Похожие презентации:
Diphtheria
1.
DIPHTHERIA?!2.
DIPHTHERIA– is an acute infectious disease caused by the toxicogenic strains
of Corynobacterium diphteriae, anthroponosis, characterizes
by a development of fibrinous inflammation in the place
of entry and remote effects resulting from toxin,
which affects the heart, kidney and peripheral nerves.
Diphthera (greek) – means “membrane” or “leathery skin”
3.
Historical reference:As the disease came to Europe from the East, it has
long been called the “Egyptian plague” or “Syrian ulcer”.
Some manifestations of the disease in the initial stage
of its development called also “throat angina” (pectoris) or
“throat plague”.
In the 18th century the disease began to be called
“croup”.
A detailed description of the clinical disease was given
in 1826 by French physician Pierre Bretonne. He first
pointed relationship of lesions of the larynx with croup (its
inflammatory narrowing) and called the disease
“diphtherit”.
Later in 1846 internist Trousseau suggested the term
“diphtheria”, which applies now
4.
1883 - Klebs E. T. discovered the pathogen in diphthericfilms and described it;
1884 - Loeffler E. identified the causative agent in culture
and described its properties;
1888 - Roux Е.P.P., Yersin А.E., Behring E.А. secreted
exotoxin and antitoxin (beginning of specific therapy
of diphtheria)
1923 - Glen and Ramon Gaston secreted anatoxin (it was
beginning of massive immunization against diphtheria)
LOEFFLER E.
BRETANNO
TRUSSO
5.
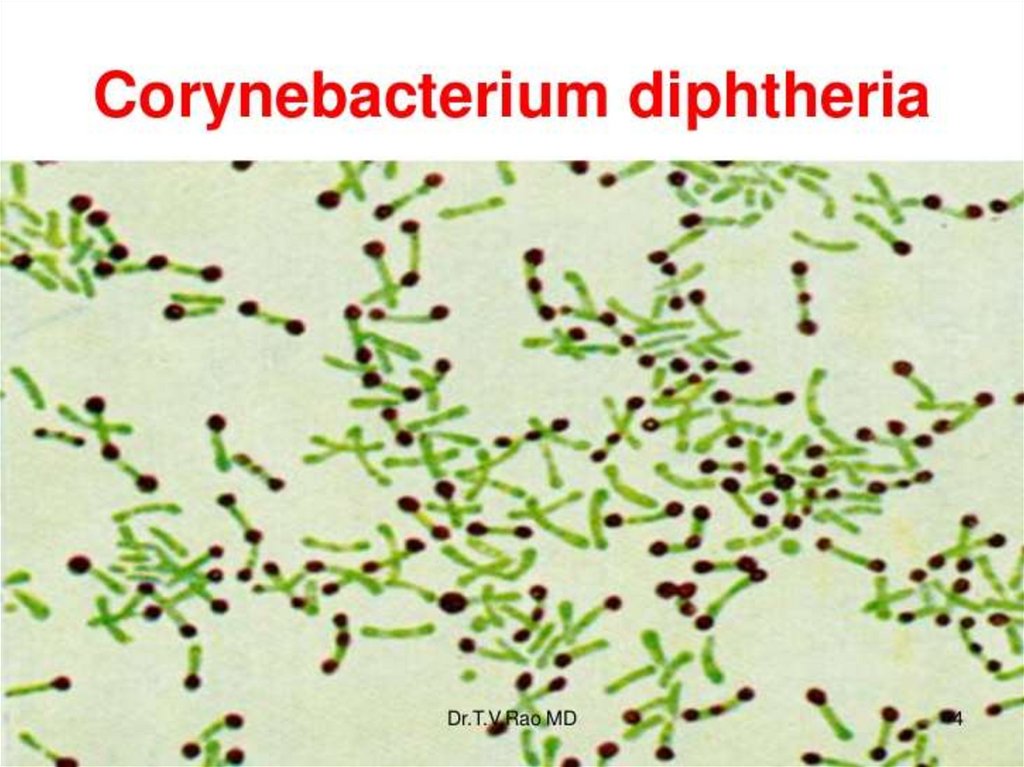
ETIOLOGYCorynobacterium (Greek, korune, “club” or “mace”,
bacterion, “small rod”) consists of a diverse group of
bacteria including animal and plant pathogens, as well as
saprophytes.
Some Corynobacteria are part of the normal flora of
humans.
Corynobacterium diphteriae (C.d.)
- Gram (+) thin rod;
- club-shaped (metachromatic grains of volutin on the end
of rod);
- Nonmotile, nonsporulating;
- Has no capsule;
- Selective aerobe;
- Large (1-12 × 0.3-0.8 microns);
6.
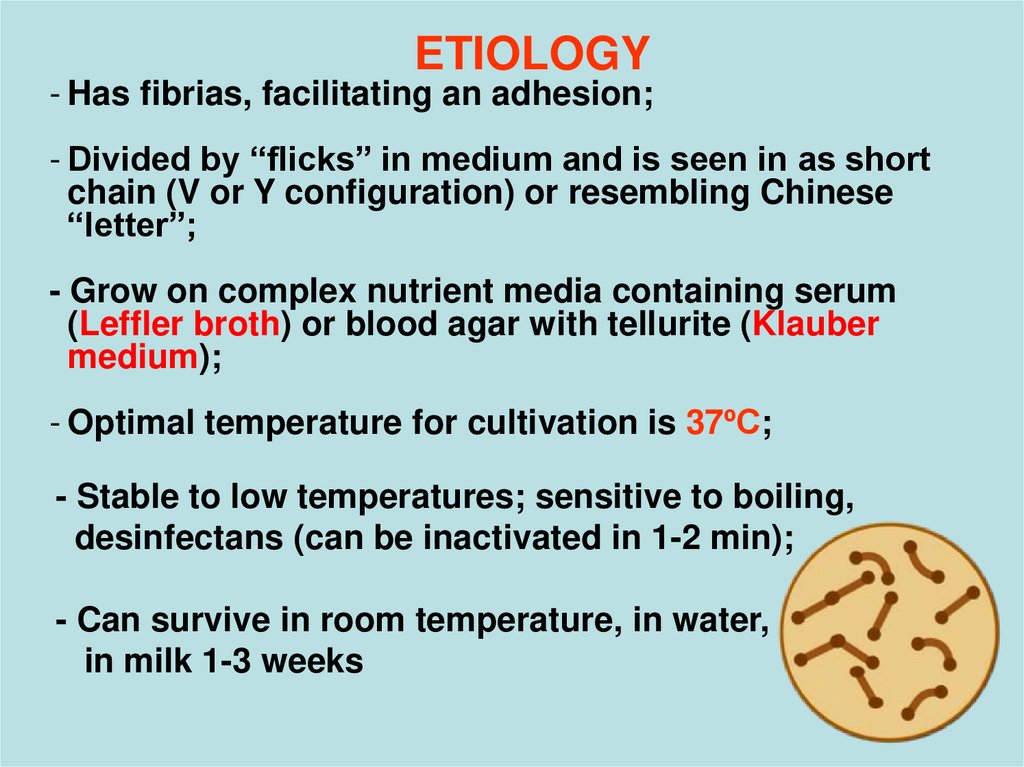
ETIOLOGY- Has fibrias, facilitating an adhesion;
- Divided by “flicks” in medium and is seen in as short
chain (V or Y configuration) or resembling Chinese
“letter”;
- Grow on complex nutrient media containing serum
(Leffler broth) or blood agar with tellurite (Klauber
medium);
- Optimal temperature for cultivation is 37ºС;
- Stable to low temperatures; sensitive to boiling,
desinfectans (can be inactivated in 1-2 min);
- Can survive in room temperature, in water,
in milk 1-3 weeks
7. - GRAVIS (R-form) - causes the most severe forms of the disease; - MITIS (S-form) - causes disease in a mild form - INTERMEDIUS
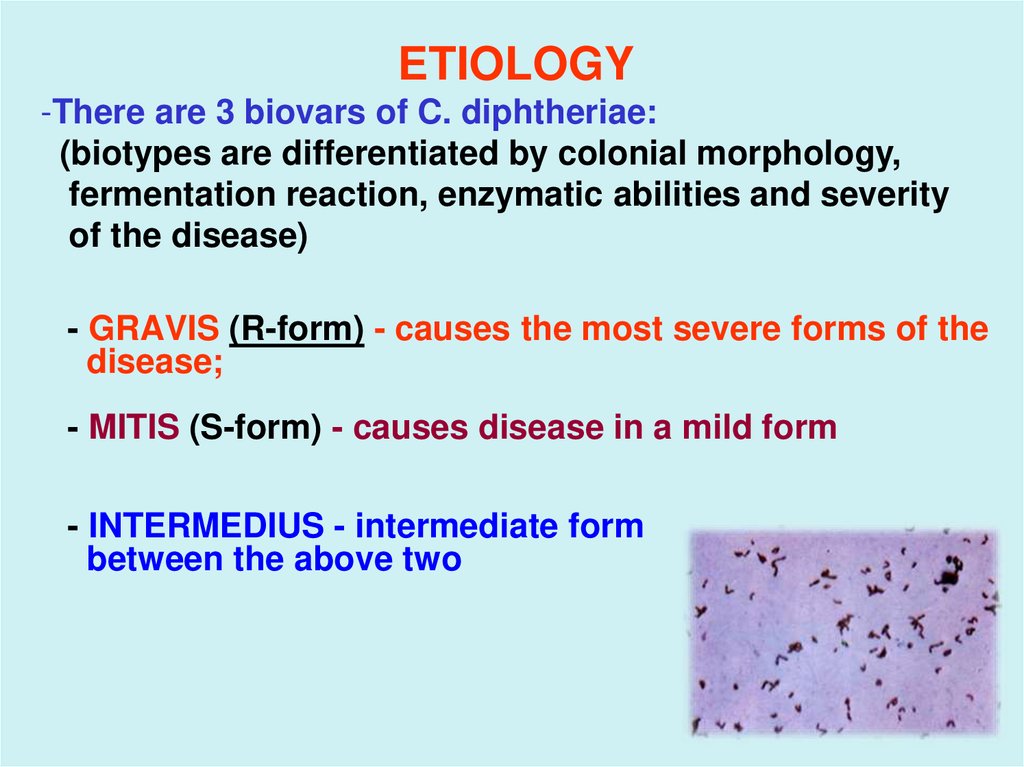
ETIOLOGY-There are 3 biovars of C. diphtheriae:
(biotypes are differentiated by colonial morphology,
fermentation reaction, enzymatic abilities and severity
of the disease)
- GRAVIS (R-form) - causes the most severe forms of the
disease;
- MITIS (S-form) - causes disease in a mild form
- INTERMEDIUS - intermediate form
between the above two
8.
