Похожие презентации:
Introduction to pharmacology in nursing
1. Introduction to Pharmacology in Nursing
2.
• Nurses need to haveknowledge about the
actions and effects of
medications
• To safely and
accurately administer
medications nurses
need to have an
understanding of
pharmacologic
principles
3. Pharmacologic Principles
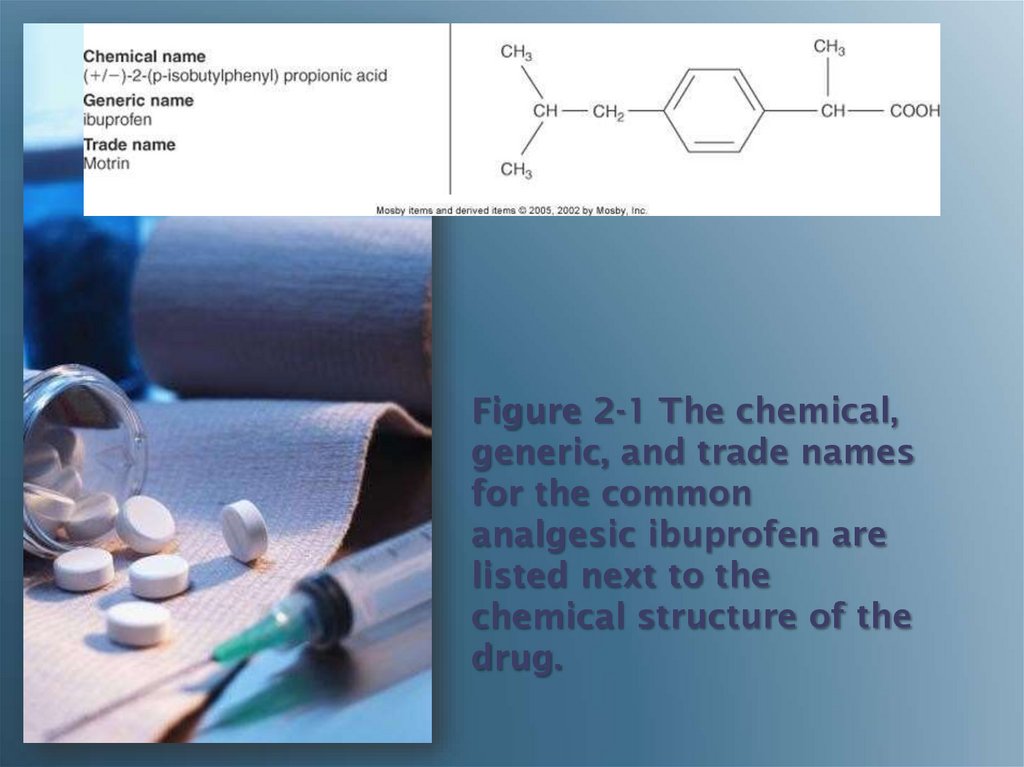
4. Chemical name
Drug NamesChemical name
• Describes the drug’s chemical
composition and molecular
structure
Generic name (nonproprietary
name)
• Name given by the United
States Adopted
Name Council
Trade name (proprietary name)
• The drug has a registered
trademark; use of the name
restricted by the drug’s patent
owner
(usually the manufacturer)
5. Chemical name
Drug Names(cont'd)
Chemical name
• (+/-)-2-(p-isobutylphenyl)
propionic acid
Generic name
• ibuprofen
Trade name
• Motrin®, Advil®
6.
Figure 2-1 The chemical,generic, and trade names
for the common
analgesic ibuprofen are
listed next to the
chemical structure of the
drug.
7.
PharmacologicalConcepts:
Classification
• Classification- Nurses learn
to categorize meds with
similar characteristics by
their class
• Medication classification
indicates the effect of the
med on the body system,
the symptom the med
relieves, or the med’s
desired effect (e.g. oral
hypoglycemics)
8.
PharmacologicalConcepts:
Classification
• A medication may also
be part of more than
one class
• Aspirin is an analgesic,
antipyretic, antiinflammatory, and antiplatelet
9.
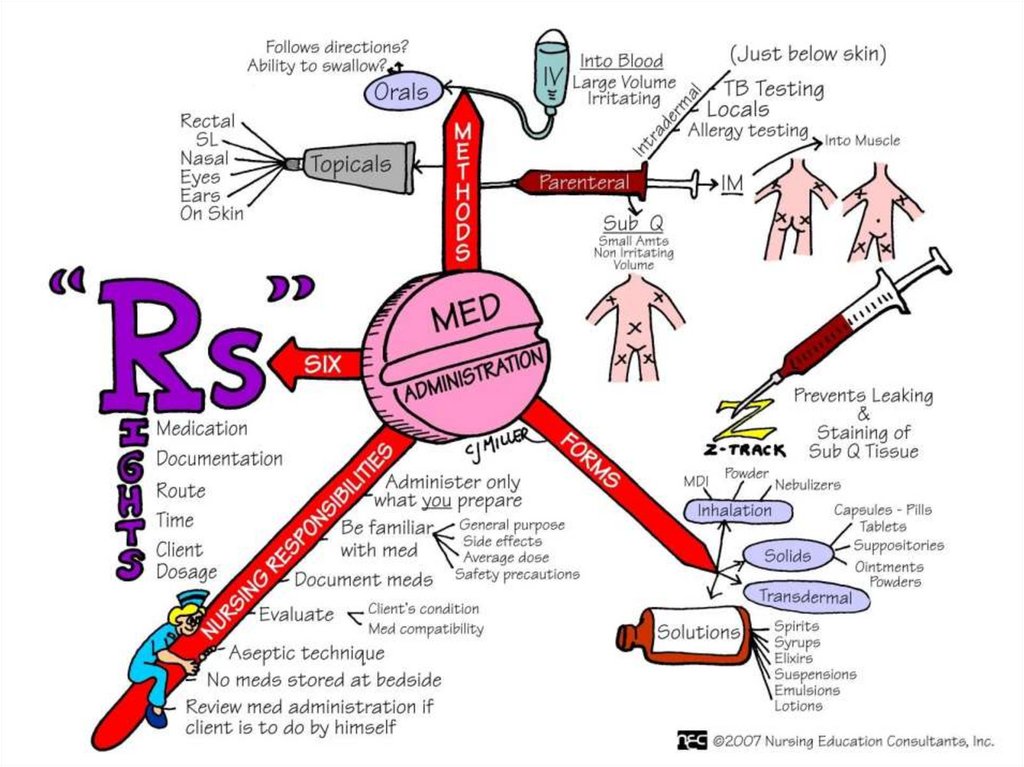
• Medications are availablePharmacological
in a variety of forms and
Concepts:
preparations
Medication
• The form of the med will
Forms
determine its route of
administration
• Composition of med is
designed to enhance its
absorption & metabolism
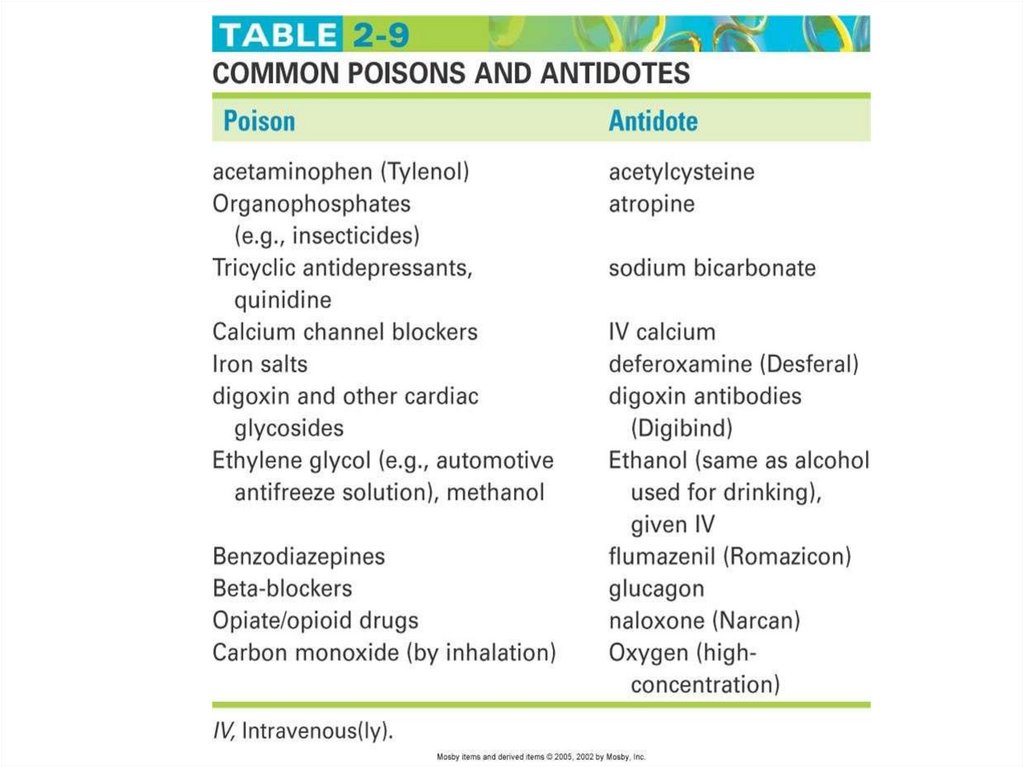
• Many meds are available in
several forms
10.
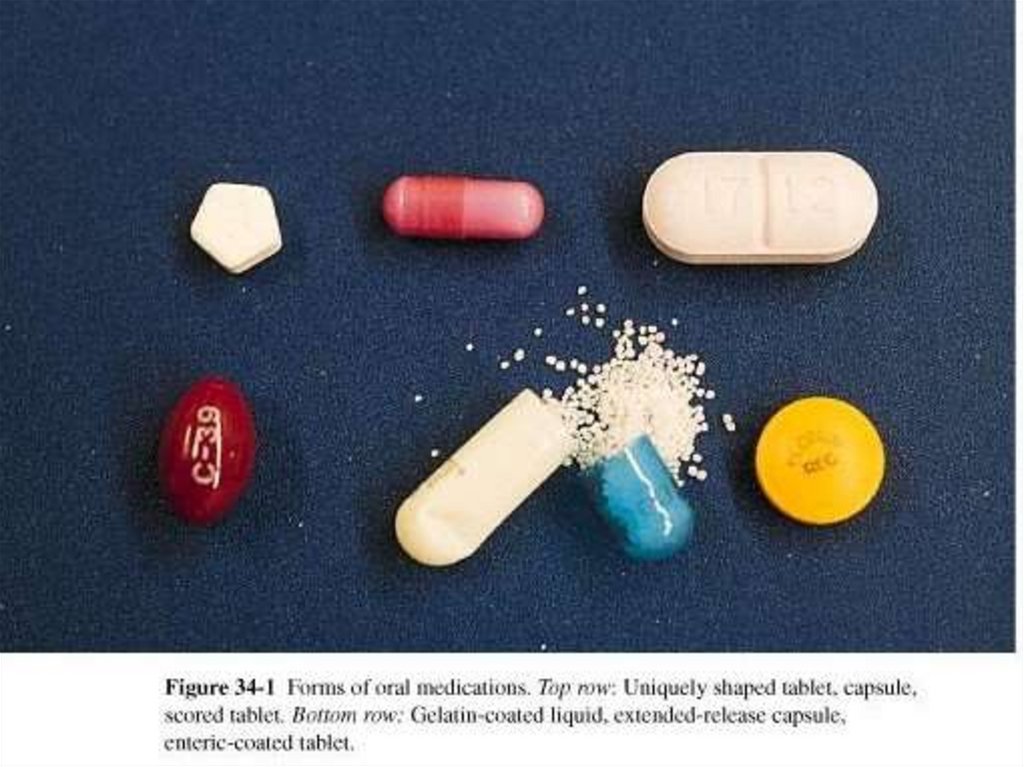
Medication FormsTablet
Capsule
Elixir
Enteric-coated
Suppository
Suspension
Transdermal patch
11.
12.
13.
