Похожие презентации:
Immunophysiology of renal system
1. Immunophysiology of renal system
2.
3.
4.
5.
6.
7.
8.
9.
10.
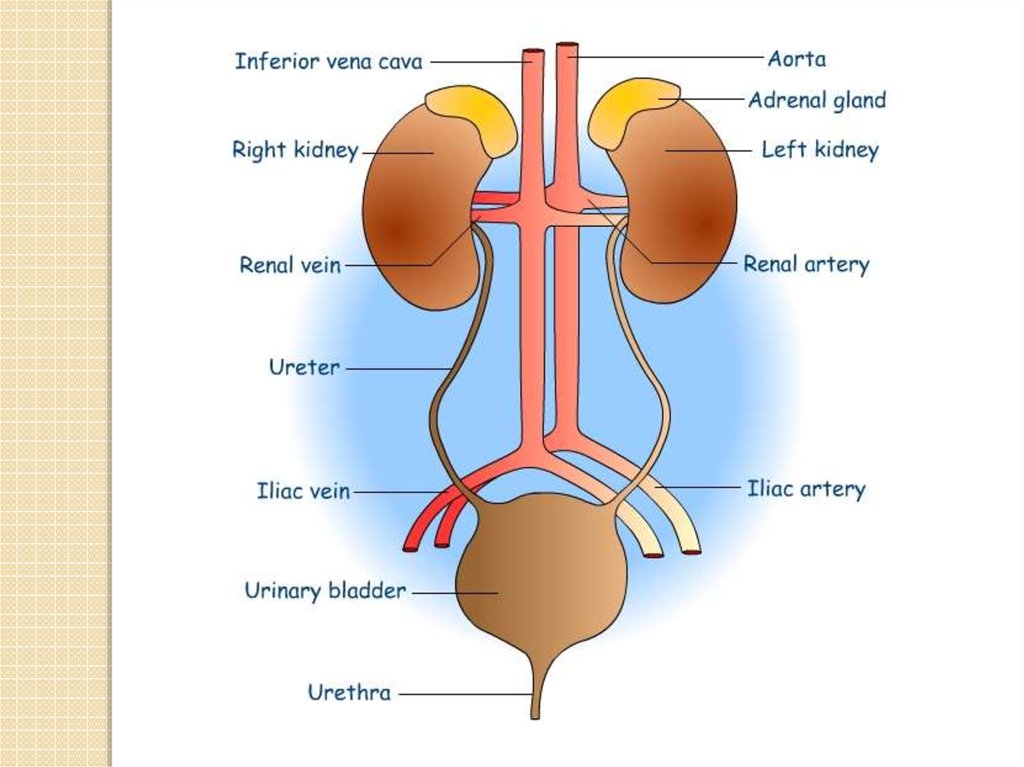
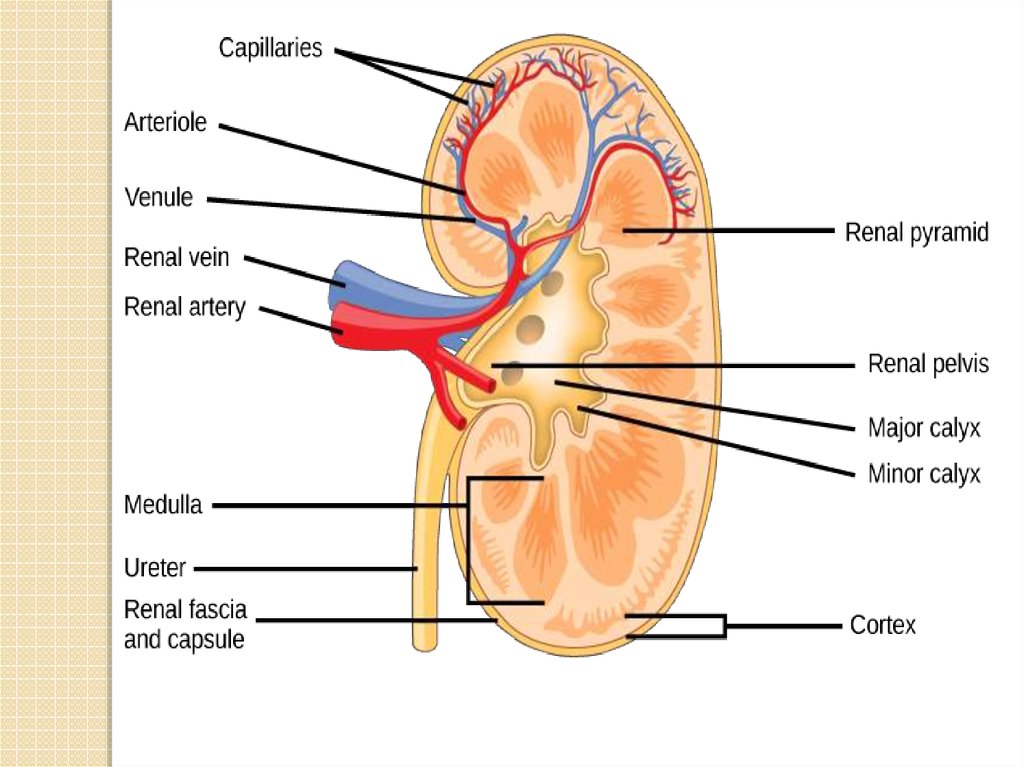
