Похожие презентации:
VUR, UTI and antibiotic prophylaxis. How to use an article about therapy or prevention
1. VUR, UTI, and Antibiotic Prophylaxis How to Use an Article About Therapy or Prevention
2. The Case
Kali is a 14mo female who presents to WRAMCED with fever to 102. Your stellar Peds Intern
suggests obtaining a UA/UCx, which results in
the diagnosis of acute pyelonephritis.
3. The Case
Kali is a 14mo female who presents to WRAMCED with fever to 102. Your stellar Peds Intern
suggests obtaining a UA/UCx, which results in
the diagnosis of acute pyelonephritis.
Kali is admitted to Wd51 for 48hrs of IV abx,
then, afebrile, discharged to complete po course.
4. The Case
Kali is a 14mo female who presents to WRAMCED with fever to 102. Your stellar Peds Intern
suggests obtaining a UA/UCx, which results in
the diagnosis of acute pyelonephritis.
Kali is admitted to Wd51 for 48hrs of IV abx,
then, afebrile, discharged to complete po course.
She undergoes renal US and VCUG 3 weeks
later, which reveal grade II VUR on the left.
5. The Question
Should we treat her prophylactically?Short-term:
Will this decrease recurrent infections?
Long-term:
Will this decrease renal scarring?
Why else would it matter?
6. Background
Vesicoureteral Reflux (VUR)Primary – congenital incompetence of VU valve
(shortened submucosal tunnel)
Secondary – multiple anatomic abnormalities
7. Background
Incidence 1-10%Siblings 30-45% (3/4 asymptomatic)
Diagnosed via VCUG
UTI workup – 40% (girls); 70% (infants <1yo)
Antenatal hydronephrosis – 9% (boys)
Why worry?
VUR pyelonephritis renal scarring
HTN, renal insufficiency, ESRD, pre-eclampsia
8. Background
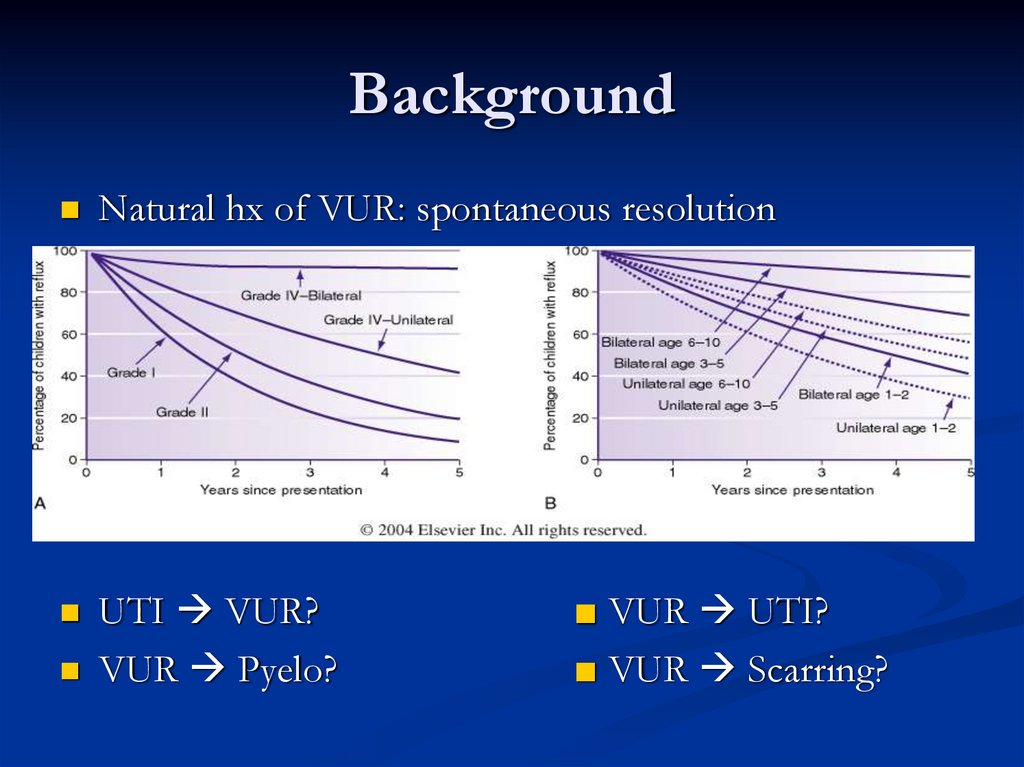
Natural hx of VUR: spontaneous resolutionUTI VUR?
VUR Pyelo?
■ VUR UTI?
■ VUR Scarring?
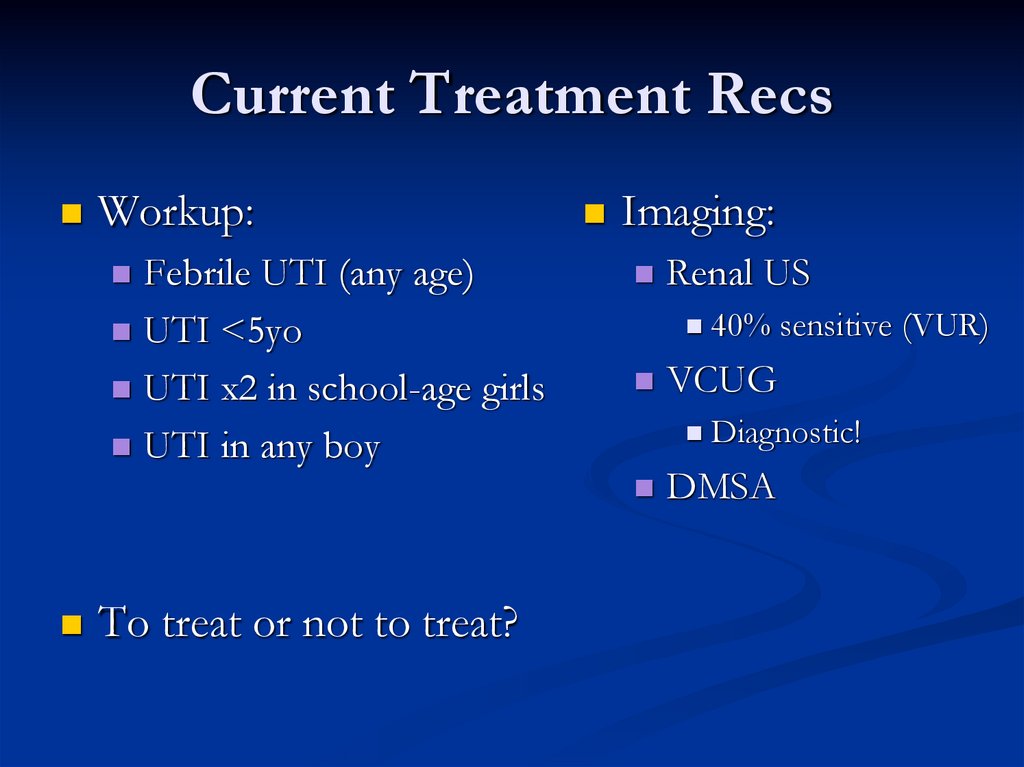
9. Current Treatment Recs
Workup:Febrile UTI (any age)
UTI <5yo
UTI x2 in school-age girls
UTI in any boy
Imaging:
To treat or not to treat?
