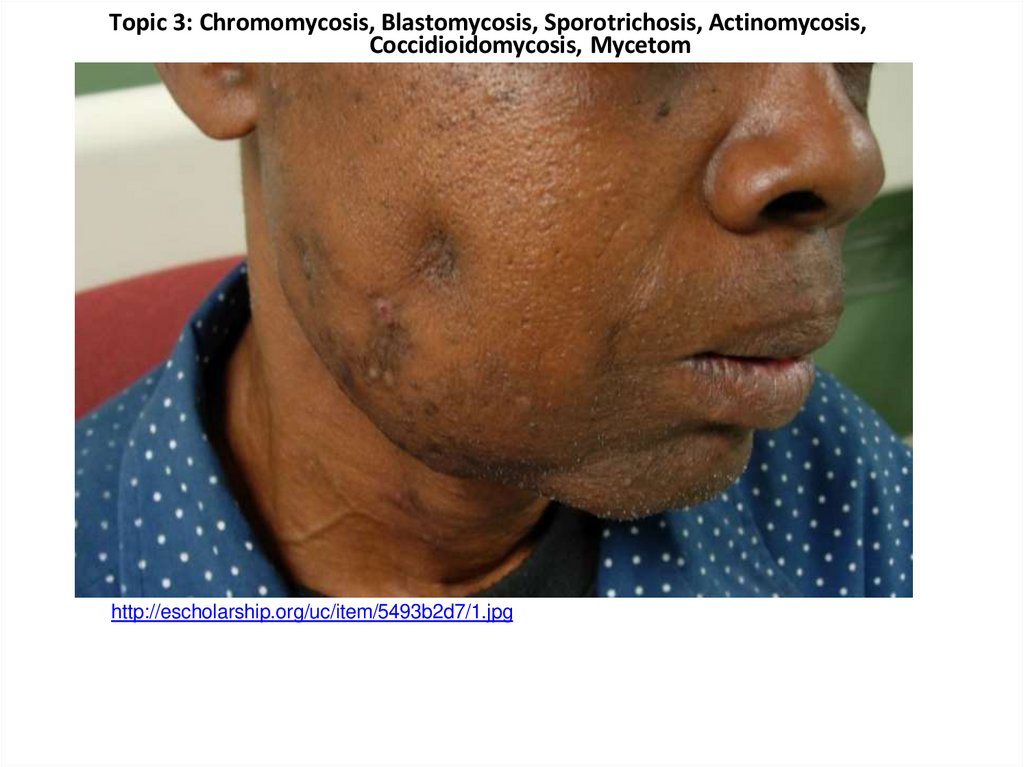
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://escholarship.org/uc/item/5493b2d7/1.jpg
114.
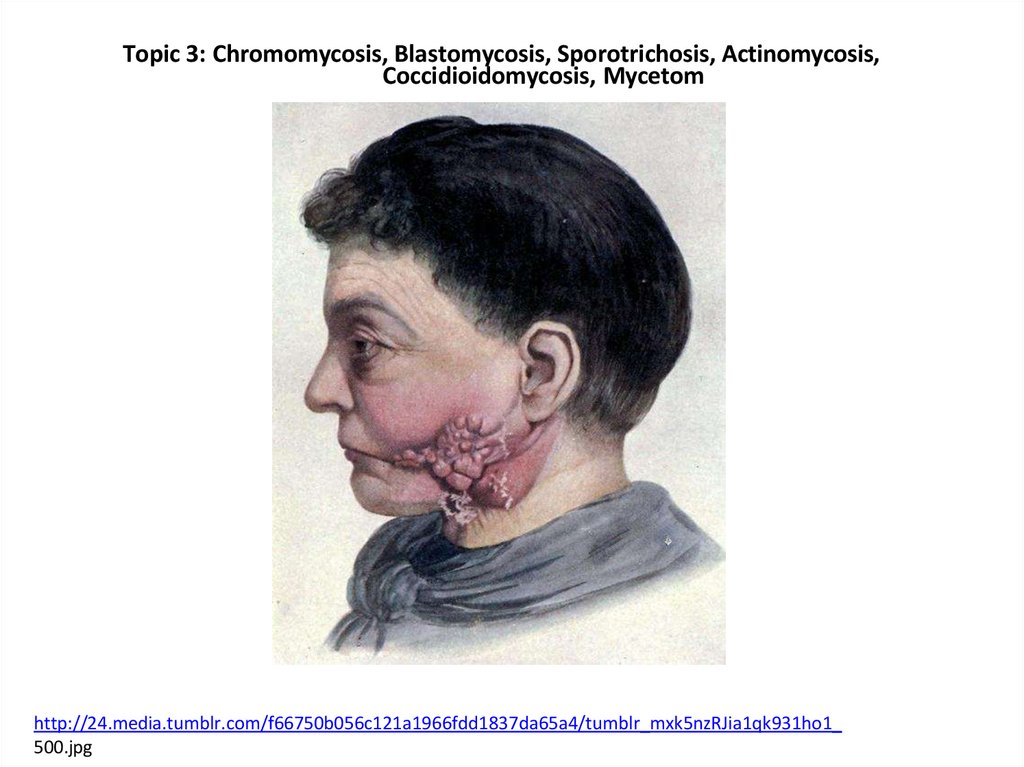
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://24.media.tumblr.com/f66750b056c121a1966fdd1837da65a4/tumblr_mxk5nzRJia1qk931ho1_
500.jpg
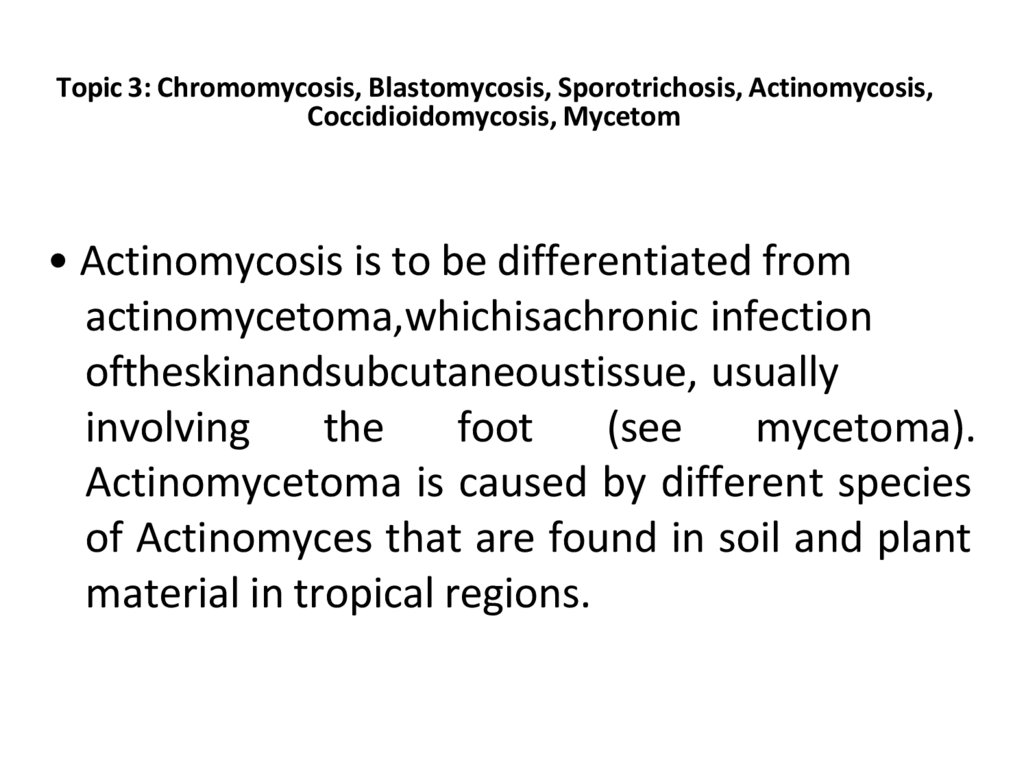
115. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
• Actinomycosis is to be differentiated fromactinomycetoma,whichisachronic infection
oftheskinandsubcutaneoustissue, usually
involving
the
foot
(see
mycetoma).
