Похожие презентации:
Inflammation. Exudative inflammation
1. INFLAMMATION. EXUDATIVE INFLAMMATION
Department of Histology, Embryology and Cytology ofPirogov Russian National Research Medical University
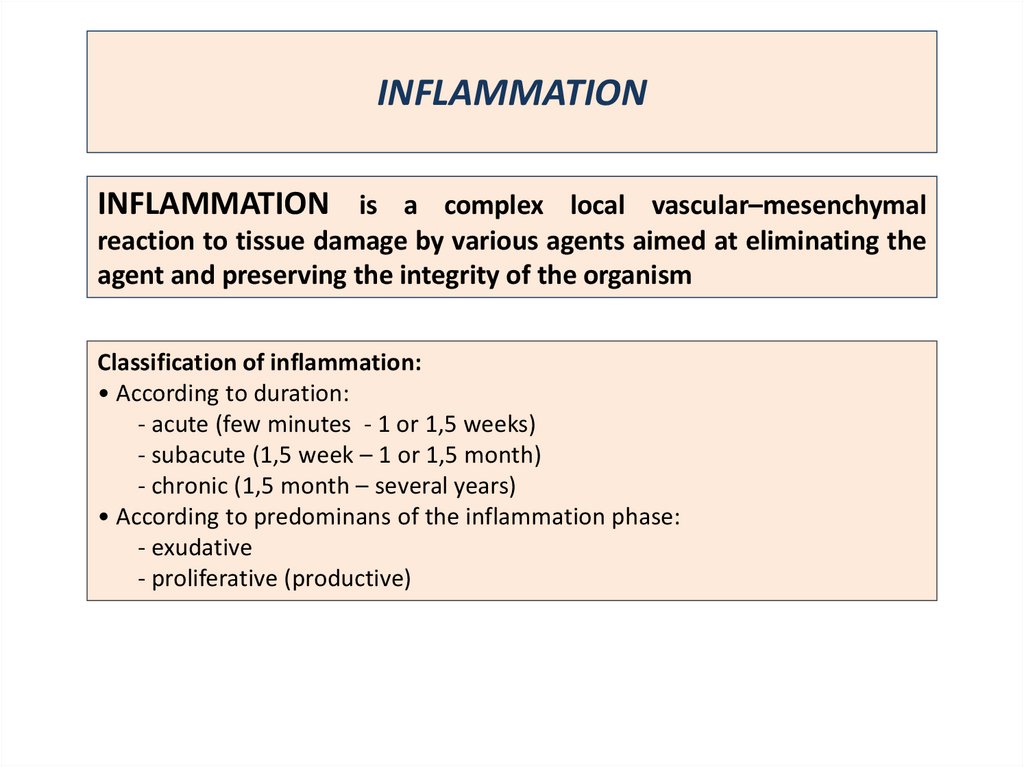
2. INFLAMMATION
INFLAMMATION is a complex local vascular–mesenchymalreaction to tissue damage by various agents aimed at eliminating the
agent and preserving the integrity of the organism
Classification of inflammation:
• According to duration:
- acute (few minutes - 1 or 1,5 weeks)
- subacute (1,5 week – 1 or 1,5 month)
- chronic (1,5 month – several years)
• According to predominans of the inflammation phase:
- exudative
- proliferative (productive)
3.
ETIOLOGY OF INFLAMMATIONBiologic agents: viruses, bacteria, fungi, parasites, immunologic
factors (antibodies, immune complexes, activated lymphocytes) &
so on.
Physical agents: radiation, electricity, high & low temperature,
trauma, foreign body.
Chemical agents: endotoxins, exotoxins, poisons, drags & so on.
Unknown factors
3
4. INFLAMMATION
5. STEPS OF INFLAMMATORY REACTIONS
PHASES OF INFLAMMATION :• Alteration (injury)
• Exudation
• Proliferation
The external manifestations of
inflammation,
often
called
its
cardinals signs, are fever (calor),
hyperemia (rubor), swelling (tumor),
pain (dolor), and loss of function.
6. ALTERATION
It is the initial phase of inflammation. It is characterized by the release ofinflammatory mediators - biological active substances that provide chemical
and molecular connections between processes in the inflammatory focus.
ALTERATION:
• PRIMARY - it develops immediately after the direct action of the etiological
factor and is formed at the level of cells and subcellular structures
• SECONDARY - due to the action of lysosomal enzymes activating the
processes of glycolysis, lipolysis and proteolysis.
MORPHOLOGICAL CHANGES
DYSTROPHY
(mucoid,
fibrinoid
swelling);
NECROSIS.
BIOCHEMICAL CHANGES
Activation of lysosomal enzymes;
Release of chemical mediators of
inflammation.
