Похожие презентации:
Biochemistry of thyroid hormones
1.
Prepared by: Zhumakanova T.MChecked by: Irina Ivanovna
Course: 2
Faculty: Dentistry
Semey 2017
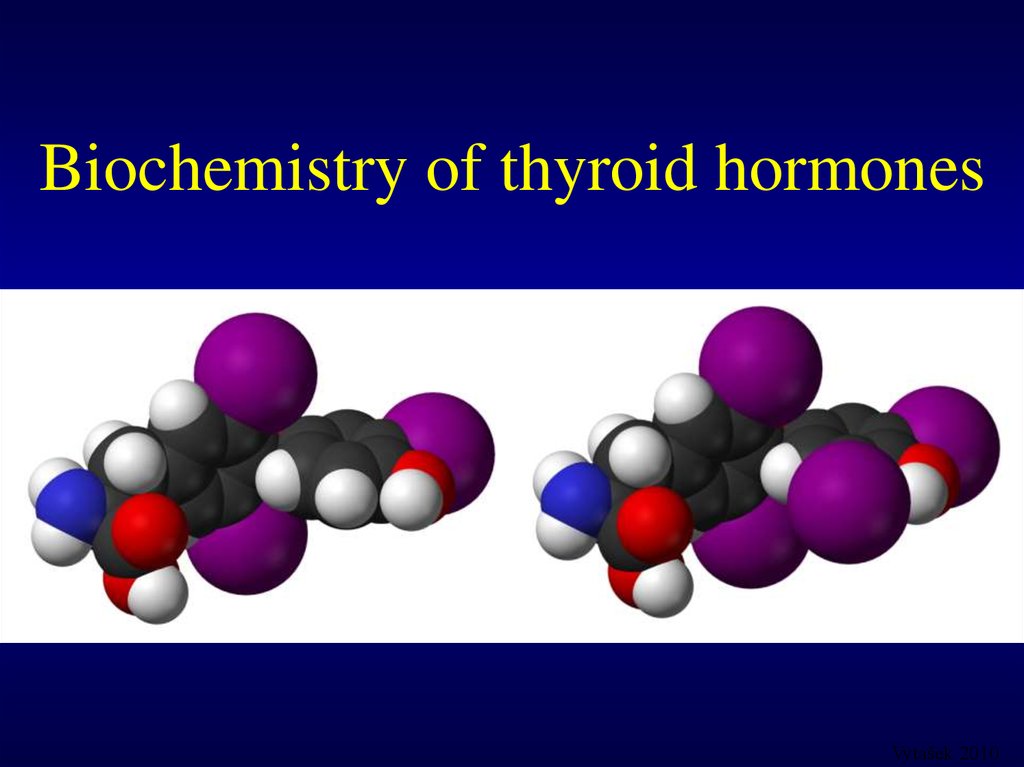
2. Biochemistry of thyroid hormones
Vytášek 20103.
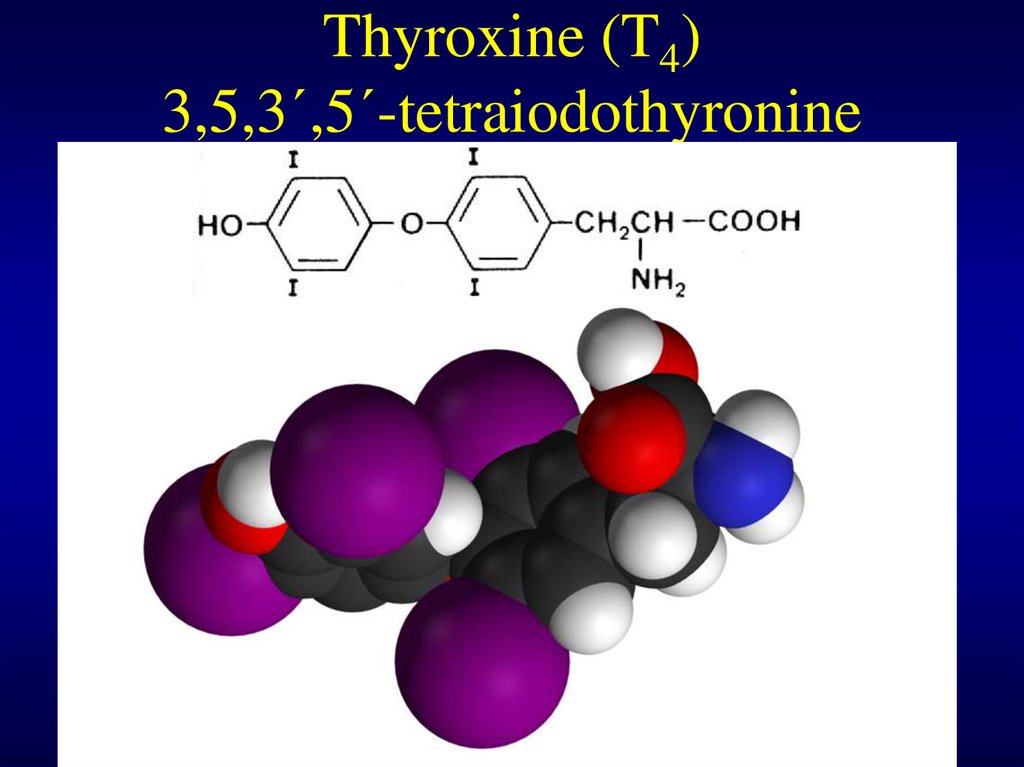
3,5,3´-triiodothyronine (T3)4. Thyroxine (T4) 3,5,3´,5´-tetraiodothyronine
5.
1) Biosynthesis of thyroid hormones andiodine metabolismus
2) Receptor for thyroid hormones and
mechanisms of regulation of basal
metabolismus by thyroid hormones
3) Regulation of production of thyroid
hormones, TSH, receptor of TSH, TRH
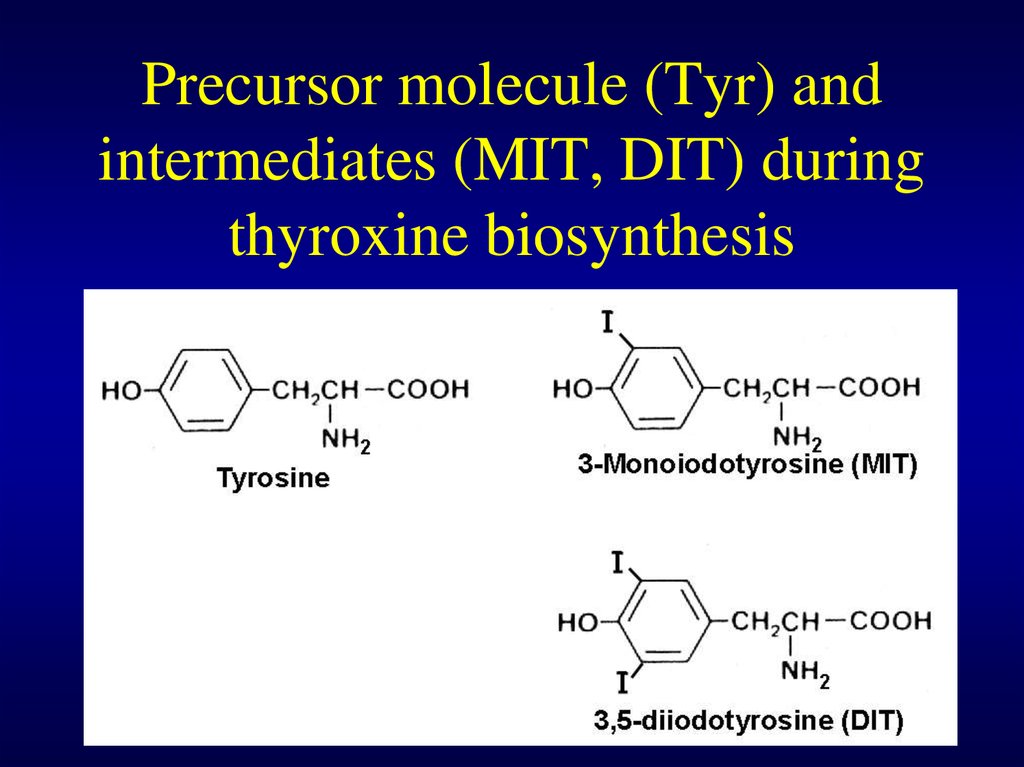
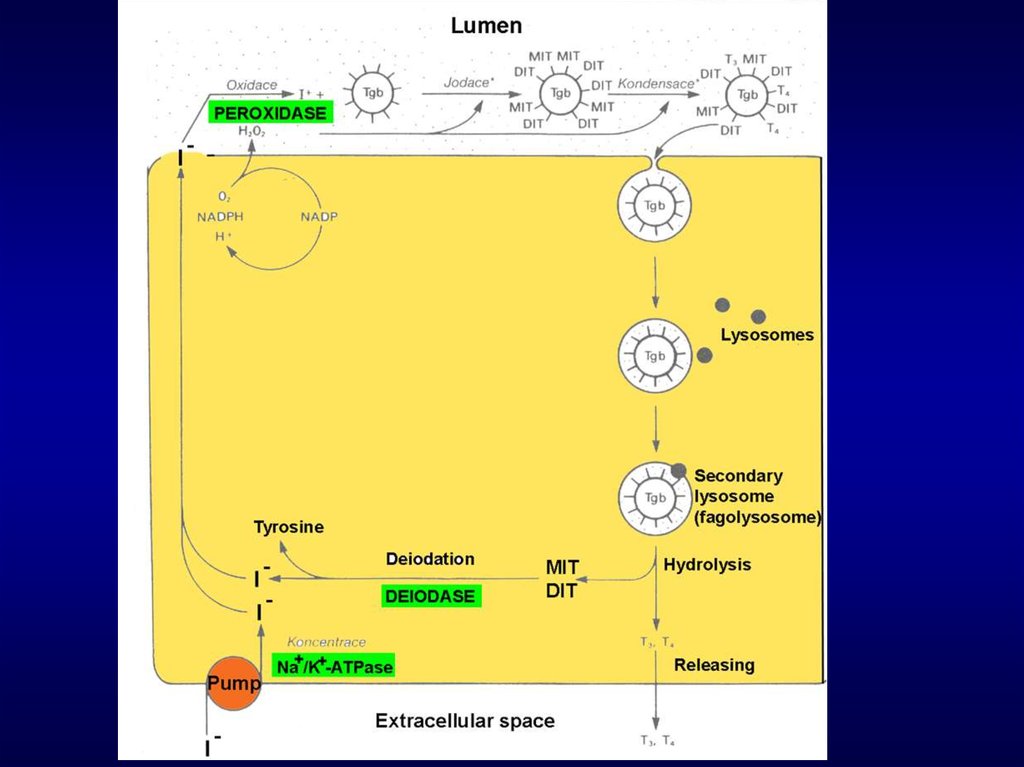
6. Biosynthesis of thyroxine
• The main synthetized thyroid hormone isthyroxine, but triiodothyronine is tentimes more
potent
• Precursor molecule for synthesis thyroid
hormones is tyrosine derivative