Actinomycetoma is caused by different species
of Actinomyces that are found in soil and plant
material in tropical regions.
116. Clinical features
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Clinical features
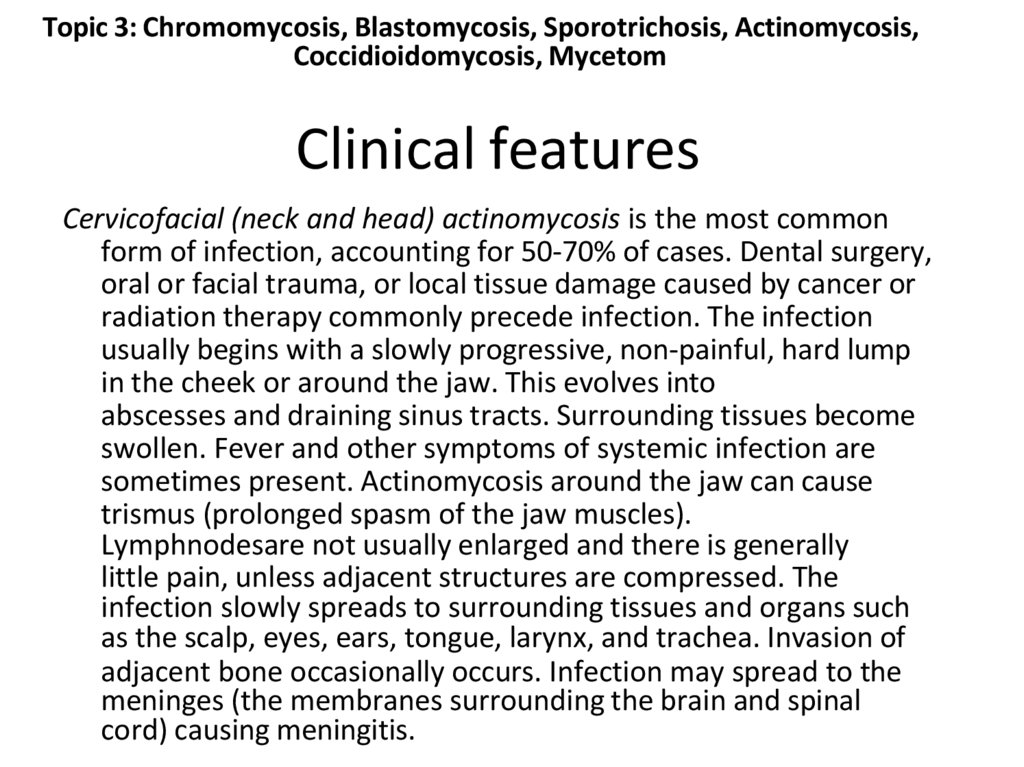
Cervicofacial (neck and head) actinomycosis is the most common
form of infection, accounting for 50-70% of cases. Dental surgery,
oral or facial trauma, or local tissue damage caused by cancer or
radiation therapy commonly precede infection. The infection
usually begins with a slowly progressive, non-painful, hard lump
in the cheek or around the jaw. This evolves into
abscesses and draining sinus tracts. Surrounding tissues become
swollen. Fever and other symptoms of systemic infection are
sometimes present. Actinomycosis around the jaw can cause
trismus (prolonged spasm of the jaw muscles).
Lymphnodesare not usually enlarged and there is generally
little pain, unless adjacent structures are compressed. The
infection slowly spreads to surrounding tissues and organs such
as the scalp, eyes, ears, tongue, larynx, and trachea. Invasion of
adjacent bone occasionally occurs. Infection may spread to the
meninges (the membranes surrounding the brain and spinal
cord) causing meningitis.
117.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
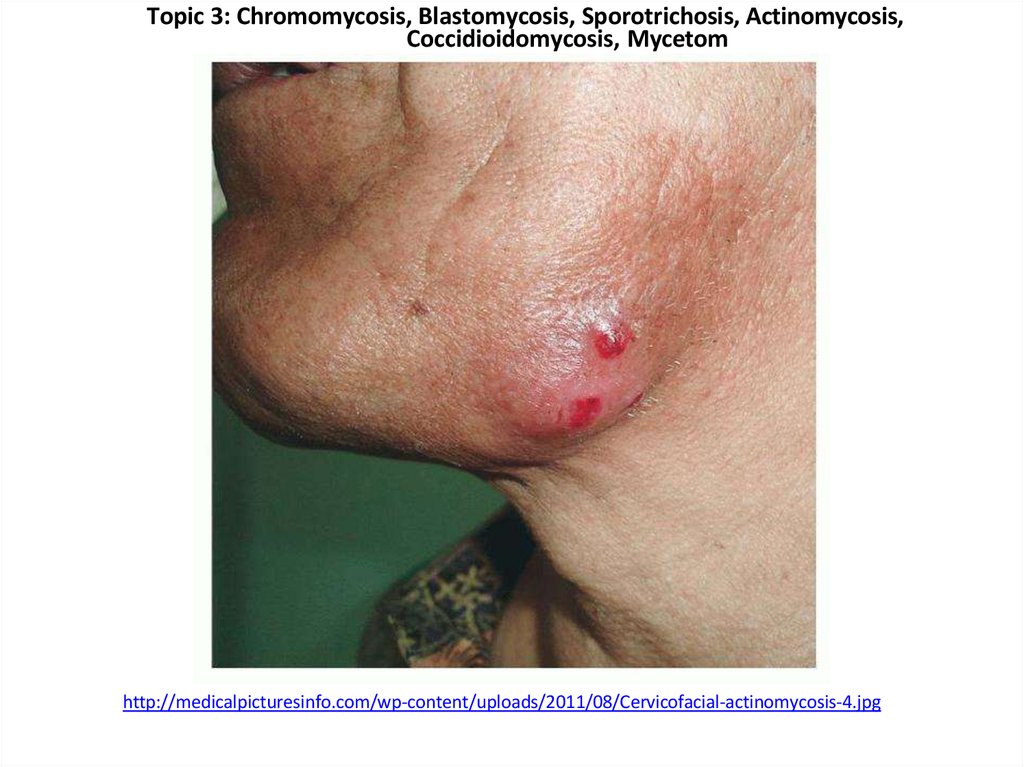
http://medicalpicturesinfo.com/wp-content/uploads/2011/08/Cervicofacial-actinomycosis-4.jpg
118.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
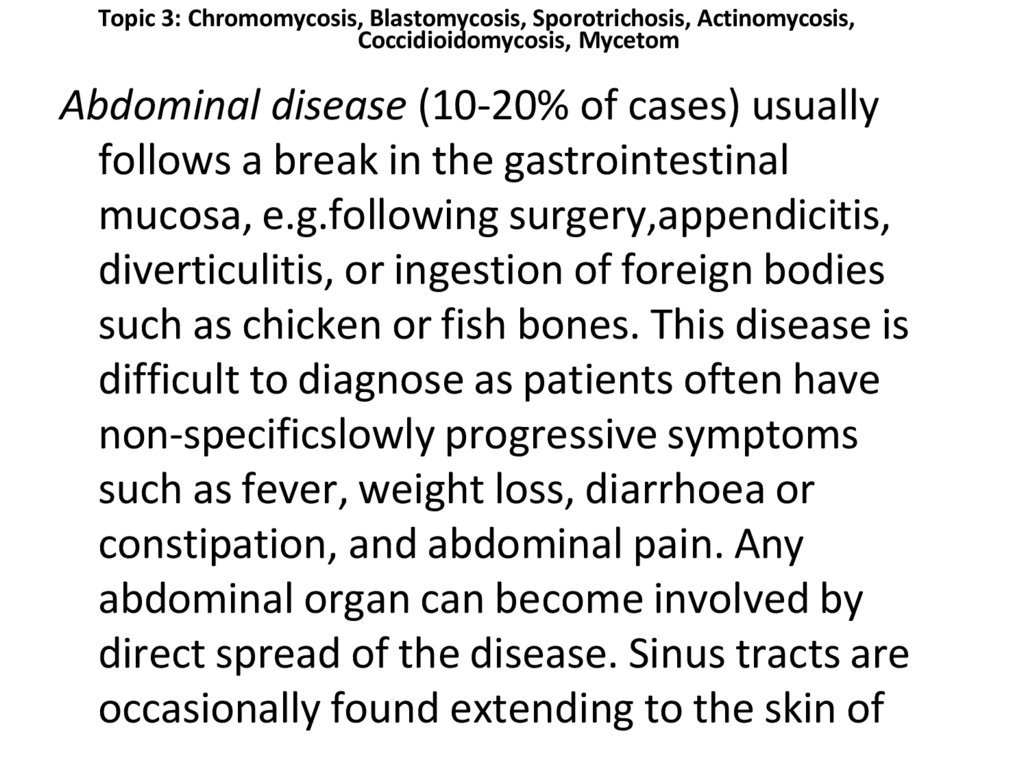
Abdominal disease (10-20% of cases) usually
follows a break in the gastrointestinal
mucosa, e.g.following surgery,appendicitis,
diverticulitis, or ingestion of foreign bodies
such as chicken or fish bones. This disease is
difficult to diagnose as patients often have
non-specificslowly progressive symptoms
such as fever, weight loss, diarrhoea or
