Похожие презентации:
Guidelines in Rheumatology
1. Guidelines in Rheumatology
The Diagnosis and Management ofAnkylosing Spondylitis
1
2. Genetic Predisposition for Development of Ankylosing Spondylitis (AS)
• AS and HLA-B27 – strong association• Ethnic and racial variability in presence and
expression of HLA-B27
2
HLA-B27
positive
AS and HLAB27 positive
Western European
Whites
8%
90%
African Americans
2% to 4%
48%
3. Natural History of AS
• Highly variable• Early stages: spontaneous remissions and
exacerbations
• Spectrum of severity
– Mild with limited sacroiliac or lumbar joint
involvement to severe, debilitating disease
• “Pre-spondylitic” phase – unrecognized period
of progressive structural damage over a
5-to-10-year period
– Average delay in diagnosis is 8.9 years
3
4. Burden of Illness
• Functional disability• Potential complications
• Quality-of-life issues
– Pain, stiffness, fatigue, sleep problems
• Healthcare costs = $6720 annually
– 75% indirect medical costs
• Missed workdays
• Limited-activity days
4
5. Obstacles to Desirable Outcomes in AS Until Recently
• Diagnostic and classification limitations• Lack of universally accepted instruments to
assess AS
• Until recently, limited treatment options
– NSAIDs, COX-2 inhibitors, DMARDs
• Mostly symptomatic relief only
• Minimal impact on natural course of disease
5
6. Advances in Medicine: Hope for Patients With AS
• Increased understanding of pathophysiologicprocesses
