Похожие презентации:
Role of Ca2+ ions in mechanisms of cell signaling
1. Role of Ca2+ ions in mechanisms of cell signaling
Done by: Maulenova RMoldakozhayev A.
Naizabayeva D.
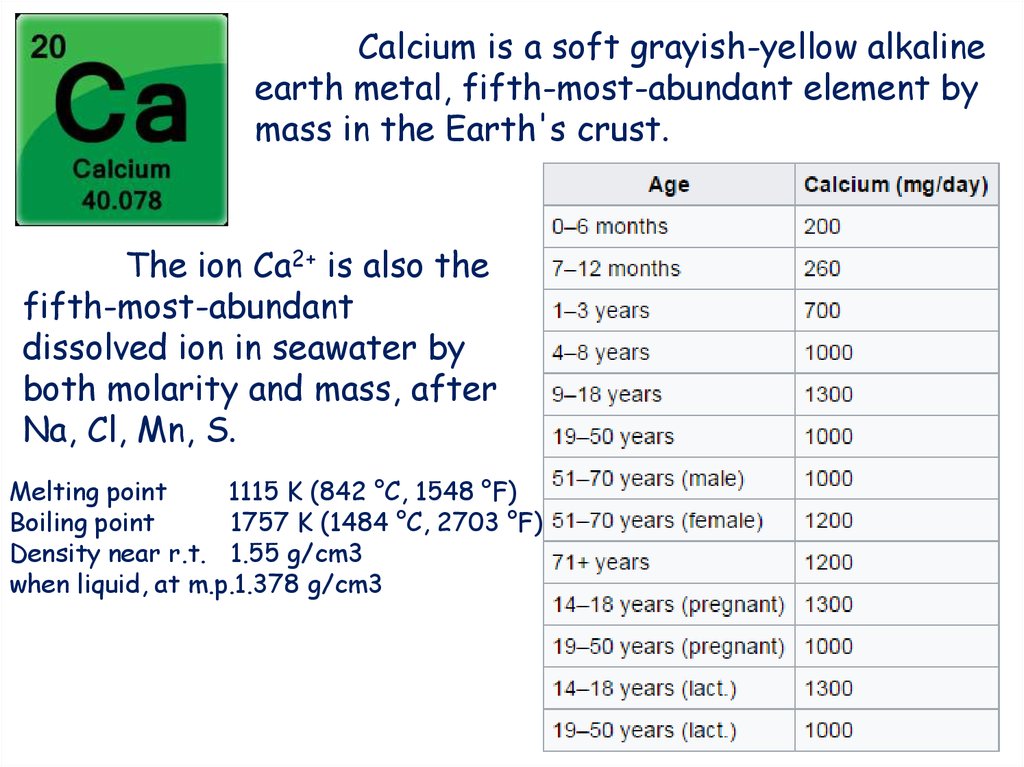
2. The ion Ca2+ is also the fifth-most-abundant dissolved ion in seawater by both molarity and mass, after Na, Cl, Mn, S.
Calcium is a soft grayish-yellow alkalineearth metal, fifth-most-abundant element by
mass in the Earth's crust.
The ion Ca2+ is also the
fifth-most-abundant
dissolved ion in seawater by
both molarity and mass, after
Na, Cl, Mn, S.
Melting point
1115 K (842 °C, 1548 °F)
Boiling point
1757 K (1484 °C, 2703 °F)
Density near r.t. 1.55 g/cm3
when liquid, at m.p.1.378 g/cm3
3.
4.
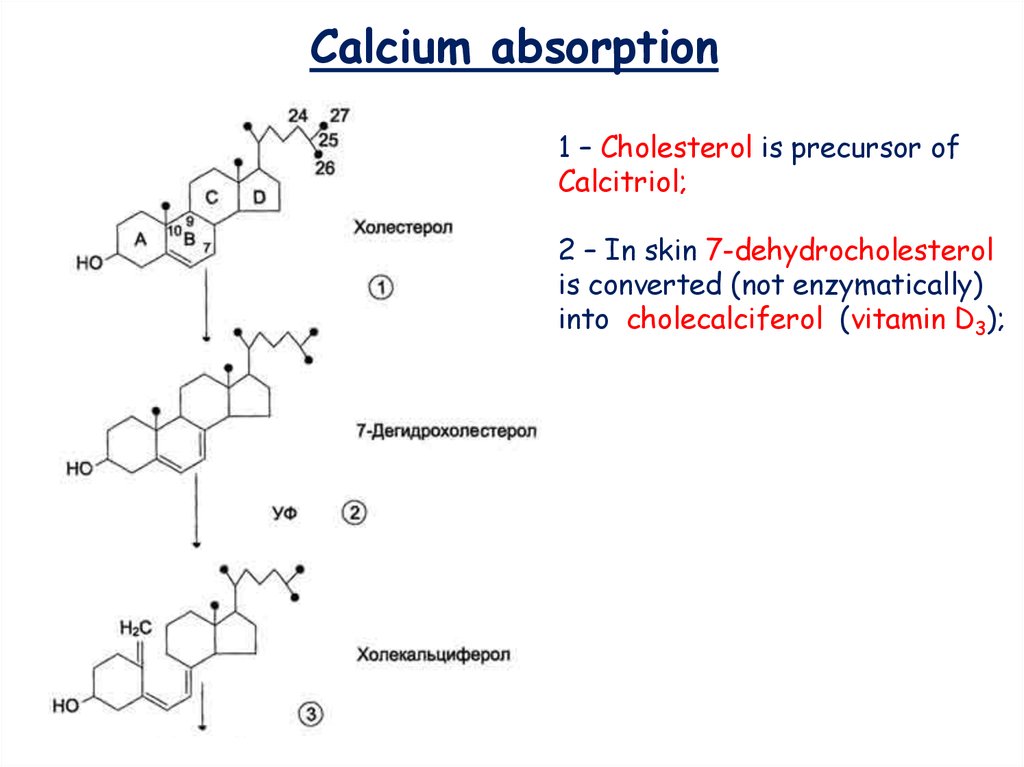
Calcium absorption1 – Cholesterol is precursor of
Calcitriol;
2 – In skin 7-dehydrocholesterol
is converted (not enzymatically)
into cholecalciferol (vitamin D3);
5.
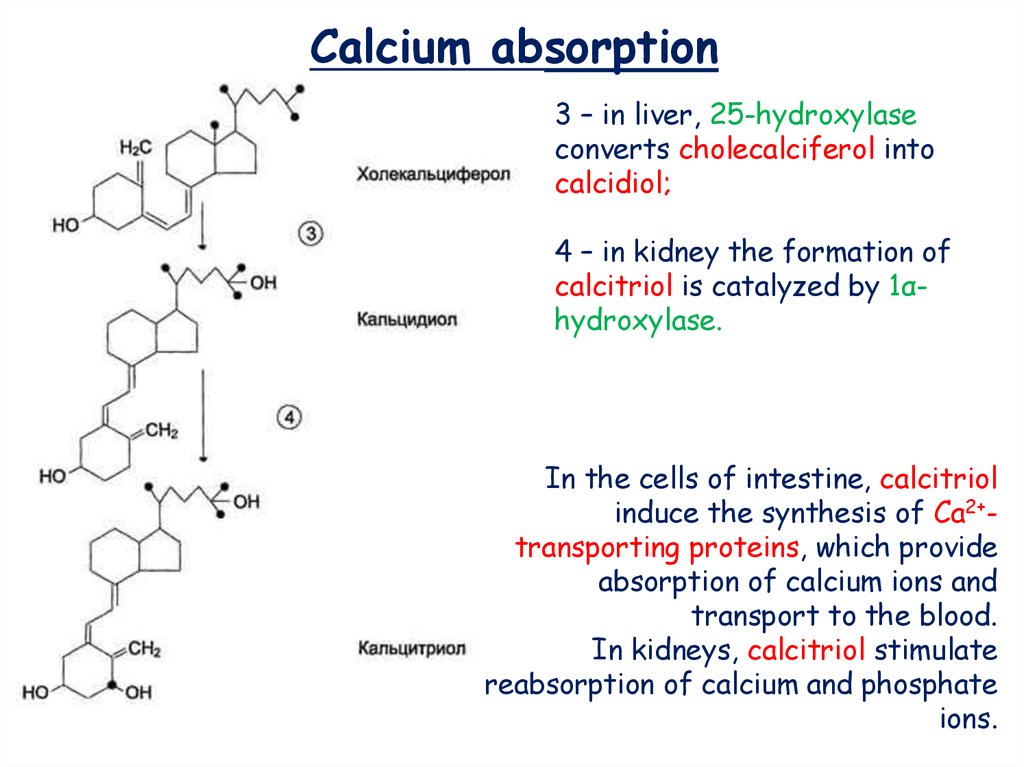
Calcium absorption3 – in liver, 25-hydroxylase
converts cholecalciferol into
calcidiol;
4 – in kidney the formation of
calcitriol is catalyzed by 1αhydroxylase.
In the cells of intestine, calcitriol
induce the synthesis of Са2+transporting proteins, which provide
absorption of calcium ions and
transport to the blood.
In kidneys, calcitriol stimulate
reabsorption of calcium and phosphate
ions.
6.
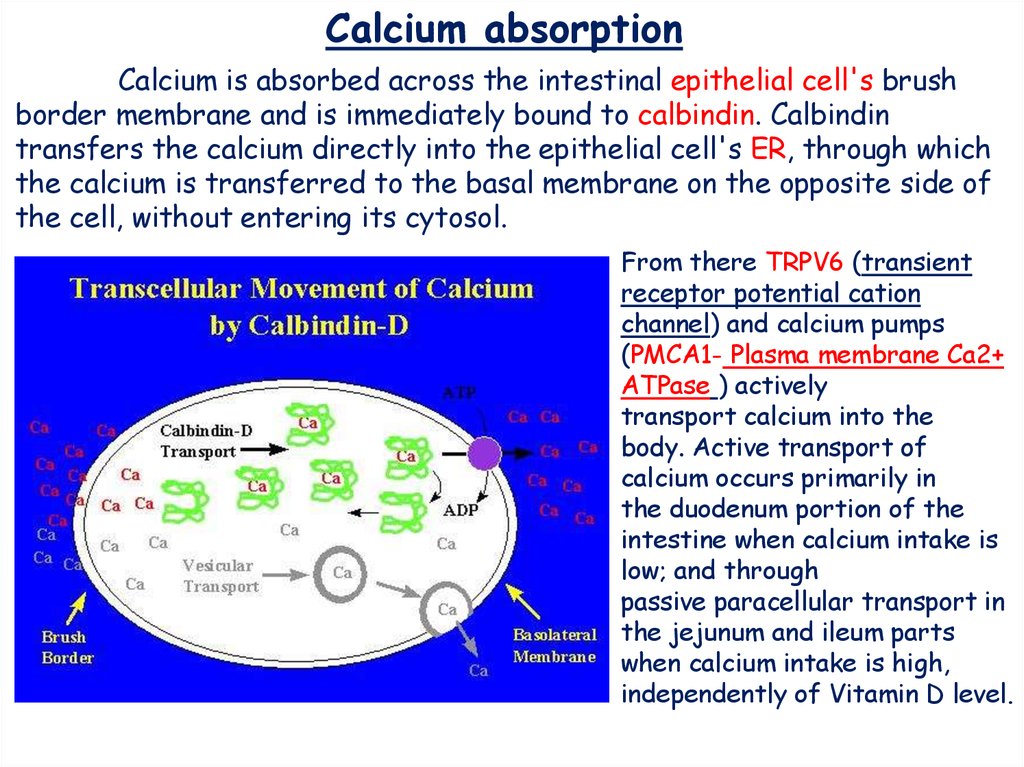
Calcium absorptionCalcium is absorbed across the intestinal epithelial cell's brush
border membrane and is immediately bound to calbindin. Calbindin
transfers the calcium directly into the epithelial cell's ER, through which
the calcium is transferred to the basal membrane on the opposite side of
the cell, without entering its cytosol.
