Похожие презентации:
Mixed medicine case
1. Mixed medicine case 2018
DR. RACHNA SINGH(MBBS, M.MED, M.BIOTECH, GRAD.DIP, MPH , AMC (CERTIFICATE)
2. Case 1
Your next patient in general practice is a 45 year old Mr. Snider who isconcerned because his 48 year old brother recently had a cardiac bypass
operation and he seeks your advice what sort of risk he has for a heart attack.
Your task is to:
Take a focused history
Ask physical examination findings to examiner
Advise the patient regarding investigations and management
3. history
I’m sorry that your brother passed away recently. I know that it is hard.Assess risk factors:
ROS:Chest pain, palpitation, sob, leg edema, calf pain
Appetite and weight changes:
Waterworks and bowel motion
Obstructive sleep apnea
4. History
Diet: what kind of food you eatWhat is your level of exercise?
SAD and quantify how much and how long
Any Past medical condition like diabetes, hypertension, stroke, peripheral
vascular disease or intermittent claudication, checked blood lipids before
How is you job like? – is it a stressful one
Family history of hypocholesteremia
Family history - + brother died of hear attack
5. Physical examination
General Appearance - Acromegaly- bossing of forehead, CyanosisVitals – Normal
BMI – normal
FUNDOSCOPY(haemorrhage, cotton wool, neovascularisation, silver wiring, AV
nipping, exudates)
Heart - Inspect- scars, deformity, visible apex beat, abnormal pulsation, pacemaker
Palpation- Apex beat(normal or displaced), parasternal Impulses(palm), palpable
thrills(finger tips)
Auscultation- S1S2, murmurs(mitral, aortic, pulmonary, tricuspid)
If systolic murmur present- Carotid bruit Bilateral
SPECIAL POSITIONS
Left lateral position(MS)- auscultate at apex and axillary area(MR)
Dynamic Auscultation- AS
6. Investigations
FBE, U&E,BSL lipid profile,
serum uric acid,
TFTs,
ECG Stress test
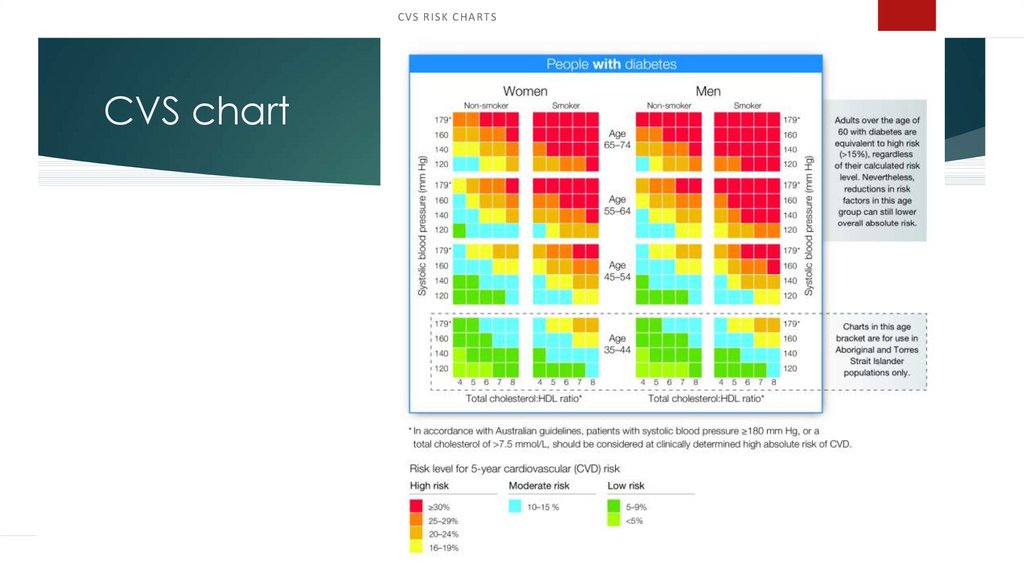
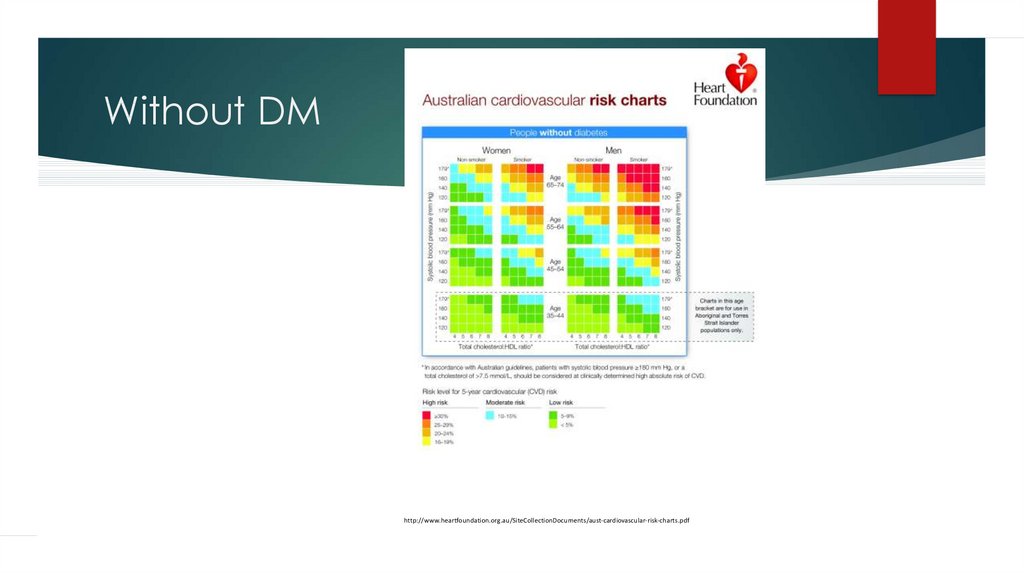
7. CVS chart
CVS RISK CH ARTSCVS chart
8. Without DM
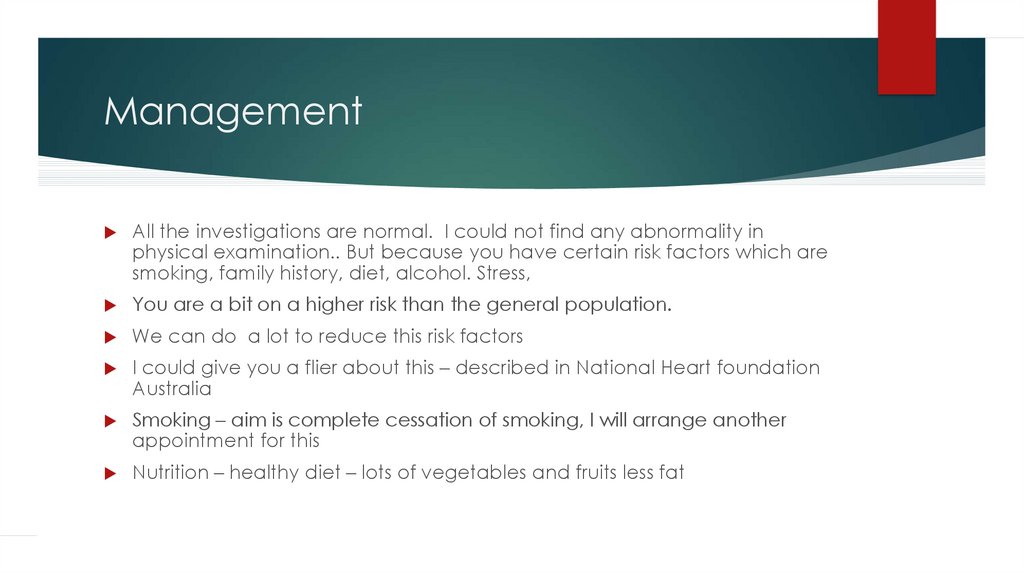
http://www.heartfoundation.org.au/SiteCollectionDocuments/aust-cardiovascular-risk-charts.pdf9. Management
All the investigations are normal. I could not find any abnormality inphysical examination.. But because you have certain risk factors which are
smoking, family history, diet, alcohol. Stress,
You are a bit on a higher risk than the general population.
