Похожие презентации:
Pathophysiology of the liver failure
1.
Pathophysiology of liverfailure
2.
Basic liver functionsparticipation in the metabolism of carbohydrates,
fats and proteins (synthesis of amino acids, urea,
plasma proteins, glycogen, cholesterol,
gluconeogenesis, etc.)
synthesis of hemostatic factors
synthesis and secretion of bile
barrier (detoxification) function
participation in the regulation of total blood volume
participation in the exchange of microelements
(iron, copper) and vitamins
participation in hormone metabolism
hematopoiesis in the fetus
Kupffer cells – a protective function
3.
Liver failureis a condition in which one or more
liver functions decrease below the
level necessary to ensure normal
functioning of the body.
4.
Classification of liver failureDownstream
- acute - chronic
By the number of broken functions
- partial (glycogenosis - glycogen storage
disease; Gilbert`s sd – enzymopathic
jaundice)
- total (most of the liver pathologies)
By etiology and pathogenesis
- hepatic-cellular
- hepatic-vascular
- cholestatic
5.
Etiology of liver failure1. Hepatic-cellular:
Viral (A, B, C, D, E,G... ), toxic hepatitis,
autoimmune hepatitis
dystrophy (including alcoholic, fatty,
carbohydrate)
mechanical injuries
parasitic infections (alveococcosis,
echinococcosis)
tumors, etc.
2. Hepatic-vascular:
hepatic circulatory disorders (portal vein
thrombosis, hepatic veins, hepatic artery,
shock)
3. Cholestatic:
acute ore chronic violation of the outflow of
bile (gallstones, tumors, primary biliary
cholangitis
6.
Acute liver failureEtiology: acute hepatitis, injuries, portal
vein thrombosis, hepatic veins, "shock"
liver, etc.
The leading value is a violation of the
detoxification function of the liver
7.
Chronic liver failureEtiology-chronic hepatitis, cirrhosis of
the liver, parasitic infestations, tumor
growth
The main value is a violation of all
types of metabolism and a decrease in
the detoxification function of the liver
8.
Viral hepatitisCentral link - cytolysis syndrome
HAV (hepatitis A virus) and HEV have a
direct cytopathogenic effect on hepatocytes
→ acute hepatitis
In hepatitis B (HBV), C (HCV) and D (HDV)
- immune damage to hepatocytes (mainly
associated with the cellular link of immunity
- Tctl) – apoptosis, cytolysis → chronic
hepatitis
9.
Alcoholic liver diseaseAverage daily dose of pure ethanol:
more than 40-80 g for men; more than
20 g for women; 10-12 years old
Liver steatosis – fatty degeneration
Alcoholic hepatitis - subacute
inflammation of the liver tissue
Cirrhosis of the liver
10.
PathogenesisAcetaldehyde causes:
gain lipid peroxidation (LP)
mitochondrial dysfunction
suppression of DNA repair and enhancement of
apoptosis
disruption of microtubule function due to the formation
of acetaldehyde-protein complexes. Microtubule
tubulin polymerization is disrupted, and Mallory