9.
ETIOLOGY- Produces exotoxin
Toxigenicity is depended on the presence
of the tox+ gene, carried by a lysogenic
bacteriophage;
Cases of non-toxigenic strain of C.d. have been documented.
- Produces aggressive enzymes –
different active bioligical substances
(hyaluronidase, neurominidase, fibrinоlysin, hemolysin,
necrotiс and hydropic factors) that promote the
action of the diphterial toxin and spreding of C.b.
10.
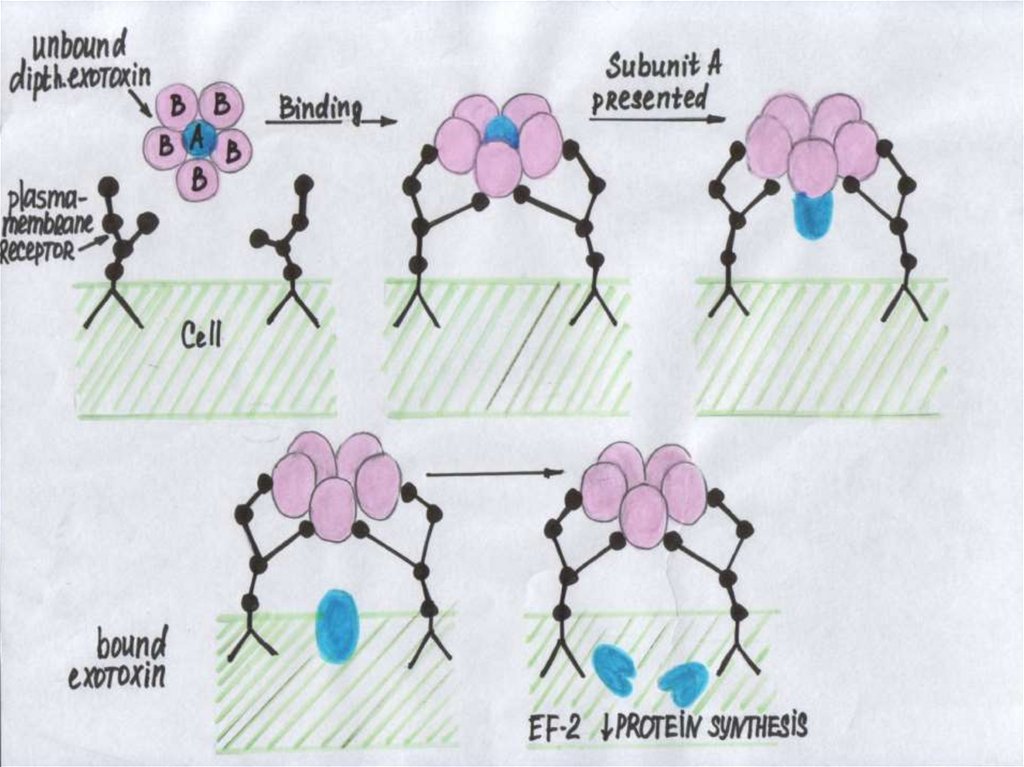
DIFTERIAL TOXIN- is polypeptide composed of 2 joined segments (A and B);
- A - is actually a toxin that inactivates RNA translocase and
inhibits protein synthesis in the cell with a subsequent death;
- B - recognizes the target-cells, binds to their receptors
and facilitate the entry part A;
-Toxin is in unbound condition in the blood during 10 min and
next 30-40 min fixed on the surface of the target cells;
- Then diphterial toxin penetrates the cells, it couldnʹt be bound
by
antitoxin ( that why should be early administration of the
antitoxin!!!).
Donʹt be slow in case of diphteria!
The diphterial toxin is on the 3-d place
by action (1-st – botulism, 2-d – tetanus).
11.
12.
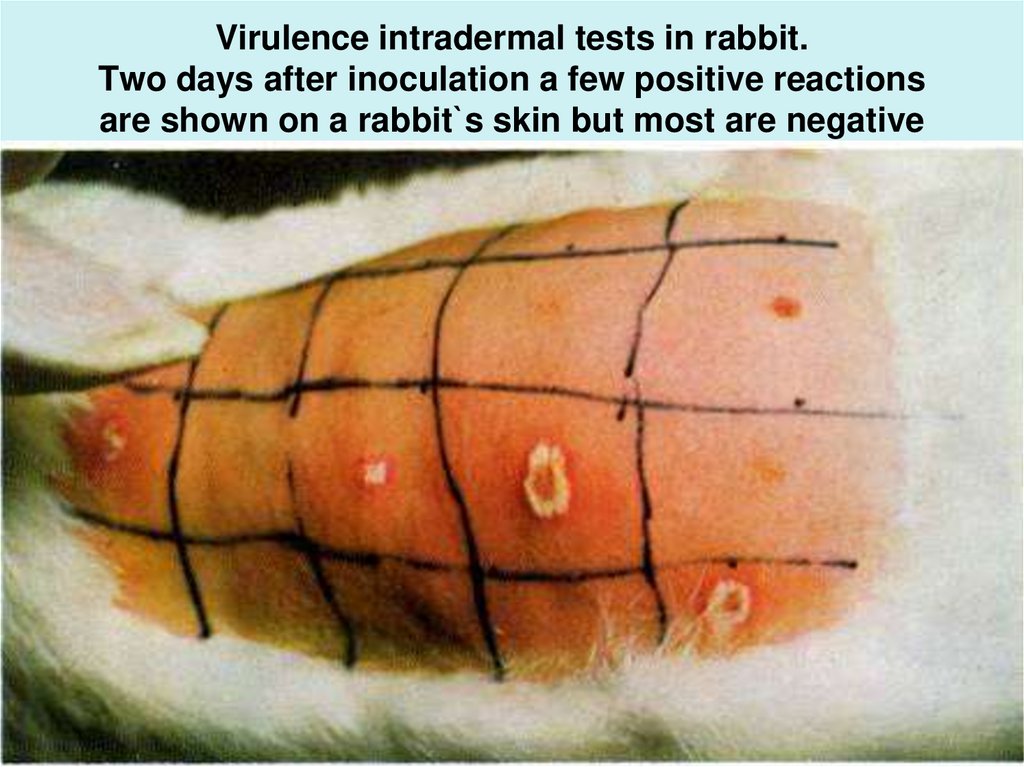
13. Mode of action of the diphtheria toxin
14. Virulence intradermal tests in rabbit. Two days after inoculation a few positive reactions are shown on a rabbit`s skin but
most are negative15.
By intensity:1. Sick persons
2. Convalescents
3. Bacteriocarrier
EPIDEMIOLOGY
Source of infection:
By epidemiologic significance:
1. Bacteriocarrier
2. Convalescents
3. Sick persons
Sanation of convalescents
are completed in 15 - 20 days,
but sometimes 90 days.
The frequency of a carrier
state in population is 1-10 %
16.
17.
