Похожие презентации:
Plague. Causative agent
1.
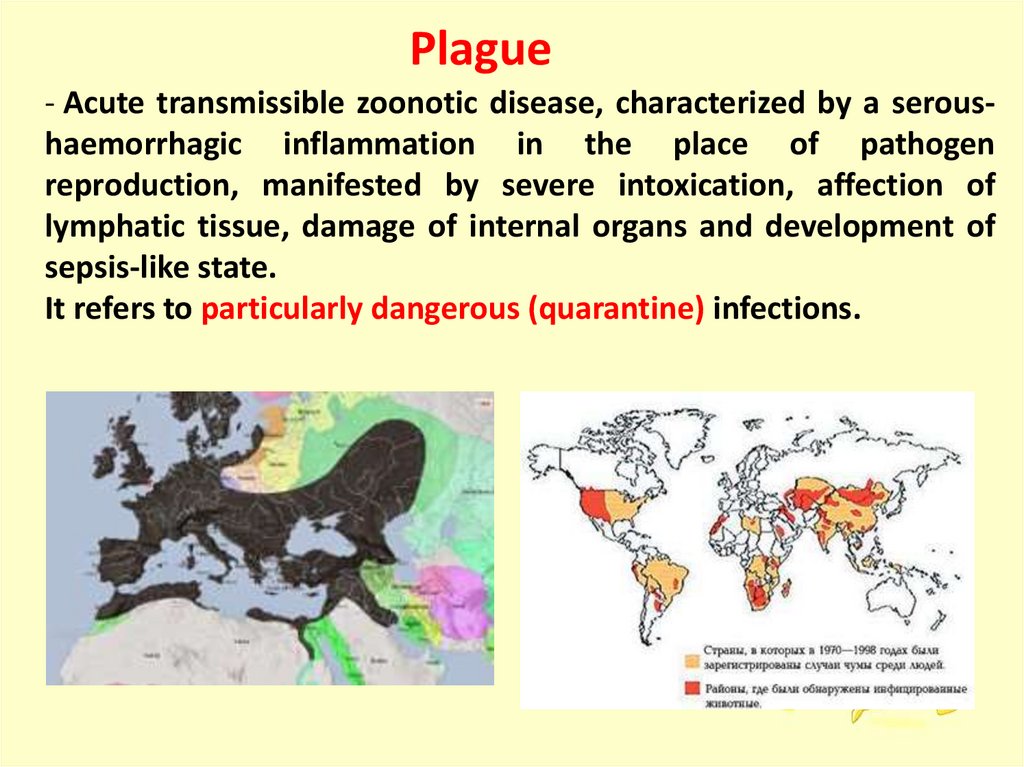
Plague- Acute transmissible zoonotic disease, characterized by a seroushaemorrhagic inflammation in the place of pathogen
reproduction, manifested by severe intoxication, affection of
lymphatic tissue, damage of internal organs and development of
sepsis-like state.
It refers to particularly dangerous (quarantine) infections.
2.
Causative agent :1.
2.
3.
4.
5.
6.
7.
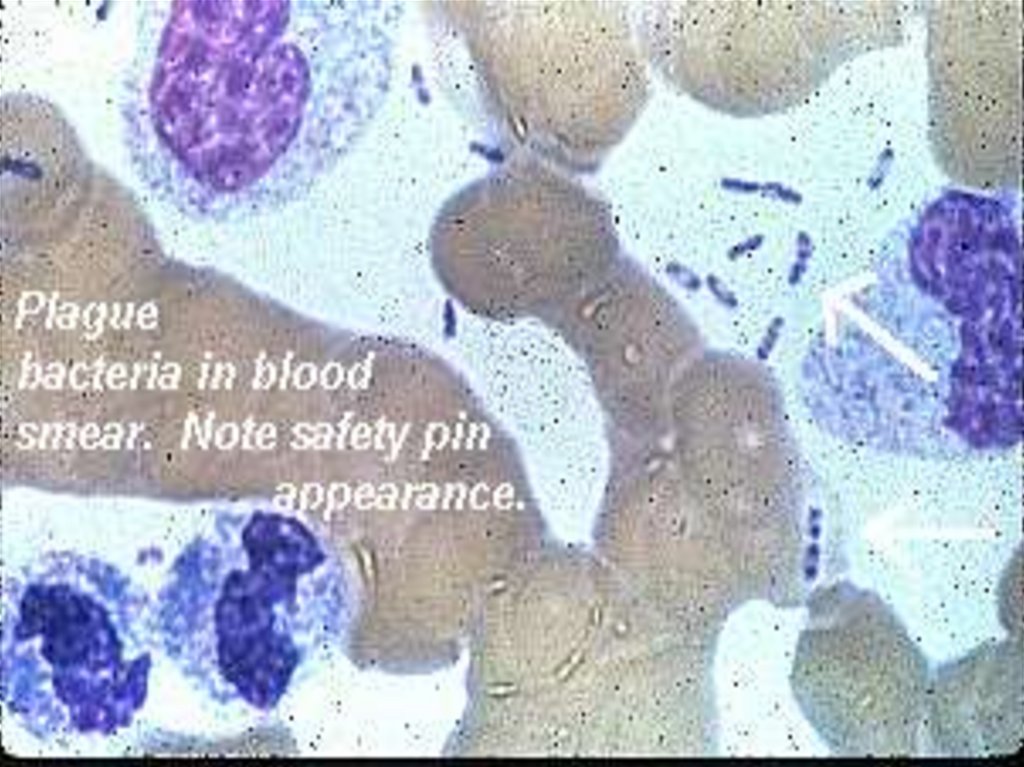
Yersinia pestis – genus - Yersinia, family Enterobacteria
Nonmotile, ovoid shaped with rounded ends;
No spores, no flagella, has a delicate capsule;
Gram – negative;
Obligate intracellular parasite;
Facultative anaerobe;
Grows slowly at T-37 ͦC
on the simple nutrient mediums;
8. Sensitivity: to heating, boiling, disinfection, antibiotics
(streptomycin, tetracycline, chloramphenicol);
9. Resistancy: drying, freezing,
low temperature
3.
