Похожие презентации:
Traumatic brain injury
1.
Traumatic brain injury2.
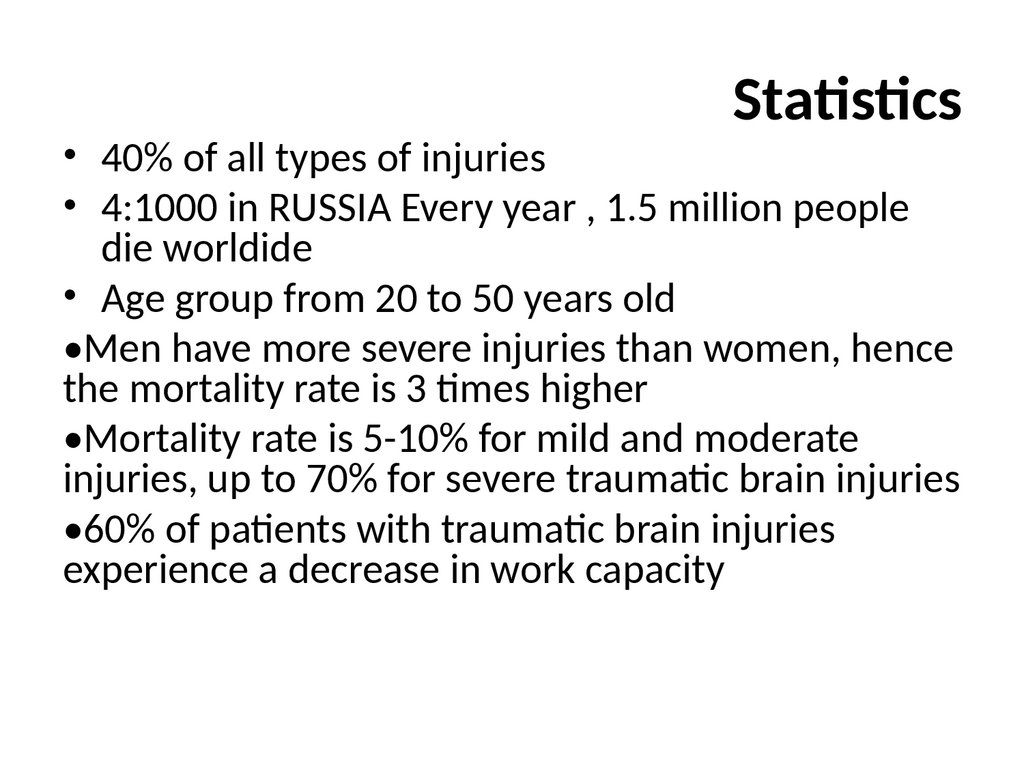
Statistics• 40% of all types of injuries
• 4:1000 in RUSSIA Every year , 1.5 million people
die worldide
• Age group from 20 to 50 years old
•Men have more severe injuries than women, hence
the mortality rate is 3 times higher
•Mortality rate is 5-10% for mild and moderate
injuries, up to 70% for severe traumatic brain injuries
•60% of patients with traumatic brain injuries
experience a decrease in work capacity
3.
Traumatic brain injury is damage caused bymechanical energy to the bones of the skull,
brain, blood vessels, cranial nerves, and
meninges.
4.
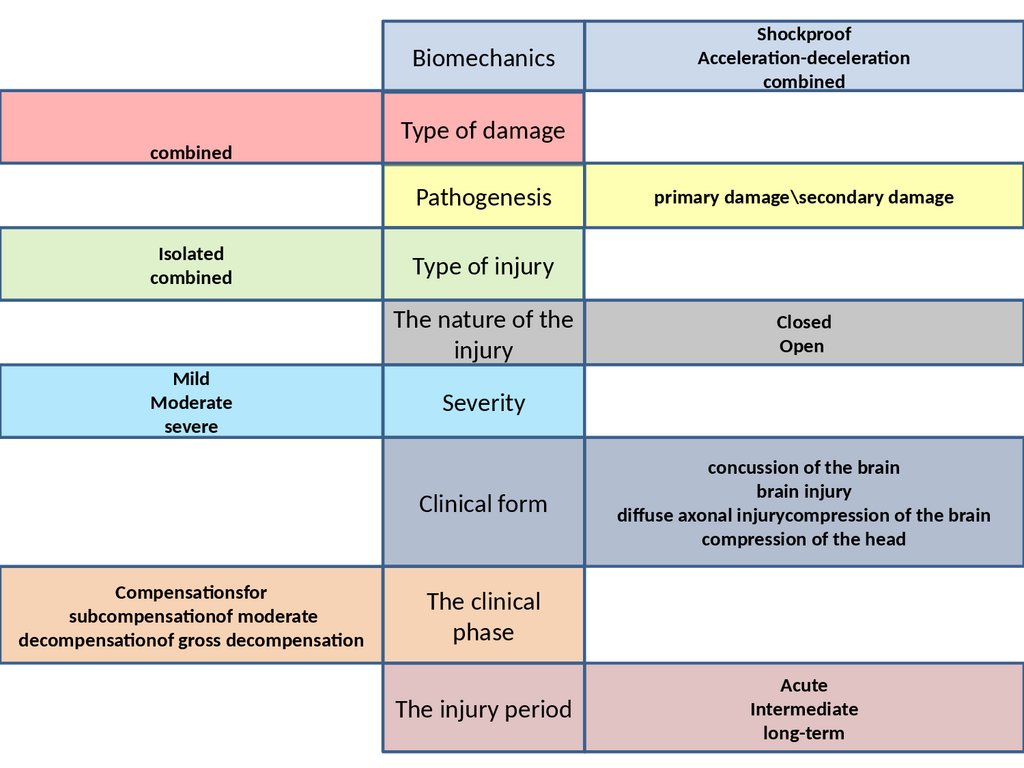
Biomechanicscombined
Type of damage
Pathogenesis
Isolated
combined
Mild
Moderate
severe
primary damage\secondary damage
Type of injury
The nature of the
injury
Closed
Оpen
Severity
Clinical form
Compensationsfor
subcompensationof moderate
decompensationof gross decompensation
Shockproof
Acceleration-deceleration
combined
concussion of the brain
brain injury
diffuse axonal injurycompression of the brain
compression of the head
The clinical
phase
The injury period
Acute
Intermediate
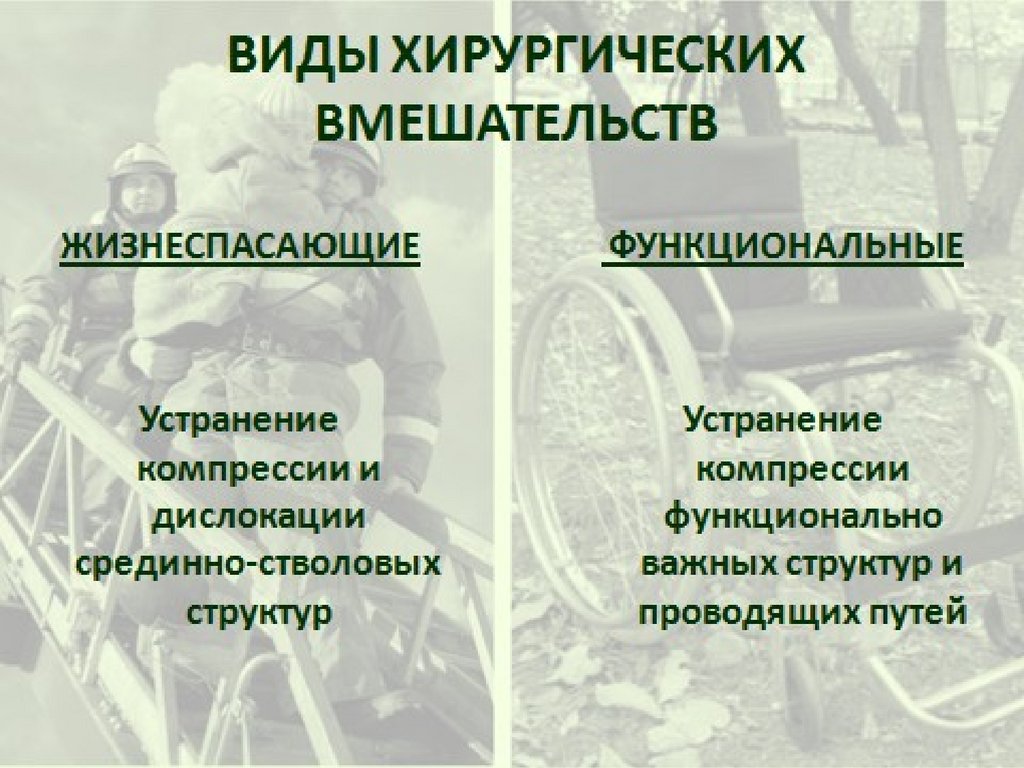
long-term
5.
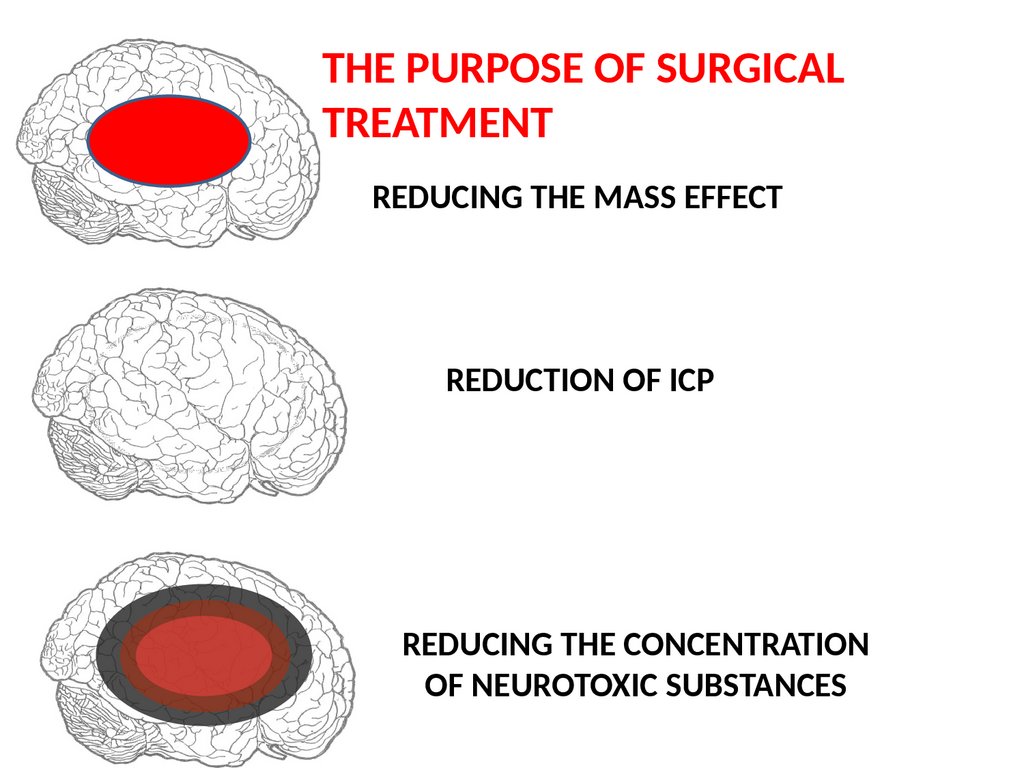
MECHANISMS OFDYNAMICIMPACTS
"ACCELERATION - DECELERATION"diffuse damage
"BLOW - COUNTERATTACK"- focal
(local)"COMBINED"
6.
severity of primarybrain damage
7.
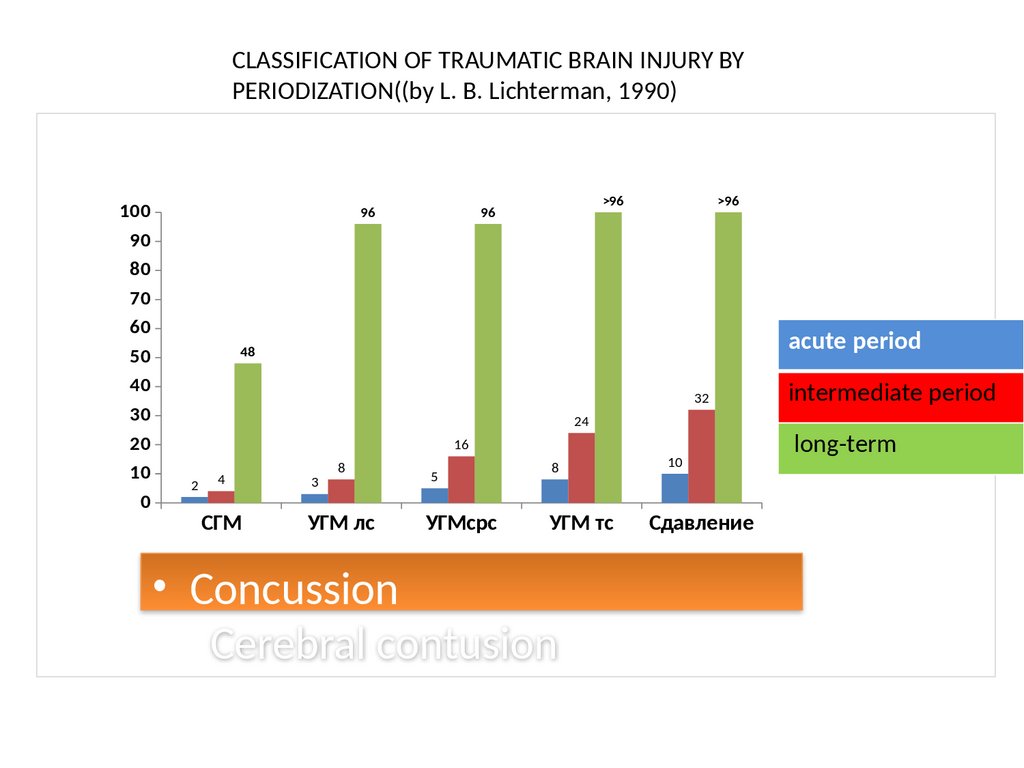
CLASSIFICATION OF TRAUMATIC BRAIN INJURY BYPERIODIZATION((by L. B. Lichterman, 1990)
100
90
80
70
60
50
40
30
20
10
0
96
>96
96
>96
acute period
48
32
24
16
2
4
СГМ
3
8
УГМ лс
5
УГМсрс
8
УГМ тс
• Concussion
Cerebral contusion
10
Сдавление
intermediate period
long-term
8.
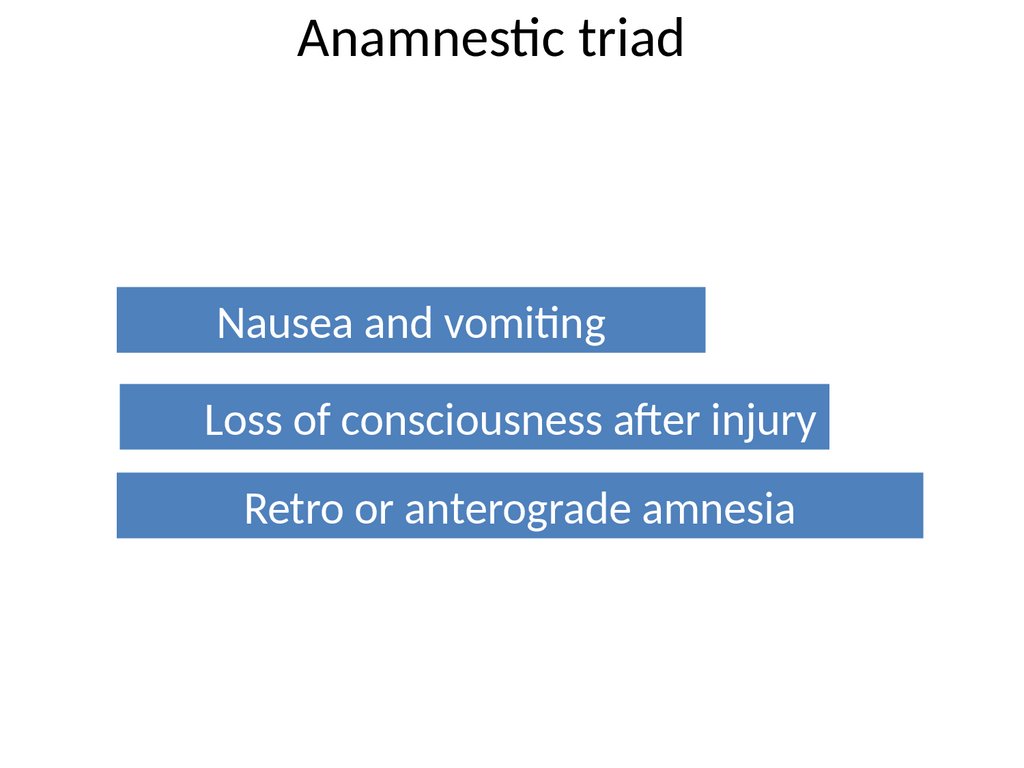
Diagnostics1. Anamnestic triad
2. 2. External examination and palpation
3. 3.Neurological examination:General cerebral
symptomsFocal symptoms...Meningial symptom
complex
4. 4. ECHO ES
5. 5. R-graphy of the skull
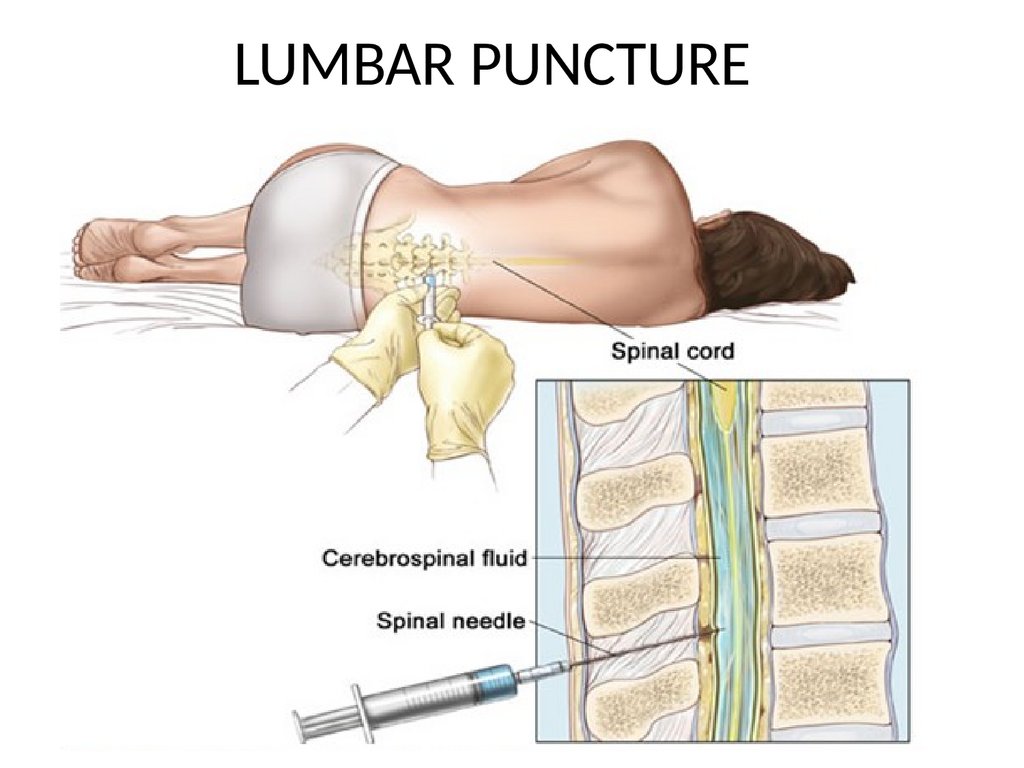
6. 6. Lumbar puncture
7. 7. CTscan of the brain
8. 8. Cerebral angiography
9. 9. Application of diagnostic trefinationholes
9.