We can do a lot to reduce this risk factors
I could give you a flier about this – described in National Heart foundation
Australia
Smoking – aim is complete cessation of smoking, I will arrange another
appointment for this
Nutrition – healthy diet – lots of vegetables and fruits less fat
10. Management
Alcohol – up to 2 standard drinks for 5 days a weekPhysical activity – find sometime to exercise
30mins for 5 days a week
Brisk walking, jogging, cycling, swimming
Body weight – BMI should be 18.5 -25
Lipids should be in the normal range – accdg to guideline diet alone or
diet with medication
BP <140/90
SNAP Approach
11. Case 2
A 63 year old car sales man, John, presents to the emergency department withcrushing anterior chest pains. The triage nurse took an ECG which was normal and
she assessed the patient as having angina.
She gave him an aspirin and sublingual GTN tablet immediately and about 5
minutes later you see the patient who still complains about most severe anterior
chest pains radiating into his jaws. This started very suddenly about 1 hour ago
and has not improved at all.
Your task is to:
Take a focused history
Ask physical examination findings from examiner
Organise appropriate investigations
Advise the patient on diagnosis and suggested management
12. History
John was woken up from an afternoon nap by sudden onset of severe, tearing pain in hischest, which radiated into his jaw but also seemed to go through to his back and was not
relieved by panadeine or by the tablet the triage nurse gave him.
PHx:
John has suffered from moderate hypertension for about 10 years, poor compliance with
medication. He still smokes about 15 cigarettes a day and is mildly overweight.
No other history
SHx:
Married, 3 children, car sales man, no financial or family worries. No allergies, medication:
beta-blocker.
FHx:
Unremarkable
13. History Of Presenting Complaint- SOCRATES
Site: where exactly do you have the pain?Onset: how did it start- sudden or gradual? Is it getting worse?
Character: what is the nature of the pain- burning, throbbing, dull ache?
Radiation: does the pain go anywhere else?
Associated symptoms
Timing: continuous/ on and off? Any variation with day and night?
Exacerbating/ relieving factors: does anything make it better or worse?
Severity: how severe the symptom is?
14. Previous Episodes
Is this the first episode or have you had similar episodes before?If previous episodes are present then:
When did they start?
How often do they occur?
How long does each episode last?
What sets them off (trigger factors)?
Are they increasing in frequency or duration?
What do you do to relieve them?
Effect on your life (personal, work and social)
15. physical examination
BP 155/100, no BP difference between right and left arm, P 78, RR 18, T 37No abnormal findings on physical examination.
(The finding of a blowing diastolic murmur in the aortic area (upper right
sternal border),
however, is always abnormal and requires urgent evaluation for proximal
aortic pathology in patients with chest pain and hypertension.)
16. Causes risk factors
Bicuspid aortic diseaseMarfan syndrome and Ehlers-Danlos syndrome
Other connective tissue disorders (Marfanoid)
Atherosclerosis
Miscellaneous infectious and inflammatory conditions
Hypertension
Smoking
Trauma
17. Thoracic aortic dissection
Aortic dissection is the tearing of the inner layer of the aortic wall, allowingblood to leak into the wall itself and cause the separation of the inner and
outer layers. It is usually associated with severe chest pain radiating to the
back.
18.
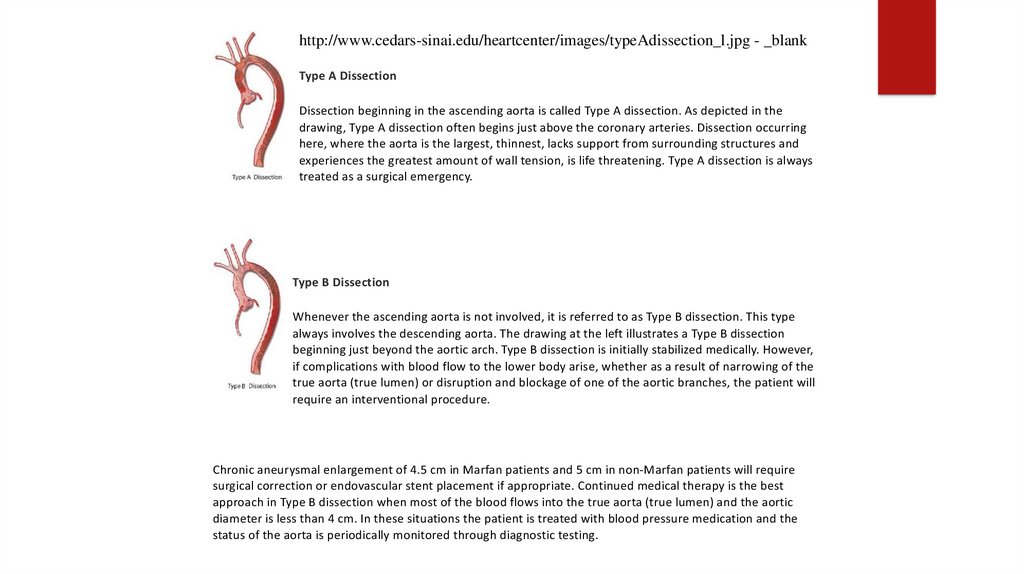
http://www.cedars-sinai.edu/heartcenter/images/typeAdissection_l.jpg - _blankType A Dissection
Dissection beginning in the ascending aorta is called Type A dissection. As depicted in the
drawing, Type A dissection often begins just above the coronary arteries. Dissection occurring
here, where the aorta is the largest, thinnest, lacks support from surrounding structures and
experiences the greatest amount of wall tension, is life threatening. Type A dissection is always
treated as a surgical emergency.
Type B Dissection
Whenever the ascending aorta is not involved, it is referred to as Type B dissection. This type
always involves the descending aorta. The drawing at the left illustrates a Type B dissection
beginning just beyond the aortic arch. Type B dissection is initially stabilized medically. However,
if complications with blood flow to the lower body arise, whether as a result of narrowing of the
true aorta (true lumen) or disruption and blockage of one of the aortic branches, the patient will
require an interventional procedure.
Chronic aneurysmal enlargement of 4.5 cm in Marfan patients and 5 cm in non-Marfan patients will require
surgical correction or endovascular stent placement if appropriate. Continued medical therapy is the best
approach in Type B dissection when most of the blood flows into the true aorta (true lumen) and the aortic
diameter is less than 4 cm. In these situations the patient is treated with blood pressure medication and the
status of the aorta is periodically monitored through diagnostic testing.
Causes and Risk Factors for Both Type A and Type B Thoracic Aortic Dissections:
19. Management
Supportive: AB
C
Oxygen Analgesia Monitoring
Arterial/CVP lines
Medical Management:
BP reduction to 100 mmHG
Nitroprusside or betablockers
Surgical Intervention (Emergency in Type A dissection!)
20. CT scan of Type A
Arterial/CVP lines
Medical Management:
BP reduction to 100 mmHG
Nitroprusside or betablockers
Surgical Intervention (Emergency in Type A dissection!)
