Похожие презентации:
Pathology of respiration. (Subject 15)
1. Pathology of Respiration
24 March 20152. Respiratory failure
Lungs are unable to provide:an adequate supply of O2
and/or to remove CO2 efficiently
In arterial blood: pO2 - 95 - 100 mm Hg
pCO2 - 43 - 46 mm Hg
Classification:
Acute failure – minutes to hours (bronchial asthma
attack, acute pneumonia).
Subacute –days to weeks (pneumonia, bronchitis).
Chronic – months to years (emphysema of lungs,
disseminated lung fibrosis).
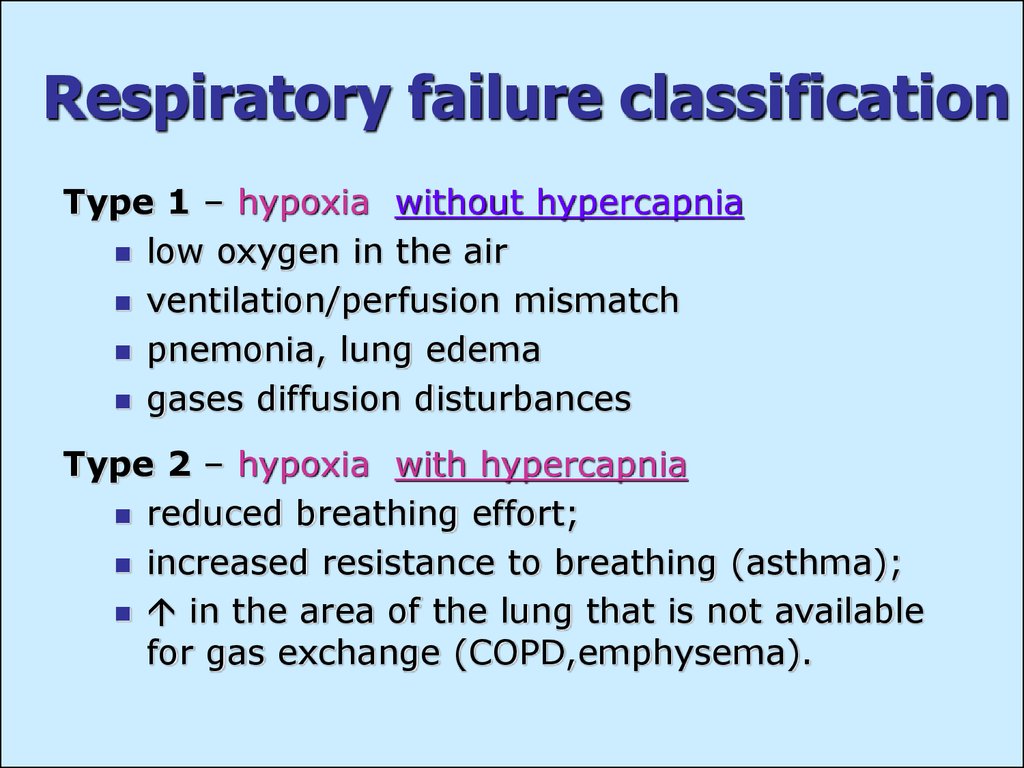
3. Respiratory failure classification
Type 1 – hypoxia without hypercapnialow oxygen in the air
ventilation/perfusion mismatch
pnemonia, lung edema
gases diffusion disturbances
Type 2 – hypoxia with hypercapnia
reduced breathing effort;
increased resistance to breathing (asthma);
in the area of the lung that is not available
for gas exchange (COPD,emphysema).
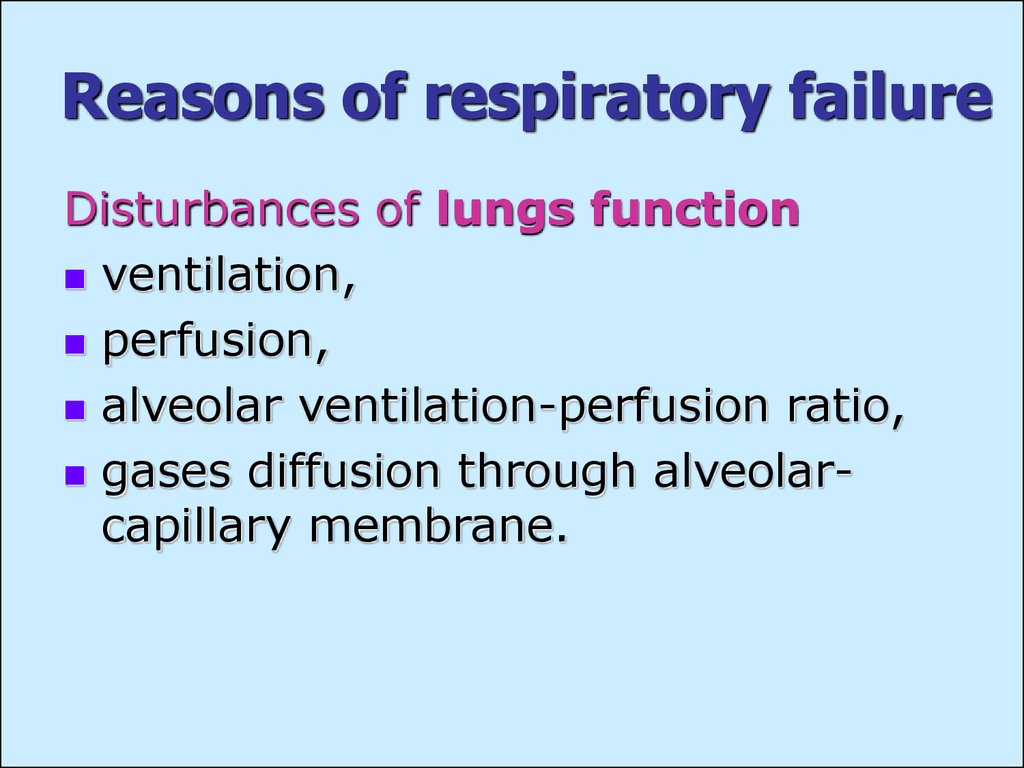
4. Reasons of respiratory failure
Disturbances of lungs functionventilation,
perfusion,
alveolar ventilation-perfusion ratio,
gases diffusion through alveolarcapillary membrane.
