Похожие презентации:
Acne, . Etiopathogenesis, Clinical History, Modern Methods of Treatment
1. Medical Academy Named after S. I. Georgievsky of Crimea Federal University Skin and Venereal Diseases Department Seborrhea,
Acne, .Etiopathogenesis,
Clinical History,
Modern Methods of Treatment
1
2.
PAPULAR AND PUSTULAR ERUPTION ON THE FACEWITH SCARRING .
CASE 1
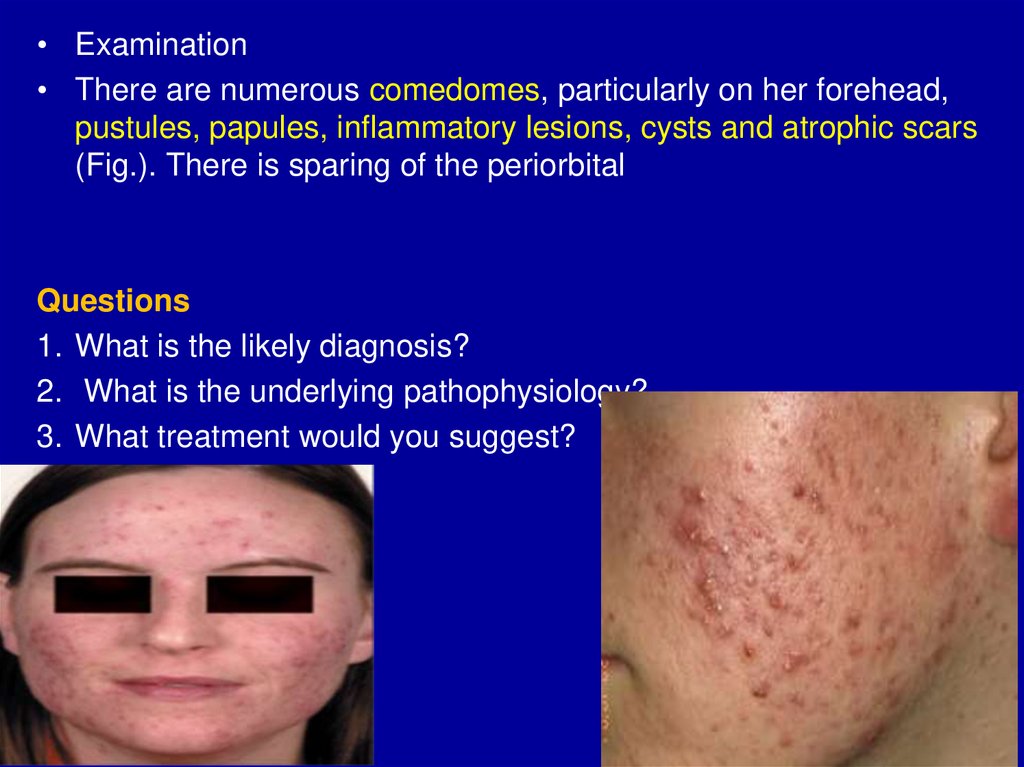
A 25-year-old woman presents to the dermatology clinic with a
long history of a facial eruption that has been getting worse
progressively over the past few years. Some of the lesions on
her face are painful at times and sometimes heal with scarring.
The rest of her skin is unaffected. Her GP(general practitioner)
had prescribed several prolonged courses of tetracycline
antibiotics with little benefit, and she was unable to tolerate
erythromycin due to its gastrointestinal side effects. She took
Dianette (oral contraceptive pill) for several months
but this had to be stopped as it was significantly lowering her
mood.
skin
2
3.
• Examination• There are numerous comedomes, particularly on her forehead,
pustules, papules, inflammatory lesions, cysts and atrophic scars
(Fig.). There is sparing of the periorbital
Questions
1. What is the likely diagnosis?
2. What is the underlying pathophysiology?
3. What treatment would you suggest?
3
4.
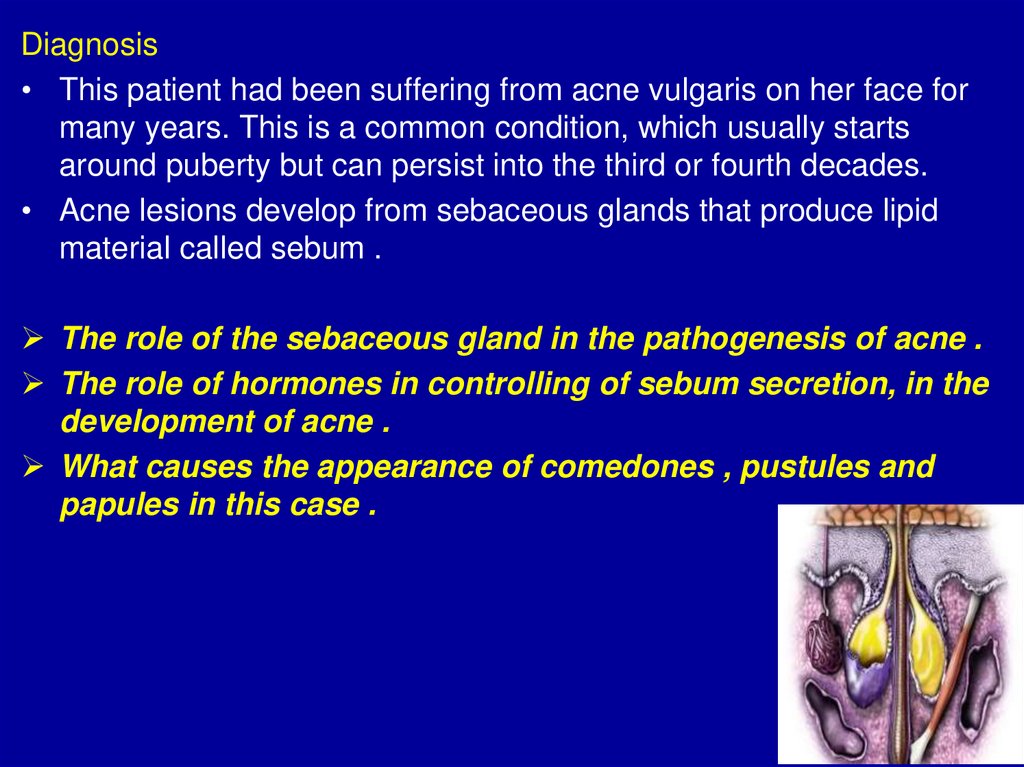
Diagnosis• This patient had been suffering from acne vulgaris on her face for
many years. This is a common condition, which usually starts
around puberty but can persist into the third or fourth decades.
• Acne lesions develop from sebaceous glands that produce lipid
material called sebum .
The role of the sebaceous gland in the pathogenesis of acne .
The role of hormones in controlling of sebum secretion, in the
development of acne .
What causes the appearance of comedones , pustules and
papules in this case .
4
5.
Sebaceous Glands• Sebaceous glands are
exocrine glands that release
sebum. These glands are
connected with the hair
follicles, and, in most cases,
sebum is released through
the same pore through which
hair grows.
• Sebaceous glands are
located on every surface of
your skin, with the exception
of your palms, bottom lip, and
the soles of your feet.
5
6.
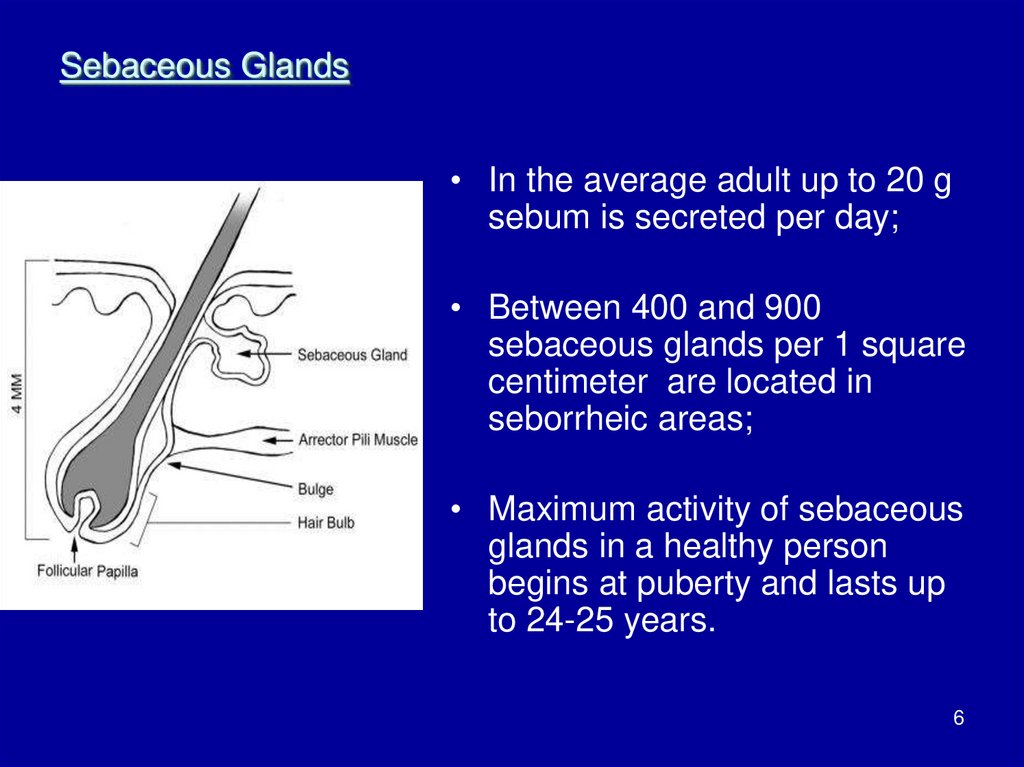
Sebaceous Glands• In the average adult up to 20 g
sebum is secreted per day;
• Between 400 and 900
sebaceous glands per 1 square
centimeter are located in
seborrheic areas;
• Maximum activity of sebaceous
glands in a healthy person
begins at puberty and lasts up
to 24-25 years.