PharmacologicPrinciples
Pharmaceutics
Pharmacokinetics
Pharmacodynamics
Pharmacotherapeutics
Pharmacognosy
14. The study of how various drug forms influence pharmacokinetic and pharmacodynamic activities
PharmaceuticsThe study of how various
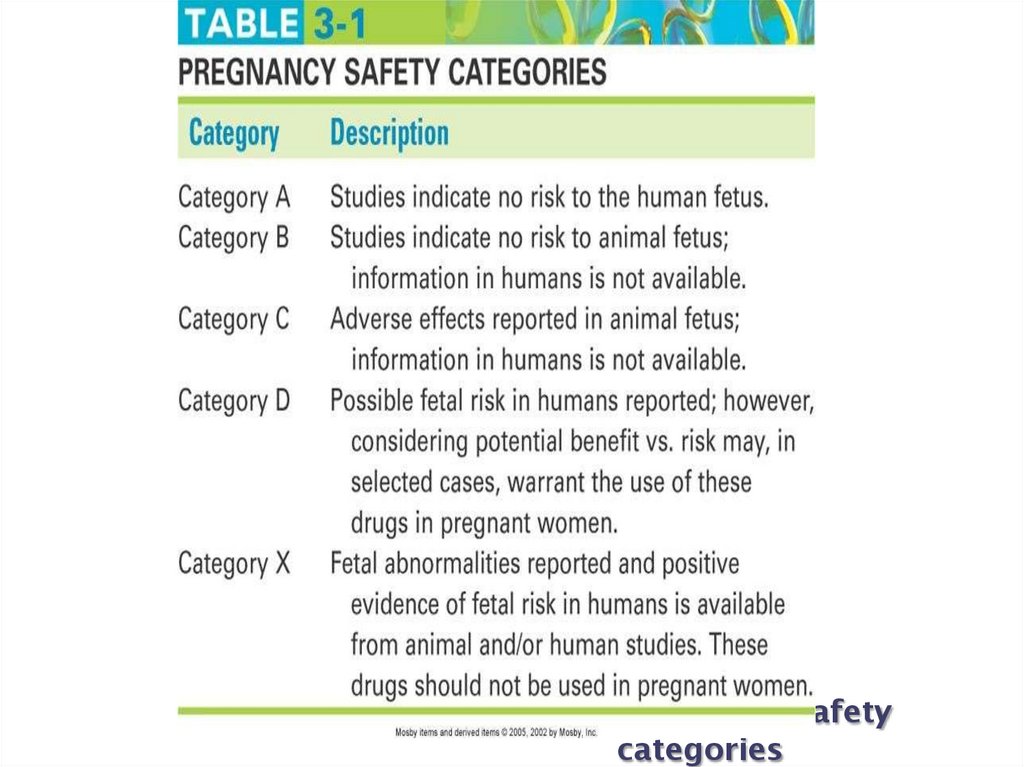
drug forms influence
pharmacokinetic and
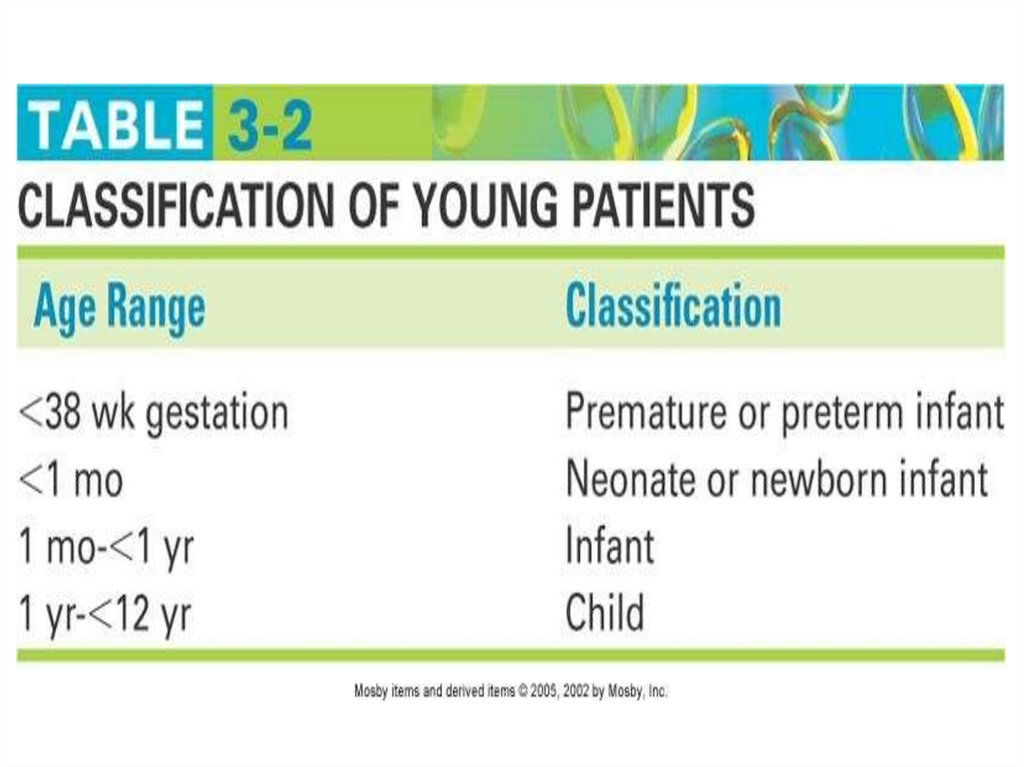
pharmacodynamic activities
15.
PharmacokineticsThe study of what the
body does to the drug
– Absorption
– Distribution
– Metabolism
– Excretion
16. Pharmacodynamics
The study of what the
drug does to the body
– The mechanism of drug
actions in living tissues
17.
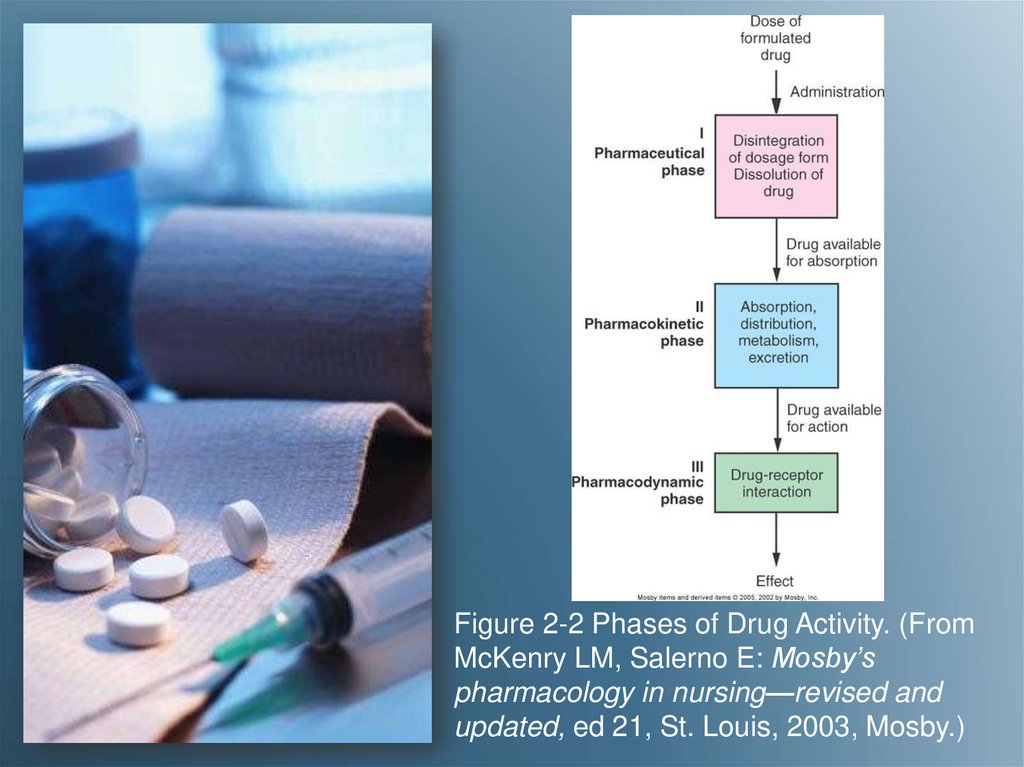
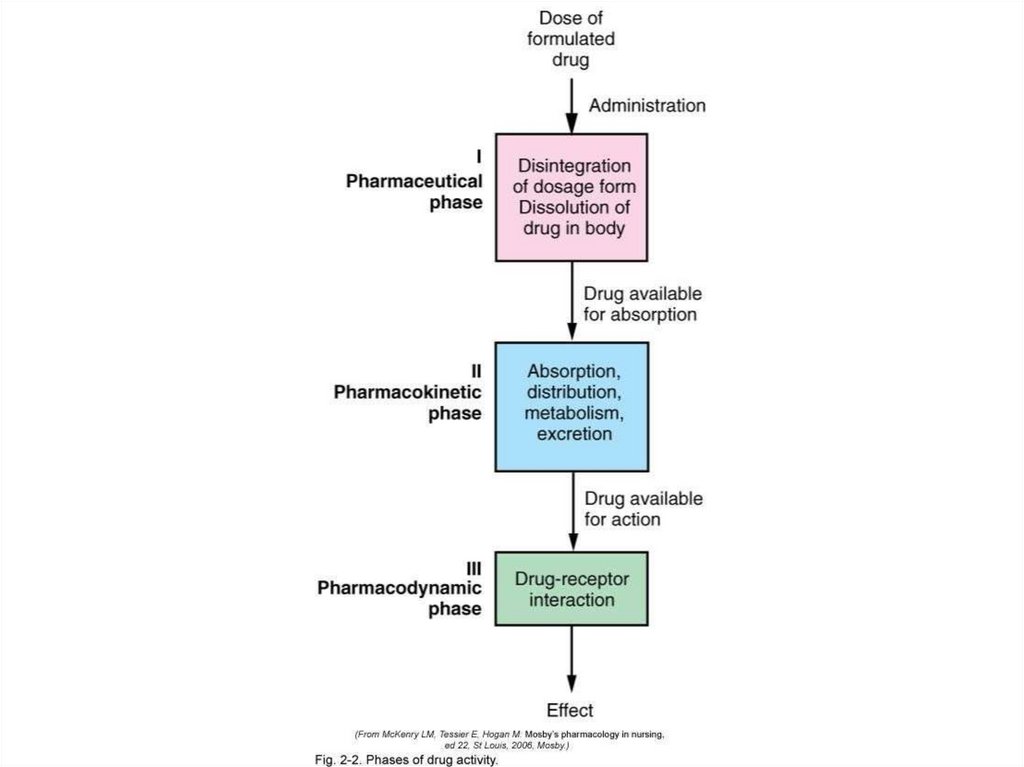
Figure 2-2 Phases of Drug Activity. (FromMcKenry LM, Salerno E: Mosby’s
pharmacology in nursing—revised and
updated, ed 21, St. Louis, 2003, Mosby.)
