Похожие презентации:
Atherosclerosis. Hypertensive disease. Ischemic heart disease
1.
ATHEROSCLEROSIS.HYPERTENSIVE DISEASE.
ISCHEMIC HEART DISEASE
Lecture reader: M.D., Ph.D, D.M.Sci,
Professor DYADYK E.A.
2.
Atherosclerosis (athere – latin gruel) is achronic disease which is characterized by
formation of vascular intimal lesions called
atheromas or fibrofatty plaques in the
elastic and muscular arteries with
subsequent damage of organs and tissues
due to reduced blood supply.
3.
Etiology (risk factors)1. Age (reducing of sex hormones synthesis and tissue
regeneration, i.e. reducing of cholesterol consumption by
tissues).
2. Genetic predisposition to hypercholesterolemia.
3. Acquired metabolic disturbances with hypercholesterolemia (> 5,2 mmol/l): cholesterol-rich diet,
hormonal misbalances, and diabetes mellitus.
4. Hypertension.
5. Smoking.
6. Obesity.
7. Herpesvirus, cytomegalovirus and Chlamydia
pneumoniae infection.
4.
Pathogenesis (steps of development)1. Development of focal regions of chronic endothelial injury
leading to increased vascular permeability and increased
leukocyte adhesion.
2. Insudation of lipoproteins into the vessel wall, mainly LDL
and VLDL, and modification of such lipoproteins by
oxidation.
3. Adhesion of blood monocytes to the endothelium, their
migration into the intima and transformation into
macrophages and foam cells.
4. Oxidative modification of lipid by free radicals generated
in macrophages or endothelial cells. Oxidized LDL inhibits
the motility of macrophages thus favoring the recruitment
and retention of macrophages in plaques.
5.
Pathogenesis (steps of development)5. Adhesion of platelets to the focal areas of endothelial
injury.
6. Release of biologically active substances that cause
migration of smooth muscle cells from media into the
intima.
7. Proliferation of immigrant smooth muscle cells in the
intima, they gain secretory phenotype and synthesize
extracellular matrix, leading to accumu-lation of
collagen and proteoglycans in the plaque. Connective
tissue is particularly prominent on the intimal aspect,
where it produces fibrous cap.
6.
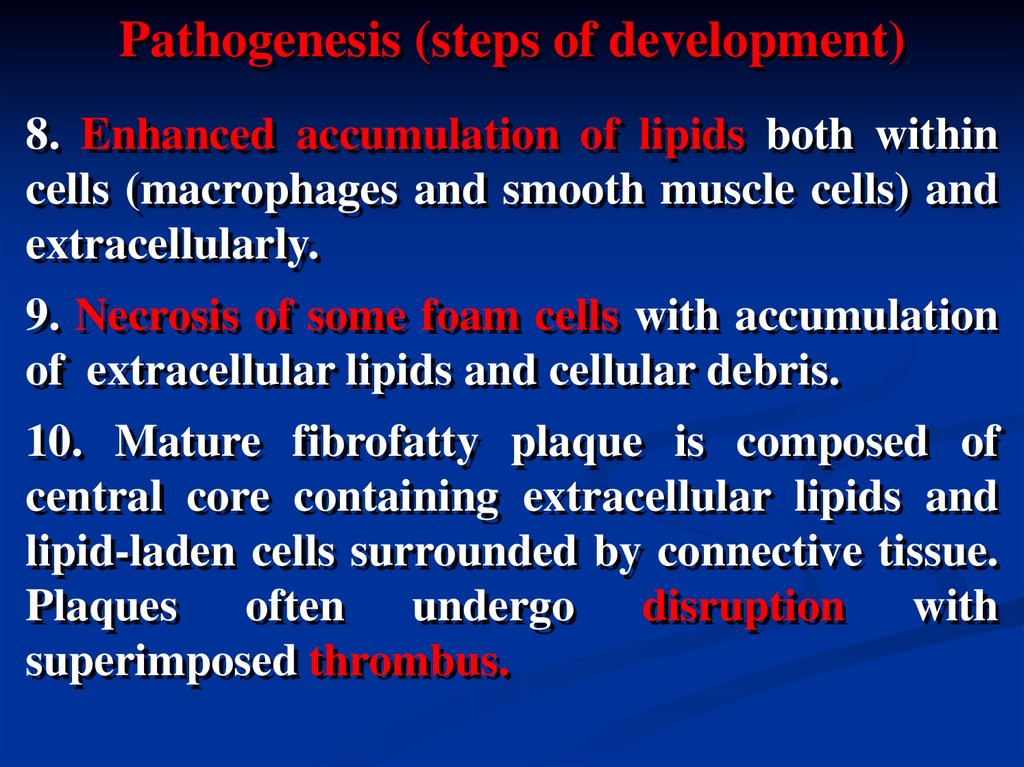
Pathogenesis (steps of development)8. Enhanced accumulation of lipids both within
cells (macrophages and smooth muscle cells) and
extracellularly.
9. Necrosis of some foam cells with accumulation
of extracellular lipids and cellular debris.
10. Mature fibrofatty plaque is composed of
central core containing extracellular lipids and
lipid-laden cells surrounded by connective tissue.
Plaques often undergo disruption with
superimposed thrombus.
7.
LocalizationAorta is usually the most involved vessel, the
aortic lesions tend to be much more prominent
around the ostia of its major branches.
In descending order the most heavily involved
vessels are:
thoracic aorta;
coronary arteries;
popliteal arteries;
thoracic aorta;
internal carotid arteries;
vessels of the circle of Willis.
8.
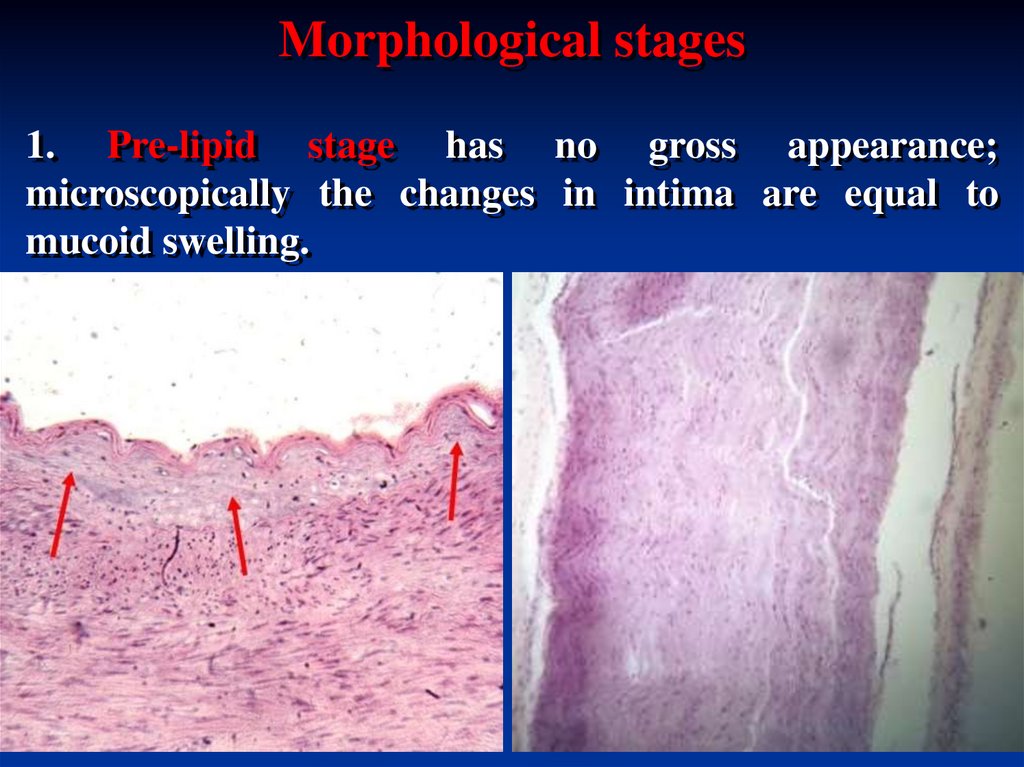
Morphological stages1. Pre-lipid stage has no gross appearance;
microscopically the changes in intima are equal to
mucoid swelling.
9.
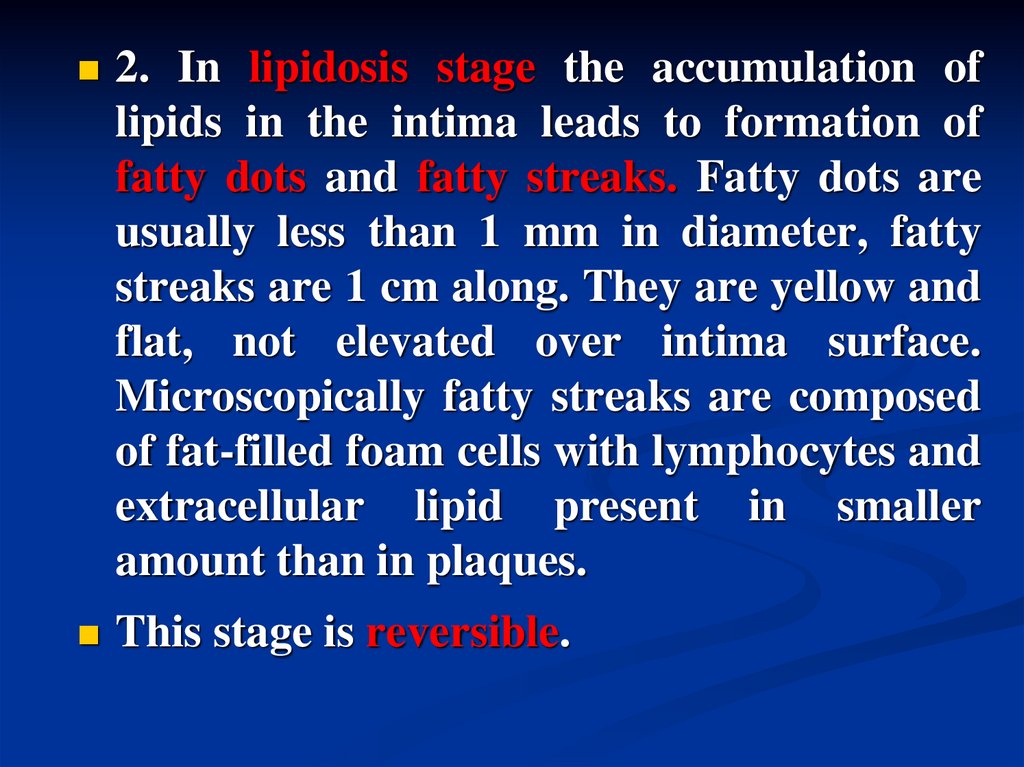
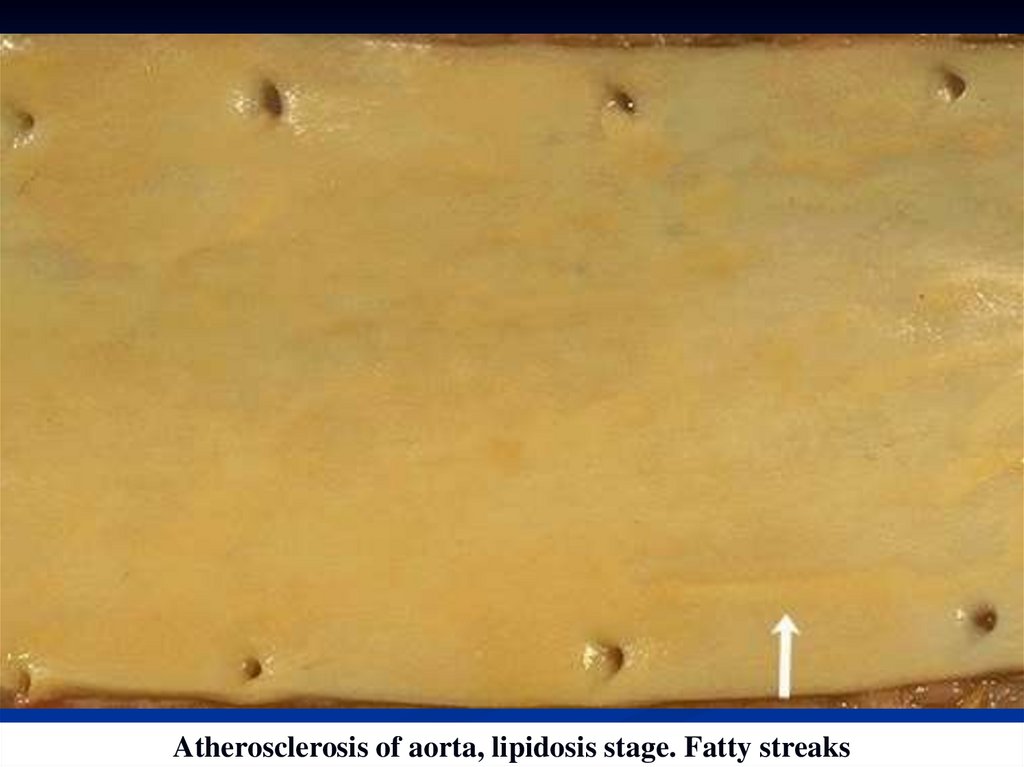
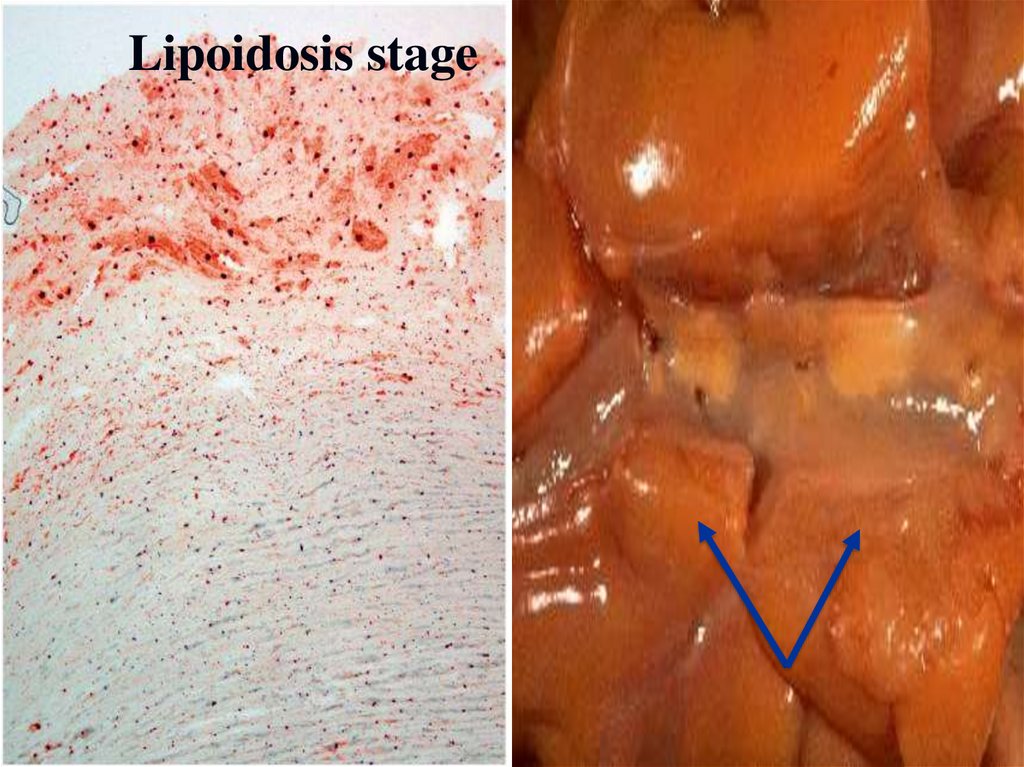
2. In lipidosis stage the accumulation oflipids in the intima leads to formation of
fatty dots and fatty streaks. Fatty dots are
usually less than 1 mm in diameter, fatty
streaks are 1 cm along. They are yellow and
flat, not elevated over intima surface.