• Advent of Anti-TNF agents
• International meetings by ASAS (ASsessment in
AS working group) to address need for universal
standards
• Development of ASAS guidelines
– US modifications to the ASAS International
Guidelines to meet realities of clinical practice in the
United States
6
7. Pathogenesis of AS
• Incompletely understood, but knowledgeincreasing
• Interaction between HLA-B27 and T-cell
response
• Increased concentration of T-cells,
macrophages, and proinflammatory cytokines
– Role of TNF
• Inflammatory reactions produce hallmarks
of disease
7
8. Clinical Features of AS
SkeletalAxial arthritis (eg, sacroiliitis and spondylitis)
Arthritis of ‘girdle joints’ (hips and shoulders)
Peripheral arthritis uncommon
Others: enthesitis, osteoporosis, vertebral,
fractures, spondylodiscitis, pseudoarthrosis
Extraskeletal Acute anterior uveitis
Cardiovascular involvement
Pulmonary involvement
Cauda equina syndrome
Enteric mucosal lesions
Amyloidosis, miscellaneous
8
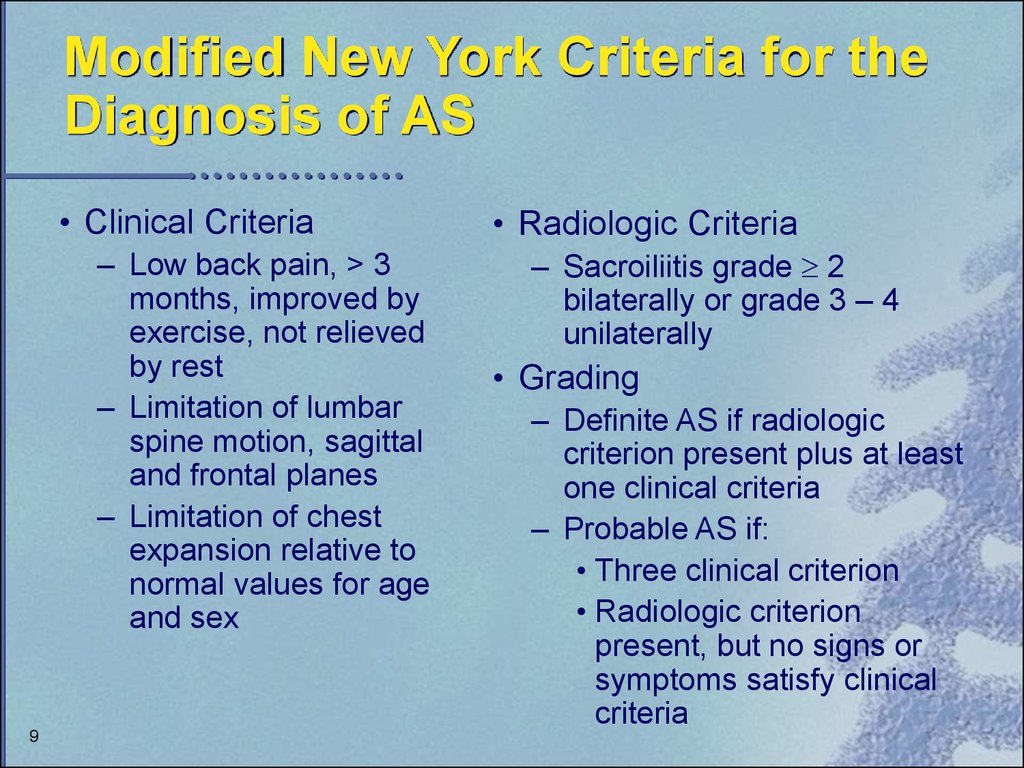
9. Modified New York Criteria for the Diagnosis of AS
• Clinical Criteria– Low back pain, > 3
months, improved by
exercise, not relieved
by rest
– Limitation of lumbar
spine motion, sagittal
and frontal planes
– Limitation of chest
expansion relative to
normal values for age
and sex
9
• Radiologic Criteria
– Sacroiliitis grade 2
bilaterally or grade 3 – 4
unilaterally
• Grading
– Definite AS if radiologic
criterion present plus at least
one clinical criteria