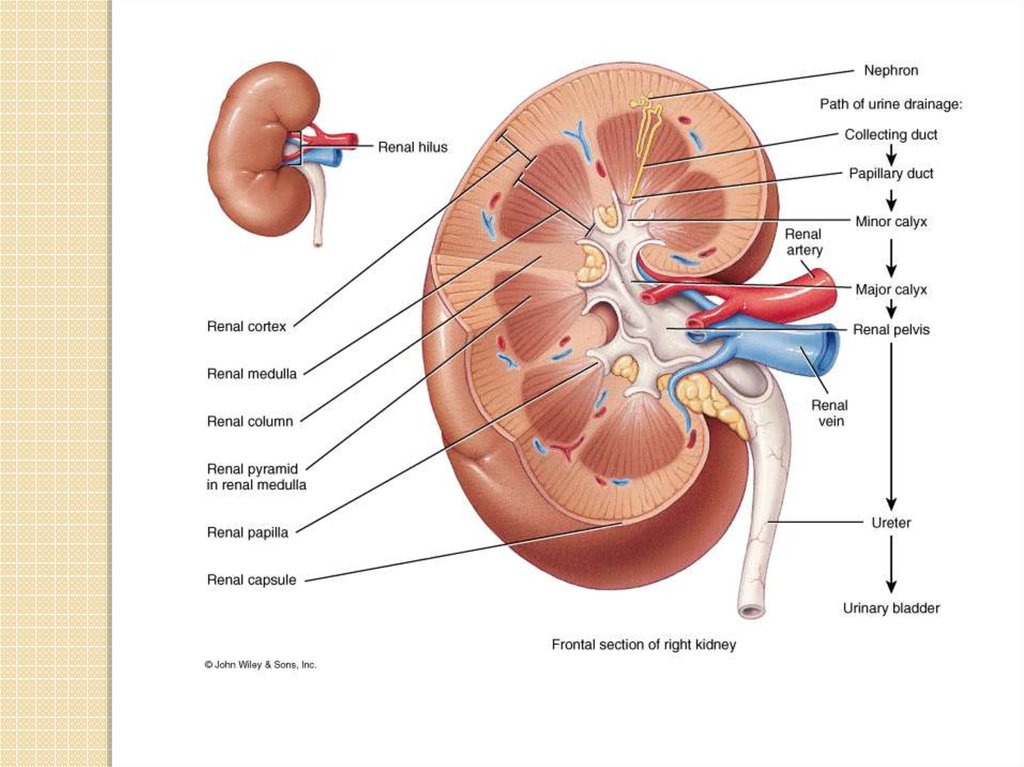
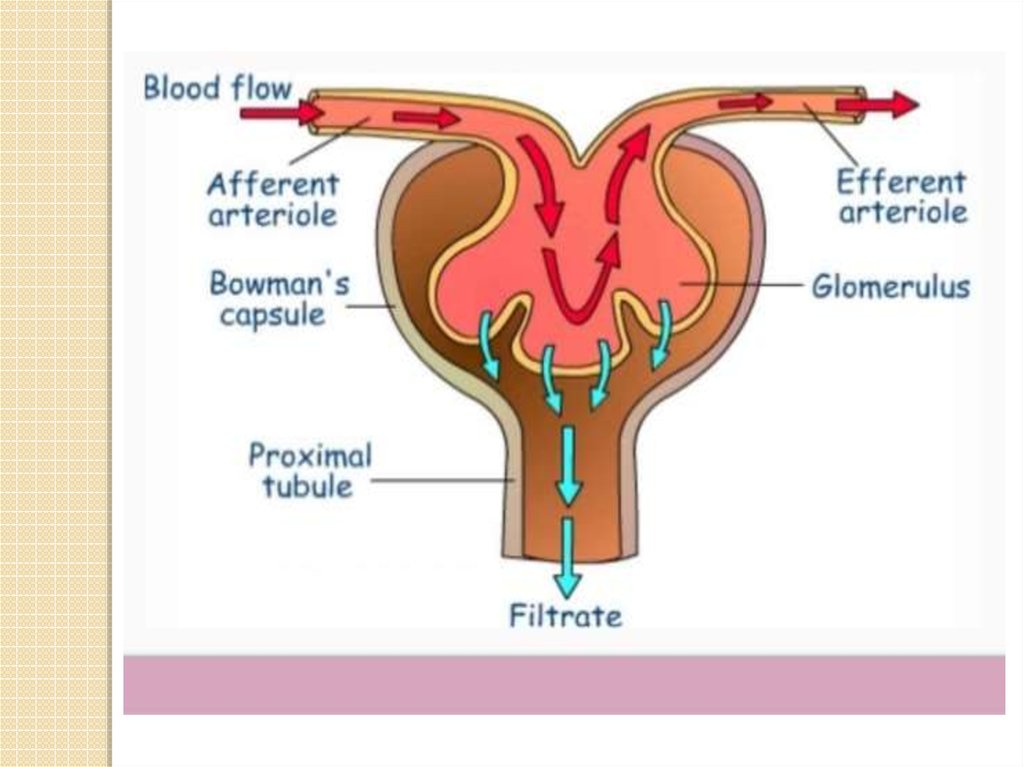
The kidneys purify toxic metabolic waste products from the blood in severalhundred thousand functionally independent units called nephrons.
