Похожие презентации:
Cardiac emergencies and cpr
1. Cardiac Emergencies and CPR
Lesson 59-1
2. HISTORICAL REVIEW
5000 - 3000 BC - first artificial mouth to mouthventilation
1780 – first attempt of newborn resuscitation by
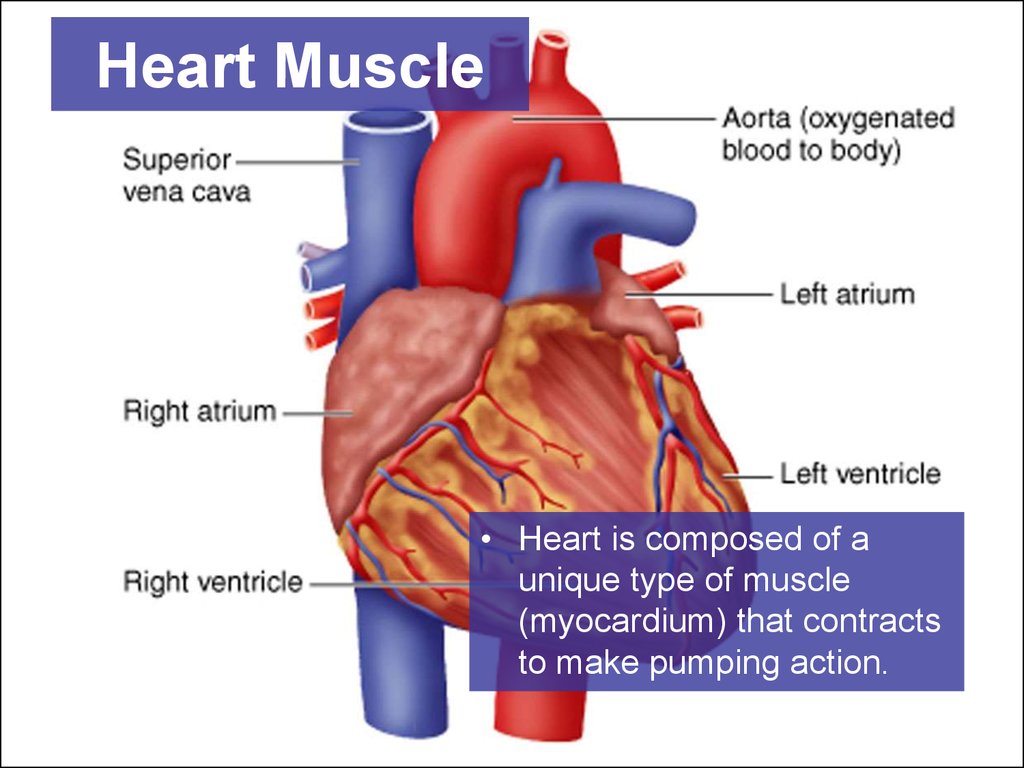
blowing
1874 – first experimental direct cardiac massage
1901 – first successful direct cardiac massage in man
1946 – first experimental indirect cardiac massage and
defibrillation
1960 – indirect cardiac massage
1980 – development of cardiopulmonary resuscitation
due to the works of Peter Safar
9-2
2
3. Introduction
• Basic Life Support needed for patient whosebreathing or heart has stopped
• Ventilations are given to oxygenate blood when
breathing is inadequate or has stopped
• If heart has stopped, chest compressions are
given to circulate blood to vital organs
• Ventilation combined with chest compressions is
called cardiopulmonary resuscitation (CPR)
• CPR is commonly given to patients in cardiac
arrest as a result of heart attack
9-3
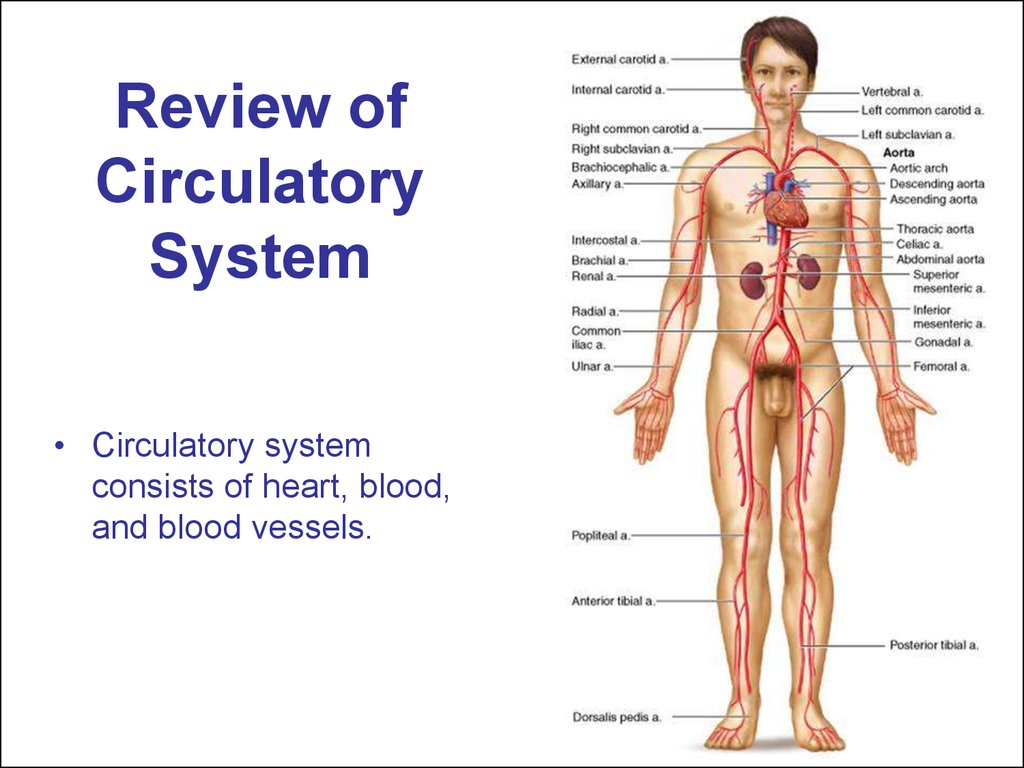
4. Review of Circulatory System
• Circulatory systemconsists of heart, blood,
and blood vessels.
5. Cardiovascular System: Primary Functions
• Transports blood to lungs– Delivers carbon dioxide and picks up oxygen
• Transports oxygen and nutrients to all
parts of body
• Helps regulate body temperature
• Helps maintain body’s fluid balance
9-5
6. Anatomy and Physiology of the Heart
• Ventricles pump blood through two loops or cycles inbody
• Right ventricle pumps blood to lungs to pick up oxygen
and release carbon dioxide
• Blood returns to left atrium and then flows into left
ventricle
• Left ventricle pumps oxygenated blood through arteries
to all areas of body
• Blood returns through veins to right atrium, to be
pumped again to lungs
• Within heart, valves prevent back flow of blood so that it
moves only in one direction through these cycles
9-6
7. Heart Muscle
• Heart is composed of aunique type of muscle
(myocardium) that contracts
to make pumping action.
