Похожие презентации:
Maximizing the medical treatment of endometriosis, the double progestin system (DPS) for difficult endometriosis
1. Maximizing the medical treatment of endometriosis, the double progestin system (DPS) for difficult endometriosis
Moamar Al-Jefout MD, PhD2. Declaration
• I declare no conflict of interests3. Notion
Medical treatment should be the first linemodality for Deep Endometriosis (DE) in
women with pain symptoms
4. Facts
• No medical therapy is effective on all patientswith a chronic condition;
• Effective drugs with no side effects just do not
exist;
• Medications for chronic disorders are, by
definition, symptomatic.
• Rapid symptom recurrence at drug
discontinuation is expected
• “Inefficacy,” is defined as lack of symptom
relief during treatment and not after treatment
5. Current status regarding surgical Rx for DE
• For almost a century, the surgical treatment of endometriosis has been basedmainly on a straightforward oncologic principle, i.e. radical removal of lesions.
• Endometriotic deep lesions are benign and usually not progressive (Fedele L,
2004)
• The outcome and complications of surgical treatment for DE are difficult to
assess, because they are influenced by numerous variables including severity
of the disease, number and location of endometriotic nodules, degree of
infiltration of the bowel or the urinary tract and overall experience of the
surgical team
• There are no specific guidelines from any society regarding the indication and
surgical approach for bladder and bowel DE. (Kho, RM ., 2018)
• Currently, the general recommendation by ACOG, ESHRE, and SOGC for the
definitive treatment of pain associated with DE is still hysterectomy with or
without bilateral salpingo-oophorectomy in women with no desire for future
fertility, associated intractable pelvic pain, adnexal masses, or multiple
previous conservative surgical procedures
(G.A.J. Dunselman, 2014; American College of Obstetricians and Gynecologists,
2010; N. Leyland, 2010)
6. Population-based data do not suggest that conservative surgery constitutes a durable remedy for severely symptomatic
endometriosis patients.• Weir et al. (2005) analysed the clinical records of 53 385 hospital
admissions for the treatment of endometriosis in the province of
Ontario, Canada, from 1994 to 2002.
• The records of 7993 patients with 15 years of age or older, with no
prior hospital admission for endometriosis in the preceding 2 years,
who underwent ‘minor’ or ‘intermediate’ conservative surgery for
early disease, constituted the base for a 4 year longitudinal study.
• During the observation period, the likelihood of hospital readmission for additional surgical treatment was 27% and that of
having a hysterectomy was 12%.
• However, in spite of a substantial risk of re-operation, operative
laparoscopy is increasingly performed for treating symptomatic
endometriosis.
• On the basis of large epidemiologic databases, it has been
estimated that ∼1 in 400 North American women aged 15–45 years
is hospitalized for surgical treatment of endometriosis each year
(Weir et al., 2005).
7. Recurrence of deep lesions after surgery
Recurrence of deep lesions
after surgery
A repeat procedure within 5 years from primary surgery because of recurrence of pain was
reported in about one in five women (19%) who underwent bowel resection (C. De
Cicco,2011)
The 24 month cumulative probability of moderate or severe dysmenorrhoea recurrence was
20% in the former group and 25% in the latter, without statistically significant differences.
Crosignani et al. (1996)
A similar rate of pain recurrence (22%), 2 years after laparoscopic surgery for stage III–IV
disease, was reported by Busacca et al. (1999) in a group of 141 patients.
Abbott et al. (2003) investigated the outcomes of laparoscopic excision of endometriosis up
to 5 years after surgery in 176 women with severe pain symptoms, the 5 year cumulative
probability of requiring further surgery was 36%.
Vignali et al. (2005) evaluated the risk of pain and disease recurrence after conservative
surgery for endometriosis in a series of 115 women with deep lesions. After a minimum
follow-up of 12 months, recurrence of pain was observed in 28 patients (24%) and
recurrence of lesions in 15 (13%). Twelve subjects (10%) underwent repetitive surgery.
Multivariate analysis demonstrated that only age was a significant predictor of pain
recurrence, enhancing the risk in younger patients. Recurrence of lesions was predicted by
obliteration of the Douglas pouch and re-operation was predicted by non-radical first-line
surgery.