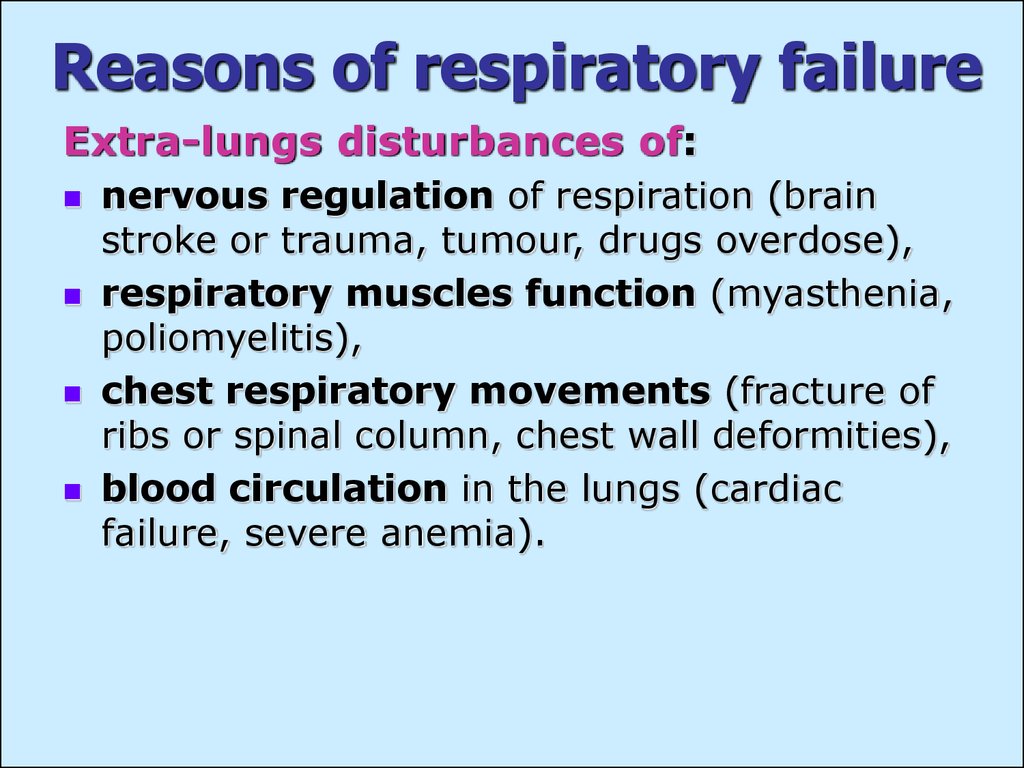
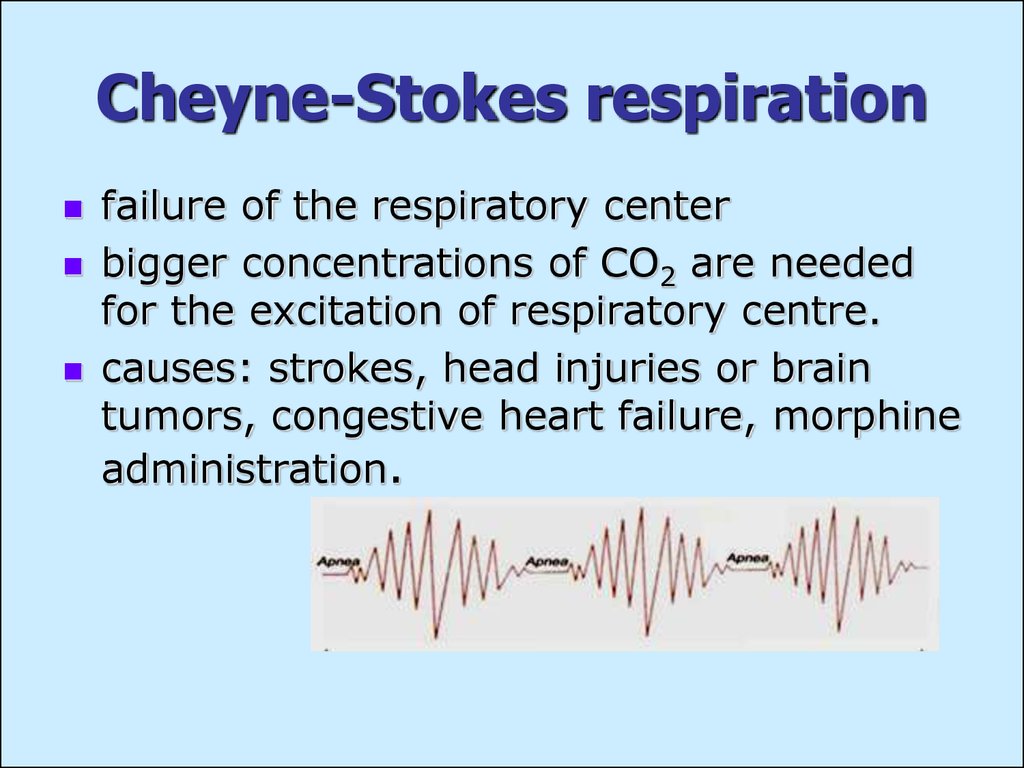
5. Reasons of respiratory failure
Extra-lungs disturbances of:nervous regulation of respiration (brain
stroke or trauma, tumour, drugs overdose),
respiratory muscles function (myasthenia,
poliomyelitis),
chest respiratory movements (fracture of
ribs or spinal column, chest wall deformities),
blood circulation in the lungs (cardiac
failure, severe anemia).
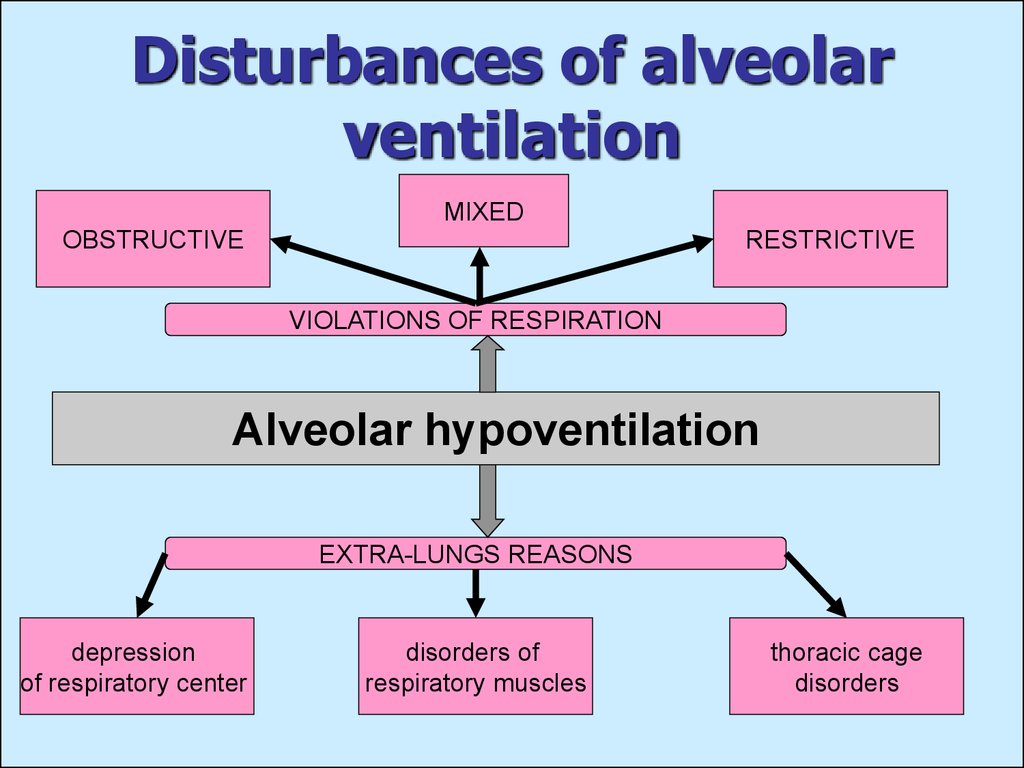
6. Disturbances of alveolar ventilation
MIXEDOBSTRUCTIVE
RESTRICTIVE
VIOLATIONS OF RESPIRATION
Alveolar hypoventilation
EXTRA-LUNGS REASONS
depression
of respiratory center
disorders of
respiratory muscles
thoracic cage
disorders
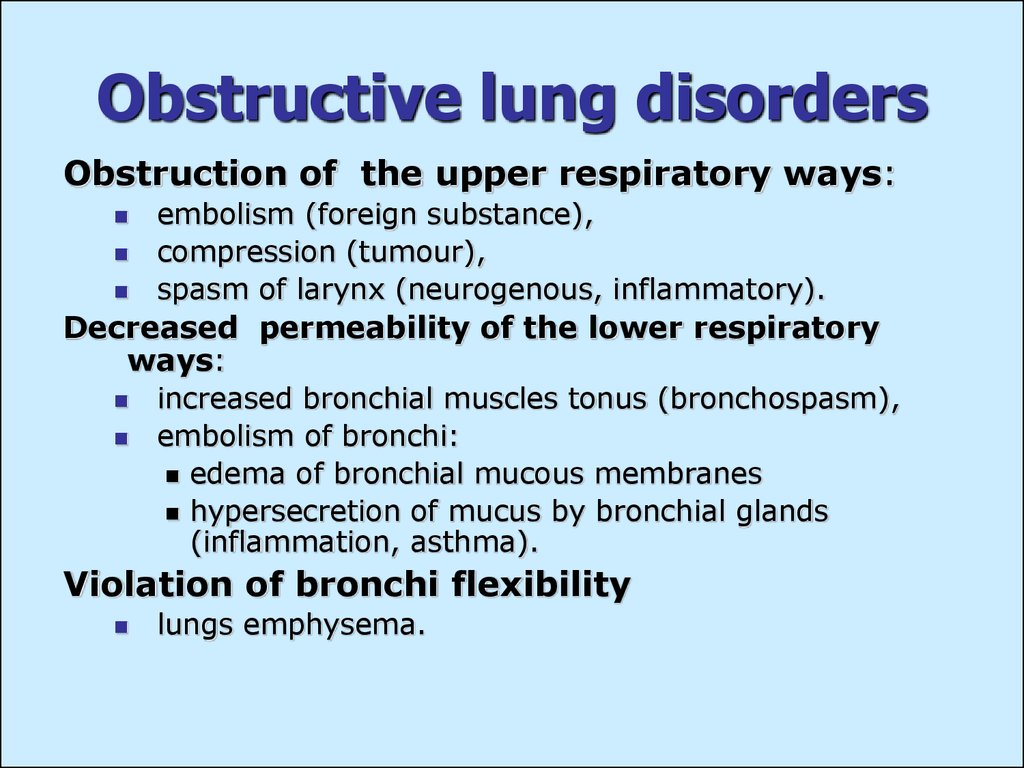
7. Obstructive lung disorders
Obstruction of the upper respiratory ways:embolism (foreign substance),
compression (tumour),
spasm of larynx (neurogenous, inflammatory).
Decreased permeability of the lower respiratory
ways:
increased bronchial muscles tonus (bronchospasm),
embolism of bronchi:
edema of bronchial mucous membranes
hypersecretion of mucus by bronchial glands
(inflammation, asthma).