– Probable AS if:
• Three clinical criterion
• Radiologic criterion
present, but no signs or
symptoms satisfy clinical
criteria
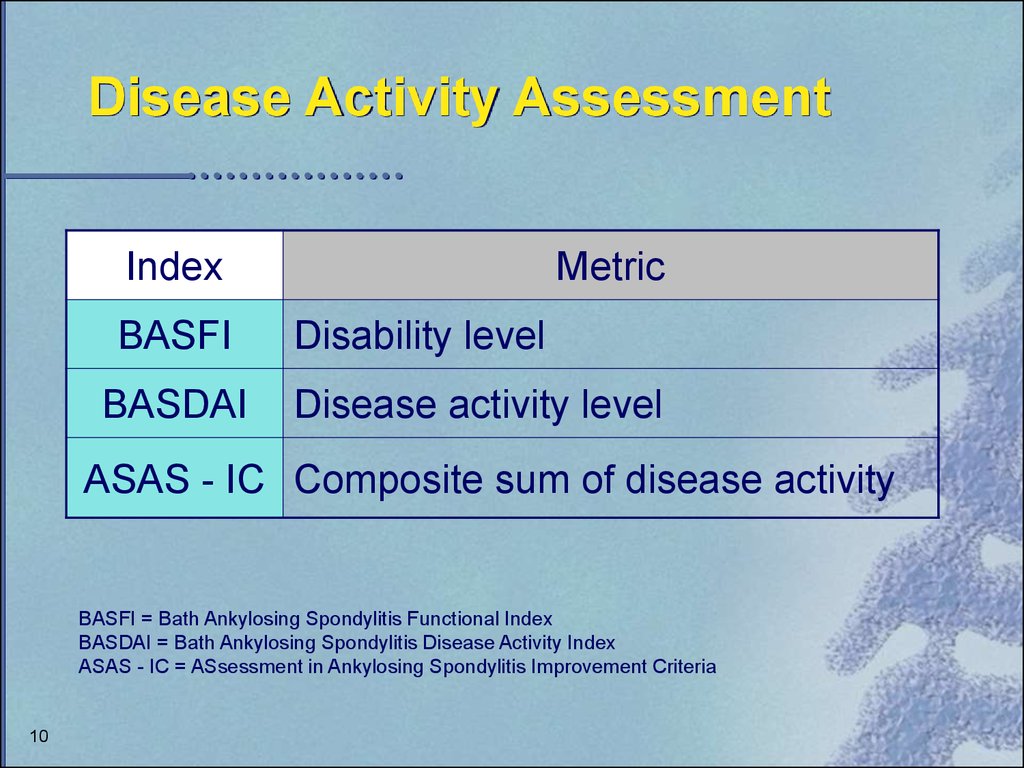
10. Disease Activity Assessment
IndexBASFI
BASDAI
Metric
Disability level
Disease activity level
ASAS - IC Composite sum of disease activity
BASFI = Bath Ankylosing Spondylitis Functional Index
BASDAI = Bath Ankylosing Spondylitis Disease Activity Index
ASAS - IC = ASsessment in Ankylosing Spondylitis Improvement Criteria
10
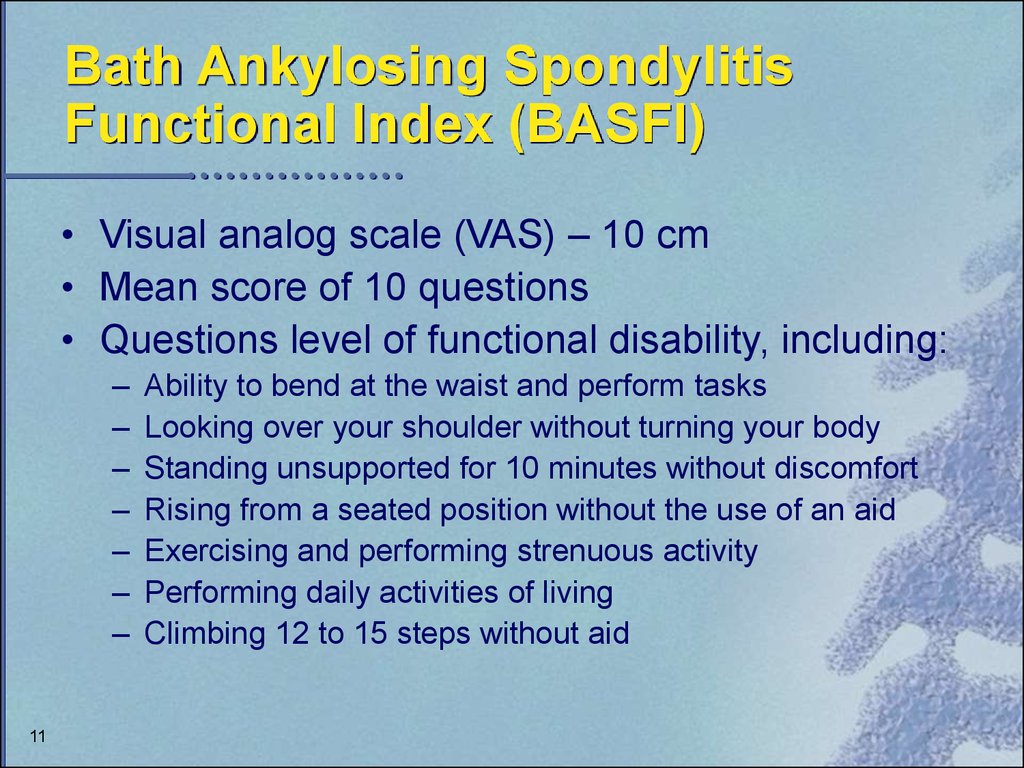
11. Bath Ankylosing Spondylitis Functional Index (BASFI)
• Visual analog scale (VAS) – 10 cm• Mean score of 10 questions
• Questions level of functional disability, including:
–
–
–
–
–
–
–
11
Ability to bend at the waist and perform tasks
Looking over your shoulder without turning your body
Standing unsupported for 10 minutes without discomfort
Rising from a seated position without the use of an aid
Exercising and performing strenuous activity
Performing daily activities of living
Climbing 12 to 15 steps without aid
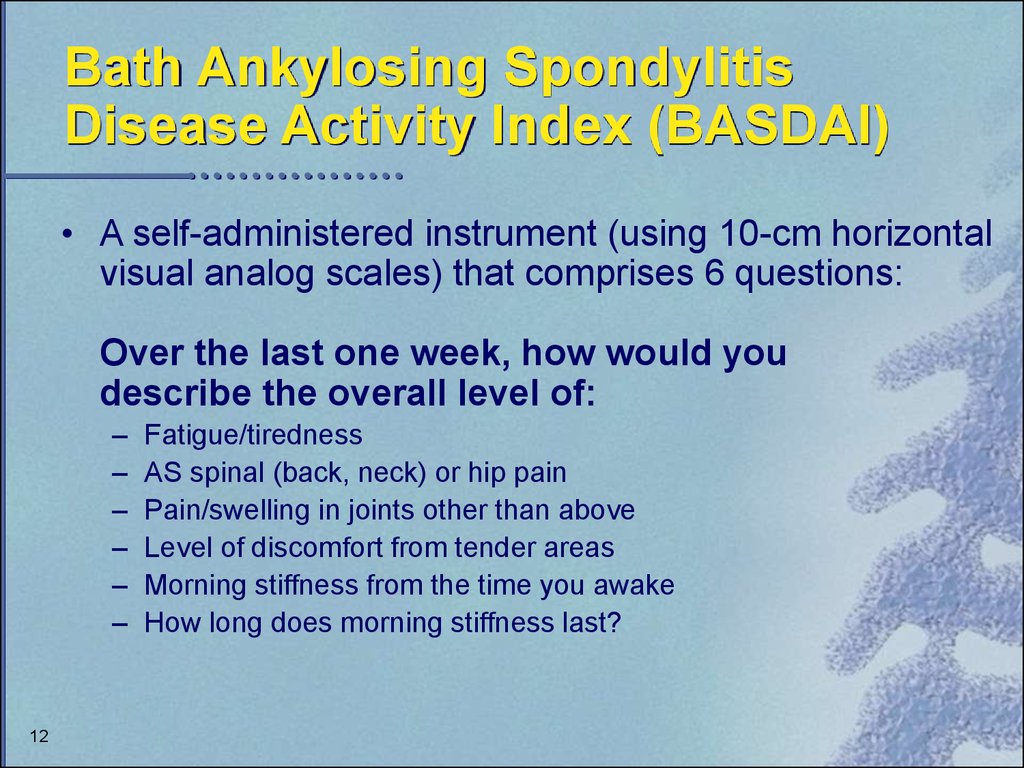
12. Bath Ankylosing Spondylitis Disease Activity Index (BASDAI)
• A self-administered instrument (using 10-cm horizontalvisual analog scales) that comprises 6 questions:
Over the last one week, how would you
describe the overall level of:
–
–
–
–
–
–
12
Fatigue/tiredness
AS spinal (back, neck) or hip pain
Pain/swelling in joints other than above