8. Heart Muscle
• Contractions arecontrolled by electrical
signals under nervous
system control
9. Arteries
• Arterial blood is oxygenated, bright red, andunder pressure
• Carotid arteries — major arteries passing
through neck to head
• Femoral arteries — major arteries to legs
passing through thigh
• Brachial arteries — in upper arm
• Radial arteries — major artery of lower arm
• Arteries are generally deeper in body than
veins and more protected
9-9
10. Pulse
• When left ventriclecontracts, wave of
blood is sent through
arteries causing pulsing
blood pressure
changes in arteries that
can be palpated in
certain body locations
• A pulse can be felt
anywhere an artery
passes near skin
surface and over a
bone
• Palpate carotid pulse
on either side of neck
Pulse
11. Pulse continued
• Palpate femoralpulse in crease
between abdomen
and thigh
• Palpate radial pulse
on the palm side of
wrist proximal to
base of thumb
• Palpate brachial
pulse on the inside
of arm between
elbow and shoulder
12. Capillaries
• Arteries progressively branch into smallervessels that eventually reach capillaries
• Capillaries are very small blood vessels
connecting arteries with veins throughout body
• Capillaries have thin walls through which oxygen
and carbon dioxide are exchanged with body
cells
9-12
13. Veins
• From capillaries, blood drains back to heartthrough extensive system of veins
• Venous blood is dark red, deoxygenated, and
under less pressure than arterial blood
• Blood flows more evenly through veins, which
don’t have a pulse
• Veins have valves that prevent blood backflow
9-13
14. Heart Rate
• Heart rate, measured as pulse, is affected bymany factors
• With exercise, fever, or emotional excitement,
heart rate increases to meet body’s greater need
for oxygen
• Various injuries and illnesses may either
increase or decrease heart rate
9-14
15. Circulatory System: Emergencies
• Any condition that affects respiration– Reduces ability to deliver oxygen
• Severe bleeding
– Shock
• Stroke
– Reduces blood flow to brain
• Heart conditions
– Reduce tissue oxygenation
9-15
16. Circulatory System: Emergencies continued
• Heart attack– Can lead to cardiac arrest
• Ventricular fibrillation
– Heart muscle flutters rather than pumping
blood
9-16
17. Cardiac Arrest
• Heart may stop (cardiac arrest) as a result ofheart attack
• Brain damage begins 4 - 6 minutes after cardiac
arrest
• Brain damage becomes irreversible in 8 - 10
minutes
• Dysrhythmia, an abnormal heartbeat, may also
reduce heart’s pumping effectiveness
9-17
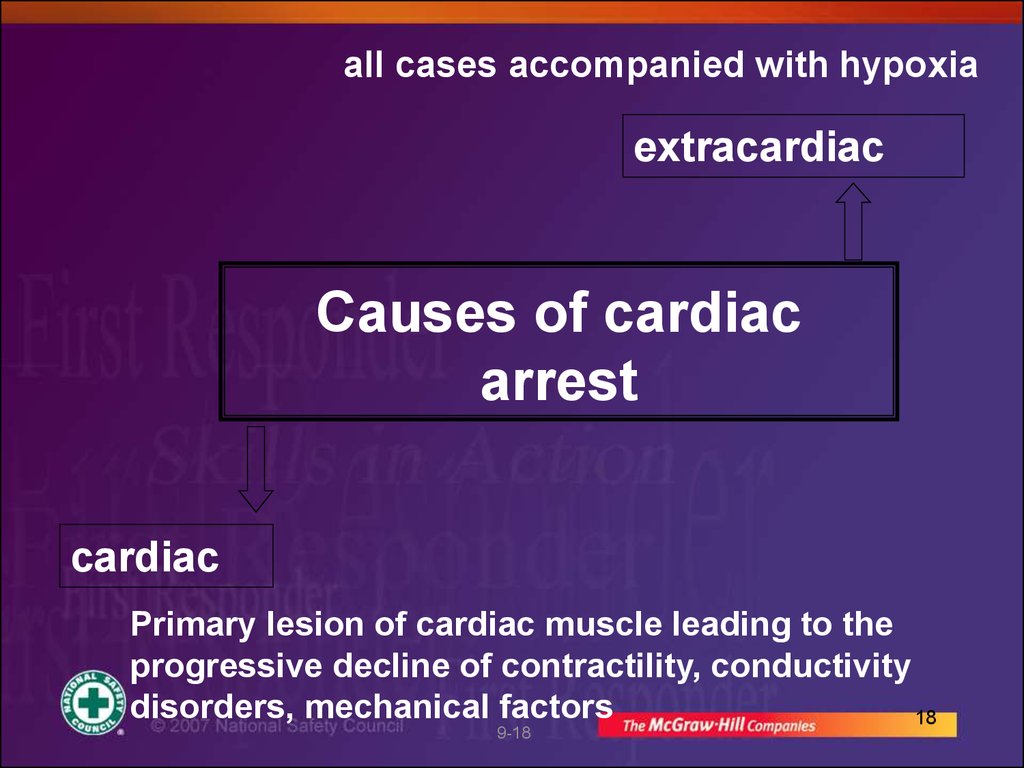
18.
all cases accompanied with hypoxiaextracardiac
Causes of cardiac
arrest
cardiac
Primary lesion of cardiac muscle leading to the
progressive decline of contractility, conductivity
disorders, mechanical factors
18
9-18
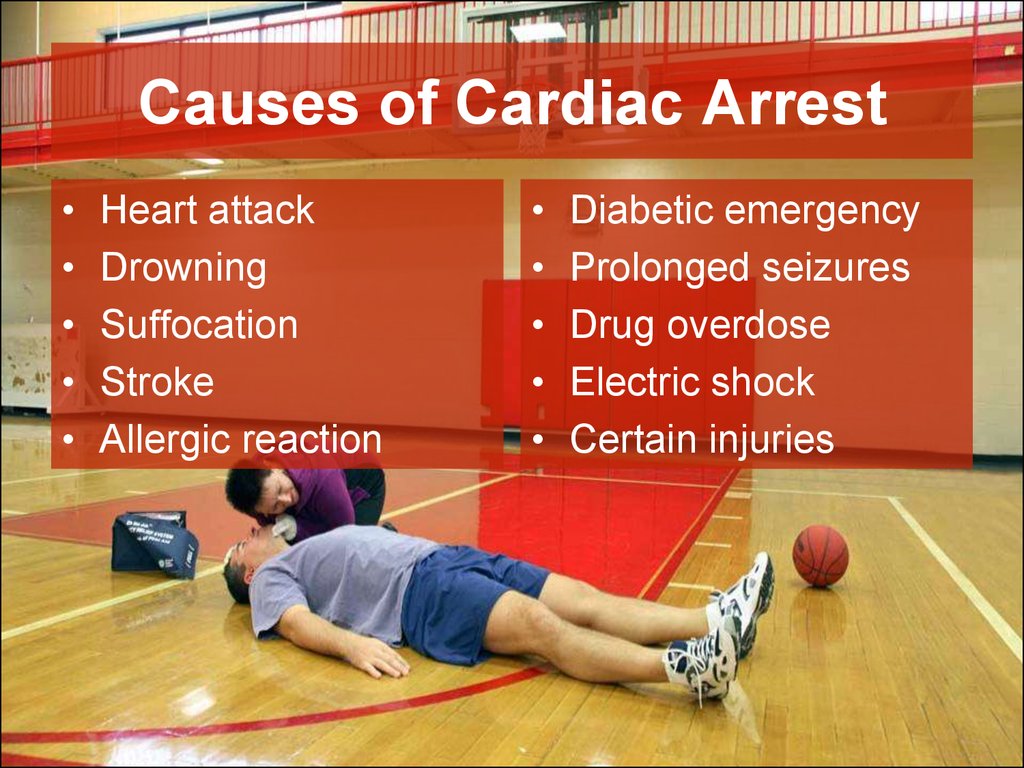
19. Causes of Cardiac Arrest
Heart attack
Drowning
Suffocation
Stroke
Allergic reaction
9-19
Diabetic emergency
Prolonged seizures
Drug overdose
Electric shock
Certain injuries
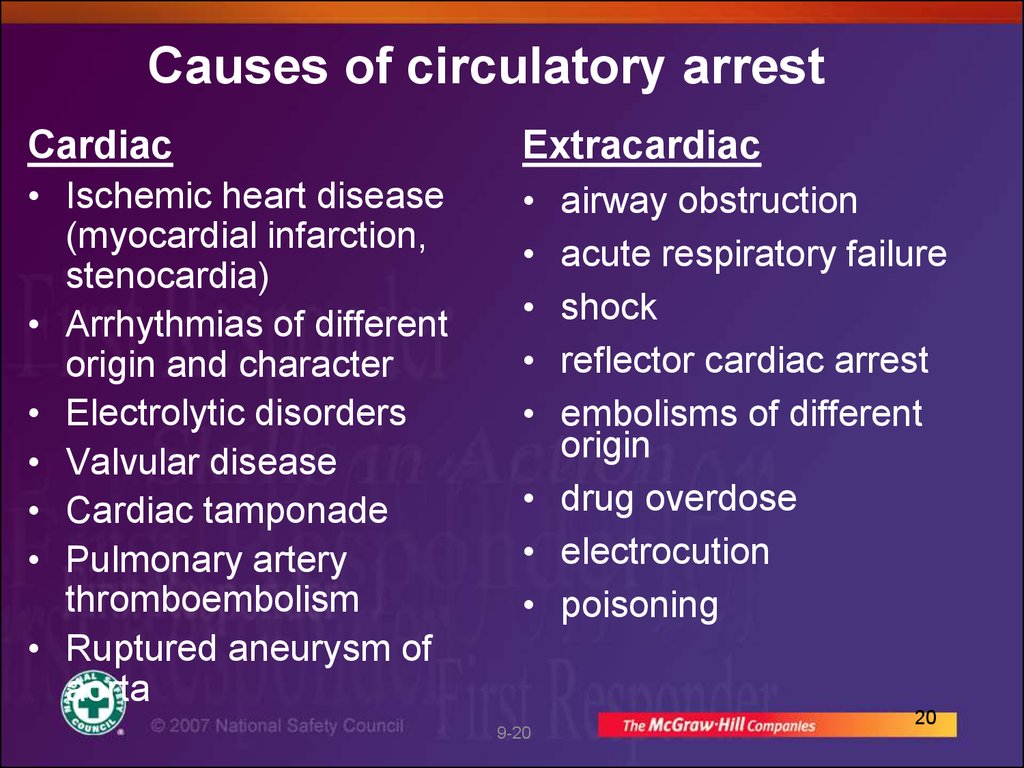
20. Causes of circulatory arrest
CardiacExtracardiac
• Ischemic heart disease
(myocardial infarction,
stenocardia)
• Arrhythmias of different
origin and character
• Electrolytic disorders
• Valvular disease
• Cardiac tamponade
• Pulmonary artery
thromboembolism
• Ruptured aneurysm of
aorta
airway obstruction
acute respiratory failure
shock
reflector cardiac arrest
embolisms of different
origin
• drug overdose
• electrocution
• poisoning
9-20
20
21. Cardiac Chain of Survival
22.
Diagnosis of cardiac arrestBlood pressure measurement
Taking the pulse on peripheral
arteries
Auscultation of cardiac tones
Loss of time !!!