6
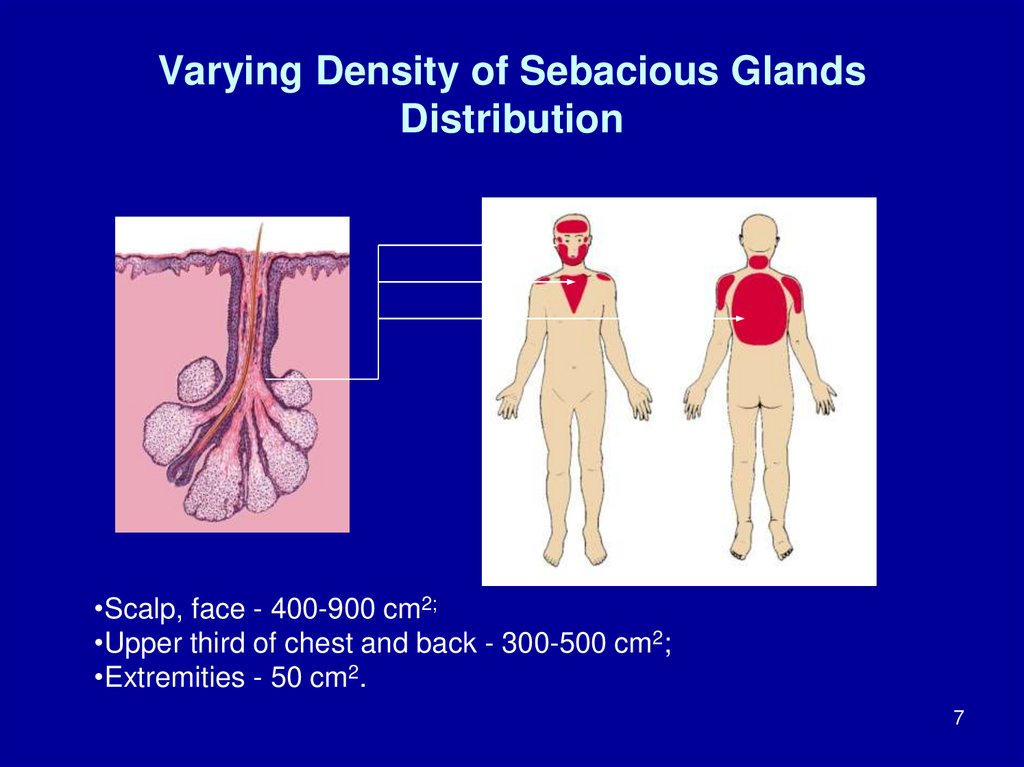
7. Varying Density of Sebacious Glands Distribution
•Scalp, face - 400-900 cm2;•Upper third of chest and back - 300-500 cm2;
•Extremities - 50 cm2.
7
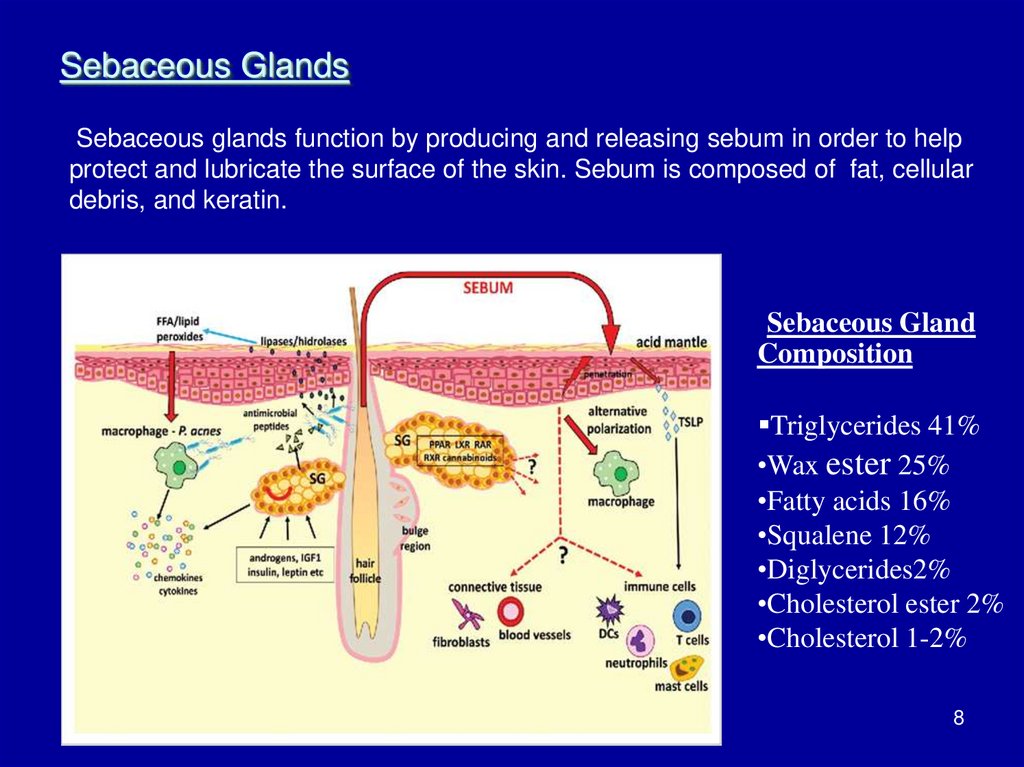
8. Sebaceous Glands
Sebaceous glands function by producing and releasing sebum in order to helpprotect and lubricate the surface of the skin. Sebum is composed of fat, cellular
debris, and keratin.
Sebaceous Gland
Composition
Triglycerides 41%
•Wax ester 25%
•Fatty acids 16%
•Squalene 12%
•Diglycerides2%
•Cholesterol ester 2%
•Cholesterol 1-2%
8
9. Sebaceous Glands Functions:
• Softens epidermis giving itwater-proofing properties;
• Regulates water evaporation;
• Blocks penetration of certain
substances from the
environment;
• Imparts antifungal and
antibacterial effect.
9
10. Sebacious Glands Regulation
Androgens increase sebum production, and estrogen reduce it.The embryologic development of the human sebaceous gland is
closely related to the differentiation of the hair follicle and the
epidermis. The number of sebaceous glands remains
approximately the same throughout life, whereas their size tends
to increase with age.
The activity of the sebaceous glands increases during puberty
because of heightened levels of androgens.
Androgens are well known for their effects on sebum excretion,
whereas terminal sebocyte differentiation is assisted by
peroxisome proliferator-activated receptor ligands .
10
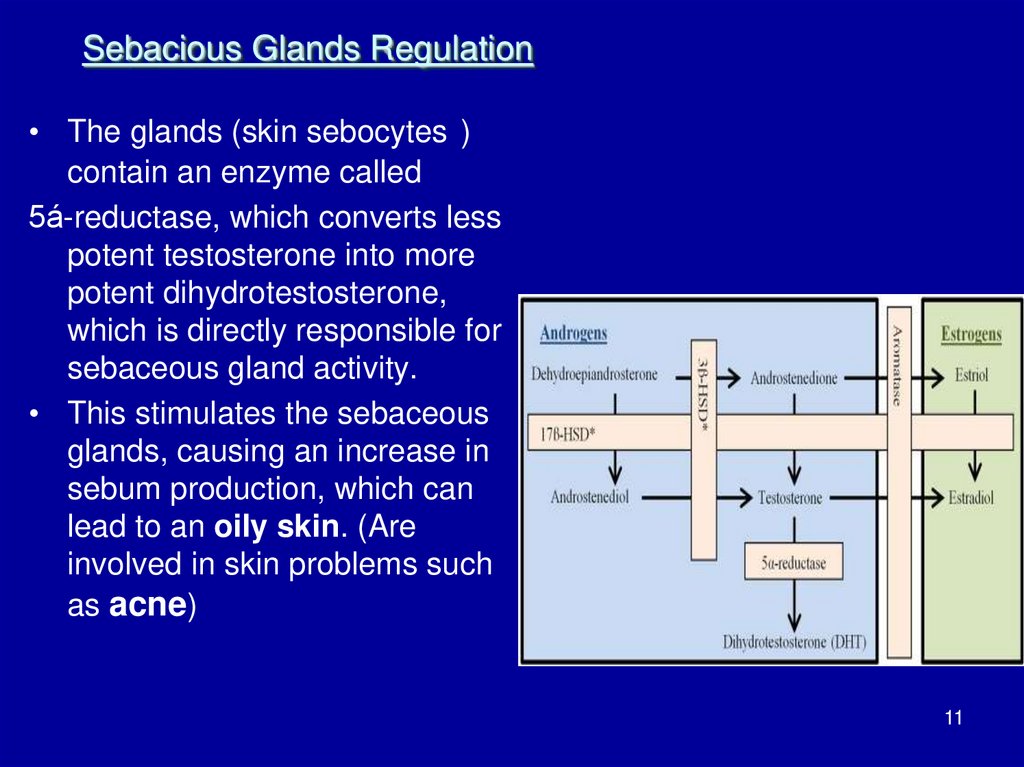
11.
Sebacious Glands Regulation• The glands (skin sebocytes )
contain an enzyme called
5á-reductase, which converts less
potent testosterone into more
potent dihydrotestosterone,
which is directly responsible for
sebaceous gland activity.
• This stimulates the sebaceous
glands, causing an increase in
sebum production, which can
lead to an oily skin. (Are
involved in skin problems such
as acne)
11
12.
Acne vulgarisAcne means eruption and Vulgaris means common so
Acne is one of the commonest skin disorders – if not the
commonest. It has been estimated that 70 per cent of the
population have some clinically evident acne at some stage
during adolescence!
Acne vulgaris is a chronic disorder of the pilosebaceous
apparatus caused by abnormal desquamation of follicular
epithelium leading to obstruction of the pilosebaceous canal,
resulting in inflammation and subsequent formation of
papules, pustules, nodules, comedones, and scarring with
varying extent and severity.
While the course of acne may be self-limiting, the sequelae
can be lifelong, with pitted or hypertrophic scar formation.
12
13. Etiology of Acne
Genetic factors. If both parents suffer from such diseaselikelihood of its development in children is 50%. The number, size
and sensitivity of receptors of the sebaceous glands is genetically
determined.
Hormonal disorders:
• Absolute hyperandrogenism (at androgen-productivity of
ovarian and adrenal glands tumors, PCOS, adrenal hyperplasia);
• Relative hyperandrogenism (elevated activity of 5-alphareductase);
• Iatrogenic hyperandrogenism (anabolic steroids, androgens,
progestins , etc. intake ).
The effects of stress.
Pathology of the immune system.
Gastrointestinal diseases.