CT Scan of Type A Aortic Dissection:
http://images.radiopaedia.org/images/956/eb73e64f7550922c98bd517453b6ab.jpg 19 June 2015
21. Case 3
You have a middle-aged clerical male coming to your GP practice with a 1day history of hematuria and lion pain. He was fine until yesterday when hehad an episode of URTI. On examination, patient’s BP is 160/95, generalized
edema, and urine dipstick blood and protein +++.
Your Tasks are:
History
Management
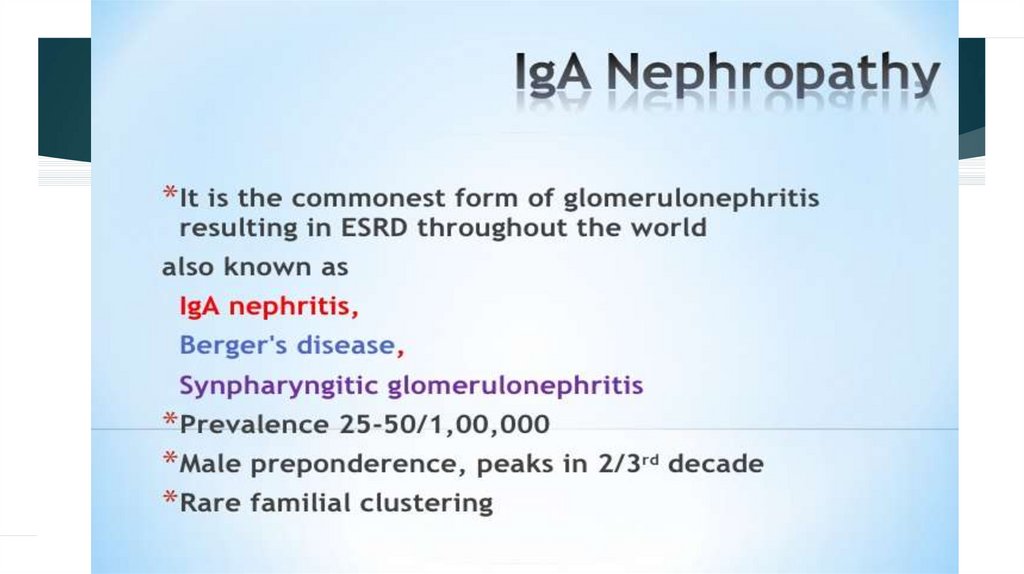
22. Differentials
PSGNIgA Nephropathy
Bladder cancer
Renal cell cancer
PCKD
23. History
How bad is it? When did it start? What is the kind of pain?Is it going anywhere?
Anything that makes it better or worse?
Any fever or chills? Is this the first time? Any fever, chills or rigors? Vomiting?
I understand that you had sore throat yesterday. Did you take any medications for
it?
Your urine is shows protein and blood. How’s your waterworks?
Any burning in urination, frequency, urgency?
Have you had any injury to the loin/pelvis/genital area?
Have you noticed whether the redness is at the start, towards the end of the stream
or throughout (kidney) or after (bladder)?
24. History
Have you noticed bleeding from anywhere else such as bruising or nosebleed?Any problem with the flow of urine?
Have you had any large amounts of beetroot, berries, or red lollies
(pseudohematuria)?
Could your problem have been sexually acquired?
Do you engage in vigorous sports or physical activities?
How’s your general health?
Any kidney problems in the past?
Did you have any problems with swelling and bloody urine during childhood?
FHx of cancers or kidney problems? SADMA?
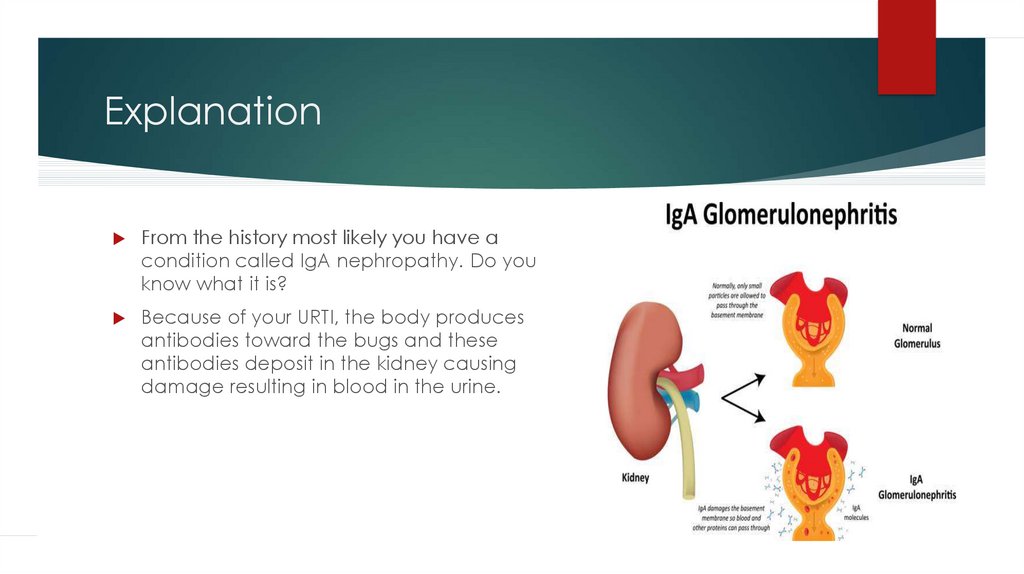
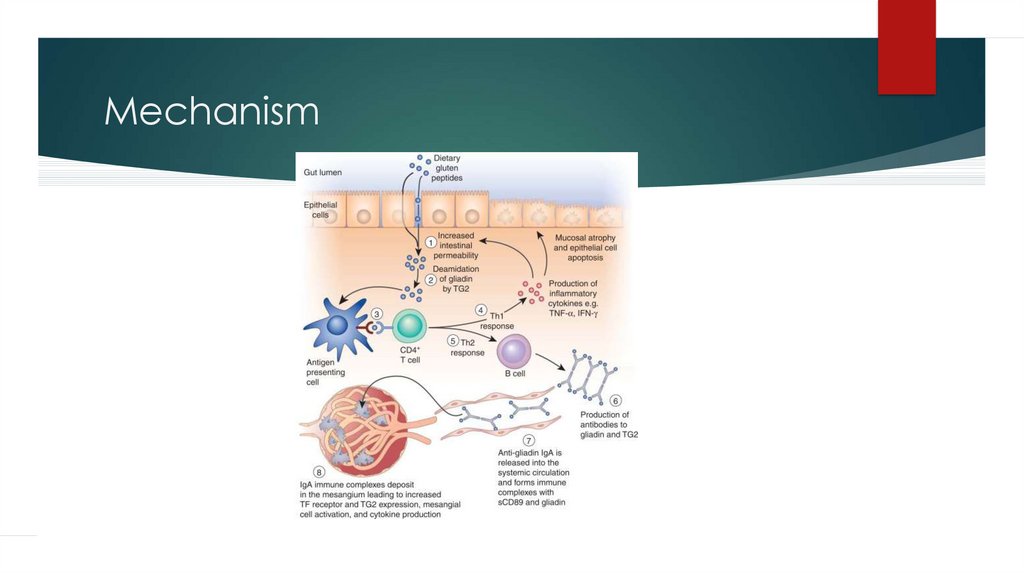
25. Explanation
From the history most likely you have acondition called IgA nephropathy. Do you
know what it is?
Because of your URTI, the body produces
antibodies toward the bugs and these
antibodies deposit in the kidney causing
damage resulting in blood in the urine.