Symptoms of cardiac arrest
absence of pulse on carotid arteries – a
pathognomonic symptom
respiratory arrest – may be in 30 sec after cardiac
arrest
pupil dilation – may be in 90 sec after cardiac arrest
9-22
22
23. Sequence of operations
Check responsivenessCall for help
Correctly place the victim and ensure
the open airway
Check the presence of spontaneous
respiration
Check pulse
Start external cardiac massage and
artificial ventilation
9-23
23
24.
In case of unconsciousness it isnecessary to estimate quickly
the open airway
respiration
hemodynamics
9-24
24
25.
Main stages of resuscitationC (Circulation) – restore the circulation by
external cardiac massage
A (Airway) – ensure open airway by preventing
the falling back of tongue, tracheal intubation if
possible
B (Breathing) – start artificial ventilation of lungs
D (Differentiation, Drugs, Defibrilation) – quickly
perform differential diagnosis of cardiac arrest,
use different medication and electric
defibrillation in case of ventricular fibrillation
9-25
25
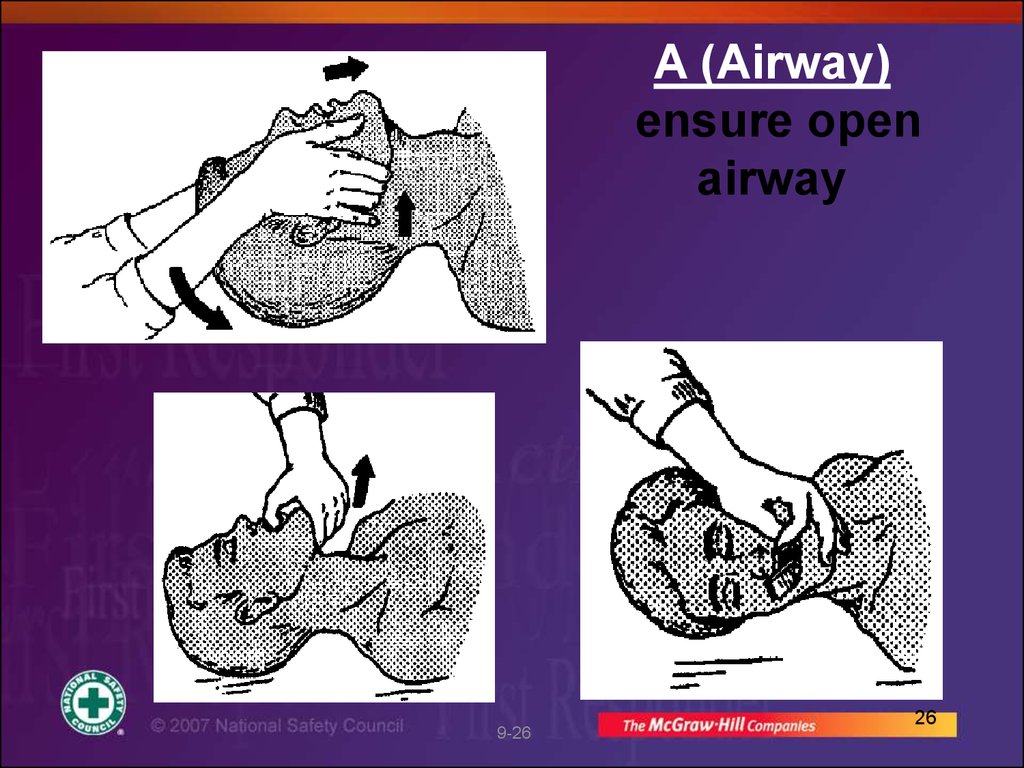
26.
A (Airway)ensure open
airway
9-26
26
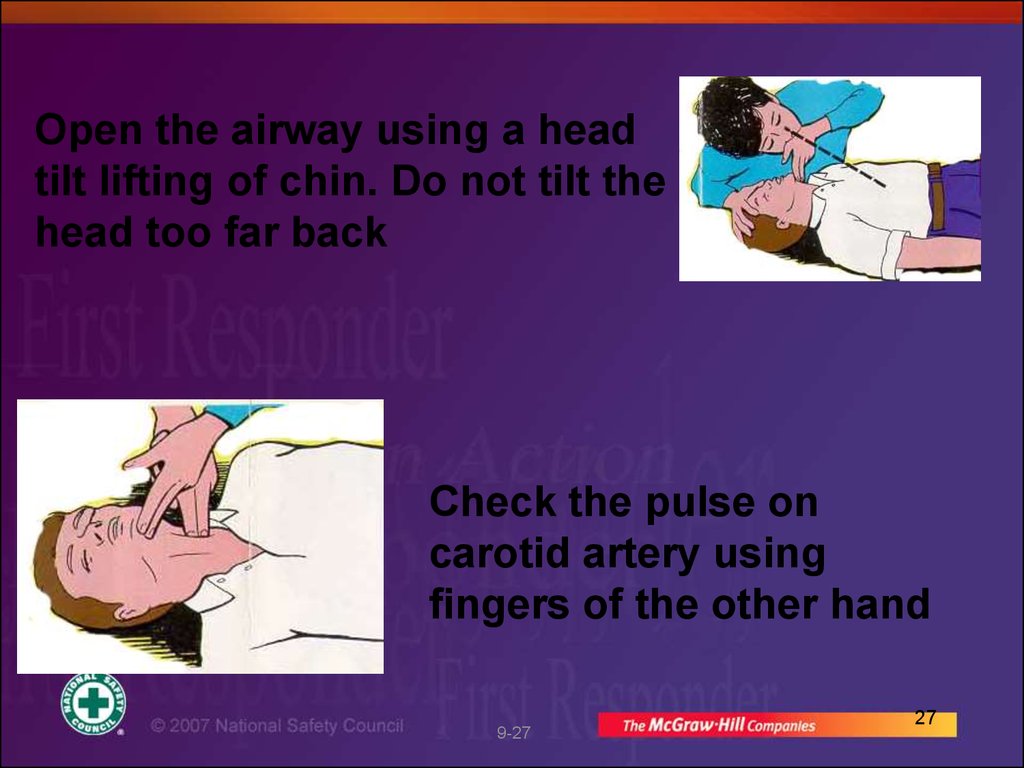
27.
Open the airway using a headtilt lifting of chin. Do not tilt the
head too far back
Check the pulse on
carotid artery using
fingers of the other hand
9-27
27
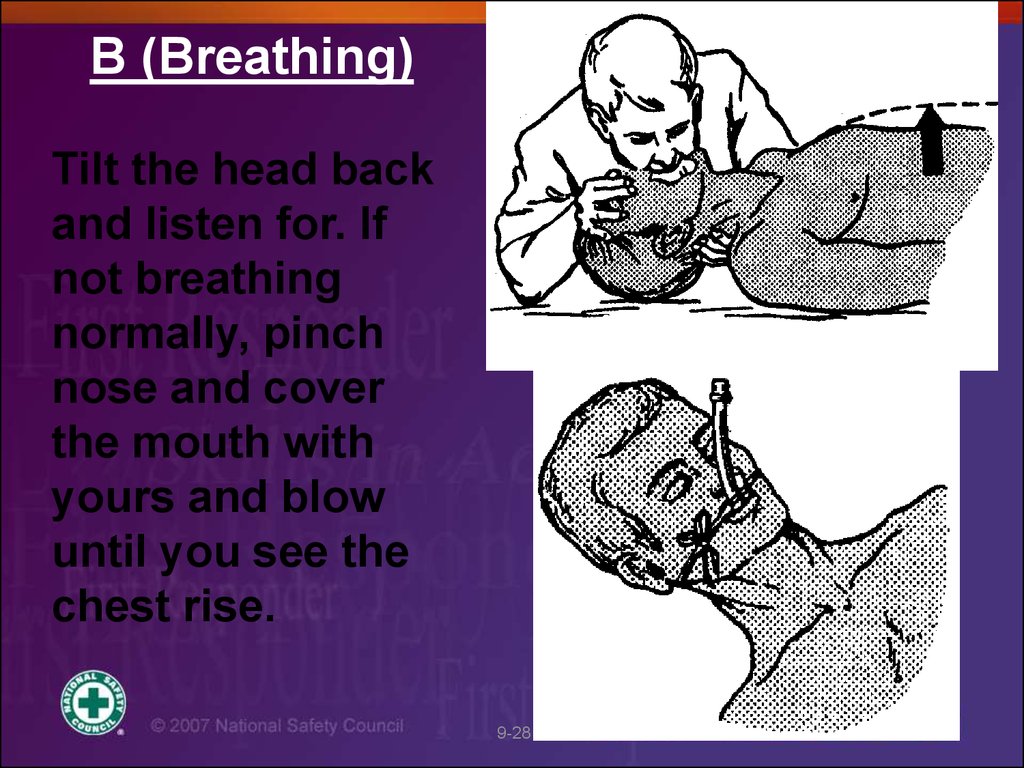
28.
B (Breathing)Tilt the head back
and listen for. If
not breathing
normally, pinch
nose and cover
the mouth with
yours and blow
until you see the
chest rise.
9-28
28
29.
Algorithm for artificial ventilationmouth to mouth or mouth
to nose respiration
ventilation by a face mask and a
self-inflating bag with oxygen
2 initial subsequent breaths
wait for the end of expiration
10-12 breaths per minute with a volume of app.