8. Recurrence after surgery
• NICE Committee maintained “in view of the high rateof recurrence of endometriosis, affecting long-term
quality of life for many women, improvement in longterm control of the condition was felt by the
Committee to be clinically very important.
• The Committee were aware of the high rate of
reoperation for endometriosis with associated risks of
surgery and, as there was strong evidence to support
this, considered that avoidance of repeat surgery by
the use of long -term medical therapy would be
beneficial.
9. Impact of endometriosis on risk of further gynaecological surgery: a national cohort study
• The incidence of subsequent gynaecological surgery wassignificantly higher in women with endometriosis (n = 11
052; 62%) when compared with women with no evidence
of endometriosis at laparoscopy (n = 42 136; 50.6%),
women who had undergone laparoscopic sterilisation (n =
58 704; 36%) and age‐matched women from the general
population (n = 2907; 16.3%).
• The median (IQR) time for a second surgical procedure
(after the initial diagnostic operation) for the endometriosis
group was less than 2 years [1.8 (0.8, 4.6)], which was
significantly shorter than the corresponding period in
women in the three unexposed groups. Half of all women
with endometriosis had undergone repeat surgery within
5.5 years.
L Saraswat D Ayansina KG Cooper S Bhattacharya AW Horne S
Bhattacharya 2017 BJOG
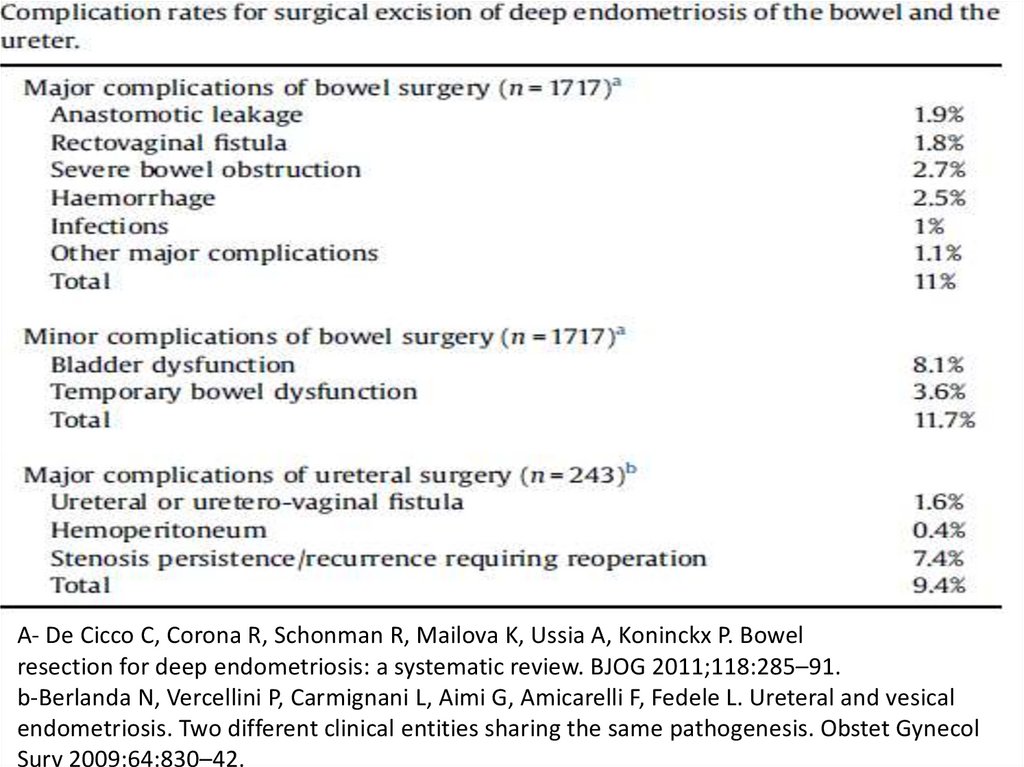
10. Complications of surgery for DE
• The overall complication rate was 24%, and the severe complicationrate (i.e., Clavien-Dindo IIIB) was 3% (n = 4). (Jayot, Aude, 2020)
• A recent systematic review revealed a 6.3% rate of major
complications following bowel endometriosis resection, including:
– Transient urinary retention: The most frequently reported postoperative difficulty is urinary retention, probably due to damage to the
parasympathetic plexus resulting in temporary bladder denervation.
