Похожие презентации:
Pathomorphology of systemic and local violation of blood circulation
1.
ZAPOROZHZHIAN STATE MEDICAL UNIVERSITYThe department of pathological anatomy and
forensic medicine
PATHOMORPHOLOGY
OF SYSTEMIC AND
LOCAL VIOLATION OF
BLOOD CIRCULATION
DISORDERS OF HEMOSTASIS
Lecture on pathological anatomy for the
3-rd year students
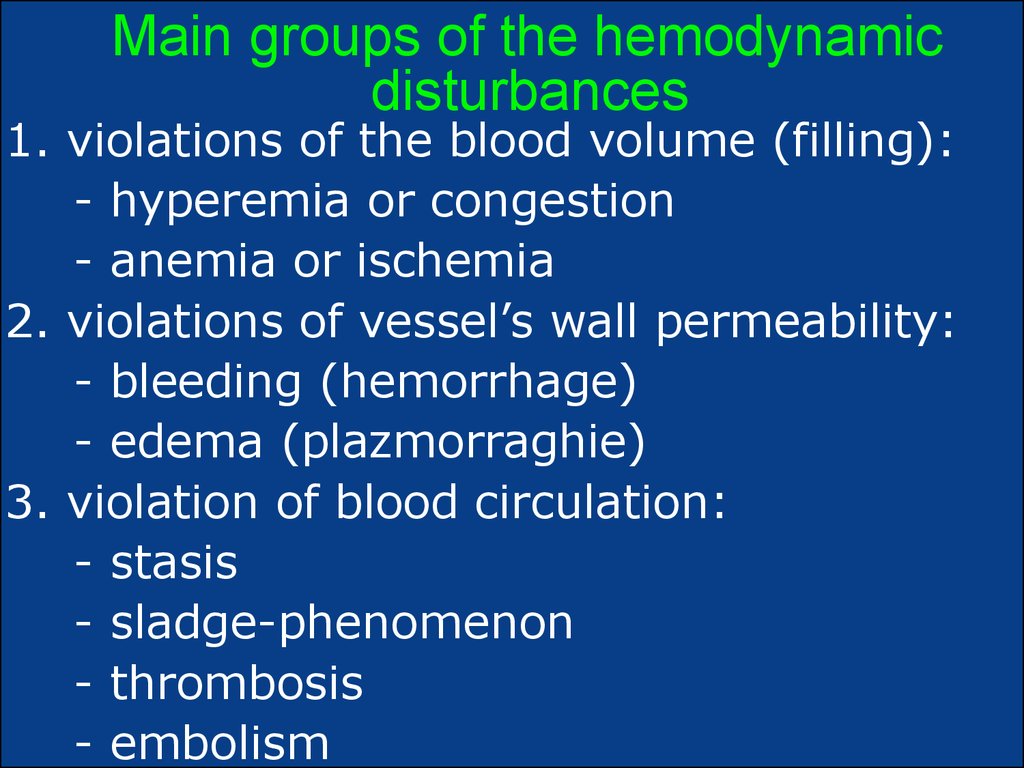
2. Main groups of the hemodynamic disturbances
1. violations of the blood volume (filling):- hyperemia or congestion
- anemia or ischemia
2. violations of vessel’s wall permeability:
- bleeding (hemorrhage)
- edema (plazmorraghie)
3. violation of blood circulation:
- stasis
- sladge-phenomenon
- thrombosis
- embolism
3.
Reasons of circulatory disturbances1.Heart failure:
- of the myocardium (pump function failure)
- obstruction of blood outflow (valvular disease)
2. Vascular changes:
- constrictions caused by vascular spasm
- dilatations of vessels
- obstructions of vessels
- abnormal arterial-venous communications
- rupture of vessel’s wall
- increased vascular permeability
3.Blood disturbances, such as changes in the
volume, composition, viscosity, or coagulation
ability of blood.
4. Multi-systemic organ failure (shock or sepsis).
4.
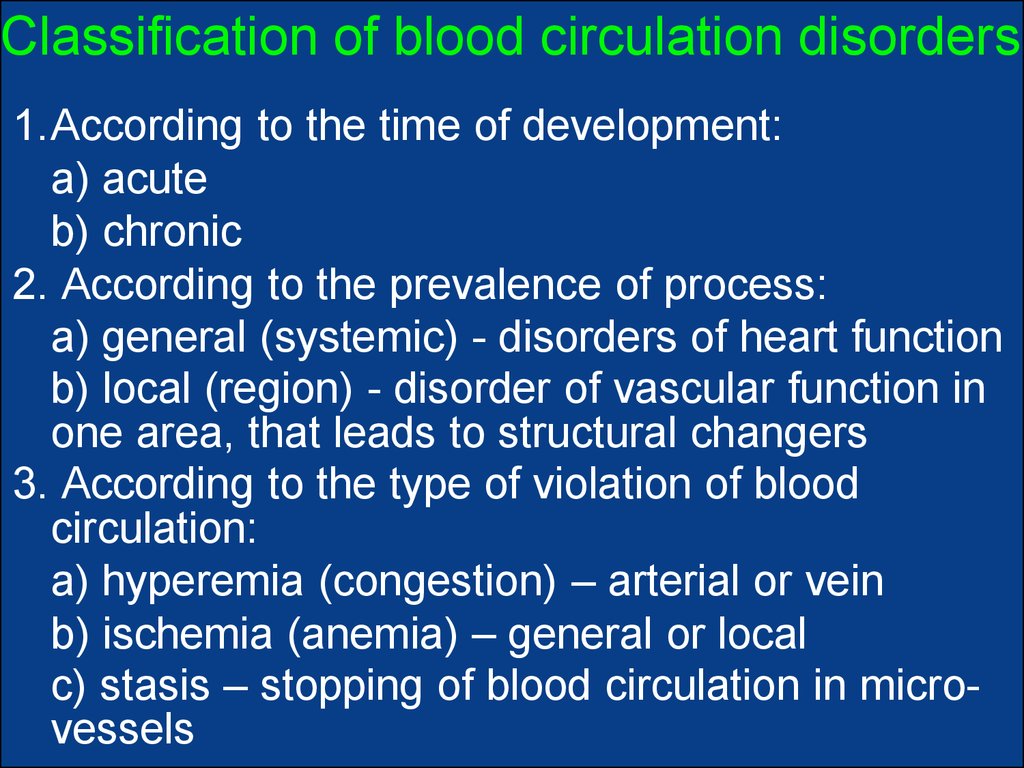
Classification of blood circulation disorders1.According to the time of development:
а) acute
b) chronic
2. According to the prevalence of process:
а) general (systemic) - disorders of heart function
b) local (region) - disorder of vascular function in
one area, that leads to structural changers
3. According to the type of violation of blood
circulation:
а) hyperemia (congestion) – arterial or vein
b) ischemia (anemia) – general or local
c) stasis – stopping of blood circulation in microvessels
5.
