Похожие презентации:
Acute myeloid leukemia
1. Acute myeloid leukemia
С.Ж.АСФЕНДИЯРОВ АТЫНДАҒЫҚАЗАҚ ҰЛТТЫҚ МЕДИЦИНА УНИВЕРСИТЕТІ
КАЗАХСКИЙ НАЦИОНАЛЬНЫЙ МЕДИЦИНСКИЙ
УНИВЕРСИТЕТ ИМЕНИ С.Д.АСФЕНДИЯРОВА
Department of Pathological Anatomy
Acute myeloid
leukemia
Prepared by:
GM 14-24-2
Imangali Maira
Sotsialova Aidana
Checked by:
Head of department of Pathological Anatomy
Sapargaliyeva Aigul
2. PLAN
Introduction
Pathogenesis
Classification
Types
Conclusion
3. INTRODUCTION
• Acute myeloid leukemia (AML),• also known as acute myelogenous leukemia or
acute nonlymphocytic leukemia (ANLL),
• is a cancer of the myeloid line of blood cells,
characterized by the rapid growth of abnormal
white blood cells that accumulate in the bone
marrow and interfere with the production of normal
blood cells.
4. Pathogenesis
5.
6.
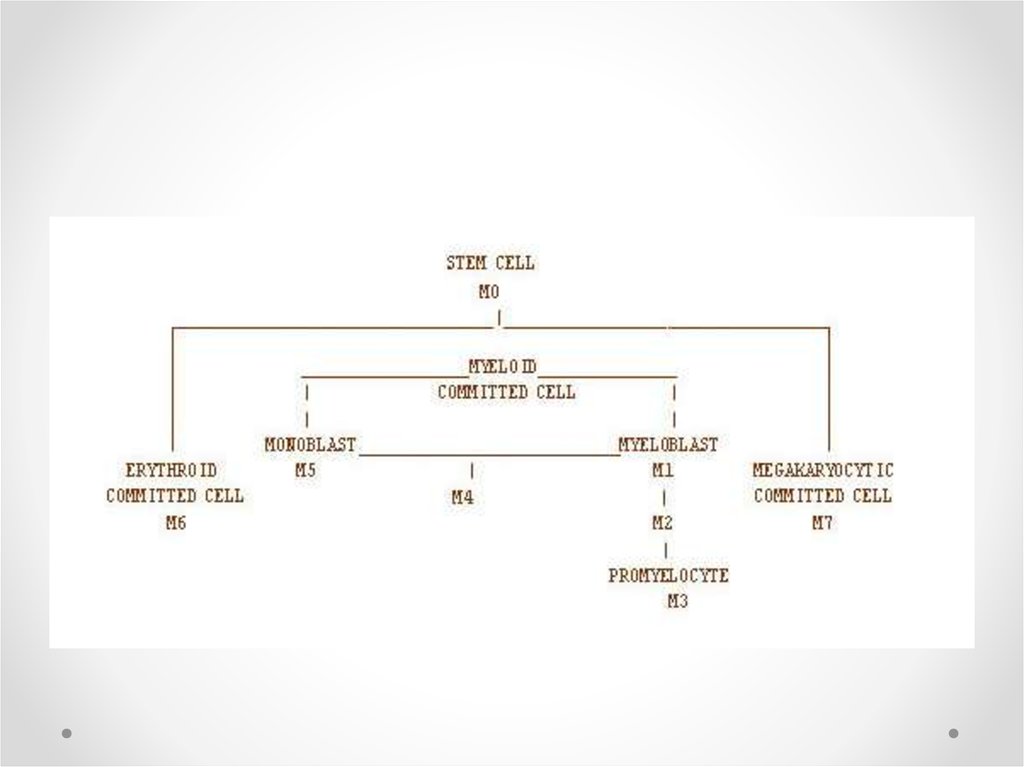
• Modern classification schemes for AML recognizethe characteristics and behavior of the leukemic