A nephron consists of one glomerulus and one double hairpin-shaped tubule that
drains the filtrate into the renal pelvis. The glomeruli located in the kidney
cortex are bordered by the Bowman's capsule. They are lined with parietal
epithelial cells and contain the mesangium with many capillaries to filter the
blood. The glomerular filtration barrier consists of endothelial cells, the
glomerular basement membrane and visceral epithelial cells (also known as
podocytes). All molecules below the molecular size of albumin (that is, 68
kDa) pass the filter and enter the tubule, which consists of the proximal
convoluted tubule, the loop of Henle and the distal convoluted tubule. An
intricate countercurrent (противоточная) system forms a high osmotic
gradient in the renal medulla that concentrates the filtrate. The tubular
epithelial cells reabsorb water, small proteins, amino acids, carbohydrates
and electrolytes, thereby regulating plasma osmolality, extracellular volume,
blood pressure and acid–base and electrolyte balance. Non-reabsorbed
compounds pass from the tubular system into the collecting ducts to form
urine. The space between the tubules is called the interstitium and contains
most of the intrarenal immune system, which mainly consists of
dendritic cells, but also of macrophages and fibroblasts.
11.
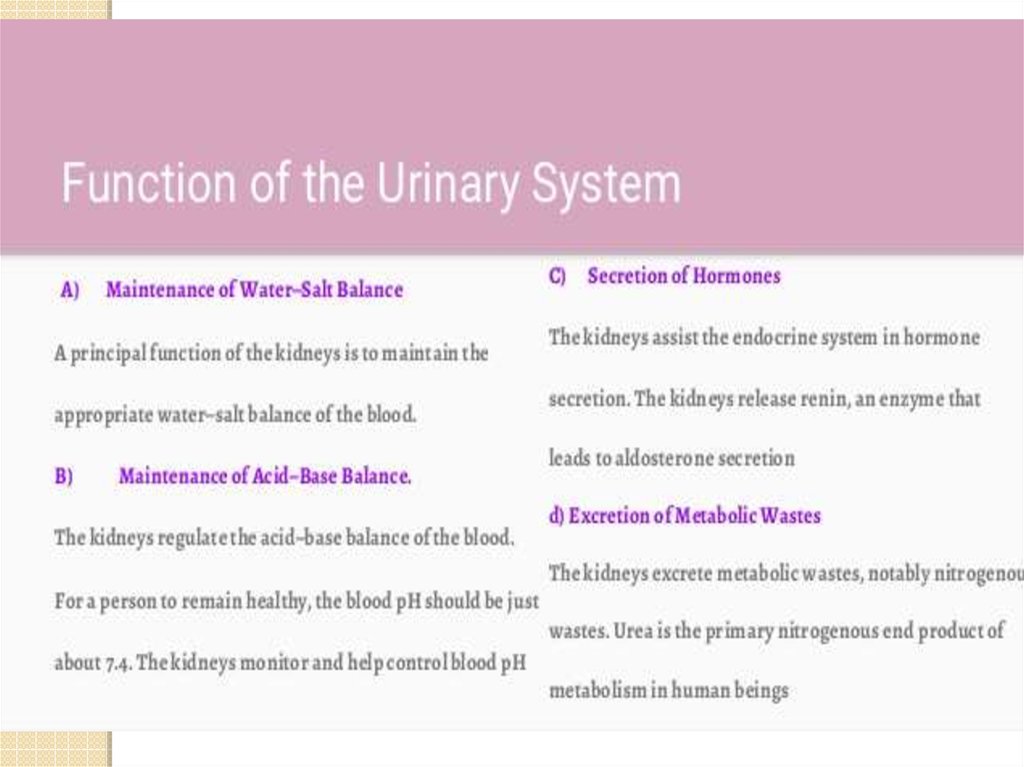
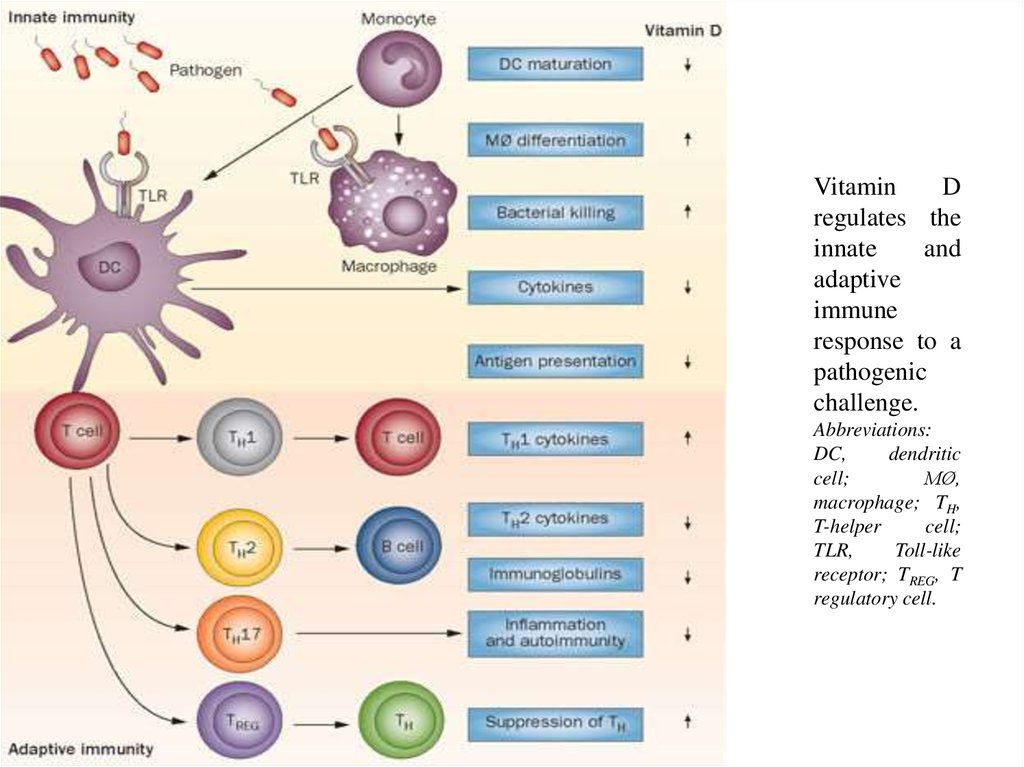
The kidneys produce several hormones thatdirectly or indirectly affect immune responses,
including vitamin D, which regulates bone
homeostasis
and
phagocyte
function,
erythropoietin, which is induced in response
to hypoxia to regulate erythropoiesis, and
renin, which induces angiotensin and