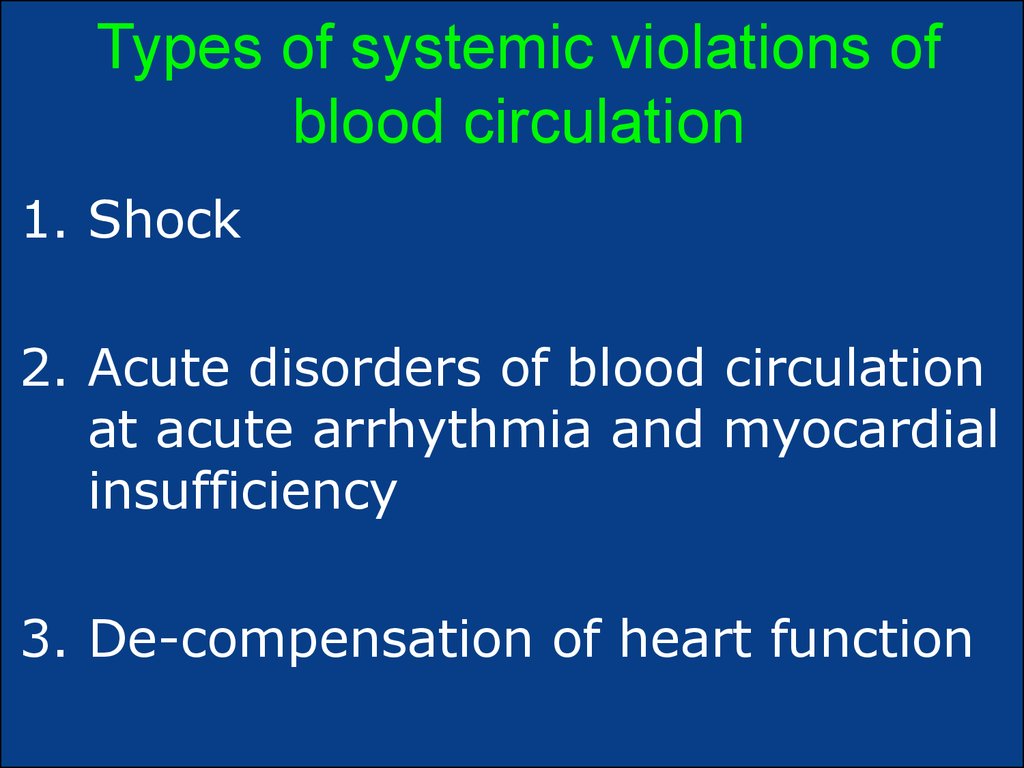
Types of systemic violations ofblood circulation
1. Shock
2. Acute disorders of blood circulation
at acute arrhythmia and myocardial
insufficiency
3. De-compensation of heart function
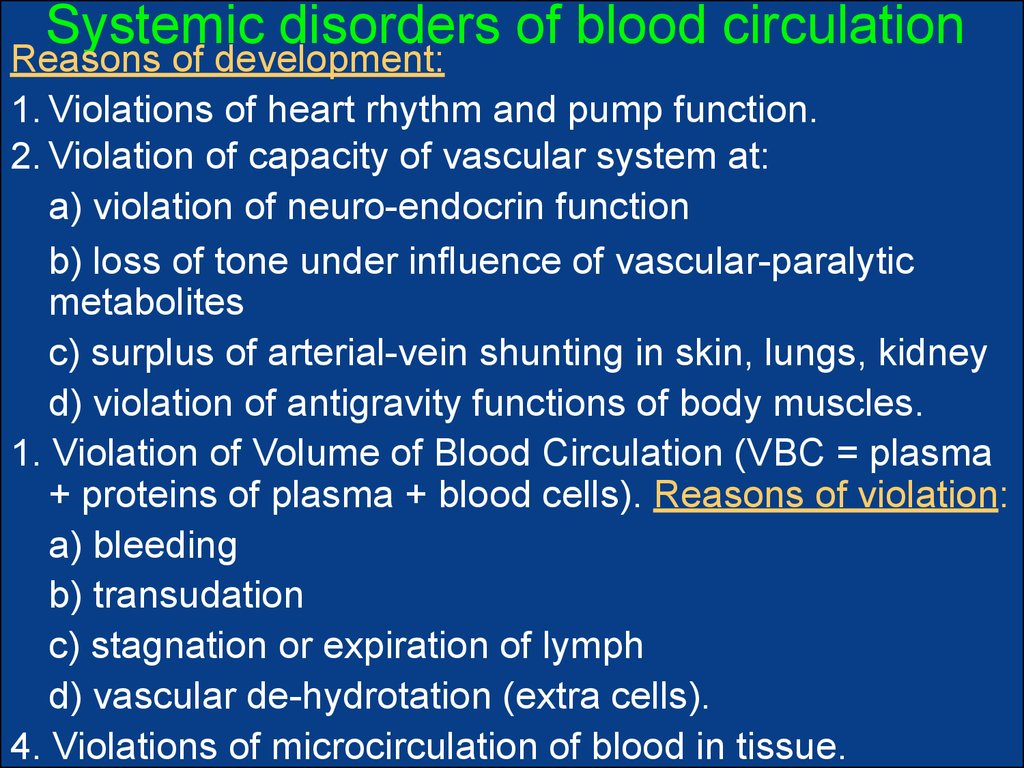
6. Systemic disorders of blood circulation
Reasons of development:1. Violations of heart rhythm and pump function.
2. Violation of capacity of vascular system at:
а) violation of neuro-endocrin function
b) loss of tone under influence of vascular-paralytic
metabolites
c) surplus of arterial-vein shunting in skin, lungs, kidney
d) violation of antigravity functions of body muscles.
1. Violation of Volume of Blood Circulation (VBC = plasma
+ proteins of plasma + blood cells). Reasons of violation:
а) bleeding
b) transudation
c) stagnation or expiration of lymph
d) vascular de-hydrotation (extra cells).
4. Violations of microcirculation of blood in tissue.
7.