18. Pharmacotherapeutics
The use of drugs and theclinical indications for
drugs to prevent and
treat diseases
19. The study of natural (plant and animal) drug sources
PharmacognosyThe study of natural
(plant and animal) drug
sources
20. Pharmacokinetics:
Absorption• The rate at which a
drug leaves its site of
administration, and the
extent to which
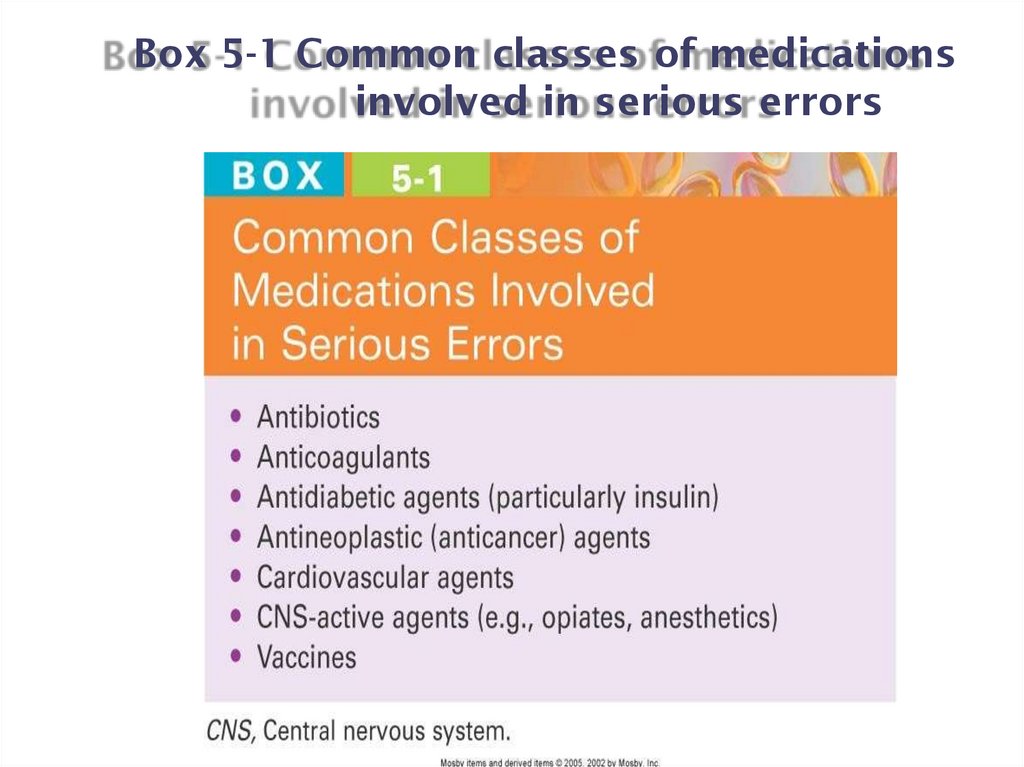
absorption occurs
– Bioavailability
– Bioequivalent
21. Factors That Affect Absorption
• Administration route of thedrug
• Ability of Med to Dissolve
• Food or fluids
administered with the drug
• Body Surface Area
• Status of the absorptive
surface
• Rate of blood flow to the
small intestine
• Lipid Solubility of Med
• Status of GI motility
22.
Routes ofAdministration
• A drug’s route of
administration affects
the rate and extent of
absorption of that drug
– Enteral (GI tract)
– Parenteral
– Topical
23.
Enteral Route• Drug is absorbed into
the systemic circulation
through the oral or
gastric mucosa, the
small intestine, or
rectum
– Oral
– Sublingual
– Buccal
– Rectal
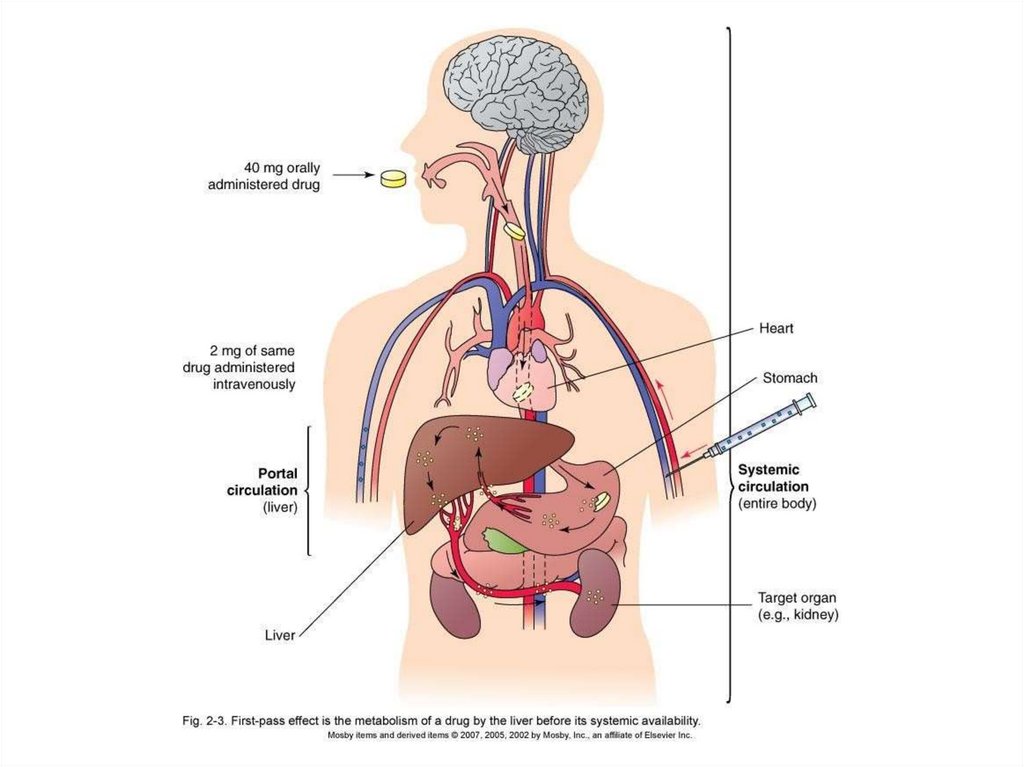
24. First-Pass Effect
• The metabolism of a drug andits passage from the liver into
the circulation
– A drug given via the oral route
may be extensively metabolized
by the liver before reaching the
systemic
circulation (high
first- pass effect)
– The same drug—given IV—
bypasses the liver, preventing
the first-pass effect from taking
place, and more drug reaches
the circulation
25.
26.
Box 2-1 Drug Routes and First-Pass Effects27.
Parenteral Route• Intravenous (fastest
delivery into the blood
circulation)
• Intramuscular
• Subcutaneous
• Intradermal
• Intrathecal
• Intraarticular
28.
Topical Route• Skin (including
transdermal patches)
• Eyes
• Ears
• Nose
• Lungs (inhalation)
• Vagina
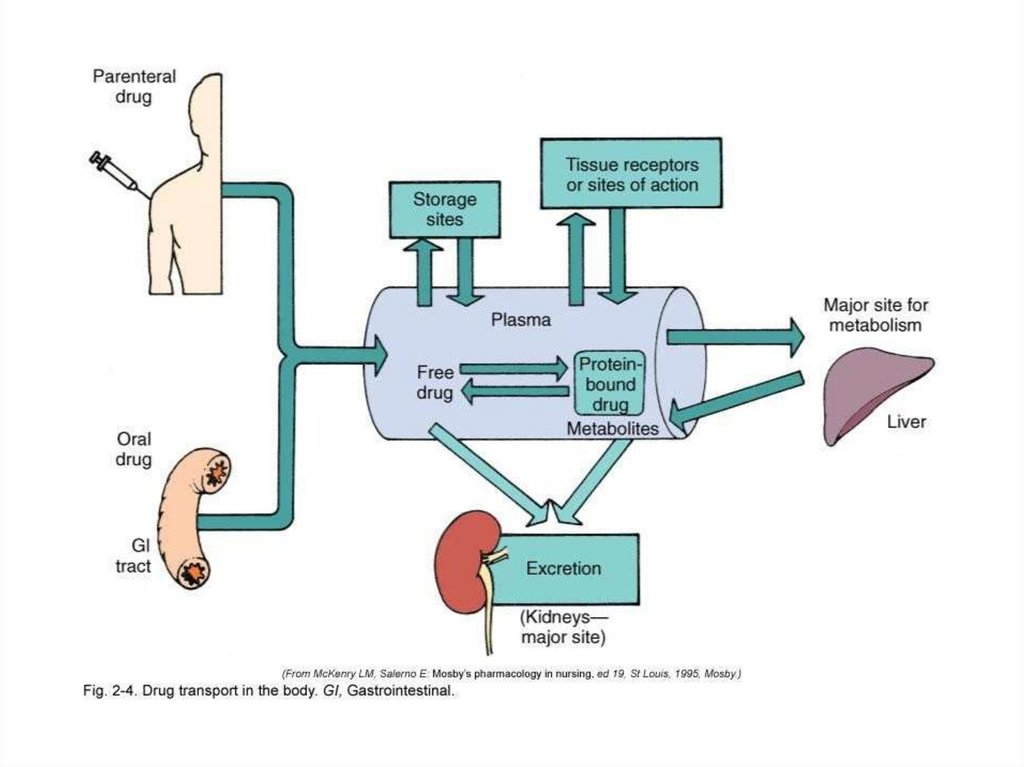
29. Distribution
The transport of a drug in thebody by the bloodstream to
its site of action
•Protein-binding
•Water soluble vs. fat soluble
•Blood-brain barrier
•Areas of rapid distribution:
heart, liver,
kidneys, brain
•Areas of slow distribution:
muscle, skin, fat
30.
31. Metabolism (Also Known As Biotransformation)
The biologic transformationof a drug into
an inactive metabolite, a
more soluble compound, or a
more potent metabolite
•Liver (main organ)
•Kidneys
•Lungs
•Plasma
•Intestinal mucosa
32. Delayed drug metabolism results in:
Metabolism/Biotransformation(cont'd)
Delayed drug metabolism
results in:
• Accumulation of drugs
• Prolonged action of the
drugs
Stimulating drug
metabolism causes:
• Diminished pharmacologic
effects
33. The elimination of drugs from the body
ExcretionThe elimination of drugs
from the body
• Kidneys (main organ)
• Liver
• Bowel
– Biliary excretion
– Enterohepatic circulation
34.
1. You are caring for a client who has diabetes complicated
by kidney disease. You will need to make a detailed assessment
when administering medications because this client may
experience problems with:
A. Absorption
B. Biotransformation
C. Distribution
D. Excretion
35 - 34
35.
The nurse is administering a sustained-release capsule to a new patient. Thepatient insists that he cannot swallow pills. What is the nurse's next best
course of action?
A. Ask the prescriber to change the order
B. Crush the pill with a mortar and pestle
C. Hide the capsule in a piece of solid food
D. Open the capsule and sprinkle it over pudding
36.
The nurse is administering a sustained-release capsule to a new patient. Thepatient insists that he cannot swallow pills. What is the nurse's next best
course of action?
A. Ask the prescriber to change the order
B. Crush the pill with a mortar and pestle
C. Hide the capsule in a piece of solid food
D. Open the capsule and sprinkle it over pudding
A. Rationale: Enteric-coated or sustained-release capsules should not be
crushed; the nurse needs to contact the prescriber to change the
medication to a form that is liquid or can be crushed.
37.
A nursing student takes a patient's antibiotic to his room. The patient asks thenursing student what it is and why he should take it. Which information does
the nursing student include when replying to the patient?
A. Only the patient's physician can give this information.
B. The student provides the name of the medication and a description of its
desired effect.
C. Information about medications is confidential and cannot be shared.
D. He has to speak with his assigned nurse about this.
B. Rationale: Patients need to know information about their medications so
they can take them correctly and safely.
38.
After seeing a patient, the physician gives a nursing student a verbalorder for a new medication. The nursing student first needs to:
A. Follow ISMP guidelines for safe medication abbreviations.
B. Explain to the physician that the order needs to be given to a
registered nurse.
C. Write down the order on the patient's order sheet and read it back to
the physician.
D. Ensure that the six rights of medication administration are followed
when giving the medication.
39.
After seeing a patient, the physician gives a nursing student a verbalorder for a new medication. The nursing student first needs to:
A. Follow ISMP guidelines for safe medication abbreviations.
B. Explain to the physician that the order needs to be given to a
registered nurse.
C. Write down the order on the patient's order sheet and read it back to
the physician.
D. Ensure that the six rights of medication administration are followed
when giving the medication.
B. Rationale: Nursing students cannot take orders.
40.
• Study of thePharmacodynamics
mechanism of drug
actions in living tissue
• Drug-induced
alterations to normal
physiologic function
• Positive changeTherapeutic effect-Goal
of therapy
41.
Mechanism ofAction
• Ways in which a drug
can produce a
therapeutic effect
• The effects that a
particular drug has
depends on the cells or
organ targeted by the
drug
• Once the drug hits its
“site of action” it can
modify the rate at
which a cell or tissue
functions
42.
Mechanism ofAction
• Receptor Interaction
• Enzyme Interaction
• Non-Specific
Interaction
43.