aldosterone to regulate electrolyte balance,
extracellular osmolarity and blood pressure.
12.
VitaminD
regulates the
innate
and
adaptive
immune
response to a
pathogenic
challenge.
Abbreviations:
DC,
dendritic
cell;
MØ,
macrophage; TH,
T-helper
cell;
TLR,
Toll-like
receptor; TREG, T
regulatory cell.
13.
14.
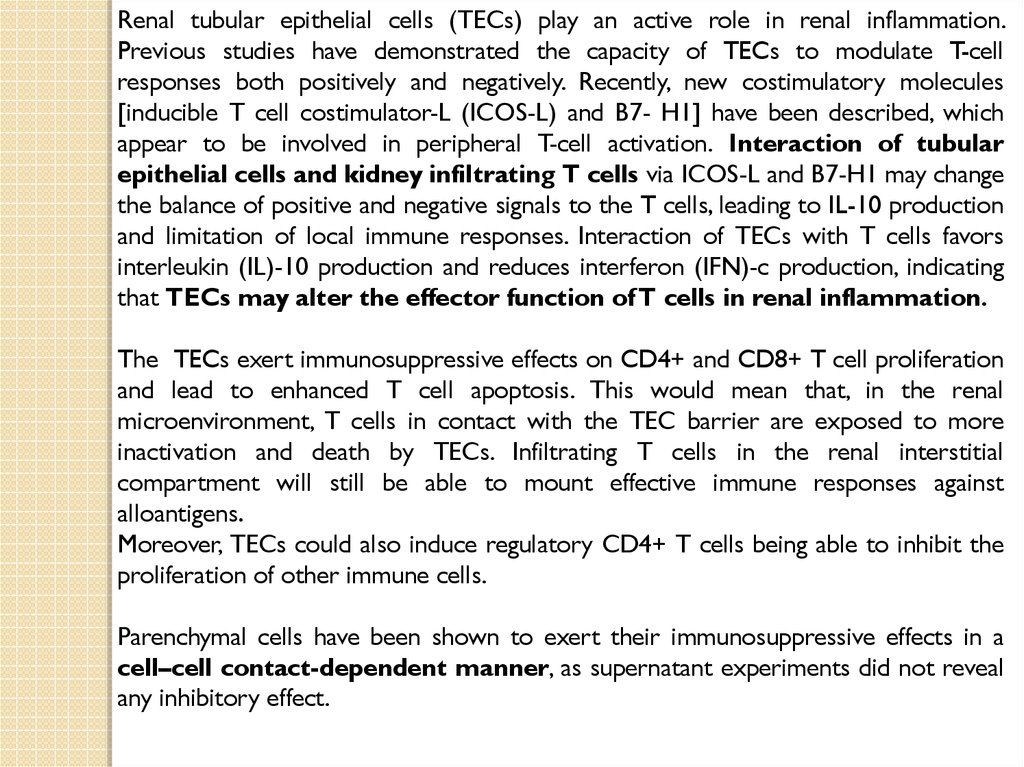
Renal tubular epithelial cells (TECs) play an active role in renal inflammation.Previous studies have demonstrated the capacity of TECs to modulate T-cell
responses both positively and negatively. Recently, new costimulatory molecules
[inducible T cell costimulator-L (ICOS-L) and B7- H1] have been described, which
appear to be involved in peripheral T-cell activation. Interaction of tubular
epithelial cells and kidney infiltrating T cells via ICOS-L and B7-H1 may change
the balance of positive and negative signals to the T cells, leading to IL-10 production
and limitation of local immune responses. Interaction of TECs with T cells favors
interleukin (IL)-10 production and reduces interferon (IFN)-c production, indicating
that TECs may alter the effector function of T cells in renal inflammation.
The TECs exert immunosuppressive effects on CD4+ and CD8+ T cell proliferation
and lead to enhanced T cell apoptosis. This would mean that, in the renal
microenvironment, T cells in contact with the TEC barrier are exposed to more
inactivation and death by TECs. Infiltrating T cells in the renal interstitial
compartment will still be able to mount effective immune responses against
alloantigens.
Moreover, TECs could also induce regulatory CD4+ T cells being able to inhibit the
proliferation of other immune cells.
