Похожие презентации:
Urticaria and Angioedema
1. Urticaria and Angioedema
2. Definitions
Chronic urticaria/angioedema are defined as weals,angioedema or both with daily or almost daily
symptoms lasting for more than 6 weeks.
British Society for Allergy and Clinical Immunology
(BSACI) 2015 guidelines also included episodic
acute intermittent urticaria/angioedema lasting for
hours or days and recurring over months or years.
Acute urticaria is an episode of spontaneous weals
lasting for <6 weeks
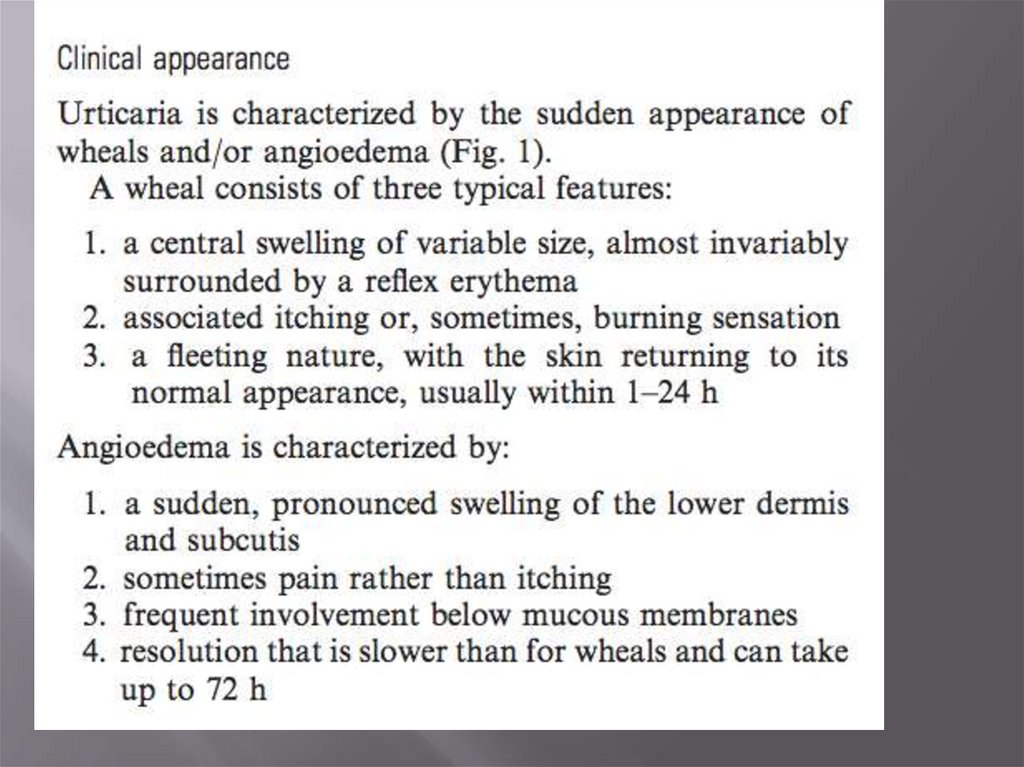
3. Urticaria
‘hives’ or ‘nettle rash’red (initially with a pale centre), raised,
superficial erythematous rash with intense
pruritus
Weals vary from a few millimetres to handsized lesions, single or numerous.
4.
5.
6. Angioedema (tissue swelling)
result of a local increase in vascular permeabilityoften notable in the face, oropharynx, genitalia and less
frequently in the gastrointestinal tract.
can be painful rather than itchy.
Weals affect the superficial skin layers (papillary dermis),
whereas angioedema can involve the submucosa, the
deeper reticular dermis and subcutaneous tissues.
Weals and angioedema often coexist, but either can occur
separately.
Characteristically the weals arise spontaneously and each
lesion resolves within 24 h.
angioedematous swellings that can persist for a few days.
7.
8.
9.
10.