40% sensitive (VUR)
VCUG
Renal US
Diagnostic!
DMSA
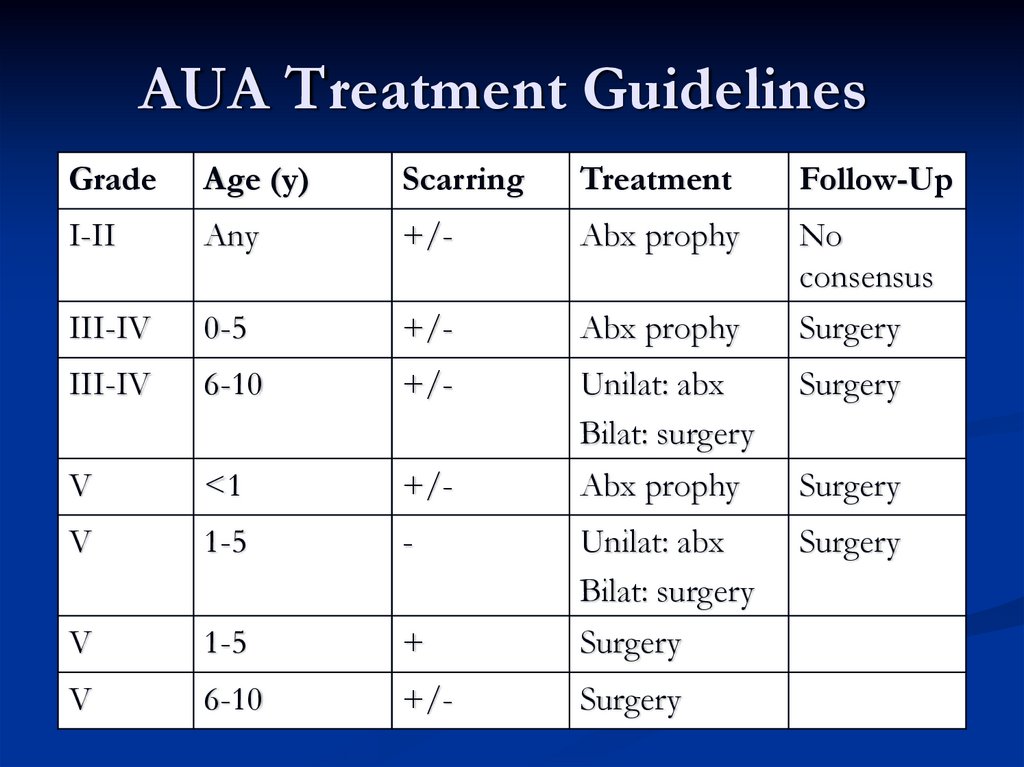
10. AUA Treatment Guidelines
GradeAge (y)
Scarring
Treatment
Follow-Up
I-II
Any
+/-
Abx prophy
III-IV
0-5
+/-
Abx prophy
No
consensus
Surgery
III-IV
6-10
+/-
Unilat: abx
Bilat: surgery
Surgery
V
<1
+/-
Abx prophy
Surgery
V
1-5
-
Unilat: abx
Bilat: surgery
Surgery
V
1-5
+
Surgery
V
6-10
+/-
Surgery
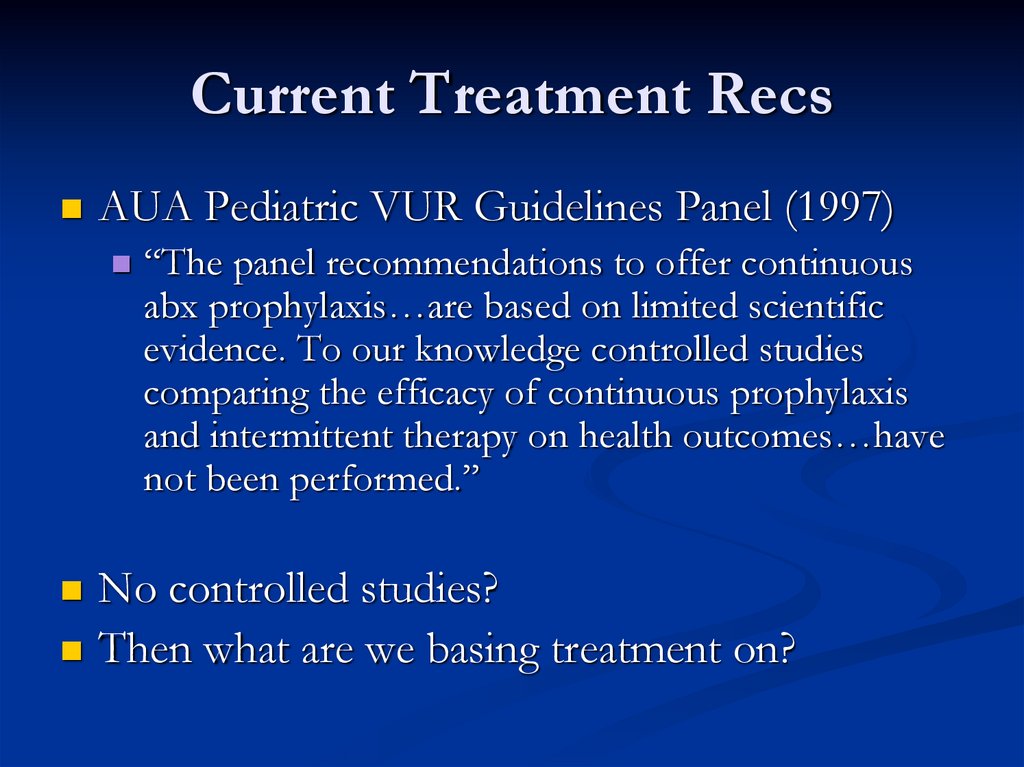
11. Current Treatment Recs
AUA Pediatric VUR Guidelines Panel (1997)“The panel recommendations to offer continuous
abx prophylaxis…are based on limited scientific
evidence. To our knowledge controlled studies
comparing the efficacy of continuous prophylaxis
and intermittent therapy on health outcomes…have
not been performed.”