Anamnestic triadNausea and vomiting
Loss of consciousness after injury
Retro or anterograde amnesia
10.
ДИФФЕРЕНЦИАЛЬНАЯДИАГНОСТИКА
Concussion
loss of
consciousness
General cerebral
symptoms
Short-term, moderate
Mild INJURY
Moderate INJURY
Severe INJURY
Seconds - minutes
Minutes hours
Hours - weeks
Short-term, moderate Persistent, pronounced
Persistent,
Focal symptoms
Short-term
Short-term - long-term
Long-term
Meningeal
symptoms
Possibly short-term
Long-term
Long-term
Rarely (secondary)
Often (primary)
Possible
Possible (often)
Short-term
Long-term
Stem symptoms
Fractures of the
skull bones
Vital disorders
Possible
11.
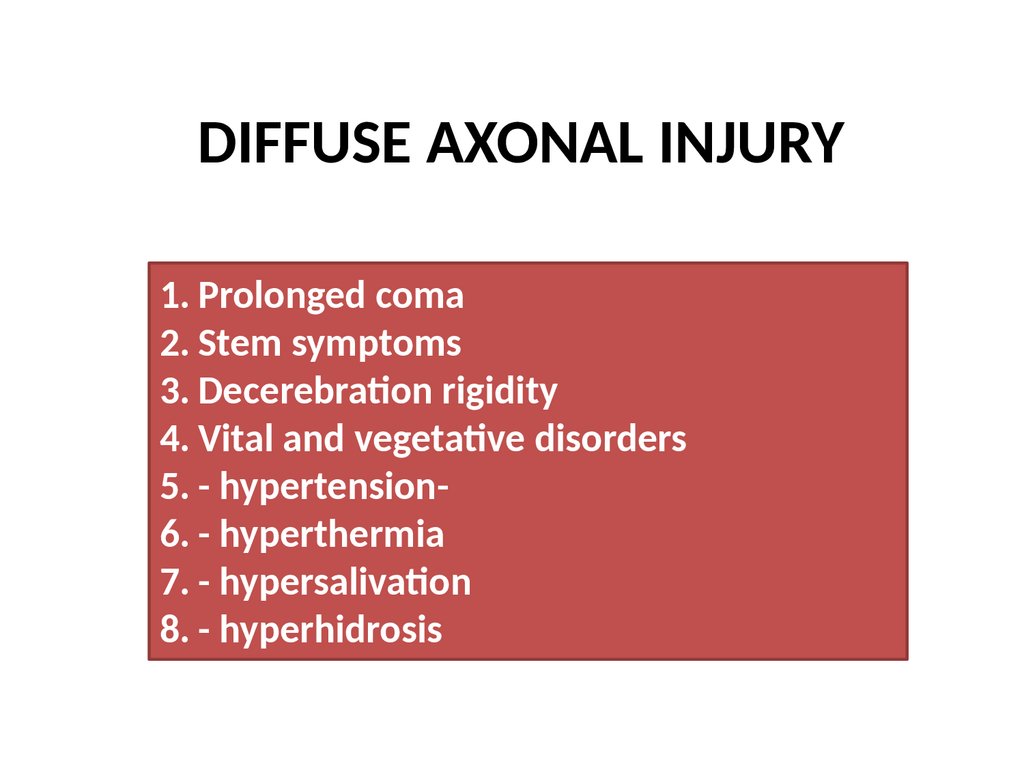
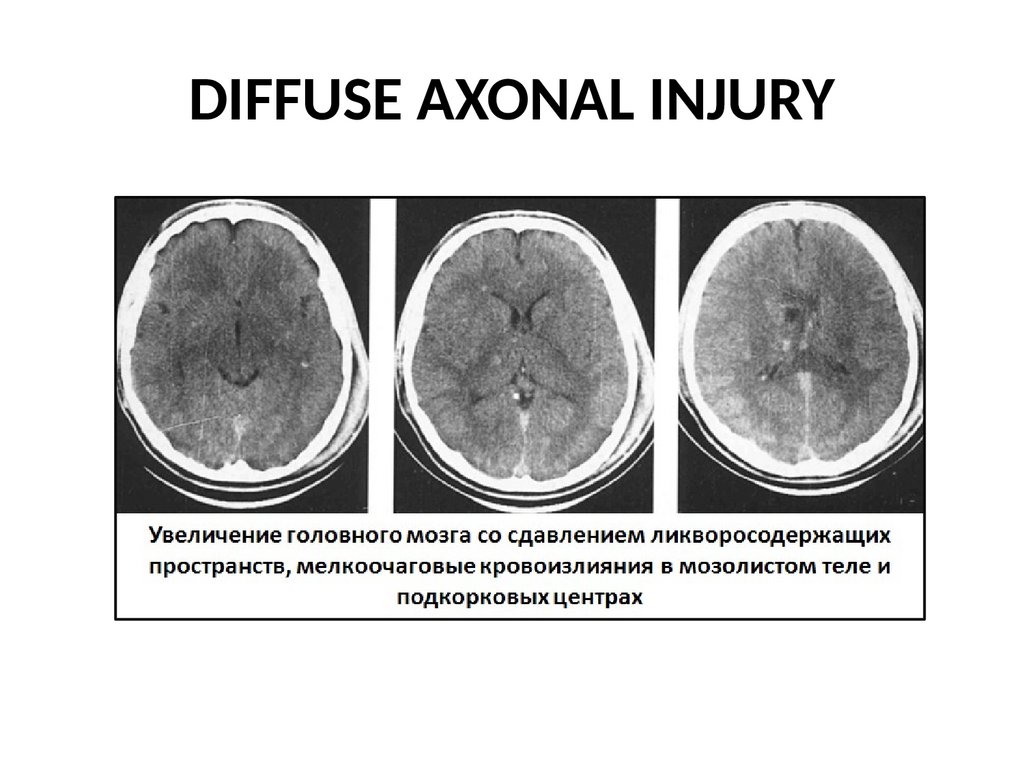
DIFFUSE AXONAL INJURY1. Prolonged coma
2. Stem symptoms
3. Decerebration rigidity
4. Vital and vegetative disorders
5. - hypertension6. - hyperthermia
7. - hypersalivation
8. - hyperhidrosis
12.
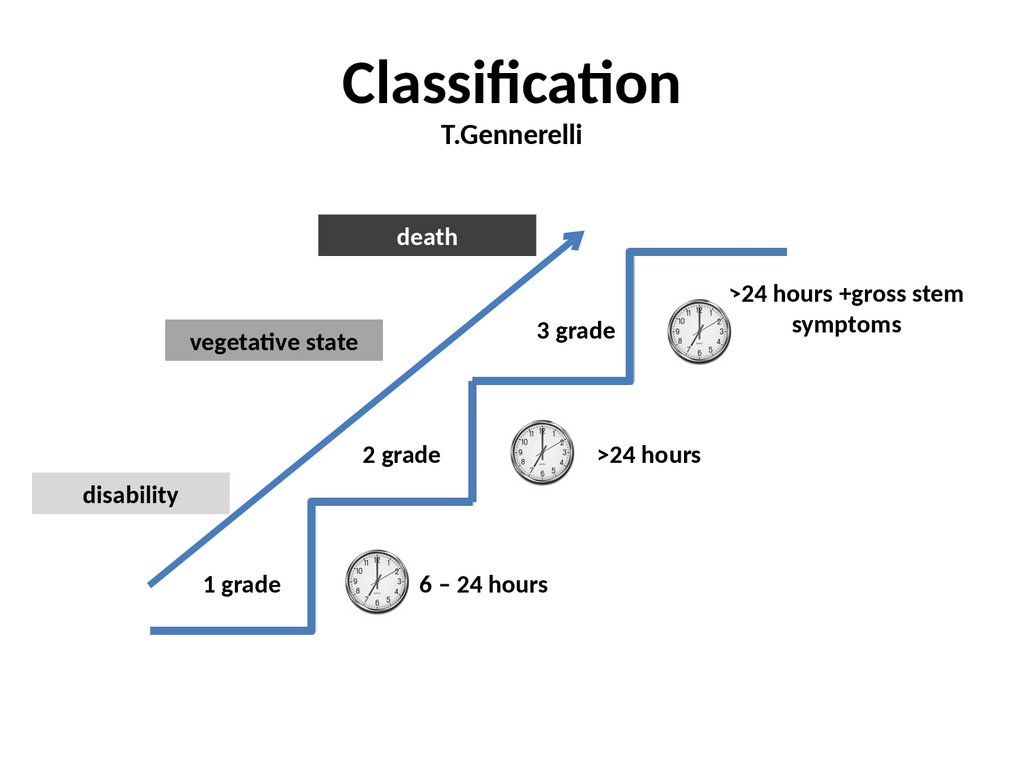
ClassificationT.Gennerelli
death
3 grade
vegetative state
2 grade
disability
1 grade
6 – 24 hours
>24 hours
>24 hours +gross stem
symptoms
13.
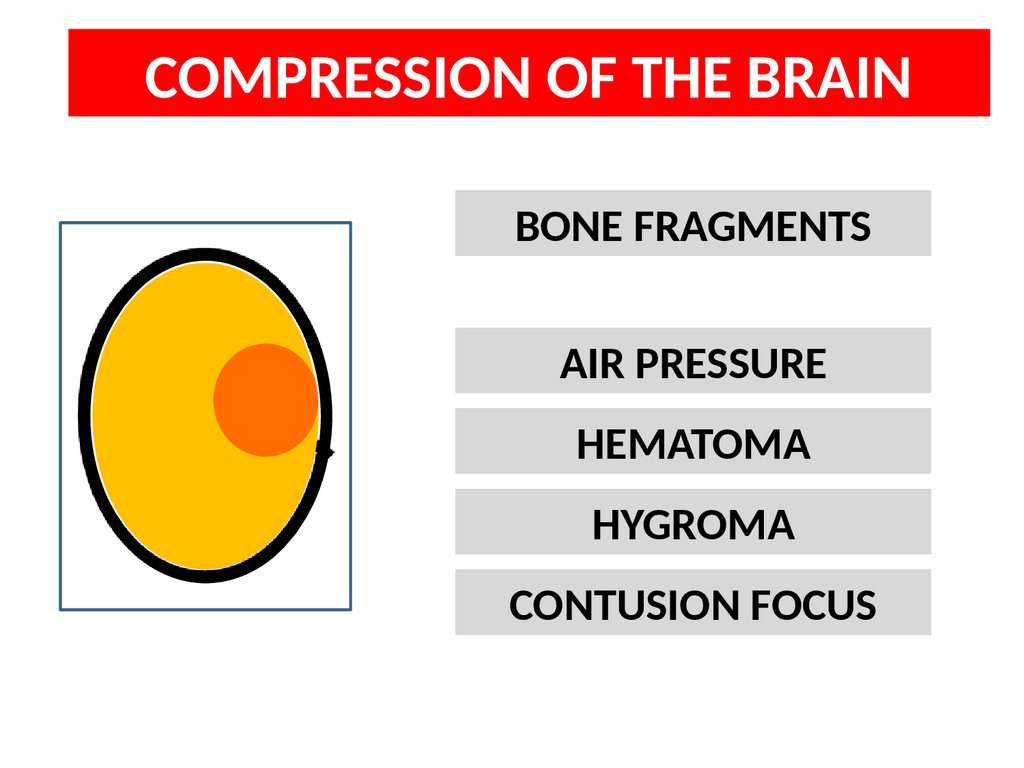
COMPRESSION OF THE BRAINBONE FRAGMENTS
AIR PRESSURE
HEMATOMA
HYGROMA
CONTUSION FOCUS
14.
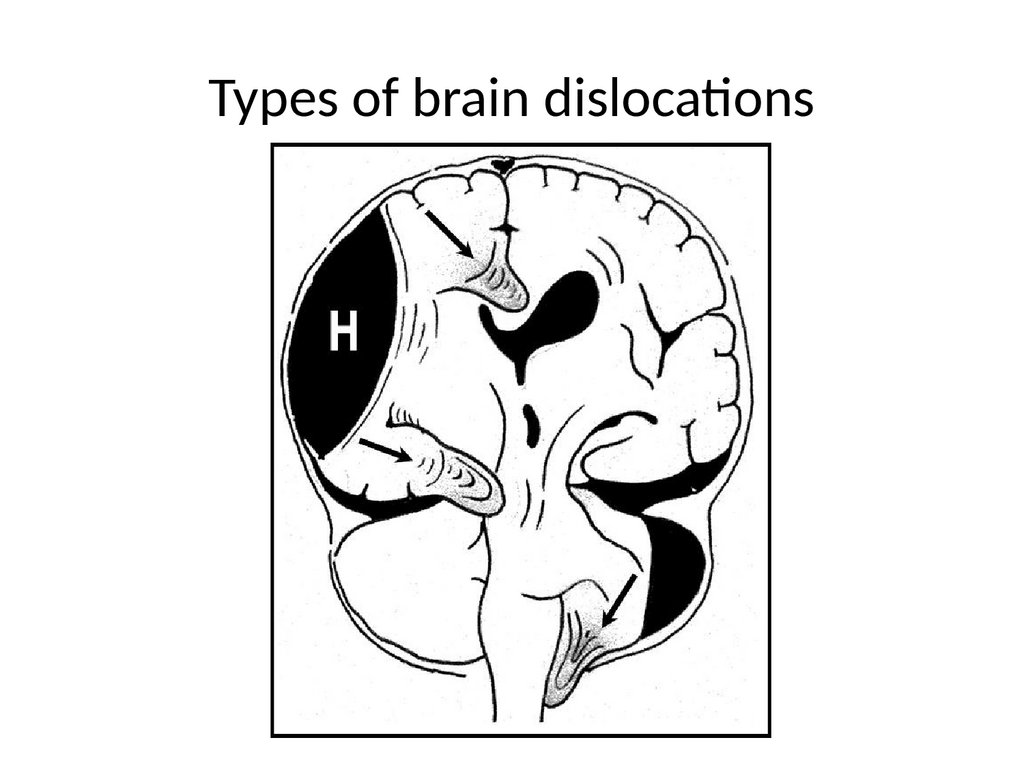
Types of brain dislocations15.