This problem is associated with, but it is not exclusive to, colorectal
resection (Dubernard et al., 2008).
– Fistula: with a reported risk as high as 10% even in expert hands (Darai
et al., 2005; Dubernard et al., 2006).
– Anastomotic leakage (0.8% of cases).
– Anastomotic stricture (6.3%) of a total of 1643 patients who
underwent laparoscopic rectosigmoid resection. Protective ileostomy
is the sole modifiable factor related to anastomotic stenosis
(Bertocchi, E, 2019).
• Many women prefer to live with residual dyschezia than to risk a
fecaloid fistula or a derivative colostomy.
11. A- De Cicco C, Corona R, Schonman R, Mailova K, Ussia A, Koninckx P. Bowel resection for deep endometriosis: a systematic
review. BJOG 2011;118:285–91.b-Berlanda N, Vercellini P, Carmignani L, Aimi G, Amicarelli F, Fedele L. Ureteral and vesical
endometriosis. Two different clinical entities sharing the same pathogenesis. Obstet Gynecol
Surv 2009;64:830–42.
12. So what advice could we sensibly give women who need to decide on whether they opt for surgical treatment of lower bowel
endometriosis?• Until we have robust data, it is difficult to provide women with
accurate information about the surgical risk.
• Based on the larger studies in the review by De Cicco et al., we can
advise that the chances of having a major surgical complication are
probably around 10%.
• The case series of Kondo et al. suggests that the major complication
rate is likely to be lower in women undergoing a mucosal skimming
procedure relative to those having a segmental resection.
• Women also need to be advised that the complication rate may be
higher in units that have relatively little experience of this surgery
and, as recommended by the Royal College of Obstetricians and
Gynaecologists (RCOG), the surgeon should quote his/her own
complication rate.
De Cicco C, 2011; Kondo W, 2011; Royal College of Obstetricians and
Gynaecologists. 2008
13.
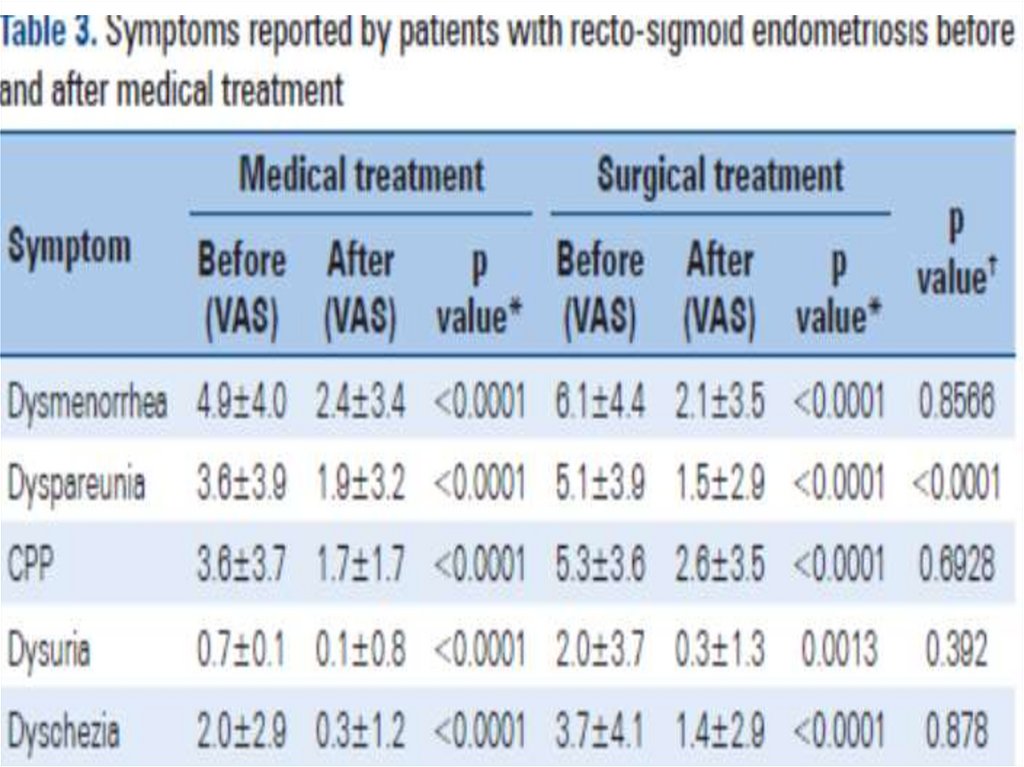
Medical rx for endometriosis14. Medical treatment for DE (Andres,MP, 2019)
• Methods: Retrospective study based on data extracted frommedical records of 238 women with recto-sigmoid endometriosis.
