Похожие презентации:
Angina Pectoris
1. ANGINA PECTORIS
2. International classification of Ischaemic heart disease (ESC-2013)
Sudden coronary death
Angina pectoris
Acute myocardial infarction
Painless myocardial ischaemia
Heart failure
Disturbences of rhythm and
conductivity
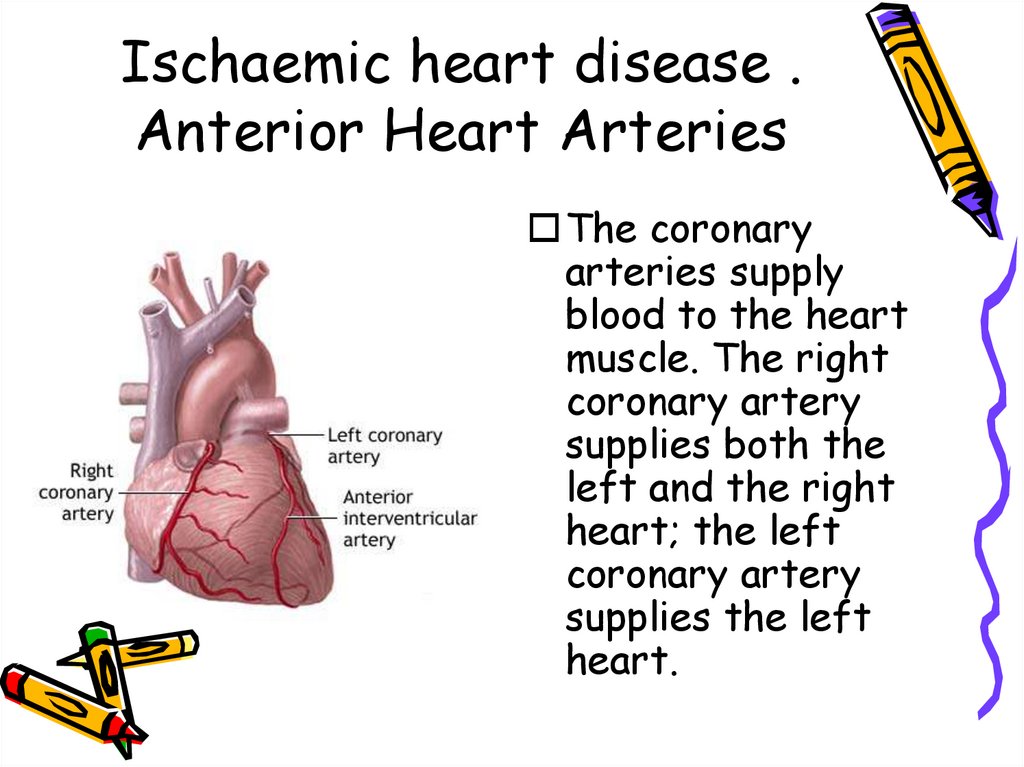
3. Ischaemic heart disease . Anterior Heart Arteries
The coronaryarteries supply
blood to the heart
muscle. The right
coronary artery
supplies both the
left and the right
heart; the left
coronary artery
supplies the left
heart.
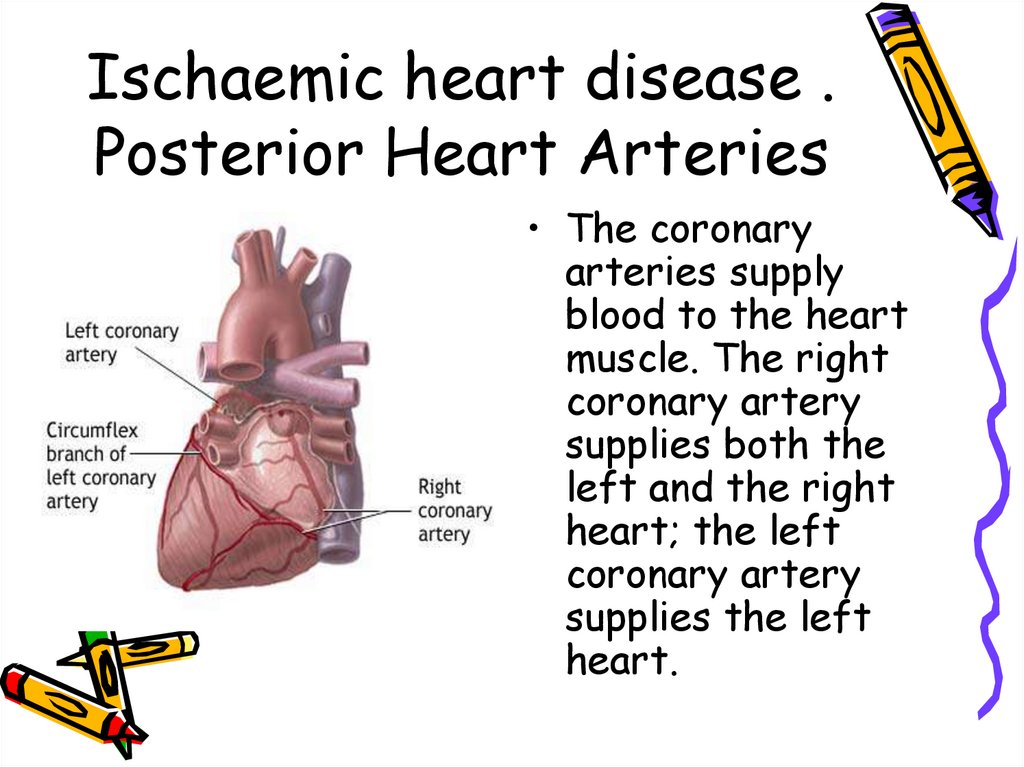
4. Ischaemic heart disease . Posterior Heart Arteries
• The coronaryarteries supply
blood to the heart
muscle. The right
coronary artery
supplies both the
left and the right
heart; the left
coronary artery
supplies the left
heart.
5. Ischaemic heart disease
• Ischaemic heart disease (Coronary arterydisease) – is the most common form of
heart disease and the single most
important cause of premature death in
Europe, Russia, North and South America,
Australia and New Zealand.
• Ischaemic heart disease (IHD) – heart
disease due to imbalance between
myocardial oxygen supply and demand,
which assotiated with atherosclerosis of
coronary arteries in 95-96% cases.
6.
ANGINA PECTORIS-DEFINITION•Angina pectoris is the clinical symptom
complex caused by transient myocardial
ischaemia and may occur whenever there is
an imbalance between myocardial oxygen
supply and demand.
7. ANGINA PECTORIS-DEFINITION
ANGINA PECTORISDEFINITION• Angina pectoris is the medical term used to describe
chest pains caused by poor blood flow to certain
areas of the heart muscle. Often, the name is
shortened to angina. Having angina means patients
have an increased risk of having a heart attack
(myocardial infarction). Angina can be a useful
warning sign if it makes patient seek timely medical
help and avoid a heart attack. Prolonged or unchecked
angina can lead to a heart attack or increase risk of
having a heart rhythm abnormality. That could lead to
sudden death.
8.
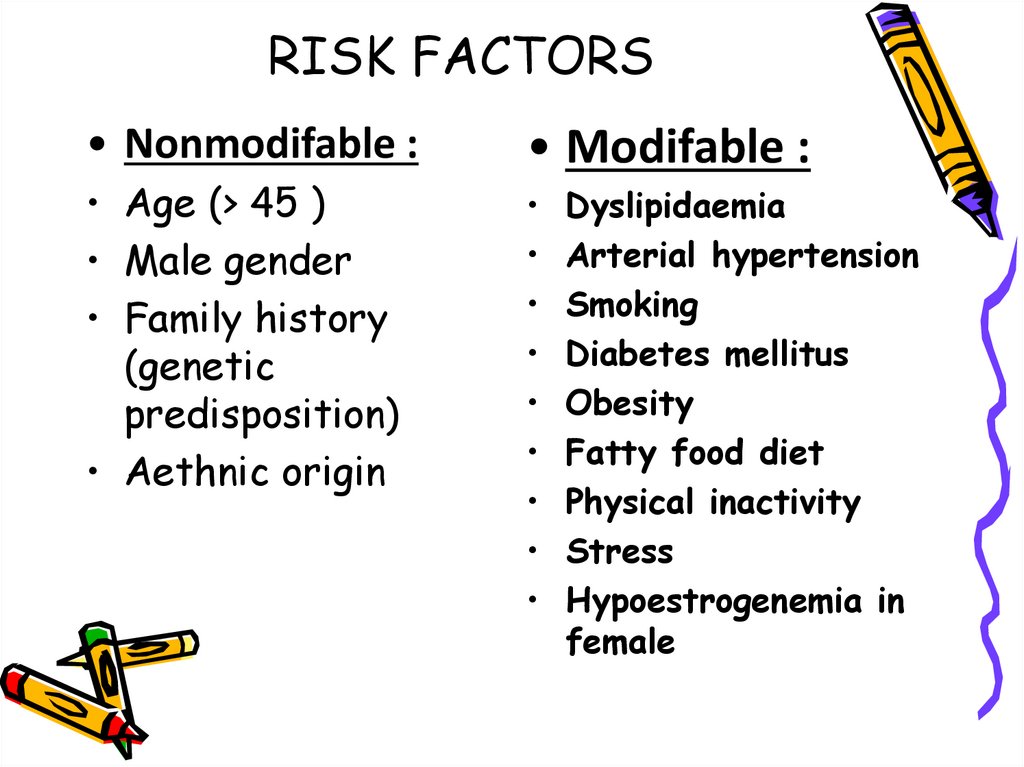
9. RISK FACTORS
• Nonmodifable :• Age (> 45 )
• Male gender
• Family history
(genetic
predisposition)
• Aethnic origin
• Modifable :
Dyslipidaemia
Arterial hypertension
Smoking
Diabetes mellitus
Obesity
Fatty food diet
Physical inactivity
Stress
Hypoestrogenemia in
female
10.
11.