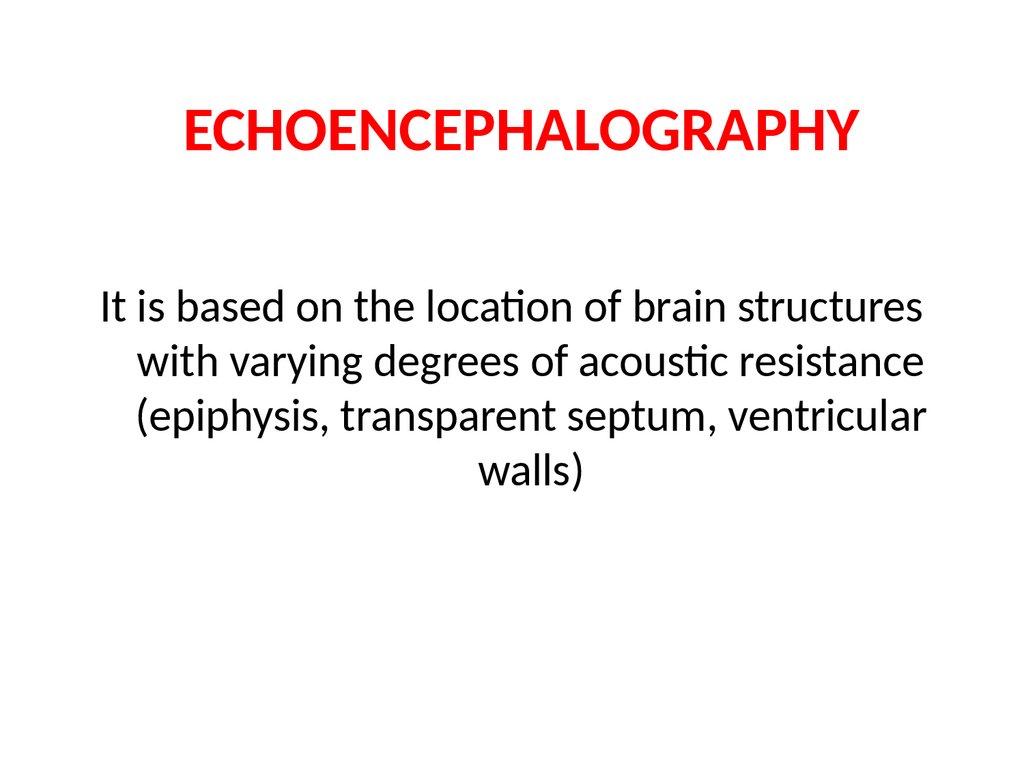
ECHOENCEPHALOGRAPHYIt is based on the location of brain structures
with varying degrees of acoustic resistance
(epiphysis, transparent septum, ventricular
walls)
16.
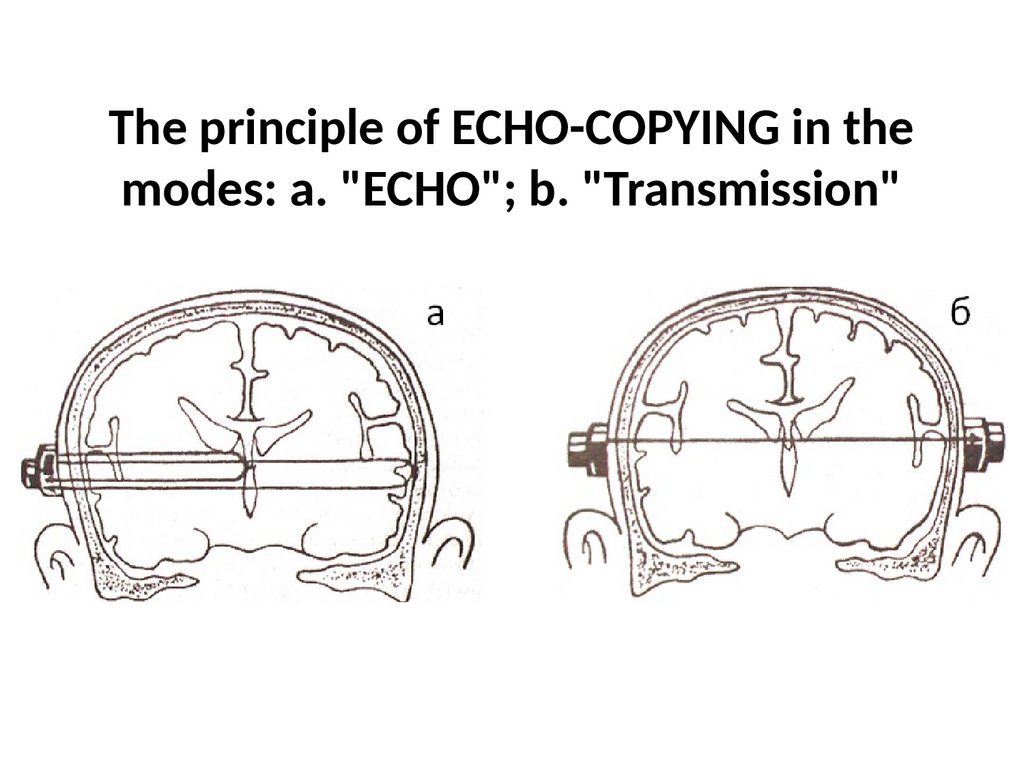
The principle of ECHO-COPYING in themodes: a. "ECHO"; b. "Transmission"
17.
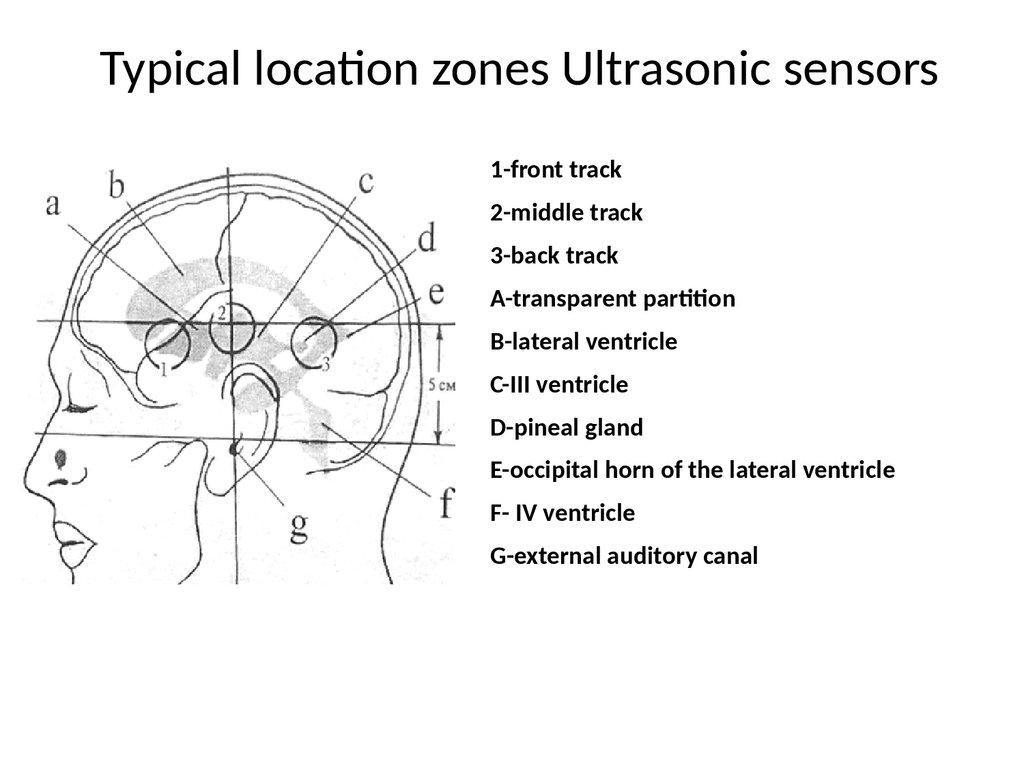
Typical location zones Ultrasonic sensors1-front track
2-middle track
3-back track
A-transparent partition
B-lateral ventricle
C-III ventricle
D-pineal gland
E-occipital horn of the lateral ventricle
F- IV ventricle
G-external auditory canal
18.
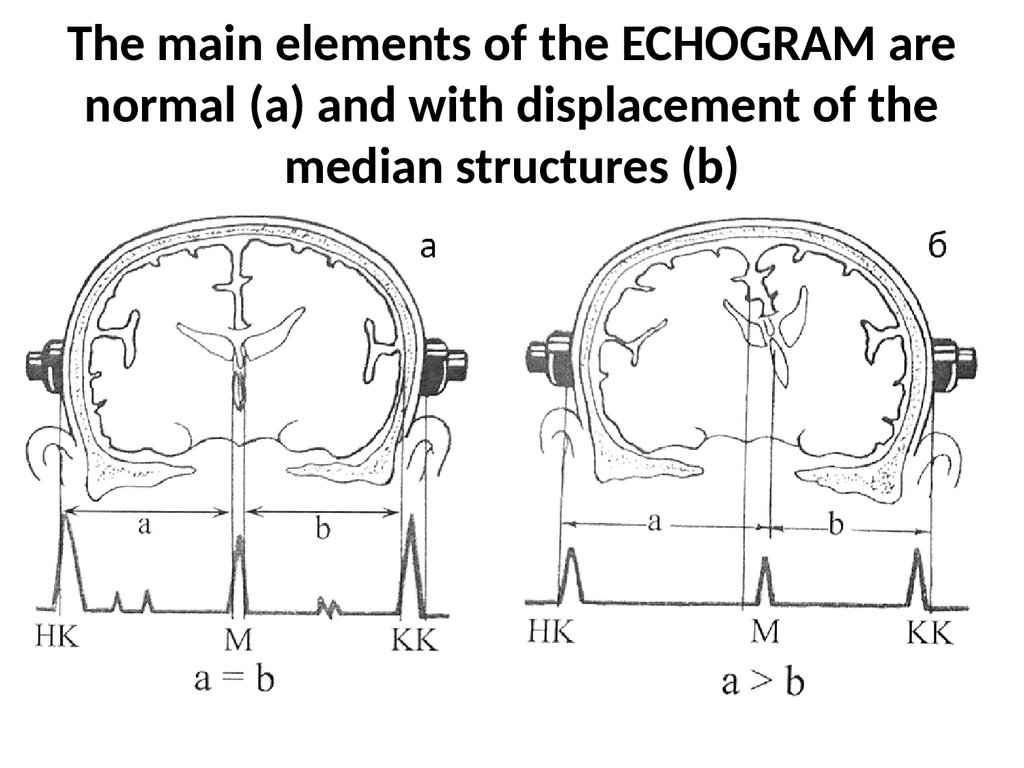
The main elements of the ECHOGRAM arenormal (a) and with displacement of the
median structures (b)
19.
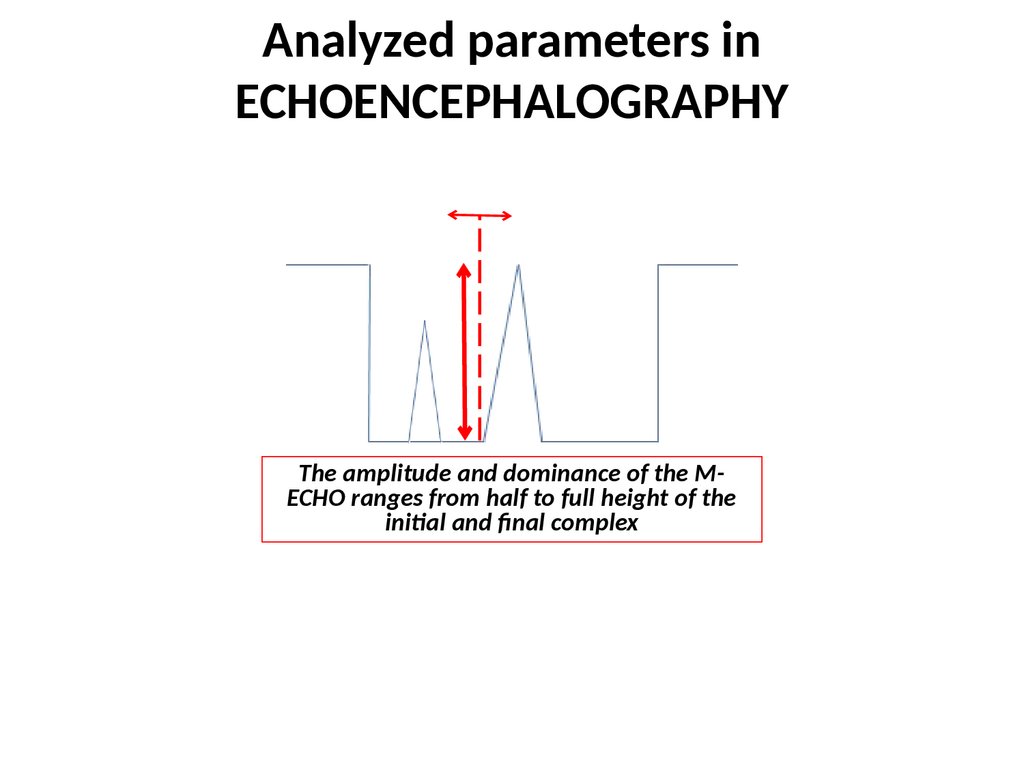
Analyzed parameters inECHOENCEPHALOGRAPHY
The amplitude and dominance of the MECHO ranges from half to full height of the
initial and final complex
20.
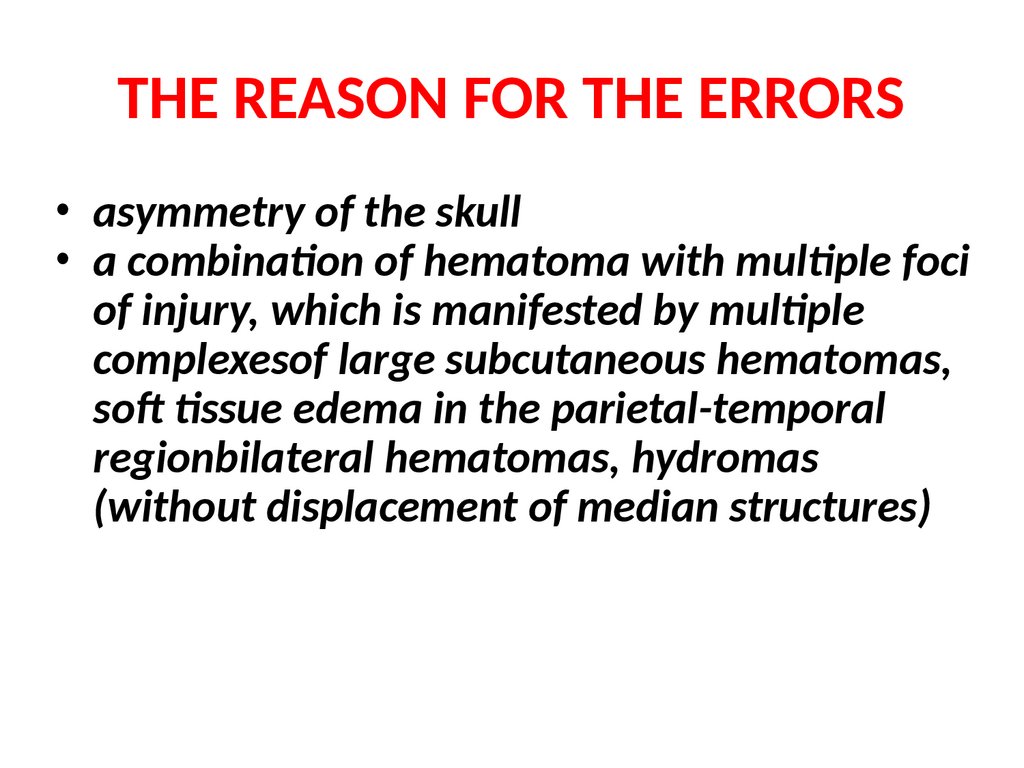
THE REASON FOR THE ERRORS• asymmetry of the skull
• a combination of hematoma with multiple foci
of injury, which is manifested by multiple
complexesof large subcutaneous hematomas,
soft tissue edema in the parietal-temporal
regionbilateral hematomas, hydromas
(without displacement of median structures)
21.
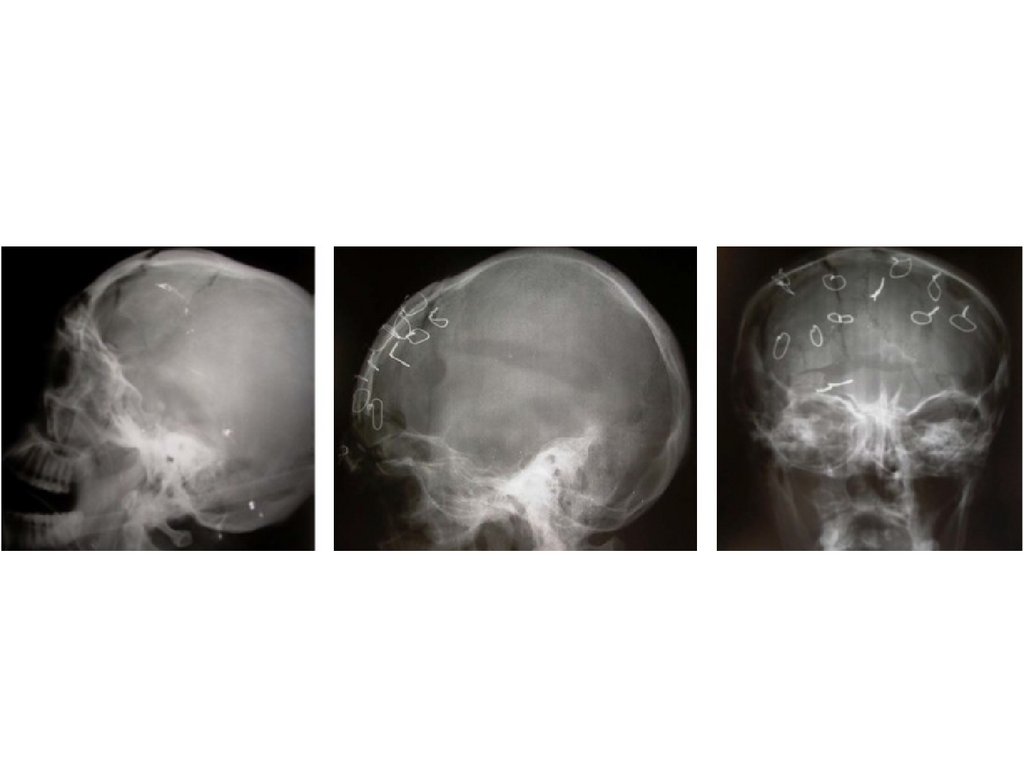
Roentgenography22.
