Похожие презентации:
Acute respiratory failure
1. Acute respiratory failure
2. respiratory failure.
the inability of the lungs to provide gasexchange, adequate to metabolic demands
of the body is respiratory failure.
Respiratory failure is inadequate gas exchange by the
respiratory system, with the result that levels of arterial
oxygen, carbon dioxide or both cannot be maintained
within their normal ranges
3.
respiratory failure..
РаО2 < 80 мм рт.ст. и/или
РаСО2 > 45 мм рт.ст.
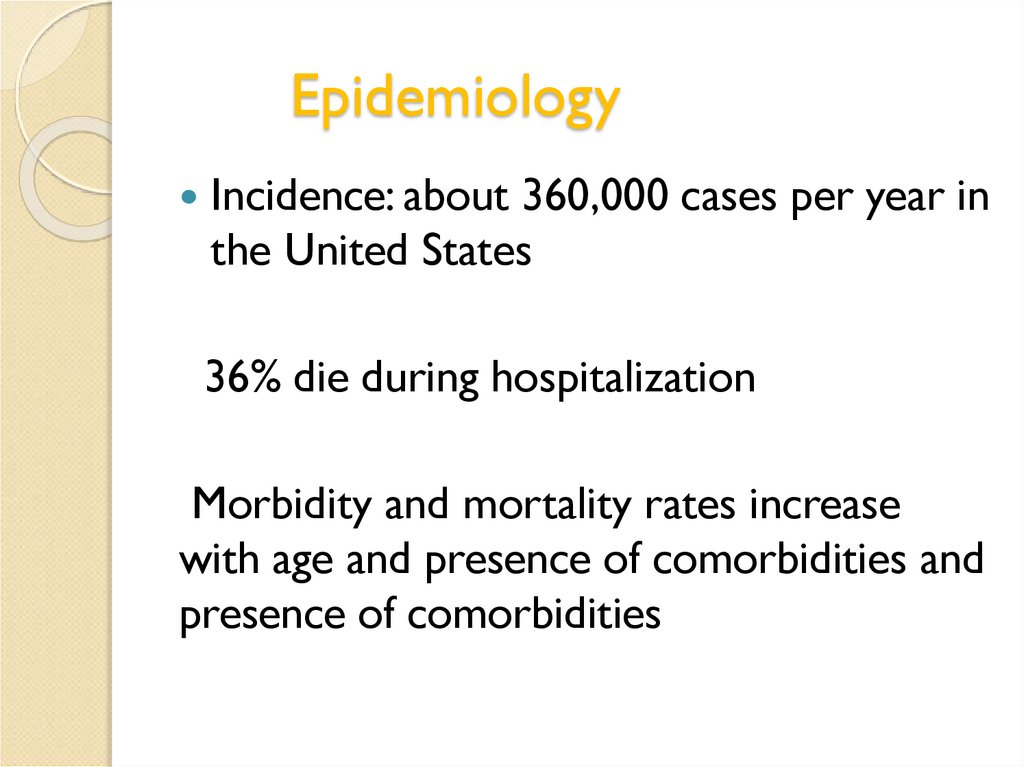
4. Epidemiology
Incidence: about 360,000 cases per year inthe United States
36% die during hospitalization
Morbidity and mortality rates increase
with age and presence of comorbidities and
presence of comorbidities
5. PATHOPHYSIOLOGY
Gas exchange between the externalenvironment and the blood has three main
mechanisms:
◦ ventilation,
◦ diffusion,
◦ perfusion.
Respiratory failure can be viewed as the
impairment one or more of these
functions.
6. Respiratory function
-External respirationthe exchange of gases between the
external environment and the alveoli of
the lungs;
-Internal respiration
transport of gases by blood from the
alveoli to the cell membrane and back;
-Тissue breathing- utilization of oxygen
and the release of carbon dioxide
7.
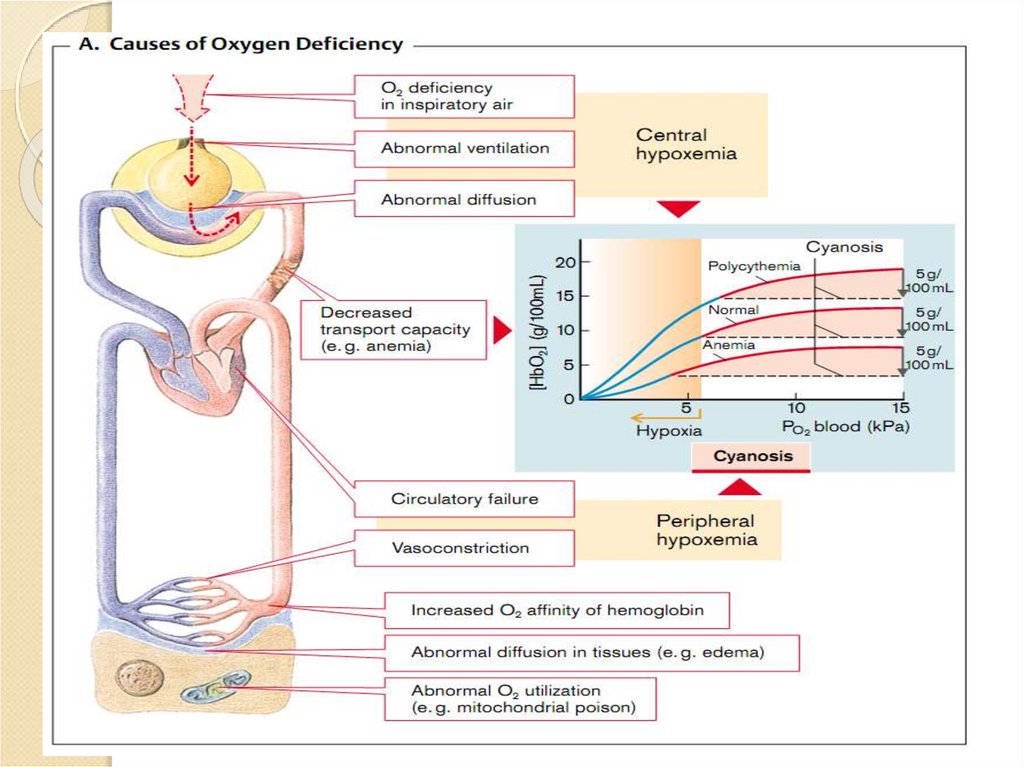
Hypoxiave forms of hypoxia:
pulmonary (hypoxic, or
espiratory)
circulatory
hemic
gistotogenous (tissue)
mixed
J.Shneerson,1995;
D.F.Rochester,1993
8.
9.
10.
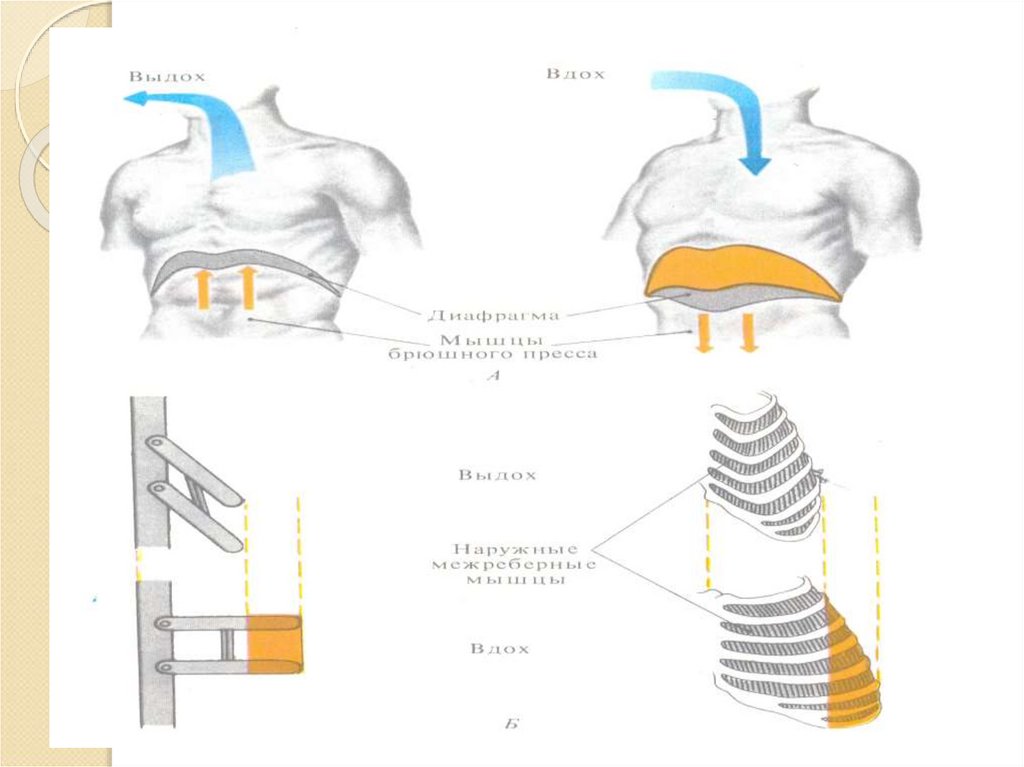
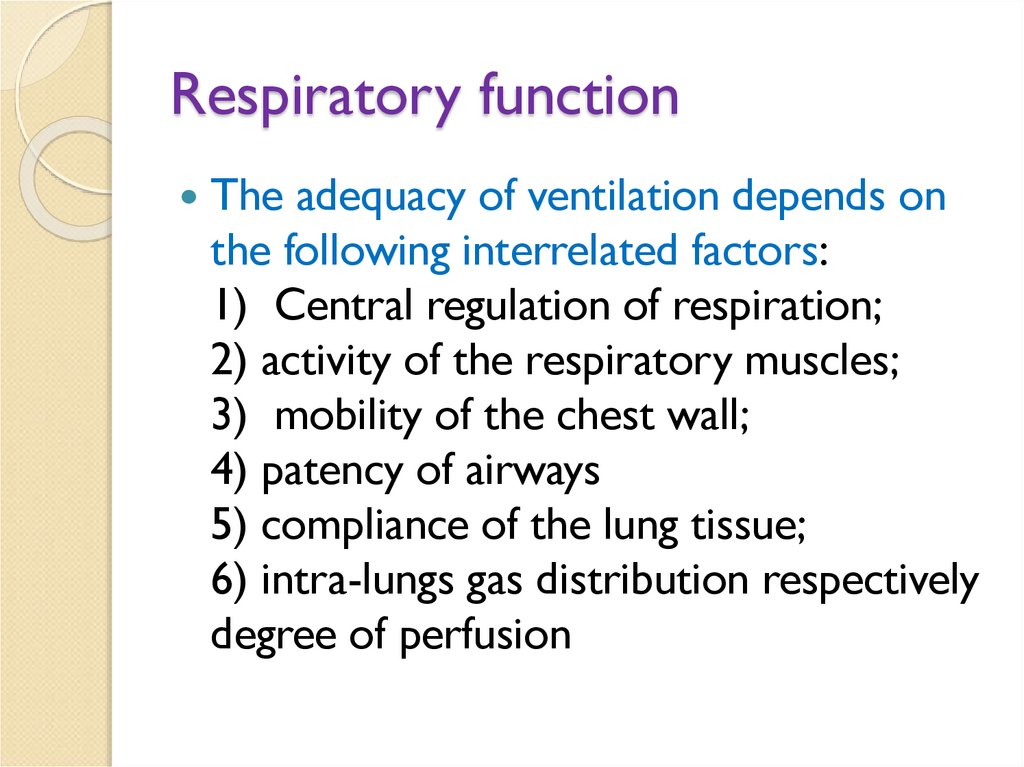
11. Respiratory function
The adequacy of ventilation depends onthe following interrelated factors:
1) Central regulation of respiration;
2) activity of the respiratory muscles;
3) mobility of the chest wall;
4) patency of airways
5) compliance of the lung tissue;
6) intra-lungs gas distribution respectively
degree of perfusion
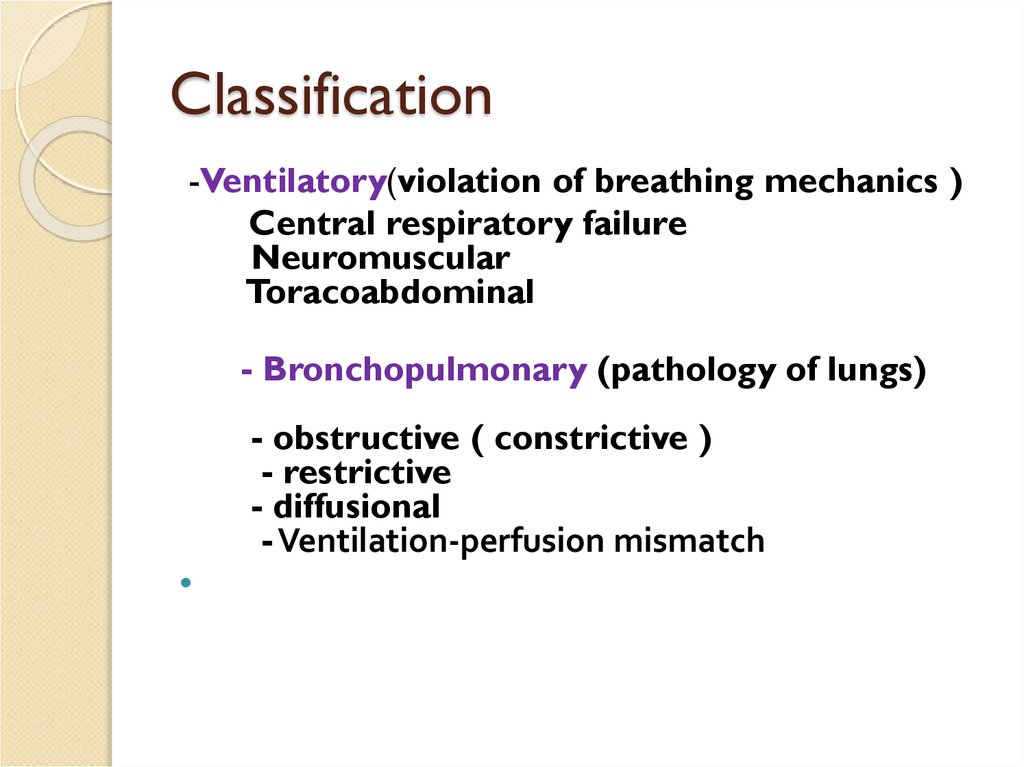
12. Classification
-Ventilatory(violation of breathing mechanics )Central respiratory failure
Neuromuscular
Toracoabdominal
- Bronchopulmonary (pathology of lungs)
- obstructive ( constrictive )
- restrictive
- diffusional
- Ventilation-perfusion mismatch
13. Classification
Primary(damage thesystem of external
breathing)
Secondary(pathology in
other systems, which
increase oxygen
demand, which cannot
be replaced by a system
of breathing)
14. Ventilatory Failure: Hypoventilation
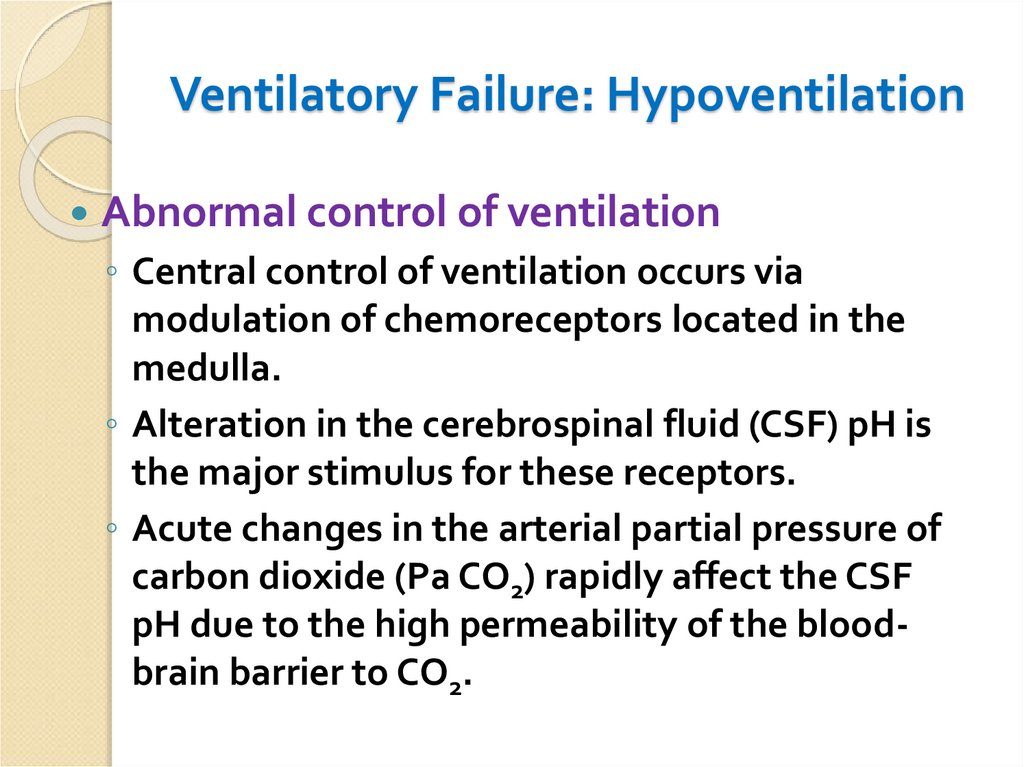
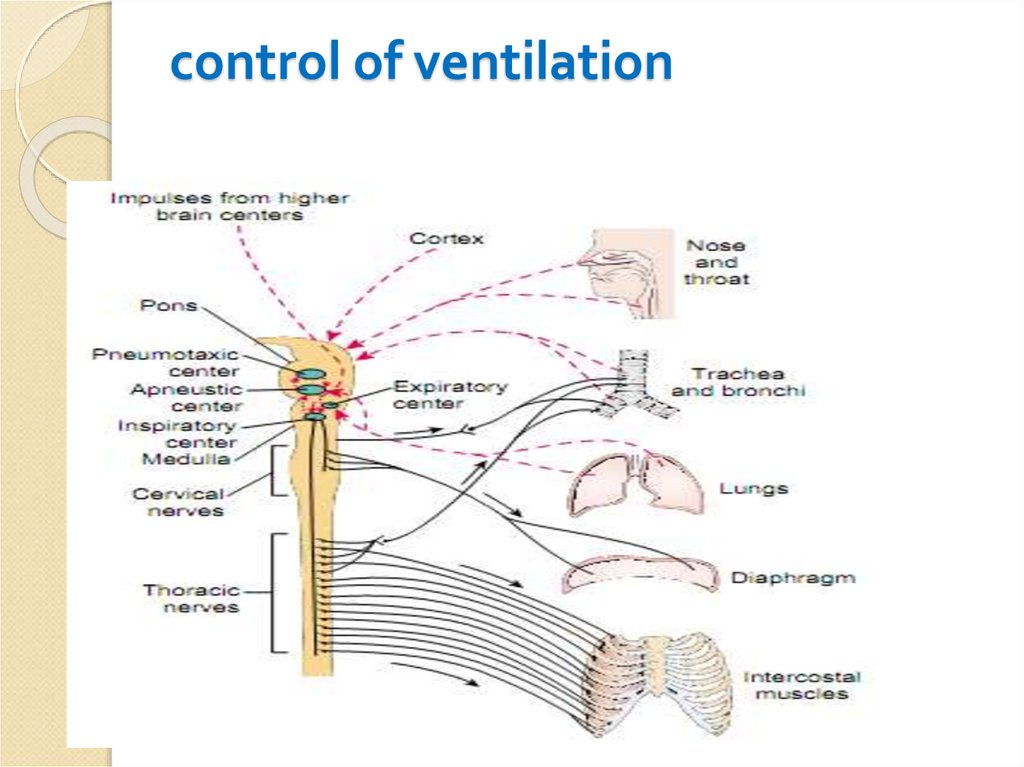
Abnormal control of ventilation◦ Central control of ventilation occurs via
modulation of chemoreceptors located in the
medulla.
◦ Alteration in the cerebrospinal fluid (CSF) pH is
the major stimulus for these receptors.
◦ Acute changes in the arterial partial pressure of
carbon dioxide (Pa CO2) rapidly affect the CSF