Level of discomfort from tender areas
Morning stiffness from the time you awake
How long does morning stiffness last?
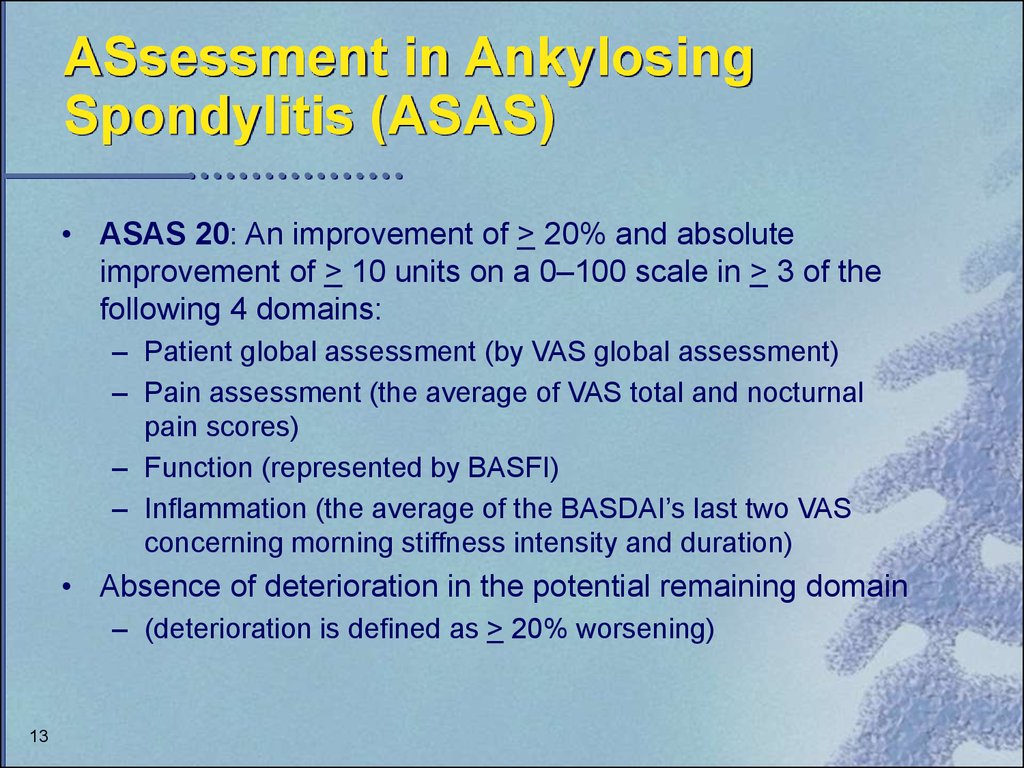
13. ASsessment in Ankylosing Spondylitis (ASAS)
• ASAS 20: An improvement of > 20% and absoluteimprovement of > 10 units on a 0–100 scale in > 3 of the
following 4 domains:
– Patient global assessment (by VAS global assessment)
– Pain assessment (the average of VAS total and nocturnal
pain scores)
– Function (represented by BASFI)
– Inflammation (the average of the BASDAI’s last two VAS
concerning morning stiffness intensity and duration)
• Absence of deterioration in the potential remaining domain
– (deterioration is defined as > 20% worsening)
13
14. Introduction of Anti-TNF Agents for the Treatment of Ankylosing Spondylitis
US Modifications of the ASASInternational Guidelines for Use of
Anti-TNF Agents
14
15. Tumor Necrosis Factor: Functions of the Proinflammatory Cytokine
• Stimulation of endothelial cells to express adhesionmolecules
• Recruitment of white blood cells in inflamed
synovium and skin
• Induction of inflammatory cytokine production
(e.g., IL-1, IL-6)
• Stimulation of synovial cells to release
collagenases
• Induction of bone and cartilage resorption
• Stimulation of fibroblast proliferation
15
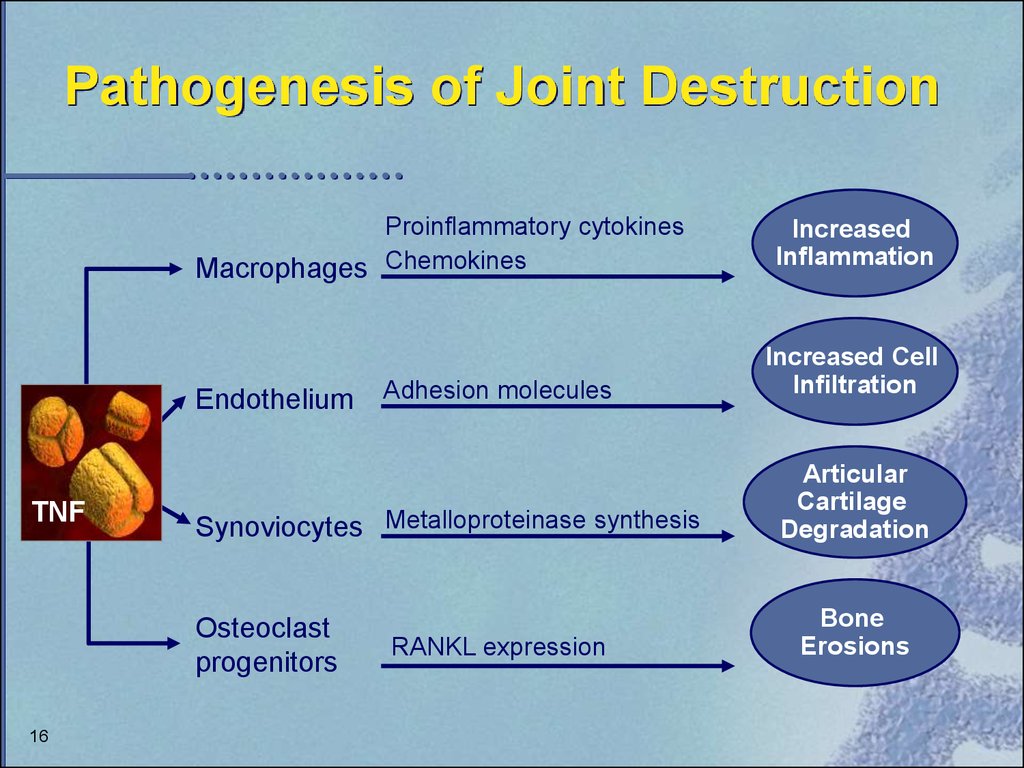
16. Pathogenesis of Joint Destruction
Proinflammatory cytokinesMacrophages Chemokines
Endothelium
TNF
Synoviocytes Metalloproteinase synthesis