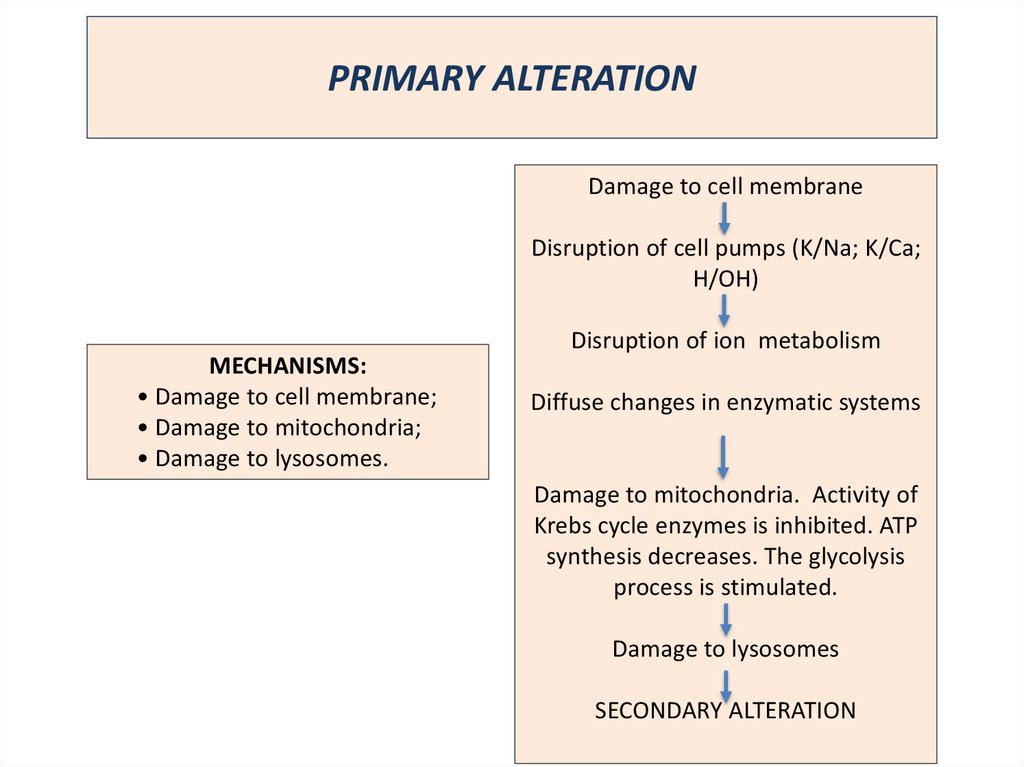
7. PRIMARY ALTERATION
Damage to cell membraneDisruption of cell pumps (K/Na; K/Ca;
H/OH)
MECHANISMS:
• Damage to cell membrane;
• Damage to mitochondria;
• Damage to lysosomes.
Disruption of ion metabolism
Diffuse changes in enzymatic systems
Damage to mitochondria. Activity of
Krebs cycle enzymes is inhibited. ATP
synthesis decreases. The glycolysis
process is stimulated.
Damage to lysosomes
SECONDARY ALTERATION
8. SECONDARY ALTERATION
Lysosomal enzymesAccumulation of breakdown products of fat and carbohydrate metabolism
Tissue acidosis
Accumulation of biological active substances – inflammatory mediators
PLASMA MEDIATORS :
kallikrein-kinin system: Kallikrein,
Kinins
(bradykinin);
complement system (C5a, C3a, C3b, complex C
5 a - Usa);
blood coagulation system
(Hageman
factor);
fibrinolytic blood system
CELLULAR MEDIATORS :
vasoactive amines: Histamine, Serotonin;
arachidonic acid metabolites: Prostaglandins,
Leukotrienes;
FAT ( Platelet activation factor);
cytokines: IL-1, TNF (a, b), IL-8, g-interferon;
the contents of lysosomes.