cell (and the leukemia) may depend on the stage
at which differentiation was halted.
7. Classification
8.
9.
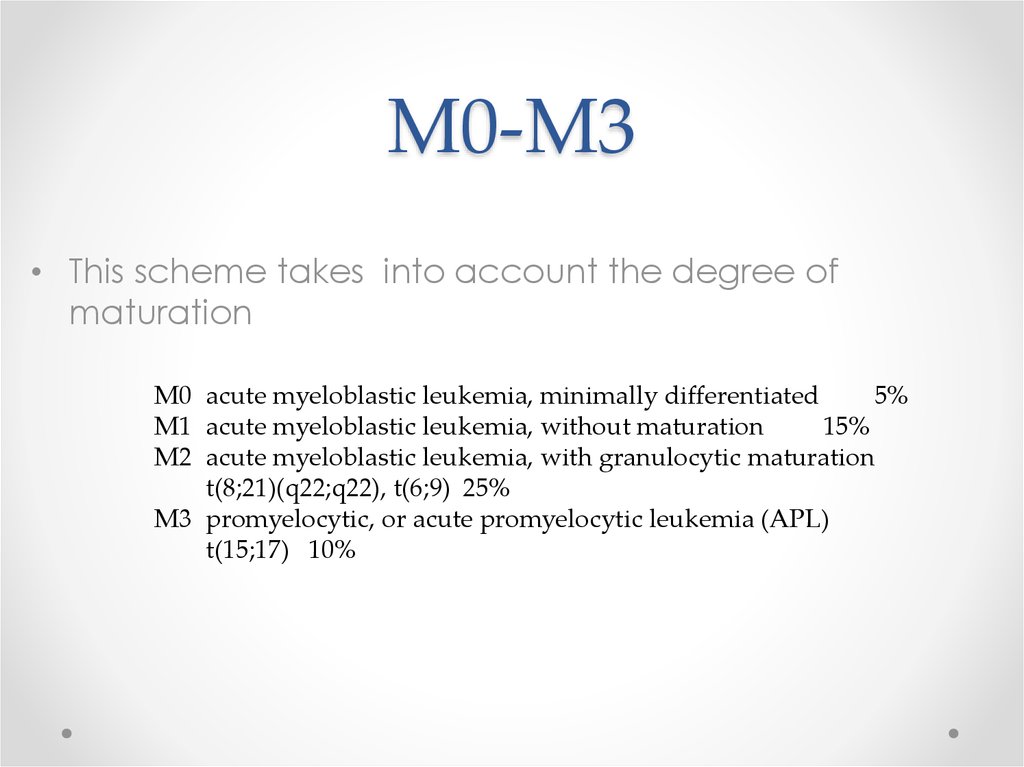
10. M0-M3
• This scheme takes into account the degree ofmaturation
M0 acute myeloblastic leukemia, minimally differentiated
5%
M1 acute myeloblastic leukemia, without maturation
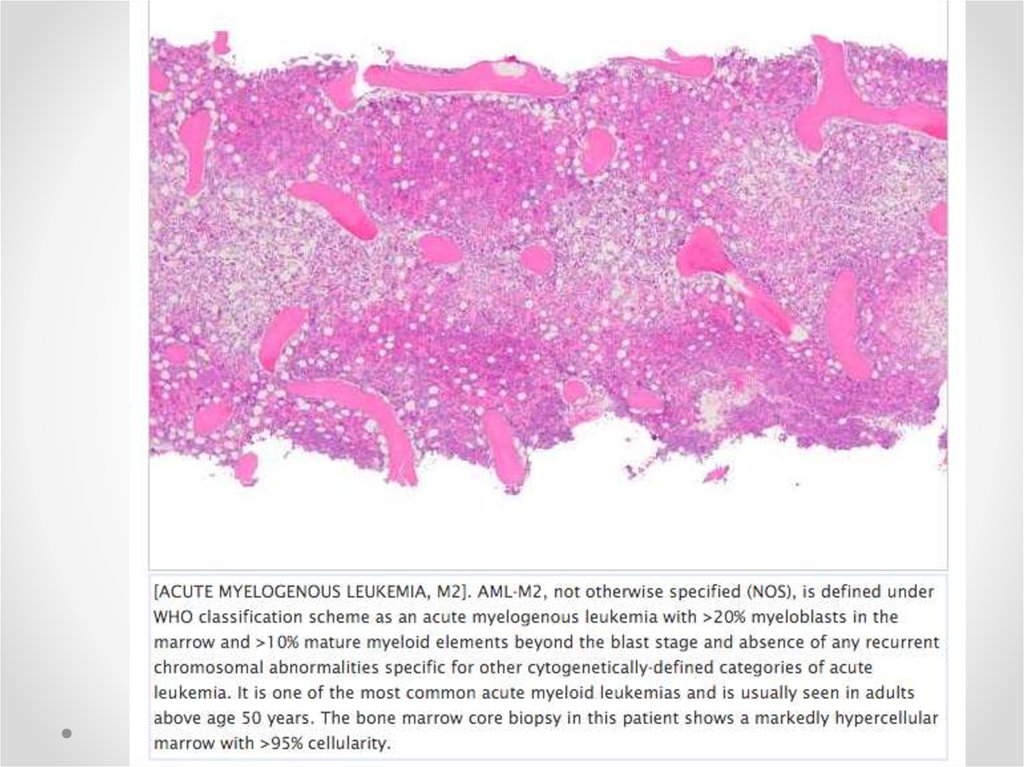
15%
M2 acute myeloblastic leukemia, with granulocytic maturation
t(8;21)(q22;q22), t(6;9) 25%
M3 promyelocytic, or acute promyelocytic leukemia (APL)
t(15;17) 10%
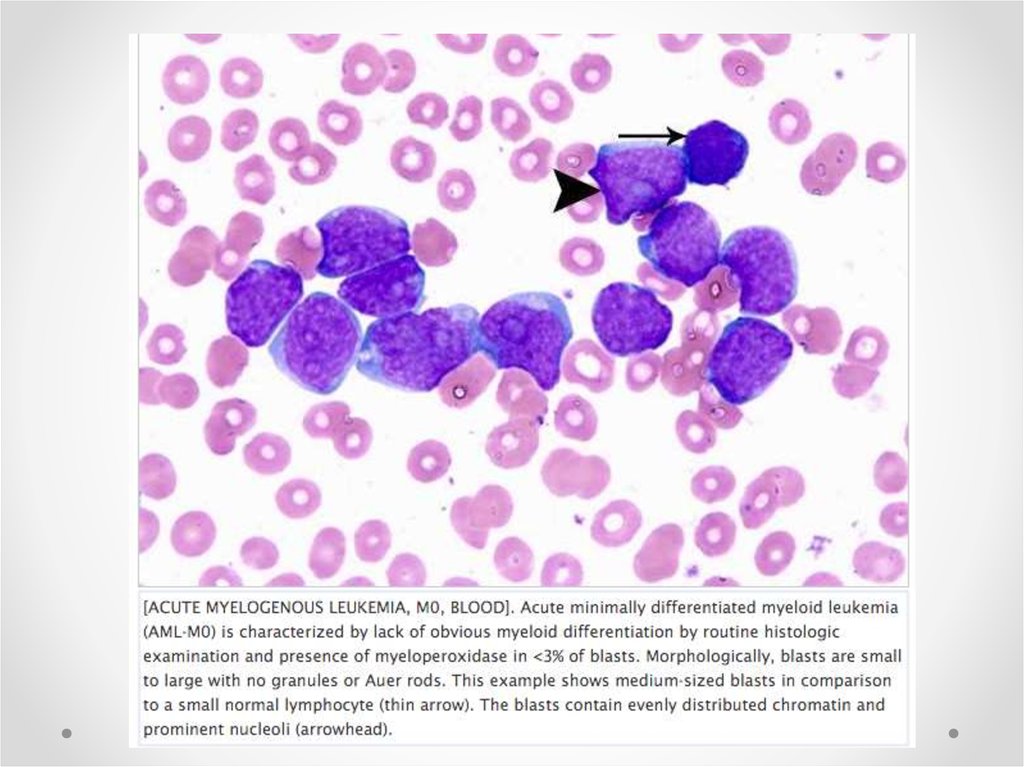
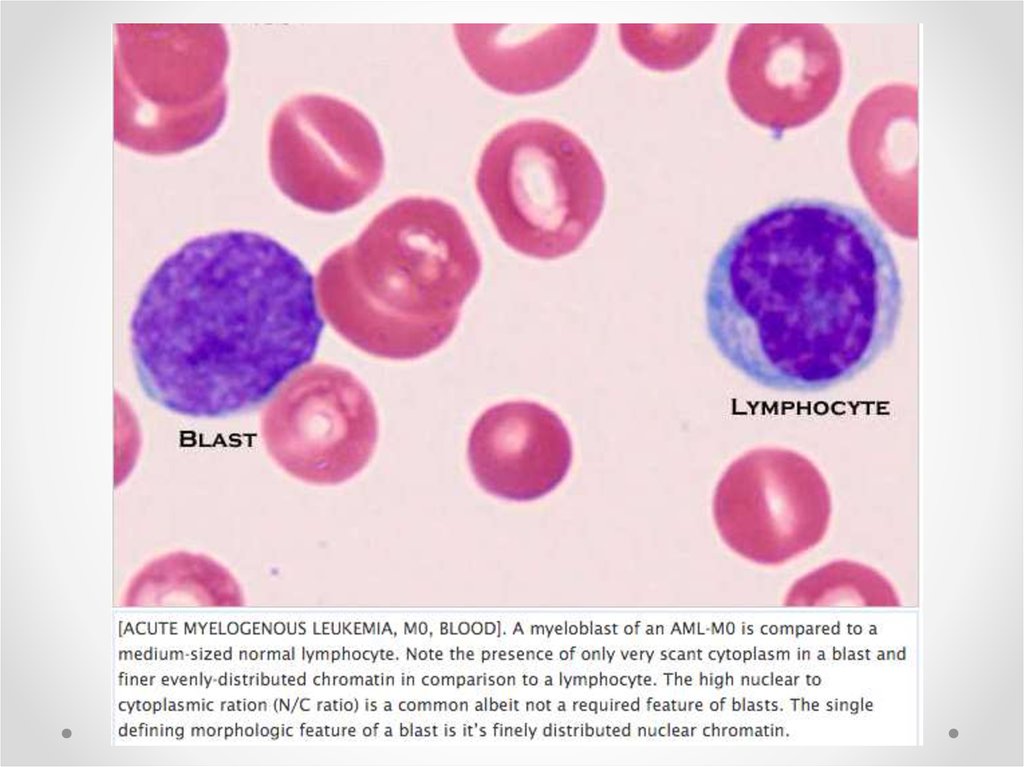
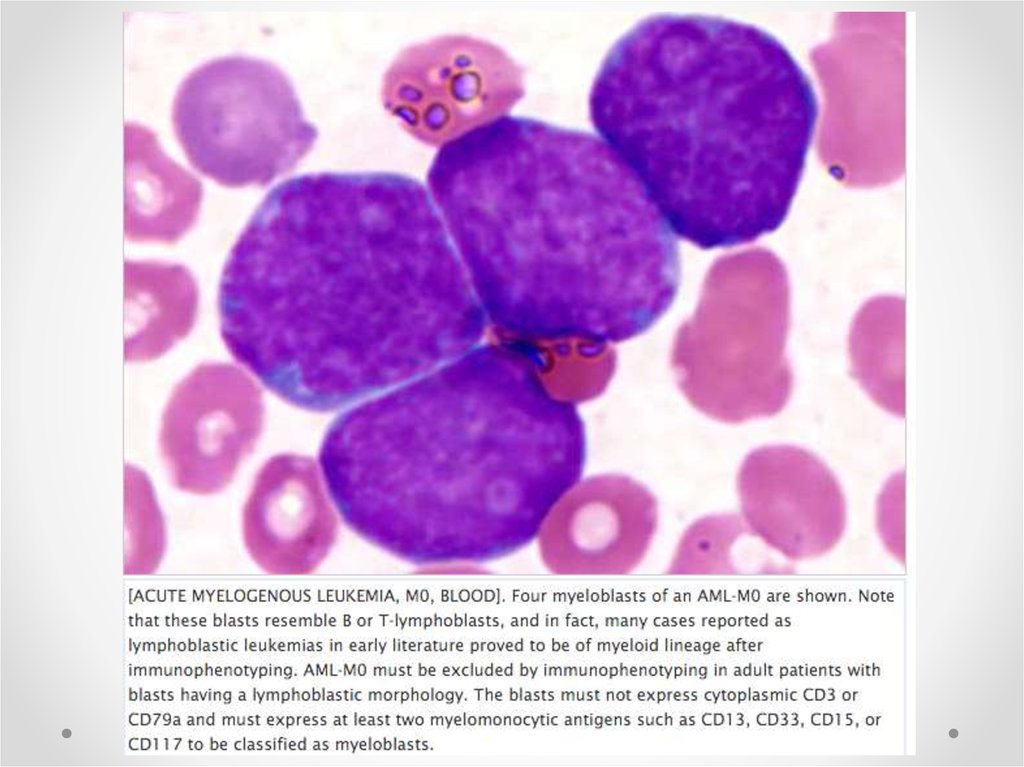
11. Minimally differentiated acute myeloblastic leukemia(M0)
12.
13.
14.
15. Acute myeloblastic leukemia without maturation(M1)
16.
[ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. AML-M1 is defined by presenceof more than 90% myeloblasts in blood and/or bone marrow and lack of any recurring
