Похожие презентации:
Hemorrhagic vasculitis
1. JSW “Astana Medical University” Department of internal illnesses IWS Theme: Hemorrhagic vasculitis Made by: Zhumagaliyeva M.
434 GMChecked by: Baydurin S.A.
Astana
2018 year
2. History
The disease is named after Eduard HeinrichHenoch (1820–1910), a German pediatrician (nephew
of Moritz Heinrich Romberg) and his teacher Johann
Lukas Schönlein (1793–1864), who described it in the
1860s. Schönlein associated the purpura and arthritis,
and Henoch the purpura and gastrointestinal
involvement. The English physician William
Heberden (1710–1801) and the dermatologist Robert
Willan (1757–1812) had already described the disease in
1802 and 1808, respectively, but the name Heberden–
Willan disease has fallen into disuse. William Osler was
the first to recognise the underlying allergic mechanism
of HSP.
Eduard Heinrich Henoch
(1820-1910)
Johann Lukas Schönlein
(1793-1864)
3.
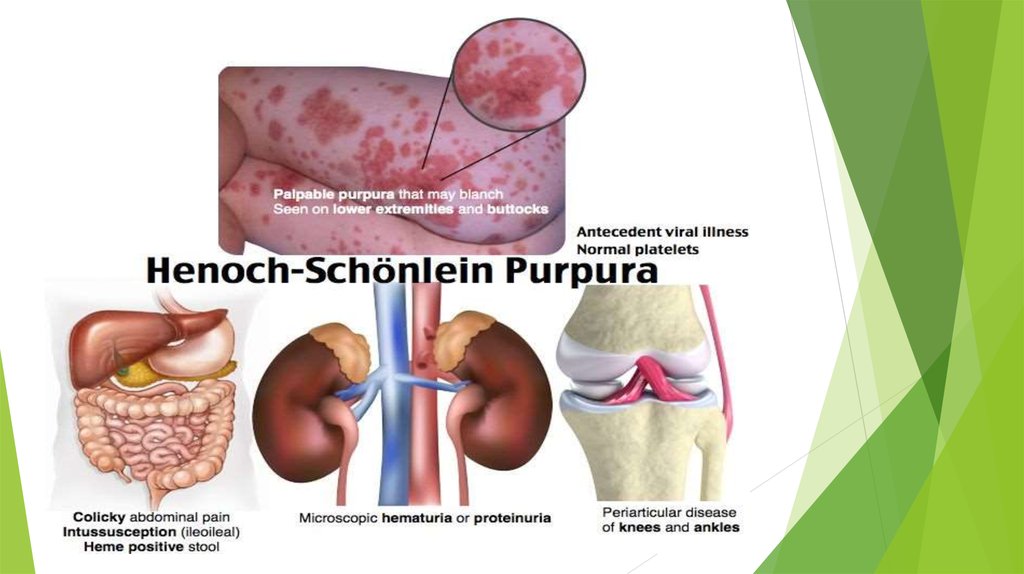
Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, anaphylactoidpurpura, purpura rheumatica, and Schönlein–Henoch purpura,is a disease of
the skin, mucous membranes, and sometimes other organs that most commonly
affects children. In the skin, the disease causes palpable purpura(small, raised areas
of bleeding underneath the skin), often with joint pain and abdominal pain.
With kidney involvement, there may be a loss of small amounts
of blood and protein in the urine (hematuria and proteinuria), but this usually goes
unnoticed; in a small proportion of cases, the kidney involvement proceeds
to chronic kidney disease.
4.
5. Etiology
The etiology is unknown. There may be a connection withstreptococcal and viral infection. Provocative factors,
along with infections are vaccinations, food and drug
allergies, cooling, sensitization with endogenous proteins
and metabolites. In many cases, the provoking factor can
not be determined. The relationship of the disease with
allergic heredity
6.