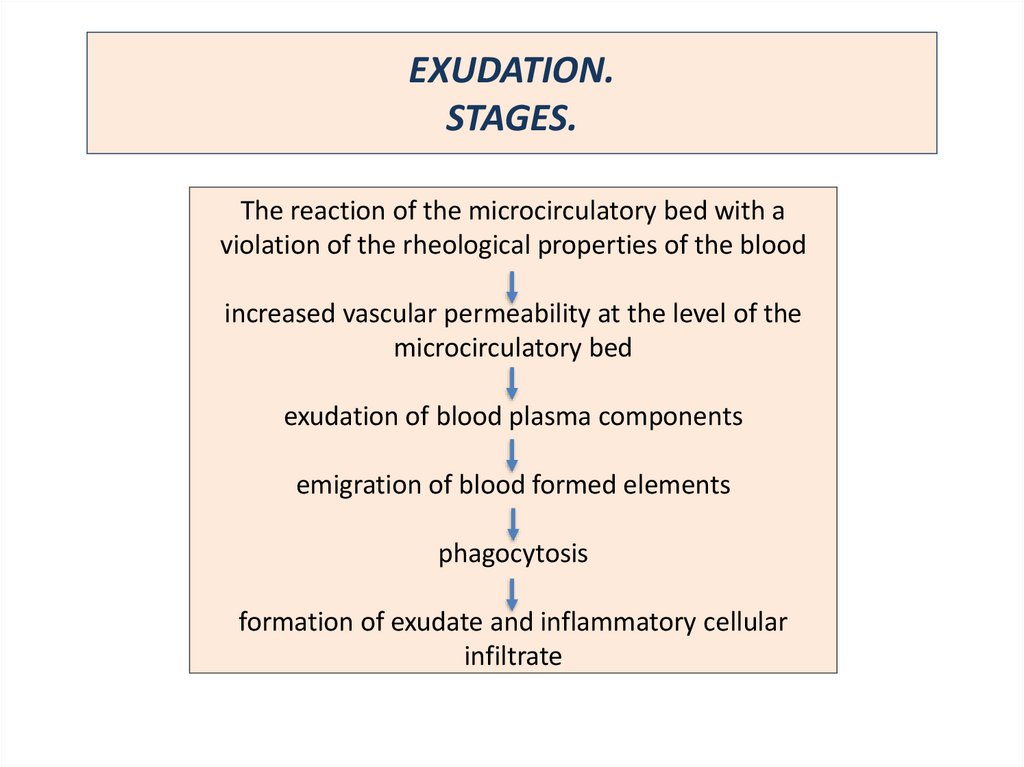
9. EXUDATION. STAGES.
The reaction of the microcirculatory bed with aviolation of the rheological properties of the blood
increased vascular permeability at the level of the
microcirculatory bed
exudation of blood plasma components
emigration of blood formed elements
phagocytosis
formation of exudate and inflammatory cellular
infiltrate
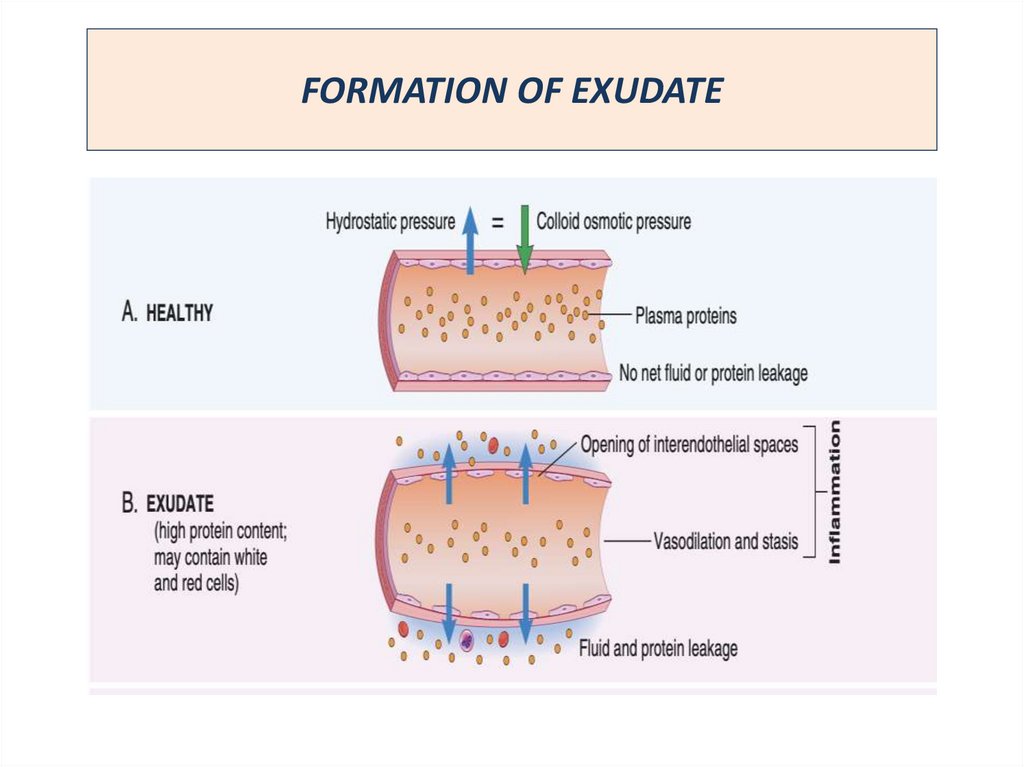
10. FORMATION OF EXUDATE
11. Process of leukocyte migration through blood vessels
• interendothelial• transendothelial (T – lymphocytes)
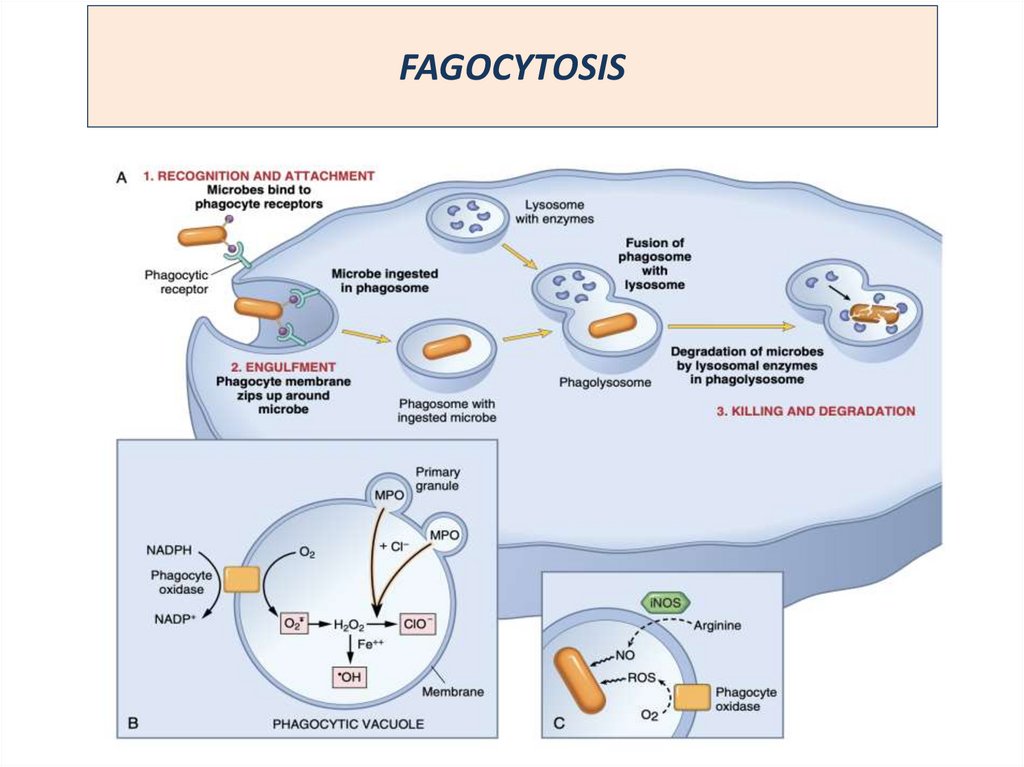
12. FAGOCYTOSIS
13. PROLIFERATION
Proliferation is the final phase of inflammation, aimed at restoring thedamaged tissue. In the focus of inflammation, cells multiply, differentiate and
