Похожие презентации:
Atopic dermatitic. Definition
1. Atopic dermatitic
2. Definition
Atopic dermatitis is a chronic, pruriticinflammatory skin disease that occurs most
frequently in children, but can also affect
adults. It follows a relapsing course.
often associated with elevated serum
immunoglobulin (IgE) levels and a personal or
family history of type I allergies, allergic
rhinitis, and asthma.
Atopic eczema is synonymous with AD.
3. Epidemiology
affects up to 25% of children and 2–3% ofadults
onset is most common between 3 and 6 months
of age
approximately 60% of patients develop the
eruption in the first year of life and 90% by 5
years of age
Majority have resolution by adulthood, 10 to
30% develop symptoms as adults
4. Pathogenesis
complexgenetic, immunologic, and environmental
factors
dysfunctional skin barrier and dysregulation of
the immune system
5. risk factors
family history of atopy - 70%; develops 2- 3-fold higher in oneatopic parent, 3-5-fold if both parents are atopic; maternal history
- more predictive
loss of function mutations in the filaggrin (FLG) gene encoding
profilaggrin (degradation products - filaggrin monomers - key
roles in the terminal differentiation of the epidermis and
formation of the skin barrier including the stratum corneum)
Filaggrin breakdown products are part of natural moisturizing
factor, which contributes to epidermal hydration and barrier
function.
FLG null mutations confer a risk for earlier-onset AD, and for
more severe, persistent disease
most studies of dietary modification of the maternal or infant diet
do not show a protective effect, except breastfeeding for the first 6
months
6. clinical findings
ErythemaEdema
Xerosis
erosions/excoriations
oozing and crusting, and lichenification
vary by patient age and chronicity of lesions
Pruritus is a hallmark of the condition that is
responsible for much of the disease burden
borne by patients and their families.
7. Essential features— must be present
PruritusEczema (acute, subacute, chronic)
Typical morphology and age specific patterns:
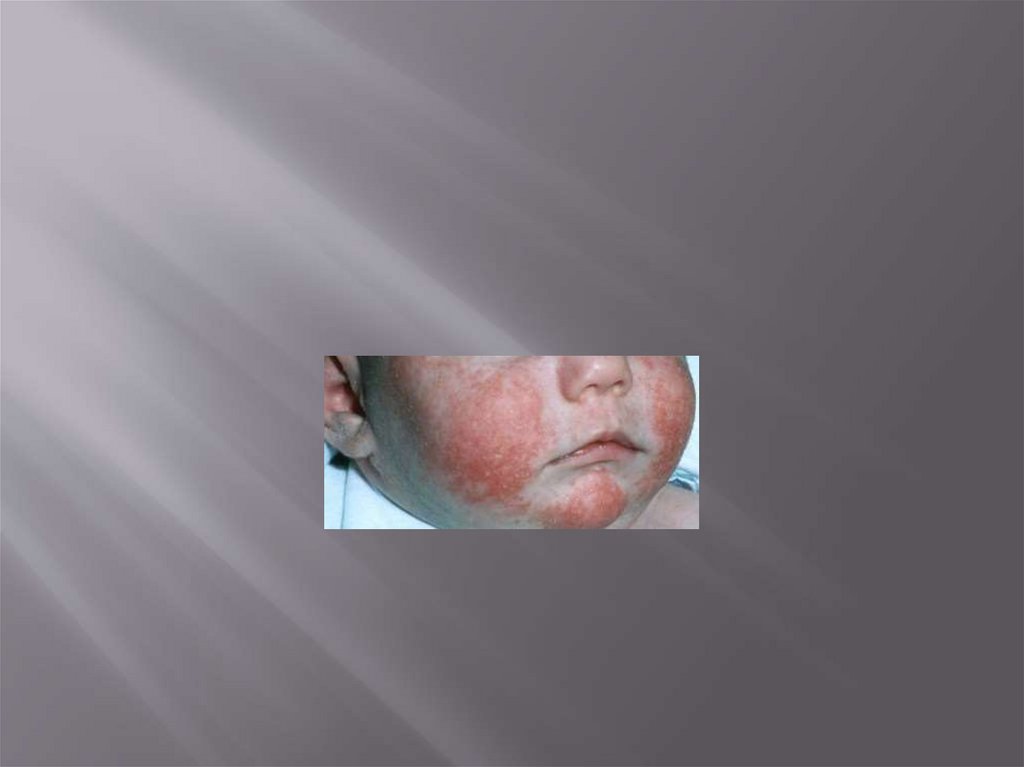
1. Facial, neck, and extensor involvement in infants
and children
2. Current or previous flexural lesions in any age
group
3. Sparing of the groin and axillary regions
Chronic or relapsing history
8.
