Похожие презентации:
Systemic Lupus Erythematosus
1. Systemic Lupus Erythematosus
2. History
• 1948 – Malcolm Hargraves discovers thelupus erythematosus (LE) cell.
• 1957 – The first anti-DNA antibody is
identified.
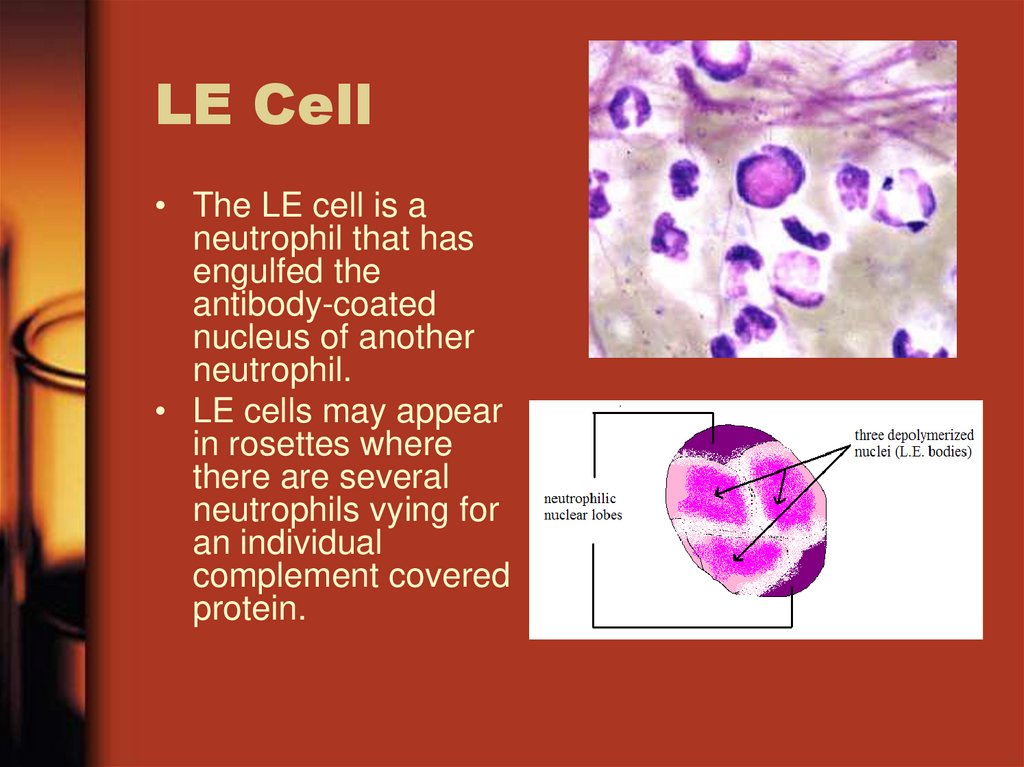
3. LE Cell
• The LE cell is aneutrophil that has
engulfed the
antibody-coated
nucleus of another
neutrophil.
• LE cells may appear
in rosettes where
there are several
neutrophils vying for
an individual
complement covered
protein.
4. Genetic Associations
• HLA’s are loci on genes that codefor certain β chain on the MHC
complex
• HLA-DR2
• HLA-DR3
• HLA-DQB1 – Involved in mediating
production of antibodies to ds-DNA
5. Symptoms
• Non-specific:–
–
–
–
–
–
Fatigue
Weight loss
Malaise = generally feeling ill
Fever
Anorexia (over time)
Arthritis
• 90% of patients experience arthritic symptoms
• Symmetrical
• Appears in hands, wrists, and knees mainly
6. Skin Manifestations
• Malar or ButterflyRash
• Discoid Rash –
Stimulated by UV
light
• Skin
manifestations
only appear in 3040% of lupus
patients.