Violation of bronchi flexibility
lungs emphysema.
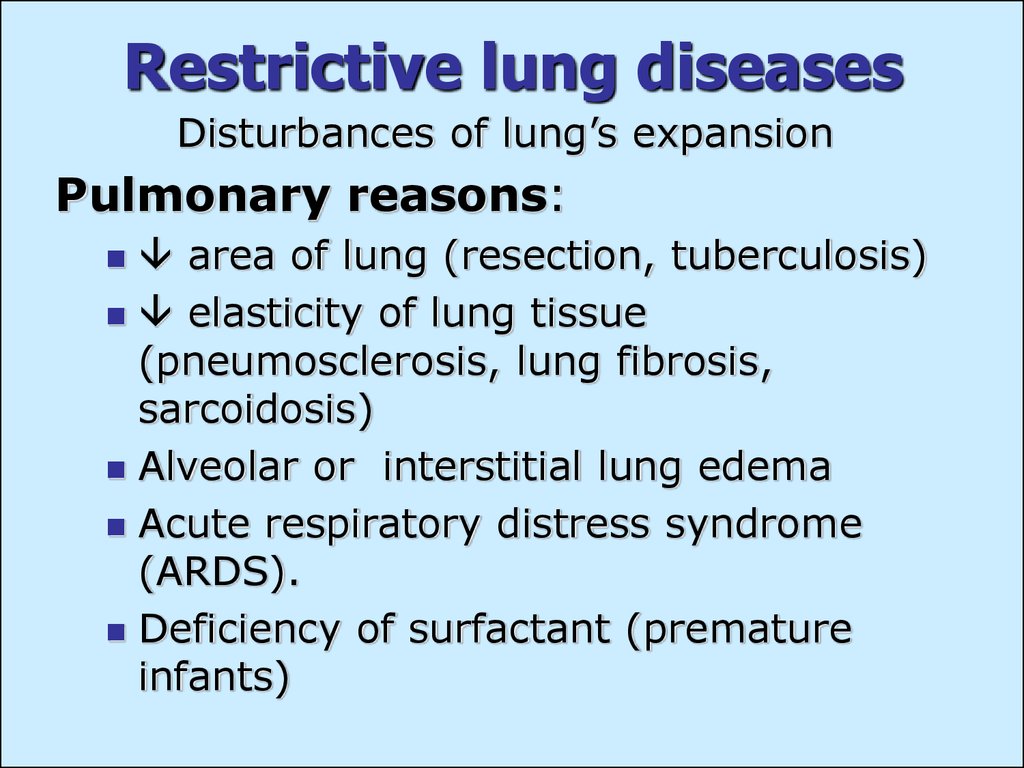
8. Restrictive lung diseases
Disturbances of lung’s expansionPulmonary reasons:
area of lung (resection, tuberculosis)
elasticity of lung tissue
(pneumosclerosis, lung fibrosis,
sarcoidosis)
Alveolar or interstitial lung edema
Acute respiratory distress syndrome
(ARDS).
Deficiency of surfactant (premature
infants)
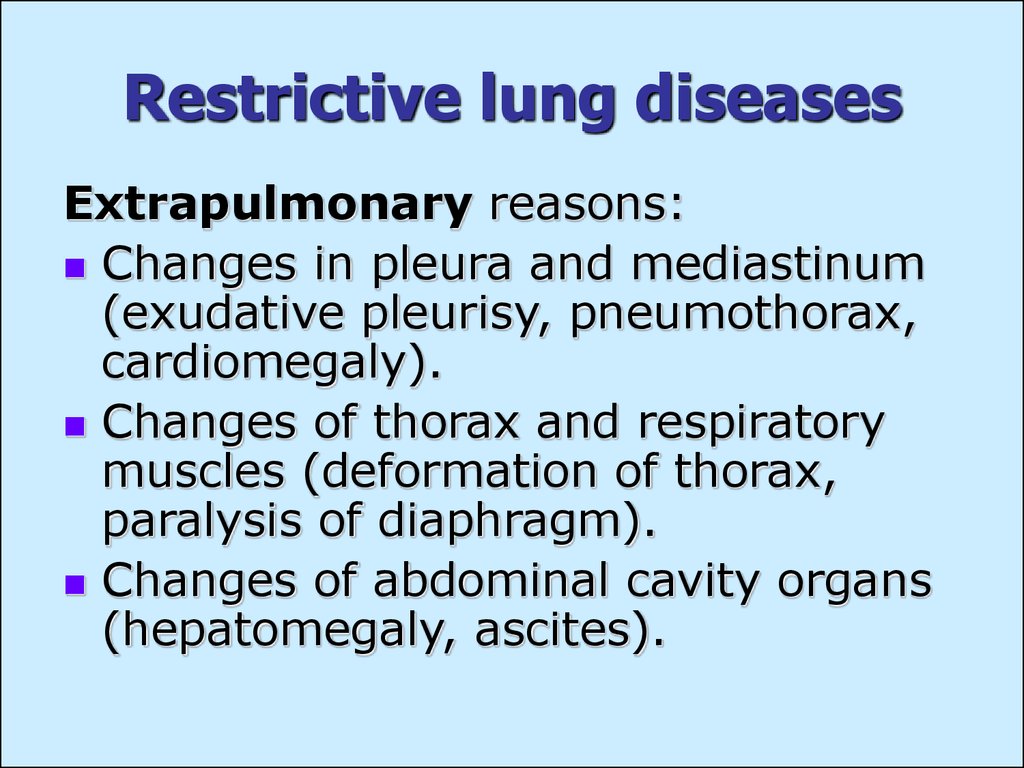
9. Restrictive lung diseases
Extrapulmonary reasons:Changes in pleura and mediastinum
(exudative pleurisy, pneumothorax,
cardiomegaly).
Changes of thorax and respiratory
muscles (deformation of thorax,
paralysis of diaphragm).
Changes of abdominal cavity organs
(hepatomegaly, ascites).
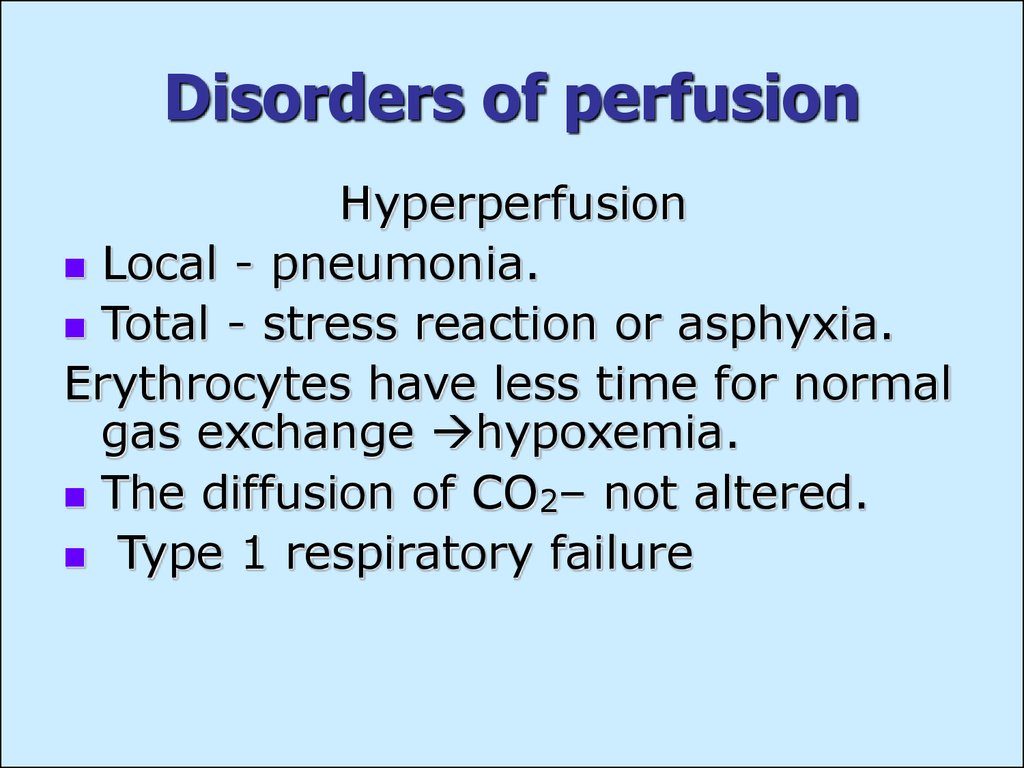
10. Disorders of perfusion
HyperperfusionLocal - pneumonia.
Total - stress reaction or asphyxia.
Erythrocytes have less time for normal
gas exchange hypoxemia.
The diffusion of CO2– not altered.