4.
Causative agent :10. Has a thermostable O-Ag, K-Ag (capsule),
V-Ag, W-Ag (protection from phagocytosis);
11. Produces exotoxin, factors of aggression:
- coagulase,
- hyaluronidase,
- hemolysin,
- fibrinolysin
promote pathogen dissemination,
increased vessel permeability,
thromboformation and disorde of
hemocirculation
12. Endotoxin liberating at distraction has tropicity to the
vascular endothelium and blood cells;
5.
6.
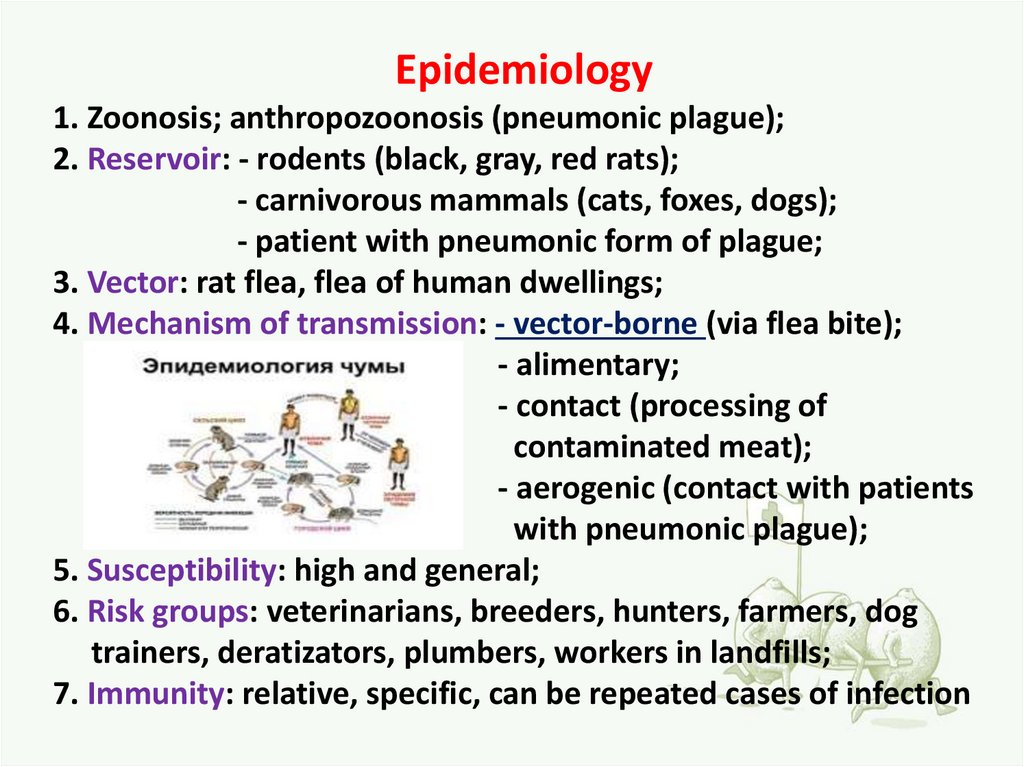
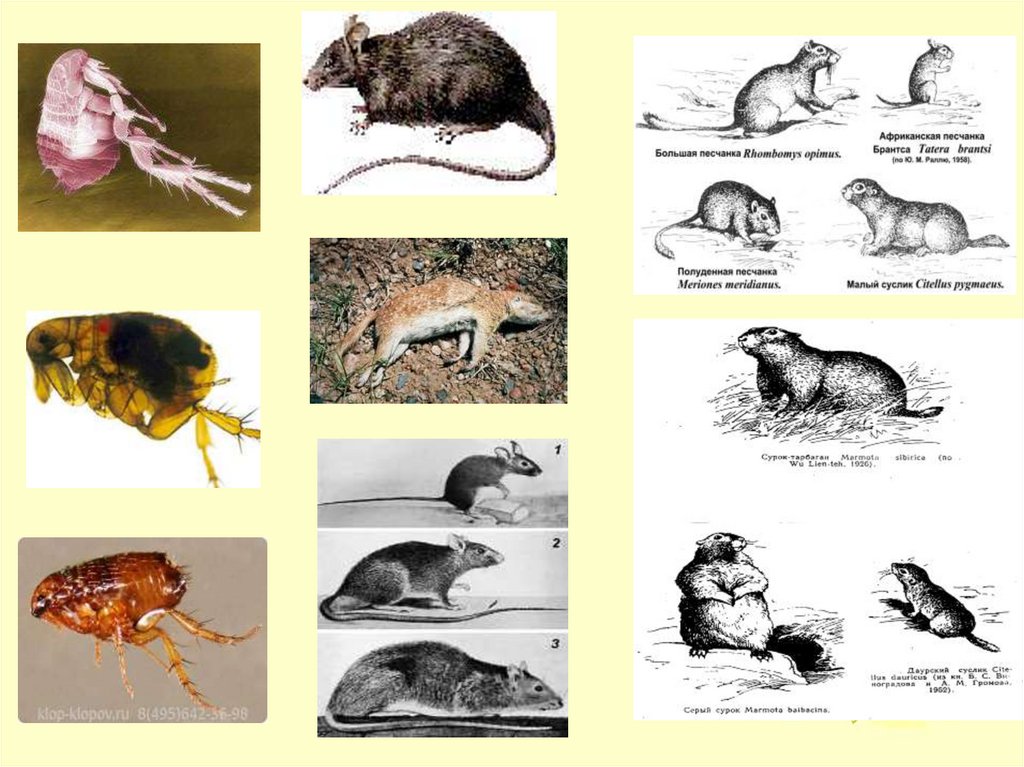
Epidemiology1. Zoonosis; anthropozoonosis (pneumonic plague);
2. Reservoir: - rodents (black, gray, red rats);
- carnivorous mammals (cats, foxes, dogs);
- patient with pneumonic form of plague;
3. Vector: rat flea, flea of human dwellings;
4. Mechanism of transmission: - vector-borne (via flea bite);
- alimentary;
- contact (processing of
contaminated meat);
- aerogenic (contact with patients
with pneumonic plague);
5. Susceptibility: high and general;
6. Risk groups: veterinarians, breeders, hunters, farmers, dog
trainers, deratizators, plumbers, workers in landfills;
7. Immunity: relative, specific, can be repeated cases of infection
7.