From there TRPV6 (transient
receptor potential cation
channel) and calcium pumps
(PMCA1- Plasma membrane Ca2+
ATPase ) actively
transport calcium into the
body. Active transport of
calcium occurs primarily in
the duodenum portion of the
intestine when calcium intake is
low; and through
passive paracellular transport in
the jejunum and ileum parts
when calcium intake is high,
independently of Vitamin D level.
7.
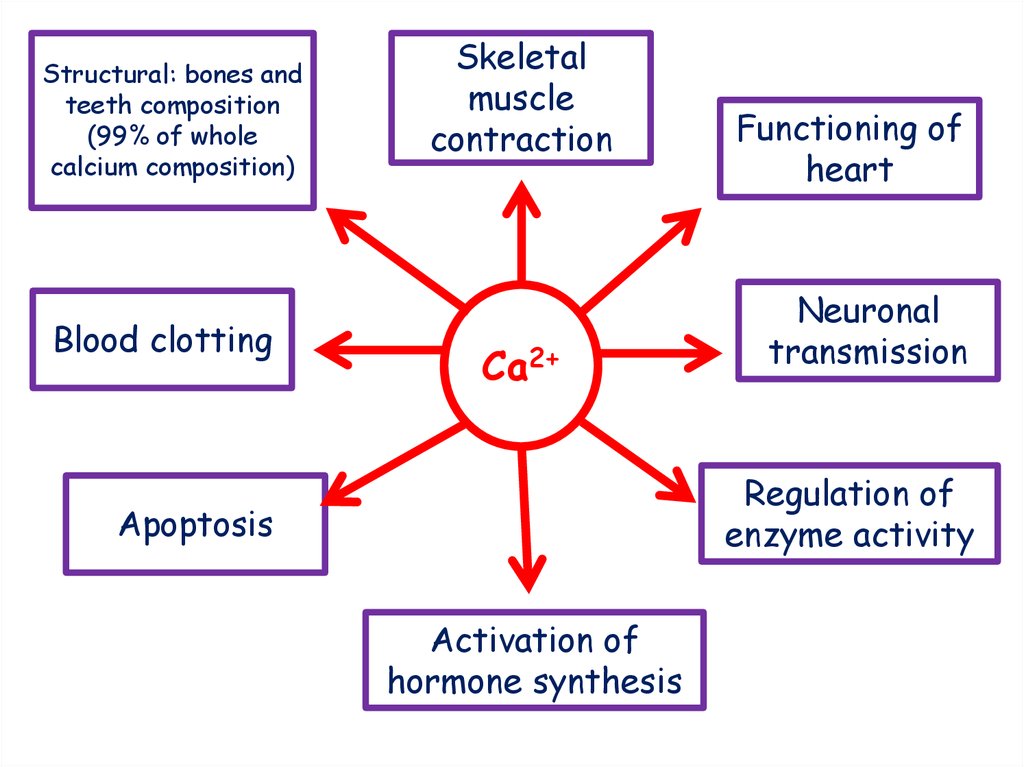
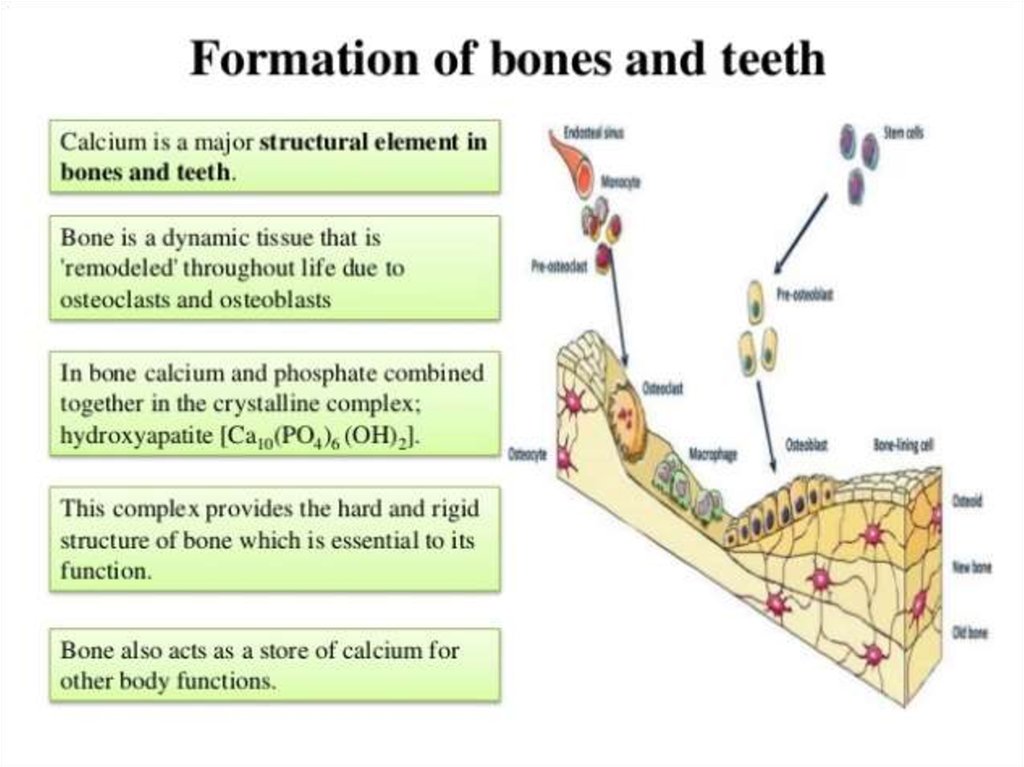
Structural: bones andteeth composition
(99% of whole
calcium composition)
Blood clotting
Skeletal
muscle
contraction
Ca2+
Functioning of
heart
Neuronal
transmission
Regulation of
enzyme activity
Apoptosis
Activation of
hormone synthesis
8.
9.
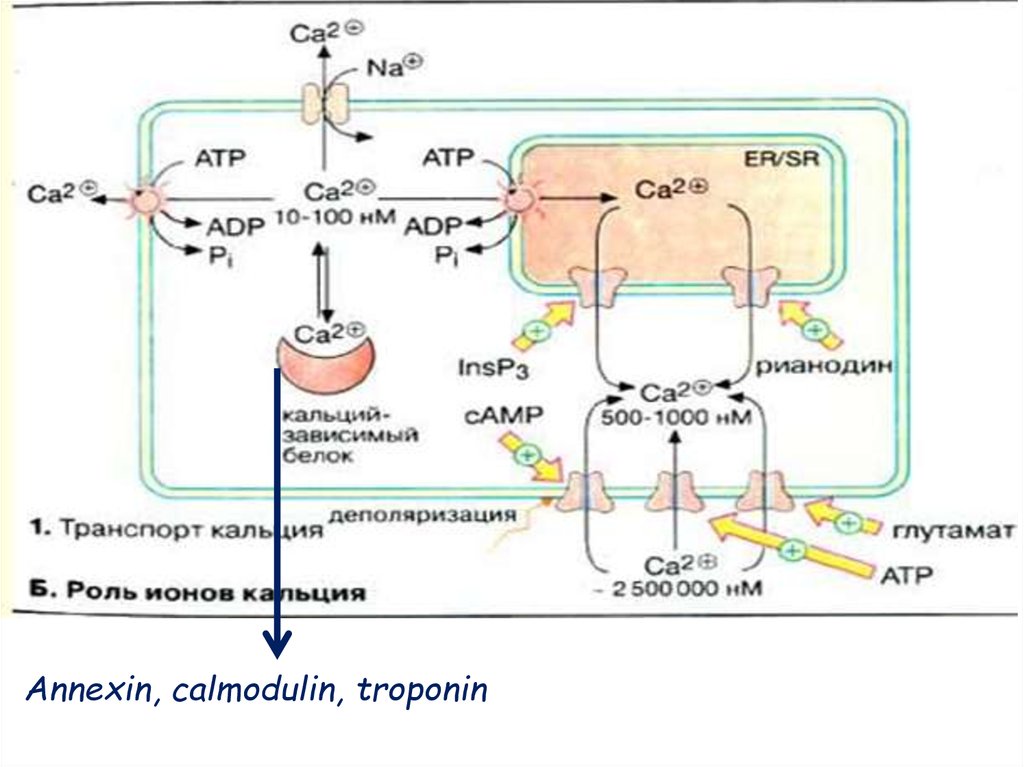
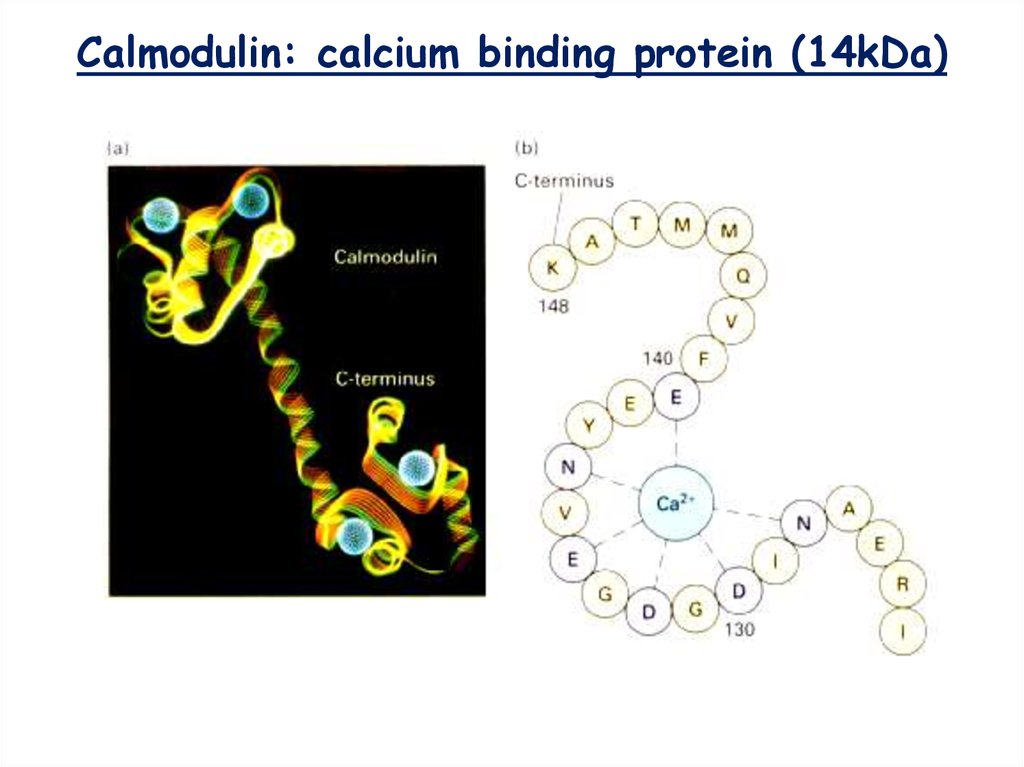
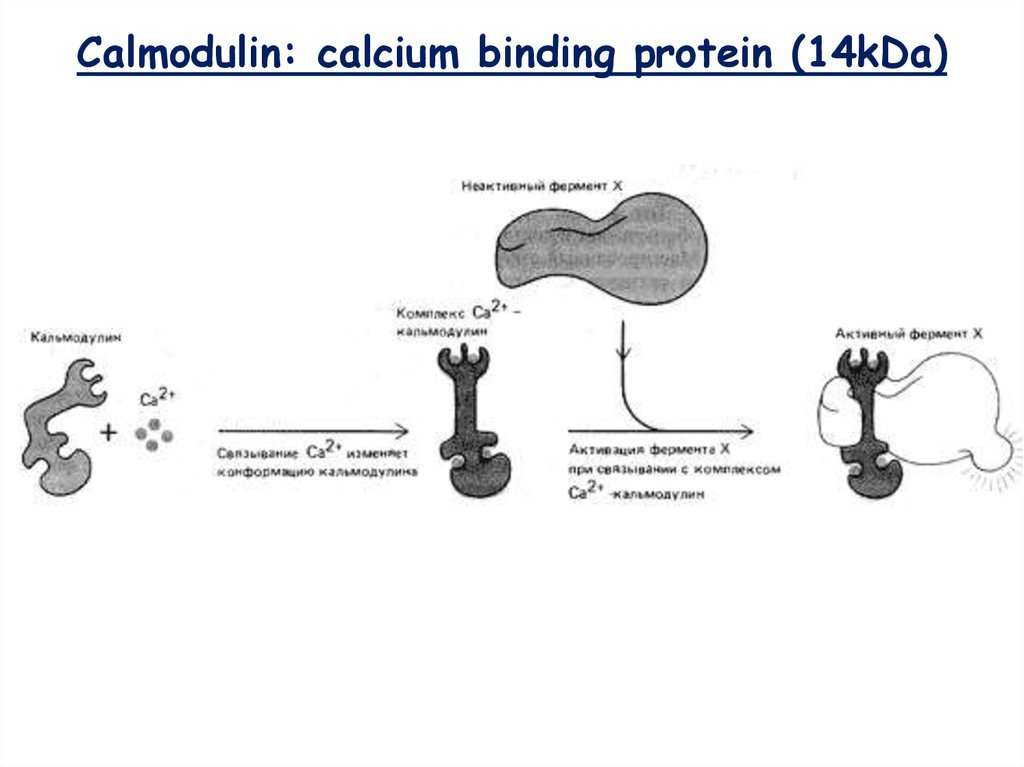
Annexin, calmodulin, troponin10.