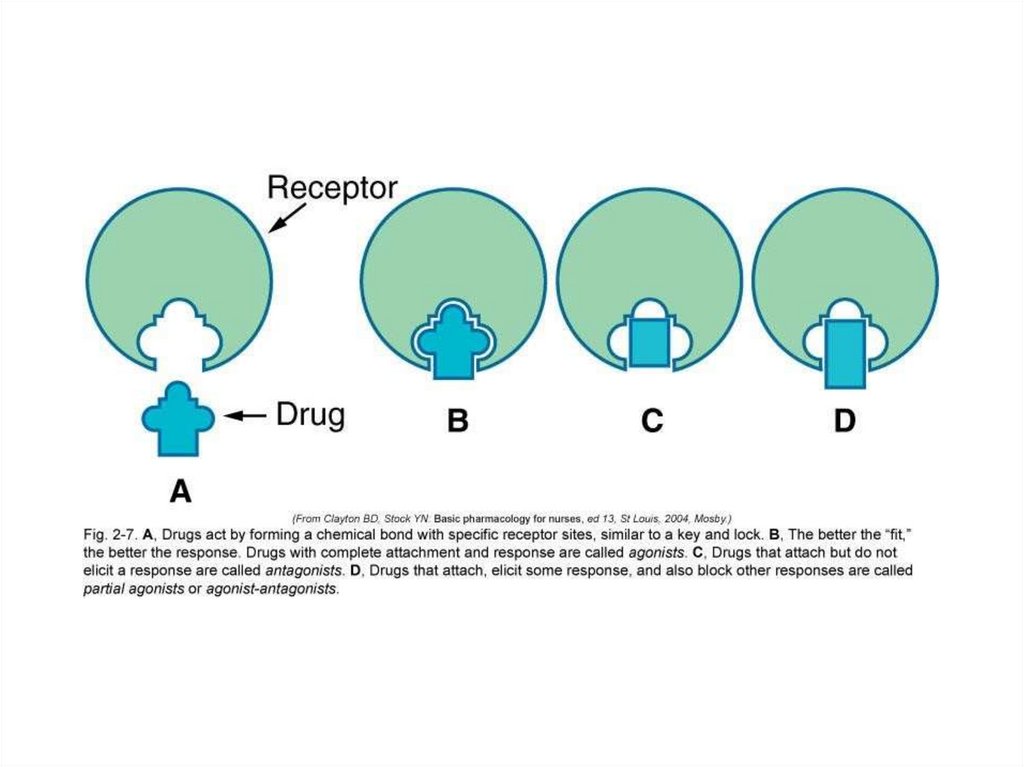
Receptor Interaction• Drug structure is essential
• Involves the selective
joining of drug molecule
with a reactive site on the
cell surface that elicits a
biological effect
• Receptor is the reactive site
on a cell or tissue
• Once the substance binds
to and interacts with the
receptor, a pharmacologic
response is produced
44.
ReceptorInteraction
• Affinity- degree to which a
drug binds with a receptor
• The drug with the best “fit”
or affinity will elicit the
best response
• Drug can mimic body’s
endogenous substances
that normally bind to
receptor site
• Drugs that bind to
receptors interact with
receptors in different ways
to either block or elicit a
response
45.
ReceptorInteraction
• Agonist-Drug binds to
receptor-there is a
response (Adrenergic
Agents)
• Antagonist-drug binds
to receptor-no
response-prevents
binding of agonists
(Alpha & Beta Blockers)
46.
47.
• Enzymes are substancesEnzyme Interaction
that catalyze nearly every
biochemical reaction in a
cell
• Drugs can interact with
enzyme systems to alter a
response
• Inhibits action of enzymesenzyme is “fooled” into
binding to drug instead of
target cell
• Protects target cell from
enzyme’s action (ACE
Inhibitors)
48.
Non-SpecificInteraction
• Not involving a receptor
site or alteration in enzyme
function
• Main site of action is cell
membrane or cellular
process
• Drugs will physically
interfere or chemically alter
cell process
• Final product is altered
causing defect or cell death
• Cancer drugs, Antibiotics
49.
50.
The nurse is giving a medication that has ahigh first-pass effect. The physician has
changed the route from IV to PO. The nurse
expects the oral dose to be:
1.Higher because of the first-pass effect.
2.Lower because of the first-pass effect.
3.The same as the IV dose.
4.Unchanged.
51.
.A patient is complaining of severe pain
and has orders for morphine sulfate. The
nurse knows that the route that would
give the slowest pain relief would be
which route?
1. IV
2. IM
3. SC
4. PO
52.
.A patient is complaining of severe pain and
has orders for morphine sulfate. The nurse
knows that the route that would give the
slowest pain relief would be which route?
1. IV
2. IM
3. SC
4. PO
Rationale: Parenteral routes result in the fastest
absorption and therefore also the fastest effects
53.
Type ofMedication Action
Therapeutic Effect
Side Effects
Adverse Effects
Toxic Effect
Idiosyncratic Reactions
Allergic Reaction
Medication Interactions
Iatrogenic Response
54.
Therapeutic Effect• The expected or
predictable
physiological response
a medication causes
• A single med can have
several therapeutic
effects (Aspirin)
• It is important for the
nurse to know why
med is being prescribed
55.
Side Effects• Unintended secondary
effects a medication
predictably will cause
• May be harmless or serious
• If side effects are serious
enough to negate the
beneficial effect of meds
therapeutic action, it may
be D/C’d
• People may stop taking
medications because of the
side effects
56.
Adverse Effects• Undesirable response of a
medication
• Unexpected effects of drug
not related to therapeutic
effect
• Must be reported to FDA
• Can be a side effect or a
harmful effect
• Can be categorized as
pharmacologic,
idiosyncratic,
hypersensitivity, or drug
interaction
57.
Adverse Effects• Adverse Drug Events
• Adverse Drug
Reactions (ADR)
58.
Toxic Effect• May develop after
prolonged intake or when
a med accumulates in the
blood because of impaired
metabolism or excretion, or
excessive amount taken
• Toxic levels of opioids can
cause resp.depression
• Antidotes available to
reverse effects
59.
IdiosyncraticReactions
• Unpredictable effectsoverreacts or under reacts
to a medication or has a
reaction different from
normal
• Genetically determined
abnormal response
• Idiosyncratic drug
reactions are usually
caused by abnormal levels
of drug-metabolizing
enzymes (deficiency or
overabundance)
60.
Allergic Reaction• Unpredictable response to
a medication
• Makes up greater than 10%
of all medication reactions
• Client may become
sensitized immunologically
to the initial dose, repeated
administration causes an
allergic response to the
med, chemical preservative
or a metabolite
61.
Allergic Reaction• Medication acts as an
antigen triggering the
release of the body’s
antibodies
• May be mild or severe
• Among the different
classes of meds, antibiotics
cause the highest incidence
of allergic reaction
• Severe reactionAnaphylactic reaction
• Mild reaction-hives, rash,
pruritis
62.
63.
64.
• 2. A postoperative client is receiving morphine sulfate via aPCA. The nurse assesses that the client’s respirations are
depressed. The effects of the morphine sulfate can be classified
as:
• A. Allergic
• B. Idiosyncratic
• C. Therapeutic
• D. Toxic
35 - 59
65.
Other DrugReactions
• Teratogenic-Structural
effect in unborn fetus
(thalidomide)
• Carcinogenic-Causes
cancer
• Mutagenic- Changes
genetic composition
(radiation, chemicals)
66.
DrugInteractions
• Occurs when one med
modifies the action of
another
• Common in people
taking several
medications at once
• One med may
potentiate or diminish
the action of another or
alter the way it is
absorbed, metabolized
or eliminated
• Warfarin and
Amiodarone
67.
IatrogenicResponses
• Unintentional adverse
effects that occur during
therapy
• Treatment-Induced
Dermatologic-rash, hives,
acne
• Renal DamageAminoglycoside
antibiotics,
NSAIDS,
contrast medium
• Blood DyscrasiasDestruction of blood cells
(Chemotherapy)
• Hepatic Toxicity-Elevated
liver enzymes (hepatitislike symptoms)
68.
SynergisticEffect
• Effect of 2 meds combined
is greater than the meds
given separately
• Alcohol & Antihistamines,
antidepressants,
barbiturates, narcotics
• Not always undesirable,
physician may combine
meds to create an
interaction that will have
beneficial effects
(Vasodilators & diuretics to
control high BP)
69.
Medication DoseResponses
• Except when administered
IV, meds take time to enter
bloodstream
• The quantity & distribution
of med in different body
compartments change
constantly
• Goal is to keep constant
blood level within a safe
therapeutic range
• Repeated doses are
required to achieve a
constant therapeutic
concentration of a med
because a portion of med is
always being excreted
70.
Medication DoseResponses
• Serum Half-Life:Time it
takes for excretion
processes to lower the
serum medication
concentration by ½
• Regular fixed doses must
be given to maintain
therapeutic concentration
• Dosage schedules set by
institutions (TID, q8h, HS,
AC, STAT, PRN)
• Peak & Trough levels
• Therapeutic drug
monitoring
71.
Half-life• The time it takes for one
half of the original amount
of a drug in the body to be
removed
• A measure of the rate at
which drugs are removed
from the body
72. Onset
Onset, Peak, andDuration
Onset
• The time it takes for the drug
to elicit a
therapeutic response
Peak
• The time it takes for a drug
to reach its
maximum
therapeutic response
Duration
• The time a drug
concentration is sufficient to
elicit a therapeutic response
73. Pharmacotherapeutics: Types of
TherapiesAcute therapy
Maintenance therapy
Supplemental therapy
Palliative therapy
Supportive therapy
Prophylactic therapy
Empiric therapy
74.
Monitoring• The effectiveness of the
drug therapy must be
evaluated
• One must be familiar
with the drug’s:
– Intended therapeutic
action (beneficial)
– Unintended but
potential side effects
(predictable, adverse
reactions)
75.
Monitoring(cont'd)
• Therapeutic index
– The ratio between a
drug’s therapeutic
benefits and its toxic
effects
76.
Monitoring(cont'd)
• Tolerance
– A decreasing response to
repetitive drug doses
77.
Monitoring(cont'd)
• Dependence
– A physiologic or
psychological need for a
drug
78. Interactions may occur with other drugs or food
Monitoring(cont'd)
Interactions may occur
with other drugs or food
•Drug interactions: the
alteration of action of
a drug by:
– Other prescribed drugs
– Over-the-counter
medications
– Herbal therapies
79.
Monitoring(cont'd)
• Drug interactions
– Additive effect
– Synergistic effect
– Antagonistic effect
– Incompatibility
80.
Monitoring(cont'd)
• Medication
misadventures
– Adverse drug events
– Adverse drug reactions
– Medication errors
81. Some adverse drug reactions are classified as side effects
Monitoring(cont'd)
Some adverse drug
reactions are classified
as side effects
• Expected, well-known
reactions that result in little
or no change in patient
management
• Predictable frequency
• The effect’s intensity and
occurrence are related to
the size of the dose
82. An adverse outcome of drug therapy in which a patient is harmed in some way
Adverse DrugReaction
Pharmacologic reactions
Idiosyncratic reactions
Hypersensitivity reactions
Drug interactions
83.
Other DrugRelated Effects• Teratogenic
• Mutagenic
• Carcinogenic
84. The study of poisons and unwanted responses to therapeutic agents
ToxicologyThe study of poisons
and unwanted
responses to
therapeutic agents
85.
86. The Nursing Process (cont'd)
• Assessment• Nursing diagnosis
• Planning (with outcome
criteria)
• Implementation
• Evaluation
87.
The NursingProcess
• An
organizational
framework for the
practice of nursing
• Orderly, systematic
• Central to all nursing
care
• Encompasses all steps
taken by the nurse in
caring for a patient
• Flexibility is important
88. Assessment
The NursingProcess (cont'd)
Assessment
• Data collection
– Subjective, objective
– Data collected on the patient,
drug, environment
Medication history
Nursing assessment
Physical assessment
Data analysis
89. Nursing diagnosis
The NursingProcess (cont'd)
Nursing diagnosis
• Judgment or conclusion
about the
need/problem (actual
or at risk for) of the
patient
• Based upon an accurate
assessment
• NANDA format
90. Planning
The NursingProcess (cont'd)
Planning
• Identification of goals
and outcome criteria
• Prioritization
• Time frame
91. Goals
The NursingProcess (cont'd)
Goals
Objective, measurable,
realistic
• Time frame specified
Outcome criteria
Specific standard(s) of
measure
• Patient oriented
92. Implementation
The NursingProcess (cont'd)
Implementation
• Initiation and completion
of the nursing care plan
as defined by the nursing
diagnoses and outcome
criteria
• Follow the “five rights” of
medication
administration
93. The “Five Rights”
Right drug
Right dose
Right time
Right route
Right patient
94. Another “Right”—Constant System Analysis
• A “double-check”• The entire “system” of
medication
administration
• Ordering, dispensing,
preparing, administering,
documenting
• Involves the physician,
nurse, nursing unit,
pharmacy department,
and patient education
95.