• Biosynthesis is perfomed on tyrosine residues
bound in protein of thyroid gland – thyreoglobulin
• The first step is transport of iodide into cells of
folicle cells of thyroid gland
• Active transport of iodide into the follicle cell is
mediated iodide pump (the concentration outside
is 25times lower than inside)
7. Biosynthesis of thyroxine
• Thyreoglobulin, secreted into the lumen ofthyroid gland, is iodinated in one or two
positions of phenol ring of tyrosine residues
• Iodination reagent is iodosyl cation I+, vhich
is produced by two electron oxidation of
iodide with hydrogen peroxide under
catalysis of enzyme thyroid peroxidase
• Electrophilic substitution of tyrosine ring by
iodine in position 3 and 5 is pure chemical
reaction
8. Precursor molecule (Tyr) and intermediates (MIT, DIT) during thyroxine biosynthesis
9. Biosynthesis of T4 from DIT
• Next reaction of DIT leads probably tocreation reactive radical of DIT
• This reactive radical condensates with other
DIT residue and generates thyroxine residue
(bound in thyreoglobulin)
• Under normal condition 70% of tyrosine
residues of thyreoglobulin are in the form
MIT and DIT and 30% as thyroxine (with
minor part of T3)
10. Schematic draw of condensation of DIT
11. Secretion of thyroid hormones
• Endocytosis of iodinated thyreoglogulin fromlumen into the cell
• Fusion of endocytic vesicles with primary
lysosomes
• Degradation of thyreoglobulin in secondary
lysosomes and liberating T3 a T4 into the
circulation out of cell
• 70% of iodine bound by threoglobulin is in the
form MIT and DIT and after liberation from
thyreoglobulin these compounds are deionidated
by enzyme deionidase and tyrosine and iodide is
returned to further utilisation
12.
