Похожие презентации:
Endocrine System
1. ENDOCRINE SYSTE
PATHOPHYSIOLOGY2.
3.
4.
5.
6.
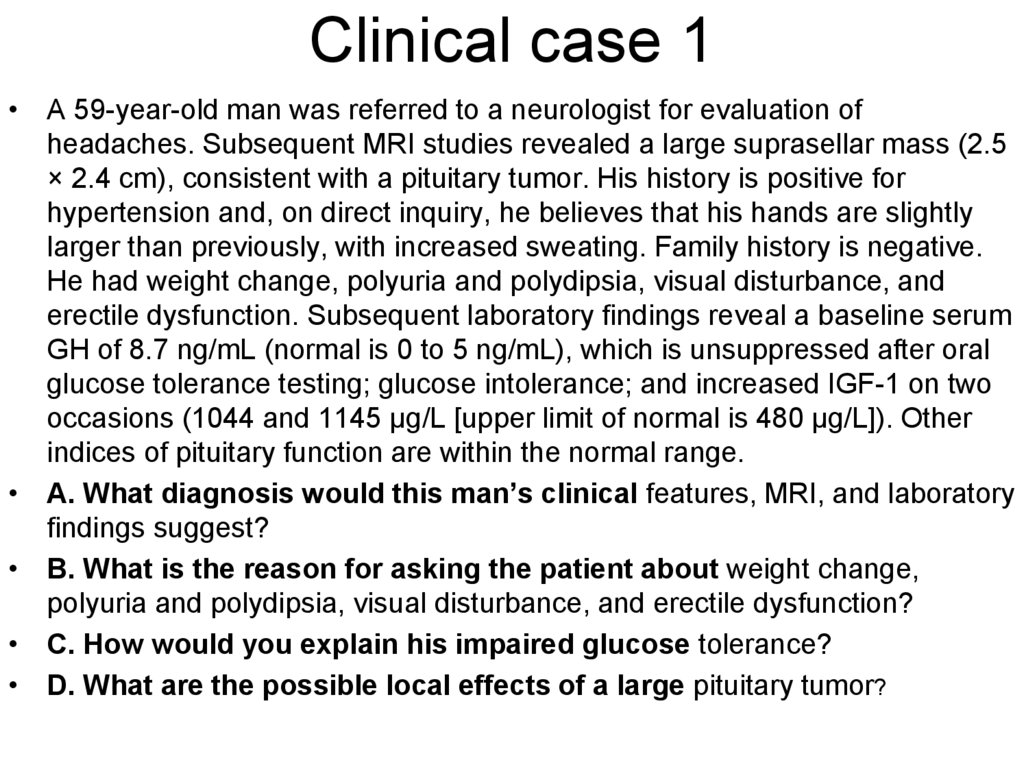
7. Clinical case 1
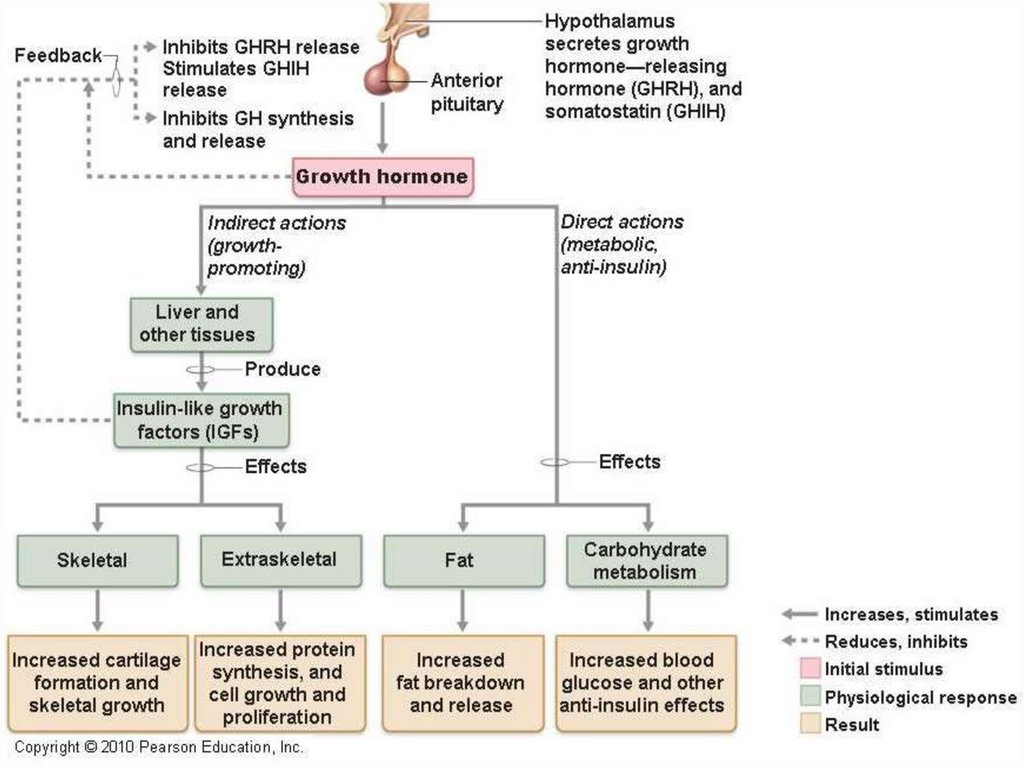
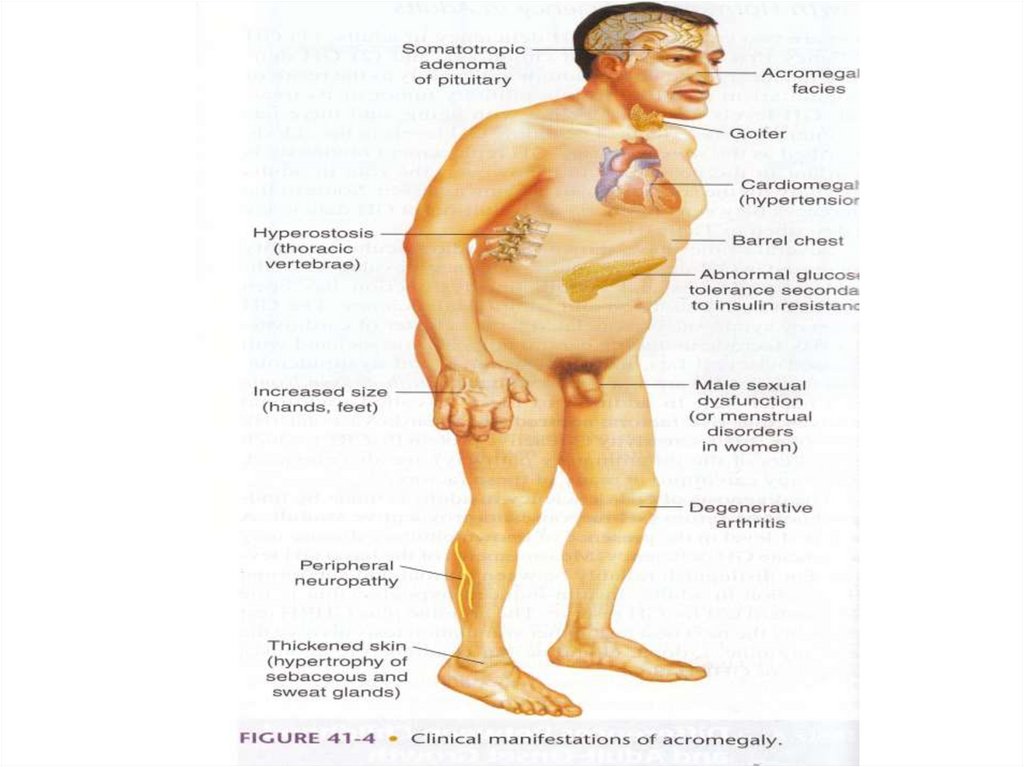
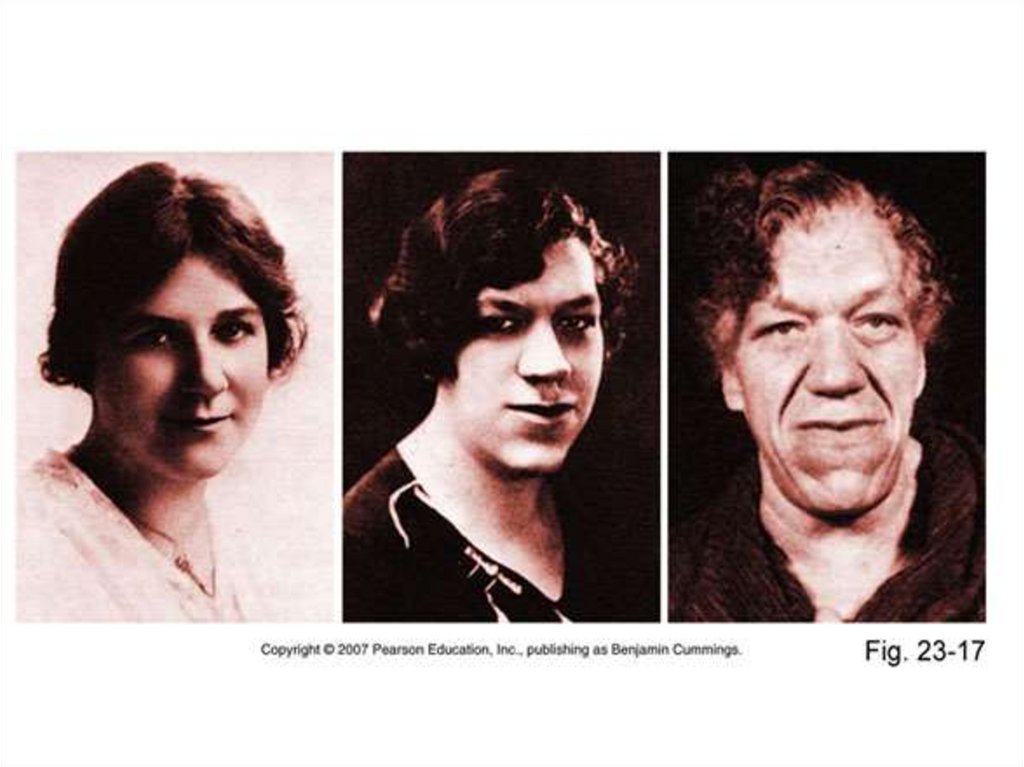
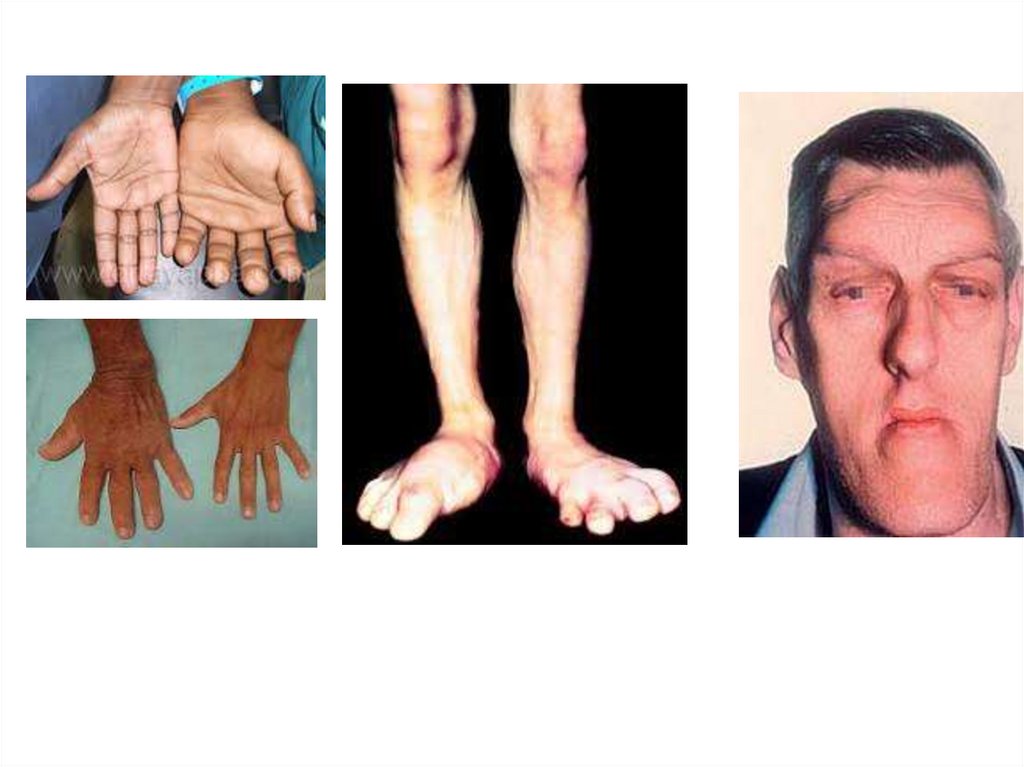
• A 59-year-old man was referred to a neurologist for evaluation ofheadaches. Subsequent MRI studies revealed a large suprasellar mass (2.5
× 2.4 cm), consistent with a pituitary tumor. His history is positive for
hypertension and, on direct inquiry, he believes that his hands are slightly
larger than previously, with increased sweating. Family history is negative.
He had weight change, polyuria and polydipsia, visual disturbance, and
erectile dysfunction. Subsequent laboratory findings reveal a baseline serum
GH of 8.7 ng/mL (normal is 0 to 5 ng/mL), which is unsuppressed after oral
glucose tolerance testing; glucose intolerance; and increased IGF-1 on two
occasions (1044 and 1145 μg/L [upper limit of normal is 480 μg/L]). Other
indices of pituitary function are within the normal range.
• A. What diagnosis would this man’s clinical features, MRI, and laboratory
findings suggest?
• B. What is the reason for asking the patient about weight change,
polyuria and polydipsia, visual disturbance, and erectile dysfunction?
• C. How would you explain his impaired glucose tolerance?
• D. What are the possible local effects of a large pituitary tumor?