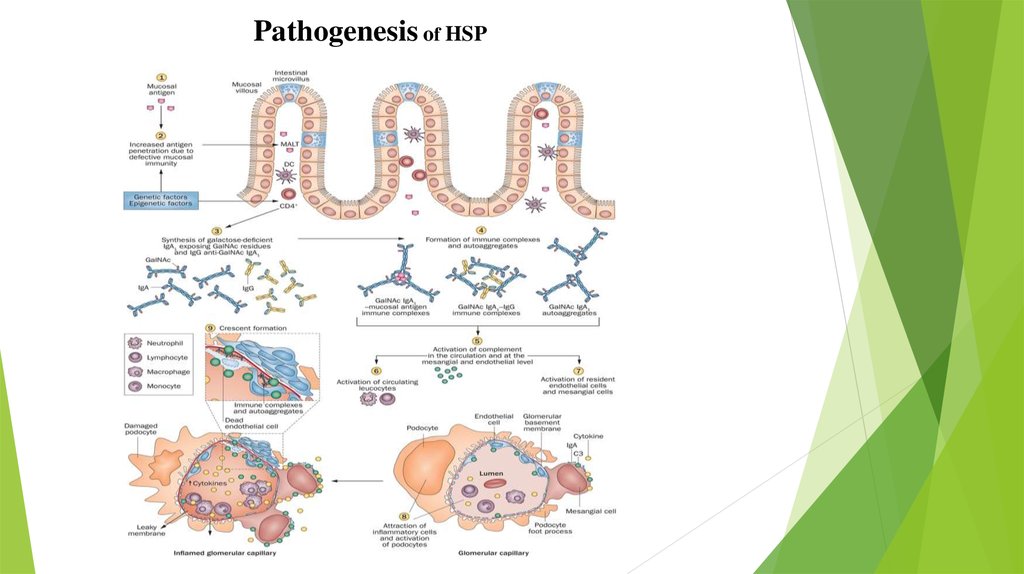
7. Pathogenesis
At present, it has been shown that HS belongs toimmunocomplex diseases, in which microvessels undergo
aseptic inflammation with more or less deep destruction of
the walls, thrombosis and the formation of extravasates
due to the damaging effect of circulating low molecular
weight immune complexes and activated components of
the complement system
8.
Antigen-antibody complexes (AA) with an equimolarplasma ratio are known to precipitate and are eliminated
from circulation by phagocytic cells. Soluble or circulating
complexes form with a significant quantitative
predominance of the antigen over the antibodies. It is they
who activate the copication that cause vasculitis with
fibrinoid necrosis, perivascular edema, microcirculation
blockage, leukocyte infiltration, hemorrhages and
dystrophic changes to the extent of necrosis in the lesions.
9.
Along with the above-mentioned main pathogeneticmechanism, a number of variants of the disease show a
more or less pronounced participation in the process of
cell-mediated immune mechanisms. Activated by antigen
and immune complexes, monocytes and lymphocytes
accumulate in the lesions, release monokines, tissue
thromboplastin, lymphokines, lysosomal enzymes and
other components, as a result of which disorganization of
the vascular wall and local thrombus formation are
intensified, perivascular granulomas are formed.
10.
Pathogenesis of HSP11. Classification of hemorrhagic vasculitis
In the clinical course of hemorrhagic vasculitis, an acute phase (initial period or exacerbation)and a phase of abating (improvement) are noted. According to the prevailing symptoms of the
disease, hemorrhagic vasculitis is classified into the following clinical forms: simple,
rheumatoid (articular), abdominal and fulminant. The degree of severity of hemorrhagic
vasculitis is:
Hemorrhagic vasculitis of mild severity - a satisfactory condition of patients and
unpronounced nature of the rash, arthralgia.
Moderately severe hemorrhagic vasculitis is a condition of a moderate patient, rashes are
abundant, arthralgia is accompanied by changes in joints according to the type of arthritis,
periodic pains in the abdomen and microhematuria are noted.
Severe hemorrhagic vasculitis - the patient has a serious condition, excessive spills with
necrotic areas, angioedema, nephrotic syndrome, macromuturia and gastrointestinal
hemorrhage, and acute renal failure is possible.
According to the nature of the flow, acute (up to 2 months), prolonged (up to six months)
and chronic hemorrhagic vasculitis are classified.
12. Clinical symptoms
1)SKIN SYNDROME occurs mostoften and is characterized by a
symmetrical appearance on the limbs,
buttocks and rarely on the body of the
papulose-hemorrhagic rash sometimes
with urticar elements. The eruptions are
monomorphic, have an inflammatory
basis distinctly expressed in the initial
period, in many cases palpable, i.e. to
the touch are defined as seals or
elevations.
13.
2)JOINT SYNDROME occurs often with the cutaneous or several hours or daysafter. In large joints (knee, etc.), pain of different intensity is noted.
14.
3)ABDOMINAL SYNDROME is often observed in childhood (in54-72% of patients), and in 1/3 it dominates the clinical picture,
and in some cases precedes skin changes. This makes it
particularly difficult to correctly diagnose.