Type 1 respiratory failure
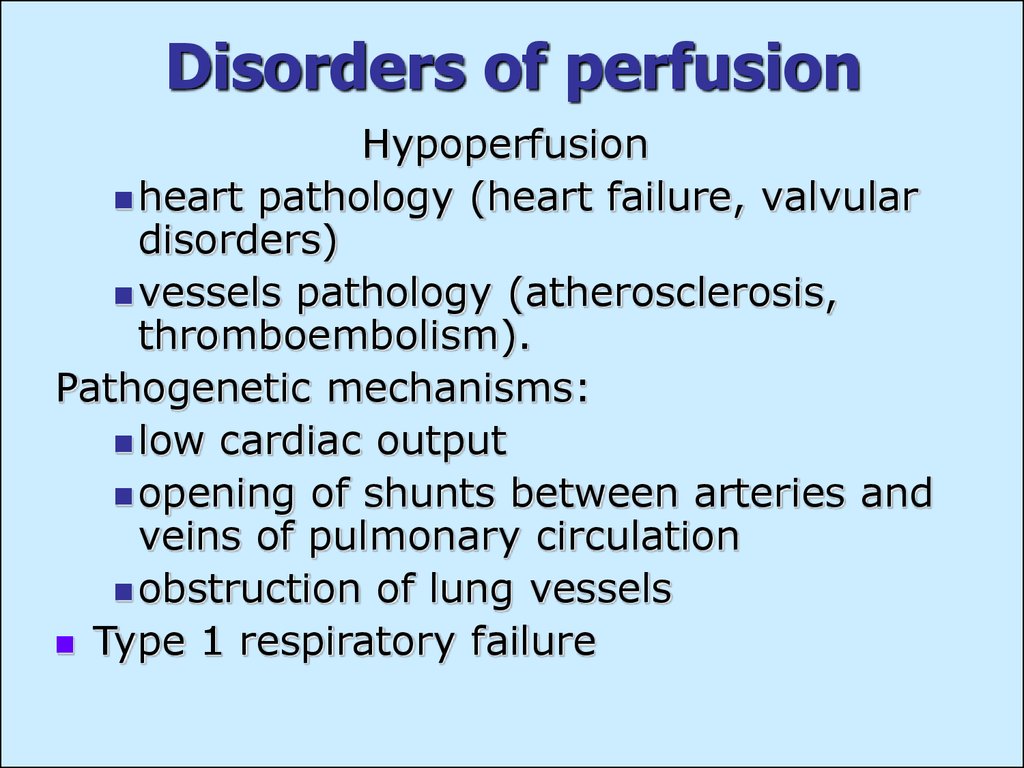
11. Disorders of perfusion
Hypoperfusionheart pathology (heart failure, valvular
disorders)
vessels pathology (atherosclerosis,
thromboembolism).
Pathogenetic mechanisms:
low cardiac output
opening of shunts between arteries and
veins of pulmonary circulation
obstruction of lung vessels
Type 1 respiratory failure
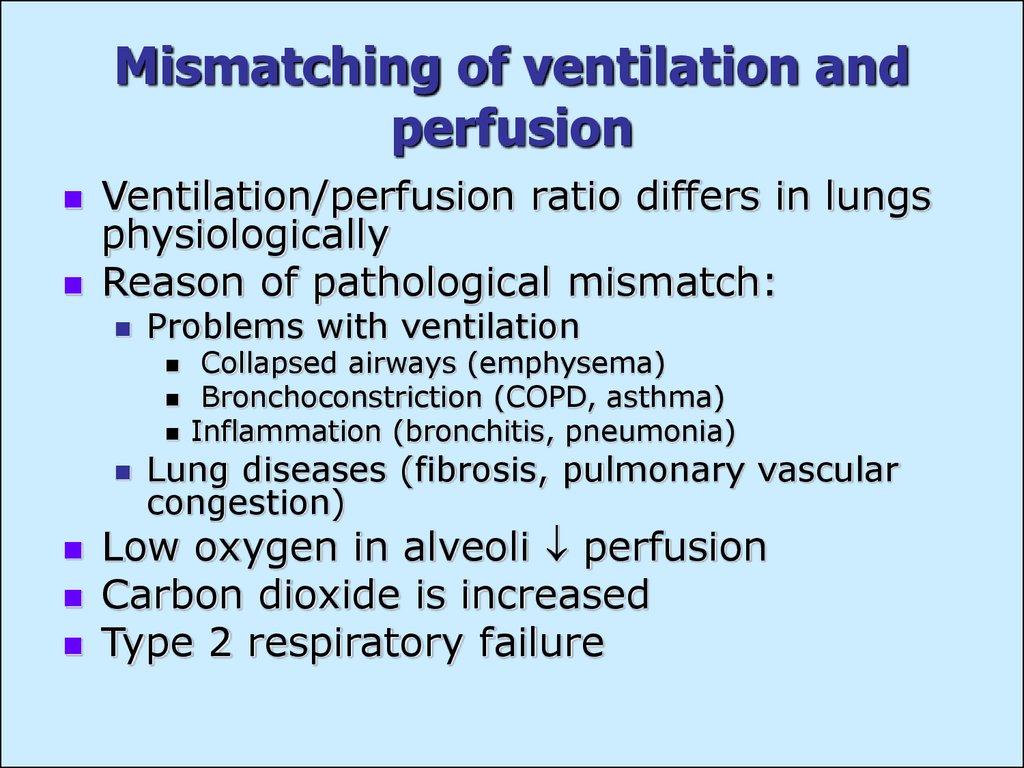
12. Mismatching of ventilation and perfusion
Ventilation/perfusion ratio differs in lungsphysiologically
Reason of pathological mismatch:
Problems with ventilation
Collapsed airways (emphysema)
Bronchoconstriction (COPD, asthma)
Inflammation (bronchitis, pneumonia)
Lung diseases (fibrosis, pulmonary vascular
congestion)
Low oxygen in alveoli perfusion
Carbon dioxide is increased
Type 2 respiratory failure
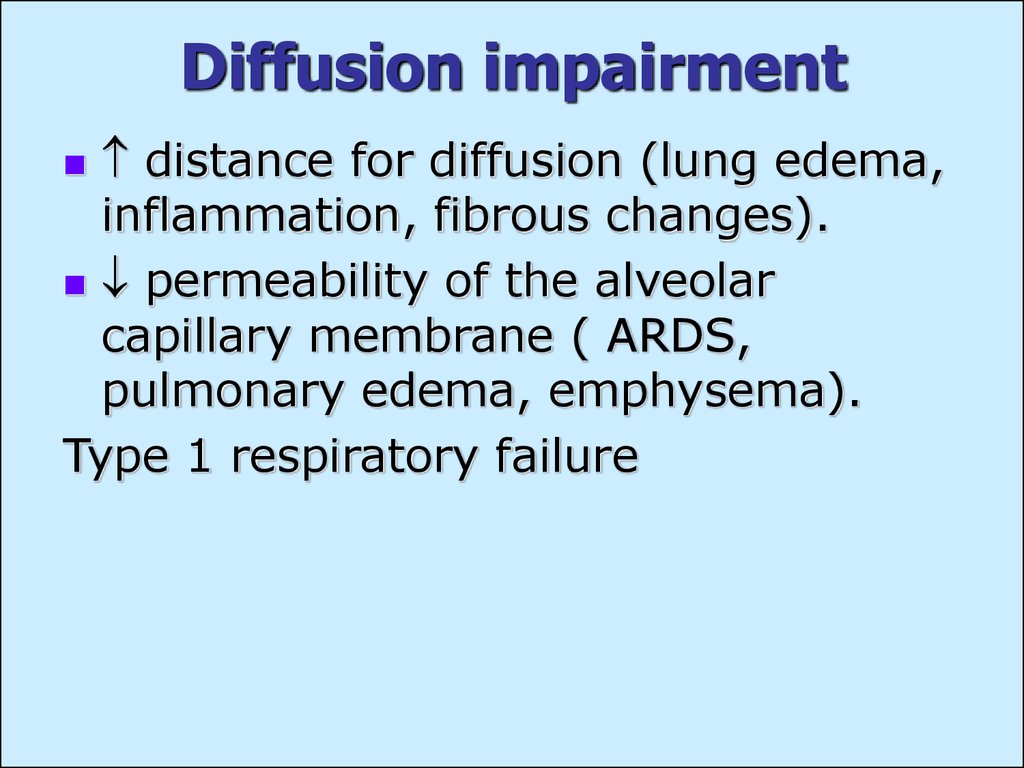
13. Diffusion impairment
distance for diffusion (lung edema,inflammation, fibrous changes).
permeability of the alveolar
capillary membrane ( ARDS,
pulmonary edema, emphysema).
Type 1 respiratory failure
14. Manifestations of respiratory failure
Hypoxemia - pO2 < 50 mm HgHypercapnia - pCO2 >50 mm Hg.