26. Mechanism
27.
Difference Between Nephrotic and NephriticSyndrome
Nephrotic Syndrome
Nephritic Syndrome
Can have URTI history before
Can have URTI/sore throat/ skin
infection before
BP normal
High BP
No haematuria
Haematuria present
ASO titre and C3 C4 NORMAL
High Cholesterol level
ASO titre high C3 C4 low
28.
29.
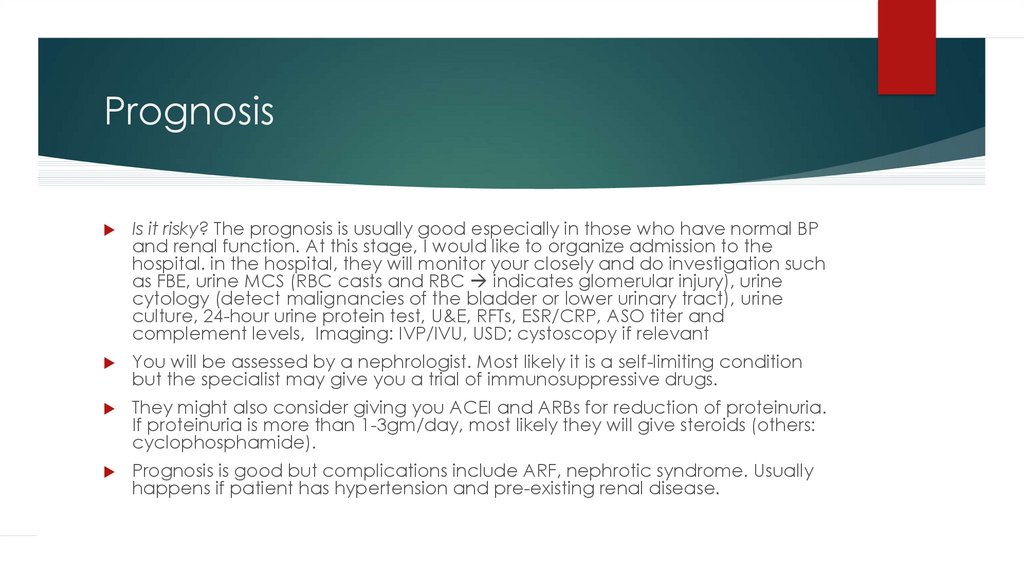
30. Prognosis
Is it risky? The prognosis is usually good especially in those who have normal BPand renal function. At this stage, I would like to organize admission to the
hospital. in the hospital, they will monitor your closely and do investigation such
as FBE, urine MCS (RBC casts and RBC indicates glomerular injury), urine
cytology (detect malignancies of the bladder or lower urinary tract), urine
culture, 24-hour urine protein test, U&E, RFTs, ESR/CRP, ASO titer and
complement levels, Imaging: IVP/IVU, USD; cystoscopy if relevant
You will be assessed by a nephrologist. Most likely it is a self-limiting condition
but the specialist may give you a trial of immunosuppressive drugs.
They might also consider giving you ACEI and ARBs for reduction of proteinuria.
If proteinuria is more than 1-3gm/day, most likely they will give steroids (others:
cyclophosphamide).
Prognosis is good but complications include ARF, nephrotic syndrome. Usually
happens if patient has hypertension and pre-existing renal disease.
31. Case 4
76 year old Mr. Aaron Samuels, who is your patient for last 7 years came tovisit you again after you’ve organized an urgent abdominal ultrasound. The
ultrasound was organized at his previous visit after you detected a pulsatile
mass on his abdomen. He came back after the USD confirmed an aneurysm
on the abdominal aorta below the renal arteries with a size 3.5cms. He came
to check the situation as he is planning to go on a wagon caravan trip next
week.
Task
Explain the diagnosis
Advise further management
Explain consequences and answer his questions
32. AAA
33. Guideline
34. 5 A’s approach
Hello Aaron, How have been from last week?Hmm, you are excited about trip!!! Okay, but Aaron, I
believe that I do not have some good news for you.
• Do not worry, I will explain what has happened, why it happened and what can happen in future and what we need to do
from now?
• Are you with me?
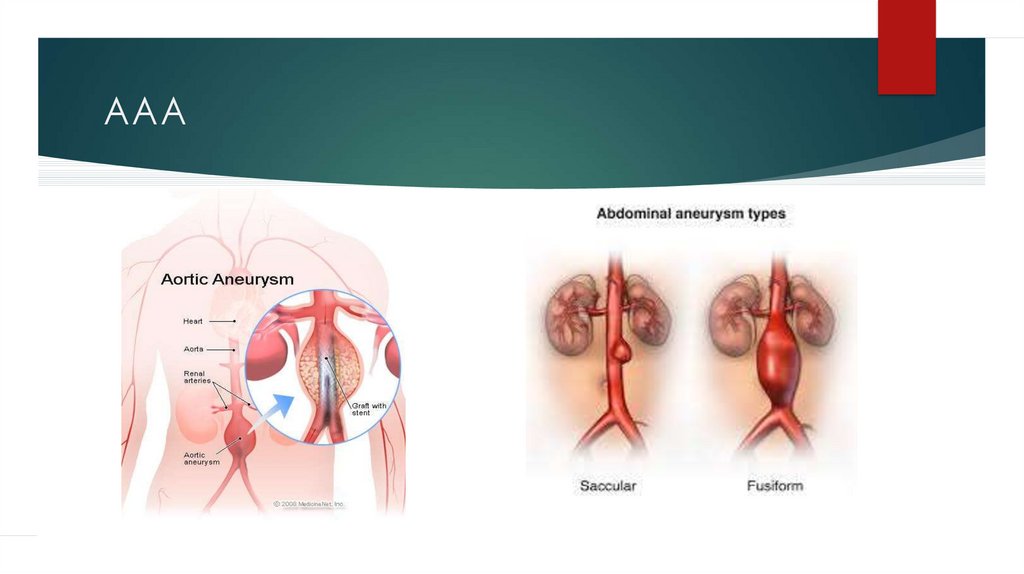
• Okay, you have a condition called (abdominal) aortic aneurysm. Don’t worry about the name, I will explain you what it is....
It is an abnormal dilation of the main blood vessel in our body which comes from the heart and crosses the chest, abdomen,
and supplies almost every part of the body with blood, known as aorta.
You have this dilatation at the level of your tummy.
Patients developed this dilatation due to weakness in the wall of the blood vessel which happens due to a degenerative
process happening in all layers of the aortic wall.
There are some risk factors that can lead to this degeneration process
35. Risk factors
Can be completely asymptomatic, but occasionally can give back ortummy pain.