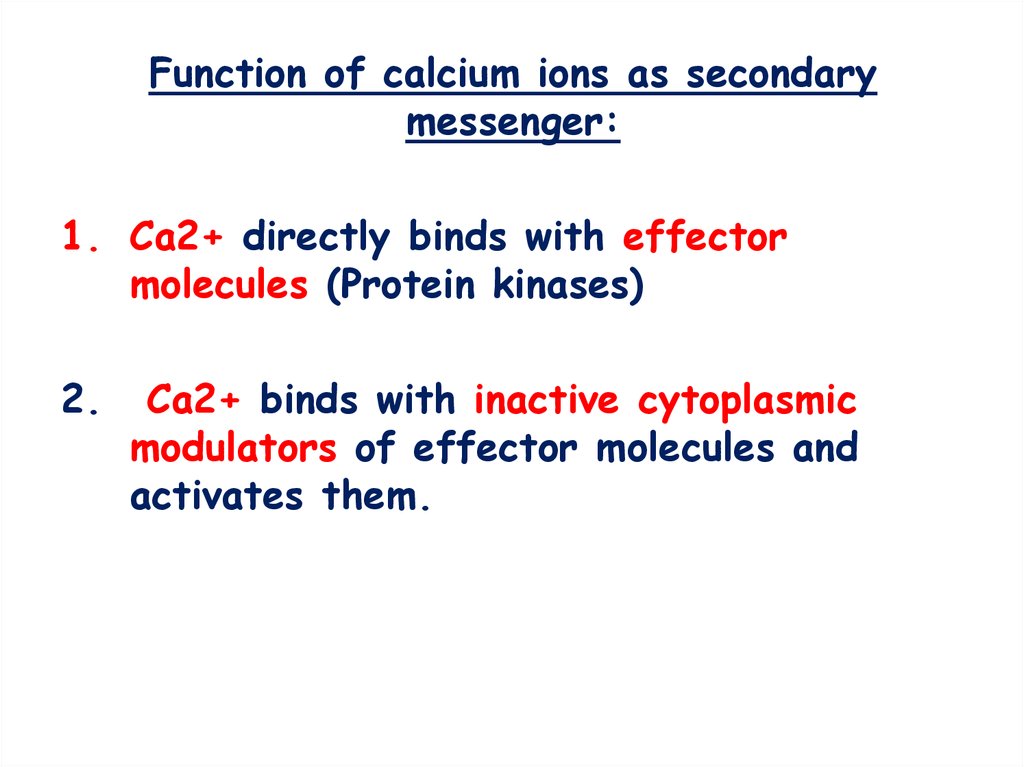
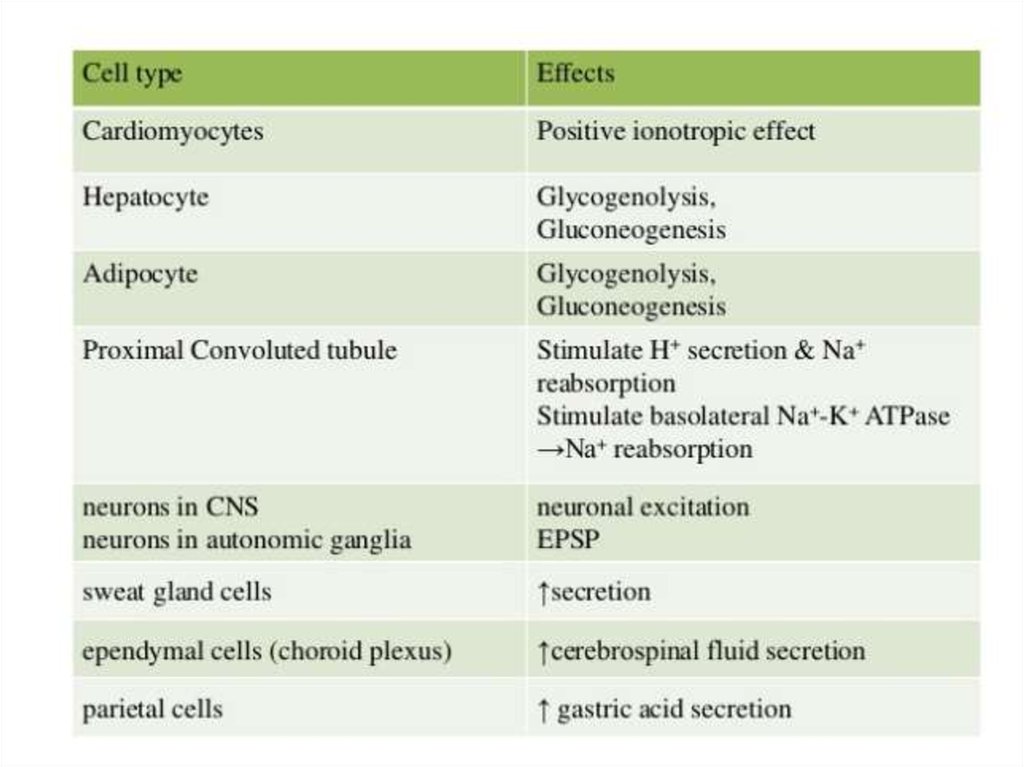
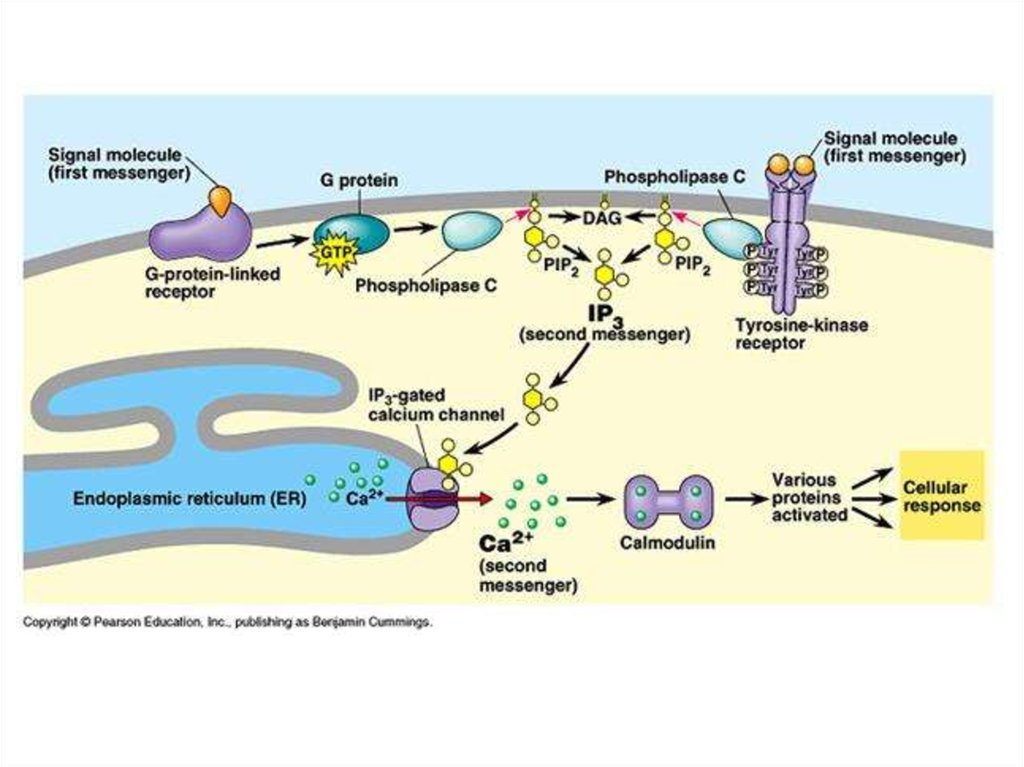
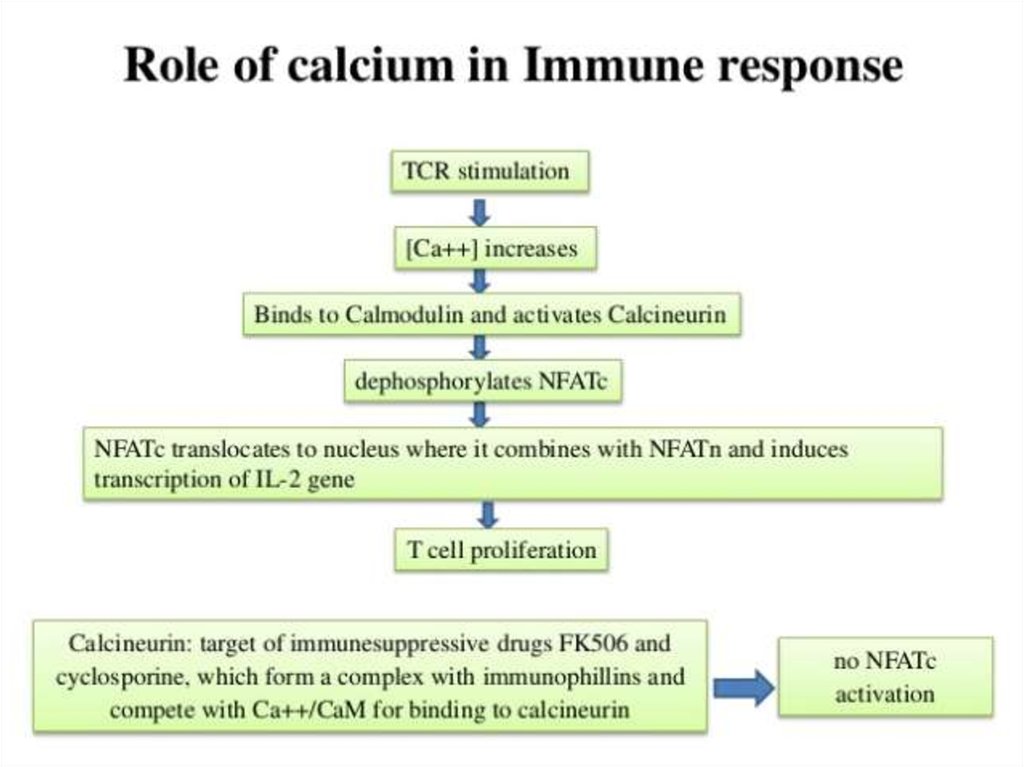
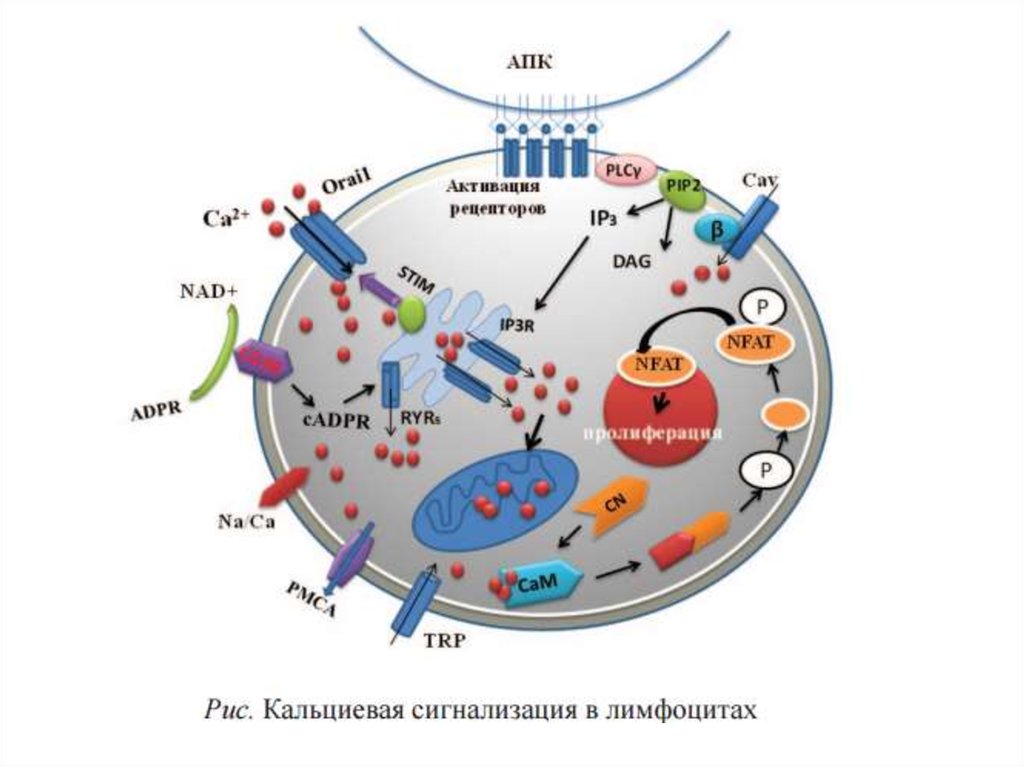
Function of calcium ions as secondarymessenger:
1. Са2+ directly binds with effector
molecules (Protein kinases)
2.
