Похожие презентации:
Pancreatic Cancer
1. Pancreatic Cancer- 2017
Valeriya SemenistyDepartment of Oncology,
Rambam Medical Center,
Haifa, Israel
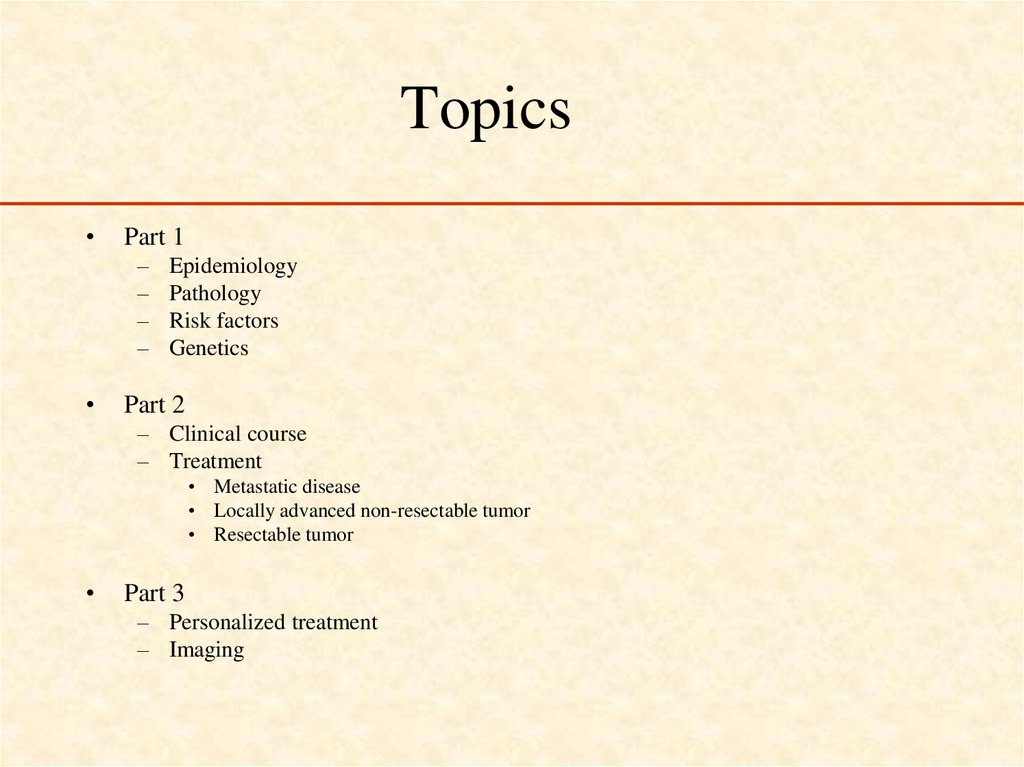
2. Topics
Part 1
–
–
–
–
Epidemiology
Pathology
Risk factors
Genetics
Part 2
– Clinical course
– Treatment
• Metastatic disease
• Locally advanced non-resectable tumor
• Resectable tumor
Part 3
– Personalized treatment
– Imaging
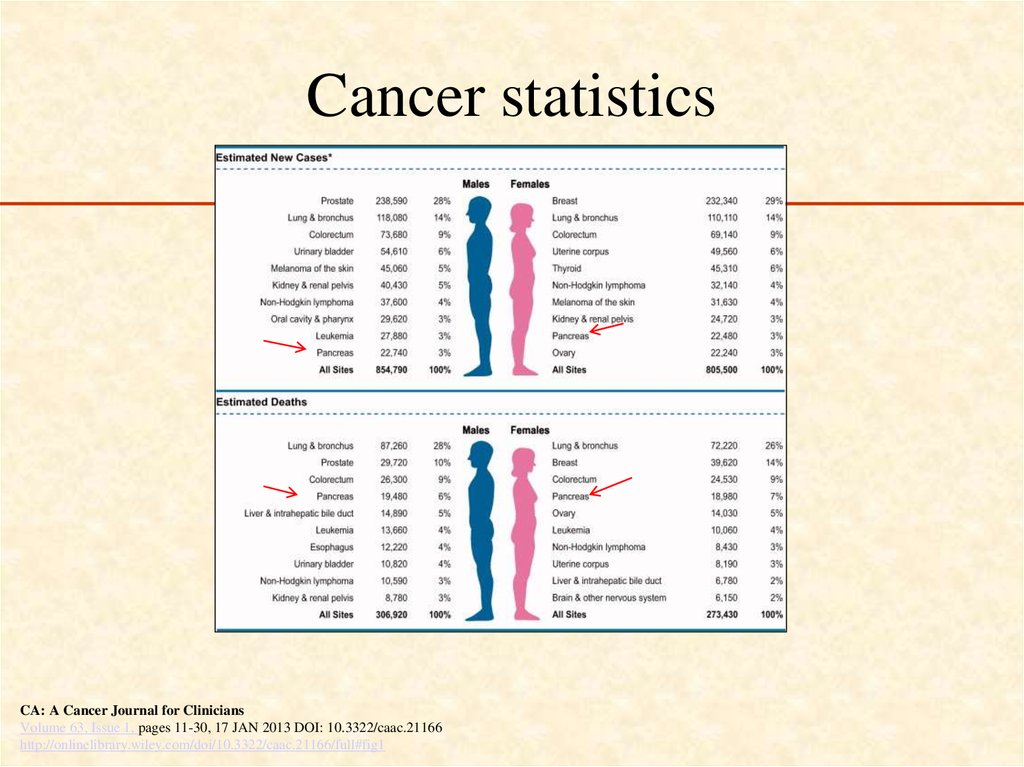
3. Cancer statistics
CA: A Cancer Journal for CliniciansVolume 63, Issue 1, pages 11-30, 17 JAN 2013 DOI: 10.3322/caac.21166
http://onlinelibrary.wiley.com/doi/10.3322/caac.21166/full#fig1
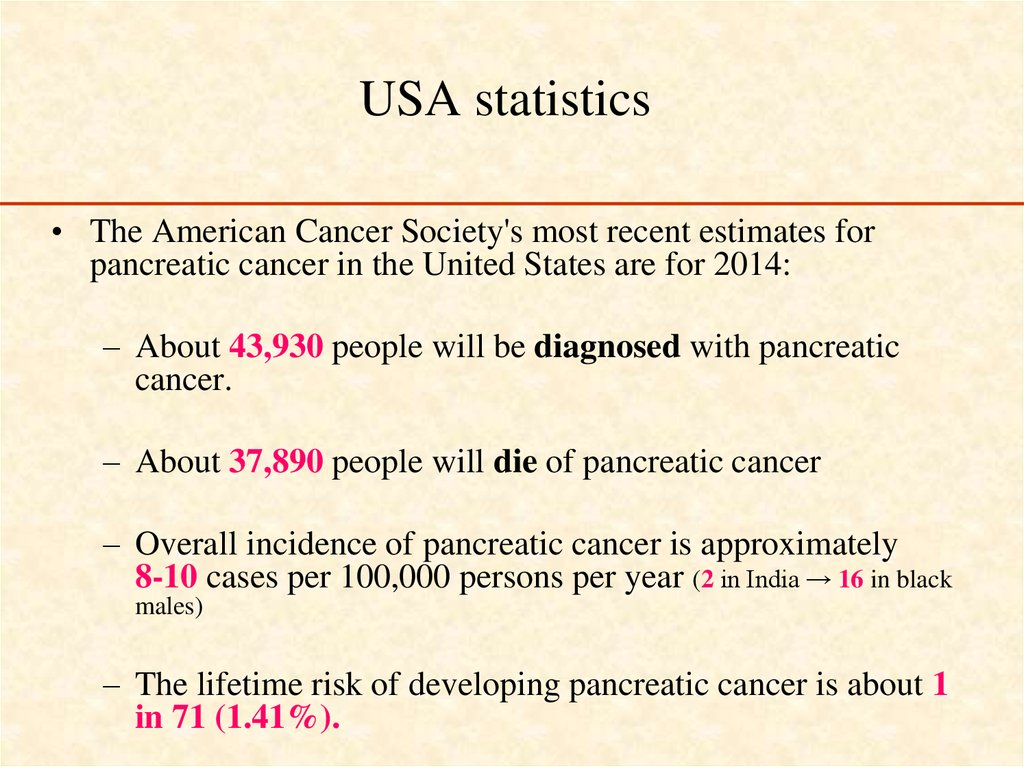
4. USA statistics
• The American Cancer Society's most recent estimates forpancreatic cancer in the United States are for 2014:
– About 43,930 people will be diagnosed with pancreatic
cancer.
– About 37,890 people will die of pancreatic cancer
– Overall incidence of pancreatic cancer is approximately
8-10 cases per 100,000 persons per year (2 in India → 16 in black
males)
– The lifetime risk of developing pancreatic cancer is about 1
in 71 (1.41%).
5.
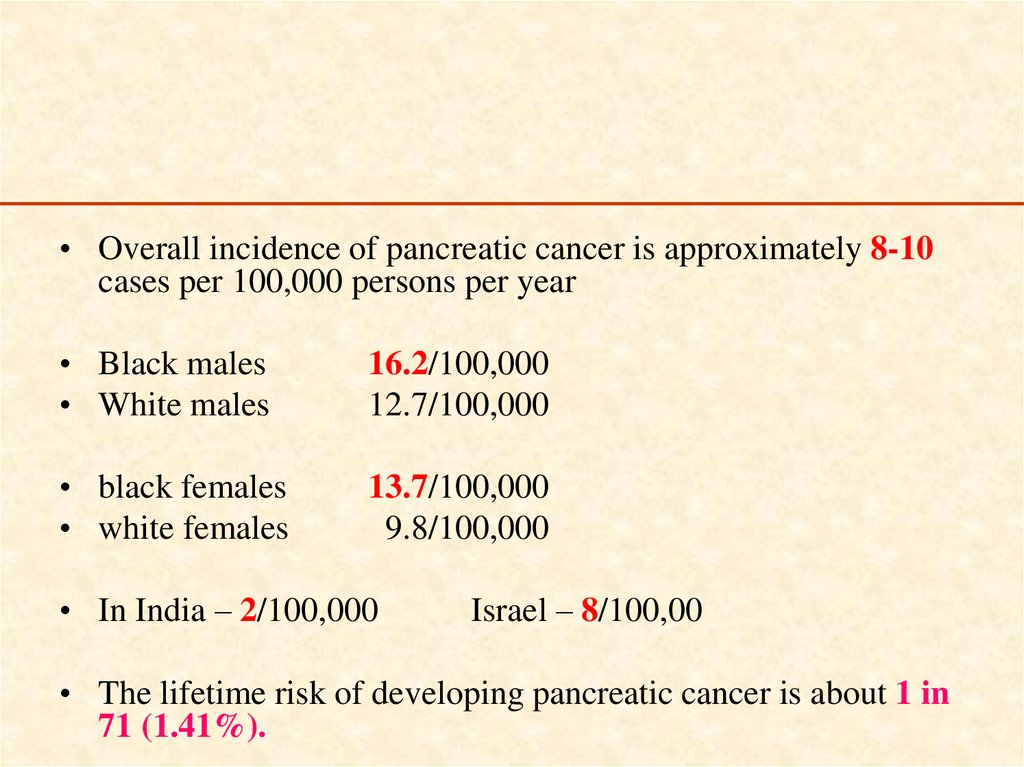
• Overall incidence of pancreatic cancer is approximately 8-10cases per 100,000 persons per year
• Black males
• White males
16.2/100,000
12.7/100,000
• black females
• white females
13.7/100,000
9.8/100,000
• In India – 2/100,000
Israel – 8/100,00
• The lifetime risk of developing pancreatic cancer is about 1 in
71 (1.41%).
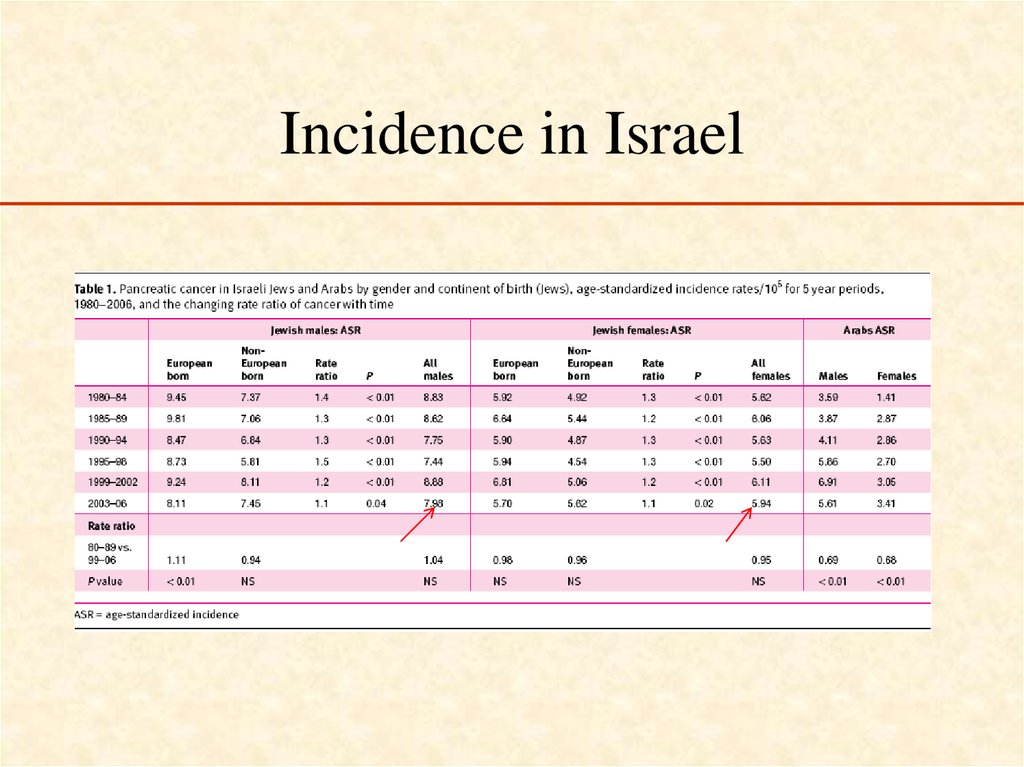
6. Incidence in Israel
7.
