Похожие презентации:
Vision Therapy
1. Vision Therapy
Dr. Rajnish KishoreRachana Eye Care & Optical
Hetauda, Makwanpur
2. What is Vision Therapy?
Vision therapy (visual training,vision training) is an individualized
supervised treatment program
designed to correct visual-motor
and/or perceptual-cognitive
deficiencies
3. Why Vision Therapy?
Behavioral Optometrists believe that visionis a learned skill; Vision plays the largest
role in learning.
“There's more to vision than just having 20/20
eyesight. A strong visual system is needed for
reading, using a computer, and playing sports.”
4. Vision Related Learning Problems
Physical Symptoms• Jerky eye movements, one
eye turning in or out
• Squinting, eye rubbing, or
excessive blinking
• Blurred or double vision
• Headaches, dizziness, or
nausea after reading
• Head tilting, closing or
blocking one eye when
reading
Secondary Symptoms
• Smart in everything but
school
• Low self-esteem, poor self
image
• Temper flare ups,
aggressiveness
• Frequent crying
• Short attention span
• Fatigue, frustration, stress
• Irritability
• Day dreaming
5. Vision Related Learning Problems
Performance Clues• Avoidance of near work
• Frequent loss of place
• Omits, inserts, or rereads
letters/words
• Confuses similar looking words
• Failure to recognize the same
word in the next sentence
• Poor reading comprehension
• Difficulty copying from the
chalkboard
• Book held too close to the eyes
• Inconsistent or poor sports
performance
Social Labels
• Lazy
• Dyslexic
• Attention Deficit Disorder
• Slow learner
• Behavioral problems
• Working below potential
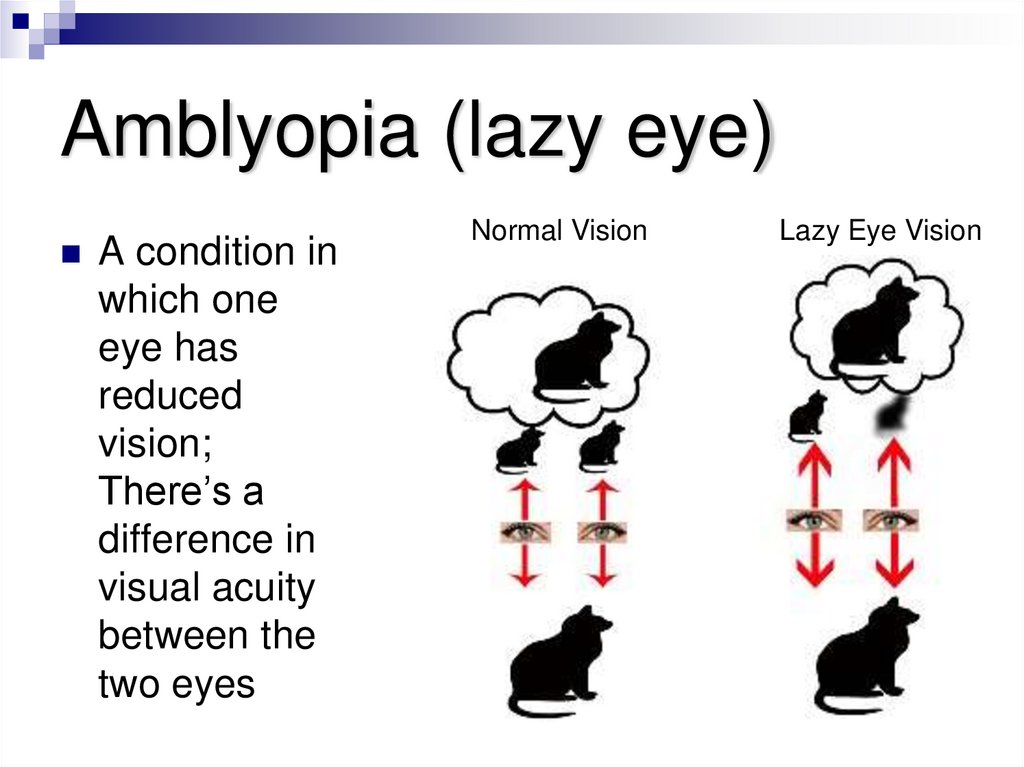
6. Amblyopia (lazy eye)
A condition inwhich one
eye has
reduced
vision;
There’s a
difference in
visual acuity
between the
two eyes
Normal Vision
Lazy Eye Vision
7. Causes
An obstruction of vision within one eye due toinjury or disease
Significant differences between the clearness
of the images seen by each eye due to
farsightedness, nearsightedness or
astigmatism
Misaligned eyes or crossed eyes (strabismus)
8. Clinical Symptoms
Frequent squinting or closing one eye to see,poor visual acuity, eyestrain, headaches
Lack of brain stimulation from the weaker eye
causes the strong eye to become dominant. The
amblyopic eye is suppressed and may even
become blind.