The main symptom is severe abdominal pain, constant or
cramping, sometimes reaching such a high intensity that the
patients writhe in bed and for many hours cry.
Periods of severe pain can alternate with completely painless
intervals lasting ~ 1-3 hours. This facilitates the differentiation of
abdominal syndrome with acute surgical diseases of the
abdominal organs. Especially difficult is this differentiation in the
absence of skin-joint manifestations and the presence of
symptoms of irritation of the peritoneum. Most often, the
abdominal syndrome stimulates OKN (invagination), appendicitis,
torsion of the ovarian cysts, perforation of the ulcer of the
intestine.
15.
4)RENAL SYNDROME is found in 1 / 3-1 /2 of the patients and proceeds most often as a
type of acute or chronic glomerulonephritis with micro- or macrogematuria, proteinuria
(from 0.33 to 30% protein in the urine),
cylindruria. Arterial hypertension with this
form of jade is rare. Sometimes a nephrotic
syndrome develops. Kidney damage often
occurs not immediately, after 1-4 weeks After
The onset of the disease.
16. Diagnostics
In the blood test, patients with hemorrhagic vasculitis usually have nonspecific signs ofmoderate inflammation (leukocytosis and a slight increase in ESR), an increase in the
number of platelets and eosinophils. In the analysis of urine there is hematuria,
proteinuria, cylindruria. A biochemical blood test shows an increase in immunoglobulin A
and CRP.
The results of the coagulogram are of great diagnostic importance. The lack of data in it
for a clotting disorder in the presence of clinical signs of hemorrhagic syndrome clearly
supports the hemorrhagic vasculitis.
With the development of renal syndrome, a patient with hemorrhagic vasculitis needs
consultation of the nephrologist, monitoring changes in the analysis of urine, biochemical
analysis of urine, Zimnitsky's test, kidney ultrasound, ultrasound of kidney vessels.
In severe diagnostic cases, a skin biopsy is indicated. Histological examination of the
biopsy reveals characteristic changes: the deposition of immunoglobulin A and CEC on
the endothelium and in the thickness of the vascular wall of venules, arterioles and
capillaries; formation of microthromboses; the exit of blood elements beyond the vessel.
17.
18.
The following studies are important for assessing the severity and variation of theprocess flow:
1. Quantitative determination of the content of von Willebrand factor in plasma.
2. Determination of the content of circulating immune complexes in the plasma
confirms the association of the disease with this basic mechanism.
3. Hyperfibrinogenemia, anemia in the plasma
Globulins, as well as acidic glycoprotein reflect the severity and severity of the
disease.
4. Determination in the serum of cryoglobulins
5. Determination of antithrombin III and heparin resistance of plasma.
19. Treatment
Patients with signs of hemorrhagic vasculitis in the acute phase must comply with bed rest andhypoallergenic diet, exclude the use of antibiotics and other medications that can enhance the
sensitization of the body.
The main drug in the treatment of hemorrhagic vasculitis is heparin. Therapy with prednisolone is still
a controversial issue among doctors. Perhaps its appointment in severe cases of hemorrhagic vasculitis.
In the absence of the effect of corticosteroid therapy, stock preparations are cytostatics. Severe course
of the disease is also an indication for carrying out extracorporal hemocorrection (hemosorption,
immunosorption, plasmapheresis).
The expressed articular syndrome of hemorrhagic vasculitis is stopped by the carrying out of antiinflammatory therapy (indomethacin, ibuprofen). Many authors note the ineffectiveness of
antihistamines in the treatment of hemorrhagic vasculitis. However, their use can be justified in
patients with an allergic anamnesis (allergic dermatitis, pollinosis, allergic rhinitis, etc.) or
manifestations of exudative-catarrhal diathesis. When the disease is associated with food allergy and
the presence of abdominal syndrome, enterosorbents are additionally prescribed.
20. Prognosis
Light forms of hemorrhagic vasculitis are prone tospontaneous cure after the first attack of the disease. With
lightning-fast form, death of patients can occur in the first
few days from the onset of the disease. Most often, it is
associated with the defeat of the central nervous system
and the emergence of intracerebral hemorrhage. Another
cause of death can be severe kidney syndrome, leading to
the development of uremia.
21. References
1. “Hematology in childhood” Papayan A.V., 19922. “Great Medical Encyclopedy” Vorob’ev A.I. 1979
3. “Internal illnesses” 2 book V.S.Mukhin, A.I.Martynov,V.S
Moiseev 2010







 Медицина
Медицина