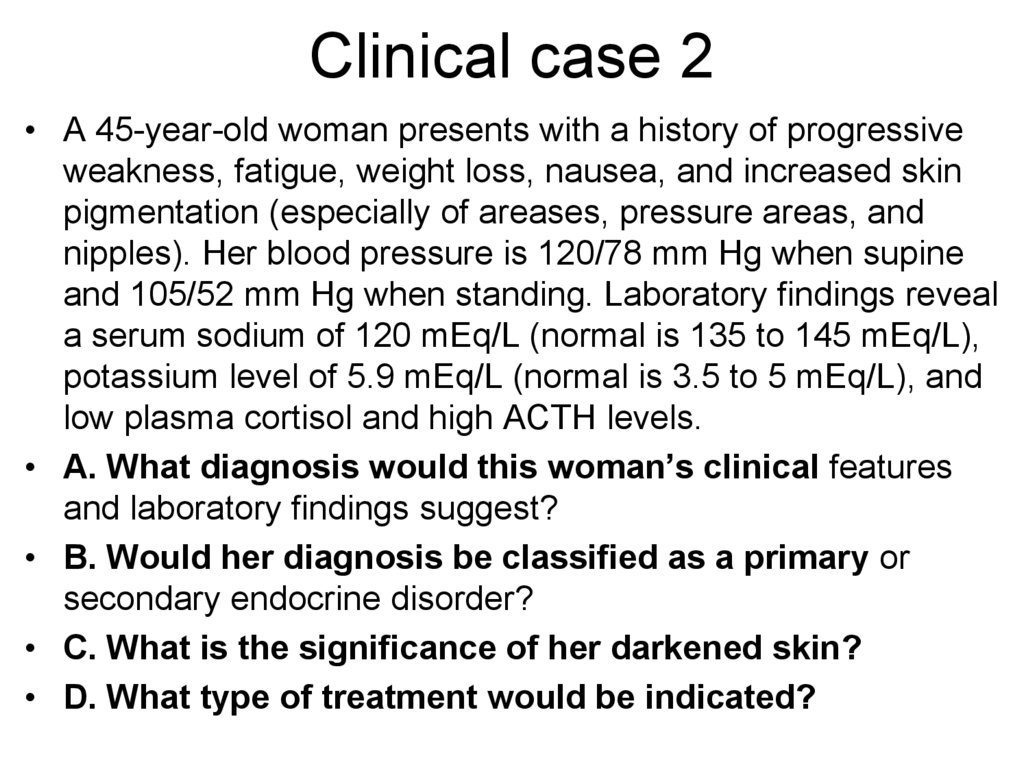
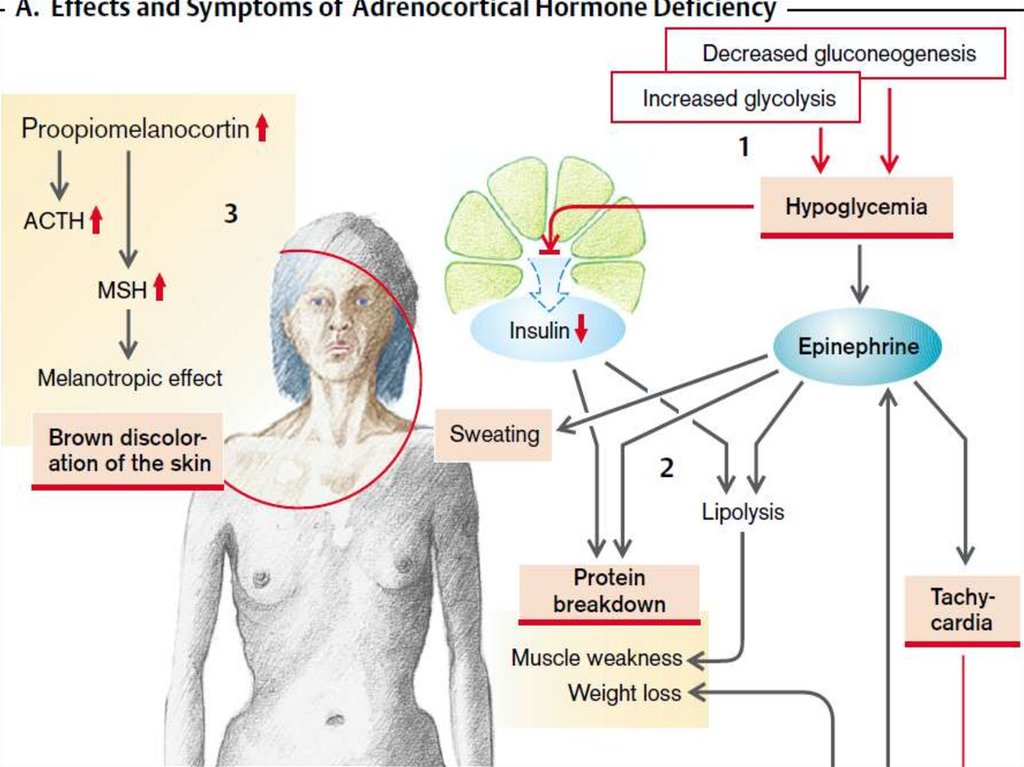
8. Clinical case 2
• A 45-year-old woman presents with a history of progressiveweakness, fatigue, weight loss, nausea, and increased skin
pigmentation (especially of areases, pressure areas, and
nipples). Her blood pressure is 120/78 mm Hg when supine
and 105/52 mm Hg when standing. Laboratory findings reveal
a serum sodium of 120 mEq/L (normal is 135 to 145 mEq/L),
potassium level of 5.9 mEq/L (normal is 3.5 to 5 mEq/L), and
low plasma cortisol and high ACTH levels.
• A. What diagnosis would this woman’s clinical features
and laboratory findings suggest?
• B. Would her diagnosis be classified as a primary or
secondary endocrine disorder?
• C. What is the significance of her darkened skin?
• D. What type of treatment would be indicated?
9. Clinical case 3
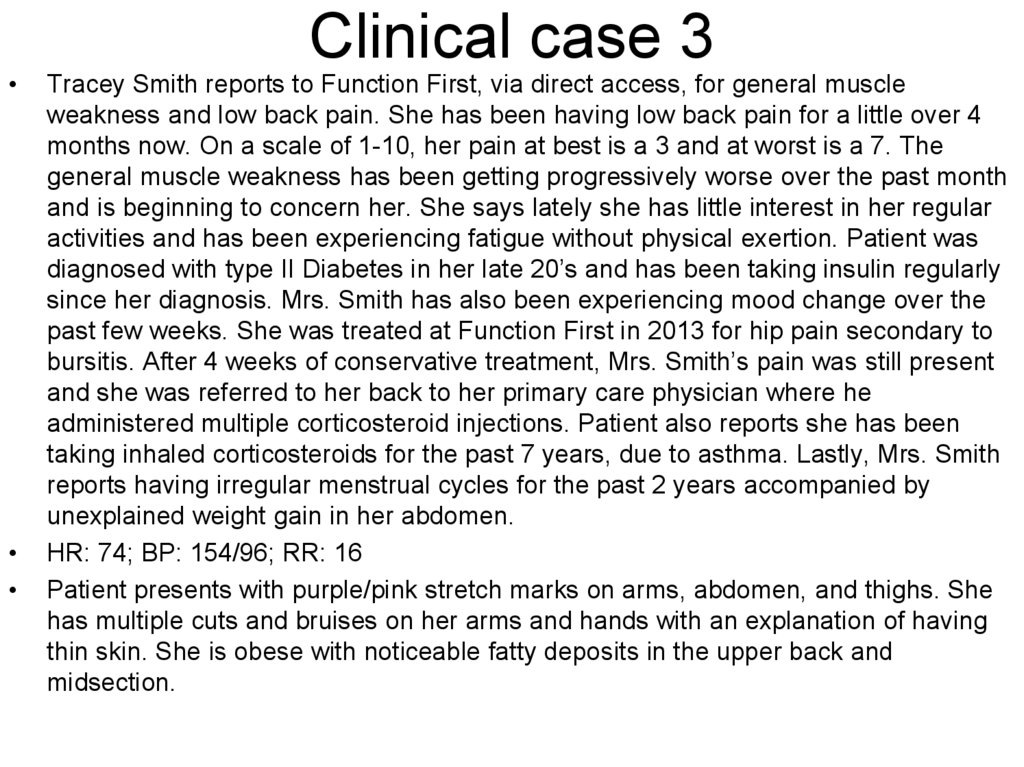
Clinical case 3
Tracey Smith reports to Function First, via direct access, for general muscle
weakness and low back pain. She has been having low back pain for a little over 4
months now. On a scale of 1-10, her pain at best is a 3 and at worst is a 7. The
general muscle weakness has been getting progressively worse over the past month
and is beginning to concern her. She says lately she has little interest in her regular
activities and has been experiencing fatigue without physical exertion. Patient was
diagnosed with type II Diabetes in her late 20’s and has been taking insulin regularly
since her diagnosis. Mrs. Smith has also been experiencing mood change over the
past few weeks. She was treated at Function First in 2013 for hip pain secondary to
bursitis. After 4 weeks of conservative treatment, Mrs. Smith’s pain was still present
and she was referred to her back to her primary care physician where he
administered multiple corticosteroid injections. Patient also reports she has been
taking inhaled corticosteroids for the past 7 years, due to asthma. Lastly, Mrs. Smith
reports having irregular menstrual cycles for the past 2 years accompanied by
unexplained weight gain in her abdomen.
HR: 74; BP: 154/96; RR: 16
Patient presents with purple/pink stretch marks on arms, abdomen, and thighs. She
has multiple cuts and bruises on her arms and hands with an explanation of having
thin skin. She is obese with noticeable fatty deposits in the upper back and
midsection.
10.
11.
12.
13.
14.
15.
16.
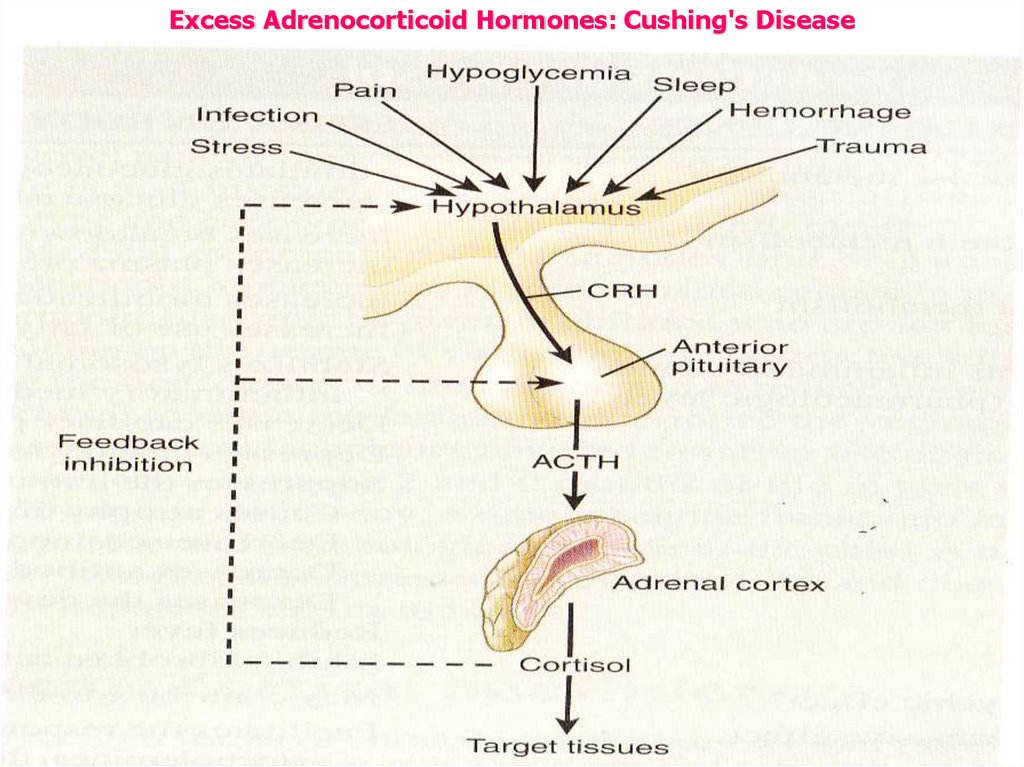
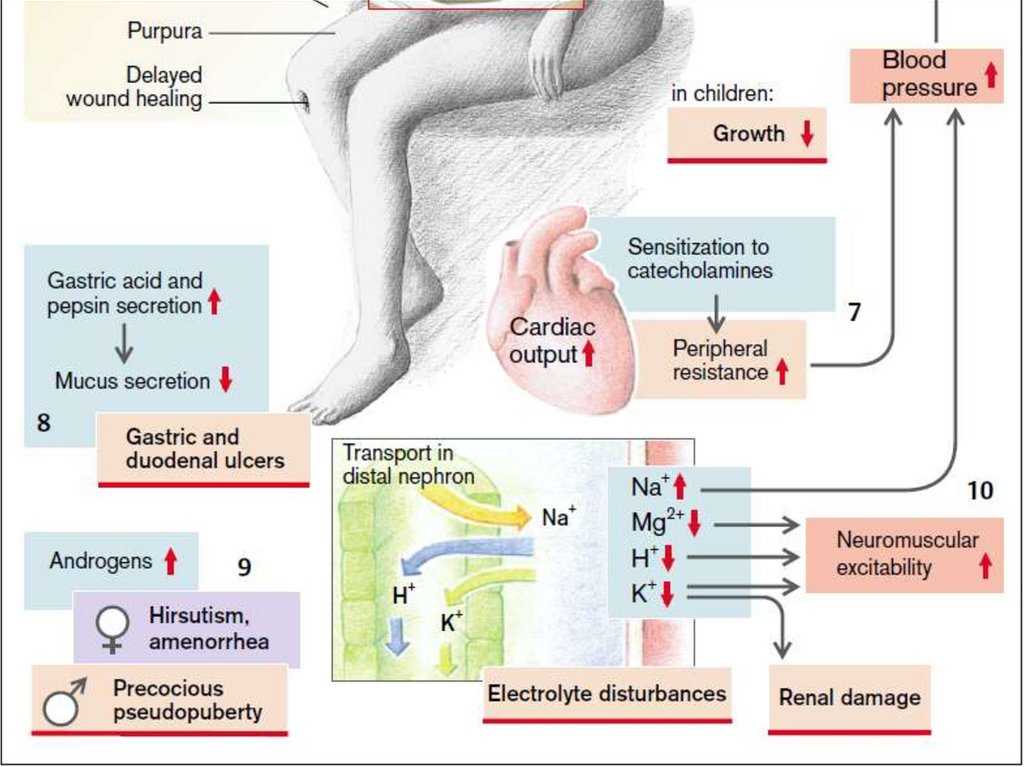
Excess Adrenocorticoid Hormones: Cushing's Disease17.