8.
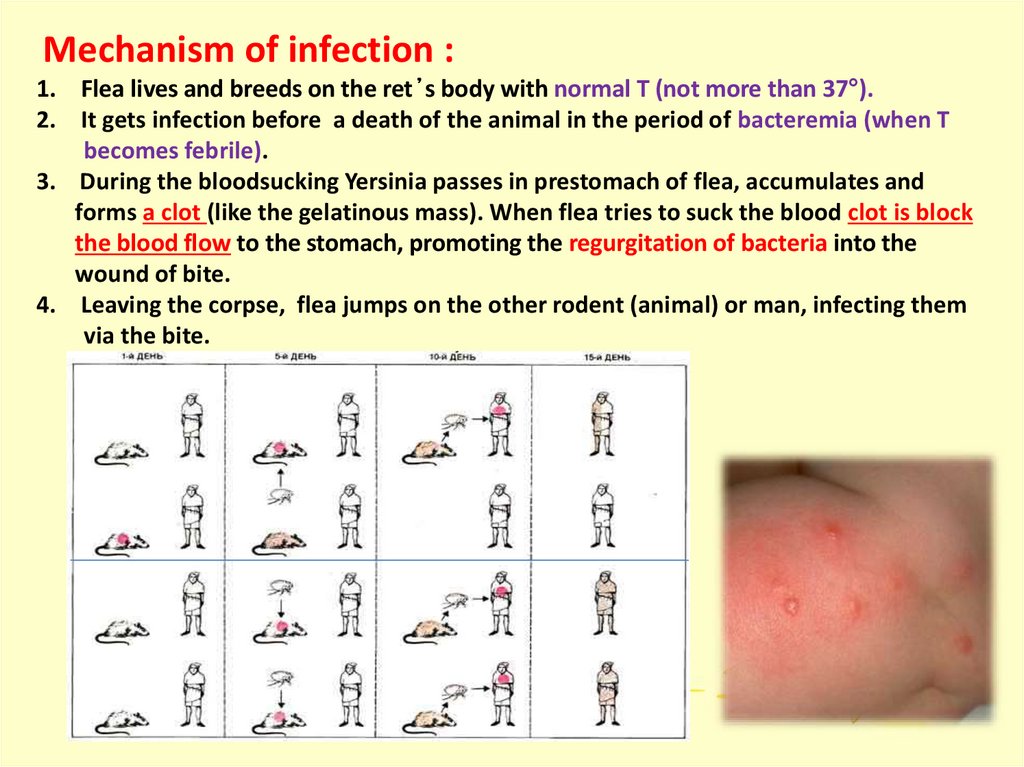
Mechanism of infection :1. Flea lives and breeds on the ret ̓s body with normal T (not more than 37°).
2. It gets infection before a death of the animal in the period of bacteremia (when Т
becomes febrile).
3. During the bloodsucking Yersinia passes in prestomach of flea, accumulates and
forms a clot (like the gelatinous mass). When flea tries to suck the blood clot is block
the blood flow to the stomach, promoting the regurgitation of bacteria into the
wound of bite.
4. Leaving the corpse, flea jumps on the other rodent (animal) or man, infecting them
via the bite.
9.