Са2+ binds with inactive cytoplasmic
modulators of effector molecules and
activates them.
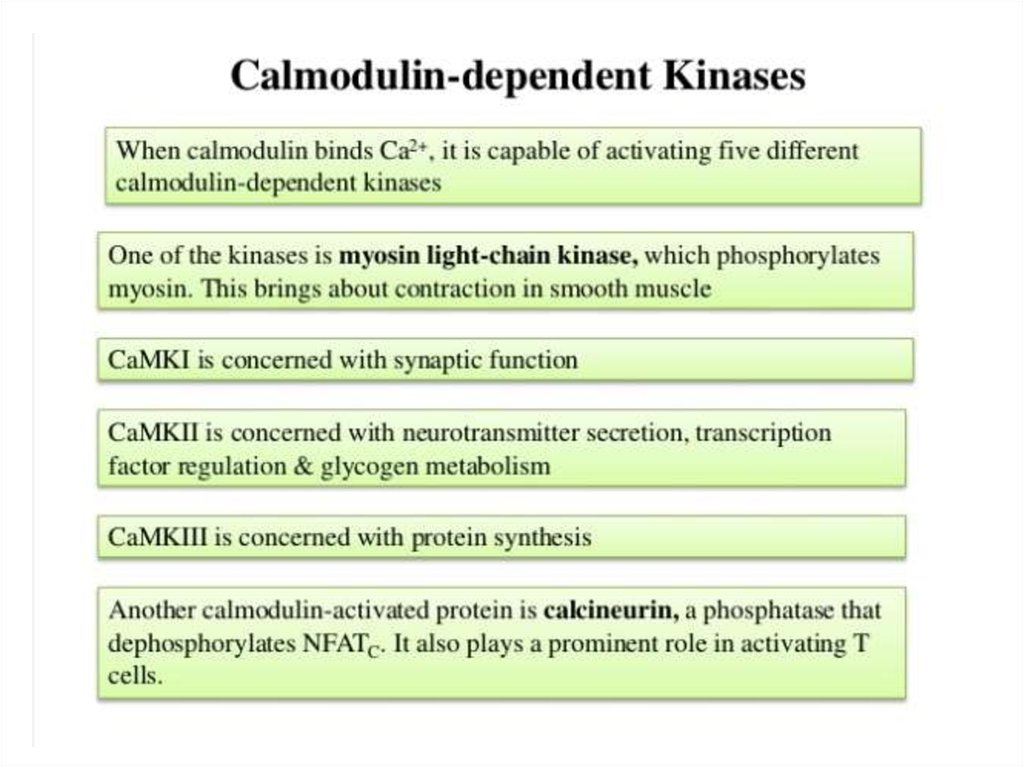
11.
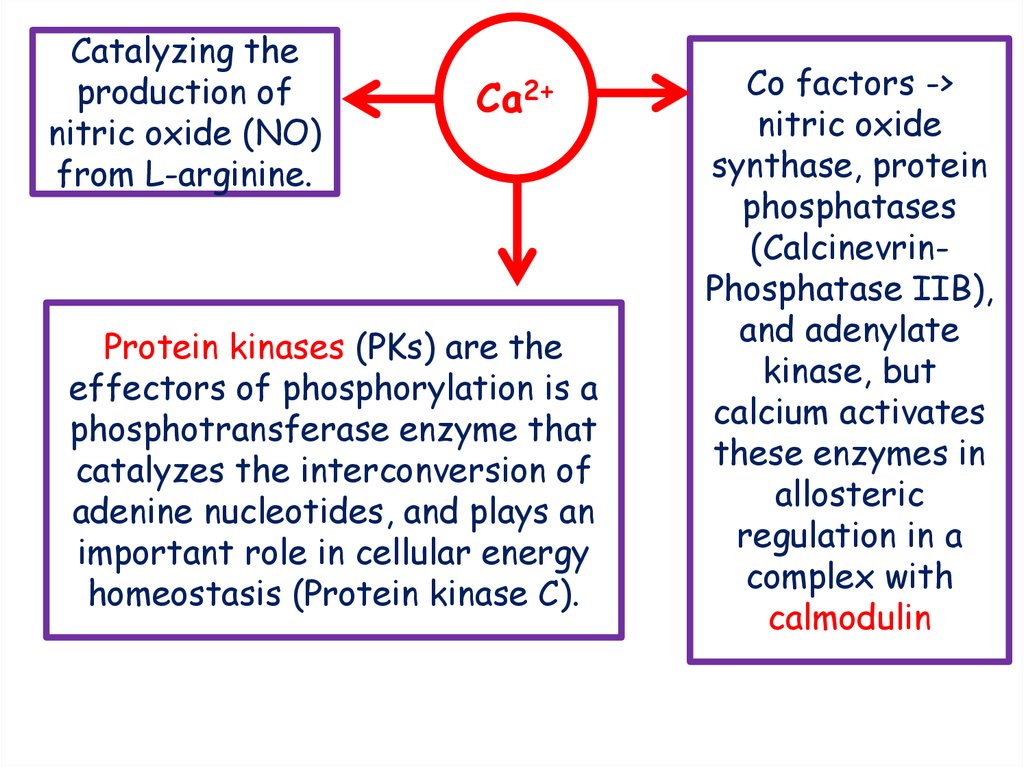
Catalyzing theproduction of
nitric oxide (NO)
from L-arginine.
Ca2+
Protein kinases (PKs) are the
effectors of phosphorylation is a
phosphotransferase enzyme that
catalyzes the interconversion of
adenine nucleotides, and plays an
important role in cellular energy
homeostasis (Protein kinase C).
Co factors ->
nitric oxide
synthase, protein
phosphatases
(CalcinevrinPhosphatase IIB),
and adenylate
kinase, but
calcium activates
these enzymes in
allosteric
regulation in a
complex with
calmodulin
12.
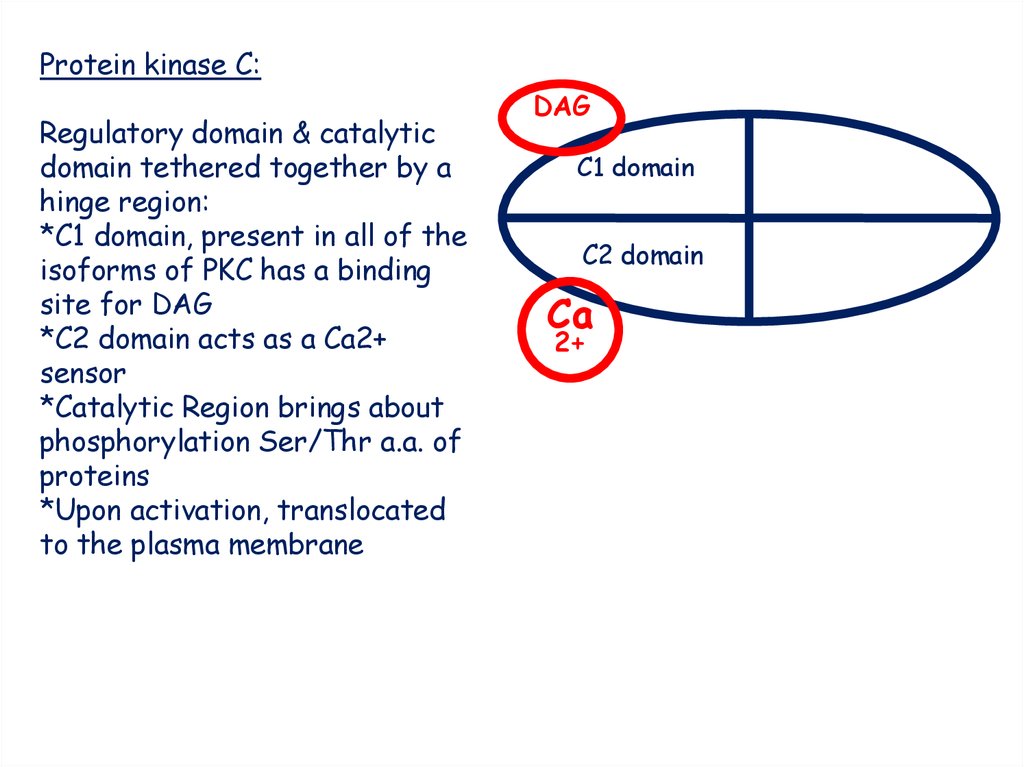
Protein kinase C:Regulatory domain & catalytic
domain tethered together by a
hinge region:
*C1 domain, present in all of the
isoforms of PKC has a binding
site for DAG
*C2 domain acts as a Ca2+
sensor
*Catalytic Region brings about
phosphorylation Ser/Thr a.a. of
proteins
*Upon activation, translocated
to the plasma membrane
DAG
C1 domain
C2 domain
Ca
2+
13.
14.
15.
16. Calmodulin: calcium binding protein (14kDa)
17. Calmodulin: calcium binding protein (14kDa)
18.
19.
