Похожие презентации:
Morphological analysis for health care systems planning
1.
MORPHOLOGICAL ANALYSIS FOR HEALTHCARE SYSTEMS PLANNING
RICHARD E. TUBLEY, WILLIAM C. RICHARDSON* and JAMES V. HANSENt
Departmentof Mechanical Engineering, University of Utah, Salt Lake City, Utah, U.S.A.
(Receiued 16April 1974)
Abstract-Health care planners are continually challenged by the difficulty of ordering and understanding of the
complexities of health care delivery systems. Methods are needed which can aid in extending thought processes into
multi-dimensional solution space and rationalizing the thinking of various health care interests. This paper describes
a useful approach to designing and evaluating health care systems utilizing a case study of a large metropolitan
community.
represented as a horizontal relevance tree. The vertical
axis enumerates individual parts or functions of the
system. The horizontal axis describes the available and
anticipitated subdimensions.
Morphological analysis may be applied at nearly any
level of aggregation. It may, for example, be used to
investigate alternative methods of designing a public
health system, a preventive care program, or a health
maintenance organization (HMO). The approach is
basically the same for each of these objectives.
An important advantage of the morphological method is
its formal approach to discovering and examining solution
alternatives. It forces the planner to work systematically
from “morphological space”, which reflects the known,
into nearby space, which is not known. A typical
procedure is to vary the parameters of the initial
conhguration one at a time keeping the others fixed as the
examination moves into the unknown region[5].
Another advantage of this technique centers on its total
enumeration approach. It provides a means of examining
all possible configurations which may be appropriate to a
given objective. This process often reveals gaps in
required services (or technology) and forces the analyst to
include alternatives which might otherwise be overlooked
or summarily dismissed as being infeasible. Under closer
examination, combinations having the superficial appearance of absurdity may turn out to be viable alternativesor they may suggest modifications which will promote
viability. Zwicky, for example, ultimately identified or
invented fourteen new telescope designs as the result of
preparing a lecture on the morphological method applied
to telescope design[3].
There are, of course, limitations to the morphological
method. One is that it is limited to existing technologiesalthough it can prove valuable in pointing up areas of
needed technologies. Another constraint is that the
analysts must have a thorough knowledge of the field to
which it is being applied. The use of a team of experts can
generally improve the quality and completeness of
solution alternatives.
The first step in constructing the morphological space is
to formulate the problem to be investigated. The narrower
the scope of problem definition, the less complex will be
the subsequent analysis. The second step is to select the
dimensions upon which the attainment of the objective
depends. Next, elements which represent alternatives at
each level are identified as entries or vertices of the tree.
The fourth step is to establish sets of criteria for each of
the levels. Finally, applications of methods drawn from
Health care planners are frequently confronted with the
problem of assessing current system effectiveness, and
developing and evaluating alternatives for meeting health
care needs. This is a particularly difficult task as modern
day health care has become a highly complex system
having numerous components whose relationships are not
generally well understood[l]. Further, major changes in
the arrangements for the delivery of personal health
services have been occurring in recent years, and many
policy questions have arisen as a consequence. Several
substantive problem areas appear to be of particular
concern in the present process of public policy reformulation. These problems include: the types of care rendered
and its continuity, the evenness of access opportunities
across various segments of the population, the utilization
of scarce manpower, and finally, the structuring and
consequences of existing incentives within the health
field. Because proposed solutions within any of these
areas impact other problem areas in complex ways,
increasing attention has been focused on development
and evaluation of diverse health care delivery modes[2].
In order to cope with the need for innovation in the face
of increasing complexity, methods need to be developed
and applied which can upgrade our ability to extend our
thinking into multi-dimensional solution space.
MORPHOLOGICAL ANALYSIS
One approach which can facilitate this type of thinking
is morphological analysis. This methodology, formulated
more than two decades ago by Fritz Zwicky [3,4] has not
received wide attention despite his efforts to promote its
application to technological and social problems. The
general objective of morphological analysis is to visualize
all possible solutions to any given problem and to point
the way toward the general performance evaluation of
these solutions. The methodology is based on graph
theory with the morphological space representing a graph
consisting of dimensions which are sets of nodes
representing parameters. If the morphological space
consists of two dimensions it may be expressed as- a
matrix. If it consists of three dimensions it may be
expressed as a box. An n-dimensional space is best
*School of Public Health and Community Medicine, University
of Washington U.S.A.