• Results: Over the course of follow-up, 143 (60.1%) women
remained in medical treatment while 95 (39.9%) presented with
worsening of pain symptoms or intestinal lesion growth (failure of
medical treatment group), with surgical resection performed in 54
cases.
• Conclusion: Patients with recto-sigmoid endometriosis who failed
to respond to medical treatment were younger and had larger
intestinal lesions. Hormonal therapy was equally efficient in
improving pain symptoms other than dyspareunia compared to
surgery, and was associated with lower complication rates in
women with recto-sigmoid endometriosis.
• Medical treatment should be offered as a first-line therapy for
patients with bowel endometriosis. Surgical treatment should be
reserved for patients with pain symptoms unresponsive to
hormonal therapy, lesion growth or suspected intestinal
subocclusion.
15.
16.
17.
18. Symptom progression in patients with recto-sigmoid endometriosis submitted to medical or surgical treatment
19. Factors to be considered before treatment plan decision for DE
• Severity of symptoms• Size of the lesions
• Pain symptoms unresponsive to hormonal
therapy,
• Lesion growth or suspected intestinal
subocclusion.
• Age of the patient- younger patients seems to
have more recurrence
• BMI- high BMI is associated with recurrence
• Feasibility of surgery
20. A lesion-based, three-tiered risk stratification system
• a. Low-risk lesion: superficial peritoneal implantsprogressed in only one third of women- may be bettercandidates for treatment with OCs rather than
with progestogen monotherapies.
• b.Medium-risk lesions: Ovarian endometriomas-low
association with malignancy, typically less than 0.8%asymptomatic endometriomas do not require intervention
for infertility- low-dose OCs, used cyclically or continuously.
• High-risk lesions: Deep fibrotic nodules- Progestogens,
instead of OCs, should generally be considered the first-line
medical treatment- two-thirds of patients with deep
endometriosis respond favorably to progestogen treatment
P. Vercellini, 2016
21. A symptom-based, stepped-care approach
• NICE Committee confirmed two fundamental principles (1):• (1) “all treatments led to a clinically significant reduction in
pain on the VAS when compared to placebo. The magnitude
of this treatment effect was similar for all treatments,
suggesting that there was little difference between them in
their capacity to reduce pain. No other significant
differences were found between the hormonal treatments”;
and
• (2) “it is known that there are a cluster of extremely cheap
hormonal treatments (including the combined oral
contraceptive pill) and a cluster of extremely high-cost
treatments including dienogest and GnRHas”
1- National Institute for Health and Care Excellence, 2017
22. A symptom-based, stepped-care approach
• low-dose OCs should be used cyclically in women withperitoneal and ovarian endometriosis, stepping up to
continuous use with tailored cycling only in those
women with persistent dysmenorrhea despite cyclic OC
use.
• In case of inefficacy on pain during OC use, patients
should step up to a low-cost progestogen such as NETA.
• Starting directly with a low-cost progestogen should be
considered in patients with deep lesions or with
deep dyspareunia as their main complaint.
• In case of inefficacy of or intolerance to progestogens,
patients may step up to GnRH-agonists or antagonists
23. The goal of endometriosis therapy
• “the goal of endometriosis therapy shouldalways be absence of pain; if this end point is not
achieved with oral contraceptives, the patient
should be offered more definitive therapy. Many
patients fail to adequately respond to oral
contraceptives while others develop progestin
resistance with disease progression despite using
a progestin based therapy […] The realization that
all therapies have different efficacy and the
availability of new endometriosis drugs will allow
more rapid progression to definitive therapy”
H.S. Taylor, 2017
24. The burden of illness and the burden of treatment
• The burden of illness: Women with severely symptomaticendometriosis, in addition to pain, usually experience
major worsening in health-related quality of life,
psychological status, sexual functioning and marital
relationship, social life, and school or work productivity.