corpuscles appear
formation of complexes with proteins, violation of the
function of phospholipids of cell membranes
stimulation of collagen synthesis and fibrosis
development
immune disorders
disorders of lipid metabolism: the level of free fatty
acids increases, fatty liver develops
11.
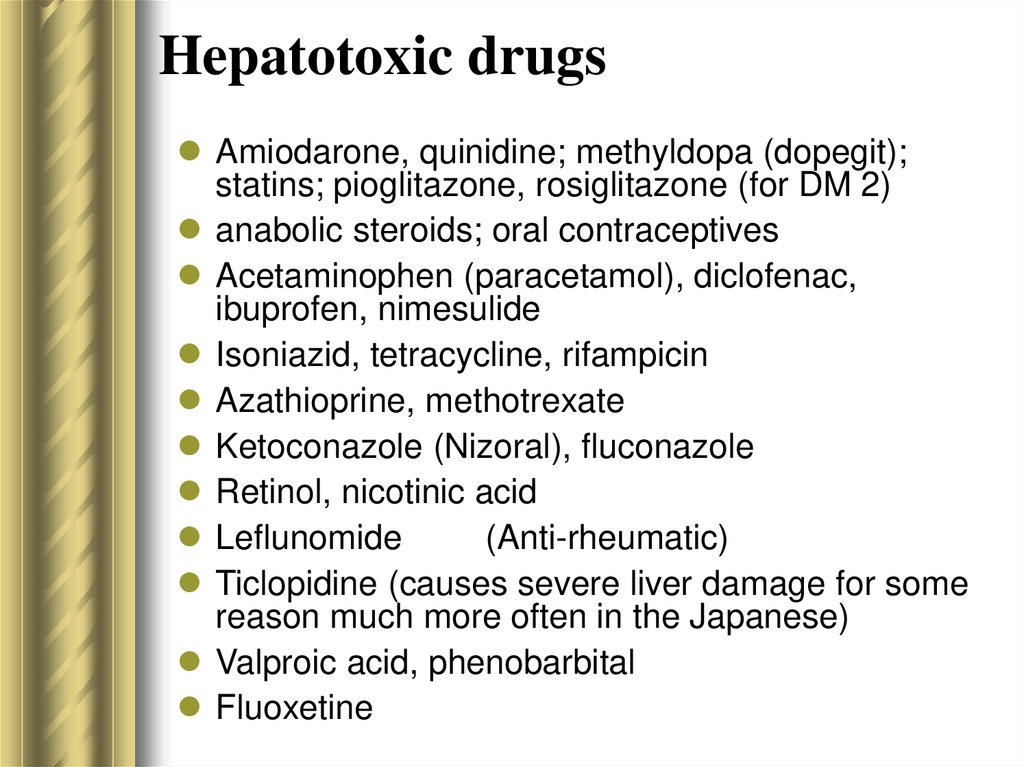
Hepatotoxic drugsAmiodarone, quinidine; methyldopa (dopegit);
statins; pioglitazone, rosiglitazone (for DM 2)
anabolic steroids; oral contraceptives
Acetaminophen (paracetamol), diclofenac,
ibuprofen, nimesulide
Isoniazid, tetracycline, rifampicin
Azathioprine, methotrexate
Ketoconazole (Nizoral), fluconazole
Retinol, nicotinic acid
Leflunomide
(Anti-rheumatic)
Ticlopidine (causes severe liver damage for some
reason much more often in the Japanese)
Valproic acid, phenobarbital
Fluoxetine
12.
Metabolic disorders inhepatic failure
13.
Violations of nitrogen metabolismViolation of deamination of
amino acids (AA) and amines
Hyperaminoacidemia
↑ histamine levels
Hyperemia
of the skin,
Low blood
pressure
Hyperaminoaciduria
(amino acids loss)
Accumulation
aromatic AA
(cerebrotoxic
action)
!!!Breaking the transformation
ammonia to urea
and increased ammonia level
Reduced synthesis
of plasma proteins
System violations
hemostasis –
hemorrhagic syndrome
Reducing the oncotic effect
plasma proteins –
ascites, hydrothorax, edema
Transport violations
iron, copper, BAS, etc. IDA (iron deficiency anemia),
hyperthyroidism
Immune system disorders
14.
Disorders of carbohydratemetabolism
Impaired glucose storage as glycogen →
postprandial (after meal) hyperglycemia and
fasting (between meals) hypoglycemia
Violation of gluconeogenesis from fructose, AA,
FA (fatty acids) → tendency to hypoglycemia
Increased blood insulin levels
15.
Disorders of fat metabolismImpaired fatty acid metabolism → ketoacidosis
Impaired cholesterol and lipoprotein synthesis
→ hypocholesterolemia
Deposition of neutral fats in hepatocytes – fatty
liver disease
Violation of steroid hormone metabolism →
hyperestrogenemia, secondary
hyperaldosteronism
16.
Disorders of pigment metabolismFirst stage (pre-jaundice): appearance in blood and
urine urobilinogen (damage to the enzyme
mechanisms of its capture and oxidation); high
blood levels of hepatic transaminases (AST, ALT).
17.
Disorders of pigment metabolismSecond stage (jaundice)
Damaged hepatocytes secrete bile into the blood.
Compression of the bile capillaries by damaged
edematous hepatocytes makes it difficult to
evacuate bile → increase its resorption into the
blood capillaries → cholestasis syndrome
(hypocholia; cholemia - the appearance of free bile
acids in the blood, increased levels of direct
bilirubin, its appearance in the urine).
The process of conjugation of indirect bilirubin with
glucuronic acid is disrupted, the level of indirect
bilirubin slightly increases
18.