11. Pathophysiology-1
mast cell activationrelease of histamine (and other inflammatory
mediators)
vasodilatation, increased blood flow and
increased vascular permeability
These mechanisms usually well respond to
antihistamines
12. swelling in the deeper layers in angioedema: additional mechanisms
several inflammatory mediators LTB4 and C5a lead toplasma leakage via neutrophil-dependent pathways
For this, adhesion of neutrophils to the vessel wall is
sufficient to initiate plasma leakage, neutrophil is not
passing through vascular endothelium
increase microvascular permeability leading to plasma
leakage and oedema formation.
More poor response on antihistamnies
Other mechanisms: perivascular infiltrates of CD4+
lymphocytes, monocytes and granulocytes (neutrophils,
basophils and eosinophils).
Diff.diagnosis – urticarial vasculitis - small vessels
vasculitis with deposition of immunoglobulin and
complement
13.
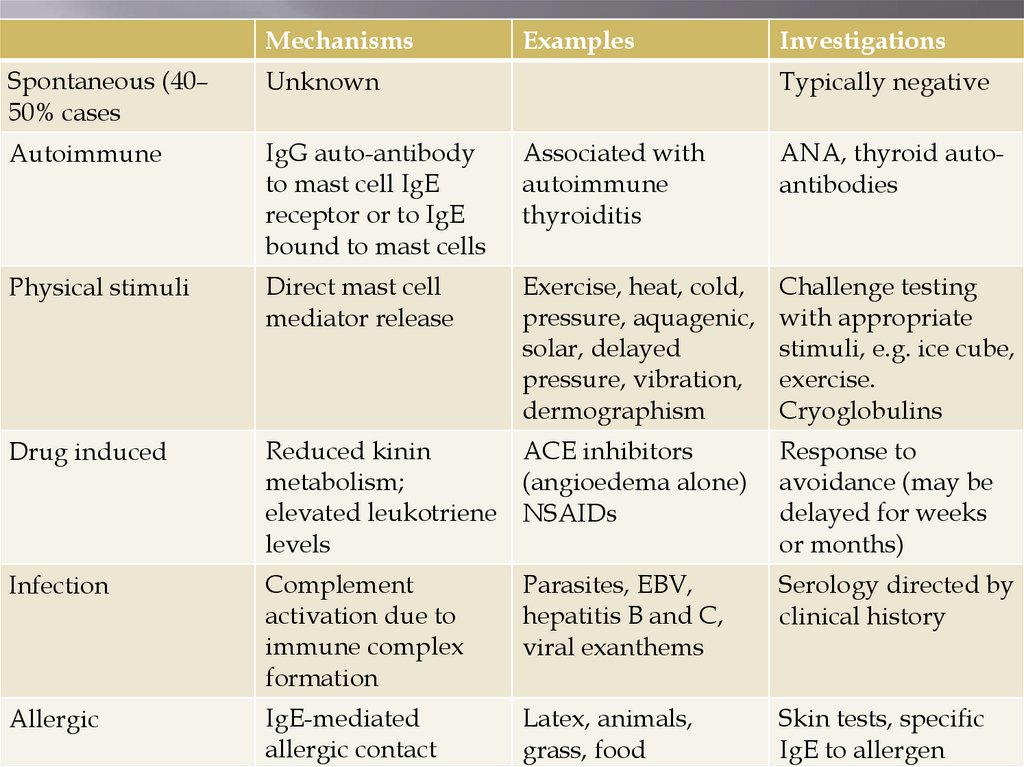
MechanismsExamples
Investigations
Spontaneous (40–
50% cases
Unknown
Autoimmune
IgG auto-antibody
to mast cell IgE
receptor or to IgE
bound to mast cells
Associated with
autoimmune
thyroiditis
ANA, thyroid autoantibodies
Physical stimuli
Direct mast cell
mediator release
Exercise, heat, cold,
pressure, aquagenic,
solar, delayed
pressure, vibration,
dermographism
Challenge testing
with appropriate
stimuli, e.g. ice cube,
exercise.