transform in to another types (f.e. macrophages
The giant multinucleated
Pirogov-Langhans cell)
FOMATION OF INFILTRATE:
1.
2.
3.
4.
Epithelioid cells
giant multinucleated cell
Labrocytes
Polynuclear leucocytes
Lymphocytes, plasma cells
ORGANISATION
1. Fibroblasts
2. Glucogenogenesis
14.
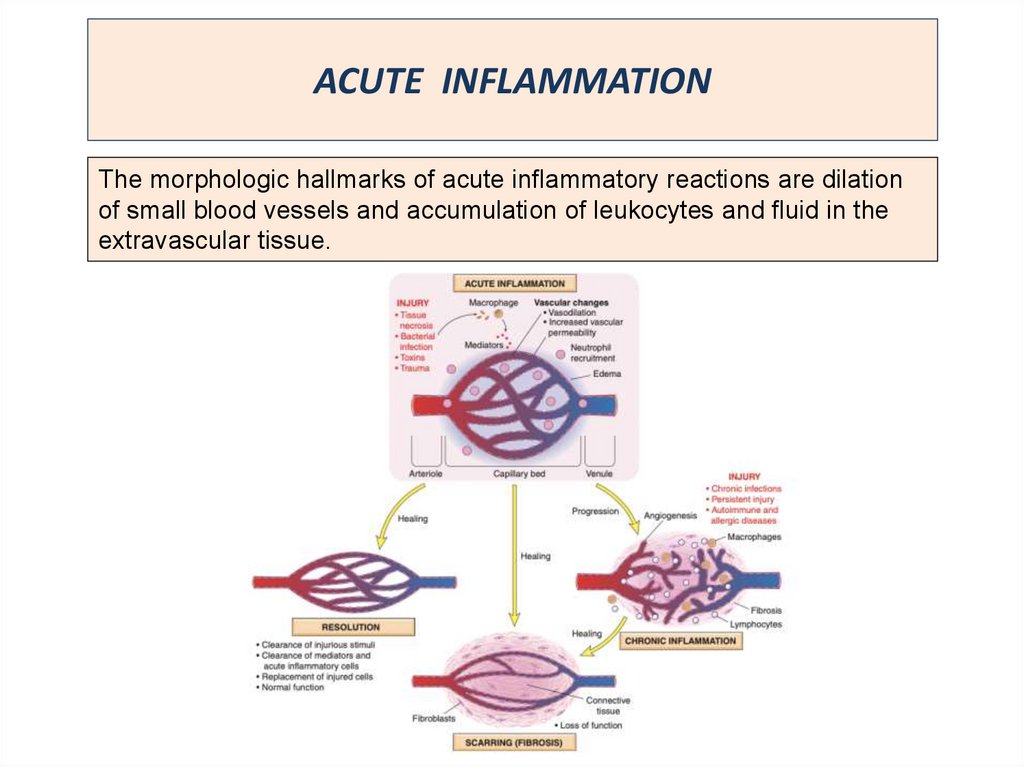
ACUTE INFLAMMATIONThe morphologic hallmarks of acute inflammatory reactions are dilation
of small blood vessels and accumulation of leukocytes and fluid in the
extravascular tissue.
15. EXUDATIVE INFLAMMATION
EXUDATIVE INFLAMMATION is the type of inflammation, characterized bypredominance of exudation over alteration & proliferation.