Signs of traumatic suture divergence• Fractures of the teeth
• Seam gaping and tooth disappearance
• The incongruence of the edges forming the
seam
• Step-like deformation
23.
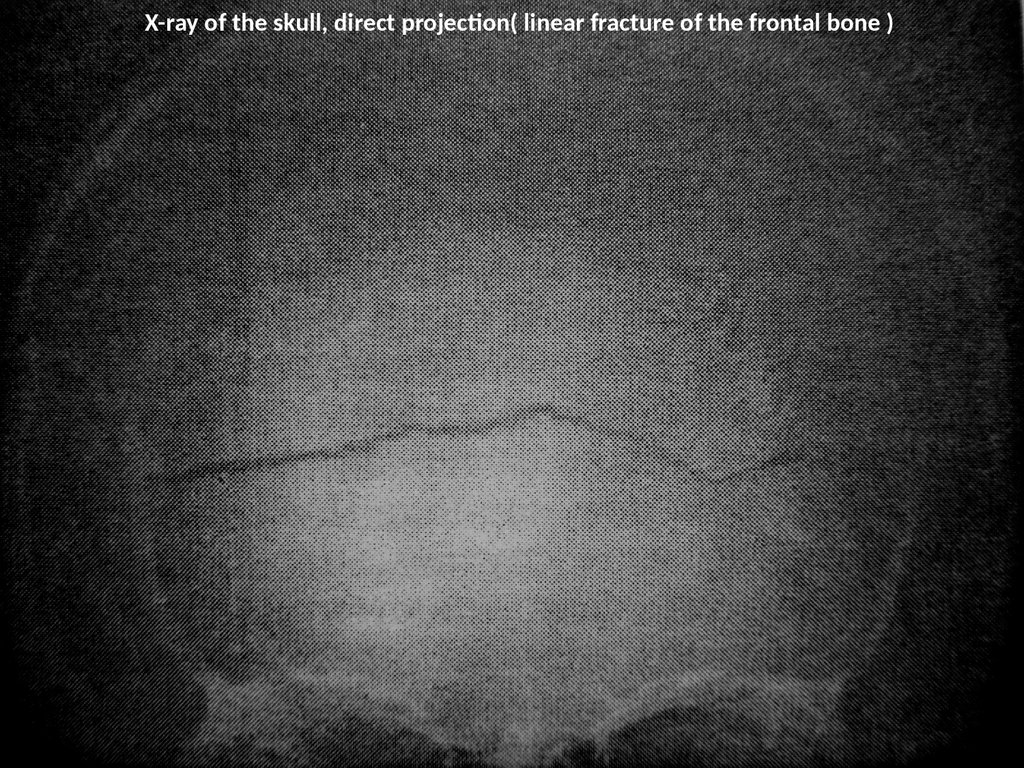
X-ray of the skull, direct projection( linear fracture of the frontal bone )24.
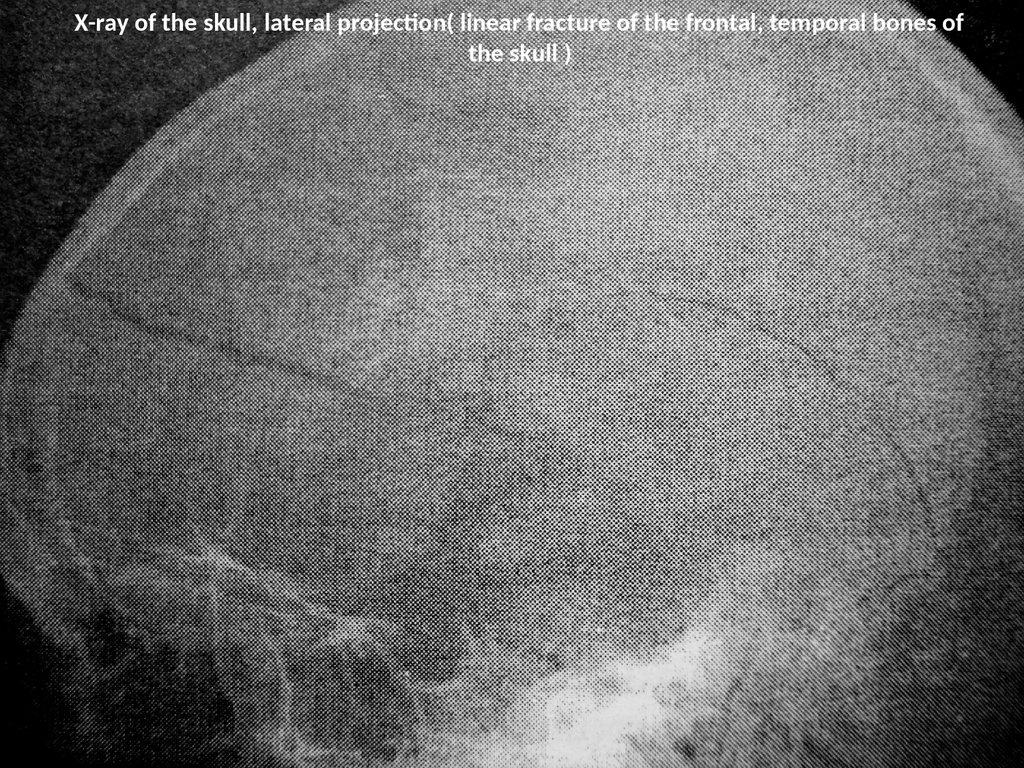
X-ray of the skull, lateral projection( linear fracture of the frontal, temporal bones ofthe skull )
25.
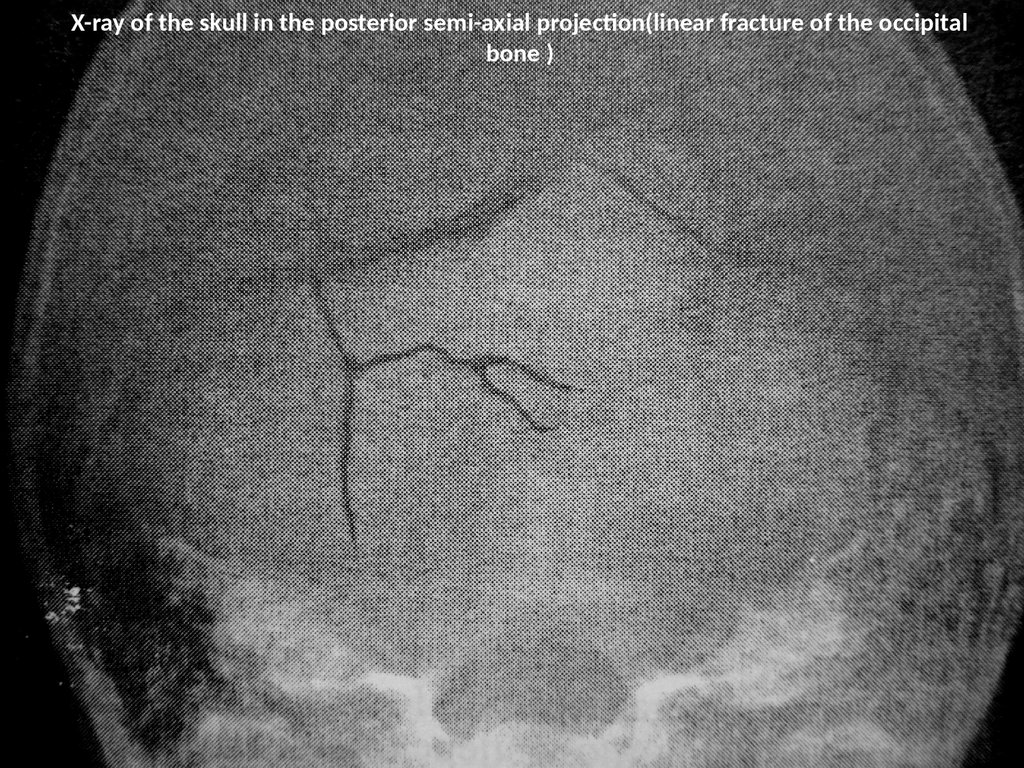
X-ray of the skull in the posterior semi-axial projection(linear fracture of the occipitalbone )
26.
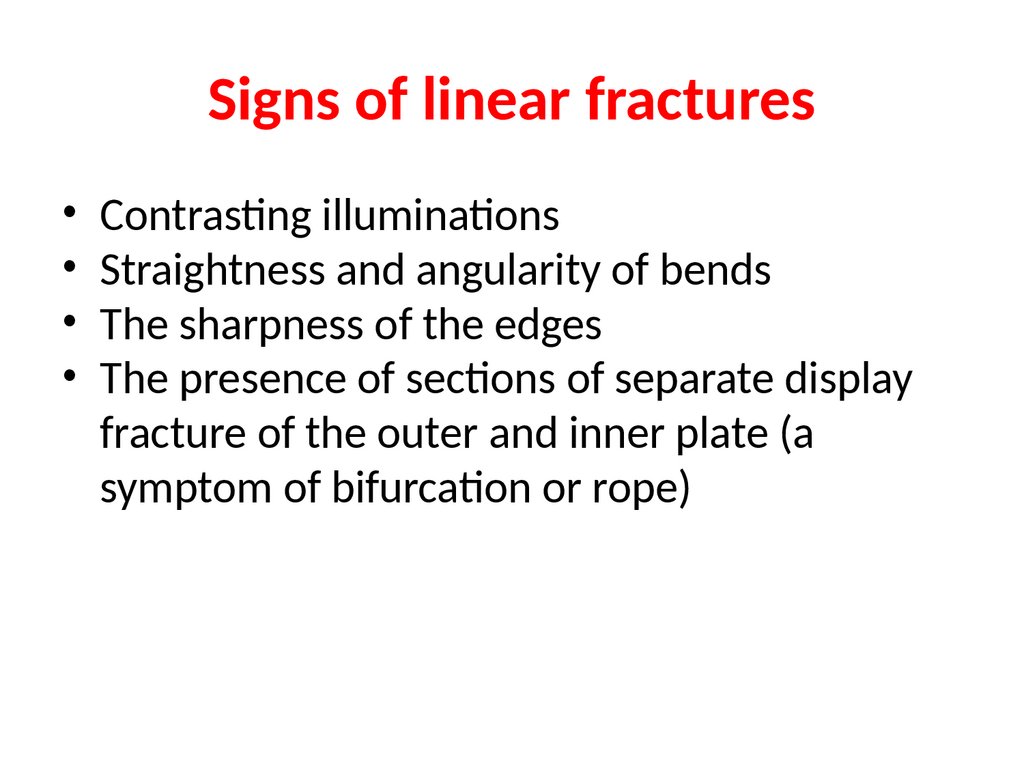
Signs of linear fractures• Contrasting illuminations
• Straightness and angularity of bends
• The sharpness of the edges
• The presence of sections of separate display
fracture of the outer and inner plate (a
symptom of bifurcation or rope)
27.
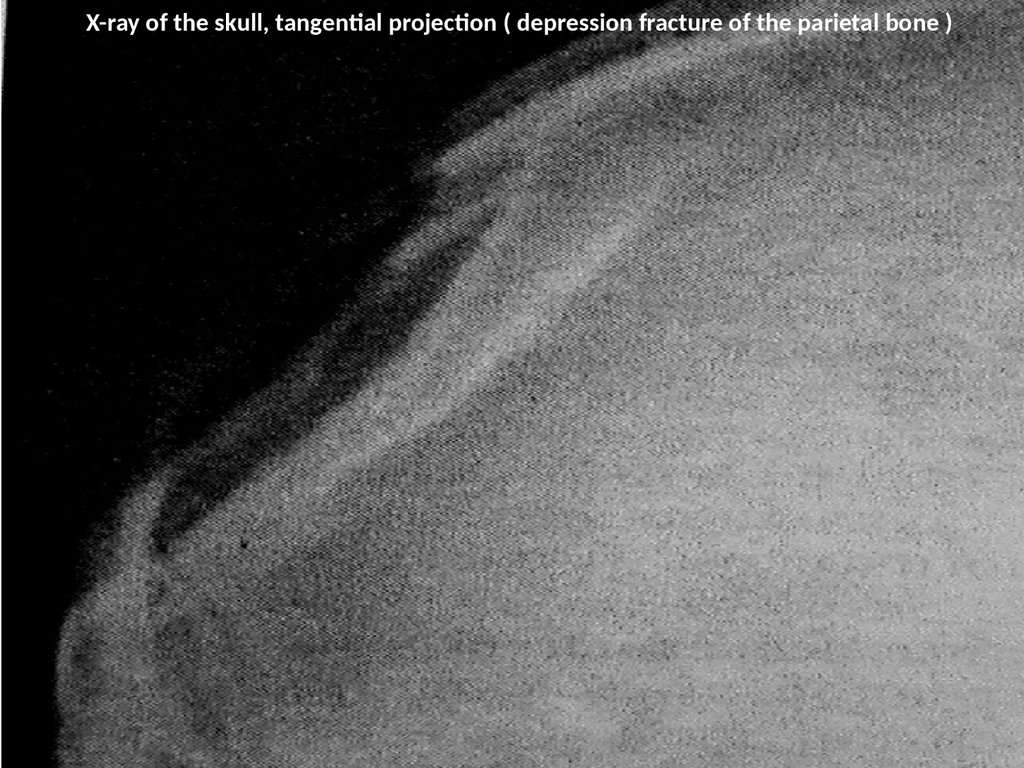
X-ray of the skull, tangential projection ( depression fracture of the parietal bone )Образец текста
Второй уровень
Третий уровень
Четвертый уровень
Пятый уровень
28.
LUMBAR PUNCTURE29.
NEUROIMAGING CHARACTERISTICSTRAUMATIC BRAIN INJURY
30.
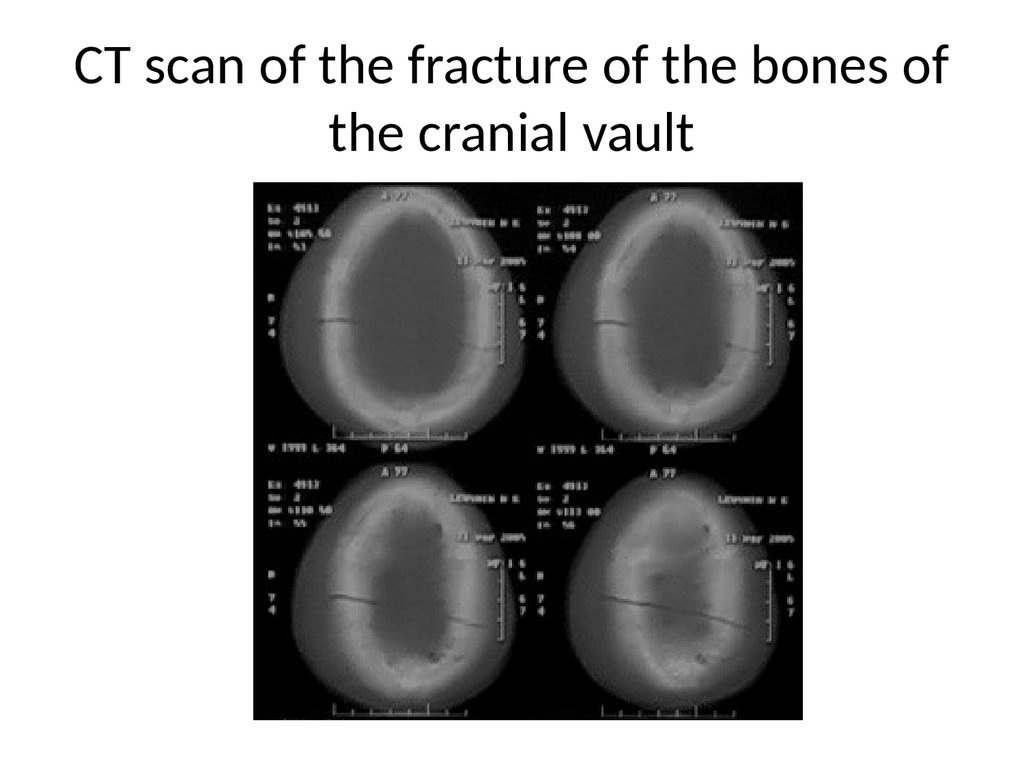
CT scan of the fracture of the bones ofthe cranial vault
31.