13
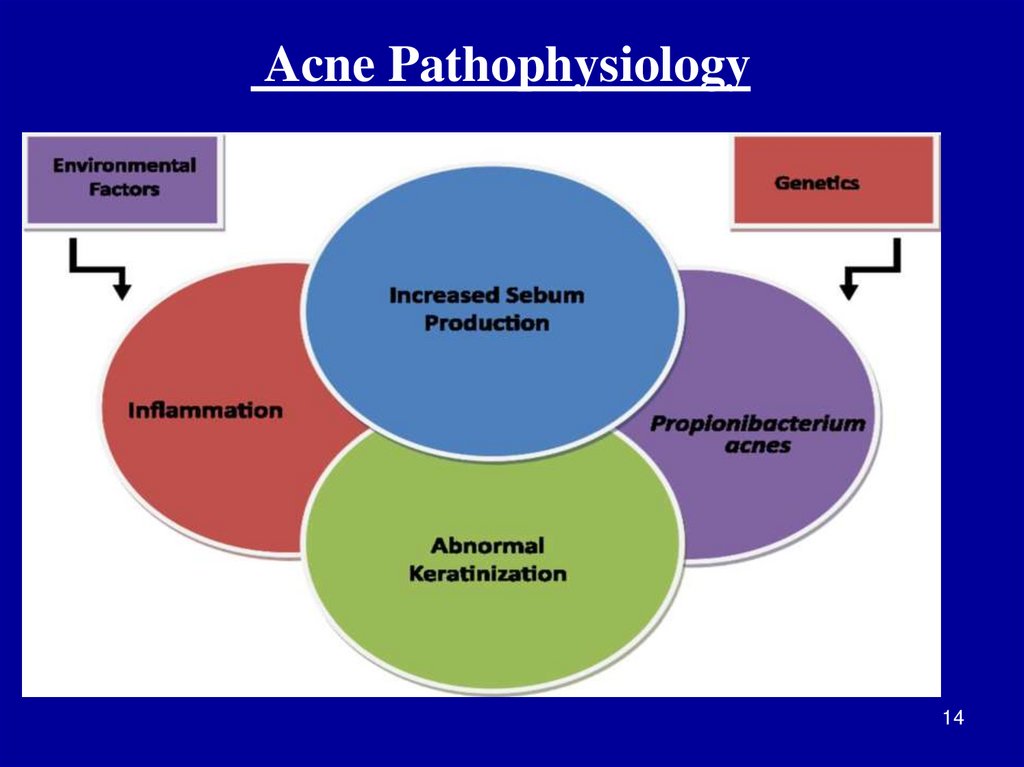
14.
Acne Pathophysiology14
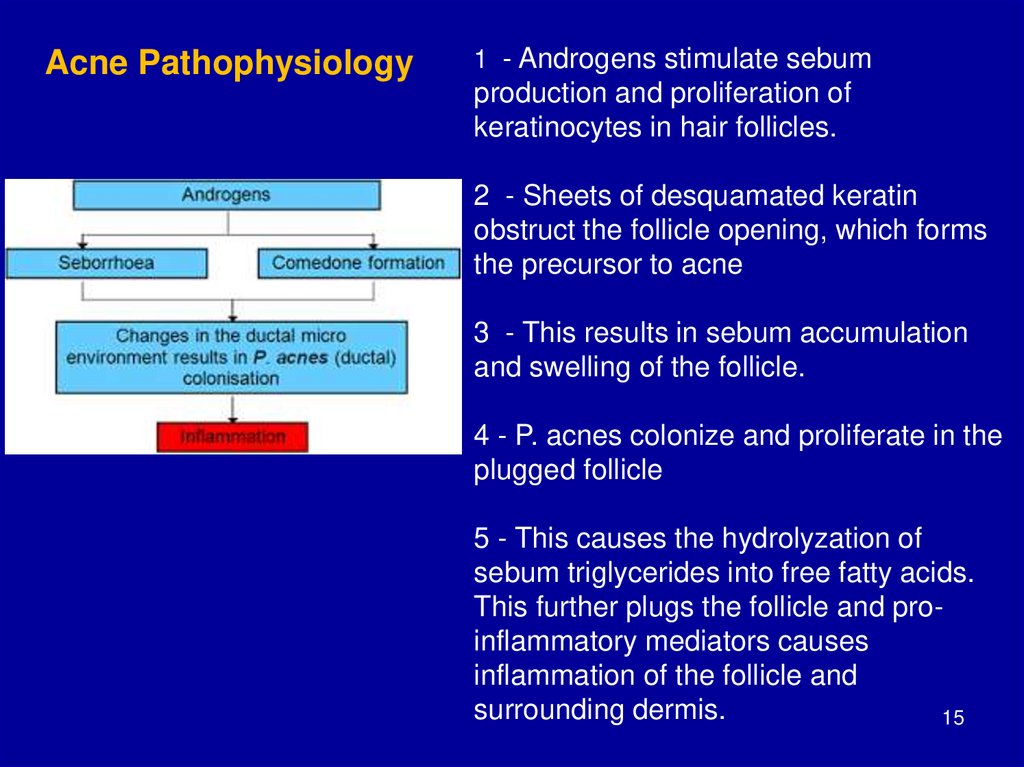
15.
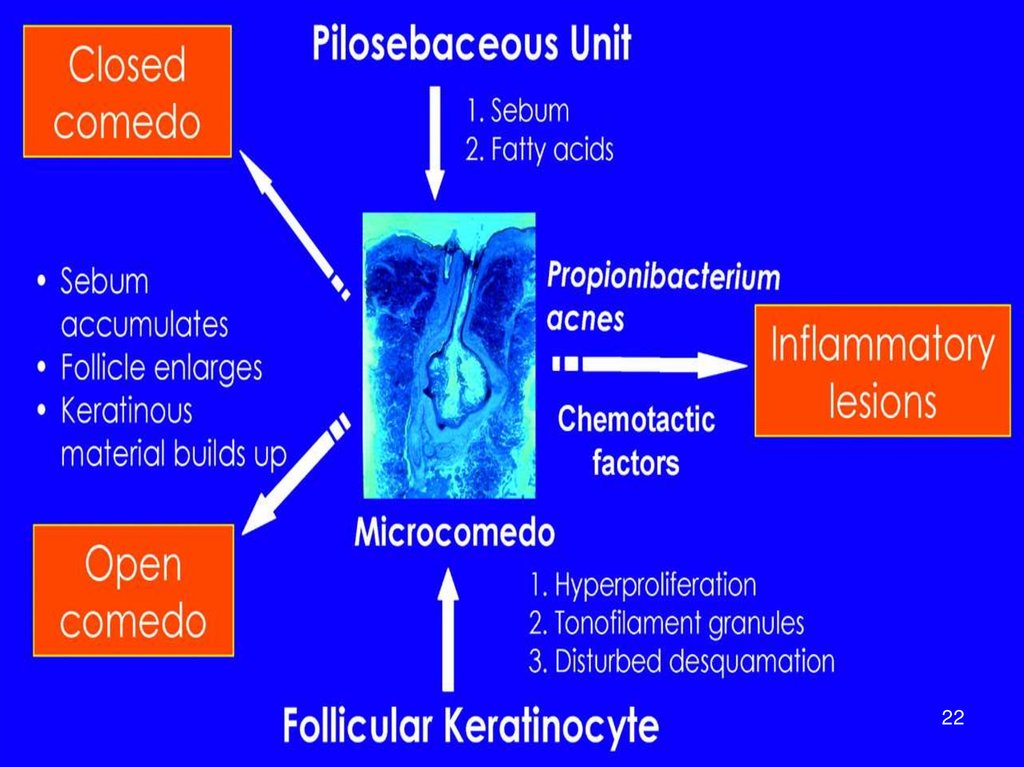
Acne Pathophysiology1 - Androgens stimulate sebum
production and proliferation of
keratinocytes in hair follicles.
2 - Sheets of desquamated keratin
obstruct the follicle opening, which forms
the precursor to acne
3 - This results in sebum accumulation
and swelling of the follicle.
4 - P. acnes colonize and proliferate in the
plugged follicle
5 - This causes the hydrolyzation of
sebum triglycerides into free fatty acids.
This further plugs the follicle and proinflammatory mediators causes
inflammation of the follicle and
surrounding dermis.
15
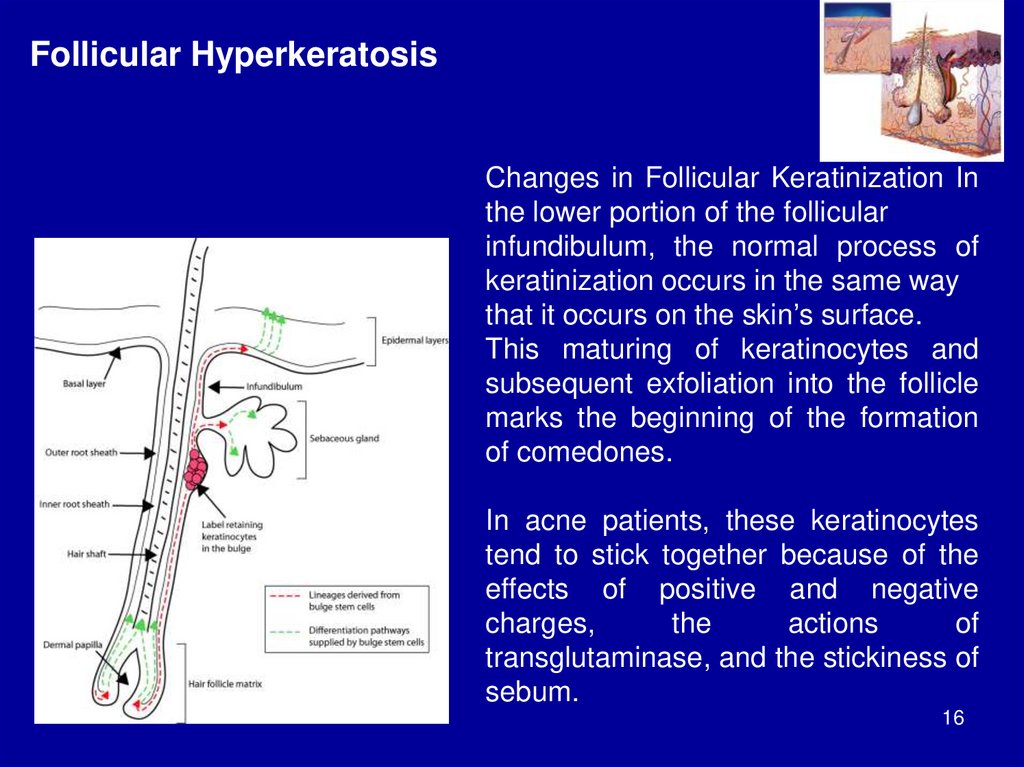
16.