It occurs as a consequence of severe injuries, with result to greater
vascular permeability to allow larger molecules (specifically fibrinogen) to
pass the endothelial barrier.
TYPES OF EXUDATIVE INFLAMMATION :
serous;
fibrinous;
purulent;
hemorrhagic;
rotten (putrid);
catarrhal;
mixed.
TYPE OF INFLAMMATION DEPENDS ON :
• Severity of injury;
• Vascular of injuring permeability;
• Type of injuring agent;
• Prolongation of its influence.
Exudative inflammation usually is acute,
but purulent & catarrhal inflammation
may be acute or chronic.
16. SEROUS INFLAMMATION
Serous inflammation is marked by the accumulation of serum -likeprotein-rich exudates in body cavities lined by the peritoneum, pleura, or
pericardium or spaces created by tissue injury.
Exudate contains fluid, up to 2% proteins, a few cells (neutrophils,
macrophages, epithelium.
APPEARES:
• on the serous membranes (rheumatic fever, uremia);
• on the mucous membranes;
• skin;
• Meninges;
• peripheral nerves;
• parenchymal organs.
ETHIOLOGY:
• streptococcus (erysipelas);
• viral infections (chicken pox, natural small pox, herpetic fever);
• thermal and chemical factors.
OUTCOMES:
• resorption of exudate;
• transition to purulent or fibrinous inflammation;
• Sclerosis or Hyalinosis.
17. SEROUS INFLAMMATION in the parenchymal organs
LIVER – serous hepatitis;KIDNEY – serous glomerulonephritis;
HEART – serous myocarditis;
LUNG – serous pneumonia.
Outcomes of the serous inflammation:
• resolution with complete regeneration
of structure;
• progression to other types of
inflammation.
Erysipelas
Etiology – streptococcus
Macro: skin is edematous, red with
inflammatory hyperemia
Micro: epidermis is separated from derma by a
local collection of serous effusion.
Dermis with hyperemia and some cellular
infiltrate
18.
Serous dermatitis ("bullous erysipelas")Hematoxilin - eosin
2
3
3
1
1 - detachment of the epidermis
2 - fullness of vessels in the dermis
3 - leukocyte infiltrate in the dermis
19. FIBRINOUS INFLAMMATION
It is the type of exudative inflammation, characterized by exudation,which is reached by fibrin.
It occur as a consequence of severe injuries, with result to greater
vascular permeability to allow larger molecules (specifically fibrinogen)
to pass the endothelial barrier.
ETIOLOGY:
TOXIC FACTORS
(UREMIA);
BACTERIAL INFECTIONS;
VIRUS INFECTIONS.
Fibrinous pericarditis:
The thick epicardium
covered with friable grey
masses with hair – like
spongeous
form.
Figurative name is
“hair heart”
20.
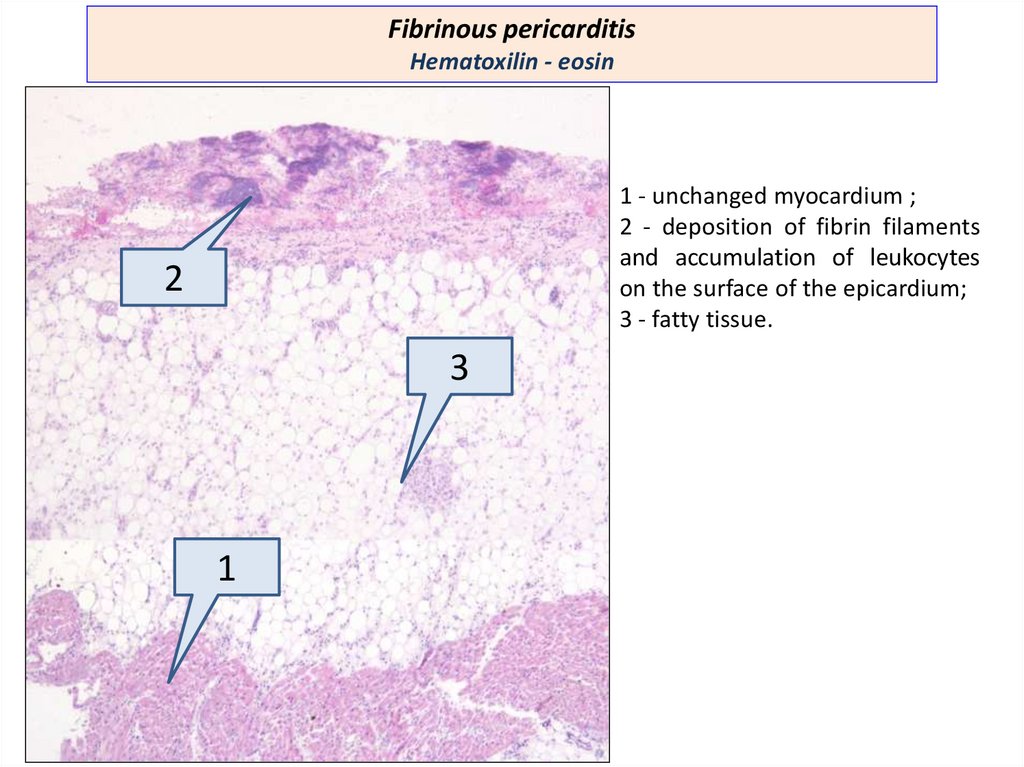
Fibrinous pericarditisHematoxilin - eosin
1 - unchanged myocardium ;
2 - deposition of fibrin filaments
and accumulation of leukocytes
on the surface of the epicardium;
3 - fatty tissue.