800 ml, each breath should take 1,5-2 seconds
Control over the ventilation
check chest movements during ventilation
check the
9-29air return
29
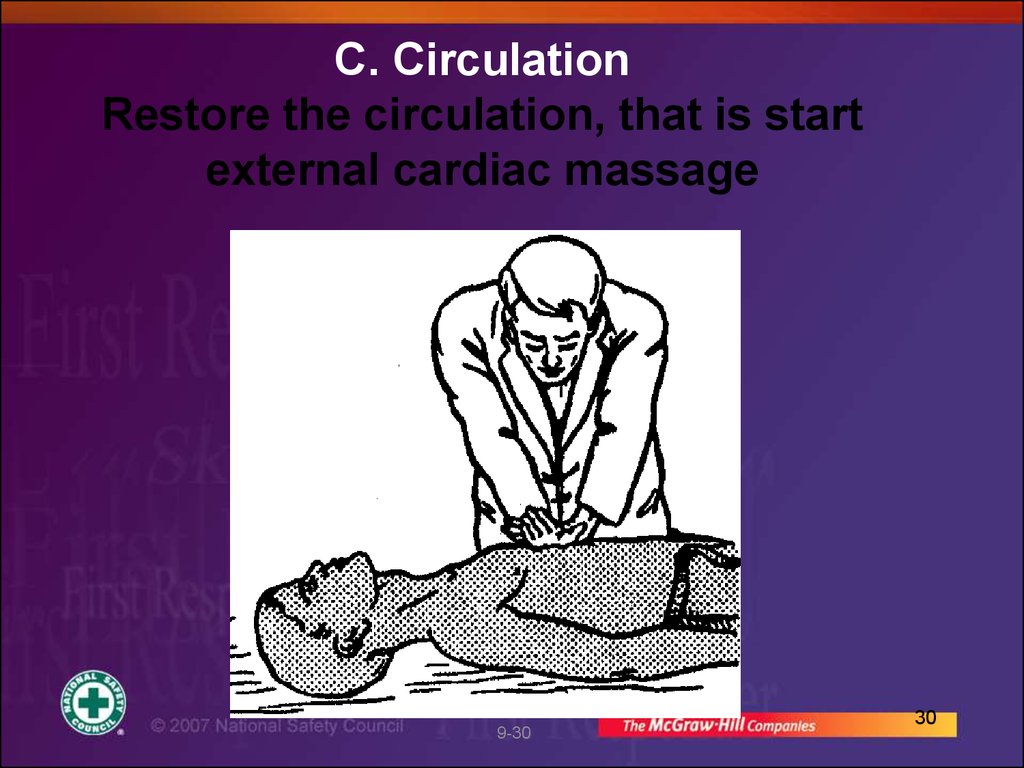
30.
C. CirculationRestore the circulation, that is start
external cardiac massage
9-30
30
31.
2 mechanisms explaining therestoration of circulation by
external cardiac massage
Cardiac
pump
Thoracic
pump
9-31
31
32.
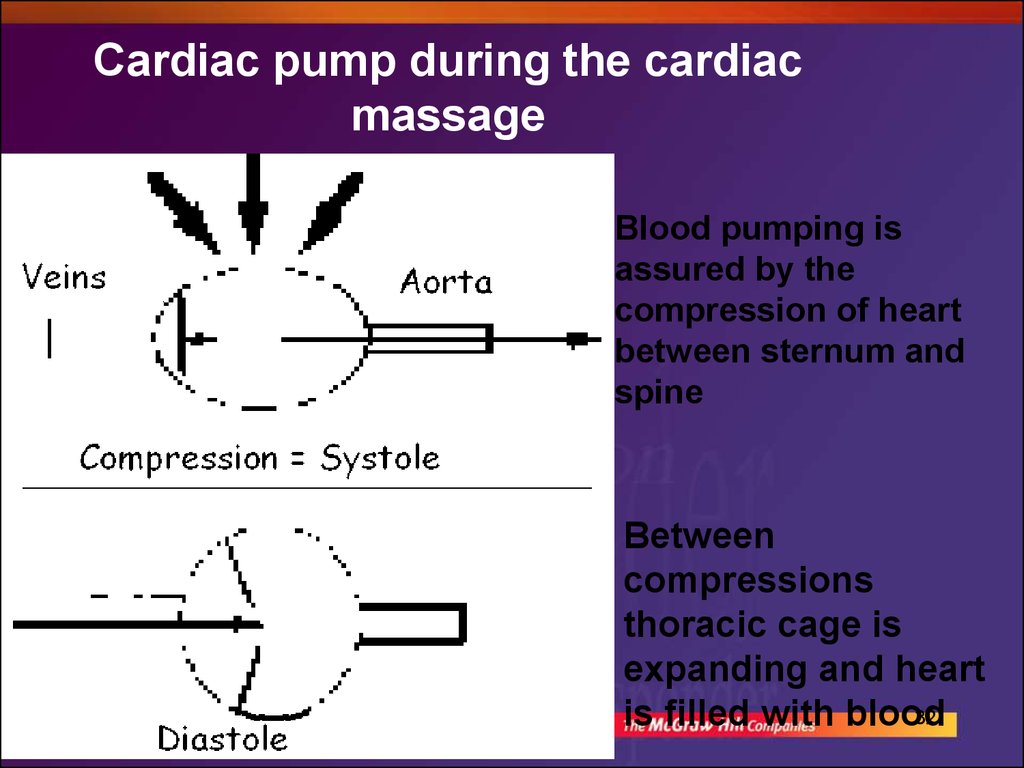
Cardiac pump during the cardiacmassage
Blood pumping is
assured by the
compression of heart
between sternum and
spine
9-32
Between
compressions
thoracic cage is
expanding and heart
32
is filled with blood
33.
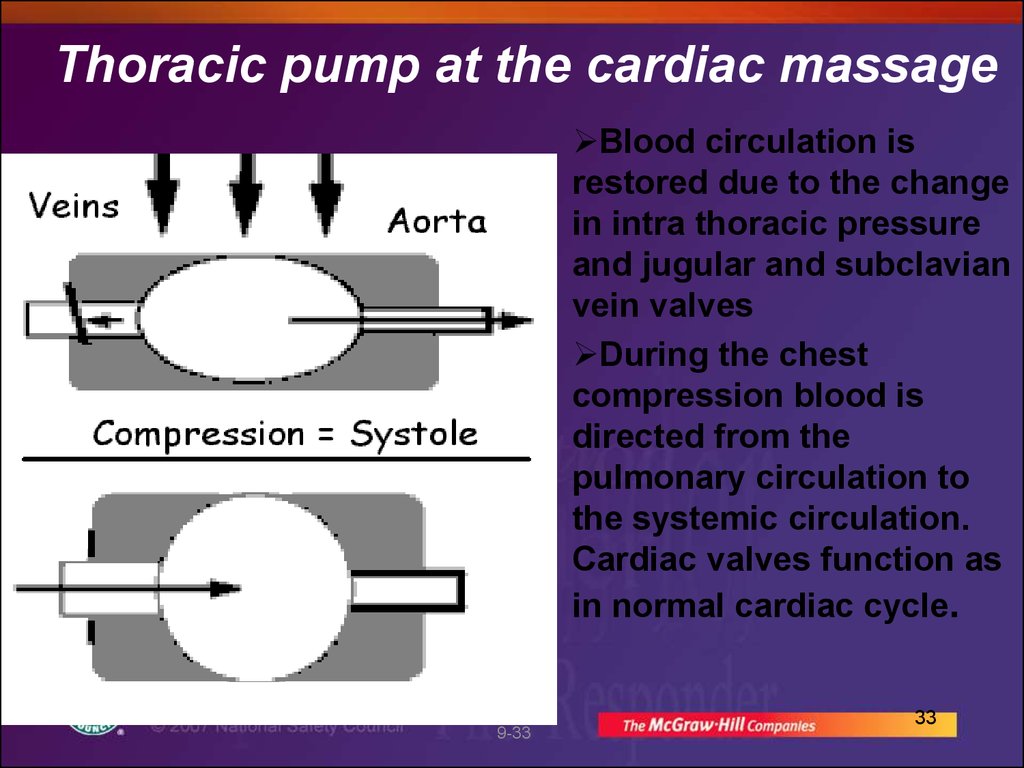
Thoracic pump at the cardiac massageBlood circulation is
restored due to the change
in intra thoracic pressure
and jugular and subclavian
vein valves
During the chest
compression blood is
directed from the
pulmonary circulation to
the systemic circulation.
Cardiac valves function as
in normal cardiac cycle.
9-33
33
34.