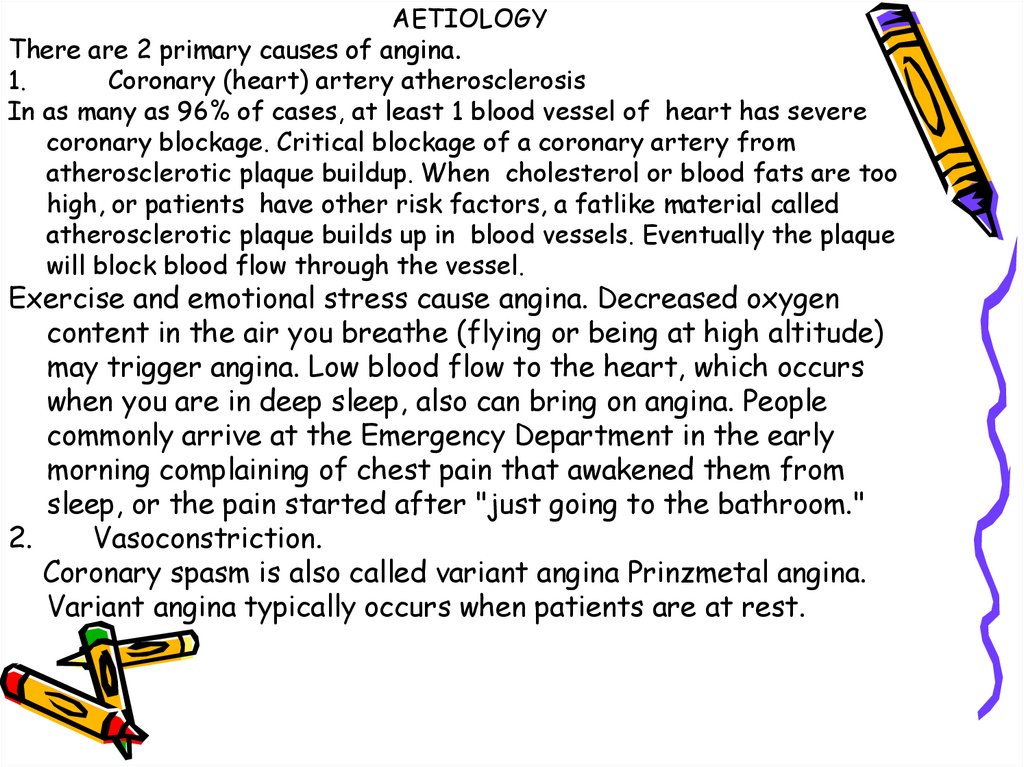
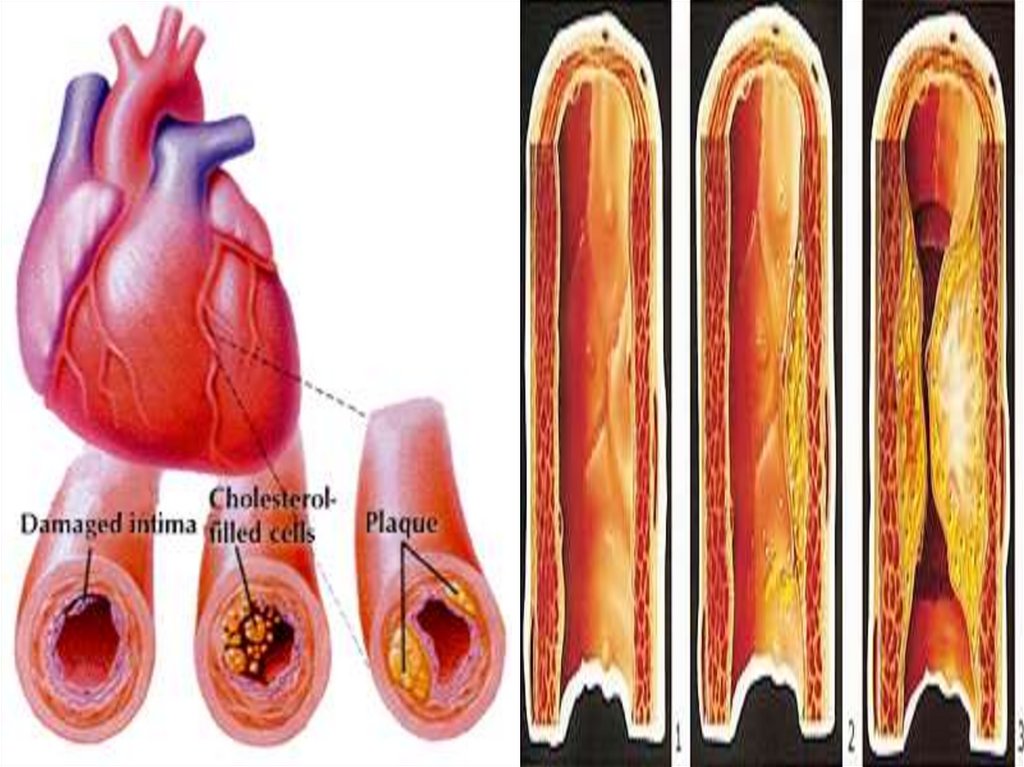
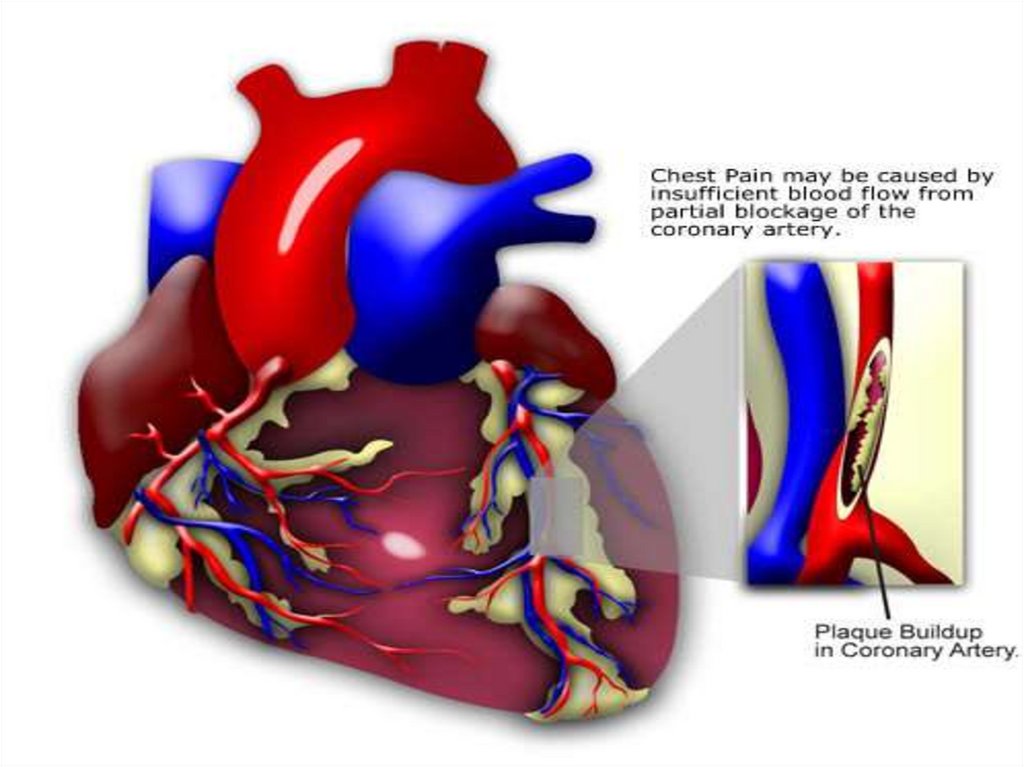
AETIOLOGYThere are 2 primary causes of angina.
1.
Coronary (heart) artery atherosclerosis
In as many as 96% of cases, at least 1 blood vessel of heart has severe
coronary blockage. Critical blockage of a coronary artery from
atherosclerotic plaque buildup. When cholesterol or blood fats are too
high, or patients have other risk factors, a fatlike material called
atherosclerotic plaque builds up in blood vessels. Eventually the plaque
will block blood flow through the vessel.
Exercise and emotional stress cause angina. Decreased oxygen
content in the air you breathe (flying or being at high altitude)
may trigger angina. Low blood flow to the heart, which occurs
when you are in deep sleep, also can bring on angina. People
commonly arrive at the Emergency Department in the early
morning complaining of chest pain that awakened them from
sleep, or the pain started after "just going to the bathroom."
2.
Vasoconstriction.
Coronary spasm is also called variant angina Prinzmetal angina.
Variant angina typically occurs when patients are at rest.
12.
13.
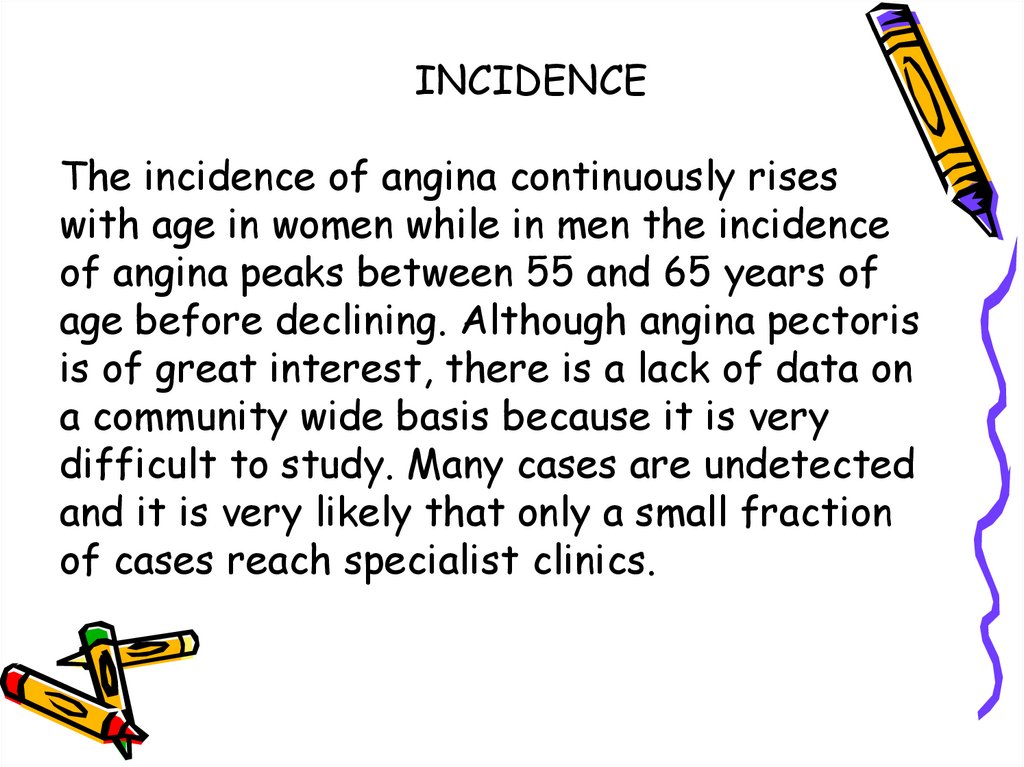
INCIDENCEThe incidence of angina continuously rises
with age in women while in men the incidence
of angina peaks between 55 and 65 years of
age before declining. Although angina pectoris
is of great interest, there is a lack of data on
a community wide basis because it is very
difficult to study. Many cases are undetected
and it is very likely that only a small fraction
of cases reach specialist clinics.