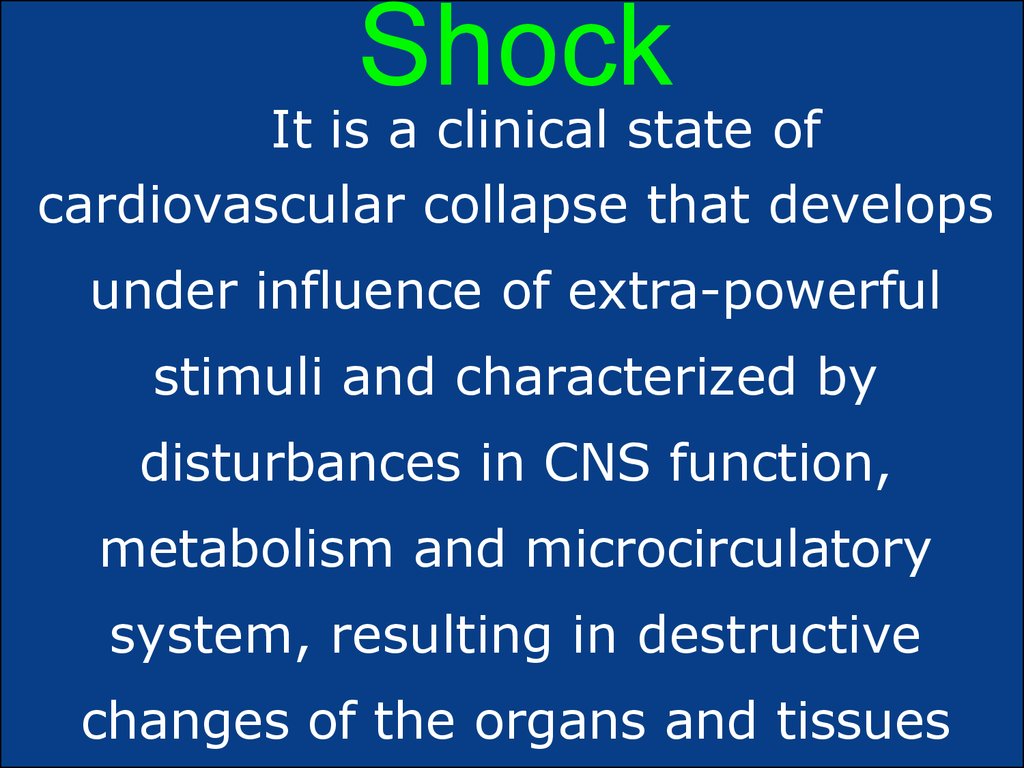
ShockIt is a clinical state of
cardiovascular collapse that develops
under influence of extra-powerful
stimuli and characterized by
disturbances in CNS function,
metabolism and microcirculatory
system, resulting in destructive
changes of the organs and tissues
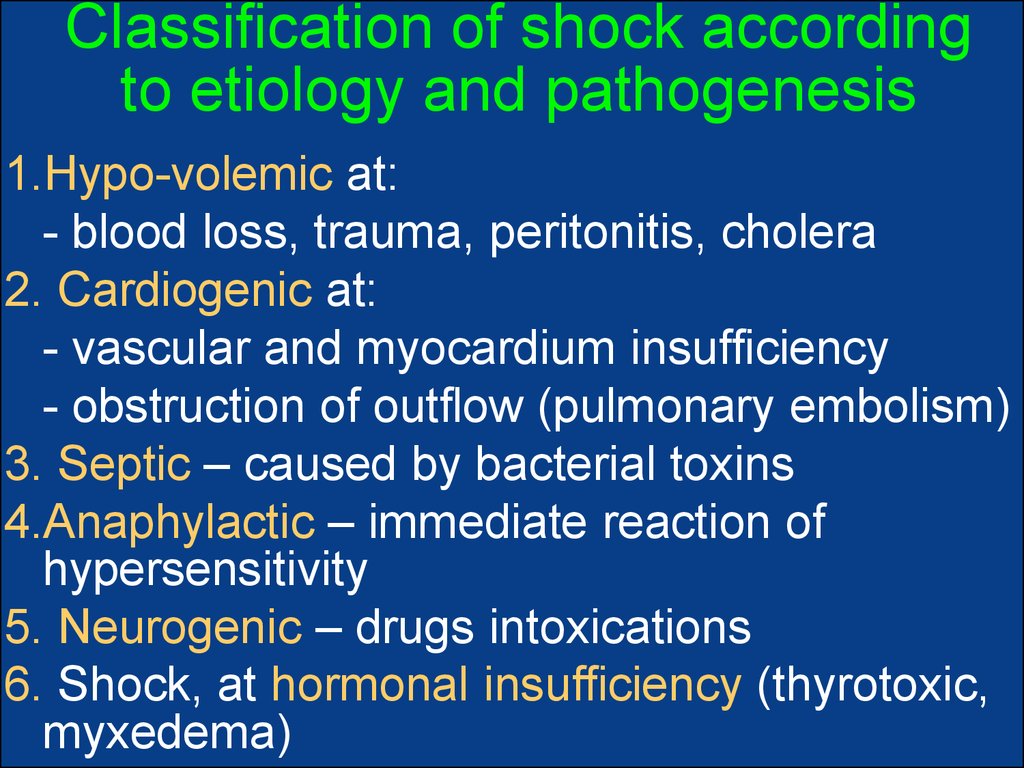
8. Classification of shock according to etiology and pathogenesis
1.Hypo-volemic at:- blood loss, trauma, peritonitis, cholera
2. Cardiogenic at:
- vascular and myocardium insufficiency
- obstruction of outflow (pulmonary embolism)
3. Septic – caused by bacterial toxins
4.Anaphylactic – immediate reaction of
hypersensitivity
5. Neurogenic – drugs intoxications
6. Shock, at hormonal insufficiency (thyrotoxic,
myxedema)
9.
Stages of shock1.Compensation (non-progressive) – it is stage of
centralization of blood circulation:
а) blood come out from organs-depots
b) arteriole-venous shunting began in skin,
lungs, kidneys
c) increased concentration of adrenalin and
noradrenalin (tachycardia, spasm of arteriole)
2.Progressive de-compensative stage – it is
violations of microcirculation in tissue that leads
to acute poly-organ insufficiency
3.Stage of hemodynamic de-compensation
(irreversible) – firm vasodilatation, loss of
sensitiveness to medicines
10.