pH due to the high permeability of the bloodbrain barrier to CO2.
15. control of ventilation
16. Ventilatory Failure: Hypoventilation
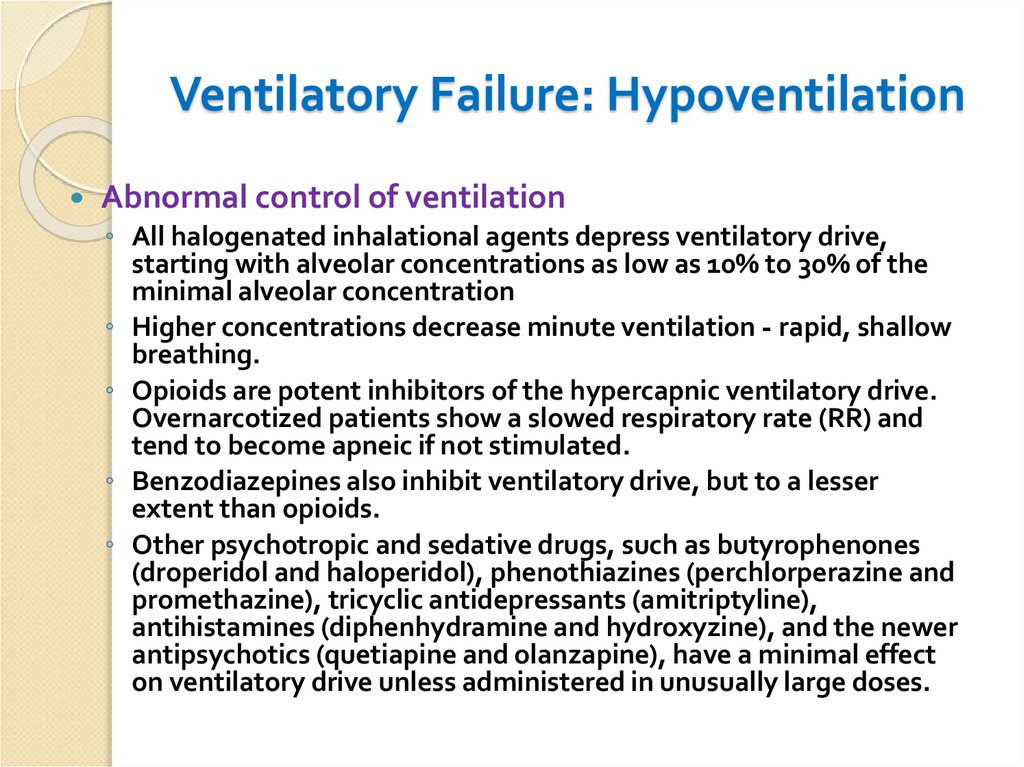
Abnormal control of ventilation◦ Peripheral chemoreceptors, located in the carotid bodies, are
sensitive to changes in the arterial partial pressure of oxygen
(PaO2) and, to a lesser extent, the PaCO2.
◦ These receptors drive the increase in alveolar ventilation that
occurs as the PaO2 decreases below 60 mm Hg.
After bilateral carotid surgery, patients may lose a significant portion of their
hypoxic ventilatory response due to mechanical disruption.
◦ If PaO2 range is normal, PaCO2 is the main determinant of
alveolar ventilation.
◦ Alveolar ventilation increases by 1 to 3 L/minute for each 1 mm Hg
increase in PaCO2.
17. Ventilatory Failure: Hypoventilation
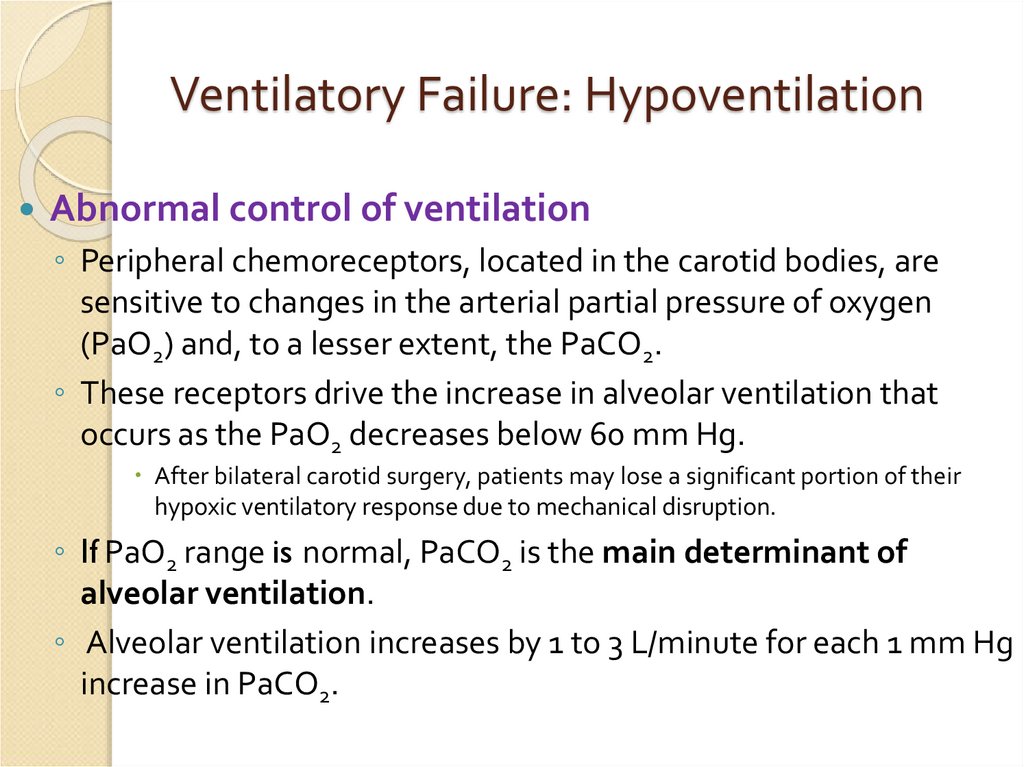
Abnormal control of ventilation◦ All halogenated inhalational agents depress ventilatory drive,
starting with alveolar concentrations as low as 10% to 30% of the
minimal alveolar concentration
◦ Higher concentrations decrease minute ventilation - rapid, shallow
breathing.
◦ Opioids are potent inhibitors of the hypercapnic ventilatory drive.
Overnarcotized patients show a slowed respiratory rate (RR) and
tend to become apneic if not stimulated.
◦ Benzodiazepines also inhibit ventilatory drive, but to a lesser
extent than opioids.
◦ Other psychotropic and sedative drugs, such as butyrophenones
(droperidol and haloperidol), phenothiazines (perchlorperazine and
promethazine), tricyclic antidepressants (amitriptyline),
antihistamines (diphenhydramine and hydroxyzine), and the newer
antipsychotics (quetiapine and olanzapine), have a minimal effect
on ventilatory drive unless administered in unusually large doses.
18. Ventilatory Failure: Hypoventilation
Abnormal control ofventilation
◦ Intracranial pathology (e.g.,
brain injury, neoplasm, or
major traumatic
cerebrovascular accidents)
that causes cerebral edema or
interrupts the vascular supply
to the medulla may affect
control of ventilation.
19. Ventilatory Failure: Hypoventilation
Neuromuscular dysfunction◦ Upper motor neuron lesions, depending on their
location, can result in variable degrees of
ventilatory dysfunction through disruption of
descending motor inputs.
intracranial or neuraxial neoplasms
strokes
demyelinating disorders
spinal anesthesia
syringomyelia
and CNS trauma
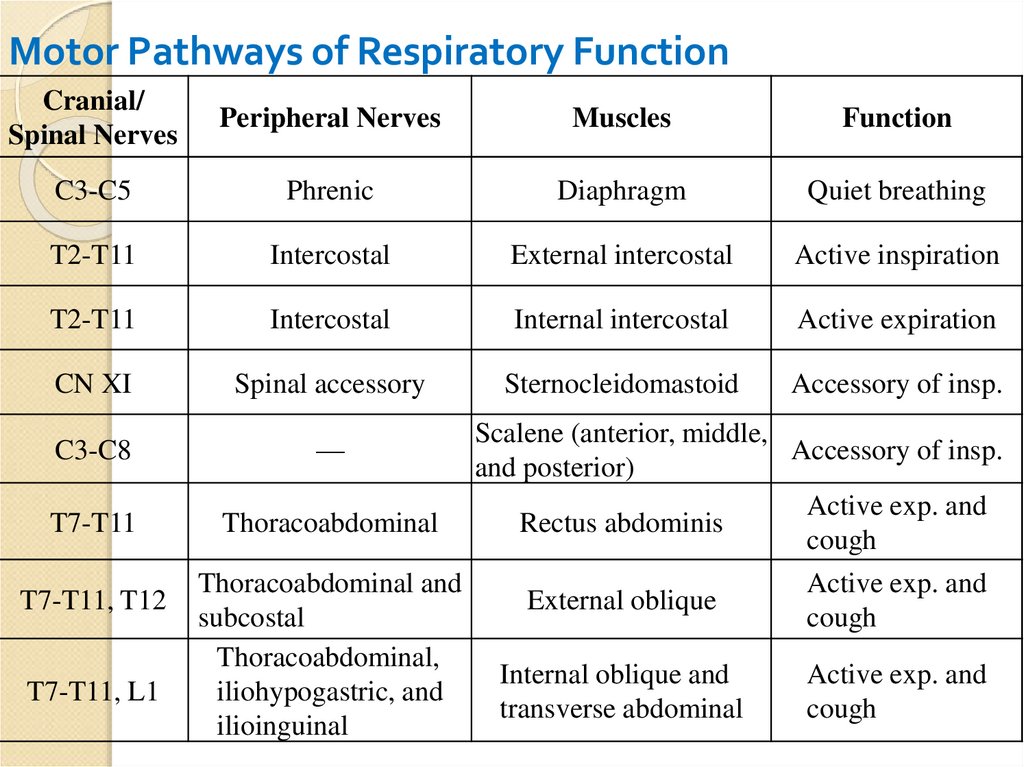
20. Motor Pathways of Respiratory Function
Cranial/Spinal Nerves
Peripheral Nerves
Muscles
Function
C3-C5
Phrenic
Diaphragm
Quiet breathing
T2-T11
Intercostal
External intercostal
Active inspiration
T2-T11
Intercostal
Internal intercostal
Active expiration
CN XI
Spinal accessory
Sternocleidomastoid
Accessory of insp.