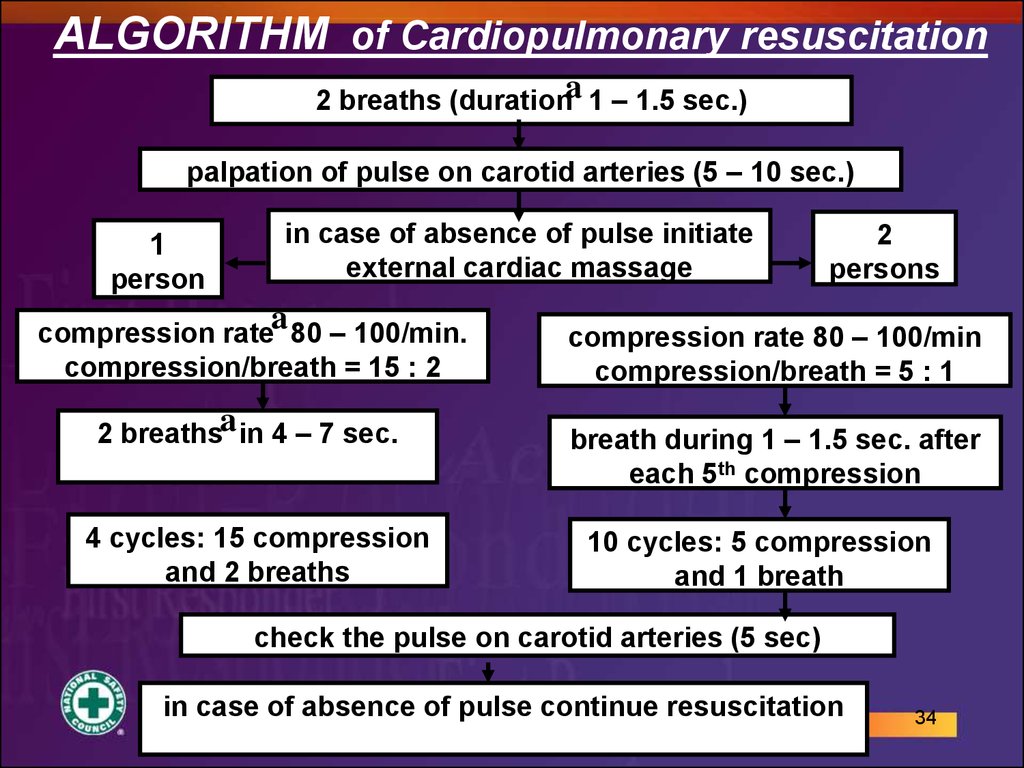
ALGORITHM of Cardiopulmonary resuscitation2 breaths (durationa 1 – 1.5 sec.)
palpation of pulse on carotid arteries (5 – 10 sec.)
1
person
in case of absence of pulse initiate
external cardiac massage
a
compression rate 80 – 100/min.
compression/breath = 15 : 2
2
persons
compression rate 80 – 100/min
compression/breath = 5 : 1
2 breathsa in 4 – 7 sec.
breath during 1 – 1.5 sec. after
each 5th compression
4 cycles: 15 compression
and 2 breaths
10 cycles: 5 compression
and 1 breath
check the pulse on carotid arteries (5 sec)
in case of absence of pulse continue resuscitation
9-34
34
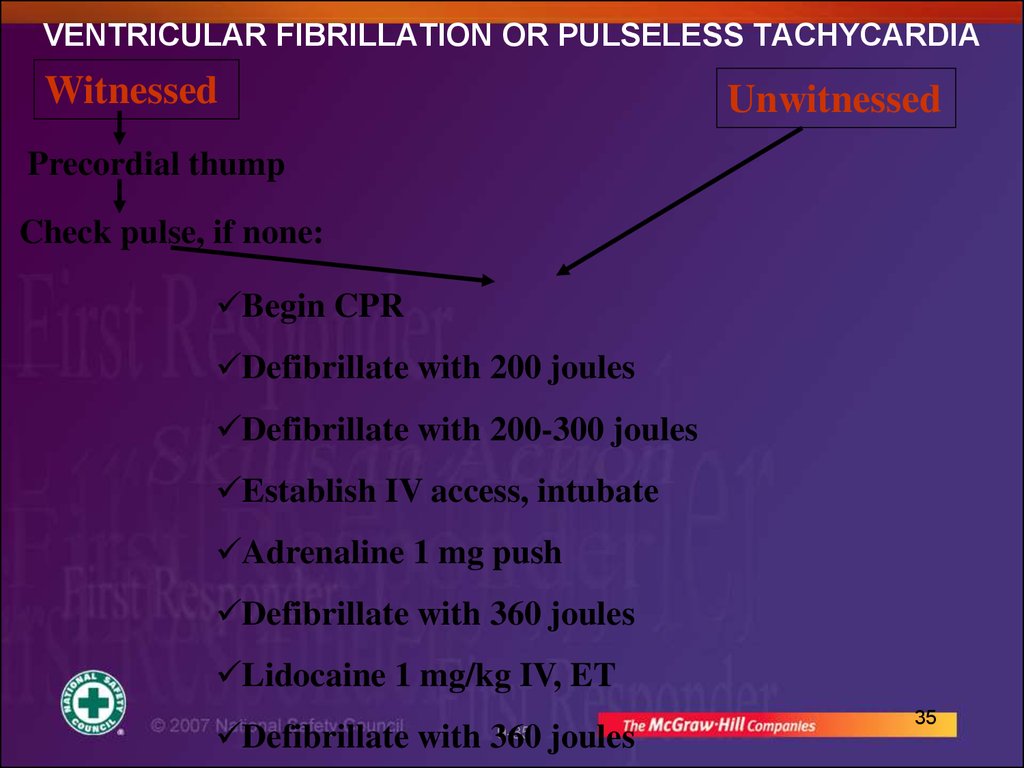
35. VENTRICULAR FIBRILLATION OR PULSELESS TACHYCARDIA
WitnessedUnwitnessed
Precordial thump
Check pulse, if none:
Begin CPR
Defibrillate with 200 joules
Defibrillate with 200-300 joules
Establish IV access, intubate
Adrenaline 1 mg push
Defibrillate with 360 joules
Lidocaine 1 mg/kg IV, ET
Defibrillate with 360 joules
9-35
35
36.
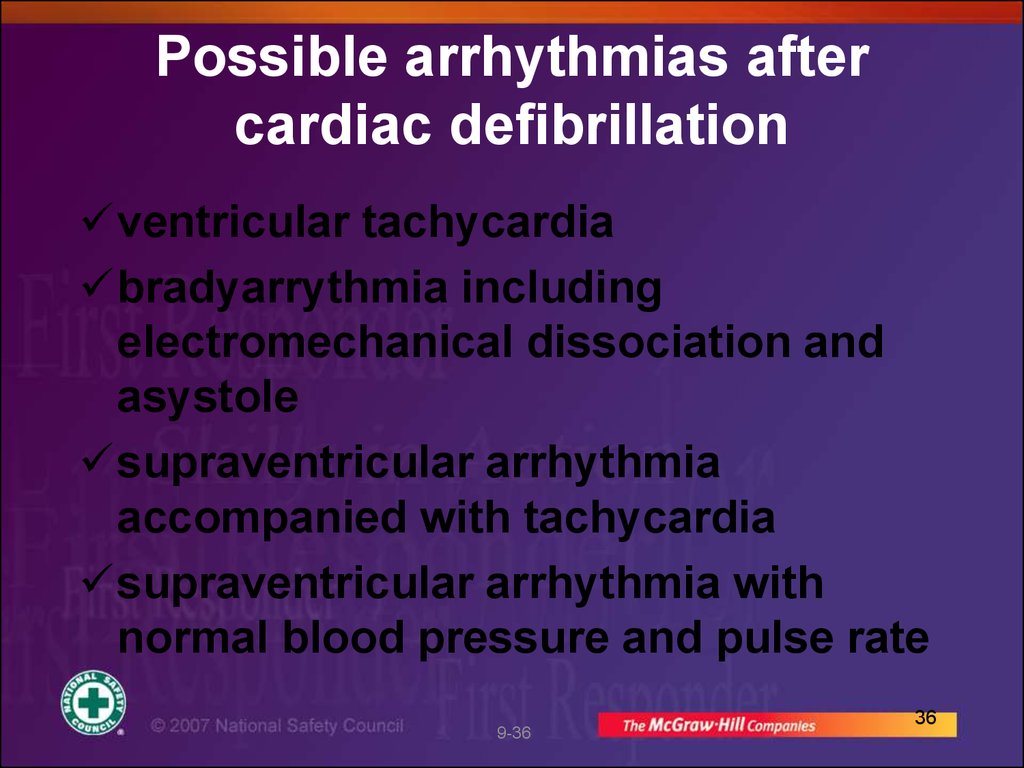
Possible arrhythmias aftercardiac defibrillation
ventricular tachycardia
bradyarrythmia including
electromechanical dissociation and
asystole
supraventricular arrhythmia
accompanied with tachycardia
supraventricular arrhythmia with
normal blood pressure and pulse rate
9-36
36
37.
