Похожие презентации:
Total neoadjuvant chemotherapy with FOLFIRINOX regimen in patients with resectable locally advanced gastric
1.
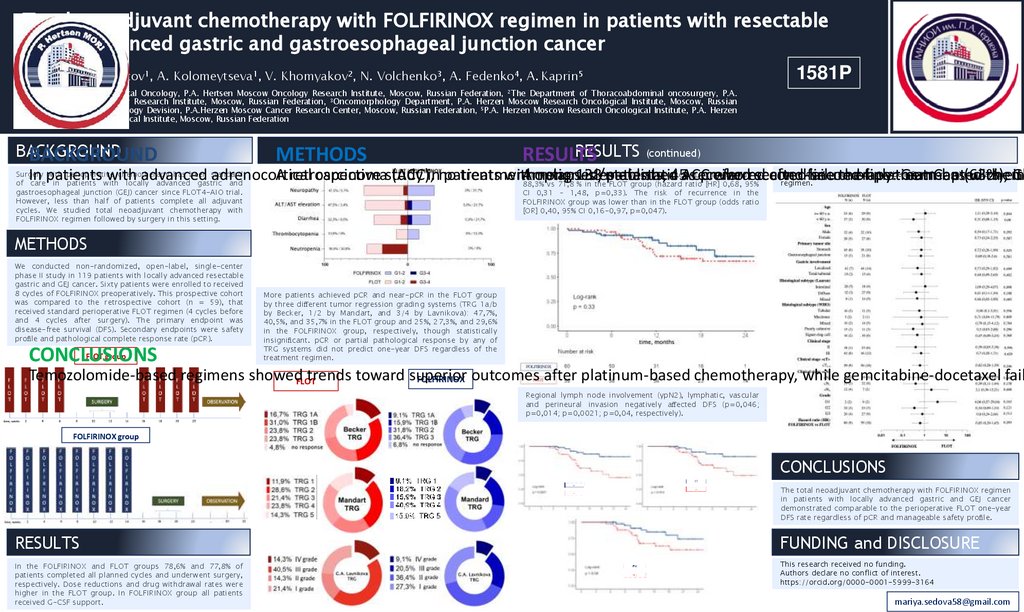
Total neoadjuvant chemotherapy with FOLFIRINOX regimen in patients with resectablelocally advanced gastric and gastroesophageal junction cancer
M. Sedova1, M. Batov1, A. Kolomeytseva1, V. Khomyakov2, N. Volchenko3, A. Fedenko4, A. Kaprin5
1581P
1The
Department of Medical Oncology, P.A. Hertsen Moscow Oncology Research Institute, Moscow, Russian Federation, 2The Department of Thoracoabdominal oncosurgery, P.A.
Hertsen Moscow Oncology Research Institute, Moscow, Russian Federation, 3Oncomorphology Department, P.A. Herzen Moscow Research Oncological Institute, Moscow, Russian
Federation, 4Medical Oncology Devision, P.A.Herzen Moscow Cancer Research Center, Moscow, Russian Federation, 5P.A. Herzen Moscow Research Oncological Institute, P.A. Herzen
Moscow Research Oncological Institute, Moscow, Russian Federation
BACKGROUND
RESULTS (continued)
BACKGROUND
METHODS
RESULTS
There wasn’t
a subgroup
that benefited
from either
treatment
Surgery
with perioperative
chemotherapy
has been standard
One-year
DFS was
higher in 45
theas
FOLFIRINOX
group
In patients
with
advanced
adrenocortical
A retrospective
carcinomastudy
(ACC),inno
patients
treatment
with
Among
option
relapsed/metastatic
138
isnumerically
established
patients,
ACC
received
preferred
who
received
second-line
after
failure
second-line
therapy:
of platinum-based
treatment
GemCap
(63%),
with
chemo
eith
Ge
regimen.
of care in patients with locally advanced gastric and
88,3% vs 71,8 % in the FLOT group (hazard ratio [HR] 0,68, 95%
gastroesophageal junction (GEJ) cancer since FLOT4-AIO trial.
However, less than half of patients complete all adjuvant
cycles. We studied total neoadjuvant chemotherapy with
FOLFIRINOX regimen followed by surgery in this setting.
CI 0,31 – 1,48, p=0,33). The risk of recurrence in the
FOLFIRINOX group was lower than in the FLOT group (odds ratio
[OR] 0,40, 95% CI 0,16-0,97, p=0,047).
METHODS
We conducted non-randomized, open-label, single-center
phase II study in 119 patients with locally advanced resectable
gastric and GEJ cancer. Sixty patients were enrolled to received
8 cycles of FOLFIRINOX preoperatively. This prospective cohort
was compared to the retrospective cohort (n = 59), that
received standard perioperative FLOT regimen (4 cycles before
and 4 cycles after surgery). The primary endpoint was
disease-free survival (DFS). Secondary endpoints were safety
pro le and pathological complete response rate (pCR).
FLOT group
CONCLUSIONS
More patients achieved pCR and near-pCR in the FLOT group
by three di erent tumor regression grading systems (TRG 1a/b
by Becker, 1/2 by Mandart, and 3/4 by Lavnikova): 47,7%,
40,5%, and 35,7% in the FLOT group and 25%, 27,3%, and 29,6%
in the FOLFIRINOX group, respectively, though statistically
insigni cant. pCR or partial pathological response by any of
TRG systems did not predict one-year DFS regardless of the
treatment regimen.
Temozolomide-based regimens showedFLOT
trends toward superior
FOLFIRINOX outcomes after platinum-based chemotherapy, while gemcitabine-docetaxel faile
Regional lymph node involvement (ypN2), lymphatic, vascular
and perineural invasion negatively a ected DFS (p=0,046;
p=0,014; p=0,0021; p=0,04, respectively).
FOLFIRINOX group
CONCLUSIONS
The total neoadjuvant chemotherapy with FOLFIRINOX regimen
in patients with locally advanced gastric and GEJ cancer
demonstrated comparable to the perioperative FLOT one-year
DFS rate regardless of pCR and manageable safety pro le.
RESULTS
FUNDING and DISCLOSURE
In the FOLFIRINOX and FLOT groups 78,6% and 77,8% of
patients completed all planned cycles and underwent surgery,
respectively. Dose reductions and drug withdrawal rates were
higher in the FLOT group. In FOLFIRINOX group all patients
received G-CSF support.
This research received no funding.
Authors declare no conflict of interest.
https://orcid.org/0000-0001-5999-3164
mariya.sedova58@gmail.com
 Медицина
Медицина