C3-C8
—
T7-T11
Thoracoabdominal
T7-T11, T12
T7-T11, L1
Thoracoabdominal and
subcostal
Thoracoabdominal,
iliohypogastric, and
ilioinguinal
Scalene (anterior, middle,
Accessory of insp.
and posterior)
Active exp. and
Rectus abdominis
cough
External oblique
Active exp. and
cough
Internal oblique and
transverse abdominal
Active exp. and
cough
21. Ventilatory Failure: Hypoventilation
Neuromuscular dysfunction◦ Lower motor neurons supplying the
respiratory muscles may be interrupted by
trauma,
regional anesthesia
by diseases involving nerve axons or myelin
Guillain-Barré syndrome
amyotrophic lateral sclerosis
various other polyneuropathies
22. Ventilatory Failure: Hypoventilation
Neuromuscular dysfunction◦ Disorders of the neuromuscular junction
myasthenia gravis,
Eaton-Lambert syndrome
organophosphate overdose
residual neuromuscular blockade
23. Ventilatory Failure: Hypoventilation
Neuromuscular dysfunction◦ In patients who have been critically ill for prolonged
periods of time
◦ Malnutrition
◦ Infection
◦ Polyneuropathy of critical illness
24. Ventilatory Failure: Hypoventilation
Neuromuscular dysfunction◦ Respiratory muscle dysfunction
may result from any of the causes listed above
Primary myopathic processes muscular dystrophies and
myotonic dystrophy
preexisting respiratory disease may indirectly lead to muscle
dysfunction
In chronic obstructive pulmonary disease (COPD), flattening of
the diaphragm decreases its range of contraction.
Restrictive diseases of the chest wall, such as scoliosis, can
significantly alter the normal mechanics of respiratory muscles.
Transient ventilatory impairment has been documented after
upper abdominal and thoracic surgery, primarily related to
diaphragmatic dysfunction.
Although the extent of such compromise is generally limited, it
may become significant when other factors affecting ventilation
coexist.
25. obstructive respiratory failure
respiratory insufficiency develops due toobstruction of the respiratory tract inside
by foreign bodies, endophytic tumors of
the upper respiratory tract), and from
the outside (strangulation asphyxia,
compression of the trachea by the
tumor).
In obstructive respiratory failure, there is a
mechanical problem that blocks or tightens the
passage of the air. Examples of conditions that
can produce this include Asthma and Cystic
fibrosis.
26. consrtiction
respiratory failure develops due tonarrowing of the lumen of the
respiratory tract when
bronchospasm. Most often this is the
result of reflex reactions muscles of
bronchi on various irritating gases
or allergens
27. restrictive respiratory failure
In restrictive respiratory failure, thevolume of the rib cage is reduced.
An example for this is Scoliosis,
Pneumothorax and Hemothorax
28. Ventilatory Failure: Hypoventilation
Increased ventilatory load. Hypoventilation can alsooccur when the action of the respiratory muscles is
hindered by either an increased airway resistance
(Raw) or a decreased compliance of the respiratory
system (Crs).
◦ Increased Raw is commonly caused by bronchospasm,
copious bronchial secretions, compression or narrowing of
the airway, and inappropriately small endotracheal tubes
◦ Decreased Crs occurs because of pathologic processes of the
lung parenchyma (edema, pneumonia, and interstitial
fibrosis), pleura (effusions and pneumothorax), or the
musculoskeletal apparatus (kyphoscoliosis, increased intraabdominal pressure, and active splinting from pain).
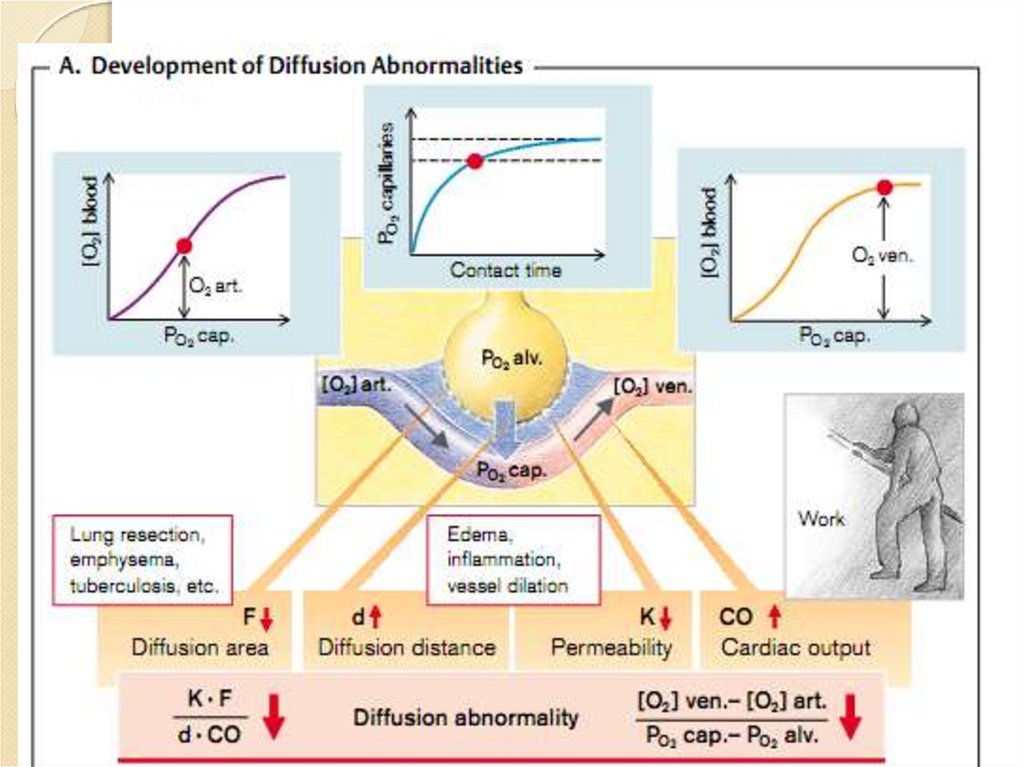
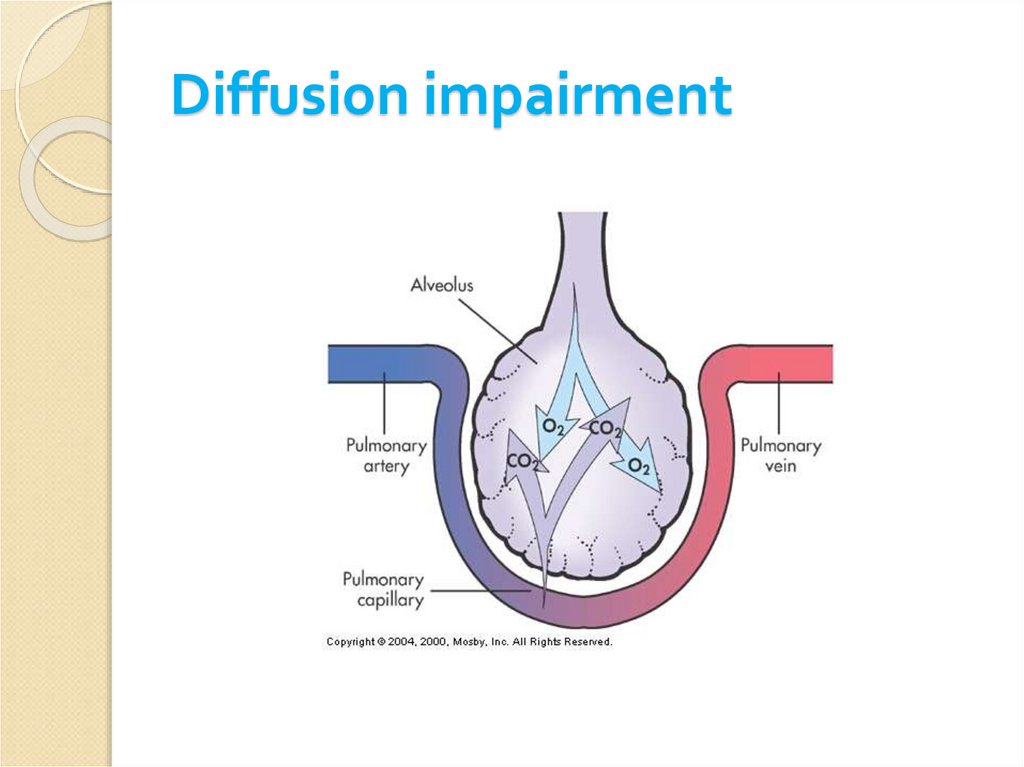
29. Diffusion impairment
uncommon because capillary PCO2 equilibratesvery rapidly with alveolar PO2 (PAO2).
When diffusion is limited by disease, as
◦ Asbestosis
◦ Sarcoidosis
◦ collagen vascular disease
◦ idiopathic pulmonary fibrosis
◦ alveolar cell carcinoma
◦ Interstitial edema
supplemental O2 is effective to correct hypoxemia
30.
31. Diffusion impairment
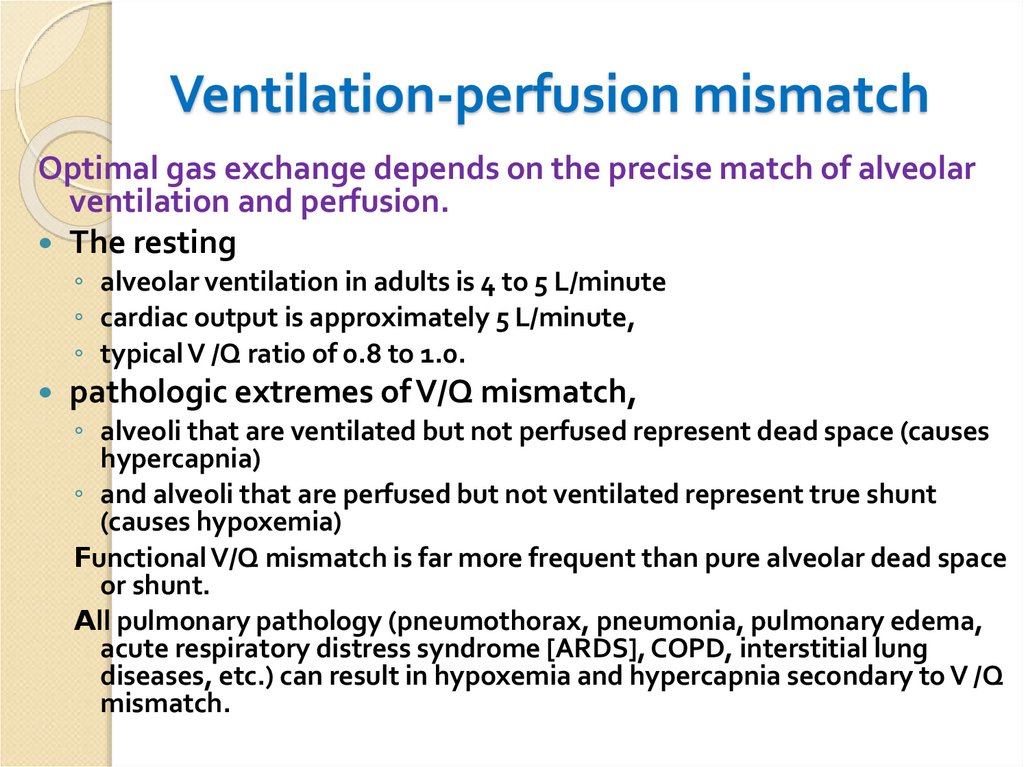
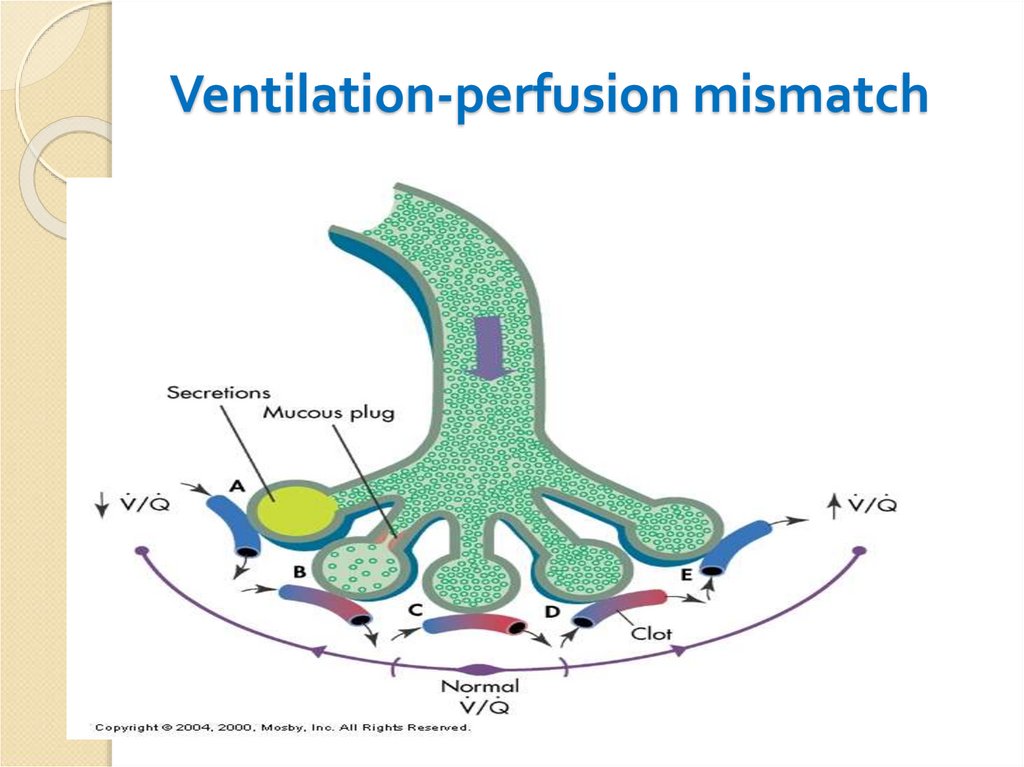
32. Ventilation-perfusion mismatch
Optimal gas exchange depends on the precise match of alveolarventilation and perfusion.
The resting
◦ alveolar ventilation in adults is 4 to 5 L/minute
◦ cardiac output is approximately 5 L/minute,
◦ typical V /Q ratio of 0.8 to 1.0.
pathologic extremes of V/Q mismatch,
◦ alveoli that are ventilated but not perfused represent dead space (causes
hypercapnia)
◦ and alveoli that are perfused but not ventilated represent true shunt
(causes hypoxemia)
Functional V/Q mismatch is far more frequent than pure alveolar dead space
or shunt.
All pulmonary pathology (pneumothorax, pneumonia, pulmonary edema,
acute respiratory distress syndrome [ARDS], COPD, interstitial lung
diseases, etc.) can result in hypoxemia and hypercapnia secondary to V /Q
mismatch.
33. Ventilation-perfusion mismatch
34. Insufficient O2 delivery
Decreased cardiac outputhypovolemia
congestive heart failure
◦ The subsequent increase in O2 extraction by the tissues decreases the mixed
venous PO2, which in turn may decrease PaO2.
Increased O2 demand
◦ Basal O2 consumption averages 200 to 250 mL/minute in adults.
◦ Hypermetabolic conditions such as fever, increased muscle activity from
shivering, seizures, hyperthyroidism, and, to a lesser degree, sepsis may
increase tissue O2 consumption 2- to 10-fold.
◦ This may result in a decrease in PvO2 and consequently a decrease in PaO2.
◦ In patients with limited reserve, such as those with respiratory failure,
coronary artery disease, and cerebrovascular disease, this phenomenon
may result in significant morbidity.