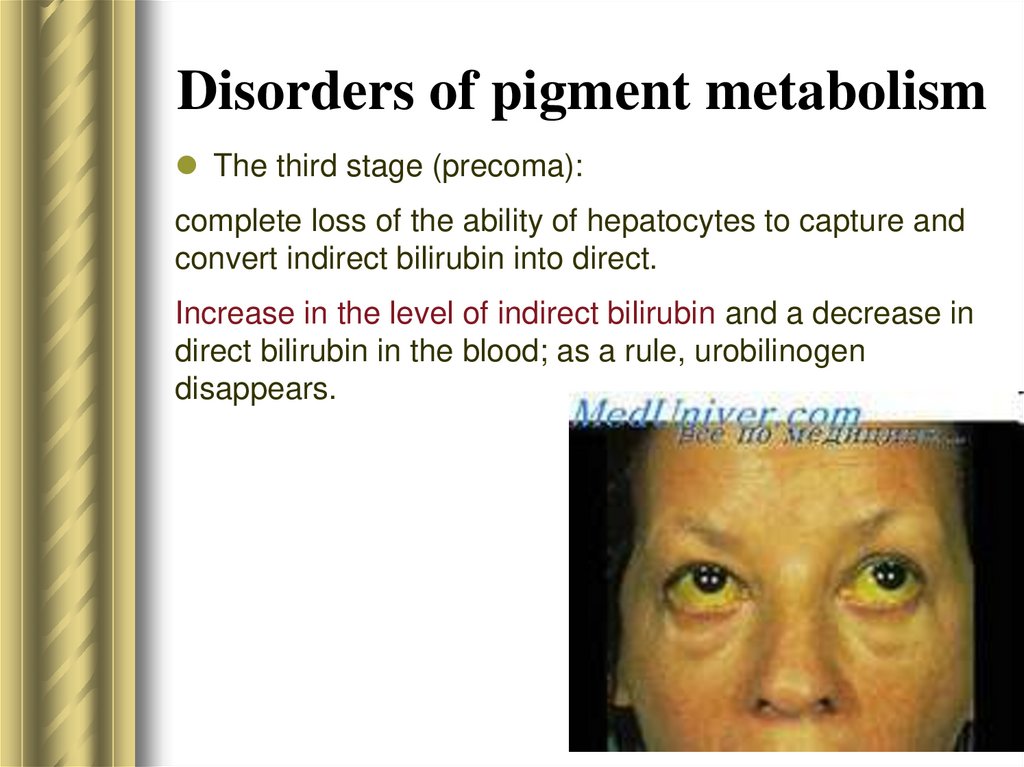
Disorders of pigment metabolismThe third stage (precoma):
complete loss of the ability of hepatocytes to capture and
convert indirect bilirubin into direct.
Increase in the level of indirect bilirubin and a decrease in
direct bilirubin in the blood; as a rule, urobilinogen
disappears.
19.
Violation of detoxificationfunction
! Violation of the conversion of ammonia to urea.
Ammonia converts alpha-ketoglutaric acid to
glutamic acid → alpha-ketoglutaric acid deficiency
→ reduced oxidation and phosphorylation
processes → ATP deficiency.
Ammonia weakens the inhibitory processes in the
central nervous system, contributes to the
occurrence of hyperkinesis and convulsions.
In high concentrations, ammonia irritates the
respiratory center and increases shortness of
breath.
20.
Violation of detoxificationfunction
Development of intestinal
autointoxication (indole, skatole,
phenols, cadaverine, putrescine)
Violation of the metabolism of drugs,
alcohol
21.
Acute hepatic-cellularinsufficiency
Development of massive liver necrosis:
progressive reduction of its size - "melting liver"
syndrome
Cytolysis syndrome. A higher rise in AsAT
compared to AlAT is a bad sign
The level of procoagulants (prothrombin,
fibrinogen), cholesterol, and albumin in the
blood decreases
"Hepatic" bad breath, jaundice, bleeding, and
progressive signs of encephalopathy
22.
Acute hepatic-cellularinsufficiency
Accumulation of cerebrotoxic substances (disrupt the
energy balance and transmission of nerve impulses),
synthesis of false neurotransmitters, hypoglycemia due to
inhibition of gluconeogenesis
Metabolic acidosis is associated with the accumulation of
lactic and pyruvic acids (impaired permeability of cell
membranes can cause brain edema), causes
hyperventilation and respiratory alkalosis
Pronounced hyperbilirubinemia mainly due to the growth of
the conjugated form
Arterial hypotension worsens the violation of blood flow in
the liver and causes the development of acute renal failure,
as well as contributes to a violation of mental status and
the progression of tissue hypoxia
23.