• The burden of treatment: endometriosis, includes taking
medications, managing side effects, attending gynecologic
visits, performing imaging investigations and repeated
blood tests, undergoing surgical procedures, selfmonitoring, lifestyle changes, administrative task to access
and coordinate care, full or partial payment of treatments,
and other hidden costs.
G. Spencer-Bonilla, 2017
25. Pros and cons of combined oral contraceptives
• In a large, multicenter, placebo-controlled RCT conducted in womenwith symptomatic endometriosis, a low-dose oral contraceptive (OC)
substantially improved not only dysmenorrhea but also other pain
symptoms including nonmenstrual pain and deep dyspareunia (1).
• However, Casper suggested that progestogens should be preferred to
OCs as a first-line treatment, based on the consideration that
estrogen and progesteron receptors would be, respectively, over- and
underexpressed in ectopic endometrial implants- potential risk of
lesion progression (2).
• The currently available epidemiological data do not support a
pathogenic role of OCs in the development of endometriosis (3)
• OCs when chosen as a modality to manage endometriosis,
combinations with the lowest possible estrogen dose should be
chosen, such as those with only 15–20 μg of EE or 1.5 mg of 17 βoestradiol (E2)
1- T. Harada, 2017. 2- R.F. Casper, 2017. 3- P. Vercellini, 2011
26. Use of OCs continuously instead of cyclically!!
• When pooling published data, no statistically significantdifferences were observed between the two treatment
schedules in other pain symptoms as well as in
postoperative ovarian endometrioma recurrence rate (1).
• Using OC continuously increases the likelihood of erratic
bleeding that, if not promptly dealt with by tailored
cycling (2), may cause prolonged pain (3)
• Cyclic OC use may increase therapeutic compliance in
patients (amenorrhea).
• Continuous and tricycling (where three packets are taken in
a row, followed by a pill free interval) may be the best
approach (4)
1- L. Muzii, 2014. 2- T. Harada, 2017. 3- P. Vercellini, 2013.
4- National Institute for Health and Care Excellence,2017
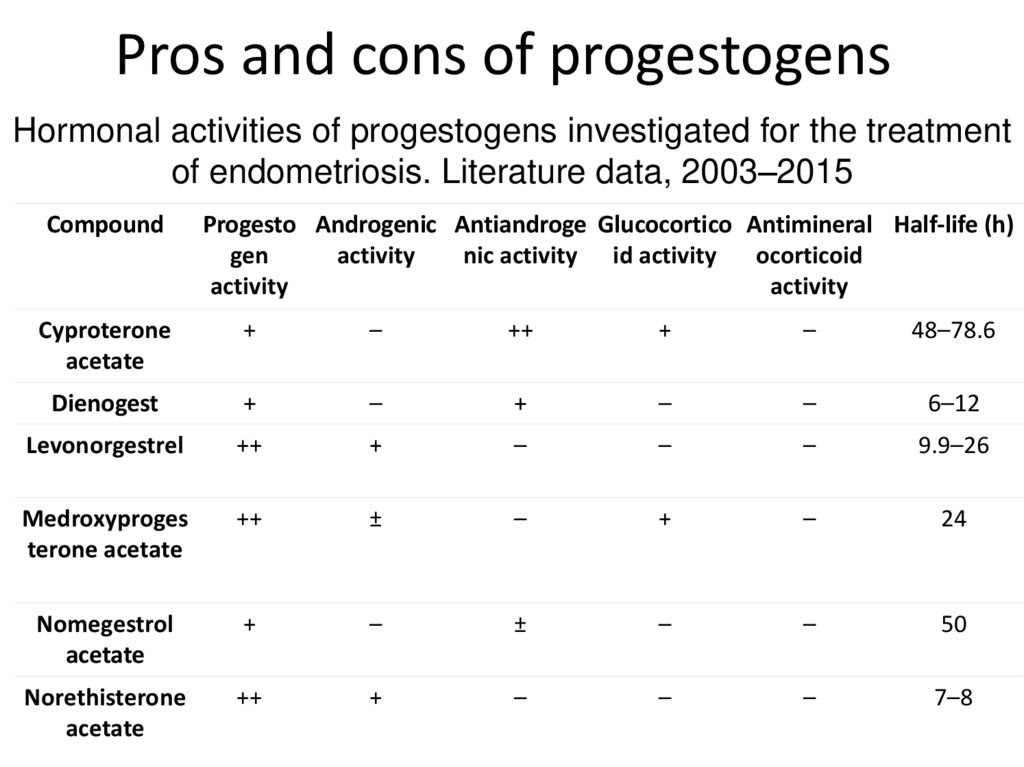
27. Pros and cons of progestogens
Hormonal activities of progestogens investigated for the treatmentof endometriosis. Literature data, 2003–2015
Compound
Progesto Androgenic Antiandroge Glucocortico Antimineral Half-life (h)
gen
activity
nic activity id activity
ocorticoid
activity
activity
Cyproterone
acetate
+
–
++
+
–
48–78.6
Dienogest
+
–
+
–
–
6–12
Levonorgestrel
++
+
–
–
–
9.9–26
Medroxyproges
terone acetate
++
±
–
+
–
24
Nomegestrol
acetate
+
–
±
–
–
50
Norethisterone
acetate
++
+
–
–
–
7–8
28. Cost of progestogens
• Low-cost progestogens includemedroxyprogesterone acetate (MAP),
norethisterone acetate (NETA), levonorgestrel
(LNG), and nomegestrol acetate (NOMAC).
• Dienogest (DNG) is the only high-cost