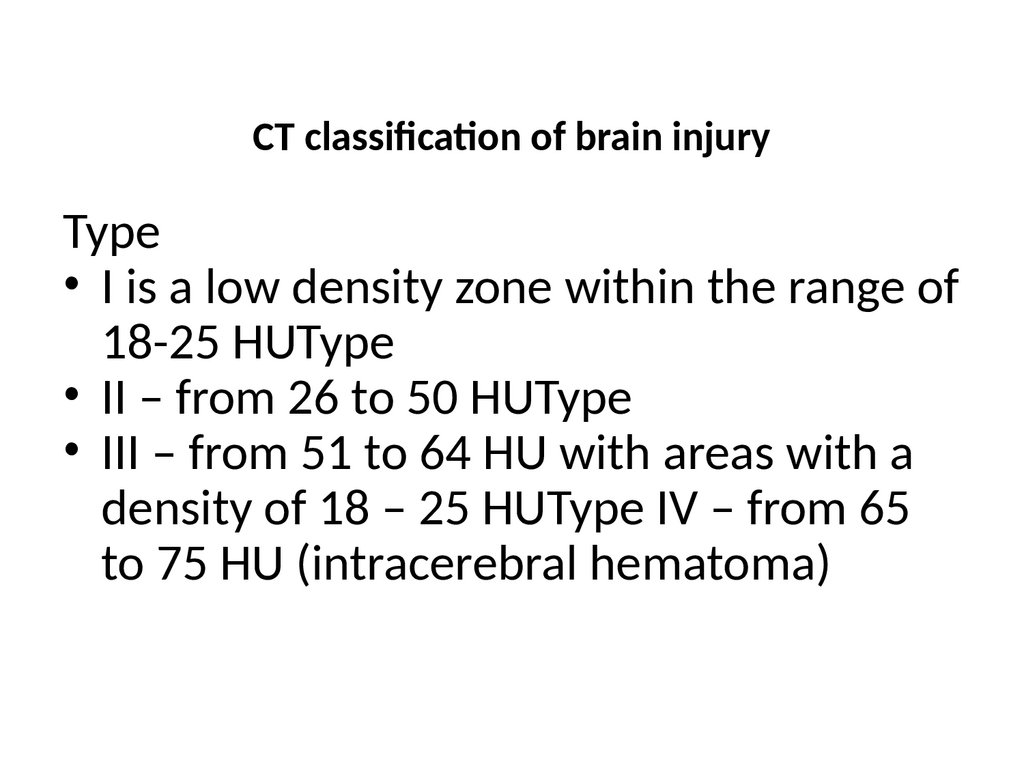
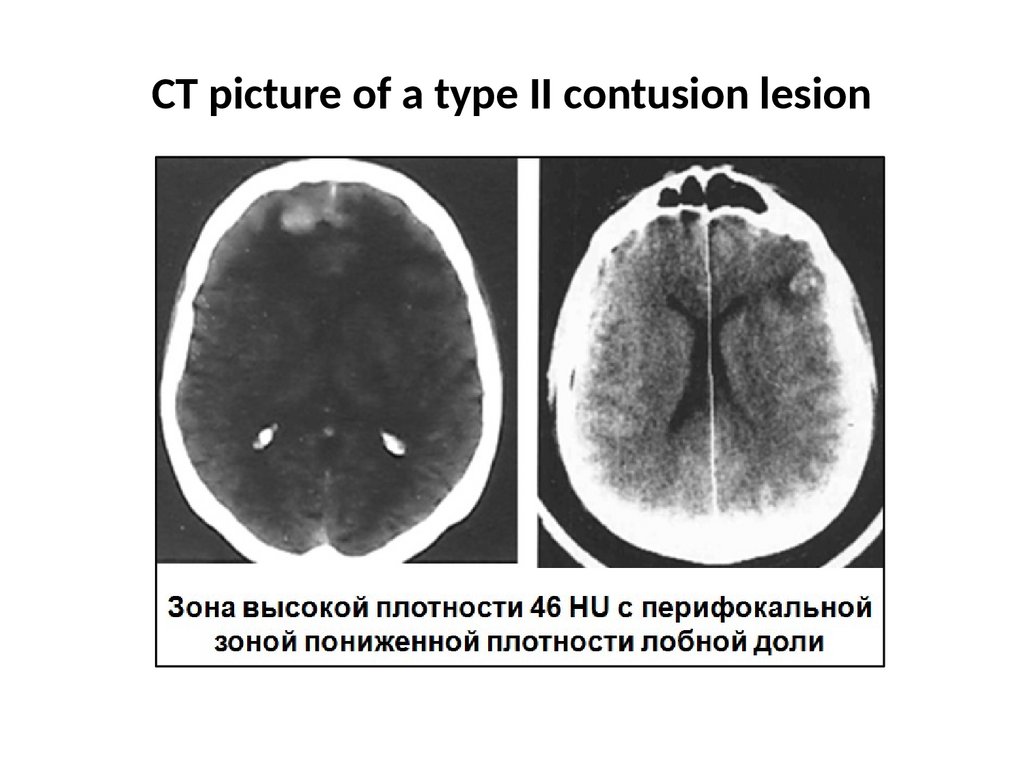
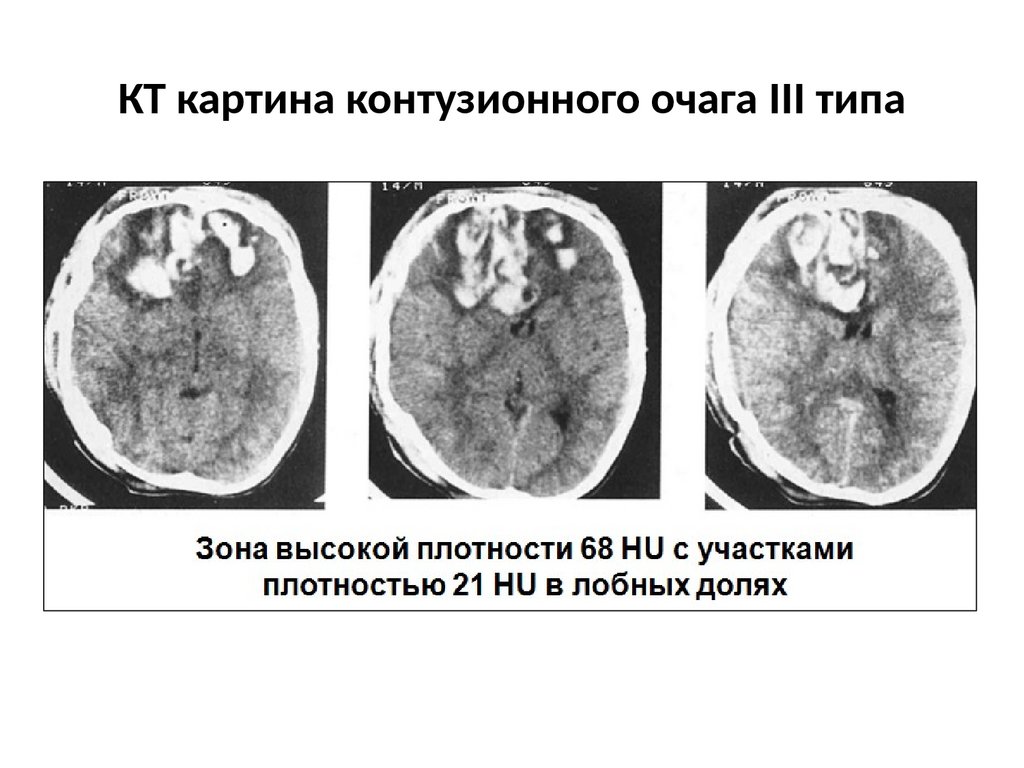
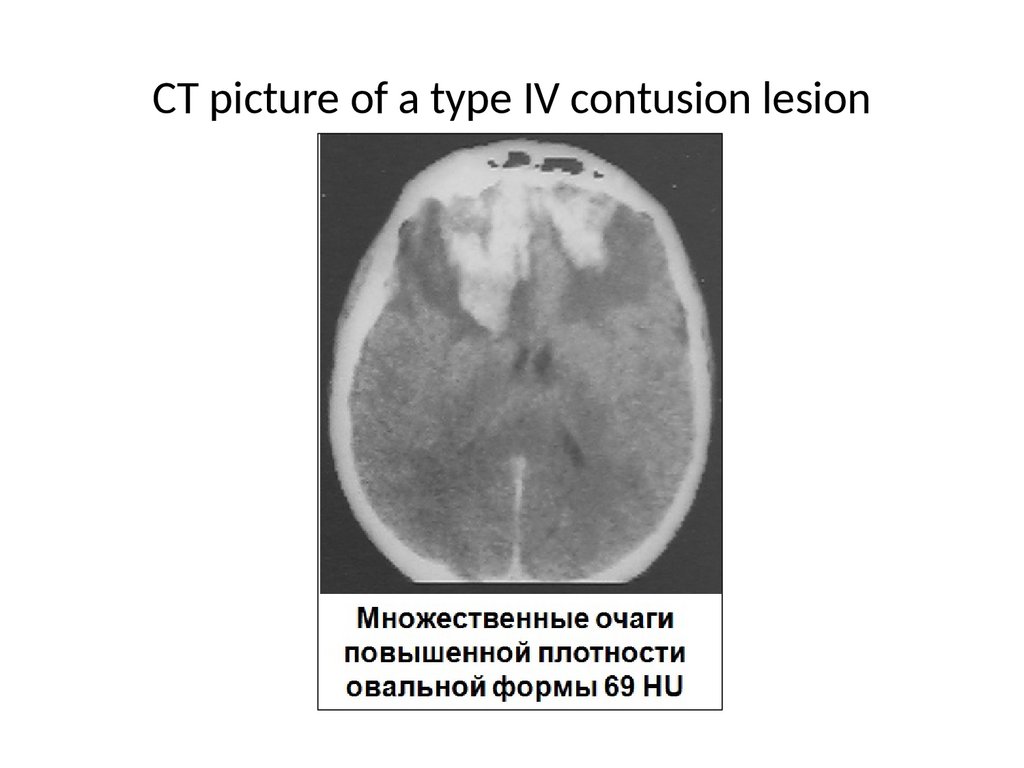
CT classification of brain injuryType
• I is a low density zone within the range of
18-25 HUType
• II – from 26 to 50 HUType
• III – from 51 to 64 HU with areas with a
density of 18 – 25 HUType IV – from 65
to 75 HU (intracerebral hematoma)
32.
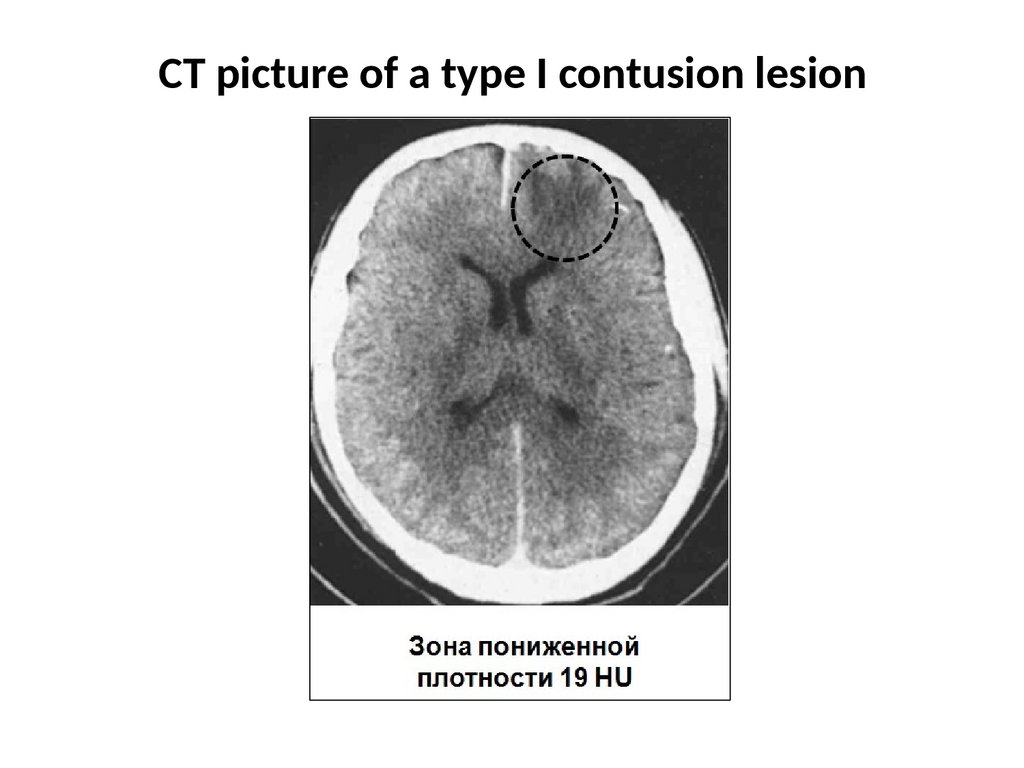
CT picture of a type I contusion lesion33.
CT picture of a type II contusion lesion34.
КТ картина контузионного очага III типа35.
CT picture of a type IV contusion lesion36.
DIFFUSE AXONAL INJURY37.
Classification of hematomas by volume• Up to 40 cm3 – small
• From 40 to 60 cm3 – medium *
• From 60 to 90 cm3 – large
• More than 90 cm3 - massive
* Subdural hematomas of more than 50 cm3 lead to edema, dislocation of
the brain substance. Hemorrhages with a smaller volume usually occur
without edema.
38.
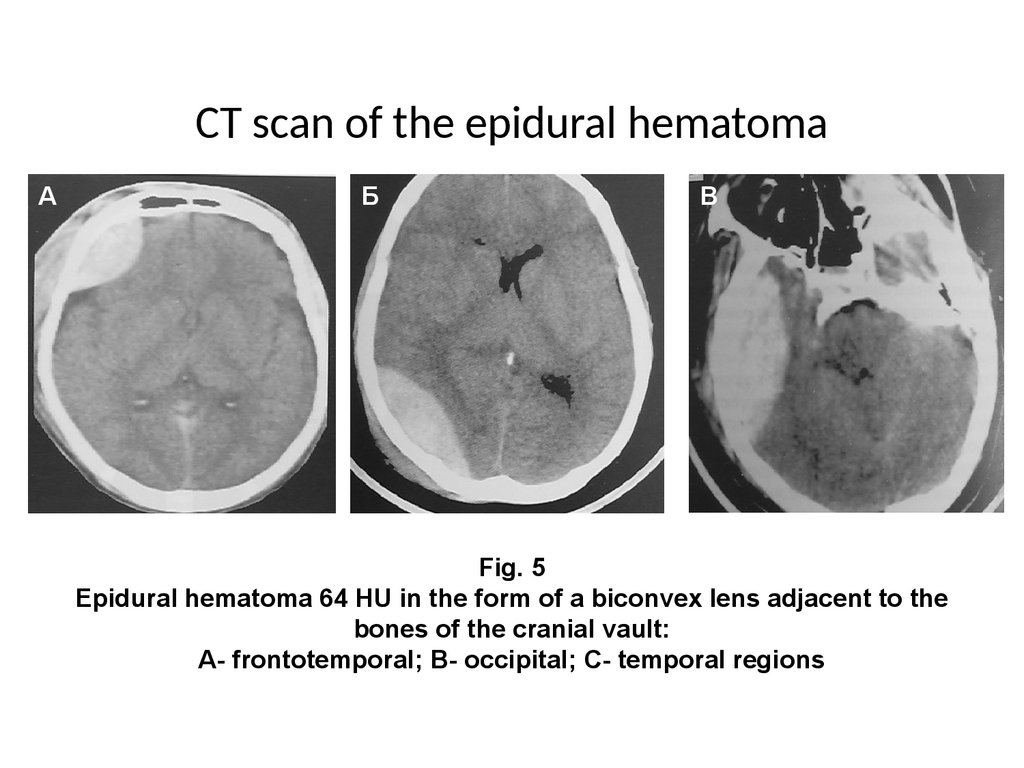
CT scan of the epidural hematomaА
Б
В
Fig. 5
Epidural hematoma 64 HU in the form of a biconvex lens adjacent to the
bones of the cranial vault:
A- frontotemporal; B- occipital; C- temporal regions
39.
40.