While an amblyopic eye may look normal, it is
not being used normally.
9. Early Diagnosis
Amblyopia can be prevented through early diagnosis andtreatment. Without treatment, an amblyopic eye may
never develop properly, and even become blind. Some
vision loss can be restored if the diagnosis is early
enough, usually before age 5. This early treatment is
necessary because an amblyopic eye has problems in
its connections with the brain, rather than in and of itself.
Often, it is first necessary to treat the underlying cause of
amblyopia before strengthening the child’s weaker eye.
10. Treatment Options
Wearing eyeglasses or contact lenses to align or focusthe eyes
Wearing a patch on the stronger eye for weeks or
months, which forces the amblyopic eye to work,
developing more connections with the brain.
Surgery on the eye muscles
A program of Vision Therapy to help equalize vision in
both eyes, improve eye coordination, and restore clear
single vision.
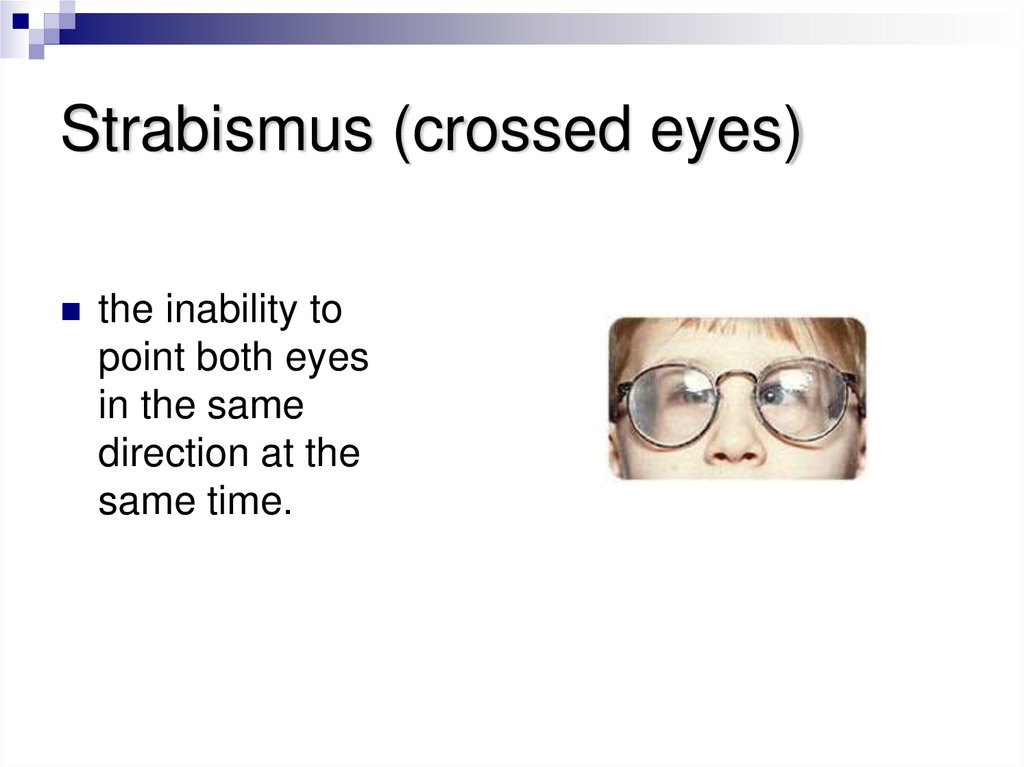
11. Strabismus (crossed eyes)
the inability topoint both eyes
in the same
direction at the
same time.