Cryoglobulins
Drug induced
Reduced kinin
ACE inhibitors
metabolism;
(angioedema alone)
elevated leukotriene NSAIDs
levels
Response to
avoidance (may be
delayed for weeks
or months)
Infection
Complement
activation due to
immune complex
formation
Parasites, EBV,
hepatitis B and C,
viral exanthems
Serology directed by
clinical history
Allergic
IgE-mediated
allergic contact
Latex, animals,
grass, food
Skin tests, specific
IgE to allergen
Typically negative
14.
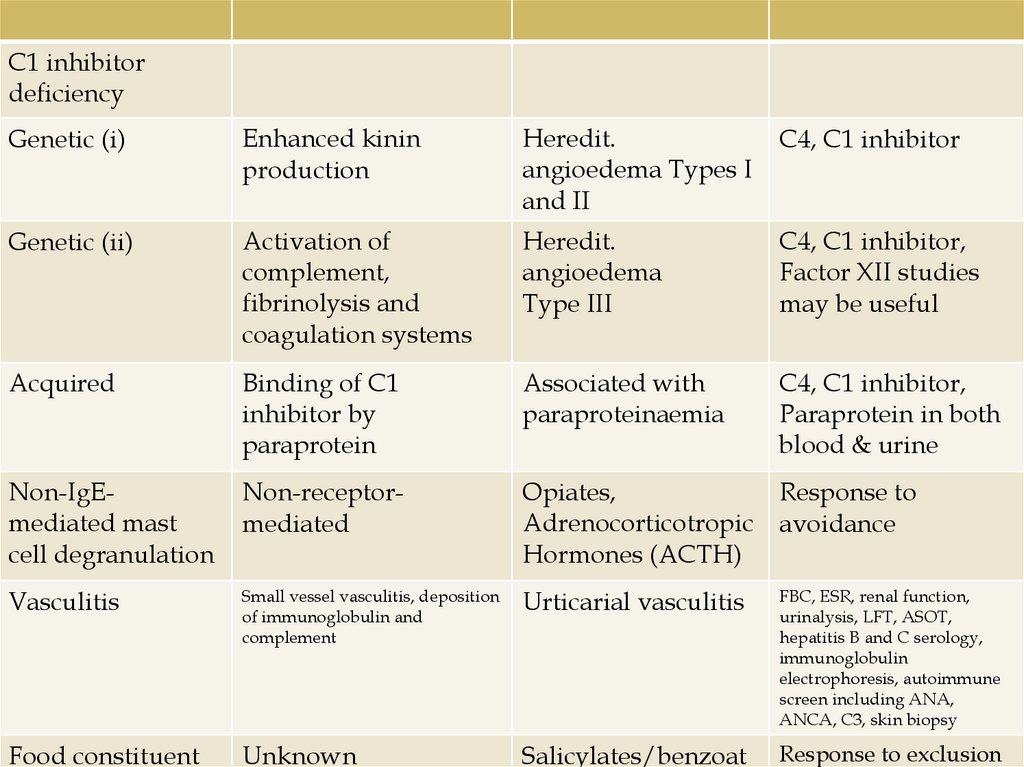
C1 inhibitordeficiency
Genetic (i)
Enhanced kinin
production
Heredit.
angioedema Types I
and II
C4, C1 inhibitor
Genetic (ii)
Activation of
complement,
fibrinolysis and
coagulation systems
Heredit.