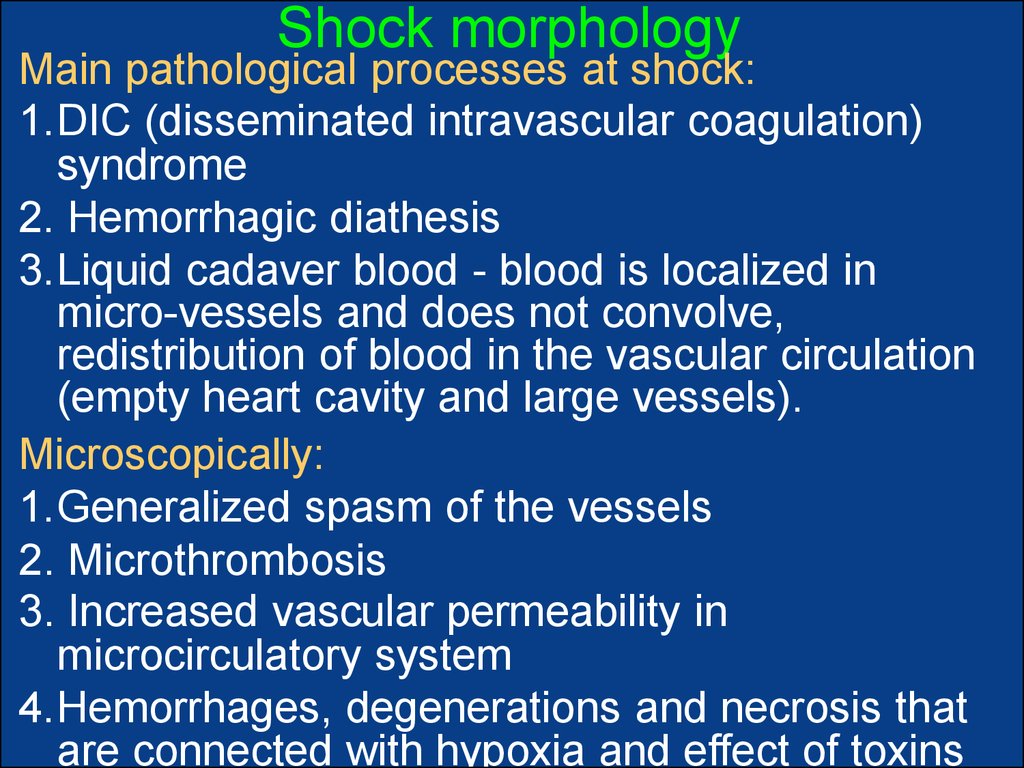
Shock morphologyMain pathological processes at shock:
1.DIC (disseminated intravascular coagulation)
syndrome
2. Hemorrhagic diathesis
3.Liquid cadaver blood - blood is localized in
micro-vessels and does not convolve,
redistribution of blood in the vascular circulation
(empty heart cavity and large vessels).
Microscopically:
1.Generalized spasm of the vessels
2. Microthrombosis
3. Increased vascular permeability in
microcirculatory system
4.Hemorrhages, degenerations and necrosis that
are connected with hypoxia and effect of toxins
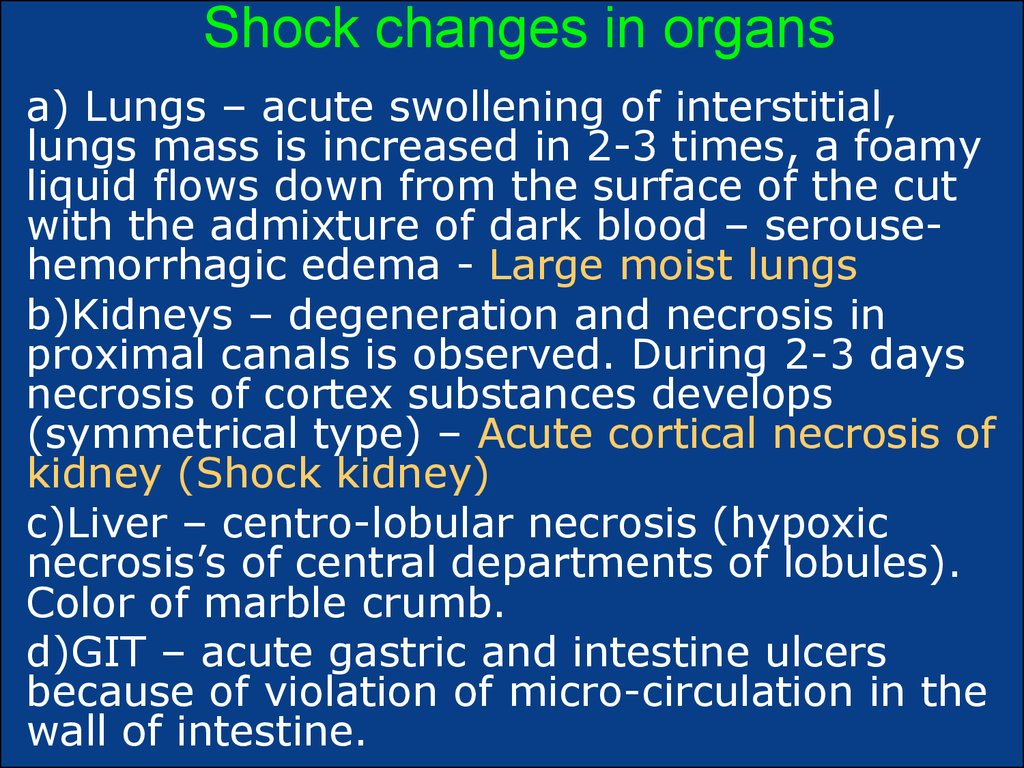
11. Shock changes in organs
а) Lungs – acute swollening of interstitial,lungs mass is increased in 2-3 times, a foamy
liquid flows down from the surface of the cut
with the admixture of dark blood – serousehemorrhagic edema - Large moist lungs
b)Kidneys – degeneration and necrosis in
proximal canals is observed. During 2-3 days
necrosis of cortex substances develops
(symmetrical type) – Acute cortical necrosis of
kidney (Shock kidney)
c)Liver – centro-lobular necrosis (hypoxic
necrosis’s of central departments of lobules).
Color of marble crumb.
d)GIT – acute gastric and intestine ulcers
because of violation of micro-circulation in the
wall of intestine.
12.