Mode of transmission:- Aerogenic mechanism
(C.d. spreads via respiratory droplets, contact with
nasopharingeal secretions)
- contact and alimentary mode (less often)
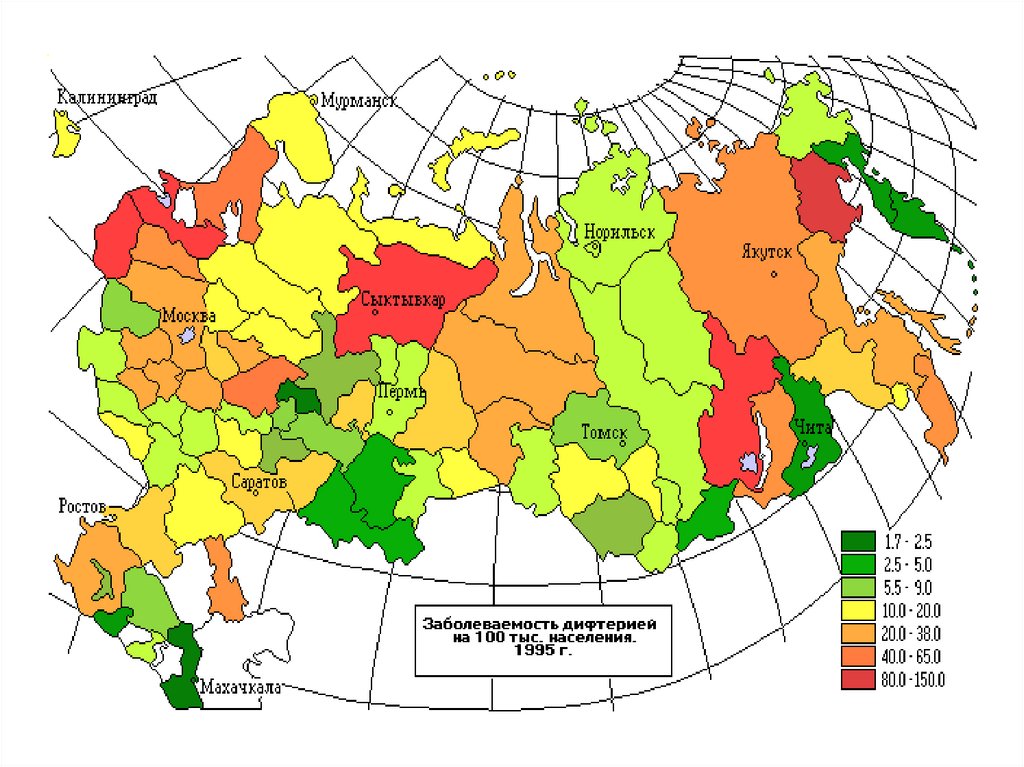
- Peak of incidence - in autumn-winter period
- Periodicity of outbreaks is every 5 - 7 years
- No racial, sex predilection
- Before immunization was introduced, D. was a primarily infection of children
affecting populations younger than 12 years.
- But now, D. shifted into the adult population. This trend is increased due to
uncomplite immune status or total inhibition of it
(alcohol or immunocompromised drugs).
-D. is a controllable disease now, but the scheduled vaccination of children led to
increased morbidity of the diseases among the adults!!!
18.
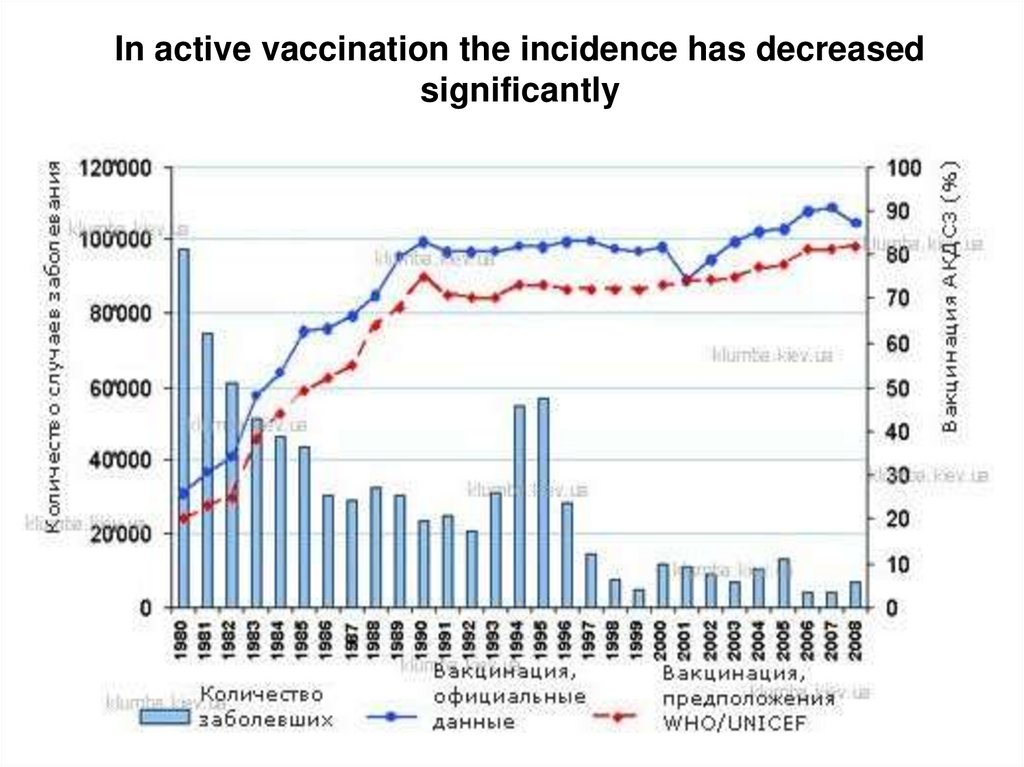
In active vaccination the incidence has decreasedsignificantly
19.
Increased risk for diphtheria infection includesthe following factors:
1. Incomplete or absent immunization (in adult population).
In some cases immunity does not prevent infection
but lessens the severity of the disease;
2. Low public immunity;
3. Travel to endemic areas with current epidemics;
4. Immunocompromised state;
5. Low socioeconomic status, large-scale population
movements, poor healthcare system infrastructure and
overcrowding
20.
PATHOGENESIS1. In place of the penetration ( mucous membranes or skin)
bacteria intensively multiplies and produces exotoxin
that is accompanied by hyperemia, edema and vascular
congestion with increased permeability of small blood
vessels and epithelial necrosis;
This leads to local damage
2. Fibrinogen of serum leaves the capillaries, reacts with
thromboplastin of the necrotic epithelium) a transforms
into the insoluble fibrin (diphteric membranes);
- Fibrin tightly holding a fibrinous film on the surface
of the mucosa.
- Membranes increase and thicken up to 5 – 6 days
of illness !!!
21.
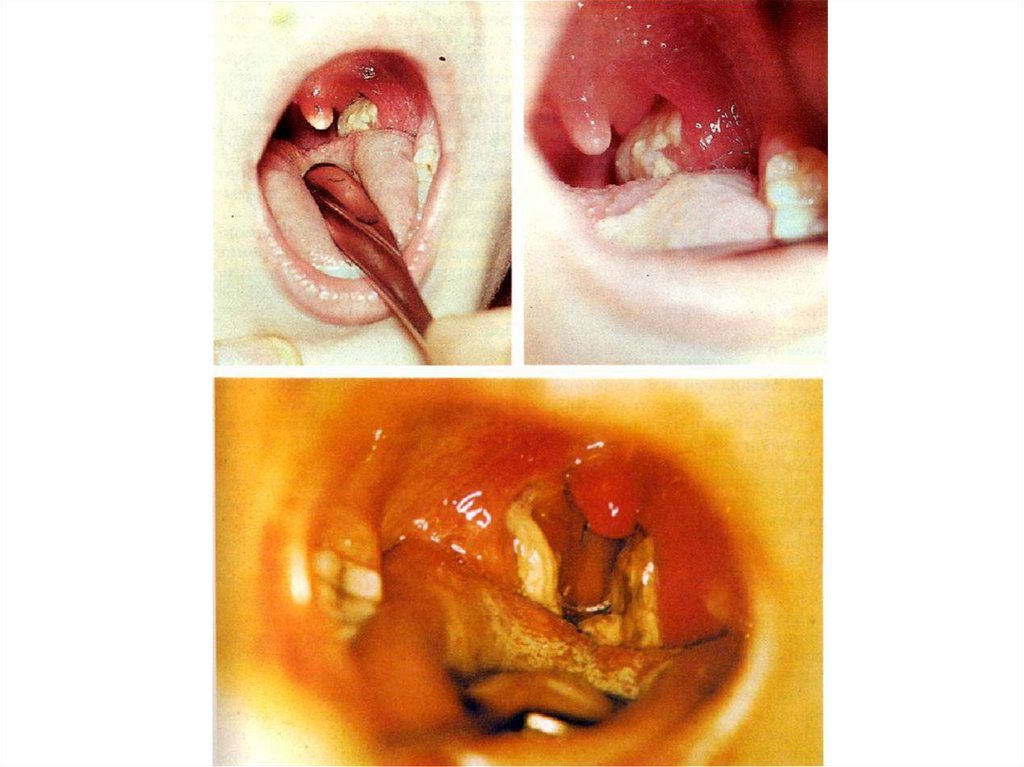
- Membrane is thick, leathery, grey-white andcomposed of bacteria, necrotic epithelium,
phagocytes and fibrin;
- It is firmly adherent to the underlying tissues,
bleeding follows its forsible removing.
- Has tendency to extend to another organs.
- Can detach in 5-6 days.
3. C. d. remains under the film, but exotoxin invades
the regional lymph nodes and subcutaneous tissue
(lymphadenitis and edema of the subcutaneous
layer) and bloodstream, fixes on the target cells
with their subsequent toxic and allergic lesions:
22.
- the heart – the myocardium and conductingsystem;
- nervous system - demyelination of
nerve fibers (paresis, paralysis and
lesion of the peripheral
sympathetic ganglia);
- adrenal glands - hemorrhage,
tissue necrosis;
- kidneys – symptoms of nephrosis
23. The target organs for C. diphtheria
24.
4. Cord - factor С.d. takes certain role in pathogenesis ofdiphtheria, inhibits phosphorylation and tissue
respiration
5. Recovery after the toxic damage is in 4- 5 weeks to
6 months if the patient survives
6. Disease forms antitoxic and antibacterial immunity
but short-term. The disease can repeat!
25.