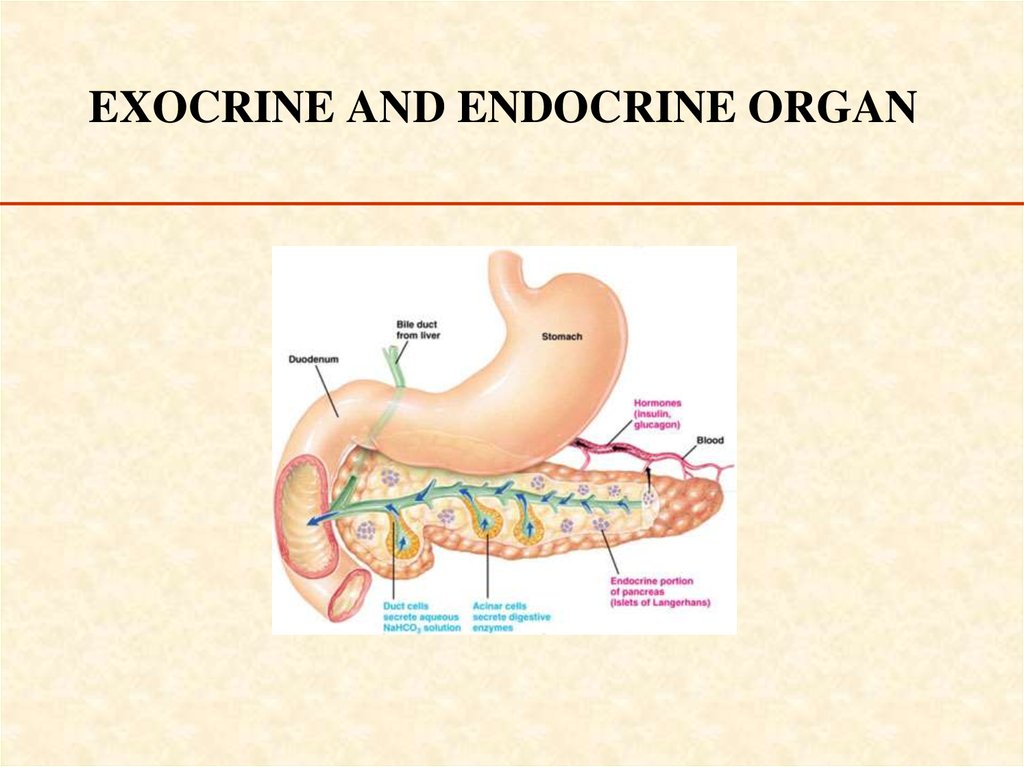
8. EXOCRINE AND ENDOCRINE ORGAN
9. Pathology
• Exocrine tumors– Solid
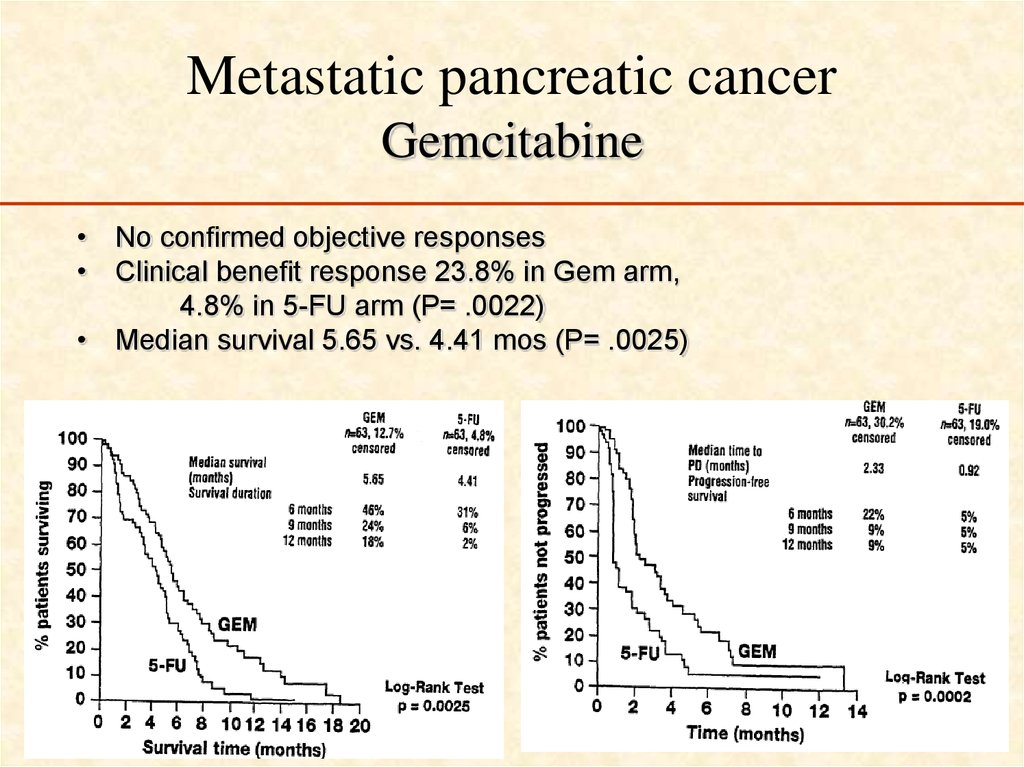
– Cystic
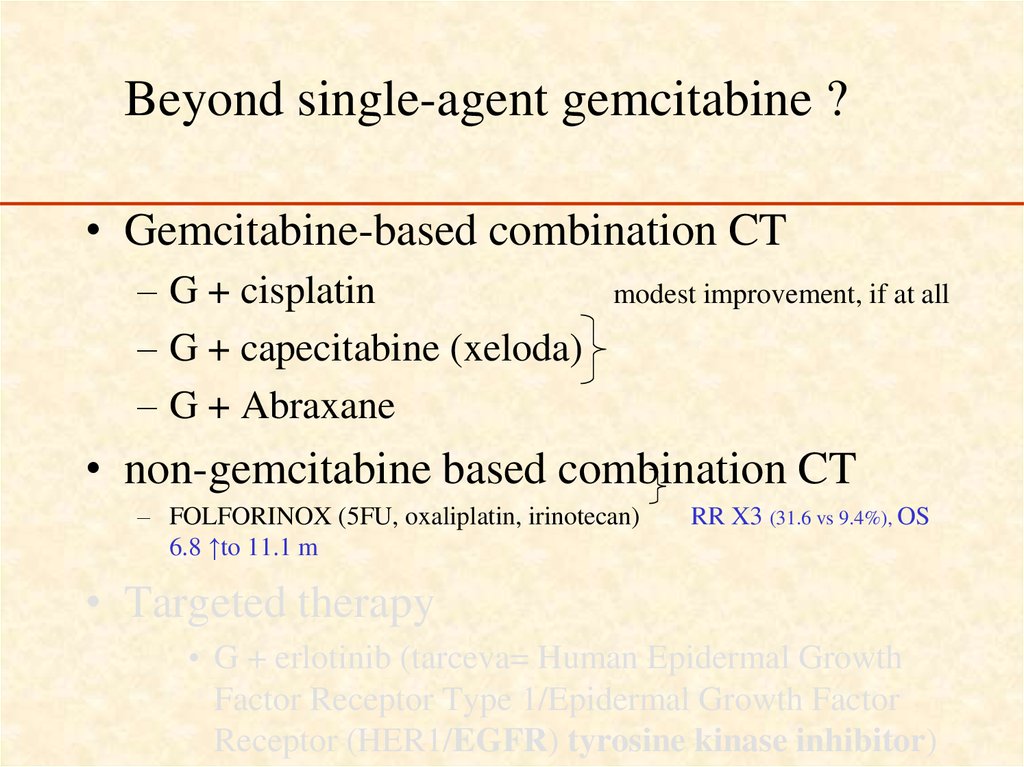
• Endocrine tumors
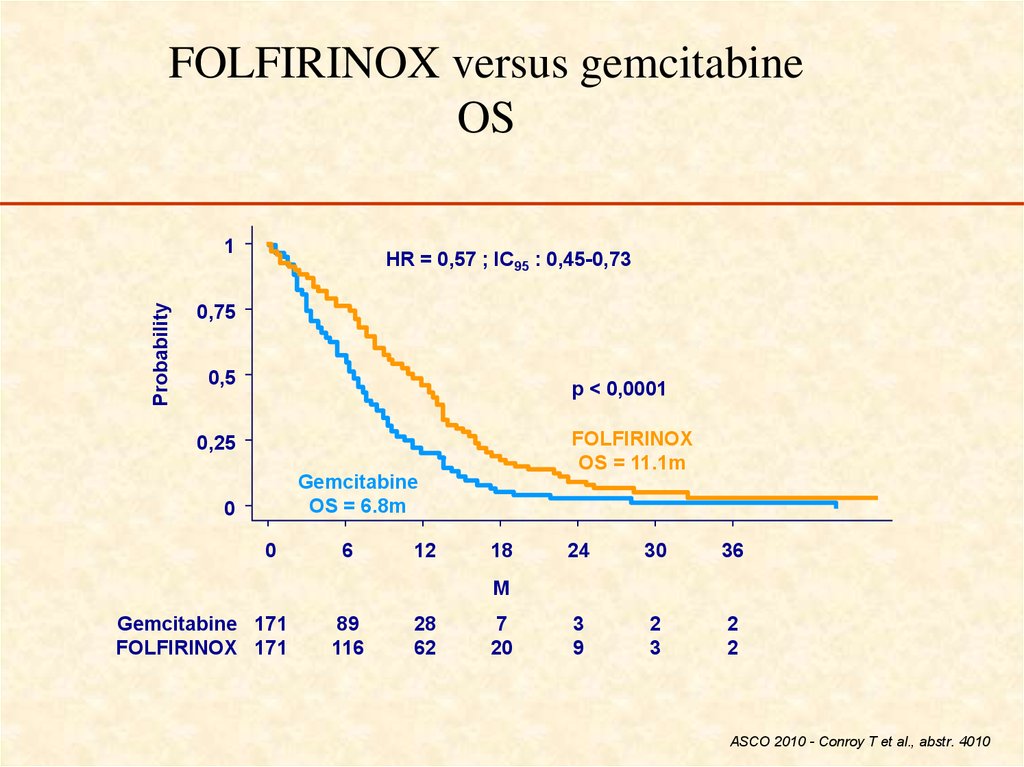
10. Solid Epithelial Tumors
• Adenocarcinomas: 75-80%, white yellow,poorly defined, often obstruct bile duct or
main pancreatic duct.
• Often associated with a desmoplastic
reaction that causes fibrosis and chronic
pancreatitis.
11.
• Infiltrate into vascular, lymphatic, perineural spaces.• At resection, most mets to lymph nodes.
• Mets to liver (80%), peritoneum (60%), lungs and pleura
(50-70%), adrenal (25%). Direct invasion of adjacent
organs as well.
• Others include adenosquamous, acinar cell (1%, better
prognosis), giant cell (5%, poorer prognosis),
pancreatoblastoma (children 1-15 years, more favorable).
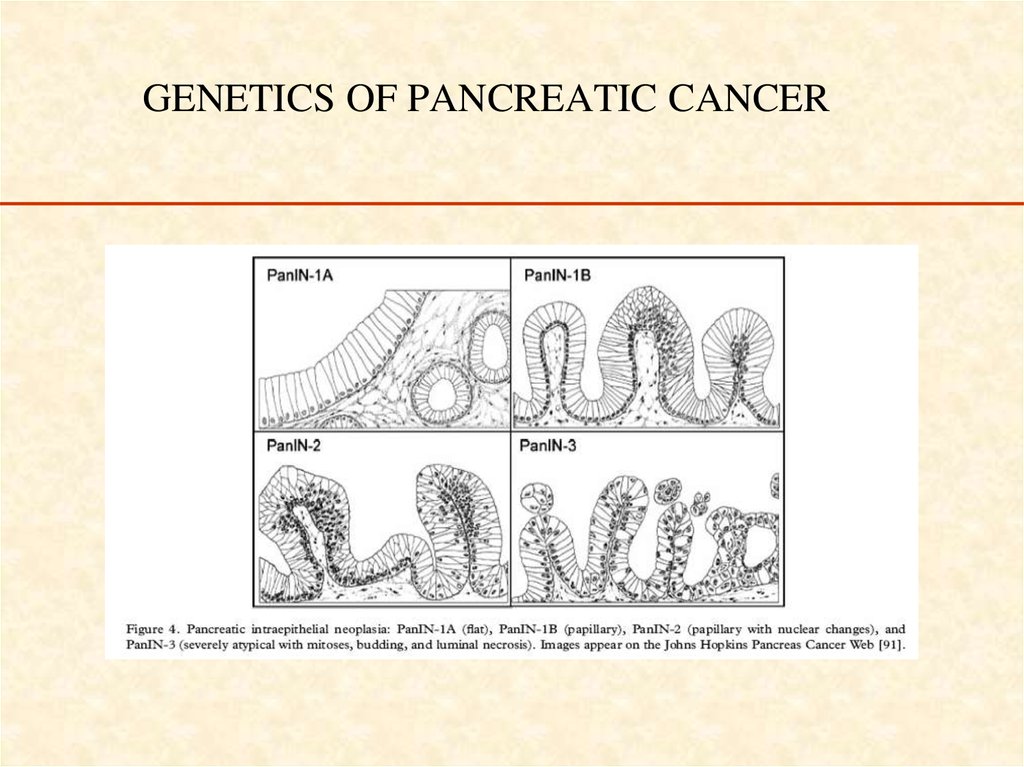
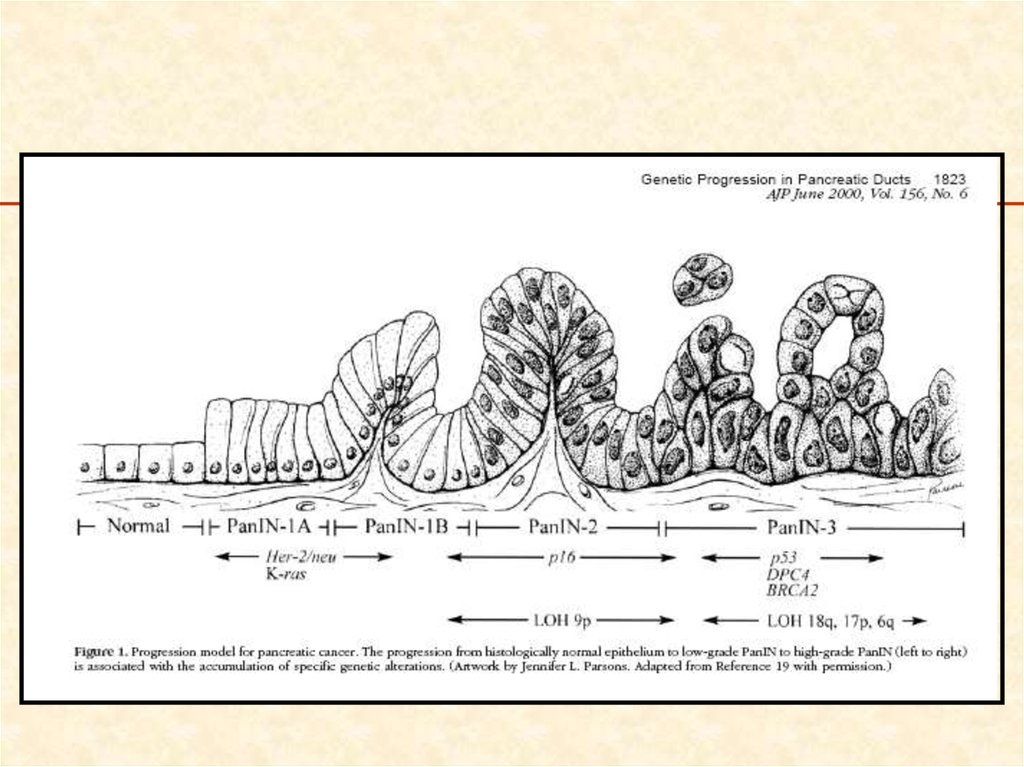
12. GENETICS OF PANCREATIC CANCER
13.
14.