Follicular HyperkeratosisChanges in Follicular Keratinization In
the lower portion of the follicular
infundibulum, the normal process of
keratinization occurs in the same way
that it occurs on the skin’s surface.
This maturing of keratinocytes and
subsequent exfoliation into the follicle
marks the beginning of the formation
of comedones.
In acne patients, these keratinocytes
tend to stick together because of the
effects of positive and negative
charges,
the
actions
of
transglutaminase, and the stickiness of
sebum.
16
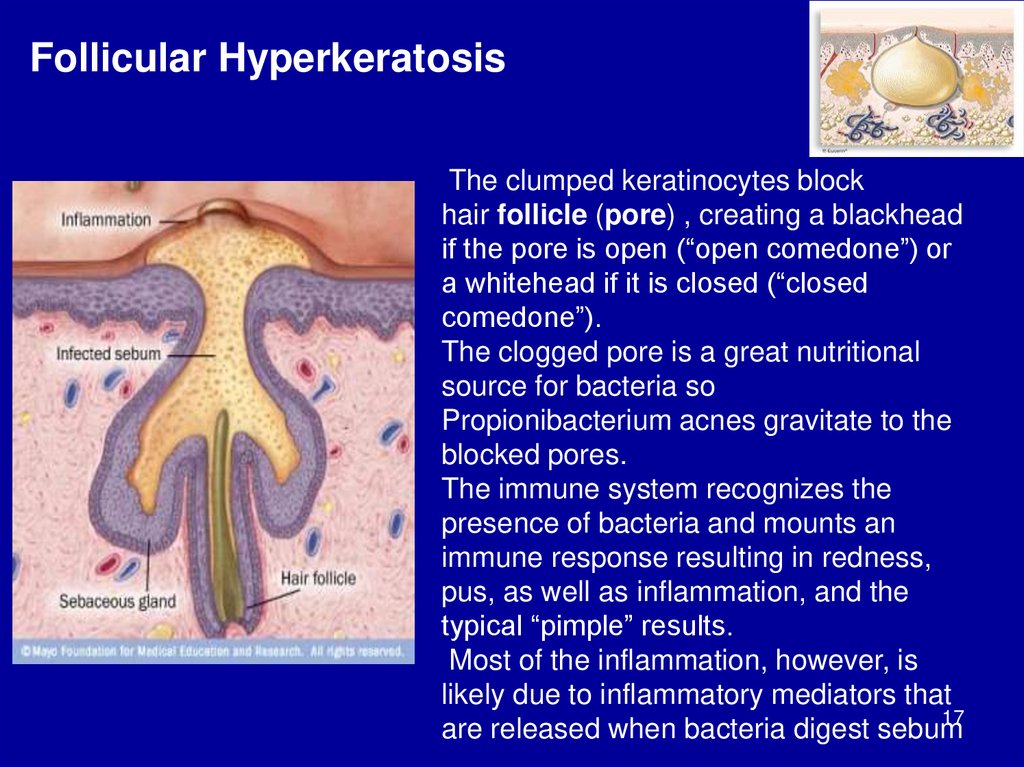
17.
Follicular HyperkeratosisThe clumped keratinocytes block
hair follicle (pore) , creating a blackhead
if the pore is open (“open comedone”) or
a whitehead if it is closed (“closed
comedone”).
The clogged pore is a great nutritional
source for bacteria so
Propionibacterium acnes gravitate to the
blocked pores.
The immune system recognizes the
presence of bacteria and mounts an
immune response resulting in redness,
pus, as well as inflammation, and the
typical “pimple” results.
Most of the inflammation, however, is
likely due to inflammatory mediators that
17
are released when bacteria digest sebum
18.
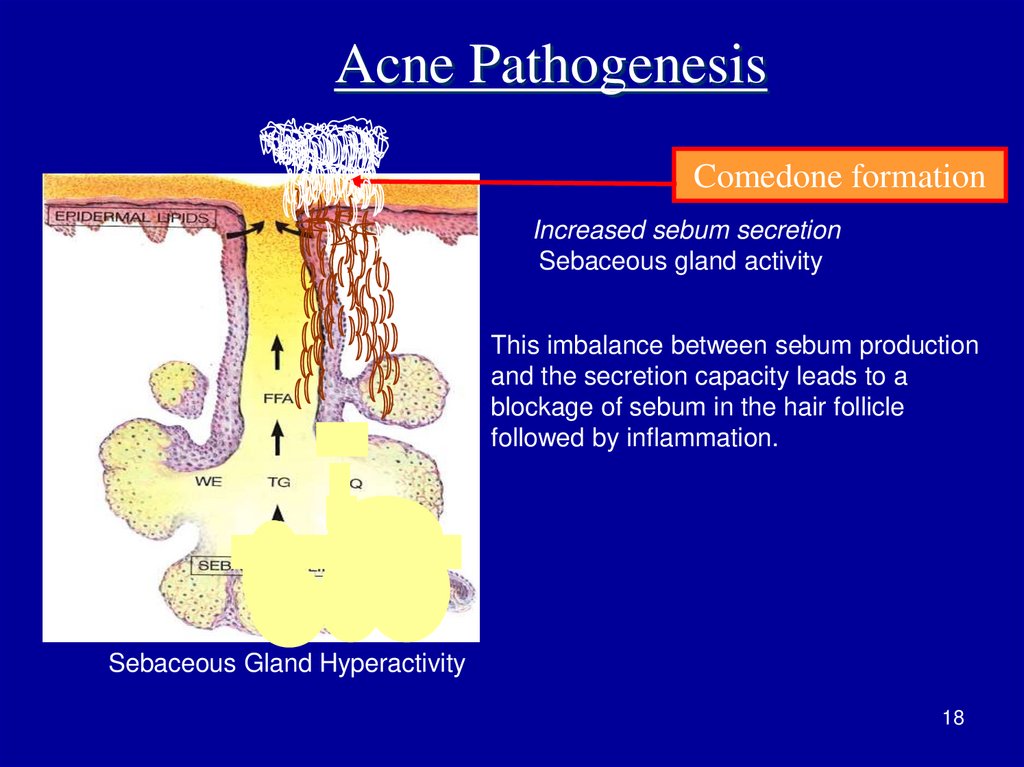
Acne PathogenesisComedone formation
Increased sebum secretion
Sebaceous gland activity
This imbalance between sebum production
and the secretion capacity leads to a
blockage of sebum in the hair follicle
followed by inflammation.
Sebaceous Gland Hyperactivity
18
19. Acne Pathogenesis (to be continued)
Occlusion of thefollicular canal
Follicular hyperkeratosis;
Abnormal follicular keratinization
• ↑ Corneocyte cohesiveness and
proliferation.
Pilosebaceous orifice in acne is
occluded by a keratinous plug
induced by: Chemicals (present as
ingredients of cosmetics).
19
20.
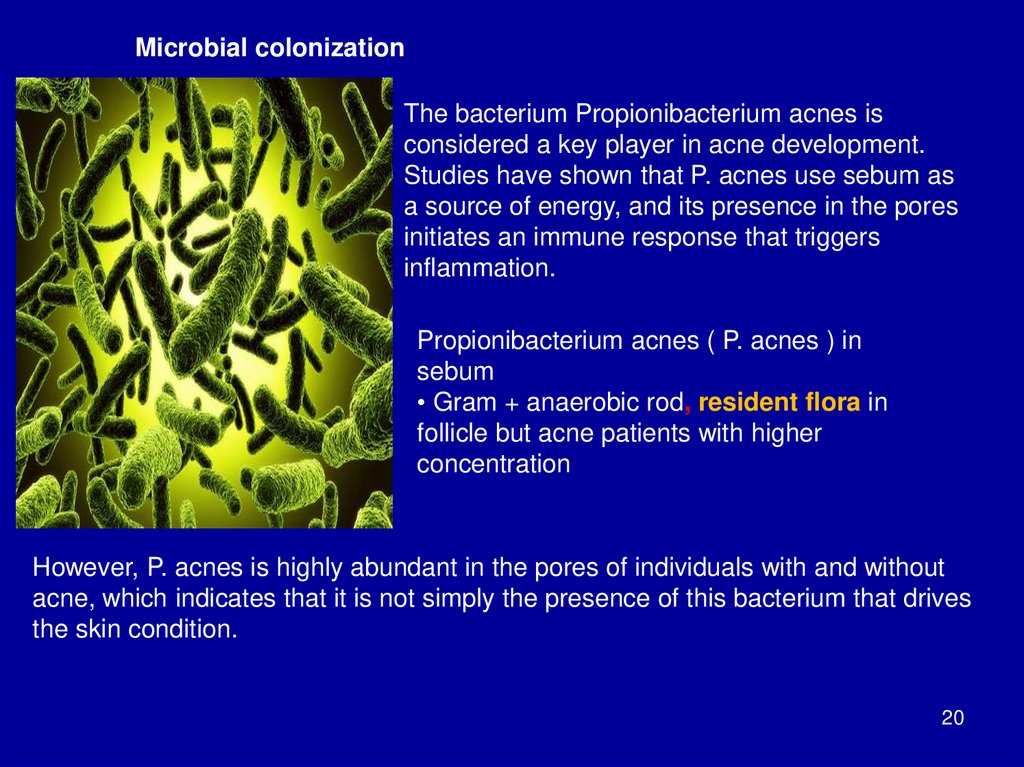
Microbial colonizationThe bacterium Propionibacterium acnes is
considered a key player in acne development.
Studies have shown that P. acnes use sebum as
a source of energy, and its presence in the pores
initiates an immune response that triggers
inflammation.
Propionibacterium acnes ( P. acnes ) in
sebum
• Gram + anaerobic rod, resident flora in
follicle but acne patients with higher
concentration
However, P. acnes is highly abundant in the pores of individuals with and without
acne, which indicates that it is not simply the presence of this bacterium that drives
the skin condition.
20
21.
Acne Pathogenesis(to be continued)
Inflammation
development
Release of inflammatory
mediators
• Distended follicle ruptures,
releasing inflammatory
chemicals into the dermis,
stimulating intense
inflammation.
• Ductal epithelium also
produces cytokines,
triggering
an inflammatory cascade.
• Microbes also produce
extracellular enzymes,
which attract inflammatory
cells.
21
22.
2223. KERATINIZATION IN EPIDERMIS
2324.