2
3
1
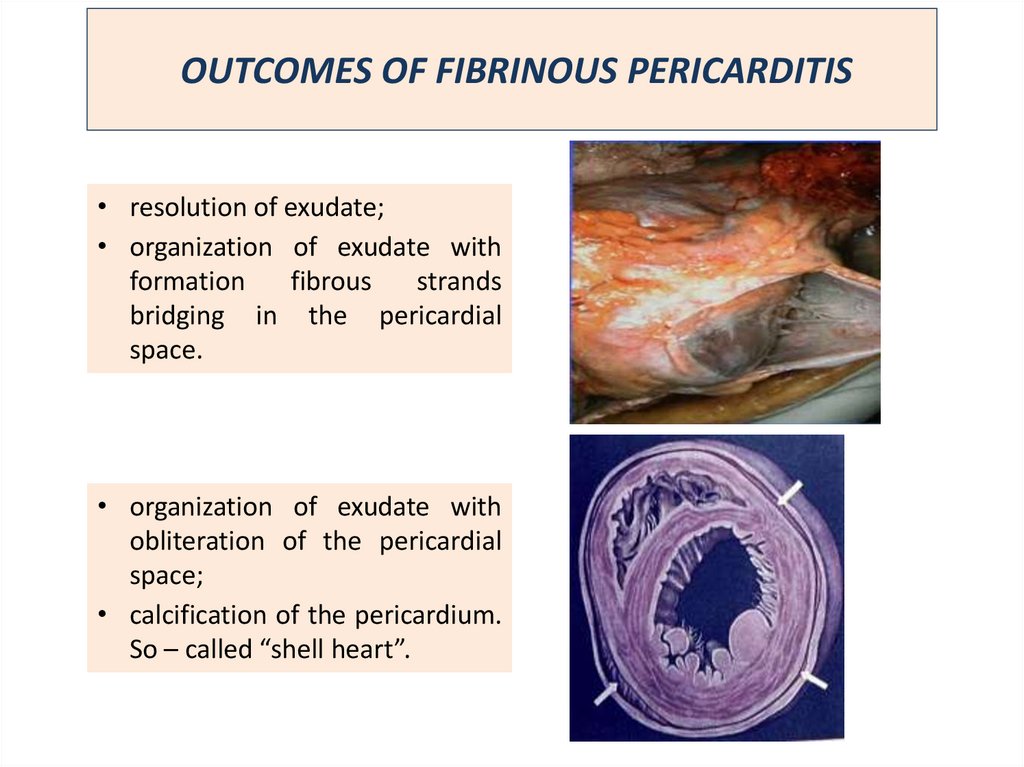
21. OUTCOMES OF FIBRINOUS PERICARDITIS
• resolution of exudate;• organization of exudate with
formation
fibrous
strands
bridging in the pericardial
space.
• organization of exudate with
obliteration of the pericardial
space;
• calcification of the pericardium.
So – called “shell heart”.
22. FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANES
According to the force of connection with tissues:• croupous
• diphtheritic
CROUPOUS INFLAMMATION develops on the mucous
membranes covered with cuboidal or columnar epithelium
laying on thin solid base connective tissue. Necrosis is not
deep
GROSSLY: gray friable film lie on the erosion mucous
surface. The fibrinous films are thin and may be remove
easily
23. FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANES
CROUPOUS TRACHEITIS:(diphtheria, uraemia).
COMPLICATION: friable film
asphyxia (true croup)
CROUPOUS COLITIS (disenteria,
uraemia).