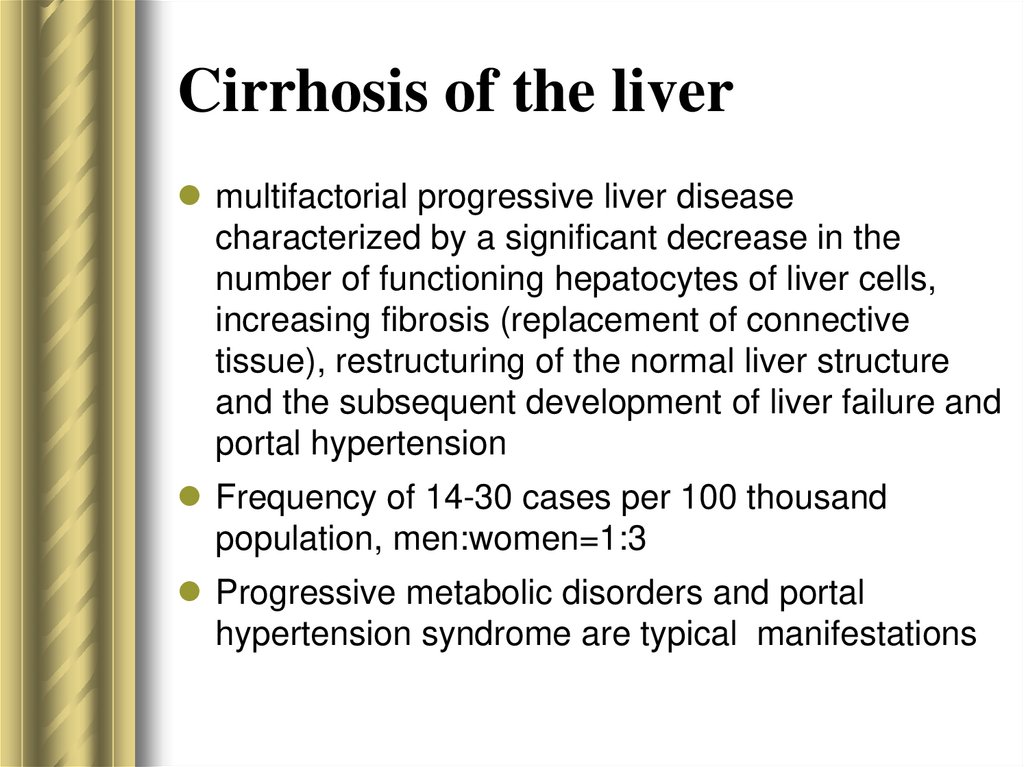
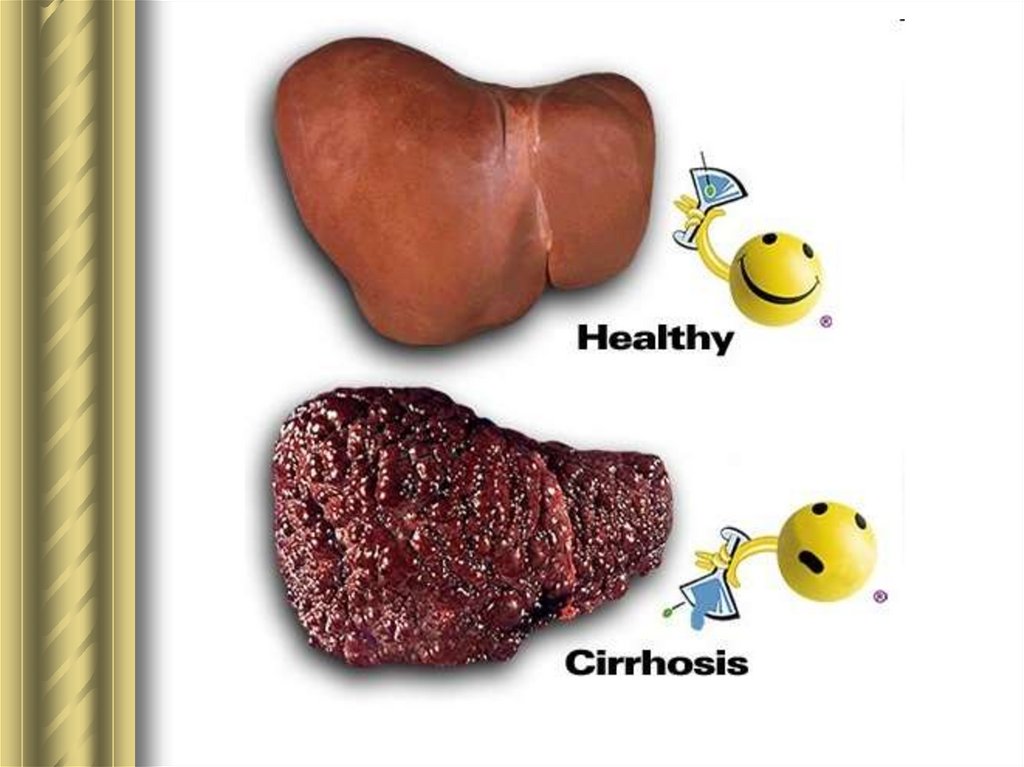
Cirrhosis of the livermultifactorial progressive liver disease
characterized by a significant decrease in the
number of functioning hepatocytes of liver cells,
increasing fibrosis (replacement of connective
tissue), restructuring of the normal liver structure
and the subsequent development of liver failure and
portal hypertension
Frequency of 14-30 cases per 100 thousand
population, men:women=1:3
Progressive metabolic disorders and portal
hypertension syndrome are typical manifestations
24.
25.
Portal hypertensionsyndrome
26.
Portal hypertension syndromesyndrome of increased pressure in the
portal vein system caused by impaired
blood flow in the portal vessels,
hepatic veins and inferior vena cava
increased pressure in the portal vein
system above 12 mmHg.