CLASSIFICATION of DIPHTHERIA :1. Localization of the process:
- Stomatopharyngeal diphtheria A 36.0
- Nasal diphtheria
A 36.1
- Laryngeal diphtheria
A 36.2
- Cutaneous diphtheria
A 36.3
- diphtheria of other localization
A 36 8
- diphtheria hypothetical
(unspecified)
A 36.9
26.
2. Spreading of the process:- Localized (if membranes are localized at the tonsils)
- Diffuse (if membranes extend into contiguous regions)
- Combined (if membranes are localized on the different anatomic regions)
3. Degree of severity:
- Bacteriocarrier
-Subclinical
-Mild
-Moderate
-Severe
-Hypertoxic
4. Character of local inflammation:
- catarral
- insular-like («island»)
- membraneous
5. Complication of diphtheria (TIS, myocarditis, neuritis ets.)
27.
CLINICS1. Incubation period is 2 to 10 days
Carrier state of С.d. (usually asymptomatic) formes after:
- the disease (convalescent carrier)
- in healthy persons (1 - 10 % in population ).
No increasing level of antidiphtherical antibodies in blood.
Carrier stage revealed only by bacteriologic detection in
smears.
Carriage С.d. may be:
- Short-term
- till 2 weeks
- Moderate duration - 2 - 4 weeks
- Lingering
- more than 4 weeks
- Chronic
- more than 6 months
28.
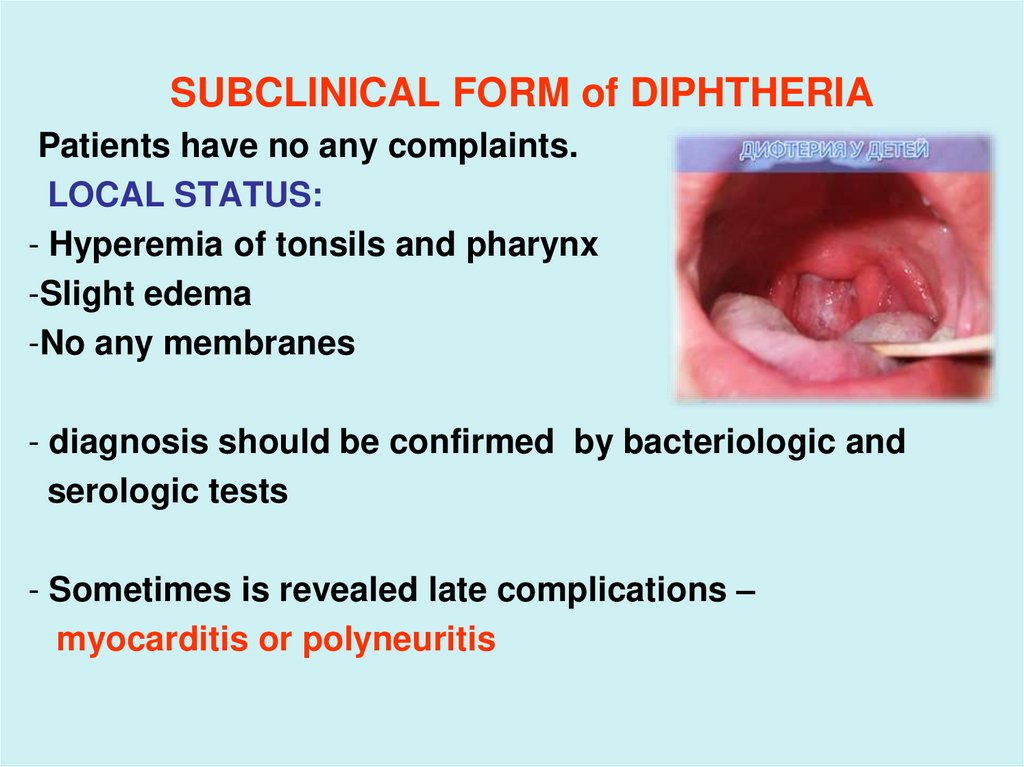
SUBCLINICAL FORM of DIPHTHERIAPatients have no any complaints.
LOCAL STATUS:
- Hyperemia of tonsils and pharynx
-Slight edema
-No any membranes
- diagnosis should be confirmed by bacteriologic and
serologic tests
- Sometimes is revealed late complications –
myocarditis or polyneuritis
29.
DIPHTHERIA of TONSILS and PHARYNXThe mild form of disease:
- mild weakness with normal BP, normal or
subfebrile temperature
LOCAL STATUS:
- hyperemia and edema of tonsils and mucous membranes;
- tonsils are covered with spots of grey or with exudates
(insula-form). These spots often form pseudomembranes
(membranouse-form)
- increased and slight painfull submandibular and cervical
lymph nodes
- often confuses with tonsillitis, pharyngitis , ARVD
30.
31.
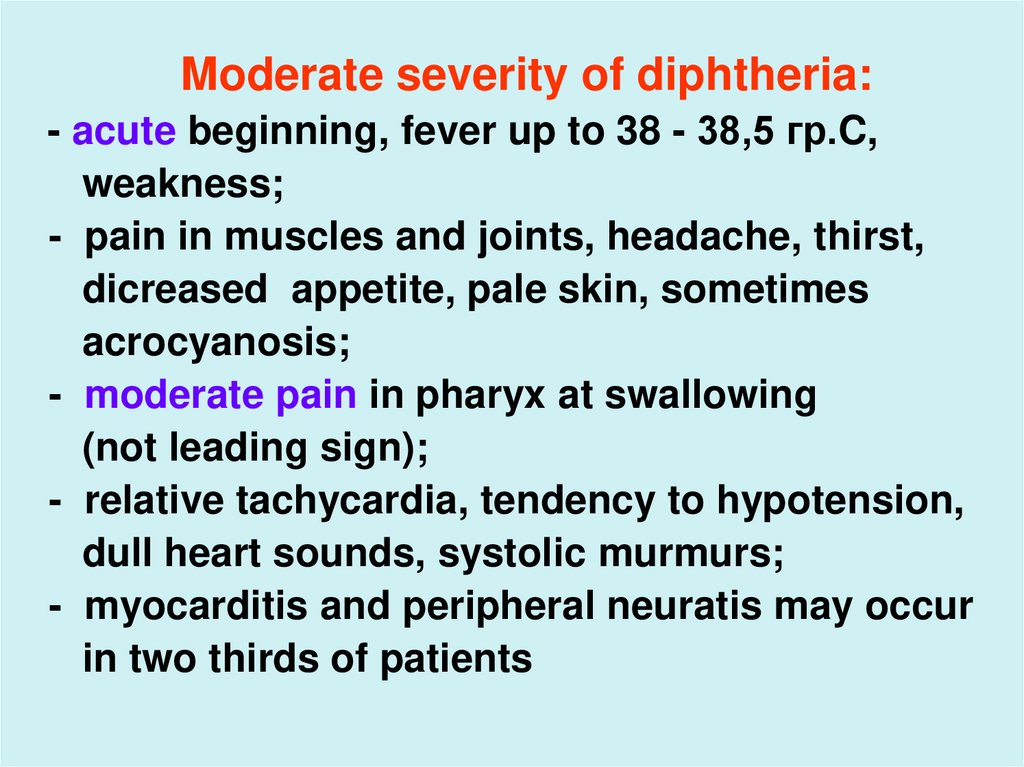
Moderate severity of diphtheria:- acute beginning, fever up to 38 - 38,5 гр.C,
weakness;
- pain in muscles and joints, headache, thirst,
dicreased appetite, pale skin, sometimes
acrocyanosis;
- moderate pain in pharyx at swallowing
(not leading sign);
- relative tachycardia, tendency to hypotension,
dull heart sounds, systolic murmurs;
- myocarditis and peripheral neuratis may occur
in two thirds of patients
32.