angioedema
Type III
C4, C1 inhibitor,
Factor XII studies
may be useful
Acquired
Binding of C1
inhibitor by
paraprotein
Associated with
paraproteinaemia
C4, C1 inhibitor,
Paraprotein in both
blood & urine
Non-IgEmediated mast
cell degranulation
Non-receptormediated
Opiates,
Adrenocorticotropic
Hormones (ACTH)
Response to
avoidance
Vasculitis
Small vessel vasculitis, deposition
of immunoglobulin and
complement
Urticarial vasculitis
FBC, ESR, renal function,
urinalysis, LFT, ASOT,
hepatitis B and C serology,
immunoglobulin
electrophoresis, autoimmune
screen including ANA,
ANCA, C3, skin biopsy
Food constituent
Unknown
Salicylates/benzoat
Response to exclusion
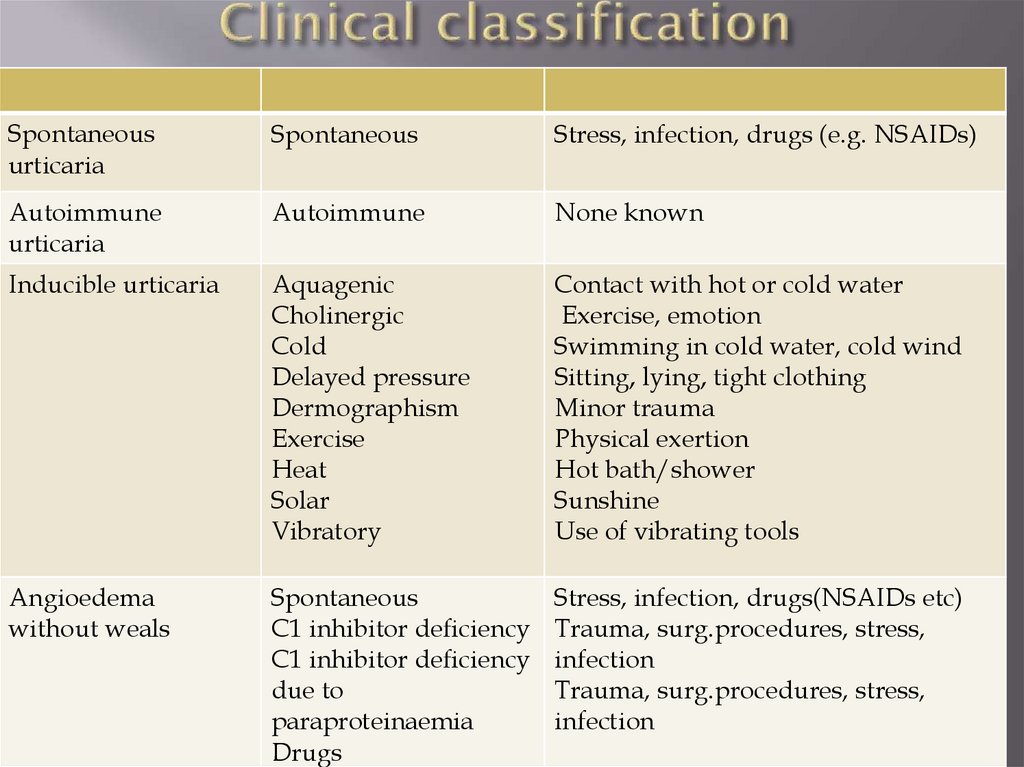
15. Clinical classification
Spontaneousurticaria
Spontaneous
Stress, infection, drugs (e.g. NSAIDs)
Autoimmune
urticaria
Autoimmune
None known
Inducible urticaria
Aquagenic
Cholinergic
Cold
Delayed pressure
Dermographism
Exercise
Heat
Solar
Vibratory
Contact with hot or cold water
Exercise, emotion
Swimming in cold water, cold wind
Sitting, lying, tight clothing
Minor trauma
Physical exertion
Hot bath/shower
Sunshine
Use of vibrating tools
Angioedema
without weals
Spontaneous
C1 inhibitor deficiency
C1 inhibitor deficiency
due to
paraproteinaemia
Drugs
Stress, infection, drugs(NSAIDs etc)
Trauma, surg.procedures, stress,
infection
Trauma, surg.procedures, stress,
infection
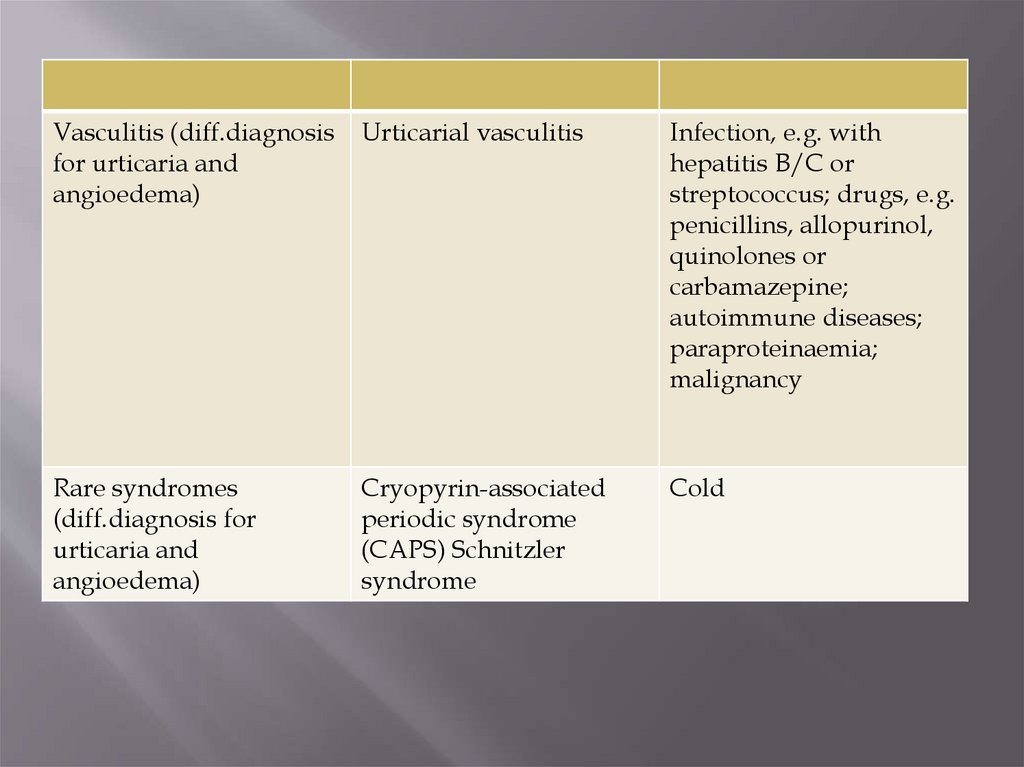
16.
Vasculitis (diff.diagnosisfor urticaria and
angioedema)
Urticarial vasculitis
Infection, e.g. with
hepatitis B/C or
streptococcus; drugs, e.g.
penicillins, allopurinol,
quinolones or
carbamazepine;
autoimmune diseases;
paraproteinaemia;
malignancy
Rare syndromes
(diff.diagnosis for
urticaria and
angioedema)