35. Typs of ARF
Hypoxemic respiratory failure (type I) ischaracterized by an arterial oxygen
tension (PaO2) lower than 60 mm Hg
with a normal or low arterial carbon
dioxide tension (PaCO2).
Some examples of type I respiratory
failure are cardiogenic or noncardiogenic
pulmonary edema, pneumonia, and
pulmonary hemorrhage.
36. Typs of ARF
Hypercapnic respiratory failure (type II) ischaracterized by a PaCO2 higher than 50 mm
Hg. Hypoxemia is common in patients with
hypercapnic respiratory failure.
Common etiologies include drug overdose,
neuromuscular disease, chest wall abnormalities,
and severe airway disorders (eg, asthma
and chronic obstructive pulmonary
disease [COPD]).
37. Effects of hypoxemia
Effects of hypoxemia◦ Build up of lactic acid →
metabolic acidosis → cell
death
◦ CNS depression
◦ Heart tries to compensate →
↑ HR and CO
◦ If no compensation: ↓ O2, ↑
acid, heart fails, shock,
multi-system organ failure
38. DIAGNOSIS
Signs of impending respiratory failure include:dyspnea
tachypnea (RR >30 breaths/minute)
bradypnea (RR < 6) breaths/minute
shallow respirations
use of accessory respiratory muscles
dyscoordinate motions of the chest and abdomen
cyanosis
obtundation.
39. DIAGNOSIS
Arterial Blood Gas Analysis.A normal PaO2 while breathing air is 90 to 100 mm Hg. It
decreases slightly with age due to progressive
worsening of V /Q matching.
A PaO2 less than 60 mm Hg requires consideration and
treatment.
A normal PaCO2 is 40 mm Hg. An acute increase may
indicate impending respiratory failure.
A normal arterial pH is 7.40 ± 0.02. As a rule of thumb,
for each 10 mm Hg of acute increase of PaCO2, the pH
decreases by 0.08.
Long-standing CO2 retention is associated with a nearly
normal pH because of compensatory reabsorption of
bicarbonate by the kidneys.
40.
The gold standard diagnostic ARF:gas analysis of arterial blood
41.
pulseoxymetry42. DIAGNOSIS
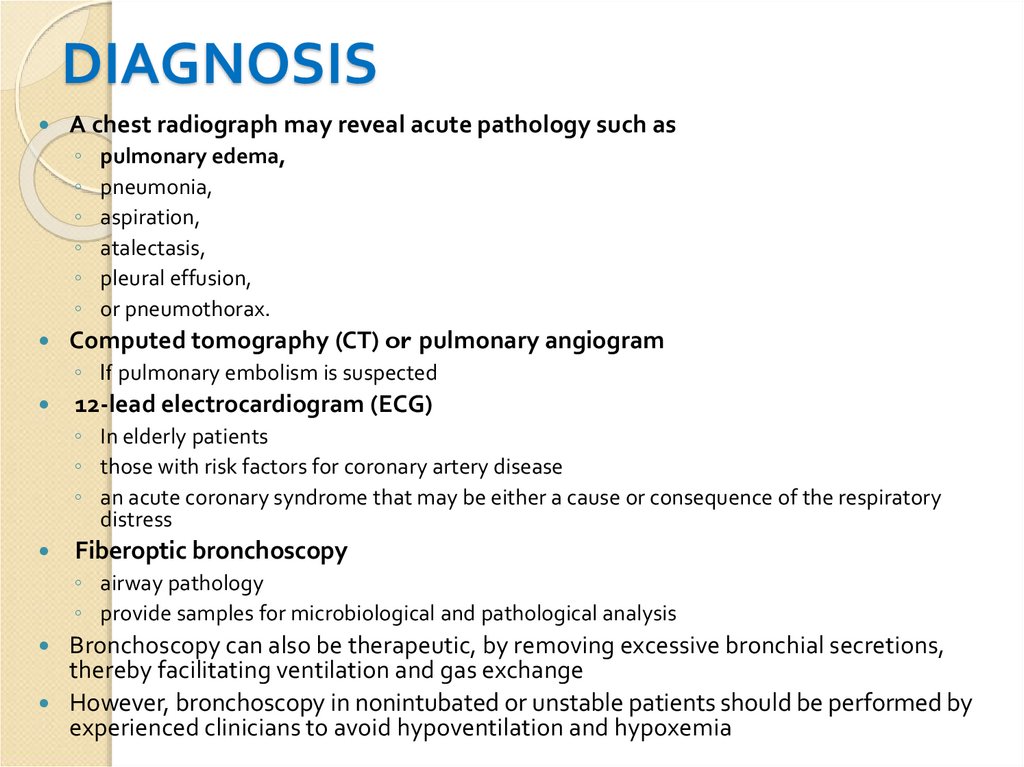
A chest radiograph may reveal acute pathology such as◦
◦
◦
◦
◦
◦
pulmonary edema,
pneumonia,
aspiration,
atalectasis,
pleural effusion,
or pneumothorax.
Computed tomography (CT) or pulmonary angiogram
◦ If pulmonary embolism is suspected
12-lead electrocardiogram (ECG)
◦ In elderly patients
◦ those with risk factors for coronary artery disease
◦ an acute coronary syndrome that may be either a cause or consequence of the respiratory
distress
Fiberoptic bronchoscopy
◦ airway pathology
◦ provide samples for microbiological and pathological analysis
Bronchoscopy can also be therapeutic, by removing excessive bronchial secretions,
thereby facilitating ventilation and gas exchange
However, bronchoscopy in nonintubated or unstable patients should be performed by
experienced clinicians to avoid hypoventilation and hypoxemia
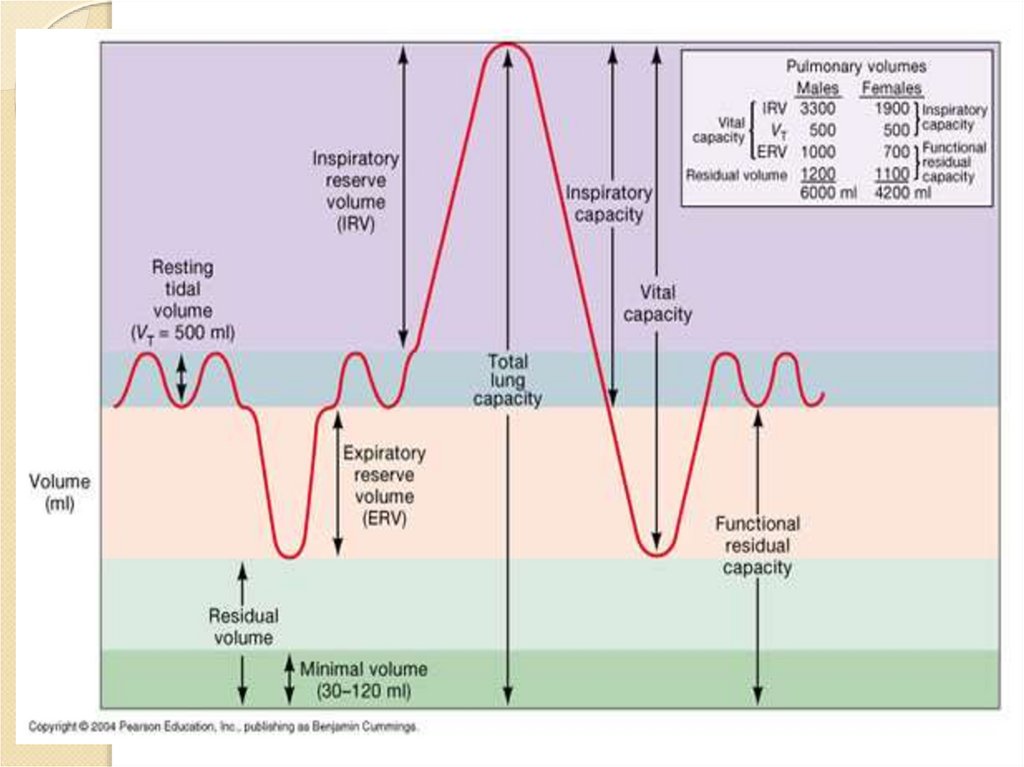
43. Дыхательные объемы и емкости
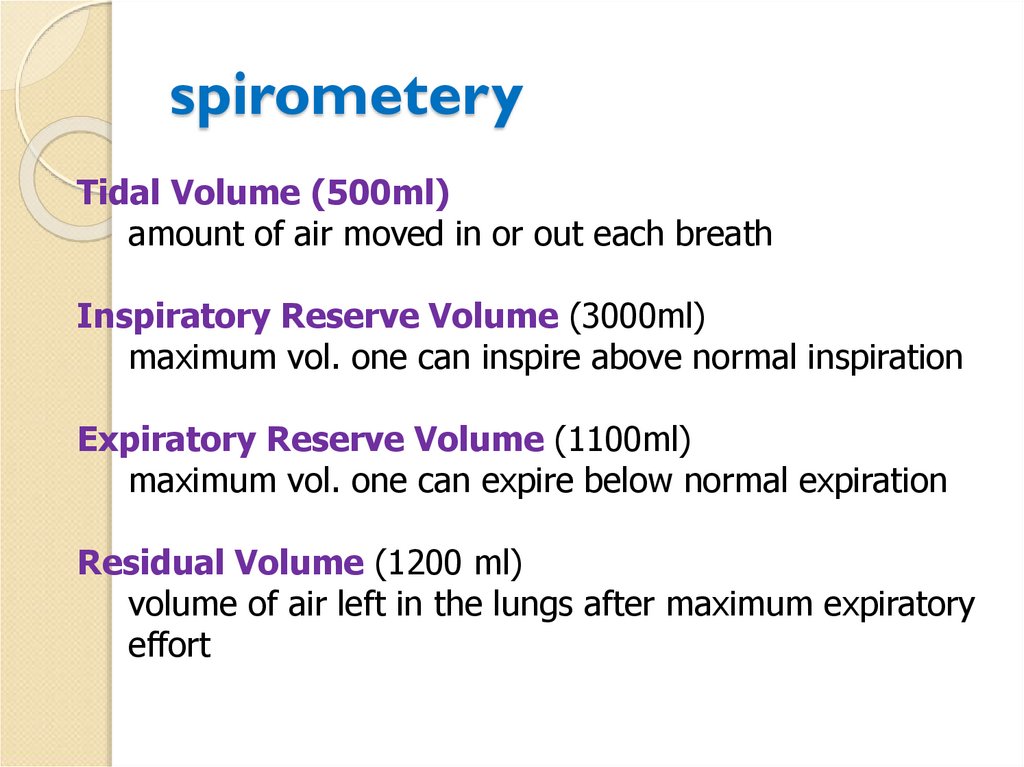
44. spirometery
Tidal Volume (500ml)amount of air moved in or out each breath
Inspiratory Reserve Volume (3000ml)
maximum vol. one can inspire above normal inspiration
Expiratory Reserve Volume (1100ml)
maximum vol. one can expire below normal expiration
Residual Volume (1200 ml)
volume of air left in the lungs after maximum expiratory
effort
45. Three main principles of ARF intensive care
1) patency of airways;2) optimization of gas composition of
breathing mixtures;
3) replacement of spontaneous ventilation
to artificial.
46. TREATMENT
Urgent resuscitationOxygenation
Airway control
Ventilator management
Stabilization of the
circulation
Bronchodilators/Steroids
47. Goal of oxygen therapy
To maintain adequate tissue oxygenation whileminimizing cardiopulmonary work
O2 Therapy : CLINICAL OBJECTIVES
1. Correct documented or suspected hypoxemia
2. Decrease the symptoms associated with chronic
hypoxemia
3. Decrease the workload hypoxemia imposes on
the cardiopulmonary system
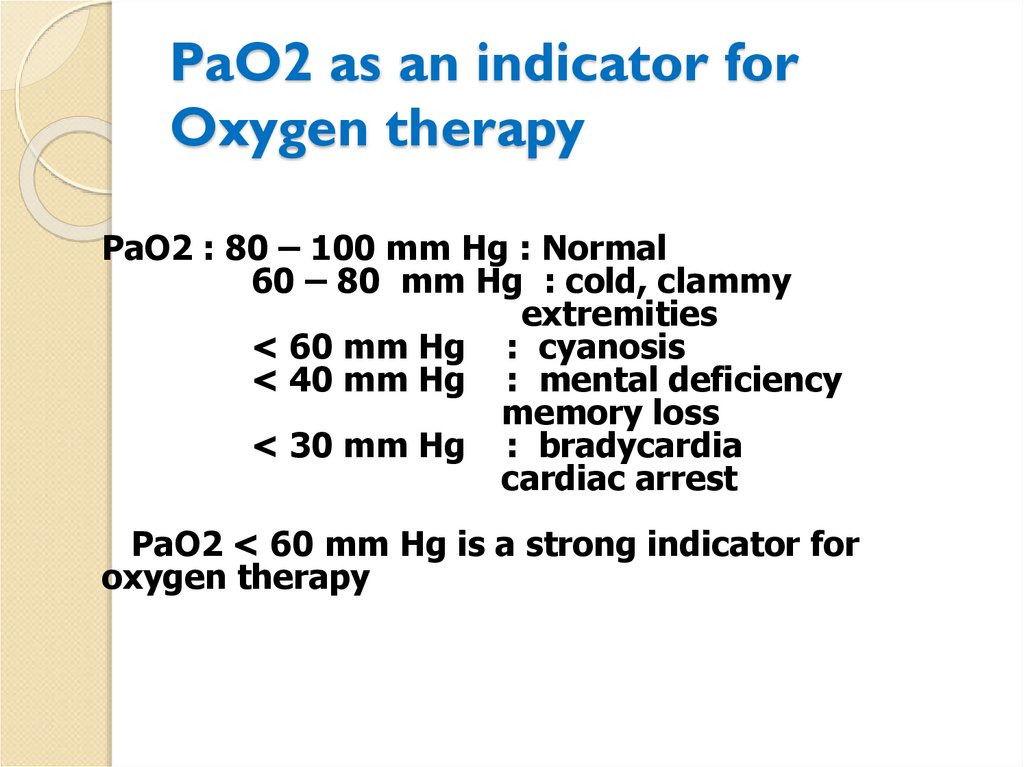
48. PaO2 as an indicator for Oxygen therapy
PaO2 : 80 – 100 mm Hg : Normal60 – 80 mm Hg : cold, clammy
extremities
< 60 mm Hg : cyanosis
< 40 mm Hg : mental deficiency
memory loss
< 30 mm Hg : bradycardia
cardiac arrest
PaO2 < 60 mm Hg is a strong indicator for
oxygen therapy
49. TREATMENT: Supplemental O2
Indication is hypoxemia of any origin.principles of the oxygenotherapy:
1) moisture;
2) dosing;
3) continuity.
50. O2 toxicity
1. O2 toxicity. High FiO2 (usually greater than 0.6)delivered over long periods of time causes acute
tracheobronchitis, impairment of ciliary motion, and
alveolar damage.
However, when high FiO2 is administered for short
periods of time, such as in the perioperative period,
toxicity is not a significant concern.
More relevant to the perioperative period is that a
high FiO2 causes absorption atelectasis, a
consequence of absorption of alveolar gas when
little or no nitrogen is present.
51.