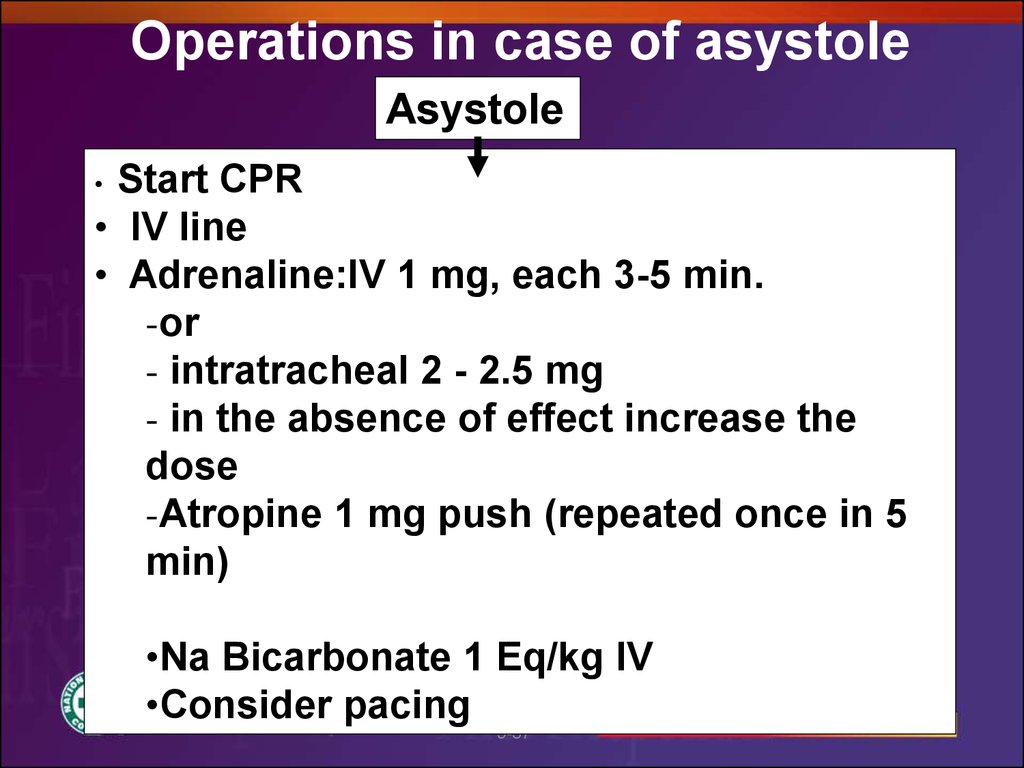
Operations in case of asystoleAsystole
Start CPR
• IV line
• Adrenaline:IV 1 mg, each 3-5 min.
-or
- intratracheal 2 - 2.5 mg
- in the absence of effect increase the
dose
-Atropine 1 mg push (repeated once in 5
min)
•Na Bicarbonate 1 Eq/kg IV
•Consider pacing
9-37
37
38. Call First vs. Call Fast
• Call First– If alone with adult victim
– Any victim of any age seen to collapse
suddenly
• Call Fast
– If alone with child victim
– Unresponsive victim in cardiac arrest because
of respiratory arrest
9-38
39. Cardiopulmonary Resuscitation (CPR)
• CPR helps keep patient alive bycirculating some oxygenated blood to
vital organs
• Ventilations move oxygen into lungs
where it is picked up by blood
• Compressions on sternum increase
pressure inside chest, moving some
blood to brain/other tissues
9-39
40. CPR continued
• Blood circulation resulting fromchest compressions not as strong
as circulation from heartbeat
–Can help keep brain/other
tissues alive until normal heart
rhythm restored
9-40
41. CPR continued
• Often electric shock from AED isneeded to restore a heartbeat—and
CPR can keep patient viable until
then
• CPR effective only for a short time
• CPR should be started as soon as
possible
• In some instances, the heart may
start again spontaneously with CPR
9-41
42. CPR Saves Lives
• CPR and defibrillation within 3-5 minutescan save over 50% of cardiac arrest
victims
• CPR followed by AED saves thousands of
lives each year
• In most cases CPR helps keep victim alive
until EMS or AED arrives
9-42
43. General Technique of CPR
• If unresponsive, not breathing, and nopulse, start chest compressions
• Find the correct hand position
–Two hands for adults
–One or 2 hands for child
–Two fingers for infant
9-43
44. General Technique of CPR continued
• Compress chest hard and fast at a rate of 100compressions/minute
– Adult = 4-5 santimeters deep
– Infant/child = 1/3 to 1/2 chest depth
• Release completely between compressions
9-44
45. General Technique of CPR continued
• If alone, alternate 30 chest compressionsand 2 ventilations for any age patient
• In two-rescuer CPR for infant/child,
alternate 15 compressions and 2
ventilations
– Chest-encircling method in infant
• Give each ventilation over 1 second
• Follow local protocol regarding oxygen
9-45
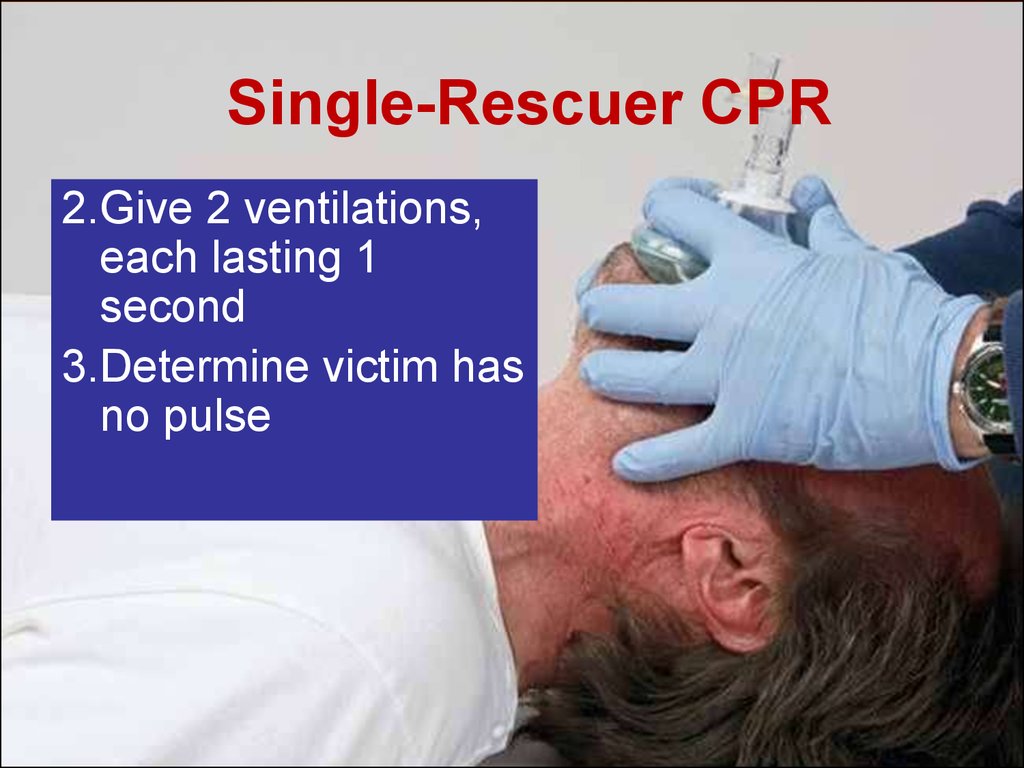
46. Single-Rescuer CPR
1. Check patient’s responsiveness,open airway,
and determine that patient is not
breathing adequately
2. Give 2 ventilations, each lasting 1 second
3. Determine victim has no pulse
9-46
47. Single-Rescuer CPR
2.Give 2 ventilations,each lasting 1
second
3.Determine victim has
no pulse
9-47
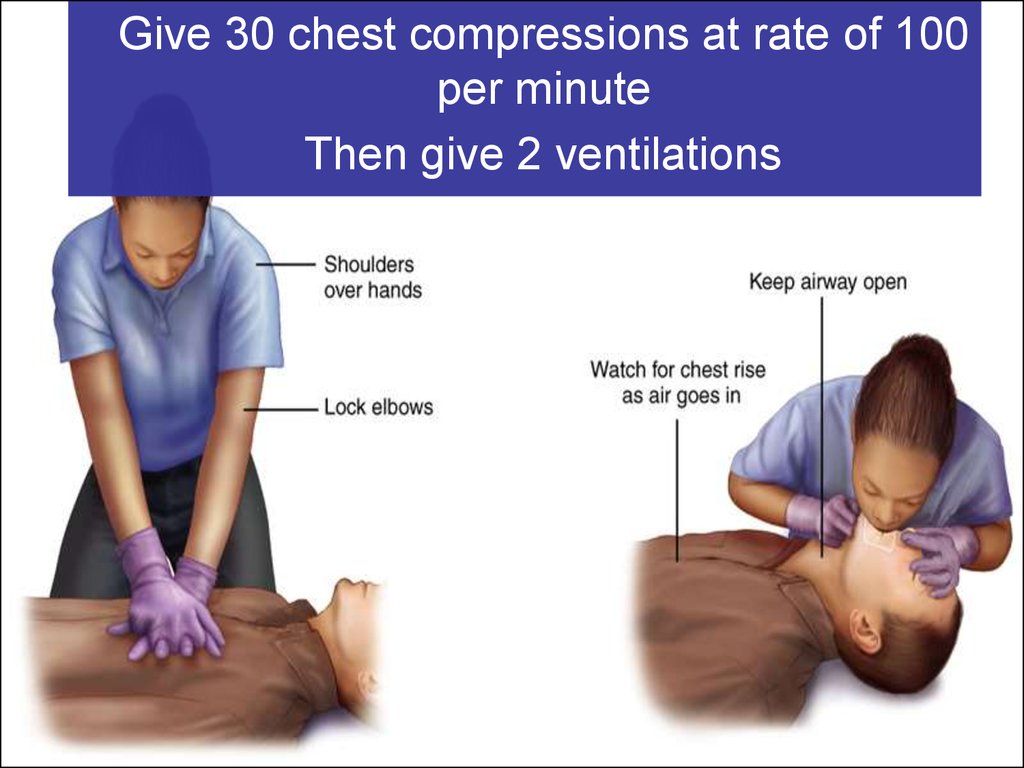
48.