13. Transport of thyroid hormones by blood
• Thyroid hormones are hydrophobic compounds andtherefore they used for its transport carrier protein
• The main transporting protein is thyroxine binding
globulin (TBG). Its affinity for T4 is 10 times higher than
for T3 . The further proteins, binding thyroid hormones, are
thyroxine binding prealbumin and albumin. More than
99% of T4 is bound on plasma proteins.
• During this period the part of T4 is deionidated to T3
because this form is tentimes more metabolically active.
Conversion of T4 to T3 is also observed in cytosol after
transport into the target cell
14. Structural similarities among receptors for steroid and thyroid hormones
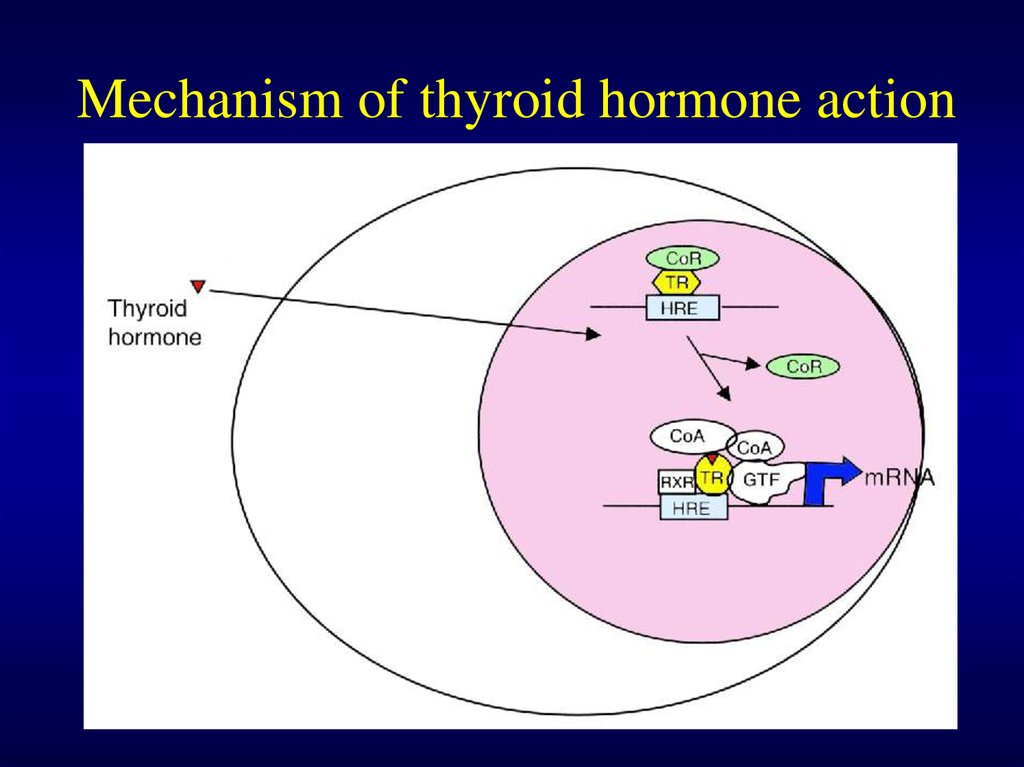
15. Mechanism of thyroid hormone action
• Receptors for thyroid hormones are nuclear and its affinityis tentimes higher for T3 than T4
• The amount of nuclear receptors is very low
• Four variants of nuclear receptor were observed and
mitochondrial receptor for T3 was also described
• Free thyroid hormone receptor (TR) without bound
hormone is bound to hormone response element of DNA
(HRE) and corepressor (CoR)
• After binding T3 to receptor - CoR is liberated and
coactivators (CoA) is bound and the transcription to
mRNA begins
16. Mechanism of thyroid hormone action
17. Increased expression of proteins by thyroid hormones