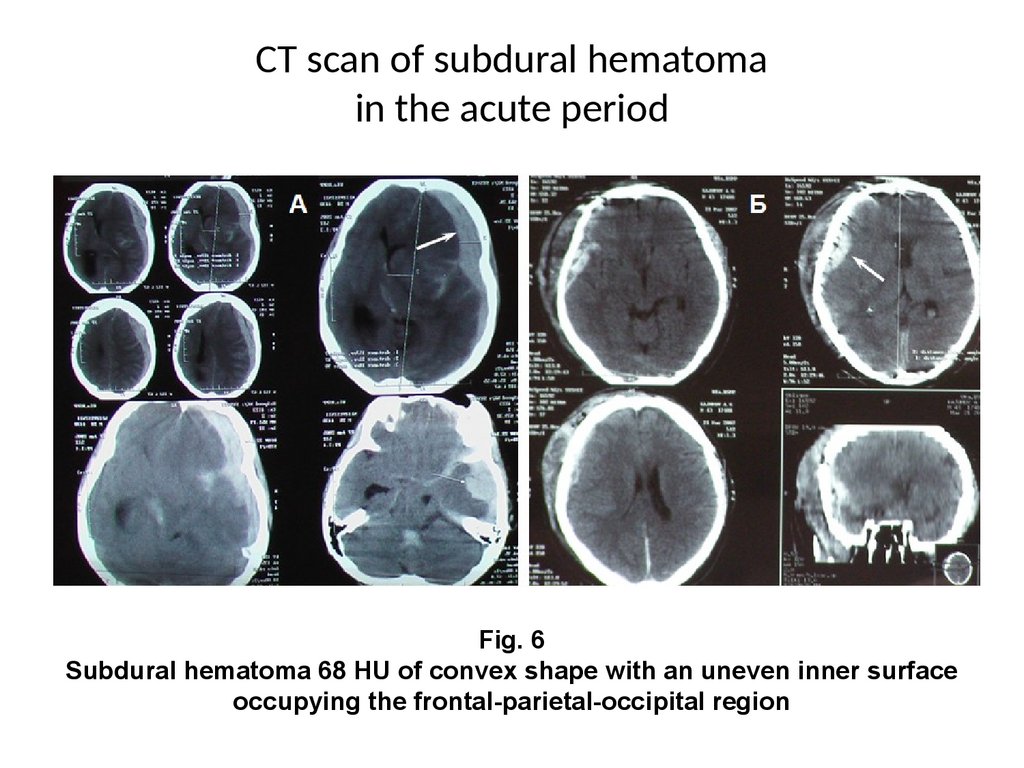
CT scan of subdural hematomain the acute period
Fig. 6
Subdural hematoma 68 HU of convex shape with an uneven inner surface
occupying the frontal-parietal-occipital region
41.
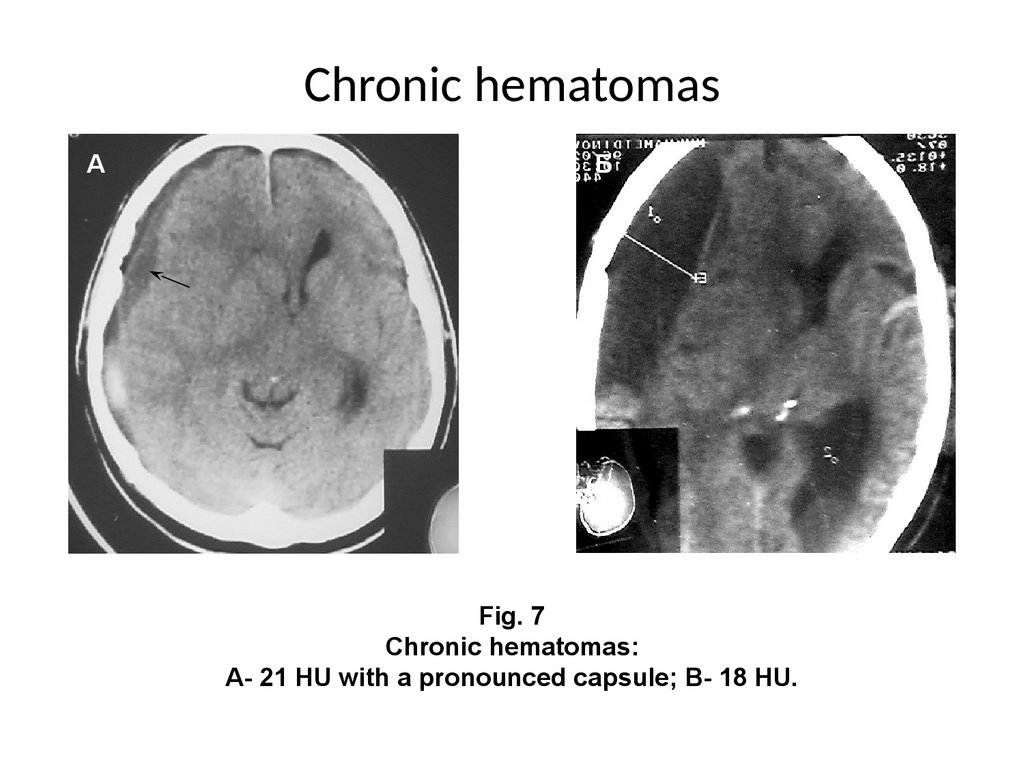
Chronic hematomasА
Б
Fig. 7
Chronic hematomas:
A- 21 HU with a pronounced capsule; B- 18 HU.
42.
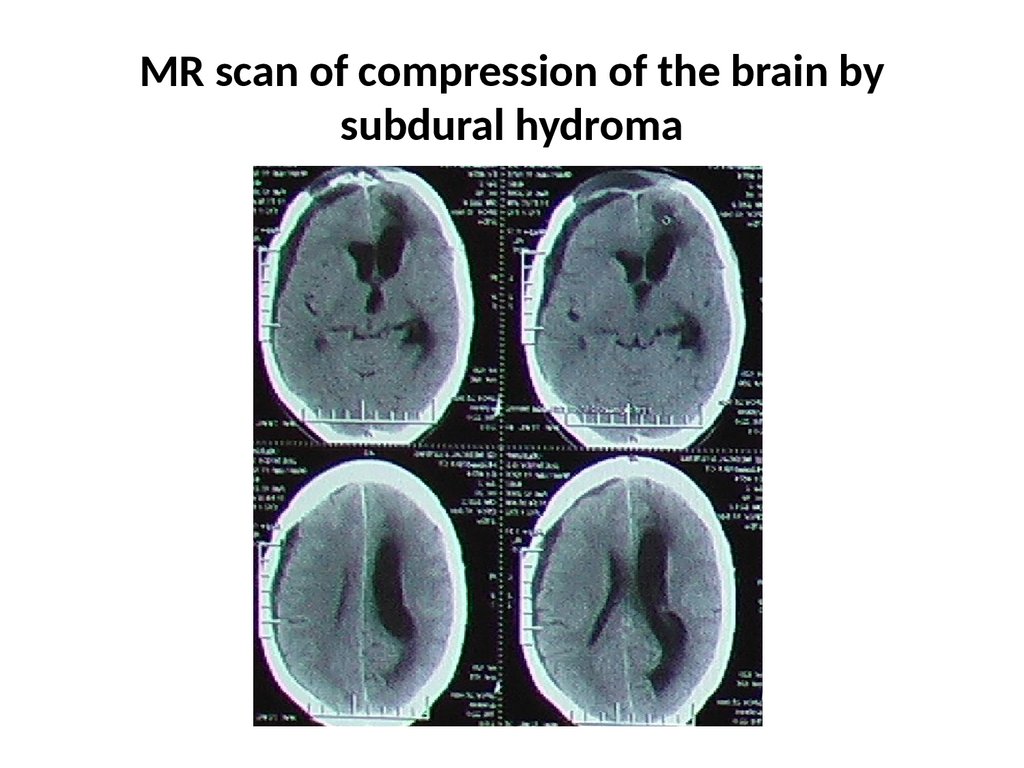
MR scan of compression of the brain bysubdural hydroma
43.
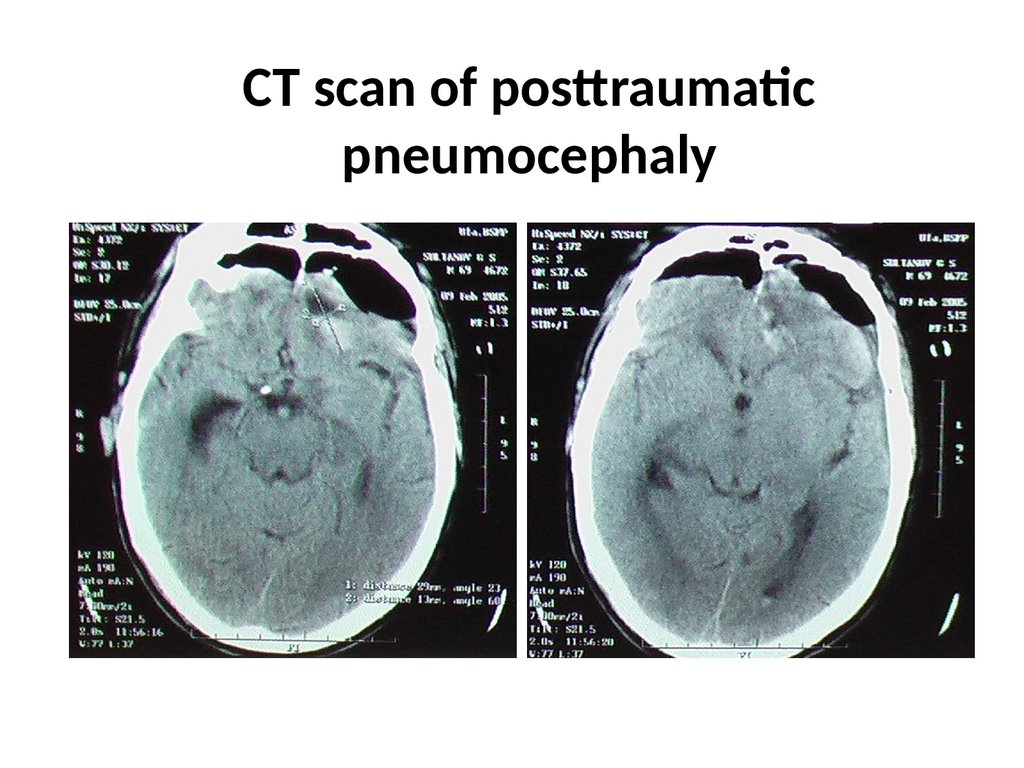
CT scan of posttraumaticpneumocephaly
44.
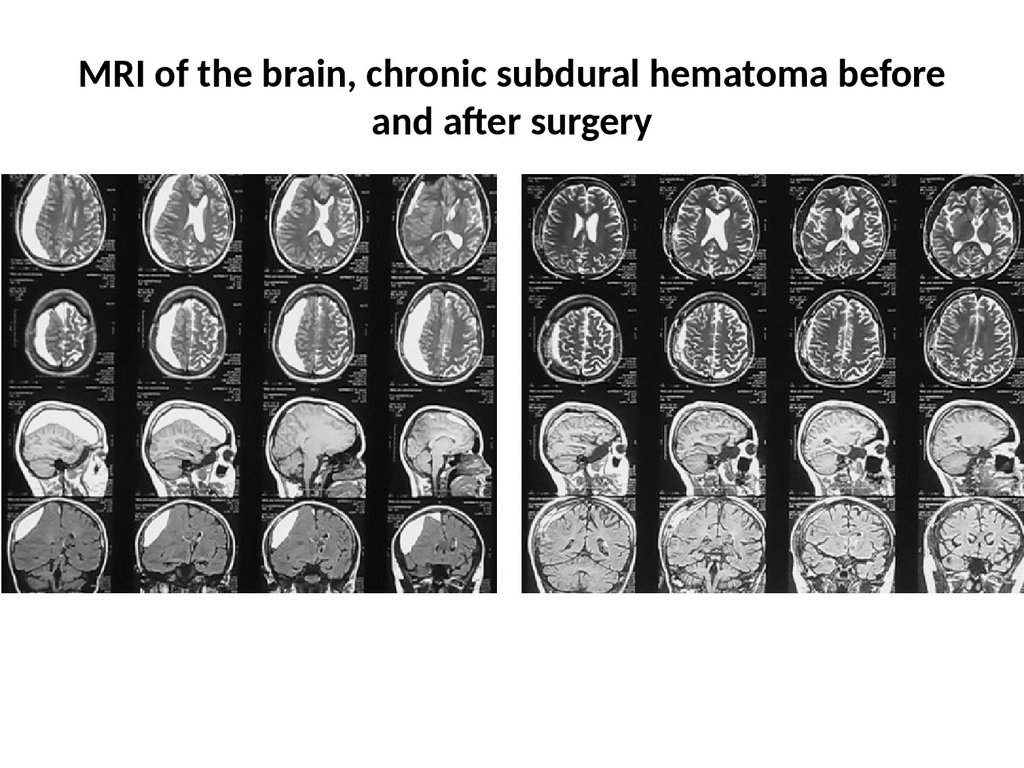
MRI of the brain, chronic subdural hematoma beforeand after surgery
45.
Treatment• Conservative
• Operational
46.
The main directions of conservative treatment forconcussion
1.
2.
3.
4.
5.
6.
7.
observance of bed rest for a period of 1 week*.
sedative (elenium, sanosan, sibazone)
hyposensitizing drugs (diphedrol, pipolfen)
vegetotropic drugs (platyphylline, belloid, betacerc, euphyllin) in normal doses
orally.
dehydrating drugs (furosemide, diacarb, ethacric acid) 1 tab. in the morning for
4-6 days with correction of possible potassium deficiency (diet, panangin).
With persistent asthenia, it is advisable to use caffeine (2 ml of 10% solution 2
times a day) and other psychostimulants (acephen, sydnocarb, centedrine, 1
table each morning and afternoon).
from 3 days neuroprotectors - nootropil, gliatilin, picamilon and others
The duration of hospital stay is limited to 7-10 days. During this period, in
addition to the implementation of a course of therapeutic measures, dynamic
monitoring of the patient is carried out, excluding the compensated phase of
traumatic compression of the brain (“light gap”). It is this circumstance that
largely determines the need for hospitalization
47.
The main directions of conservative treatment for mildand moderate brain injuries
improvement of cerebral blood flow
- improvement of rheological properties of blood (rheopolyglucin, cavinton, euphyllin)
- relief of cerebral vascular spasm (nimotop *, complamin, stugeron, papaverine, etc.)
improvement of energy supply to the brain (10% glucose solution in the form of a polarizing
mixture with subcutaneous insulin injection, )
• elimination of pathological shifts of water sectors in the cranial cavity (lasix 0.5-0.75 mg/ kg,
glycerin 70-75 ml., euphyllin 10.0 ml. 2.4%, diacarb)**
• metabolic therapy (nootropics, cerebrolysin, actovegin, gliatilin)
• hemastatic, anti-enzyme therapy (dicinone, kontrical, gordox, trasilol)
• hyposensitizing therapy 1-11/2 weeks. (diphenhydramine, pipolfen, suprastin, diazoline, tavegil,
etc.)
• sedative therapy
• analgesics
• anticonvulsants according to indications (depakin, phenazepam, finlepsin, benzonal)
• anti-inflammatory treatment
____________________________________________________________________________________
* with spasms caused by subarachnoid hemorrhage (2 mg /hour for 2 weeks, then switch to Table.
form)
** dehydration therapy is performed only after diagnostic lumbar puncture
48.
Indications for the conservative treatment of severebrain contusions
• the victim's stay in the subcompensation phase or moderate
clinical decompensation
• consciousness – stunning 1-2 (at least 10 points on the scale)
• absence of signs of dislocation of the brain stem
• the volume of the fracture site according to CT or MRI data is not
more than 30 cm3 in the temporal lobe, not more than 50 cm3
for the frontal lobe
• Absence of signs of dislocation of the median structures by CT
and MRI of no more than 10 mm, without a pattern of
deformation covering the tank
49.
50.
Indications for surgical intervention• Brain compression syndrome
• The severity of hypertension-dislocation
syndrome
51.
THE PURPOSE OF SURGICALTREATMENT
REDUCING THE MASS EFFECT
REDUCTION OF ICP
REDUCING THE CONCENTRATION
OF NEUROTOXIC SUBSTANCES
52.
Indications for surgical treatment of severe braincontusions
• Persistent stay of the victim in the phase of gross clinical
decompensation
• consciousness – (less than 10 points on the scale)
• pronounced clinical signs of brain stem dislocation
• the volume of the fracture site according to CT or MRI data is
more than 30 cm3 in the temporal lobe, more than 50 cm3 for
the frontal lobe with homogeneity of its structure
• the presence of signs of dislocation of the median structures
on CT and MRI of more than 10 mm, the pattern of
deformation of the enclosing tank
53.
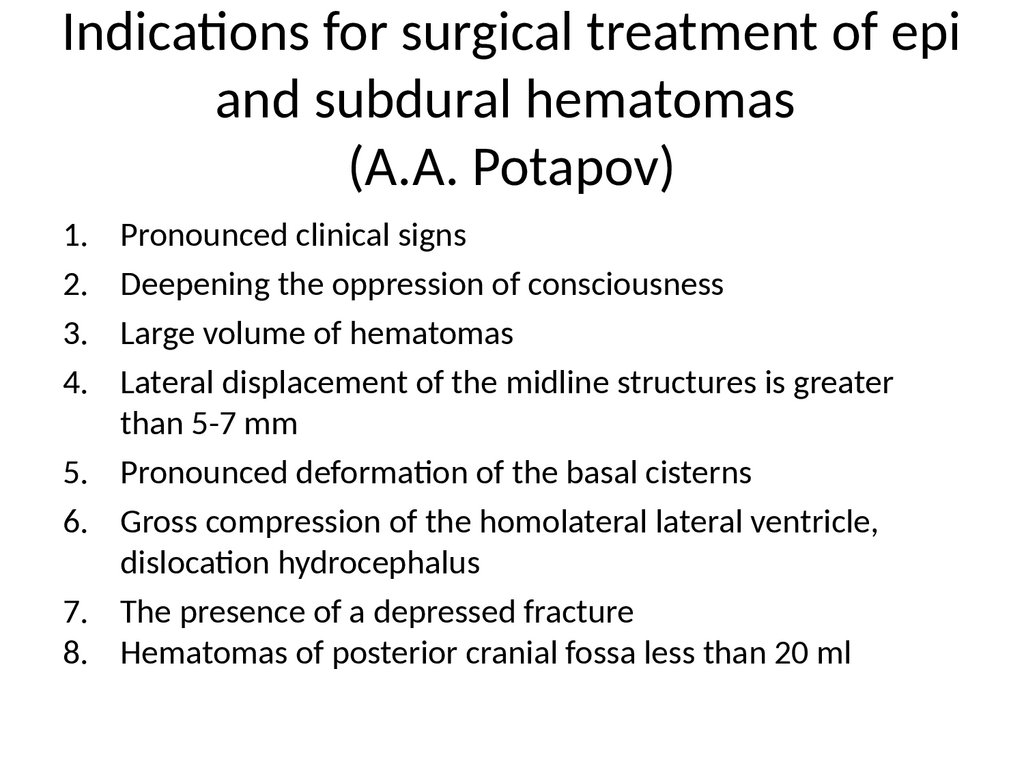
Indications for surgical treatment of epiand subdural hematomas
(A.A. Potapov)
1.