Parenchymal cells have been shown to exert their immunosuppressive effects in a
cell–cell contact-dependent manner, as supernatant experiments did not reveal
any inhibitory effect.
15.
Proximal tubule epithelial cells (PTEC) of the kidney line the proximal tubuledownstream of the glomerulus and play a major role in the re-absorption of small
molecular weight proteins that may pass through the glomerular filtration process.
In the perturbed disease state PTEC also contribute to the inflammatory disease
process via both positive and negative mechanisms via the production of
inflammatory cytokines which chemo-attract leukocytes and the subsequent downmodulation of these cells to prevent uncontrolled inflammatory responses. It is well
established that dendritic cells are responsible for the initiation and direction of
adaptive immune responses. Both resident and infiltrating dendritic cells are
localised within the tubulointerstitium of the renal cortex, in close apposition to
PTEC, in inflammatory disease states. Primary human PTEC are able to
modulate autologous DC phenotype and function via multiple complex
pathways. The presence of autologous PTEC skew MoDC to become
phenotypically less mature and functionally less stimulatory.
16.
17.
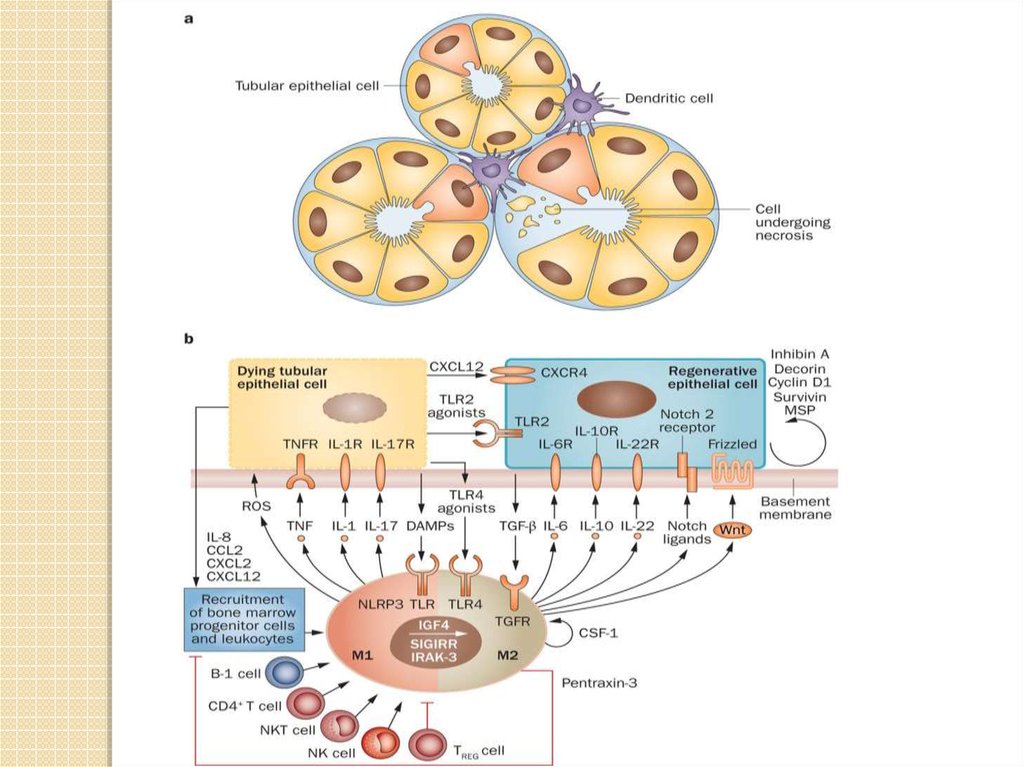
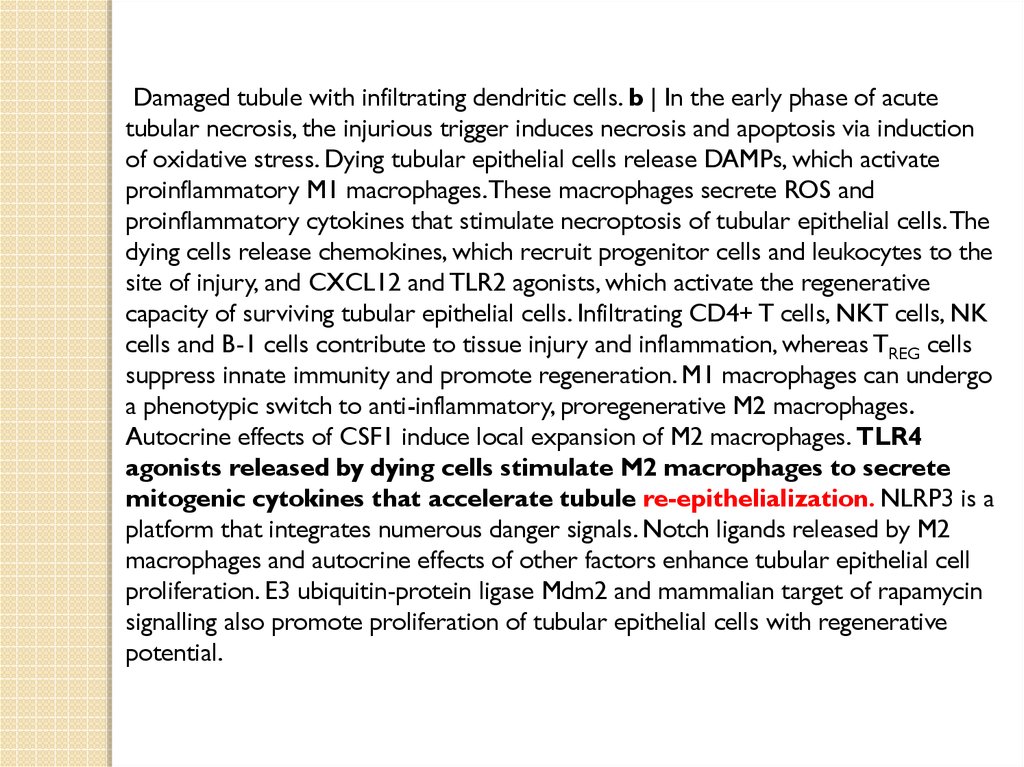
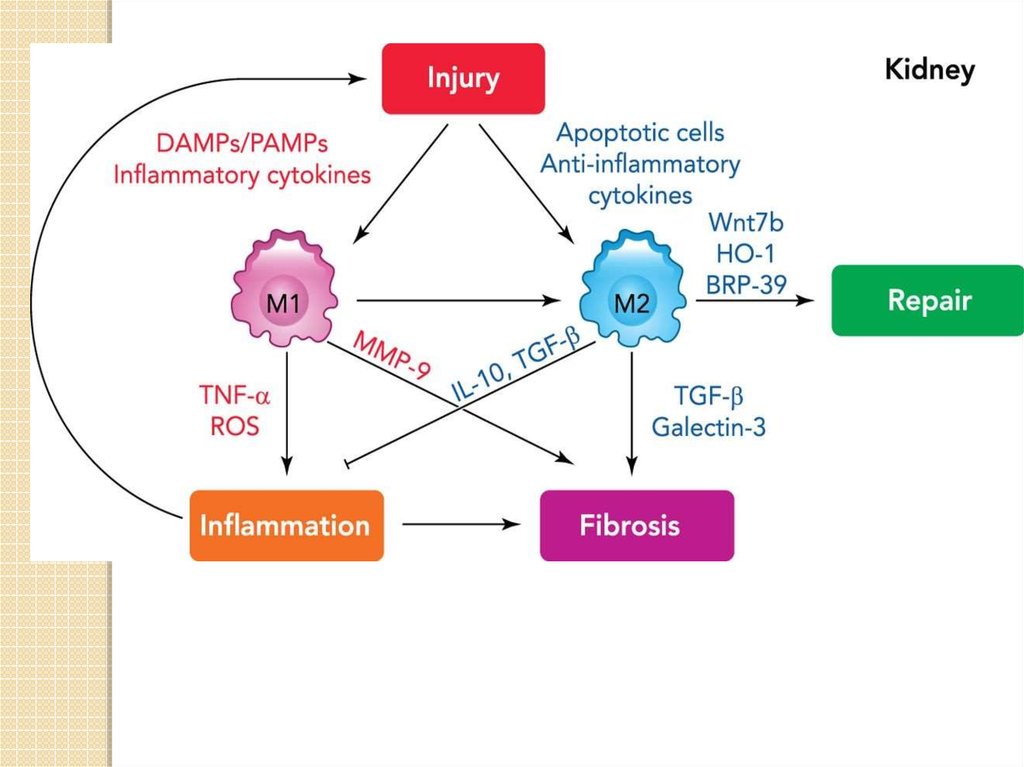
Damaged tubule with infiltrating dendritic cells. b | In the early phase of acutetubular necrosis, the injurious trigger induces necrosis and apoptosis via induction
of oxidative stress. Dying tubular epithelial cells release DAMPs, which activate
proinflammatory M1 macrophages. These macrophages secrete ROS and
proinflammatory cytokines that stimulate necroptosis of tubular epithelial cells. The