constipation, and abdominal pain. Any
abdominal organ can become involved by
direct spread of the disease. Sinus tracts are
occasionally found extending to the skin of
119. Pulmonary actinomycosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
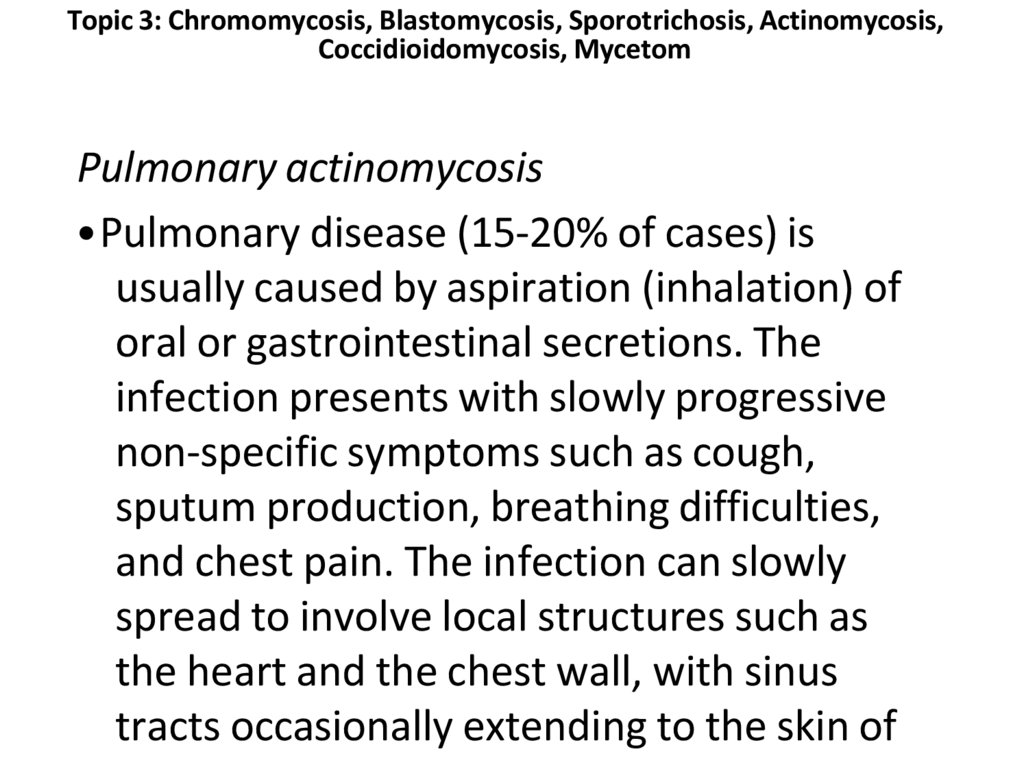
Pulmonary actinomycosis
• Pulmonary disease (15-20% of cases) is
usually caused by aspiration (inhalation) of
oral or gastrointestinal secretions. The
infection presents with slowly progressive
non-specific symptoms such as cough,
sputum production, breathing difficulties,
and chest pain. The infection can slowly
spread to involve local structures such as
the heart and the chest wall, with sinus
tracts occasionally extending to the skin of
120. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Pelvic actinomycosis is rare and is associatedwith the use of intrauterine contraceptive
devices. Common symptoms of this
infection include lower abdominal
discomfort, abnormal vaginal bleeding, and
vaginal discharge.
Primary cutaneous actinomycosis is very
uncommon and affects exposed skin after
direct implantation of the organism during
an injury.Ï
121. Diagnosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Diagnosis
• Material obtained from aspirating an abscess
or sinustract, or fromabiopsy specimencan
be culturedin the laboratory; strictgrowth
conditions are required. Often a variety of
accompanying bacteria will be present.
• Sulphur granules may be examined under a
microscope for features characteristic of
Actinomyces; however this is not a conclusive
test, as another bacterium called Nocardia has
a similar appearance.
122. Treatment
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Treatment
• Actinomycosis is treated with antibiotics, such
aspenicillin. Alternative antibiotics include
tetracyclines, erythromycin,andclindamycin.