Microscopically fatty streaks are composed
of fat-filled foam cells with lymphocytes and
extracellular lipid present in smaller
amount than in plaques.
This stage is reversible.
10.
Atherosclerosis of aorta, lipidosis stage. Fatty streaks11.
Lipoidosis stage12.
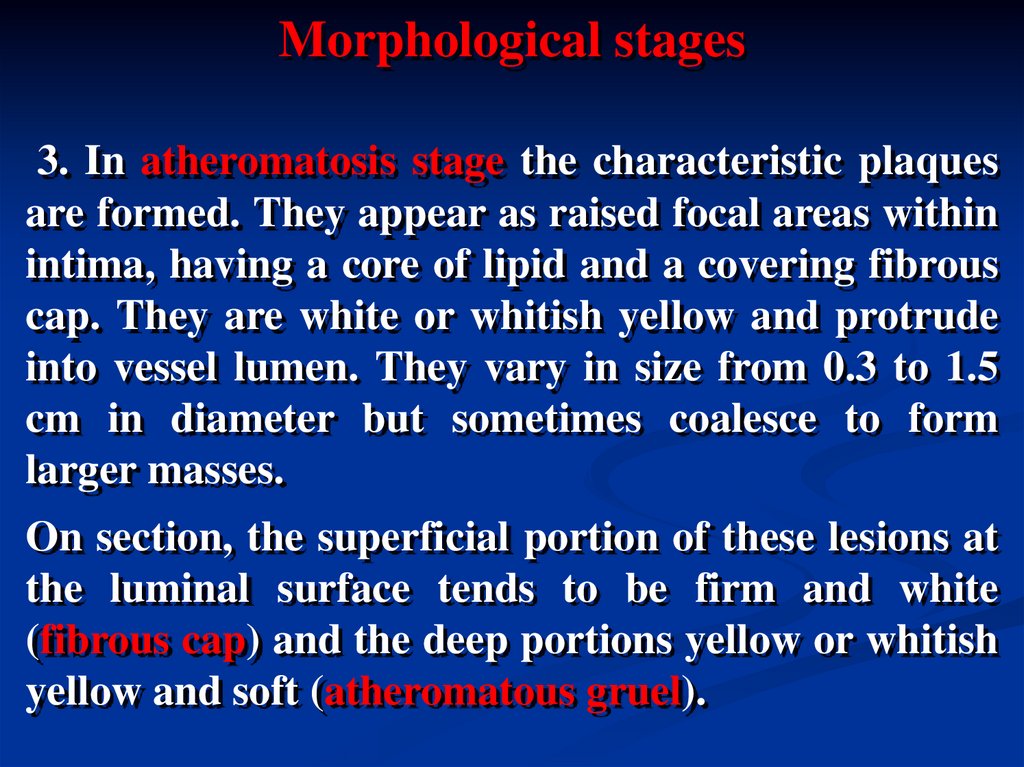
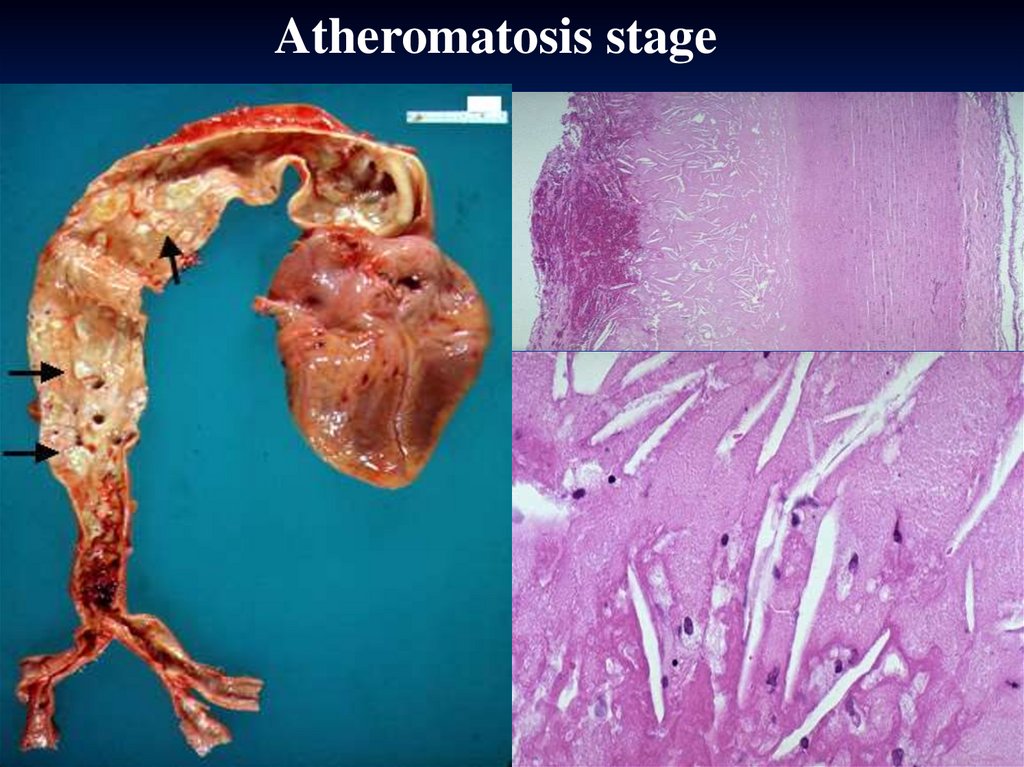
Morphological stages3. In atheromatosis stage the characteristic plaques
are formed. They appear as raised focal areas within
intima, having a core of lipid and a covering fibrous
cap. They are white or whitish yellow and protrude
into vessel lumen. They vary in size from 0.3 to 1.5
cm in diameter but sometimes coalesce to form
larger masses.
On section, the superficial portion of these lesions at
the luminal surface tends to be firm and white
(fibrous cap) and the deep portions yellow or whitish
yellow and soft (atheromatous gruel).
13.
Atheromatosis stage14.
Atherosclerosis of aorta, three different degrees of damage15.
Atherosclerosis of coronary artery16.
АТЕРОСКЛЕРОЗ ВІНЦЕВИХ АРТЕРІЙ СЕРЦЯ17.
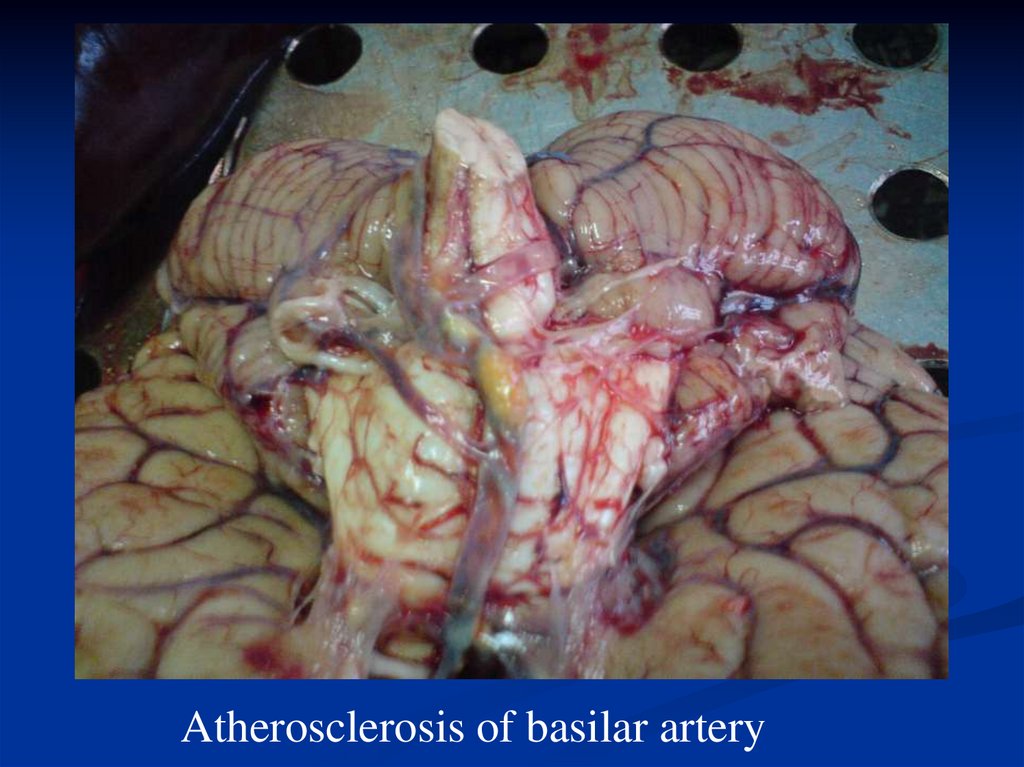
Atherosclerosis of basilar artery18.
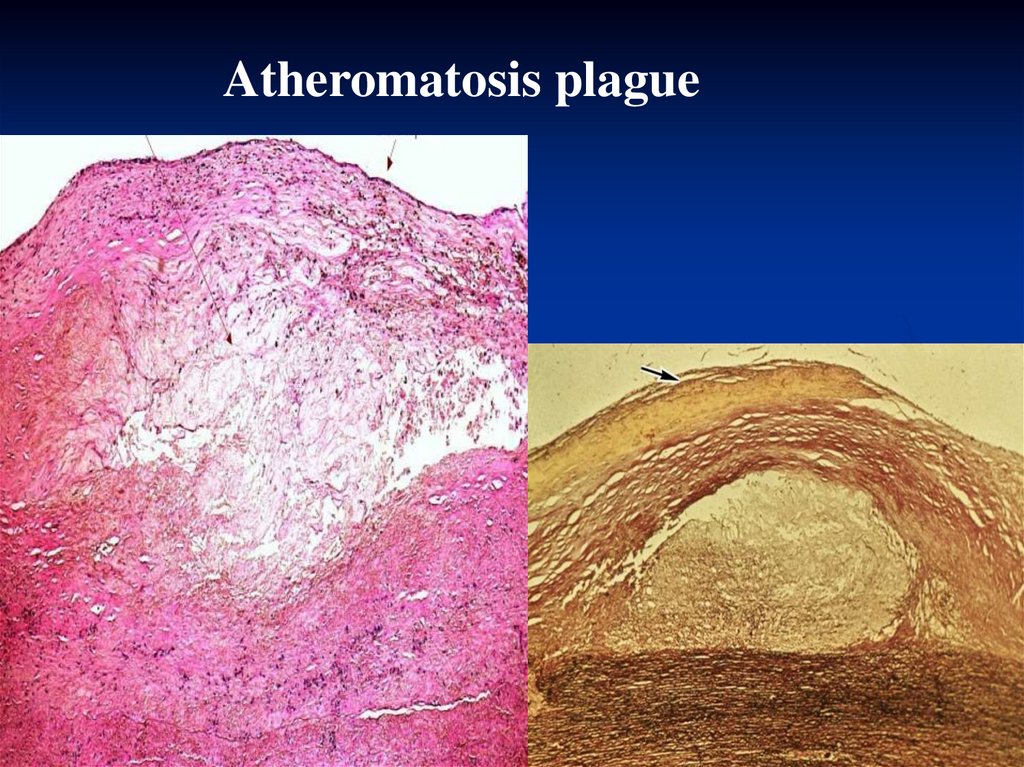
Atheromatosis plague19.