TPacbic Northwest Laboratories, Battelle Memorial Institute
Richland, Washington 99352,U.S.A.
83
2.
RICHARDE. TURLEY, WILLIAMC. RICHARDSON
and JAMESV. HANSEN
a4
systems analysis and operations research may be utilized
to order the analysis into a logical framework.
A MORPHOLOGY
OF HEALTH CARE DELIYERY
The authors were recently engaged in a study of health
care delivery in a large metropolitan community with the
objectives of assessing the current system’s effectiveness
and developing and evaluating alternatives for meeting
community health care needs. The impetus for this
research derived from a group of concerned community
health care providers who felt that unmet health care
needs existed in the community and that its health care
resources could be utilized more effectively.
Subsequent investigations supported this concern. In
particular, it was determined that a double standard of
health care was being perpetuated in the community. The
individual or family adequately insured or able to pay for
health care was able to exercise freedom in choosing a
provider. Freedom of choice for the poor was, however,
greatly limited. As a consequence, the poor felt rejected
by the county system of health care. While access to the
nongovernmental system was restricted, the poor were
concerned that even if barriers to access were removed
there would be no assurance that they would receive the
same level of treatment and consideration as the
non-poor.
Preliminary analysis suggested that much of the
problem could be eliminated if a means could be found to
pay providers adequately for their services, while at the
same time encouraging
the establishment
of
patient-physician relationships between the poor and
primary care practitioners. This prompted the need for a
framework for thinking about the problem which would
enhance the prospects for developing a sound solutionone which would (1) be operationally feasible, (2) meet the
unsatisfied health care needs of the cornunity, and (3)
receive support from community providers and recipients
of health care, as well as government agencies and the
community at large.
It was clearly evident that in order to promote
development of such a solution there was need for an
approach which would: (1) minimize the possibility of
overlooking an important combination of system dimensions; and (2) help in organizing and directing the thinking
of community health care providers, as well as those
whose cooperation would be necessary for any concept to
be successfully implemented. Morphological analysis
appeared to offer a framework which would facilitate
meeting this need.
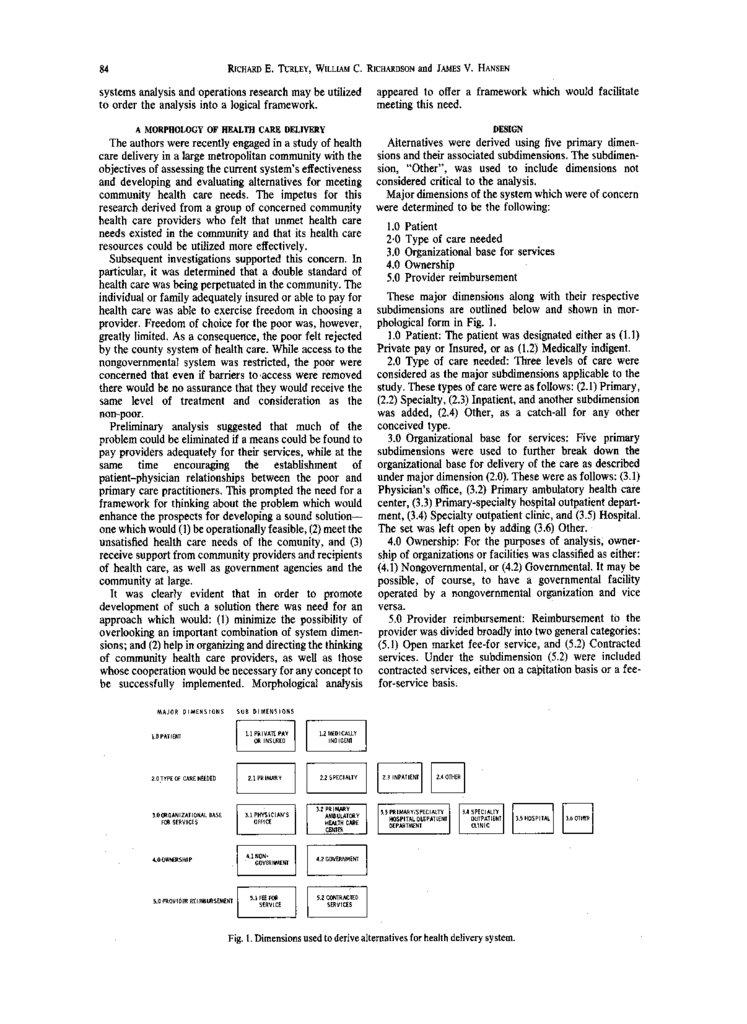
DESIGN
Alternatives were derived using five primary dimensions and their associated subdimensions. The subdimension, “Other”, was used to include dimensions not
considered critical to the analysis.