Cryopyrin-associated
periodic syndrome
(CAPS) Schnitzler
syndrome
Cold
17. Autoimmune urticaria
In 30% of patients with chronic urticariaIgG to alpha subunit of the IgE receptor on mast
cells/less commonly IgG antibodies to IgE
antibodies are disease specific
Associated with more intense and protracted disease
course
Both IgE and IgG related degranulation of mast cells
+ classical complement pathway activation
18. Vasculitis/immune complex-associated urticaria
Complement activation can mediate/ augmenthistamine release via anaphylatoxin C5a.
This pathway is triggered by immune
complexes formation (for example in hepatitis
C, hepatitis B, EBV and possibly parasitic
infections)
19. Inducible urticarias
triggering by heat, cold, pressure, vibration, water,ultraviolet light, etc.
induced reproducibly after a specific physical
stimulus is applied
Weals appear immediately and characteristically
fade within 1 h
delayed pressure urticaria develops more slowly
after physical pressure and lasts several hours or
days.
may require higher dose antihistamine therapy and
delayed pressure urticaria may remain refractory
20. Possible food triggers.
typically non-allergic with most patients havingspontaneous or autoimmune urticaria/ angioedema.
patients or their parents frequently analyse foods and food
additives eaten over the previous 24 h or longer in the search
for a connection with the symptoms
in IgE-mediated food allergy, symptoms occur reproducibly
within 60 min of exposure to the food rather; do not last
several days.
urticaria and angioedema associated with IgEmediated food
allergic reactions seldom occur in isolation, usually present
oropharyngeal itching and discomfort, wheezing, vomiting
or abdominal pain.