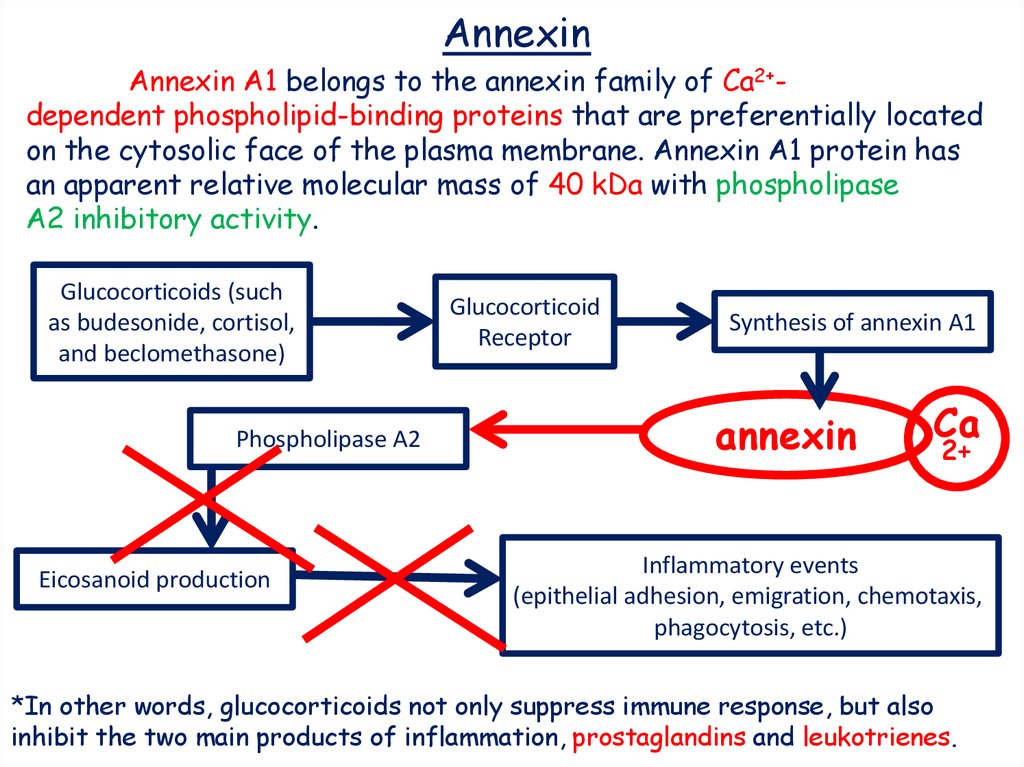
AnnexinAnnexin A1 belongs to the annexin family of Ca2+dependent phospholipid-binding proteins that are preferentially located
on the cytosolic face of the plasma membrane. Annexin A1 protein has
an apparent relative molecular mass of 40 kDa with phospholipase
A2 inhibitory activity.
Glucocorticoids (such
as budesonide, cortisol,
and beclomethasone)
Phospholipase A2
Eicosanoid production
Glucocorticoid
Receptor
Synthesis of annexin A1
annexin
Ca
2+
Inflammatory events
(epithelial adhesion, emigration, chemotaxis,
phagocytosis, etc.)
*In other words, glucocorticoids not only suppress immune response, but also
inhibit the two main products of inflammation, prostaglandins and leukotrienes.
20.
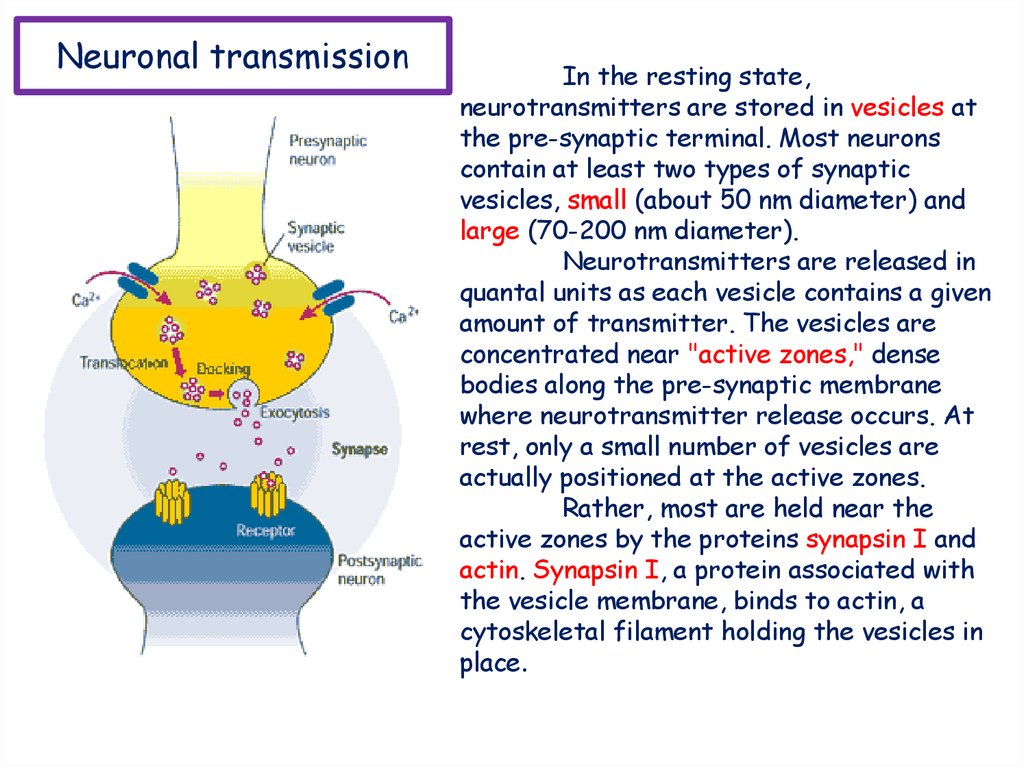
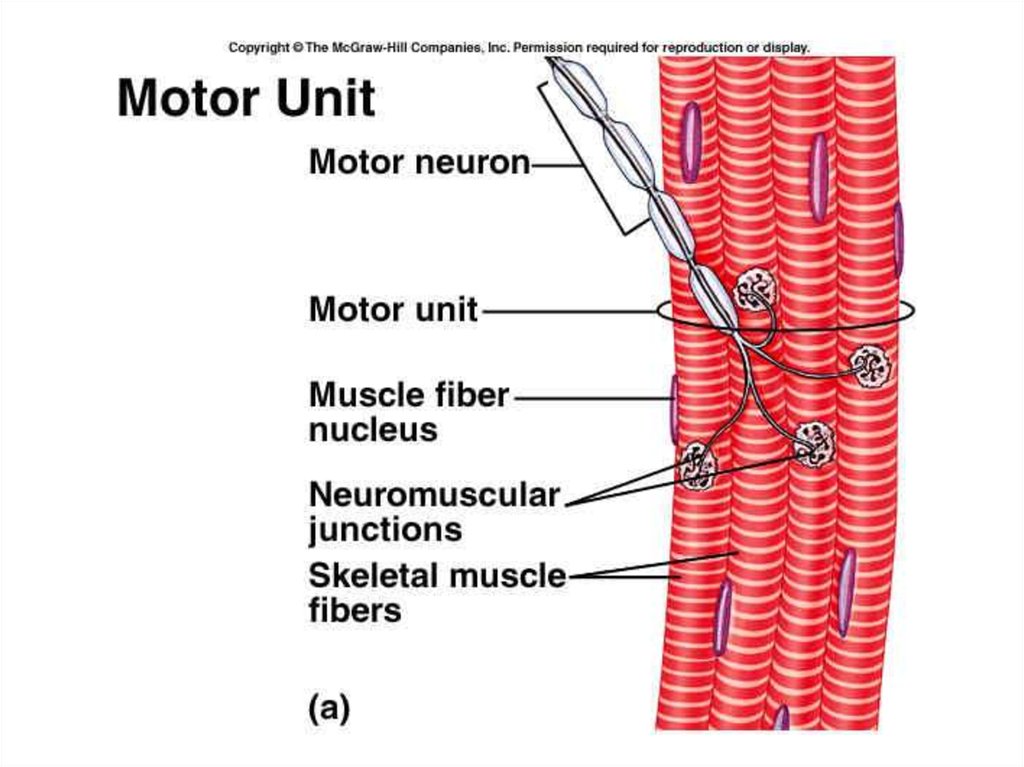
Neuronal transmissionIn the resting state,
neurotransmitters are stored in vesicles at
the pre-synaptic terminal. Most neurons
contain at least two types of synaptic
vesicles, small (about 50 nm diameter) and
large (70-200 nm diameter).
Neurotransmitters are released in
quantal units as each vesicle contains a given
amount of transmitter. The vesicles are
concentrated near "active zones," dense
bodies along the pre-synaptic membrane
where neurotransmitter release occurs. At
rest, only a small number of vesicles are
actually positioned at the active zones.
Rather, most are held near the
active zones by the proteins synapsin I and
actin. Synapsin I, a protein associated with
the vesicle membrane, binds to actin, a
cytoskeletal filament holding the vesicles in
place.
21.
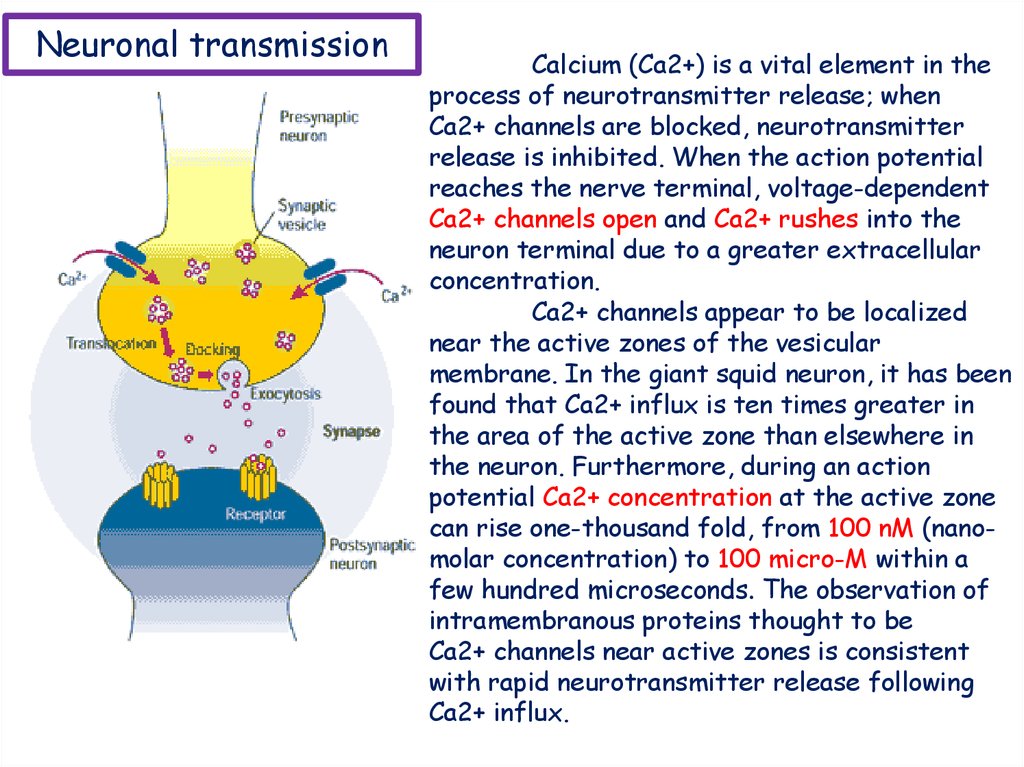
Neuronal transmissionCalcium (Ca2+) is a vital element in the
process of neurotransmitter release; when
Ca2+ channels are blocked, neurotransmitter
release is inhibited. When the action potential
reaches the nerve terminal, voltage-dependent
Ca2+ channels open and Ca2+ rushes into the
neuron terminal due to a greater extracellular
concentration.
Ca2+ channels appear to be localized
near the active zones of the vesicular
membrane. In the giant squid neuron, it has been
found that Ca2+ influx is ten times greater in
the area of the active zone than elsewhere in
the neuron. Furthermore, during an action
potential Ca2+ concentration at the active zone
can rise one-thousand fold, from 100 nM (nanomolar concentration) to 100 micro-M within a
few hundred microseconds. The observation of
intramembranous proteins thought to be
Ca2+ channels near active zones is consistent
with rapid neurotransmitter release following
Ca2+ influx.
22.
23.
24.
25.
26.
27.
28.
29.