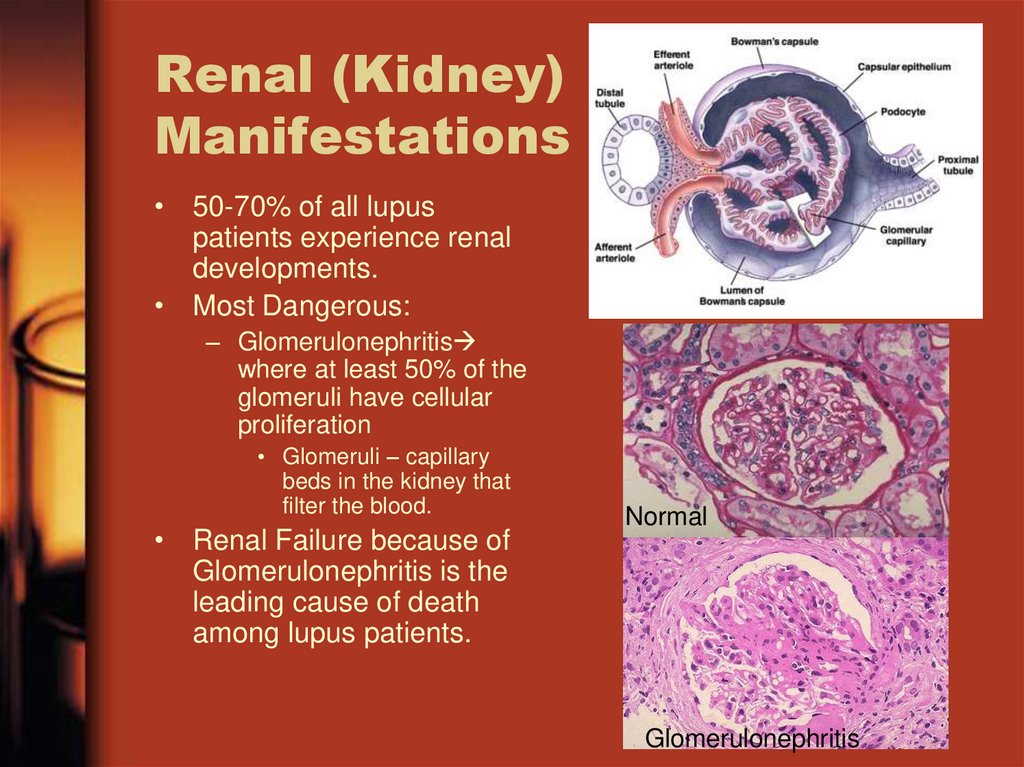
7. Renal (Kidney) Manifestations
• 50-70% of all lupuspatients experience renal
developments.
• Most Dangerous:
– Glomerulonephritis
where at least 50% of the
glomeruli have cellular
proliferation
• Glomeruli – capillary
beds in the kidney that
filter the blood.
• Renal Failure because of
Glomerulonephritis is the
leading cause of death
among lupus patients.
Normal
Glomerulonephritis
8. Other Manifestations
• Cardiac• Central Nervous System
• Hematological
9. Main Pathology
• The plasma cells are producingantibodies that are specific for self
proteins, namely ds-DNA
• Overactive B-cells
• Suppressed regulatory function in T-cells
• Lack of T-cells
• Activation of the Complement system
10. Overactive B-cells
• Estrogen is a stimulator of B-cell activity– Lupus is much more prevalent in females of
ages 15-45
• Height of Estrogen production
• IL-10, also a B-cell stimulator is in high
concentration in lupus patient serum.
– High concentration linked to cell damage
caused by inflammation
11. T-cell Malfunctions
• Fc region switch– ζ εγ
– Leads to malfunction in signaling and
decreased IL-2 production
• Increased levels of Ca2+
– Leads to spontaneous apoptosis
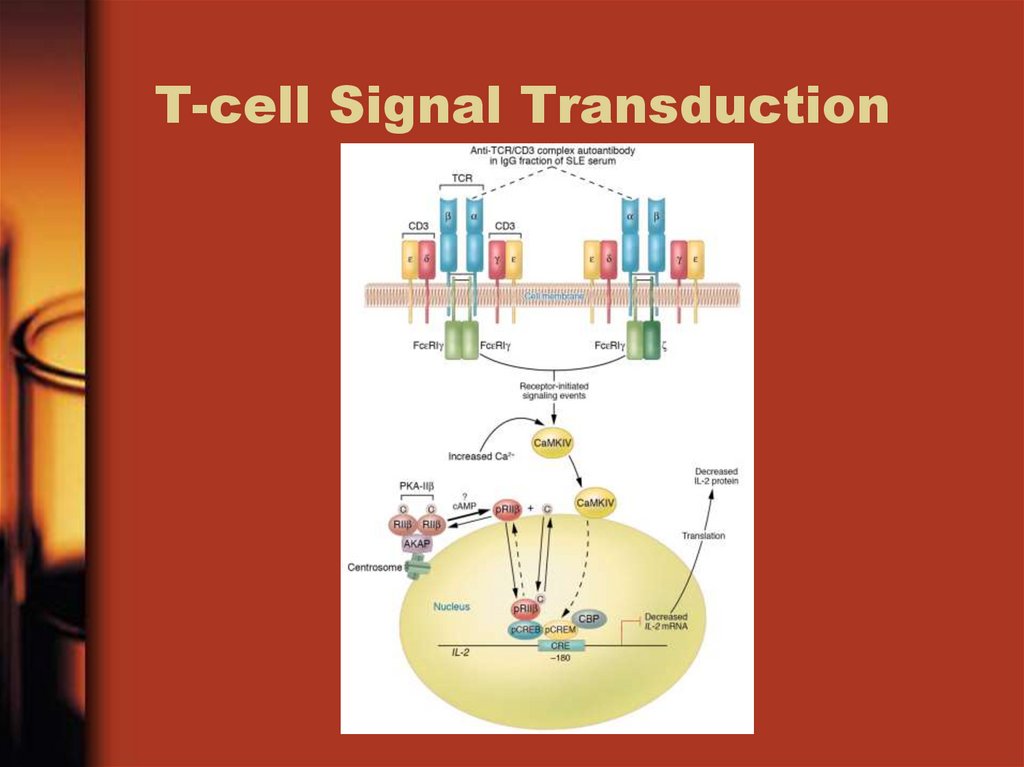
12. T-cell Signal Transduction
13. Activation of Complement System
• Complement system is activated bythe binding of antibodies to foreign
debris.