2.
3.
4.
5.
6.
7.
8.
Pronounced clinical signs
Deepening the oppression of consciousness
Large volume of hematomas
Lateral displacement of the midline structures is greater
than 5-7 mm
Pronounced deformation of the basal cisterns
Gross compression of the homolateral lateral ventricle,
dislocation hydrocephalus
The presence of a depressed fracture
Hematomas of posterior cranial fossa less than 20 ml
54.
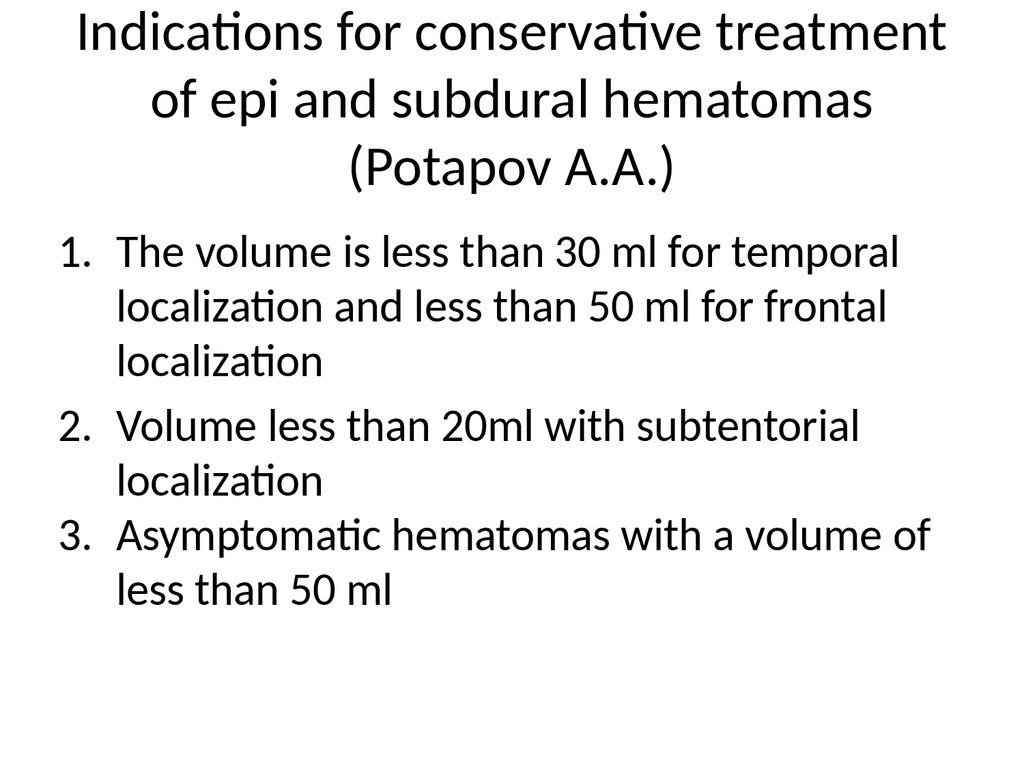
Indications for conservative treatmentof epi and subdural hematomas
(Potapov A.A.)
1. The volume is less than 30 ml for temporal
localization and less than 50 ml for frontal
localization
2. Volume less than 20ml with subtentorial
localization
3. Asymptomatic hematomas with a volume of
less than 50 ml
55.
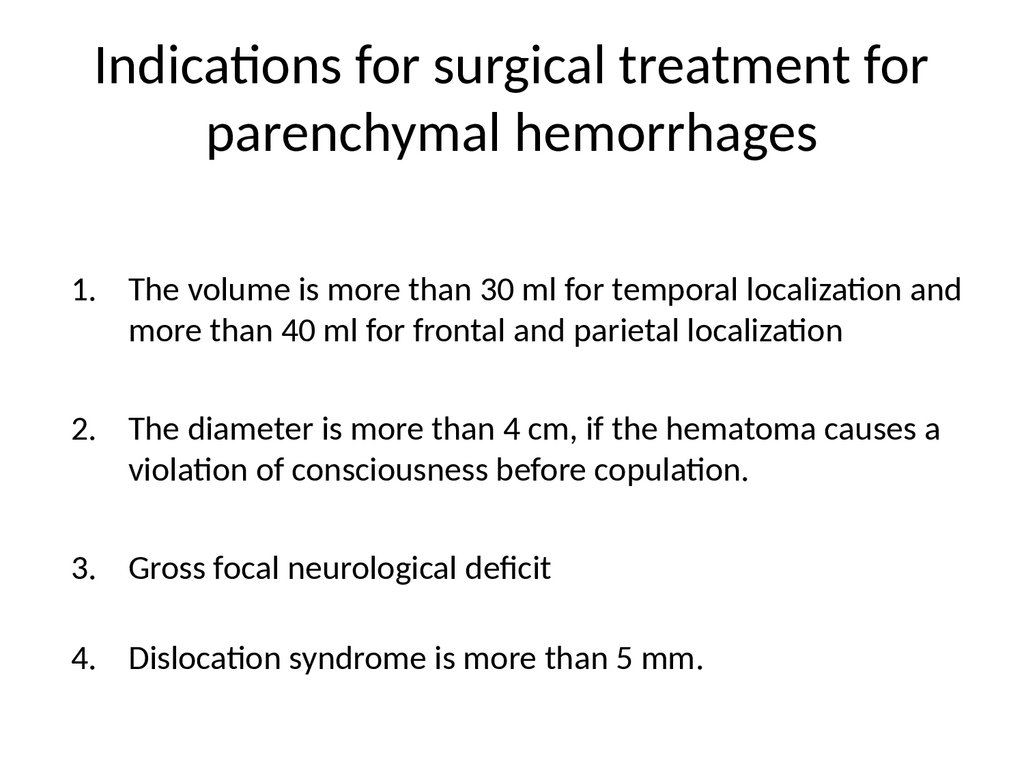
Indications for surgical treatment forparenchymal hemorrhages
1. The volume is more than 30 ml for temporal localization and
more than 40 ml for frontal and parietal localization
2. The diameter is more than 4 cm, if the hematoma causes a
violation of consciousness before copulation.
3. Gross focal neurological deficit
4. Dislocation syndrome is more than 5 mm.
56.
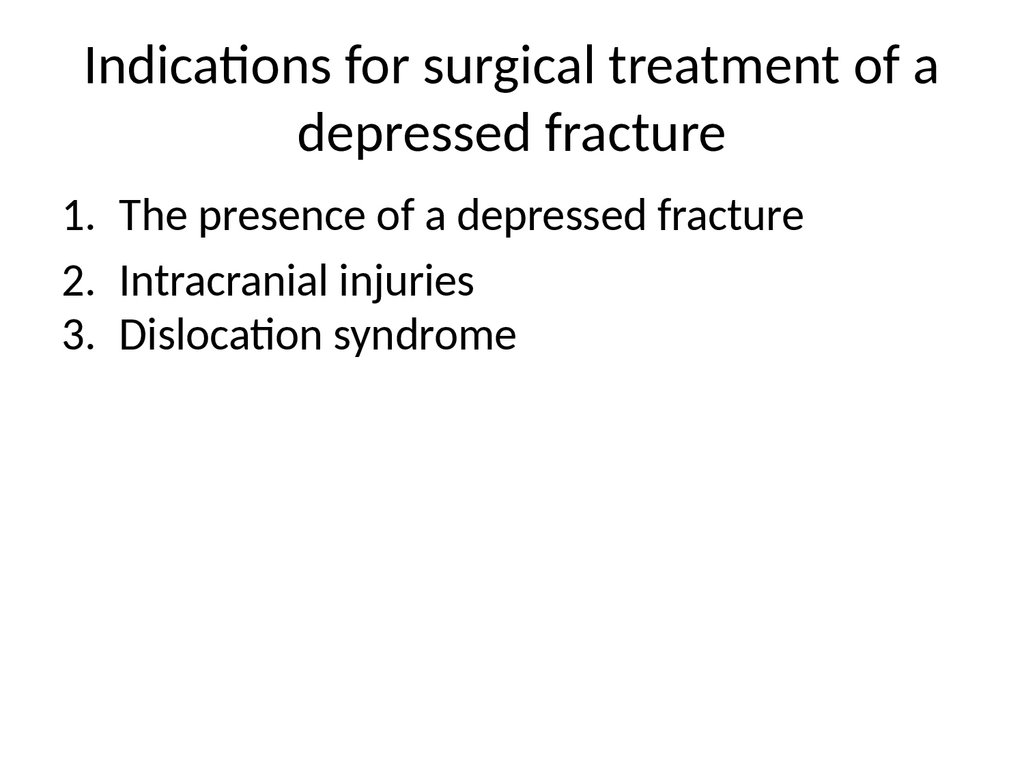
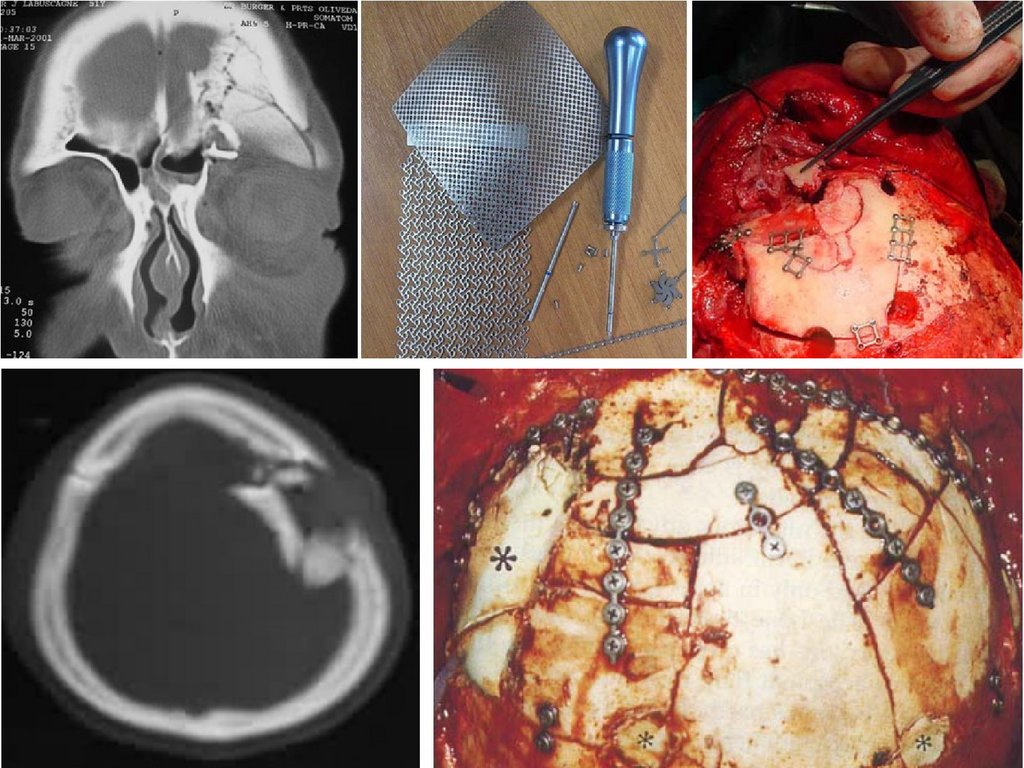
Indications for surgical treatment of adepressed fracture
1. The presence of a depressed fracture
2. Intracranial injuries
3. Dislocation syndrome
57.
Indications for conservative treatmentof a depressed fracture
1. Asymptomatic course
2. Absence of intracranial substrates
3. The affected area is outside the functionally
significant zones.
4. The area is less than 10 cm2 and the depth is
less than 1 cm
Dynamic EEG
58.
59.
60.
Trepanation of the skull• Bone and plastic surgery
• Resection
• Diagnostic trefining holes
61.
General principles of trepanation• Skin incision, taking into account the localization of blood
vessels and nerves
• The base of the cutaneous aponeurotic flap is directed to
the base of the skull
• The autopsy of TMO is X – shaped or horseshoe-shaped
in the vascular-free zone
• The main stage of the operation
• TMO suturing
• Fixation of the bone flap during osteoplastic trepanation
62.
Epidural hematomas• The most common cause is damage to the
branches of the middle meningeal artery
• Bone plastic trepanation is used for removal
• Search for the source of bleeding
• Prevention of recurrence of hematoma
63.
Subdural hematomas• Source – cortical vessels
• Wide resection trepanation
• Search for the source of bleeding
64.
Damage to venous sinuses• Suturing of the rupture site
• Repair of the defect with a muscle, a
hemostatic sponge
• Temporary sinus tamponade
65.
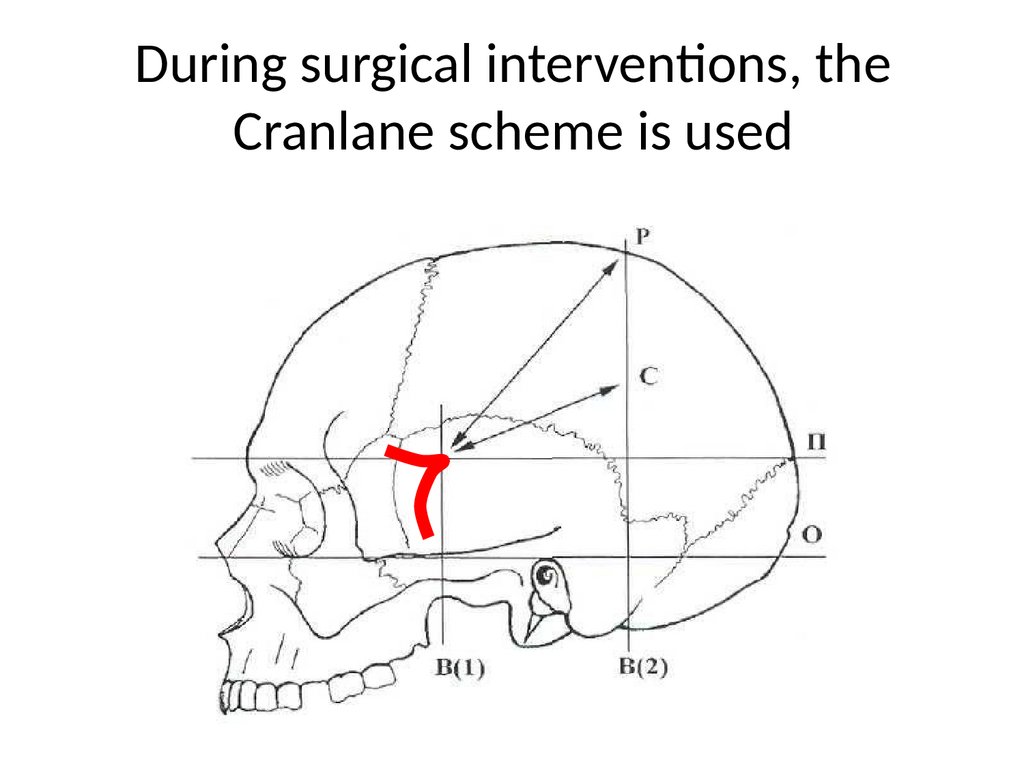
During surgical interventions, theCranlane scheme is used
66.