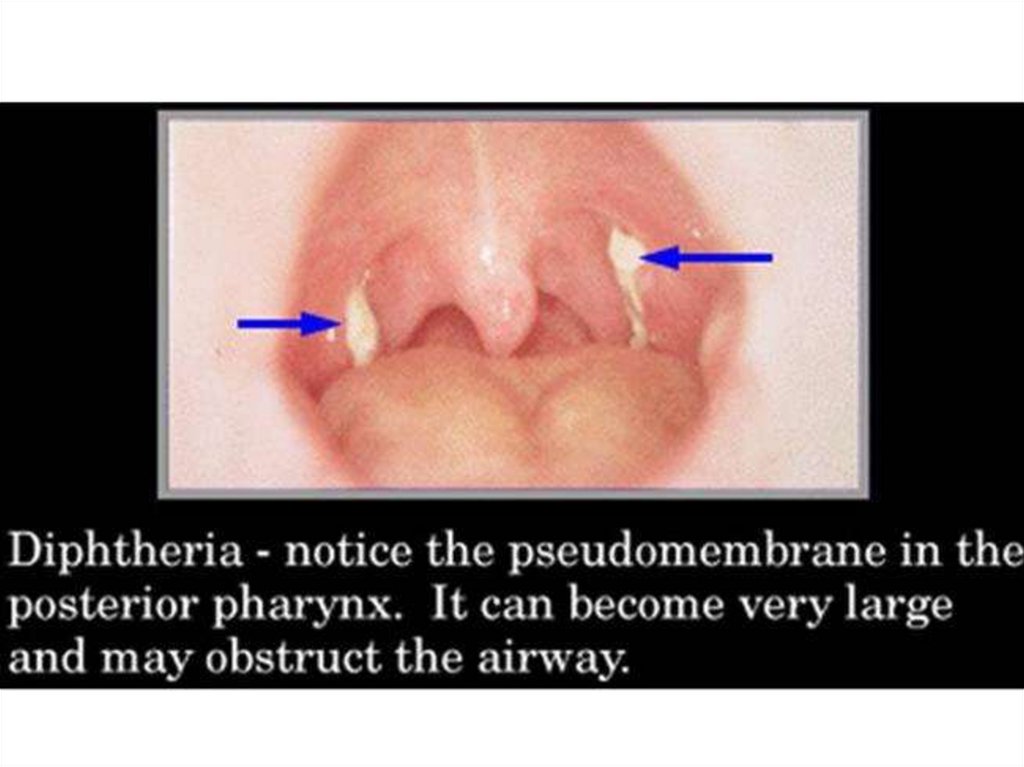
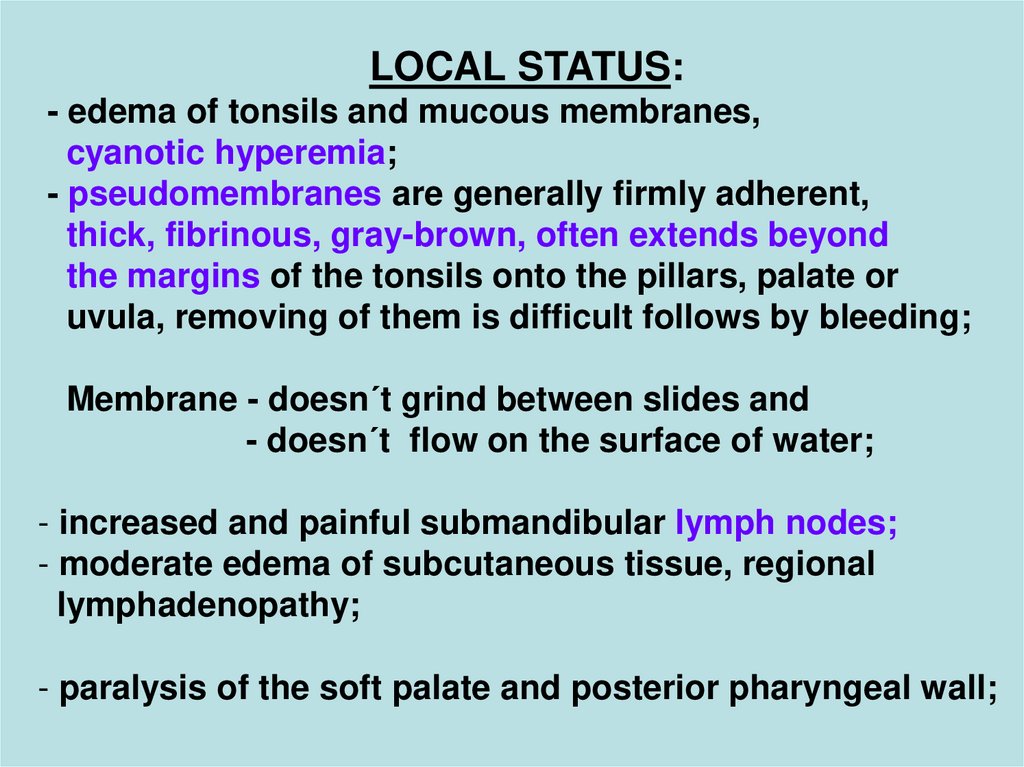
LOCAL STATUS:- edema of tonsils and mucous membranes,
cyanotic hyperemia;
- pseudomembranes are generally firmly adherent,
thick, fibrinous, gray-brown, often extends beyond
the margins of the tonsils onto the pillars, palate or
uvula, removing of them is difficult follows by bleeding;
Membrane - doesnʹt grind between slides and
- doesnʹt flow on the surface of water;
- increased and painful submandibular lymph nodes;
- moderate edema of subcutaneous tissue, regional
lymphadenopathy;
- paralysis of the soft palate and posterior pharyngeal wall;
33.
34.
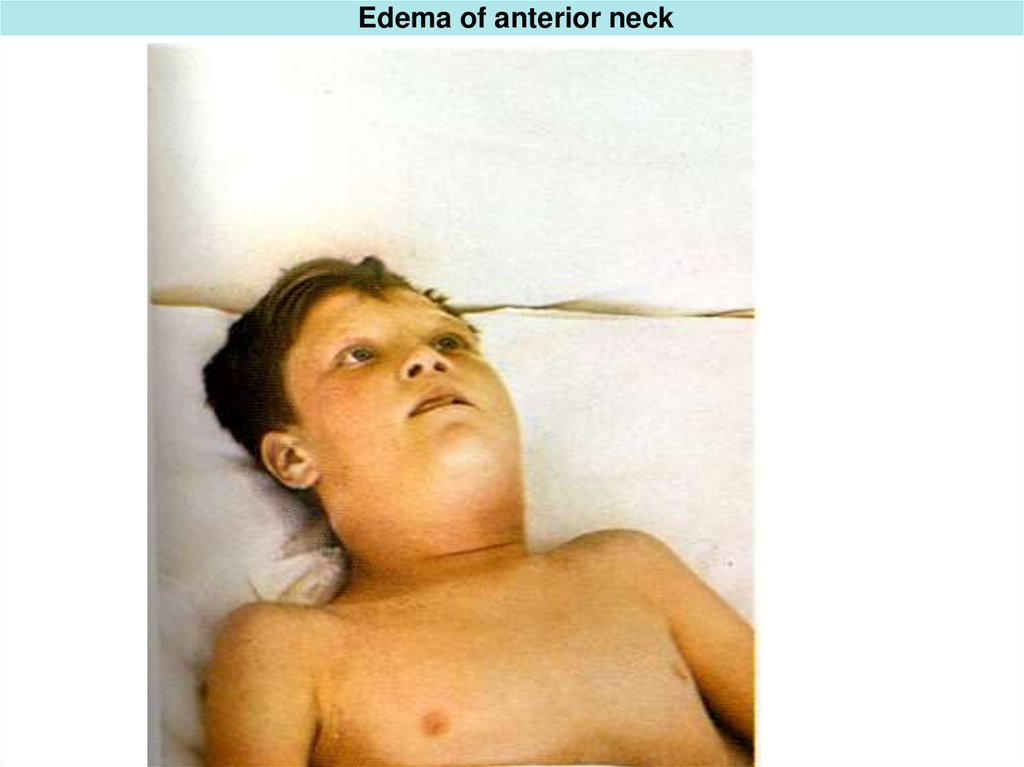
35. Edema of anterior neck
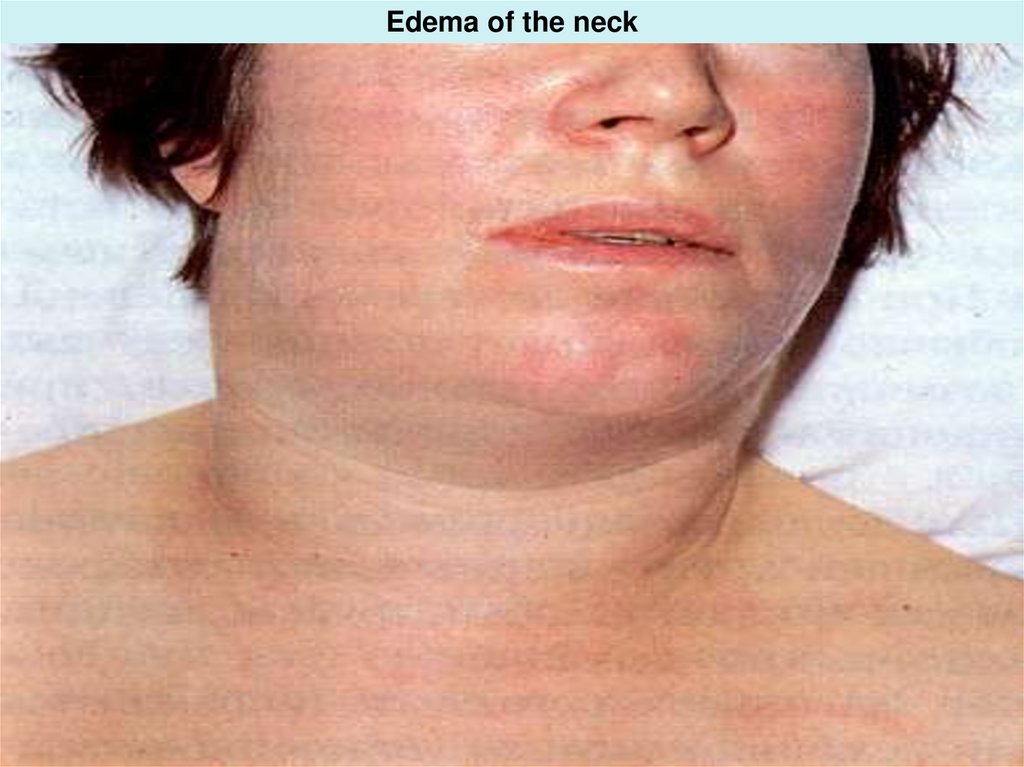
36. Edema of the neck
37.