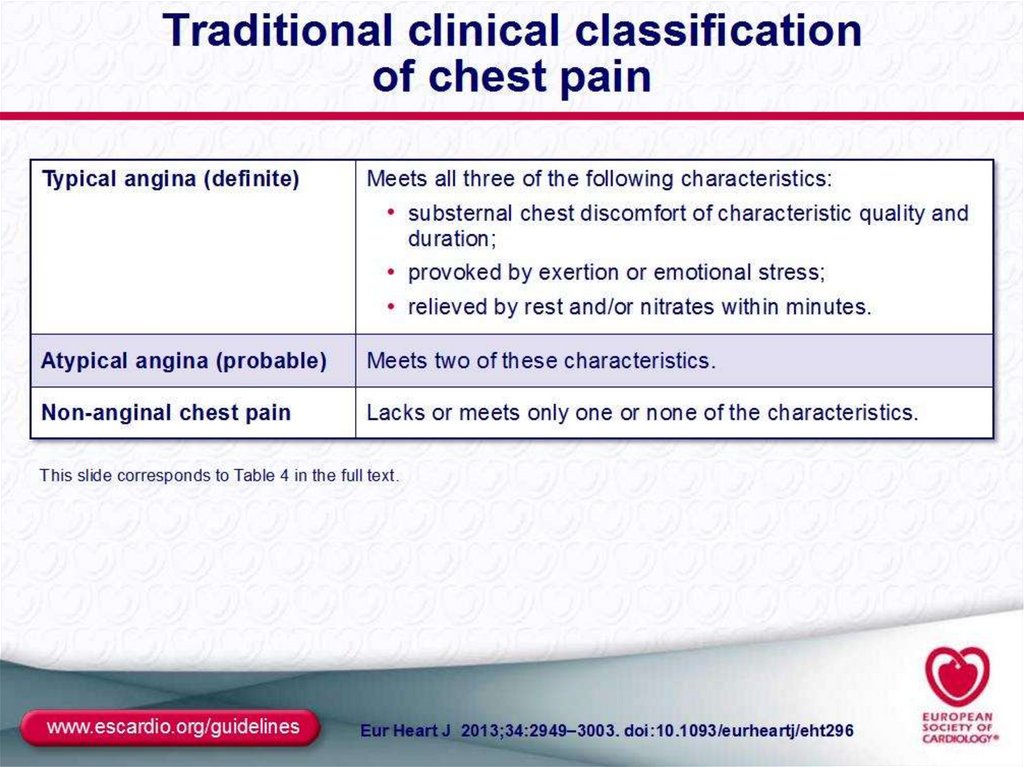
14. Identifying ischaemic cardiac chest pain
Identifying ischaemic cardiac chest
pain
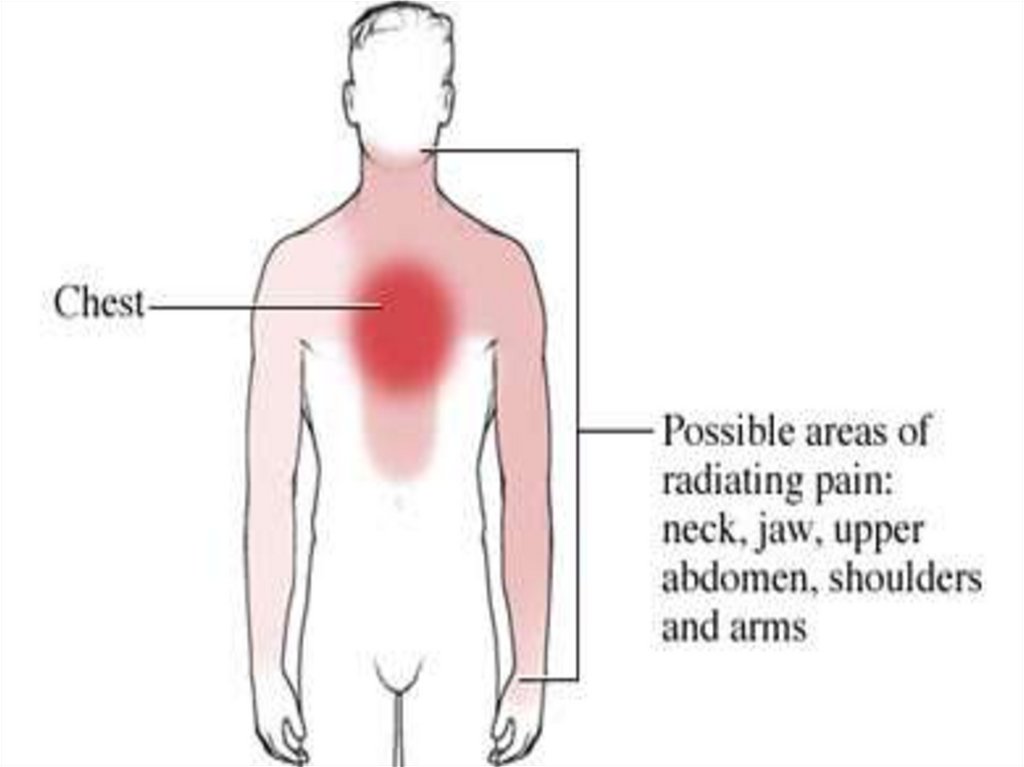
Ischaemic cardiac chest pain:
Location - central, diffuse
Radiation -Jaw/neck/shoulder/ arm/back
Character -tight, burning ,squeezing,
choking
Duration – less than 15 min (3-5 min)
Precipitation -by exertion and/or emotion
Relieving factors - rest, quick response to
nitrates
Associated features- Breathlessness
15.
SIGNS N SYMPTOMSThese are signs and symptoms of angina as well:
• An uncomfortable pressure, fullness, squeezing or pain in the
center of chest
• Pain spreading to your shoulders, neck, or arms and lasting
more than a few minutes.The pain may be mild to intense.
• It may feel like pressure, tightness, burning, or a heavy
weight.
• It may be located in the chest, upper abdomen, back, neck,
jaw, or inside your arms or shoulders.
• Chest discomfort with light headedness
• Anxiety, nervousness or fainting, sweating, nausea, or
shortness of breath
• Increased or irregular heart rate
• Paleness
• Cold sweaty skin
• Feeling of impending doom
16.
17.
18.
19.
20.
CLASSIFICATIONTypes of Angina Pectoris
•Stable Angina
•Unstable Angina
•Prinzmetal’s or variant angina
•Microvascular angina
21.
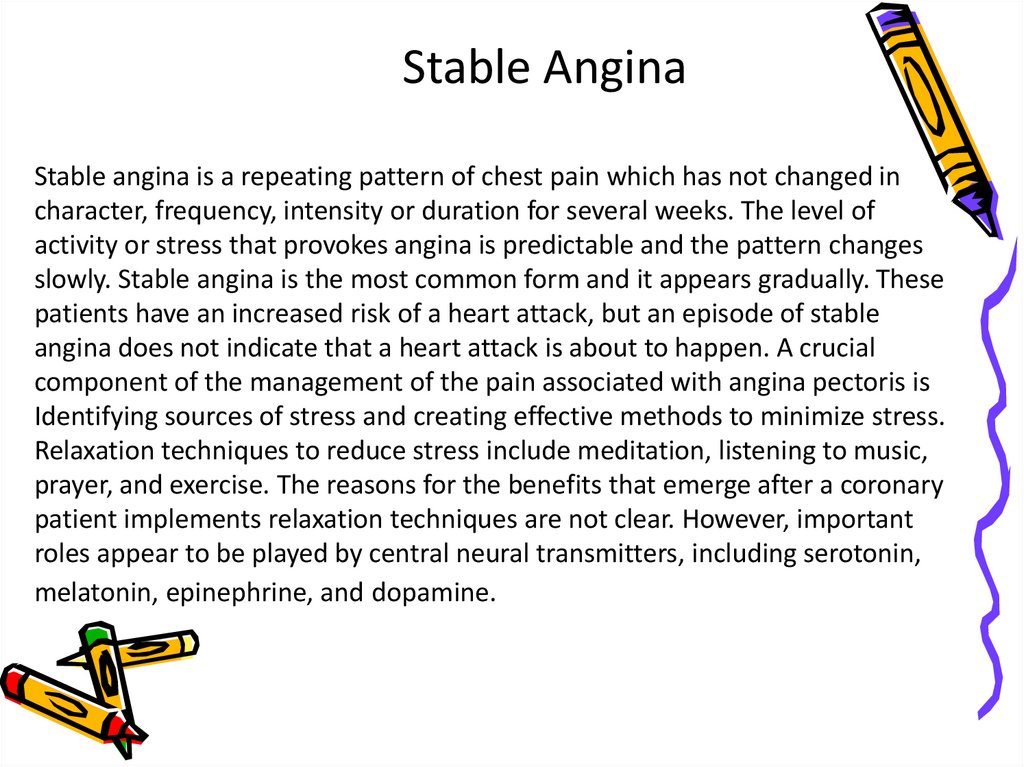
Stable AnginaStable angina is a repeating pattern of chest pain which has not changed in
character, frequency, intensity or duration for several weeks. The level of
activity or stress that provokes angina is predictable and the pattern changes
slowly. Stable angina is the most common form and it appears gradually. These
patients have an increased risk of a heart attack, but an episode of stable
angina does not indicate that a heart attack is about to happen. A crucial
component of the management of the pain associated with angina pectoris is
Identifying sources of stress and creating effective methods to minimize stress.
Relaxation techniques to reduce stress include meditation, listening to music,
prayer, and exercise. The reasons for the benefits that emerge after a coronary
patient implements relaxation techniques are not clear. However, important
roles appear to be played by central neural transmitters, including serotonin,
melatonin, epinephrine, and dopamine.