chromosomal abnormalities such as t(8;21), t(15;17), inv(16) or t(16;16)(p13;q22). The
distinction between AML-M1 and AML-M2 not otherwise specified can be arbitrary
than real since it merely depends on the blast count. AML-M1 is also known as AML
without maturation. Most blasts are large and typical of myeloblasts with prominent
nucleoli.
17.
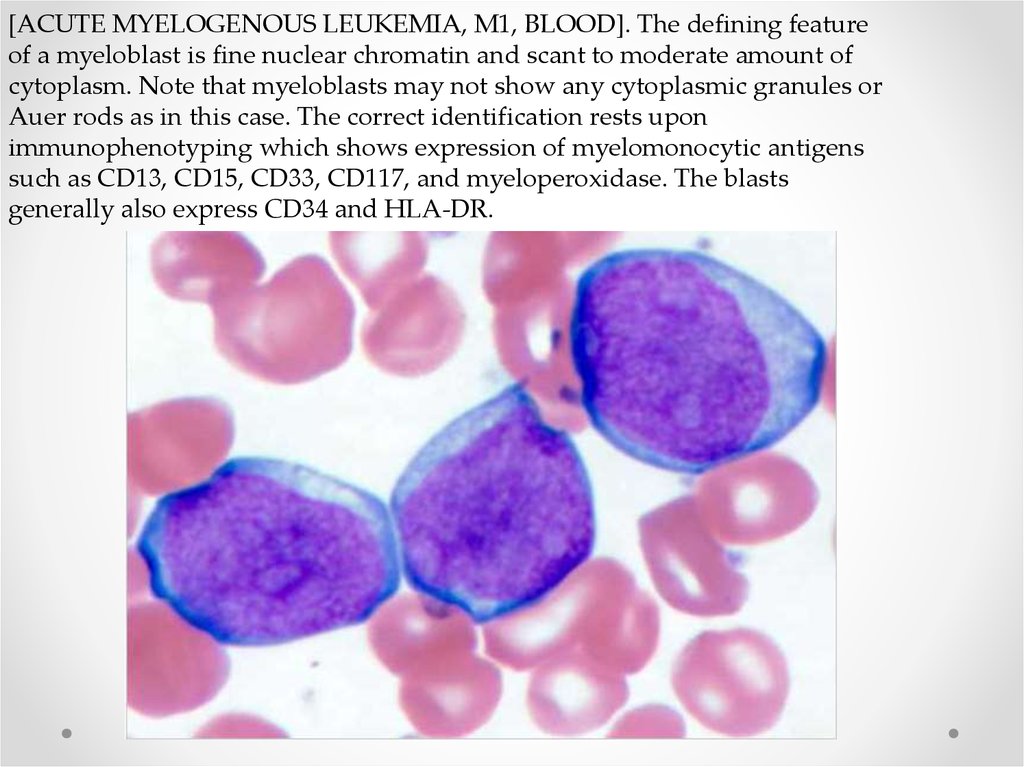
[ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. The defining featureof a myeloblast is fine nuclear chromatin and scant to moderate amount of
cytoplasm. Note that myeloblasts may not show any cytoplasmic granules or
Auer rods as in this case. The correct identification rests upon
immunophenotyping which shows expression of myelomonocytic antigens
such as CD13, CD15, CD33, CD117, and myeloperoxidase. The blasts
generally also express CD34 and HLA-DR.
18.