9.
10. Important features
seen in most cases, adding support to thediagnosis:
• Early age of onset
• Atopy
• Personal and/or family history
• Immunoglobulin E reactivity
• Xerosis
11. Associated features
help to suggest the diagnosis of atopicdermatitis but are too nonspecific to be used
for defining or detecting atopic dermatitis for
research and epidemiologic studies:
• Atypical vascular responses (facial pallor,
white dermographism, delayed blanch
response)
• Keratosis pilaris/ pityriasis alba/ hyperlinear
palms/ icthyosis
• Ocular/periorbital changes
• Perifollicular accentuation/ lichenification/
prurigo lesions
12. Exclusionary conditions
• Scabies• Seborrheic dermatitis
• Contact dermatitis (irritant or allergic)
• Icthyoses
• Cutaneous T-cell lymphoma
• Psoriasis
• Photosensitivity dermatoses
• Immune deficiency diseases
• Erythroderma of other causes
13.
Patients with presumed atopic dermatitisshould have their diagnosis based on the
criteria summarized above
skin biopsy or other tests (such as serum IgE,
potassium hydroxide (KOH) preparation,
patch testing, and/or genetic testing) may be
helpful to rule out other or associated skin
conditions.
14. Common associations/comorbidities
food allergies, asthma, and allergicrhinitis/rhinoconjunctivitis.