No controlled studies?
Then what are we basing treatment on?
12. The State of the Art
Williams et.al. (2001)Systematic review of RCTs on UTI/abx prophy
Five trials, 1968-1978
Best 2: 71 patients total, normal anatomy, 92% girls
Garin et.al. (1998)
UTI VUR? no
VUR UTI? no
VUR Scarring? no
■ VUR Pyelo?
■ Degree VUR Scars?
13. We Need A Study That…
Will help us decide whether or not to prophylaxthis patient
Includes patients with symptomatic VUR
Compares antibiotic prophylaxis to a control
Looks at clinically important outcomes
14. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a
multicenter, randomized, controlled study.Garin EH, Olavarria F, Garcia Nieto V, Valenciano
B, Campos A, Young L.
Pediatrics 2006;117:626-632.
15. Study Questions
Does VUR correlate with UTI/renal scarring?Does antibiotic prophylaxis correlate with
UTI/renal scarring?
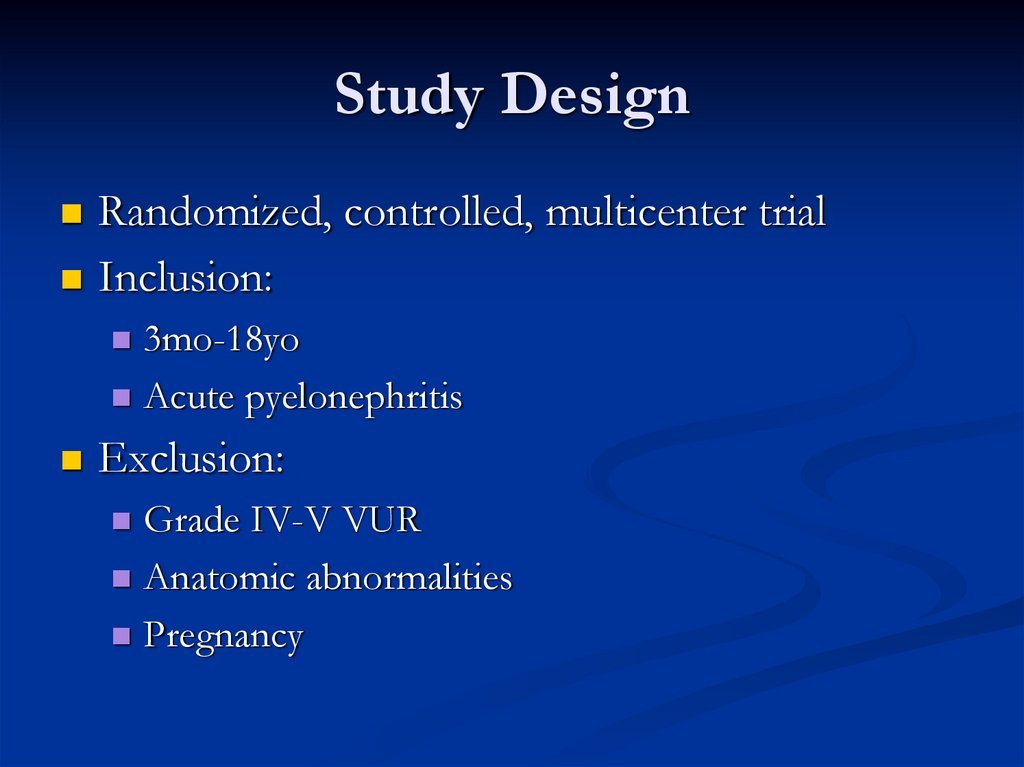
16. Study Design
Randomized, controlled, multicenter trialInclusion:
3mo-18yo
Acute pyelonephritis
Exclusion:
Grade IV-V VUR
Anatomic abnormalities
Pregnancy
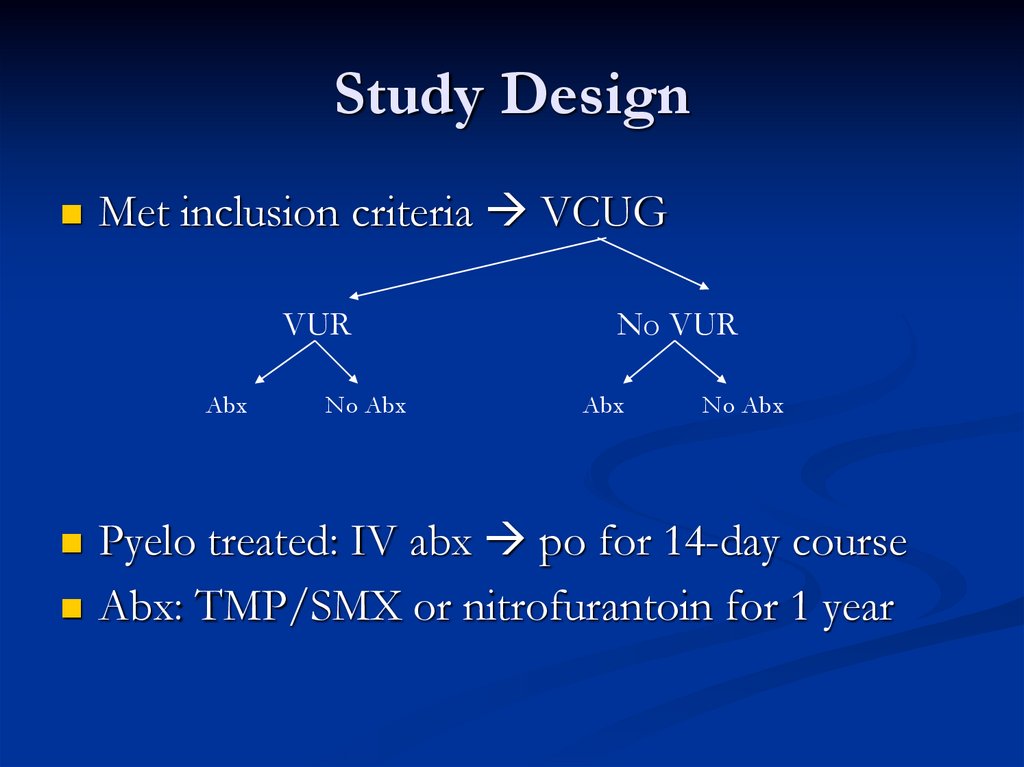
17. Study Design
Met inclusion criteria VCUGVUR
Abx
No Abx
No VUR
Abx
No Abx
Pyelo treated: IV abx po for 14-day course
Abx: TMP/SMX or nitrofurantoin for 1 year
18. Follow Up
At entry: UA/UCx, DMSA, VCUG, Renal USAt Q3mo clinic visit: UA/UCx
At 6mo: DMSA
At 12mo: VCUG, Renal US
Endpoints:
Recurrent UTI
Renal scarring
19. Study Results
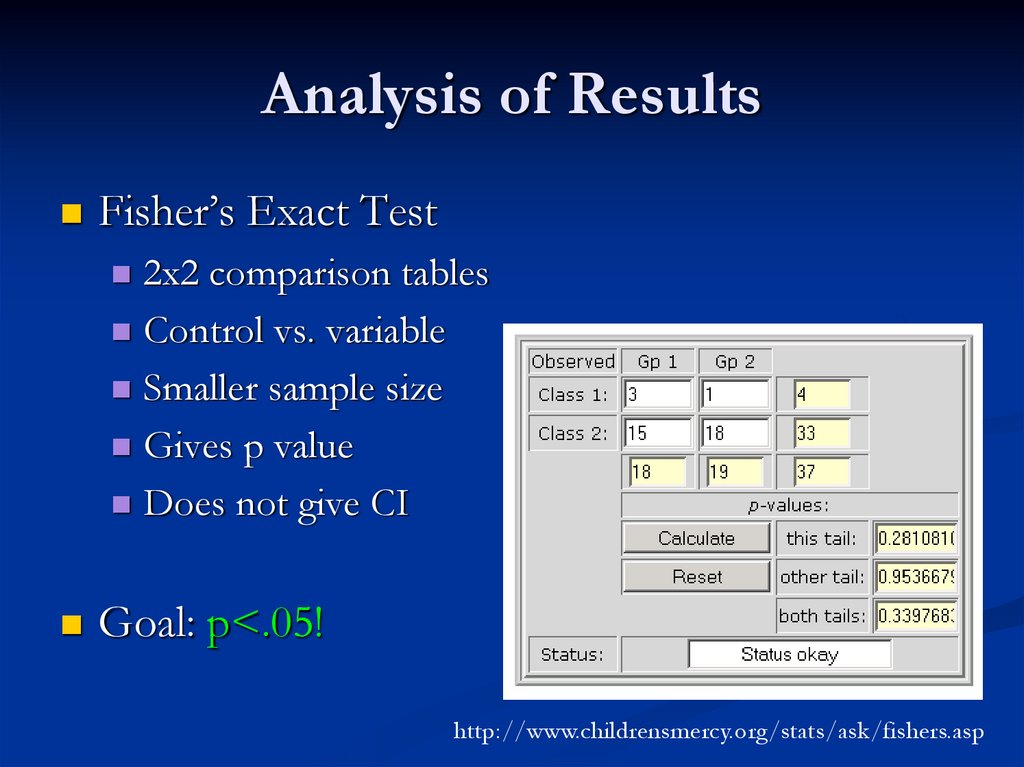
20. Analysis of Results
Fisher’s Exact Test2x2 comparison tables
Control vs. variable
Smaller sample size
Gives p value
Does not give CI
Goal: p<.05!