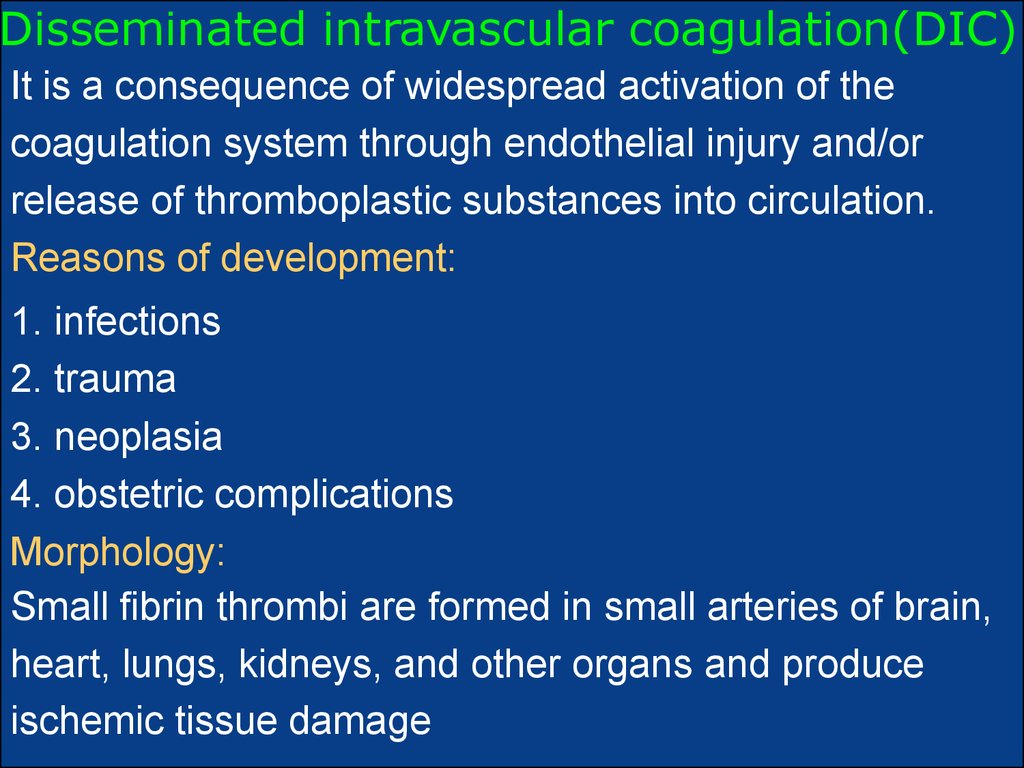
Disseminated intravascular coagulation(DIC)It is a consequence of widespread activation of the
coagulation system through endothelial injury and/or
release of thromboplastic substances into circulation.
Reasons of development:
1. infections
2. trauma
3. neoplasia
4. obstetric complications
Morphology:
Small fibrin thrombi are formed in small arteries of brain,
heart, lungs, kidneys, and other organs and produce
ischemic tissue damage
13.
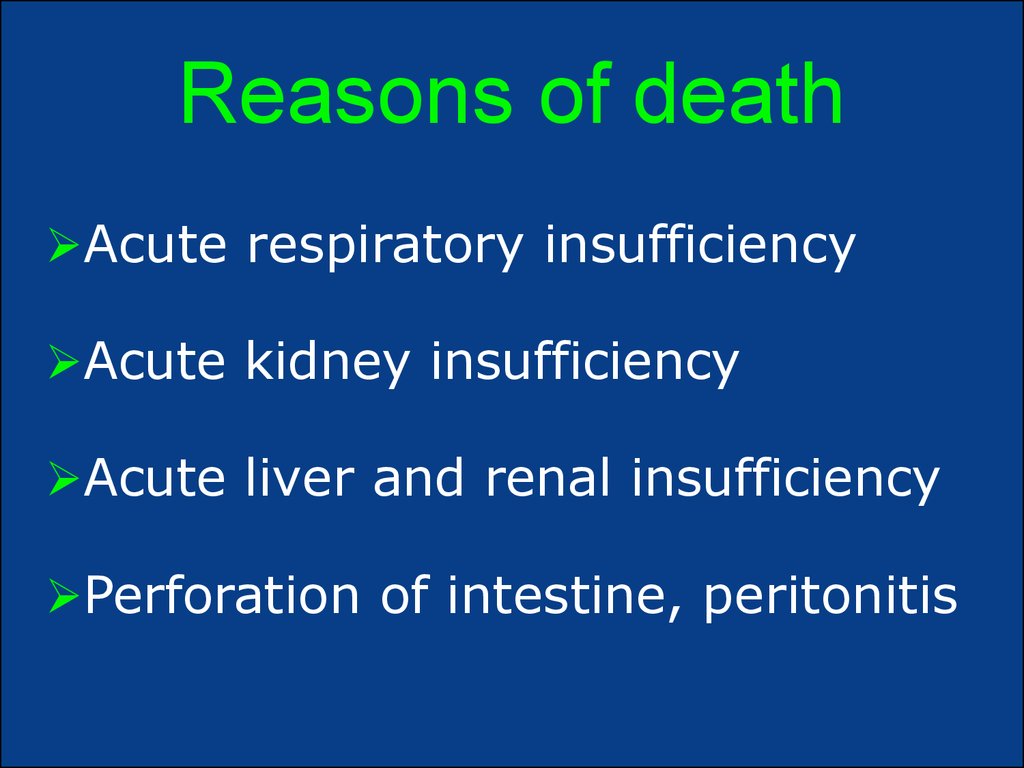
Reasons of deathAcute respiratory insufficiency
Acute kidney insufficiency
Acute liver and renal insufficiency
Perforation of intestine, peritonitis
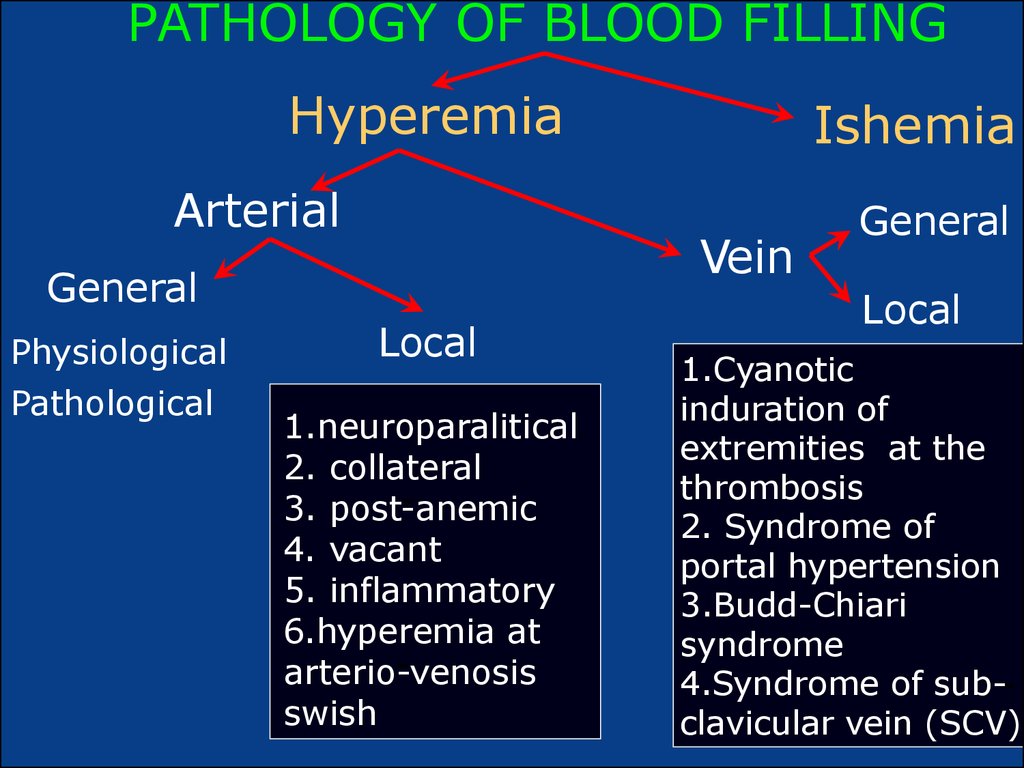
14. PATHOLOGY OF BLOOD FILLING
HyperemiaArterial
Vein
General
Physiological
Pathological
Ishemia
Local
1.neuroparalitical