Hypoxemia Manifestations.
resulting from impaired function of
vital centers
resulting from activation of
compensatory mechanisms
15. Hypoxemia Manifestations
impairment of mental performanceand behavior
peripheral vasoconstriction
diaphoresis (sweating)
central or peripheral cyanosis
blood pressure
heart rate, hyperventilation
16. Hypercapnia Manifestations
pH and respiratory acidosiscompensated by renal bicarbonate
retention
vasodilating effect of CO2 :
increase in cerebral blood flow and cerebral
spinal fluid pressure (headache);
hyperemic conjunctivae;
warm and flushed skin.
Nervous system effects of CO2 progressive somnolence, disorientation,
coma.
17. Acute respiratory distress syndrome (ARDS)
Causesaspiration of gastric contents, toxic
gases
trauma (with or without fat emboli),
sepsis
acute pancreatitis
pneumonia, alveolar bleedings
reactions to drugs and toxins.
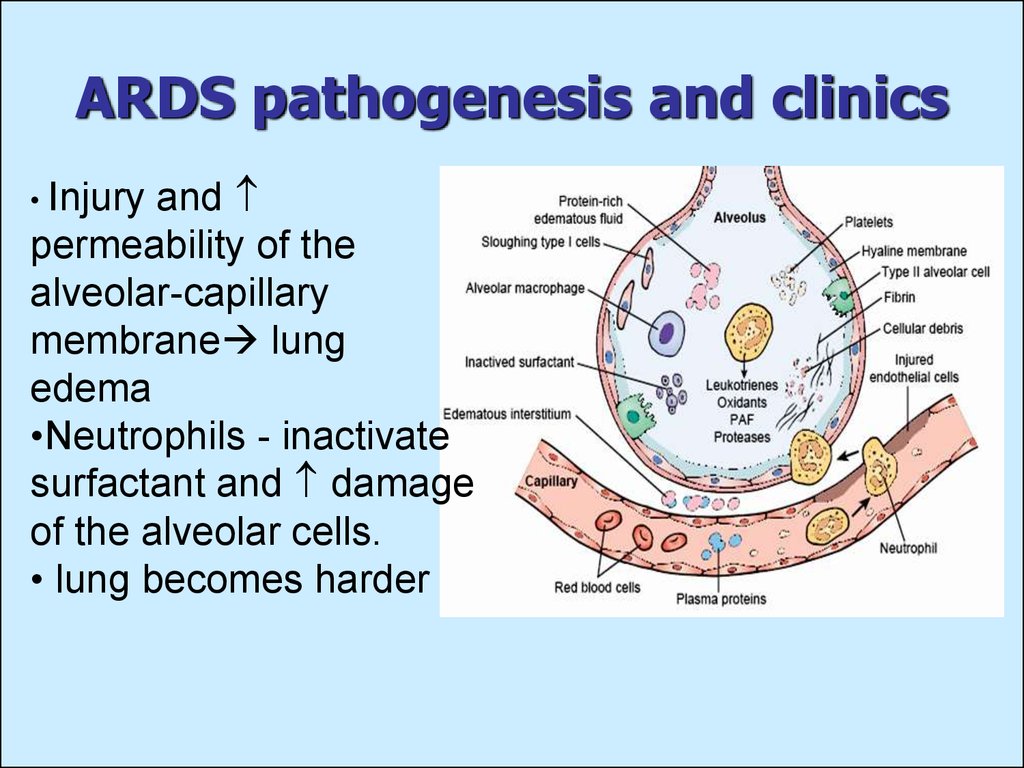
18. ARDS pathogenesis and clinics
andpermeability of the
alveolar-capillary
membrane lung
edema
•Neutrophils - inactivate
surfactant and damage
of the alveolar cells.
• lung becomes harder
• Injury
19. ARDS clinical manifestation
rapid onset, 12 to 18 hours afterinitial event
in respiratory rate
signs of respiratory failure
diffuse bilateral consolidation of the
lung tissue
marked hypoxemia
multiple organ failure (kidneys, GIT,
CNS, and cardiovascular system)
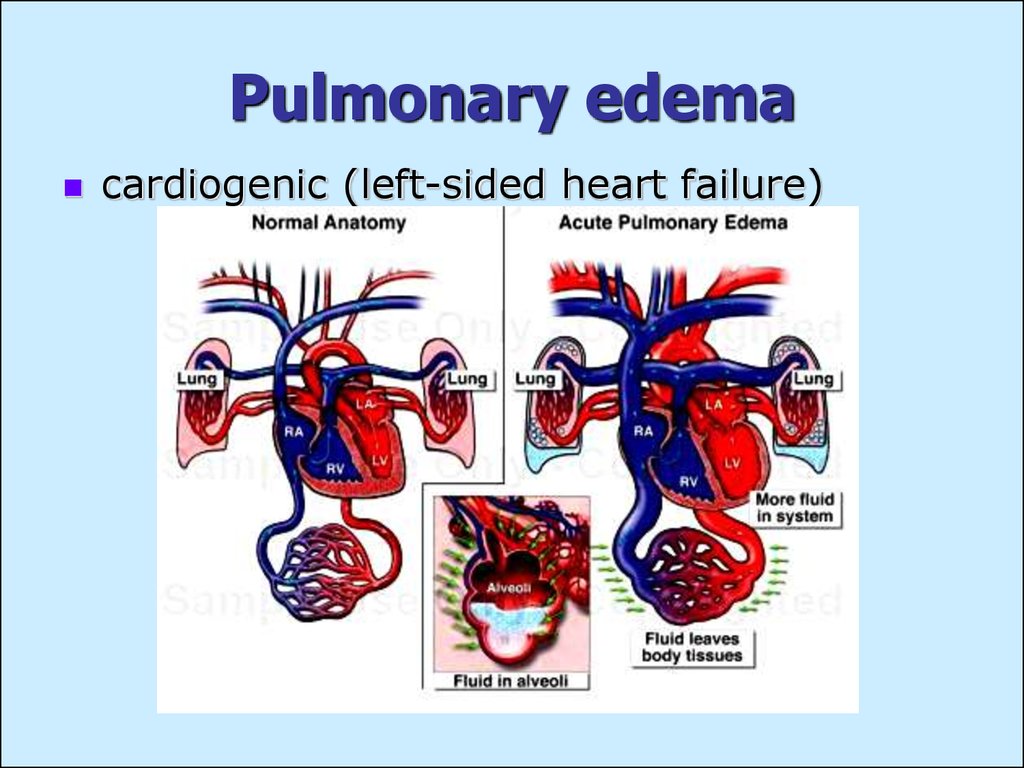
20. Pulmonary edema
cardiogenic (left-sided heart failure)21. Non-cardiogenic pulmonary edema
alveolar walls damage by toxic compounds(Phosporus), proteolytic enzymes (a.
pancreatitis)
microbe affection of lungs (local – bacterial
pneumonia, systemic – sepsis)
quick intravenous infusion of big amount of
fluid (physiological solution, blood substitutes)
– due to ”blood dilution”
anaphylactic allergic reaction – due to BAS
influence
catecholamines – generalized
vasoconstriction lung hypertension and
blood congestion.
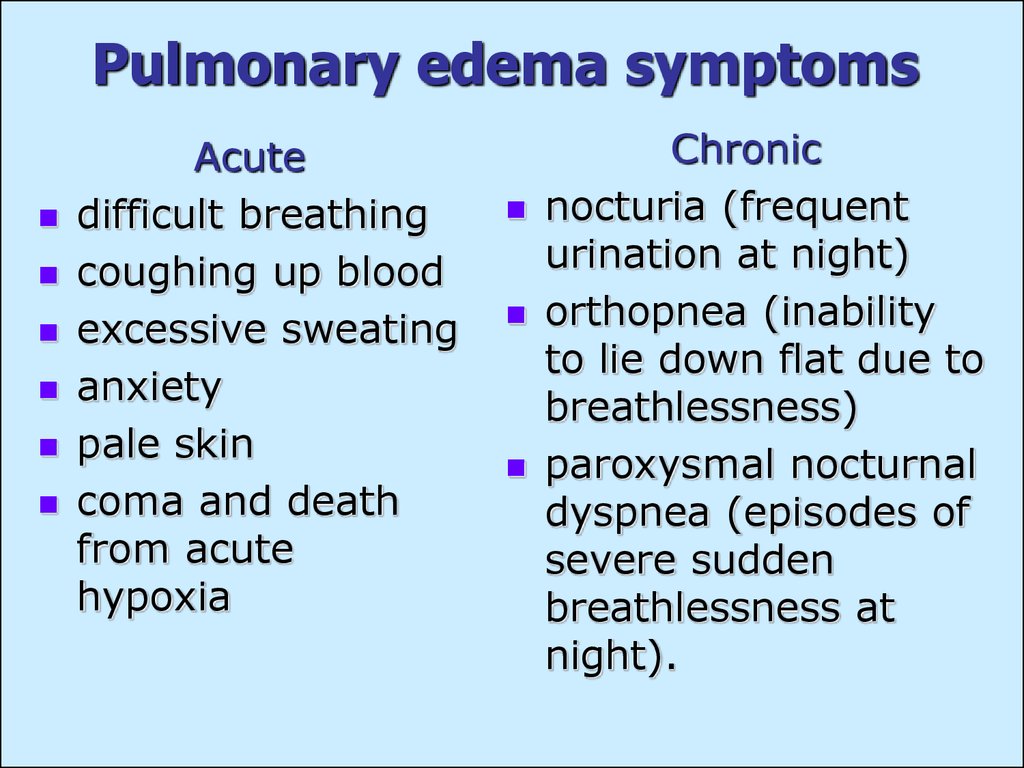
22. Pulmonary edema symptoms
Acutedifficult breathing
coughing up blood
excessive sweating
anxiety
pale skin
coma and death
from acute
hypoxia
Chronic
nocturia (frequent
urination at night)
orthopnea (inability
to lie down flat due to
breathlessness)
paroxysmal nocturnal
dyspnea (episodes of
severe sudden
breathlessness at
night).