Exceptions: reactions to allergens like omega-5 gliadin in
wheat and lipid transfer proteins in plant-derived foods
(present as intermittent spontaneous urticaria/exerciseinduced anaphylaxis)
21. Mechanisms specifically related to angioedema without weals
ACE inhibitorshereditary angioedema (HAE)
NSAIDs and antibiotics
acquired forms of C1 inhibitor deficiency due
to serum paraproteins having auto-antibody
activity against C1 inhibitor.
Immune complex formation by IgG with
tumour surface antigens results in complement
consumption (decrease C4, low C1 inhibitor)
22. ACE-related
first weeks of treatmentMore rare - after many years of use
mechanism - reduced metabolism of bradykinin
Same - angioedema associated with angiotensin receptor
blockers (ARB’s)
swelling of tongue, sometimes also lips, pharynx, larynx
and viscera; fatal cases reported
may persist for several months after withdrawal of the ACE
inhibitor
individuals of Afro-Caribbean origin are at increased risk of
ACE inhibitor-induced angioedema
Treatment: antihistamines, corticosteroids and adrenaline;
also bradykinin antagonists, such as icatibant, can be
effective
23.
Chronic urticariaChronic spontaneous urticaria (previously
called CiU – chronic idiopathic urticaria (not
associated with the antibodies)
Chronic autoimmune urticaria (associated with
h antibodies to IgE/IgE receptor - high-affinity
IgE receptor FceR1)
Hereditary Angioedema (typically associated
with C1 inhibitor deficiency)
24. Prevalence
lifetime prevalence for all types of urticaria is8.8%
Chronic urticaria develops in 30–45% of these
individuals
25.
Urticaria alone in 50% of casesurticaria with angioedema in 40%
angioedema without weals in 10%
26. Prognosis
At least 20% of chronic urticaria patients withsymptoms severe enough to warrant hospital
referral remain symptomatic 10 years after first
presentation
Increased duration of chronic urticaria
correlates with clinical severity, the presence of
angioedema and positive antithyroid
antibodies
positive autologous serum test has been
correlated with more severe symptoms but not
prolonged disease duration
27. Diagnosis: allergic cause
Could it be related to any drugs the patient hastaken (ACE inhibitor/aspirin/NSAID)
Does it occur only and reproducibly within 60
min (usually within 20 min) of eating a
particular food? Exceptions meat and
crustaceans (such as prawn).
Does it occur only if a particular food (wheat
etc) eaten followed by exercise?
Does it occur after contact with an allergen to
which the patient is sensitized (animals, grass,
food, latex, etc.)?
28. Investigation
skin prick testing to a panel of aeroallergens andsuspect foods.
Negative results - non-allergic
symptoms are linked to exertion or exercise:
limited specific IgE testing to related food
allergens (omega-5-gliadin or lipid transfer
proteins etc)
In certain Mediterranean areas, Anisakis simplex
hypersensitivity associated with the consumption
of raw fish should be considered
Full blood count (FBC): eosinophils may be
elevated in parasitic infections and some drug
induced reactions
29. Dif.diagnosis: vascilitis/autoimmune
Are episodes of urticaria/angioedema persistentrather than self-limiting?
Do individual lesions last more than 24 h?
Are urticarial lesions tender and painful rather
than itchy?
Does skin show evidence of residual petechial
haemorrhage, purpura or bruising?
Does patient have any symptoms and signs of
underlying disease, e.g. fever, significant malaise,
arthralgia, hypertension, and blood or protein in
urine?
30. Investigations
Blood count: neutrophils elevation – associatedwith urticarial vasculitis.
Urinalysis: haematuria and proteinuria
Acute phase response (ESR/CRP)
high ESR with normal CRP – paraproteinaemia
Thyroid function and auto-antibodies
(autoimmune urticaria)
31. Others: Complement studies—
C1inhibitor deficiency – for angioedemawithout weals (C4 and C1 inhibitor); C4 level is
low in most cases of Types I and II even
between attacks.