2. collateral
3. post-anemic
4. vacant
5. inflammatory
6.hyperemia at
arterio-venosis
swish
General
Local
1.Cyanotic
induration of
extremities at the
thrombosis
2. Syndrome of
portal hypertension
3.Budd-Chiari
syndrome
4.Syndrome of subclavicular vein (SCV)
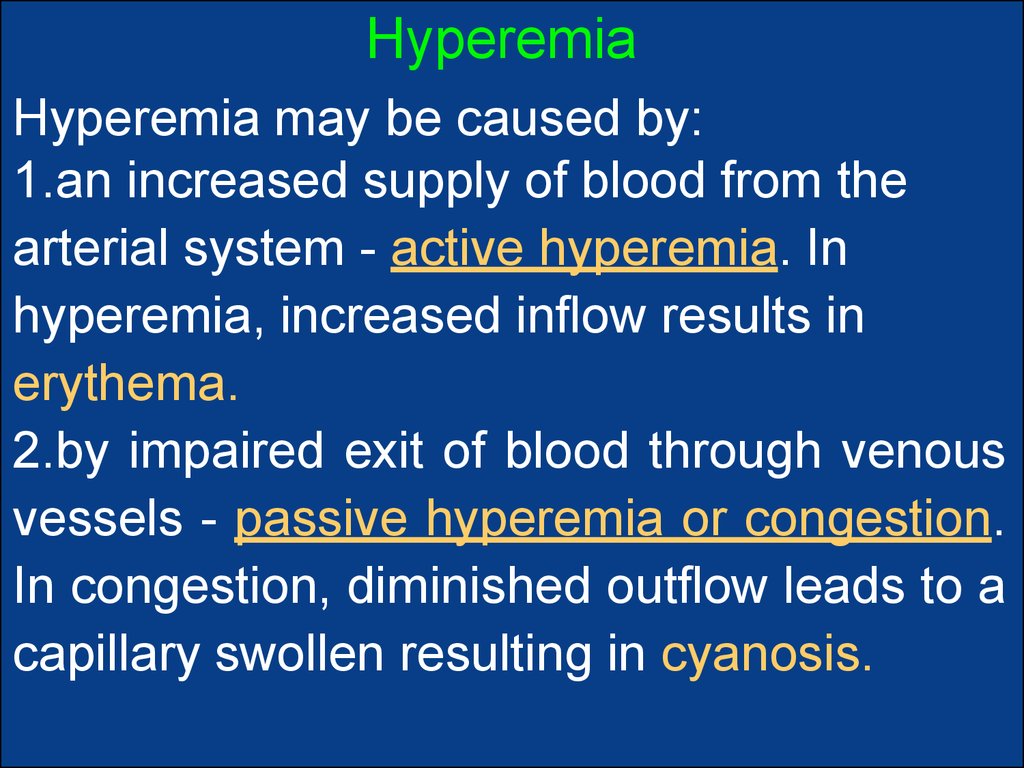
15. Hyperemia
Hyperemia may be caused by:1.an increased supply of blood from the
arterial system - active hyperemia. In
hyperemia, increased inflow results in
erythema.
2.by impaired exit of blood through venous
vessels - passive hyperemia or congestion.
In congestion, diminished outflow leads to a
capillary swollen resulting in cyanosis.
16.
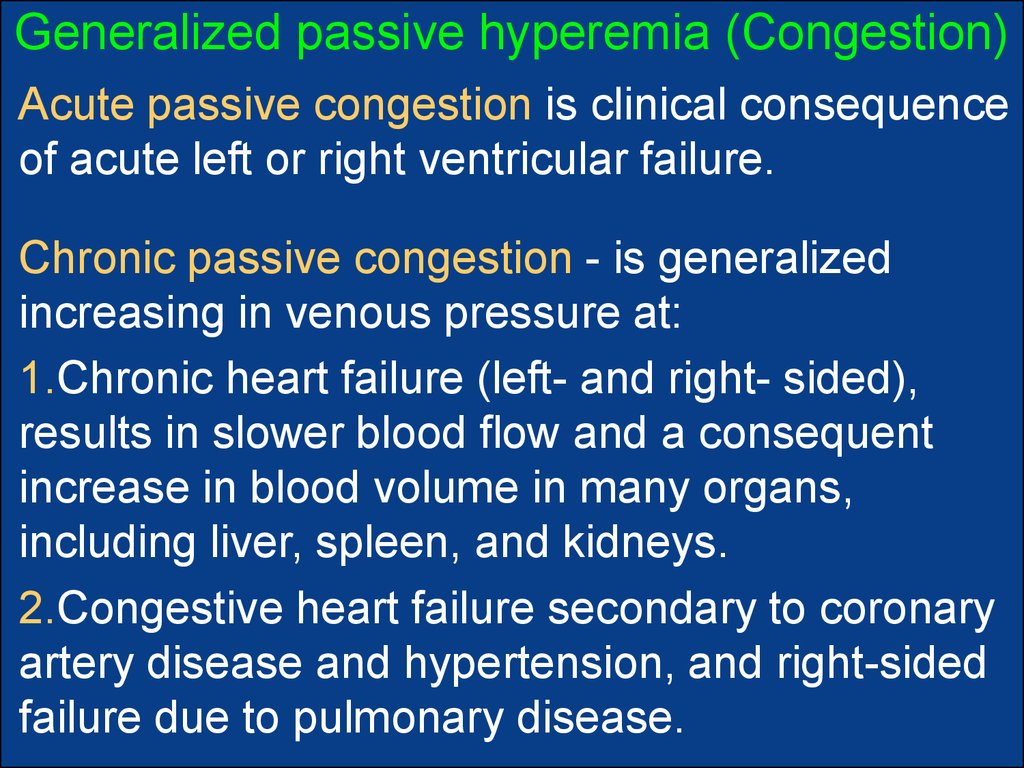
Generalized passive hyperemia (Congestion)Acute passive congestion is clinical consequence
of acute left or right ventricular failure.