dying cells release chemokines, which recruit progenitor cells and leukocytes to the
site of injury, and CXCL12 and TLR2 agonists, which activate the regenerative
capacity of surviving tubular epithelial cells. Infiltrating CD4+ T cells, NKT cells, NK
cells and B-1 cells contribute to tissue injury and inflammation, whereas TREG cells
suppress innate immunity and promote regeneration. M1 macrophages can undergo
a phenotypic switch to anti-inflammatory, proregenerative M2 macrophages.
Autocrine effects of CSF1 induce local expansion of M2 macrophages. TLR4
agonists released by dying cells stimulate M2 macrophages to secrete
mitogenic cytokines that accelerate tubule re-epithelialization. NLRP3 is a
platform that integrates numerous danger signals. Notch ligands released by M2
macrophages and autocrine effects of other factors enhance tubular epithelial cell
proliferation. E3 ubiquitin-protein ligase Mdm2 and mammalian target of rapamycin
signalling also promote proliferation of tubular epithelial cells with regenerative
potential.
18.
19.
Resident renal mononuclear phagocytes (rMoPh)The ability of rMoPh to change functions over time may be an important general
property of the renal mononuclear phagocytic system. Classic examples of rMoPh
plasticity include the maturation of renal DCs to educate T lymphocytes and the
polarization of renal Mø to M1 or M2 functional phenotypes in response to
environmental cues. More recent studies show that bone marrow-derived Mø or
rMoPh display biphasic expression of proinflammatory factors followed by
anti-inflammatory and reparative factors in response to challenge with
lipopolysaccharide or ischemic injury, respectively.