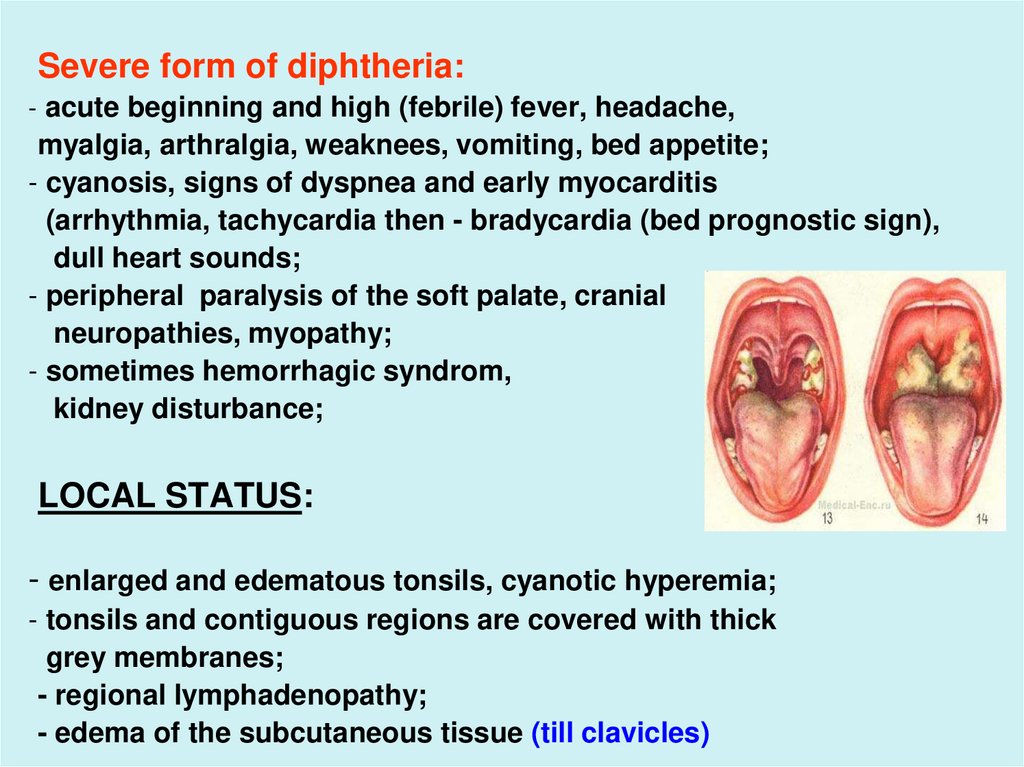
Severe form of diphtheria:- acute beginning and high (febrile) fever, headache,
myalgia, arthralgia, weaknees, vomiting, bed appetite;
- cyanosis, signs of dyspnea and early myocarditis
(arrhythmia, tachycardia then - bradycardia (bed prognostic sign),
dull heart sounds;
- peripheral paralysis of the soft palate, cranial
neuropathies, myopathy;
- sometimes hemorrhagic syndrom,
kidney disturbance;
LOCAL STATUS:
- enlarged and edematous tonsils, cyanotic hyperemia;
- tonsils and contiguous regions are covered with thick
grey membranes;
- regional lymphadenopathy;
- edema of the subcutaneous tissue (till clavicles)
38.
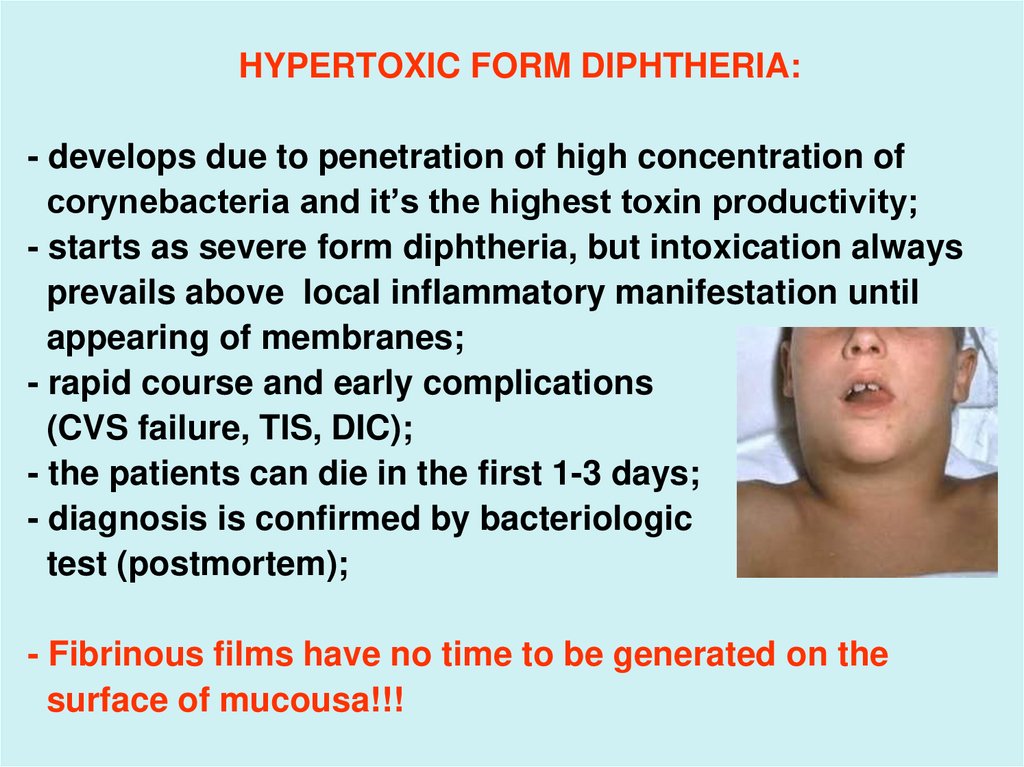
HYPERTOXIC FORM DIPHTHERIA:- develops due to penetration of high concentration of
corynebacteria and it’s the highest toxin productivity;
- starts as severe form diphtheria, but intoxication always
prevails above local inflammatory manifestation until
appearing of membranes;
- rapid course and early complications
(CVS failure, TIS, DIC);
- the patients can die in the first 1-3 days;
- diagnosis is confirmed by bacteriologic
test (postmortem);
- Fibrinous films have no time to be generated on the
surface of mucousa!!!
39.
LARINGEAL DIPHTHERIA:(DIPHTHERIC CROUP, TRUE CROUP)
1. General intoxication is mild (larynx is covered with
single-layer epithelium);
2. HYPOXIA – is dominant sign in the pathogenesis (upper
respiratory obstraction due to membrane);
3. Involvement of the larynx is ussually secondary – the
result of extension of the diphtheric membranes from
the pharynx;
4. Primary laryngeal diphtheria is rare;
5. There are 3 stages of diphtheric (true) croup:
a) dysphonic (catarral),
b) stenotic,
c) asphyxia
40.
a) Catarral stage:- cotinues 1- 2 days;
- begins with subfebrie TºC, weekness, malaise;
- cough which becomes burking cough
and hoarseness with sputum;
- laryngoscopy reveals hyperemia and edema
of the mucousa of larynx, the vocal cords
and trachea
(the films on the mucousa are absent !!!)
41.
b) laringostenosis:(MORE OFTEN ON the 2 – 3-d DAY of ILLNESS)
- duration of the stage - several hours to 2 - 3 days)
- appearance of embarrassed breathing and noisy
respiration (early symptoms);
- retraction of acceassory muscles and intercostal spaces;
- aphonia and soundless cough;
- the patient is anxious and has forced position in the bed leaning on
hands;
- cyanosis of skin and mucous;
- tachycardia, tachypnea, reduced BP, dull heart sounds;
- laryngoscopy reveals edema, hyperemia with cyanosis and
pseudomembranes;
- if the petient does not received treatment in this stage, he can die.
42.
43. forced position in bed
44.
45.
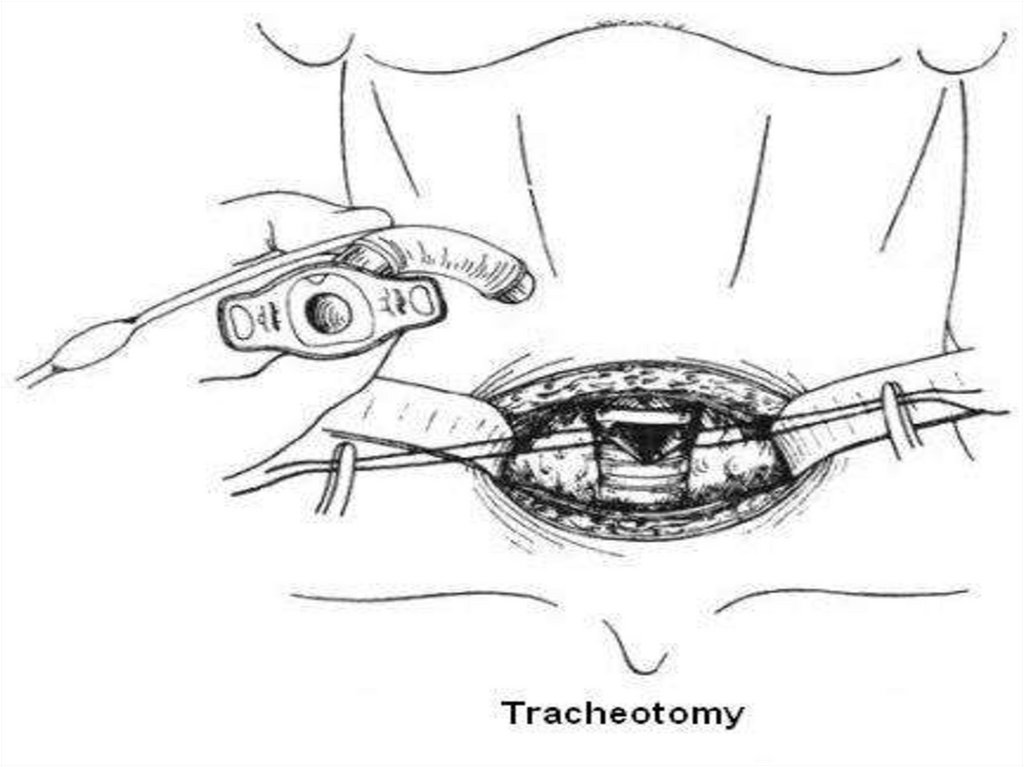
c) asphyxia (duration about 8 minutes !!!)- fast development of respiratory unsufficiency;
- frequent, shallow, noisy, respiratory arrhythmia;
- total cyanosis, chills, forced position;
- anxiety which is followed by drowsiness;
- weak and arrhythmic pulse, hypotonia;
- loss of consciousness, convulsions and death of suffocation
(without immediate tracheostomy!!)