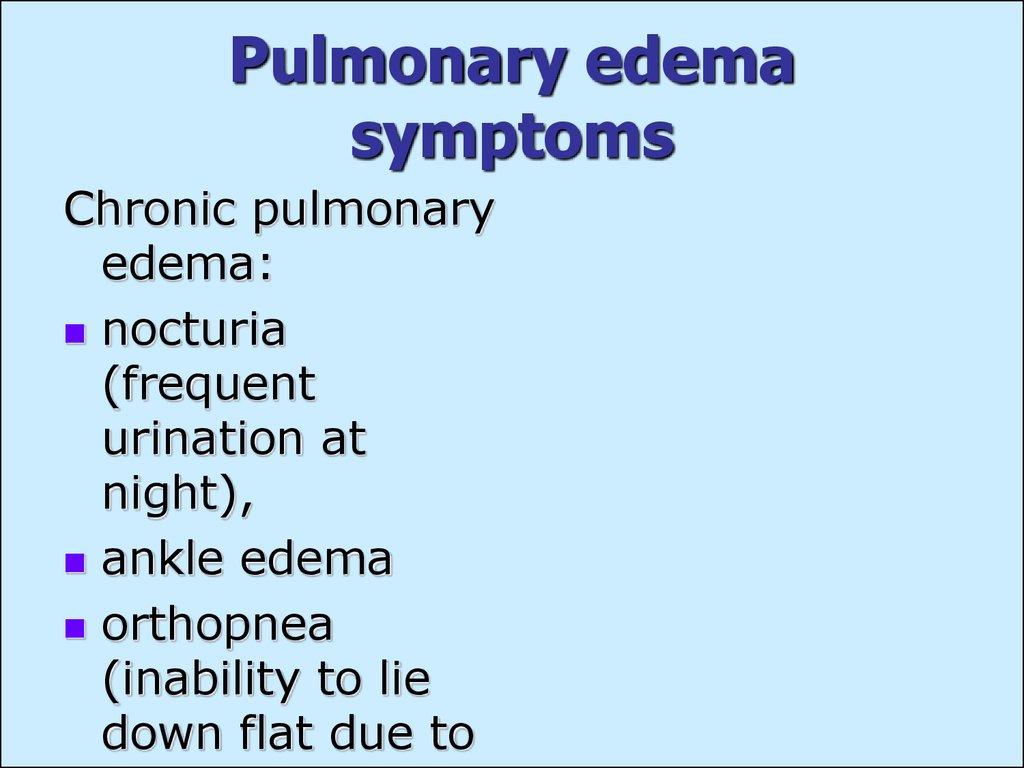
23. Pulmonary edema symptoms
Chronic pulmonaryedema:
nocturia
(frequent
urination at
night),
ankle edema
orthopnea
(inability to lie
down flat due to
24. Short breath (dyspnea)
violation of frequency, depth, rhythmof breath
changes of respiratory movements
“air hunger”
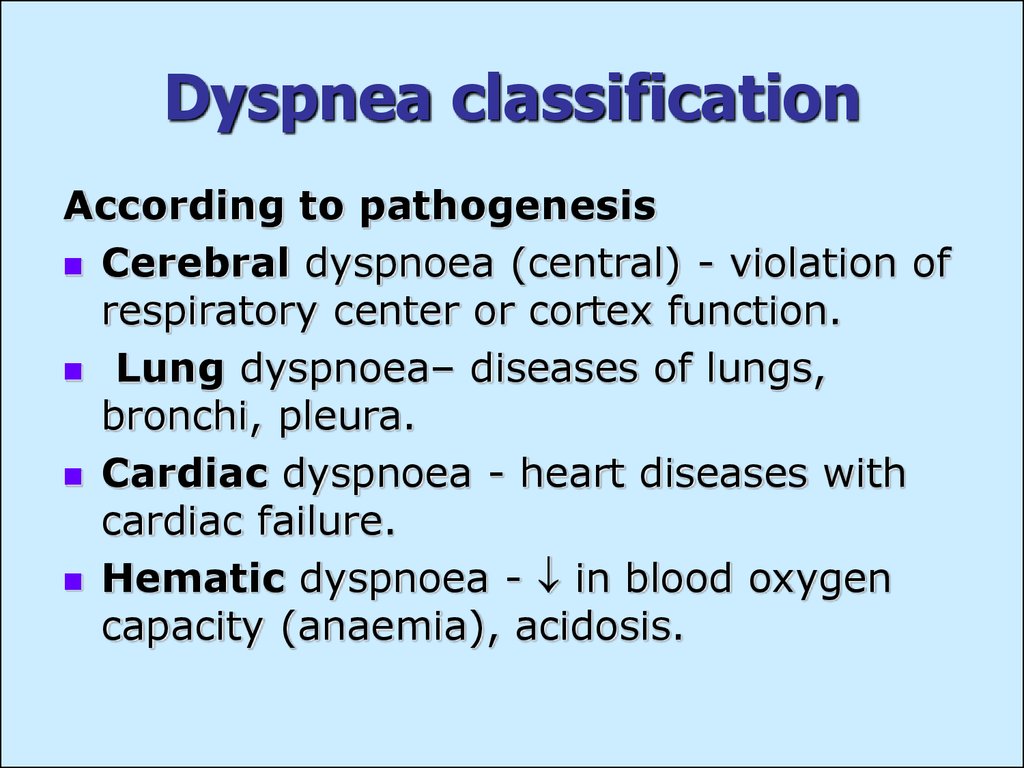
25. Dyspnea classification
According to pathogenesisCerebral dyspnoea (central) - violation of
respiratory center or cortex function.
Lung dyspnoea– diseases of lungs,
bronchi, pleura.
Cardiac dyspnoea - heart diseases with
cardiac failure.
Hematic dyspnoea - in blood oxygen
capacity (anaemia), acidosis.
26. Dyspnea classification
Due to dyspnea character:Hyperpnea
Tachypnea
Bradypnea
Apnoea
Due to altered phase of respiration:
Inspiratory dyspnea
Expiratory dyspnea
Mixed dyspnoea
27. Dyspnoe mechanisms
Humoral – increase of pCO2 anddecrease of pO2, shift of pH to the
acid side.
Neuroregulatory – violated
impulsion from chemoreceptors
and baroreceptors.
Central – dysfunction of respiratory
center, or cortex neurons.
28. Cerebral dyspnea
Excitation of respiratory centre - frequentdeep respiration.
Inhibition of respiratory center - frequent
superficial respiration.
Periodic breathing appears at brain
affections by:
trauma
stroke
tumour
inflammation
endogenous and exogenous intoxications
29. Cheyne-Stokes respiration
failure of the respiratory centerbigger concentrations of CO2 are needed
for the excitation of respiratory centre.
causes: strokes, head injuries or brain
tumors, congestive heart failure, morphine
administration.