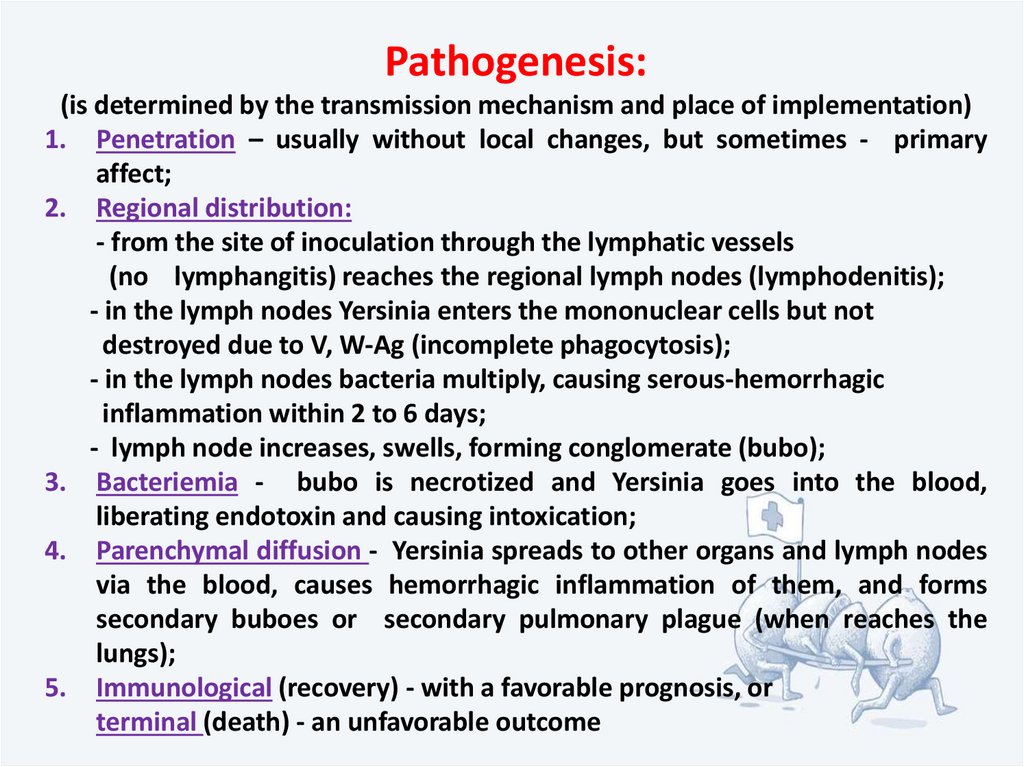
Pathogenesis:(is determined by the transmission mechanism and place of implementation)
1. Penetration – usually without local changes, but sometimes - primary
affect;
2. Regional distribution:
- from the site of inoculation through the lymphatic vessels
(no lymphangitis) reaches the regional lymph nodes (lymphodenitis);
- in the lymph nodes Yersinia enters the mononuclear cells but not
destroyed due to V, W-Ag (incomplete phagocytosis);
- in the lymph nodes bacteria multiply, causing serous-hemorrhagic
inflammation within 2 to 6 days;
- lymph node increases, swells, forming conglomerate (bubo);
3. Bacteriemia - bubo is necrotized and Yersinia goes into the blood,
liberating endotoxin and causing intoxication;
4. Parenchymal diffusion - Yersinia spreads to other organs and lymph nodes
via the blood, causes hemorrhagic inflammation of them, and forms
secondary buboes or secondary pulmonary plague (when reaches the
lungs);
5. Immunological (recovery) - with a favorable prognosis, or
terminal (death) - an unfavorable outcome
10.
1.Penetration – usually without local changes, but sometimes - primary affect;
2. Regional distribution:
No lymphangitis !
-
from the site of inoculation
through the lymphatic vessels
(no
the
lymphangitis) reaches
regional
(lymphadenitis);
- in the lymph nodes Yersinia enters the mononuclear cells but
not destroyed due to V, W,-Ag (incomplete phagocytosis);
- in the lymph nodes, the bacteria multiply, causing serous
hemorrhagic inflammation within 2 to 6 days;
- lymph node increases, swells, forming conglomerate (bubo);
lymph
nodes
11.
Clinical classification1) Localized: - cutaneous;
- bubonic (70 – 80%);
- cutaneous-bubonic;
2) Pneumonic (5 – 10%): - primary;
- secondary;
3) Septicemic (15 – 20%): - primary;
- secondary;
4) Plague meningitis;
5) Other forms (abortive);
6) Unverificated plague;
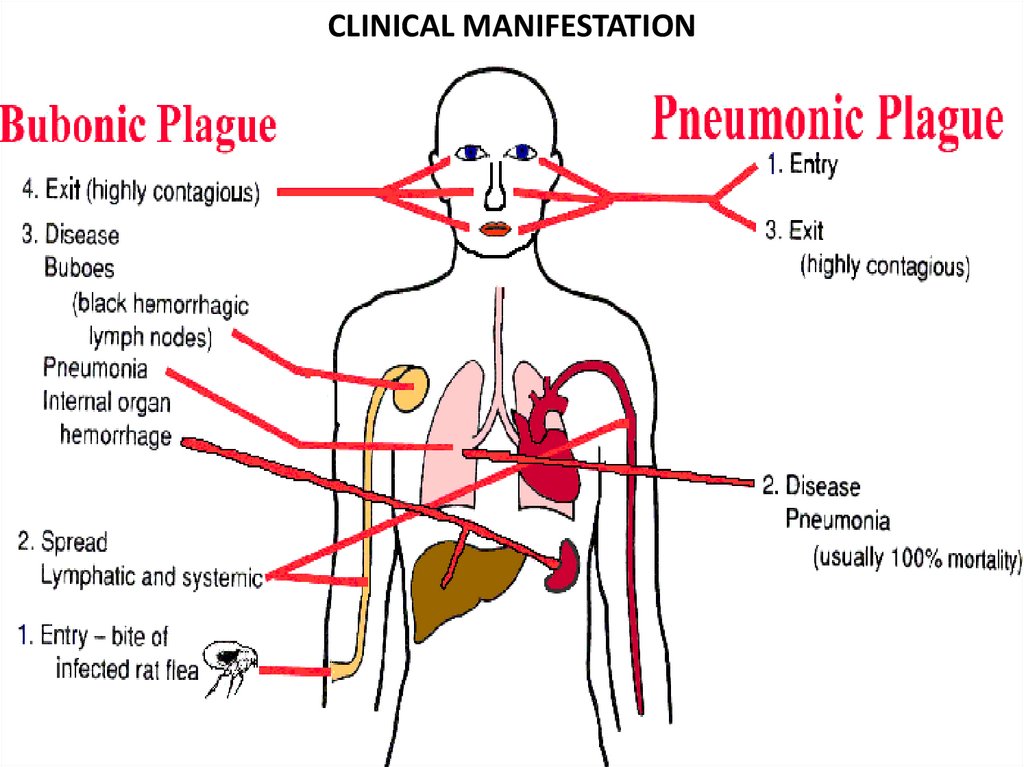
12. CLINICAL MANIFESTATION
13.