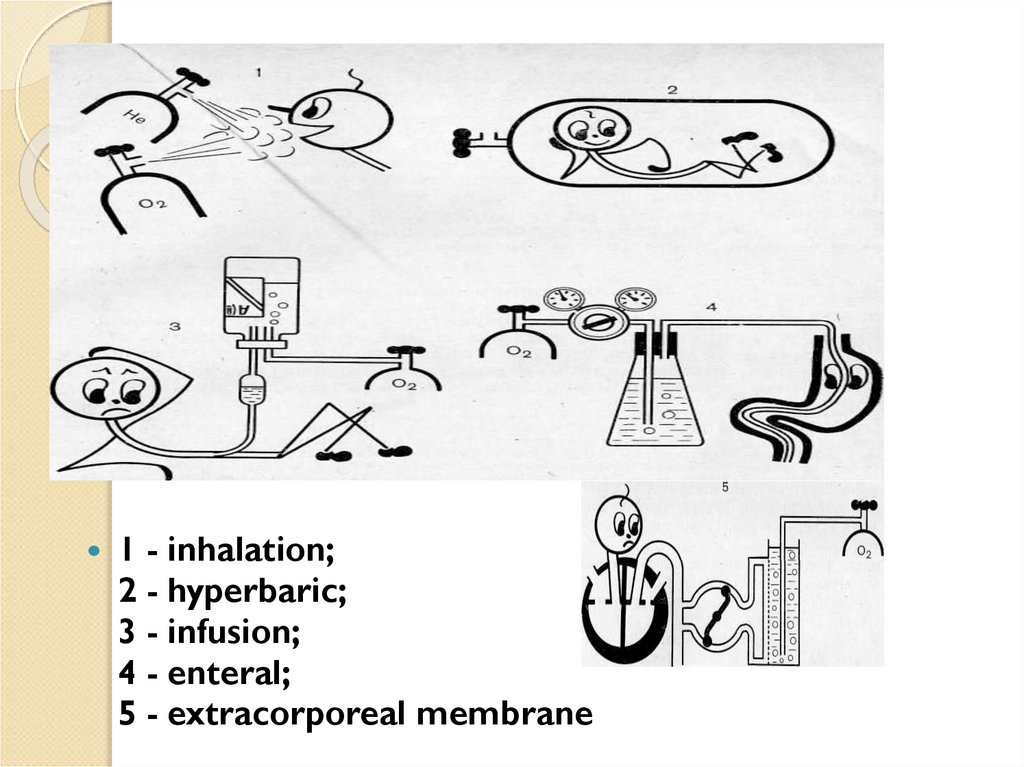
1 - inhalation;2 - hyperbaric;
3 - infusion;
4 - enteral;
5 - extracorporeal membrane
52. TREATMENT: Supplemental O2
Low-flow O2 systems are simple and readily available.They produce a limited and variable inspired O2
concentration (FiO2) that is inversely proportional to the
patient's peak inspiratory flow rate and minute
ventilation due to entrainment of room air during
inspiration.
53. TREATMENT: Supplemental O2
◦ Nasal cannulae increase the FiO2 by approximately0.03 to 0.04 (3% to 4%) per L/minute of O2 flow.
◦ Flows above 4 L/minute dry the nasal mucosa and
may produce nasal irritation and bleeding
◦ The nasal passages must be patent
◦ nasal breathing is not required because of the
effective anatomic reservoir of the upper airway
54.
Nasal cannulaeМаска Вентури
Venturi mask
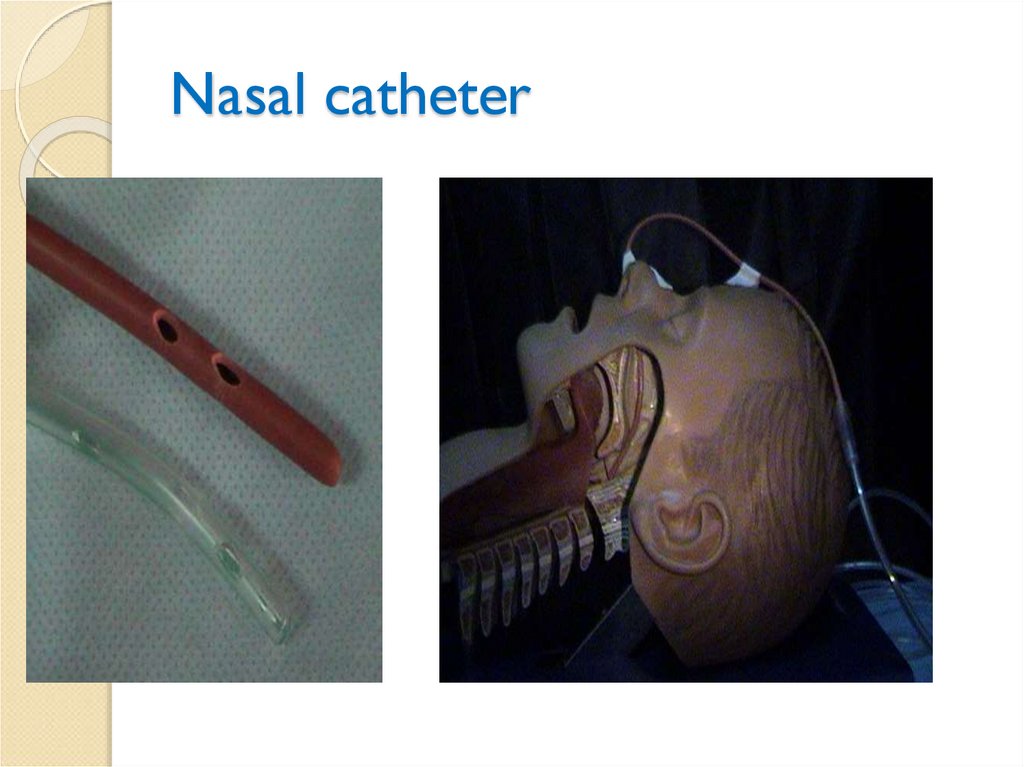
55. Nasal catheter
56. TREATMENT: Supplemental O2
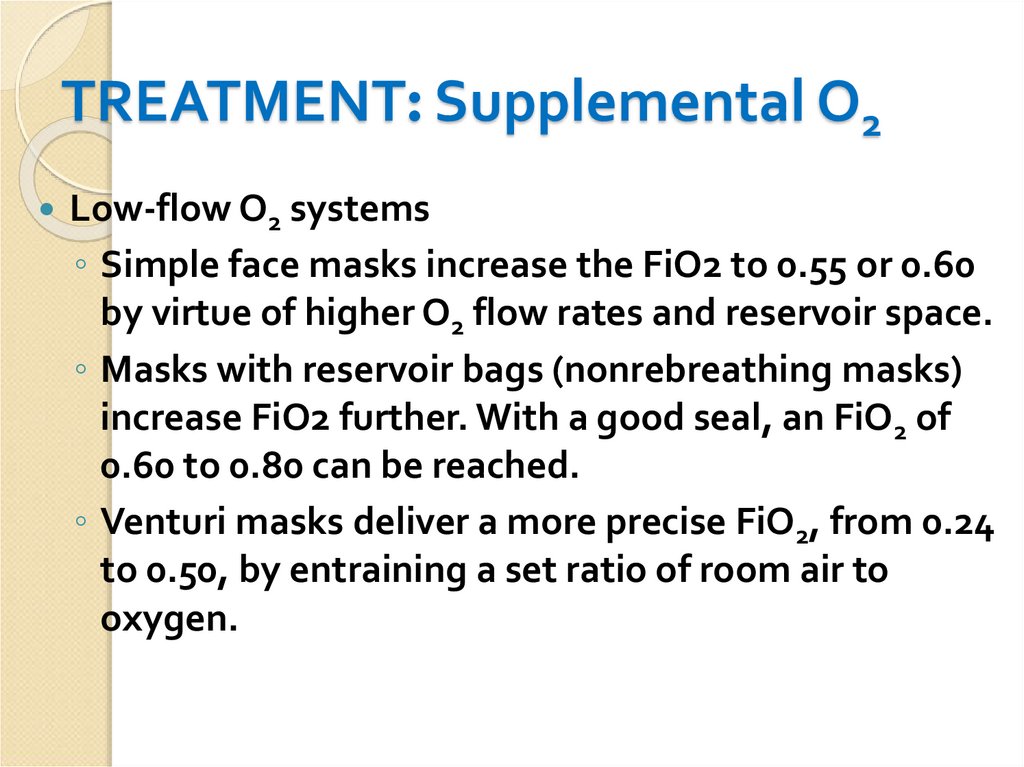
Low-flow O2 systems◦ Simple face masks increase the FiO2 to 0.55 or 0.60
by virtue of higher O2 flow rates and reservoir space.
◦ Masks with reservoir bags (nonrebreathing masks)
increase FiO2 further. With a good seal, an FiO2 of
0.60 to 0.80 can be reached.
◦ Venturi masks deliver a more precise FiO2, from 0.24
to 0.50, by entraining a set ratio of room air to
oxygen.
57.
• SaO2 < 90% при FiО2 = 0.21 (фракция кислорода вовдыхаемой смеси)
или
• РаО2 < 60 мм рт.ст.
58.
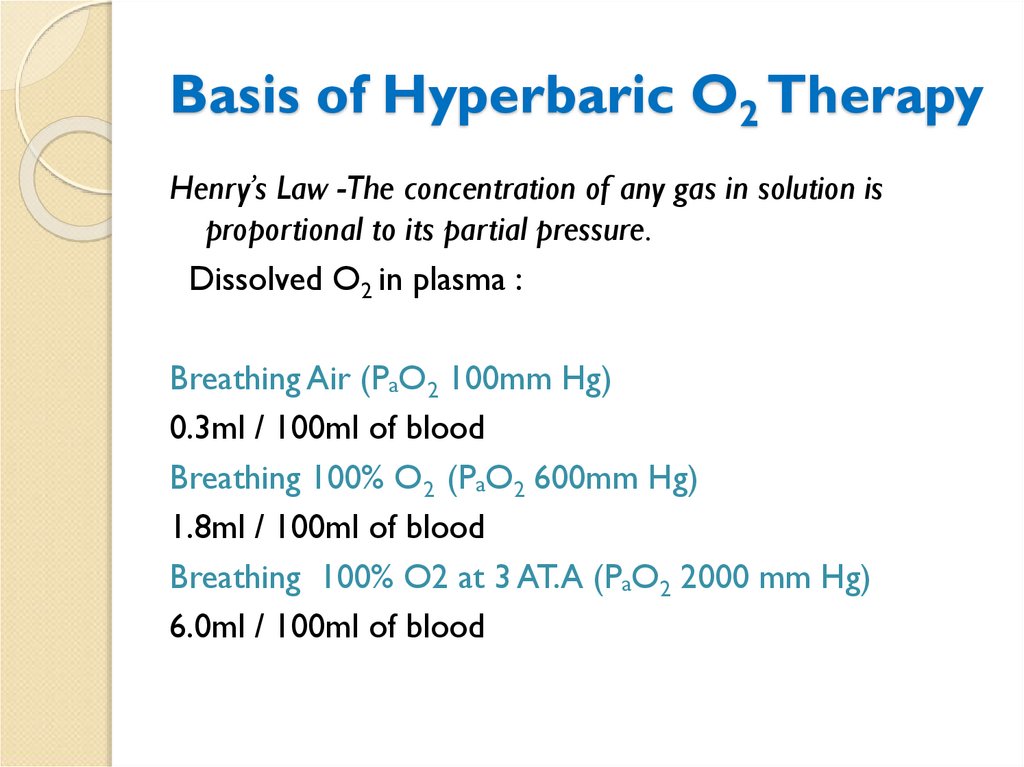
59. Basis of Hyperbaric O2 Therapy
Henry’s Law -The concentration of any gas in solution isproportional to its partial pressure.
Dissolved O2 in plasma :
Breathing Air (PaO2 100mm Hg)
0.3ml / 100ml of blood
Breathing 100% O2 (PaO2 600mm Hg)
1.8ml / 100ml of blood
Breathing 100% O2 at 3 AT.A (PaO2 2000 mm Hg)
6.0ml / 100ml of blood
60. INDICATIONS OF HBOT
Decompression sicknessAir embolism
Carbon monoxide poisoning
Severe crush injuries
Thermal burns
Acute arterial insufficiency
Clostridial gangrene
Necrotizing soft-tissue infection
Ischemic skin graft or flap
61. Problems with HBOT
Barotrauma◦ Ear/ sinus trauma
◦ Tympanic membrane rupture
◦ Pneumothorax
Oxygen toxicity
Fire hazards
Clautrophobia
Sudden decompression
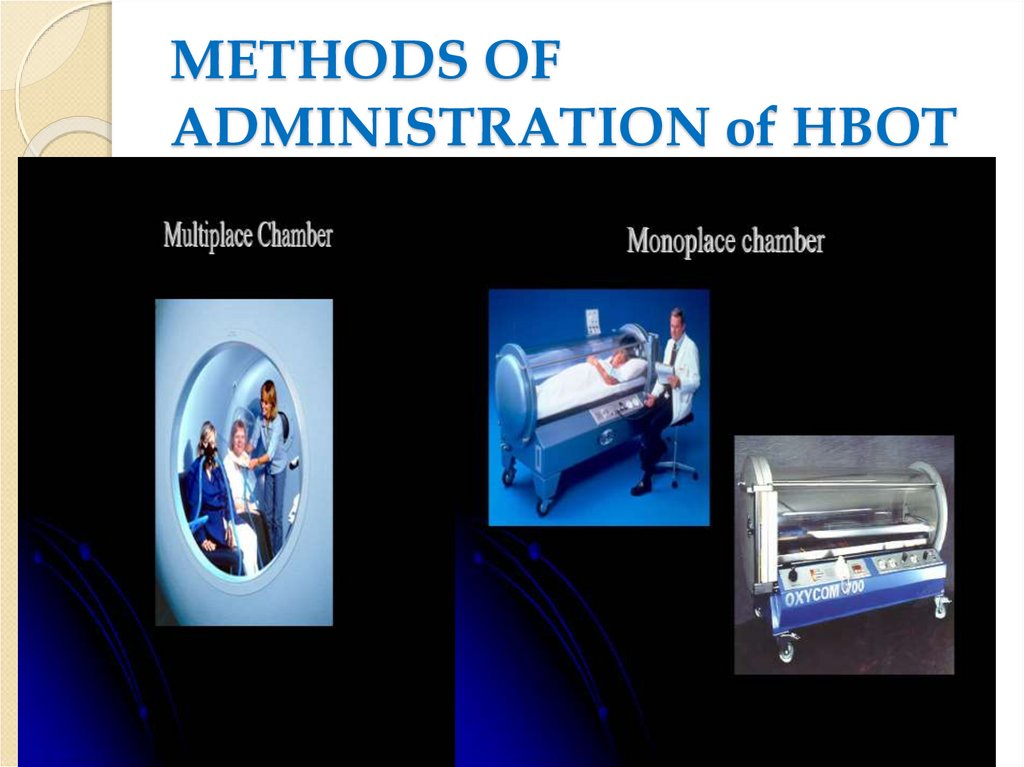
62. METHODS OF ADMINISTRATION of HBOT
63. TREATMENT:Secretion Clearance.
Retained secretions increase airway resistance and promotealveolar collapse. Secretion clearance may be facilitated in
several ways.
Humidification and warming of inspired gases.
◦ passive heat and moisture exchangers can be placed between
the endotracheal or supraglottic device and the breathing
circuit.
64. TREATMENT:Secretion Clearance.
Suctioning.◦ Pain, sedation, and general debilitation can limit
patients' ability to cough and expel secretions.