C3 and C4 - suspected urticarial vasculitis, if
reduced, measurement of anti-C1q antibodies
may be useful.
32. Immunoglobulins
older than 40 years with systemic symptoms(malaise, fever, polyarthralgia,
lymphadenopathy, leukocytosis) – serum Ig
and electrophoresis undertaken (IgM
paraprotein - Schnitzler syndrome)
Cryoglobulins - secondary cold urticaria
Acquired angioedema without urticaria - can
be associated with a B cell lymphoma and a
search for a paraprotein may be indicated.
33. Skin biopsy
in unusual presentation or in cases ofsuspected vasculitis
Clinical clues include systemic symptoms
(fever and arthralgia or arthritis) and lesions
lasting for more than 24 h, or associated with
tenderness, petechiae, purpura or skin staining
as the lesions fade. Linear bruising suggests
excessive scratching
34. Autologous serum skin test
research toolautologous serum skin test (ASST) intradermal injection of the patient’s own
serum; positive weal and flare reaction is
considered indicative of circulating
autoantibodies to the high-affinity IgE receptor
on the mast cell
35. Nasendoscopy
In unexplained pharyngeal obstruction(establish or exclude the presence of
angioedema of the throat)
differential diagnoses of ‘swelling, lump or
discomfort in the throat’ - gastro-oesophageal
reflux and vocal cord dysfunction.
36. See scheme
37.
Avoidance strategies: patient educationSymptom control:
Standard dose non-sedating H1
Higher dose of H1 up to 4 times dose
recommended/add in second antihistamine
Consider a second line agent, anti-leukotriene or,
if angioedema is present, use tranexamic acid
At severe exacerbations: short course of
corticosteroids (up to 40 mg total per day, for 3
days, then decrease)
Consider immunomodulant (omalizumab,
cyclosporine etc)
38.
Tranexamic acid— benefit patients withangioedema particularly those without weals
(inhibits conversion of plasminogen to plasmin
and consequently production of bradykinin)
39. adult patients with weals
Check that symptomatic episodes have not followed ingestion of anon-steroidal anti-inflammatory drug such as aspirin or
ibuprofen.
Give explanation of the symptoms and reassurance that the
histamine-induced chronic urticaria symptoms do not involve the
respiratory tract (upper and/or lower) or cardiovascular system –
as occurs in anaphylaxis. There are, however, very rare exceptions
to this rule.
Give a once-daily dose of a long acting, nonsedating
antihistamine (prn, if symptoms are infrequent).
If necessary, double the dose of antihistamine (usually given at
night), and/or add a second antihistamine.
Consider further increase in dose of antihistamine up to 4
recommended dose.
Consider adding one or more second-line drugs
Consider short-term oral corticosteroid rescue treatment.
40. with angioedema with weals in adults (addition to above mentioned)
If taking ACE inhibitor, stopin patients not taking ACE inhibitor, avoid in future.
Consider addition of tranexamic acid for higher dose
antihistamine-resistant angioedema.
An adrenaline auto-injector is rarely required and
should only be considered if there is a history of
significant angioedema affecting the upper airway
(rare in angioedema with urticaria). The patient should
then be shown how to use the device and provided
with a written self-management protocol.
Consider short-term oral corticosteroid rescue
treatment
41. angioedema without weals in adults
Exclude C1 inhibitor deficiency – normal: plasma C4during an attack/normal C4, C1 inhibitor; C1 inhibitor
function, between attacks
If taking an ACE inhibitor, stop; if not taking – avoid
once-daily dose of a long acting, non-sedating
antihistamine; consider higher doses of antihistamines.
Consider tranexamic acid in antihistamine-resistant
angioedema.
adrenaline auto-injector and short-term oral
corticosteroids are unlikely to be beneficial unless an
underlying histaminergic mechanism is considered to
be responsible for the angioedema.










 Медицина
Медицина