Familial
Smoking
Alcohol
Diabetes mellitus
Hypertension
Hyperlipidemia
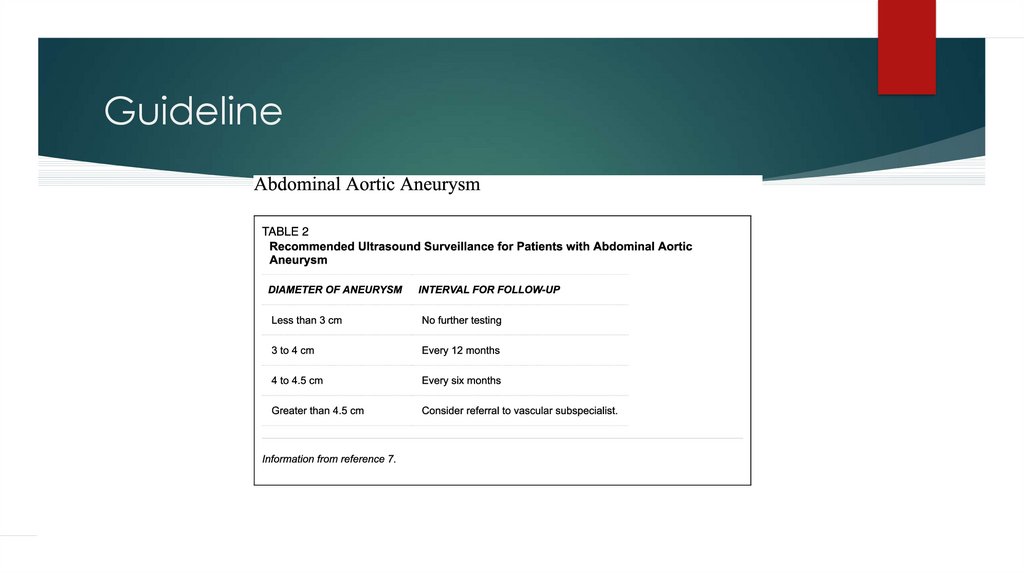
36. <5cm – Is it serious ? Can I go for trip doctor?
<5cm – Is it serious ? Can I go for trip doctor?The better news in your case is, it is <5cm wide, which is good.
It is still serious and we need to keep monitoring you.
Better to get the surgery done at the earliest to avoid complications.
In your case, you are welcome to go and enjoy your trip. But, before you leave, try to get
accommodation which is close to a hospital or G.P clinic.
Try not to exert too much during your trip.
No contact sports
RRRR
Red flags:- Tummy pain or back pain
Sudden dizziness or fainting feeling, N/V, loss of consciousness.
37. >5cm – Is it dangerous Doctor? Can I travel?
>5cm – Is it dangerous Doctor? Can Itravel?
When it is more than 5cm, you are at risk of rupture of aneurysm.
Even if you don’t have any serious symptoms when it is >5cms, we refer patients ASAP for
an elective surgery done by the vascular surgeon at the hospital, the sooner the better as
this condition is serious.
And I am sorry to say that you will have to reschedule your caravan trip.
If it is done electively, success rate is 95%.
If operation is delayed, the risk of rupture is 25%, but if ruptured, 80- 90% of cases lead to
death.
It is a better outcome if an elective operation is done ASAP.
Give a sick certificate – so that he can get a refund for caravan or to reschedule
Screening for your Son from age 50 is indicated .
38. Case 5
You are a HMO in the psychiatric department of the major hospital. You have been calledto see 26 year old , Jane , who just had a colonoscopy for her recurrent abdominal pain. The
result was normal. Before and during the procedure she was given i.v midazolam as she
was a bit agitated. In the recovery room she woke up quite anxious and you were called
because she said that she needs to talk someone as she is scared. She appears to be very
emotional and tearful.
Tasks:
Take further history from the patient
Explain the most probable cause of the symptoms (diagnosis for the patient)
39. History
CONFIDENTIALITYHOPC
Psychiatry H/O - PTSD, depression, suicidal ideas
HEADSS – alcohol, drug use is important
In this case need to ask about sexual life
Co morbidities (Important to ask about this in history)
Depression
Anxiety
Alcohol & Drug Abuse
If Co morbidities are present then referral to Psychiatrist is a MUST
40.
Acute Stress Disorder is the term used when symptoms develop within the first month after atraumatic event. The term PTSD with delayed onset (or delayed expression) is used when
symptoms surface 6 months or more after the traumatic event.
PTSD symptoms must last for at least 1 month and must seriously affect the ability to function
normally at home, at work or in social situations.
41. Management
DO YOU WANT TO REPORT THIS TO THE POLICE, so that the person who assaulted you may beprosecuted? It’s up to you?
Refer to the Psychologist for CBT (trauma focused treatment, EMDR)
Family meeting for support: Do you want to your family involves this? support group for rape victims
If she consider to the referral to a psychiatrist
Reading materials regarding to the delayed PTSD
Review : arrange a review with her in 1 month
42. Case 6
GP, 24 years old woman who is pregnant come to see you complain of nothearing well.
Task –
History, PEFE from the examiner
inform patient of cause and management
History 6month ago, gradually both side, no infection , no pain
43. History
Any injury, any infection, any painany exposure to very loud noise
Did you need to turn up the volume TV or radio to hear in compare to past.
Can you better in a noisy background
hearing distance
any trigger factory - pregnancy , post-partum
Family history - Hearing problem ( mother got operation before ear problem)
Drug - Gentamycin, Streptomycin
44. Physical examination
Inspection -External ear - pulling ear -pain?-Press mastoid bone - tenderness ( cholesteatoma)
-Otoscope - 1. any external ear infection
2. wax, Discharge
3. Tympanic in - intact , bulging
Hearing capacity-
I will whisper number. Can you repeat? 60cm away from tested ear, Other
ear close - both ear ( lost in both)
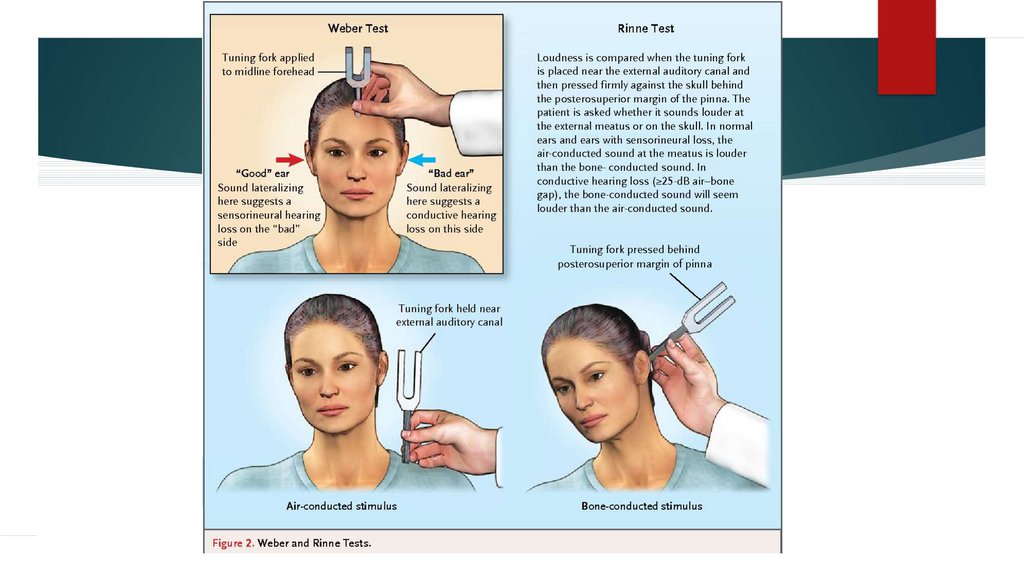
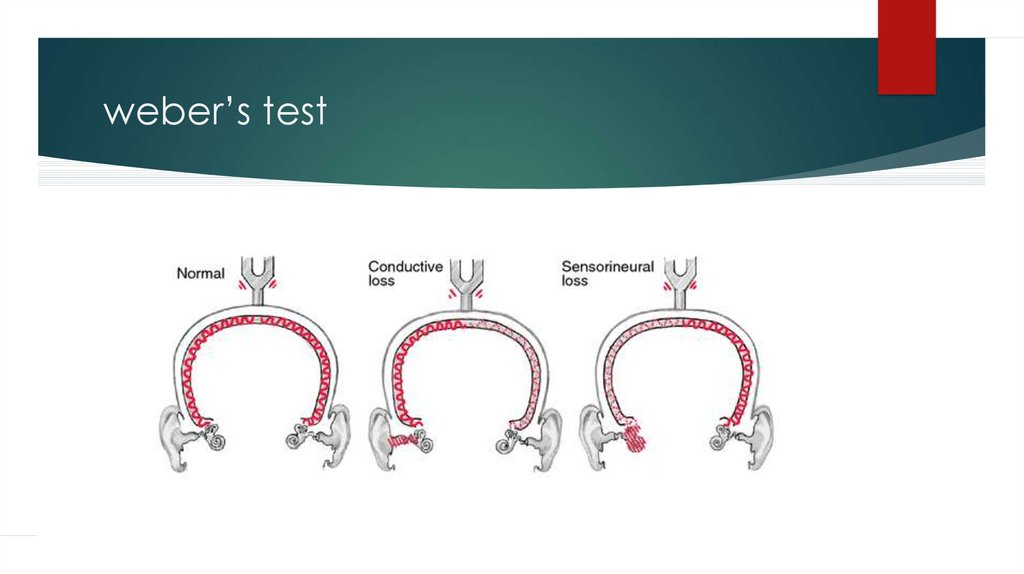
45. Examination
Special test-Tunning fork ( 256 Hz)
-Rinnie -mastoid and ear which one better?