How Acne or Pimple Forms Under Skin24
25.
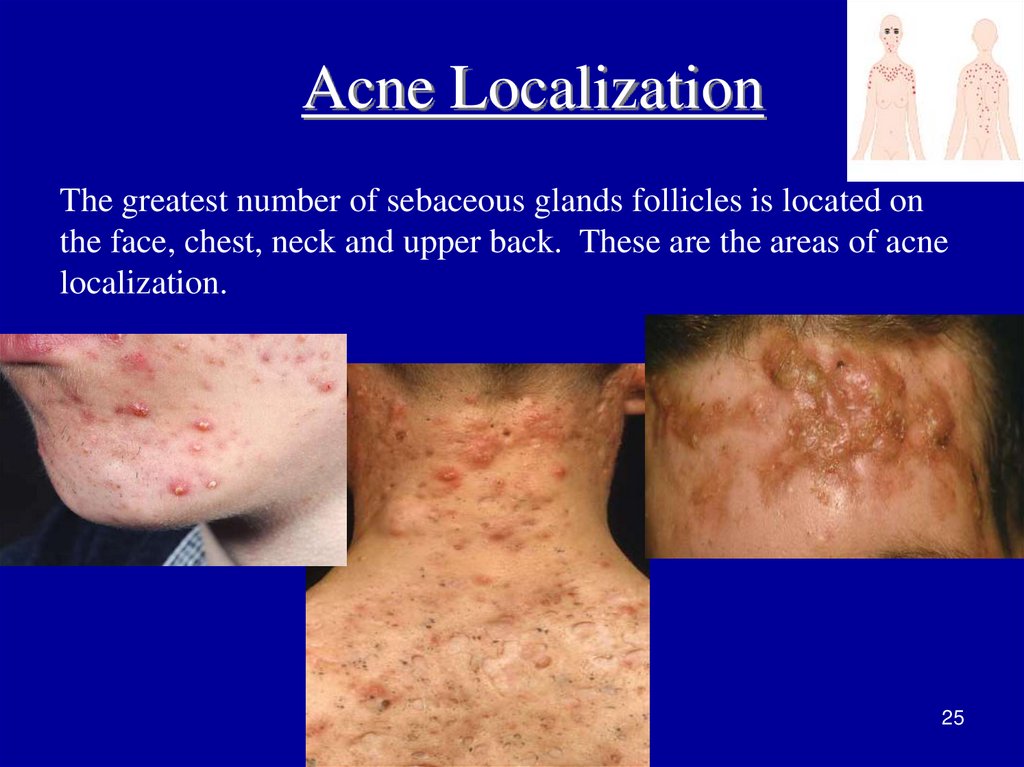
Acne LocalizationThe greatest number of sebaceous glands follicles is located on
the face, chest, neck and upper back. These are the areas of acne
localization.
25
26.
clinical featuresIndividual lesions are centred on the pilosebaceous unit, ie the hair follicle and its
associated oil gland.
Superficial lesions
Open and closed comedones (blackheads and whiteheads)
Papules
Pustules
Deeper lesions
Nodules (large painful red lumps)
Pseudocysts (cyst-like fluctuant swellings)
Secondary lesions
Excoriations (picked or scratched spots)
Erythematous macules
Pigmented macules
Scars or various types
26
27.
ComedonesComedones are non-inflammatory elements
resulting from blockage of the mouths of hair
follicles.
Closed" comedones
open" comedones
Submarine comedones respond poorly to
medical treatment.
27
28. Clinical History of Acne
• Comedones (comedo sou acne comedonica);• Acne papulosa and acne pustulosa (acne
papulosa et papulopustulosa);
• Acne indurata (acne indurativa);
• (acne phlegmonosa);
• Acne conglobata;
• Acne fulminans (also known as "Acute febrile
ulcerative acne" ;
• Acne inversa or hidradenitis suppurativa.
28
29.
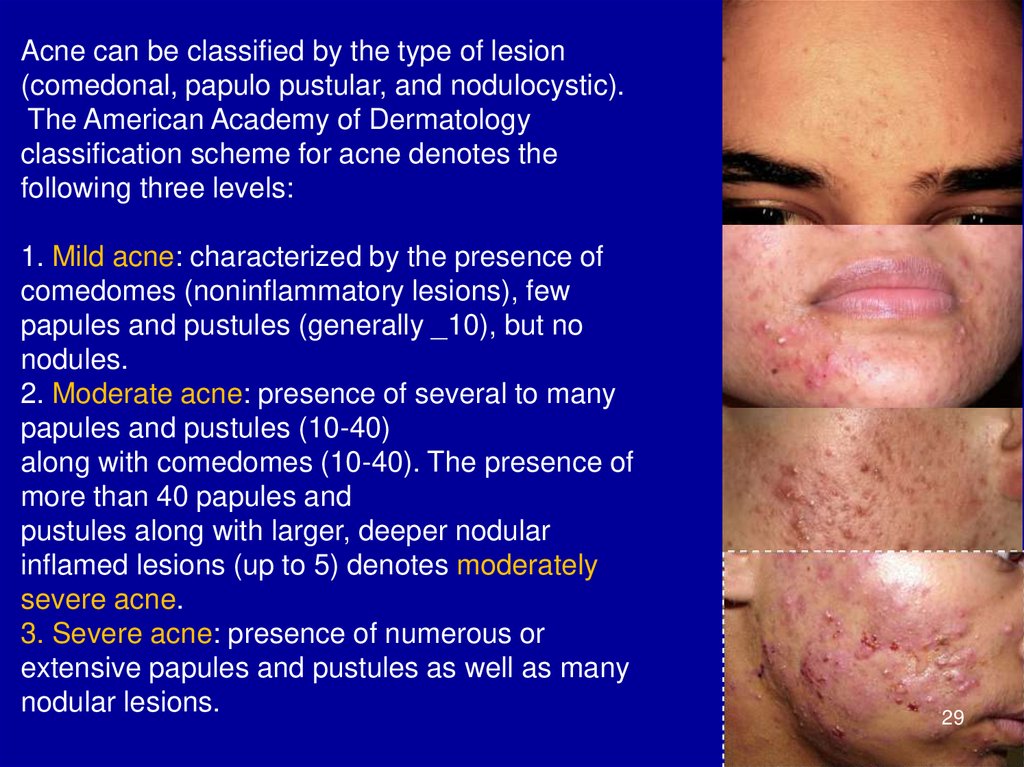
Acne can be classified by the type of lesion(comedonal, papulo pustular, and nodulocystic).
The American Academy of Dermatology
classification scheme for acne denotes the
following three levels:
1. Mild acne: characterized by the presence of
comedomes (noninflammatory lesions), few
papules and pustules (generally _10), but no
nodules.
2. Moderate acne: presence of several to many
papules and pustules (10-40)
along with comedomes (10-40). The presence of
more than 40 papules and
pustules along with larger, deeper nodular
inflamed lesions (up to 5) denotes moderately
severe acne.
3. Severe acne: presence of numerous or
extensive papules and pustules as well as many
nodular lesions.
29
30.
3031.
3132.
Blackheads vs. Whiteheads32
33.
Acne Indurata• Acne indurativa is characterized by the formation of deep
infiltrates with the formation of scars and is prone to
merge cystic cavities filled with pus - phlegmonous types.
Indurative and phlegmonous acnes are called
nodulocystic ones. Nodulocystic acne is a sign of fairly
severe course of acne.
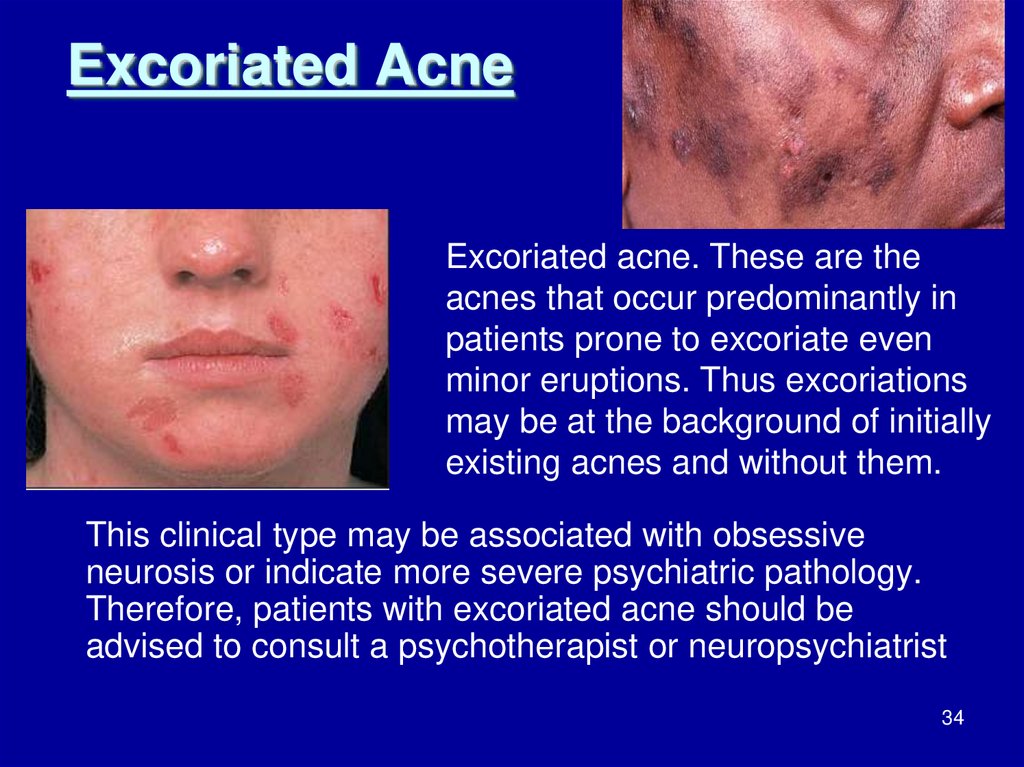
34. Excoriated Acne
Excoriated acne. These are theacnes that occur predominantly in
patients prone to excoriate even
minor eruptions. Thus excoriations
may be at the background of initially
existing acnes and without them.
This clinical type may be associated with obsessive
neurosis or indicate more severe psychiatric pathology.
Therefore, patients with excoriated acne should be
advised to consult a psychotherapist or neuropsychiatrist
34
35. Acne Conglobata
• Acne conglobata is nodulocysticelements connecting with each
other, as well as with large
comedones. Lesions can be
located everywhere. They are
resolved into keloids. They
relapse until the age of 40 and
sometimes lasts even lifelong.