Osteoclast
progenitors
16
Adhesion molecules
RANKL expression
Increased
Inflammation
Increased Cell
Infiltration
Articular
Cartilage
Degradation
Bone
Erosions
17. US Modifications of the ASAS International Guidelines: Appropriate Patients for Anti-TNF Therapy
• Definitive AS according to Modified New York Criteria• Active disease for 4 weeks
– BASDAI > 4 cm at two times, 1 month apart
– Physician Global Assessment 2 on Likert Scale
• Treatment Failures
– All types AS – lack of response/intolerability > 2 NSAIDs
for 3 months
– Patients with peripheral arthritis – lack of
response/intolerability to > 1 DMARD, sulfasalazine preferred
17
18. Contraindications for Anti-TNF Therapy
18
Current or recurrent infections
Tuberculosis
Multiple sclerosis
Lupus
Malignancy
Pregnant or lactating
19. Monitoring and Discontinuing Treatment With Anti-TNF Agents
• ASAS core set of outcome parameters tomonitor patients
– Physical function, pain, spinal mobility, patient’s
global assessment, stiffness, peripheral joints and
entheses, acute phase reactant, fatigue
• Assess at 6 to 8 weeks and discontinue
patients who do not meet response criteria
– BASDAI: Reduction of 2 units and
– Physician Global Assessment > 1
19
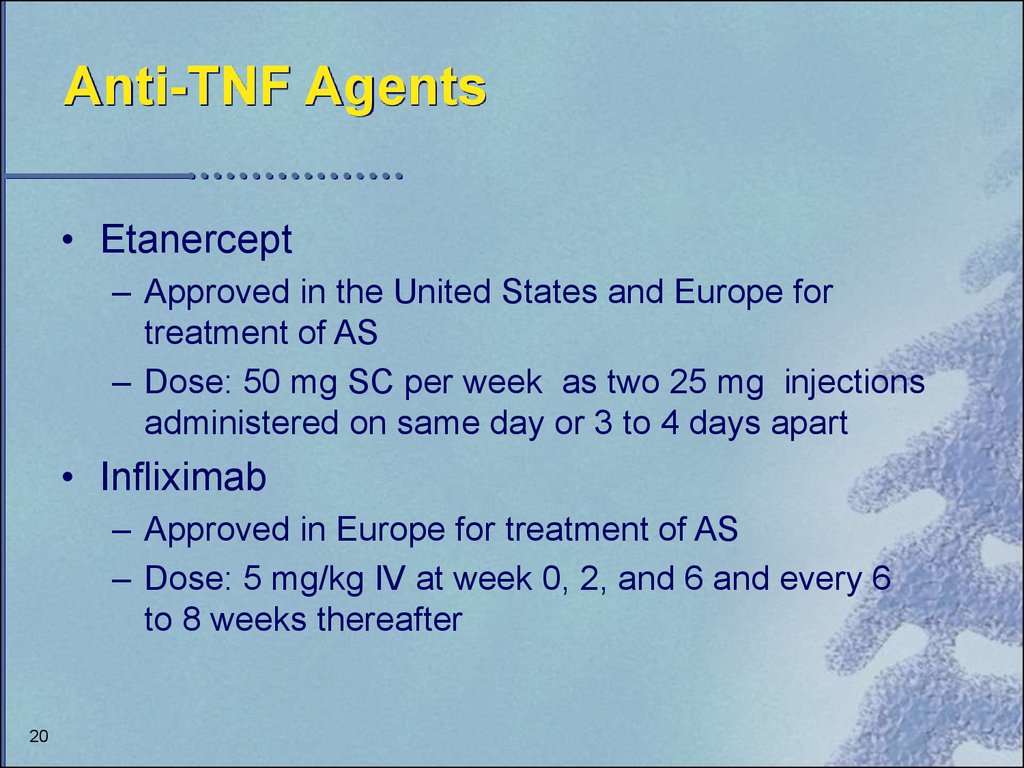
20. Anti-TNF Agents
• Etanercept– Approved in the United States and Europe for
treatment of AS
– Dose: 50 mg SC per week as two 25 mg injections
administered on same day or 3 to 4 days apart
• Infliximab