◦ Blind nasotracheal suctioning effectively clears
tracheal secretions and stimulates coughing
◦ caution - it may cause hypoxemia, vagal
stimulation, bronchospasm, and mucosal trauma.
Chest physiotherapy.
◦ Properly performed percussion, vibration, postural
drainage, and deep breathing exercises are
effective means of clearing secretions and
preventing
65. TREATMENT:Secretion Clearance.
Mucolytics. Local instillation of acetylcysteine(mucomyst, 2 to 5 mL of 5% to 20% solution every
6 to 8 hours) may decrease mucus viscosity by
reducing glycoprotein disulfide bonds.
Bronchoscopy is an effective way to remove
secretions and thick mucus plugs from the airways
66. TREATMENT: Pharmacologic Therapy
Reversal of ventilatory depression.◦ naloxone for opioids
◦ flumazenil for benzodiazepines
◦
Reversal of residual neuromuscular blockade should be carried
out to avoid ventilatory failure and inadequate airway
protection
Analgesia. Pain from surgical incisions, trauma, and
invasive procedures may hinder the effectiveness of
ventilation. Numerous analgesic options are available
67. TREATMENT:Secretion Clearance.
Bronchodilation. Agents used to treat acutebronchospasm can be administered by inhalation,
nebulization, or intravenously
Heliox (helium-oxygen) gas mixtures are less
dense than air (nitrogen -oxygen) and may be used
to increase ventilation in patients with airway
obstruction.
Treatment of the underlying condition must
be instituted.
◦ control of hemodynamics
◦ treatment of infections
◦ arrythmias,
◦ myocardial ischemia,
◦ anemia, etc.
Broad-spectrum antibiotics if the diagnosis of pneumonia is made
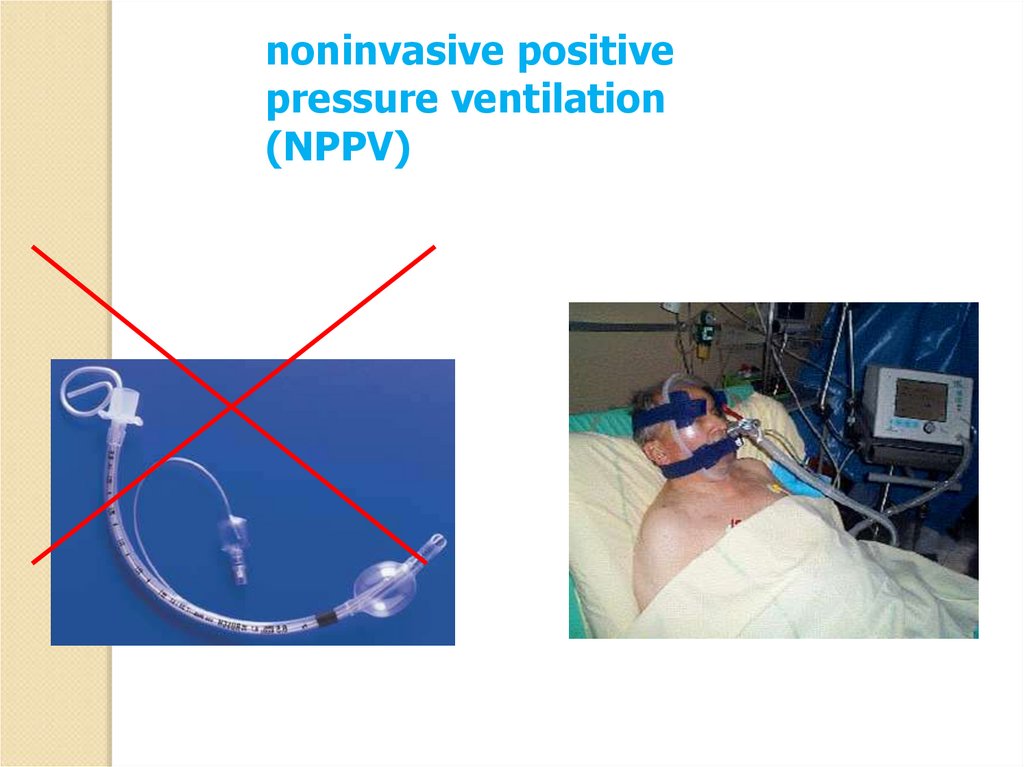
68. Respiratory Failure: Management
Mechanical ventilationNon - invasive (if patient can protect
airway and is hemodynamically stable)
Mask: usually orofacial to start
Invasive
Endotracheal tube (ETT)
Tracheostomy – if upper airway is
obstructed
69. Indications for Mechanical Ventilation
Cardiac or respiratory arrestTachypnea or bradypnea with respiratory
fatigue or impending arrest
Acute respiratory acidosis
Refractory hypoxemia (when the P a O 2 could
not be maintained above 60 mm Hg with
inspired O 2 fraction (F I O 2 )>1.0)
Inability to protect the airway associated with
depressed levels of consciousness
70. Goals of Mechanical Ventilation
Improve ventilation by augmentingrespiratory rate and tidal volume
Assistance for neural or muscle dysfunction
Sedated, comatose or paralyzed patient
Neuropathy, myopathy or muscular
dystrophy
Intra - operative ventilation
Correct respiratory acidosis
Match metabolic demand
Rest respiratory muscles
71. Invasive vs. Non - invasive Ventilation
Consider non - invasive ventilationparticularly in the following settings:
COPD exacerbation
Cardiogenic pulmonary edema
Obesity hypoventilation syndrome
Noninvasive ventilation may be tried in selected
patients with asthma or non - cardiogenic
hypoxemic respiratory failure
72. TREATMENT:Mechanical ventilation
1. Noninvasive ventilationa. Mechanical ventilation can be delivered without
tracheal intubation. In perioperative patients, adequate
levels of support in the form of either noninvasive
continuous positive airway pressure (CPAP)
b. The most common cause of failure is the inability of the
patient to tolerate the discomfort of the tight face mask
and high gas flow. It is important to recognize the failure
of noninvasive ventilation and proceed to tracheal
intubation to avoid patient exhaustion and respiratory
arrest.
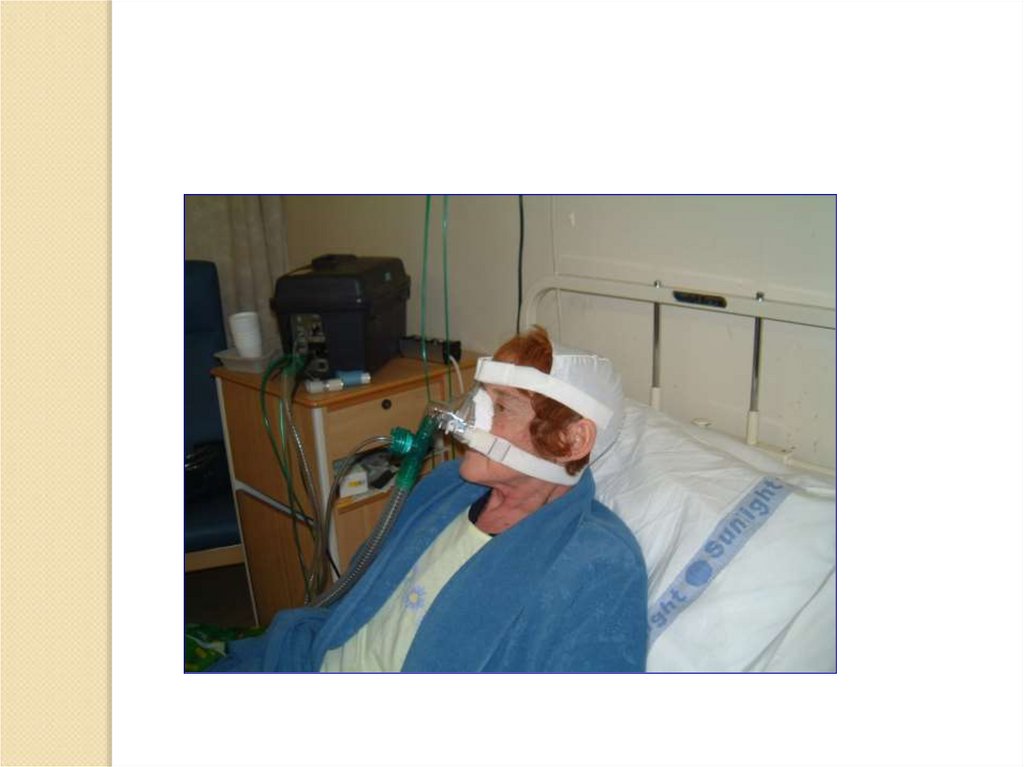
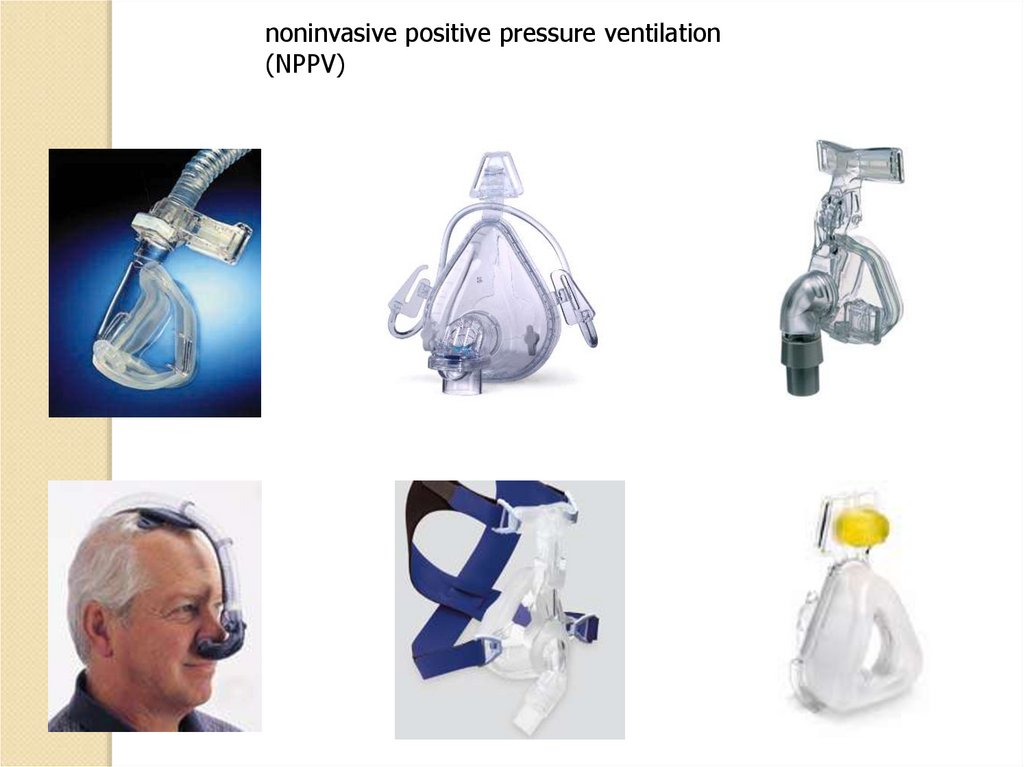
73. noninvasive positive pressure ventilation (NPPV)
noninvasive ventilation are bestadministered through an orofacial mask.
If a specialized ventilator is not available, a
standard critical care ventilator is effective.
74.
noninvasive positivepressure ventilation
(NPPV)
75.
76.
noninvasive positive pressureventilation
(NPPV)
BiPAP Harmony
(Respironics)
BiPAP Vision (Respironics)
77.
noninvasive positive pressure ventilation(NPPV)
78.
Helmethelmet
79. TREATMENT:Mechanical ventilation
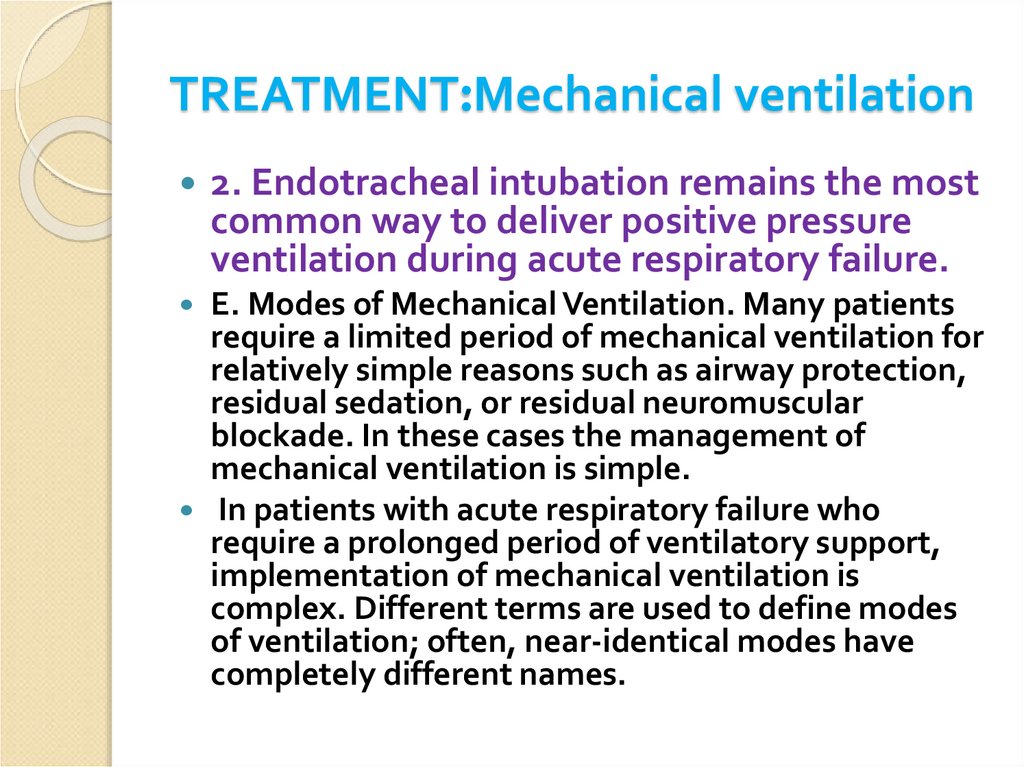
2. Endotracheal intubation remains the mostcommon way to deliver positive pressure
ventilation during acute respiratory failure.
E. Modes of Mechanical Ventilation. Many patients
require a limited period of mechanical ventilation for
relatively simple reasons such as airway protection,
residual sedation, or residual neuromuscular
blockade. In these cases the management of
mechanical ventilation is simple.
In patients with acute respiratory failure who
require a prolonged period of ventilatory support,
implementation of mechanical ventilation is
complex. Different terms are used to define modes
of ventilation; often, near-identical modes have
completely different names.
80.
81.