Prolonged treatment is often required to
prevent relapse. In some cases, surgery may
also be necessary to drain deep abscesses and
to remove the sinuses.
123.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
• http://www.dermnetnz.org/bacterial/actinomycosis.html
• http://www.nlm.nih.gov/medlineplus/ency/article/000599.
htm
• http://www.healthline.com/health/actinomycosis#Overvie
w
• http://www.medicalnewstoday.com/articles/245144.php
• http://emedicine.medscape.com/article/211587-overview
• http://emedicine.medscape.com/article/1092133-overview
• http://www.nhs.uk/conditions/actinomycosis/Pages/Introd
uction.aspx
124. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Mycetoma125.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.who.int/neglected_diseases/diseases/massive_foot_mycetoma.jpg
126.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
• is a chronic subcutaneous infection caused
by actinomycetes or fungi
• This infection results in a granulomatous
inflammatory response in the deep dermis
and subcutaneous tissue, which can extend
to the underlying bone.
• Mycetoma is characterized by the formation
of grains containing aggregates of the
causative organisms that may be discharged
onto the skin surface through multiple
sinuses.
127. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
• Mycetoma caused by microaerophilicactinomycetes is termed actinomycetoma,
and mycetoma caused by true fungi is called
eumycetoma.
• Eumycetoma usually involves the
subcutaneous tissue after a traumatic
inoculation of the causative
organism. Swelling and formation of sinus
tracts characterize mycetoma. The sinuses
usually discharge purulent and seropurulent
exudate containing grains. It may spread to
involve the skin and the deep structures
128.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.dermaamin.com/site/images/clinical-pic/m/mycetoma/mycetoma13.jpg
129.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
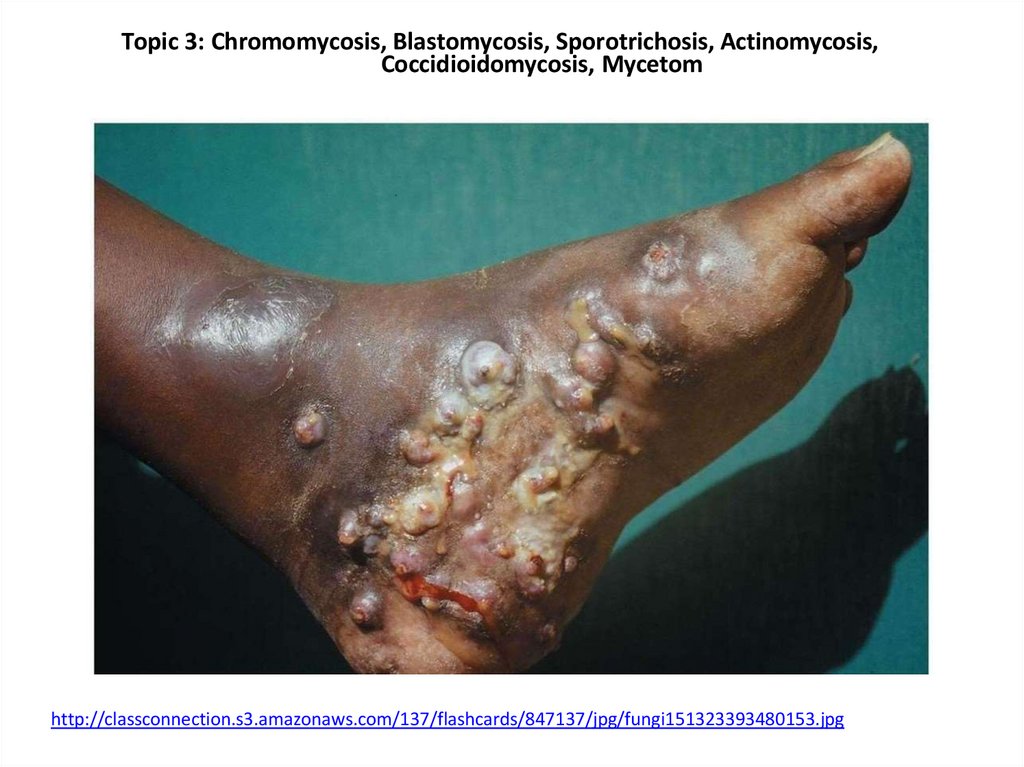
http://classconnection.s3.amazonaws.com/137/flashcards/847137/jpg/fungi151323393480153.jpg
130. Pathogenesis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Pathogenesis
• The disease is usually acquired while
performing agricultural work, and it generally afflicts men
between 20 and 40 years old.
• The disease is acquired by contacting grains of
fungal spores that have been discharged onto the soil.
• Infection usually involves an open area or break in the skin.
• Pseudoallescheria boydiiis one of many fungi spp. that
causes the fungal form of madura foot
• The disease is characterized by a yogurt-like discharge upon
maturation of the infection. Hematogenous or lymphatic
spread is uncommon. Infections normally start in the foot
or hand and travel up the leg or arm
131. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Eumycetoma may be one of several varieties,depending upon color of the granulous discharge:
• red
• Actinomadura pelletieri
• white or yellow
• Acremonium strictum
• Actinomadura madurae
• Aspergillus nidulans
• Noetestudina rosatii
• Phaeoacremonium krajdenii
• Pseudallescheria boydii
• black
• Curvularia lunata Exophiala
• jeanselmei
• Leptosphaeria senegalensis
• Leptosphaeria tompkinsii
• Madurella grisea Madurella
• mycetomatis
• Pyrenochaeta romeroi
132. Diagnosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Diagnosis
• radiology, ultrasound or by fine needle
aspiration of the fluid with in an afflicted area
of the body.
133. Treatment
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Treatment
• surgery,
• ketoconazole,
• voriconazole,
• itraconazole and
• amputation of the affected limb.
• There is novaccinefor mycetoma.
134. References:
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
References:
• http://www.dermnetnz.org/pathology/mycet
oma-path.html
• http://www.dermnetnz.org/fungal/mycetoma
.html
• http://emedicine.medscape.com/article/2114
59-overview
• http://www.who.int/neglected_diseases/dise
ases/mycetoma/en/
• http://www.ncbi.nlm.nih.gov/pubmed/17007
542
135. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Coccidioidomycosis136.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://www.life-worldwide.org/assets/uploads/images/coccidioidomycosis-cutaneous.jpg
137. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
• is caused by Coccidioides immitis, a soilfungus native to the San Joaquin Valley of
California and by C posadasii, which is
endemic to certain arid-to-semiarid areas of
the southwestern United States, northern
portions of Mexico, and scattered areas in
Central America and South America. Although
genetically distinct, the 2 species are
morphologically identical.