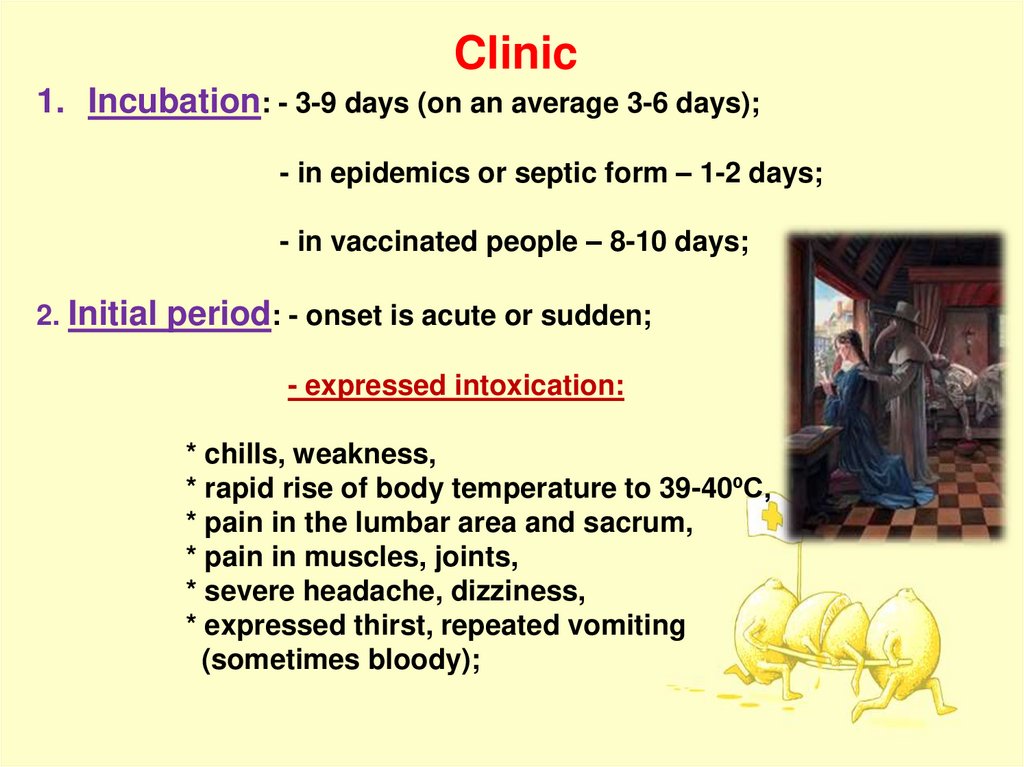
Clinic1. Incubation: - 3-9 days (on an average 3-6 days);
- in epidemics or septic form – 1-2 days;
- in vaccinated people – 8-10 days;
2. Initial period: - onset is acute or sudden;
- expressed intoxication:
* chills, weakness,
* rapid rise of body temperature to 39-40ºC,
* pain in the lumbar area and sacrum,
* pain in muscles, joints,
* severe headache, dizziness,
* expressed thirst, repeated vomiting
(sometimes bloody);
14.
- psychomotor agitation:* the patient is restless, overly active,
* delirium, hallucinations (1-st day of the disease),
* disorded gait, coordination, disturbed speech,
* tremor of tongue
- hood-symptom:
* hyperemic, edematous face, neck and shoulders,
* injected sclera, on the face – expression of suffering “facies pestica”;
- catarrhal syndrome:
* thickened coated tongue with white fir (chalk-like);
* can be enlarged tonsils, covered with white pseudomembranes,
* hemorrhagic enanthema on the soft palate (sometimes);
- cardiovascular syndrome:
* severe tachycardia, arrhythmia,
* hypotension,
* dull heart sounds, increased heart sizes;
- tachypnea, dyspnea;
- hepatosplenomegaly;
- oliguria;
15.
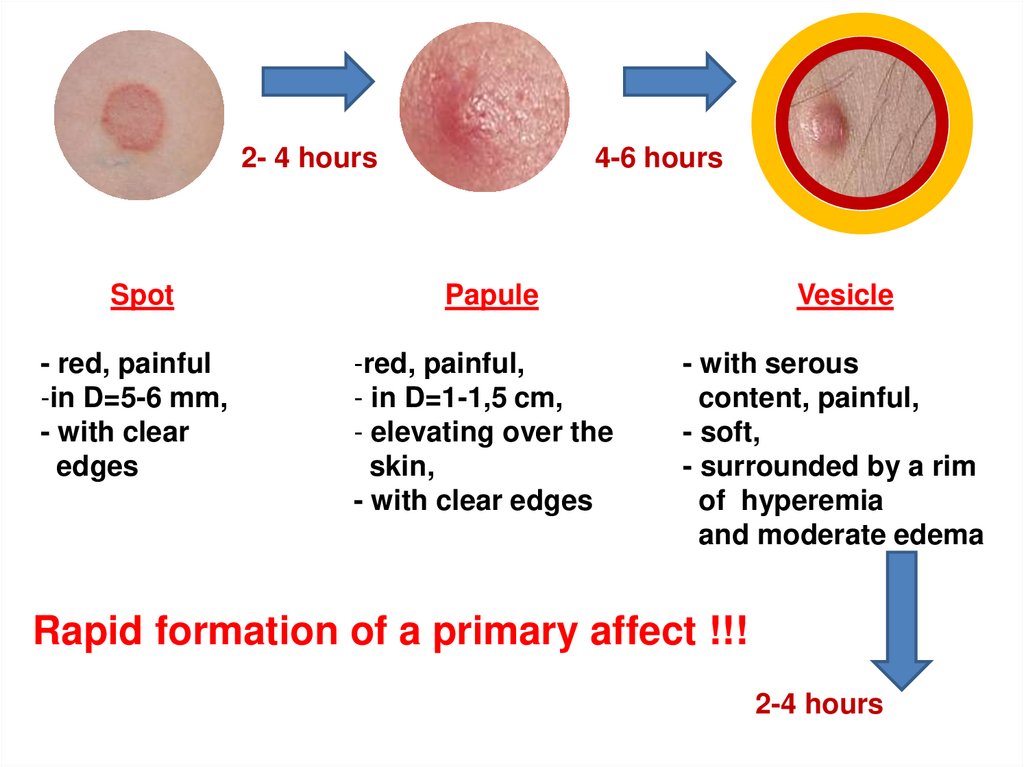
3. Climax period: clinic depends on routs of transmissionCutaneous form (3-4%)
(with formation of primary affect – ulcer in place of penetration)
Local lesions:
1.