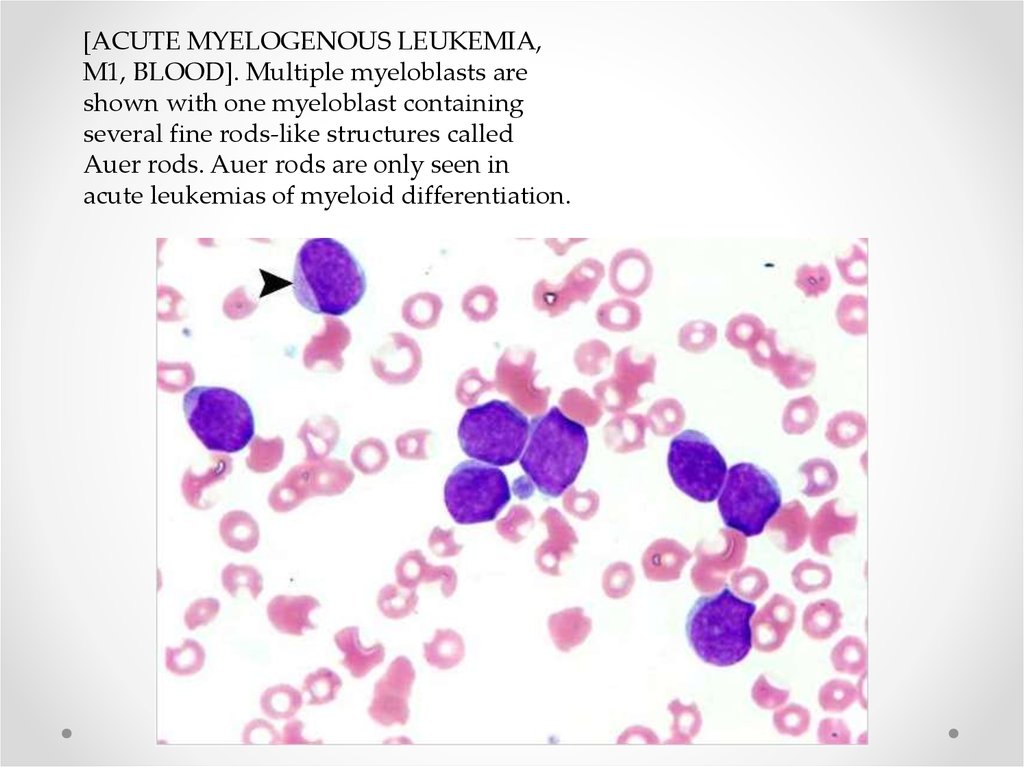
[ACUTE MYELOGENOUS LEUKEMIA,M1, BLOOD]. Multiple myeloblasts are
shown with one myeloblast containing
several fine rods-like structures called
Auer rods. Auer rods are only seen in
acute leukemias of myeloid differentiation.
19. Acute Myeloid Leukemia with Maturation (AML-M2)
Acute Myeloid Leukemiawith Maturation (AMLM2)
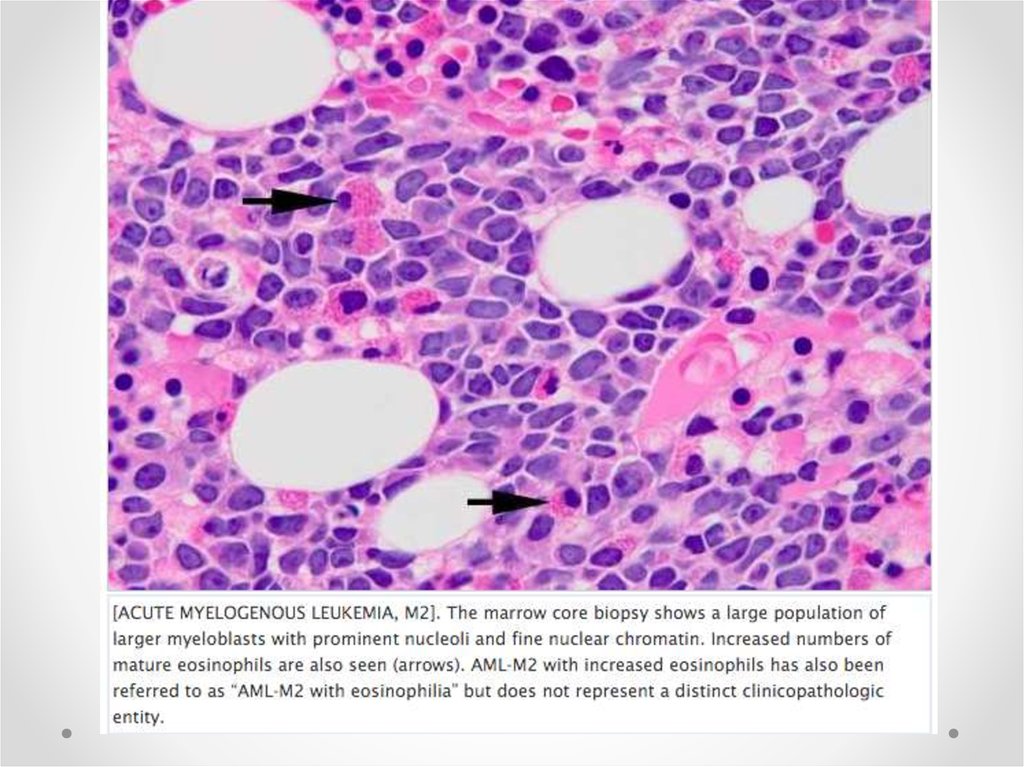
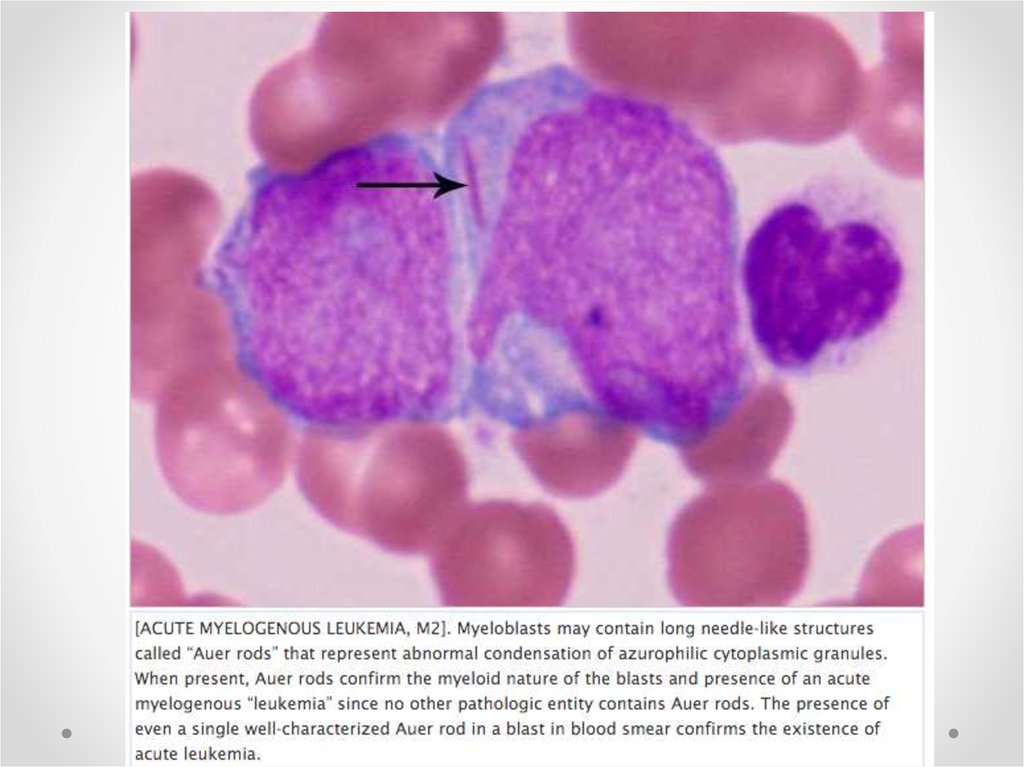
20.