138. Histology of coccidioidomycosis
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
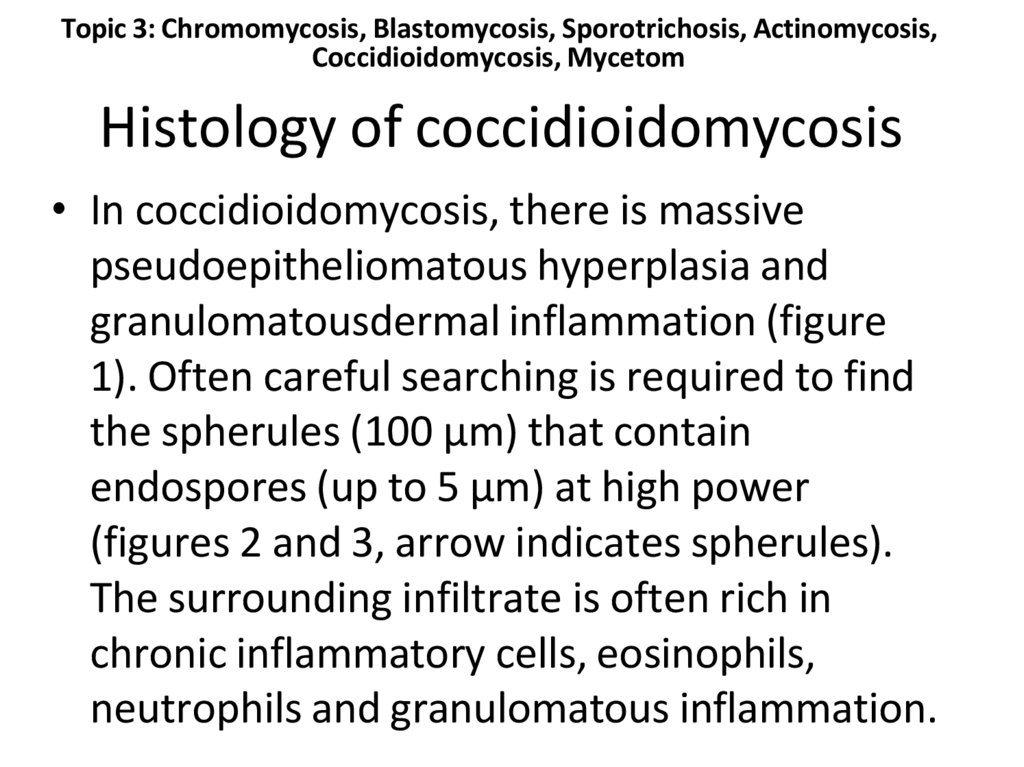
Histology of coccidioidomycosis
• In coccidioidomycosis, there is massive
pseudoepitheliomatous hyperplasia and
granulomatousdermal inflammation (figure
1). Often careful searching is required to find
the spherules (100 µm) that contain
endospores (up to 5 µm) at high power
(figures 2 and 3, arrow indicates spherules).
The surrounding infiltrate is often rich in
chronic inflammatory cells, eosinophils,
neutrophils and granulomatous inflammation.
139. Clinical aspects
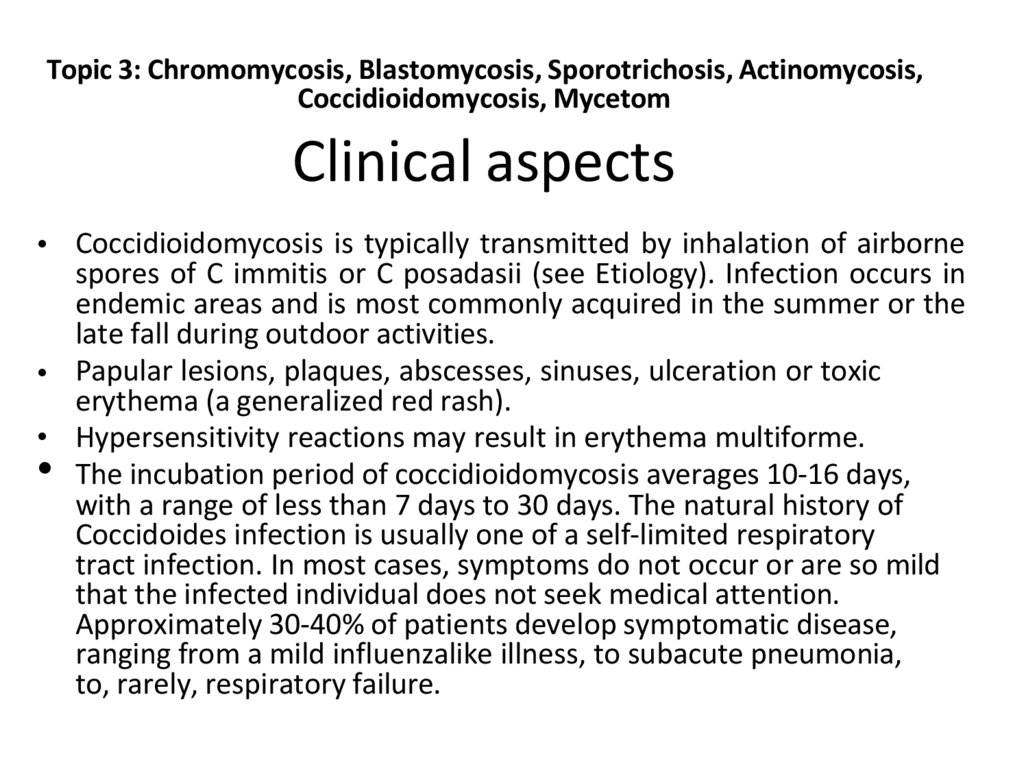
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Clinical aspects
• Coccidioidomycosis is typically transmitted by inhalation of airborne
spores of C immitis or C posadasii (see Etiology). Infection occurs in
endemic areas and is most commonly acquired in the summer or the
late fall during outdoor activities.
• Papular lesions, plaques, abscesses, sinuses, ulceration or toxic
erythema (a generalized red rash).
• Hypersensitivity reactions may result in erythema multiforme.
• The incubation period of coccidioidomycosis averages 10-16 days,
with a range of less than 7 days to 30 days. The natural history of
Coccidoides infection is usually one of a self-limited respiratory
tract infection. In most cases, symptoms do not occur or are so mild
that the infected individual does not seek medical attention.
Approximately 30-40% of patients develop symptomatic disease,
ranging from a mild influenzalike illness, to subacute pneumonia,
to, rarely, respiratory failure.