http://www.childrensmercy.org/stats/ask/fishers.asp
21. Study Results
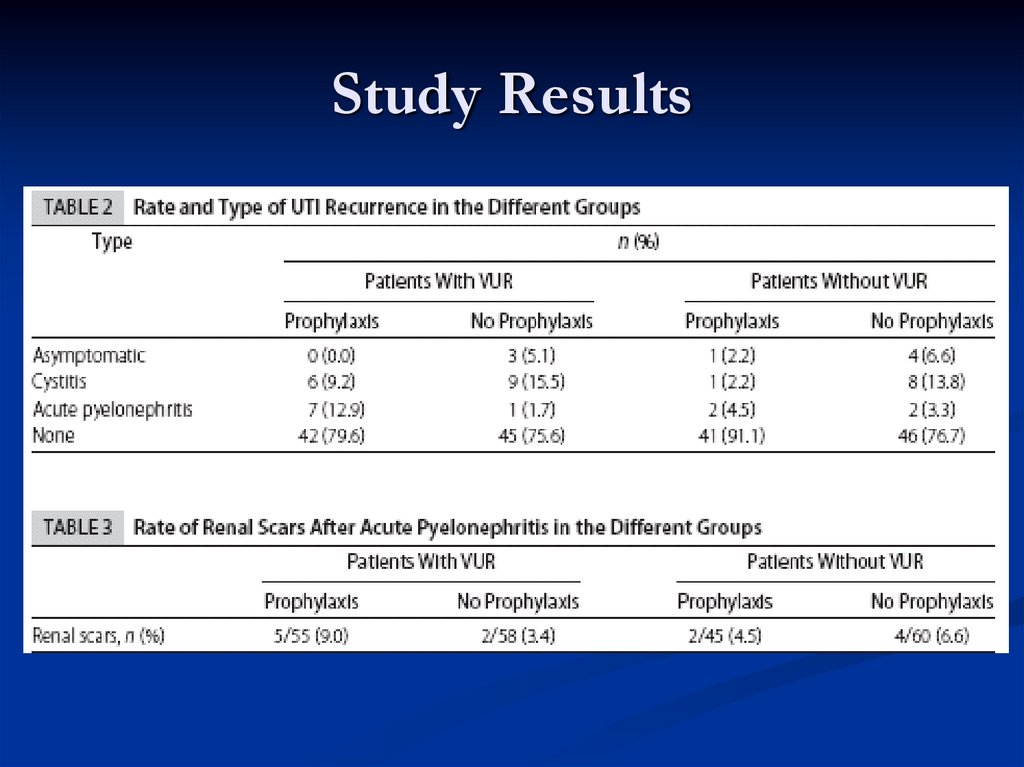
Recurrence of UTIsTiming
Type
Recurrent Pyelonephritis & Antibiotics
Recurrent Pyelonephritis & VUR Degree
Renal Scarring
VUR
Antibiotics
22. Study Results
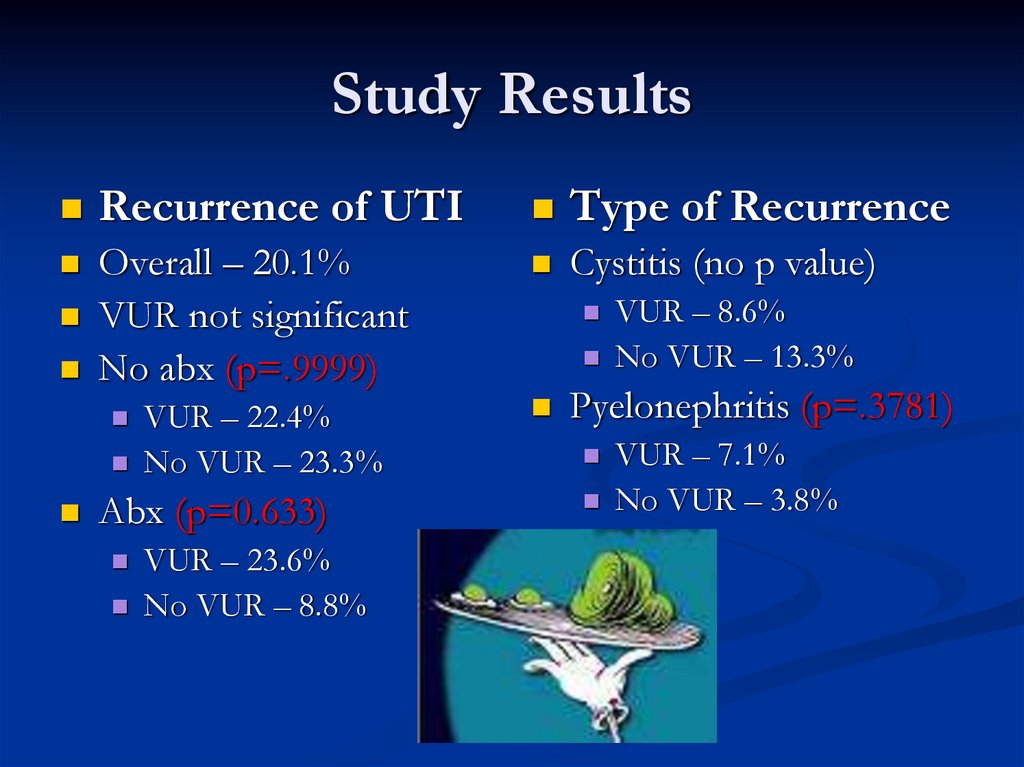
Recurrence of UTIType of Recurrence
Overall – 20.1%
VUR not significant
No abx (p=.9999)
Cystitis (no p value)
VUR – 22.4%
No VUR – 23.3%
Abx (p=0.633)
VUR – 23.6%
No VUR – 8.8%
VUR – 8.6%
No VUR – 13.3%
Pyelonephritis (p=.3781)
VUR – 7.1%
No VUR – 3.8%
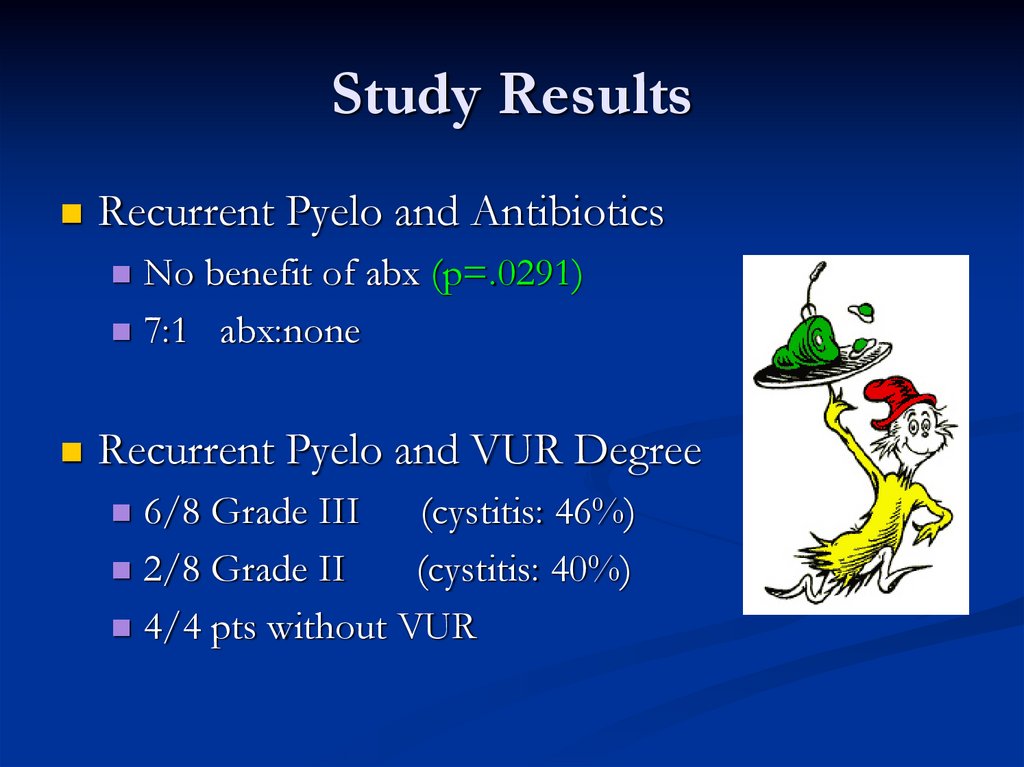
23. Study Results
Recurrent Pyelo and AntibioticsNo benefit of abx (p=.0291)
7:1 abx:none
Recurrent Pyelo and VUR Degree
6/8 Grade III
(cystitis: 46%)
2/8 Grade II
(cystitis: 40%)
4/4 pts without VUR
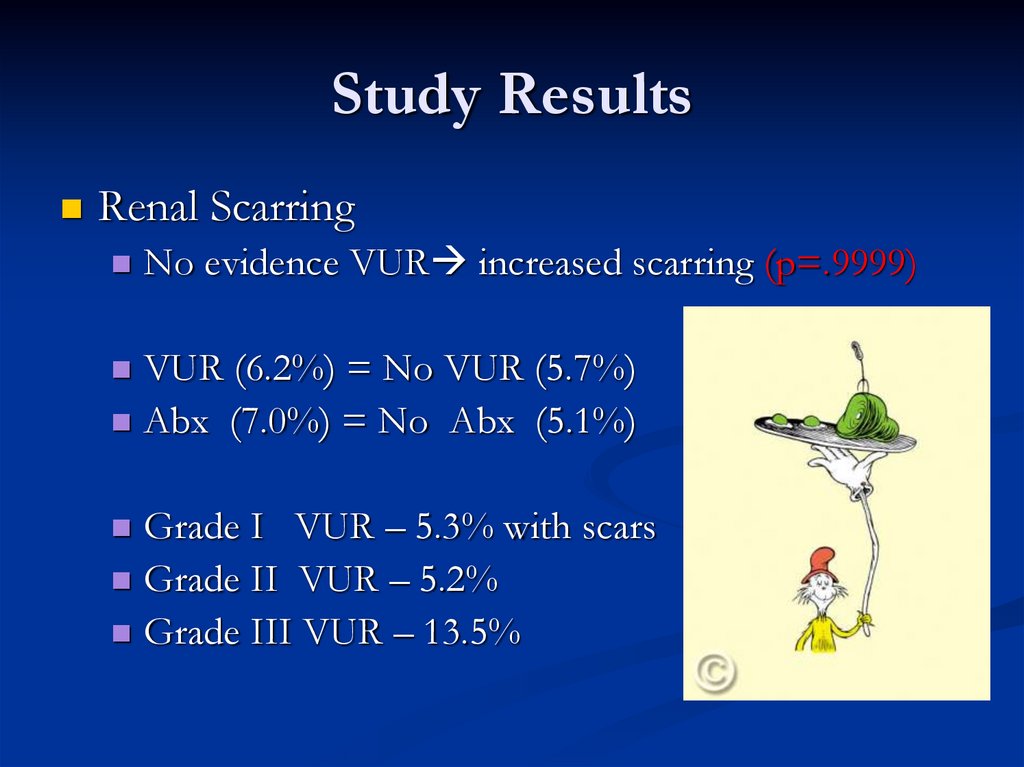
24. Study Results
Renal ScarringNo evidence VUR increased scarring (p=.9999)
VUR (6.2%) = No VUR (5.7%)
Abx (7.0%) = No Abx (5.1%)
Grade I VUR – 5.3% with scars
Grade II VUR – 5.2%
Grade III VUR – 13.5%
25. Study Conclusions
Mild/moderate VUR not associated withUTI, pyelonephritis, or scarring
Antibiotic prophylaxis not associated with
UTI, pyeloneprhitis, or scarring
26. Critically Evaluating… (JAMA Users’ Guide)
Arethe results valid?
What were the results?
Will the results help me to take care of
my patient?
27. Are the results valid? Primary Guides
Was the assignment of patients to treatmentrandomized? YES.
Were all who entered the study accounted for?
Was follow-up complete?
NO. Enrolled 236, lost 18
Lost from what groups?
Would this change results?
Were patients analyzed in the groups assigned to?