27.
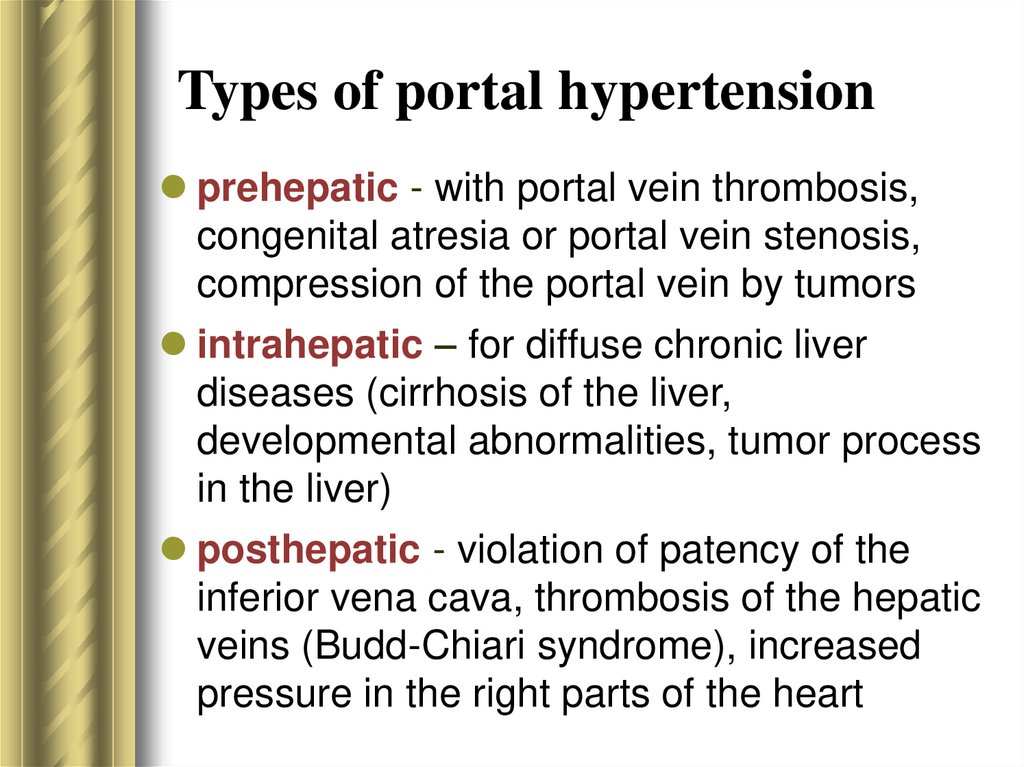
Types of portal hypertensionprehepatic - with portal vein thrombosis,
congenital atresia or portal vein stenosis,
compression of the portal vein by tumors
intrahepatic – for diffuse chronic liver
diseases (cirrhosis of the liver,
developmental abnormalities, tumor process
in the liver)
posthepatic - violation of patency of the
inferior vena cava, thrombosis of the hepatic
veins (Budd-Chiari syndrome), increased
pressure in the right parts of the heart
28.
Manifestations of the portalhypertension syndrome
29.
Portocaval anastomoses openinganastomoses in the area of the cardiac part
of the stomach and abdominal part of the
esophagus (vena cava superior and portal
vein)
anastomoses between the upper, middle
and lower rectal veins (vena cava inferior
and portal vein)
anastomoses between the external
abdominal veins and the umbilical vein
(cava-porto-caval anastamoses)
30.
Portocaval anastamoses"+"- reduction of pressure in the portal vein
system
"- "- blood bypass surgery, ingestion of
substances coming from the intestines into
the systemic bloodstream, without
neutralization in the liver; intestinal
autointoxication
"- "- bleeding from dilated veins (high
pressure in the veins, disorders in the
hemostatic system)
31.
Splenomegaly and hypersplenismMechanism-violation of venous outflow
from the splenic vein
Venous congestion and increased
organ volume
Slowing of blood flow, increasing the
time of contact of blood cells with
spleen phagocytes → increased
destruction of blood elements
32.
Ascitesaccumulation of fluid (transudate) in the
abdominal cavity
Effects:
increased intra-abdominal pressure →
- restriction of respiratory movements of the
lungs
- violation of the heart's activity
- increased resistance to blood flow in the
abdominal organs
33.