Major dimensions of the system which were of concern
were determined to be the following:
1.O Patient
2.0 Type of care needed
3.0 Organizational base for services
4.0 Ownership
5.0 Provider reimbursement
These major dimensions along with their respective
subdimensions are outlined below and shown in morphological form in Fig. 1.
1.0 Patient: The patient was designated either as (1.1)
Private pay or Insured, or as (1.2) Medically indigent.
2.0 Type of care needed: Three levels of care were
considered as the major subdimensions applicable to the
study. These types of care were as follows: (2.1) Primary,
(2.2) Specialty, (2.3) Inpatient, and another subdimension
was added, (2.4) Other, as a catch-all for any other
conceived type.
3.0 Organizational base for services: Five primary
subdimensions were used to further break down the
organizational base for delivery of the care as described
under major dimension (2.0). These were as follows: (3.1)
Physician’s office, (3.2) Primary ambulatory health care
center, (3.3) Primary-specialty hospital outpatient department, (3.4) Specialty outpatient clinic, and (3.5) Hospital.
The set was left open by adding (3.6) Other.
4.0 Ownership: For the purposes of analysis, ownership of organizations or facilities was classified as either:
(4.1) Nongovernmental, or (4.2) Governmental. It may be
possible, of course, to have a governmental facility
operated by a nongovernmental organization and vice
versa.
5.0 Provider reimbursement: Reimbursement to the
provider was divided broadly into two general categories:
(5.1) Open market fee-for service, and (5.2) Contracted
services. Under the subdimension (5.2) were included
contracted services, either on a capitation basis or a feefor-service basis.
Fig. 1. Dimensions used to derive alternatives for health delivery system.
3.
Morphologicalanalysisfor healthcare systemsplanningSELECTEDSYSTEMALTERNATIVES
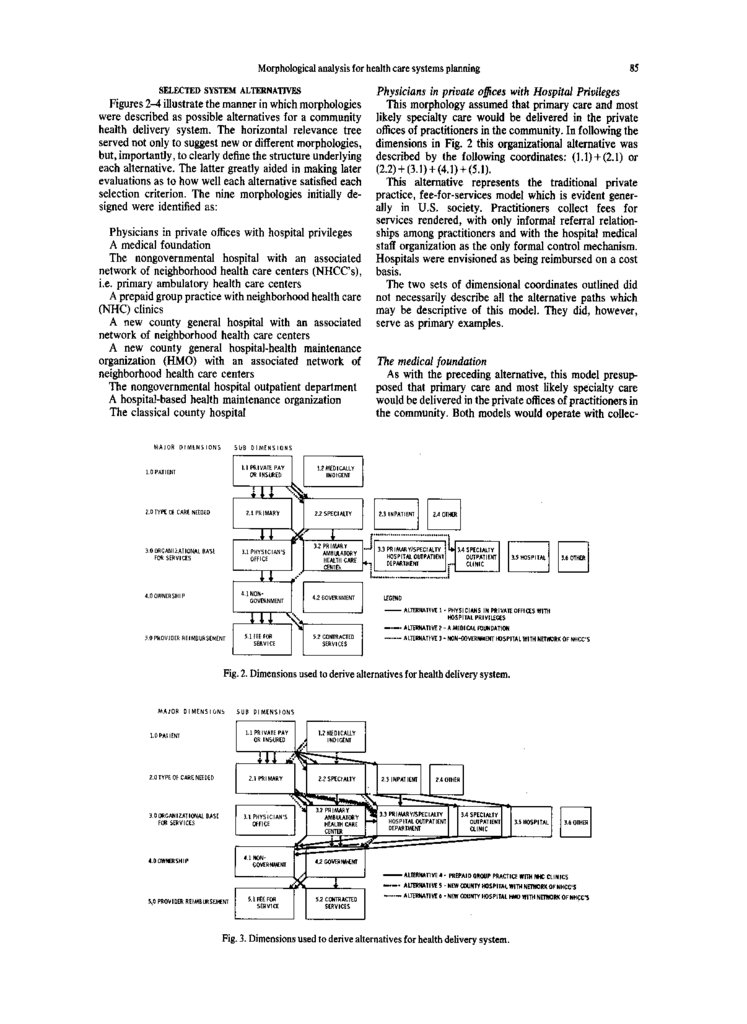
Figures 2-4 illustrate the manner in which morphologies
were described as possible alternatives for a community
health delivery system. The horizontal relevance tree
served not only to suggest new or different morphologies,
but, importantly, to clearly define the structure underlying