Atherosclerosis of coronary artery, 40 magnification, H&E stain20.
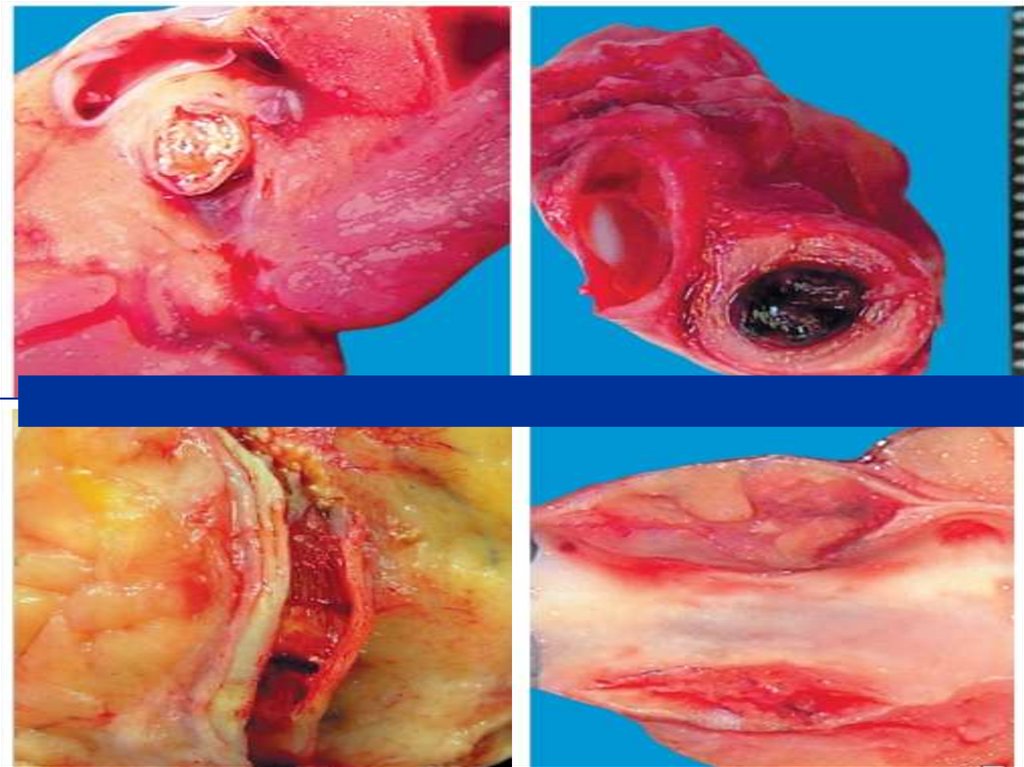
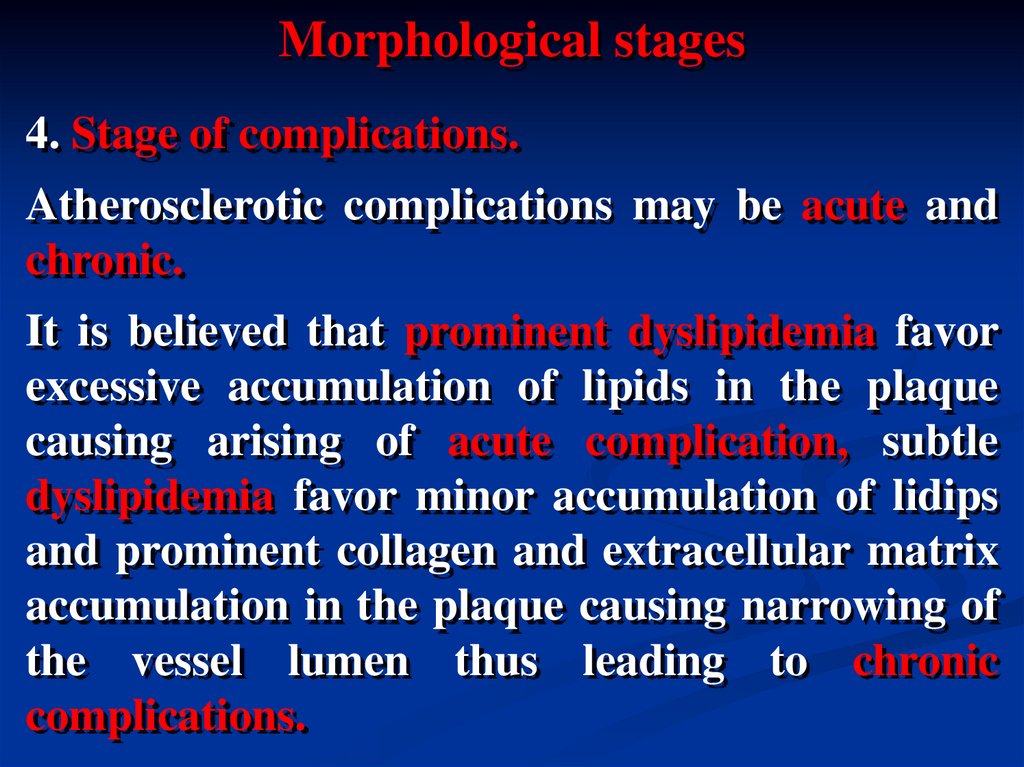
Morphological stages4. Stage of complications.
Atherosclerotic complications may be acute and
chronic.
It is believed that prominent dyslipidemia favor
excessive accumulation of lipids in the plaque
causing arising of acute complication, subtle
dyslipidemia favor minor accumulation of lidips
and prominent collagen and extracellular matrix
accumulation in the plaque causing narrowing of
the vessel lumen thus leading to chronic
complications.
21.
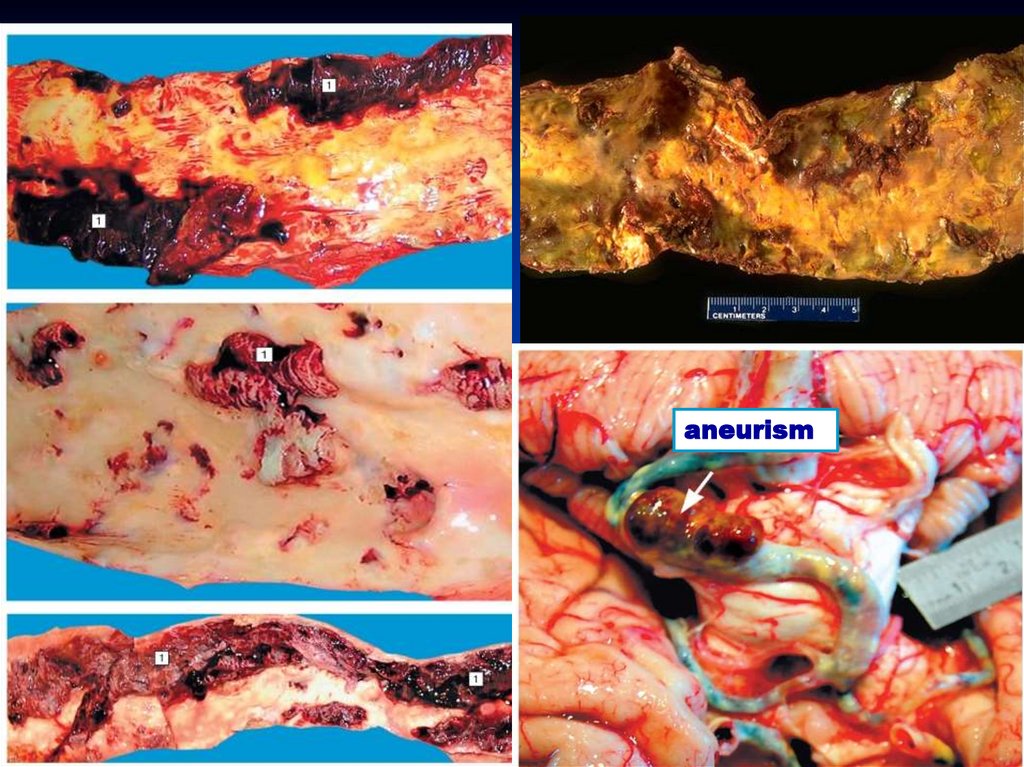
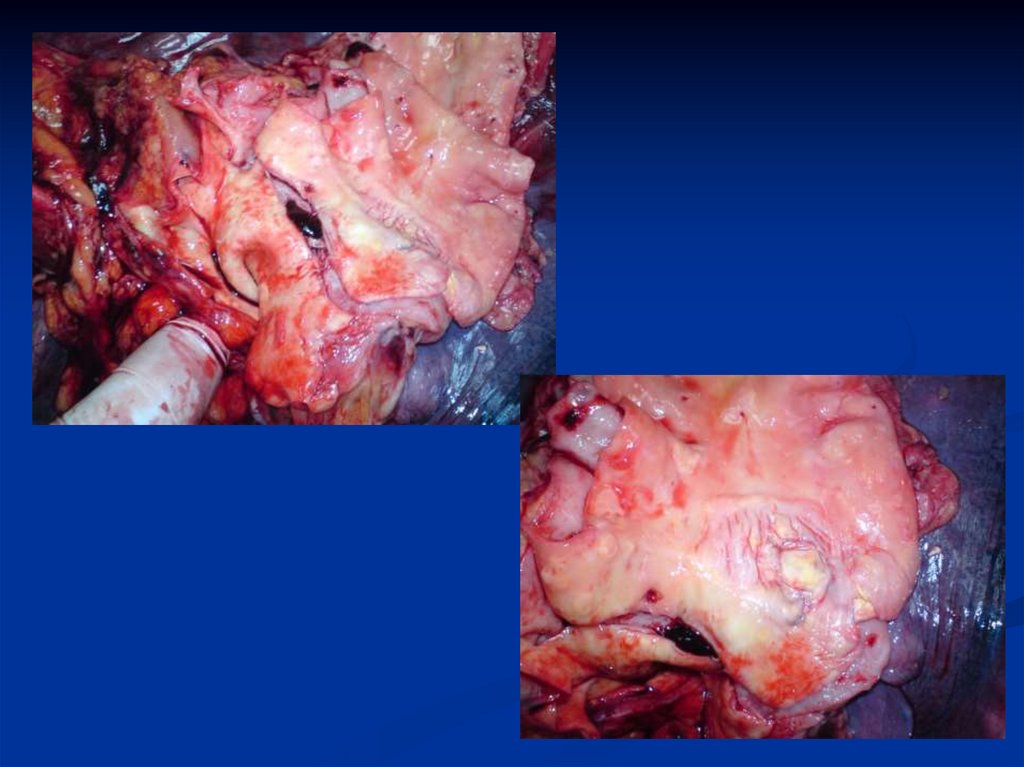
aneurism22.
23.
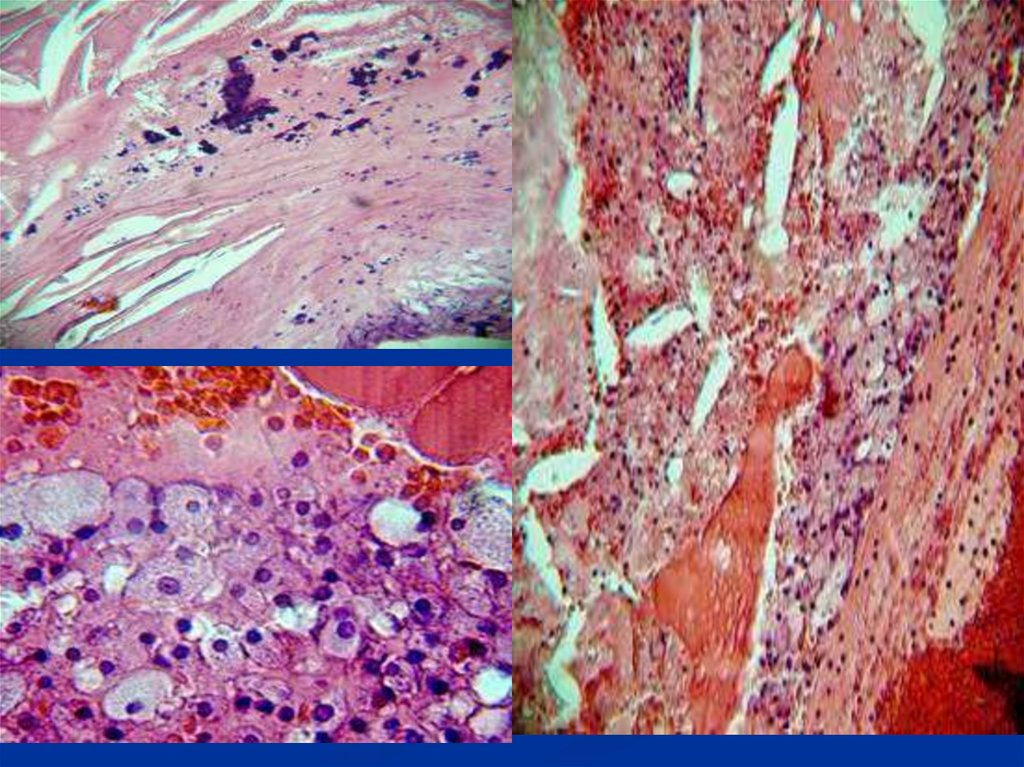
Acute complications1. Focal rupture or gross ulceration, or both, of the
luminal surface of atheromatous plaques may result
in exposure of highly thrombogenic substances that
induce thrombus formation or discharge of debris
into the bloodstream, producing microemboli
(cholesterol emboli or atheroemboli).