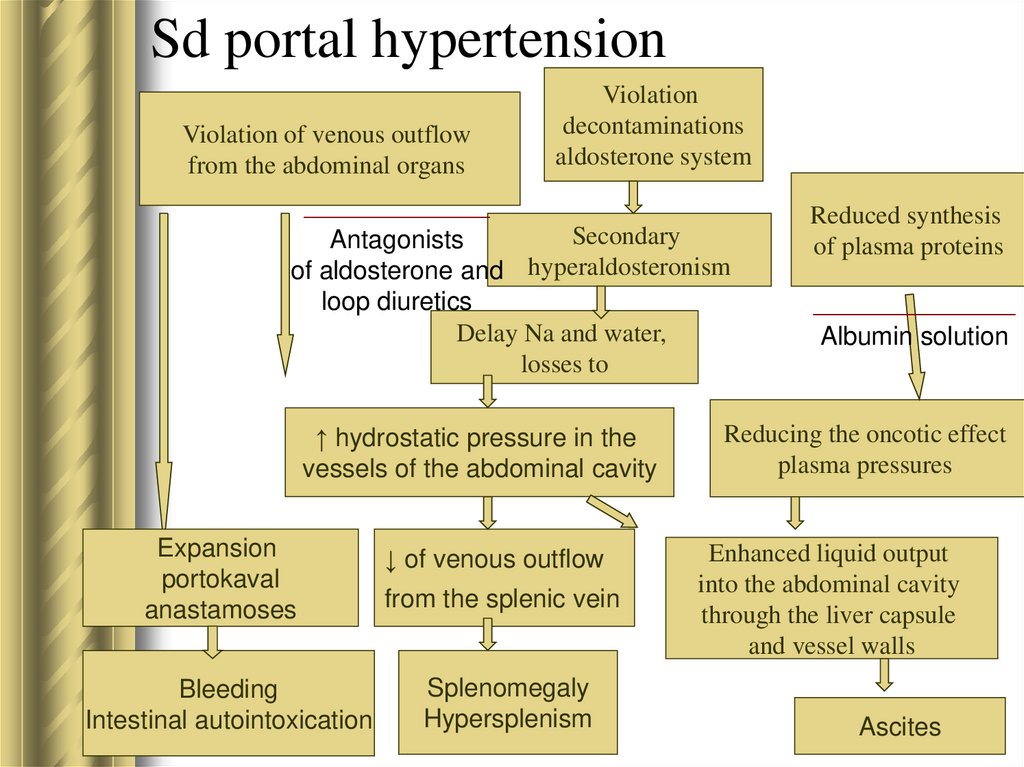
Sd portal hypertensionViolation of venous outflow
from the abdominal organs
Violation
decontaminations
aldosterone system
Secondary
Antagonists
of aldosterone and hyperaldosteronism
loop diuretics
Delay Na and water,
losses to
↑ hydrostatic pressure in the
vessels of the abdominal cavity
Expansion
portokaval
anastamoses
↓ of venous outflow
Bleeding
Intestinal autointoxication
Splenomegaly
Hypersplenism
from the splenic vein
Reduced synthesis
of plasma proteins
Albumin solution
Reducing the oncotic effect
plasma pressures
Enhanced liquid output
into the abdominal cavity
through the liver capsule
and vessel walls
Ascites
34.
Hepatic encephalopathy35.
Pathogenesis of hepaticencephalopathy and coma
Metabolic theory: impaired detoxification function of
the liver and the effect of toxic compounds on the
central nervous system
Shunted blood containing the end products of
protein breakdown bypasses the liver and enters
the systemic circulation
Ammonia, low-molecular-weight fatty acids
(gamma-aminobutyric acid), serotonin, false
mediators (tyramine, octapramine, etc.), acting on
the brain, cause a violation of energy metabolism,
transmission of nerve impulses
36.
Stages of hepatic encephalopathyStage 1 (prodromal): prevalence of emotional and mental
disorders.
Behavioral disorders, emotional instability, anxiety, apathy,
euphoria, slow thinking. Mental reactions and speech are
slowed down, some psychomotor agitation is possible, but
orientation and criticism are preserved.
Stage 2 (precoma): deepening of mental and neurological
disorders.
Patients commit meaningless acts. Delirious states with
seizures and motor arousal occur periodically, during which
patients become aggressive. Ataxia, dysarthria, dysgraphy
appear, reflexes are increased. Deafness develops, and
consciousness is often confused. Breathing is rapid and
deep.
37.
Stages of hepatic encephalopathyStage 3 (stupor). Patients in a coma with periodic
awakenings. The reaction to the light of the pupils
persists, trismus, fibrillar twitching and muscle spasms,
urinary incontinence are noted. Jaundice is pronounced,
petechiae and hemorrhages appear on the skin.
Gastrointestinal bleeding may occur. There is tachycardia
with a decrease in blood pressure. Respiratory rate
increased.
Stage 4 (hepatic coma) - loss of consciousness, reactions
to painful stimuli disappear. There is rigidity of the
muscles of the extremities, occiput. In the terminal phase,
the pupils dilate, the reaction to light disappears, and the
reflexes fade.
The prognosis for stages 1 and 2 of hepatic
encephalopathy is favorable, and in stages 3 and 4 it is
much worse.
38.
39.