• Nature 467, 1114-1117 (28 October 2010)• Distant metastasis occurs late during
the genetic evolution of pancreatic
cancer
Shinichi Yachida1et al7,
Department of Pathology, The Sol Goldman Pancreatic Cancer Research Center, Johns
Hopkins Medical Institutions, Baltimore, Maryland 21231, USA
15. A quantitative analysis of the timing of the genetic evolution of pancreatic cancer
–At least a
decade between
the occurrence
of the initiating
mutation and the
birth of the
parental, nonmetastatic
founder cell.
–
At least five
more years are
required for the
acquisition of
metastatic
ability
–
Patients die an
average of two
years thereafter.
There is a broad time window of opportunity for early detection to
prevent deaths from metastatic disease.
16.
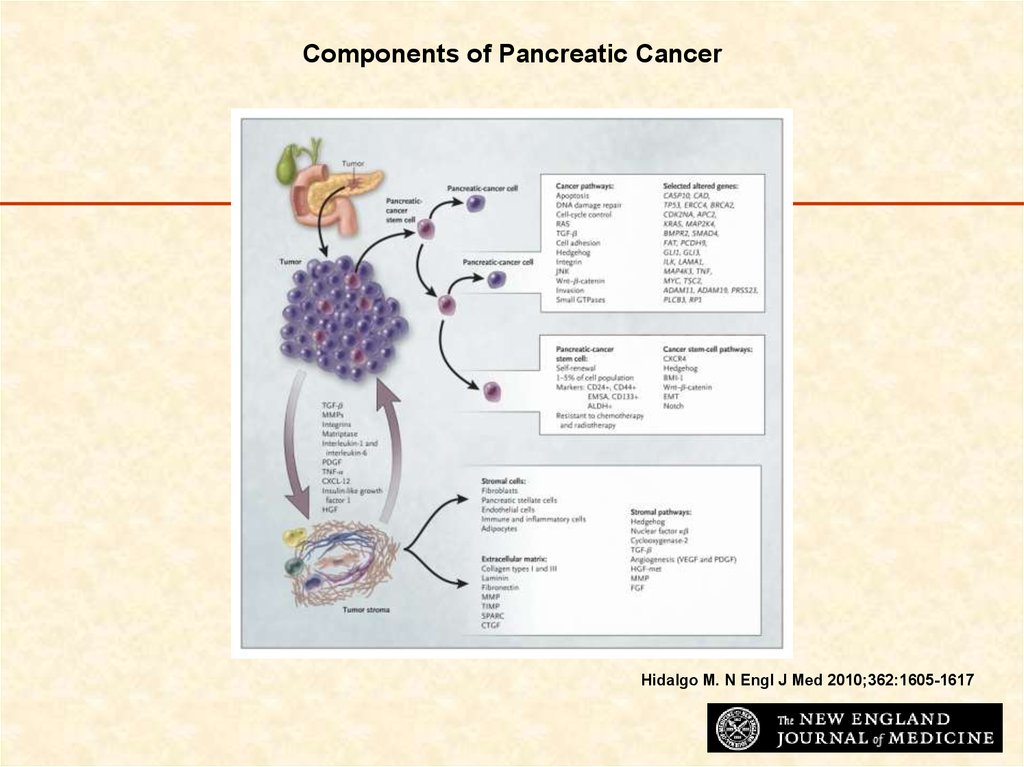
Components of Pancreatic CancerHidalgo M. N Engl J Med 2010;362:1605-1617
17. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
18. Age
• Age is the most significant risk factor for pancreaticcancer .
• In the absence of predisposing conditions pancreatic cancer
is unusual in persons younger than 45 years. Only 10% of
patients are diagnosed when younger than 50 years of age.
• After age 50 years, the frequency of pancreatic cancer
increases linearly.
• The median age at diagnosis is 69 years in whites and 65
years in blacks
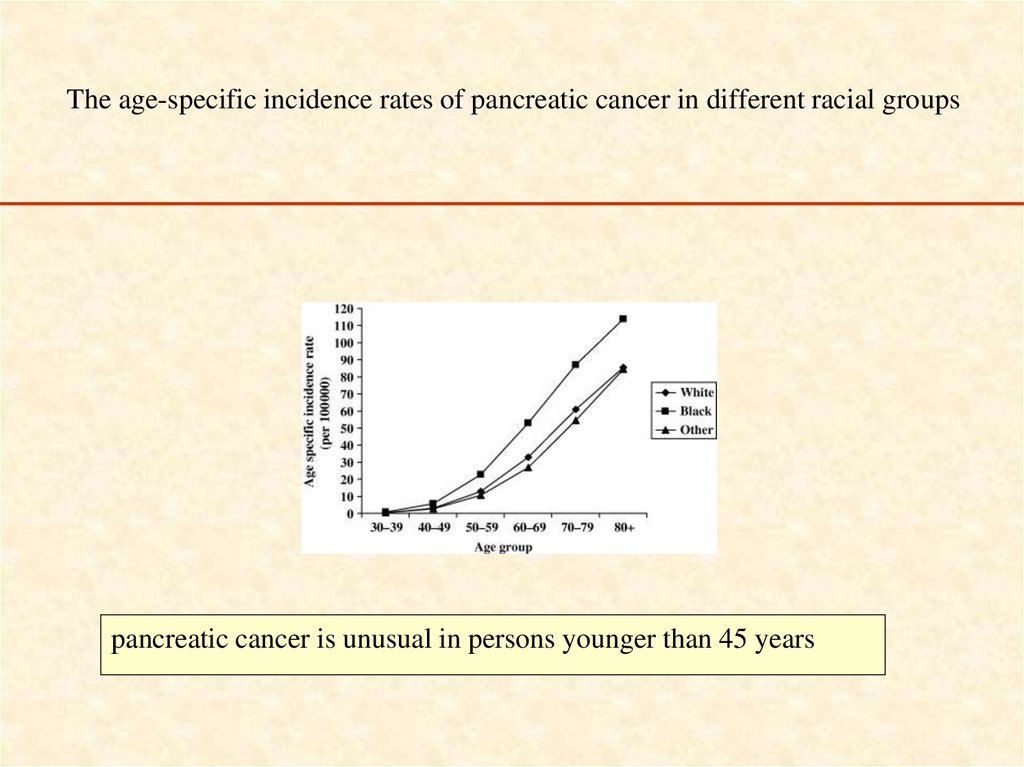
19. The age-specific incidence rates of pancreatic cancer in different racial groups
pancreatic cancer is unusual in persons younger than 45 years20. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
21. Smoking
• Associated with 20-25% of PC cases• People who smoke have 2.7-3.7 -fold increased risk for
pancreatic cancer.
• Current smokers with over a 40 pack-year history of smoking
may have up to a 5-fold increase risk of the disease.
• It takes 5-10 years of discontinued smoking to reduce the
increased risk of smoking to approximately that of
nonsmokers.
22. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
23. Obesity & nutrition
Obesity & nutrition• High caloric intake & obesity are risk
factors for PC
• Red meat consumption, especially
processed, is associated with a higher risk
of pancreatic cancer
24. Anthropometric Measures, Body Mass Index, and Pancreatic Cancer A Pooled Analysis From the Pancreatic Cancer Cohort Consortium
(PanScan)Arch Intern Med. 2010;170(9):791-802.
• A positive association between increasing BMI
and risk of pancreatic cancer was observed
(adjusted OR for the highest vs lowest BMI
quartile, 1.33; 95% CI, 1.12-1.58; Ptrend < .001).
• Increased waist to hip ratio was associated with
increased risk of pancreatic cancer in women
(adjusted OR for the highest vs lowest quartile,
1.87; 95% CI, 1.31-2.69; Ptrend = .003) but less so in men.
25. Obesity & nutrition
Obesity & nutrition• High caloric intake & obesity are risk
factors for PC
• Red meat consumption, especially
processed, is associated with a higher risk
of pancreatic cancer
26.
Alcohol Intake and Pancreatic Cancer Risk: A Pooled Analysisof Fourteen Cohort Studies.
Cancer Epidemiol Biomarkers Prev 2009;18(3):765–76
“…a modest increase in risk of pancreatic cancer with consumption of 30 or more grams of
alcohol per day.”
Soft Drink and Juice Consumption and Risk of Pancreatic
Cancer: The Singapore Chinese Health Study
Cancer Epidemiol Biomarkers Prev; 19(2); 447–55, 2010
“Individuals consuming ≥2 soft drinks/wk experienced a statistically significant increased risk of pancreatic
cancer (hazard ratio, 1.87; 95% confidence interval, 1.10-3.15) compared with individuals who did not
consume soft drinks after adjustment for potential confounders. There was no statistically significant
association between juice consumption and risk of pancreatic cancer”
27. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
28.
• 14-fold increased risk of PC in chronicpancreatitis patients
• Hereditary pancreatitiis → 40-55% lifetime
risk of PC
29. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
30.
• Increased risk of PC in type II diabetes (RR2.1-2.6)
– Etiologic factor ?
– Manifestation of PC ?
31. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
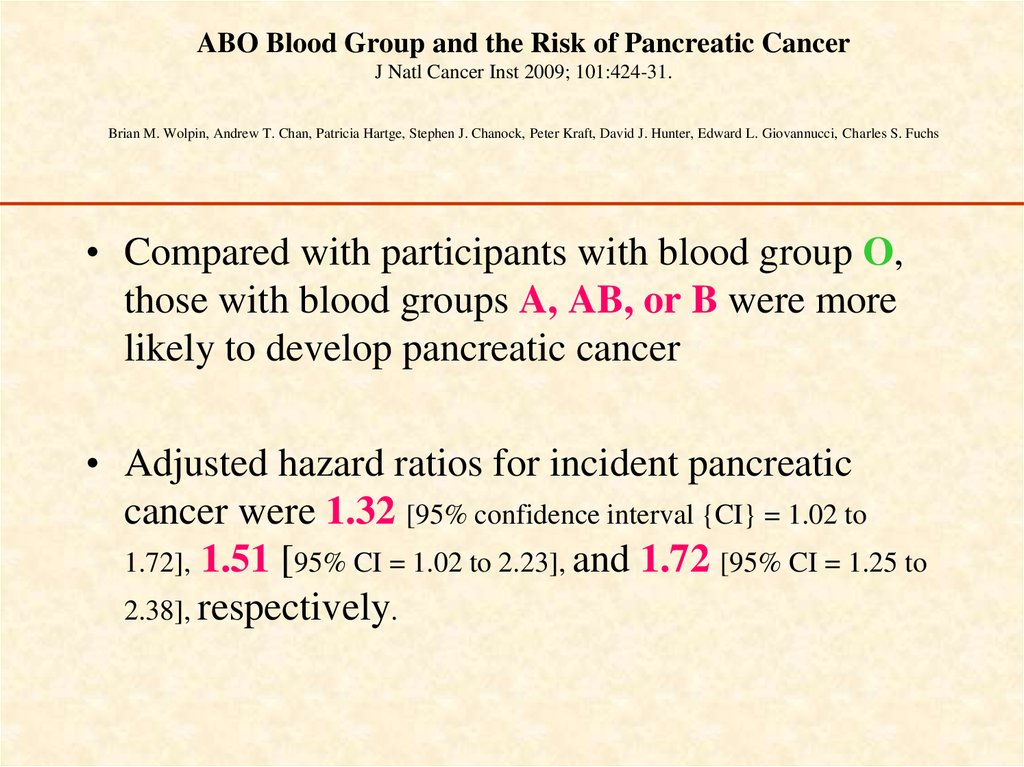
32. ABO Blood Group and the Risk of Pancreatic Cancer J Natl Cancer Inst 2009; 101:424-31. Brian M. Wolpin, Andrew T. Chan,
Patricia Hartge, Stephen J. Chanock, Peter Kraft, David J. Hunter, Edward L. Giovannucci, Charles S. Fuchs• Compared with participants with blood group O,
those with blood groups A, AB, or B were more
likely to develop pancreatic cancer
• Adjusted hazard ratios for incident pancreatic
cancer were 1.32 [95% confidence interval {CI} = 1.02 to
1.72], 1.51 [95% CI = 1.02 to 2.23], and 1.72 [95% CI = 1.25 to
2.38], respectively.
33. RISK FACTORS
Advanced age
Smoking
diet
Chronic pancreatitis
• Diabetes mellitus
• Blood type A, B, AB
• Family history
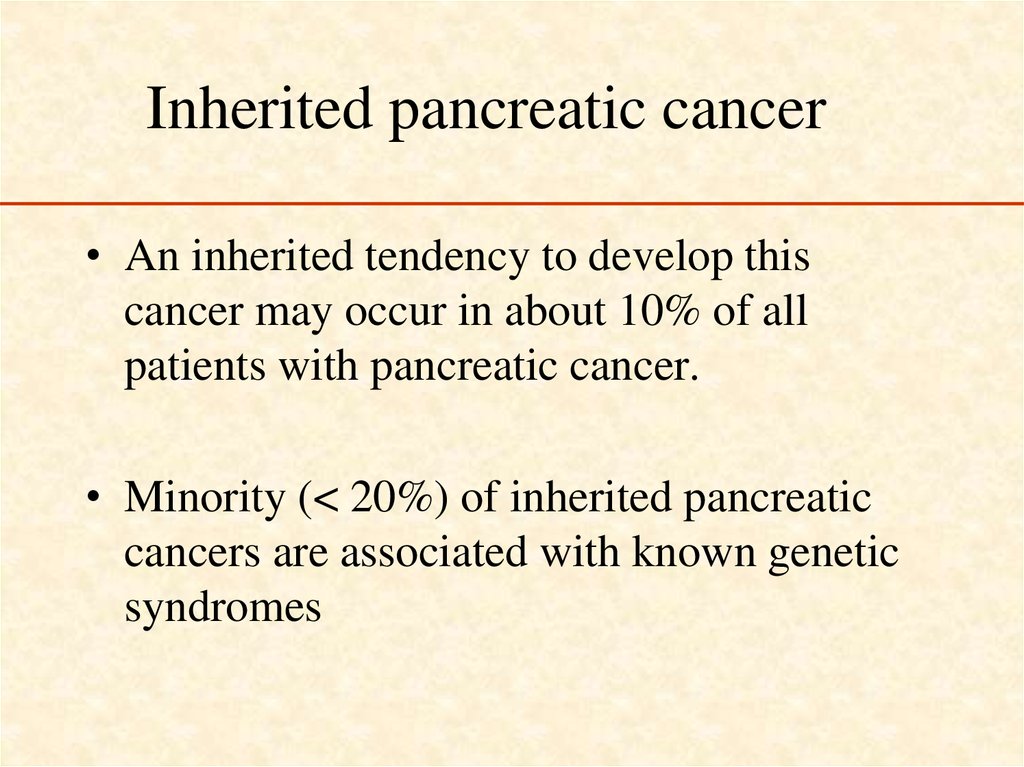
34. Inherited pancreatic cancer
• An inherited tendency to develop thiscancer may occur in about 10% of all
patients with pancreatic cancer.