21.
22.
23. Acute promyelocytic leukemia M3
24.
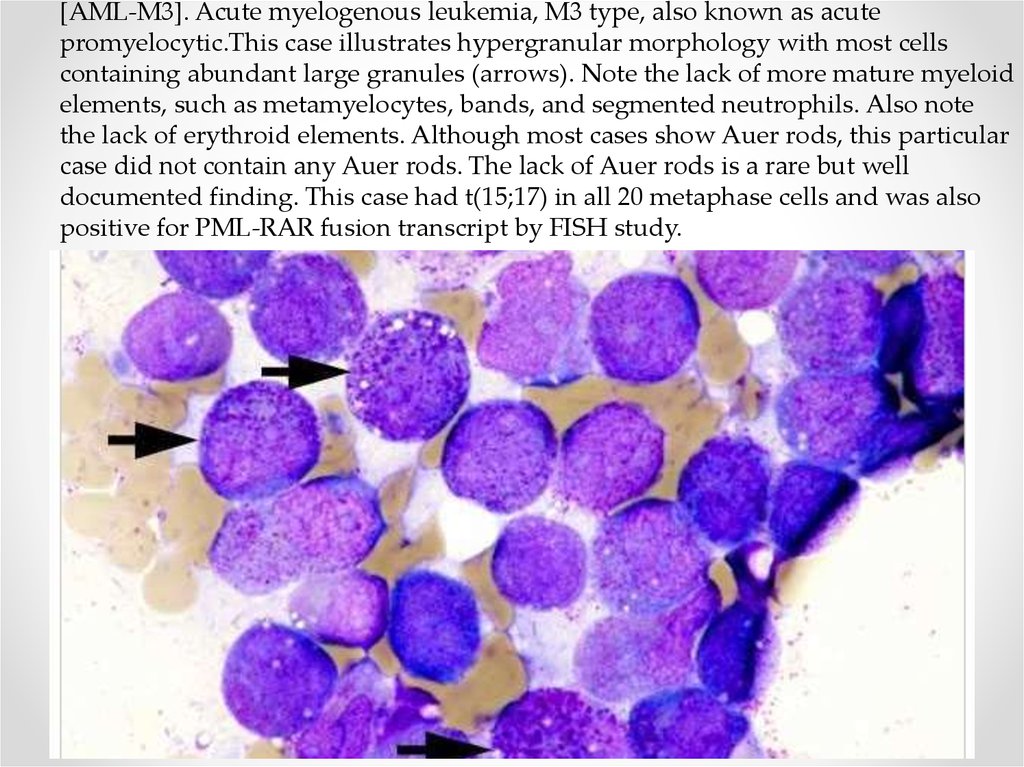
[AML-M3]. Acute myelogenous leukemia, M3 type, also known as acutepromyelocytic.This case illustrates hypergranular morphology with most cells
containing abundant large granules (arrows). Note the lack of more mature myeloid
elements, such as metamyelocytes, bands, and segmented neutrophils. Also note
the lack of erythroid elements. Although most cases show Auer rods, this particular
case did not contain any Auer rods. The lack of Auer rods is a rare but well
documented finding. This case had t(15;17) in all 20 metaphase cells and was also
positive for PML-RAR fusion transcript by FISH study.
25.
[AML-M3].This photomicrograph shows another important morphologic feature ofhypergranular type; specifically, not only intact cells with abundant granulation are
identified (arrow) but many ruptured cells are also seen releasing their granules free
onto the slide (four arrowheads). The leukemic cells appear to be more fragile than
normal promyelocytes and break apart upon smearing on the slides. In the absence
of Auer rods, presence of abundant free large granules helps in differentiating
leukemic promyelocytes from normal promyelocytes.
26.
AML-M3. This image depicts another morphologic feature of acute promyelocyticleukemia, that is, polarity of cytoplasmic granulation. In many cells the granules tend to
polarize toward one portion of the cytoplasm and the nucleus on the opposite side
(arrows). In normal promyelocytes the granules are distributed rather evenly
throughout the cytoplasm and polarization is not a distinct and obvious feature. When
cytoplasmic granulation is heavy and polarized it is a good telltale morphologic sign of
acute promyelocytic leukemia in the appropriate clinical context.
27.