DIPHTHERIA of NOSE:
- can be localized or wide-spread;
- mild intoxication;
LOCAL STATUS:
- rhinoscopy reveals edema, hyperemia of mucous or membranes
on the nasal septum;
- serosasanguineous discharge, irritation of nostrils and lips;
- nasal breathing is impeded;
- diagnosis is confirmed by bacteriologic test
46.
47.
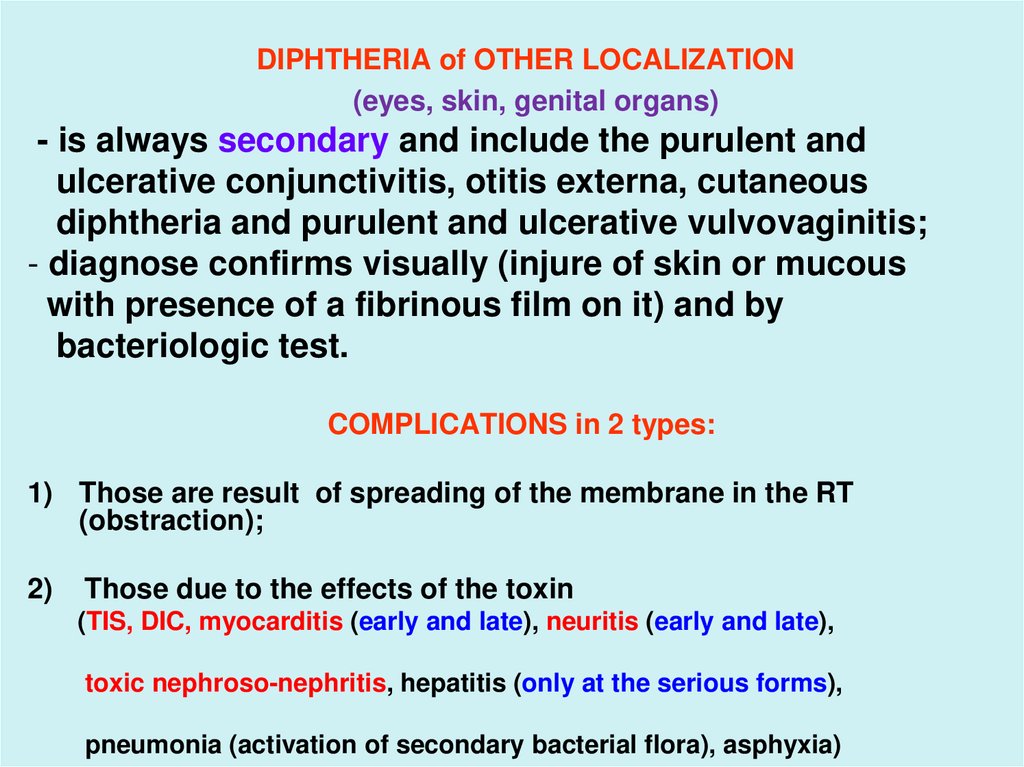
DIPHTHERIA of OTHER LOCALIZATION(eyes, skin, genital organs)
- is always secondary and include the purulent and
ulcerative conjunctivitis, otitis externa, cutaneous
diphtheria and purulent and ulcerative vulvovaginitis;
- diagnose confirms visually (injure of skin or mucous
with presence of a fibrinous film on it) and by
bacteriologic test.
COMPLICATIONS in 2 types:
1) Those are result of spreading of the membrane in the RT
(obstraction);
2)
Those due to the effects of the toxin
(TIS, DIC, myocarditis (early and late), neuritis (early and late),
toxic nephroso-nephritis, hepatitis (only at the serious forms),
pneumonia (activation of secondary bacterial flora), asphyxia)
48.
LABORATORY DIAGNOSTICS:SPESIFIC:
- Microscopy of the smears and its bacteriologic
investigation (swabs should be taken from nose and
tonsils beneath the membrane thrice and
before AB-therapy);
-Bacteriologic culture
is essential to confirm the DS;
- Serologic test – double serums
(quantity of antibody titer
to diphtherical exotoxin);
- Toxigenisity test (PCR, ELISA);
49.
NONSPESIFIC- CBC – moderate leucocytosis, increased ESR;
- UA – leukocytes,erythrocytes, proteinuria (10 g/l) and
casts;
- biochemical tests - АSТ, LDG, acid-base equilibrium,
electrolytes, serum protein, coagulogram, renal and
hepatic enzymes;
- ECG, medical consultations of neurologist, cardiologist
and ENT.
DIFFERENTIAL DIAGNOSTICS:
1.Diphtheria of a stomatopharynx:
- Streptococcal and staphylococcal angina
- Vincent tonsillitis
- Infectious mononucleosis
- Scarlet fever
- Paratonsillitis or аbscess
- Candidiasis of oral cavity
50. Streptococcal and staphylococcal angina
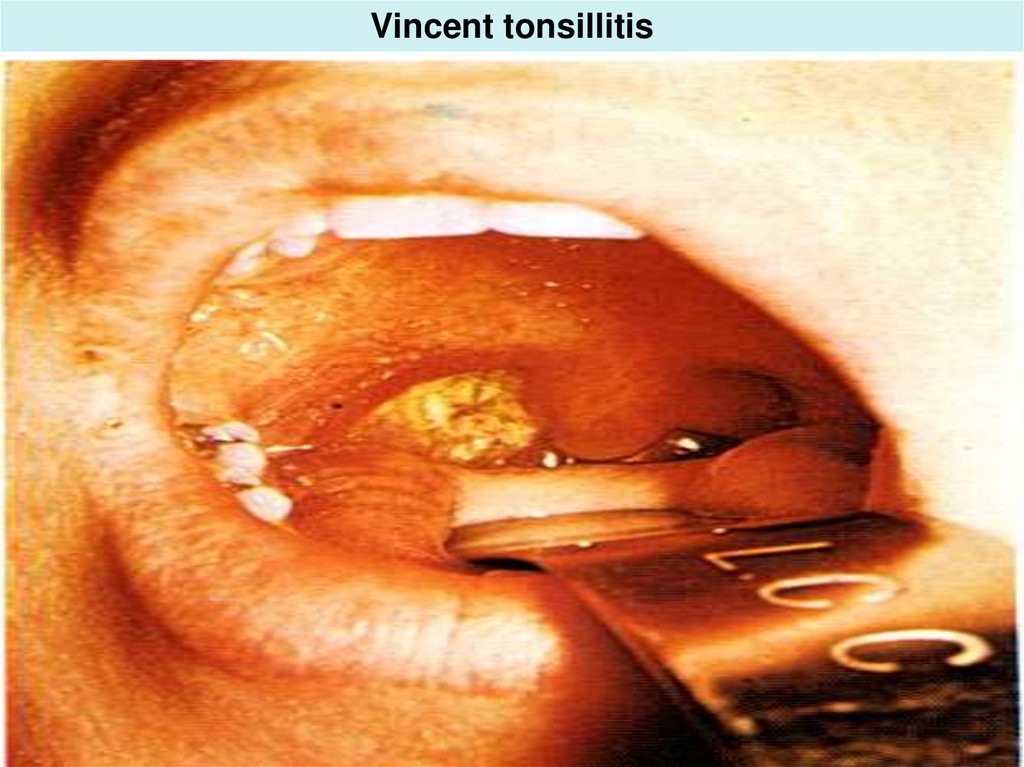
51. Vincent tonsillitis
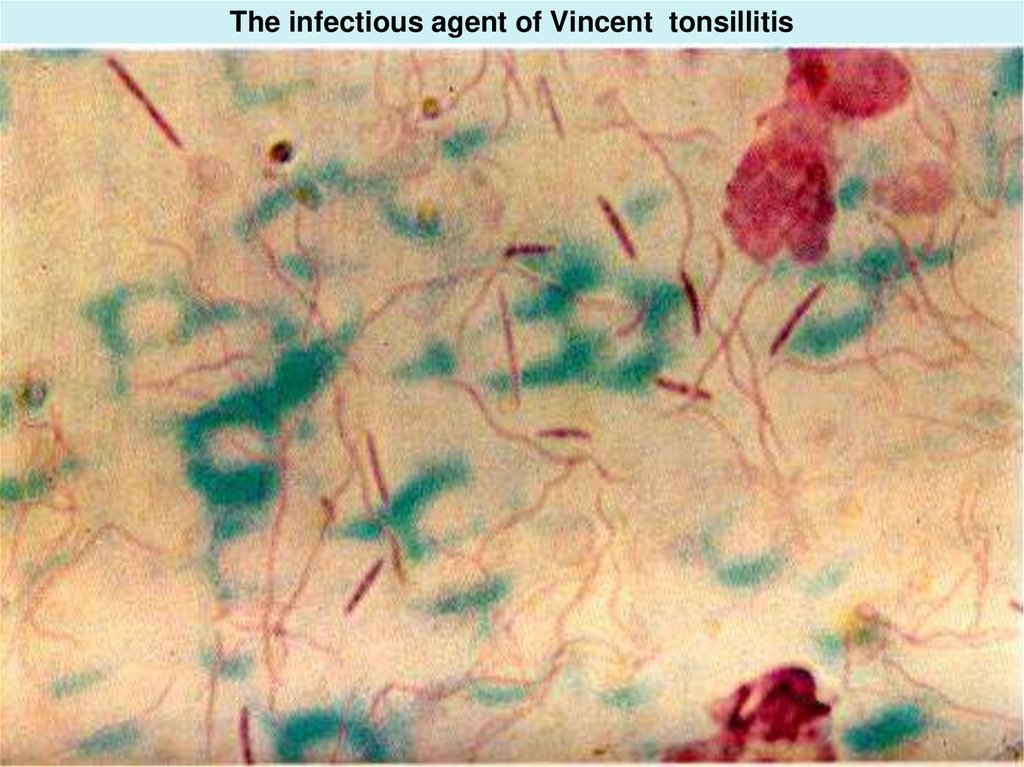