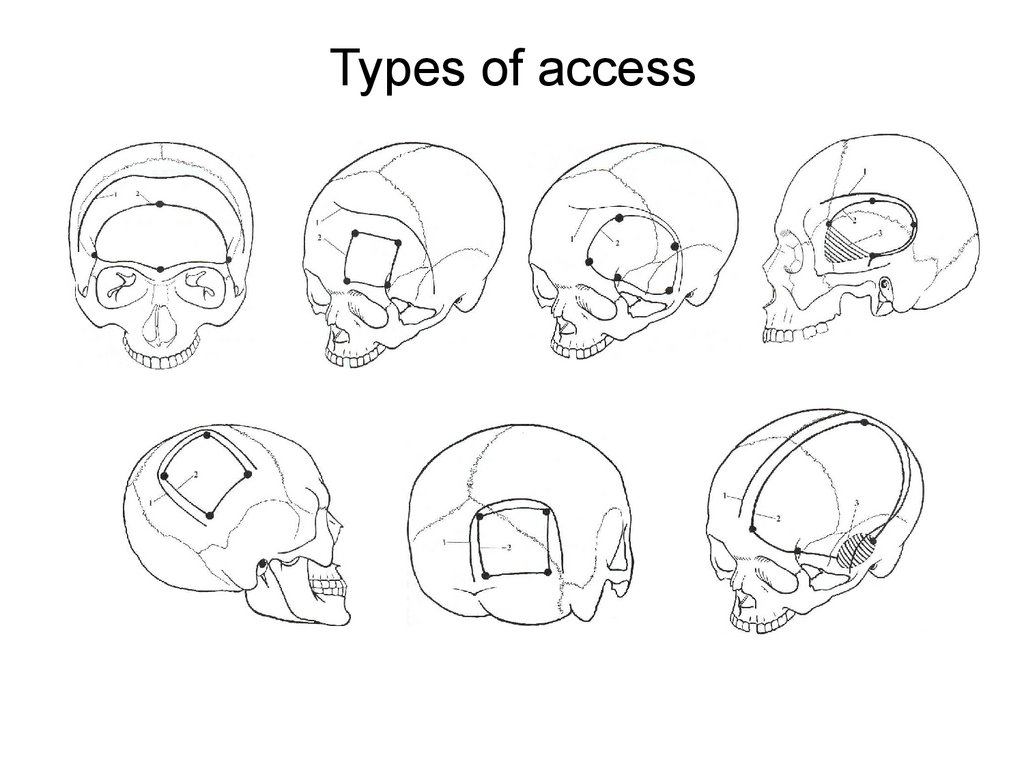
Types of access67.
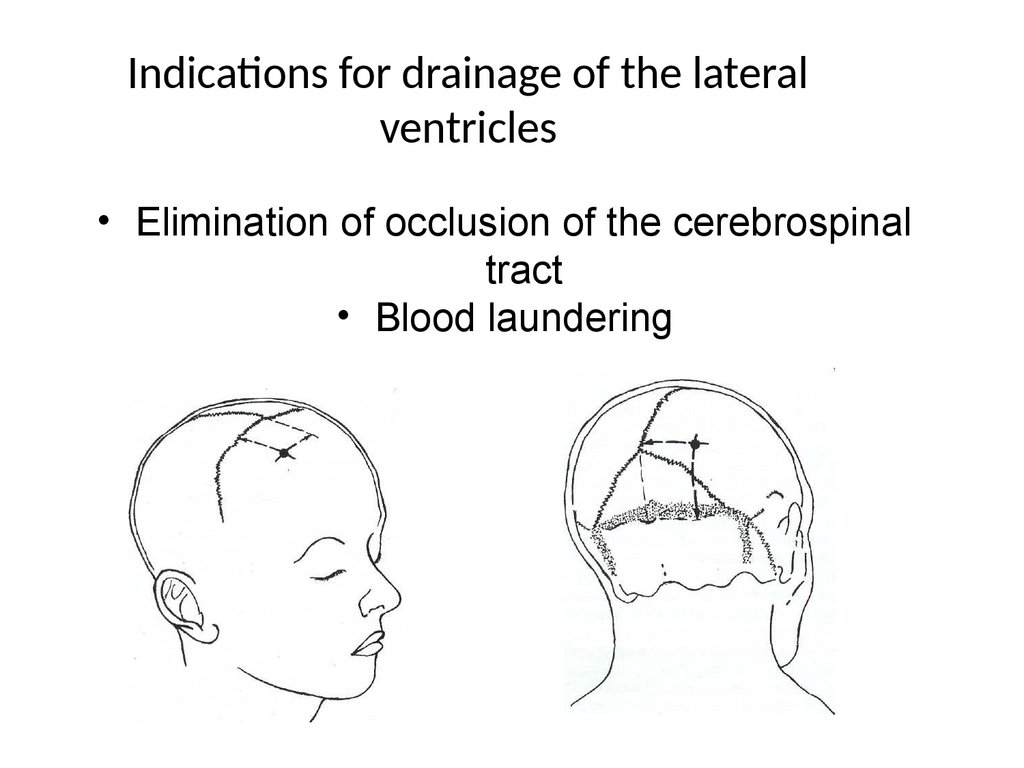
Indications for drainage of the lateralventricles
• Elimination of occlusion of the cerebrospinal
tract
• Blood laundering
68.
DECOMPRESSIVE TREPANATION OFTHE SKULL
69.
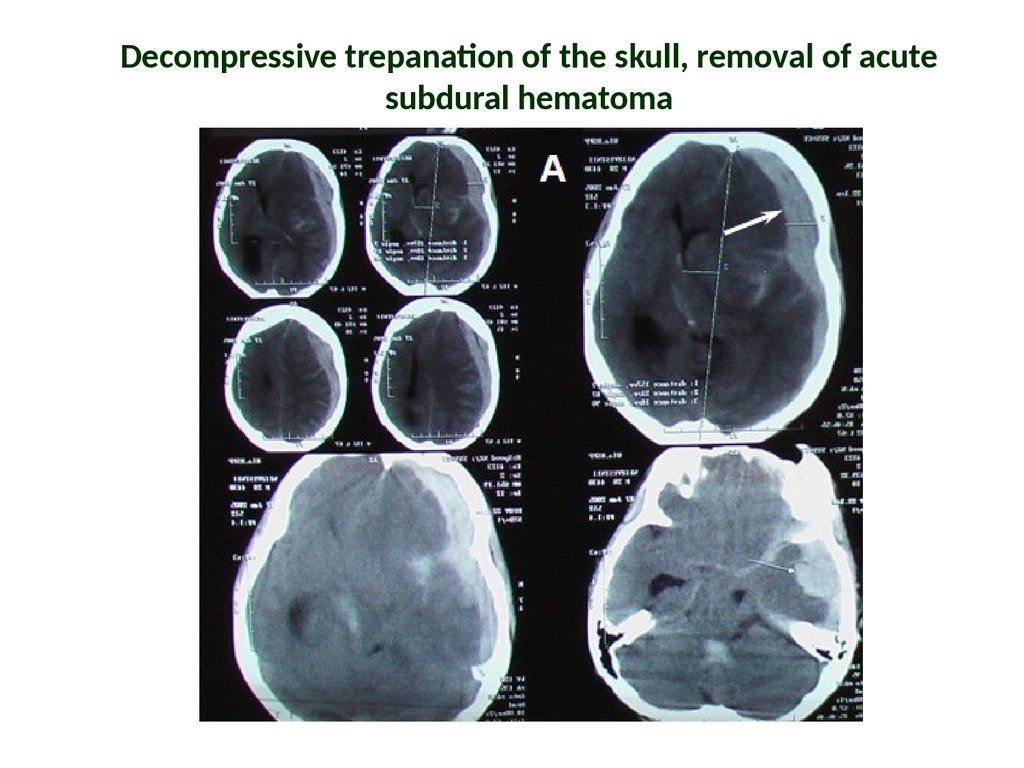
Decompressive trepanation of the skull, removal of acutesubdural hematoma
70.
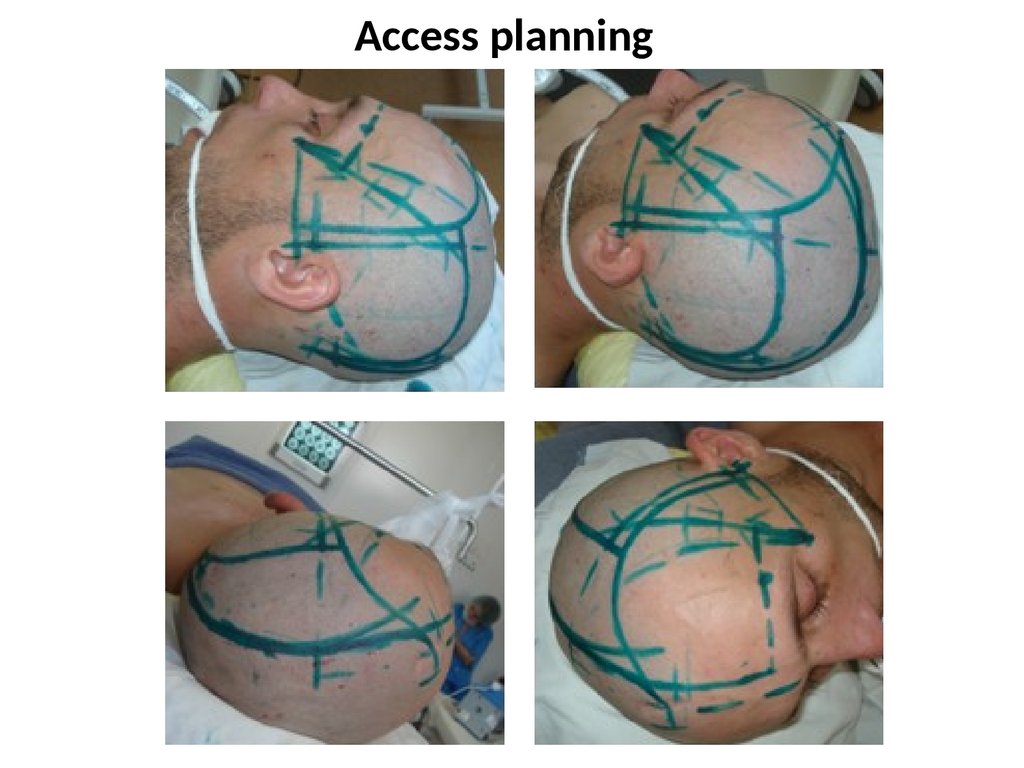
Access planning71.
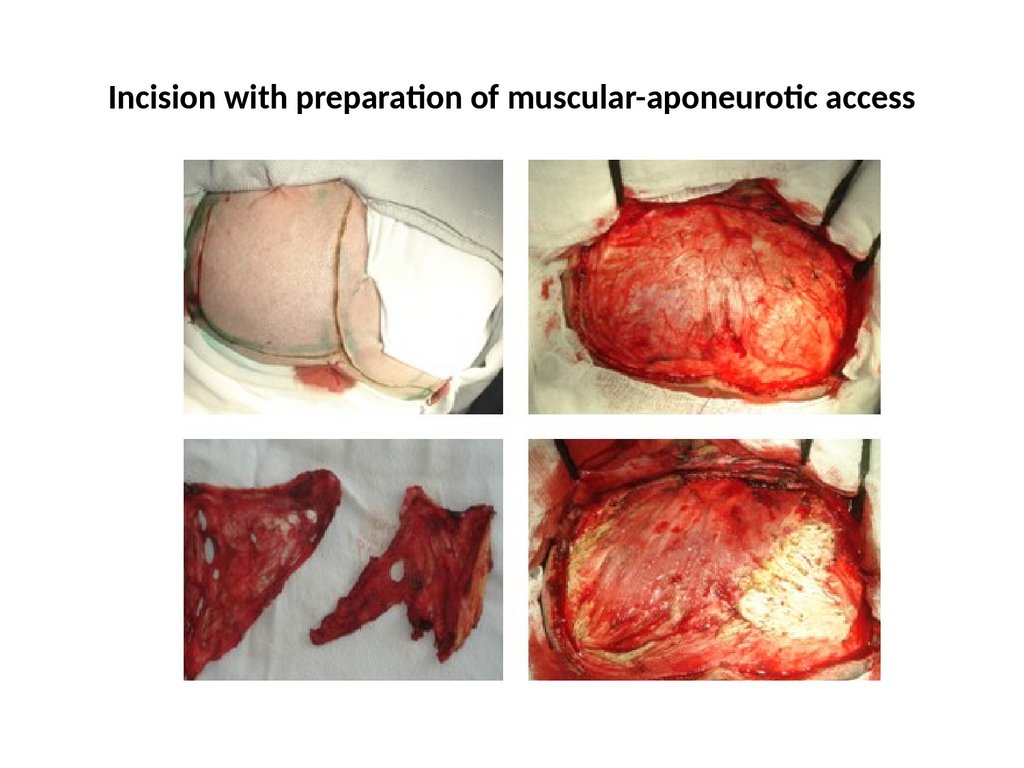
Incision with preparation of muscular-aponeurotic access72.
73.
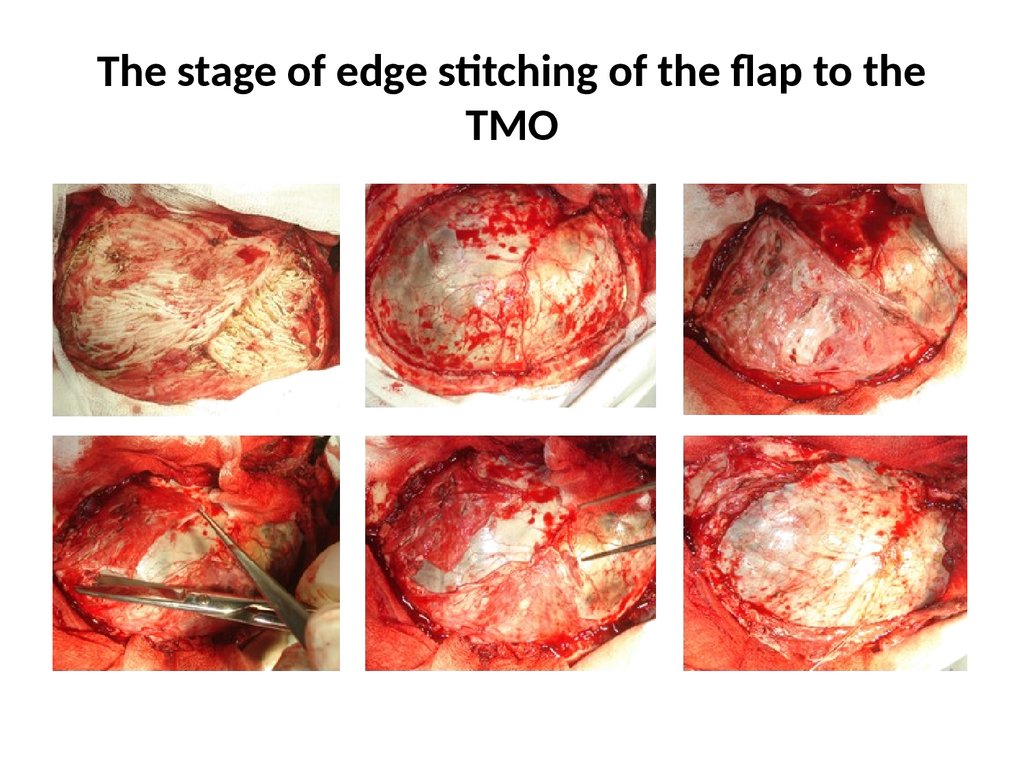
The stage of edge stitching of the flap to theTMO
74.
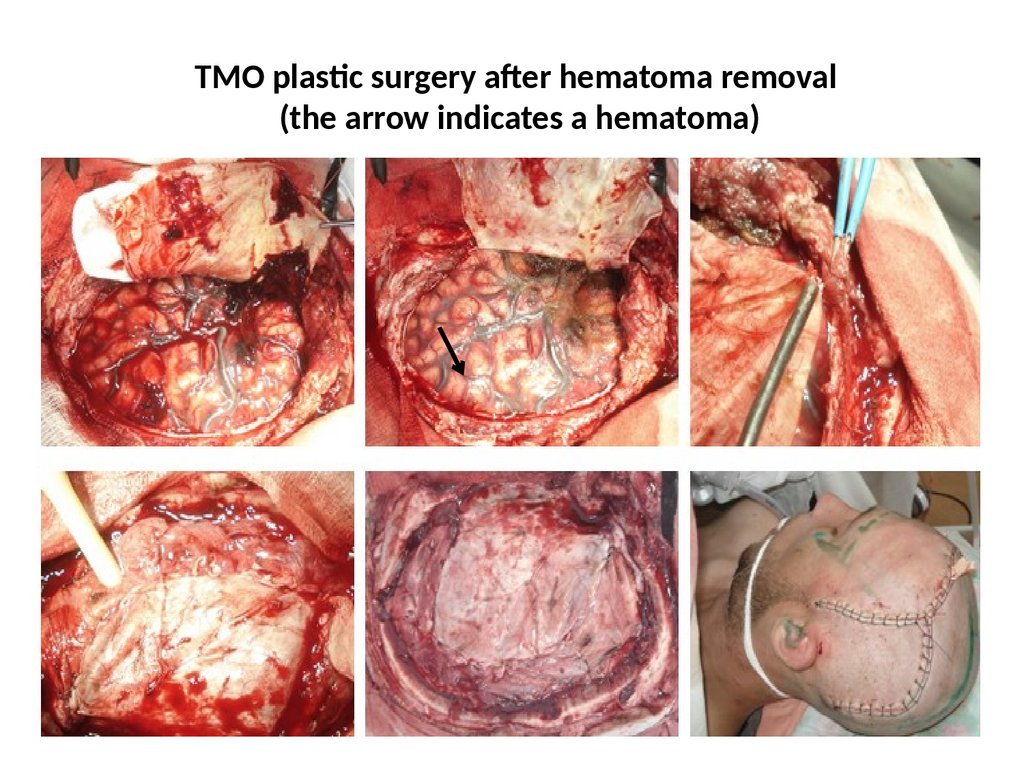
TMO plastic surgery after hematoma removal(the arrow indicates a hematoma)
75.
ResultTHE CONSEQUENCES OF
TRAUMATIC BRAIN INJURY
Tissue
Cerebrospinal fluid dynamics
Vascular
Good recovery
Moderate disability
Gross disability
Vegetative state
Death



 Медицина
Медицина