-Weber test
Normal AC>BC
46.
47. weber’s test
48. causes of Sensorineural deafness
causes of Sensorineural deafness-Cochlear degeneration
-Acoustic neuroma
-Drug -Ototoxicity - Streptomycin
-Fracture of petrous temporal bone
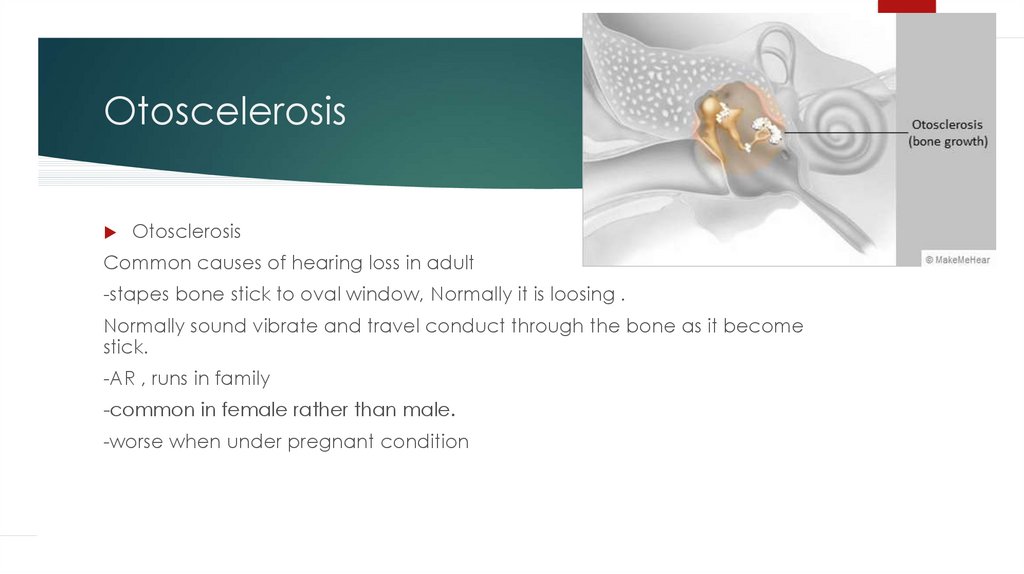
49. Otoscelerosis
OtosclerosisCommon causes of hearing loss in adult
-stapes bone stick to oval window, Normally it is loosing .
Normally sound vibrate and travel conduct through the bone as it become
stick.
-AR , runs in family
-common in female rather than male.
-worse when under pregnant condition
50. Management
hearing contain 2 parts - air conduction and nerve conduction.your cases is air conduction defect, we called otoscleroiss.
Management
At the moment, all the test is only screening test. I 'll refer you to specialist
to do "audiometry" and ENT specialist, I will do full assessment.
Tx - If it is otoscelerosis, prosthetic stapestectomy and vein graft . It 'll
improve your hearing condition.
Unfortunately, hearing aid is less effective in this condition.
51. Case 7
A young woman at 10 weeks’ gestational age comes to see you in your GPpractice. She is concerned about having a baby with Down syndrome as
recently, her sister had a baby with Down syndrome.
Task
■ Counsel patient
52. History
GM, I am Dr. XYZ… how are you today? I understand that you are here for informationabout Down Syndrome, we will talk about this. Is this a planned pregnancy?
Congratulations.
I understand from the notes that you are here to discuss about Down syndrome
screening. I appreciate your initiative to do that. I understand your anxiety. I will give
you all the information regarding the tests which can be done and how effective they
are.
How is your pregnancy going so far? Are you getting your antenatal care? Are you
done with your blood tests? Any concerns or issues? Any issues about your general
health.
Down syndrome is one of the most common genetic abnormality with trisomy 21.
There are some indications in doing Down syndrome screening in pregnant women:
– Increased maternal age (>30)
– Previous down syndrome baby
– History of down syndrome in the family
53. History
Reassure her that she will be monitored. Antenatal screening should bediscussed with all pregnant women so that they can make an informed
decision whether to proceed with testing. In Victoria, 80% of pregnant
women have an antenatal screening test. There are no specific
contraindications or precautions.
We have screening tests and confirmatory tests. Women must understand
that the screening test is a risk assessment and places their pregnancy in
an increased or decreased risk category. Women must also understand
that if the test suggests a high risk they will be offered a
diagnostic(confirmatory) test that carries a small risk of miscarriage.
54. First trimester screening test
Combined Test-■ A non-fasting blood test which is done at 9-13 weeks AOG. We check Free beta-HCG (increase) &
Pregnancy Associated Plasma Protein-A (PAPP-A) (decreased). We combine it with an Ultrasound
done at 11-13 weeks AOG. Here we check
– Fetal nuchal translucency i.e. skin fold thickness at back of baby's neck. Increased thickness (more
than 2.5 mm) may be suggestive of chromosomal abnormalities.
– Nasal bone ossification: The presence of an ossified nasal bone conveys lower risk for Down
syndrome i.e. absence of nasal bone increases the risk of down Syndrome.
55. risk factor
Information from the ultrasound scan is reported to the pathologylaboratory to allow the calculation of the pregnancy specific risk factor.
This risk factor takes into account the woman’s age, weight, pregnancy
gestation, serum markers and the ultrasound scan markers.
Reports often classify the risk as ‘increased’ or ‘decreased’ using a cut-off
value for Down syndrome of one in 300. Risk values less than 1 in 300 are
considered decreased risk and no further testing is required.
56. 2nd trimester screening test
15 -17 weeks-solely blood tests.– Triple test (a, b, e) (detection -71%) or
– Quadruple {afp (decrease), b hCG (increased), estriol (decrease), inhibin A (increased)},
detection 81%
Second trimester screening is less sensitive that FTS ( first trimester screening). It is less
useful for risk of trisomy-21 and 18, but the α-fetoprotein assessment does define the
risk of a neural tube defect.
FTS is not performed in addition to STS (second), but is used in women who misses out
FTS. For first trimester screening, women require two separate forms – one for the
ultrasound and one for the blood test.
Antenatal screening tests are considered a private opt-in test and therefore out-ofpocket costs will be incurred.
57. In high-risk pregnancies, diagnostic tests:
■ CVS– Done ideally at 11-14 weeks.