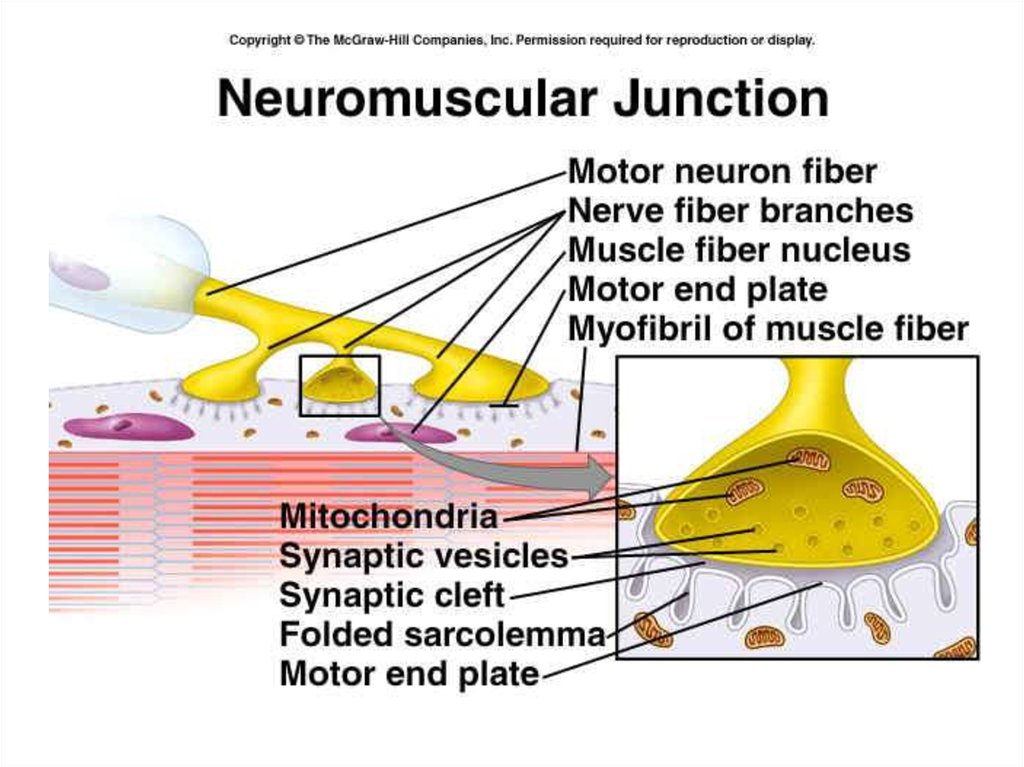
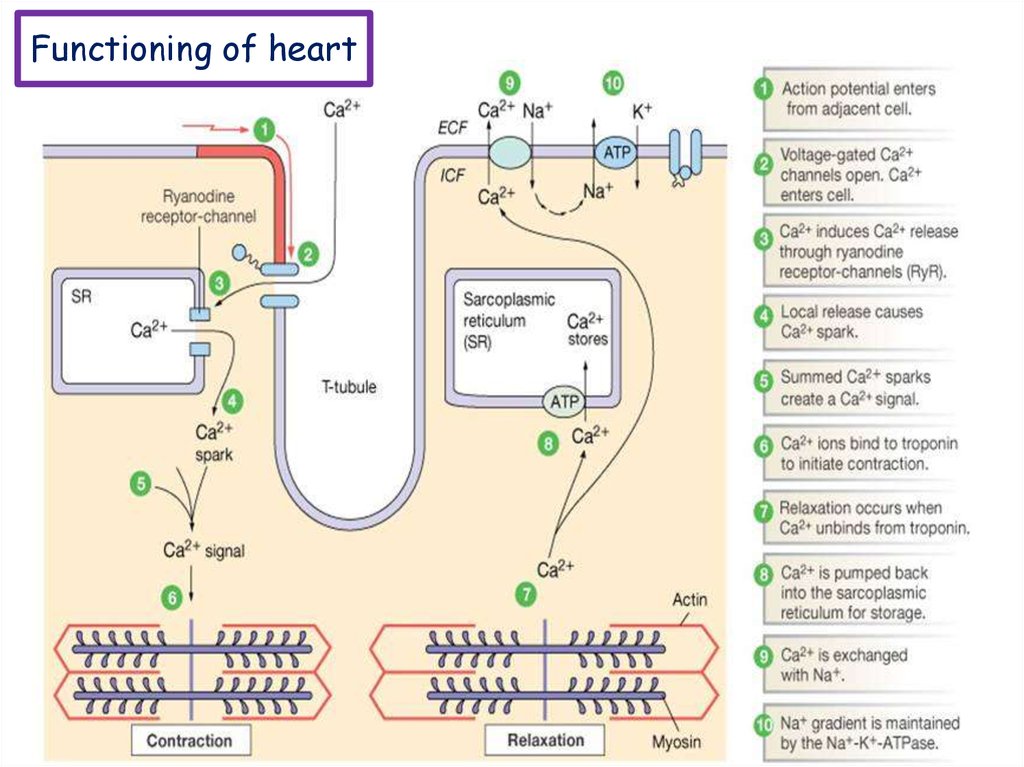
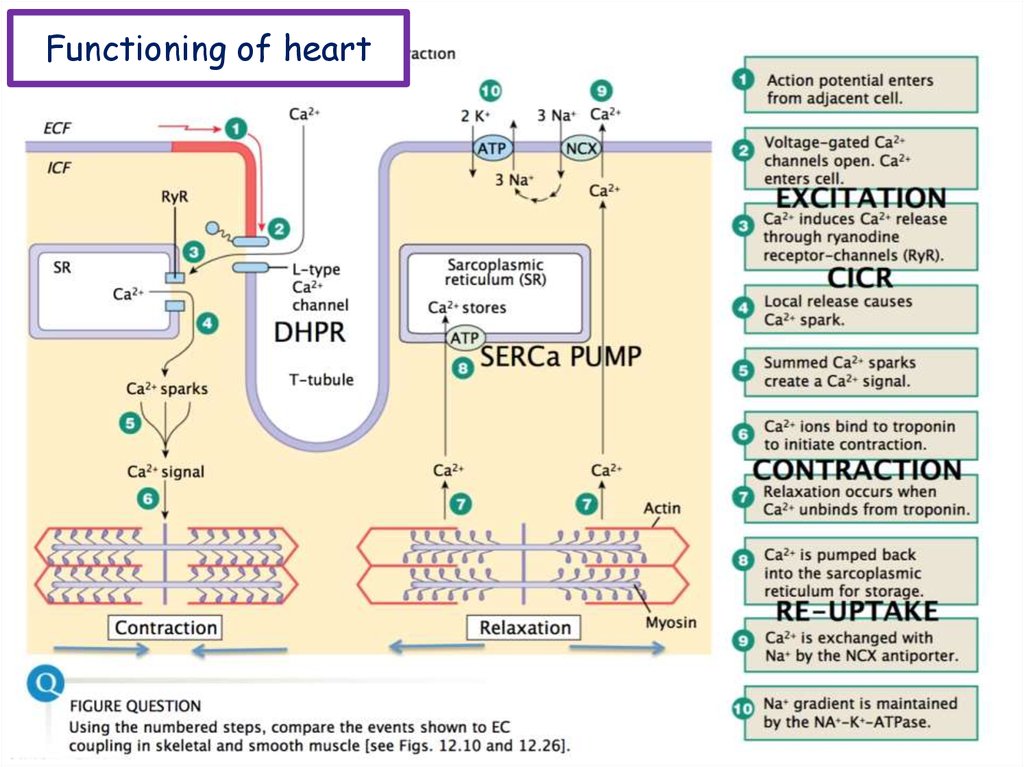
Functioning of heartThe importance of calcium-dependent signaling in the heart
has been appreciated for decades. For example, it is well accepted
that intracellular calcium release from the sarcoplasmic reticulum
(SR) is required for cardiac muscle contraction. Indeed, with each
heart beat the calcium concentration in the cytosol of cardiac
myocytes is elevated approximately 10-fold from a resting level of
∼100 nM to ∼1 μM.
Presumably, a defect in signaling that prevents effective
elevation of cytosolic calcium would impair contractility as the
contraction of heart muscle is directly determined by the level of
calcium elevation during systole. Similarly, a defect in the removal
of calcium from the cytosol during diastole would impair cardiac
relaxation, which is critically important in that it allows the heart
chambers to refill with blood in preparation for the next beat.
30.
Functioning ofheart
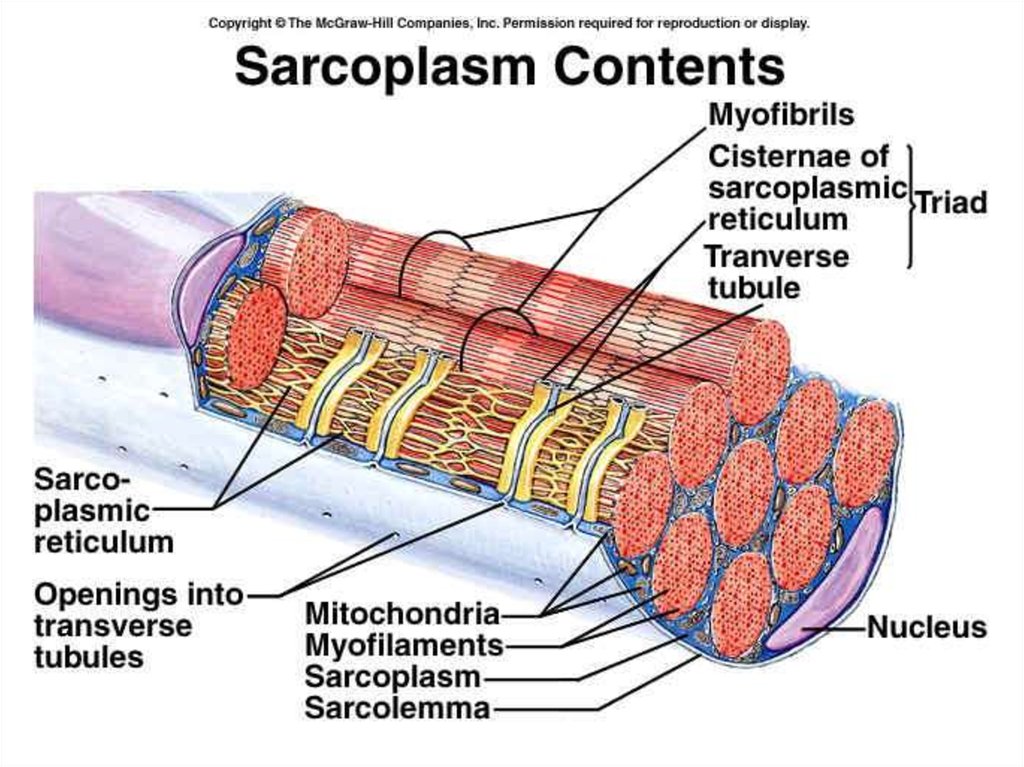
Cardiac muscle fibers contract via excitationcontraction coupling, using a mechanism unique to
cardiac muscle called calcium-induced calcium release.
CICR is A process whereby calcium can trigger
release of further calcium from the muscle sarcoplasmic
reticulum.
31.
Functioning ofheart
During stimulation of the muscle cell, the motor
neuron releases the neurotransmitter acetylcholine,
which then binds to a post-synaptic nicotinic
acetylcholine receptor. The inward flow of calcium from
the L-type calcium channels activates ryanodine
receptors to release calcium ions from the sarcoplasmic
reticulum.
32.