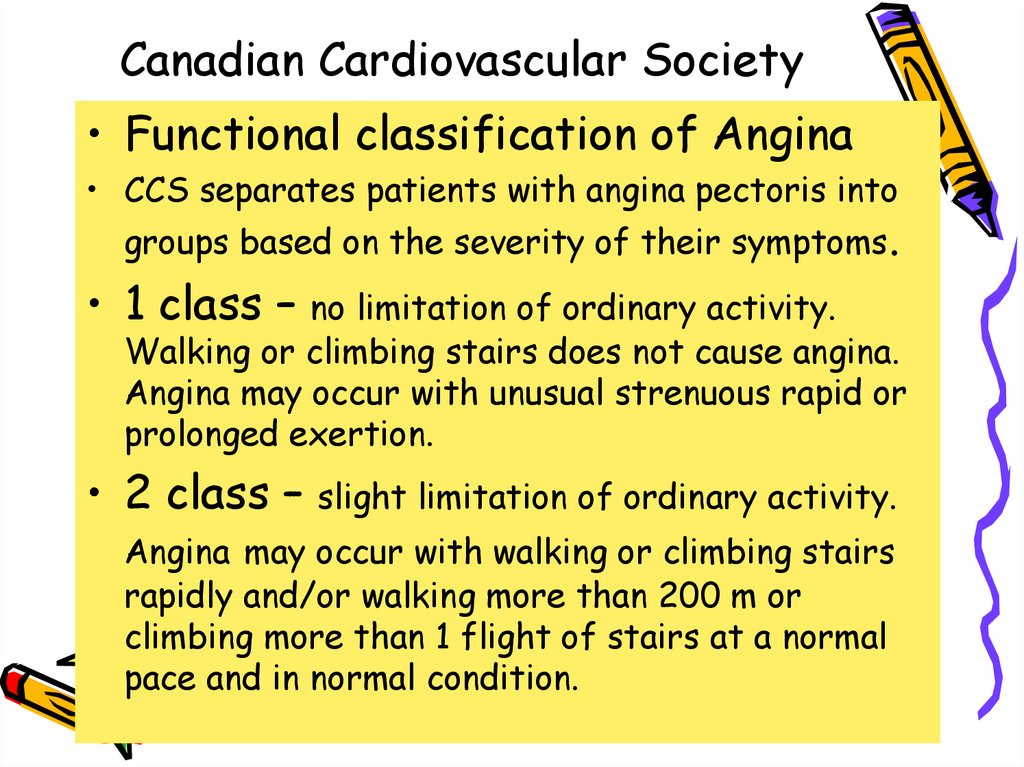
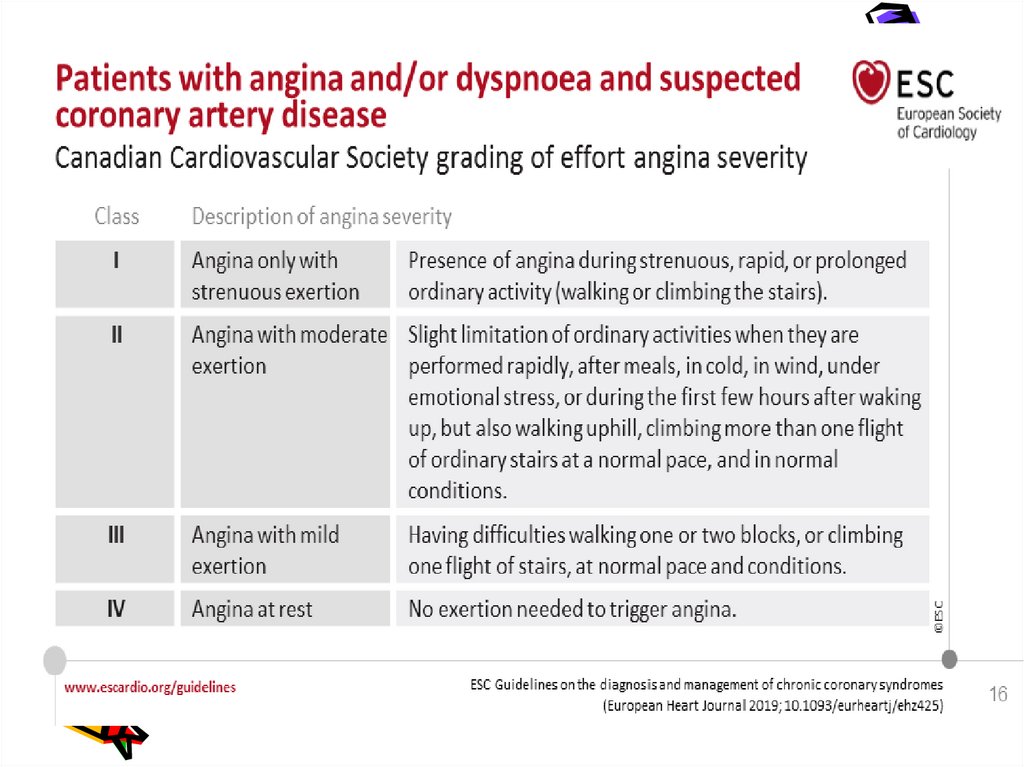
22. Сanadian Cardiovascular Society
• Functional classification of Angina• ССS separates patients with angina pectoris into
groups based on the severity of their symptoms.
• 1 class –
no limitation of ordinary activity.
Walking or climbing stairs does not cause angina.
Angina may occur with unusual strenuous rapid or
prolonged exertion.
• 2 class –
slight limitation of ordinary activity.
Angina may occur with walking or climbing stairs
rapidly and/or walking more than 200 m or
climbing more than 1 flight of stairs at a normal
pace and in normal condition.
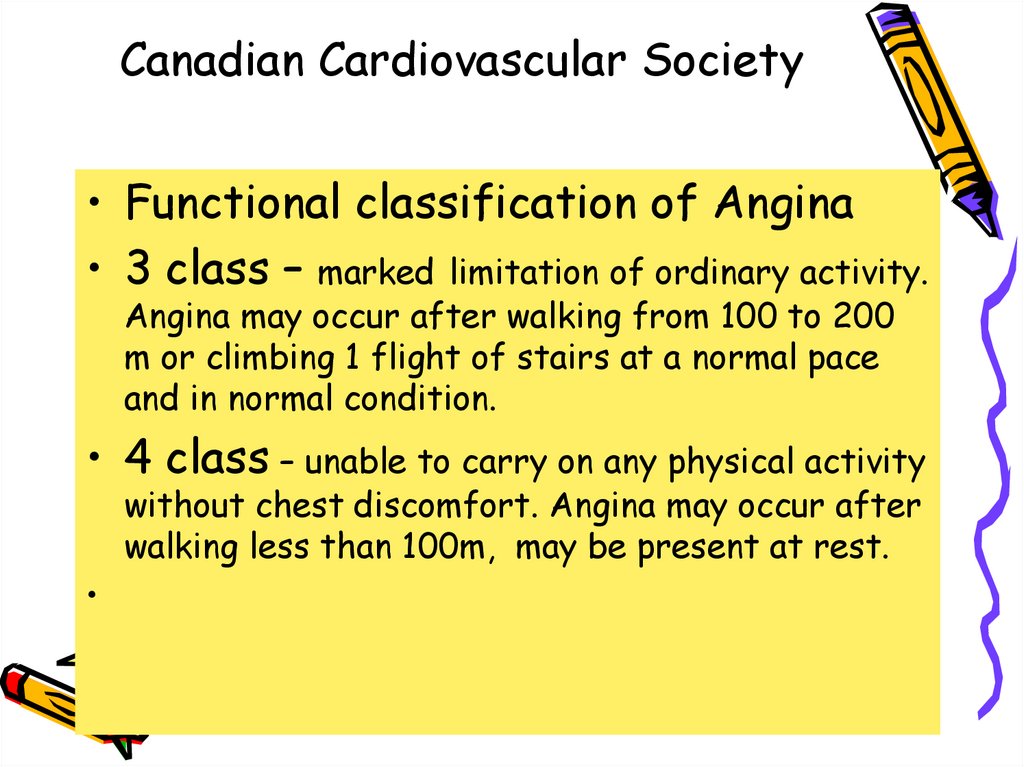
23. Сanadian Cardiovascular Society
• Functional classification of Angina• 3 class – marked limitation of ordinary activity.
Angina may occur after walking from 100 to 200
m or climbing 1 flight of stairs at a normal pace
and in normal condition.
• 4 class – unable to carry on any physical activity
without chest discomfort. Angina may occur after
walking less than 100m, may be present at rest.
24.
25.
Unstable AnginaUnstable angina is chest pain that is variable, either
increasing in frequency or intensity and with irregular
timing or duration. Unlike stable angina, unstable angina
does not appear gradually, it first appears as a severe
episode. An established stable angina might change
suddenly or be provoked by less stress than in the past
or an episode might suddenly occur while at rest. If the
pattern of an episode changes, for example if a previous
episode was only brought on during physical exertion,
but an episode suddenly occurred at rest it is likely to
be unstable angina.
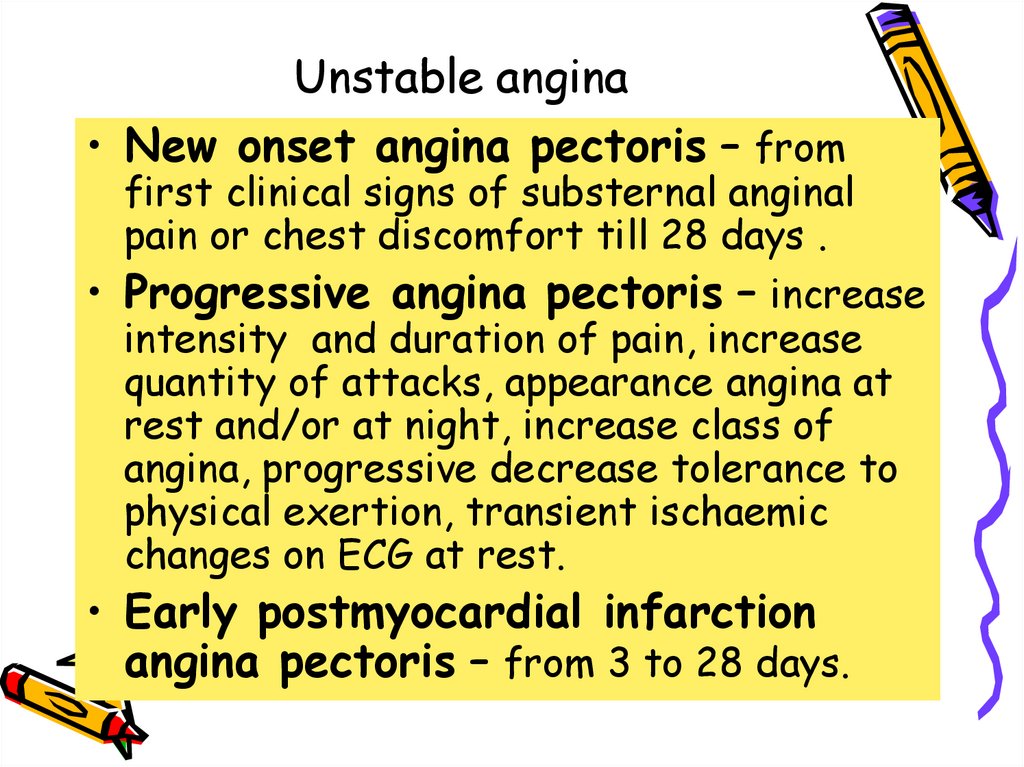
26. Unstable angina
• New onset angina pectoris – fromfirst clinical signs of substernal anginal
pain or chest discomfort till 28 days .