Other “Rights”• Proper drug storage
• Proper documentation
• Accurate dosage
calculation
• Accurate dosage
preparation
• Careful checking of
transcription of
orders
• Patient safety
96.
Other “Rights”(cont'd)
• Close consideration of
special situations
• Prevention and
reporting of medication
errors
• Patient teaching
• Monitoring for
therapeutic effects, side
effects, toxic effects
• Refusal of medication
97.
Evaluation• Ongoing part of the
nursing process
• Determining the status
of the goals and
outcomes of care
• Monitoring the
patient’s response to
drug therapy
– Expected and unexpected
responses
98.
The day shift charge nurse is making rounds. Apatient tells the nurse that the night shift nurse
never gave him his medication, which was due at
11 PM. What should the nurse do first to
determine whether the medication was given?
1.Call the night nurse at home.
2.Check the Medication Administration Record.
3.Call the pharmacy.
4.Review the nurse’s notes.
99.
The patient’s Medication Administration Recordlists two antiepileptic medications that are due at
0900, but the patient is NPO for a barium study.
The nurse’s coworker suggests giving the
medications via IV because the patient is NPO.
What should the nurse do?
1.Give the medications PO with a small sip of
water.
2.Give the medications via the IV route because
the patient is NPO.
3.Hold the medications until after the test is
completed.
4.Call the physician to clarify the instructions.
100. Life Span Considerations
101.
Life SpanConsiderations
Pregnancy
Breast-feeding
Neonatal
Pediatric
Geriatric
102.
Pregnancy• First trimester is the
period of greatest
danger for druginduced developmental
defects
• Drugs diffuse across the
placenta
• FDA pregnancy safety
categories
103.
Table 3-1Pregnancy safety
categories
104.
Breast-feeding• Breast-fed infants are at
risk for exposure to
drugs consumed by the
mother
• Consider risk-to-benefit
ratio
105.
Table 3-2 Classification ofyoung patients
106. Pediatric Considerations: Pharmacokinetics
• Absorption– Gastric pH less acidic
– Gastric emptying is
slowed
– Topical absorption faster
through the skin
– Intramuscular
absorption faster and
irregular
107. Pediatric Considerations: Pharmacokinetics (cont'd)
• Distribution– TBW 70% to 80% in fullterm infants, 85% in
premature newborns, 64%
in children 1 to 12 years
of age
– Greater TBW means fat
content is lower
– Decreased level of protein
binding
– Immature blood-brain
barrier
108. Pediatric Considerations: Pharmacokinetics (cont'd)
• Metabolism– Liver immature, does
not produce enough
microsomal enzymes
– Older children may have
increased metabolism,
requiring higher doses
– Other factors
109. Pediatric Considerations: Pharmacokinetics (cont'd)
• Excretion– Kidney immaturity
affects glomerular
filtration rate and
tubular secretion
– Decreased perfusion rate
of the kidneys
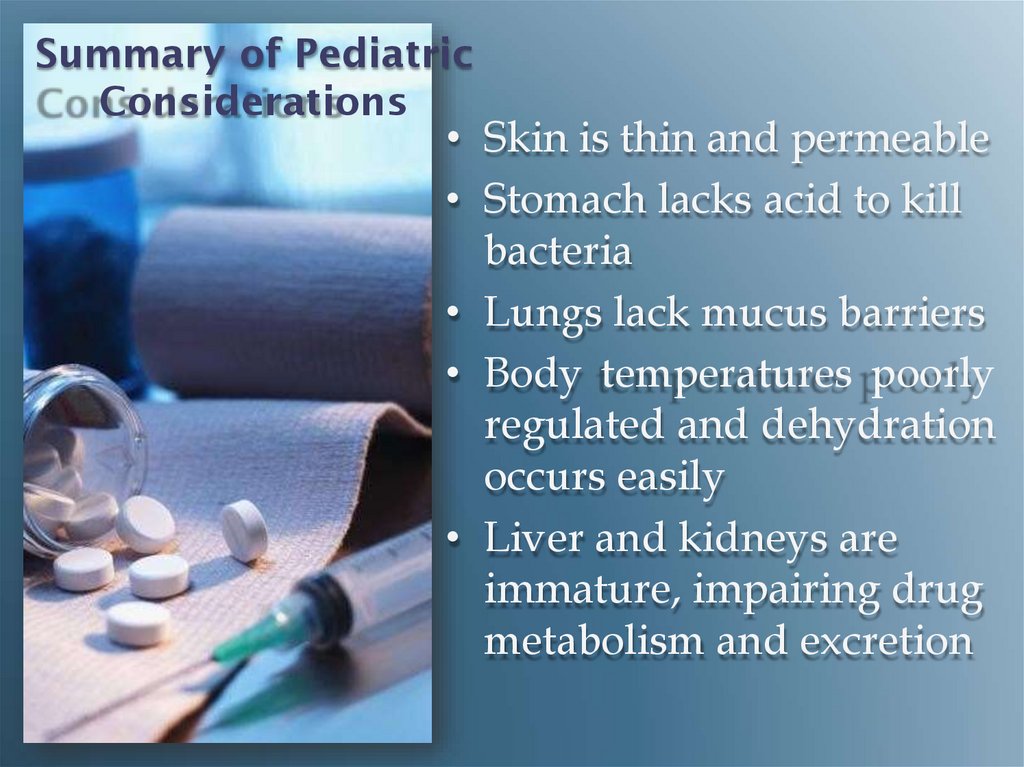
110. Summary of Pediatric Considerations
• Skin is thin and permeable• Stomach lacks acid to kill
bacteria
• Lungs lack mucus barriers
• Body temperatures poorly
regulated and dehydration
occurs easily
• Liver and kidneys are
immature, impairing drug
metabolism and excretion
111.
Methods of Dosage Calculation forPediatric Patients
•Body weight dosage calculations
•Body surface area method
112.
GeriatricConsiderations
• Geriatric: older than
age 65
– Healthy People 2010:
older than age 55
• Use of OTC
medications
• Polypharmacy
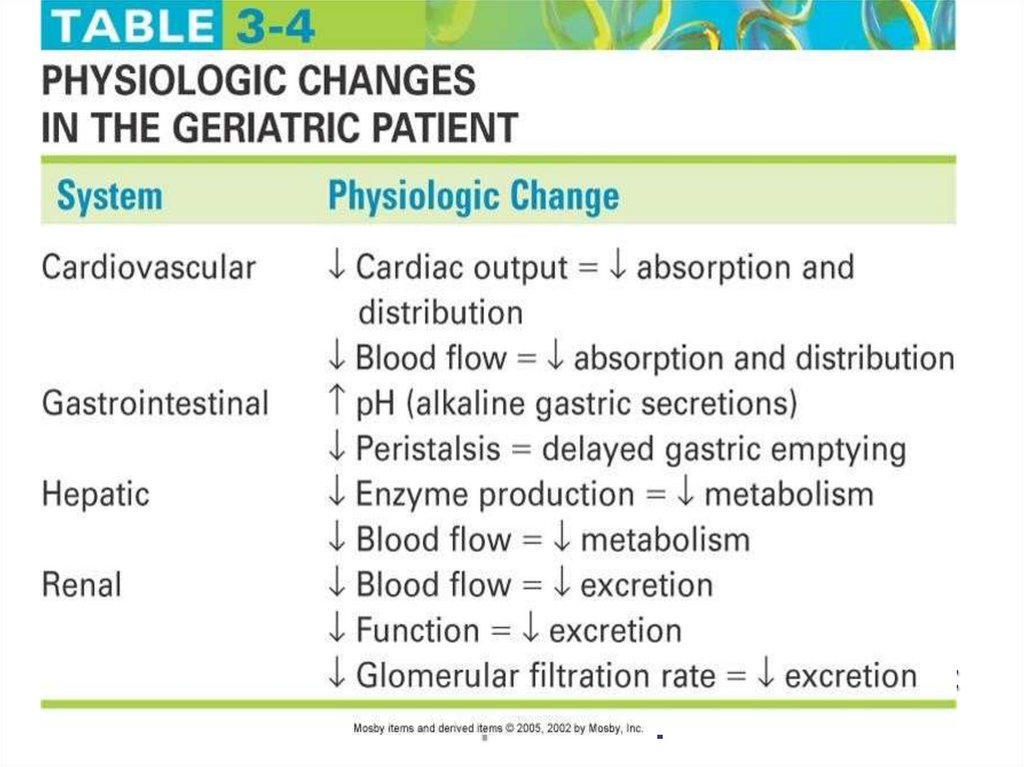
113. Table 3-4 Physiologic changes in the geriatric patient
114. Geriatric Considerations: Pharmacokinetics
• Absorption– Gastric pH less acidic
– Slowed gastric emptying
– Movement through GI
tract slower
– Reduced blood flow to the
GI tract
– Reduced absorptive
surface area due to
flattened intestinal villi
115. Geriatric Considerations: Pharmacokinetics (cont'd)
• Distribution– TBW percentages lower
– Fat content increased
– Decreased production of
proteins by the liver,
resulting in decreased
protein binding of drugs
116. Geriatric Considerations: Pharmacokinetics (cont'd)
• Metabolism– Aging liver produces
less microsomal
enzymes, affecting drug
metabolism
– Reduced blood flow to
the liver
117. Geriatric Considerations: Pharmacokinetics (cont'd)
• Excretion– Decreased glomerular
filtration rate
– Decreased number of
intact nephrons
118.
Geriatric Considerations: ProblematicMedications
•Analgesics
•Anticoagulants
•Anticholinergics
•Antihypertensives
•Digoxin
•Sedatives and hypnotics
•Thiazide diuretics
119. Legal, Ethical, and Cultural Considerations
120.
U.S. DrugLegislation
• 1906: Federal Food and
Drug Act
• 1912: Sherley
Amendment (to the
Federal Food and Drug
Act of 1906)
• 1914: Harrison Narcotic
Act
• 1938: Federal Food,
Drug, and Cosmetic Act
(revision of 1906 Act)
121. U.S. Drug Legislation (cont'd)
• 1951: DurhamHumphreyAmendment (to the
1938 act)
• 1962: Kefauver-Harris
Amendment (to the
1938 act)
• 1970: Controlled
Substance Act
122. U.S. Drug Legislation (cont'd)
• 1983: Orphan Drug Act• 1991: Accelerated drug
approval
123.
124.
125.
New DrugDevelopment
• Investigational new
drug (IND) application
• Informed consent
• Investigational drug
studies
• Expedited drug
approval
126. U.S. FDA Drug Approval Process
• Preclinicalinvestigational drug
studies
• Clinical phases of
investigational drug
studies
– Phase I
– Phase II
– Phase III
– Phase IV
127.
Ethical NursingPractice
• American Nurses
Association (ANA)
Code of Ethics for
Nurses
128.
Cultural Considerations•Assess the influence of a patient’s cultural
beliefs, values, and customs
•Drug polymorphism
•Compliance level with therapy
•Environmental considerations
•Genetic factors
•Varying responses to specific agents
129.
CulturalAssessment
• Health beliefs and
practices
• Past uses of medicine
• Folk remedies
• Home remedies
• Use of nonprescription
drugs and herbal
remedies
• OTC treatments
130.
Cultural Assessment (cont'd)•Usual response to treatment
•Responsiveness to medical treatment
•Religious practices and beliefs
•Dietary habits
131.
MedicationErrors:
Preventing
and
Responding
132.
MedicationMisadventures
• Medication errors
(MEs)
• Adverse drug events
(ADEs)
• Adverse drug reactions
(ADRs)
133.