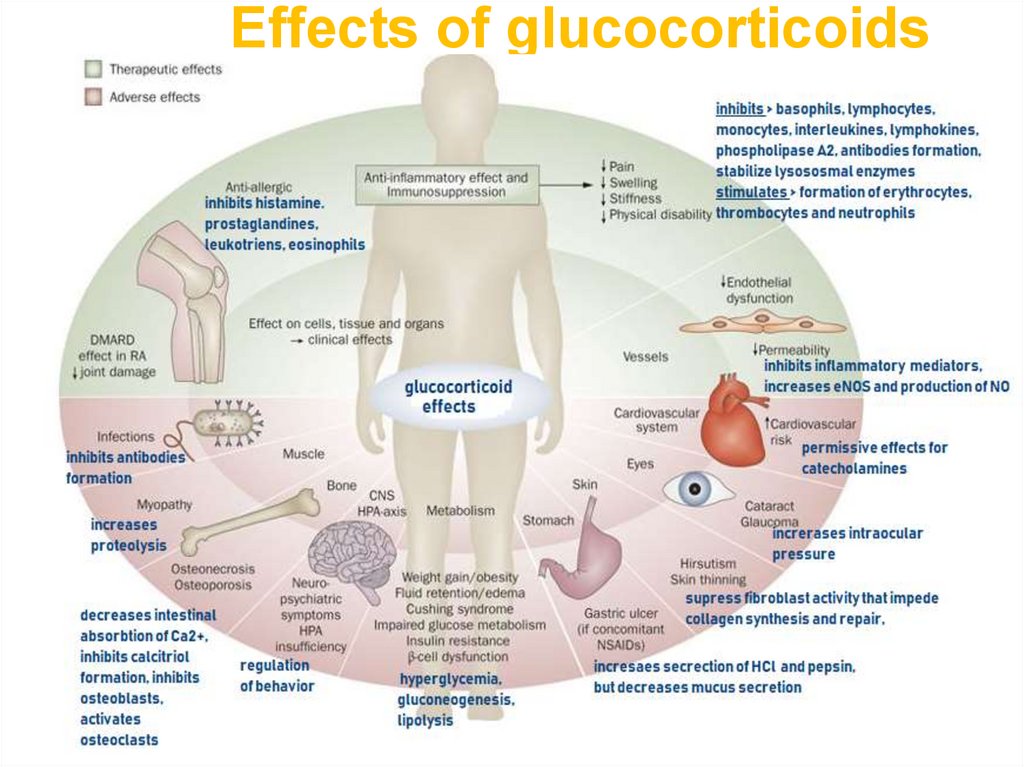
18. Effects of glucocorticoids
1819.
20.
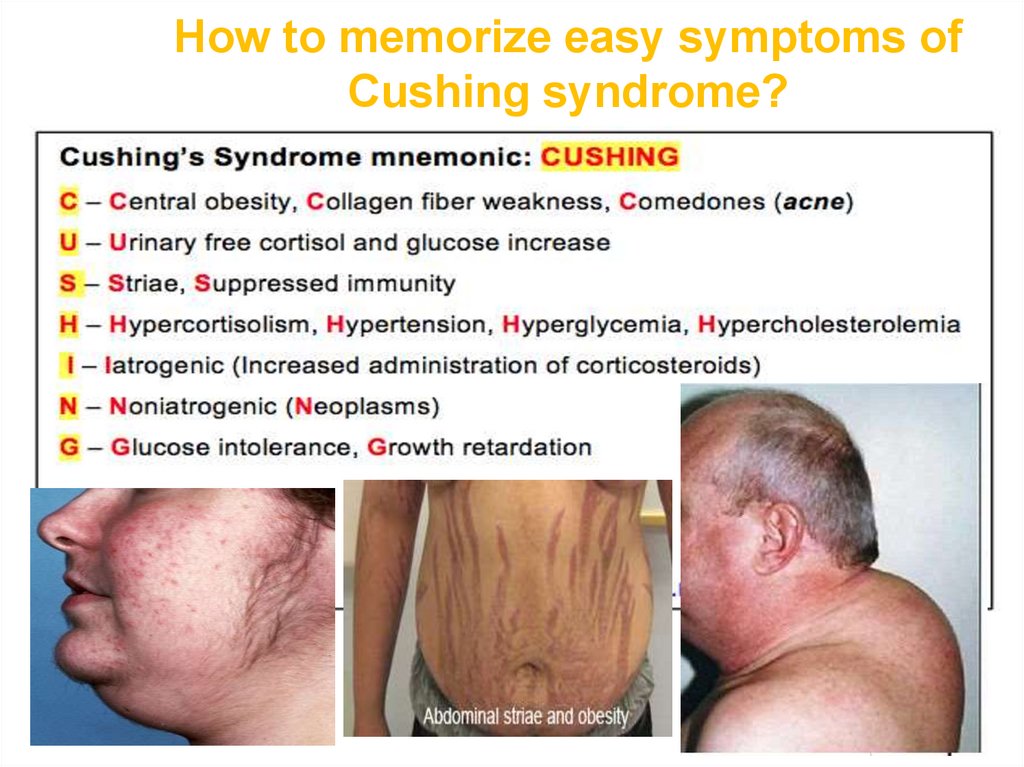
21. How to memorize easy symptoms of Cushing syndrome?
2122.
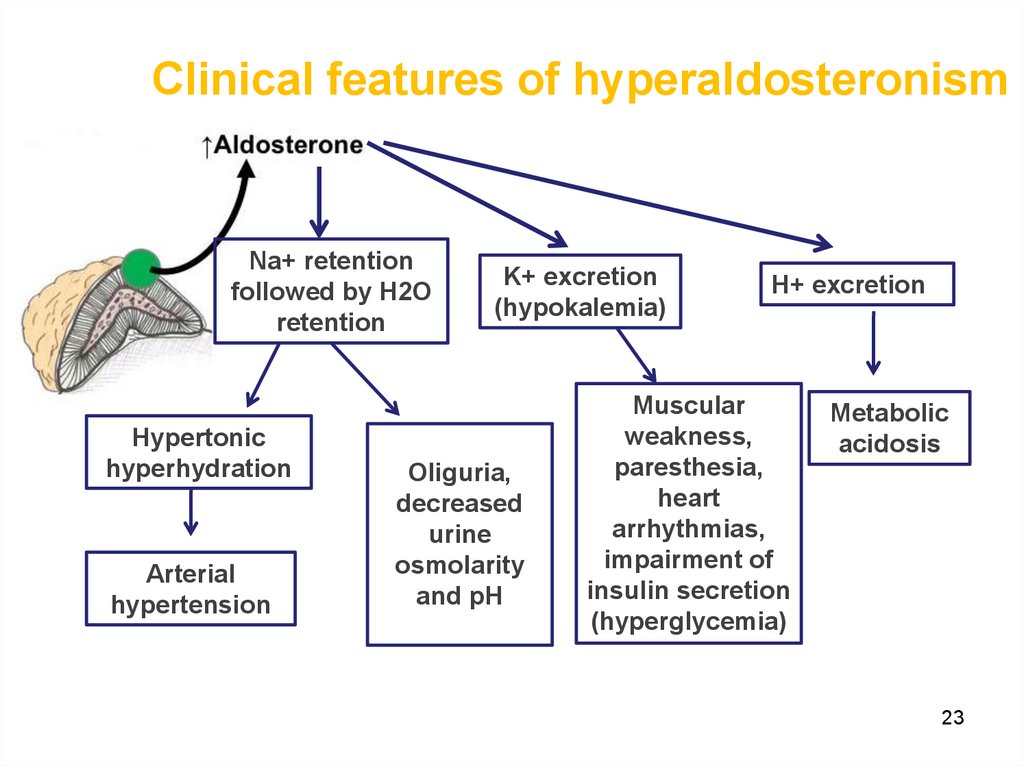
23. Clinical features of hyperaldosteronism
Na+ retentionfollowed by H2O
retention
Hypertonic
hyperhydration
Arterial
hypertension
K+ excretion
(hypokalemia)
Oliguria,
decreased
urine
osmolarity
and pH
H+ excretion
Muscular
weakness,
paresthesia,
heart
arrhythmias,
impairment of
insulin secretion
(hyperglycemia)
Metabolic
acidosis
23
24.
25.
26.
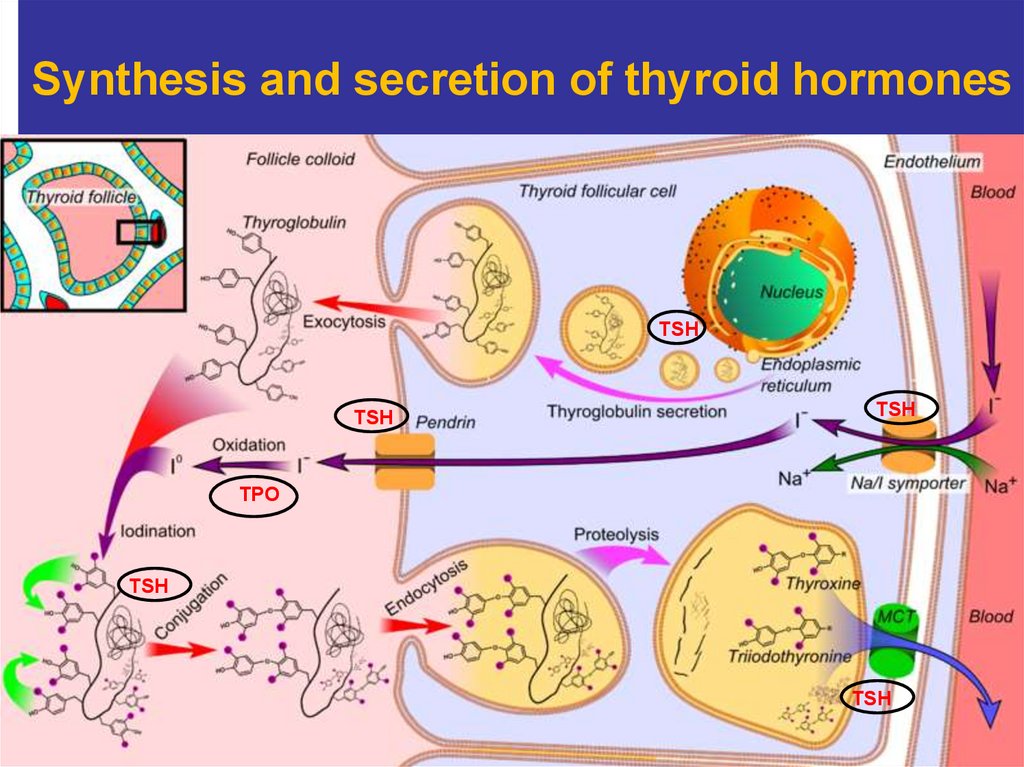
27. Synthesis and secretion of thyroid hormones
TSHTSH
TSH
TPO
TSH
TSH
27
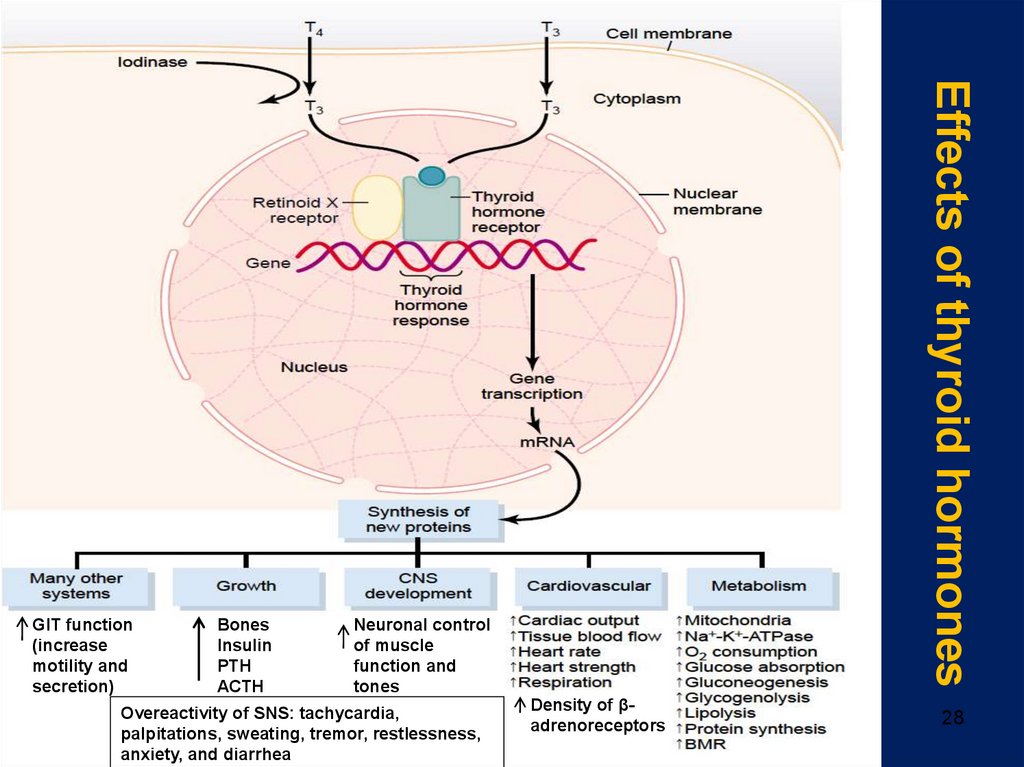
28. Effects of thyroid hormones
BonesInsulin
PTH
ACTH
Neuronal control
of muscle
function and
tones
Overeactivity of SNS: tachycardia,
palpitations, sweating, tremor, restlessness,
anxiety, and diarrhea
Effects of thyroid hormones
GIT function
(increase
motility and
secretion)
Density of βadrenoreceptors
28
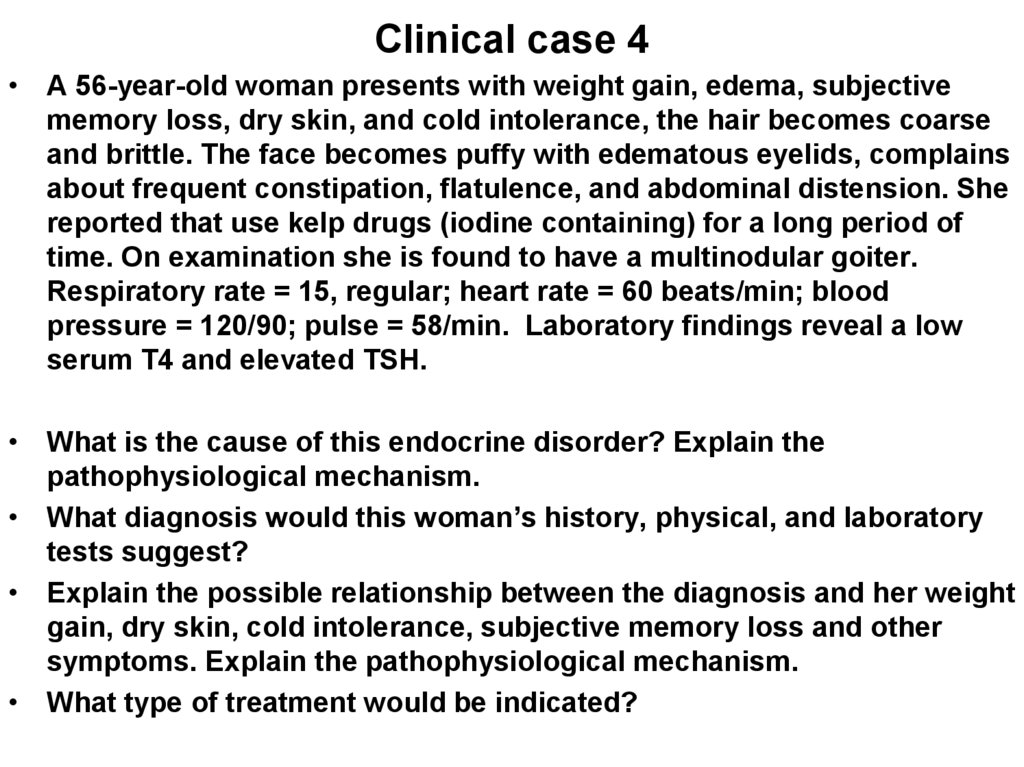
29. Clinical case 4
• A 56-year-old woman presents with weight gain, edema, subjectivememory loss, dry skin, and cold intolerance, the hair becomes coarse
and brittle. The face becomes puffy with edematous eyelids, complains
about frequent constipation, flatulence, and abdominal distension. She
reported that use kelp drugs (iodine containing) for a long period of
time. On examination she is found to have a multinodular goiter.