• Minority (< 20%) of inherited pancreatic
cancers are associated with known genetic
syndromes
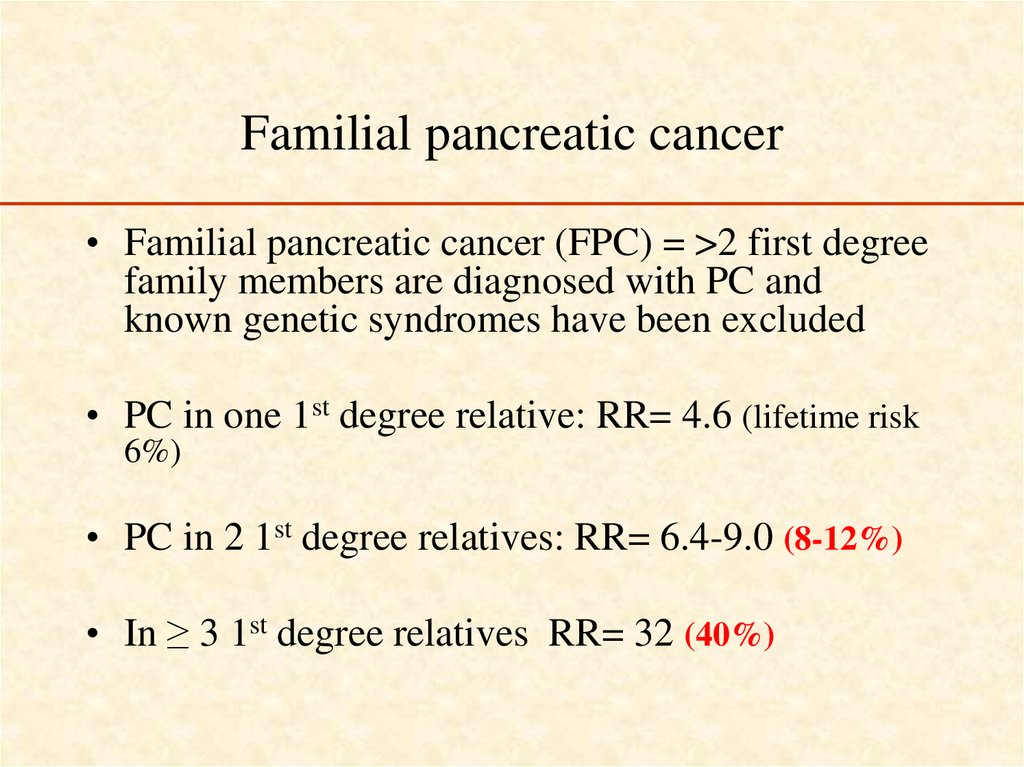
35. Familial pancreatic cancer
• Familial pancreatic cancer (FPC) = >2 first degreefamily members are diagnosed with PC and
known genetic syndromes have been excluded
• PC in one 1st degree relative: RR= 4.6 (lifetime risk
6%)
• PC in 2 1st degree relatives: RR= 6.4-9.0 (8-12%)
• In ≥ 3 1st degree relatives RR= 32 (40%)
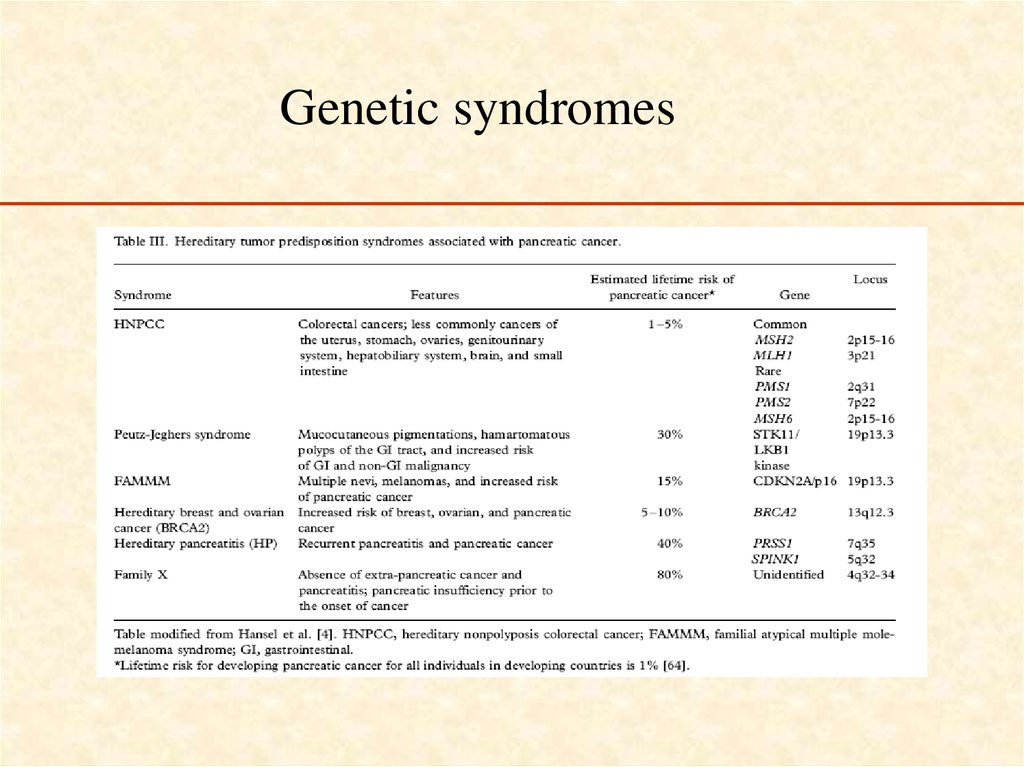
36. Genetic syndromes
37.
• Both BRCA1 (breast cancer gene1) andBRCA2 are tumor suppressor genes and are
involved in DNA repair of double-strand
breaks.
• Related mainly to breast and ovarian
cancers.
38. Pancreatic cancer in BRCA1/2
• Risk of PC in BRCA1 carriers is low (RR ~2.3)• BRCA1: Cumulative age-adjusted lifetime risk of pancreatic cancer –
3.6%
• Risk of PC in BRCA2 carriers is higher (RR ~ 6)
• BRCA2: cumulative risk – 5-10%
• Estimated population risk of PC: 1-1.3%
39. BRCA1/2 in pancreatic cancer
• BRCA2 in sporadic PC – 0.8%• BRCA germline mutations in Jewish
patients with pancreatic adenocarcinoma –
5.5%
(Ferrone et al, JCO 2009)
• In association of family history – up to 17%
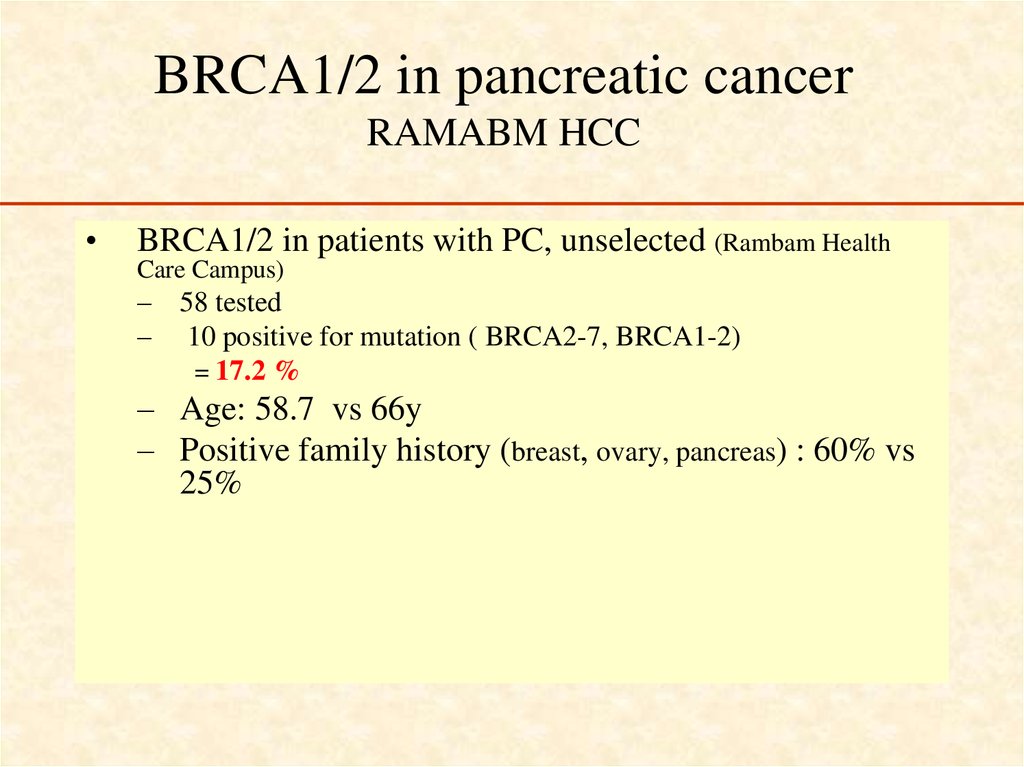
40. BRCA1/2 in pancreatic cancer RAMABM HCC
BRCA1/2 in patients with PC, unselected (Rambam Health
Care Campus)
– 58 tested
– 10 positive for mutation ( BRCA2-7, BRCA1-2)
= 17.2 %
– Age: 58.7 vs 66y
– Positive family history (breast, ovary, pancreas) : 60% vs
25%
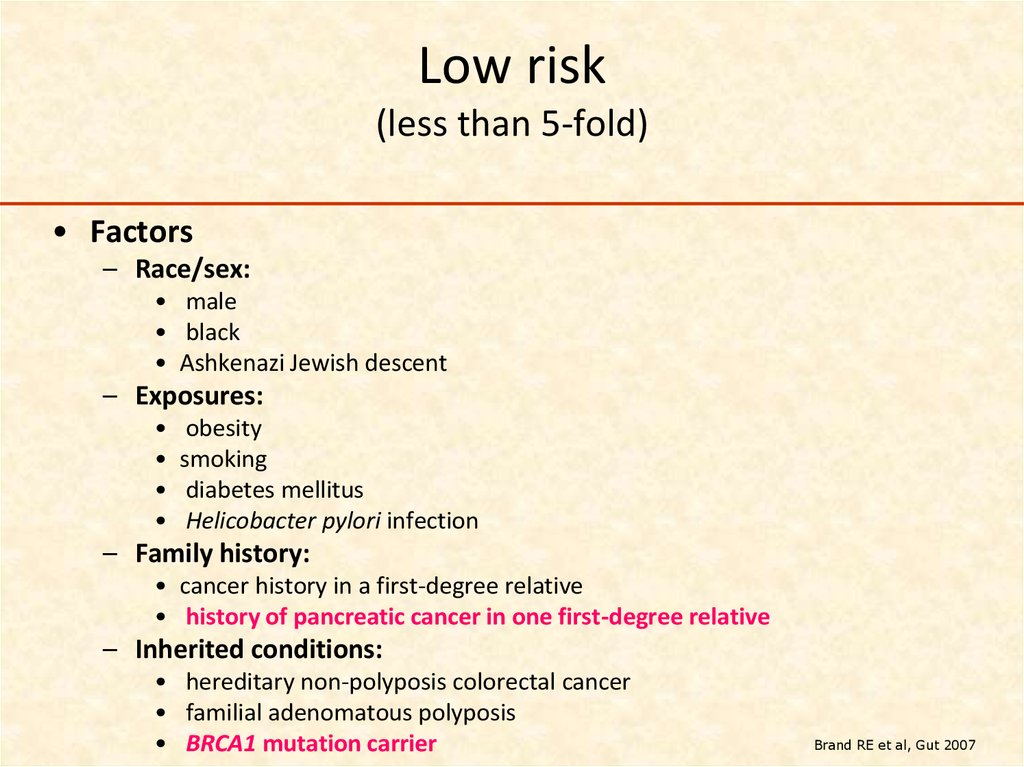
41. Low risk (less than 5-fold)
• Factors– Race/sex:
• male
• black
• Ashkenazi Jewish descent
– Exposures:
obesity
smoking
diabetes mellitus
Helicobacter pylori infection
– Family history:
• cancer history in a first-degree relative
• history of pancreatic cancer in one first-degree relative
– Inherited conditions:
• hereditary non-polyposis colorectal cancer
• familial adenomatous polyposis
• BRCA1 mutation carrier
Brand RE et al, Gut 2007
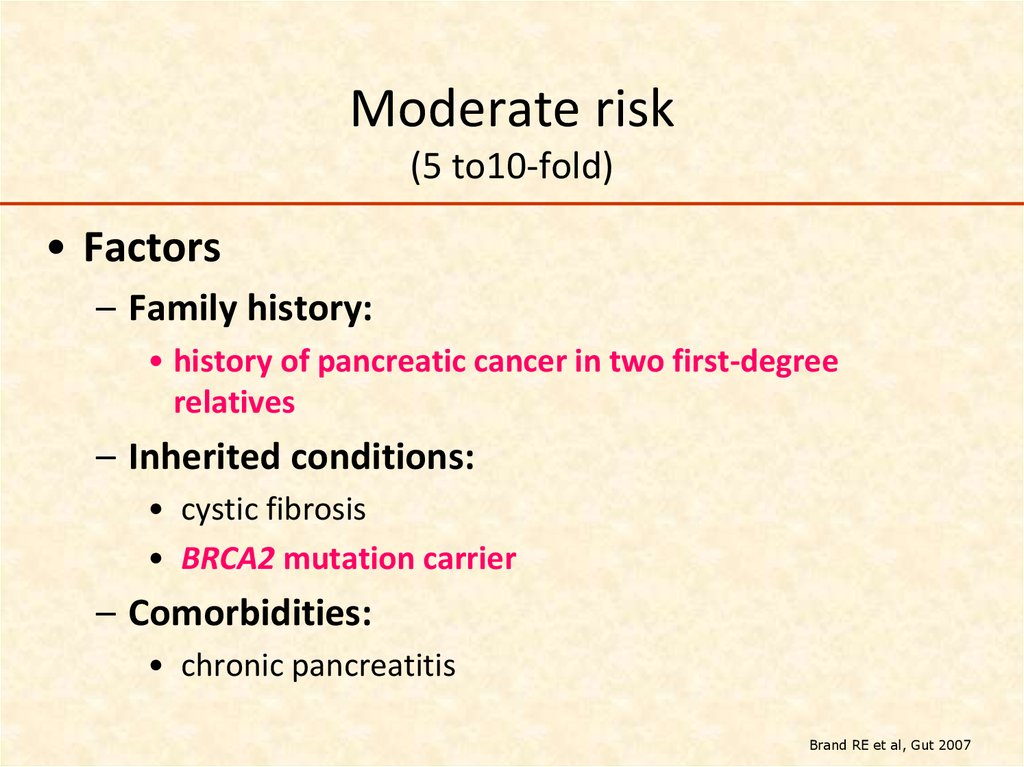
42. Moderate risk (5 to10-fold)
• Factors– Family history:
• history of pancreatic cancer in two first-degree
relatives
– Inherited conditions:
• cystic fibrosis
• BRCA2 mutation carrier
– Comorbidities:
• chronic pancreatitis
Brand RE et al, Gut 2007
43. High risk (greater than 10-fold)
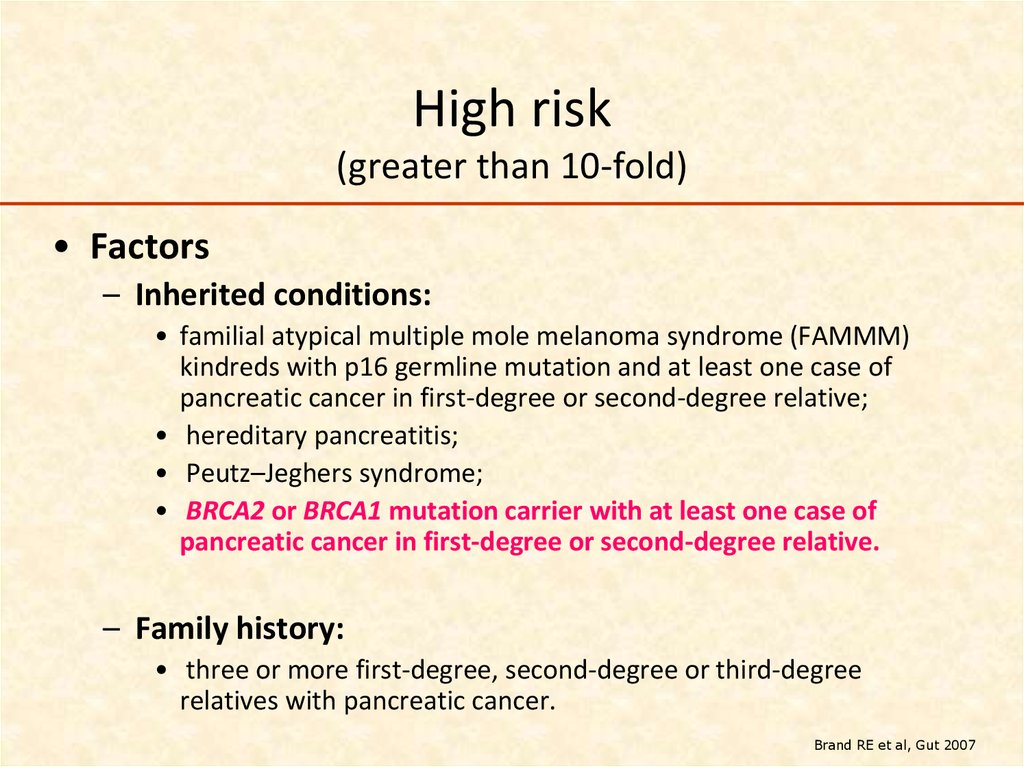
• Factors– Inherited conditions:
• familial atypical multiple mole melanoma syndrome (FAMMM)
kindreds with p16 germline mutation and at least one case of
pancreatic cancer in first-degree or second-degree relative;
• hereditary pancreatitis;
• Peutz–Jeghers syndrome;
• BRCA2 or BRCA1 mutation carrier with at least one case of
pancreatic cancer in first-degree or second-degree relative.