• Glycerol 3-phosphate dehydrogenase – maincomponent of glycerol 3-phosphate shuttle in
mitochondria (one of transport systems for NADH into
mitochondria)
• Cytochrome c oxidase – the complex mitochondrial
enzyme in the electron transport chain (from
cytochrome c to oxygen)
• ATPases – (eg. Ca ATPase of muscle cells)
• Carbamyl phosphate synthase – enzyme of urea
cycle
• Growth hormone
18. Increased respiration during hyperthyreodism
Increased synthesis of ATP – increasedsynthesis of cytochrome c oxidase –
increased oxidative phosphorylation (it means
the increased consumption of oxygen) –
increased production of ATP
Increased consumption of ATP – increased
synthesis of various ATPase (eg. Ca
dependent in muscles) – increased depletion
of store of ATP
19. Mechanisms increasing body temperature during hyperthyroidism
Reducing efficiency of ATP synthesis - increasedsynthesis of glycerol 3-phosphate dehydrogenase –
increased transport NADH by this shuttle than
malate/aspartate shuttle
Increased synthesis of ATP
Increased consumption of ATP
Uncoupling of phosphorylation and oxidation in
mitochondria
20. Control of thyroid hormone synthesis and secretion
• Pituitary hormone thyreotropin (TSH) upregulatesactivity of iodide pump of follicle cells of thyroid
gland
• Endocytosis of iodinated thyreoglobulin and