Respiratory rate = 15, regular; heart rate = 60 beats/min; blood
pressure = 120/90; pulse = 58/min. Laboratory findings reveal a low
serum T4 and elevated TSH.
• What is the cause of this endocrine disorder? Explain the
pathophysiological mechanism.
• What diagnosis would this woman’s history, physical, and laboratory
tests suggest?
• Explain the possible relationship between the diagnosis and her weight
gain, dry skin, cold intolerance, subjective memory loss and other
symptoms. Explain the pathophysiological mechanism.
• What type of treatment would be indicated?
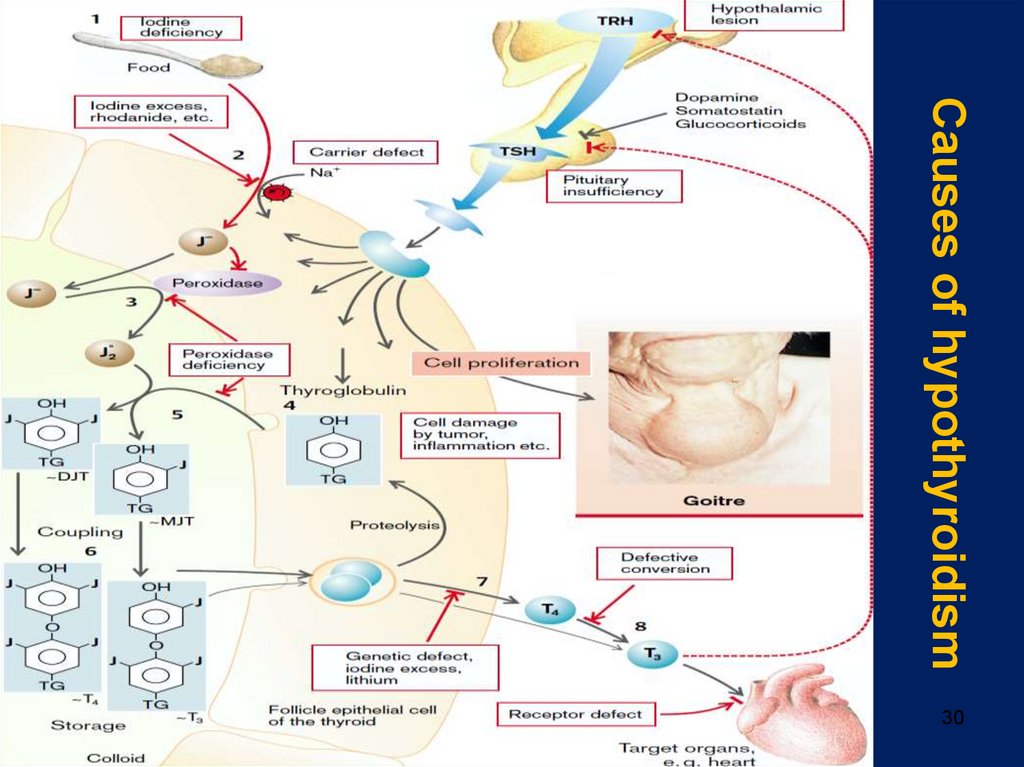
30. Causes of hypothyroidism
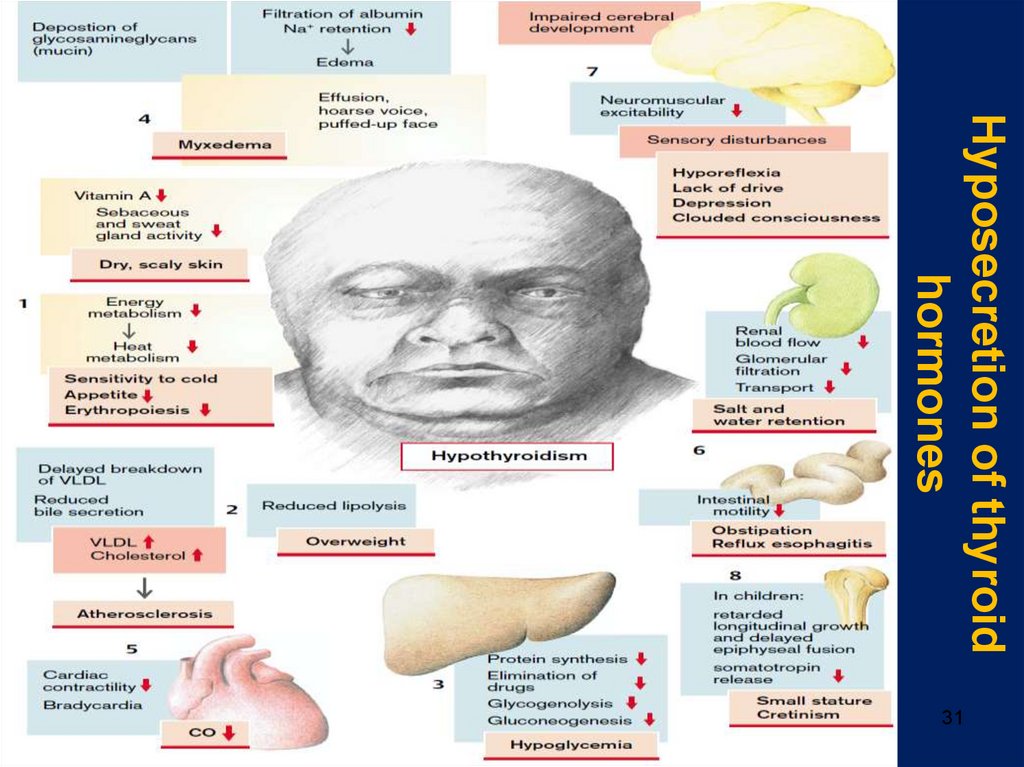
3031. Hyposecretion of thyroid hormones
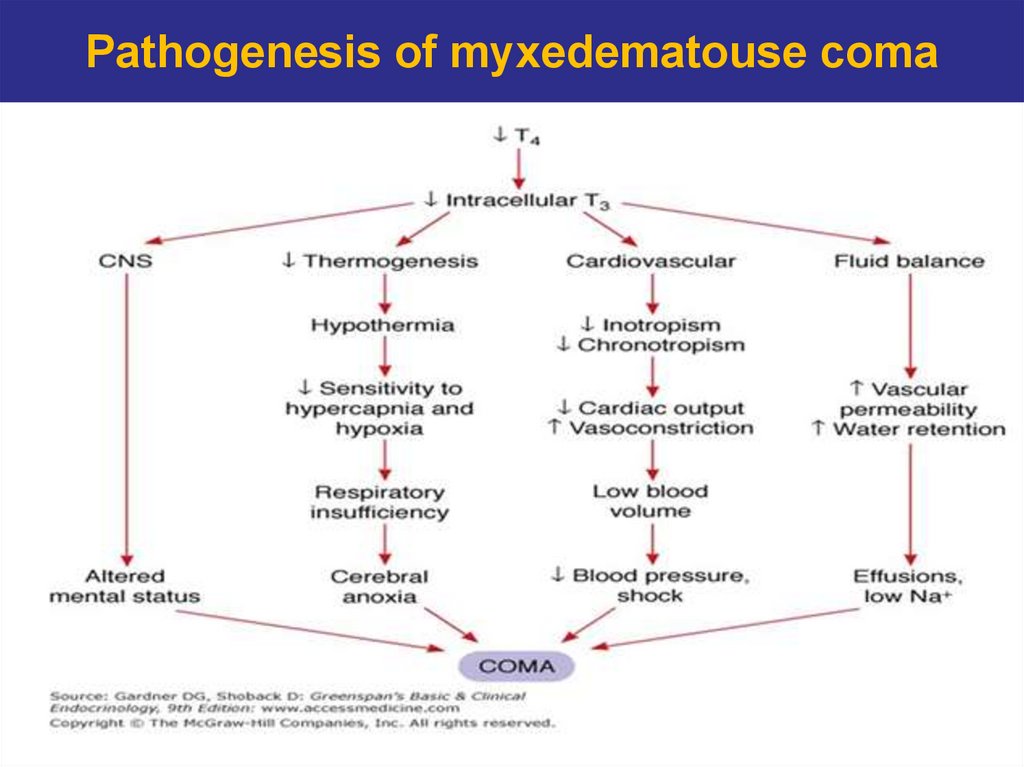
3132. Pathogenesis of myxedematouse coma
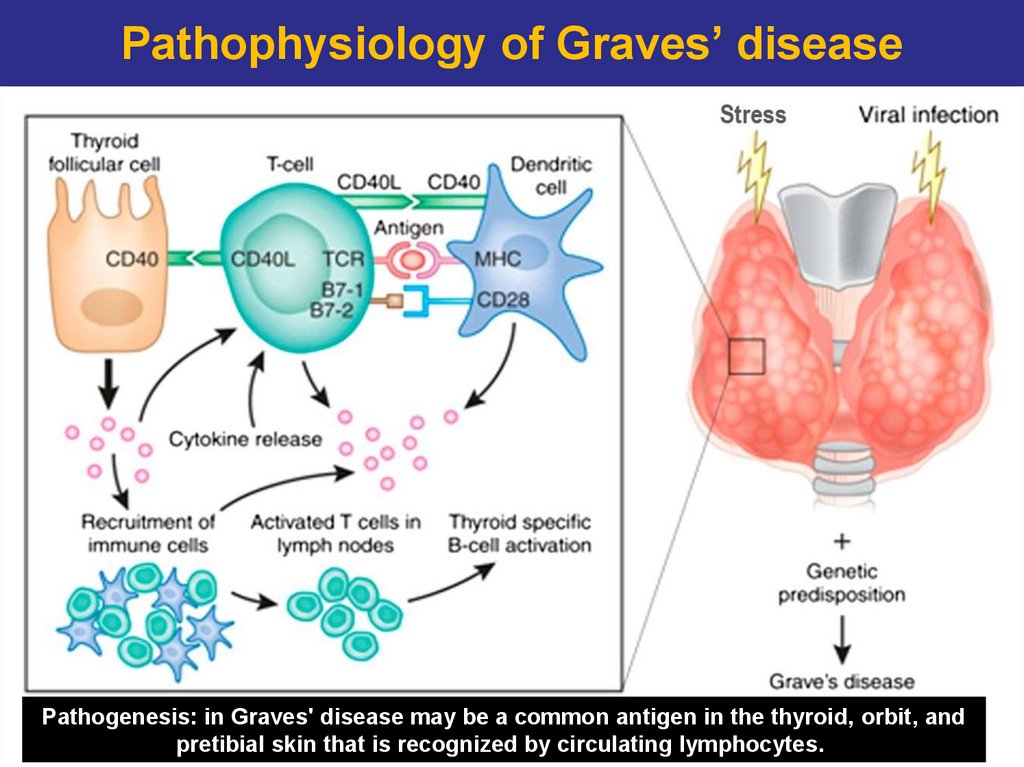
3233. Pathophysiology of Graves’ disease
Pathogenesis: in Graves' disease may be a common antigen in the thyroid, orbit, and33
pretibial skin that is recognized by circulating lymphocytes.