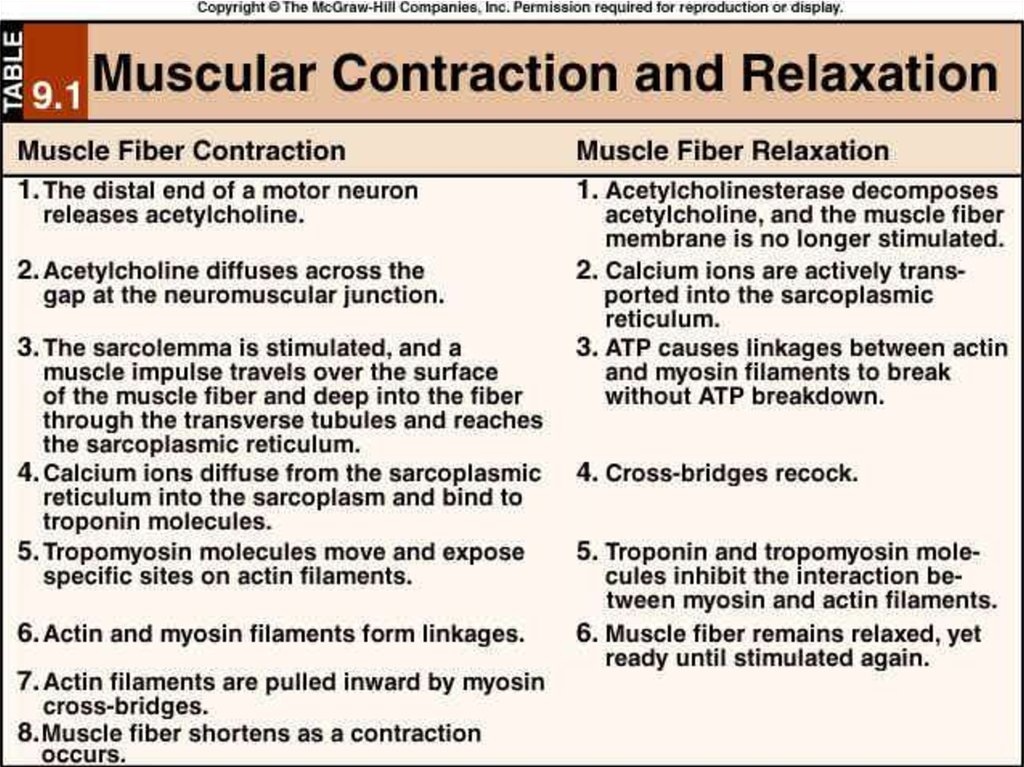
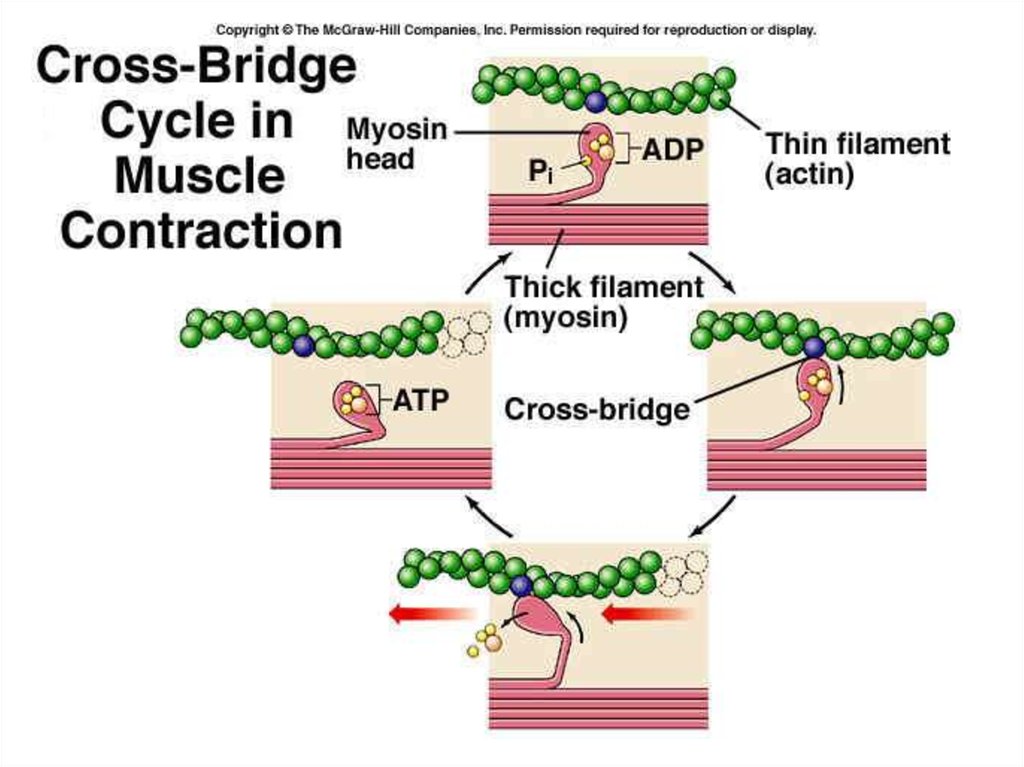
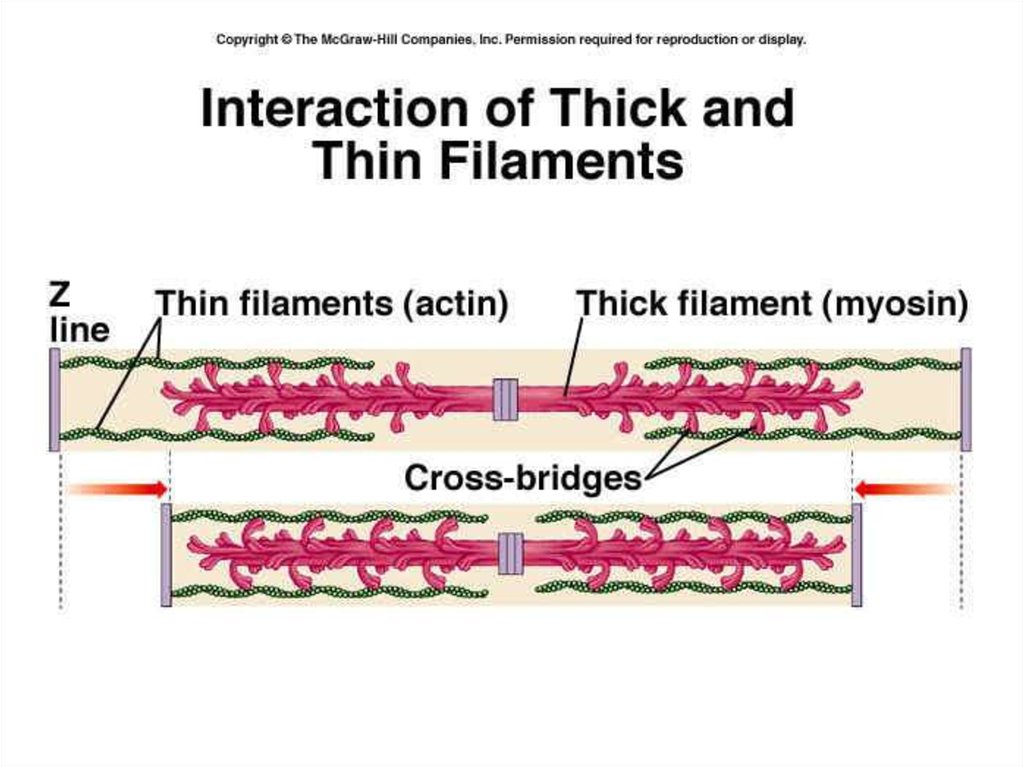
Functioning of heartExcitation-contraction coupling describes the
process of converting an electrical stimulus (action
potential) into a mechanical response (muscle contraction).
Calcium-induced calcium release involves the
conduction of calcium ions into the cardiomyocyte,
triggering further release of ions into the cytoplasm.
Calcium prolongs the duration of muscle cell depolarization
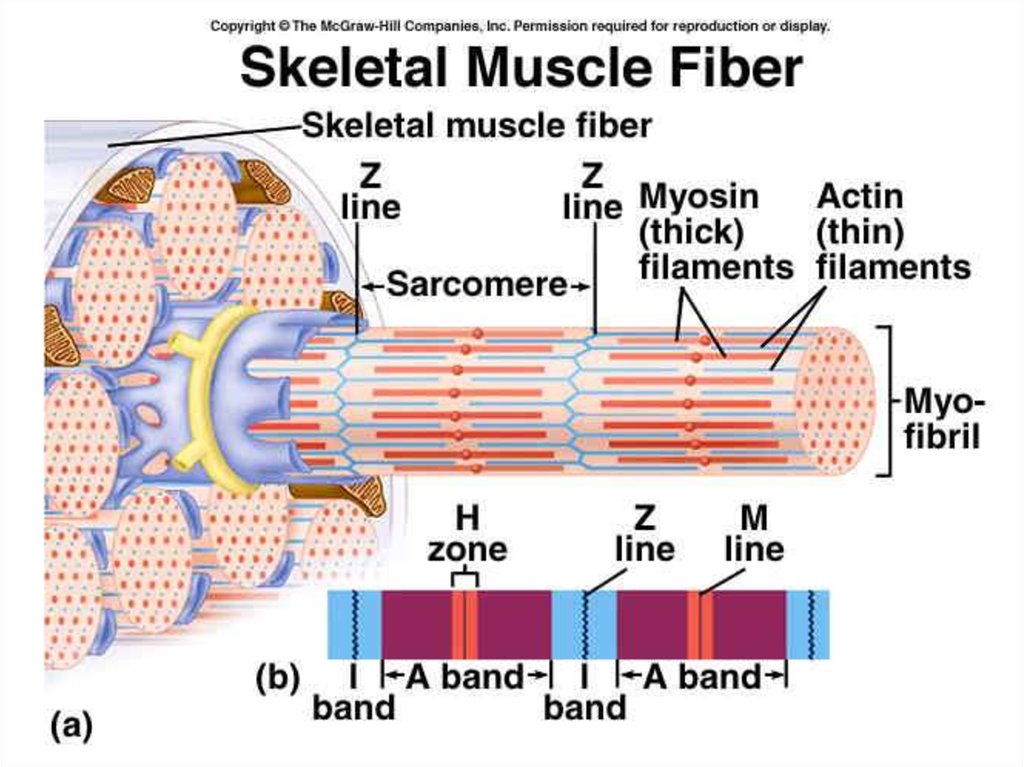
before repolarization occurs. Contraction in cardiac
muscle occurs due to the binding of the myosin head to
adenosine triphosphate (ATP), which then pulls the actin
filaments to the center of the sarcomere, the mechanical
force of contraction. In the sliding filament model, myosin
filaments slide along actin filaments to shorten or
lengthen the muscle fiber for contraction and relaxation
33.
Functioning of heartThe pathway of contraction can be described in five steps:
An action potential, induced by the pacemaker cells in the
sinoatrial (SA) and atrioventricular (AV) nodes, is conducted to
contractile cardiomyocytes through gap junctions. As the action
potential travels between sarcomeres, it activates the calcium channels
in the T-tubules, resulting in an influx of calcium ions into the
cardiomyocyte. Calcium in the cytoplasm then binds to cardiac troponinC, which moves the troponin complex away from the actin binding site.
This removal of the troponin complex frees the actin to be bound by
myosin and initiates contraction. The myosin head binds to ATP and pulls
the actin filaments toward the center of the sarcomere, contracting the
muscle.
Intracellular calcium is then removed by the sarcoplasmic
reticulum, dropping intracellular calcium concentration, returning the
troponin complex to its inhibiting position on the active site of actin, and
effectively ending contraction as the actin filaments return to their
initial position, relaxing the muscle
34.
Functioning of heart35.
Functioning of heart36.
37.
38.
39.
40.