12. Causes
Inadequate development of eye coordination inchildhood
Excessive farsightedness (hyperopia) or
differences between the vision in each eye
Problems with the eye muscles that control eye
movement
Head trauma, stroke, or other general health
problems.
13. Symptoms
One eye may appear to turn in (estropia), out (extropia),up (hypertropia), or down (hypotropia).
The eye turn may occur constantly or only occasionally
(intermittent).
Eye-turning may change from one eye to the other
(alternating).
Eye-turning may only appear when a person is tired or
has done a lot of reading.
Double vision may occur.
To avoid seeing double, vision in one eye may be
ignored resulting in a lazy eye (amblyopia).
14. Treatment
EyeglassesVision Therapy
Eye muscle surgery.
15. VT Approach & Techniques
VT Approach & TechniquesBest Diagnostic Approach: Combined Programs and Homework
Therapy Sessions include: Home Checks, Diagnosis, Tutoring, 30
minute sessions each
Therapeutic lenses (regulated medical devices)
Prisms (regulated medical devices)
Filters
Occluders or patches
Electronic targets with timing mechanisms
Computer software
Balance boards
16. VT Approach & Techniques
VT Approach & TechniquesMonocular activities designed to equalize the focusing,
tracking and pointing of each eye.
Binocular work to improve eye-teaming efficiency.
Visual-spatial tasks to develop integrated sequential and
directional concepts.
Form training stressing: visual discrimination, spatial
relationships, form constancy, figure/ground relationships and
visual closure.
A visualization program to improve the speed and span of
visual recognition as they pertain to short and long-term visual
memory.
Visuo-motor tasks to improve body awareness and control,
and visually directed fine motor skills.
Inter-sensory integration skills through visualauditory-verbal
matching.
17. Demonstrations
Pencil Tracking, Ball TrackingBlocks
Eye Patches
Prisms
Visual-motor Task
Body Balance
Paper Tearing
18. Research Studies
Binocular DysfunctionsBACKGROUND: Although vision therapy has reportedly been very successful in
elimination of asthenopic symptoms (excessive tearing, itching, burning, visual
fatigue, and headache) in adults with convergence insufficiency, controlled
studies have not been performed, and a clinical bias exists against prescribing
vision therapy for adults with convergence insufficiency.
METHODS: Sixty adult males over the age of 40 years (median age, 65 years)
with convergence insufficiency were divided into three treatment groups: officebased vision therapy with supplementary home therapy, home therapy only, and
a control group.
RESULTS: Vision therapy was successful in 61.9% of patients who received inoffice plus home therapy, in 30% of patients who received home therapy only,
and in 10.5% of the control group. The success rate for patients who received
active in-office vision therapy supplemented with home procedures was
significantly greater than that for controls. Home therapy alone was less
successful than in-office therapy. The success rate obtained with home therapy
alone was not significantly greater than that demonstrated by controls.
CONCLUSIONS: Vision therapy is effective in eliminating asthenopia (eyestrain)
and improving convergence function in adult patients. In-office therapy
combined with home therapy tends to produce better results than does home
therapy alone. (Birnbaum MH, Soden R, Cohen AH. Efficacy of vision
therapy for convergence insufficiency in an adult male population. Journal
of the American Optometric Association, April; 70(4): 225-232, 1999.)