Medication Misadventures (cont'd)•By definition, all ADRs are also ADEs
•But all ADEs are not ADRs
•Two types of ADRs
– Allergic reactions
– Idiosyncratic reactions
134. Medication Errors
• Preventable• Common cause of
adverse health care
outcomes
• Effects can range from no
significant effect to
directly causing disability
or death
135. Box 5-1 Common classes of medications involved in serious errors
136.
Preventing Medication Errors•Minimize verbal or telephone orders
– Repeat order to prescriber
– Spell drug name aloud
– Speak slowly and clearly
•List indication next to each order
•Avoid medical shorthand, including
abbreviations and acronyms
137.
PreventingMedication Errors
(cont'd)
• Never assume anything
about items not specified in
a drug order (i.e., route)
• Do not hesitate to question
a medication order for any
reason when in doubt
• Do not try to decipher
illegibly written orders;
contact prescriber for
clarification
138. Preventing Medication Errors (cont'd)
• NEVER use “trailingzeros” with medication
orders
• Do not use 1.0 mg; use
1 mg
• 1.0 mg could be
misread as 10 mg,
resulting in a tenfold
dose increase
139.
PreventingMedication Errors
(cont'd)
• ALWAYS use a
“leading zero” for
decimal dosages
• Do not use .25 mg; use
0.25 mg
• .25 mg may be misread
as 25 mg
• “.25” is sometimes
called a “naked
decimal”
140.
Preventing Medication Errors (cont'd)•Check medication order and what is available
while using the “5 rights”
•Take time to learn special administration
techniques of certain dosage forms
141. Preventing Medication Errors (cont'd)
• Always listen to andhonor any concerns
expressed by patients
regarding medications
• Check patient allergies
and identification
• Medication
Reconciliation
142. Medication Errors
• Possible consequences tonurses
• Reporting and responding to
MEs
– ADE monitoring programs
– USPMERP (United States
Pharmacopeia Medication
Errors Reporting Program)
– MedWatch, sponsored by the
FDA
– Institute for Safe Medication
Practices (ISMP)
• Notification of patient
regarding MEs
143.
• 3. Nurses are legally required to document medications thatare administered to clients. The nurse is mandated to document:
• A. Medication before administering it
• B. Medication after administering it
• C. Rationale for administering the medication
• D. Prescriber’s rationale for prescribing the medication
35 - 138
144.
• 4. If a nurse experiences a problem reading a physician’smedication order, the most appropriate action will be to:
• A. Call the physician to verify the order.
• B. Call the pharmacist to verify the order.
• C. Consult with other nursing staff to verify the order.
• D. Withhold the medication until the physician makes
rounds.
35 - 139
145. Medication Administration
146.
147.
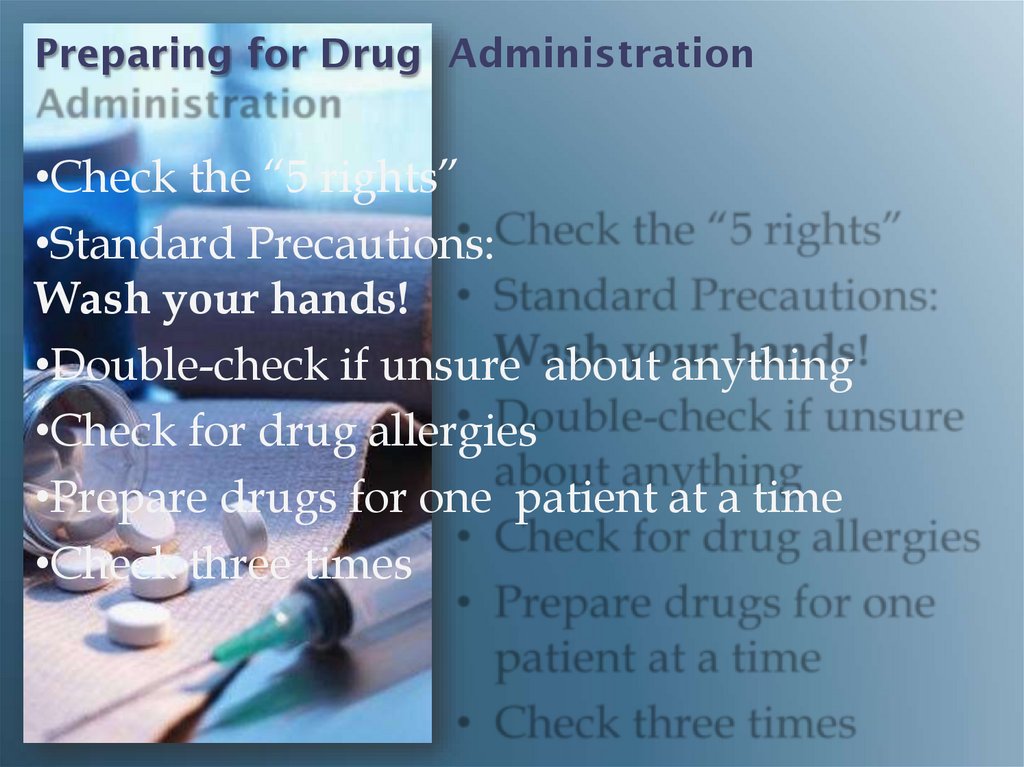
Preparing for Drug Administration•Check the “5 rights”
•Standard Precautions:
Wash your hands!
•Double-check if unsure about anything
•Check for drug allergies
•Prepare drugs for one patient at a time
•Check three times
148.
Preparing for DrugAdministration
(cont'd)
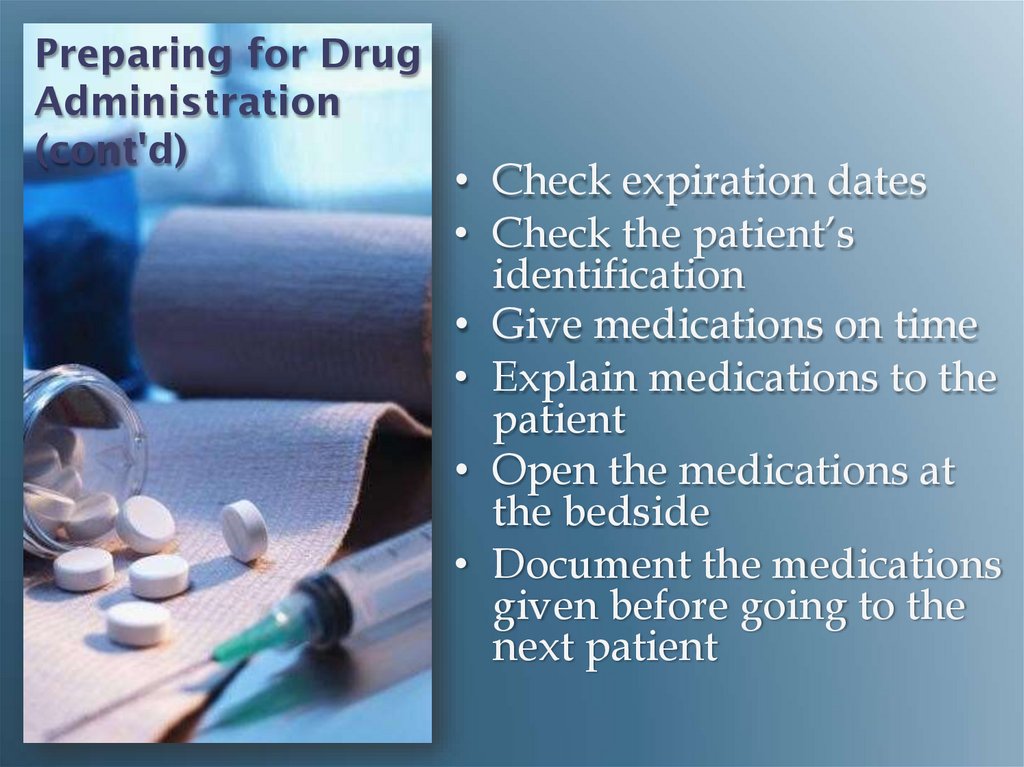
• Check expiration dates
• Check the patient’s
identification
• Give medications on time
• Explain medications to the
patient
• Open the medications at
the bedside
• Document the medications
given before going to the
next patient
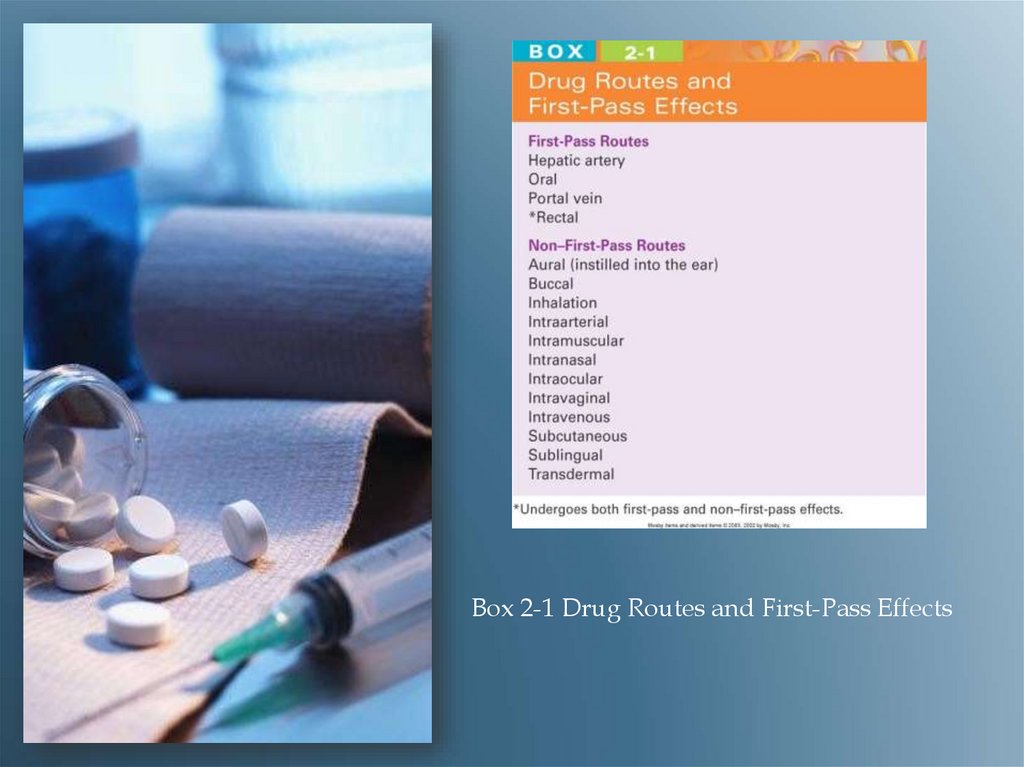
149.
Drug Routes &First Pass Effects
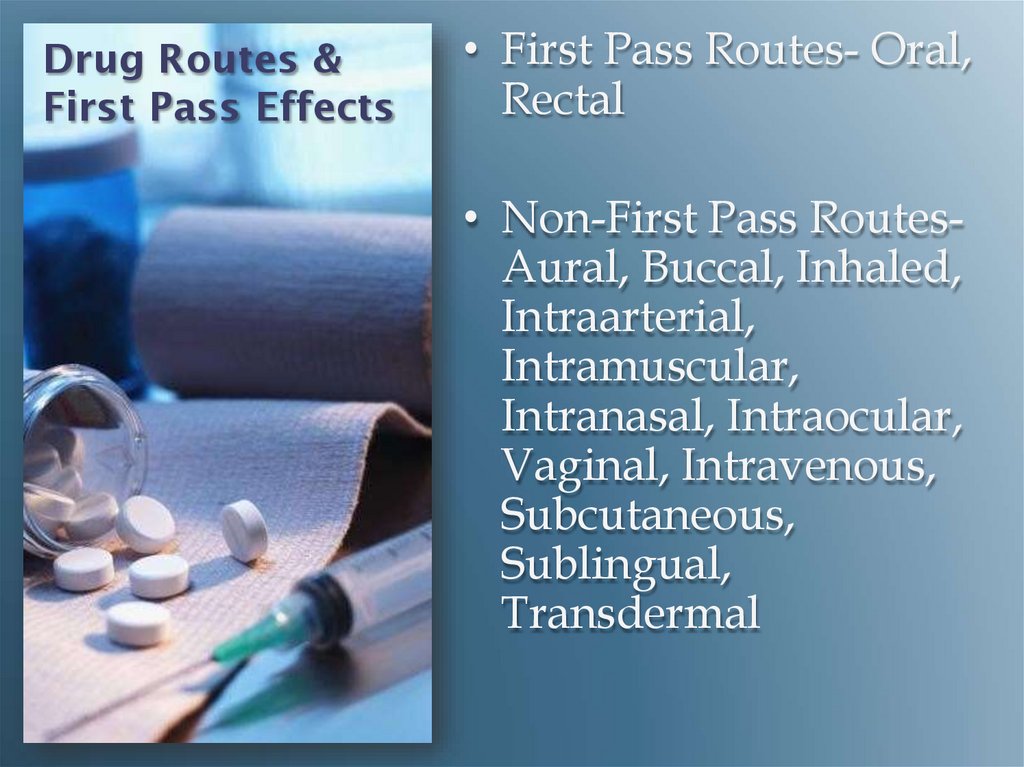
• First Pass Routes- Oral,
Rectal
• Non-First Pass RoutesAural, Buccal, Inhaled,
Intraarterial,
Intramuscular,
Intranasal, Intraocular,
Vaginal, Intravenous,
Subcutaneous,
Sublingual,
Transdermal
150.