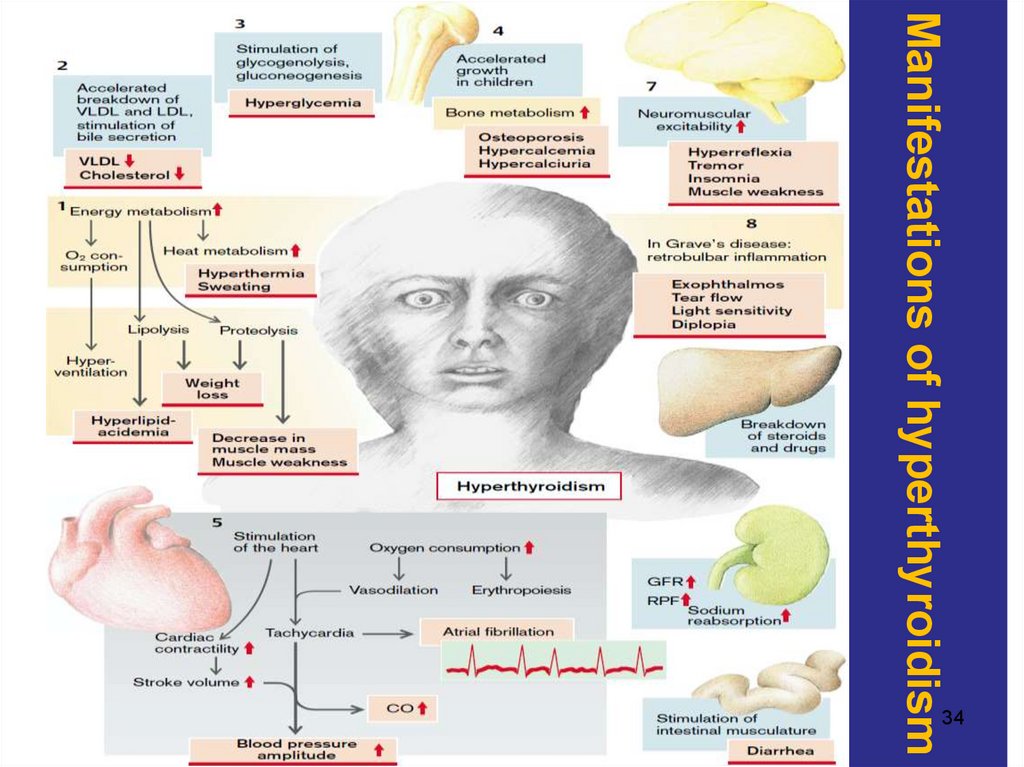
34. Manifestations of hyperthyroidism
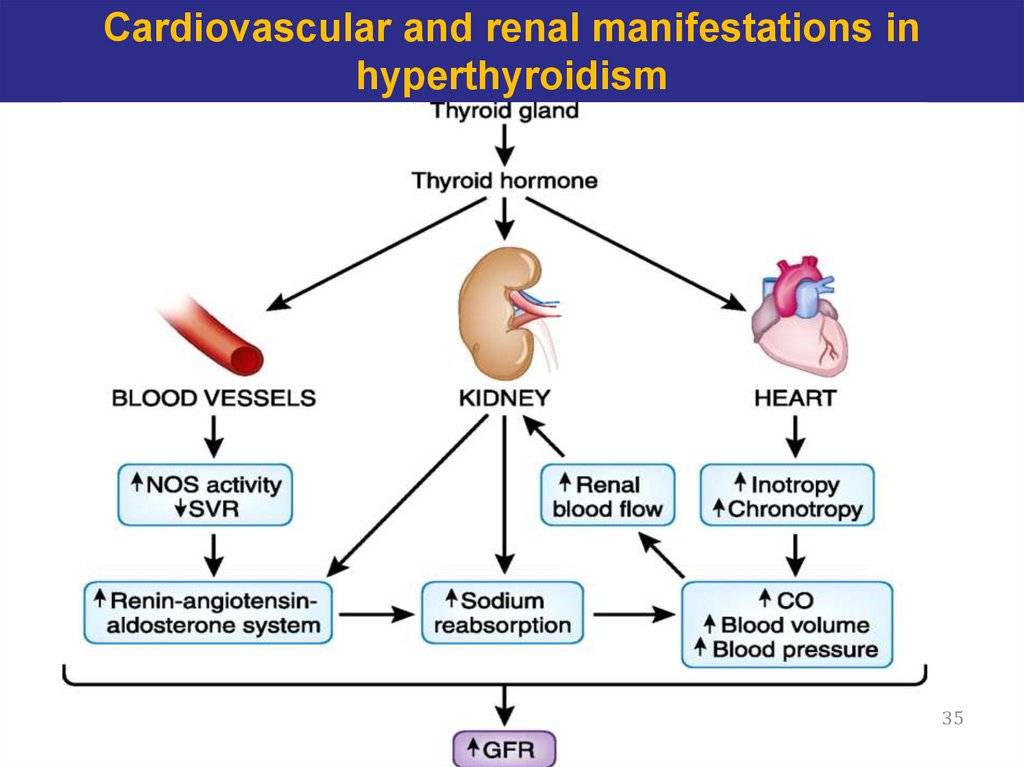
3435. Cardiovascular and renal manifestations in hyperthyroidism
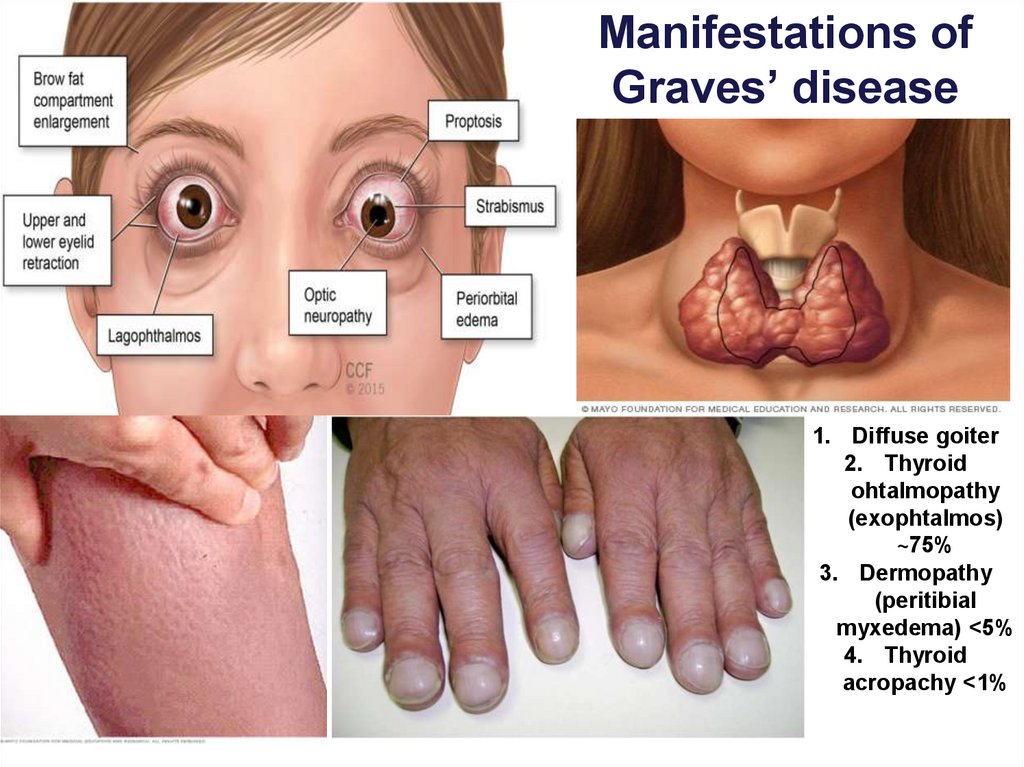
3536. Manifestations of Graves’ disease
1. Diffuse goiter2. Thyroid
ohtalmopathy
(exophtalmos)
~75%
3. Dermopathy
(peritibial
myxedema) <5%
4. Thyroid
acropachy <1%
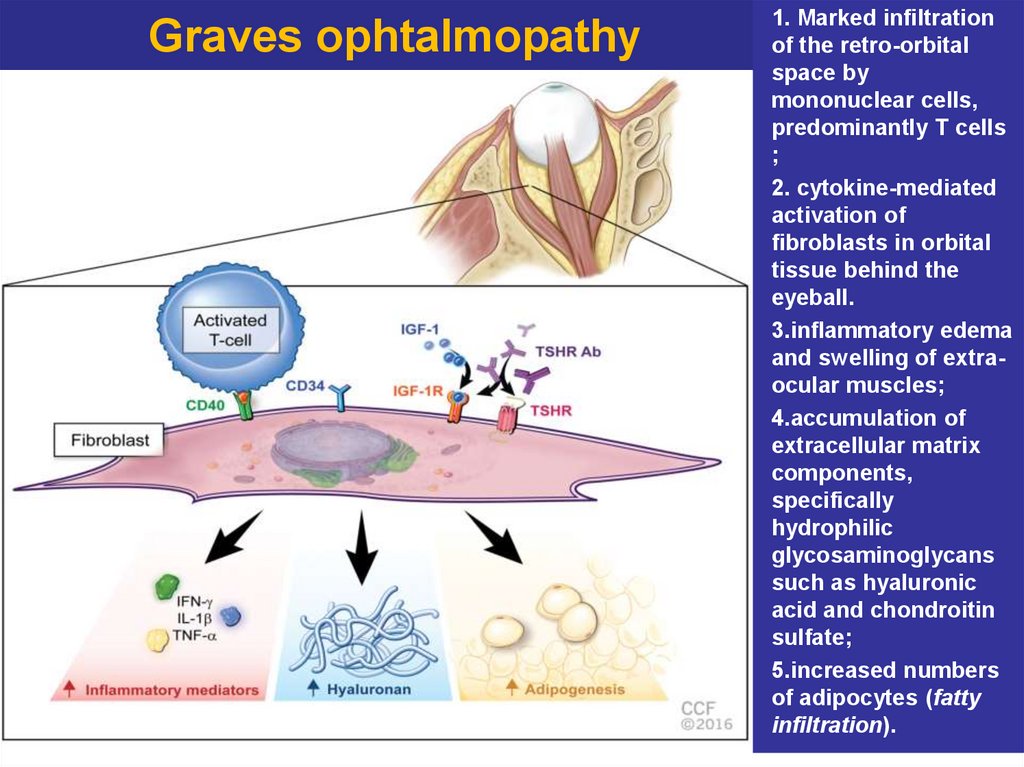
37. Graves ophtalmopathy
1. Marked infiltrationof the retro-orbital
space by
mononuclear cells,
predominantly T cells
;
2. cytokine-mediated
activation of
fibroblasts in orbital
tissue behind the
eyeball.
3.inflammatory edema
and swelling of extraocular muscles;
4.accumulation of
extracellular matrix
components,
specifically
hydrophilic
glycosaminoglycans
such as hyaluronic
acid and chondroitin
sulfate;
5.increased numbers
of adipocytes (fatty
infiltration).
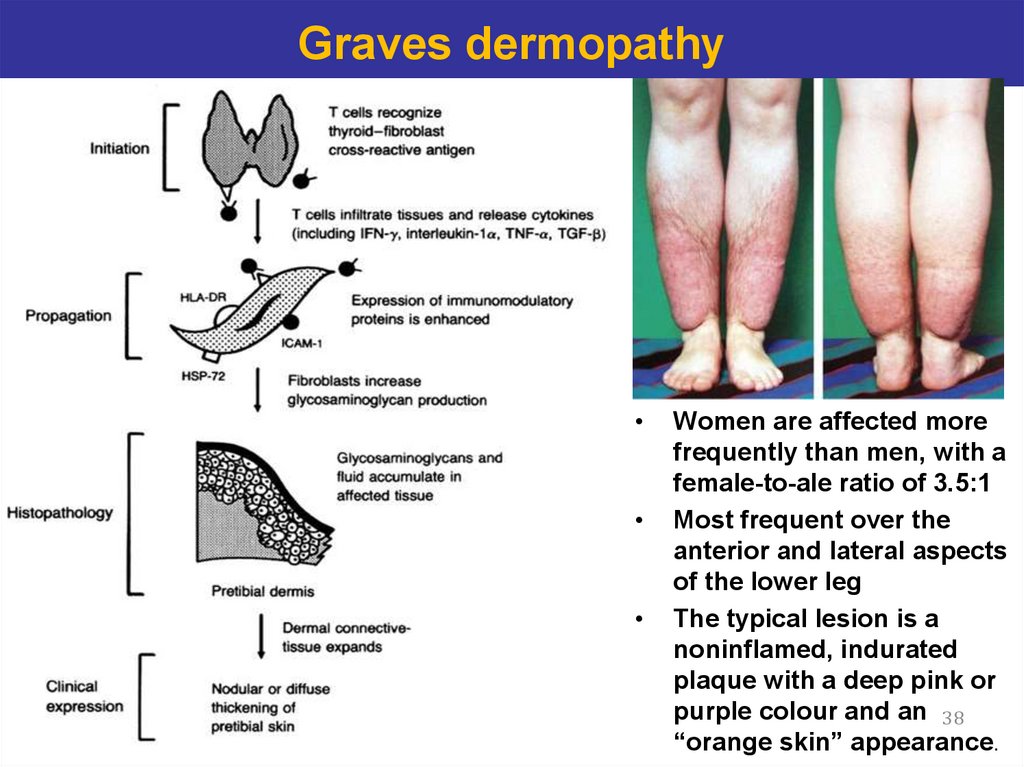
38. Graves dermopathy
Women are affected more
frequently than men, with a
female-to-ale ratio of 3.5:1
Most frequent over the
anterior and lateral aspects
of the lower leg
The typical lesion is a
noninflamed, indurated
plaque with a deep pink or
purple colour and an 38
“orange skin” appearance.
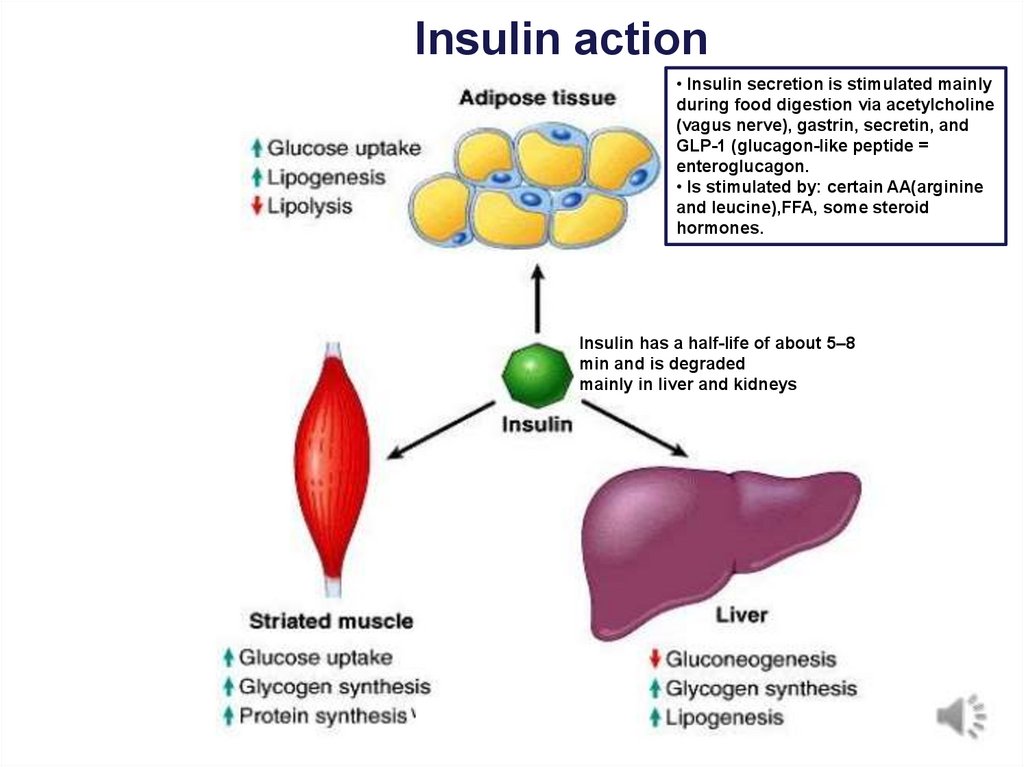
39. Insulin action
• Insulin secretion is stimulated mainlyduring food digestion via acetylcholine
(vagus nerve), gastrin, secretin, and
GLP-1 (glucagon-like peptide =
enteroglucagon.
• Is stimulated by: certain AA(arginine
and leucine),FFA, some steroid
hormones.
Insulin has a half-life of about 5–8
min and is degraded
mainly in liver and kidneys
39
40. Criteria for diagnosis
FPG (fastingplasma glucose)
OGTT (oral
glucose
tolerance test)
Glycated
hemoglobin
(HbA1C)
Normal glucose
homeostasis
<5.6 mmol/L (100
mg/dL)
<140 mg/dL (7,7
mmol/L)
<5.6%
Abnormal
glucose
homeostasis
(prediabetes)
5.6–6.9 mmol/L
(100–125 mg/dL)
7.8 - 11 mmol/L
(140 - 199
mg/dL)
5.7–6.4%.