2.
3.
4.
5.
6.
Spot;
Papule;
Vesicle;
Pustule;
Ulcer;
Scar
General changes:
1. Regional lymphadenitis – bubo-formation;
2. Intoxication
16.
2- 4 hours4-6 hours
Spot
Papule
- red, painful
-in D=5-6 mm,
- with clear
edges
-red, painful,
- in D=1-1,5 cm,
- elevating over the
skin,
- with clear edges
Vesicle
- with serous
content, painful,
- soft,
- surrounded by a rim
of hyperemia
and moderate edema
Rapid formation of a primary affect !!!
2-4 hours
17.
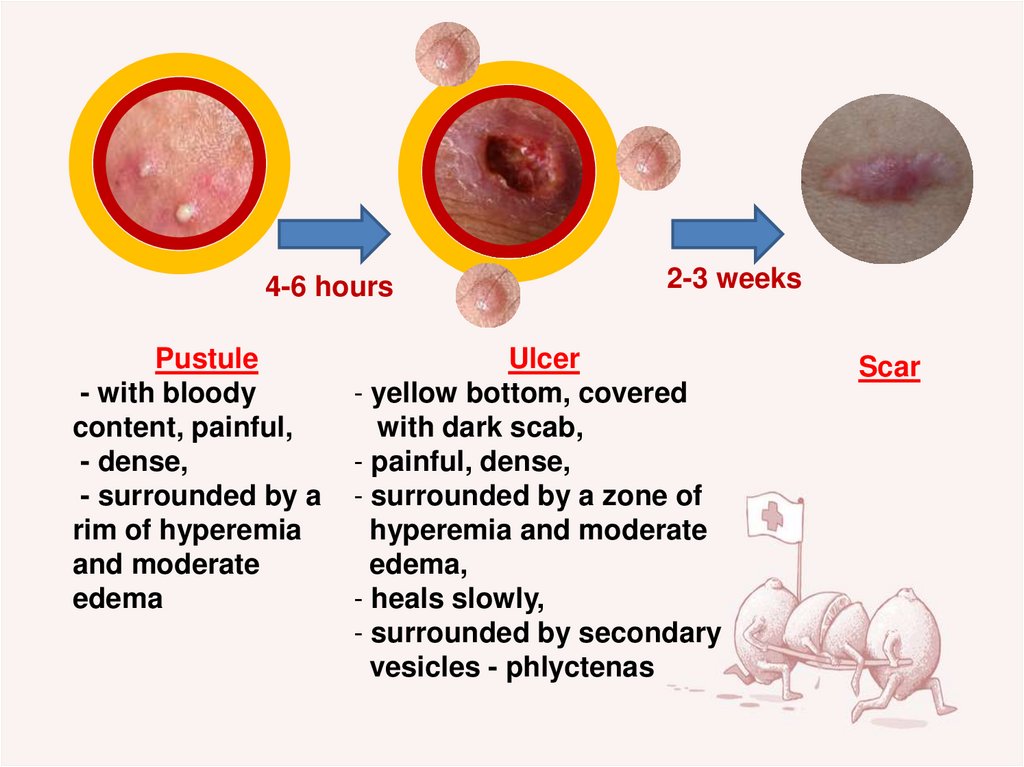
4-6 hoursPustule
- with bloody
content, painful,
- dense,
- surrounded by a
rim of hyperemia
and moderate
edema
2-3 weeks
Ulcer
- yellow bottom, covered
with dark scab,
- painful, dense,
- surrounded by a zone of
hyperemia and moderate
edema,
- heals slowly,
- surrounded by secondary
vesicles - phlyctenas
Scar
18.
19.
Bubonic form (80%)Bubo – is a conglomerate, tumor-like formation,
consisting of a single (but m. b. several) inflamed lymph
node in diameter more then 2 cm.
1. Plague bubo is often single (in 95%), D = 1 - 10 cm;
2. Localization:
- inguinal region – 60-70%,
- axillary region – 15-20%,
(more dangerous due to development
of secondary pneumonia),
- cervical area – 5%
(dangerous due to the proximity to the brain);
3. On the periphery of bubo may be secondary
elements with hemorrhagic content and Yersinia
- plague phlyctenas;
20.