AD can be the start of the “atopic march,” given the
frequent subsequent development of one or more of
the other atopic conditions.
Sleep disturbance - common due to significant itch
Depression, attention deficit hyperactivity disorder
(ADHD) in children
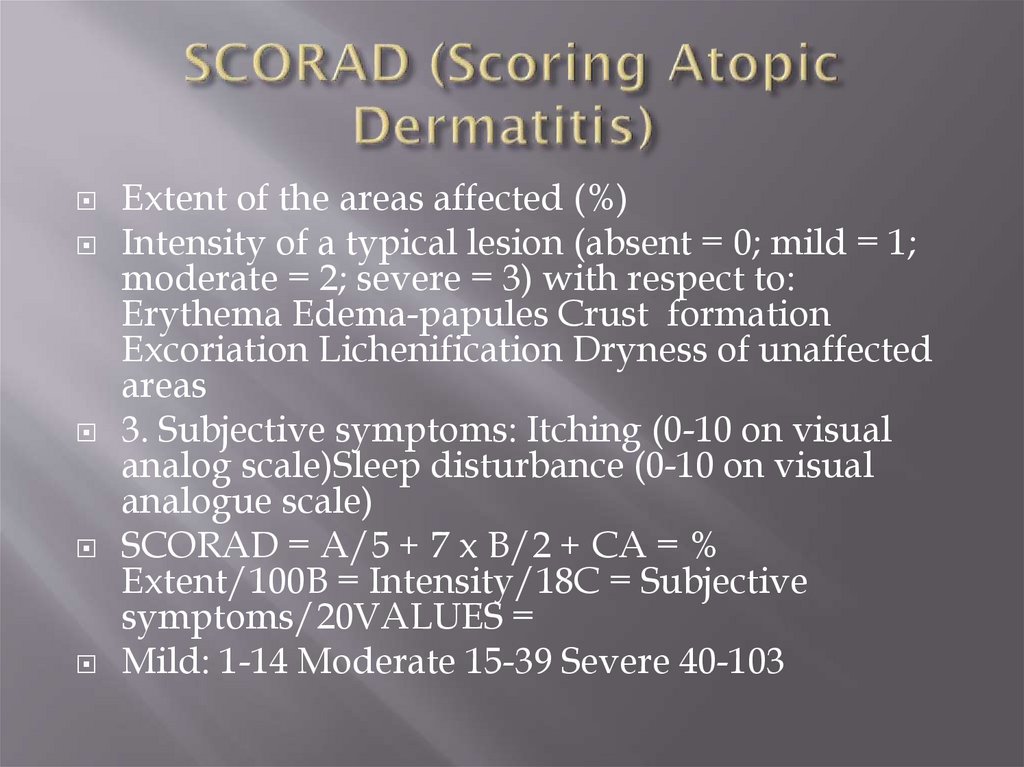
15. SCORAD (Scoring Atopic Dermatitis)
Extent of the areas affected (%)Intensity of a typical lesion (absent = 0; mild = 1;
moderate = 2; severe = 3) with respect to:
Erythema Edema-papules Crust formation
Excoriation Lichenification Dryness of unaffected
areas
3. Subjective symptoms: Itching (0-10 on visual
analog scale)Sleep disturbance (0-10 on visual
analogue scale)
SCORAD = A/5 + 7 x B/2 + CA = %
Extent/100B = Intensity/18C = Subjective
symptoms/20VALUES =
Mild: 1-14 Moderate 15-39 Severe 40-103
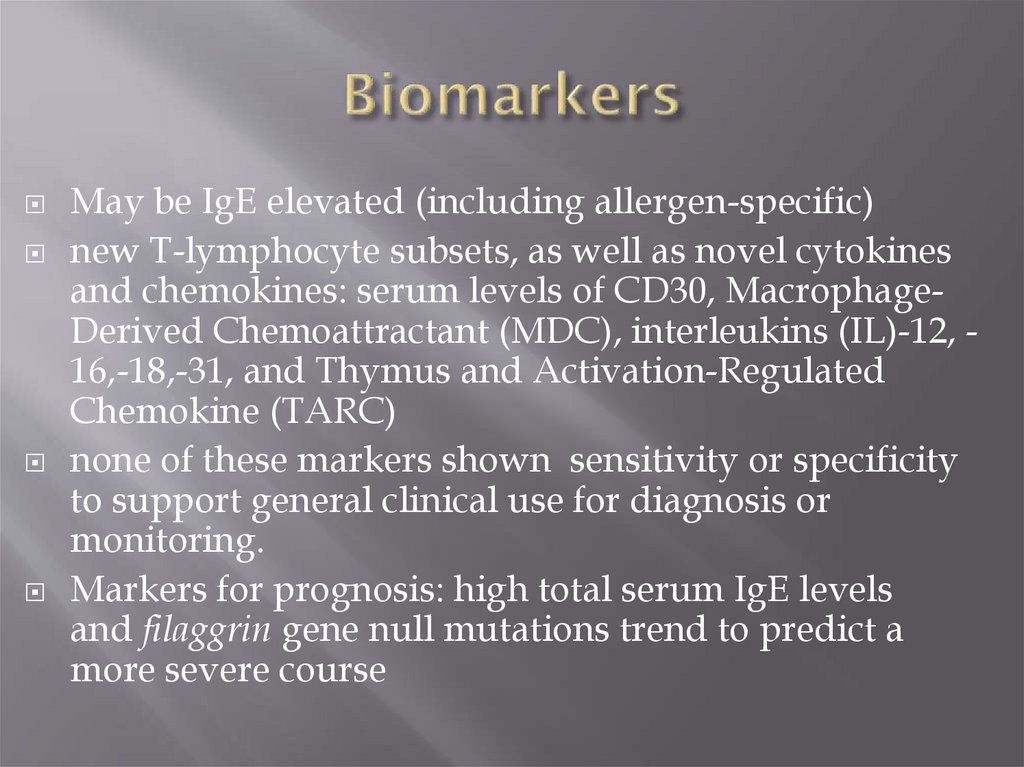
16. Biomarkers
May be IgE elevated (including allergen-specific)new T-lymphocyte subsets, as well as novel cytokines
and chemokines: serum levels of CD30, MacrophageDerived Chemoattractant (MDC), interleukins (IL)-12, 16,-18,-31, and Thymus and Activation-Regulated
Chemokine (TARC)
none of these markers shown sensitivity or specificity
to support general clinical use for diagnosis or
monitoring.