• Progressive angina pectoris – increase
intensity and duration of pain, increase
quantity of attacks, appearance angina at
rest and/or at night, increase class of
angina, progressive decrease tolerance to
physical exertion, transient ischaemic
changes on ECG at rest.
• Early postmyocardial infarction
angina pectoris – from 3 to 28 days.
27.
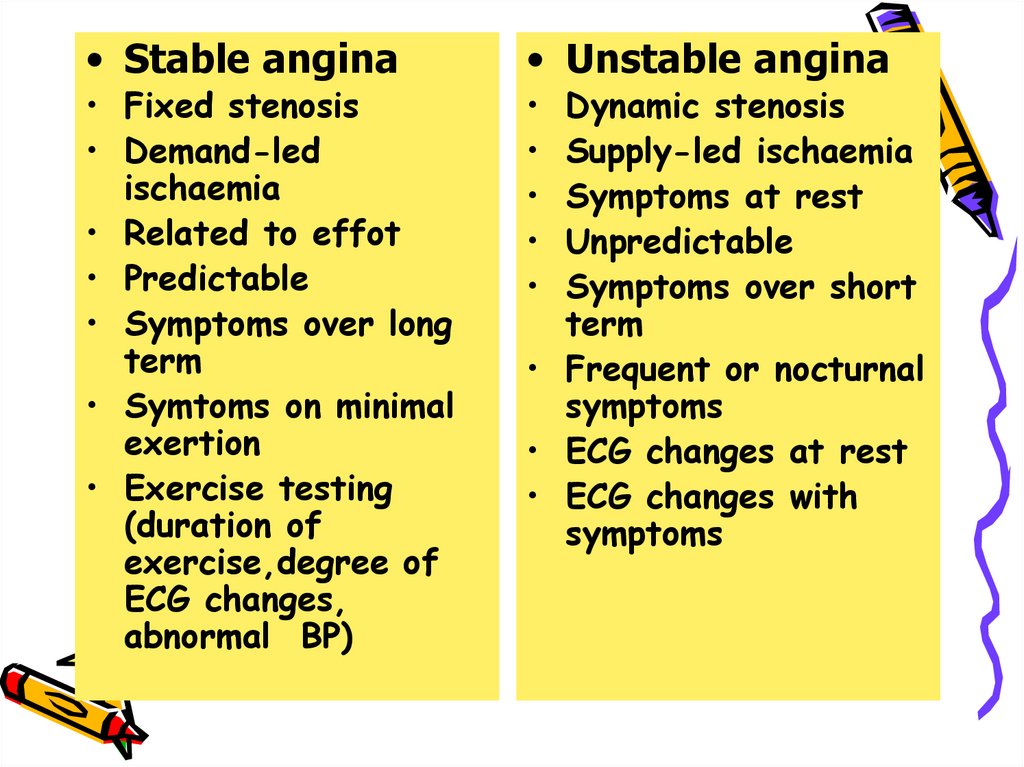
• Stable anginaangina
• Fixed stenosis
• Demand-led
ischaemia
• Related to effot
• Predictable
• Symptoms over long
term
• Symtoms on minimal
exertion
• Exercise testing
(duration of
exercise,degree of
ECG changes,
abnormal BP)
• Unstable angina
Dynamic stenosis
Supply-led ischaemia
Symptoms at rest
Unpredictable
Symptoms over short
term
• Frequent or nocturnal
symptoms
• ECG changes at rest
• ECG changes with
symptoms
28.
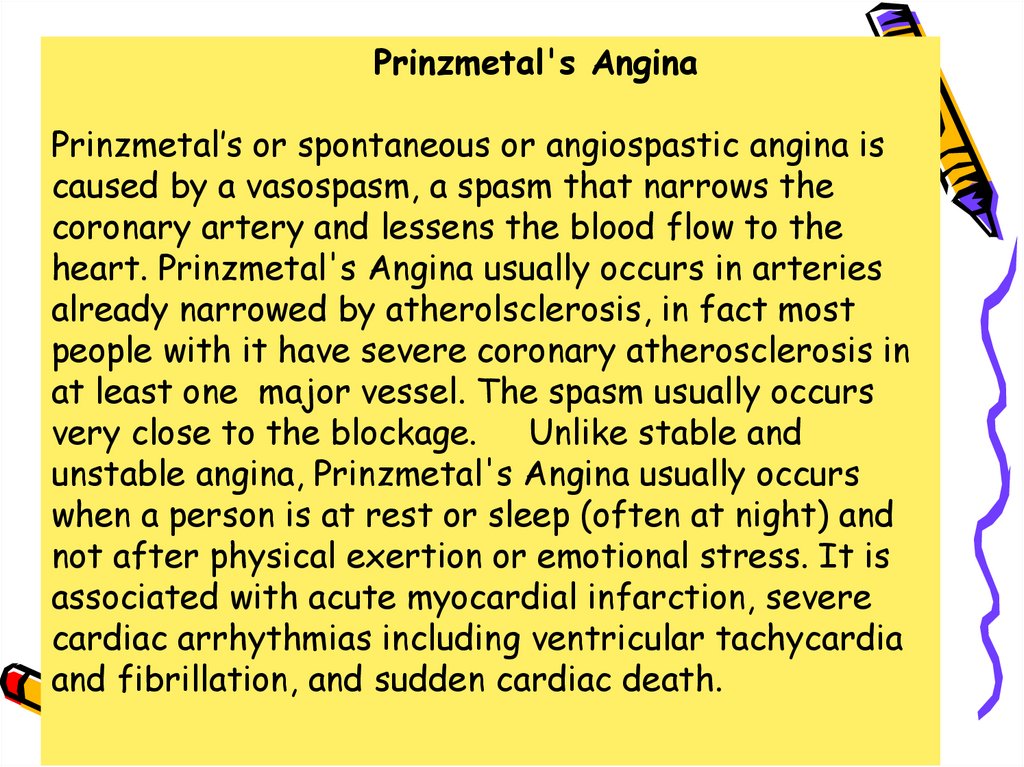
Prinzmetal's AnginaPrinzmetal’s or spontaneous or angiospastic angina is
caused by a vasospasm, a spasm that narrows the
coronary artery and lessens the blood flow to the
heart. Prinzmetal's Angina usually occurs in arteries
already narrowed by atherolsclerosis, in fact most
people with it have severe coronary atherosclerosis in
at least one major vessel. The spasm usually occurs
very close to the blockage. Unlike stable and
unstable angina, Prinzmetal's Angina usually occurs
when a person is at rest or sleep (often at night) and
not after physical exertion or emotional stress. It is
associated with acute myocardial infarction, severe
cardiac arrhythmias including ventricular tachycardia
and fibrillation, and sudden cardiac death.
29.
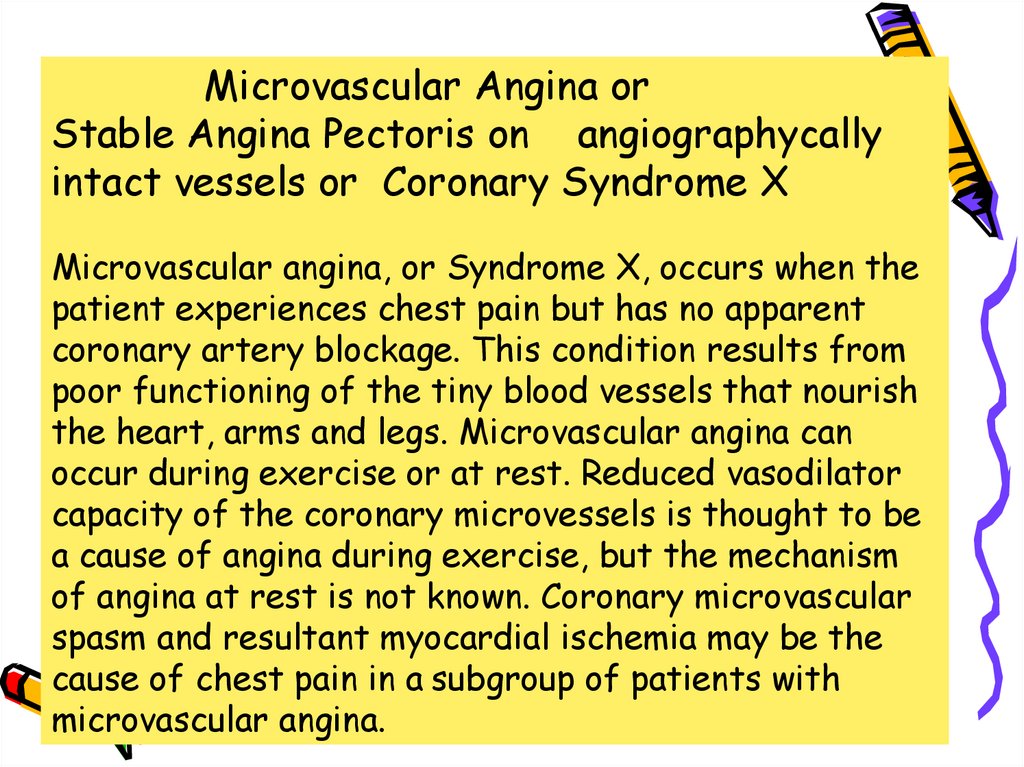
Microvascular Angina orStable Angina Pectoris on angiographycally
intact vessels or Coronary Syndrome X
Microvascular angina, or Syndrome X, occurs when the
patient experiences chest pain but has no apparent
coronary artery blockage. This condition results from
poor functioning of the tiny blood vessels that nourish
the heart, arms and legs. Microvascular angina can
occur during exercise or at rest. Reduced vasodilator
capacity of the coronary microvessels is thought to be
a cause of angina during exercise, but the mechanism
of angina at rest is not known. Coronary microvascular
spasm and resultant myocardial ischemia may be the
cause of chest pain in a subgroup of patients with
microvascular angina.
30. Coronary Syndrome X
• Characterized by 3 specific, typicalsigns as :
• Classic anginal chest pain
• ST segment depression on ECG
during stress-test
• Angiographically normal coronary
arteries without LV dysfunction
31.
Terminology ClarificationOne major association between microvascular angina and the
insulin resistance syndrome has arisen from terminological
confusion
The term syndrome X was first used in the 1970’s to refer to
a
heterogeneous group of patients with chest pain and normal
coronary angiograms.