AML-M3. Acute promyelocytic leukemia often shows cells having dumbbell shapedor convoluted nuclear lobes (arrows). This feature is more common with
hypogranular/microgranular form than hypergranular type but a few cells can
usually be found in the hypergranular type as well. Normal promyelocytes DO NOT
have dumbbell shaped or convoluted nuclear lobes.
28.
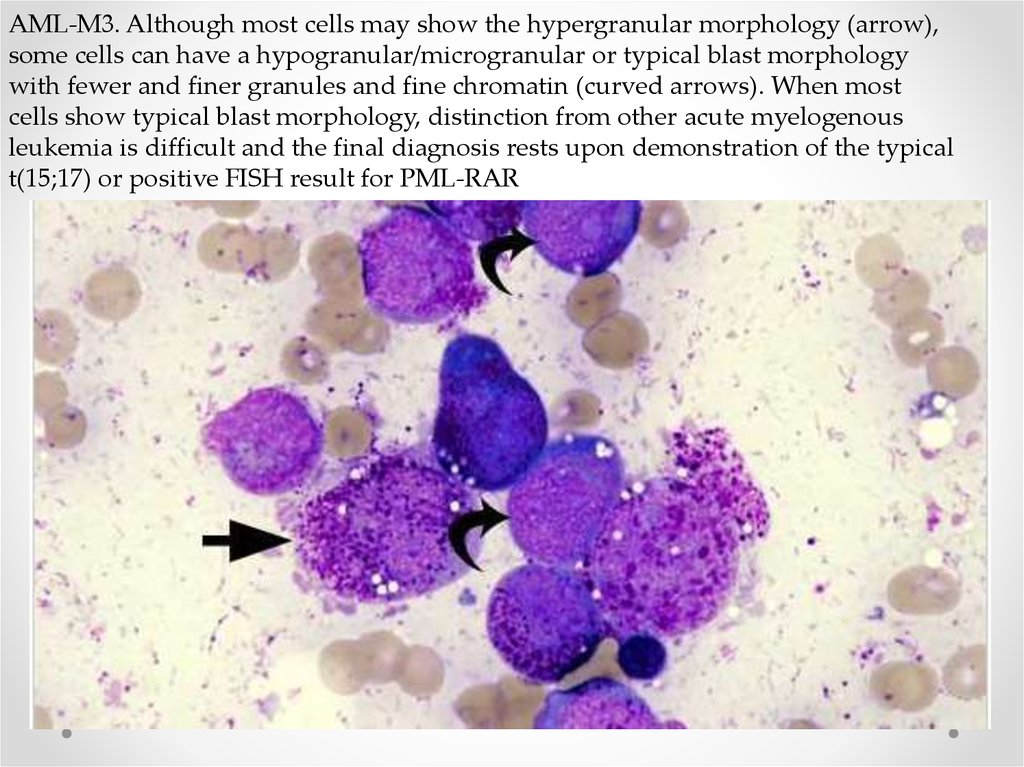
AML-M3. Although most cells may show the hypergranular morphology (arrow),some cells can have a hypogranular/microgranular or typical blast morphology
with fewer and finer granules and fine chromatin (curved arrows). When most
cells show typical blast morphology, distinction from other acute myelogenous
leukemia is difficult and the final diagnosis rests upon demonstration of the typical
t(15;17) or positive FISH result for PML-RAR
29. M4-M7
• Lineage of the leukemic blasts:M4 acute myelomonocytic leukemia
inv(16)(p13q22),
del(16q) 20%
M4eo
myelomonocytic together with bone marrow
eosinophilia inv(16), t(16;16) 5%
M5 acute monoblastic leukemia (M5a) or acute monocytic
leukemia (M5b) del (11q), t(9;11), t(11;19) 10%
M6 acute erythroid leukemias, including erythroleukemia
(M6a) and very rare pure erythroid leukemia (M6b)
5%
M7 acute megakaryoblastic leukemia t(1;22) 5%
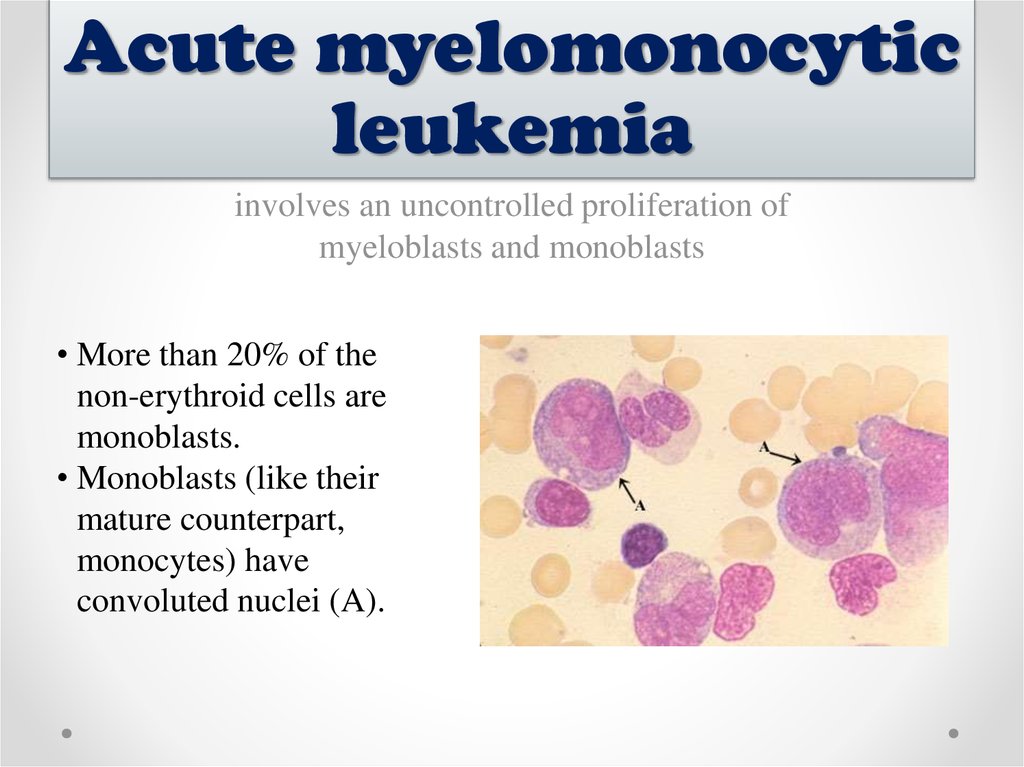
30. Acute myelomonocytic leukemia
involves an uncontrolled proliferation ofmyeloblasts and monoblasts
• More than 20% of the
non-erythroid cells are
monoblasts.
• Monoblasts (like their
mature counterpart,
monocytes) have
convoluted nuclei (A).
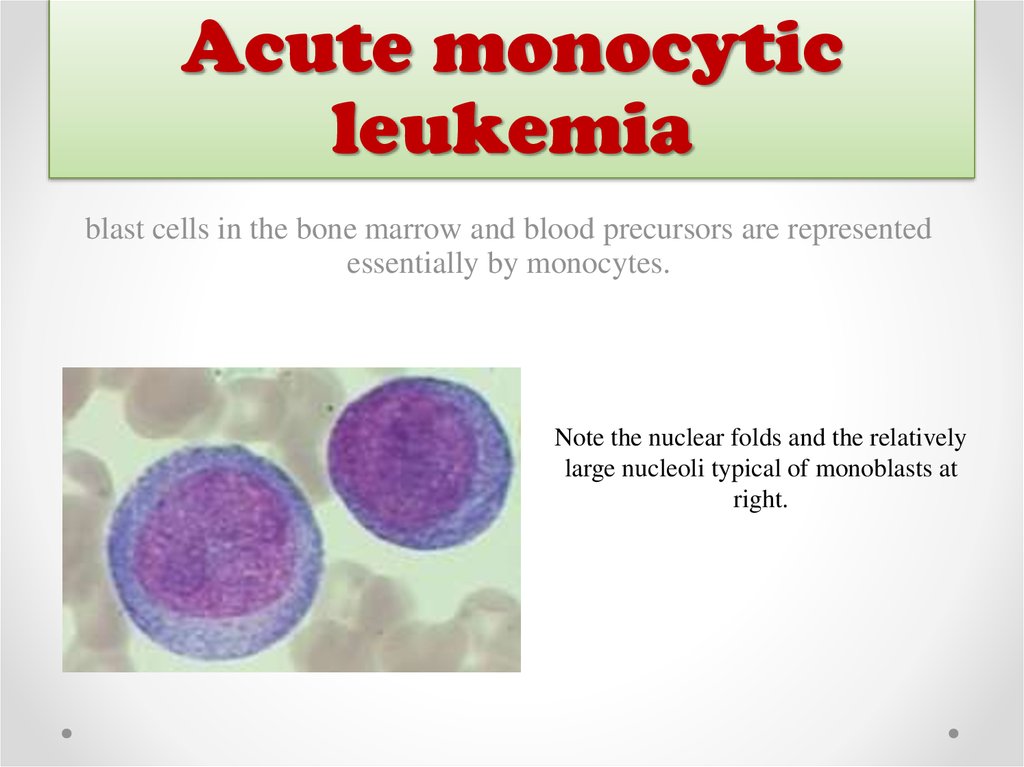
31. Acute monocytic leukemia
blast cells in the bone marrow and blood precursors are representedessentially by monocytes.
Note the nuclear folds and the relatively
large nucleoli typical of monoblasts at
right.