Put hand(s) in correct position for chestcompressions
9-48
49.
Give 30 chest compressions at rate of 100per minute
Then give 2 ventilations
50.
Continue CPR until:• Patient begins to move
• AED brought to scene and ready
to use
• Professional help arrives to take
over
• You are too exhausted to
continue
9-50
51.
• If patient starts moving, checkfor adequate breathing
• If patient is breathing
adequately, put patient in
recovery position and monitor
breathing
• When AED arrives, start AED
sequence
9-51
52. Chest Compressions Alert
• Be careful with yourhand position
• For adults/children,
keep your fingers
off patient’s chest
• Do not give
compressions over
bottom tip of
breastbone
9-52
53. Chest Compressions Alert
• When compressing,keep elbows
straight and hands
in contact with
patient’s chest at all
times
9-53
54. Chest Compressions Alert
• Compress chesthard and fast, but
let chest recoil
completely between
compressions.
Minimize amount of
time used giving
ventilations
between sets of
compressions.
9-54
55. Problems with CPR Technique
• CPR often ineffective because of poortechnique
• Compressions not delivered steadily and
constantly during resuscitation efforts
• Often compressions are too shallow,
resulting in ineffective blood flow
• Compressions may be given at too fast a
rate
• Only good-quality CPR improves chances
of survival
9-55
56. Chest Compressions: Bradycardia in Child
• Infant or child being given rescuebreaths or oxygen may have a pulse
but still inadequate perfusion
• If pulse < 60 beats/minute and infant
or child has signs of poor perfusion,
provide CPR
9-56
57. Skill:
CPR For Adultor Child
(Two Rescuers)
9-57
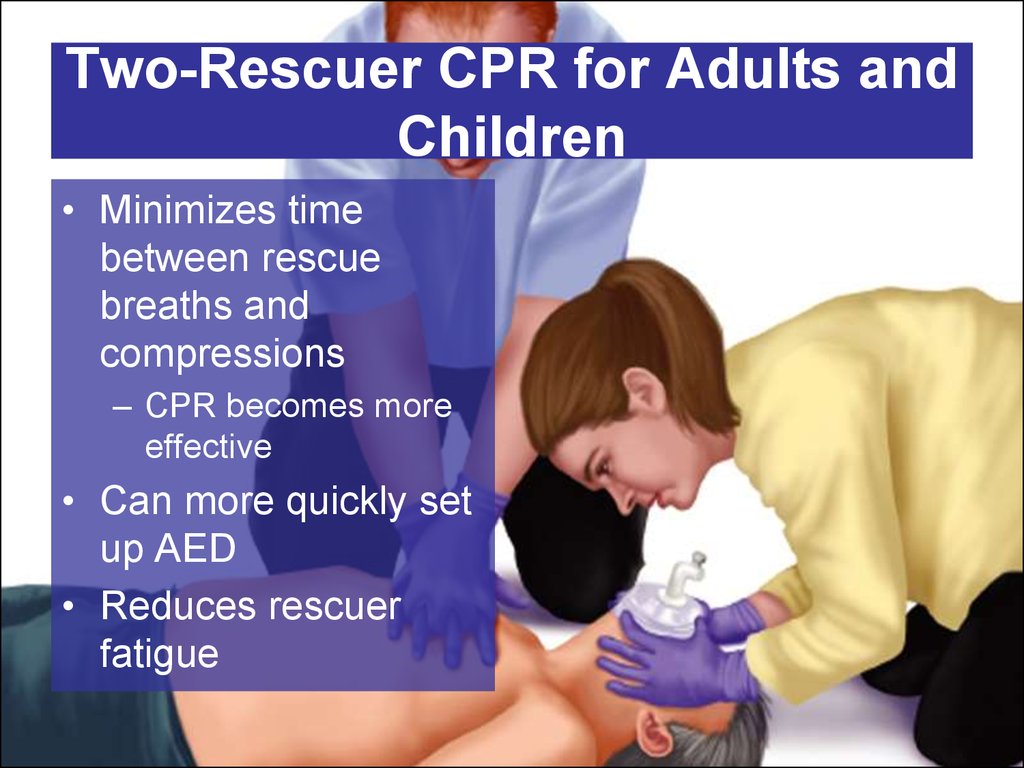
58. Two-Rescuer CPR for Adults and Children
• Minimizes timebetween rescue
breaths and
compressions
– CPR becomes more
effective
• Can more quickly set
up AED
• Reduces rescuer
fatigue
9-58
59. Two-Rescuer CPR
• Performed in cycles of 30:2 for adult (15:2for infant or child)
• One rescuer provides breaths, second
rescuer gives chest compressions
• Rescuers switch positions every 2 minutes
– Change done after full CPR cycle
– Accomplish change in < 5 seconds
9-59
60. Two-Rescuer CPR continued
• If AED present, one rescuer givesCPR while the other sets up unit
• If unit advises CPR, rescuers give
CPR together
• Third rescuer can apply cricoid
pressure
9-60
61. Two-Rescuer CPR continued
• If you are assisting another trainedrescuer who places an advanced
airway:
–Chest compressions given
continually
–No pauses for ventilations
–Give ventilations at rate of 8 – 10
breaths/ minute
9-61
62. Transitioning from One-Rescuer CPR to Two-Rescuer CPR
• Second rescuer moves into positionon other side to prepare to take over
chest compressions
• First rescuer completes a cycle of
compressions and ventilations
While first rescuer pauses to check for
a pulse, second rescuer finds correct
hand position for compressions
9-62
63. Transitioning from One-Rescuer CPR to Two-Rescuer CPR
When first rescuer says, “Nopulse, continue CPR,”
second rescuer begins chest
compressions and first rescuer
then gives only ventilations
9-63
64. Differences in Two-Rescuer Training
• If First Responder started CPR,arriving second rescuer may have
a higher level of training
• Rescuer with greater training
determines how CPR should best
be continued
9-64
65.
Rescuer 1 checks ABCs. Rescuer 2locates site for chest compressions.
9-65
66.
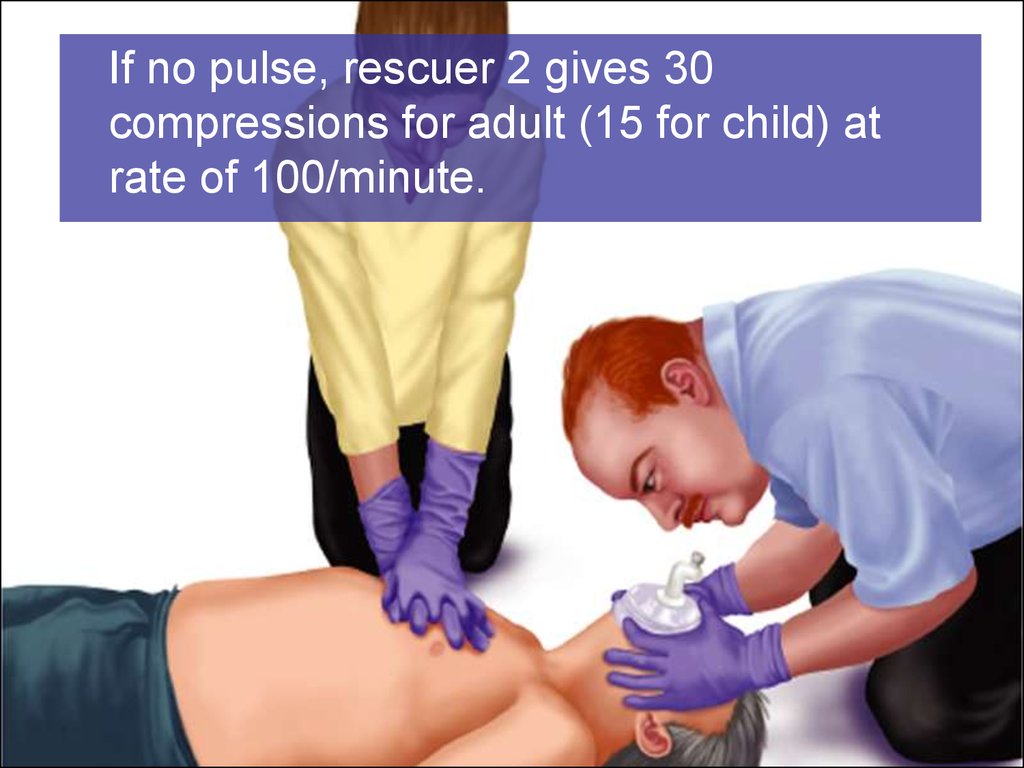
If no pulse, rescuer 2 gives 30compressions for adult (15 for child) at
rate of 100/minute.