35
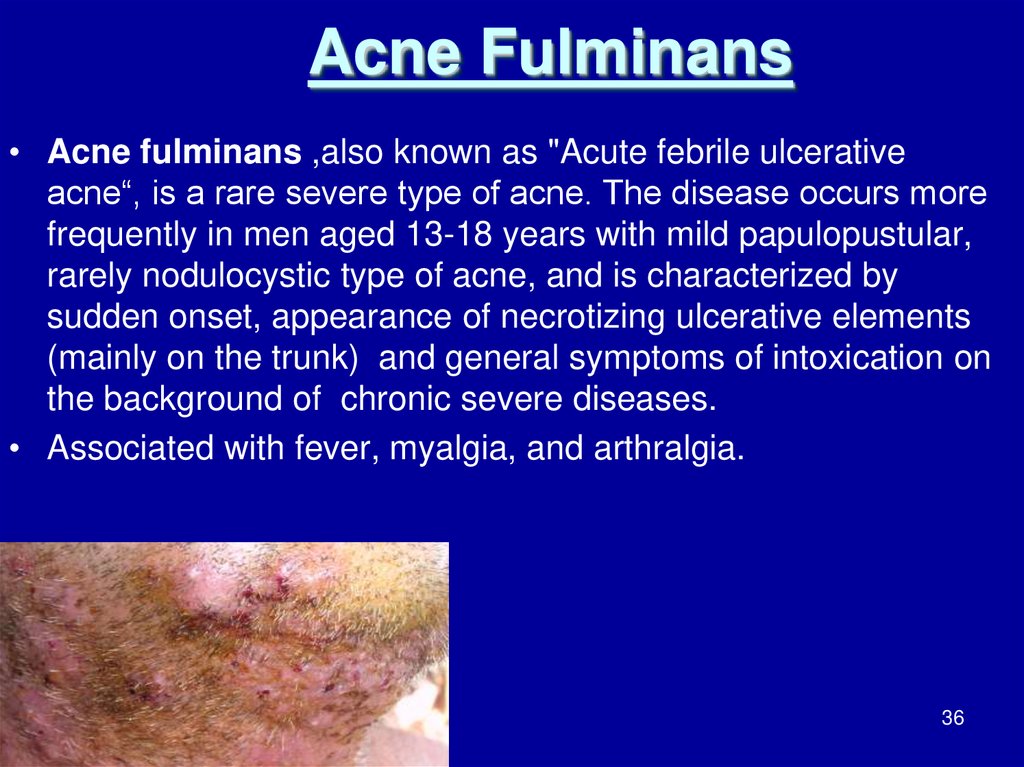
36. Acne Fulminans
• Acne fulminans ,also known as "Acute febrile ulcerativeacne“, is a rare severe type of acne. The disease occurs more
frequently in men aged 13-18 years with mild papulopustular,
rarely nodulocystic type of acne, and is characterized by
sudden onset, appearance of necrotizing ulcerative elements
(mainly on the trunk) and general symptoms of intoxication on
the background of chronic severe diseases.
• Associated with fever, myalgia, and arthralgia.
36
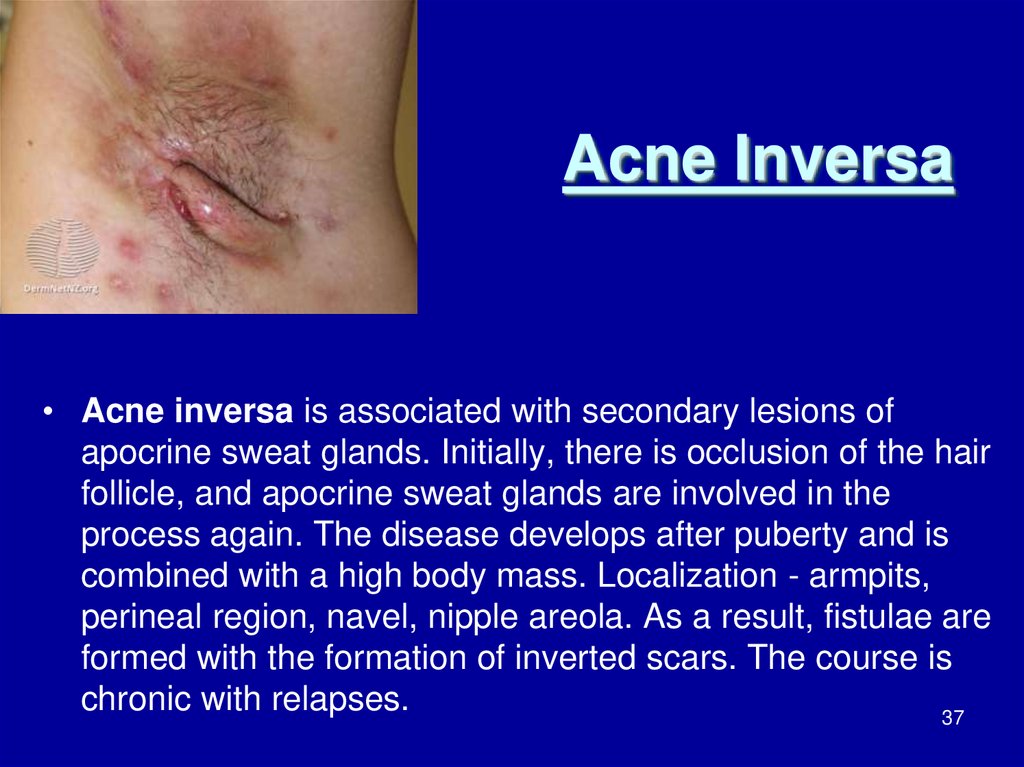
37. Acne Inversa
• Acne inversa is associated with secondary lesions ofapocrine sweat glands. Initially, there is occlusion of the hair
follicle, and apocrine sweat glands are involved in the
process again. The disease develops after puberty and is
combined with a high body mass. Localization - armpits,
perineal region, navel, nipple areola. As a result, fistulae are
formed with the formation of inverted scars. The course is
chronic with relapses.
37
38.
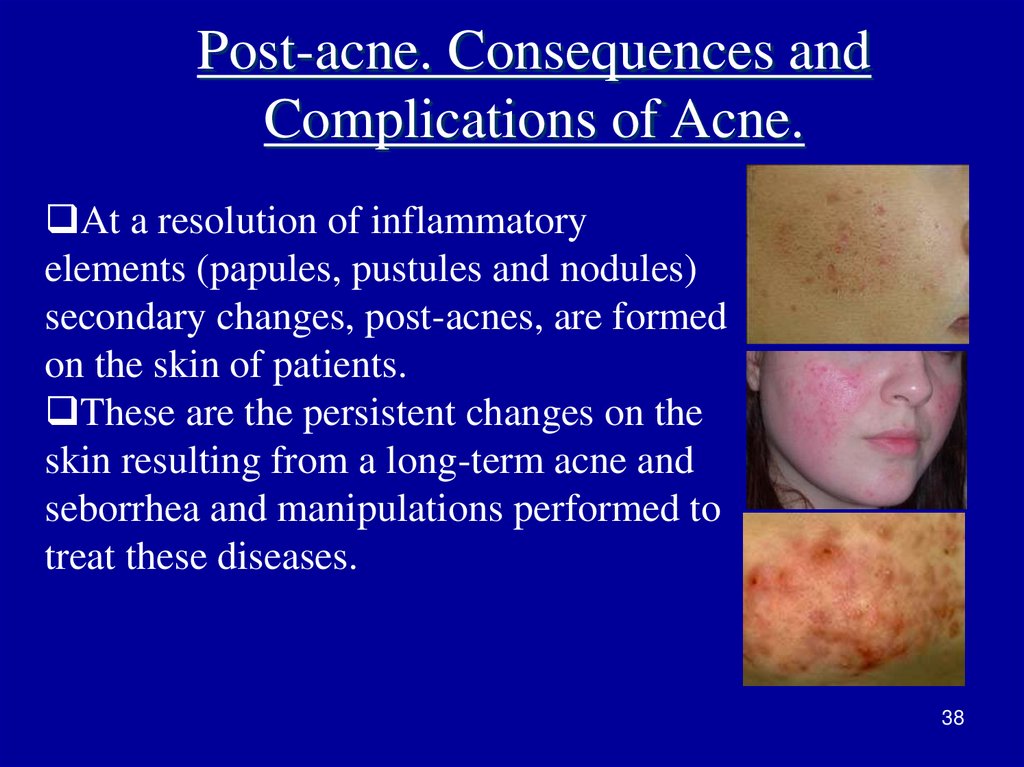
Post-acne. Consequences andComplications of Acne.
At a resolution of inflammatory
elements (papules, pustules and nodules)
secondary changes, post-acnes, are formed
on the skin of patients.
These are the persistent changes on the
skin resulting from a long-term acne and
seborrhea and manipulations performed to
treat these diseases.
38
39. Post-acne
• Uneven skin texture;• Permanent scars;
• Stagnant spots;
• Secondary hyperpigmentation;
• Persistent erythema;
• Dilation of the capillaries;
• Hyper and / or hypopigmentation;
• Psychological problems;
• Depression, anxiety, social isolation.
Intensity of post-acne is associated with age and duration of
exacerbations.
39
40. Treatment
The choice of treatment should be based on:Anamnesis;
Adequate clinical assessment of disease;
Assessment of psychosocial status of the patient
with acne.
Be sure to recommend:
Daily cleansing of the skin.
When caring for skin one should avoid fatty
creams and ointments, causing hair follicles
occlusion.
40
41.
General measuresLocal hygiene
Regular gentle cleansing (not overzealous) with soap and water
should be encouraged.
Application of oil-based cosmetics should be avoided as they
may aggravate acne, but water-based cosmetics can be used.
Diet
Stress
Acne induces stress and this needs to be handled.
Some patients with mild acne may be more distressed than those
with severe acne.
Stress itself may induce acne.
41
42.
The success of acne treatment is possible only if it affects allfactors of pathogenesis.
Treatment is multipronged, attacking the four mechanisms
which lead to acne.
42
43. Principles of Acne Treatment
4344. Benzoyl peroxide (BP)
• Benzoyl peroxide (BP)• Mode of action: Is a powerful antimicrobial, decreasing population
of P. acnes.
• Also has anti-inflammatory effect.
Indications:
• Mild acne, as stand-alone therapy, especially if few inflammatory
lesions also present.