Chronic passive congestion - is generalized
increasing in venous pressure at:
1.Chronic heart failure (left- and right- sided),
results in slower blood flow and a consequent
increase in blood volume in many organs,
including liver, spleen, and kidneys.
2.Congestive heart failure secondary to coronary
artery disease and hypertension, and right-sided
failure due to pulmonary disease.
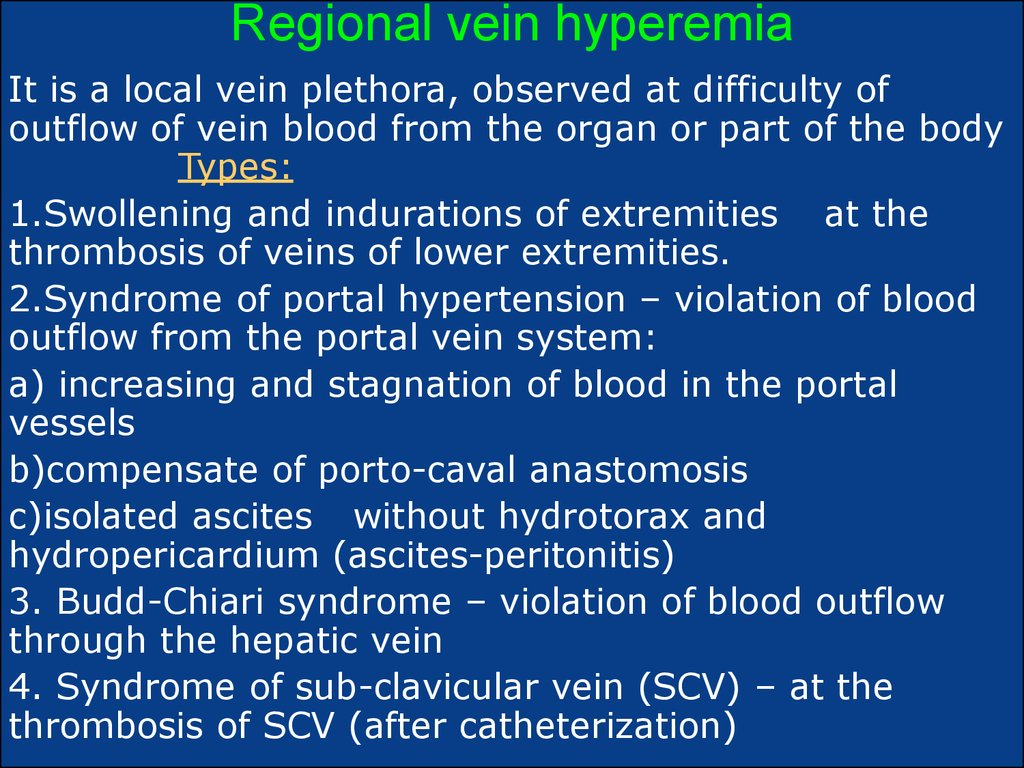
17. Regional vein hyperemia
It is a local vein plethora, observed at difficulty ofoutflow of vein blood from the organ or part of the body
Types:
1.Swollening and indurations of extremities at the
thrombosis of veins of lower extremities.
2.Syndrome of portal hypertension – violation of blood
outflow from the portal vein system:
а) increasing and stagnation of blood in the portal
vessels
b)compensate of porto-caval anastomosis
c)isolated ascites without hydrotorax and
hydropericardium (ascites-peritonitis)
3. Budd-Chiari syndrome – violation of blood outflow
through the hepatic vein
4. Syndrome of sub-clavicular vein (SCV) – at the
thrombosis of SCV (after catheterization)
18.
Arterial plethoraArterial plethora (active hyperemia) is promoted bloodinvolving of organ or tissue because of arising up of
arterial blood inflow. Can be:
1. Physiologic - at increased functional demand of heart
and skeletal muscle during exercise.
2. Pathological
Types, according to distribution:
1. general - is observed at the increased volume of
circulatory blood or number of red cells. In such cases
are marked red coloring of skin and mucous
membranes and high arterial pressure
2. local – at inflammation or at different reasons.
19. Bleeding
Bleeding (hemorrhage) — it iscoming out of blood from the
blood vessel or cavity of heart
to the surrounding outpace
(outward bleeding) or into the
tissue or cavity of body (inlaying
bleeding).
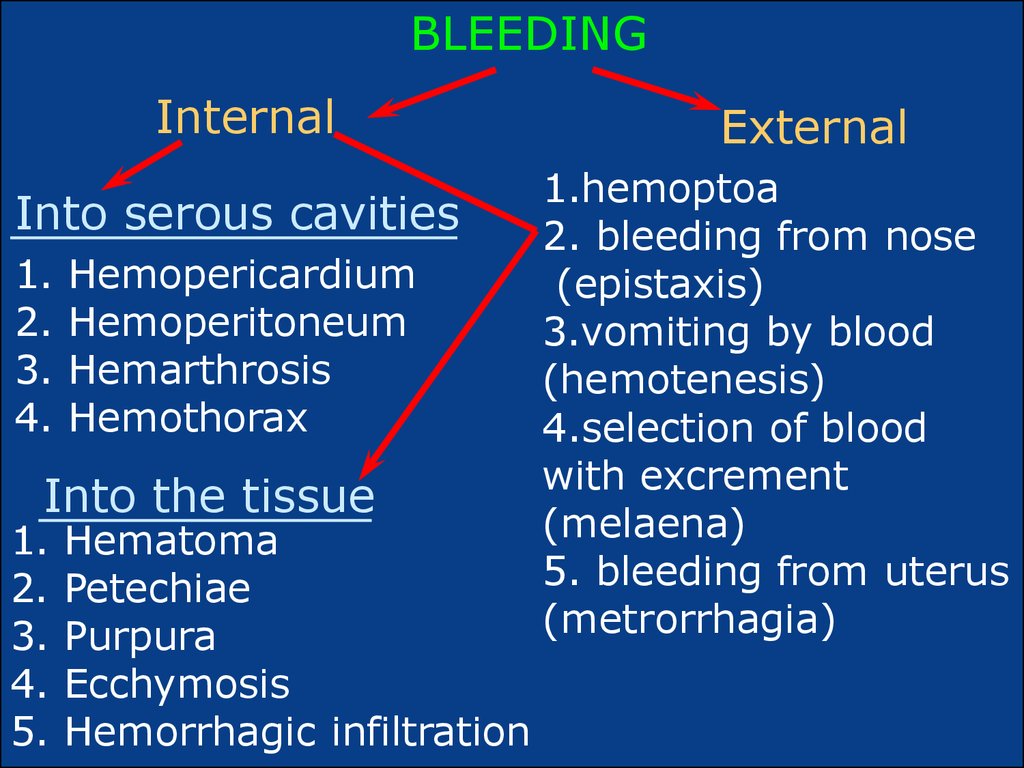
20. BLEEDING
InternalInto serous cavities
1.