9-66
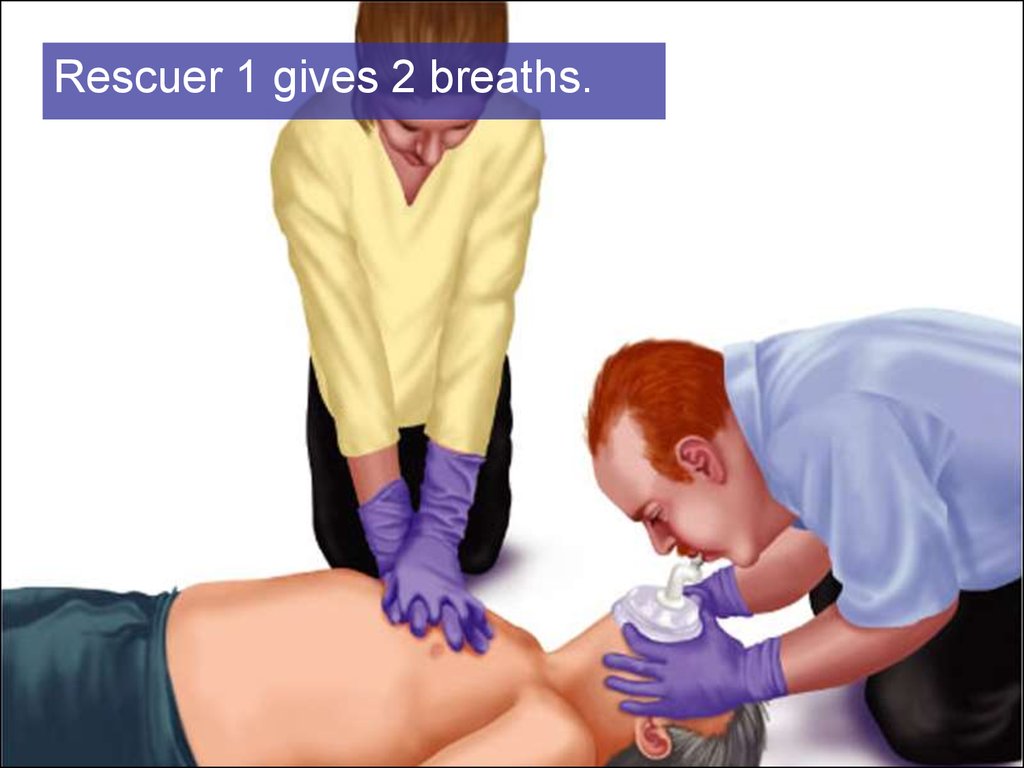
67.
Rescuer 1 gives 2 breaths.9-67
68.
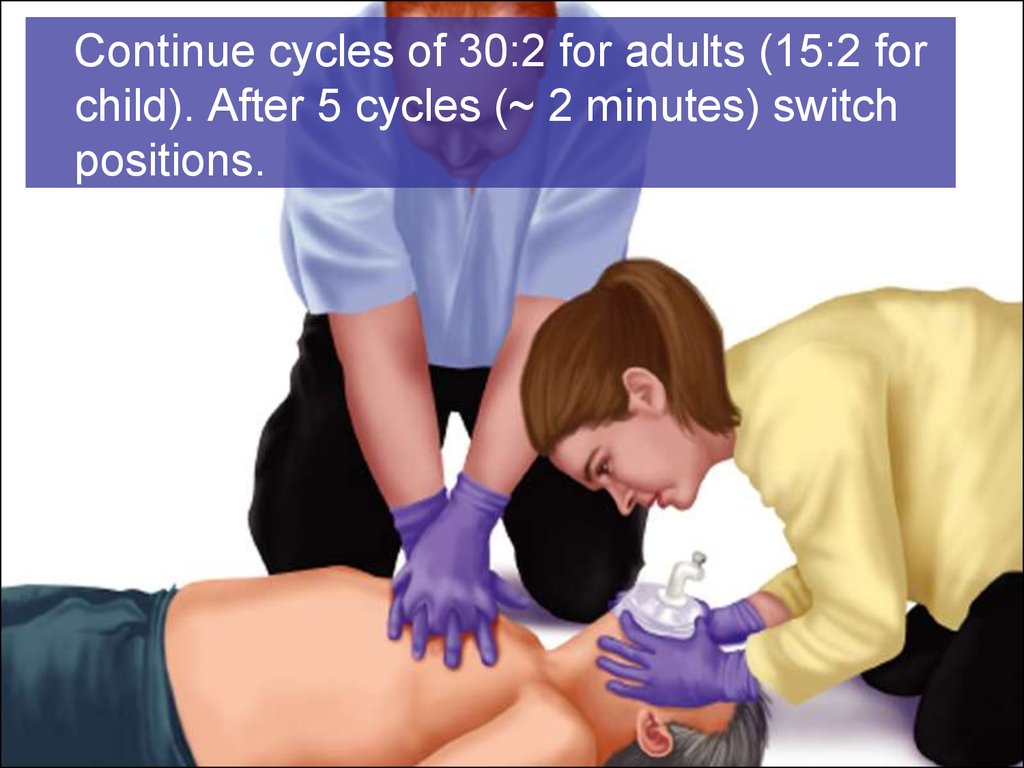
Continue cycles of 30:2 for adults (15:2 forchild). After 5 cycles (~ 2 minutes) switch
positions.
9-68
69. Adult or Child Two-Rescuer CPR Continued
• Continue CPR until:– Patient moves
– AED brought to scene and ready to use
– Advanced help arrives and takes over
• If patient starts breathing and has pulse, put in
recovery position and monitor ABCs
• If AED brought to scene, start AED sequence
9-69
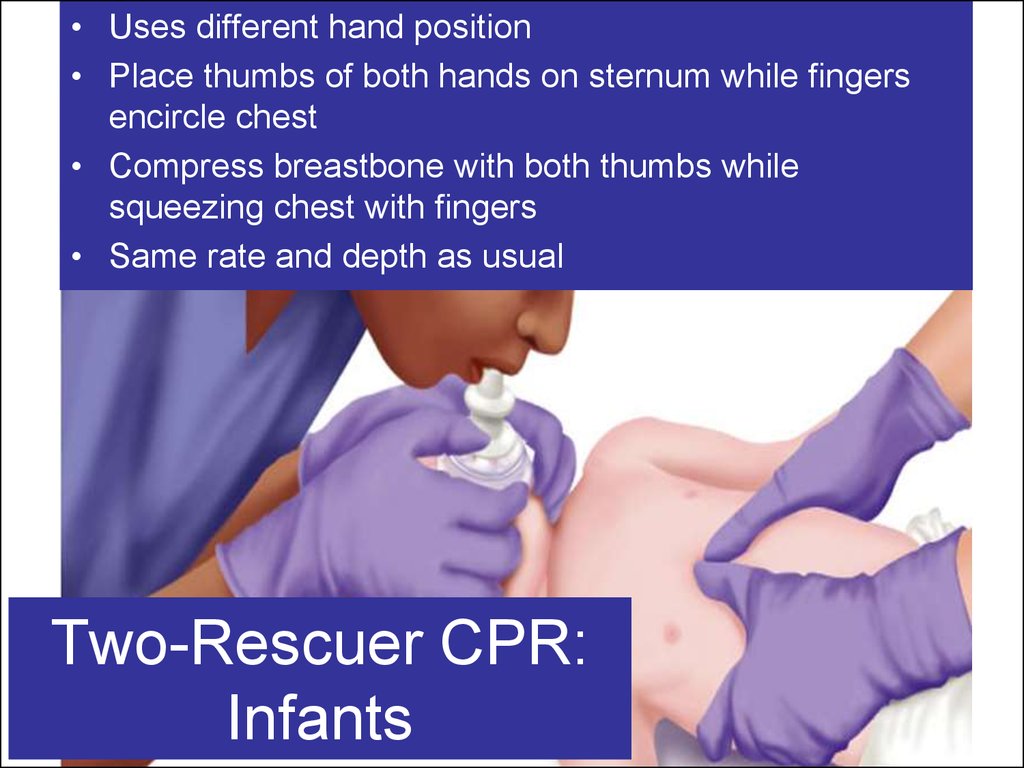
70. Two-Rescuer CPR: Infants
• Uses different hand position• Place thumbs of both hands on sternum while fingers
encircle chest
• Compress breastbone with both thumbs while
squeezing chest with fingers
• Same rate and depth as usual
Two-Rescuer CPR:
Infants
71. Skill:
CPR: InfantsTwo Rescuers
9-71
72.
Rescuer 1 checksABCs. Rescuer 2
locates site for chest
compressions.
9-72
73.
If no pulse, rescuer 2gives 15 chest
compressions.
9-73
74.
Rescuer 1 gives 2 breaths.9-74
75. Infant Two-Rescuer CPR Continued
• Continue cycles of 15:2 for ~ 2 minutes thenswitch roles
• Continue CPR until:
– Infant moves
– Advanced help arrives and takes over
• If infant starts breathing, hold in recovery
position and monitor ABCs
9-75
76. When Not to Perform CPR
• Presence of a Do-Not-Resuscitate (DNR)order
• Patient obviously dead (decapitation;
incineration; or clear signs of prolonged
death, such as rigor mortis and dependent
lividity)
• Not safe to be on the scene and the
patient cannot be moved somewhere safe
• A physician pronounces the patient dead
9-76
77.
Drugs used in CPR• Atropine – can be injected bolus, max 3 mg to
block vagal tone, which plays significant role in
some cases of cardiac arrest
• Adrenaline – large doses have been
withdrawn from the algorithm. The
recommended dose is 1 mg in each 3-5 min.
• Vasopresine – in some cases 40 U can
replace adrenaline
• Amiodarone - should be included in algorithm
• Lidocaine – should be used only in ventricular
77
fibrillation
9-77






















 Медицина
Медицина