• Always to antibiotic therapy, to reduce resistance.
• Moderate-severe acne as topical adjunct to systemic therapy
Used in both inflammatory and noninflammatory acne.
44
45. Topical antibiotics
Most frequently used topical antibiotics are clindamycin (1–2%)
and erythromycin (2–4%).
Mode of action: Suppress P. acnes and its mediators of
inflammation and so are more effective against inflammatory
acne.
Clinical use: Useful in inflammatory acne but must always be
combined with topical retinoic acid or benzoyl peroxide .
• Side effects: Resistance of microorganisms to antibiotic is a major
problem, so should be combined with topical retinoids or benzoyl
peroxide.
45
46.
Topical retinoidsTopical retinoids are comedolytic and work by normalizing follicular
keratinization.
comedones are treated with topical tretinoin cream, what are the side
effects.
at the beginning of therapy the acne may appear worse but after three to
four weeks it improves.
The side effects can appearance photosensitivity and skin irritation, which
therefore requires protective clothing and sunscreen.
It should be avoided during pregnancy, since there is risk of birth defects.
for those who cannot tolerate topical tretinoin, we can use peeling agents
like salicylic acid and gluconic acid creams.
we can use other creams but with fewer side effects, such as skin irritation
and photosensitivity adapalene and tazarotene, both are effective, like
tretinoin .
adapalene (0.1% gel or cream, applied once or twice daily).
Tazarotene (0.1% cream or gel applied daily) .
Azelaic acid (Skinoren
46
47. Topical retinoids
Tretinoin is inactivated by UV light and oxidized by benzoylperoxide; therefore, it should only be applied at night and not used
concomitantly with benzoyl peroxide
47
48. Systemic treatment
• AntibioticsDrugs used: Doxycycline and minocycline are most commonly
used. Less frequently, erythromycin and azithromycin.
Mode of action:
• Inhibit growth of P. acnes and its metabolism.
• Direct anti-inflammatory effect.
Indications:
• Moderately severe acne (being the most frequently used systemic
therapy).
• Mild acne, if acne is affecting patient’s quality of life.
• Severe acne, if oral retinoids cannot be used.
48
49. Severe Degree of Acne. Therapy
A combination of standard topical and general treatment is
necessary to treat severe degree of acne.
• Severe inflammatory acne is when we can see more than
100 commodones or more than five cysts , here it's not
enough to you antibiotics or topical tretinoin , here we have
to use our strongest drug, namely oral is so tretinoin, which
is a retinoid that is related to vitamin A the therapy should
be between 16 and 20 weeks .
• Before beginning the therapy we need to check some lab
values of the patients like fasting glucose, triglycerides,
cholesterol, complete blood count and liver function.
• Other side effects are redness, dryness, irritation, and
peeling of the skin.
49
50.
The woman should not take this drug if they are pregnantbecause birth defects can happen to the baby because this is
a very this is very serious, pregnancy tests should also be
done before the beginning the therapy and monthly until one
month of the therapy stops.
so the woman should use two methods of contraception for
one month before the treatment during the treatment and for at
least one month after the treatment.
In women with severe manifestations of acne with the
ineffectiveness of antibiotics therapy combined oral
contraceptives with estrogen profile or anti-androgenic drugs
are administered after examination by gynecologistendocrinologist.
50
51.
Isotretinoin is a powerful medication used to treat severeinflammatory acne. It is an oral medication that is taken
once or twice daily. This medication is probably best
known by the now-defunct brand name Accutane.
Isotretinoin (not to be confused with tretinoin) is classified
as a retinoid, made from a synthetic form of vitamin A. It
is taken orally, in pill form, once or twice daily.
It's considered the most effective prescription treatment
available for severe acne. Isotretinoin can successfully
treat, and completely clear up acne, even acne that has
not improved with other treatments.
51
52. Methods of Cosmetic Correction
• Cleaning of face (manual, vacuum, ultrasound);• Cosmetic anti-inflammatory treatment;
• Jacquet massage;
• Cryotherapy;
• Chemical peelings;
• Phonophoresis;
• Phototherapy;
• D'arsonvalization;
• Laser Therapy.
52
53.
5354.
5455.
5556. UV Radiation in the Treatment of Acne. Pros and Cons.
The question of administration of ultraviolet
radiation (UVR) to a patient with acne should be solved
individually without doubt:
Many patients notice improvement in the acne course in
summer, after insolation;
UVR causes surface exfoliation and in small doses;
It may stimulate an immune response in the skin on the
other hand;
UVR enhances comedogenic properties of squalene, a
component of sebum;
UVR in high erythema doses causes a sharp decrease in
local immune defense and worsening of acne disease
56
course.
57.
• A 59-year-old man attends the dermatology clinic for a skinreview following renal transplantation for hypertensive
nephropathy. He is immunosuppressed with sirolimus
• and mycophenolate mofetil. He has a few viral warts on his
hands but his main complaint is a 6-month history of facial
redness and painful ‘spots’. The erythema is exacerbated by
heat. He has applied a bland emollient cream and topical
antibacterials to the affected areas with little benefit. At the
initial consultation he is noted to have a florid facial erythema
• with multiple papules and pustules over his forehead and
cheeks. He is commenced on oral minocycline 100 mg daily
and is asked to come back in 3 months.
57
58.
RosaceaRosacea (acne rosacea, gutta rosacea, teleangiectasiasis faciei,
cuperose) is a chronic, relapsing disease, usually of facial skin
having polietiologic nature and characterized by phases of its
course. Rosacea manifests itself primarily by arising hyperemia
(redness) of face, telangiectasia (dilation of small blood
vessels) on the face as well as hyperplasia of the sebaceous
glands and connective tissue. The basis of the disease there are
changes in the tone of the surface of blood vessels of the skin
caused by the action of various external and internal factors.
58
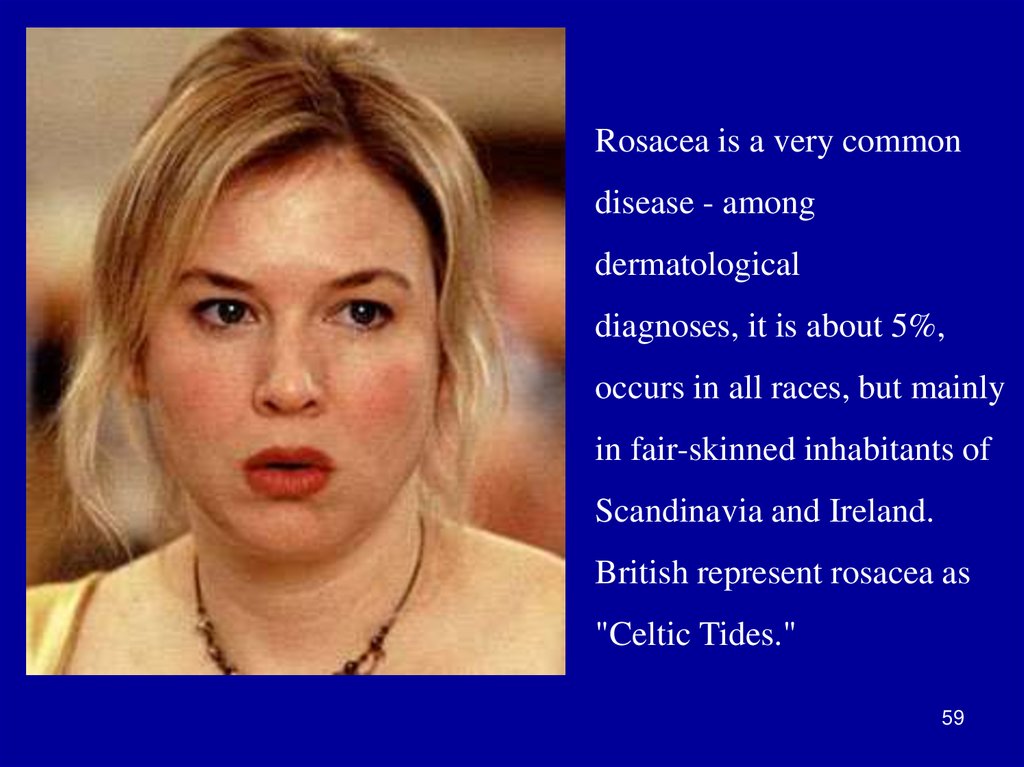
59.
Rosacea is a very commondisease - among
dermatological
diagnoses, it is about 5%,
occurs in all races, but mainly
in fair-skinned inhabitants of
Scandinavia and Ireland.
British represent rosacea as
"Celtic Tides."
59
60.
Rosacea begins in most cases at the third and fourth decadeof life flourishes between 40 and 50 years. Often affects women.
The disease should be called rosacea (from the Latin rosaceus pink) as used previously terms "rosacea" or «acne rosacea» are
untrue morphology essence of rosacea. Rosacea is a very common
disease in Caucasians, known since ancient times. So, a man with a
red face and a bulbous nose was described in the "Canterbury
Tales", written by D. Chaucer (1340-1400). Later rosacea patients
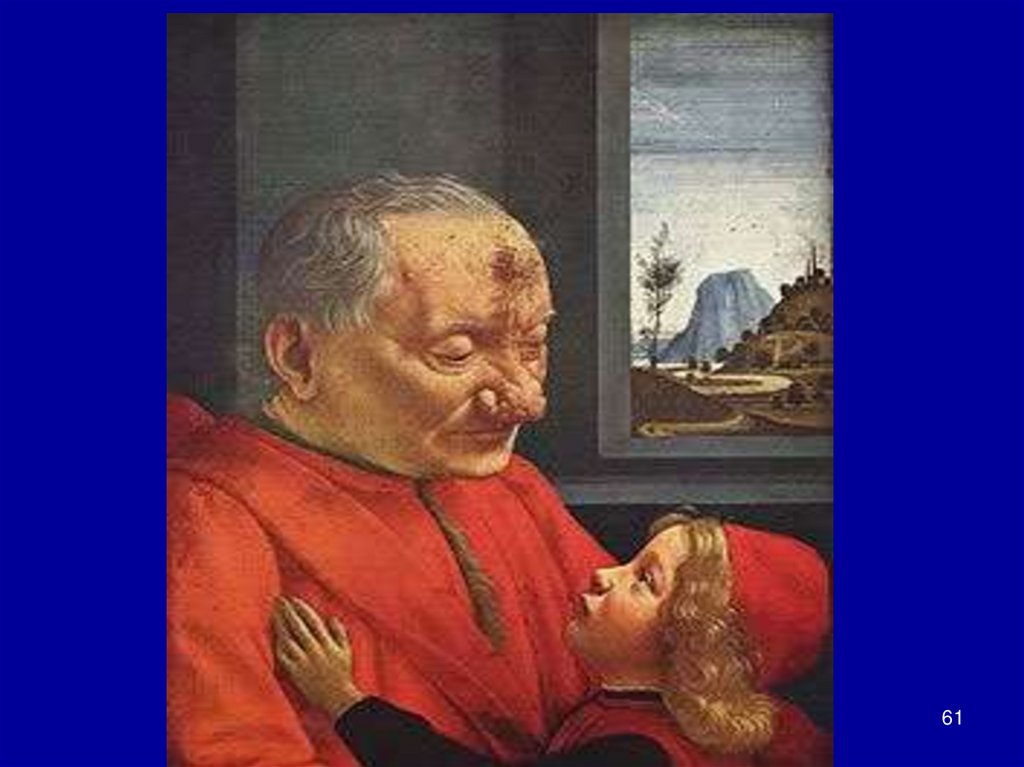
appeared in the works of Shakespeare. The famous Italian painter of
the early Renaissance D. Ghirlandaio first depicted a man suffering
from rosacea, to be strict rather a form of rosacea - rhinophyma in
the picture "An Old Man and His Grandson", done in 1480
(Louvre).