OUTCOME:
• film flakes away easily
• resolution with complete
regeneration of mucous
membrane
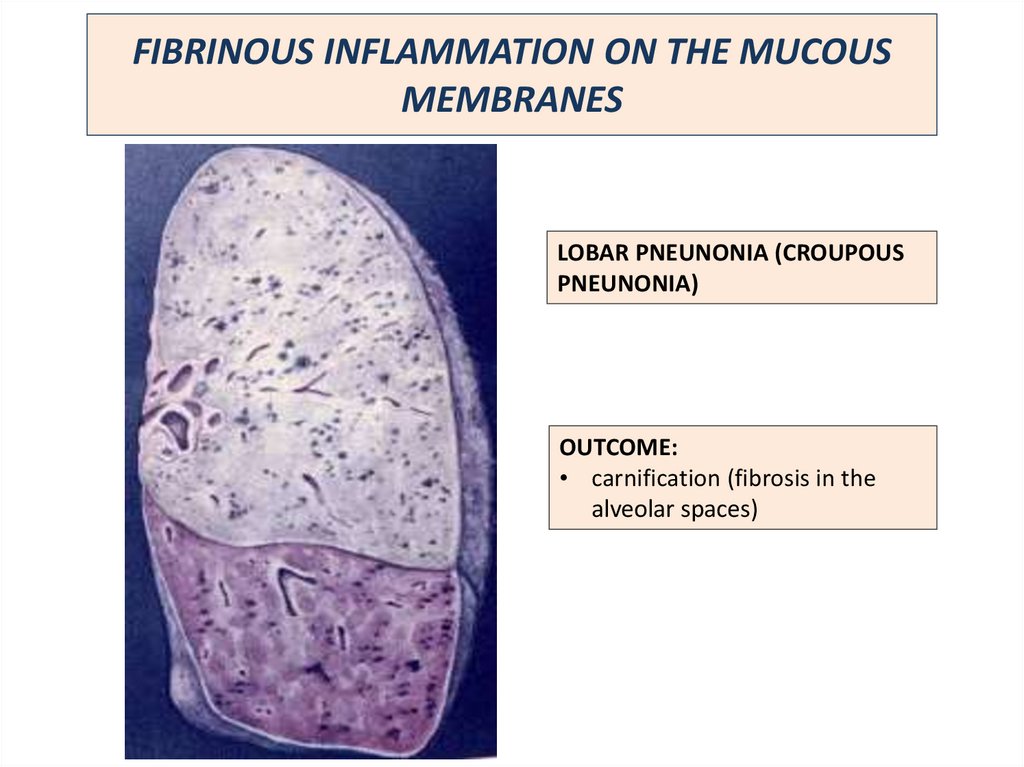
24. FIBRINOUS INFLAMMATION ON THE MUCOUS MEMBRANES
LOBAR PNEUNONIA (CROUPOUSPNEUNONIA)
OUTCOME:
• carnification (fibrosis in the
alveolar spaces)
25. DIPHTHERITIC INFLAMMATION
IT develops on the mucous membranes covered with squamous or transitionalepithelium laying on thick friable base connective tissue. Necrosis is deep
GROSSLY: The fibrinous films is thick, solid, connected strongly with injured
tissue. Removing of this cover leads to deep ulceration
ORGANS: pharynx, esophagus, uterus, vagina, intestine, stomach, urinary
bladder
26. DIPHTHERITIC INFLAMMATION
Diphtheritic amygdalates(Diphtheria)
Diphtheritic
colitis
dysentery, caused by
Dysenteria)
(severe
Shigella
Outcome is scarring after ulceration
27. HEMORRAGIC INFLAMMATION
Characterized by presence of numerous erythrocytes in the exudateAccompanied with severe infections such as pestilence, anthrax.
Accompanied with negative chemotaxis of neutrophils.
It is characteristically for influenza.
Big mottled lung
Hemorrhagic pneumonia.
Influenza
Multiple airless small and
large inflammative foci with
red color
28. PURULENT INFLAMMATION
Purulent inflammation is characterized by the production of pus, an exudateconsisting of neutrophils, the liquefied debris of necrotic cells, and edema fluid.
Accompanied with destruction of inflamed tissue, known as proteolysis
ETIOLOGY :
Pyogenic microorganizms (Staphylococcus, Streptococcus, Gonooccus, E. coli and other
Some chemical factors (turpenic, mestard) - caused aseptic purulent inflammation
CLASSIFICATION:
1. PHLEGMON – diffuse purulent inflammation;
2. ABSCESS -are localized collections of pus caused by suppuration within a
tissue, an organ, or confined space;
3. EMPYEMA - purulent inflammation of the anatomic cavity walls with the
accumulation of pus.
29. PURULENT INFLAMMATION PHLEGMON OF THE SUBCUTANEUS FAT
Subcutaneous fat is saturated withyellowish exudate
Diffuse neutrophil infiltration
30.