• In the late 1980’s this concurrence of myocardial ischaemia
and normal angiograms was called microvascular angina.
The term "metabolic" syndrome X was first used in the
late 1980’s to describe a pathological insulin-resistant condition,
characterised by high prevalences of non-insulin-dependent
diabetes, hypertension, obesity, dyslipidaemia, and
cardiovascular disease.
•The term insulin resistance syndrome is now preferred by many
to refer to this pathological insulin resistant condition.
32.
Diabetes and AnginaInsulin resistance and secondary hyperinsulinemia are recognized risk
factors for development of atherosclerosis. Hyperinsulinemia (high insulin
levels in the blood) is a marker for the Insulin Resistance Syndrome.
Hyperinsulinemia results from the body’s attempt to overcome insulin
resistance by secreting more insulin from the pancreas.
Insulin Resistance Syndrome has been demonstrated in patients with angina
pectoris irrespective of detectable atherosclerosis at coronary angiograms.
A study conducted by Botker et al provided clear evidence that patients
with microvascular angina are insulin resistant, independent of body mass
index and physical fitness.
Research by Fava et al indicated that diabetic patients with unstable angina
have a higher mortality than non-diabetic patients. The presence of
diabetes is a strong risk factor for coronary artery disease and cardiac
death in elderly hemodialysis patients. Both symptomatic and silent ischemic
heart disease may occur frequently during hemodialysis because
hemodialysis simultaneously reduces coronary artery oxygen delivery while
increasing myocardial oxygen demand.
33.
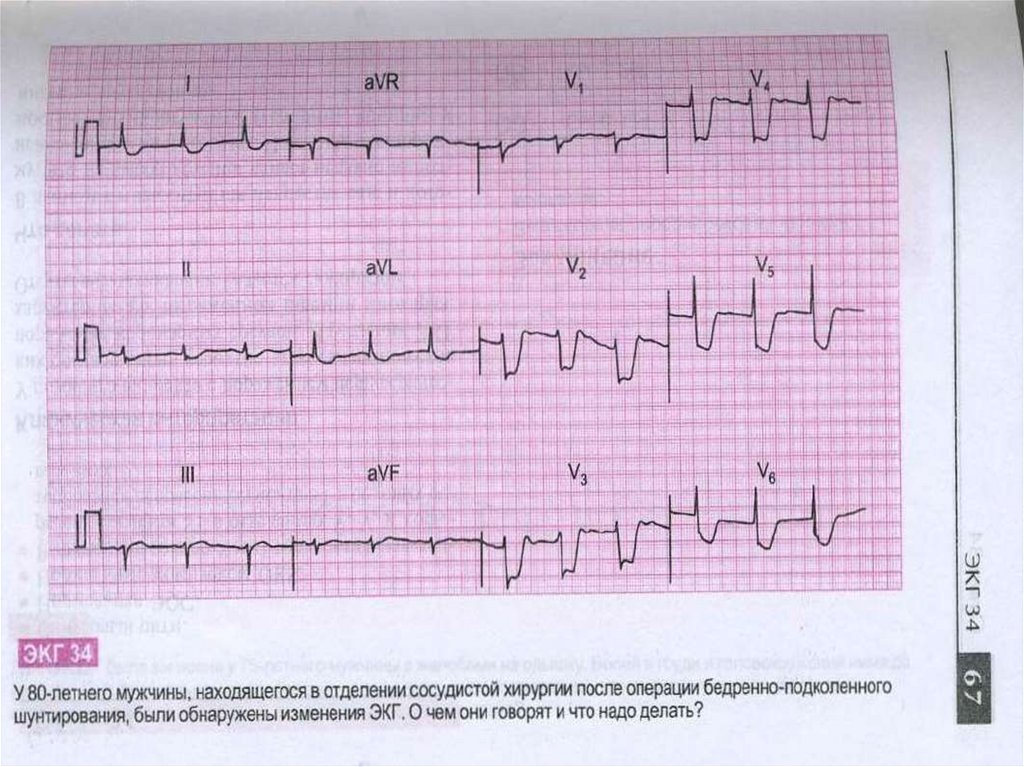
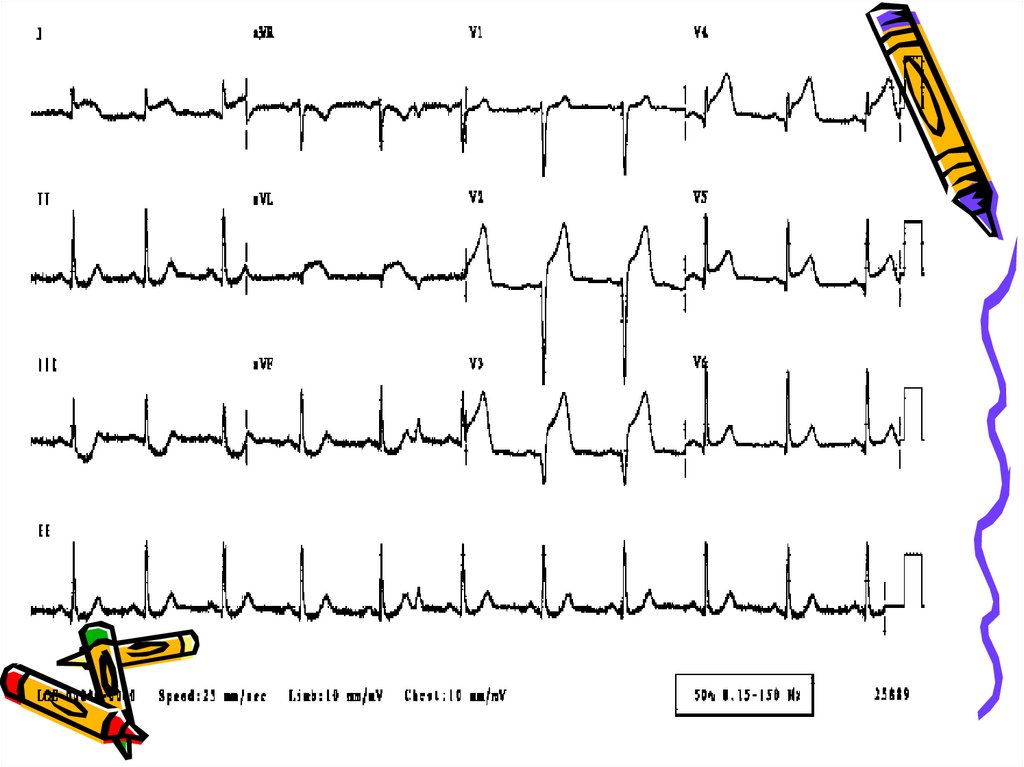
DiagnosisThe diagnosis of angina pectoris usually involves a careful
assessment and history of signs and symptoms. Diagnostic
procedures to exclude angina or establish the severity of coronary
heart disease include electrocardiogram (ECG ), a stress test, and
coronary arteriogram (or angiogram). The ECG records electrical
impulses of the heart which enables one to assess if the heart
muscle is not getting sufficient oxygen or if there are abnormal
features of the heart. A stress test is used to detect coronary
artery disease and to determine safe levels of exercise. In a
coronary arteriogram (or angiogram), x-rays are taken after a
contrast agent is injected into an artery to locate the narrowing,
occlusions, and other abnormalities of specific arteries.
There are a few conditions which mimic angina. Sources of pain
most often confused with cardiac pain are gastrointestinal
(esophageal and hiatal hernia, biliary), musculoskeletal, pulmonary,
and pericardial.
34. Laboratory investigations
• Obligatory indicators:Hb, Total Cholesterol, HDL-C, LDLC, triglycerides, glucose, AST, ALT,
creatinine (GFR)
• Additional indicators:
Cardiac troponins, thyroid function
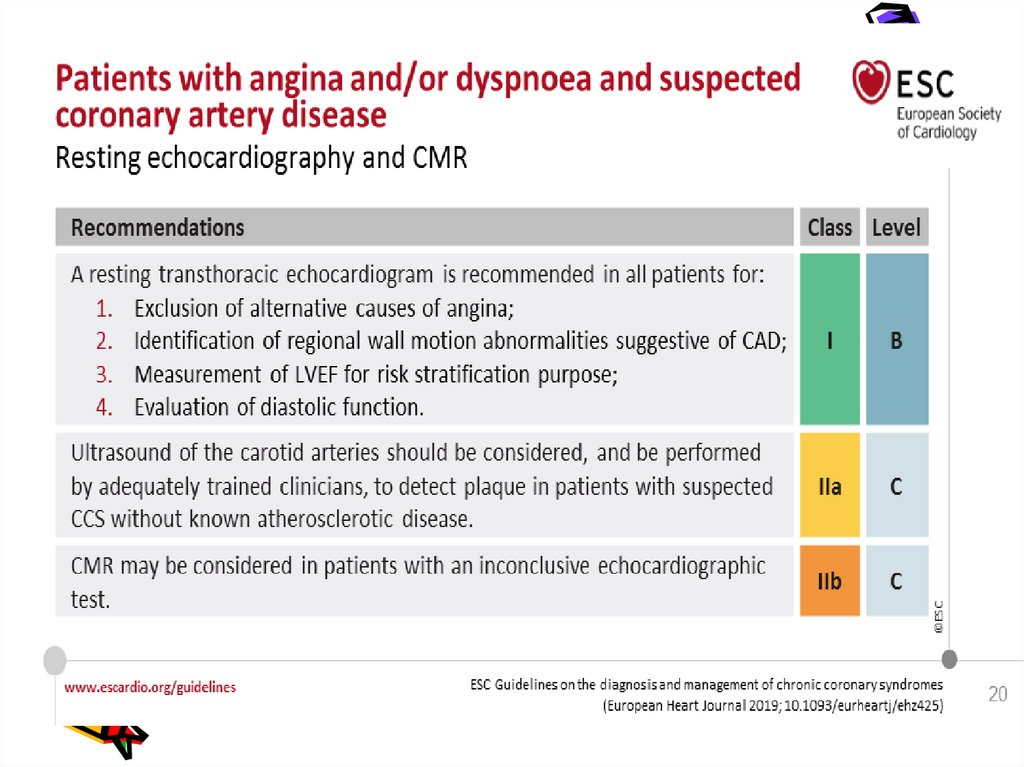
35. Investigations
• Resting ECG –reversible ST depression or
elevation with or without T-wave inversion at the
time the patient is experiencing symptoms
• Exercise ECG – stadart treadmill or bicycle
ergometer protocol. Planar or down-sloping ST
depression of 1mm or more is indicative of
ischaemia.