NO. Exclusion of noncompliants
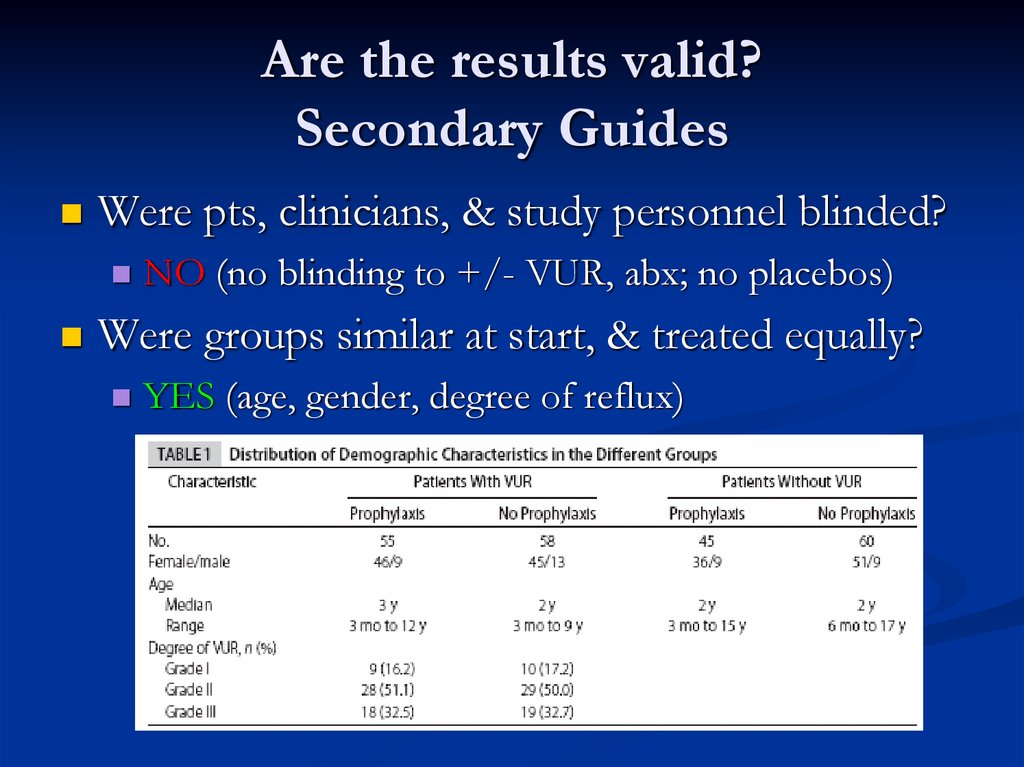
28. Are the results valid? Secondary Guides
Were pts, clinicians, & study personnel blinded?NO (no blinding to +/- VUR, abx; no placebos)
Were groups similar at start, & treated equally?
YES (age, gender, degree of reflux)
29. What were the results?
How large was the treatment effect?ARR – risk difference of variable vs. control
RRR – variable reduced risk by Z% relative to that occurring
in control patients; bigger = better!
For example, in presence of VUR:
23.6% of those on abx developed UTI (X%)
22.4% without abx developed UTI (Y%)
ARR = X-Y = .236-.224 = .012
RRR = (1-Y/X)x100% = (1-.224/.236)x100% = 5.1%
30. What were the results?
How large was the treatment effect?ARR/RRR not reported!
How precise was the estimated treatment effect?
Confidence Intervals (CIs) not reported!
95% CI:
Range that includes the true RRR 95% of time
Positive? Negative? Zero?
Statistically vs. clinically significant results
31. What were the results?
POWER!Ability of a study to detect a true difference
Directly related to sample size
1-β (β = type II error)
Study powered to detect a clinically significant difference
of 20% (power 80%), 95% CI
Need 60/group = 240 subjects
Enrolled 236, Completed 218
“POWER : research design :: SENSITIVITY : diagnostic test”
32. Will the results help me take care of my patient?
Can the results be applied? YES.Could Kali have been enrolled?
All clinically important outcomes considered? YES.
Substitute endpoints vs. “POEMS”
Adverse effects on other outcomes
Are likely benefits worth potential harms/risks?
NNT = 1/ARR
Consider baseline risk without intervention
33. Criticisms: Study Population
What about <3mo?Present earlier = Higher-grade reflux? Already abx?
Included in study?
Exclusion of noncompliants?
Exclusion of pyelonephritis x2?
Initial presentation with cystitis?
Febrile UTI without DMSA changes?
How many therefore excluded?
34. Criticisms: Study Design
DMSA as inclusion criteria (multicenter)?Account for 18 lost before study end?
Unknown prognostic factors
Recalculate results assuming they did well/poorly
Blinding of patients/personnel?
Placebo
Diagnosis
Larger sample size?
35. Criticisms: Data Analysis
Reporting of CIs, ARR/RRR?Magnitude/precision of treatment effect
Rule in/out effect different from Ho
Data crunching using Chi-Square?
Different data combinations?
Did not achieve POWER
36. Further Questions…
UTI prophylaxis vs. intermittent therapy?And risk of renal scarring
Over time, given resolution VUR
Larger sample size
VUR in context of abnormal anatomy?
Mechanism of scarring in pyelonephritis?
What else?
37. Back to our patient…
What would you do?Call Dr.Cartwright and Dr.Lechner and get
those patients enrolled!
38. References
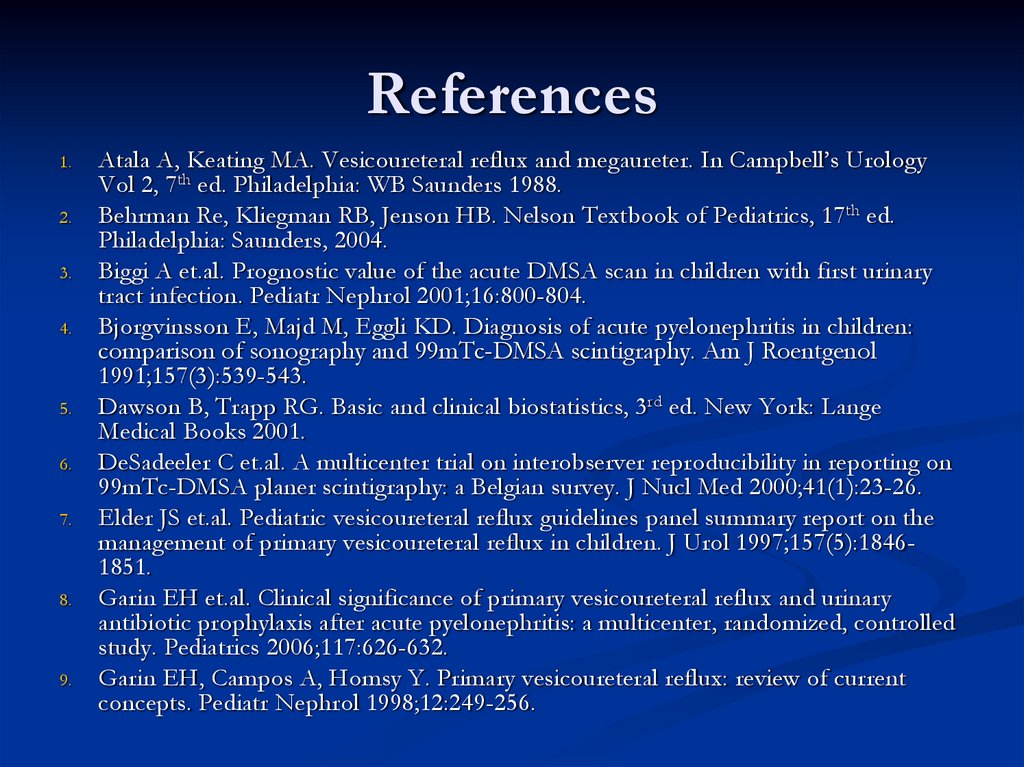
1.2.