>11.1 mmol/L
(200 mg/dL)
≥6.5%
Diabetes mellitus ≥7.0 mmol/L (126
mg/dL)
Diabetes mellitus
Symptoms of diabetes (polyuria, polydipsia, weight
40
loss) plus random blood glucose concentration ≥11.1 mmol/(200
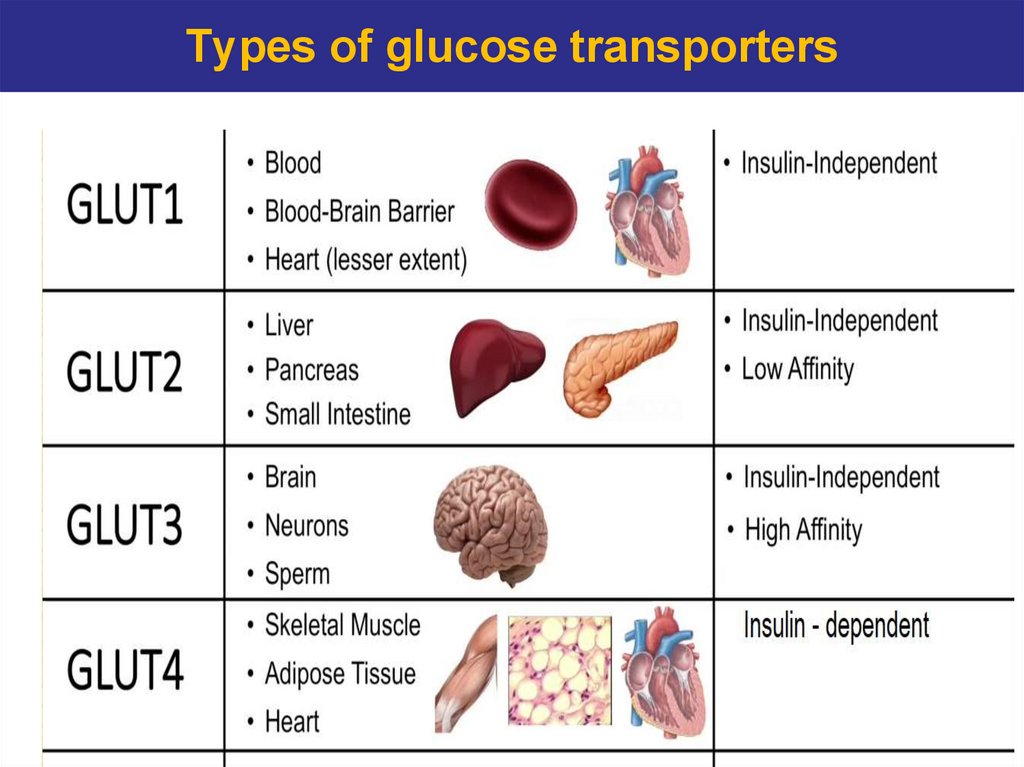
41. Types of glucose transporters
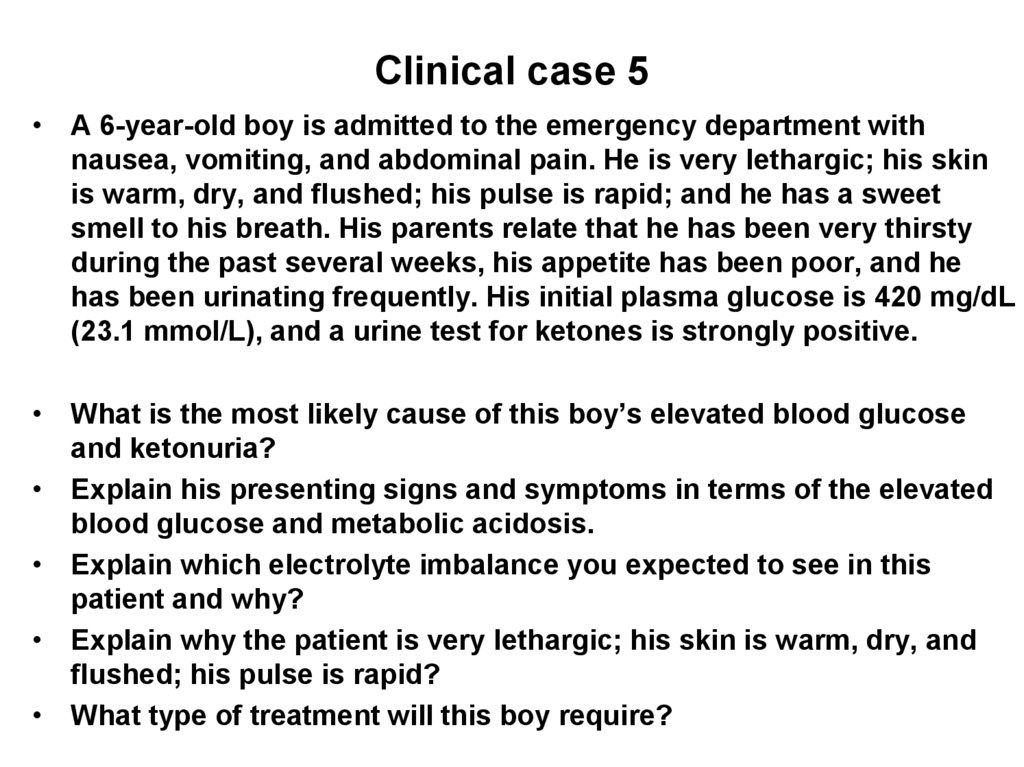
4142. Clinical case 5
• A 6-year-old boy is admitted to the emergency department withnausea, vomiting, and abdominal pain. He is very lethargic; his skin
is warm, dry, and flushed; his pulse is rapid; and he has a sweet
smell to his breath. His parents relate that he has been very thirsty
during the past several weeks, his appetite has been poor, and he
has been urinating frequently. His initial plasma glucose is 420 mg/dL
(23.1 mmol/L), and a urine test for ketones is strongly positive.
• What is the most likely cause of this boy’s elevated blood glucose
and ketonuria?
• Explain his presenting signs and symptoms in terms of the elevated
blood glucose and metabolic acidosis.
• Explain which electrolyte imbalance you expected to see in this
patient and why?
• Explain why the patient is very lethargic; his skin is warm, dry, and
flushed; his pulse is rapid?
• What type of treatment will this boy require?
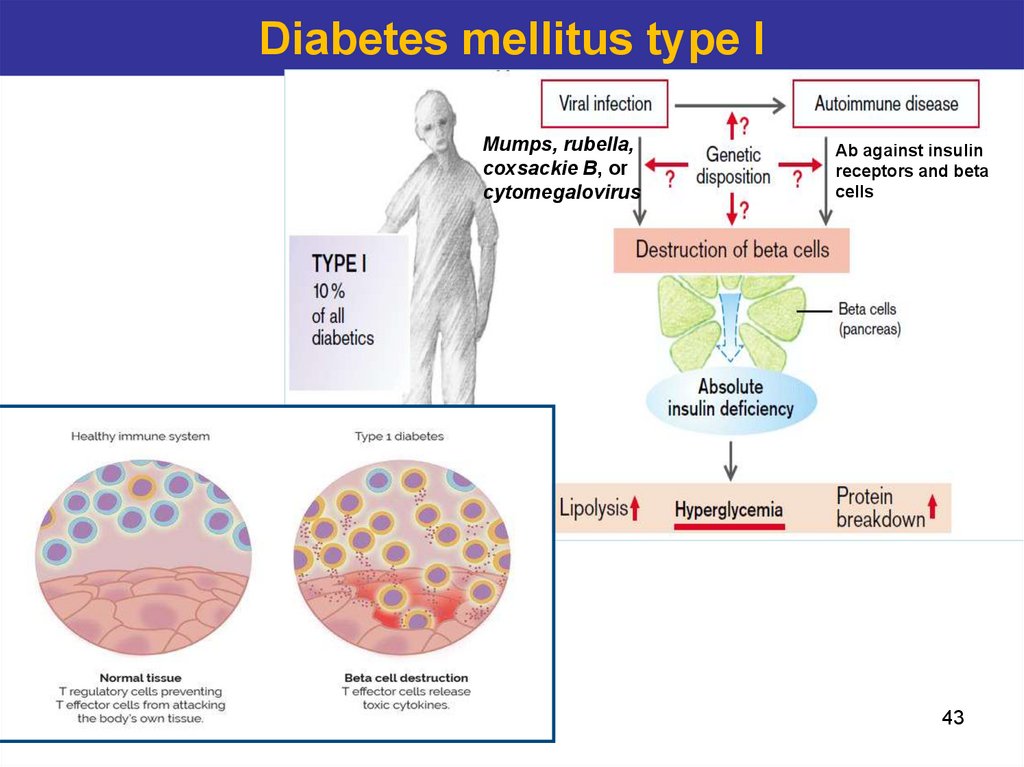
43. Diabetes mellitus type I
Mumps, rubella,coxsackie B, or
cytomegalovirus
Ab against insulin
receptors and beta
cells
43
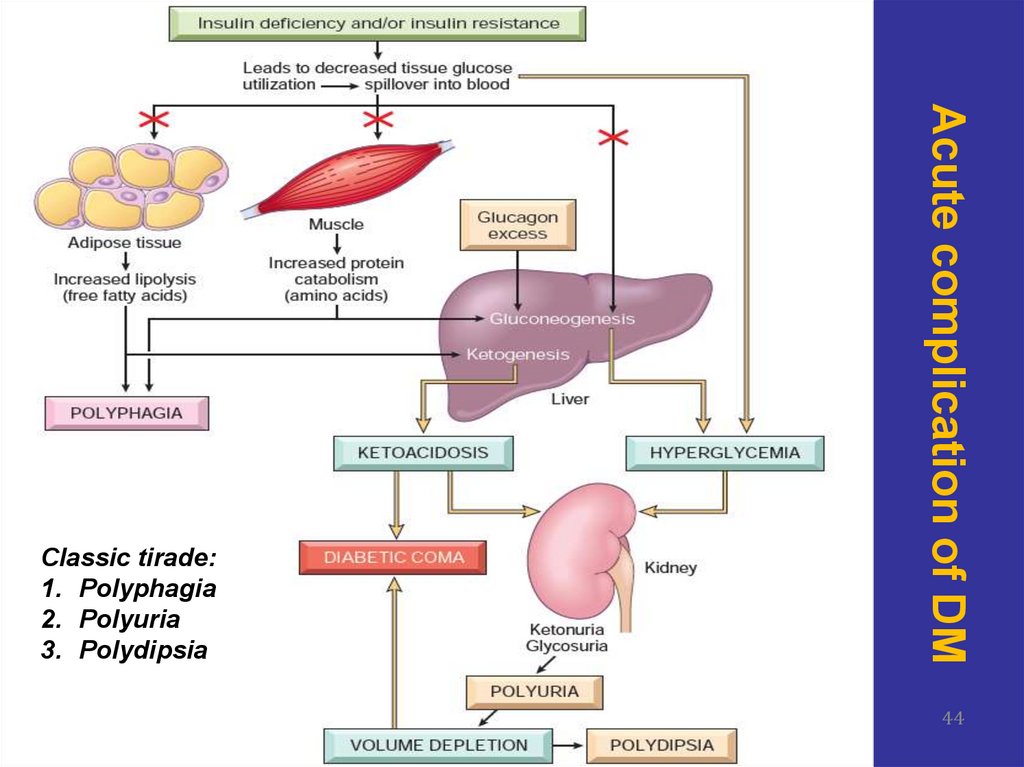
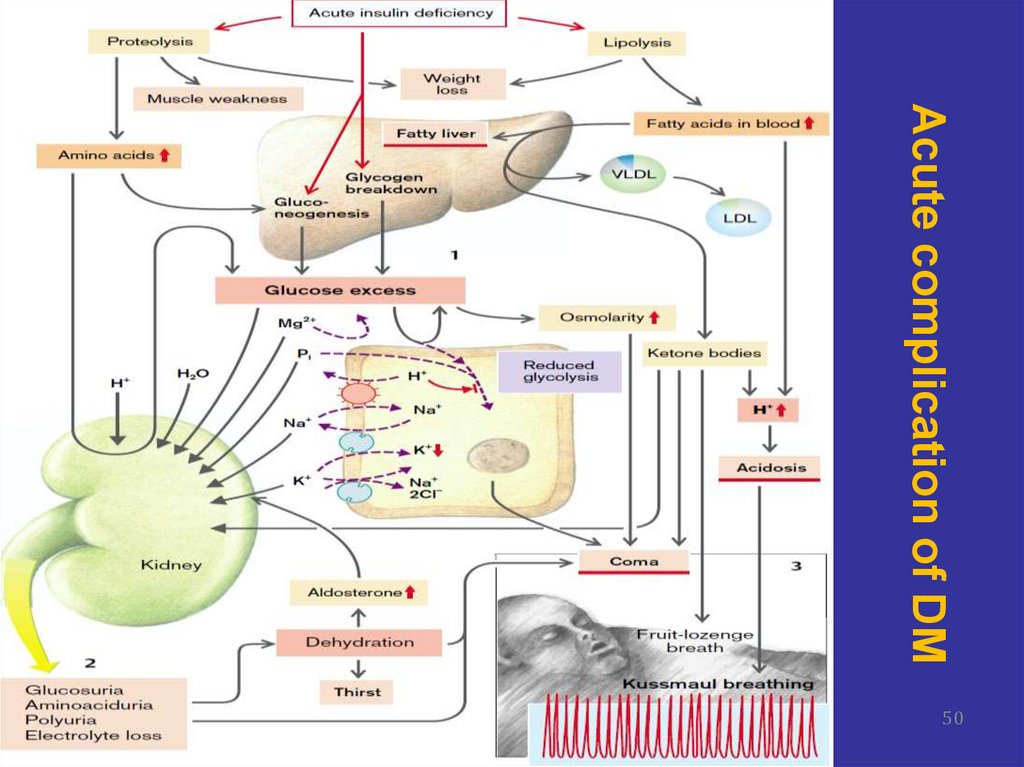
44. Acute complication of DM
Classic tirade:1. Polyphagia
2. Polyuria
3. Polydipsia
44
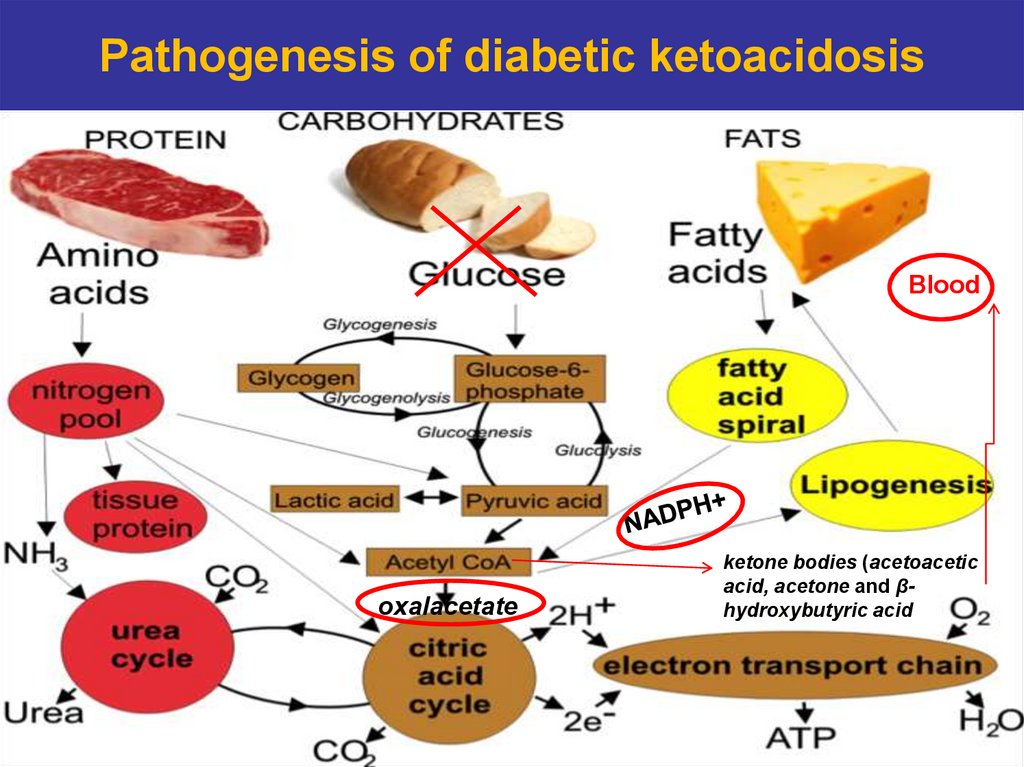
45. Pathogenesis of diabetic ketoacidosis
Bloodoxalacetate
ketone bodies (acetoacetic
acid, acetone and βhydroxybutyric acid
45
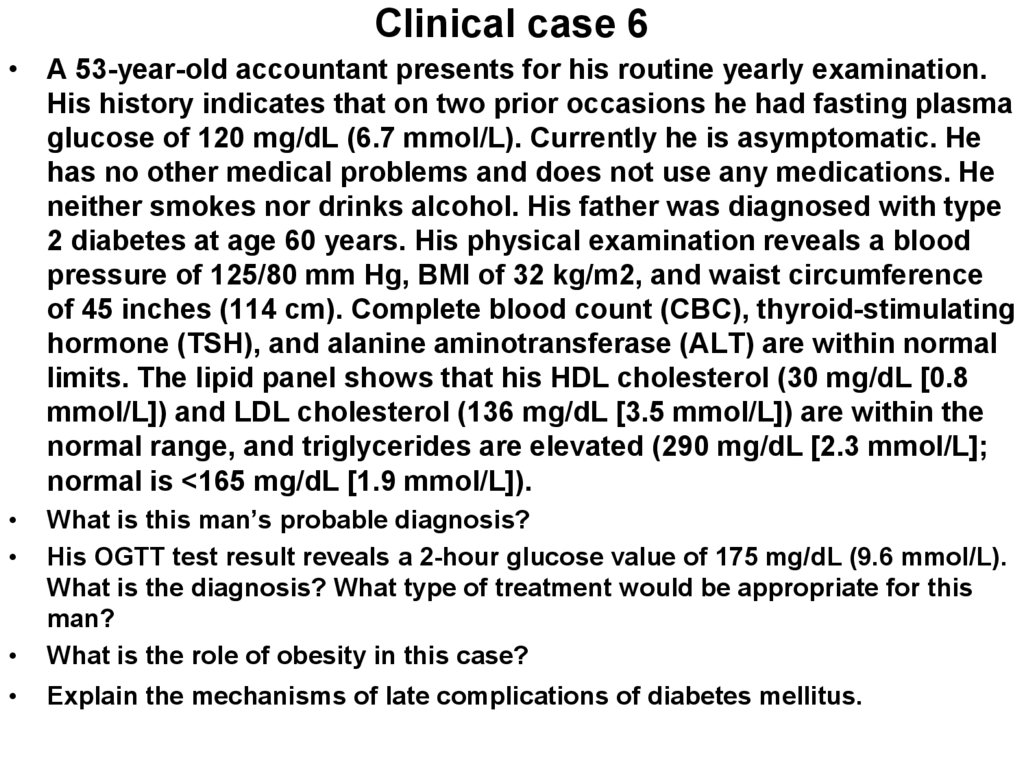
46. Clinical case 6
• A 53-year-old accountant presents for his routine yearly examination.His history indicates that on two prior occasions he had fasting plasma
glucose of 120 mg/dL (6.7 mmol/L). Currently he is asymptomatic. He
has no other medical problems and does not use any medications. He
neither smokes nor drinks alcohol. His father was diagnosed with type
2 diabetes at age 60 years. His physical examination reveals a blood
pressure of 125/80 mm Hg, BMI of 32 kg/m2, and waist circumference
of 45 inches (114 cm). Complete blood count (CBC), thyroid-stimulating
hormone (TSH), and alanine aminotransferase (ALT) are within normal
limits. The lipid panel shows that his HDL cholesterol (30 mg/dL [0.8
mmol/L]) and LDL cholesterol (136 mg/dL [3.5 mmol/L]) are within the
normal range, and triglycerides are elevated (290 mg/dL [2.3 mmol/L];
normal is <165 mg/dL [1.9 mmol/L]).