• Holter monitoring ECG during 24 hours
• Myocardial perfusion scanning helpful in
patients who are unable to exercise, its predictive
accuracy is higher than that of the exercise ECG.
36. Investigations
• Stress echocardiography –to identify
ischaemic segments of myocardium and areas of
infarction ( exhibit reversible defects in contractility during exercise or pharmacological stress
with a dobutamine)
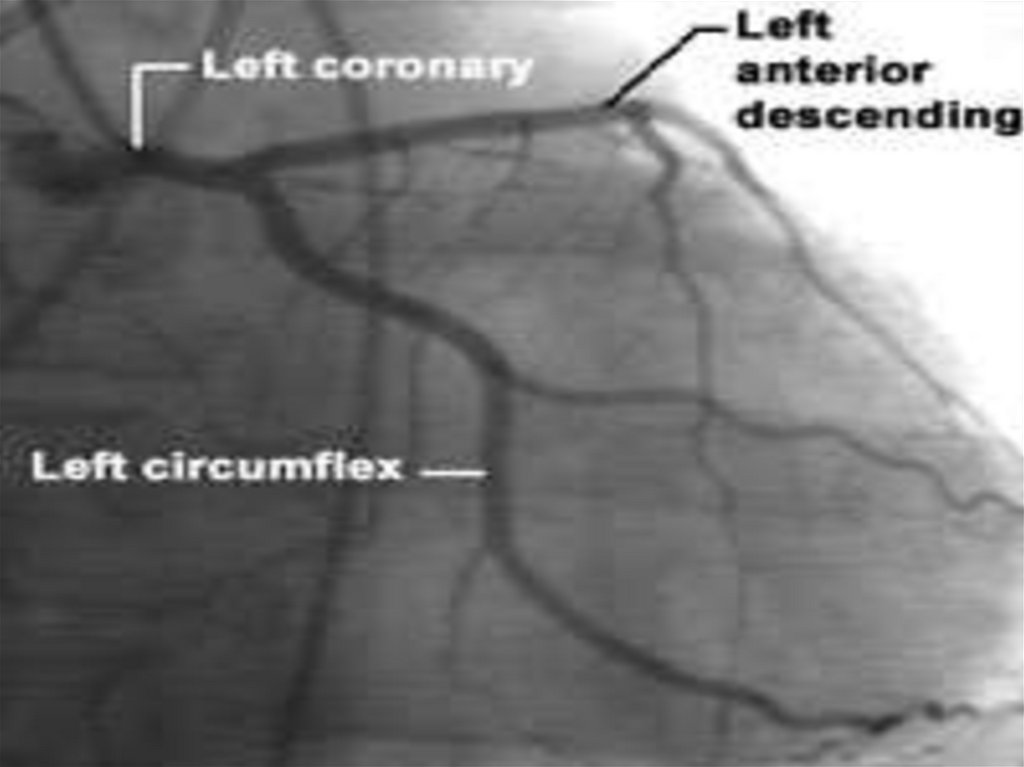
• Coronary arteriography –
provides
detailed anatomical information about the extent
and nature of coronary artery disease and is
usually performed with a view to coronary bypass
grafting or PCI. May be indicated when noninvasive tests have failed to elucidate the cause
of atypical chest pain.
37.
38.
39.
40.
41. Management
• The management of angina pectorisinvolves :
• A careful assessment of the likely extent
and severity of coronary arteri disease
• The identification and control of
significant risk factors
• The use of measures to control symptoms
• The identification of high-risk patients
and application of treatments to improve
life expectancy
42.
43.
44.
45.
46. Treatment
• Nitroglycerin is the drug most often used. It mainlyrelaxes the veins and relaxes the coronary arteries a
little. By relaxing the veins, it reduces the amount of
blood that returns to the heart and eases the heart's
workload. By relaxing the coronary arteries, it
increases the heart's blood supply.
• The heart's demand for oxygen also can be modified
with drugs that reduce blood pressure. This reduces
the heart's workload and need for oxygen. Drugs that
slow the heart rate have a similar effect. Drugs called
beta-blockers and calcium antagonists are used for
these effects. There are many different betablockers and calcium antagonists, and the specific
ones used are selected depending on the individual
characteristics of each patient.
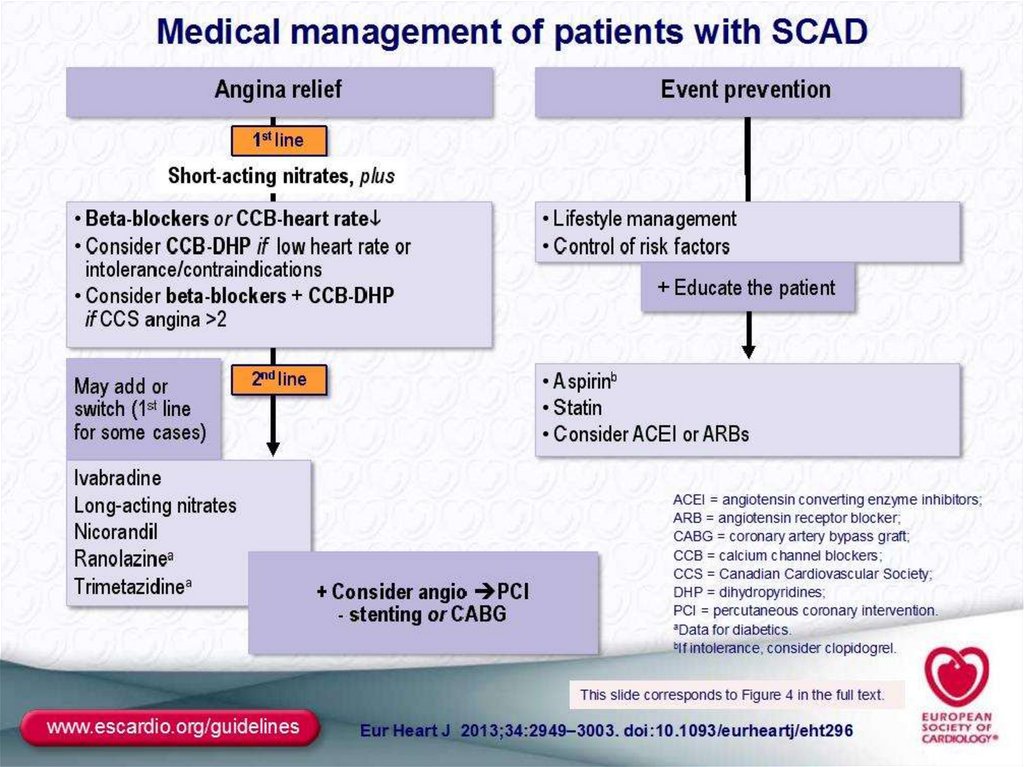
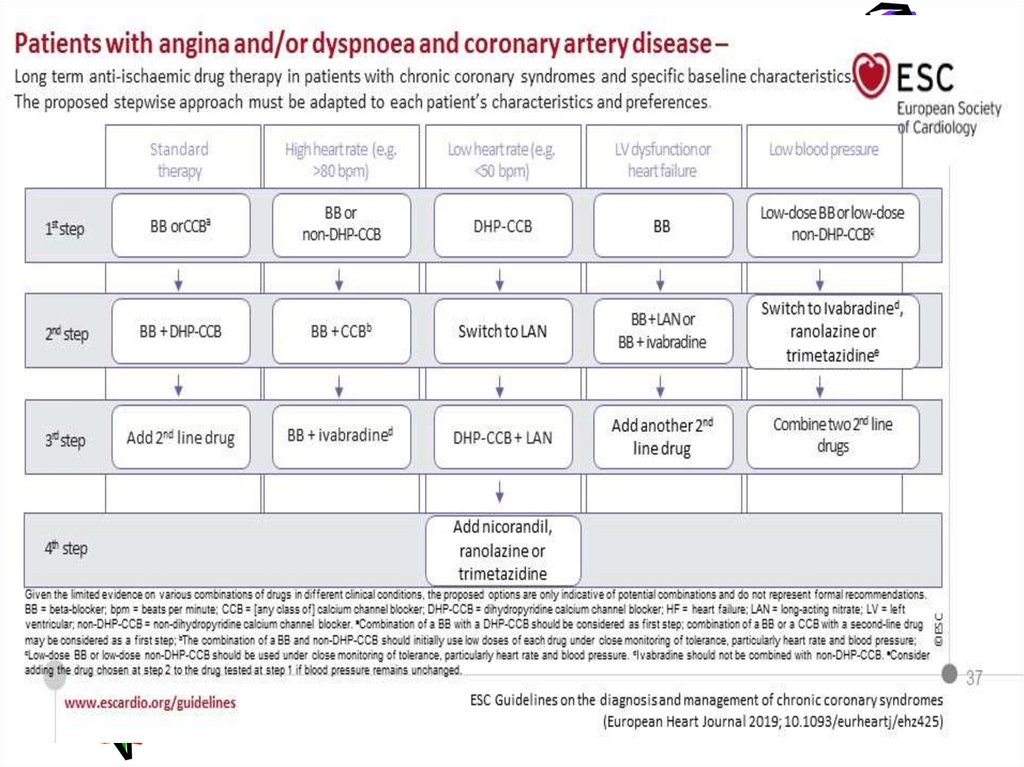
47. Anti-anginals
• - B- blockers -1st line(metoprolol,bisoprolol,nebivolol,carvedil
ol)
• - Calcium antagonists (verapamil ,
amlodipin,diltiazem if b-blockers
contraindicated)
• - Nitrates (isosorbide dinitrate,
isosorbide mononitrate )
48. Treatment
• ANTI-ANGINAL DRUG TREATMENT –GROUPS OF DRUGS ARE USED TO HELP RELIEVE OR
PREVENT THE SYMPTOMS OF ANGINA:
NITRATES, B-BLOCKERS, CALCIUM ANTAGONISTS ,
POTASSIUM CHANNEL ACTIVATORS. Angina
pectoris can be treated with drugs that affect
the blood supply to the heart muscle or the
heart's demand for oxygen or both. Drugs that
affect the blood supply are coronary vasodilators;
they cause blood vessels to relax. When this
happens, the opening inside the vessels (the
lumen) gets bigger. Then blood flow improves,
letting more oxygen and
nutrients reach the
heart muscle.
49. Drugs,which improve prognosis
• - Antiplatelet drugs (aspirin,clopidogrel )• - Statins (lovastatin,simvastatin, atorvastatin,rosuvastatin )
• - B-blockers
(atenolol,metaprolol,bisoprolol,nebivolol,
• carvedilol )
• - ACE – inhibitors
(enalapril,lisinopril,perindopril,ramipril
50. Treatment Controlling the risk factors for angina pectoris, such as high blood pressure, cigarette smoking, high cholesterol
levels, and excess weight is an essentialpart of treatment.