2. Hemorrhage into a plaque may occur, especially in
the coronary arteries. The source of blood is
ruptured vessels of overlying fibrous cap or the thinwalled capillaries that vascularize the plaque. An
enlarging hematoma may induce plaque rupture.
24.
Acute complications3. Superimposed thrombosis usually occurs on disrupted
lesions (those with rupture, ulceration, erosion, or
hemorrhage). Thrombi may partially or completely
occlude the lumen; they may become incorporated
within the intimal plaque by organization.
Complete thrombosis of vessel can cause infarction of
heart, brain, kidney and other organs, gangrene of limbs
and intestine. Myocardial infarction and stroke are the
most common causes of death in patients with advanced
atherosclerosis.
4. Complicated atherosclerotic lesions may lead to
rupture of affected vessel.
25.
Necrosis in heartwall
Dry gangrene of foot
26. Gangrene of intestine
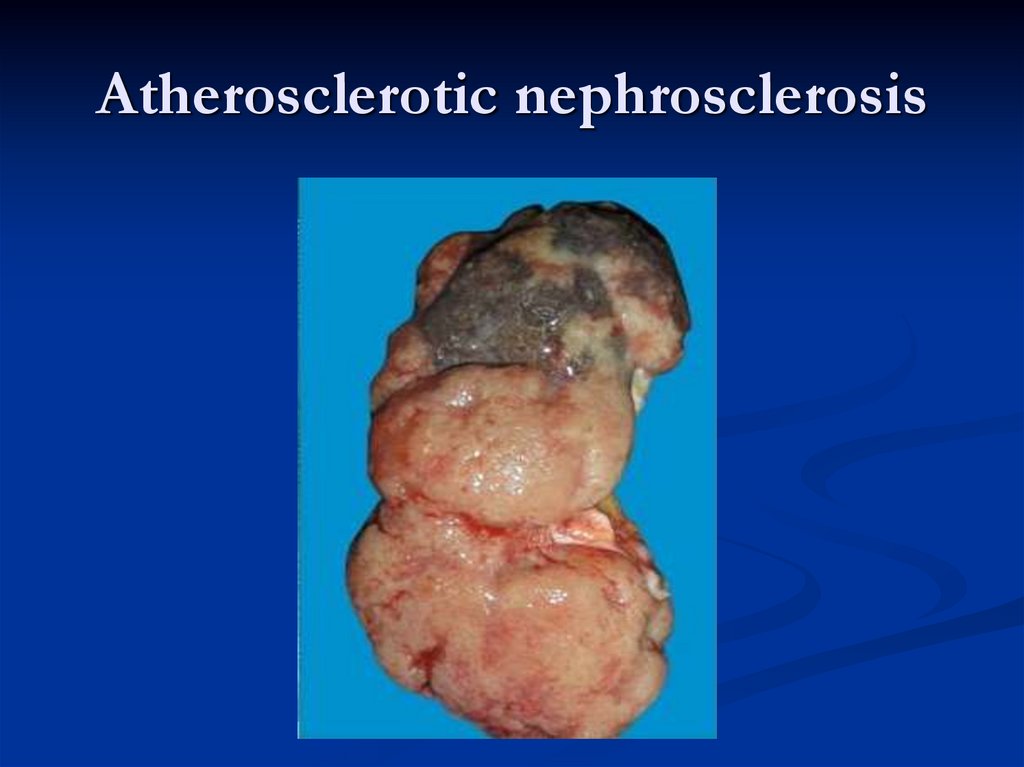
27. Atherosclerotic nephrosclеrosis
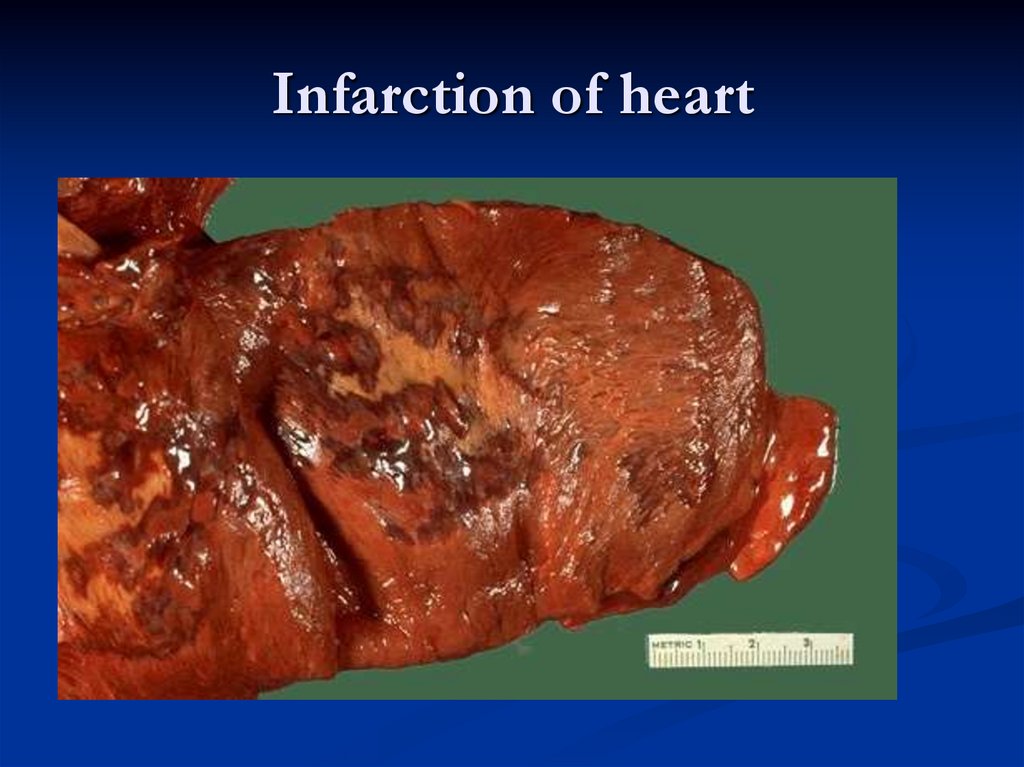
28. Infarction of heart
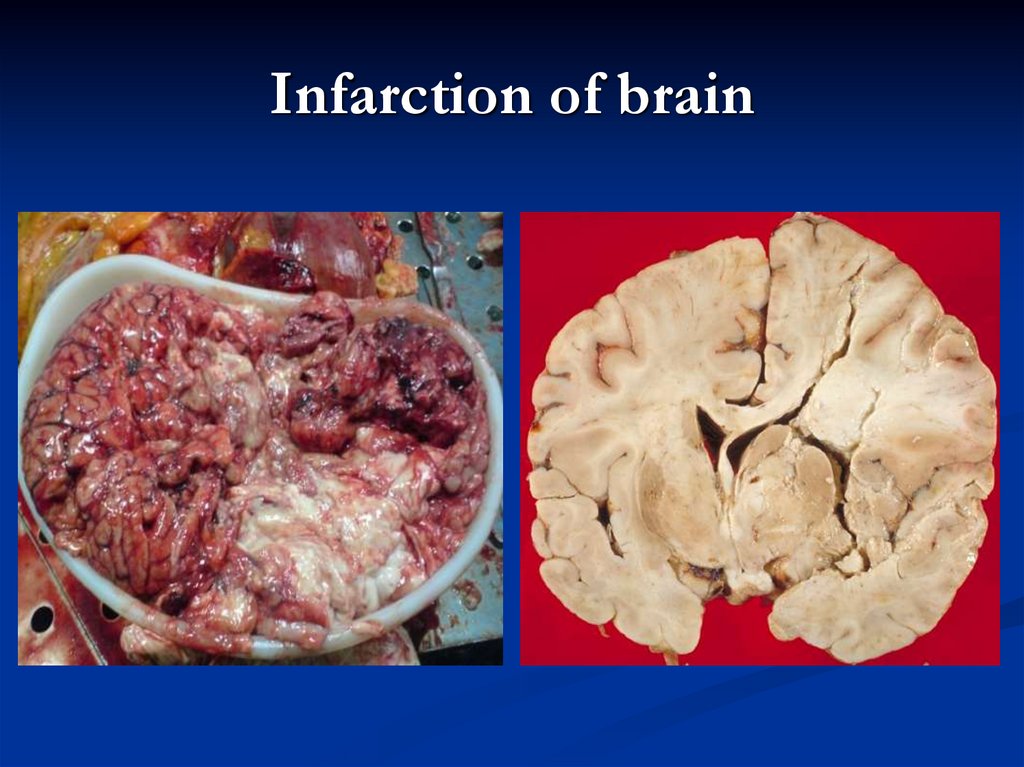
29. Infarction of brain
30.
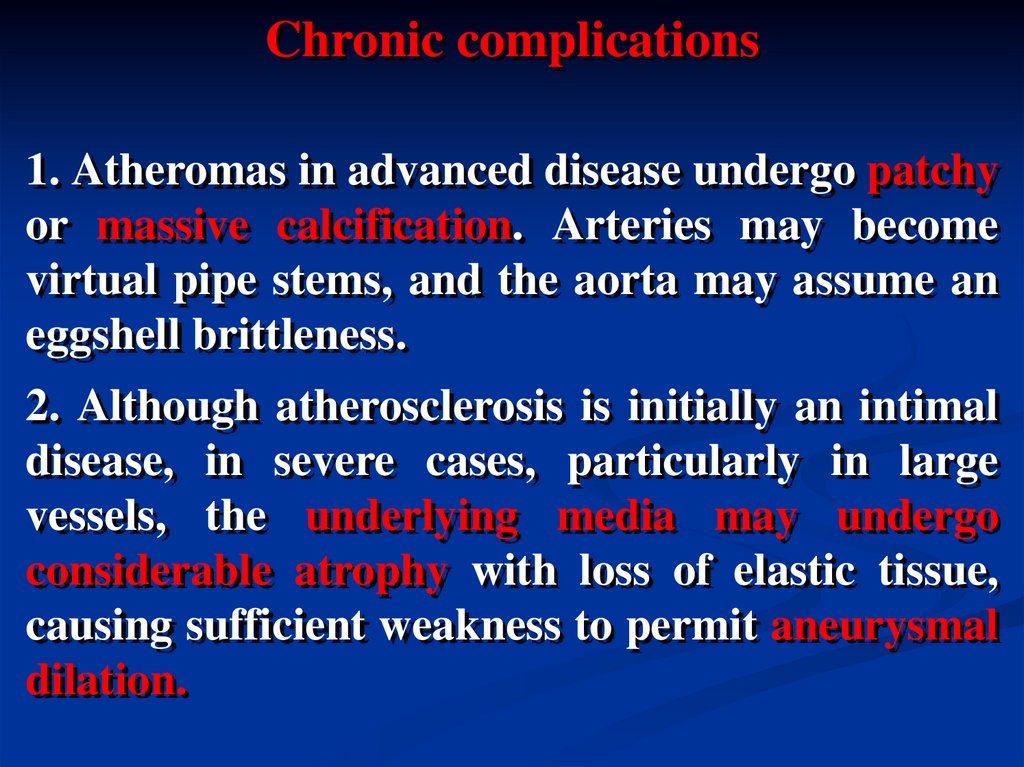
Chronic complications1. Atheromas in advanced disease undergo patchy
or massive calcification. Arteries may become
virtual pipe stems, and the aorta may assume an
eggshell brittleness.
2. Although atherosclerosis is initially an intimal
disease, in severe cases, particularly in large
vessels, the underlying media may undergo
considerable atrophy with loss of elastic tissue,
causing sufficient weakness to permit aneurysmal
dilation.
31.
32.
Chronic complications3. Uncomplicated atherosclerotic lesions usually cause
narrowing of vessel lumen leading to decreasing of blood
circulation in organs and tissues. Chronic ischemia leads
to parenchymal atrophy and stromal sclerosis.
Examples:
cardiosclerosis,
nephrosclerosis,
cerebral sclerosis (appearing as senile dotage)
muscle atrophy,
intermittent lameness,
atrophy of intestinal mucosa (appearing as
malabsorption syndrome).