20.
Apart from their role in the clearance of dying cells, fetal macrophages play atrophic role in promoting organ growth and nephrogenesis in the developing
kidney. During early mammalian development, primitive macrophages appear to
arise from a different cellular origin distinct from the blood monocyte. These
primitive fetal macrophages have a high proliferative capacity and are derived
from PU.1-negative hematopoietic cells (PU.1 is a tissue-specific transcription
factor that is expressed in cells of the hematopoietic lineage) that lack monocytic
cell surface markers. Once permanent or definitive hematopoiesis is established,
the proliferative capacity of the macrophage declines and a distinct set of
phagocytes, the monocyte-macrophages, are formed.
The kidney has a remarkable ability to regenerate following acute injury. Most
notably, the renal epithelia have the intrinsic capacity to rapidly self-duplicate.
Although the majority of regenerating tubular epithelial cells are derived from an
intrarenal source, macrophages cells may contribute to the replacement of tubular
epithelial cells through a process of cell fusion, as has been shown in the liver.
Macrophages demonstrate cell plasticity and have the ability to undergo cell-cell
fusion with themselves or other cell types, particularly in response to
inflammatory stimuli. Mature blood monocytes and inflammatory macrophages
have been shown to transform into vascular elements including endothelial
cells, myofibroblasts, and smooth muscle cells in addition to neuronal and
liver cells. It was discovered that cell fusion events occur between renal cells and
macrophages or their highly proliferative progenitors.
21.