2.
3.
4.
Hemopericardium
Hemoperitoneum
Hemarthrosis
Hemothorax
Into the tissue
1.
2.
3.
4.
5.
Hematoma
Petechiae
Purpura
Ecchymosis
Hemorrhagic infiltration
External
1.hemoptoa
2. bleeding from nose
(epistaxis)
3.vomiting by blood
(hemotenesis)
4.selection of blood
with excrement
(melaena)
5. bleeding from uterus
(metrorrhagia)
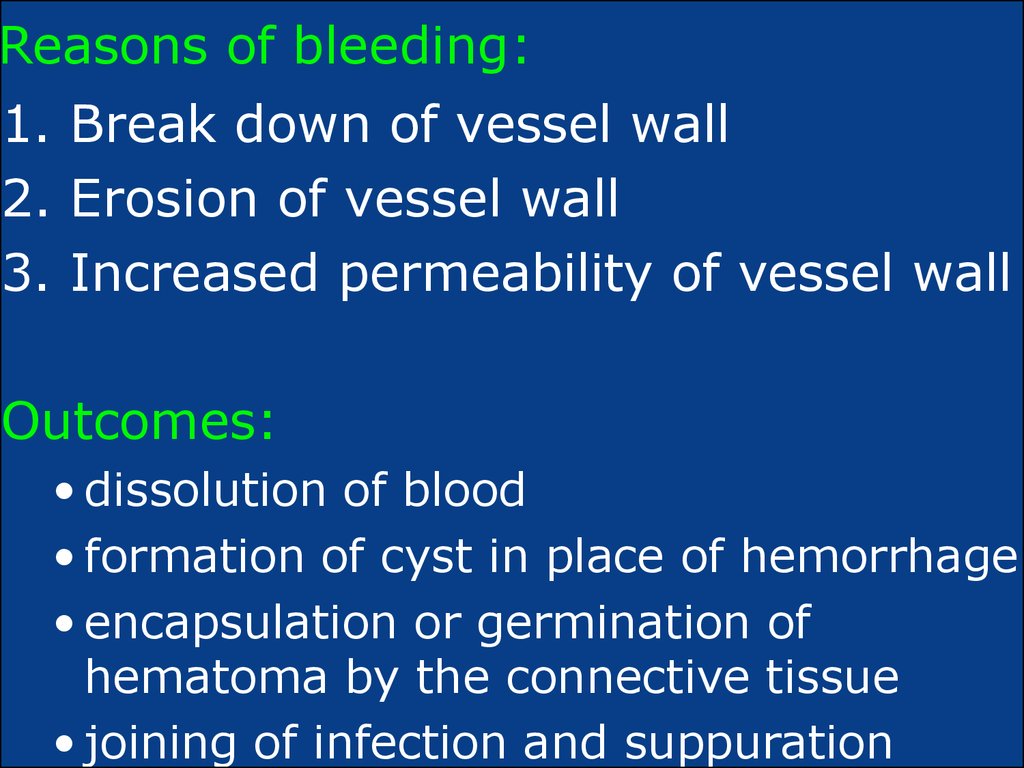
21.
Reasons of bleeding:1. Break down of vessel wall
2. Erosion of vessel wall
3. Increased permeability of vessel wall
Outcomes:
• dissolution of blood
• formation of cyst in place of hemorrhage
• encapsulation or germination of
hematoma by the connective tissue
• joining of infection and suppuration
22.
Thrombosis – It is rolling up of blood in thevessels or chambers of heart during life.
Formation of a clotted mass of blood in the
non-interrupted cardiovascular system. Basis
of thrombosis is the physiological process of
rolling up.
Thrombosis refers to the formation of a
thrombus – it is aggregate of coagulated blood
containing platelets, fibrin, and cellular
elements.
23. Virchow triad in thrombosis
1.Endothelial integrity is the single mostimportant factor,
2. Local blood flow and/or coagulability;
3. Abnormal blood flow (stasis or turbulence)
The elements of the triad may act independently or may
combine to cause thrombus formation.
24. Thrombosis macroscopically
It is necessary to distinguish a blood clotfrom the postmortem clot:
1.A thrombus is related closely to the wall
of blood vessel, and postmortem clot lies
freely.
2.A thrombus has dim, sometimes even
rough surface (lines of Zahn), and at
postmortem clot surface is smooth.
3. A thrombus has fragile consistency, while
consistency of postmortem clot is jam-like.
25.
Classification of thrombus, according tocomposition
1.red blood clot – red coloring, quickly
appears and consists of red cells mainly
2.white – yellow-white color, slowly
appears in arteries, leucocytes prevail in
composition
3. mixed
4.hyaline – in the vessels of different
tissue, plasma proteins prevail in
composition above the cells of blood.
26. Classification according to the relation to vessel’s walls
1.obstructive, that means, that a vessel isclosed by mass of blood clot
2. near-wall
3.spherical blood clots - in the chambers
of heart and in aneurism
4. dilatational
5. thromb-endocarditis – at the damage of
endocardium
6. axial – with the longitudinal axis (head,
body, tail)
27.
Outcomes1. organization - germination by the connecting
tissue
2. petrification - deposition of calcium salts in the
blood clot (in vein)
3. dissolution - aseptic autolysis
4. medicinal fibrinolisis
5. re-canalization of blood clot
6. propagandation
7. infected of blood clot with set about its particles
on organs with forming of abscesses
8. embolization
28. Outcomes of thrombosis
Arterial thrombi occlude the vesseland lead to ischemic necrosis of
tissue (infarct).
1.Thrombosis of a coronary or
cerebral artery results:
- myocardial infarct (heart attack)
- cerebral infarct (stroke),
2. End-arteries that are affected by
atherosclerosis and often suffer
thrombosis:
- mesenteric arteries (intestinal
infarction),
- renal arteries (kidney infarcts),
- arteries of the leg (gangrene).
29. Embolism
An embolism is the sudden blockage ofthe venous or arterial circulations by
any material that can lodge in a blood
vessel and obstruct its lumen.
The most common embolus is a
thromboembolus that is, a thrombus
formed in one location that detaches
from a vessel wall at its point of origin
and travels to a distant site.






 Медицина
Медицина