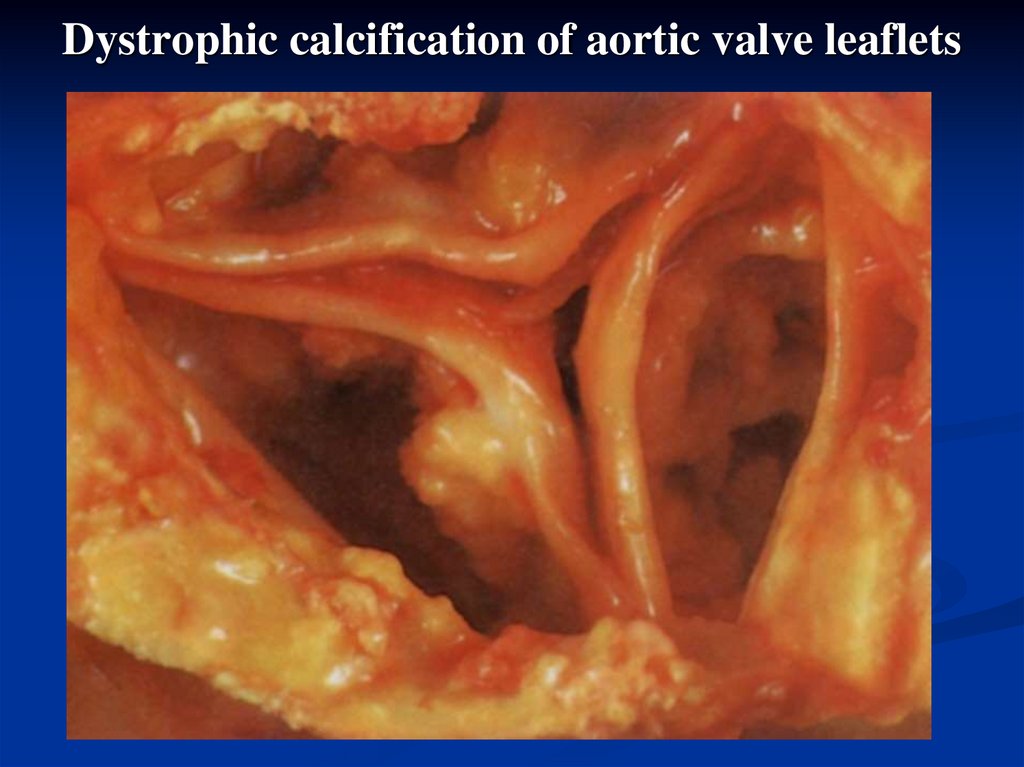
4. Deposition of atheromatous masses in heart valves can
cause valve dysfunction.
33. Dystrophic calcification of aortic valve leaflets
34.
Hypertensive disease is a chronic diseasewhich is characterized by chronic elevation
of blood pressure that affects both the
function and the structure of blood vessels,
predominantly small muscular arteries and
arterioles.
35.
ClassificationPrimary (idiopathic, essential) hypertension (9095%):
benign;
malignant (or accelerated).
Secondary hypertension that may be caused by:
- renal diseases;
- narrowing of the renal artery (due to
hypoplasia, fibro-muscular dysplasia, or
atheromatous plaque);
hyperproduction
of
glucocorticoids,
adrenaline, thyroxin, and other hormones.
36.
Etiology (risk factors)1. Age.
2. Environmental factors (e.g. frequent
stresses, increased salt intake, increased
estrogen level).
3. Genetic predisposition (deregulation in
genes which are responsible for increased
renal sodium reabsorption, blood level of
pressor substances such as angiotensin II,
reactivity of vascular smooth muscle to
pressor agents etc).
37.
PathogenesisIn hypertensive disease both increased cardiac
output and increased peripheral resistance due to
constriction of vessel muscle cells contribute to
the increased pressure.
There are 3 clinical-morphological stages:
- functional;
- prominent morphological changes in vessels;
- secondary changes in internal organs.
38.
Functional stageIn this stage there are periodical elevations of
blood pressure. Morphologically this stage is
characterized by arising of adaptive processes:
hypertrophy of vessel smooth muscle cells in
arterioles due to prolonged periods of
contraction. Rarely the reversible dystrophic
changes in the vessel walls occur. At this stage the
initial features of myocardial hypertrophy are
evident. In malignant hypertension this stage is
usually omitted.
39.
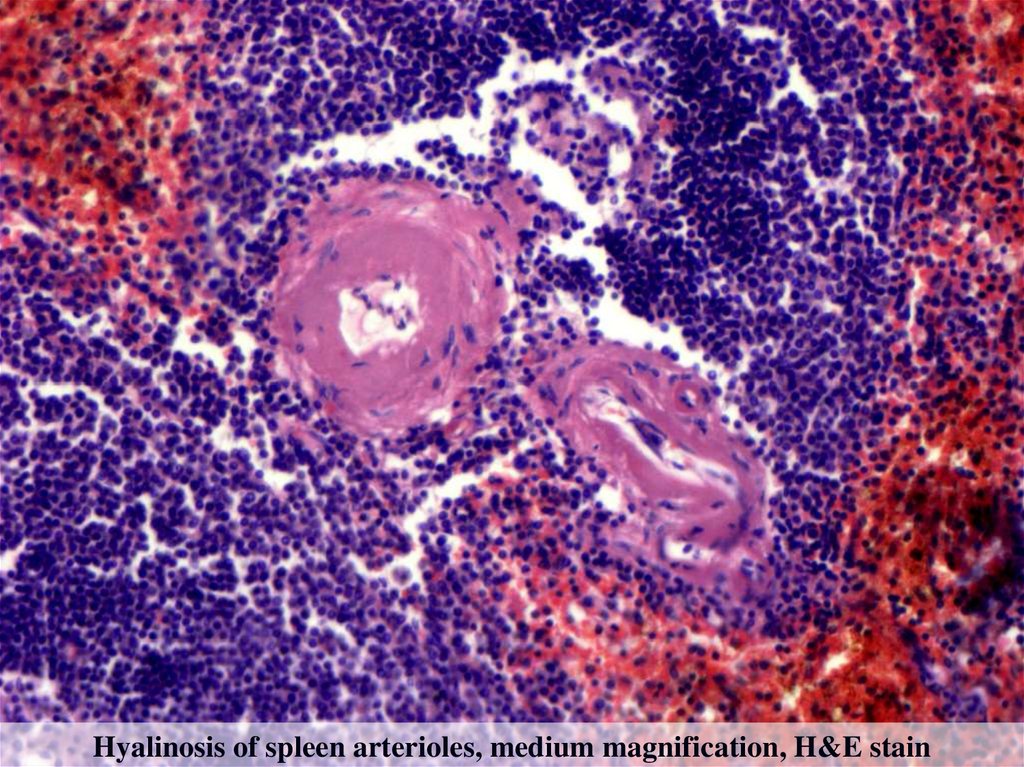
Prominent morphological changes in vesselsIn benign hypertensive diseases the prolonged
periods of arterioles constriction lead to
narrowing of vessels, decreased blood flow and
hypoxia. Hypoxia leads to dystrophic changes
similar to mucoid swelling. Increased vascular
permeability leads to leakage of blood proteins
into vessel wall (plasmatic impregnation) which
eventually progresses to hyalinosis. Such vessels
are unable to dilate, so these changes lead to
constant elevation of blood pressure.
40.
Hyalinosis of spleen arterioles, medium magnification, H&E stain41.
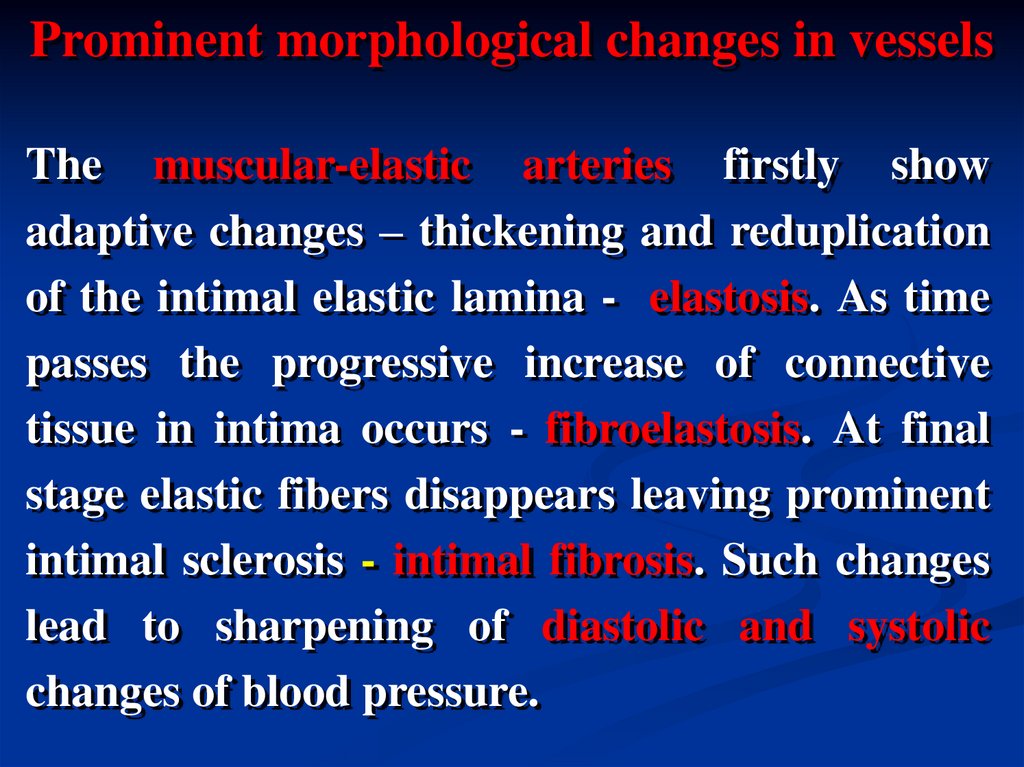
Prominent morphological changes in vesselsThe muscular-elastic arteries firstly show
adaptive changes – thickening and reduplication
of the intimal elastic lamina - elastosis. As time
passes the progressive increase of connective
tissue in intima occurs - fibroelastosis. At final
stage elastic fibers disappears leaving prominent
intimal sclerosis - intimal fibrosis. Such changes
lead to sharpening of diastolic and systolic
changes of blood pressure.
42.
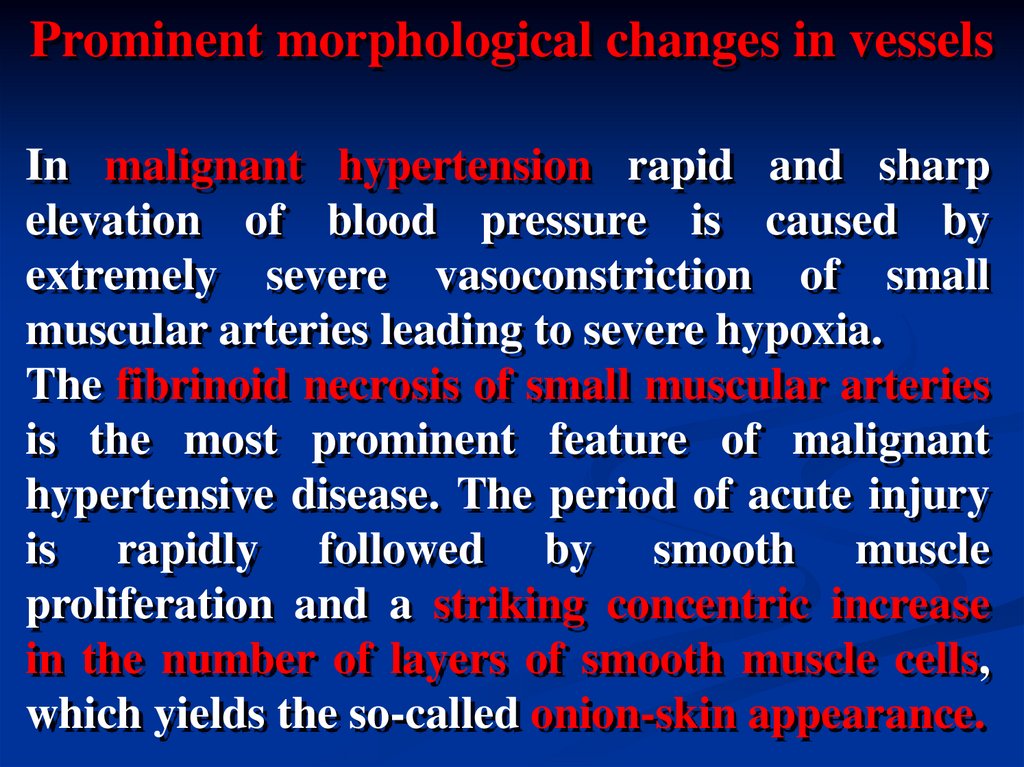
Prominent morphological changes in vesselsIn malignant hypertension rapid and sharp
elevation of blood pressure is caused by
extremely severe vasoconstriction of small
muscular arteries leading to severe hypoxia.
The fibrinoid necrosis of small muscular arteries
is the most prominent feature of malignant
hypertensive disease. The period of acute injury
is rapidly followed by smooth muscle
proliferation and a striking concentric increase
in the number of layers of smooth muscle cells,
which yields the so-called onion-skin appearance.
43.