Markers for prognosis: high total serum IgE levels
and filaggrin gene null mutations trend to predict a
more severe course
17.
Topical corticosteroids for patients who failed torespond to good skin care and regular use of
emollients alone.
twice-daily application of corticosteroids, evidence
suggests that once-daily application of some
corticosteroids may be sufficient
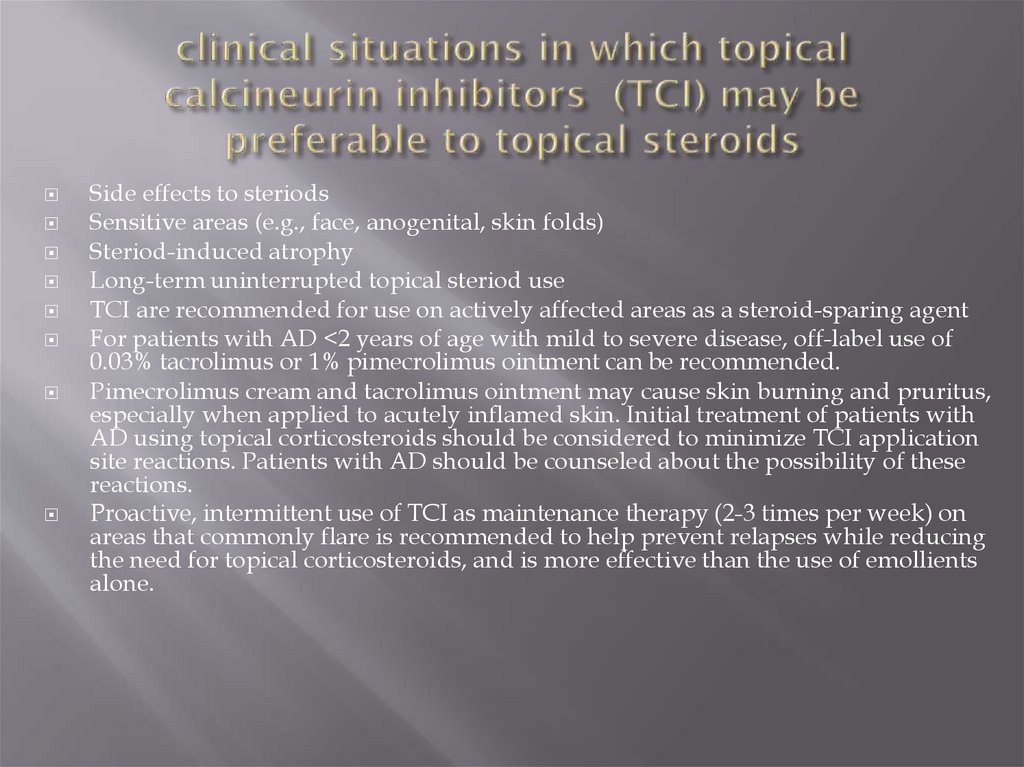
18. clinical situations in which topical calcineurin inhibitors (TCI) may be preferable to topical steroids
Side effects to steriodsSensitive areas (e.g., face, anogenital, skin folds)
Steriod-induced atrophy
Long-term uninterrupted topical steriod use
TCI are recommended for use on actively affected areas as a steroid-sparing agent
For patients with AD <2 years of age with mild to severe disease, off-label use of
0.03% tacrolimus or 1% pimecrolimus ointment can be recommended.
Pimecrolimus cream and tacrolimus ointment may cause skin burning and pruritus,
especially when applied to acutely inflamed skin. Initial treatment of patients with
AD using topical corticosteroids should be considered to minimize TCI application
site reactions. Patients with AD should be counseled about the possibility of these
reactions.