82. Mechanical ventilation
83. System to Denote all Common Modes of Mechanical Ventilation
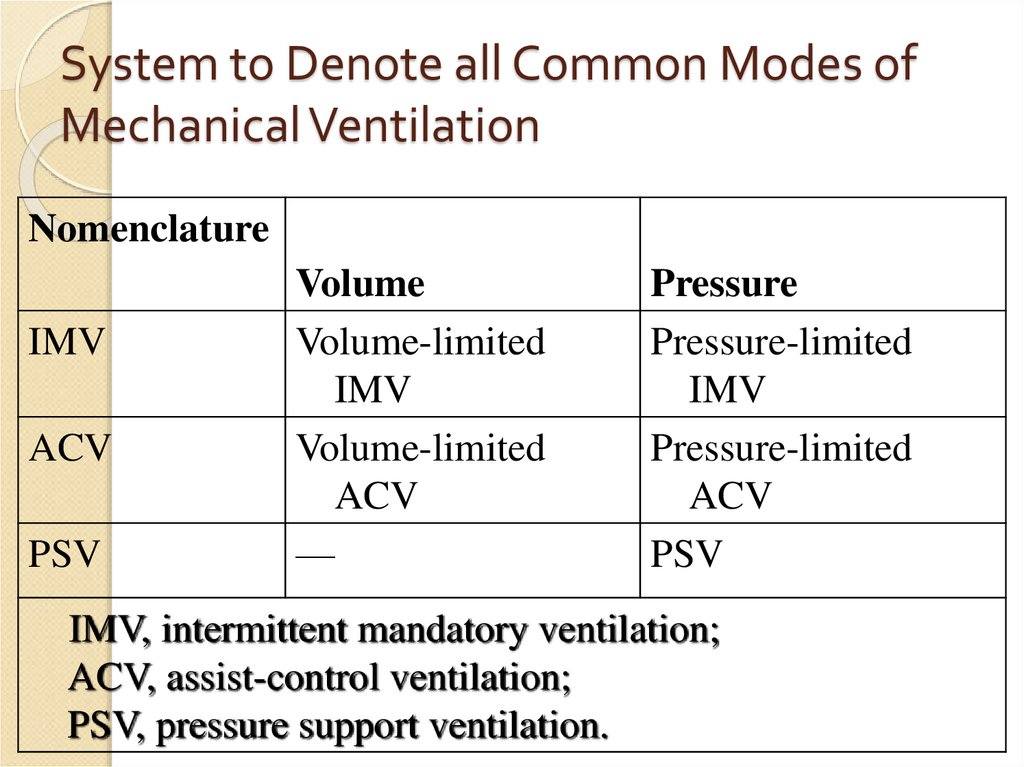
NomenclatureIMV
ACV
PSV
Volume
Volume-limited
IMV
Volume-limited
ACV
—
Pressure
Pressure-limited
IMV
Pressure-limited
ACV
PSV
IMV, intermittent mandatory ventilation;
ACV, assist-control ventilation;
PSV, pressure support ventilation.
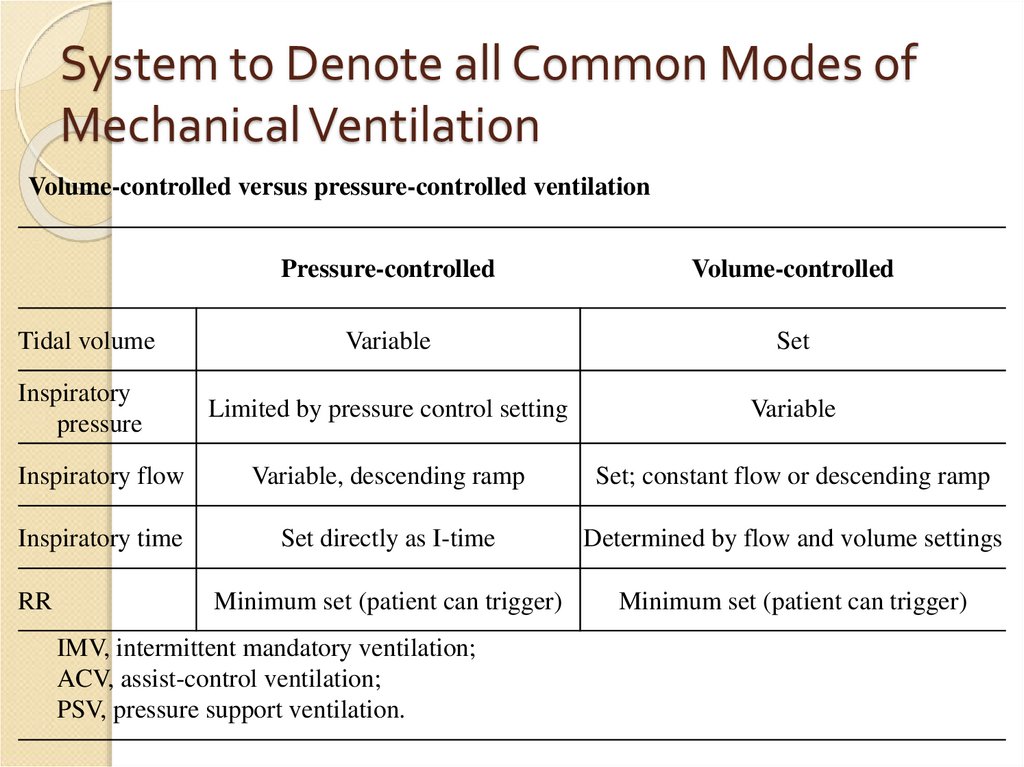
84. System to Denote all Common Modes of Mechanical Ventilation
Volume-controlled versus pressure-controlled ventilationPressure-controlled
Volume-controlled
Tidal volume
Variable
Set
Inspiratory
pressure
Limited by pressure control setting
Variable
Inspiratory flow
Variable, descending ramp
Set; constant flow or descending ramp
Inspiratory time
Set directly as I-time
Determined by flow and volume settings
Minimum set (patient can trigger)
Minimum set (patient can trigger)
RR
IMV, intermittent mandatory ventilation;
ACV, assist-control ventilation;
PSV, pressure support ventilation.
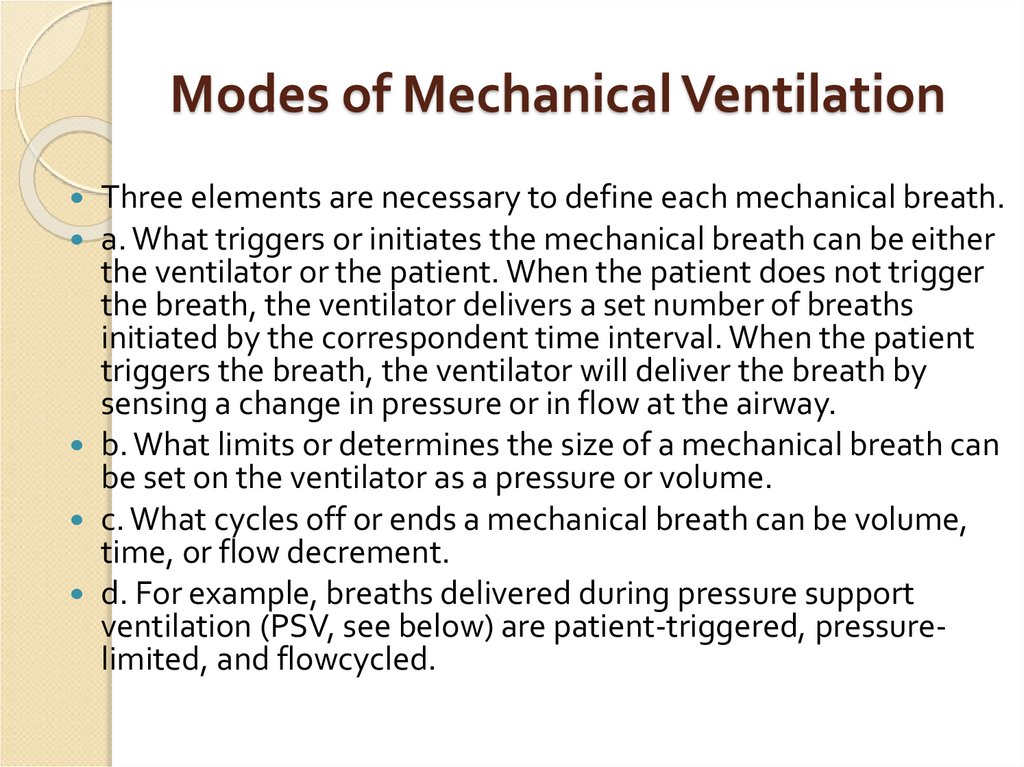
85. Modes of Mechanical Ventilation
Three elements are necessary to define each mechanical breath.a. What triggers or initiates the mechanical breath can be either
the ventilator or the patient. When the patient does not trigger
the breath, the ventilator delivers a set number of breaths
initiated by the correspondent time interval. When the patient
triggers the breath, the ventilator will deliver the breath by
sensing a change in pressure or in flow at the airway.
b. What limits or determines the size of a mechanical breath can
be set on the ventilator as a pressure or volume.
c. What cycles off or ends a mechanical breath can be volume,
time, or flow decrement.
d. For example, breaths delivered during pressure support
ventilation (PSV, see below) are patient-triggered, pressurelimited, and flowcycled.
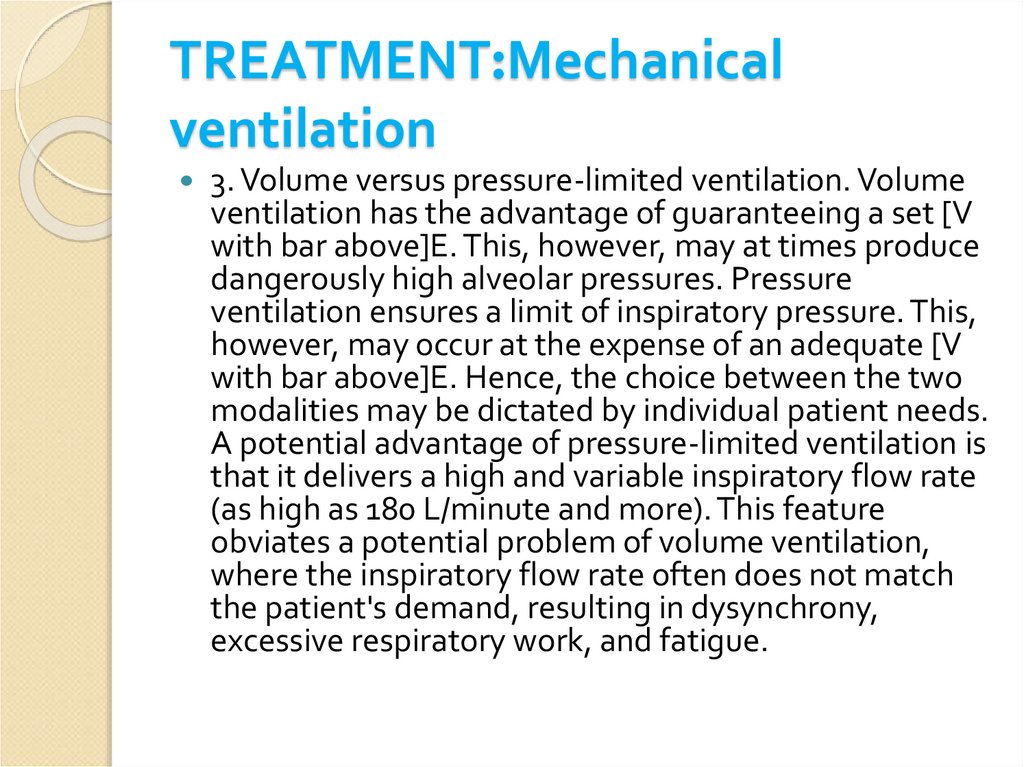
86. TREATMENT:Mechanical ventilation
3. Volume versus pressure-limited ventilation. Volumeventilation has the advantage of guaranteeing a set [V
with bar above]E. This, however, may at times produce
dangerously high alveolar pressures. Pressure
ventilation ensures a limit of inspiratory pressure. This,
however, may occur at the expense of an adequate [V
with bar above]E. Hence, the choice between the two
modalities may be dictated by individual patient needs.
A potential advantage of pressure-limited ventilation is
that it delivers a high and variable inspiratory flow rate
(as high as 180 L/minute and more). This feature
obviates a potential problem of volume ventilation,
where the inspiratory flow rate often does not match
the patient's demand, resulting in dysynchrony,
excessive respiratory work, and fatigue.
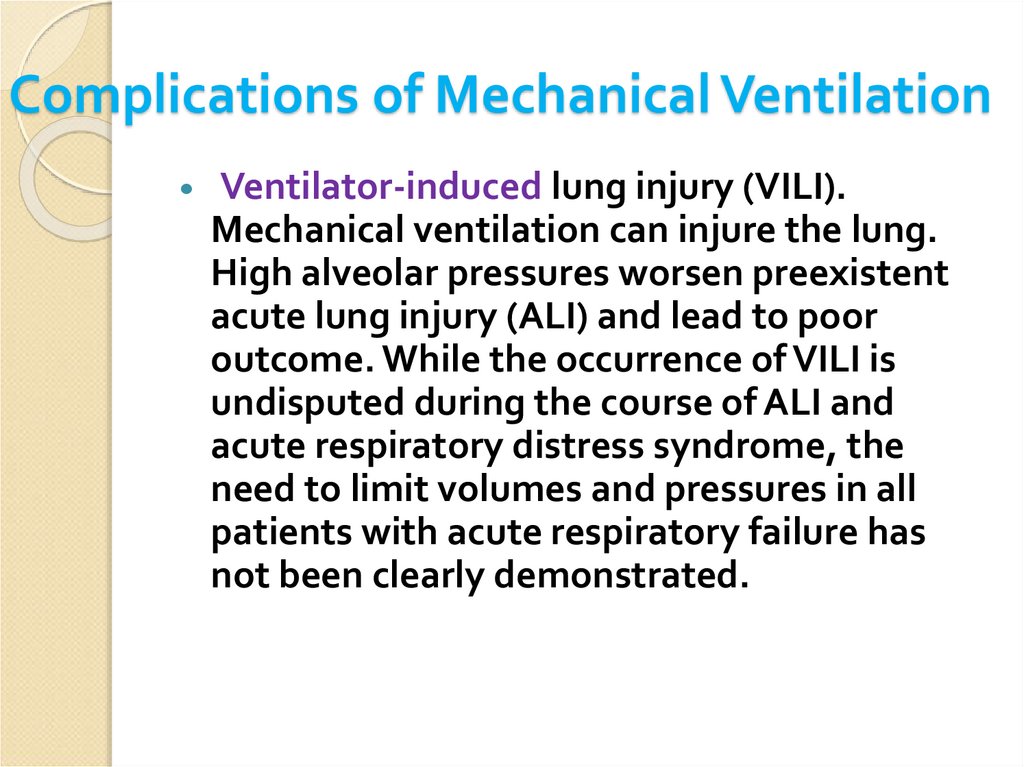
87. Complications of Mechanical Ventilation
Ventilator-induced lung injury (VILI).Mechanical ventilation can injure the lung.
High alveolar pressures worsen preexistent
acute lung injury (ALI) and lead to poor
outcome. While the occurrence of VILI is
undisputed during the course of ALI and
acute respiratory distress syndrome, the
need to limit volumes and pressures in all
patients with acute respiratory failure has
not been clearly demonstrated.
88. Complications of Mechanical Ventilation
Hemodynamic dysfunctionPositive pressure ventilation increases intrathoracic
pressure and decreases venous return to the heart.
Intravascular volume replacement counteracts these
hemodynamic effects of positive pressure
ventilation.