progestogen currently licensed for the
treatment of endometriosis.
29.
“Every woman is unique and so is her responseto progestogen, hence, we need to explore
which progestin suites each woman”
Al-Jefout Moamar
30. GnRH agonists
• The profound hypoestrogenic state achievedduring the use of these drugs explains their
efficacy in terms of pelvic pain relief and, at the
same time, their limited tolerability and safety.
• The combination of GnRH agonists with add-back
therapy (generally, a bone-sparing progestogen
such as NETA or an estrogen–progestogen
hormone replacement therapy) limits vasomotor
side effects and prevents bone resorption, but
further increases costs
31. GnRH antagonist-Elagolix,
• The GnRH antagonist at the oral daily dose of 150 or 400 mg was tested against aplacebo.
• At 3-month evaluation- a clinical response with respect to dysmenorrhea were 43–
46% and 72–76% in the lower- and the higher-dose elagolix group, respectively,
• At the end of the 6-month study period, the percentage of participants
experiencing amenorrhea in the high-dose elagolix group in the two trials varied
from 47% to 66%.
• Hot flushes - reported by 42–48% of women in the high-dose elagolix group.
• The mean percent bone mineral density (BMD) reduction at the lumbar
spine observed at 6-month follow-up in women in the high-dose elagolix group
varied from −2.49 to −2.61.
• Therefore, unless GnRH antagonists will be marketed at a price lower than that of
GnRH agonists, the advantages of the former compounds over the latter ones may
reveal smaller than expected.
• Unplanned pregnancy rate in women who used elagolix was over 1% (6/497)
H.S. Taylor, 2017
32.
Dual progestogen-delivery system (DPS)therapy with levonorgestrel intrauterine
system and etonogestrel subdermal implant for
severe and persistent endometriosis-associated
pelvic pain: An effective new therapy.
• Cecilia Hoi Man Ng (PhD), Anthony James Marren (FRANZCOG), Ian
Stewart Fraser (MD, DSc), Angela Pardey (MBBS), John Pardey (MBBS) and
Moamar Ibrahim Al-Jefout (MD, PhD)
33.
34. DPS (Dual progestogen-delivery System) for refractory endometriosis
• Objective: To explore the usefulness ofsimultaneous use of dual progestogendelivery systems (DPS) with the LNG-IUS and
etonogestrel subdermal implant (ESI) as a new
combination therapy for severe, refractory
endometriosis-associated pelvic pain
35. Women refractory to conventional therapies
• Management of endometriosis depends primarily on whether thewoman wishes to conceive or not.
• The American Society for Reproductive Medicine (ASRM), the
European Society of Human Reproduction and Embryology (ESHRE)
and the World Endometriosis Society (WES) have developed
comprehensive consensus statements for the management of
chronic pelvic pain and endometriosis. Other organizations have
also developed detailed evidence-based reviews of management
(e.g. Cochrane Collaboration).