140. Common symptoms of primary infection are nonspecific and include fever, cough, chest pain, fatigue, dyspnea, headache,
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
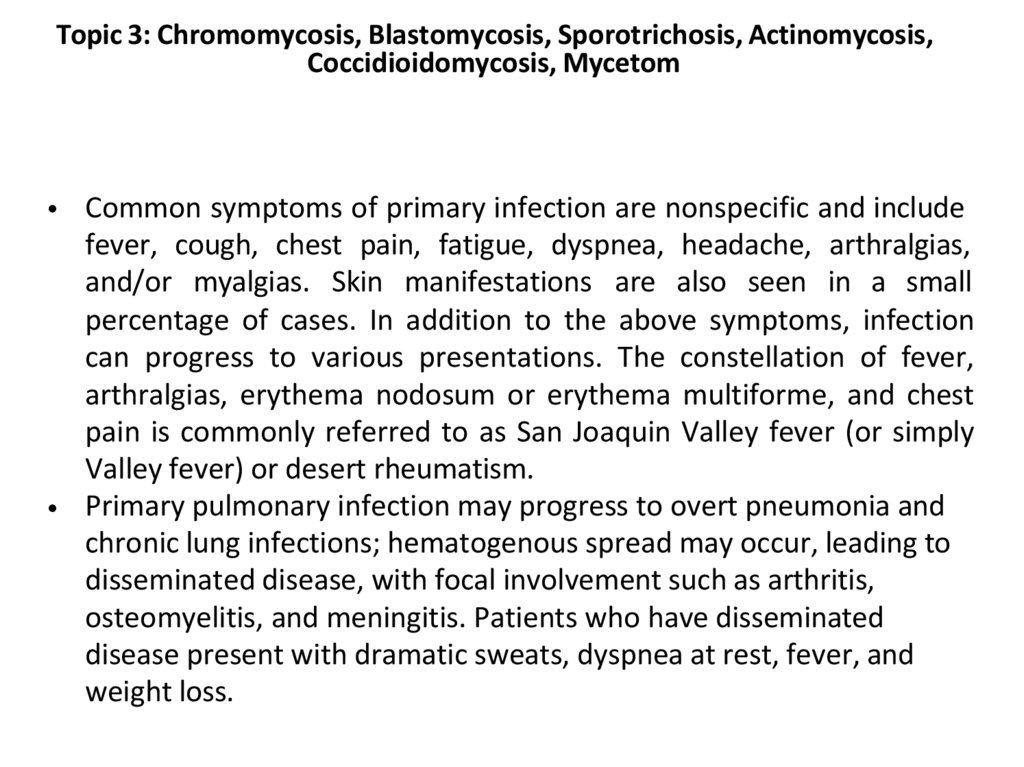
• Common symptoms of primary infection are nonspecific and include
fever, cough, chest pain, fatigue, dyspnea, headache, arthralgias,
and/or myalgias. Skin manifestations are also seen in a small
percentage of cases. In addition to the above symptoms, infection
can progress to various presentations. The constellation of fever,
arthralgias, erythema nodosum or erythema multiforme, and chest
pain is commonly referred to as San Joaquin Valley fever (or simply
Valley fever) or desert rheumatism.
• Primary pulmonary infection may progress to overt pneumonia and
chronic lung infections; hematogenous spread may occur, leading to
disseminated disease, with focal involvement such as arthritis,
osteomyelitis, and meningitis. Patients who have disseminated
disease present with dramatic sweats, dyspnea at rest, fever, and
weight loss.
141.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://dermline.ru/foto/c/4/coccidiomycosis-2-a-foto.jpg
142.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
http://farm3.staticflickr.com/2603/3679096437_e8c4b457f8_o.jpg
143. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
TreatmentLess than 5% of infected,usually immunocompromised, humans develop
a disease, and some mild asymptomatic cases often do not require any
treatment. Some patients with severe symptoms may warrrant antifungal therapy. There is a lack of prospective studies that examine
optimal anti-fungal therapy for coccidioidomycosis.
On the whole, oral fluconazole and intravenous amphotericin B are
used in progressive or disseminated disease, or in which patients are
immunocompromised. Alternatively, itraconazole or ketoconazole may
be used. Fluconazole is preferred drug for coccidioidal meningitis, due
to its penetration into CSF. Intrathecal or intraventricular amphotericin
B therapy is used if infection persists after fluconazole treatment.
Itraconazole is used for cases that involve treatment of infected
patient's bones and joints. Posaconazole and voriconazole have also
been employed.
144. References:
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
References:
• http://www.cdc.gov/fungal/coccidioidomycosis/
• http://emedicine.medscape.com/article/215978-overview
• http://www.nlm.nih.gov/medlineplus/ency/article/001322.
htm
• http://www.doctorfungus.org/aboutdrf/legal_pop.php?url
=http%3A//www.doctorfungus.org/mycoses/human/cocci/
coccidioidomycosis.php
• http://www.cdph.ca.gov/healthinfo/discond/Pages/Coccidi
oidomycosis.aspx
• http://www.healthcentral.com/encyclopedia/408/147.html
• http://cid.oxfordjournals.org/content/41/9/1217.long
145. Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis, Coccidioidomycosis, Mycetom
Whatis the primary mode of infection forchromoblastomycosis?
A)
Inhalation of fungal spores
B)
Traumatic inoculation of dematiaceous fungi through minor skin injuries
C)
Contagion through direct contact with an infected person
D)
Ingestion of contaminated food or water
146.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Which of the following is a common clinical
presentation of
chromoblastomycosis?
A.
Single, painful ulcer on the face
B.
Raised, crusted lesions on the limbs
C.
Multiple, itchy papules on the trunk
D.
Vesicular rash on the hands and
147. What is the typical mode of infection for sporotrichosis?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
What is the typical mode of infection for
sporotrichosis?
A.
B.
Inhalation of fungal spores
Traumatic inoculation through minor skin injuries, often from plants
C.
Direct contact with an infected animal
D.
Ingestion of contaminated
148. What is the primary cause of mycetoma?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
What is the primary cause of
mycetoma?
A)
Bacterial infection
B)
Fungal infection
C)
Parasitic infection
D)
Viral infection
149. Which of the following is a characteristic feature of actinomycosis?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Which of the following is a characteristic
feature of
actinomycosis?
B.
of granulomatous lesions
Presence of sulfur granules in tissue
C.
Infection primarily through inhalation
D.
Commonly affects the gastrointestinal tract
A.
Formation
150. Which of the following fungi is commonly associated with chromoblastomycosis?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Which of the following fungi is commonly
associated with
chromoblastomycosis?
A)
Fonsecaea pedrosoi
B)
Blastomyces dermatitidis
C)
Sporothrix schenckii
D)
Coccidioides immitis
151. How is coccidioidomycosis typically acquired?
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
How is coccidioidomycosis typically
acquired?
A)
Through direct contact with an infected person
B)
By ingestion of contaminated food or water
C)
By inhalation of fungal spores
D)
Through traumatic inoculation of fungal spores
152.
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
What is the typical clinical presentation of
sporotrichosis?
B)
A single lesion at the site of inoculation that may spread along lymphatic
channels
Multiple lesions scattered over the body
C)
A systemic infection with fever and chills
D)
A localized abscess
A)
153. Task 1
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Task 1
A 48-year-old forestry worker from a rural area near the Mississippi River Valley presents
with a 4-week history of cough with thick sputum, low-grade fever, chills, night sweats,
fatigue, and weight loss. He has a verrucous skin lesion on his forearm and crackles in the
right lung on exam. Chest X-ray shows right lower lobe consolidation and a cavitary lesion.
Skin biopsy reveals budding yeast forms, confirming blastomycosis. He is started on oral
itraconazole.
Diagnosis: Blastomycosis
154. Task 2
Topic 3: Chromomycosis, Blastomycosis, Sporotrichosis, Actinomycosis,Coccidioidomycosis, Mycetom
Task 2
A 48-year-old forestry worker from a rural area near the Mississippi River Valley presents
with a 4-week history of cough with thick sputum, low-grade fever, chills, night sweats,
fatigue, and weight loss. He has a verrucous skin lesion on his forearm and crackles in the
right lung on exam. Chest X-ray shows right lower lobe consolidation and a cavitary lesion.
Skin biopsy reveals budding yeast forms, confirming blastomycosis. He is started on oral
itraconazole.
Diagnosis: Blastomycosis
155. Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
156. Tropical Pyoderma
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Tropical Pyoderma
• Pyoderma means any skin disease that is pyogenic.