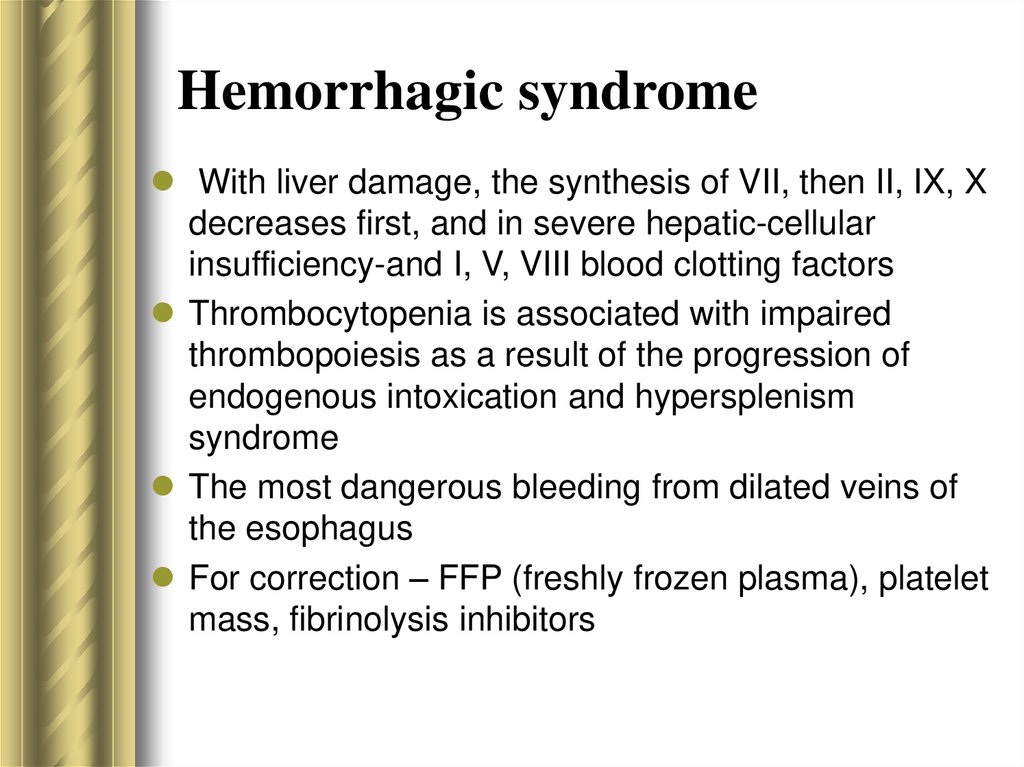
Hemorrhagic syndromeWith liver damage, the synthesis of VII, then II, IX, X
decreases first, and in severe hepatic-cellular
insufficiency-and I, V, VIII blood clotting factors
Thrombocytopenia is associated with impaired
thrombopoiesis as a result of the progression of
endogenous intoxication and hypersplenism
syndrome
The most dangerous bleeding from dilated veins of
the esophagus
For correction – FFP (freshly frozen plasma), platelet
mass, fibrinolysis inhibitors
40.
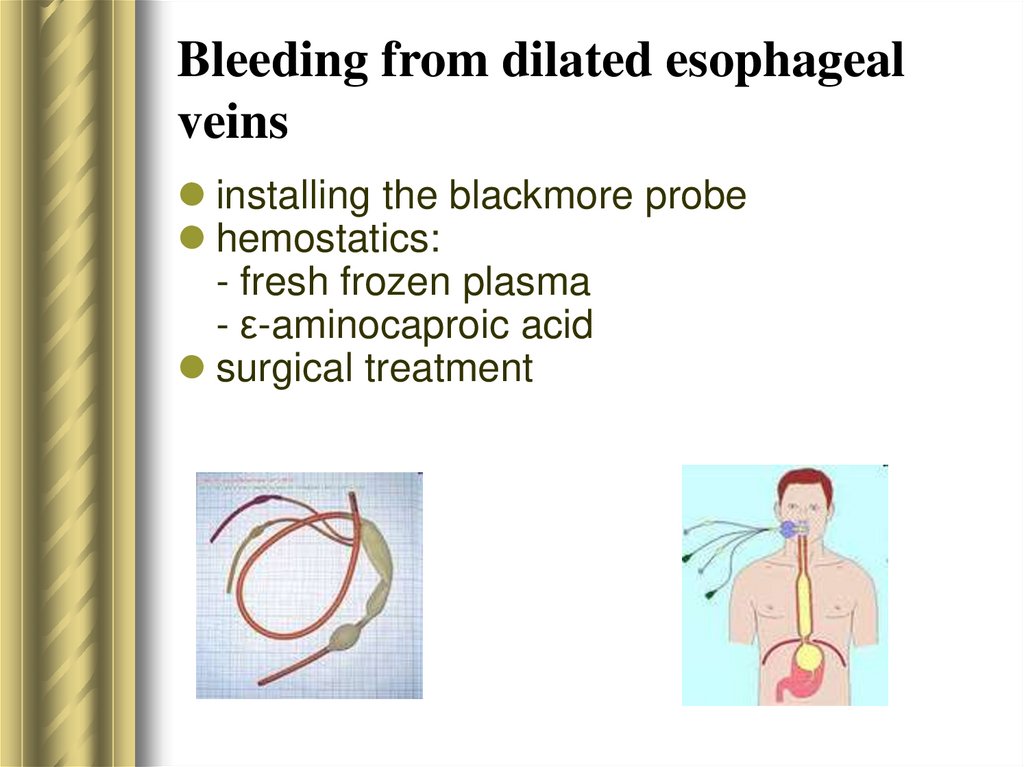
Bleeding from dilated esophagealveins
installing the blackmore probe
hemostatics:
- fresh frozen plasma
- ε-aminocaproic acid
surgical treatment
41.