– A needle will be introduced into ur tummy, guided by ultrasound to avoid damage to the
fetus and small portion pf placenta is taken and analyzed for genetic abnormalities
– Results within 24 hours with FISH
– However, the karyotyping is slightly less accurate than with amniocentesis because of
potential contamination with cells of maternal origin.
– 1% risk of abortion (1 in 100)
■ Amniocentesis
– Done ideally at around 15-18
– A small amount of fluid in bag that surround the baby is taken and analyzed for genetic
abnormalities.
– Results within 2-3 weeks but more accurate
– 0.5% risk of abortion (1 in 200)
58. patient questions
Are the tests painful? Many women find the diagnostic tests uncomfortable, and theyare often managed by local anaesthetic. You should take things easy for one to two
days after the tests.
If previous pregnancy was down syndrome, the risk of having Down syndrome in the
next pregnancy increases by 1%.
Now I will discuss with you other risks of old Age pregnancy:
– Increased chances of miscarriage, ectopic, HTN, GDM, placenta previa, preterm,
increase chance of induction and CS.
– Fetal: Can have down, NTD, renal, cardio defects but we are most concerned about down
syndrome
■ But don’t worry, we will closely monitor the pregnancy. Reassurance by saying that
many women have successful pregnancies and we will monitor you regularly.
59. Case 8
In a GP setting. An 17 year-old boy complaining of pain in the tummy . Hevomited twice, one time whitish and second time greenish vomiting. This
incidence happened when he was riding a bicycle he got the pain & this
happened 2 hours ago. Previously healthy.
Task:
take a relevant history,
Ask physical examination findings from the examiner.
Provisional diagnosis & management.
60. Differential
Duodenal injuryLocal abdominal hematoma
Gall bladder injury
Testicular torison
UTI
Gall stone
Strangulated inguinal hernia
UTI
Ureter colic/stone
Adhesion (small bowel obstruction ask previous surgery)
61. History
Vital stability of the child – B.P. -100/60, P.R- 120, RR- 35 & O2 – 92%.SOCRATES – pain – offer pain killer – scale was 8+
Vomiting how many times , CCVO – colour, consistency, volume & odour?
How did it happen?
Any swelling in your tummy, swelling in the groin area?
Any trauma, any abdominal pain, fever
Did he loose consciousness? Injury anywhere else?
Did pass flatus ? Stool ? Any blood loss?
Activity afterwards ?
Social activity ? Active in sports?
62. History
BINDS – Heel prick test was done ?( thyroid) Any concern aboutdevelopment?
Family situation ? ( child abuse)
Any mumps, family history of mumps
Any history of previous surgery?
Any significant weight loss or any lumps & bumps?
63. Physical examination
General appearance – distress & in pain , no signs of dehydrationVS: - stable
Growth chart – normal
I want to quickly go to respiratory system & CVS – normal
Abdominal examination – inspection bluish discolouration in right upper quadrant.
Palpation – guarding & tenderness present, bowel sound present
Deep palpation – no organomegaly
Groin: tenderness, any swelling, mass (hernia)?
Scrotum: tenderness, swelling, mass, redness, position of testis (horizontal) – seems
normal
64. Explanation
Your son has a Duodenal injury in the tummy as I could see bruise patch onthe abdominal region This is a surgical emergency. We are suspecting
some internal organ injury as well. I was trying to rule out testicular torrison
and other causes are not there. However we would like to admit your child
For pedatric surgeon care. If internal bleeding happen doctor may
consider for exploratory laparotomy. Mean while we do certain
investigations blood profile, blood culture and ultra sound of the tummy.
Investigation: if Doppler U/S available that’s fine, but my concern is not to
waste time, immediately take to the theatre no use of ultrasound.
65.
Case: 1026 year old John has been brought by the police from a local pub to the ED
where you are the HMO. He had a fight with one of his flatmates while
having a drink with him. He has dislocated his right little finger in the fight and
the police wants him to be medically examined by charging him assault.
When you check the previous records of John he had been at the hospital a
couple of times.
Task :
1. Take appropriate history
2. Discuss about the Diagnosis & Management with the patient.
66.
Assess patient’s injury, offer pain managementCONFIDENTIALITY
History
Can you tell me what happened at the Pub:
• He says he deserved to be punched and that he was not drunk at that time.
• Had only 1 drink.
• 1st time getting into trouble? No. A few times earlier as well.
• He thinks they are not concerned and want to do things their way.
• He is not sorry about having fights with others.
Ask for previous hospital records
Hospital admissions before :
• One following car crash ( any head injury then?)(DUI)
• Others following fights.
67.
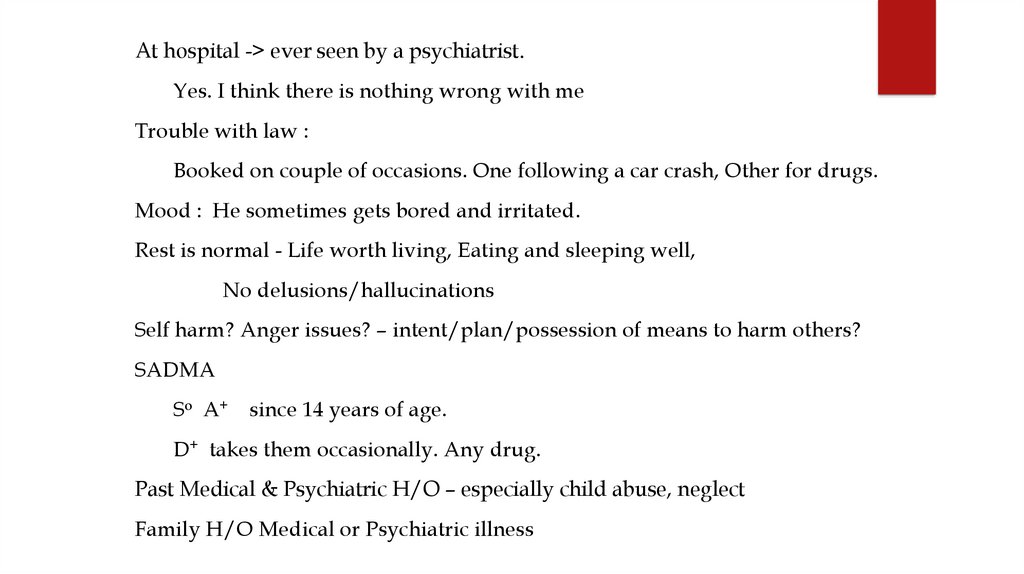
At hospital -> ever seen by a psychiatrist.Yes. I think there is nothing wrong with me
Trouble with law :
Booked on couple of occasions. One following a car crash, Other for drugs.
Mood : He sometimes gets bored and irritated.
Rest is normal - Life worth living, Eating and sleeping well,
No delusions/hallucinations
Self harm? Anger issues? – intent/plan/possession of means to harm others?
SADMA
So A+
since 14 years of age.
D+ takes them occasionally. Any drug.
Past Medical & Psychiatric H/O – especially child abuse, neglect
Family H/O Medical or Psychiatric illness
68.