– Family history:
• three or more first-degree, second-degree or third-degree
relatives with pancreatic cancer.
Brand RE et al, Gut 2007
44. BRCA1/2 in pancreatic cancer RAMABM HCC
• For the 1st degree relative – High prevalence (of BRCA) + high risk (for PC+breast) =Genetic counseling! (early detection?- EUS, markers, fecal
DNA methylation analysis, metabolomics… )
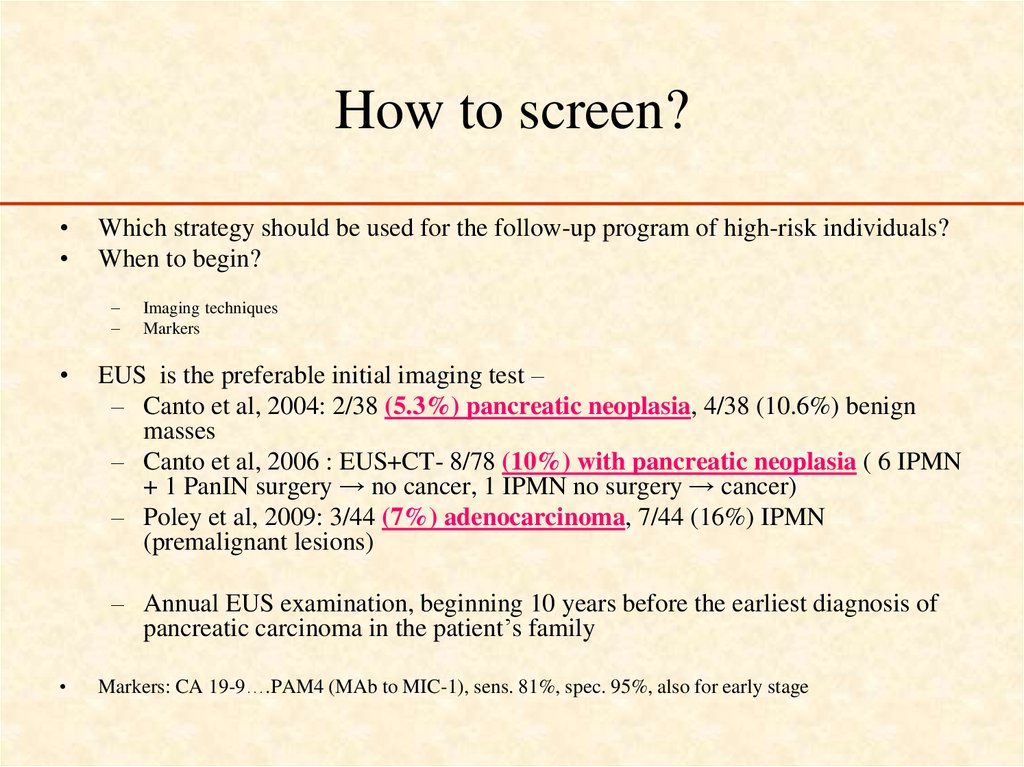
45. How to screen?
Which strategy should be used for the follow-up program of high-risk individuals?
When to begin?
–
–
Imaging techniques
Markers
EUS is the preferable initial imaging test –
– Canto et al, 2004: 2/38 (5.3%) pancreatic neoplasia, 4/38 (10.6%) benign
masses
– Canto et al, 2006 : EUS+CT- 8/78 (10%) with pancreatic neoplasia ( 6 IPMN
+ 1 PanIN surgery → no cancer, 1 IPMN no surgery → cancer)
– Poley et al, 2009: 3/44 (7%) adenocarcinoma, 7/44 (16%) IPMN
(premalignant lesions)
– Annual EUS examination, beginning 10 years before the earliest diagnosis of
pancreatic carcinoma in the patient’s family
Markers: CA 19-9….PAM4 (MAb to MIC-1), sens. 81%, spec. 95%, also for early stage
46.
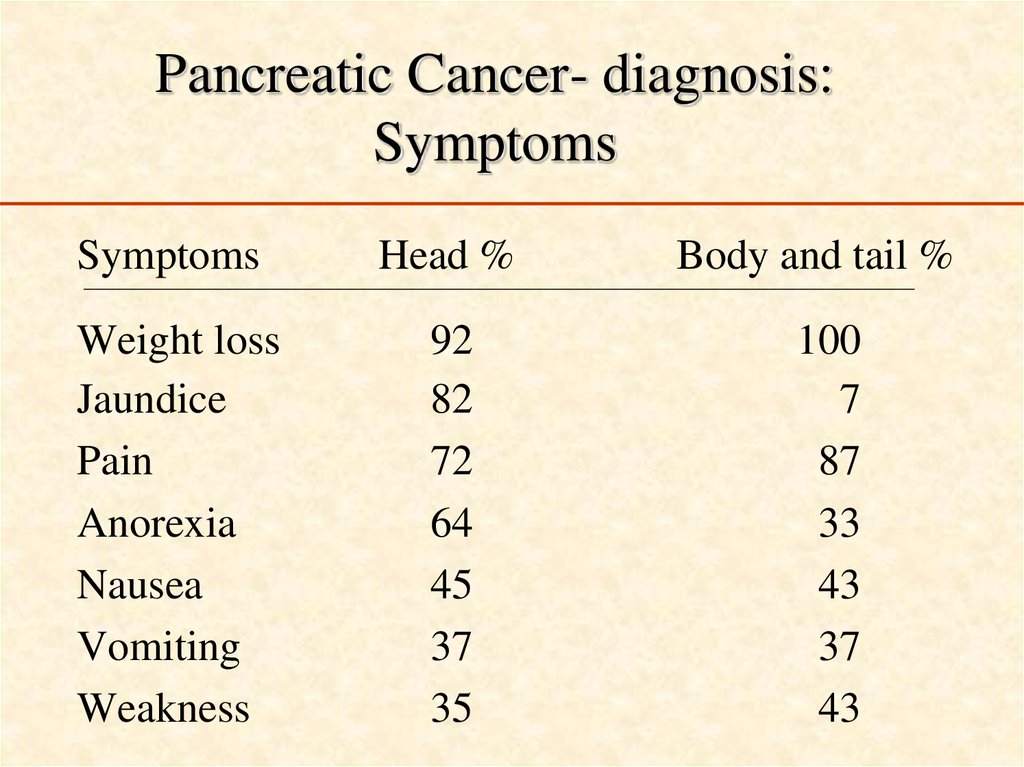
Clinical course and treatment47. Pancreatic Cancer- diagnosis: Symptoms
SymptomsHead %
Weight loss
Jaundice
Pain
Anorexia
Nausea
Vomiting
Weakness
92
82
72
64
45
37
35
Body and tail %
100
7
87
33
43
37
43
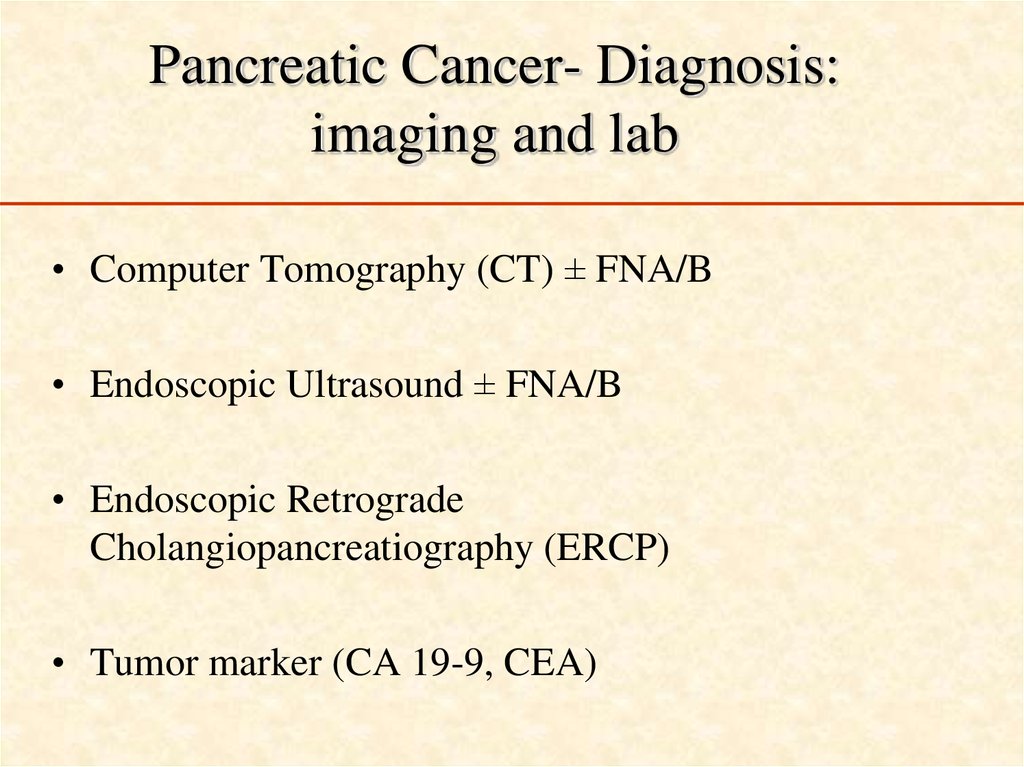
48. Pancreatic Cancer- Diagnosis: imaging and lab
• Computer Tomography (CT) ± FNA/B• Endoscopic Ultrasound ± FNA/B
• Endoscopic Retrograde
Cholangiopancreatiography (ERCP)
• Tumor marker (CA 19-9, CEA)
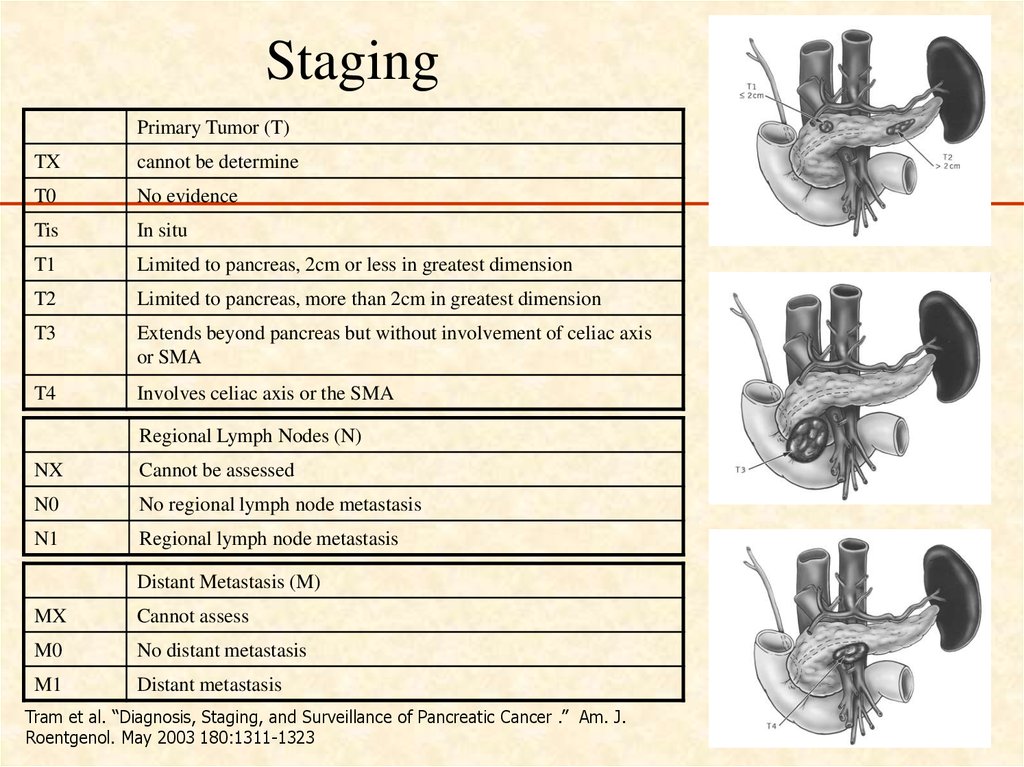
49. Staging
Primary Tumor (T)TX
cannot be determine
T0
No evidence
Tis
In situ
T1
Limited to pancreas, 2cm or less in greatest dimension
T2
Limited to pancreas, more than 2cm in greatest dimension
T3
Extends beyond pancreas but without involvement of celiac axis
or SMA
T4
Involves celiac axis or the SMA
Regional Lymph Nodes (N)
NX
Cannot be assessed
N0
No regional lymph node metastasis
N1
Regional lymph node metastasis
Distant Metastasis (M)
MX
Cannot assess
M0
No distant metastasis
M1
Distant metastasis
Tram et al. “Diagnosis, Staging, and Surveillance of Pancreatic Cancer .” Am. J.
Roentgenol. May 2003 180:1311-1323
50.
51.