Proactive, intermittent use of TCI as maintenance therapy (2-3 times per week) on
areas that commonly flare is recommended to help prevent relapses while reducing
the need for topical corticosteroids, and is more effective than the use of emollients
alone.
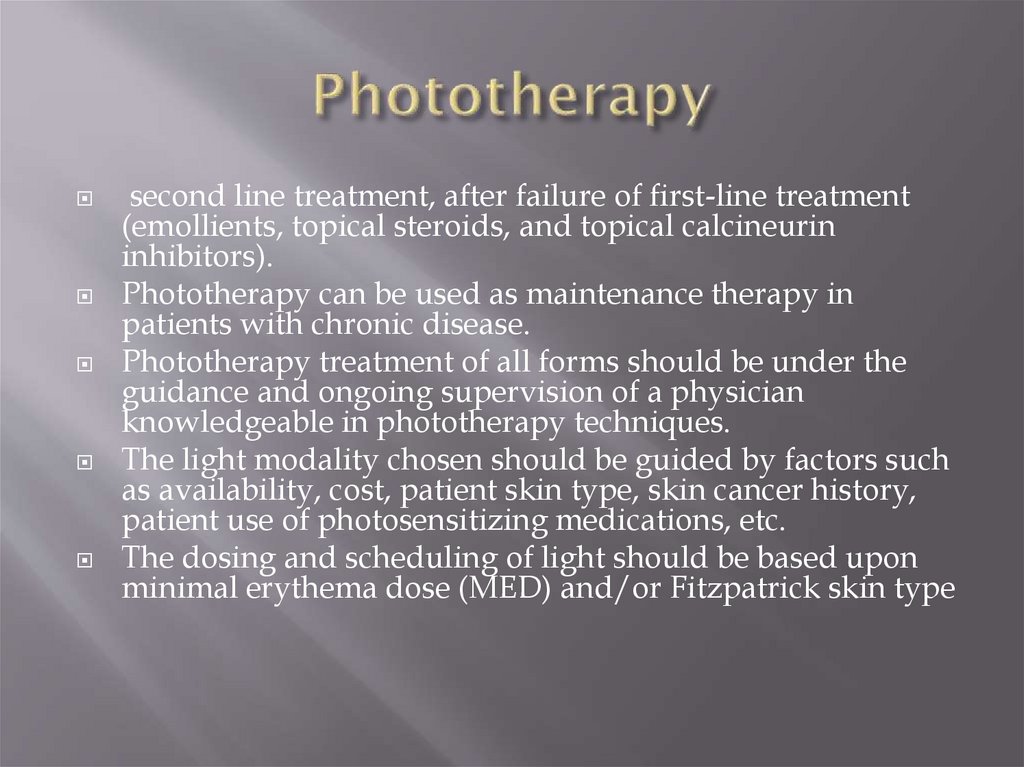
19. Phototherapy
second line treatment, after failure of first-line treatment(emollients, topical steroids, and topical calcineurin
inhibitors).
Phototherapy can be used as maintenance therapy in
patients with chronic disease.
Phototherapy treatment of all forms should be under the
guidance and ongoing supervision of a physician
knowledgeable in phototherapy techniques.
The light modality chosen should be guided by factors such
as availability, cost, patient skin type, skin cancer history,
patient use of photosensitizing medications, etc.
The dosing and scheduling of light should be based upon
minimal erythema dose (MED) and/or Fitzpatrick skin type
20.
Cyclosporine is effective and recommended as atreatment option for patients with AD refractory to
conventional topical treatment.
Azathioprine is recommended as a systemic agent
for the treatment of refractory atopic dermatitis
Methotrexate
Mycophenolate mofetil
Systemic steroids should be avoided if possible for
the treatment of AD. Their use should be
exclusively reserved for acute, severe
exacerbations and as a short-term bridge therapy
to other systemic, steroid-sparing therapy.



 Медицина
Медицина