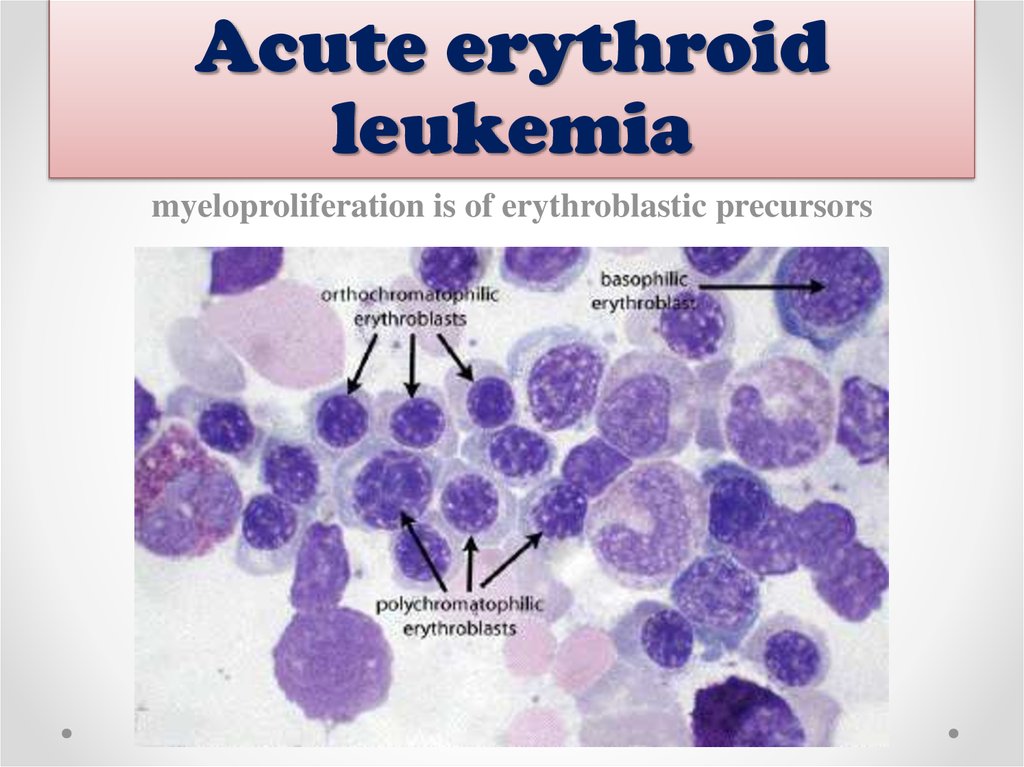
32. Acute erythroid leukemia
myeloproliferation is of erythroblastic precursors33. Types
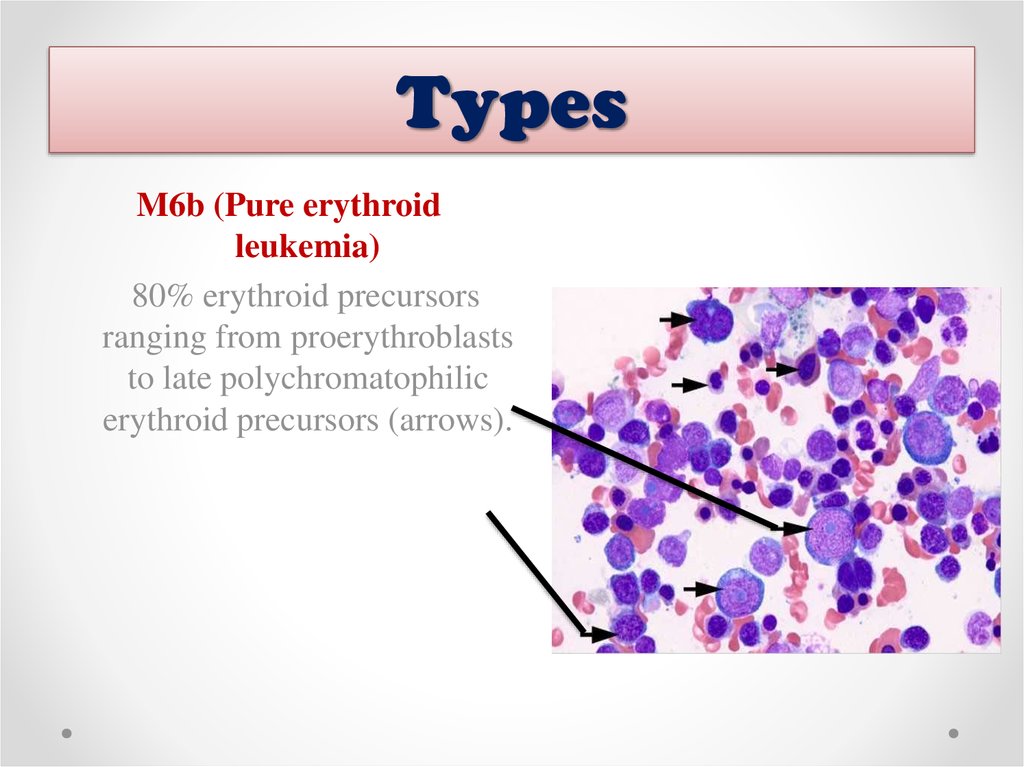
M6b (Pure erythroidleukemia)
80% erythroid precursors
ranging from proerythroblasts
to late polychromatophilic
erythroid precursors (arrows).
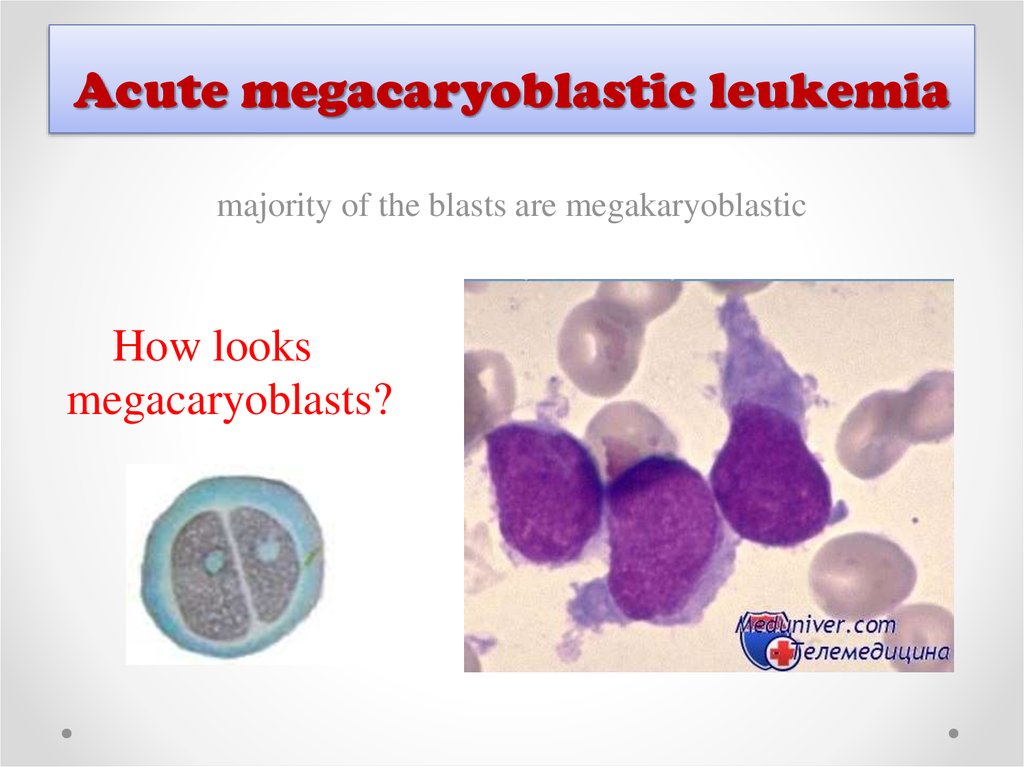
34. Acute megacaryoblastic leukemia
majority of the blasts are megakaryoblasticHow looks
megacaryoblasts?