– Approved in Europe for treatment of AS
– Dose: 5 mg/kg IV at week 0, 2, and 6 and every 6
to 8 weeks thereafter
20
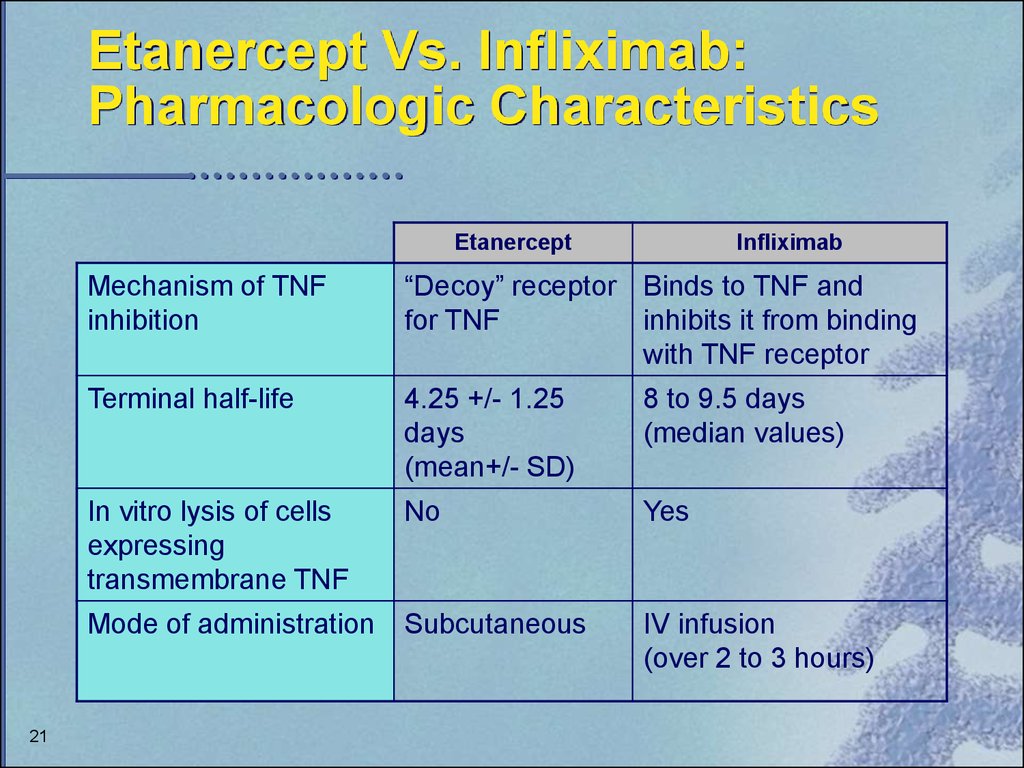
21. Etanercept Vs. Infliximab: Pharmacologic Characteristics
Etanercept21
Infliximab
Mechanism of TNF
inhibition
“Decoy” receptor Binds to TNF and
for TNF
inhibits it from binding
with TNF receptor
Terminal half-life
4.25 +/- 1.25
days
(mean+/- SD)
8 to 9.5 days
(median values)
In vitro lysis of cells
expressing
transmembrane TNF
No
Yes
Mode of administration
Subcutaneous
IV infusion
(over 2 to 3 hours)
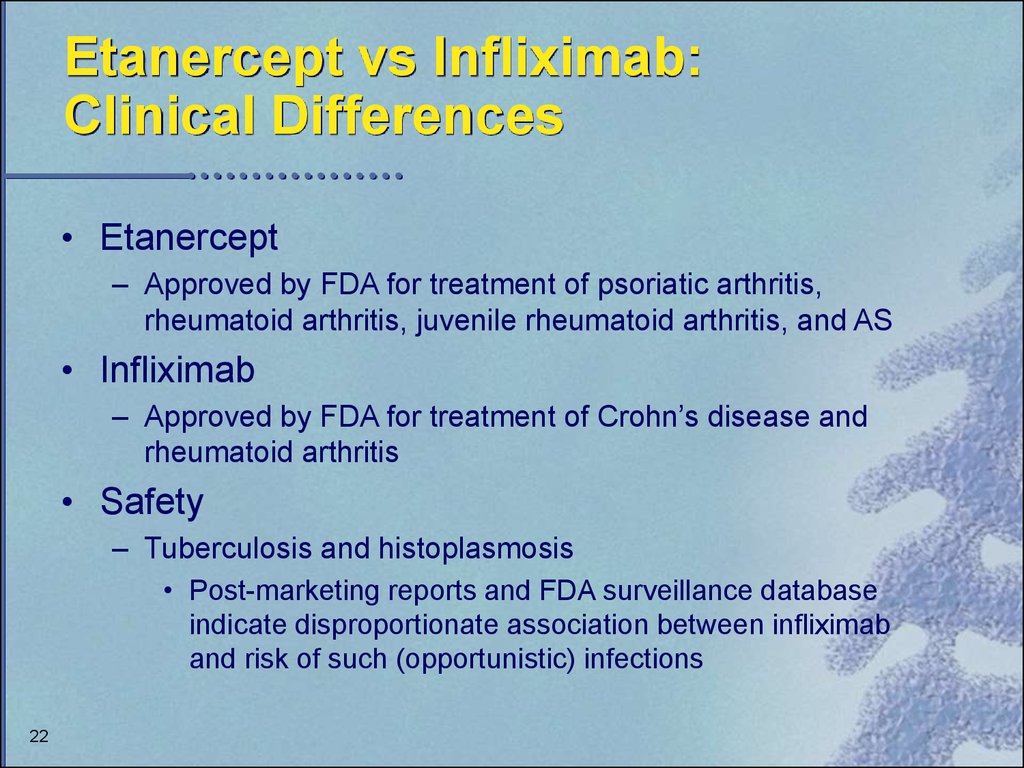
22. Etanercept vs Infliximab: Clinical Differences
• Etanercept– Approved by FDA for treatment of psoriatic arthritis,
rheumatoid arthritis, juvenile rheumatoid arthritis, and AS
• Infliximab
– Approved by FDA for treatment of Crohn’s disease and
rheumatoid arthritis
• Safety
– Tuberculosis and histoplasmosis
• Post-marketing reports and FDA surveillance database
indicate disproportionate association between infliximab
and risk of such (opportunistic) infections
22
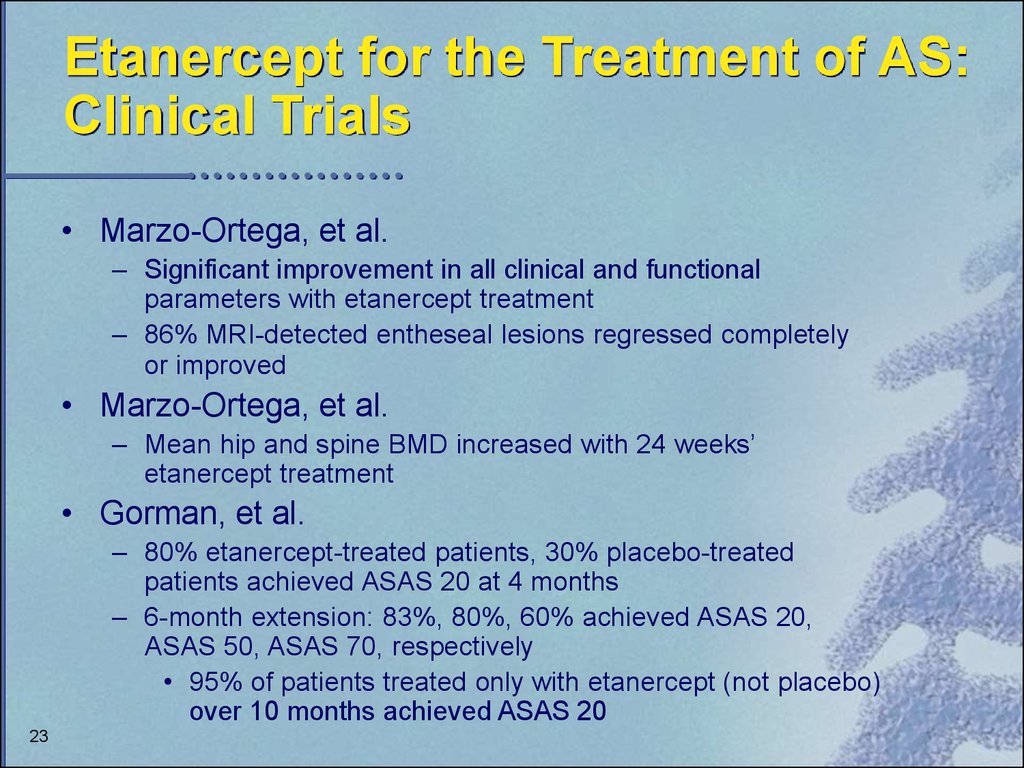
23. Etanercept for the Treatment of AS: Clinical Trials
• Marzo-Ortega, et al.– Significant improvement in all clinical and functional
parameters with etanercept treatment
– 86% MRI-detected entheseal lesions regressed completely
or improved
• Marzo-Ortega, et al.
– Mean hip and spine BMD increased with 24 weeks’
etanercept treatment
• Gorman, et al.