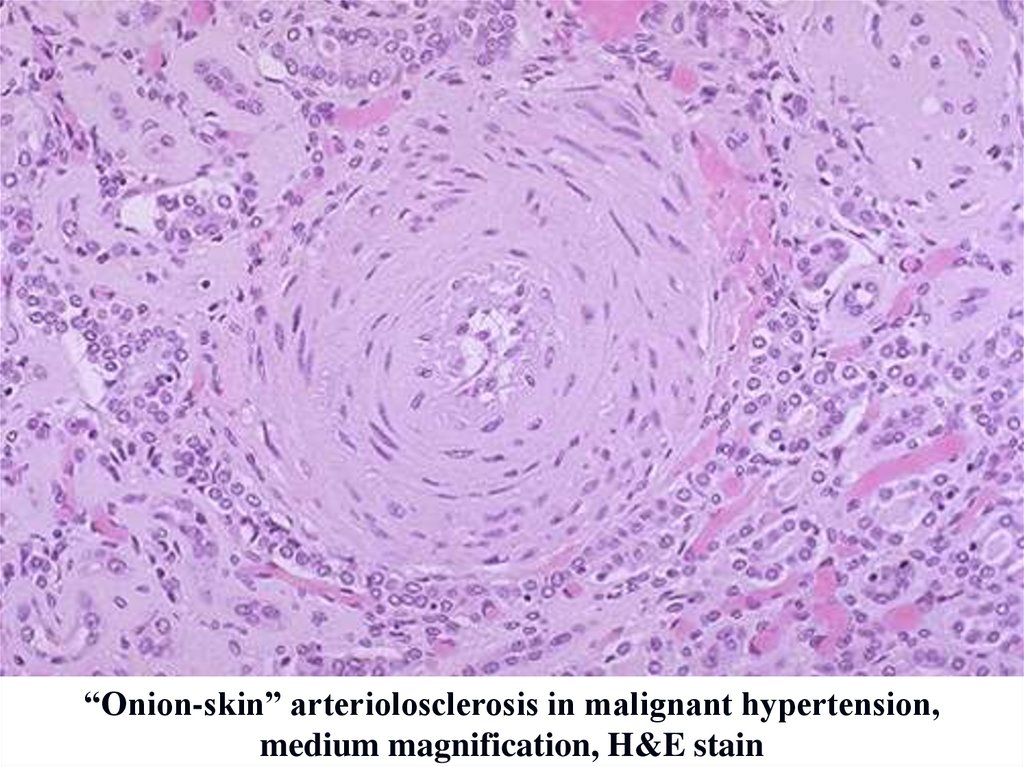
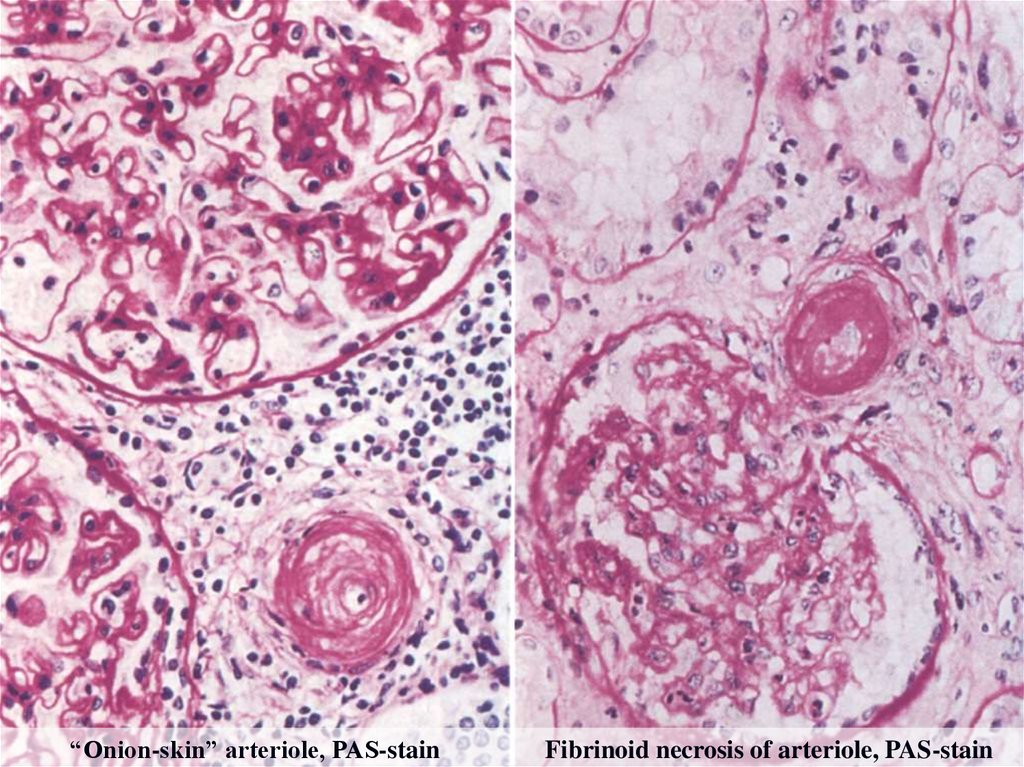
“Onion-skin” arteriolosclerosis in malignant hypertension,medium magnification, H&E stain
44.
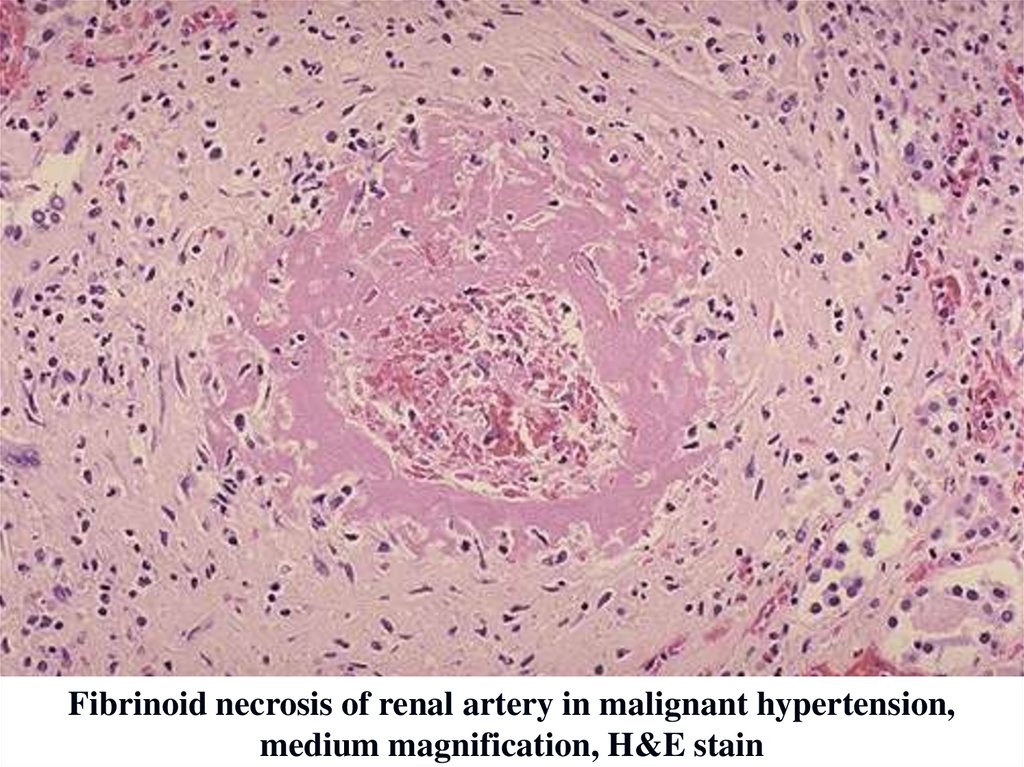
Fibrinoid necrosis of renal artery in malignant hypertension,medium magnification, H&E stain
45.
“Onion-skin” arteriole, PAS-stainFibrinoid necrosis of arteriole, PAS-stain
46.
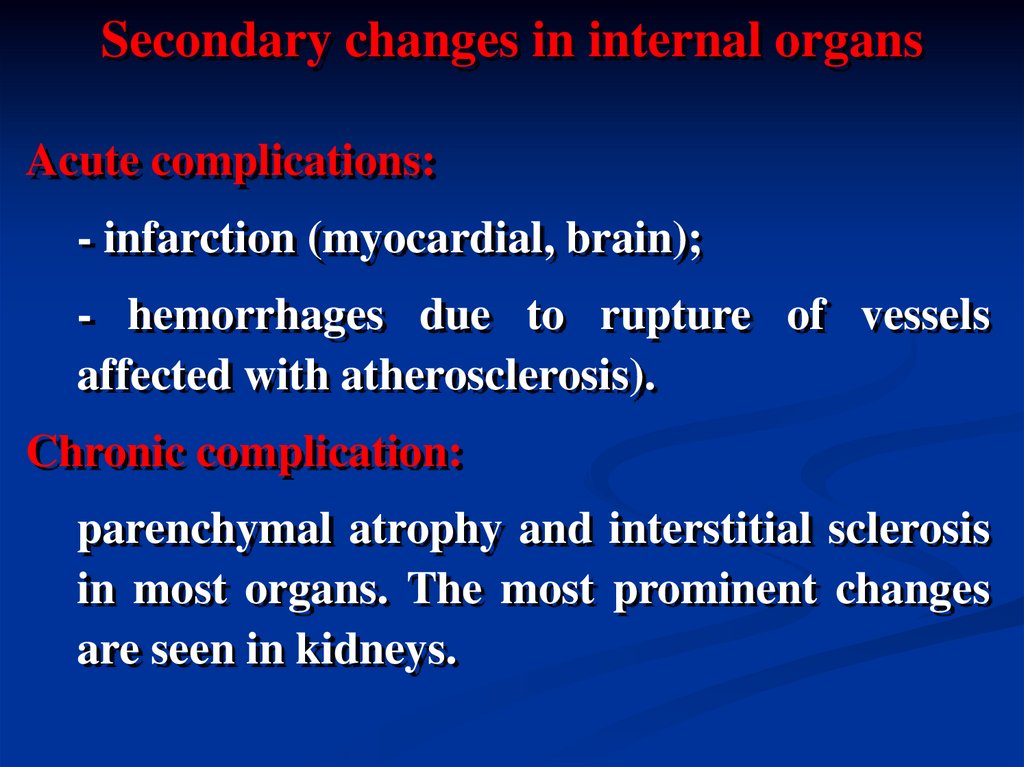
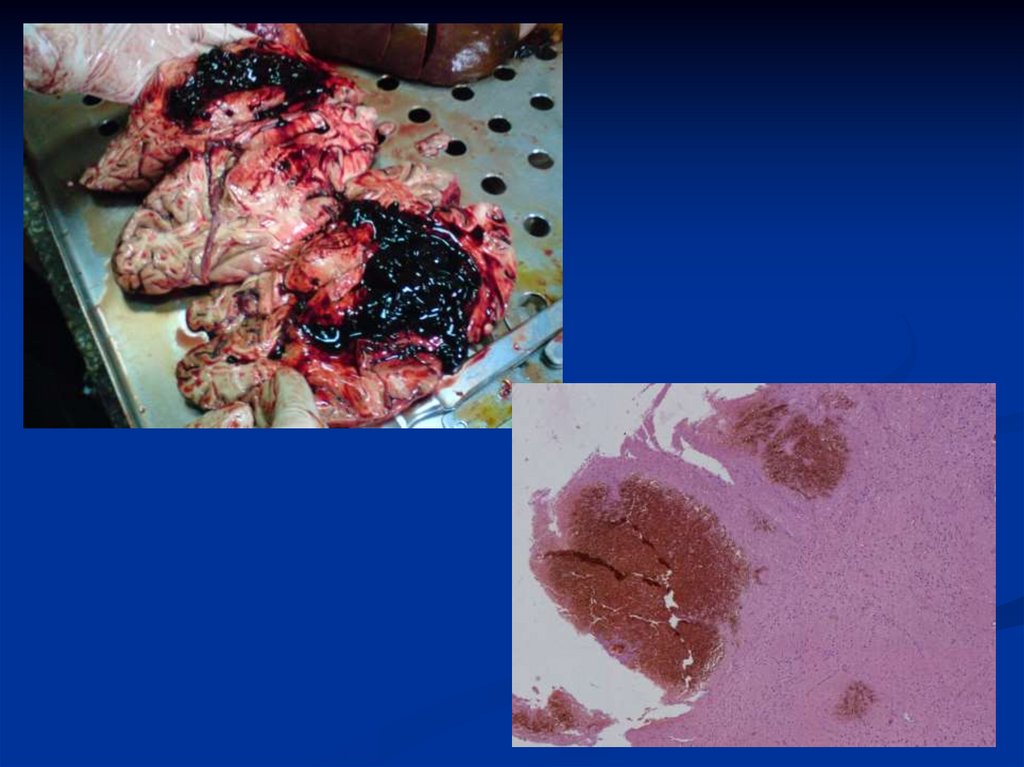
Secondary changes in internal organsAcute complications:
- infarction (myocardial, brain);
- hemorrhages due to rupture of vessels
affected with atherosclerosis).
Chronic complication:
parenchymal atrophy and interstitial sclerosis
in most organs. The most prominent changes
are seen in kidneys.
47.
48.