What is this man’s probable diagnosis?
His OGTT test result reveals a 2-hour glucose value of 175 mg/dL (9.6 mmol/L).
What is the diagnosis? What type of treatment would be appropriate for this
man?
What is the role of obesity in this case?
Explain the mechanisms of late complications of diabetes mellitus.
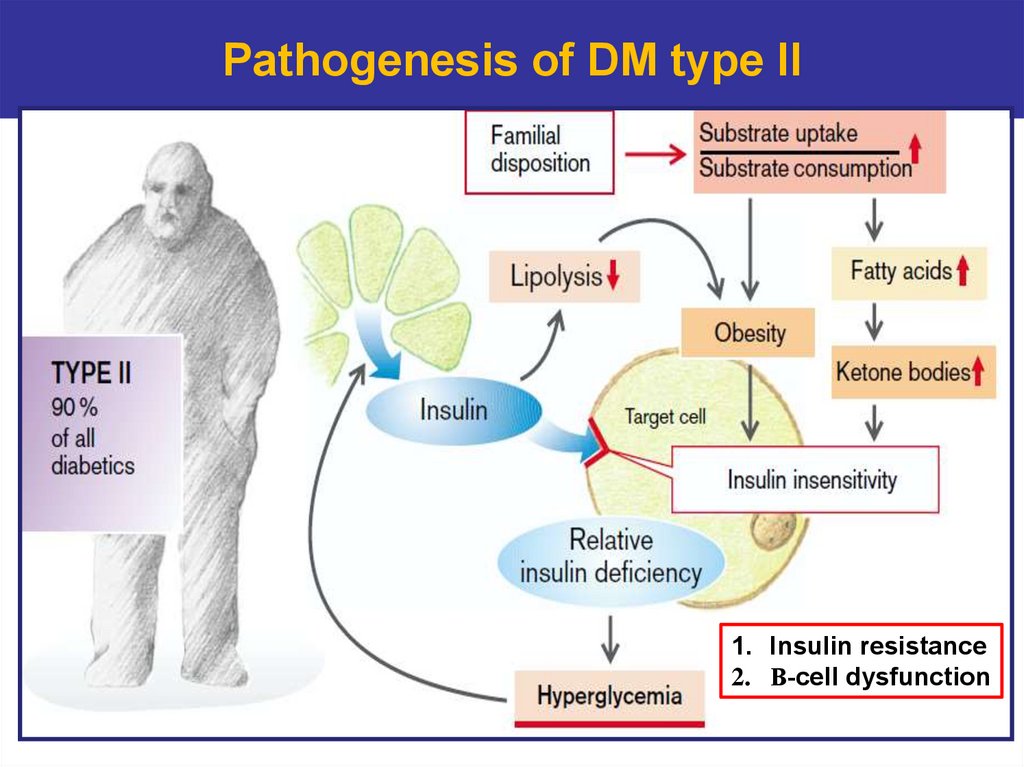
47. Pathogenesis of DM type II
1. Insulin resistance2. Β-cell dysfunction
47
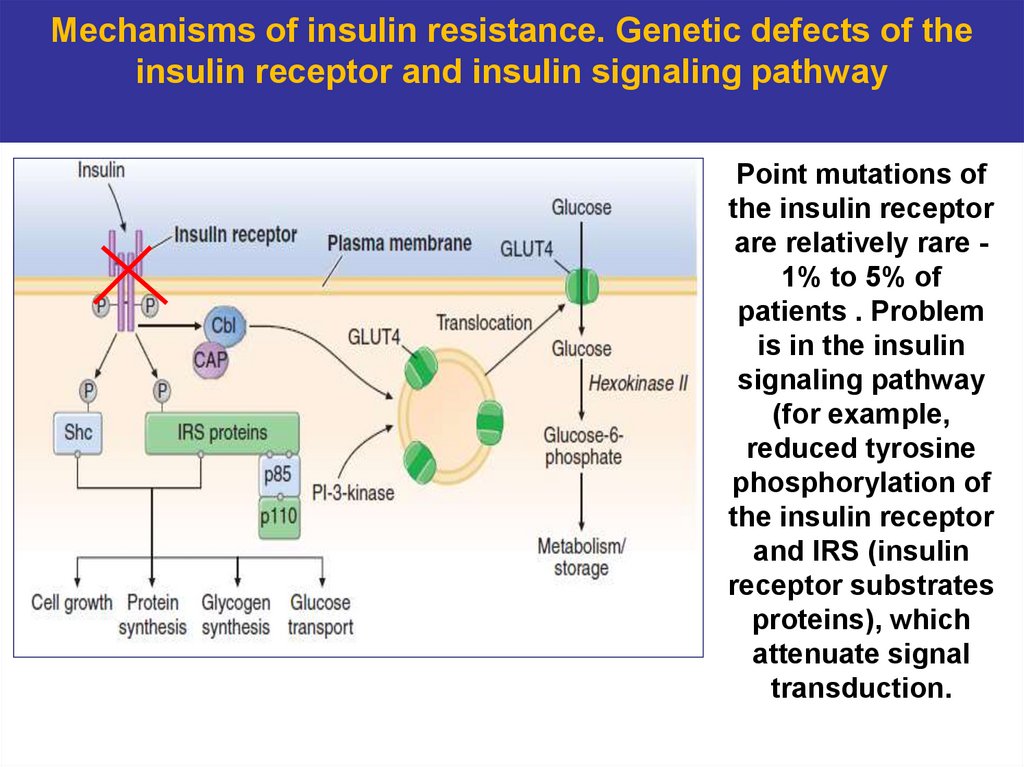
48. Mechanisms of insulin resistance. Genetic defects of the insulin receptor and insulin signaling pathway
Point mutations ofthe insulin receptor
are relatively rare 1% to 5% of
patients . Problem
is in the insulin
signaling pathway
(for example,
reduced tyrosine
phosphorylation of
the insulin receptor
and IRS (insulin
receptor substrates
proteins), which
attenuate signal
transduction.
48
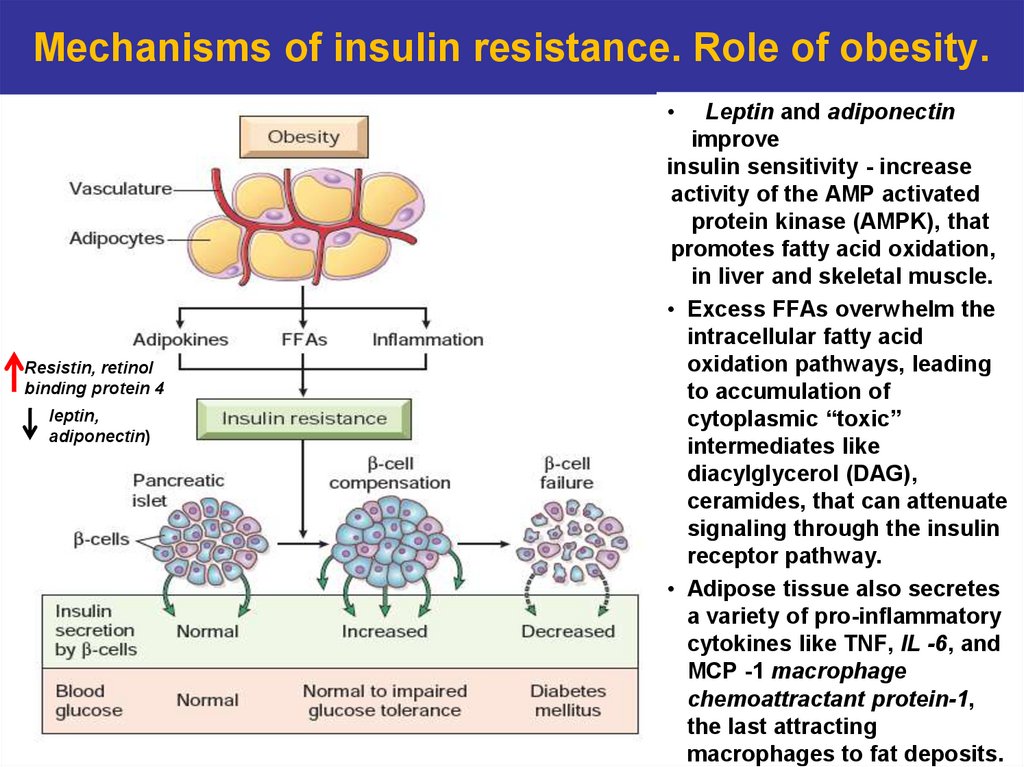
49. Mechanisms of insulin resistance. Role of obesity.
Resistin, retinol
binding protein 4
leptin,
adiponectin)
Leptin and adiponectin
improve
insulin sensitivity - increase
activity of the AMP activated
protein kinase (AMPK), that
promotes fatty acid oxidation,
in liver and skeletal muscle.
• Excess FFAs overwhelm the
intracellular fatty acid
oxidation pathways, leading
to accumulation of
cytoplasmic “toxic”
intermediates like
diacylglycerol (DAG),
ceramides, that can attenuate
signaling through the insulin
receptor pathway.
• Adipose tissue also secretes
a variety of pro-inflammatory
cytokines like TNF, IL -6, and
MCP -1 macrophage
chemoattractant protein-1,
the last attracting
macrophages to fat deposits.
50. Acute complication of DM
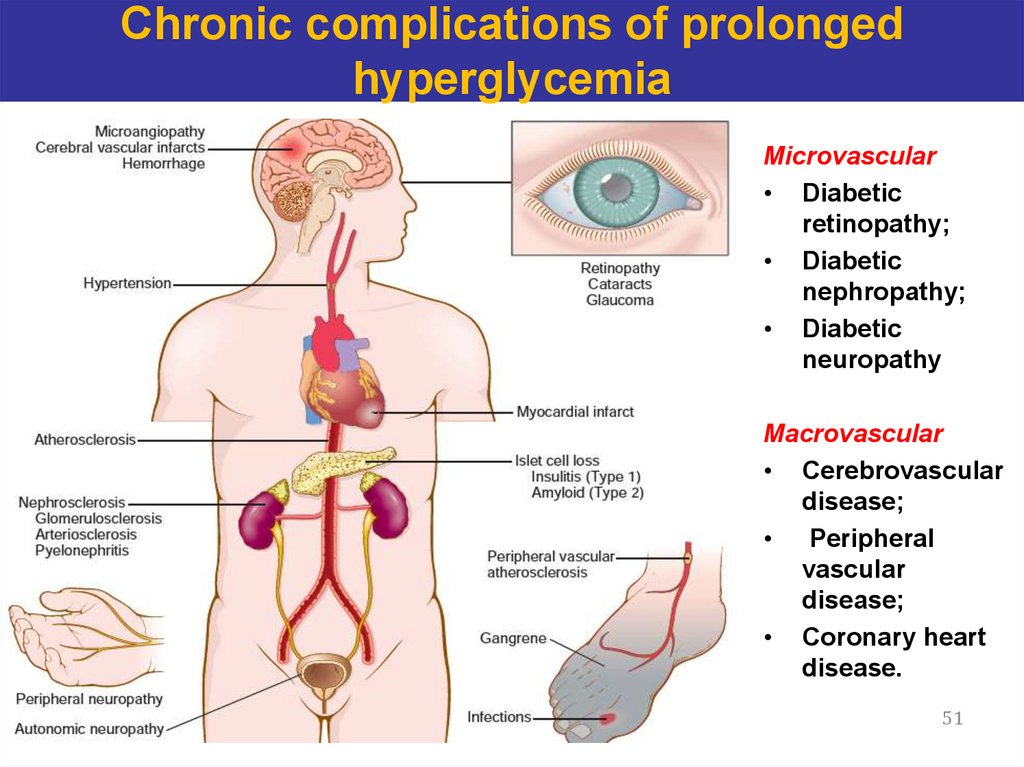
5051. Chronic complications of prolonged hyperglycemia
Microvascular• Diabetic
retinopathy;
• Diabetic
nephropathy;
• Diabetic
neuropathy
Macrovascular
• Cerebrovascular
disease;
• Peripheral
vascular
disease;
• Coronary heart
disease.