each alternative. The latter greatly aided in making later
evaluations as to how well each alternative satisfied each
selection criterion. The nine morphologies initially designed were identified as:
Physicians in private offices with hospital privileges
A medical foundation
The nongovernmental hospital with an associated
network of neighborhood health care centers (NHCC’s),
i.e. primary ambulatory health care centers
A prepaid group practice with neighborhood health care
(NHC) clinics
A new county general hospital with an associated
network of neighborhood health care centers
A new county general hospital-health maintenance
organization (HMO) with an associated network of
neighborhood health care centers
The nongovernmental hospital outpatient department
A hospital-based health maintenance organization
The classical county hospital
85
Physicians in private o&es with Hospital Privileges
This morphology assumed that primary care and most
likely specialty care would be delivered in the private
offices of practitioners in the community. In following the
dimensions in Fig. 2 this organizational alternative was
described by the following coordinates: (1.1)+ (2.1) or
(2.2)+(3.1)+(4.1)+(5.1).
This alternative represents the traditional private
practice, fee-for-services model which is evident generally in U.S. society. Practitioners collect fees for
services rendered, with only informal referral relationships among practitioners and with the hospital medical
staff organization as the only formal control mechanism.
Hospitals were envisioned as being reimbursed on a cost
basis.
The two sets of dimensional coordinates outlined did
not necessarily describe all the alternative paths which
may be descriptive of this model. They did, however,
serve as primary examples.
The medical foundation
As with the preceding alternative, this model presupposed that primary care and most likely specialty care
would be delivered in the private offices of practitioners in
the community. Both models would operate with collec-
4.0 OWNERSHIP
Fig. 2. Dimensionsusedto derivealternativesfor healthdeliverysystem.
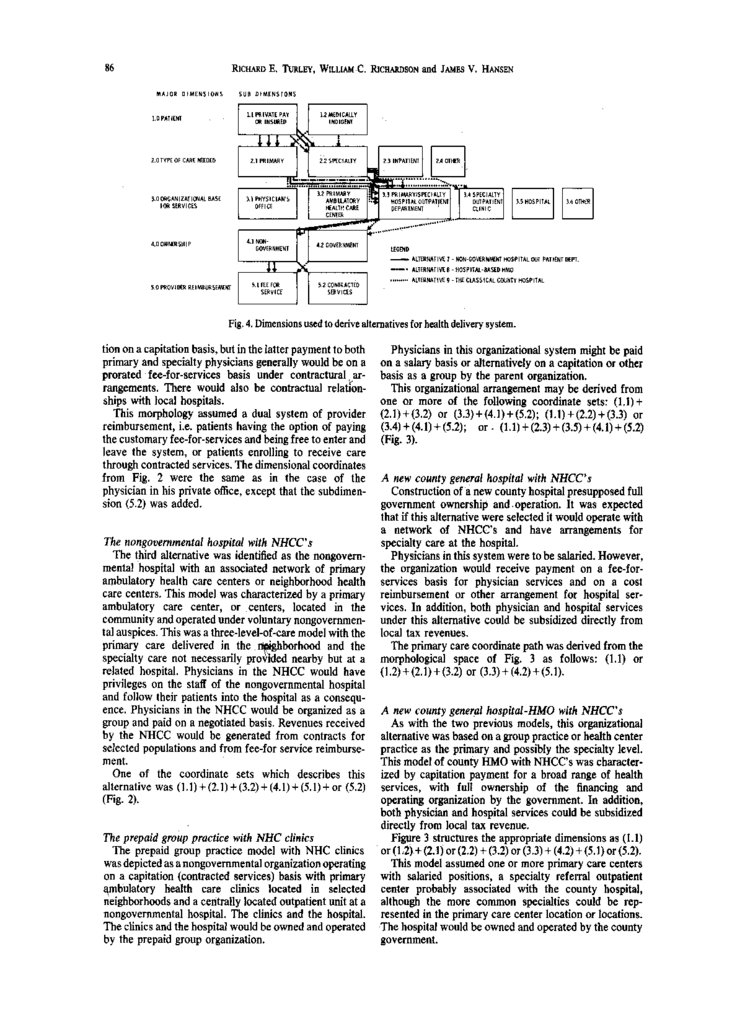
Fig. 3. Dimensionsused to derivealternativesfor healthdeliverysystem.