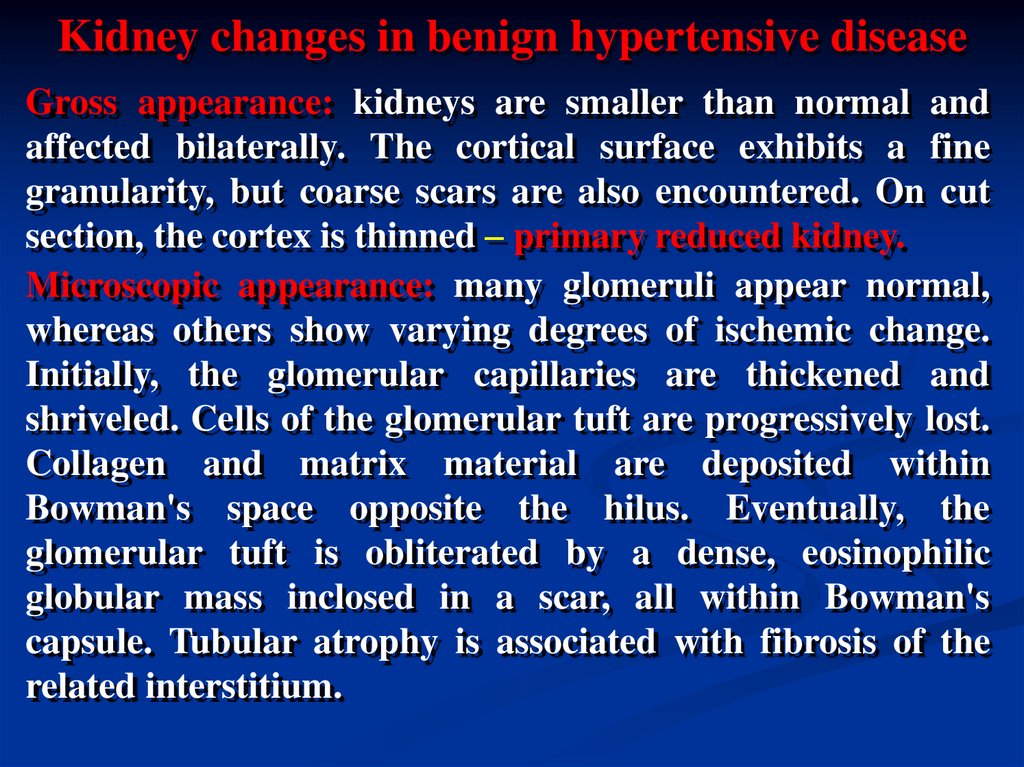
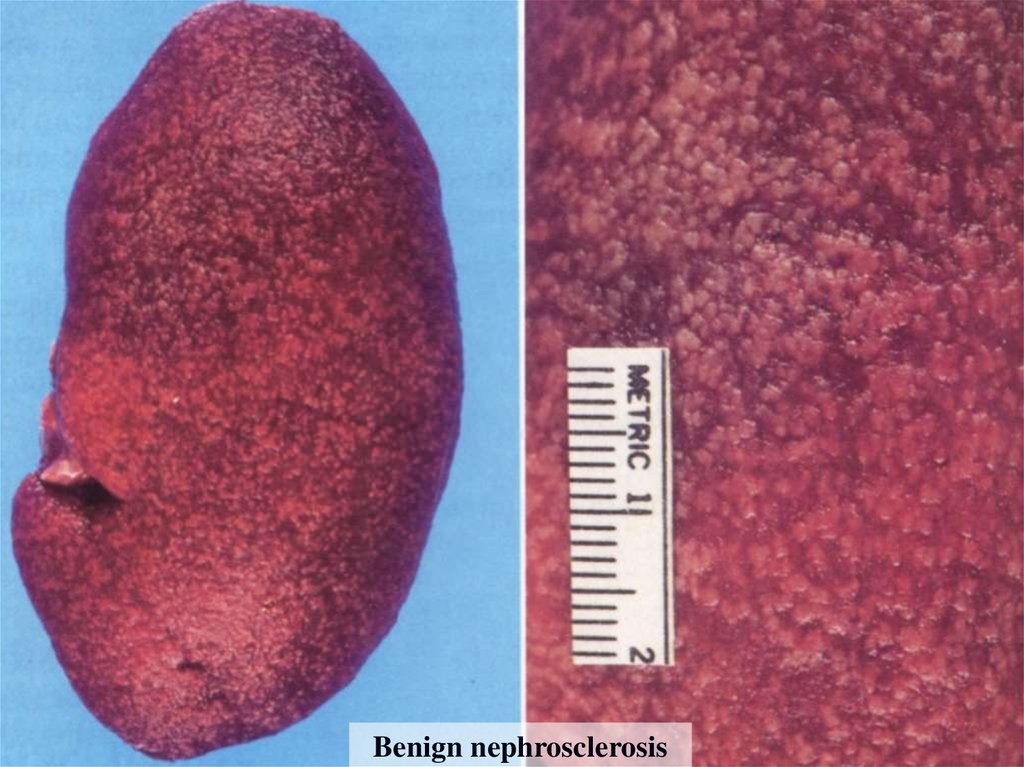
Kidney changes in benign hypertensive diseaseGross appearance: kidneys are smaller than normal and
affected bilaterally. The cortical surface exhibits a fine
granularity, but coarse scars are also encountered. On cut
section, the cortex is thinned – primary reduced kidney.
Microscopic appearance: many glomeruli appear normal,
whereas others show varying degrees of ischemic change.
Initially, the glomerular capillaries are thickened and
shriveled. Cells of the glomerular tuft are progressively lost.
Collagen and matrix material are deposited within
Bowman's space opposite the hilus. Eventually, the
glomerular tuft is obliterated by a dense, eosinophilic
globular mass inclosed in a scar, all within Bowman's
capsule. Tubular atrophy is associated with fibrosis of the
related interstitium.
49.
Benign nephrosclerosis50.
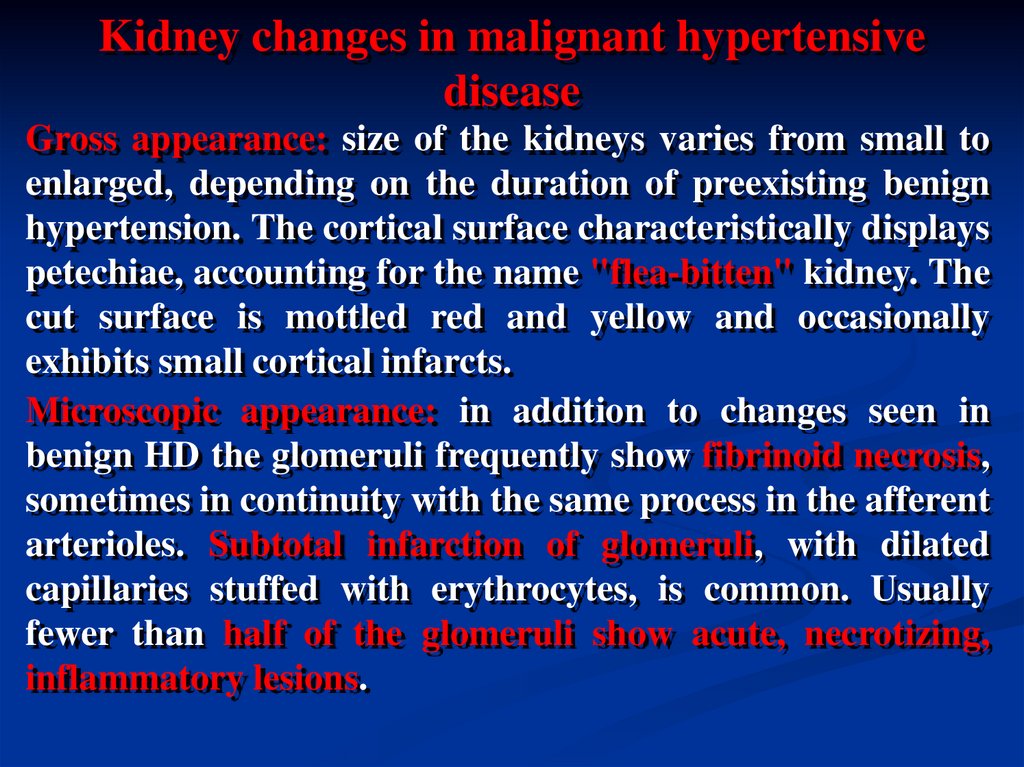
Kidney changes in malignant hypertensivedisease
Gross appearance: size of the kidneys varies from small to
enlarged, depending on the duration of preexisting benign
hypertension. The cortical surface characteristically displays
petechiae, accounting for the name "flea-bitten" kidney. The
cut surface is mottled red and yellow and occasionally
exhibits small cortical infarcts.
Microscopic appearance: in addition to changes seen in
benign HD the glomeruli frequently show fibrinoid necrosis,
sometimes in continuity with the same process in the afferent
arterioles. Subtotal infarction of glomeruli, with dilated
capillaries stuffed with erythrocytes, is common. Usually
fewer than half of the glomeruli show acute, necrotizing,
inflammatory lesions.
51.
“Flea-bitten” kidney in malignant hypertension52.
Ischemic heart disease (IHD) is caused bydecreasing of coronary blood flow due to
atherosclerosis or hypertensive disease.
Classification:
Acute IDH:
1. Angina pectoris.
2. Myocardial infarction.
Chronic IHD:
1. Diffuse tiny-focal cardiosclerosis;
2. Massive post-infarction cardiosclerosis.
53.
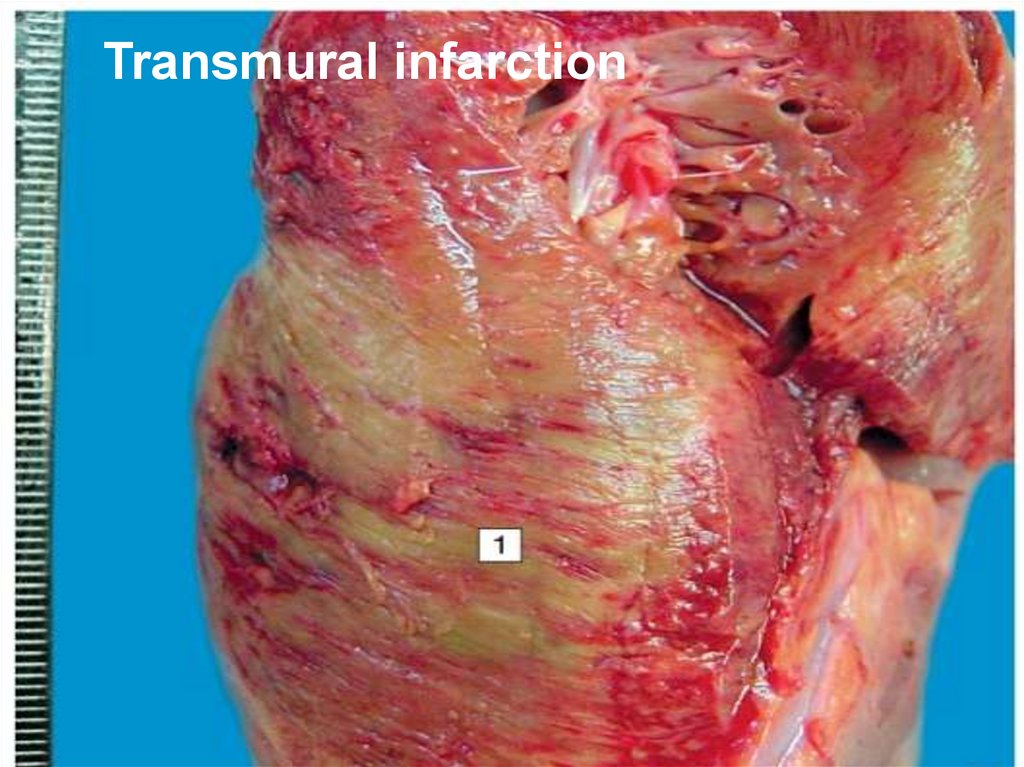
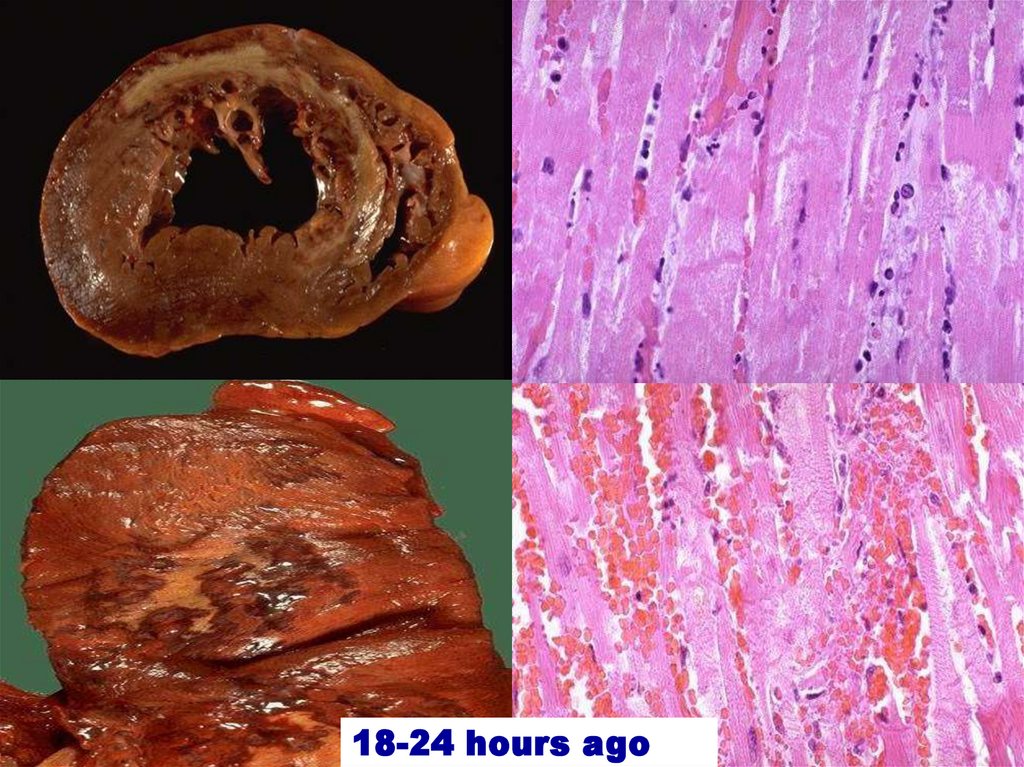
Transmural infarction54.