• These include superficial bacterial infections such
as impetigo, impetigo
contagiosa, ecthyma, folliculitis, Bockhart's
impetigo, furuncle, carbuncle, tropical ulcer, etc.
• Autoimmune conditions include pyoderma
gangrenosum.
• Pyoderma affects more than 111 million children
worldwide, making it one of the three most common
skin disorders in children along with scabies and tinea.
157. Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
Tropical ulcer158. Tropical ulcer
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Tropical ulcer
• Tropical ulcer (also known as Aden
ulcer, Junglerot, Malabar ulcer, and Tropical
phagedena) is a lesion occurring in cutaneous
leishmaniasis.
159.
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers,gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
http://itg.contente.eu/Generated/pubx/173/mm_files/do_3094/co_68239/CD_1059_060c.jpg
160. Tropical ulcer
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Tropical ulcer
• It is caused by a variety of microorganisms,
including my cobacteria.
• It is common in tropical climates.
• Ulcers occur on exposed parts of the body,
primarily on anterolateral aspect of the lower
limbs and may erode muscles and tendons, and
sometimes, the bones.
•These lesions may frequently develop on
preexisting abrasions or sores sometimes
beginning from a mere scratch.
161. Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
Pyoderma Gangrenosum162. Pyoderma Gangrenosum
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Pyoderma Gangrenosum
• Pyoderma gangrenosum is a condition that
causes tissue to become necrotic, causing
deep ulcers that usually occur on the legs.
• When they occur, they can lead to chronic
wounds.
• Ulcers usually initially look like small bug bites
or papules, and they progress to larger ulcers.
• Though the wounds rarely lead to death, they
can cause pain and scarring.
163.
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers,gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
http://upload.wikimedia.org/wikipedia/commons/1/12/Crohnie_Pyoderma_gangrenosum.jpg
164. Pyoderma Gangrenosum
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Pyoderma Gangrenosum
• The disease was identified in 1930. It affects
approximately 1 person in 100,000 in the
population.
• Equal sex distribution
• Common in middle-aged adults (30-50yr)
• About 5% affects children
165.
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers,gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
http://upload.wikimedia.org/wikipedia/commons/f/f1/Pyoderma_gangrenosum_01.jpg
166. Clinical Manifestations
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical Manifestations
• Anatomic sites –primarily legs, but can occur anywhere
–Abdomen, breast, buttucks, arms
Single or multiple lesions
Skin lesions arise suddenly as painful, erythematous, and tender papules,
pustules, vesicles,or fluctuant nodules Rapid progression to expanding
ulcers with sharply
demarcated, livid borders and a necrotic base
Ulcer edge often undermined (worn and ragged)
Surrounding skin –erythematous and indurated
167. Clinical Manifestations
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical Manifestations
•Koebner's phenomenon (also called the isomorphic
response)
–The appearance of a skin lesion as a result of
trauma
•Pathergy
– Exaggerated, uncontrolled, inflammatory response
toa nonspecific stimulus
•Lesions develop at site of minor trauma in 25-50%
– Surgery or debridement contraindicated
168. Clinical Manifestations
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical Manifestations
• Patients appear systemically unwell
–Fever, malaise, arthralgias, myalgias
Lesions often severely painful
Ulcerative PG (classic form)
Peristomal PG
– Occurs close to abdominal stomas
– Associated with inflammatory bowel disease; malignancy
169. Clinical Manifestations
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical Manifestations
• Pustular PG
– Rare, process halts at pustule stage and does not
evolve into ulcers
• Bullous PG
– Arms and face usually; painful bulla progress to
ulceration
– Associated with hematological conditions;
leukemia
• Vegetative PG
– Less aggressive, but chronic; responds to local tx
170. Differential Diagnosis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixedpyoderma, necrotizing fascitis).
Differential Diagnosis
• Bacterial Infections (including mycobacteria)
• Fungal Infections
• Chronic ulcerative HSV
• Vasculitis
• Insect reaction (i.e. brown recluse spider bite)
• Malignancy– sqamouscell, cutaneouslymphoma
• Antiphospholipid syndrome
• Systemic Conditions –SLE, RA, Behcet’s,
Wegener’s
171. Diagnosis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixedpyoderma, necrotizing fascitis).
Diagnosis
•Diagnosis of Exclusion
•Diagnosis based on clinical presentation
•and course Biopsy may help with
•diagnosis BUT
NO findings on pathologic specimens or
•laboratory evaluation that are
pathognomic for PG
•Biopsy helps to EXCLUDE malignancy,
infections, cutaneous vasculitis
Up to 10% of patients diagnosed
with PG are misdiagnosed
172. Diagnosis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Diagnosis
• Case Series (18 patients)
–Diagnostic Criteria
– Clinical features of PG
– Histopathological examination consistent with PG
– Exclusion of other dermatoses that may mimic PG
– Laboratory evaluation
– CBC, chemistries, syphilis
– serologies, immunoelectropheresis, ANA, RF, hepatitis
– serologies, HIV serology, antiphospholipid antibodies,
– ANCA
–Other investigations –CXR, BM biopsy, additional imaging
173. Associated Conditions
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixedpyoderma, necrotizing fascitis).
Associated Conditions
• 50-70% of patients have an associated systemic disease
• Onset of PG may precede, coincide, or follow that of systemic disease
• Inflammatory Bowel Disease
– 30% of patients with PG have Crohn’s or UC
– 2% of patients with IBD will have PG
RA (25% patients)
Malignancy
Other rheumatological and hematologic diseases
Hereditary hypoglobulinemia
HIV
Sarcoidosis
174. Treatment
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixedpyoderma, necrotizing fascitis).
Treatment
• Goals
– Suppression of inflammatory disease activity
– Promotion of wound healing
– Treatment of underlying associated conditions
– Control ofpain
Systemic Corticosteroids
Cyclosporin
Initial response –usually rapid; progression stops
– 60-80mg prednisone daily (up to 100-120mg)
• Resolution –very slow resolution of existing lesions
175. Treatment
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Treatment
• Infliximab (anti-TNFalpha monoclonal Ab)
–PG associated with inflammatory bowel disease
IVIG –effective in certain case reports Others
– Thalidomide
– Cellcept
– Tacrolimus
– Dapsone
– Azathioprine
176. Clinical Outcomes
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical Outcomes
•Case Series (18 patients)
–Complete remission in 83%; mean
duration to
remission 1.3yr
• –Persistent disease in 3/18; mean
duration 8yr
•Severity of systemic disease –prognostic
value in course of PG
Successful tx of associated condition
leads to improvement or remission of
PG
177. Tips
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixedpyoderma, necrotizing fascitis).
Tips
• Can occur on any skin surface
• Consider PG when any ulcer or surgical wound
fails to heal
• Develops rapidly–small lesions progresses to
crater in 24-48 hrs
• Lesions usually very painful
• Often presents with systemic illness (fever)
178. Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
Necrotizing fasciitis179. Necrotizing fasciitis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Necrotizing fasciitis
• Necrotizing fasciitis or NF, commonly known
as flesh-eating disease or flesh-eating
bacteria syndrome,is a rare infection of the
deeper layers of skin and subcutaneous
tissues, easily spreading across
the fascial plane with in the subcutaneous
tissue.