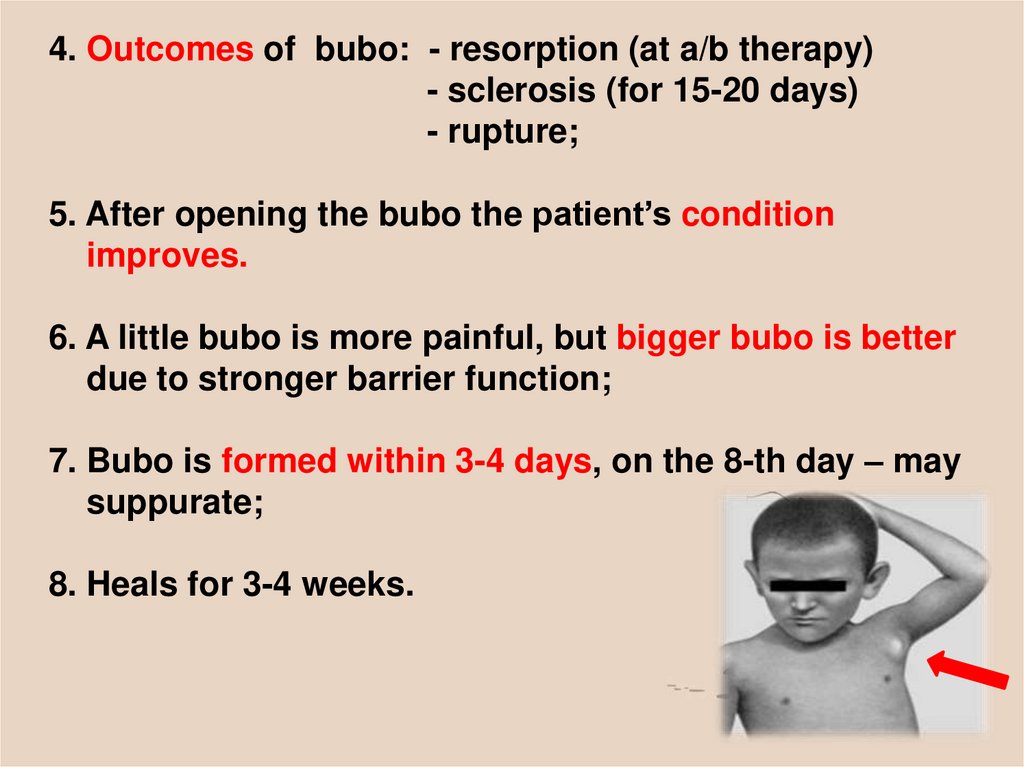
4. Outcomes of bubo: - resorption (at a/b therapy)- sclerosis (for 15-20 days)
- rupture;
5. After opening the bubo the patient’s condition
improves.
6. A little bubo is more painful, but bigger bubo is better
due to stronger barrier function;
7. Bubo is formed within 3-4 days, on the 8-th day – may
suppurate;
8. Heals for 3-4 weeks.
21.
Local lesions:1. Primary bubo – is developed in the phase of primary regional infection,
when regional lymph nodes are involved;
1) dense, sharply painful,
2) immobile,
3) connected with surrounding tissues (periadenitis),
4) has fuzzy edges,
5) skin over the bubo is hot, tense, painful, hyperemic
with cyanotic shade,
6) in the center of bubo - fluctuation, peripheraly – edema,
7) no lymphangitis;
2. Secondary bubo - is developed in the phase of dissemination, can be
involved lymph nodes of different remote localization;
1) dense, painful,
2) mobile,
3) nonconnected with surrounding tissues (no periadenitis),
4) has clear edges,
5) skin over the bubo is hot, tense, painful, hyperemic,
6) no lymphangitis,
7) size is smaller
22.
Intoxication:1.
2.
3.
4.
5.
6.
7.
8.
Develops within 1-3 days,
Increased body temperature (39-40ºC),
Headache and chills,
Nausea, vomiting, abdominal pain, diarrhea,
anorexia,
Tachycardia, tachypnea, hypotension,
Whitish tongue,
Redness and swelling of the face,
Pain at movements;
CBC: leukocytosis, shift of formula to the left,
increased ESR.
Without treatment patient dies within 3-5 days
(40-90%)
23.
24.
Septicemic formPrimary septicemic form: (1-3%)
1. Lasts 1-3 days;
2. Short incubation (4-6 hours – 1-2 days);
3. Acute or sudden onset;
4. Chills, fast rising of Тº (40-41ºC);
5. General weakness, myalgia, arthralgia, headache;
6. Nausea, vomiting (bloody);
7. Agitation, confusion, delirium, disarthria;
8. Impaired consciousness (stupor – coma);
9. FE: total cyanosis, edema of the face;
10. Cardio-vascular syndrome: tachycardia, hypotension, muffled
heart sounds, tachypnea;
11. Hepatosplenomegaly;
12. Oligo-, anuria;
13. CBC: leukocytosis, shift to the left, increased ESR;
Prognosis for untreated patient – death within 48 hours.
25.
May be in some variants:- meningo-encephalitic (meningeal sighs, focal pathological reflexes)
- hemorrhagic syndrome: epistaxis, hematemesis and bloody
diarrhea, hematuria, bleeding at the injection sites
- infectious-toxic shock
- cardiovascular failure
Secondary septicemic plague:
1. Develops as a complication of other forms;
2. Has more severe clinical manifestation;
3. Hemorrhagic syndrome, secondary lesions and
buboes dominate in the clinic;
4. Patient dies in the first hours or days of illness;
5. Diagnosis to be confirmed retrospectively.
26.
Pneumonic plaguePrimary pneumonic plague:
1. Fulminant, the most dangerous;
2. Incubation – 1-2 days;
3. Initial period: - duration 1-2 days,
- sudden onset,
- rise body- ТºC,
- chills, vomiting,
- severe headache,
Intoxication syndrome
- cutting pains in the chest,
- shortness of breath, tachypnea,
Respiratory syndrome
- cough is dry (1-st day),
later - with liquid transparent foamy
bloody sputum,
- tachycardia,
- delirium,
- at auscultation – scanty data: hard breathing, rales (seldom).
27.