Oral Route• Easiest, most
commonly used
• Slower onset of action
• More prolonged effect
• Preferred by clients
• Sublingual
Administration
• Buccal Administration
151.
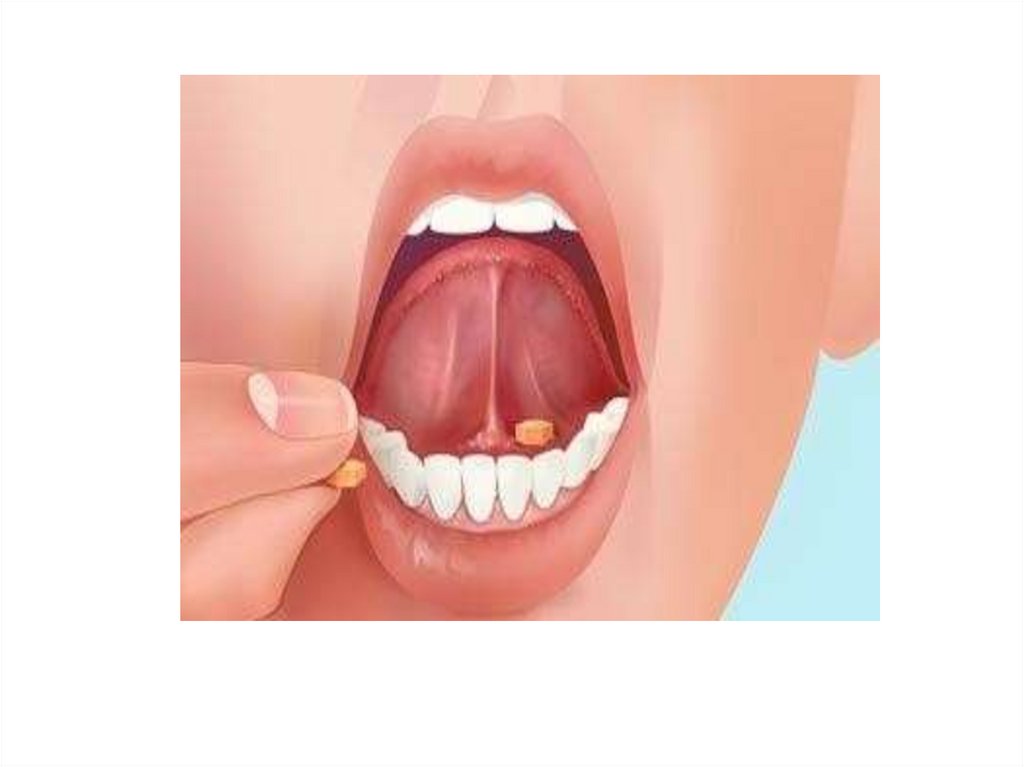
152. Enteral Drugs
• Giving oral medications• Giving sublingual or buccal
medications
• Liquid medications
• Giving oral medications to
infants
• Administering drugs
through a nasogastric or
gastrostomy tube
• Rectal administration
153. Injecting a medication into body tissues
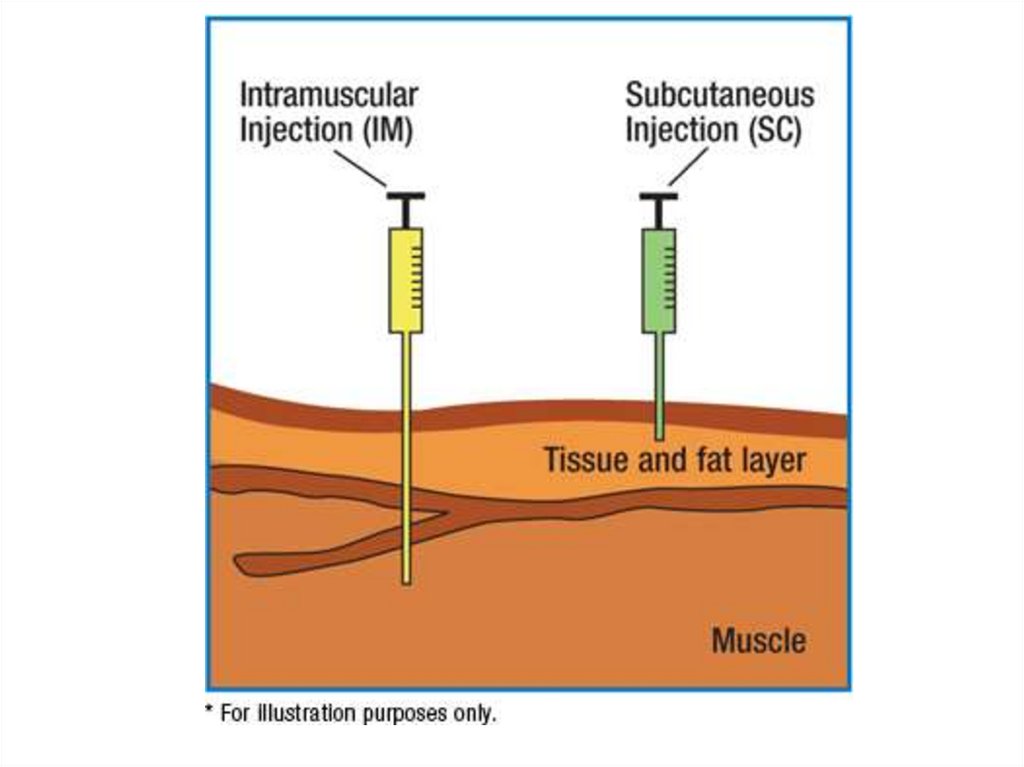
Parenteral RouteInjecting a medication
into body tissues
Subcutaneous (SQ)
Intramuscular (IM)
Intravenous (IV)
Intradermal (ID)
Advanced techniques
154.
ParenteralDrugs
• Never recap a used
needle!
• May recap an unused
needle with the “scoop
method”
• Prevention of
needlesticks
• Filter needles
155. Parenteral Drugs (cont'd)
• Removing medicationsfrom ampules
• Removing medications
from vials
• Disposal of used
needles and syringes
156.
Injections• Needle angles for
various injections
– Intramuscular (IM)
– Subcutaneous (SC or SQ)
– Intradermal (ID)
• Z-track method for IM
injections
• Air-lock technique
157.
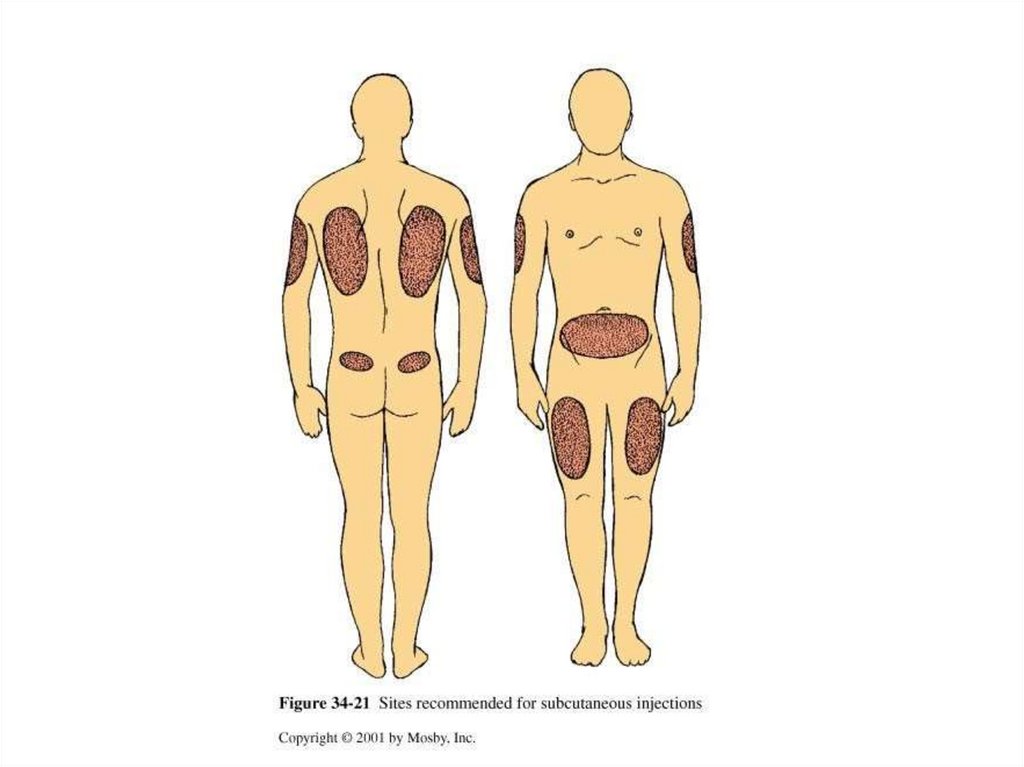
InjectionTechniques
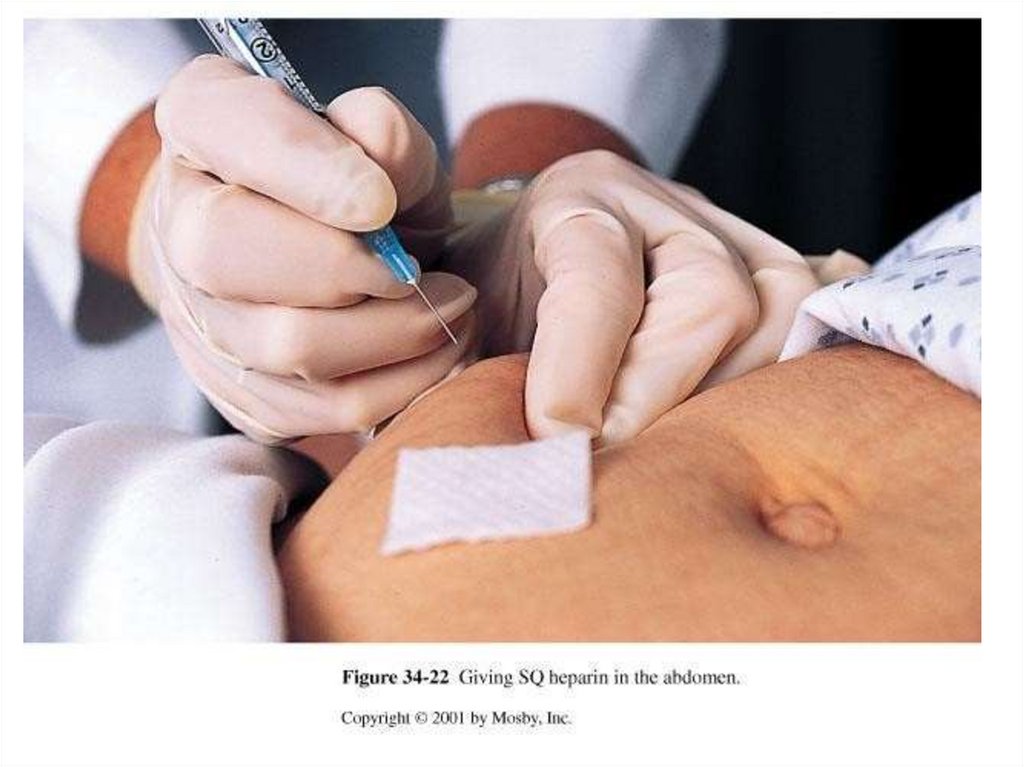
• Intradermal injections
• Subcutaneous injections
– Insulin administration
– Heparin administration
158.