60
61.
6162.
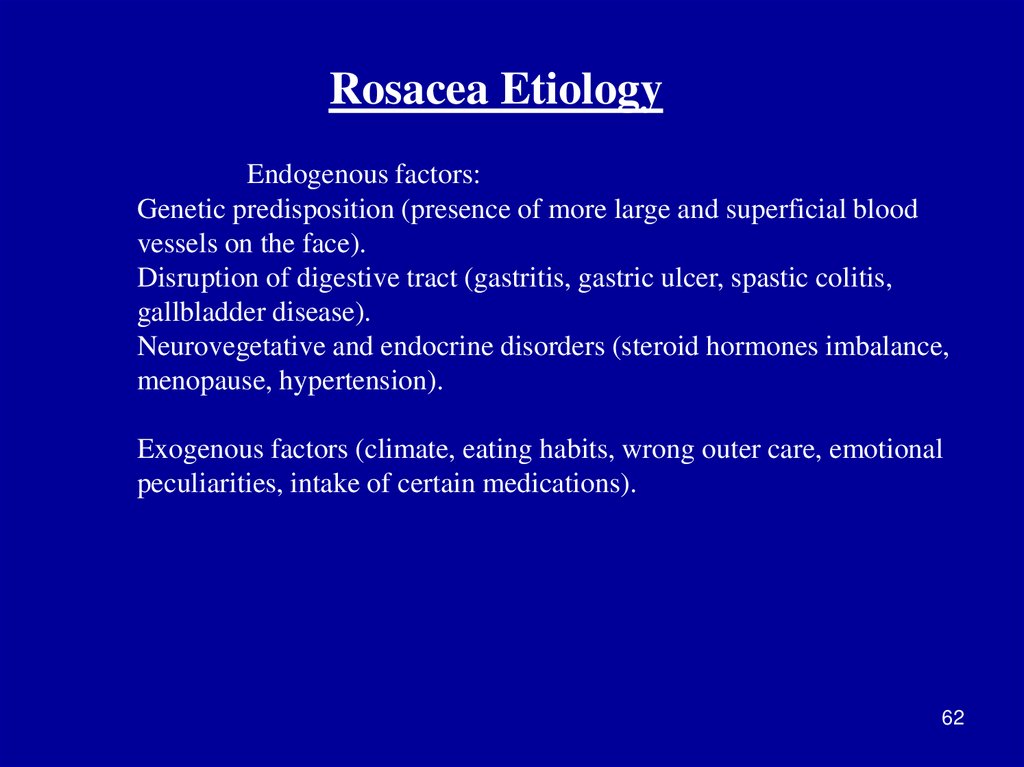
Rosacea EtiologyEndogenous factors:
Genetic predisposition (presence of more large and superficial blood
vessels on the face).
Disruption of digestive tract (gastritis, gastric ulcer, spastic colitis,
gallbladder disease).
Neurovegetative and endocrine disorders (steroid hormones imbalance,
menopause, hypertension).
Exogenous factors (climate, eating habits, wrong outer care, emotional
peculiarities, intake of certain medications).
62
63.
Rosacea Pathogenesis- Increased vascular permeability of the skin;
- Accumulation of mediators of inflammation
and metabolic products (serotonin, bradykinin,
prostaglandins, opioid peptides and gastrin);
-Degeneration of dermis matrix and vascular
endothelial damage.
63
64.
Classification of RosaceaG. Plewig and et al have proposed clinical classification based on the
sequence of stages:
I. Rosacea-diathesis is occasional hot flashes.
II. . Rosacea proper:
Stage 1: Erythematous-telangiektatic,
Stage 2: Pustulopapular (persistent erythema, telangiectasia, papules,
pustules),
Stage 3: Pustulonodular (persistent erythema, numerous telangiectasia,
papules, pustules and swollen nodes).
III. Special forms of rosacea: rosacea-steroid, granulomatous, Gramnegative, conglobate, fulminant, rosacea with a solid persistent facial
edema, ophthalmic rosacea, rhinophyma and "Phyma" of other
localizations.
64
65.
Rosacea proper is characterized bypersistent erythema predominantly of the nose
skin, usually with the presence of telangiektasia
with periodic rush of blood to the face as a result
of endogenous, psychogenic and external
stimuli. Demodex mites thus are completely
absent or are detected as single samples on the
skin, especially in the follicles of the nose.
Antiparasitic treatment has no effect in this case.
65
66.
Rosacea Proper66
67.
Rosacea ComplicatedWith DemodicosisIn this form, besides the usual phenomena of rosacea, there are
scattered micropapules and follicular micropustules, in which demodicids
are found. At anti-parasitic treatment pustules and papules disappear, but
persistent erythema and telangiectasia remain.
67
68.
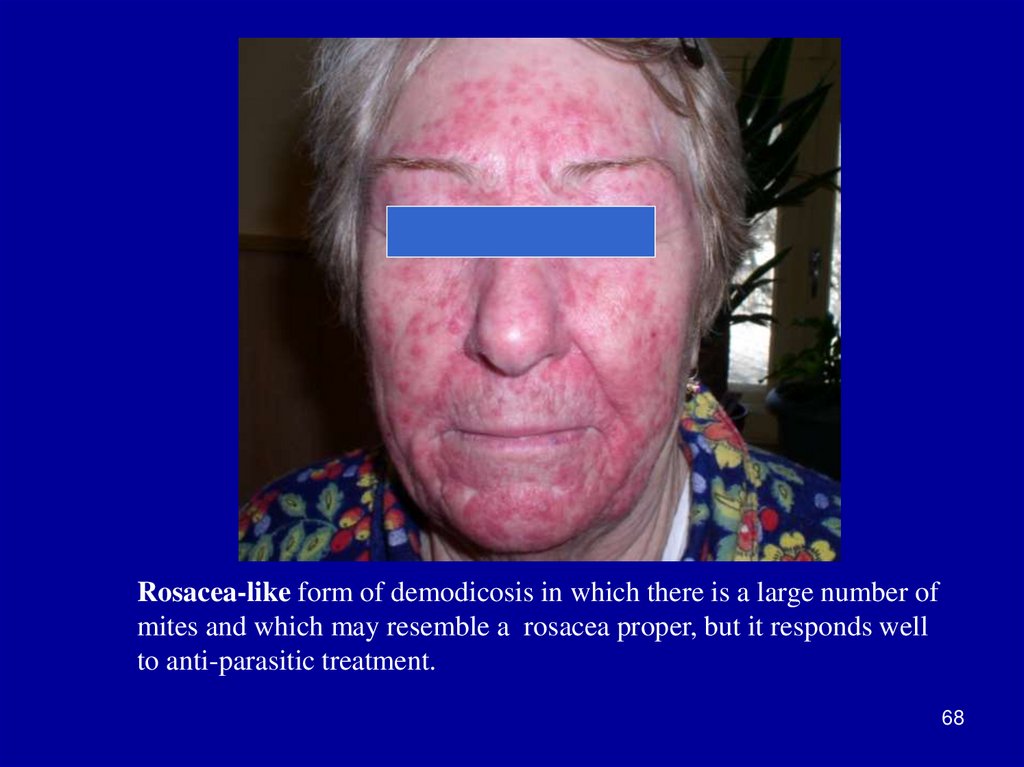
Rosacea-like form of demodicosis in which there is a large number ofmites and which may resemble a rosacea proper, but it responds well
to anti-parasitic treatment.
68
69. Ophthalmic Rosacea
• Blepharitis (erythema, desquamationand crusts on the edges of the
eyelids):
• Conjunctivitis
• Iritis
• Scleritis
Frequent symptom of rosacea, severity of the eye damage
• Keratitis
does not correspond to the severity of the skin process, in severe cases
it can lead to blindness.
69
70. Hypertrophic Rosacea
Rhinophyma;
Gnatophyma;
Metophyma;
Otophyma;
Blefarophyma.
It develops as a consequence of tissue hyperplasia of
subcutaneous fat and sebaceous glands. The skin thickens, takes on a
lumpy appearance, reminds orange peel. It is observed more frequently
in men.
70
71.
7172. Rosacea Treatment
• Elimination of etiological and precipitatingfactors;
• Treatment of comorbidity;
• Diet;
• Antibiotic treatment (imidazolesпротивогрибковые);
• Synthetic retinoids;
• Antihistamines;
• Venotonics and angioprotectors (Ascorutinum72
and Detralex).
73.
Topical TherapyTopical anti-inflammatory drugs: cold lotions with 1-2% solution
of resorcinol, boric acid, decoction of herbs, thermal water in the
form of aerosol.
Topical antibiotics and anti-parasitic (acaricidal) means prescribed
for rosacea papulopustular (Metronidazole, Erythromycin and
Clindamycin).
Azelaic acid.
Synthetic retinoids.
Cryotherapy.
For the destruction of telangiectasia laser therapy (argon, CO2
laser) is used.
Photoprotection.
Appropriate care (cosmetic Bioderma, Avene etc.).
Calcineurin inhibitors (Tacrolimus, Pimecrolimus).
73






















 Медицина
Медицина