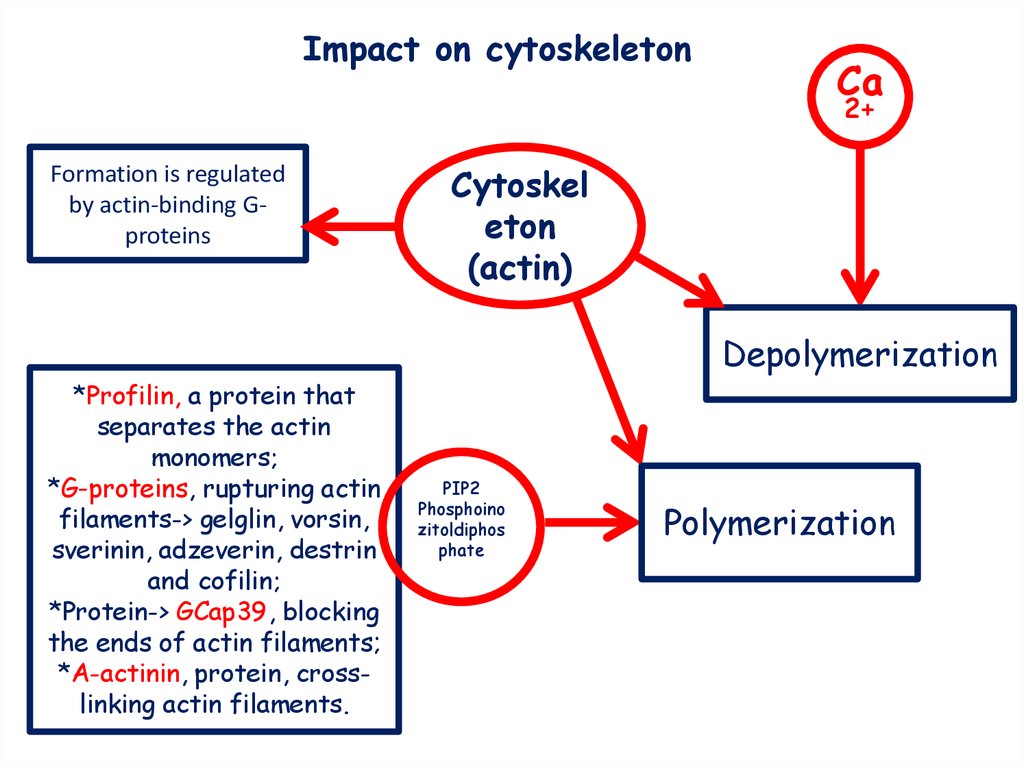
Impact on cytoskeletonCa
2+
Formation is regulated
by actin-binding Gproteins
Cytoskel
eton
(actin)
Depolymerization
*Profilin, a protein that
separates the actin
monomers;
*G-proteins, rupturing actin
filaments-> gelglin, vorsin,
sverinin, adzeverin, destrin
and cofilin;
*Protein-> GCap39, blocking
the ends of actin filaments;
*A-actinin, protein, crosslinking actin filaments.
PIP2
Phosphoino
zitoldiphos
phate
Polymerization
41.
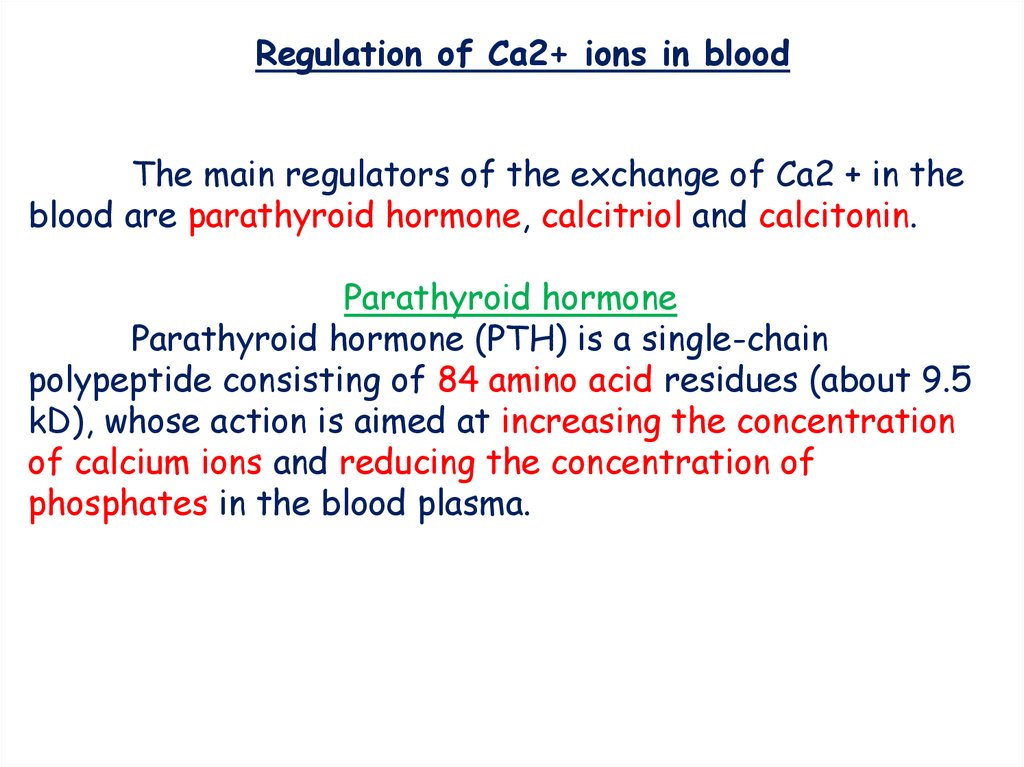
Regulation of Ca2+ ions in bloodThe main regulators of the exchange of Ca2 + in the
blood are parathyroid hormone, calcitriol and calcitonin.
Parathyroid hormone
Parathyroid hormone (PTH) is a single-chain
polypeptide consisting of 84 amino acid residues (about 9.5
kD), whose action is aimed at increasing the concentration
of calcium ions and reducing the concentration of
phosphates in the blood plasma.
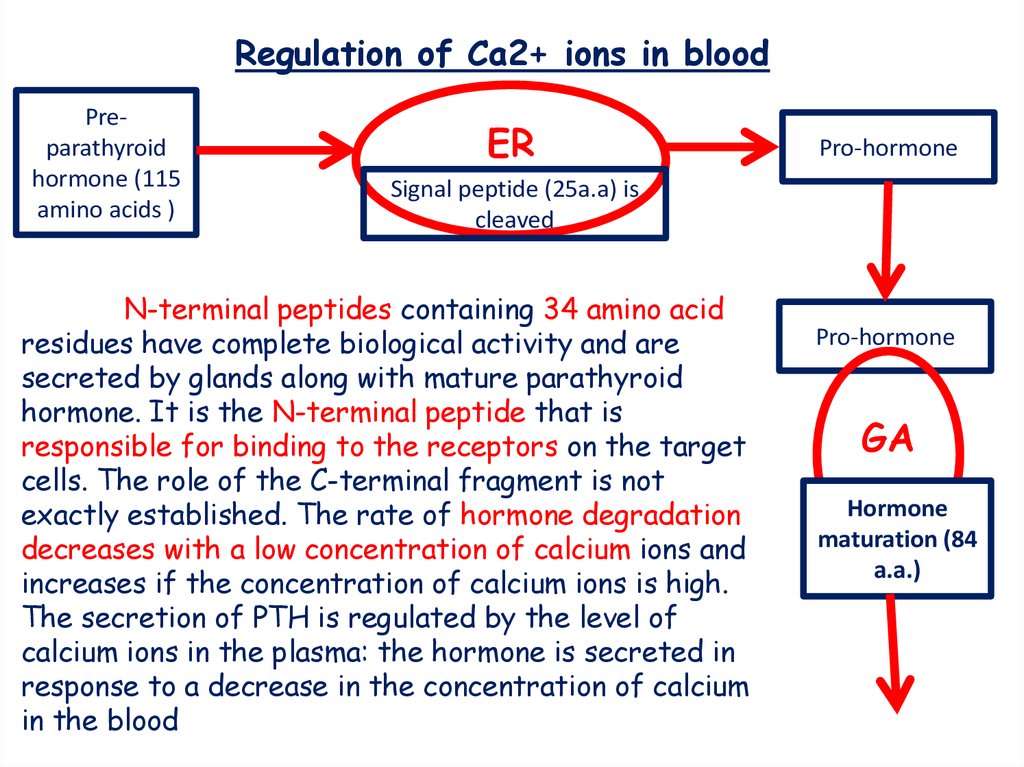
42.
Regulation of Ca2+ ions in bloodPreparathyroid
hormone (115
amino acids )
ER
Pro-hormone
Signal peptide (25a.a) is
cleaved
N-terminal peptides containing 34 amino acid
residues have complete biological activity and are
secreted by glands along with mature parathyroid
hormone. It is the N-terminal peptide that is
responsible for binding to the receptors on the target
cells. The role of the C-terminal fragment is not
exactly established. The rate of hormone degradation
decreases with a low concentration of calcium ions and
increases if the concentration of calcium ions is high.
The secretion of PTH is regulated by the level of
calcium ions in the plasma: the hormone is secreted in
response to a decrease in the concentration of calcium
in the blood
Pro-hormone
GA
Hormone
maturation (84
a.a.)
43.
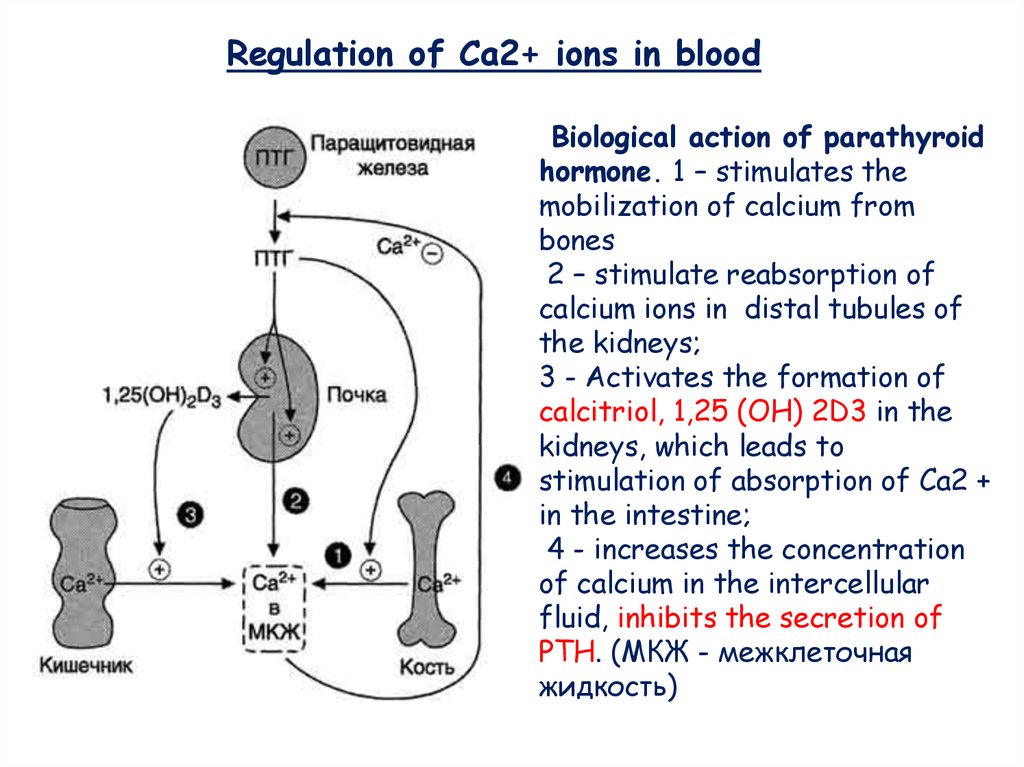
Regulation of Ca2+ ions in bloodBiological action of parathyroid
hormone. 1 – stimulates the
mobilization of calcium from
bones
2 – stimulate reabsorption of
calcium ions in distal tubules of
the kidneys;
3 - Activates the formation of
calcitriol, 1,25 (OH) 2D3 in the
kidneys, which leads to
stimulation of absorption of Ca2 +
in the intestine;
4 - increases the concentration
of calcium in the intercellular
fluid, inhibits the secretion of
PTH. (МКЖ - межклеточная
жидкость)
44.
Regulation of Ca2+ ions in bloodCalcitonin is a polypeptide consisting of 32 amino acid residues
with one disulfide bond. The hormone is secreted by parafollicular Kcells of the thyroid gland or C-cells of parathyroid glands in the form
of a high-molecular precursor protein. Secretion of calcitonin
increases with increasing concentration of Ca2 + and decreases with
decreasing Ca2 + concentration in the blood.
Calcitonin is a parathyroid hormone antagonist.
It inhibits: 1) the release of Ca2 + from the bone, reducing the
activity of osteoclasts.
2) inhibits tubular reabsorption calcium ions, stimulating their
excretion by kidneys with urea.
*The rate of secretion of calcitonin in women strongly depends
on the level of estrogens. With a lack of estrogens, the secretion of
calcitonin decreases. This causes an acceleration of the mobilization
of calcium from bone tissue, which leads to the development of
osteoporosis.
45.
Thanksfor
attention!!!

 Медицина
Медицина