Infection. Prolonged tracheal intubation is
associated with bacterial colonization of the airways
and an increased risk of nosocomial and ventilatorassociated pneumonia. Early extubation,
noninvasive ventilation, appropriate use of antibiotic
therapy, and good infection control practices limit
the incidence of nosocomial pneumonia
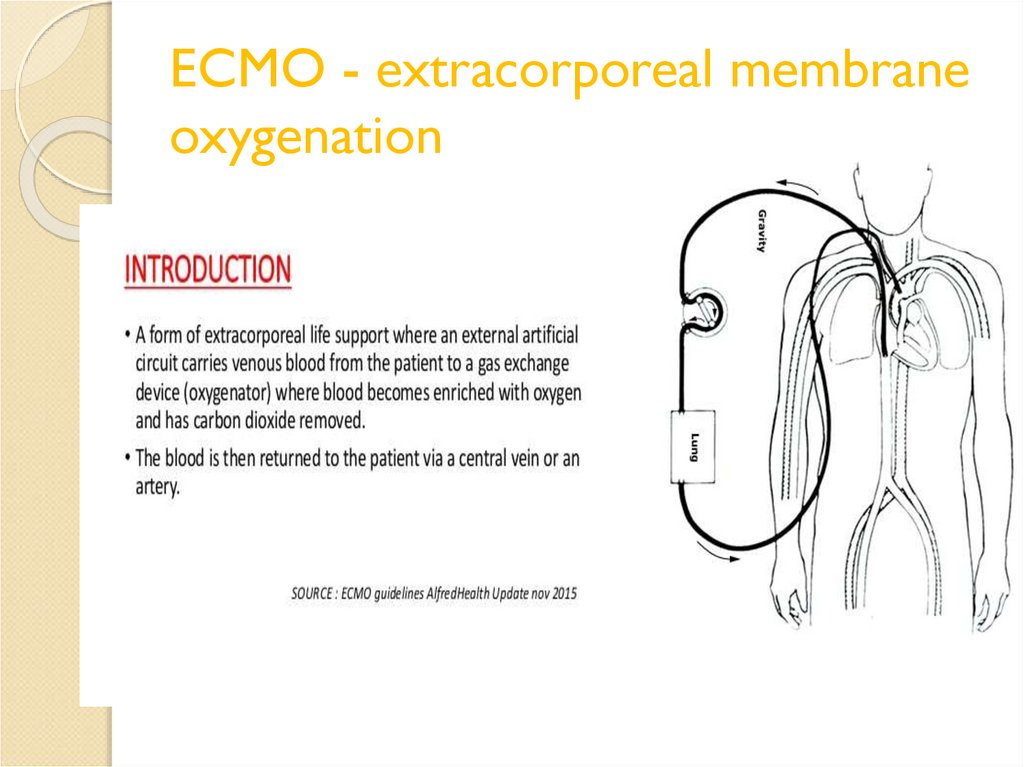
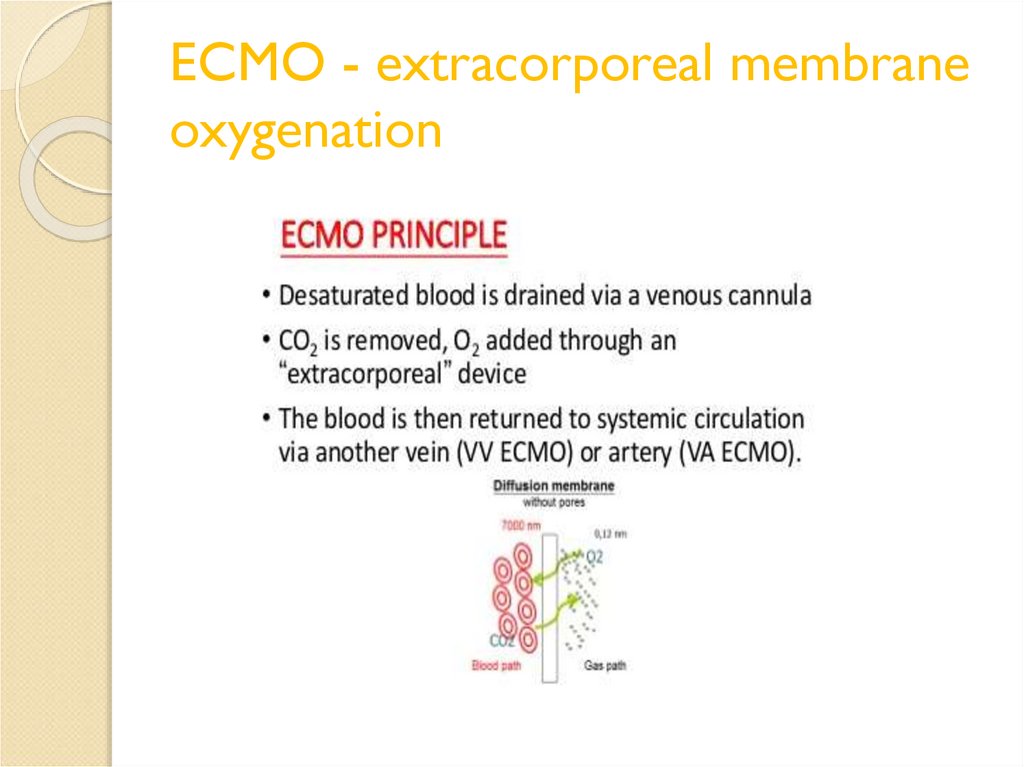
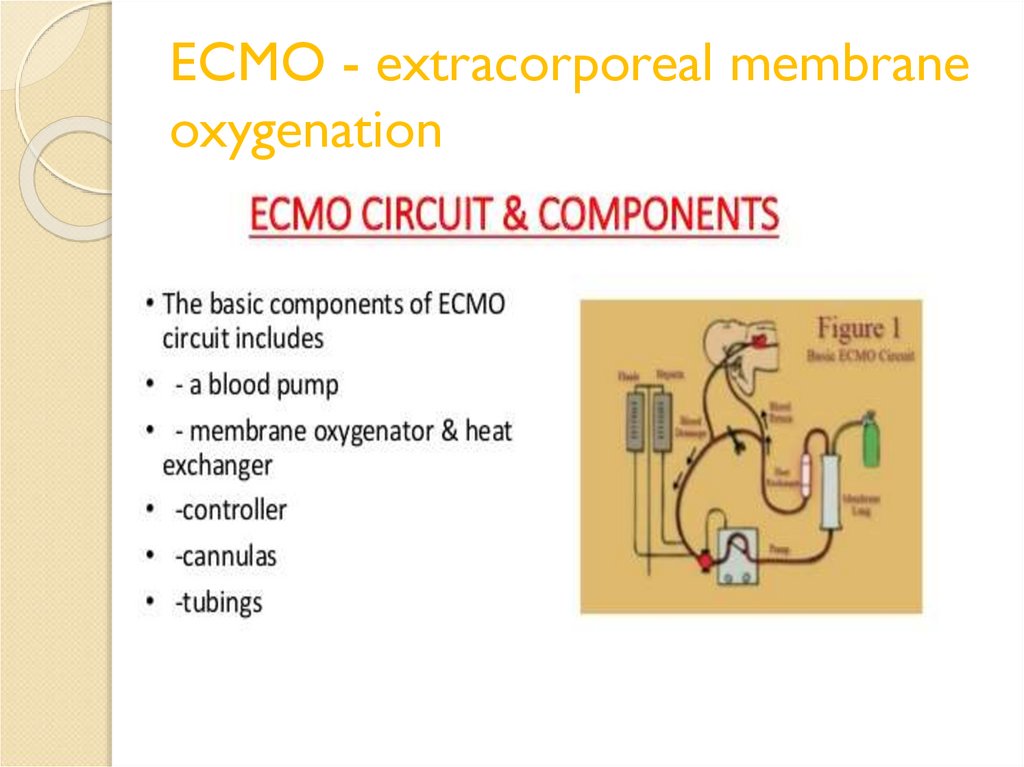
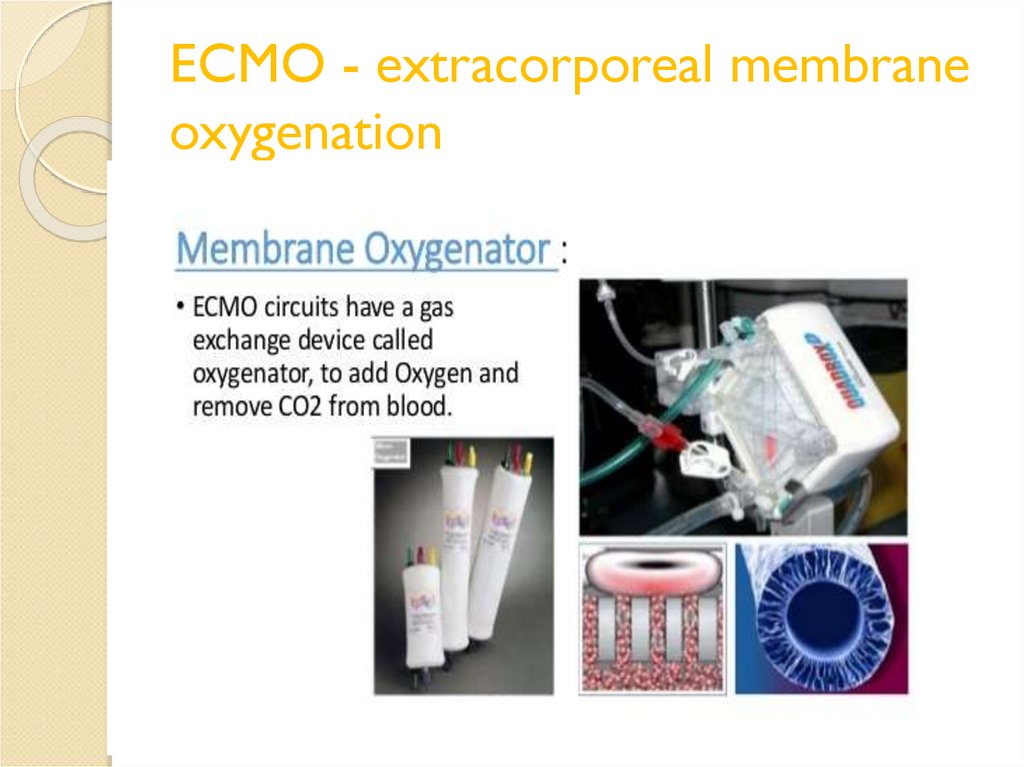
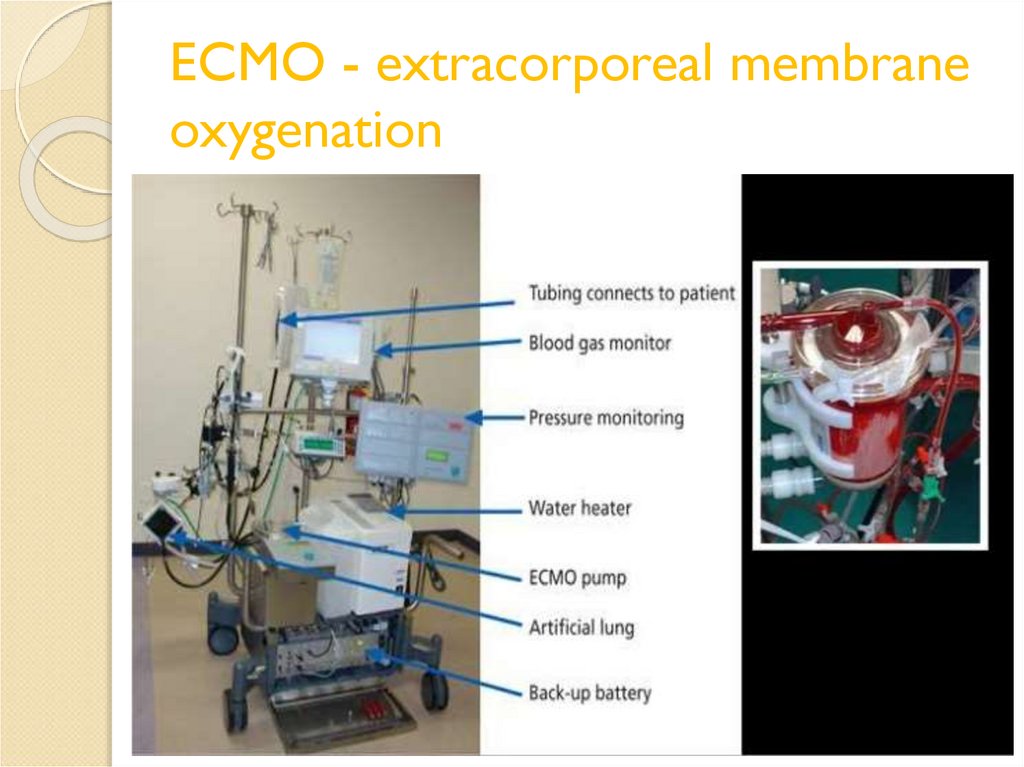
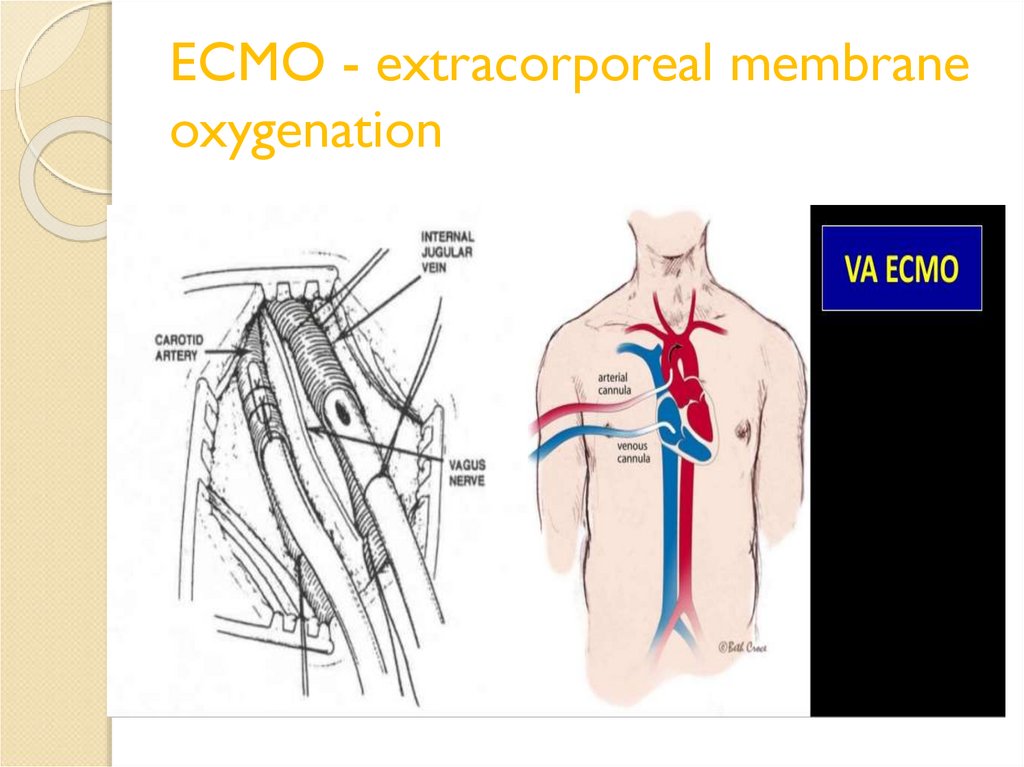
89. ECMO - extracorporeal membrane oxygenation
90. ECMO - extracorporeal membrane oxygenation
91. ECMO - extracorporeal membrane oxygenation
92. ECMO - extracorporeal membrane oxygenation
93. ECMO - extracorporeal membrane oxygenation
94. ECMO - extracorporeal membrane oxygenation
95. ECMO - extracorporeal membrane oxygenation
96.
THANK YOUFOR LISTENING!














 Медицина
Медицина