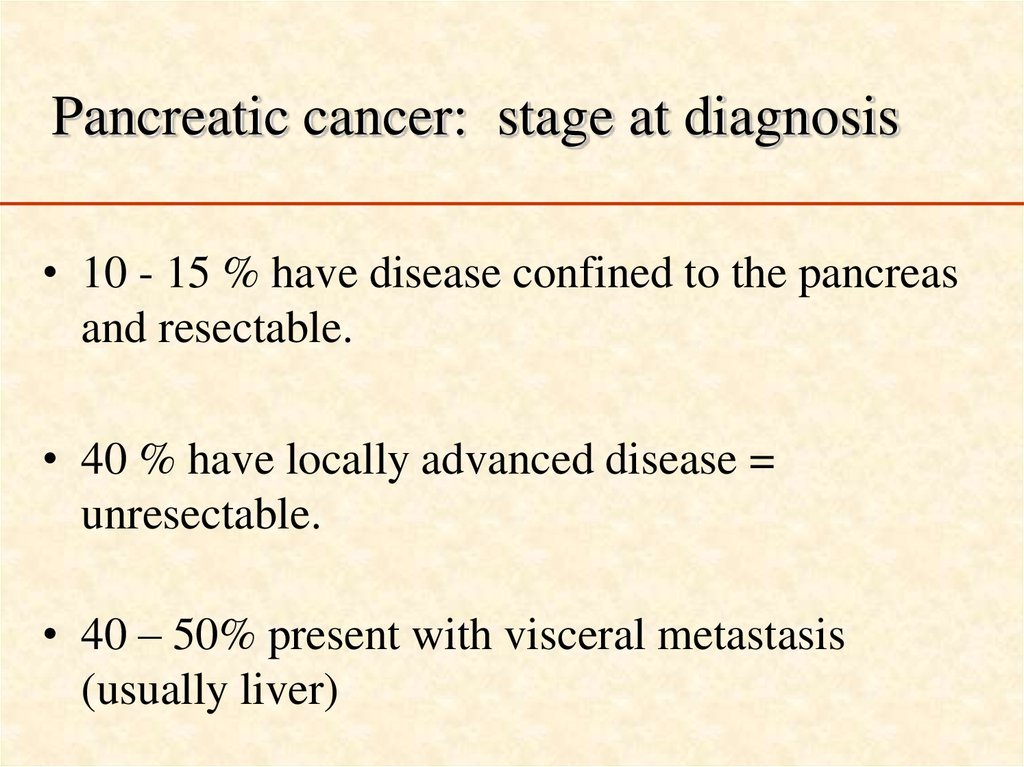
Pancreatic cancer: stage at diagnosis• 10 - 15 % have disease confined to the pancreas
and resectable.
• 40 % have locally advanced disease =
unresectable.
• 40 – 50% present with visceral metastasis
(usually liver)
52. Pancreatic cancer: stage at diagnosis
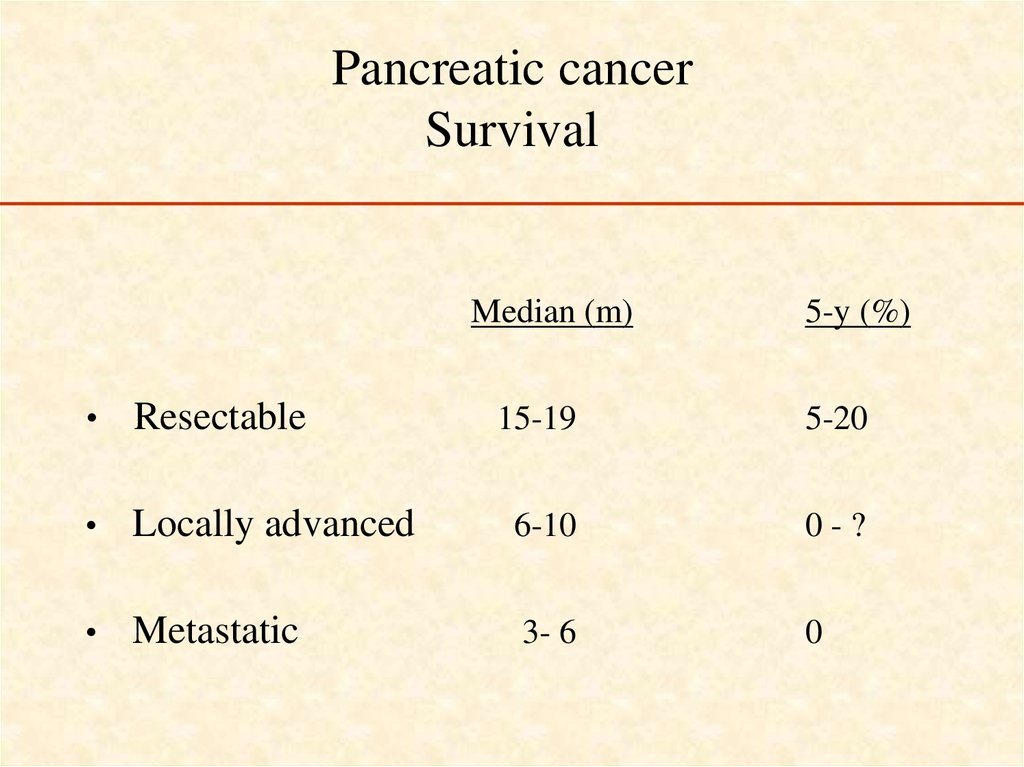
Pancreatic cancerSurvival
Median (m)
Resectable
5-y (%)
15-19
5-20
Locally advanced
6-10
0-?
Metastatic
3- 6
0
53. Pancreatic cancer Survival
• Why are the results so poor ?– Symptoms tend to occur rather late
– Surgery to remove pancreatic cancer is very
complicated
– The biology of pancreatic cancer makes it an unusually
aggressive cancer (small tumor-big effect; resistance to
treatment)
54.
Treatment of metastatic pancreaticcancer
55. Treatment of metastatic pancreatic cancer
56.
Treatment ScheduleGemcitabine
5-Fluorouracil (5FU)
Pts = 126
1000mg/m2/wk
600mg/m2/wk
57.
Metastatic pancreatic cancerGemcitabine
• No confirmed objective responses
• Clinical benefit response 23.8% in Gem arm,
4.8% in 5-FU arm (P= .0022)
• Median survival 5.65 vs. 4.41 mos (P= .0025)
58. Metastatic pancreatic cancer Gemcitabine
Beyond single-agent gemcitabine ?• Gemcitabine-based combination CT
– G + cisplatin
– G + capecitabine (xeloda)
– G + Abraxane
modest improvement, if at all
• non-gemcitabine based combination CT
– FOLFORINOX (5FU, oxaliplatin, irinotecan)
6.8 ↑to 11.1 m
RR X3 (31.6 vs 9.4%), OS
• Targeted therapy
• G + erlotinib (tarceva= Human Epidermal Growth
Factor Receptor Type 1/Epidermal Growth Factor
Receptor (HER1/EGFR) tyrosine kinase inhibitor)
59. Beyond single-agent gemcitabine ?
FOLFIRINOX versus gemcitabineOS
Probability
1
HR = 0,57 ; IC95 : 0,45-0,73
0,75
0,5
p < 0,0001
FOLFIRINOX
OS = 11.1m
0,25
Gemcitabine
OS = 6.8m
0
0
6
12
18
24
30
36
3
9
2
3
2
2
M
Gemcitabine 171
FOLFIRINOX 171
89
116
28
62
7
20
ASCO 2010 - Conroy T et al., abstr. 4010
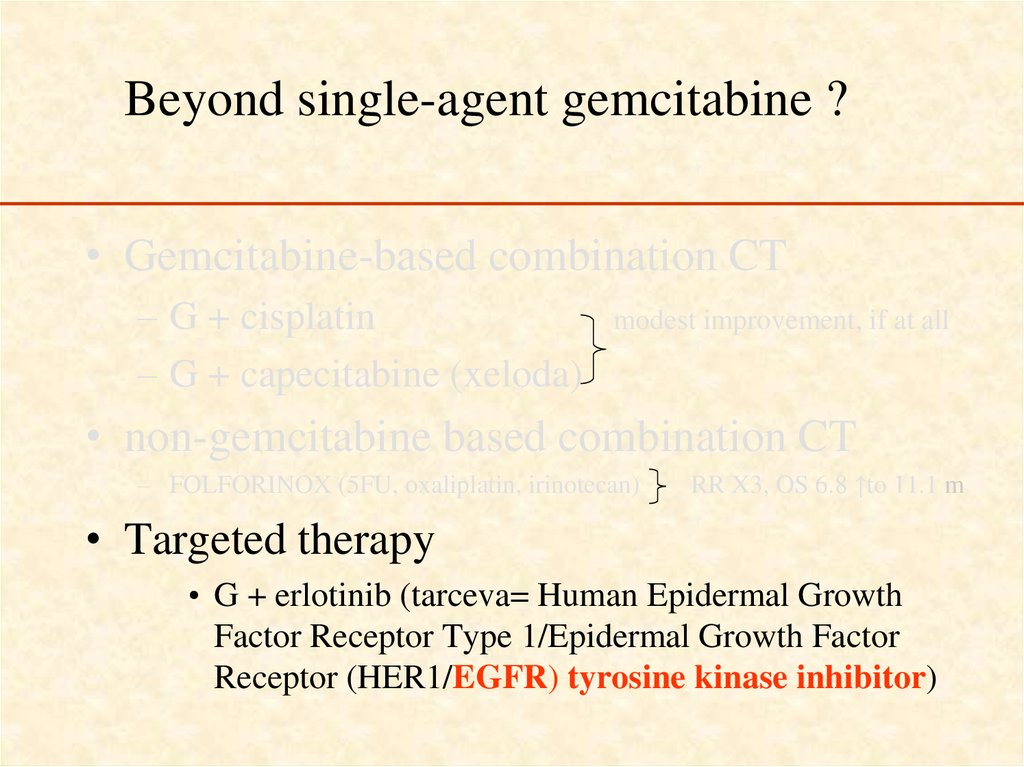
60. FOLFIRINOX versus gemcitabine OS
Beyond single-agent gemcitabine ?• Gemcitabine-based combination CT
– G + cisplatin
– G + capecitabine (xeloda)
modest improvement, if at all
• non-gemcitabine based combination CT
– FOLFORINOX (5FU, oxaliplatin, irinotecan)
RR X3, OS 6.8 ↑to 11.1 m
• Targeted therapy
• G + erlotinib (tarceva= Human Epidermal Growth
Factor Receptor Type 1/Epidermal Growth Factor
Receptor (HER1/EGFR) tyrosine kinase inhibitor)
61. Beyond single-agent gemcitabine ?
62.
GEM plus ErlotinibGemcitabine (1000 mg/m2) +
Erlotinib (100 or 150 mg/die)
vs.
Gemcitabine (1000 mg/m2) +
Placebo
Pts=569 (naïve advanced pancreatic cancer)
OS
6.24 months (GEM+ERL) vs.
5.91 months (GEM)
P=0.038
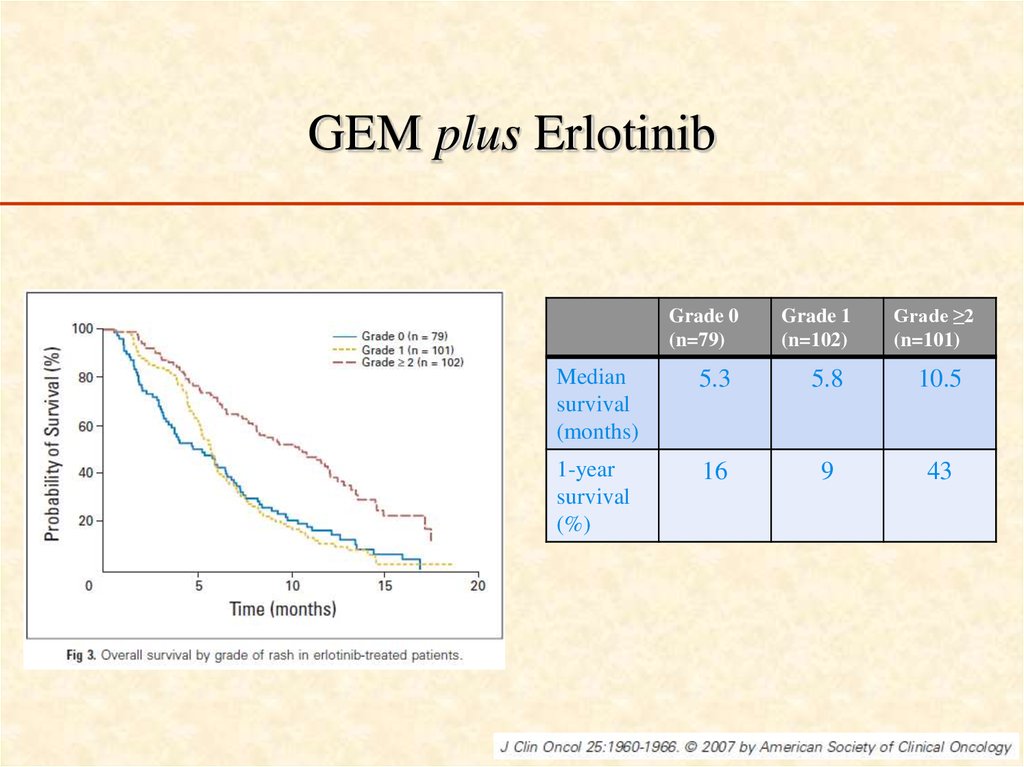
63. GEM plus Erlotinib
Grade 0(n=79)
Grade 1
(n=102)
Grade ≥2
(n=101)
Median
survival
(months)
5.3
5.8
10.5
1-year
survival
(%)
16
9
43
64. GEM plus Erlotinib
Locally advanced disease (LAD)clinical highlights
• Median survival of LAD is 6-10 months
• Most patients are symptomatic ( pain,
weight loss, fatigue)
65. Locally advanced disease (LAD) clinical highlights
LADAims of treatment
• Improvement of quality of life = clinical
benefit response (CBR)
• Local control = prolongation of survival ?
• Downstaging = resectability ?