– 80% etanercept-treated patients, 30% placebo-treated
patients achieved ASAS 20 at 4 months
– 6-month extension: 83%, 80%, 60% achieved ASAS 20,
ASAS 50, ASAS 70, respectively
• 95% of patients treated only with etanercept (not placebo)
over 10 months achieved ASAS 20
23
24. Etanercept for the Treatment of AS: Clinical Trials (cont)
• Brandt, et al.– 57% etanercept-treated patients and 6% placebo-treated
patients improved at least 50% on BASDAI
– 56% in placebo group improved following switch to etanercept
– Improvements ceased once etanercept therapy was discontinued
• Davis, et al.
– 57% etanercept-treated patients and 22% placebo-treated
patients achieved ASAS 20 at 24 weeks
24
25. Etanercept: Adverse Events
Events in > 5% of PatientsInjection site reaction
Injection site bruising
Upper respiratory infection
Headache
Accidental injury
Diarrhea
Rash
Rhinitis
Abdominal pain
Dizziness
Flu syndrome
25
*P<.0001; †P<.050; ‡P<.020
Placebo %
(n=139)
9
17
12
12
4
Etanercept %
(n=138)
30*
21
20†
14
12‡
9
7
7
5
2
7
8
11
6
6
6
4
26. Etanercept: Adverse Events (cont)
• Serious infections and sepsis– Mainly in patients with underlying illness or receiving
immunosuppressive therapy
• CNS demyelinating disorders
– Causal relationship unclear
– Use with caution or avoid use in patients with transverse myelitis,
optic neuritis, multiple sclerosis
• Pancytopenia
– Causal relationship unclear
– Use with caution in patients with history of hematologic abnormalities
• Autoantibody formation
– Discontinue if lupus-like symptoms are observed
• Heart failure
– Carefully monitor if prescribed to patients with heart failure
26
27. Infliximab for the Treatment of AS: Clinical Trials
• Brandt, et al.– 50% improvement on outcome variables (ie, BASDAI,
BASFI, pain on VAS, BASMI, QOL (SF-36) with 5 mg/kg
dose of infliximab; 15% improvement with 3 mg/kg dose
• Braun
– 53% of infliximab-treated patients and 9% placebo-treated
patients experienced regression of disease activity of 50%
– Function and quality of life significantly improved with
infliximab treatment (P<.0001)
• Van den Bosch
– Significant improvement with infliximab compared with
placebo on patient and physician global assessments of
disease activity (P<.001)
27
28. Infliximab for the Treatment of AS: Clinical Trials (cont)
• Stone, et al.– Improvement of > 60% at week 6 and > 75% at week 14
observed in BASDAI, BASFI, patient global assessment,
physician global assessment, spinal pain and total body pain,
and HAQ
– Improvement on MRI scans
• Maksymowych, et al.
– Significant improvement* on BASDAI; significant mean
reduction in BASFI, BASGI, ESR, and CRP at week 14
– Efficacy sustained at 1 year
28
*P<.001, all parameters except CRP, P=.01
29. Infliximab: Adverse Events
Placebo%(n=81)
Infliximab%
(n=430)
Acute infusion reaction
10*
20*
Upper respiratory infection
35
40
Headache
21
29
Diarrhea
19
19
Rash
7
18
Rhinitis
14
14
Abdominal pain
12
17
Fatigue
9
13
Arthralgia
7
13
Events in > 5% of Patients
29
* Approximation based on all clinical studies
30. Infliximab: Adverse Events (cont)
• Serious infections and sepsis– Cases in patients on concomitant immunosuppressive therapy