4.
86RICHARD
E. TURLEY,WILLIAM
C. RICHARDSON
and JAMES
V. HANSEN
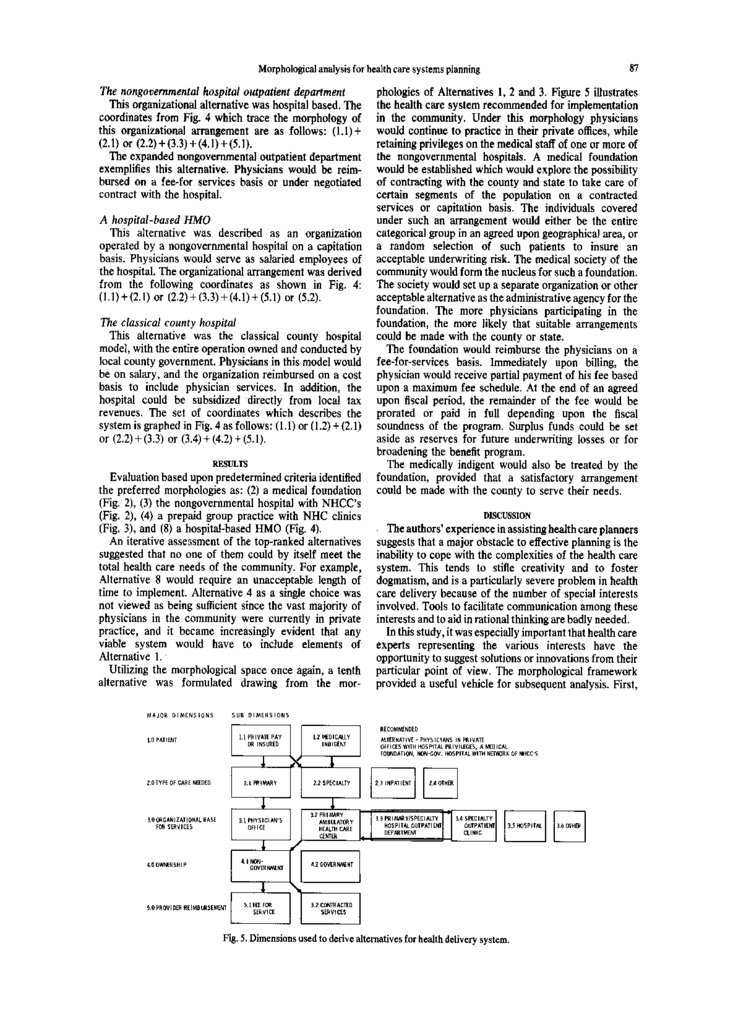
Fig.4. Dimensionsused to derivealternativesfor healthdeliverysystem.
tion on a capitation basis, but in the latter payment to both
primary and specialty physicians generally would be on a
prorated fee-for-services basis under contractural arrangements. There would also be contractual relatronships with local hospitals.
This morphology assumed a dual system of provider
reimbursement, i.e. patients having the option of paying
the customary fee-for-services and being free to enter and
leave the system, or patients enrolling to receive care
through contracted services. The dimensional coordinates
from Fig. 2 were the same as in the case of the
physician in his private office, except that the subdimension (5.2) was added.
The nongovernmental hospital with NHCC’s
The third alternative was identified as the nongovem-
mental hospital with an associated network of primary
ambulatory health care centers or neighborhood health
care centers. This model was characterized by a primary
ambulatory care center, or centers, located in the
community and operated under voluntary nongovernmental auspices. This was a three-level-of-care model with the
primary care delivered in the
* borhood and the
specialty care not necessarily prov
?Zh ed nearby but at a
related hospital. Physicians in the NHCC would have
privileges on the staff of the nongovernmental hospital
and follow their patients into the hospital as a consequence. Physicians in the NHCC would be organized as a
group and paid on a negotiated basis. Revenues received
by the NHCC would be generated from contracts for
selected populations and from fee-for service reimbursement.