18-24 hours ago55.
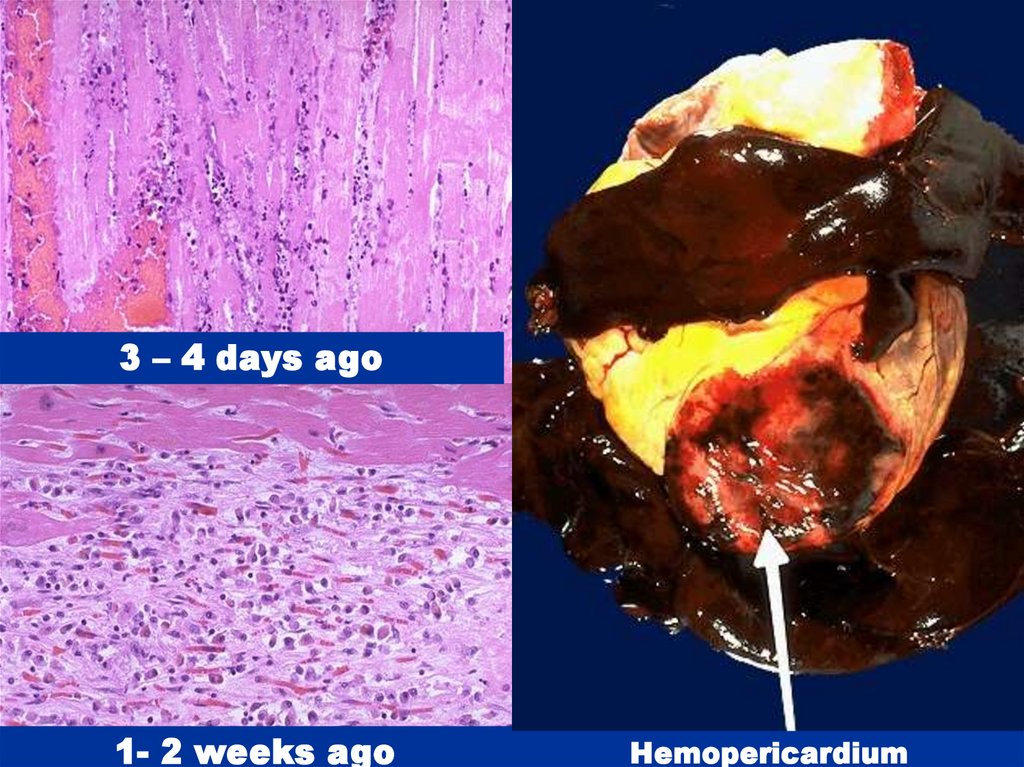
3 – 4 days ago1- 2 weeks ago
Hemopericardium
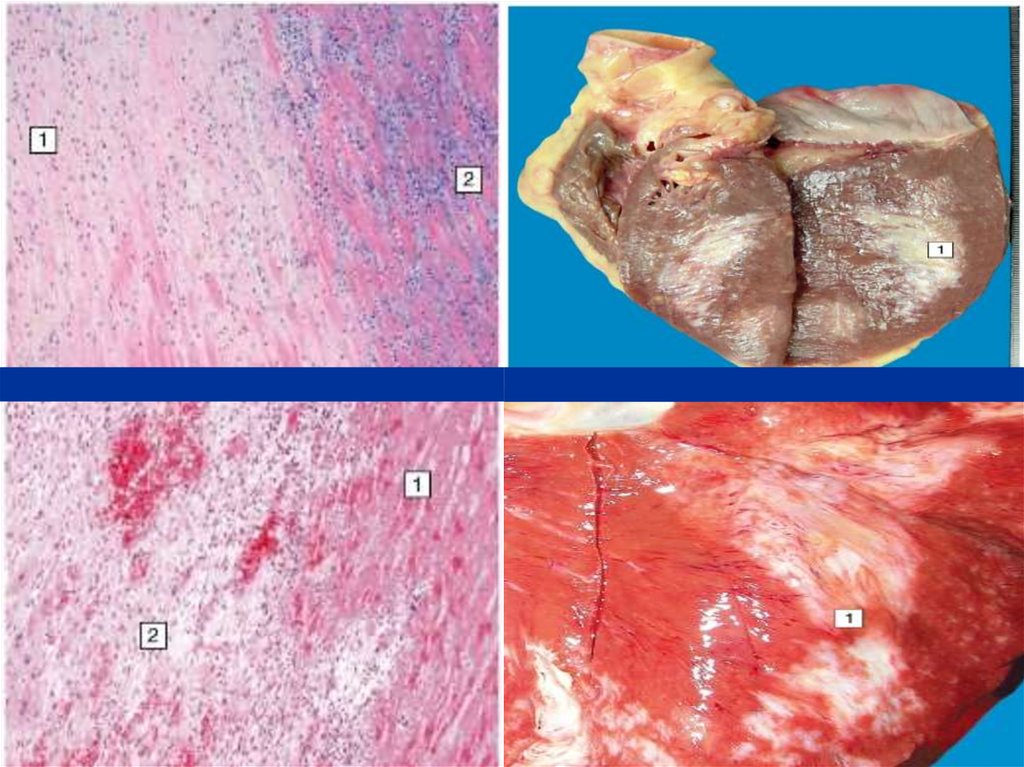
56.
57.
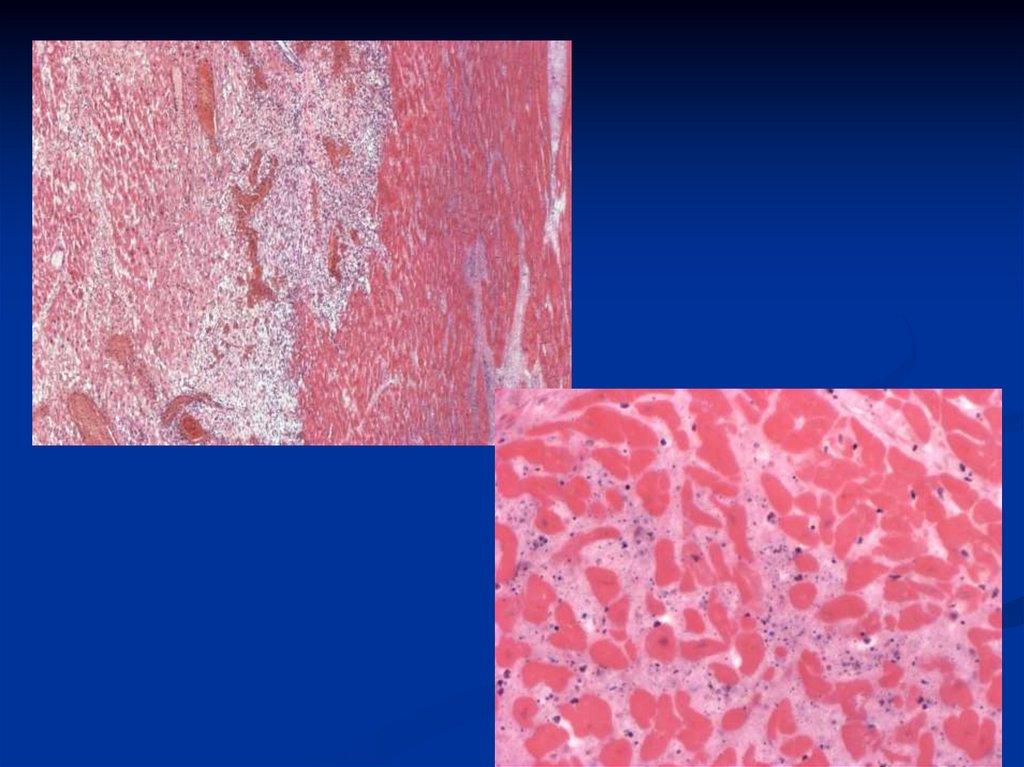
58.
59.
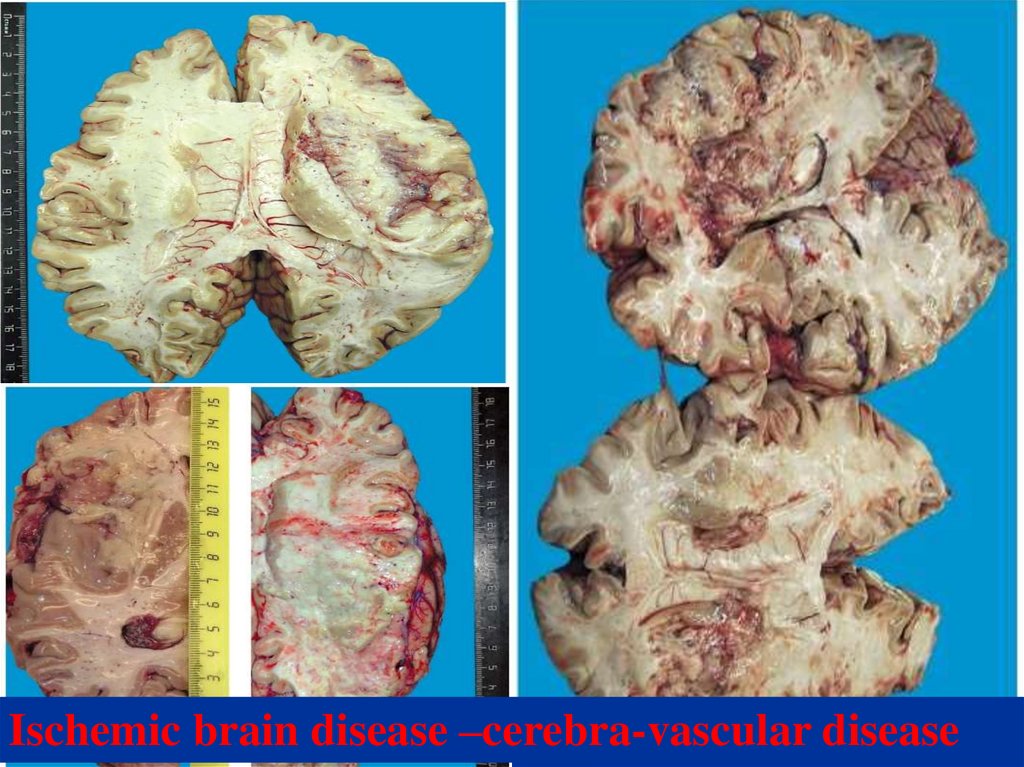
Ischemic brain disease –cerebra-vascular disease60.
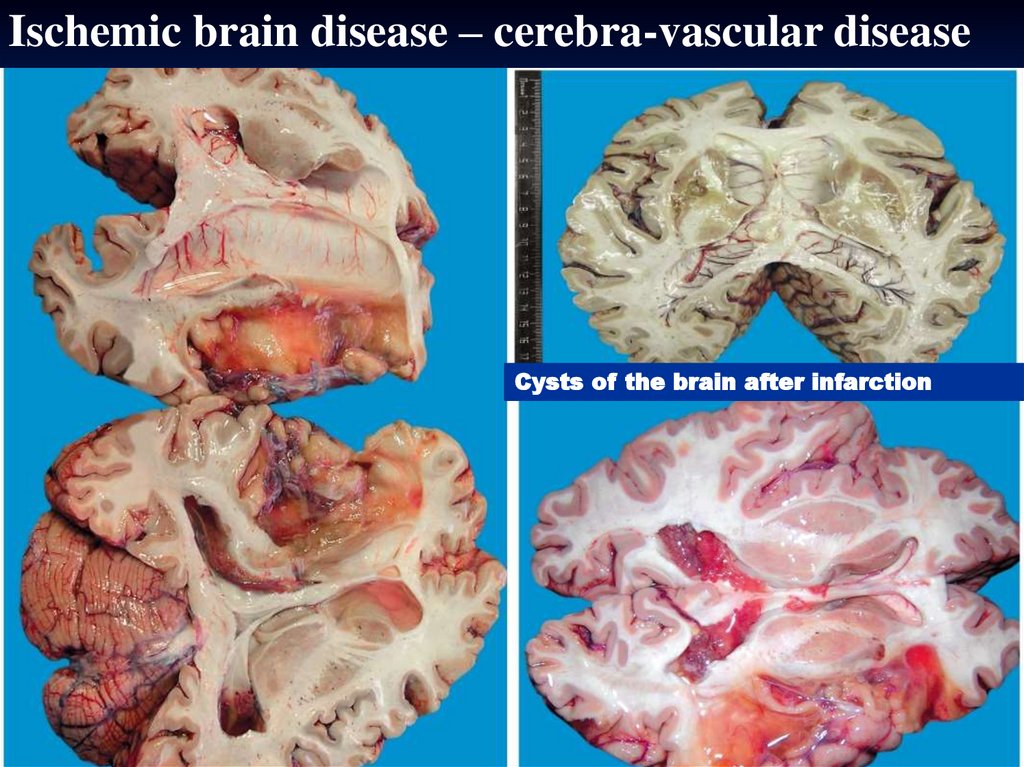
Ischemic brain disease – cerebra-vascular diseaseCysts of the brain after infarction









 Медицина
Медицина