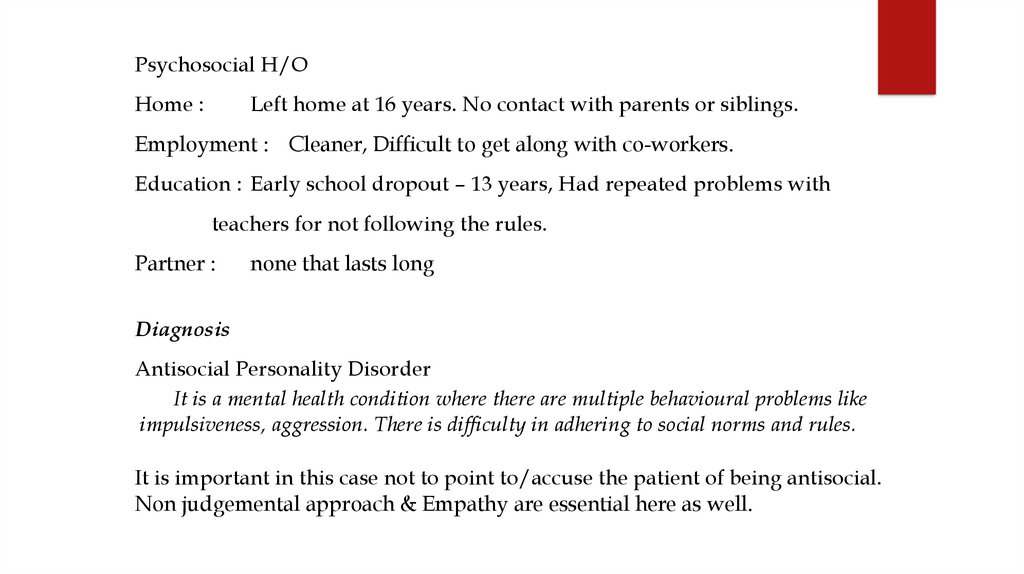
Psychosocial H/OHome :
Left home at 16 years. No contact with parents or siblings.
Employment : Cleaner, Difficult to get along with co-workers.
Education : Early school dropout – 13 years, Had repeated problems with
teachers for not following the rules.
Partner :
none that lasts long
Diagnosis
Antisocial Personality Disorder
It is a mental health condition where there are multiple behavioural problems like
impulsiveness, aggression. There is difficulty in adhering to social norms and rules.
It is important in this case not to point to/accuse the patient of being antisocial.
Non judgemental approach & Empathy are essential here as well.
69.
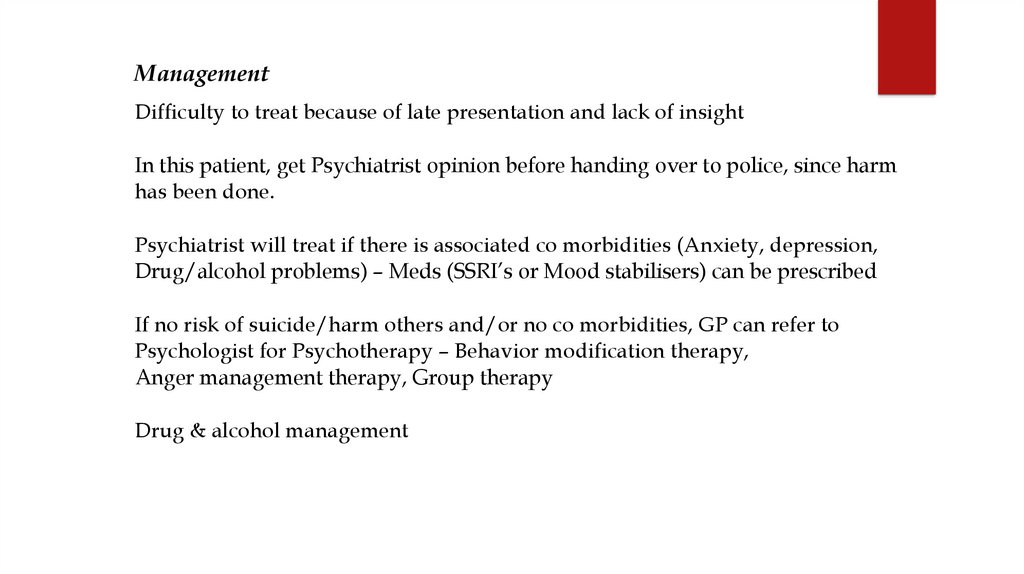
ManagementDifficulty to treat because of late presentation and lack of insight
In this patient, get Psychiatrist opinion before handing over to police, since harm
has been done.
Psychiatrist will treat if there is associated co morbidities (Anxiety, depression,
Drug/alcohol problems) – Meds (SSRI’s or Mood stabilisers) can be prescribed
If no risk of suicide/harm others and/or no co morbidities, GP can refer to
Psychologist for Psychotherapy – Behavior modification therapy,
Anger management therapy, Group therapy
Drug & alcohol management
70.
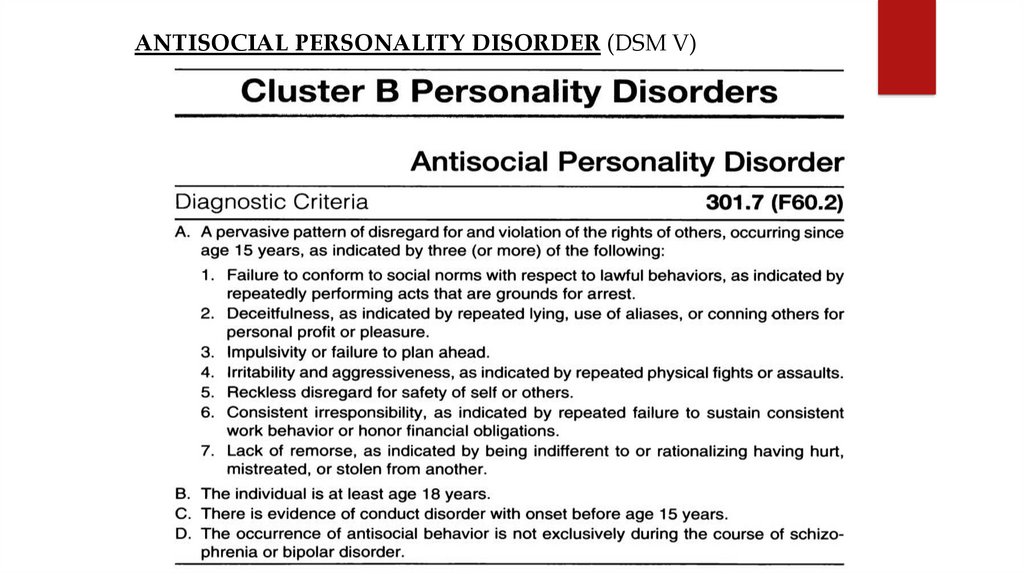
ANTISOCIAL PERSONALITY DISORDER (DSM V)71.
a mental disorder where a person shows no regard for right or wrong
and is not concerned with the feelings or rights of other people.
manipulate, antagonise and treat others with
indifference
no remorse or guilt
In order to be diagnosed with ASPD, a person must be at least 18 years
and shown signs of a Conduct Disorder before the age of 15.
A Conduct Disorder is a repetitive patter of behaviour that violates the
rights, wishes, and feelings of others.
The pattern continues to adulthood but on a larger scale.
Rules and norms are disgarded, and the person may violate the law, or have
drug and alcohol problems.
It becomes difficult for them to fulfill responsibilities and commitments.
72.
SymptomsDeceitfulness
Non Conformity no respect for the law and have no boundaries.
Impulsivity
Aggression
Irresponsibility
Causes and Development
biological
genetic - family history of ASPD
early social factors and interactions with family, friends & other children
childhood diagnosis of Conduct Disorder
childhood abuse or neglect
unstable, violent or disordered childhood, and poor social contact
73.
Referencehttps://wayahead.org.au/mental-health-information/fact-sheets/
mental-illness-and-related/antisocial-personality-disorder/








 Медицина
Медицина