Under homeostatic conditions, the resident immune cells of the kidneys includedendritic cells (DCs) and macrophages, as well as a few lymphocytes. DCs are
restricted to the tubulointerstitium and are absent from the glomeruli.
Macrophages are preferentially found in the renal medulla and capsule and have
homeostatic and repair functions.
The heterogeneous but overlapping phenotype and functions of renal DCs and
macrophages.
DCs are traditionally described as mediators of immune surveillance and antigen
presentation, and as the primary determinants of responses to antigens—through
initiation of either immune effector-cell functions or the development of tolerance.
Macrophages also function as innate immune cells, predominantly through
phagocytosis and production of toxic metabolites. However, the classical paradigm of
DC versus macrophage phenotypes and functions is increasingly indistinct
within the kidney, as these cells exhibit overlapping surface markers,
functional capabilities, and ontogenic pathways. This molecular and
phenotypic overlap between cell types and subsets complicates their identification
and evaluation.
Renal DCs and macrophages are phenotypically and functionally heterogeneous cells
that regulate tissue responses to renal injury and disease. The considerable overlap
between DCs and macrophages represents a continuum of phenotype, as well as
plasticity of cells of the myeloid–monocytic lineage both in vivo and in vitro.
22.
23.
Resident renal mononuclear phagocytes (rMoPh)At steady state, subsets of rMoPh exist that coexpress markers
previously thought to segregate Mø and DCs. These cells exhibit
functional properties considered typical of both DCs and Mø.
The renal mononuclear phagocytic system performs important
homeostatic and sentinel functions in the steady-state kidney and
maintains immune tolerance against self- and innocuous
(безопасный) antigens.
The renal mononuclear phagocytic system changes dramatically
during injury to the kidney, with resident and recruited rMoPh
exhibiting functional heterogeneity and plasticity in defense
against microbes, mediation of parenchymal injury, and promotion
of tissue repair.
24.
Møclassic functions
phagocytosis of tissue debris and pathogens
mediation of tissue injury and disease progression
activated phenotypes exhibit distinct polarized functionsa
contemporary additions
phagocytosis to remodel matrix
support for nephrogenesis and cell fate decisions
paracrine role in angiogenesis and epithelial regeneration
polarized function can be fibrogenic
potent source of chemokines and cytokinesa
mediate anti-inflammatory/immunosuppressive effects through innate responsesa
DCs
classic functions
phagocytosis of antigen in kidney
migration to renal lymph nodes
antigen presentation to T lymphocytes
contemporary additions
antigen presentation within the kidney to restimulate or modify infiltrating T lymphocytes
mediate anti-inflammatory/immunosuppressive effects through innate responses and modulation of
T lymphocytes (peripheral tolerance)a
activated phenotypes exhibit distinct polarized functionsa
potent source of chemokines and cytokinesa
25.
‘Summary at a glance’: functions of DCs1. Renal dendritic cells (rDCs) have homeostatic roles, such as
inducing immune tolerance against small innocuous antigens or crosstalk with tubular epithelial cells.
2. rDCs form an extensive surveillance network in the kidney
tubulointerstitium, alerting to infections/injury.
3. rDCs may exacerbate acute non-immune kidney injury (e.g., ischemia
reperfusion injury (IRI) or unilateral ureter obstruction (UUO)) by
inducing harmful immune effector mechanisms.
4. rDCs have protective anti-inflammatory roles in acute GN, but may
acquire injurious pro-inflammatory properties in chronic renal
inflammation.
26.
major challenges facing the field in the near future1. Current definitions of renal dendritic cells (rDCs) and macrophages overlap. Reach
consensus on phenotype, functionality, and terminology.
2. Role of rDCs in homeostasis, in particular cross-talk with intrinsic kidney cells like
tubular epithelial cells, needs to be clarified.
3. Role of rDCs in many diseases is unclear, such as pauci-immune GN and
immunoglobulin A (IgA) nephritis, but also in prevalent non-immune-mediated
diseases like diabetic or hypertensive kidney disease.
4. Define the molecular mechanisms causing rDC maturation and acquisition of proinflammatory phenotype, in order to allow the development of selective therapeutic
strategies.
5. Align murine and human dendritic cell (DC) terminology, so that information on DC
functions from experimental models can be extrapolated to kidney biopsy findings.
27.
Significant progress in understanding the renal mononuclearphagocytic system has been achieved over the past three
decades. Many typical DC and Mø-associated functions of
the major rMoPh subsets have been described, especially in
the last 5 years. However, rMoPh may fulfill definitions
and functions both of DCs and Mø, hampering definitive
classification. Indeed, parallel streams of literature have
been created that do not provide a fully integrated body of
knowledge to this point.
28.
Immune cells involved in renal tolerant recipients (DC, dendritic cells; NK, naturalkiller cells; MDSC, myeloid-derived suppressor cells).















 Медицина
Медицина