66. LAD Aims of treatment
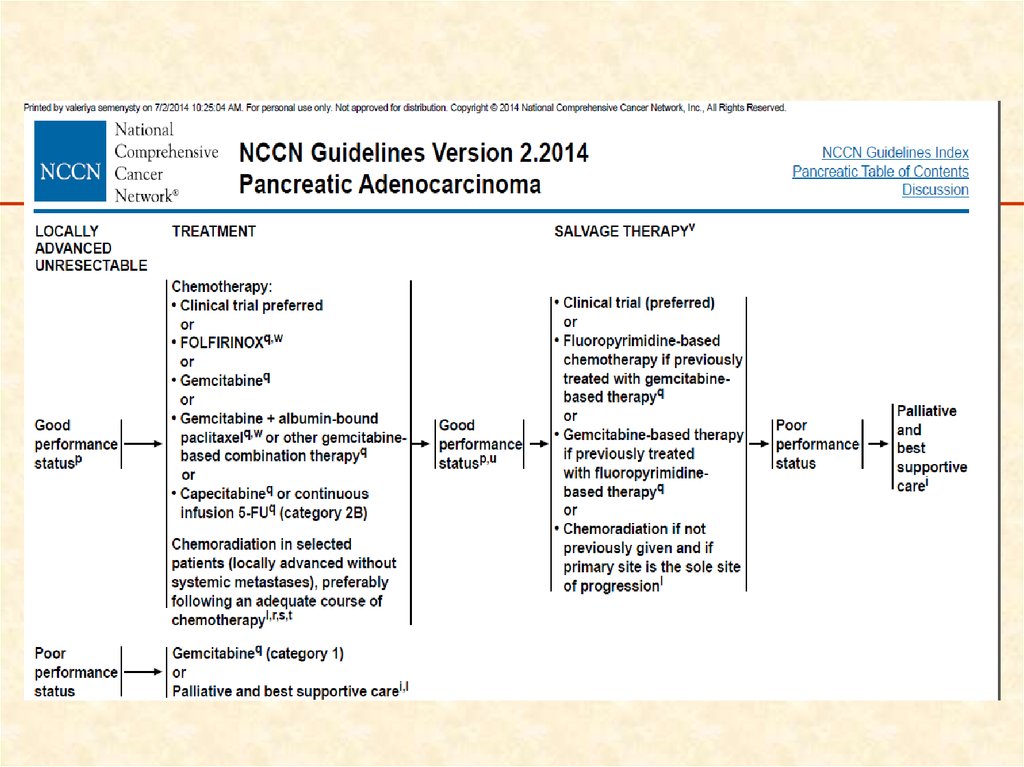
Practical guidelines 2013Rambam
• Gemcitabine-based chemotherapy for up to 4
months (as long as there is no progression), followed
by gemcitabine or 5-FU or capecitabine –based
chemoradiation.
• Single-agent gemcitabine in patients with poor
performance status.
67. Practical guidelines 2013 Rambam
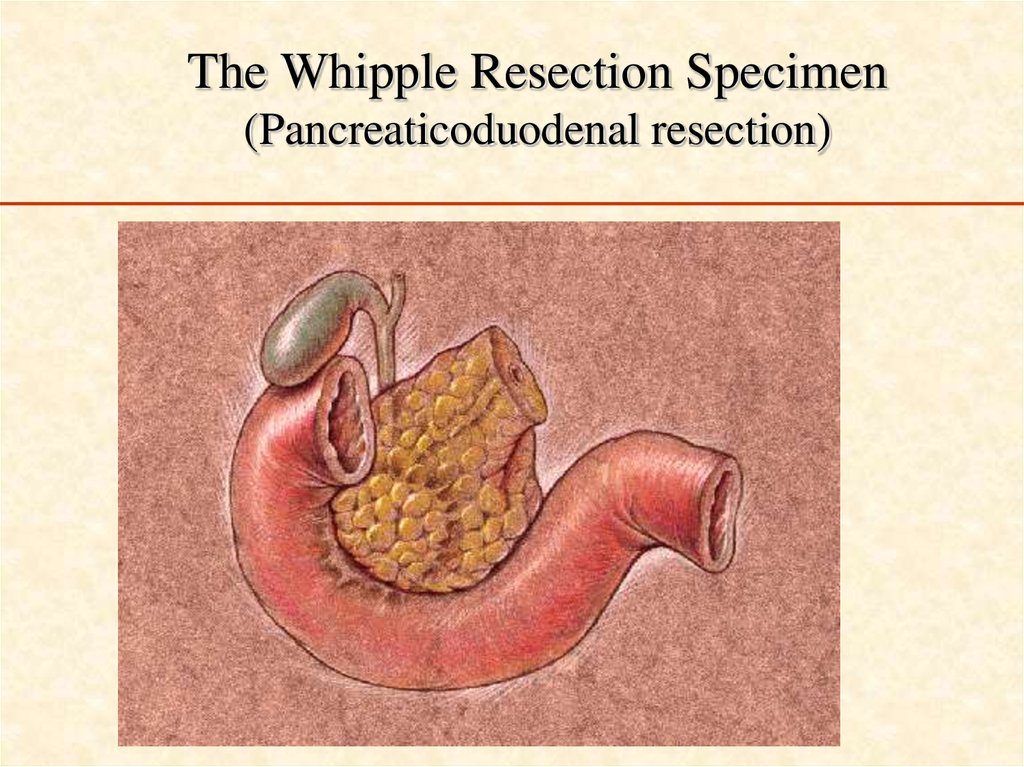
The Whipple Resection Specimen(Pancreaticoduodenal resection)
68. The Whipple Resection Specimen (Pancreaticoduodenal resection)
אלבום תמונותעל ידי אר
69. אלבום תמונות
Resectable pancreatic cancer• Long-term survival after resection (10-20% 5-y),
probably there is no plateau = no cure (10 & 20-y )
• Local recurrence (50-85%), peritoneal spread
(40%), liver metastases (60-90%).
• Do we have an effective adjuvant therapy?
70. Resectable pancreatic cancer
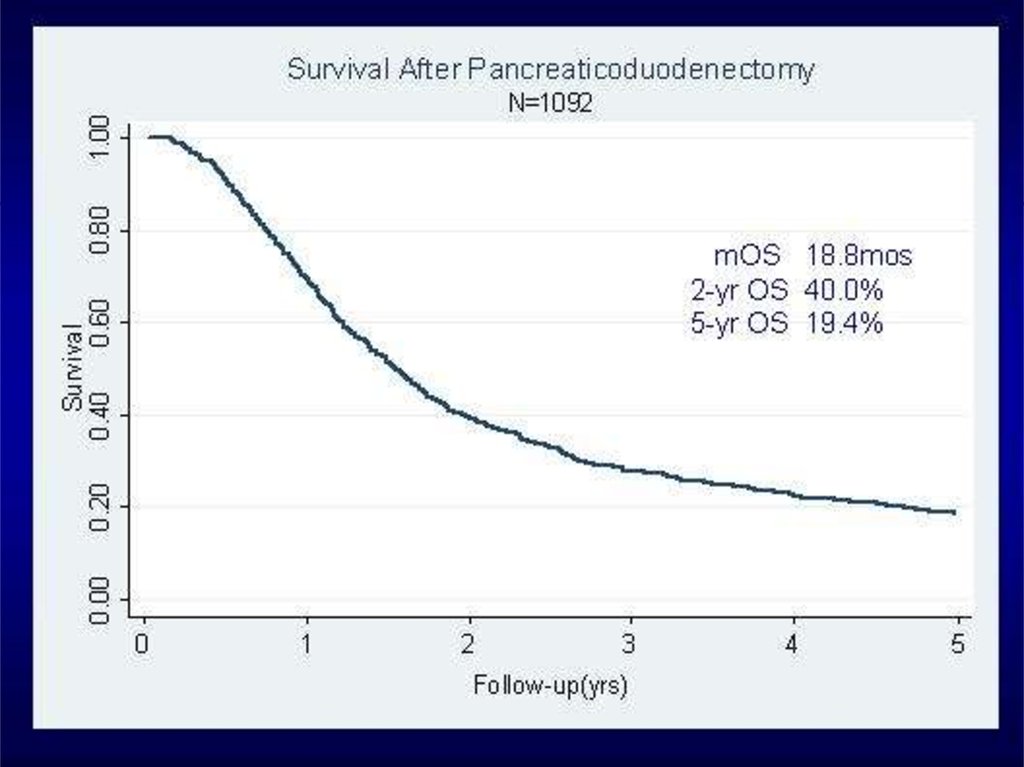
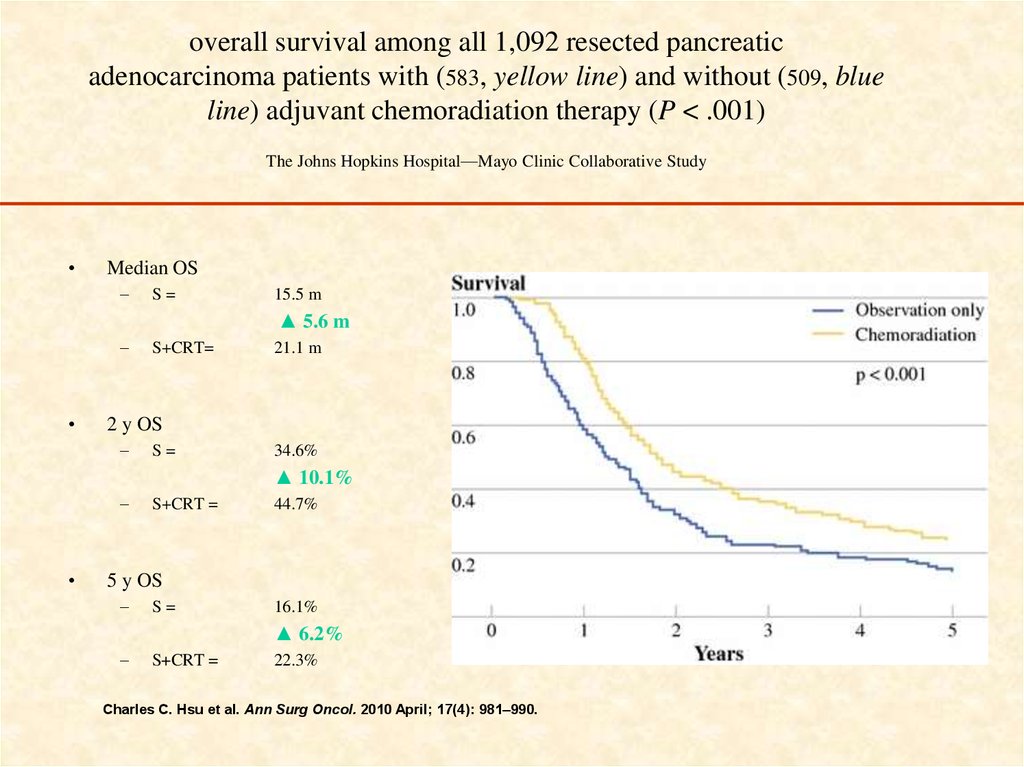
overall survival among all 1,092 resected pancreaticadenocarcinoma patients with (583, yellow line) and without (509, blue
line) adjuvant chemoradiation therapy (P < .001)
The Johns Hopkins Hospital—Mayo Clinic Collaborative Study
Median OS
–
S=
15.5 m
▲ 5.6 m
–
S+CRT=
21.1 m
2 y OS
–
S=
34.6%
▲ 10.1%
–
S+CRT =
44.7%
5 y OS
–
S=
16.1%
▲ 6.2%
–
S+CRT =
22.3%
Charles C. Hsu et al. Ann Surg Oncol. 2010 April; 17(4): 981–990.
71. overall survival among all 1,092 resected pancreatic adenocarcinoma patients with (583, yellow line) and without (509, blue
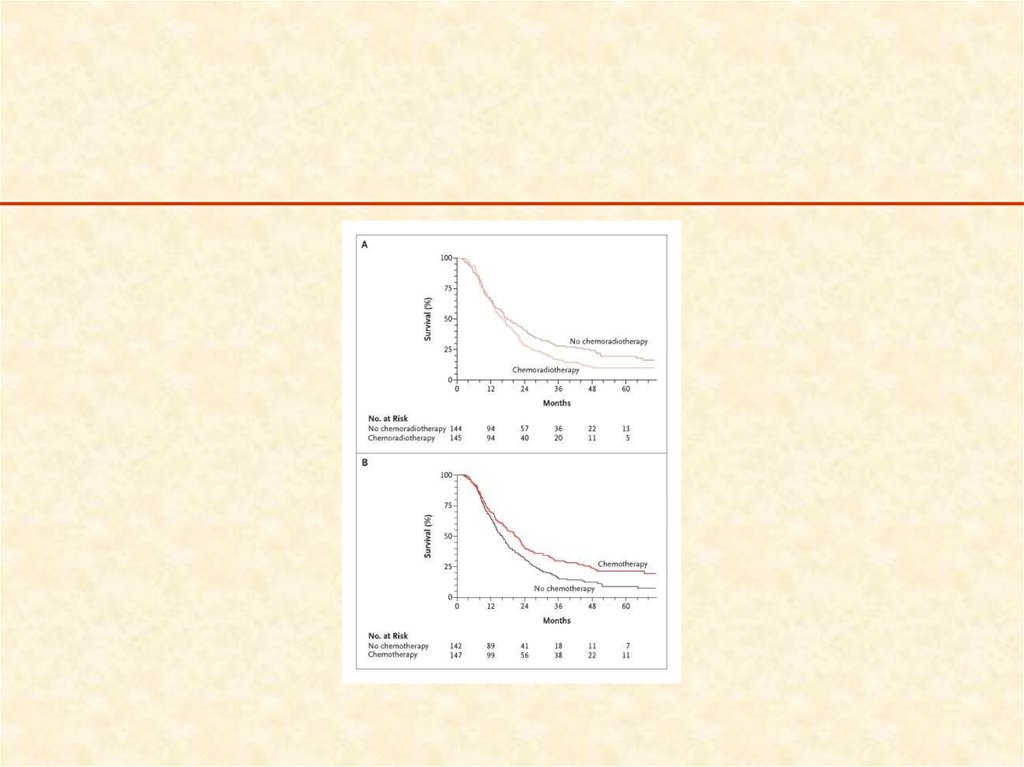
Adjuvant chemoradiotherapy –randomized studies (2)
ESPAC-1 (European Study Group for Pancreatic Cancer) , accrual 1994-2000
Neoptolemos, LANCET 2001 + NEJM 2004 (median FU=47m)
CT/RT (split-course 40 Gy + bolus 5FU daily for 3 initial days of RT)
vs.
CT ( 5FU + folinic acid, Mayo x 6 cycles)
vs
CT/RT+CT
vs.
Observation
72. Adjuvant chemoradiotherapy – randomized studies (2)
73.
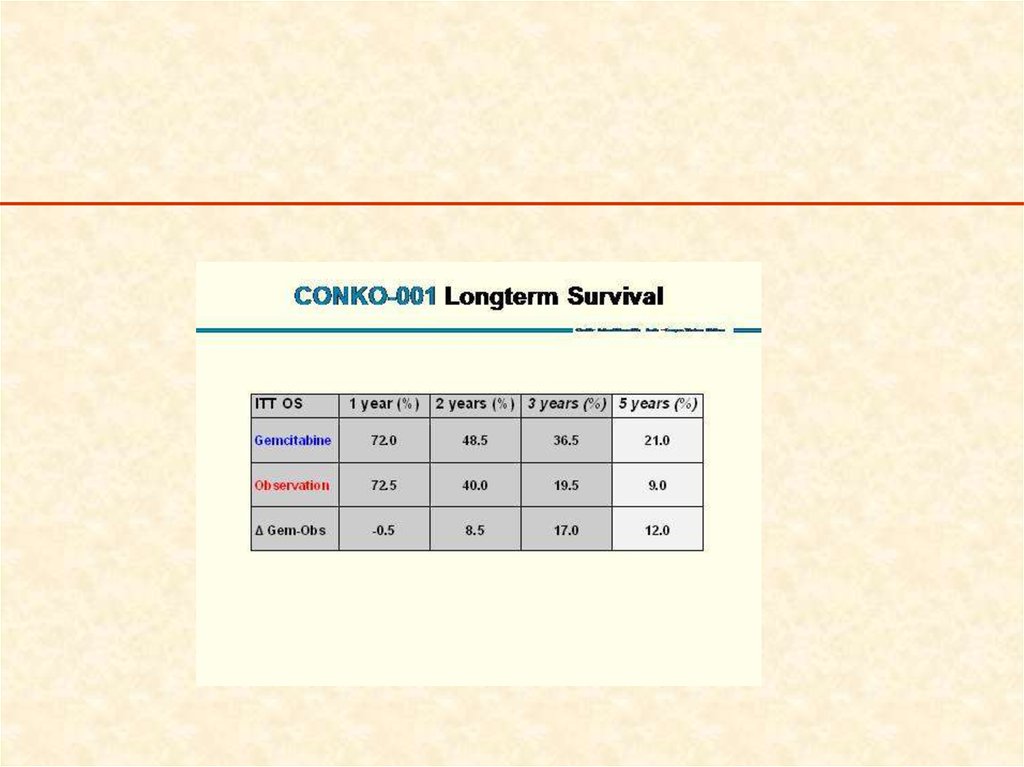
Resectable pancreatic canceradjuvant therapy
chemotherapy only?