Arterial hypotensionReduction of oncotic pressure → fluid release from
blood vessels → circulating blood volume (CBV)
reduction
Histamine accumulation (impaired deamination) and
tendency to vasodilation
Inhibition of contractile function of the heart
Leads to worsening of brain hypoxia and
encephalopathy
Deterioration - often after evacuation of ascitic fluid
(blood redistribution, increased filtration)
Correction – administration of albumin solution; in
case of severe hypotension - adrenomimetics
42.
Principles of diagnosticsCytolysis syndrome - a marker of acute
hepatocyte damage
Cholestasis syndrome (↑of direct
bilirubin, bile acids, cholesterol in the
blood; markers of cholestasis – alkaline
phosphatase, 5-nucleotidase, GGTP) –
more often in acute damage
43.
Principles of diagnosticsHepatic cell failure syndrome
- hypoproteinemia, lack of clotting factors
- postprandial hyperglycemia, fasting
hypoglycemia
- reduction of cholesterol in the blood;
ketoacidosis
- hyperbilirubinemia (direct and indirect)
- increases in ammonia and decreases in
urea in the blood
- hypokalemia
44.
Principles of diagnosticsHepatic encephalopathy syndrome
Portal hypertension syndrome - with
cirrhosis of the liver
45.
Principles of therapyA low-protein diet (up to 0.5 g / kg per
day, and in some cases completely
excluded)
For parenteral nutrition - special
amino acid mixtures
Blood glucose control and correction
of hypoglycemia
46.
Principles of therapyLactulose is a synthetic hypo-ammoniemic drug, This
shugar is not adsorbed in the gastrointestinal tract and
increases osmotic pressure in intestine.
→ the volume of intestinal contents increases, peristalsis
is activated
→ elimination of toxic substances accelerates, their
absorption into the systemic circulation decreases.
47.
Principles of therapyVitamin Therapy
- Vitamin K (vikasol) - stimulates the formation of thrombin
and prothrombin.
- Thiamine (B1) in the liver is converted to cocarboxylase, a
deficiency of which is associated with the accumulation of
lactic and pyruvic acids.
- Riboflavin (B2) promotes oxidative deamination of amino
acids.
- Pyridoxine (B6) in the body after phosphorylation is involved
in transamination and decarboxylation of amino acids.
- Folic acid and cyancobalamin are involved in the synthesis
of nucleotides.
- Ascorbic acid activates oxidative and proteolytic enzymes
involved in the regulation of carbohydrate metabolism, in
the process of blood clotting, in strengthening the walls of
blood vessels.
48.
Principles of therapyEssentiale. The drug contains phospholipids (EPL
substance) and vitamins with antihypoxant (thiamine,
riboflavin, pyridoxyl, nicotinamide) and antioxidant
(tocopherol, cyancobolamine) properties. Phospholipids,
which are the main component of the cell wall,
embedded in the cell membrane, have a normalizing
effect on the metabolism of lipids, proteins and on the
detoxification function of the liver
Heptral (ademetionine). Prevents exogenous and
endogenous hepatotoxic effects, helps maintain the
viscosity of cell membranes, which is necessary for the
normal activity of membrane-bound enzymes.
49.
Principles of therapyMaintenance of hemodynamic parameters
- infusion therapy (albumin solution, glucose
solution, correction of acidosis and hypokalemia)
- in severe cases - adrenomimetics
Correction of the hemostatic system - FFP (fresh
frozen plasma)
Sorption methods (hemo-and plasma sorption,
plasmapheresis)
With an increase in intracranial pressure, mannitol
is injected intravenously at the rate of 1 g/kg of the
patient's body weight.
Prevention and treatment of concomitant infections
50.
Thank you for yourattention!

















 Медицина
Медицина