• Neurologic events
– Use with caution in patients with pre-existing CNS
demyelinating or seizure disorders
• Autoantibody formation
– Discontinue if lupus-like symptoms are observed
• Heart failure
– Consider other treatment options in patients with heart failure
– Closely monitor patients if infliximab is administered
30
31. Anti-TNF Agents: Summary
• Anti-TNF agents target underlying inflammatory process– Alter disease progression
– Provide symptomatic relief
• Recommended treatment after trial of chronic daily
NSAIDs, physical therapy, and regular exercise
• Good safety and tolerability profiles
• Long-term data needed
• Implement treatment guidelines to ensure proper
treatment given to appropriate patients
– Treatment algorithm presented on next two slides
31
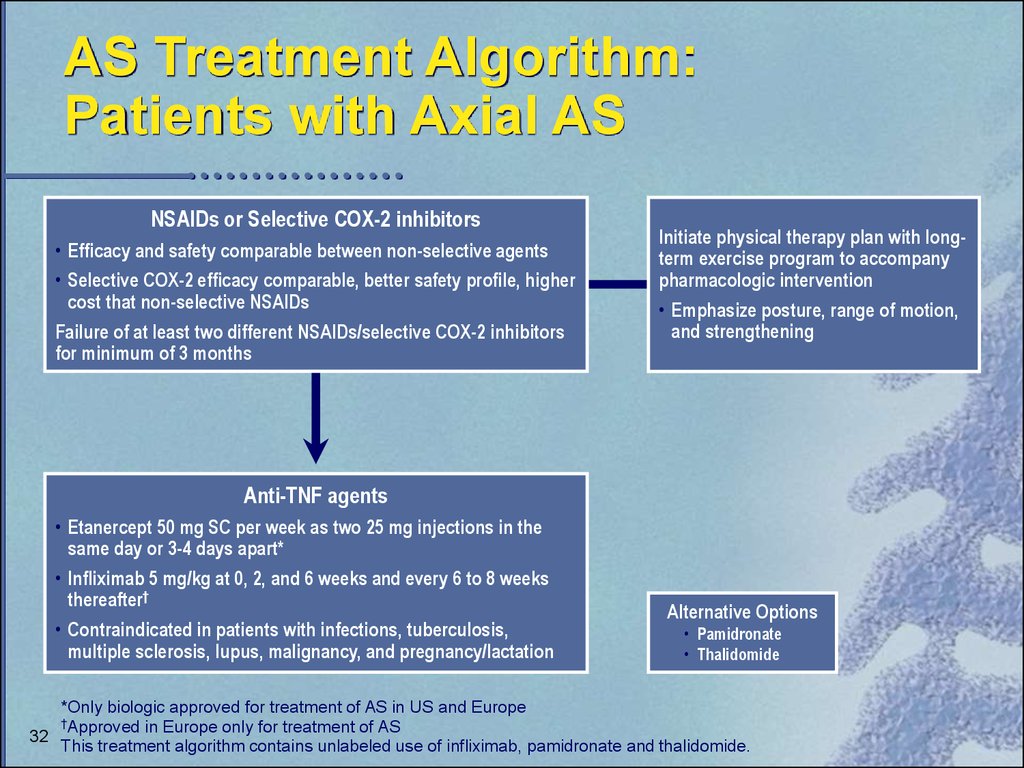
32. AS Treatment Algorithm: Patients with Axial AS
NSAIDs or Selective COX-2 inhibitors• Efficacy and safety comparable between non-selective agents
• Selective COX-2 efficacy comparable, better safety profile, higher
cost that non-selective NSAIDs
Failure of at least two different NSAIDs/selective COX-2 inhibitors
for minimum of 3 months
Initiate physical therapy plan with longterm exercise program to accompany
pharmacologic intervention
• Emphasize posture, range of motion,
and strengthening
Anti-TNF agents
• Etanercept 50 mg SC per week as two 25 mg injections in the
same day or 3-4 days apart*
• Infliximab 5 mg/kg at 0, 2, and 6 weeks and every 6 to 8 weeks
thereafter†
• Contraindicated in patients with infections, tuberculosis,
multiple sclerosis, lupus, malignancy, and pregnancy/lactation
Alternative Options
• Pamidronate
• Thalidomide
*Only biologic approved for treatment of AS in US and Europe
†Approved in Europe only for treatment of AS
32
This treatment algorithm contains unlabeled use of infliximab, pamidronate and thalidomide.
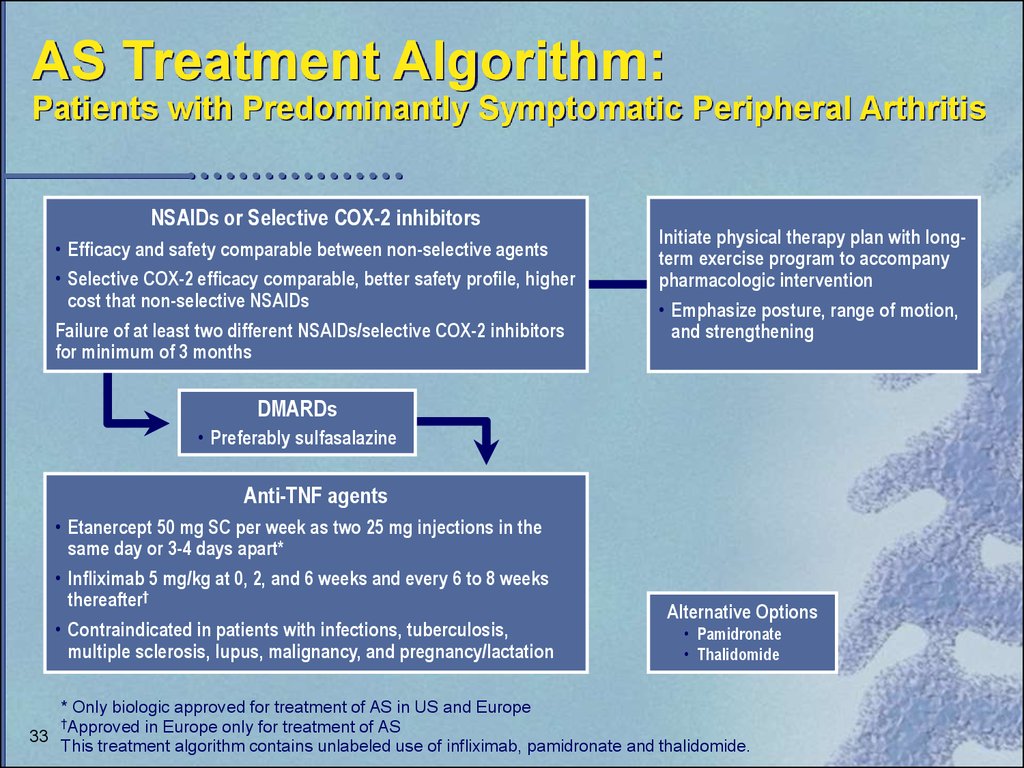
33. AS Treatment Algorithm: Patients with Predominantly Symptomatic Peripheral Arthritis
NSAIDs or Selective COX-2 inhibitors• Efficacy and safety comparable between non-selective agents
• Selective COX-2 efficacy comparable, better safety profile, higher
cost that non-selective NSAIDs
Failure of at least two different NSAIDs/selective COX-2 inhibitors
for minimum of 3 months
Initiate physical therapy plan with longterm exercise program to accompany
pharmacologic intervention
• Emphasize posture, range of motion,
and strengthening
DMARDs
• Preferably sulfasalazine
Anti-TNF agents
• Etanercept 50 mg SC per week as two 25 mg injections in the
same day or 3-4 days apart*
• Infliximab 5 mg/kg at 0, 2, and 6 weeks and every 6 to 8 weeks
thereafter†
• Contraindicated in patients with infections, tuberculosis,
multiple sclerosis, lupus, malignancy, and pregnancy/lactation
Alternative Options
• Pamidronate
• Thalidomide
* Only biologic approved for treatment of AS in US and Europe
†Approved in Europe only for treatment of AS
33
This treatment algorithm contains unlabeled use of infliximab, pamidronate and thalidomide.











 Медицина
Медицина