• Charité Onkologie [CONKO]-001)
German study
(Oettle, JAMA 2007)
(Neuhaus, ASCO 2008)
DFS-m
: Gemcitabine (6 m)
(182 pts): observation
– (189 pts)
–
13.4
22.8
6.9
20.2
p<0.001
(cross over !)
OS-m
p=0.005
74. Resectable pancreatic cancer adjuvant therapy chemotherapy only?
75.
Practical guidelines 2014Rambam Medical Center
• Chemoradiation Chemotherapy for most patients
• Chemoradiation only is also an acceptable option.
(might be 1st option for patients with R1 resection)
• An option for no adjuvant therapy for the few
“very good” patients = without any risk factor (
size↓, WD, R0, N0, perivascular/perineural
involvement) or ”very frail” patients.
• Chemotherapy: gemcitabine or 5FU (same results)
76. Practical guidelines 2014 Rambam Medical Center
Still unclear…Pancreatology. 2012 Mar;12(2):162-9. Epub 2012 Feb
• Adjuvant chemotherapy, with or without
postoperative radiotherapy, for resectable
advanced pancreatic adenocarcinoma: Continue or
stop?
Ren F, Xu YC, Wang HX, Tang L, Ma Y.
Department of Oncology, Shanghai Renji Hospital, Shanghai Jiaotong University
School of Medicine, Shanghai 200127, China.
77. Still unclear…
• Conclusions:– A significant benefit with regard to DFS and
median OS for adjuvant chemotherapy after
PAC resection was demonstrated by this
analysis.
– These results do not support the use of adjuvant
radiotherapy for PAC.
78.
Future directionsThe future is here, now…?
• Genomics
• Personalized medicine =
רפואה מתאמת אישית
79. Future directions The future is here, now…?
Personalized medicine• patients with the same cancer type respond
differently to therapies due to their unique
molecular profiles.
• Acquired or germeline changes in our DNA
that cause a cancer to develop and grow can
differ from person to person with the same
tumor.
• Molecular testing reveals those differences.
80. Personalized medicine
• Gene expression profiling, molecularprofiling, of the specific tumor of the
specific patient
• To find biomarkers with ↑, ↓, mutated genes
= potential targets for different drugs
• Metabolism
• Direct targeting
81. Personalized medicine
RRM1 → Gemcitabine• RRM1 (Ribonucleotide Reductase subunit M1) involved in DNA synthesis and inhibited by
gemcitabine
• Thus, RRM1 gene-over-expression may be
a negative predictive marker for treatment
with gemcitabine.
82. RRM1 → Gemcitabine
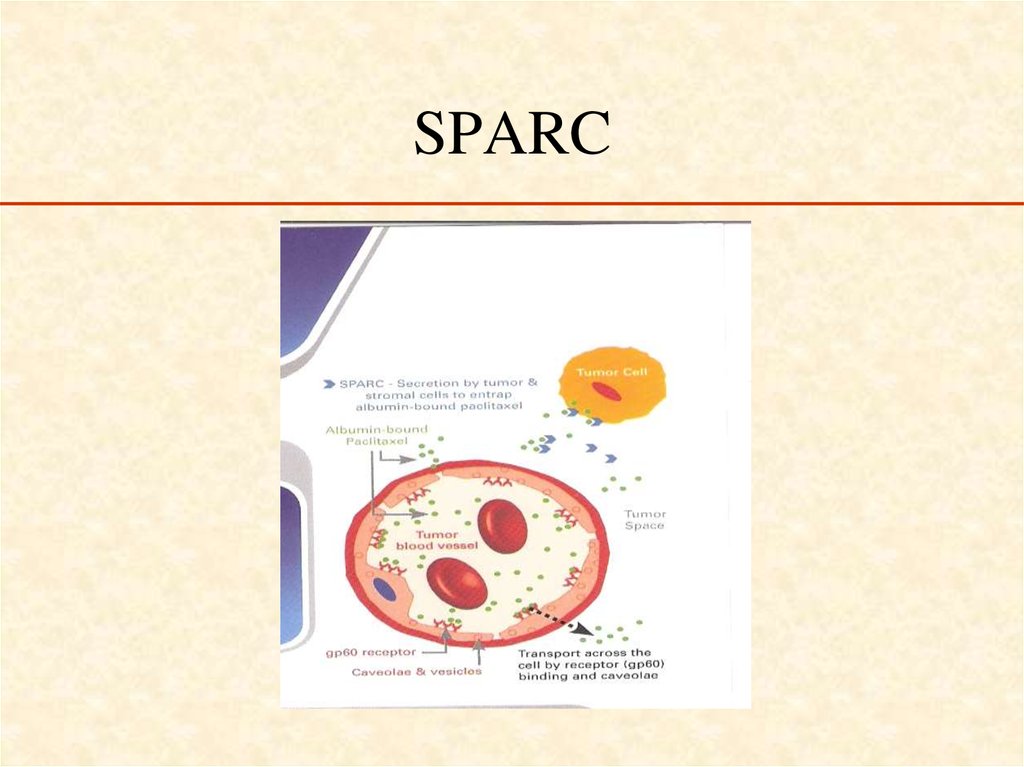
• SPARC (Secreted Protein Acidic and Rich in Cystein) is amatrix-associated protein
• Because of a SPARC-albumin interaction,
tumoral SPARC facilitates the accumulation
of albumin in the tumor and increases the
effectiveness of albumin-bound drugs
83.
SPARC84. SPARC
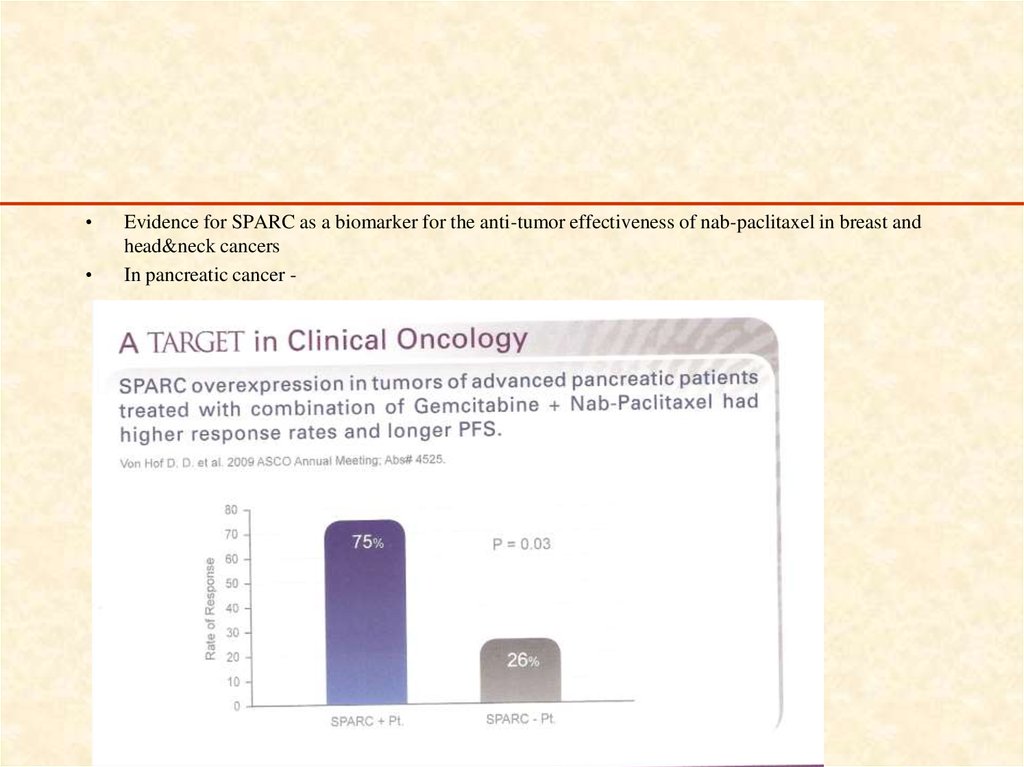
Evidence for SPARC as a biomarker for the anti-tumor effectiveness of nab-paclitaxel in breast and
head&neck cancers
In pancreatic cancer -
85.
BRCA1/2 m → PARP inhibitors86.
• immunohistochemistry )CHI(analysis:– level of important proteins in cancer cells
• Polymerase Chain Reaction (RCP(
• DNA )gnicneuqes NGS=Next Generation Sequencing) to
determine gene mutations in the DNAromut )Specific
genes, exome, whole genome sequencing)
87.
Target Now• A comprehensive patient’s tumor analysis
+
• An exhaustive clinical literature search
=
• Matching appropriate therapies to patientspecific biomarker information to generate
an evidence-based treatment approach
(= finding actionable or druggable targets).
88. Target Now
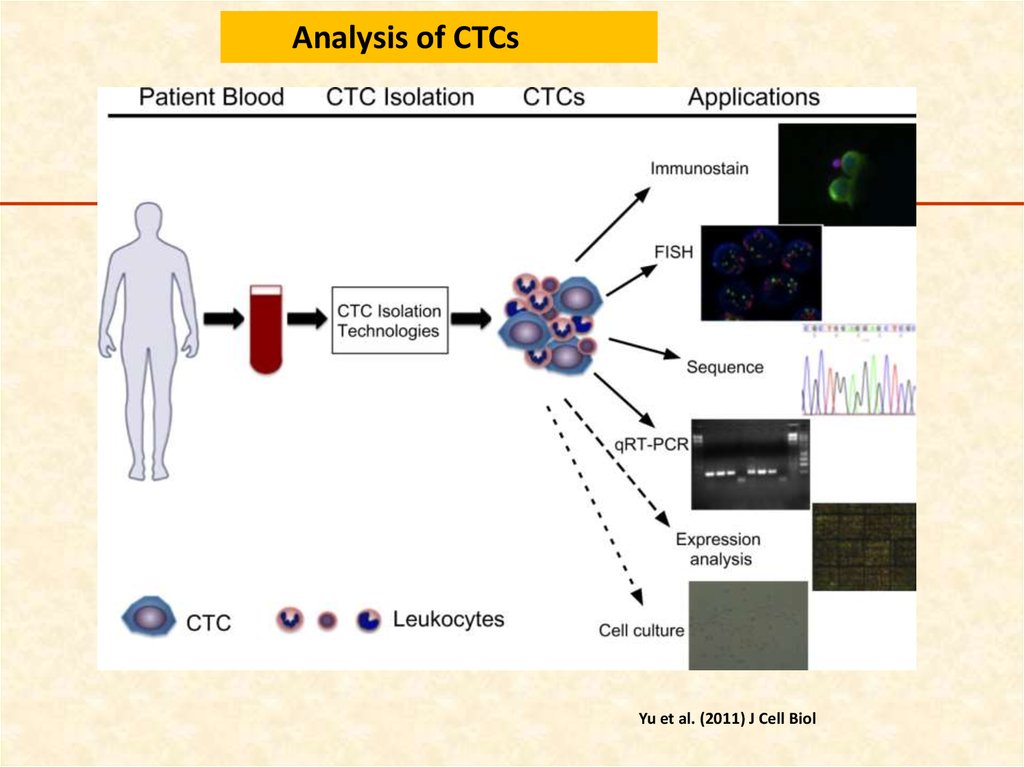
Analysis of CTCsYu et al. (2011) J Cell Biol
89. A Retrospective Investigation to Evaluate the Use of Target Now® Assay in Selecting Treatment in Patients with Advanced Stage
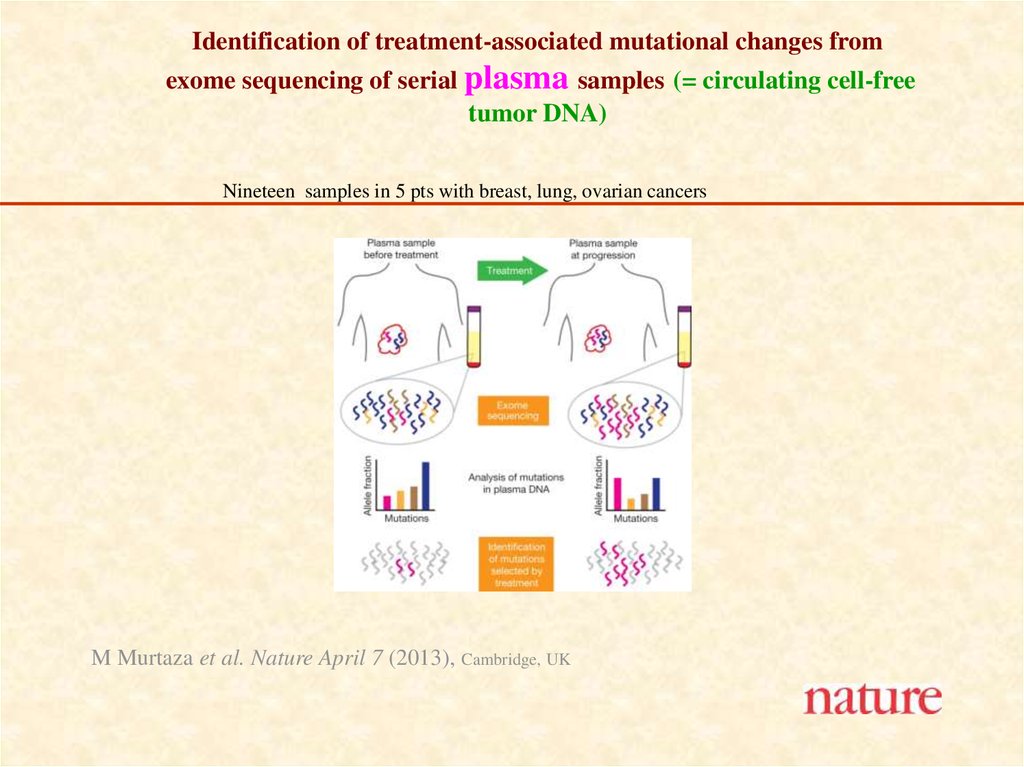
Identification of treatment-associated mutational changes fromexome sequencing of serial plasma samples (= circulating cell-free
tumor DNA)
Nineteen samples in 5 pts with breast, lung, ovarian cancers
M Murtaza et al. Nature April 7 (2013), Cambridge, UK















 Медицина
Медицина