One of the coordinate sets which describes this
alternative was (1.1)+(2.1)+(3.2)+(4.1)+(5.1)+or
(5.2)
(Fig. 2).
The prepaid group practice with NHC clinics
The prepaid group practice model with NHC clinics
was depicted as a nongovernmental organization operating
on a capitation (contracted services) basis with primary
ambulatory health care clinics located in selected
neighborhoods and a centrally located outpatient unit at a
nongovernmental hospital. The clinics and the hospital.
The clinics and the hospital would be owned and operated
by the prepaid group organization.
Physicians in this organizational system might be paid
on a salary basis or alternatively on a capitation or other
basis as a group by the parent organization.
This organizational arrangement may be derived from
one or more of the following coordinate sets: (1.1)+
(2.1)+(3.2) or (3.3)+(4.1)+(5.2); (l.l)t(2.2)+(3.3)
or
(3.4) + (4.1)t (5.2); or . (1.1)t (2.3) t (3.5) t (4.1) t (5.2)
(Fig. 3).
A new county general hospital with NHCC’s
Construction of a new county hospital presupposed full
government ownership and. operation. It was expected
that if this alternative were selected it would operate with
a network of NHCC’s and have arrangements for
specialty care at the hospital.
Physicians in this system were to be salaried. However,
the organization would receive payment on a fee-forservices basis for physician services and on a cost
reimbursement or other arrangement for hospital services. In addition, both physician and hospital services
under this alternative could be subsidized directly from
local tax revenues.
The primary care coordinate path was derived from the
morphological space of Fig. 3 as follows: (1.1) or
(1.2) t(2.1)+(3.2)
or (3.3)+(4.2)+(5.1).
A new county genecal hospital-HMO
with NHCC’s
As with the two previous models, this organizational
alternative was based on a group practice or health center
practice as the primary and possibly the specialty level.
This model of county HMO with NHCC’s was characterized by capitation payment for a broad range of health
services, with full ownership of the financing and
operating organization by the government. In addition,
both physician and hospital services could be subsidized
directly from local tax revenue.
Figure 3 structures the appropriate dimensions as (1.1)
or (1‘2)t (2.1) or (2.2) t (3.2) or (3.3) t (4.2) t (5.1) or (5.2).
This model assumed one or more primary care centers
with salaried positions, a specialty referral outpatient
center probably associated with the county hospital,
although the more common specialties could be represented in the primary care center location or locations.
The hospital would be owned and operated by the county
government.
5.
a7Morphological analysis for health care systems planning
The nongovernmental hospital outpatient department
This organizational alternative was hospital based. The
coordinates from Fig. 4 which trace the morphology of
this organizational arrangement are as follows: (l.l)t
(2.1) or (2.2) t (3.3) + (4.1) t (5.1).
The expanded nongovernmental outpatient department
exemplifies this alternative. Physicians would be reimbursed on a fee-for services basis or under negotiated
contract with the hospital.
A hospital-based HMO
This alternative was described as an organization
operated by a nongovernmental hospital on a capitation
basis. Physicians would serve as salaried employees of
the hospital. The organizational arrangement was derived
from the following coordinates as shown in Fig. 4:
(1.1) t (2.1) or (2.2)t (3.3)
t (4.1) t (5.1) or (5.2).
The classical county hospital
This alternative was the classical county hospital
model, with the entire operation owned and conducted by
local county government. Physicians in this model would
be on salary, and the organization reimbursed on a cost
basis to include physician services. In addition, the
hospital could be subsidized directly from local tax
revenues. The set of coordinates which describes the
system is graphed in Fig. 4 as follows: (1.1) or (1.2) t (2.1)
or (2.2)t (3.3) or (3.4) + (4.2) + (5.1).
RESULTS
Evaluation based upon predetermined criteria identified
the preferred morphologies as: (2) a medical foundation
(Fig. 2), (3) the nongovernmental hospital with NHCC’s
(Fig. 2), (4) a prepaid group practice with NHC clinics
(Fig. 3), and (8) a hospital-based HMO (Fig. 4).