ANTIPLATELET THERAPY -low-dose
aspirin(75-150mg) reduces the risk of
adverse events such as MI and should
be prescribed for all patients.
Clopidogrel (75mg) is an equally
effective agent that can be prescribed
if aspirin causes dyspepsia or other
side-effects.
51.
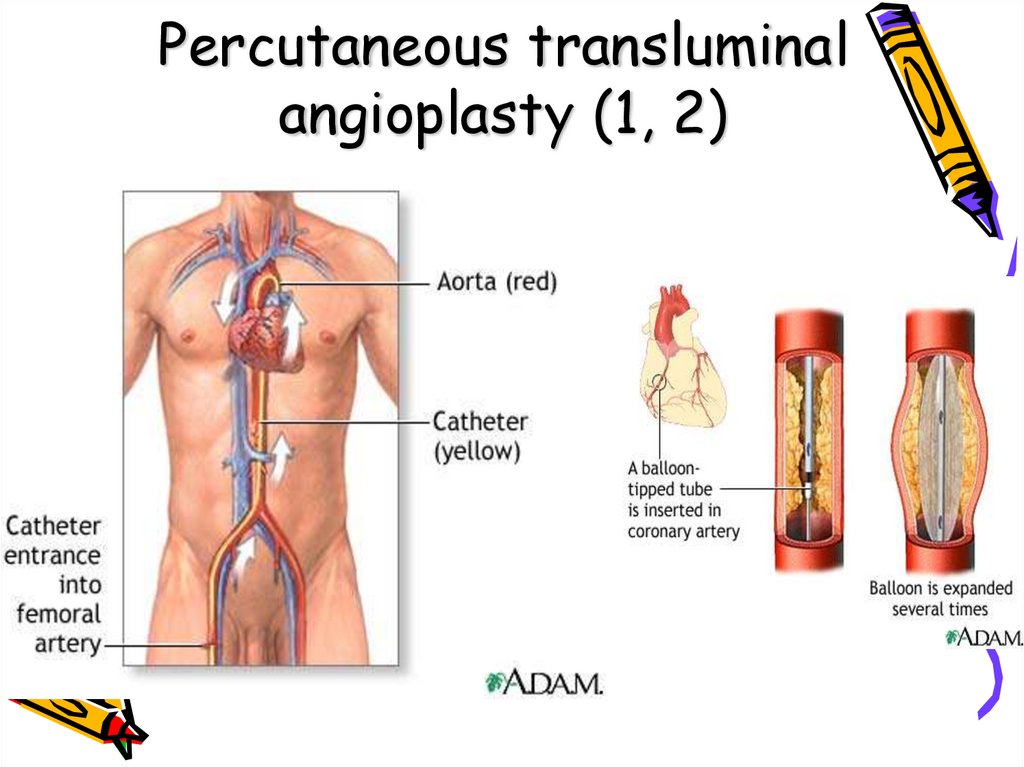
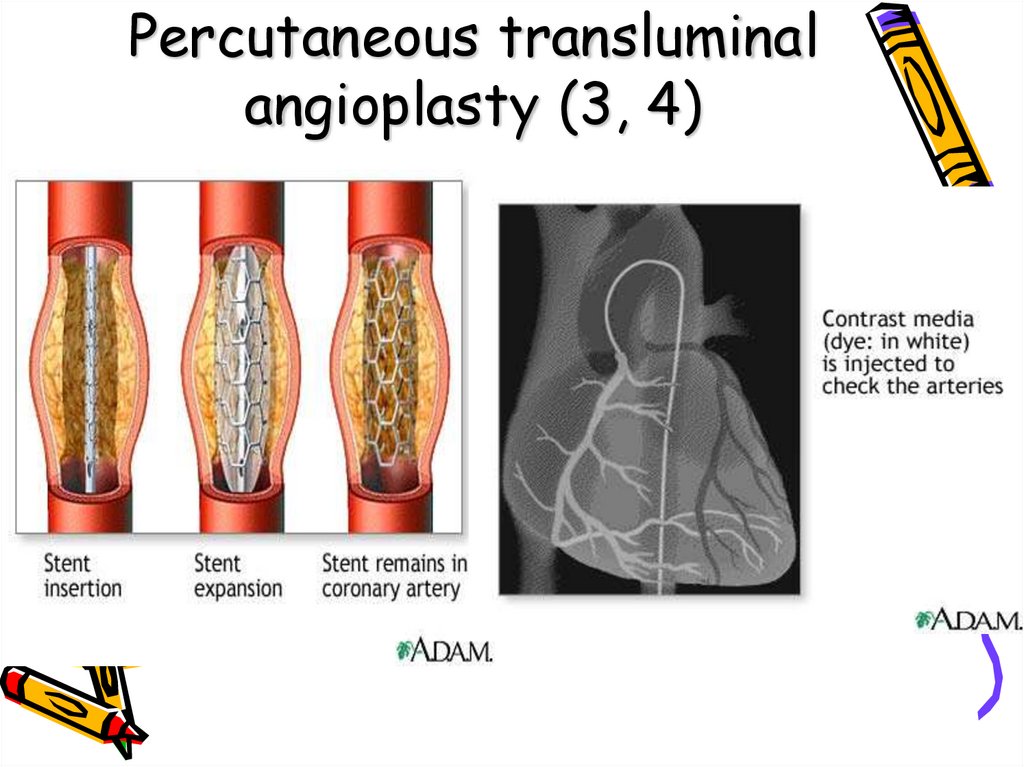
What procedures are used to treat angina?Invasive techniques that improve the heart and the heart's blood
supply also may be used. One of these is percutaneous transluminal
coronary angioplasty. It's also known as PCI, PTCA, angioplasty,
balloon dilation or balloon angioplasty. In it, a thin, flexible plastic
tube (catheter) with a balloon is inserted into an artery and
advanced to the blockage. Then the balloon is inflated, squeezing
open the fatty plaque deposit. Then the balloon is deflated and the
catheter is withdrawn. Often a stent is also placed to hold the
artery open. Two additional techniques used to reduce coronary
blockages are laser angioplasty and atherectomy. In laser
angioplasty, a catheter with a laser on its tip is used to open the
blockage. In atherectomy, a catheter has a rotating shaver on its
tip to cut away the plaque. These techniques also may be
accompanied by stent placement.
52.
Coronary artery bypass graft surgery is also used. In it, a bloodvessel is used to route blood around the blocked part of the artery,
forming a kind of detour. Before performing any of these
procedures, a doctor must find the blocked part(s) of the coronary
arteries. This requires coronary arteriography, which is done during
cardiac catheterization. In this procedure a doctor guides a
catheter through an artery in the arm or leg and into the coronary
arteries. Then the doctor injects a liquid dye through the catheter.
High-speed X-ray movies record the course of the dye as it flows
through the arteries. Doctors can identify blockages by tracing the
flow. An evaluation of how the heart works also can be done during
cardiac catheterization. Other tests can be used to evaluate how
well the heart works, and may be done before or after a heart
attack.
53.
How is variant angina or Prinzmetal's anginatreated?
Calcium antagonists are extremely effective in
preventing the coronary spasm of variant or
Prinzmetal's angina. These drugs, along with nitrates,
are the mainstays of treatment. Prinzmetal's angina
tends to be cyclic, appearing for a time, then going
away. Because of this, after six to 12 months of
treatment, the calcium antagonists may be gradually
reduced. In some cases PTCA or surgery are used
when blockages exist along with spasm.
54.
Medical TreatmentIf you have come to the hospital emergency
department, you may be sent to another care area for
further testing, treatment, or observation. On the
basis of your provider's preliminary diagnosis, you may
be sent to the following units:
•An observation unit pending test results or further
testing
•A cardiac care unit
•A cardiac catheterization unit
•The operating room for emergency cardiac bypass
surgery
55. Medical Treatment
• Regardless of where you are sent, several basictreatments may be started. Which are given to
you depends on the severity of your symptoms and
the underlying disease.
• You will have at least one intravenous line started.
This line is used to give medication or fluids.
• You will probably be given an aspirin if you haven't
already taken one.
• You may be given oxygen through a face mask or a
tube in your nose. This will help you feel better if
you are having trouble breathing or feeling
uncomfortably short of breath by raising the
oxygen content of your blood.
56.
Medical TreatmentTreatment will depend on the severity of symptoms,
severity of the underlying disease, and extent of damage
to the heart muscle, if any.
•Simple rest and observation, an aspirin, breathing
oxygen, and sublingual nitroglycerin may be all that you
need, if it is only angina.
•You may be given medication to reduce anxiety or to
treat pain.
57. Medical Treatment
• You may be given medication to lower bloodpressure or heart rate. Beta blockers,
Angiotensin Converting Enzyme Inhibitors (ACE
inhibitors), and cholesterol- lowering drugs
(statins) are commonly given if the chances of a
heart attack are likely.
• You may be given medication to reduce risk of
having a blood clot or to prevent further clotting.
• If the health care provider believes chest pain
actually represents a heart attack, you may be
given a powerful "clot-buster" medication called a
fibrinolytic.
58. Metabolic therapy
-
Trimetazidine (preductal)
Riboxin
Mildronate (vasonate)
Tiotriozaline
Vitamins
Antioxidantes
59.
Medical TreatmentAfter reviewing your immediate test results,
the hospital health care provider will make a
decision about where you should be for the
next hours and days.
•If you are feeling better, your condition is
stable, and this was only an angina attack, you
may be allowed to go home. You may be given
medications to take. You will be told to follow
up with your primary care provider within the
next day or two.
60. Medical Treatment
• If you keep having symptoms or yourcondition is unstable, you will be
admitted to the hospital. You will
probably undergo further tests and
possibly coronary angiography,
coronary artery angioplasty, or even
coronary artery bypass surgery, if all
your arteries are critically blocked.
61.
INVASIVE TREATMENTAngioplasty is a treatment used for people whose
angina does not get better with medication and/or who
are at high risk of having a heart attack.
•Before angioplasty can be done, the area(s) of
coronary artery narrowing is located with coronary
arteriography.
•A thin plastic tube called a catheter is inserted into
an artery in the arm or groin with local sedation. The
catheter has a tiny balloon attached to the end.
62. INVASIVE TREATMENT
• The catheter is threaded through the arteriesand into the artery where the narrowing is.
• The balloon is inflated, opening up the narrowing.
• This is not a permanent solution for most people.
Many require placement of a "stent," a small metal
sleeve that is placed in the narrowed artery. The
stent holds the artery open.








 Медицина
Медицина