Phlegmon of subcutaneous tissueHematoxilin - eosin
2
1
2
1
1
1 - diffuse infiltration of adipose tissue by polymorphonuclear leukocytes;
2 - adipocytes
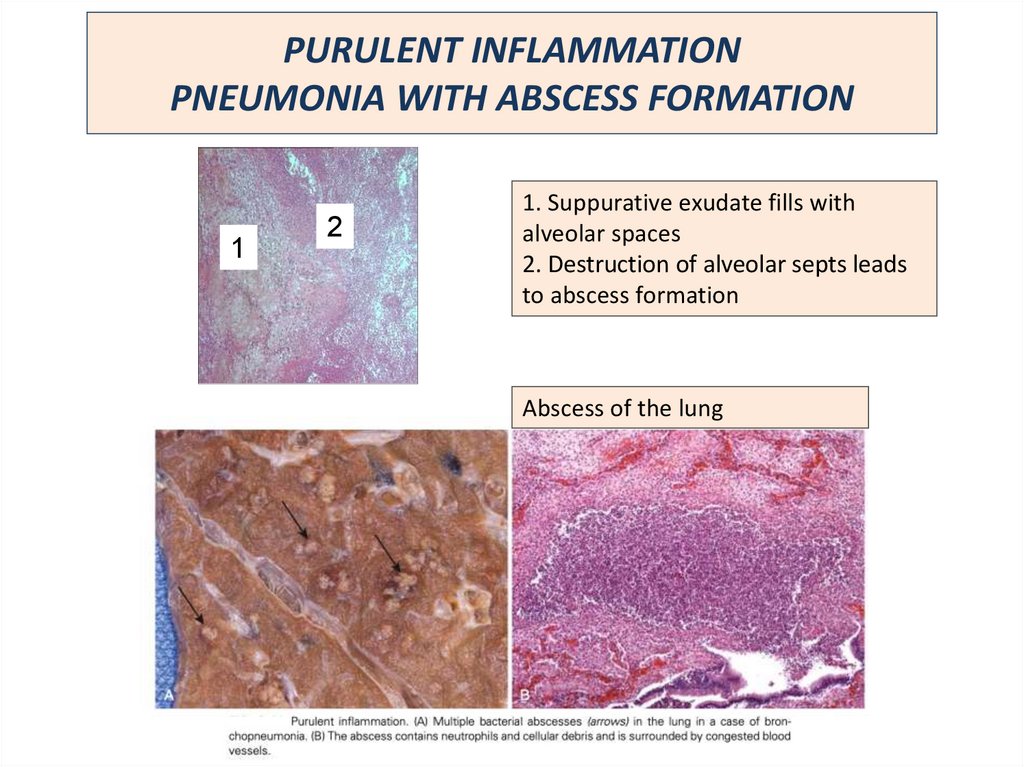
31. PURULENT INFLAMMATION PNEUMONIA WITH ABSCESS FORMATION
12
1. Suppurative exudate fills with
alveolar spaces
2. Destruction of alveolar septs leads
to abscess formation
Abscess of the lung
32. PURULENT INFLAMMATION
Phlegmonous appendicitisPurulent meningitis
33.
CATARRAL INFLAMMATIONAppears only in the mucous membranes, producing mucous exudate
CLASSIFICATION:
1. Acute;
2. Chronic: atrophic, hypertronic.
Catarrhal tracheitis
Catarrhal sinusitis
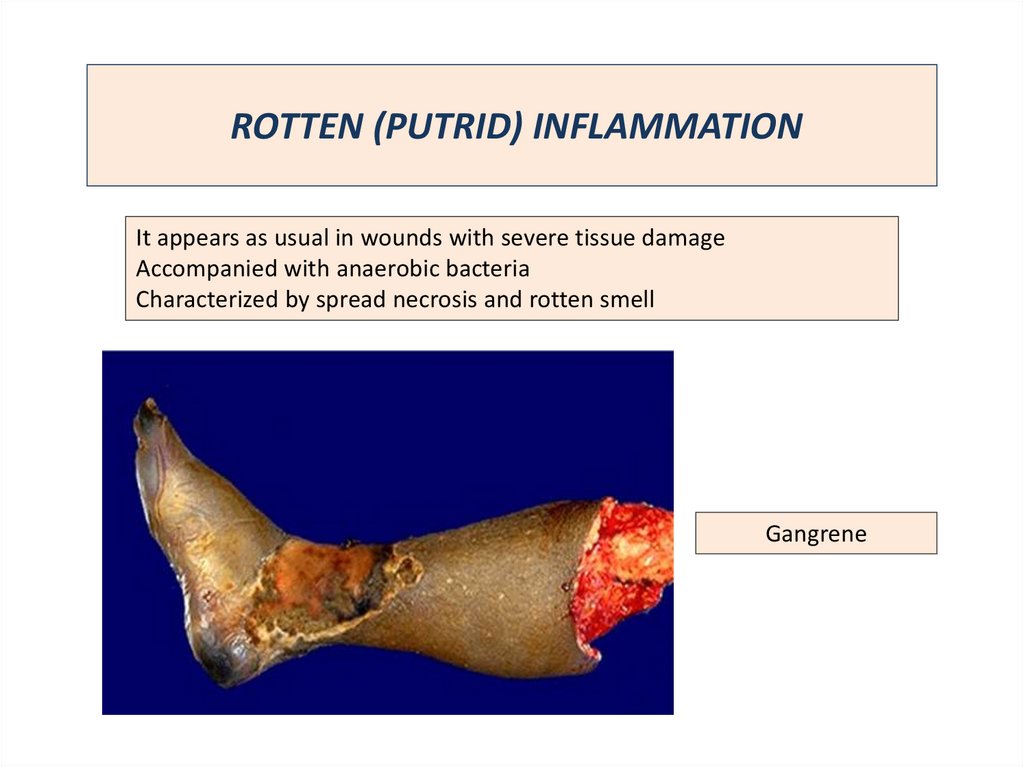
34. ROTTEN (PUTRID) INFLAMMATION
It appears as usual in wounds with severe tissue damageAccompanied with anaerobic bacteria
Characterized by spread necrosis and rotten smell
Gangrene






















 Медицина
Медицина