3.
4.
5.
6.
7.
8.
9.
Atala A, Keating MA. Vesicoureteral reflux and megaureter. In Campbell’s Urology
Vol 2, 7th ed. Philadelphia: WB Saunders 1988.
Behrman Re, Kliegman RB, Jenson HB. Nelson Textbook of Pediatrics, 17th ed.
Philadelphia: Saunders, 2004.
Biggi A et.al. Prognostic value of the acute DMSA scan in children with first urinary
tract infection. Pediatr Nephrol 2001;16:800-804.
Bjorgvinsson E, Majd M, Eggli KD. Diagnosis of acute pyelonephritis in children:
comparison of sonography and 99mTc-DMSA scintigraphy. Am J Roentgenol
1991;157(3):539-543.
Dawson B, Trapp RG. Basic and clinical biostatistics, 3rd ed. New York: Lange
Medical Books 2001.
DeSadeeler C et.al. A multicenter trial on interobserver reproducibility in reporting on
99mTc-DMSA planer scintigraphy: a Belgian survey. J Nucl Med 2000;41(1):23-26.
Elder JS et.al. Pediatric vesicoureteral reflux guidelines panel summary report on the
management of primary vesicoureteral reflux in children. J Urol 1997;157(5):18461851.
Garin EH et.al. Clinical significance of primary vesicoureteral reflux and urinary
antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled
study. Pediatrics 2006;117:626-632.
Garin EH, Campos A, Homsy Y. Primary vesicoureteral reflux: review of current
concepts. Pediatr Nephrol 1998;12:249-256.
39. References
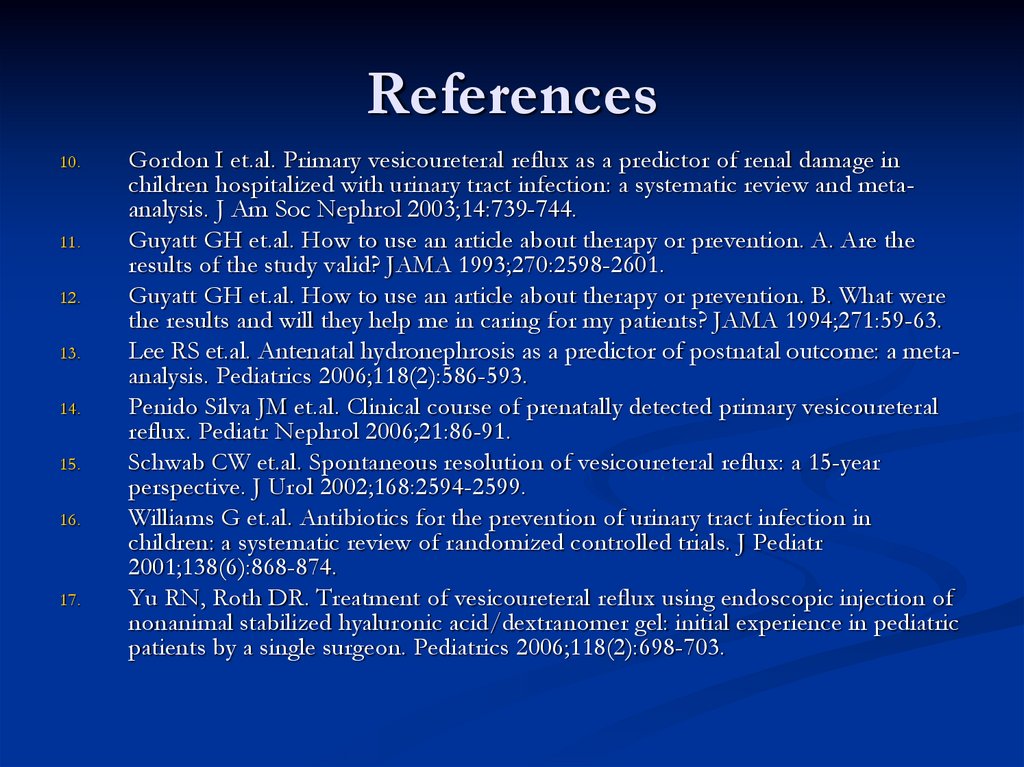
10.11.
12.
13.
14.
15.
16.
17.
Gordon I et.al. Primary vesicoureteral reflux as a predictor of renal damage in
children hospitalized with urinary tract infection: a systematic review and metaanalysis. J Am Soc Nephrol 2003;14:739-744.
Guyatt GH et.al. How to use an article about therapy or prevention. A. Are the
results of the study valid? JAMA 1993;270:2598-2601.
Guyatt GH et.al. How to use an article about therapy or prevention. B. What were
the results and will they help me in caring for my patients? JAMA 1994;271:59-63.
Lee RS et.al. Antenatal hydronephrosis as a predictor of postnatal outcome: a metaanalysis. Pediatrics 2006;118(2):586-593.
Penido Silva JM et.al. Clinical course of prenatally detected primary vesicoureteral
reflux. Pediatr Nephrol 2006;21:86-91.
Schwab CW et.al. Spontaneous resolution of vesicoureteral reflux: a 15-year
perspective. J Urol 2002;168:2594-2599.
Williams G et.al. Antibiotics for the prevention of urinary tract infection in
children: a systematic review of randomized controlled trials. J Pediatr
2001;138(6):868-874.
Yu RN, Roth DR. Treatment of vesicoureteral reflux using endoscopic injection of
nonanimal stabilized hyaluronic acid/dextranomer gel: initial experience in pediatric
patients by a single surgeon. Pediatrics 2006;118(2):698-703.



 Медицина
Медицина