An iterative assessment of the top-ranked alternatives
suggested that no one of them could by itself meet the
total health care needs of the community. For example,
Alternative 8 would require an unacceptable length of
time to implement. Alternative 4 as a single choice was
not viewed as being sufficient since the vast majority of
physicians in the community were currently in private
practice, and it became increasingly evident that any
viable system would have to include elements of
Alternative 1.
Utilizing the morphological space once again, a tenth
alternative was formulated drawing from the mor-
phologies of Alternatives 1, 2 and 3. Figure 5 illustrates
the health care system recommended for implementation
in the community. Under this morphology physicians
would continue to practice in their private offices, while
retaining privileges on the medical staff of one or more of
the nongovernmental hospitals. A medical foundation
would be established which would explore the possibility
of contracting with the county and state to take care of
certain segments of the population on a contracted
services or capitation basis. The individuals covered
under such an arrangement would either be the entire
categorical group in an agreed upon geographical area, or
a random selection of such patients to insure an
acceptable underwriting risk. The medical society of the
community would form the nucleus for such a foundation.
The society would set up a separate organization or other
acceptable alternative as the administrative agency for the
foundation. The more physicians participating in the
foundation, the more likely that suitable arrangements
could be made with the county or state.
The foundation would reimburse the physicians on a
fee-for-services basis. Immediately upon billing, the
physician would receive partial payment of his fee based
upon a maximum fee schedule. At the end of an agreed
upon fiscal period, the remainder of the fee would be
prorated or paid in full depending upon the fiscal
soundness of the program. Surplus funds could be set
aside as reserves for future underwriting losses or for
broadening the benefit program.
The medically indigent would also be treated by the
foundation, provided that a satisfactory arrangement
could be made with the county to serve their needs.
DISCUSSION
I The authors’ experience in assisting health care planners
suggests that a major obstacle to effective planning is the
inability to cope with the complexities of the health care
system. This tends to stifle creativity and to foster
dogmatism, and is a particularly severe problem in health
care delivery because of the number of special interests
involved. Tools to facilitate communication among these
interests and to aid in rational thinking are badly needed.
In this study, it was especially important that health care
experts representing the various interests have the
opportunity to suggest solutions or innovations from their
particular point of view. The morphological framework
provided a useful vehicle for subsequent analysis. First,
6.
88RICHARDE. TURLEY, WILLIAM
C. RICHARDSON
and JAMESV. HANSEN
the expert could readily determine whether all the
dimensions he perceived as being relevant were represented. Second, his suggestions for systems configurations could be quickly understood and analyzed by others.
Both of these processes stimulated rigorous discussions
which often produced new alternative structures.
It was another of the researchers’ objectives that no
important alternative be overlooked. While there is no
surety that this was accomplished, the range of alternatives considered (as well as modifications thereof) was
well beyond that which had been proposed initially.
Additionally, since the structure of each alternative
system was clearly defined, evaluations as to how well
each one satisfied the selection criteria was more easily
rationalized by the group. This was evidenced by several
preliminary evaluations which were unable to be supported under close examination of the structure and intent
of the particular alternative.
Finally, the numerous interations through the morphological graph generated the thinking which resulted in
the recommended alternative.
CONCLUSION
Many of the most pressing problems of our society lie
unsolved or partially solved because of our limited ability
to extend our thinking into a multidimensional solution
space. As a tool for stimulating ideas, morphological
analysis represents a useful approach to invention,
discovery, and innovation. Devices or ideas in a set
representing the state-of-the-art may be reduced to their
basic parameters and these parameters categorized to
establish the dimensions of morphological space. These
may, in turn, be expanded by adding other appropriate
parameters. The best combination of parameters may be
suggested through the application of elements of graph
theory and decision theory.
REFFBENCFS
1. William J. Horvath, The systems approach to the national
health problem, Mgmt Sci. 12, B391-B395(1966).
2. Richard E. Turley, William C. Richardson and James V.
Hansen, A morphological approach to designing and evaluating
health care systems. Proc. Fifth Nat. Meeting Am. Inst.
Decision Sci. (1973).
3. Fritz Zwicky, Discovery, Invention, Research. Macmillan, New
York (1%9).
4. A. G. Wilson and F. Zwicky, MorphologicalResearch. Springer,
New York (1967).
5. Robert U. Ayres, Technological Forecasting and Long-Range
Planning.McGraw-Hill,New York (1969).


 Медицина
Медицина