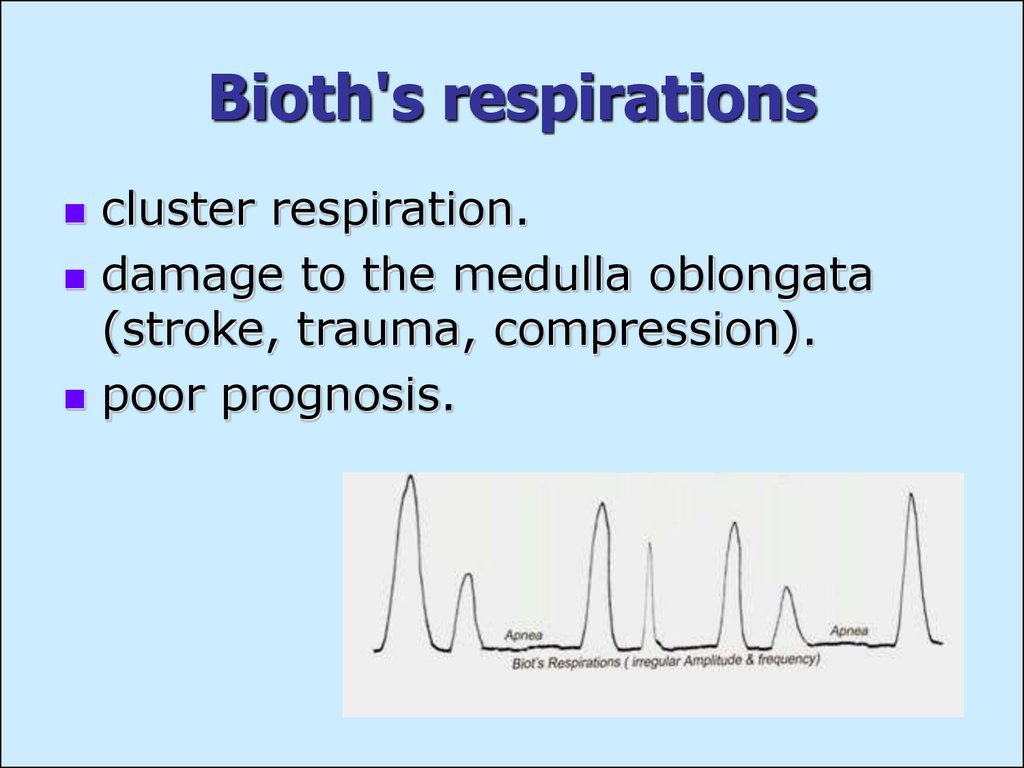
30. Bioth's respirations
cluster respiration.damage to the medulla oblongata
(stroke, trauma, compression).
poor prognosis.
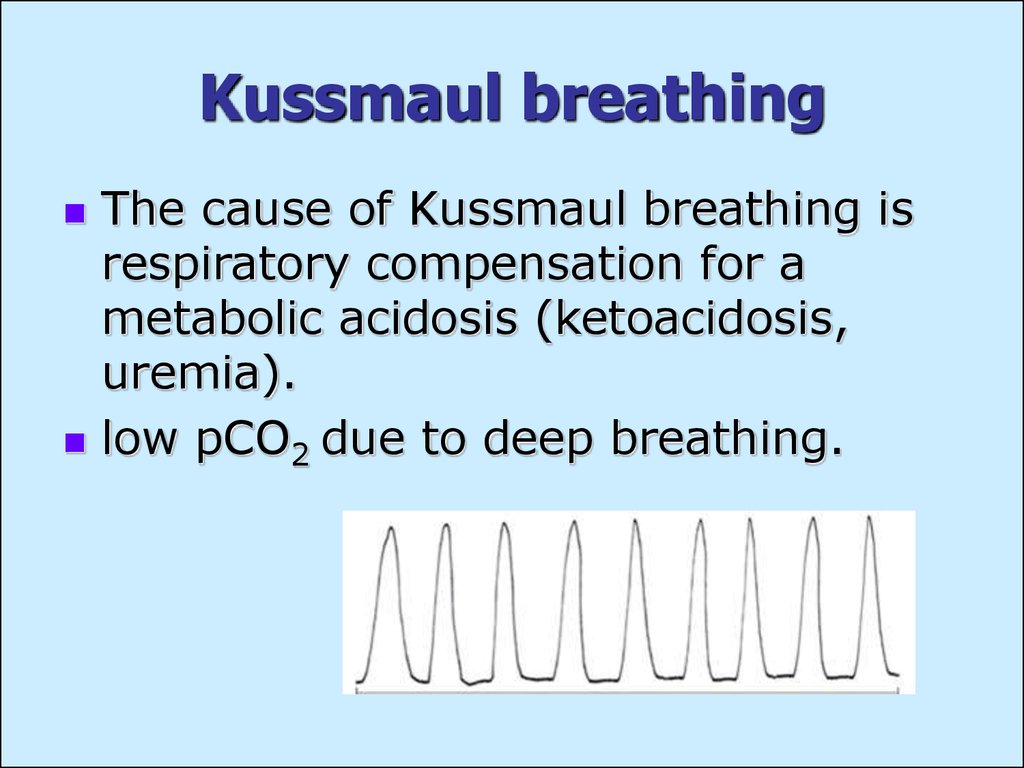
31. Kussmaul breathing
The cause of Kussmaul breathing isrespiratory compensation for a
metabolic acidosis (ketoacidosis,
uremia).
low pCO2 due to deep breathing.
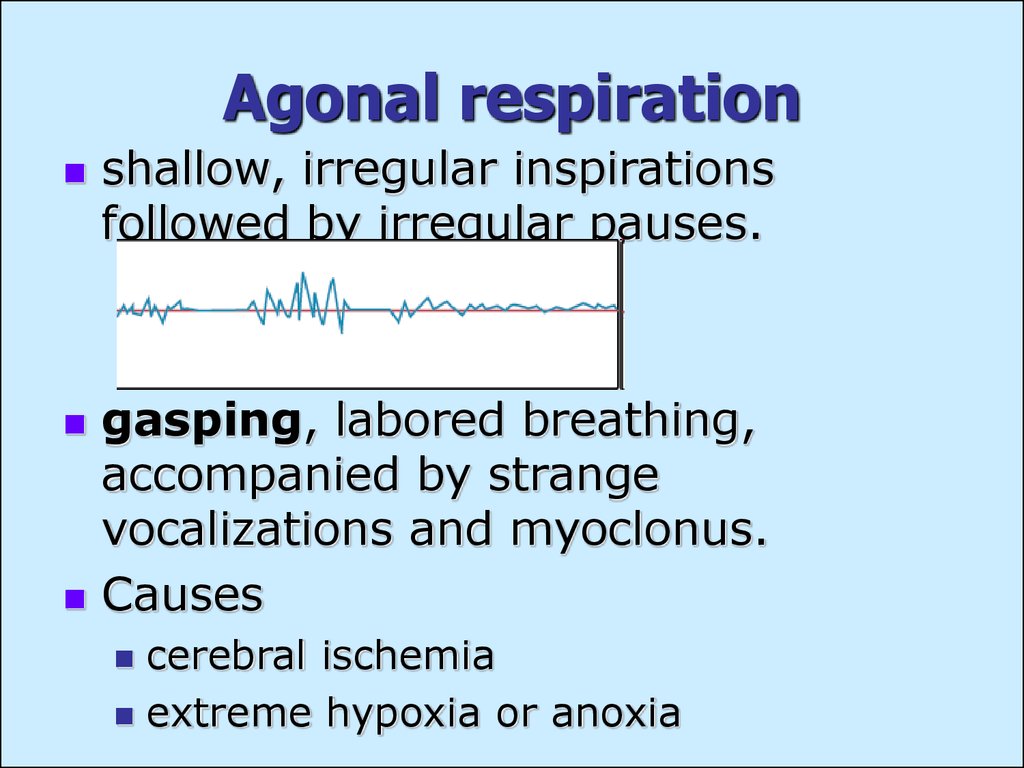
32. Agonal respiration
shallow, irregular inspirationsfollowed by irregular pauses.
gasping, labored breathing,
accompanied by strange
vocalizations and myoclonus.
Causes
cerebral ischemia
extreme hypoxia or anoxia
33. Other dyspnea types
Lungs dyspneaCardiac dyspnea
Embolism or narrowing of upper respiratory
ways (stenotic breath)
bronchial asthma (expiratory dyspnoea)
pneumonia, pleurisy
cardiac failure, heart valves pathology
Hematic dyspnea
anemia
metHb formation (CO poisoning).