180.
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers,gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
http://upload.wikimedia.org/wikipedia/commons/6/6a/Necrotizing_fasciitis_left_leg.JPEG
181. Necrotizing fasciitis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Necrotizing fasciitis
• Necrotizing fasciitis progresses rapidly, having
greater risk of developing in the
immunocompromised due to conditions such as
diabetes or cancer.
• It is a severe disease of sudden onset and is
usually treated immediately with
surgical debridement and high doses of
intravenous antibiotics, with delay in surgical
treatment being associated with higher mortality.
182. Necrotizing fasciitis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma,mixed pyoderma, necrotizing fascitis).
Necrotizing fasciitis
• Many types of bacteria can cause necrotizing fasciitis
(e.g., Group A streptococcus (Streptococcus
pyogenes), Staphylococcus aureus, Clostridium
perfringens,Bacteroides fragilis,Aeromonas
hydrophila).
• The disease is classified as Type I (polymicrobial, due to
a number of different organisms) or Type II
(monomicrobial, due to a single infecting organism).
• The majority of cases of necrotizing fasciitis are
polymicrobial, with only 15% of cases being Type II
183. Necrotizing fasciitis
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma,mixed pyoderma, necrotizing fascitis).
Necrotizing fasciitis
• Such infections are more likely to occur in people
with compromised immune systems secondary to
chronic disease.
• Historically, most cases of Type II infections have
been due to group A streptococcus and
staphylococcal species.
• However, since as early as 2001, another serious
form of monomicrobial necrotizing fasciitis has
been observed with increasing frequency, caused
by methicillin-resistantStaphylococcus
aureus (MRSA).
184. References
• Bhat RM “Management of pyoderma gangrenosum –An update”Indian J DermatolVenereolLeprol(2004)
70: 329-335.
• Brooklyn T, Dunnill G, Probert C “Diagnosis and
treatment of pyoderma gangrenosum” BMJ (2006)
333: 181-184.
• Hasselmann DO, Bens G, Tilgen W, Reichrath J
“Pyoderma gangrenosum: Clinical presentation and
outcome in 18 cases and review of the literature” JDDG
(2007) 5: 560-564.
• Moschella SL “Neutrophilic dermatoses” Up-To-Date.
185. Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenous pyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following conditions is characterized by the presence of multipleinterconnected abscesses that form a larger mass, often in areas such as the
axillae or groin?
A) Deep folliculitis
B) Furuncle
C)Carbuncle
D)Hidradenitis suppurativa
186. What is the primary causative organism associated with furuncles (boils)?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
What is the primary causative organism associated with furuncles
(boils)?
A) Staphylococcus aureus
B) Streptococcus pyogenes
C) Pseudomonas aeruginosa
D)Escherichia coli
187. In which condition do you typically find inflamed hair follicles that may progress to form painful nodules or pustules?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
In which condition do you typically find inflamed hair follicles that
may progress to form painful nodules or pustules?
A) Sycosis
B) Carbuncle
C) Hidradenitis suppurativa
D) Deep folliculitis
188. Sycosis is primarily associated with inflammation of which of the following?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Sycosis is primarily associated with inflammation of which of the
following?
A) Apocrine glands
B) Sebaceous glands
C) Hair follicles
D) Sweat glands
189. Which of the following is a common treatment option for a carbuncle?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following is a common treatment option for a
carbuncle?
A) Topical antifungals
B) Oral antibiotics
C) Corticosteroid injections
D)Cryotherapy
190. Clinical situation
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical situation
Patient G., 18 years complains of skin rash on the trunk.
Anamnesis: the patient is going in for sports, particularly athletics.
Objectively:
*There are circumscribed follicular pustules
*millet grain or pin head in size,
*found in the centre of the hair follicle and surrounded by a narrow hyperaemic band of acute
inflammation.
*Localization: the skin of the trunk, the hands and the legs
1. Put the diagnosis.
2. Treatment (systemic and external)
Answers
1. Bacterial folliculitis
2. antibiotics ,topical steoroids,antiseptic washes,antifungal treatment
191. Which of the following is a common treatment option for a carbuncle?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following is a common treatment option for a
carbuncle?
A) Topical antifungals
B) Oral antibiotics
C) Corticosteroid injections
D) Cryotherapy
192. Which of the following is a characteristic feature of pyoderma?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following is a characteristic feature of pyoderma?
A) Vesicular lesions
B) Pustular lesions
C) Bullous lesions
D) Nodular lesions
193. What is the most important step in the treatment of necrotizing fasciitis of pyoderma?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
What is the most important step in the treatment of necrotizing
fasciitis of pyoderma?
A) Administering antibiotics
B) Performing surgical debridement
C) Providing supportive care
D) All of the above
194. Which of the following is a potential complication of gangrenous pyoderma?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following is a potential complication of gangrenous
pyoderma?
A) Sepsis
B) Organ failure
C) Amputation
D) All of the above
195. Which of the following is a characteristic feature of mixed pyoderma?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following is a characteristic feature of mixed
pyoderma?
A) Presence of a single type of bacteria
B) Presence of multiple types of bacteria
C) Presence of fungi
D) Presence of viruses
196. Which of the following bacteria are commonly associated with mixed pyoderma?
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Which of the following bacteria are commonly associated with
mixed pyoderma?
A) Staphylococcus aureus and Streptococcus pyogenes
B) Escherichia coli and Klebsiella pneumoniae
C) Pseudomonas aeruginosa and Enterobacter cloacae
D) All of the above
197. Clinical situation
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical situation
Patient G., 18 years complains of skin rash on the trunk.
Anamnesis: the patient is going in for sports, particularly athletics.
Objectively:
* There are circumscribed follicular pustules
* millet grain or pin head in size,
* found in the centre of the hair follicle and surrounded by a narrow hyperaemic band of acute
inflammation.
* Localization: the skin of the trunk, the hands and the legs
1. Put the diagnosis.
2. Treatment (systemic and external)
Answers
1. Bacterial folliculitis
2. antibiotics ,topical steoroids,antiseptic washes,antifungal treatment
198. Clinical situation A10-year-old boy presents to the clinic with a 2-week history of painful, itchy, and swollen lesions on his
Topic 5: Topical pyoderma ( Madagascar's noma, tropical ulcers, gangrenouspyoderma, mixed pyoderma, necrotizing fascitis).
Clinical situation
A10-year-old boy presents to the clinic with a 2-week history of painful, itchy, and
swollen lesions on his legs and feet. The lesions started as small, red bumps and have
since progressed to form large, crusted ulcers. The boy lives in a rural area with poor
sanitation and hygiene. He has been playing barefoot in the nearby fields and forests.
Physical Examination:
- Multiple large, crusted ulcers on the legs and feet
- Lesions are painful, itchy, and swollen
- Surrounding skin is erythematous and warm to the touch
- Lymph nodes in the groin are tender and enlarged
Laboratory Results:
- Complete Blood Count (CBC): elevated white blood cell count
- Skin scrapings: presence of neutrophils and bacteria
Question:
What is the most likely diagnosis?
Tropical pyoderma (also known as tropical ulcer or jungle sore)