52. The infectious agent of Vincent tonsillitis
53. Infectious mononucleosis
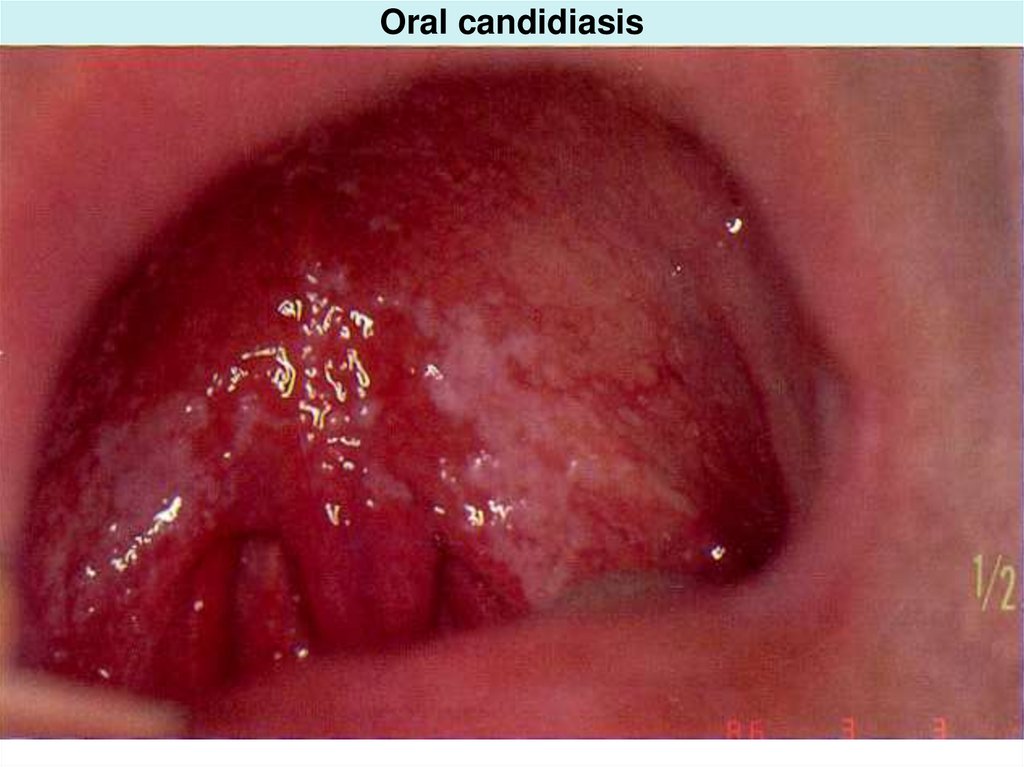
54. Oral candidiasis
55.
- Ludvig’s angina- Аngio-bubonic form of a tularemia
- Secondary angina at a typhoid, lues, tuberculosis, neoplasm, leukosis, agranulocytosis, combustions of a
mucous stomatopharynx (acid and alkaline)
2. Diphtheria of the nose:
- Meningococcal nasopharyngitis
- Streptococcal pharyngitis
- Adenoviral pharyngitis
3. Diphtheria of larynx:
- False croup (ARVD. parainfluenza, measles etc.)
- Asphyxia of foreign body
- Streptococcal pharyngitis (severe)
56.
TREATMENTObligatory hospitalization and bed regime, treatment
should be initiated even before confirmatory tests are
completed because of the high potential mortality and
morbidity!!!
2. Diet
3. Specific antitoxin – is the main therapy! Don’t be slow!
Immediate introduction of an antitoxin: (in thousand IU)
IV 40
80
120
160
mild
moderate
severe
hypertoxic
IM 60
110
160
220
Antitoxin is administered once at the emperic dose based
on the degree of toxicity, site and size of the membranes
and duration of illness. Antitoxin should be given i/v by
infusion.
57.
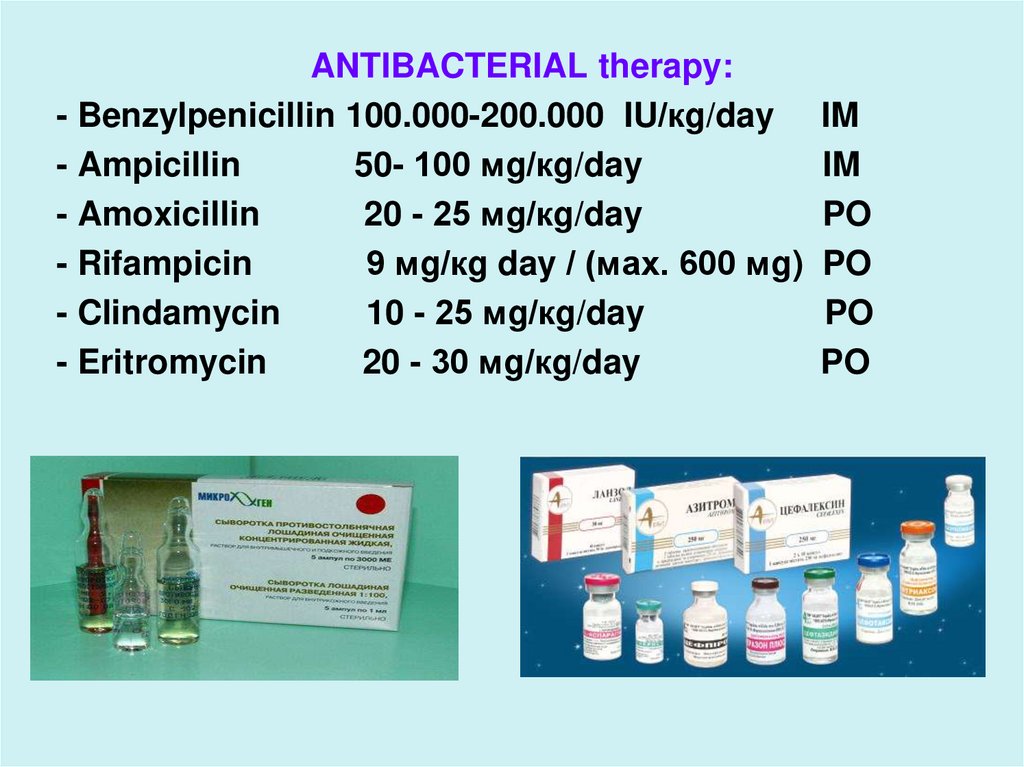
ANTIBACTERIAL therapy:- Benzylpenicillin 100.000-200.000 IU/кg/day
- Ampicillin
50- 100 мg/кg/day
- Amoxicillin
20 - 25 мg/кg/day
- Rifampicin
9 мg/кg day / (мах. 600 мg)
- Clindamycin
10 - 25 мg/кg/day
- Eritromycin
20 - 30 мg/кg/day
IM
IM
PO
PO
PO
PO
58.
PATHOGENIC THERAPY- detoxication and sufficient hydration
-
inhibitors of proteases
antioxidants
diuretics
glucocorticoids
nonsteroid antiinflammatory drugs
antihistamine drugs
treatment of myocardites, neuritises etc.
PROPHYLAXIS
- Common: - inspection of the contact persons, final disinfection in the focus,
- quarantine for 7 days
- Special (create active immunity): vaccination by diphtherial anatoxin:
- primary immunization on the 3, 4,5-th months of life,
- revaccination in 18 months, and then in 6, 11, 14, 18 years,
- the adult population should be revaccinated every 10 years.





























 Медицина
Медицина