19. Research Studies
AmblyopiaBACKGROUND: The pediatric clinic of the SUNY State College of
Optometry/University Optometric Center (New York) develops a yearly quality
management plan to monitor patient care. One of the areas retrospectively
reviewed for all outcomes is refractive amblyopia.
METHODS: A retrospective review of records was performed on patients
diagnosed with refractive amblyopia. With the use of a prescribed protocol, each
patient's progress was tracked for a period of 6 months. Major emphasis was
placed on outcome as related to treatment modality. Treatment alternatives
were optical correction alone, optical correction in conjunction with patching, and
optical correction and patching with vision therapy.
RESULTS: Improvement criteria included a 2-line increase in visual acuity on
the Snellen chart and an increase of 20 seconds of arc of stereopsis, as
measured by the Wirt circles. The groups that patched with correction and those
that received vision therapy had similar visual acuity improvement's; however,
the latter group had a significantly greater improvement in stereopsis. Both
groups performed significantly better in both categories when compared to the
group receiving optical correction alone.
CONCLUSIONS: Though patching alone may be sufficient for improvement of
visual acuity, binocular performance is significantly better when vision therapy is
included in the treatment regimen. (Krumholtz I, FitzGerald D. Efficacy of
treatment modalities in refractive amblyopia. Journal of the American
Optometric Association, June; 70(6): 399-404, 1999.)
20. Research Studies
StrabismusBACKGROUND: Occasionally, co-management involving both optometry and
ophthalmology is needed to optimize treatment outcome for the strabismic
patient. METHODS: JB, a 47-month-old consecutive esotrope presented to our
clinic (Southern California College of Optometry). Two previous attempts to
surgically correct her exotropia had failed and the parents sought another
treatment approach. We recommended optometric vision therapy (VT) to
improve sensorimotor fusion before any further surgery. After 31 VT sessions
(bi-weekly for a time, then weekly), before a third scheduled surgery,
sensorimotor fusion was good in the amblyoscope, but unstable with
neutralizing prism in free-space. We recommended surgery be postponed, but
the family proceeded. Esotropia recurred with constant suppression. After
additional VT, JB developed stable sensorimotor fusion and random dot
stereopsis in free-space with neutralizing prism. A fourth surgery was then
performed resulting in esophoria at all distances with good sensory fusion.
RESULTS: Twenty-one months postoperatively, JB remains nonstrabismic with
good sensory fusion.
CONCLUSIONS: Clinicians should understand the roles and limitations of
available treatment options. Surgery reduces the magnitude of the deviation,
whereas optometric VT (vision therapy) provides the unique role of establishing
normal sensory processing. (Garriott RS, Heyman CL, Rouse MW. Role of
optometric vision therapy for surgically treated strabismus patients. Optometry
and Vision Science, April;74(4): 179-184, 1997.)
21. References
“About vision problems” Vision-Therapy January 2005 <http://www.visiontherapy.com/About_Vision.htm>“Vision Related Learning Programs” Insight Vision Center
<http://www.insightvision.org/vrlearningprograms.html>
“What is Vision Therapy?” College of Optometrists in Vision Development
<http://www.covd.org/od/vt_whatis.html>
“Unite for Sight Amblyopia Module” Unite for Sight
<http://www.uniteforsight.org/course/amblyopia.php>
“Strabismus/Crossed Eyes” COVD <http://www.covd.org/od/strabismus.html>
“Strabismus – What is it?” Optometrists Network <http://www.strabismus.org/>
“Introduction to Vision & Brain Injury” NORA
<http://www.nora.cc/patient_area/vision_and_brain_injury.html>
“Research Studies & Vision Therapy” Vision-Therapy <http://www.visiontherapy.com/vt_research_studies.htm#Binocular%20Dysfunction>

 Английский язык
Английский язык