• These have all tried to offer sound, evidence-based
recommendations from randomized trials on large numbers of
women.
• However, little attention has been given specifically to that small
group of women with refractory symptoms who have responded
poorly to more conventional therapies.
36. LNG-IUS & etonogestrel subdermal implant for endometriosis
LNG-IUS & etonogestrel subdermalimplant for endometriosis
• Recently, there has been a gradual move towards greater use of
local delivery of progestogen via LNG-IUS; Mirena®, which delivers
levonorgestrel into the uterine cavity at a steady rate of 20 mg/day
from the time of insertion.
• It has been demonstrated to be an effective therapy in the
prevention of recurrence of endometriosis following laparoscopic
treatment, as well as moderately effective in control of pain
symptoms in many women with endometriosis.
• There has also been occasional use of a systemic but constant
delivery of progestogen through the etonogestrel subdermal
implant (ESI; Implanon®, which delivers etonogestrel at a steady
initial rate of 60 – 70 mg/day into the systemic circulation.
• It has been reported that the ESI may be effective in improving
primary dysmenorrhea and also pelvic pain associated with
endometriosis.
37. Rational for combination
• When both systems are combined a steady low-dose delivery ofprogestogens is maintained that should offer simultaneous dual
targeting of local uterine and more distant lesions, as well as
preventing new lesions from forming.
• A constant local and systemic combined delivery of progestogen
offered by the LNG-IUS and ESI should offer a logical extension of
conventional hormonal treatment of “difficult” endometriosis.
• Simultaneous use of the LNG-IUS and the ESI for a case of
debilitating adolescent endometriosis was first reported by AlJefout, et al. 2009.
• The case study of a 13-year-old female with pelvic pain secondary
to endometriosis, refractory to a series of conventional medical and
conservative surgical therapies and whose life was completely
dominated by the persistent pain of endometriosis.
• In this case a combination of LNG-IUS and ESI proved to be a highly
effective dual therapy, allowing her to return to school studies and
a completely normal lifestyle.
38. Ethics approval & Indications for the combined therapy
Ethics approval & Indications for thecombined therapy
• This retrospective case series was approved by
the Ethics Review Committees from Royal Prince
Alfred Hospital, Sydney and the University of
Sydney.
• The patients, and where relevant, their parents,
gave informed consent to undertake this off-label
therapy
• Prior to the insertion of the DPS, all women had
undergone a series of attempts at various
medical and/or surgical treatments, without
satisfactory control of symptoms
39. DPS
• Objective: To explore the usefulness ofsimultaneous use of dual progestogen-delivery
systems (DPS) with the LNG-IUS and etonogestrel
subdermal implant (ESI) as a new combination
therapy for severe, refractory endometriosisassociated pelvic pain.
• Methods: This report details the very successful
simultaneous use of LNG-IUS and ESI for
debilitating and refractory endometriosis in 40
women with refractory pelvic pain secondary to
endometriosis.
40. Results:
• The mean duration of use of the DPS was 28.1 (range 9 – 98) months.• The mean age at first review was 25.2 (range 13 – 50) years. The mean
duration of symptomatology was 7.9 (range 0.5 – 30) years – 39/40
recorded dysmenorrhea; 16/19 deep dyspareunia; 12/40 dyschezia;
and 4/40 dysuria; 16/40 recorded additional symptoms (e.g. heavy
menstrual bleeding, erratic pelvic pain, and painful abdominal
bloating).
• A small proportion of the teenagers (n = 4; 10% of the total) could be
classified as “dramatic” improvement, defined as the development of
amenorrhea with no pelvic pain. “Marked” improvement, as defined by
the major resolution of most symptomatology was reported in 26/40
(65%).
• Three had a “borderline” initial response (i.e. some improvement in
symptoms) but then obtained marked and ongoing improvement after
short-term supplementation with an oral progestogen or 3 months of a
GnRH analogue.
• Persistent borderline benefit was reported in 5/40 (13%).
41. Conclusions:
• The combination DPS appears to be aneffective new medical option in management
of refractory endometriosis-associated pelvic
pain. This DPS is a promising, sustainedrelease approach for severe, persistent
endometriosis pain, especially in young
women.



















 Медицина
Медицина