51
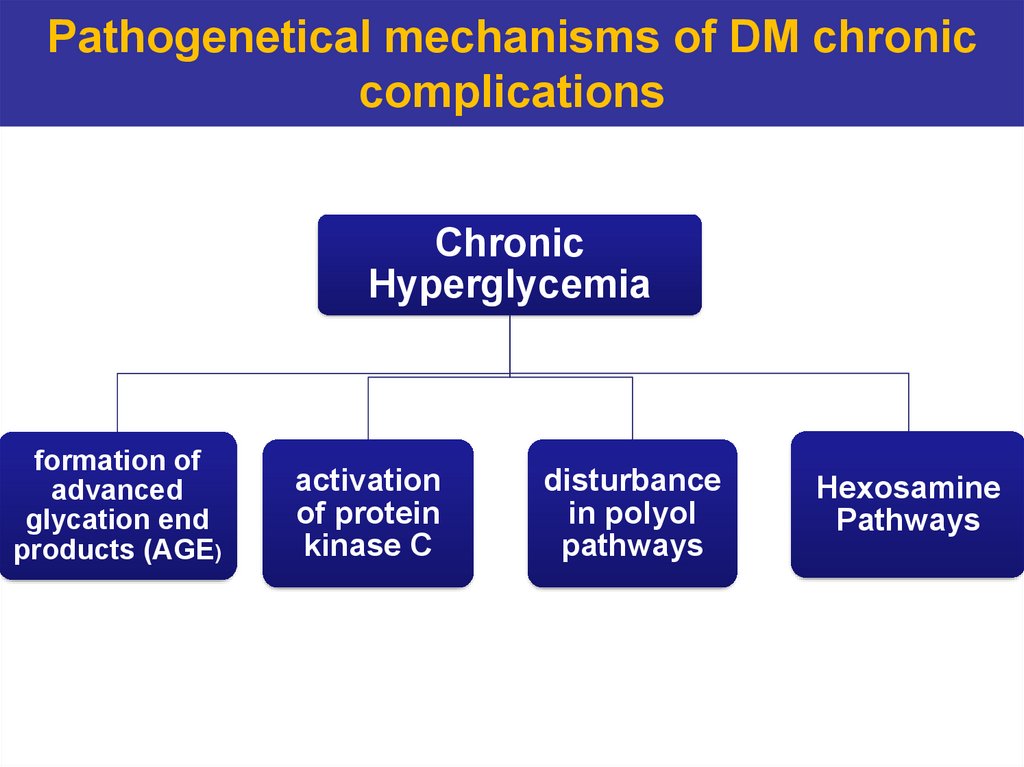
52. Pathogenetical mechanisms of DM chronic complications
ChronicHyperglycemia
formation of
advanced
glycation end
products (AGE)
activation
of protein
kinase C
disturbance
in polyol
pathways
Hexosamine
Pathways
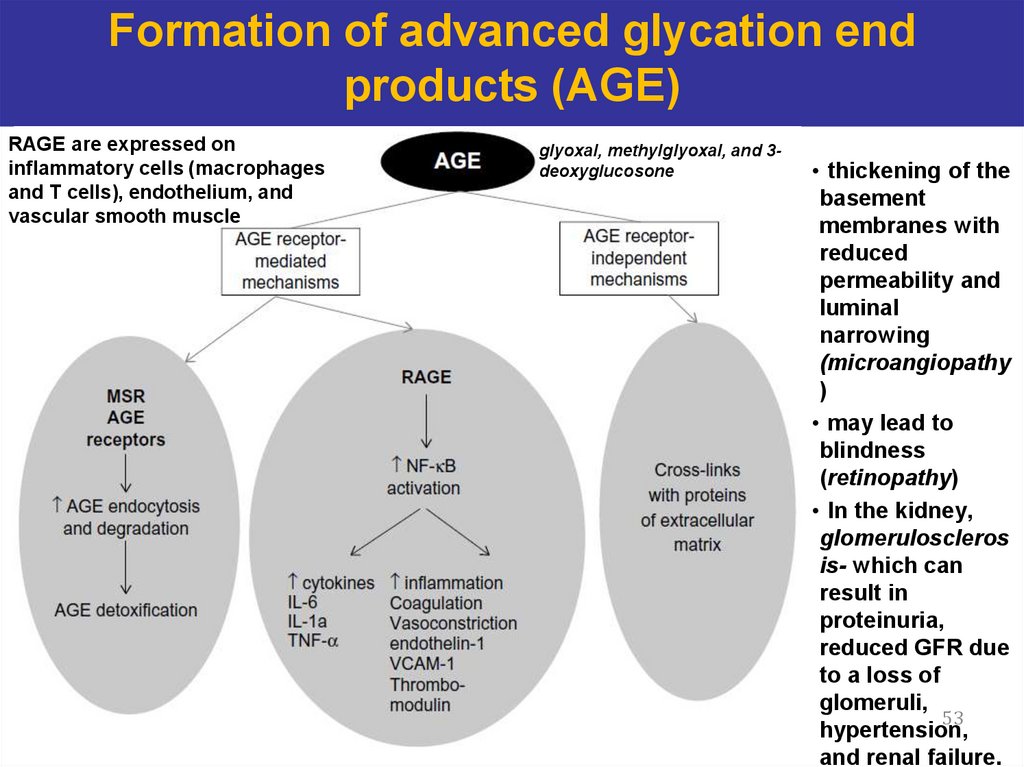
53. Formation of advanced glycation end products (AGE)
RAGE are expressed oninflammatory cells (macrophages
and T cells), endothelium, and
vascular smooth muscle
glyoxal, methylglyoxal, and 3deoxyglucosone
• thickening of the
basement
membranes with
reduced
permeability and
luminal
narrowing
(microangiopathy
)
• may lead to
blindness
(retinopathy)
• In the kidney,
glomeruloscleros
is- which can
result in
proteinuria,
reduced GFR due
to a loss of
glomeruli,
53
hypertension,
and renal failure.
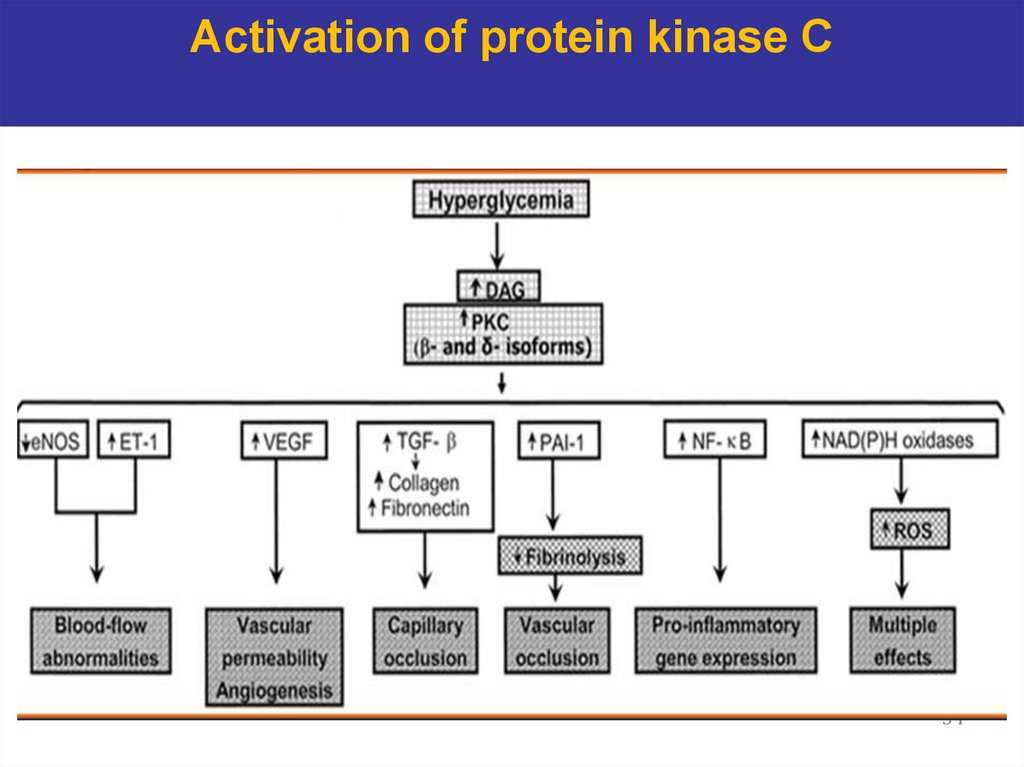
54. Activation of protein kinase C
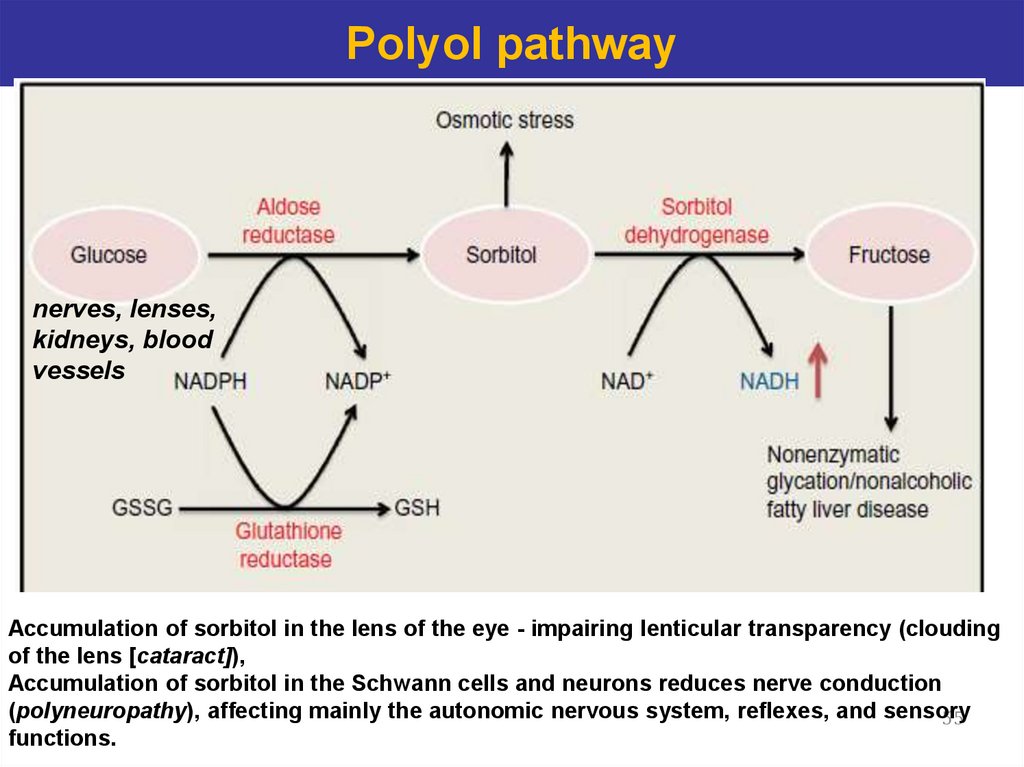
5455. Polyol pathway
nerves, lenses,kidneys, blood
vessels
Accumulation of sorbitol in the lens of the eye - impairing lenticular transparency (clouding
of the lens [cataract]),
Accumulation of sorbitol in the Schwann cells and neurons reduces nerve conduction
(polyneuropathy), affecting mainly the autonomic nervous system, reflexes, and sensory
55
functions.
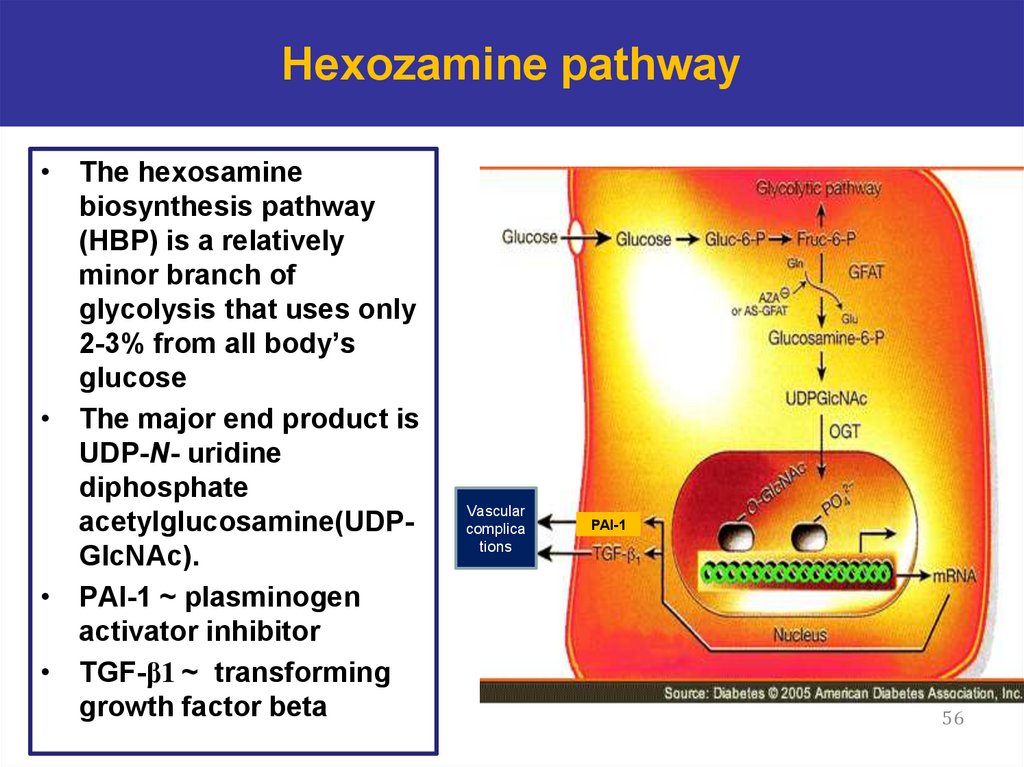
56. Hexozamine pathway
• The hexosaminebiosynthesis pathway
(HBP) is a relatively
minor branch of
glycolysis that uses only
2-3% from all body’s
glucose
• The major end product is
UDP-N- uridine
diphosphate
acetylglucosamine(UDPGlcNAc).
• PAI-1 ~ plasminogen
activator inhibitor
• TGF-β1 ~ transforming
growth factor beta
Vascular
complica
tions
PAI-1
56








 Биология
Биология