following secretion of T3 and T4 is also
upregulated by TSH
• Production of TSH is upregulated by TRH and
controled by thyroid hormones via negative
feedback
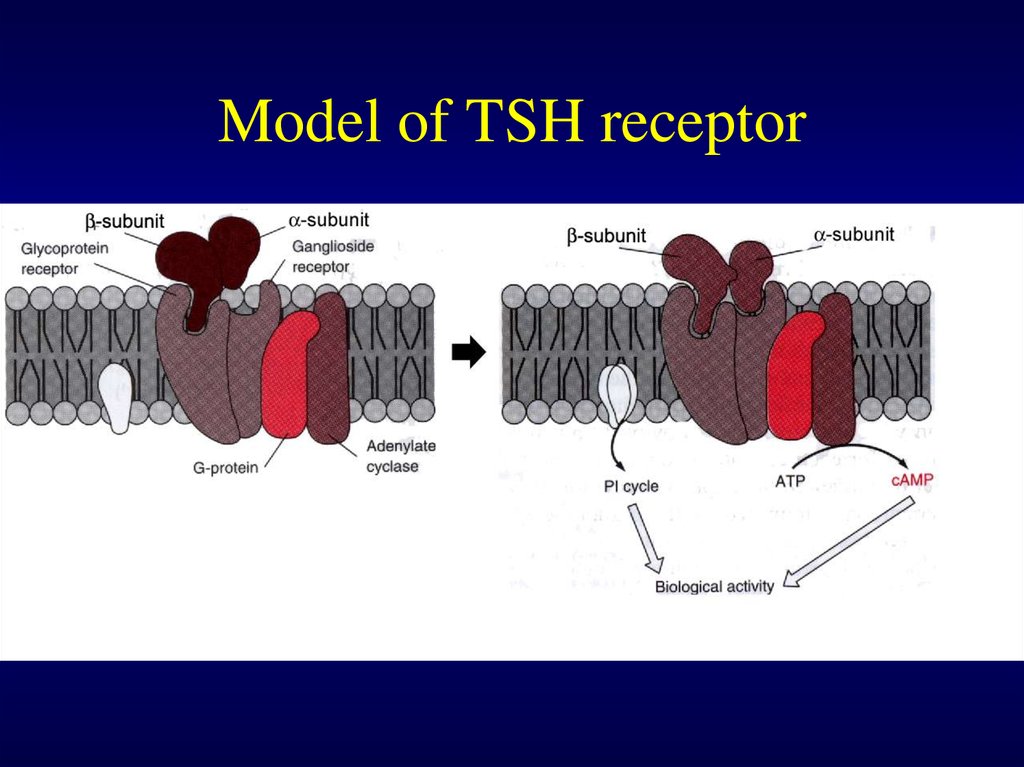
21. Model of TSH receptor
22. Myxedema (myxoedema)
• Hypothyreoid myxedema is specific form of skinedema
• Increased activity of connective tissues leads to
increased deposition of components of extracellular
matrix (mainly glycosaminoglycans, proteoglycans)
which retains large amounts of sodium ions and water
• Stimulation of fibroblasts is caused by increased
amount of TSH which is able to bind to some
membrane receptors and by this way it activates
biosynthesis of extracellular matrix
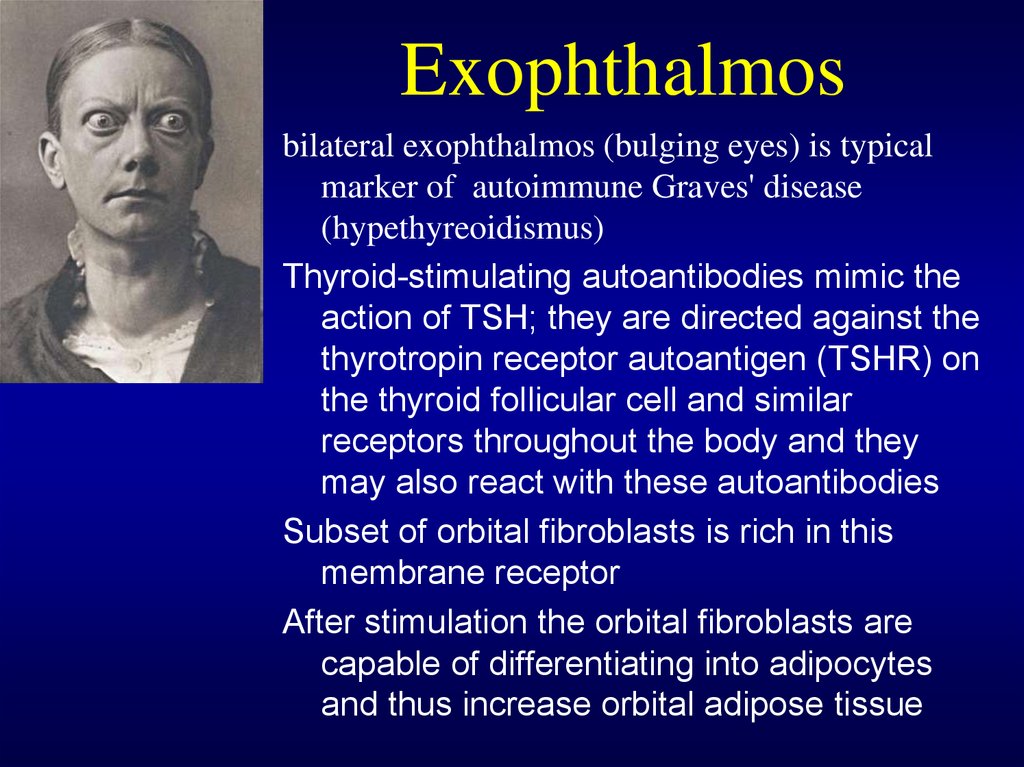
23. Exophthalmos
bilateral exophthalmos (bulging eyes) is typicalmarker of autoimmune Graves' disease
(hypethyreoidismus)
Thyroid-stimulating autoantibodies mimic the
action of TSH; they are directed against the
thyrotropin receptor autoantigen (TSHR) on
the thyroid follicular cell and similar
receptors throughout the body and they
may also react with these autoantibodies
Subset of orbital fibroblasts is rich in this
membrane receptor
After stimulation the orbital fibroblasts are
capable of differentiating into adipocytes
and thus increase orbital adipose tissue





 Биология
Биология Химия
Химия