35.
Diagnosis requires more than 20% Blasts in the marrow/peripheral blood with more than 50% demonstrating
megakaryocytic derivation by morphology
20%
50%
36.
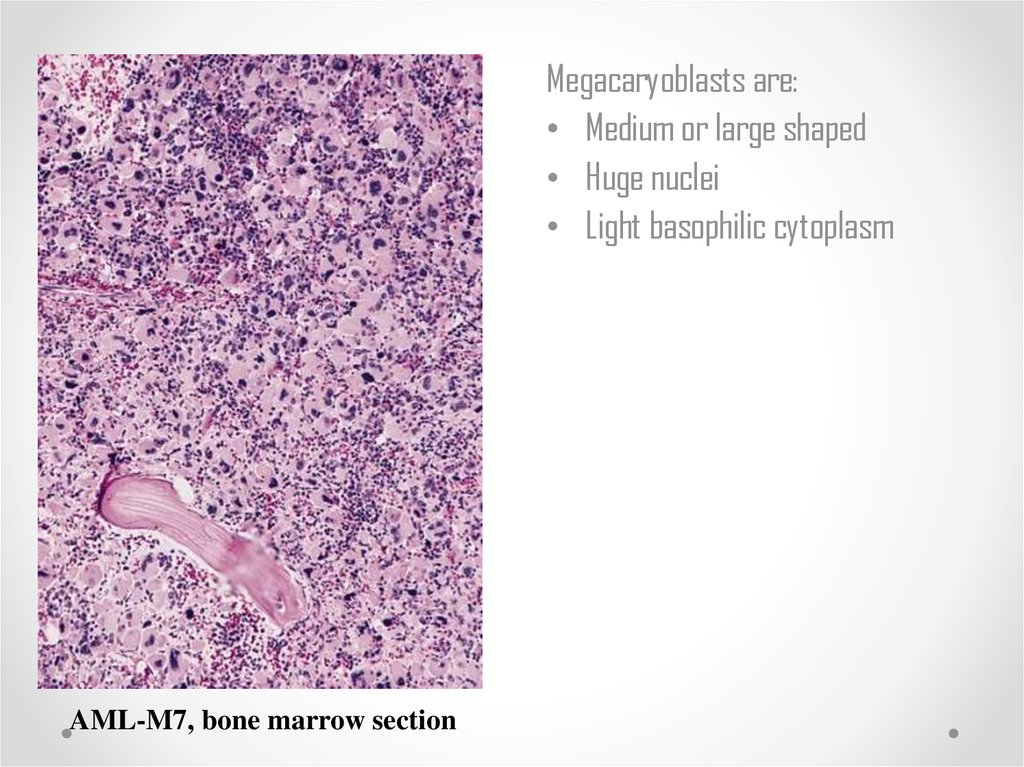
Megacaryoblasts are:• Medium or large shaped
• Huge nuclei
• Light basophilic cytoplasm
AML-M7, bone marrow section
37. Causes
• GATA-1 is a protein that in humans is encoded bythe GATA1 gene
• Risk group: Children with Down Syndrome
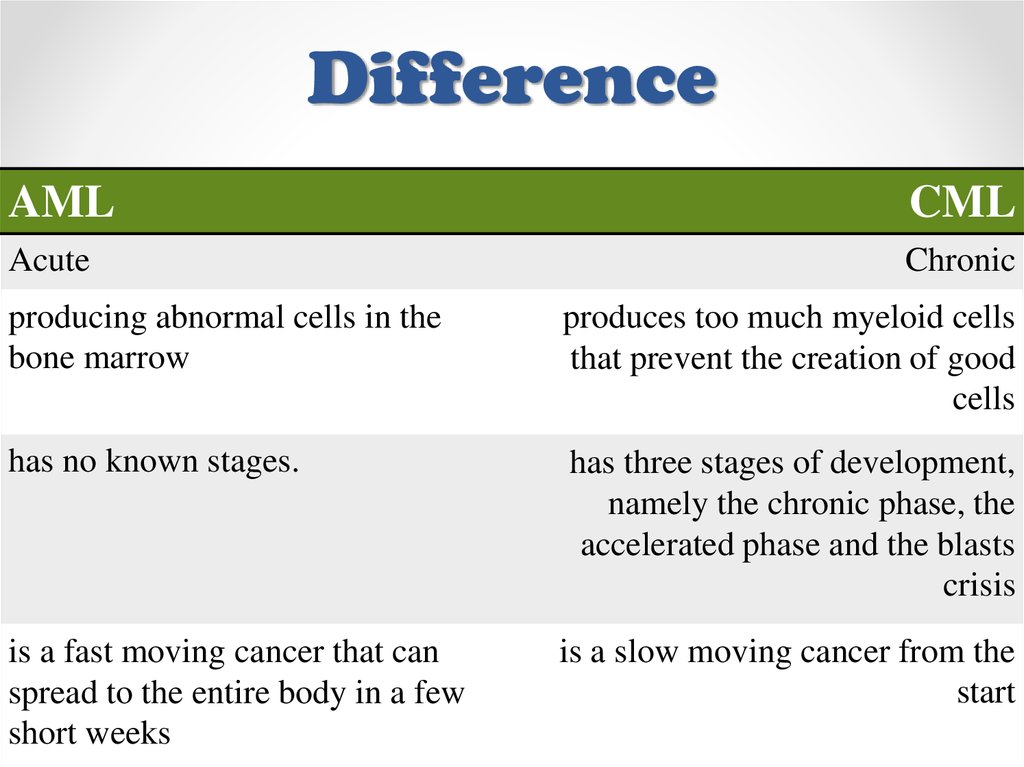
38. Difference
AMLCML
Acute
Chronic
producing abnormal cells in the
bone marrow
produces too much myeloid cells
that prevent the creation of good
cells
has no known stages.
has three stages of development,
namely the chronic phase, the
accelerated phase and the blasts
crisis
is a fast moving cancer that can
spread to the entire body in a few
short weeks
is a slow moving cancer from the
start
39. Conclusion
Classification is based on the type of cell from which theleukemia developed and its degree of maturity.
This is done by examining the appearance of the malignant
cells with light microscopy and/or by using cytogenetics to
characterize any underlying chromosomal abnormalities.
40. References
• http://www.pathpedia.com/education/eatlas/histopathology/blood_cells/aml-m1.aspx
• http://www.cancernetwork.com/oncologyjournal/managing-acute-myeloid-leukemia-elderly
• https://quizlet.com/17133006/hematology-myeloidlymphoid-leukemia-flash-cards/
• Textbook of Pathology © 2010, Harsh Mohan
• http://taml.uchicago.edu/background/understandingacute-myeloid-leukemia/










 Медицина
Медицина