– In this case its over activation
• RBCs lack CR1 receptor
– Decreasing the affective removal of
complexes
14. IgG Pathogen
• IgG is the most “pathogenic”because it forms intermediate sized
complexes that can get to the small
places and block them.
15. DNA is the Main man
• DNA is the main antigen for whichantibodies are formed.
• Extracellular DNA has an affinity for
basement membrane where it is
bound by autoantibodies.
• Classical thickening of the basement
membrane
16. Testing
• ESR• Urinalysis
• Complement Test
– Tests levels of C3, C4, CH50
– Low levels indicates possible presence of
disease
• FANA – Fluorescent antinuclear antibody
• Ouchterlony Test – shows interactions
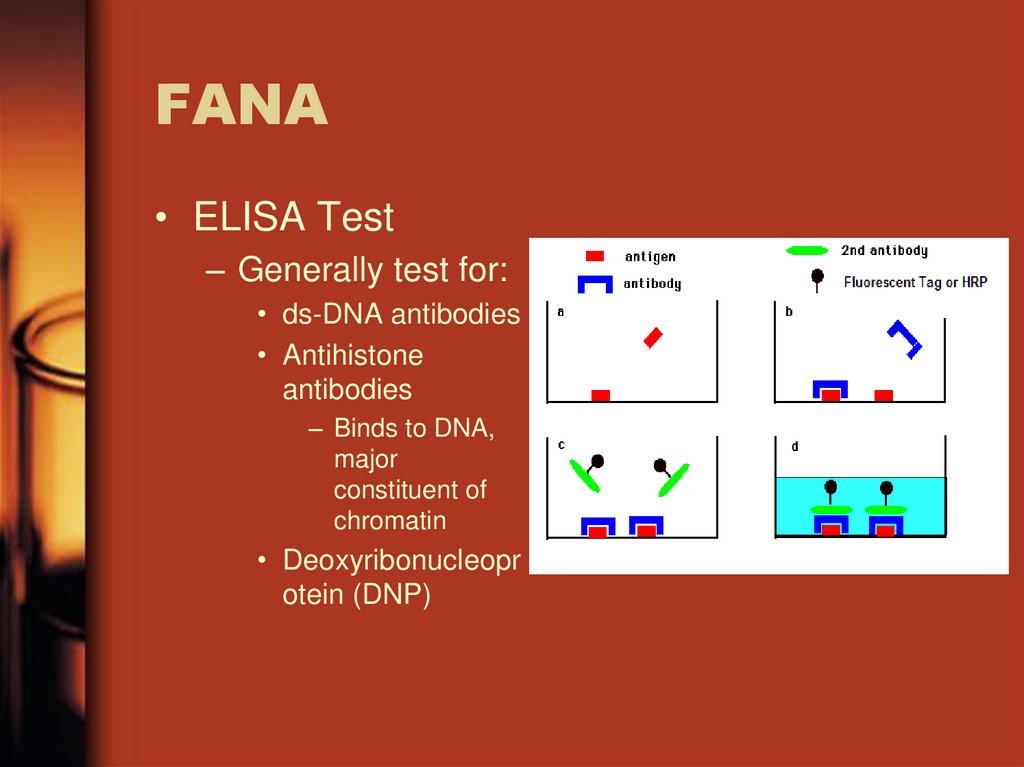
17. FANA
• ELISA Test– Generally test for:
• ds-DNA antibodies
• Antihistone
antibodies
– Binds to DNA,
major
constituent of
chromatin
• Deoxyribonucleopr
otein (DNP)
18. Ouchterlony Test
• Used to determineimmunological
specificity
• Rules out a false
positive
• Shows the serum
does or does not
have antinuclear
antibodies
19. Summary
• Lupus = Autoimmunity– Systemic and affects connective tissue
• Caused by malfunctions of:
–
–
–
–
T-cells
B-cells
Complement System
Signal Transduction
• Can be lethal or not
• Unique to each individual