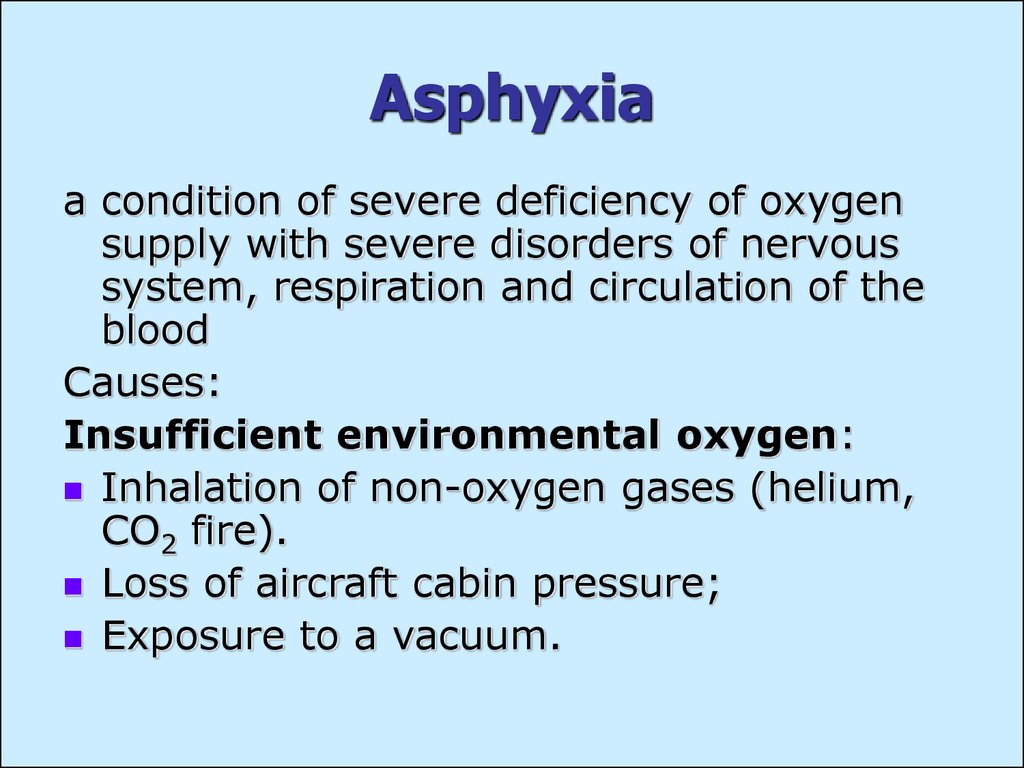
34. Asphyxia
a condition of severe deficiency of oxygensupply with severe disorders of nervous
system, respiration and circulation of the
blood
Causes:
Insufficient environmental oxygen:
Inhalation of non-oxygen gases (helium,
CO2 fire).
Loss of aircraft cabin pressure;
Exposure to a vacuum.
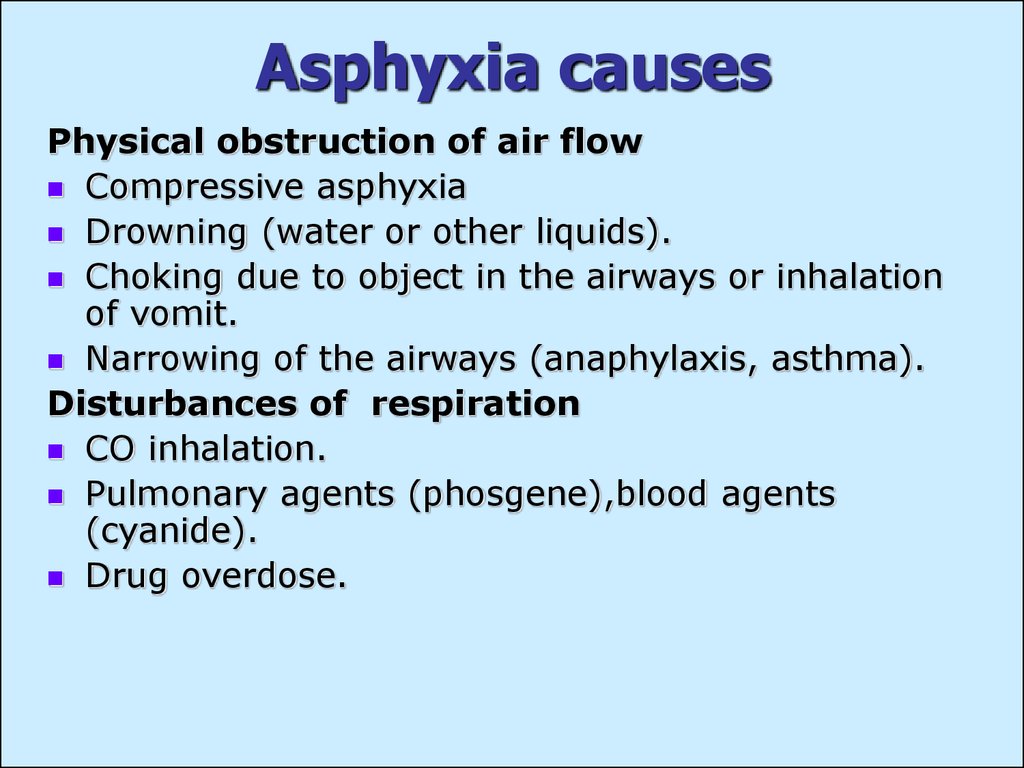
35. Asphyxia causes
Physical obstruction of air flowCompressive asphyxia
Drowning (water or other liquids).
Choking due to object in the airways or inhalation
of vomit.
Narrowing of the airways (anaphylaxis, asthma).
Disturbances of respiration
CO inhalation.
Pulmonary agents (phosgene),blood agents
(cyanide).
Drug overdose.
36. Asphyxia stages
1st stage - frequency of breathing, BPand heart rate - phase of inspiratory
dyspnea – compensation of acute hypoxia.
2nd stage- more rare respiration with
enforced expiration, slowing-down of heart
rate and BP - phase of expiratory
dyspnea.
3rd stage - temporary (from several
seconds to several minutes) stopping of
breathing (preterminal pause); low BP,
reflexes, loss of consciousness.
4th stage - terminal or agonal breathing
(rare deep convulsive «sighs» during
several minutes); respiratory centre
paralysis and death.
37. Lung volumes measurement
Forced expiratory volume in one second(FEV1) is the 1-s-volume exhaled with forceful
pressure from maximal inspiration.
Forced vital capacity (FVC) is the maximum
amount of air forcibly expired after maximum
inspiration.
Total lung capacity (TLC) is the total volume of
air in the lungs, when they are maximally
inflated.
Residual volume (RV) the volume of air left in
the lungs after a maximal expiration.
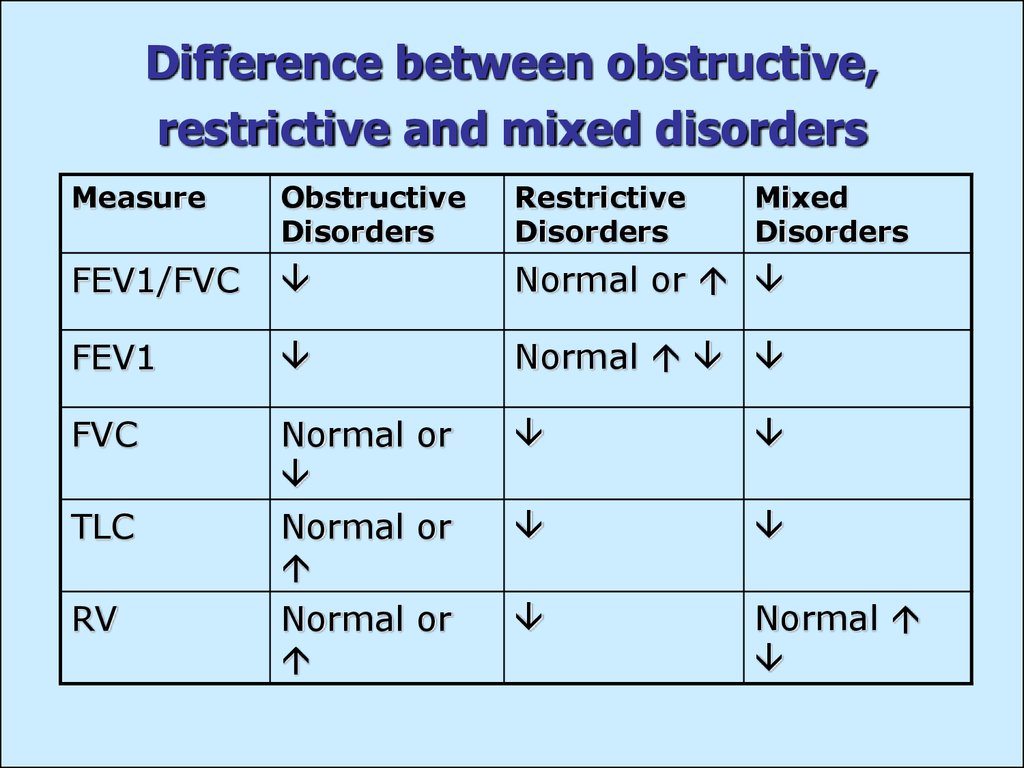
38. Difference between obstructive, restrictive and mixed disorders
MeasureObstructive
Disorders
Restrictive
Disorders
Mixed
Disorders
FEV1/FVC
Normal or
FEV1
Normal
FVC
Normal or
TLC
Normal or
RV
Normal or
Normal



 Медицина
Медицина Биология
Биология