159.
160.
161.
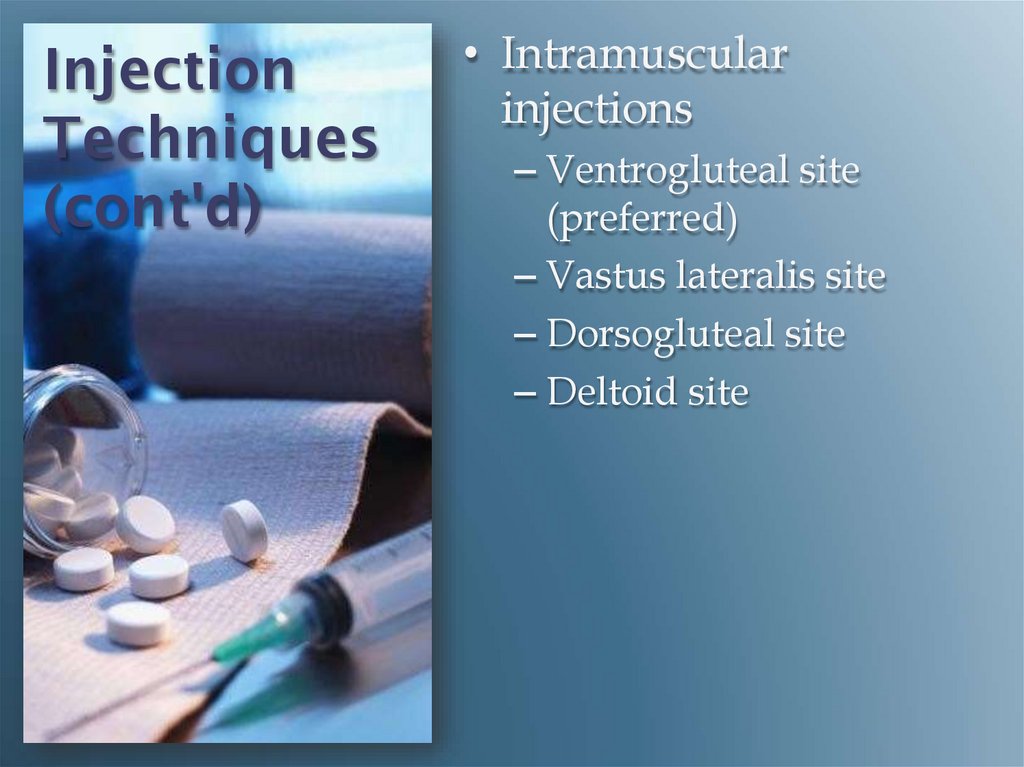
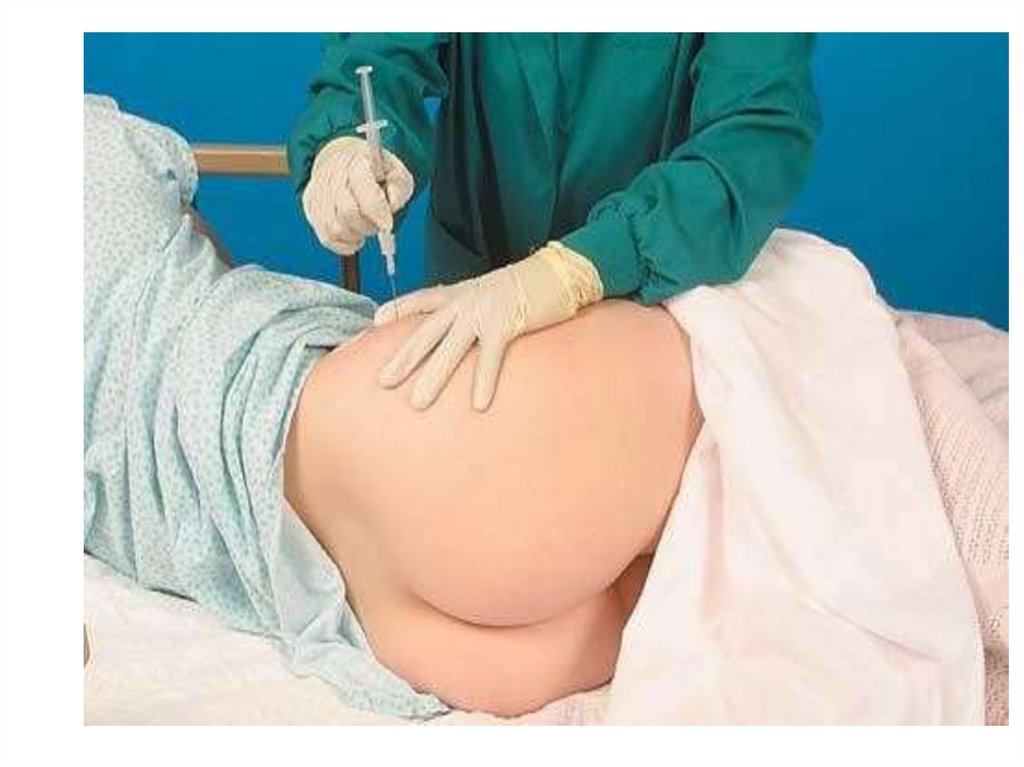
InjectionTechniques
(cont'd)
• Intramuscular
injections
– Ventrogluteal site
(preferred)
– Vastus lateralis site
– Dorsogluteal site
– Deltoid site
162.
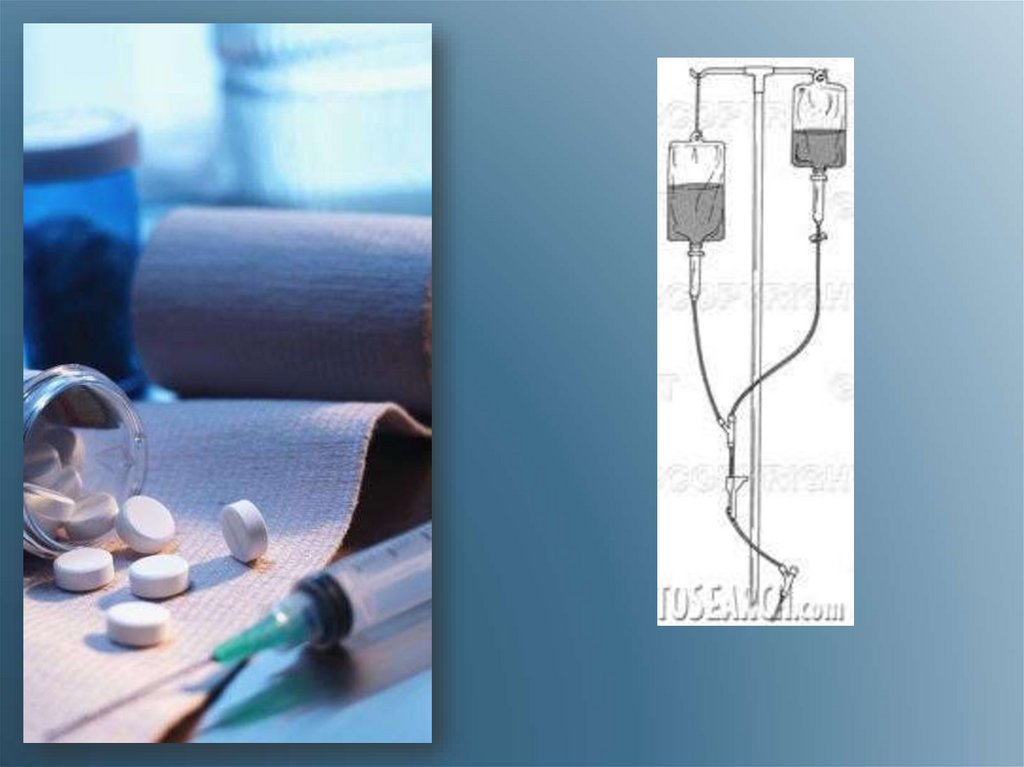
163. Preparing Intravenous Medications
Needleless systemsCompatibility issues
Expiration dates
Mixing intravenous
piggyback (IVPB)
medications
• Labeling intravenous (IV)
infusion bags when
adding medications
164.
165.
166. Intravenous Medications
• Adding medications to aprimary infusion bag
• IVPB medications
(secondary line)
• IV push medications
(bolus)
– Through an IV lock
– Through an existing IV
infusion
167.
168.
169. Intravenous Medications (cont'd)
• Volume-controlledadministration set
• Using electronic
infusion pumps
• Patient-controlled
analgesia (PCA) pumps
170.
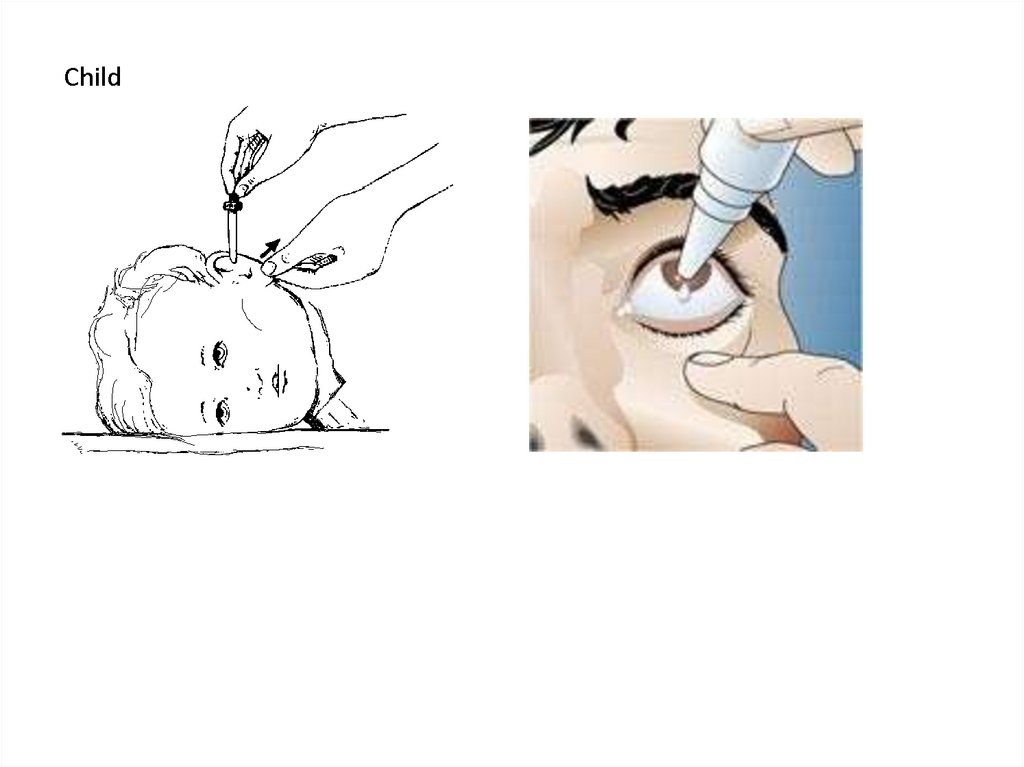
171. Topical Drugs
• Eye medications– Drops
– Ointments
• Ear drops
– Adults
– Infant or child younger
than 3 years of age
172.
173.
TopicalDrugs
(cont'd)
• Nasal drugs
– Drops
– Spray
• Inhaled drugs
– Metered-dose inhalers
– Small-volume nebulizers
174.
175.
TopicalDrugs
(cont'd)
• Administering
medications to the skin
– Lotions, creams,
ointments, powders
– Transdermal patches
• Vaginal medications
– Creams, foams, gels
– Suppositories
























 Медицина
Медицина