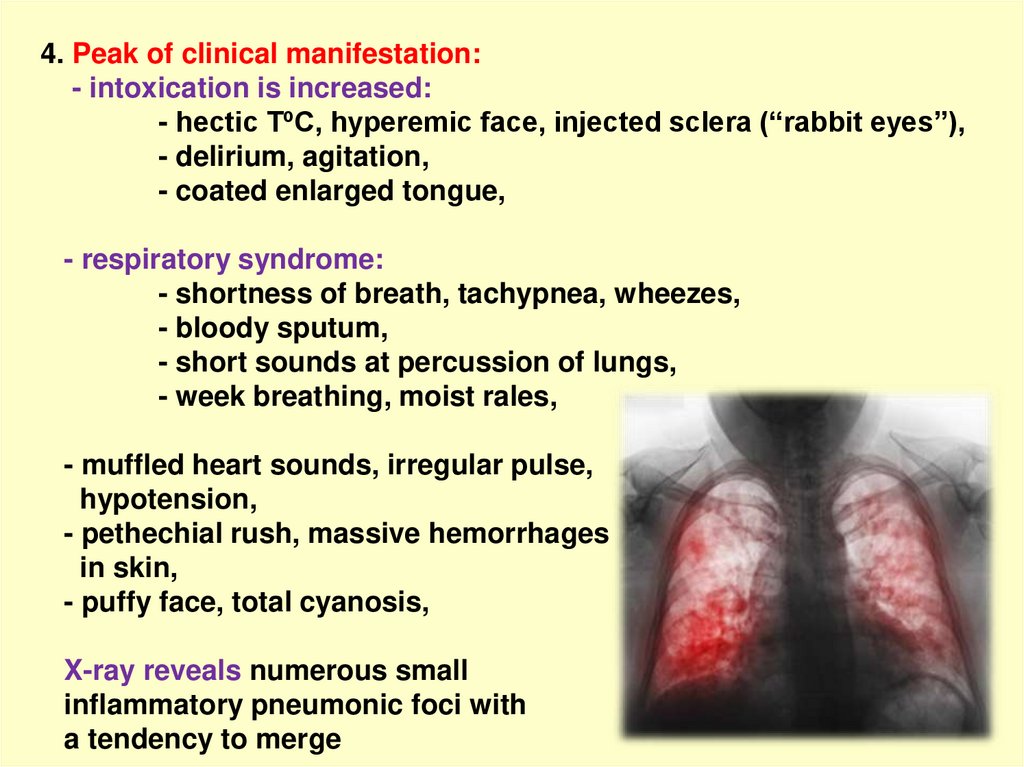
4. Peak of clinical manifestation:- intoxication is increased:
- hectic ТºC, hyperemic face, injected sclera (“rabbit eyes’’),
- delirium, agitation,
- coated enlarged tongue,
- respiratory syndrome:
- shortness of breath, tachypnea, wheezes,
- bloody sputum,
- short sounds at percussion of lungs,
- week breathing, moist rales,
- muffled heart sounds, irregular pulse,
hypotension,
- pethechial rush, massive hemorrhages
in skin,
- puffy face, total cyanosis,
X-ray reveals numerous small
inflammatory pneumonic foci with
a tendency to merge
28.
5. Terminal period:-respiratory distress,
- symptoms of brain edema, desorded consciousness,
- CV failure, ARF,
- Hemorrhagic syndrome, DIS-syndrome,
-Total cyanosis, fear of death,
- Buboes do not have time to form,
- Patient dies on the 3-5 day, often due to pulmonary
edema and ITS
Secondary pneumonic form:
a complication of bubonic
plague, similar to primary
pneumonic plague.
Prognosis: serious, usually - unfavorable
29.
Feature of primary pneumonic plague1. Prevalence of intoxication over pneumonia
in the 1-st days of illness.
2. Tachypnea is always detected at all patients but
does not correspond to the process in the lungs.
3. In the beginning of the disease rare wheezing,
breathing is moderately hard. X-ray: focal,
segmental, lobar pneumonia.
4. On the 2-d day – moist rales, shortening of
percussion sound over the lungs.
5. Cough with mucus, bloody sputum.
6. Pain in the chest on the inhale and pleuropneumonia.
7. Early development of ITS.
8. Hepatosplenomegaly.
9. Lymphadenopathy (paratracheal, parabronchial).
10. Death in 18 hours.
30.
Complications(depend on the clinical forms of plague)
1. Bubonic form - activation of secondary microflora,
- formation of phlegmon,
- development of secondary
septicemia;
2. Pneumonic form: - hemorrhagic pulmonary edema,
- acute respiratory failure,
- ITS;
3. Septicemic form: - ITS,
- acute heart failure,
- meningitis,
- bleeding;
The mortality rate:
- bubonic form: untreated - 70%, in treatment - 10-20%,
- pneumonic form: untreated - 100%, treated - 30 to 50%,
- septicemic form: - untreated - 100%
31.
32.
The clinical and epidemiological criteria1. Epidemiological:
- stay in the natural plague focus (visit in country, unfavorable
for plague),
- contact with source of plague (sick human, animal),
- using of meat of infected animals,
- hunting, skinning rodents or infected animals;
2. Clinical:
- sudden onset,
- hyperthermia, severe intoxication, toxic encephalopathy,
- whitish tongue (as chalk),
- dense, sharply painful, nonmotile bubo with a red-cyanotic skin
over it,
- hemorrhagic syndrome,
- progressive pneumonia;
3. In CBC: leukocytosis, shift formula to the left, increased ESR,
4. GUT: microhematuria, proteinuria, oliguria
33.
Specific diagnosis(only in specific laboratories for especially dangerous infections)
1. Material for the study:
- punctate of bubo, contents of vesicles, pustules,
- smear-imprint of ulcers, smear from the oropharynx,
- sputum, blood, urine, vomiting mass;
2. Bacterioscopy (result in 1-2 h) - ovoid gram-negative bacillus,
painted bipolar;
3. Rapid test (result in 15 min) – IFR;
4. Bacteriological examination: growing of
material on Martin‘s or Hottinger agar;
5. Biological test on animals
(mice and Guinea pigs);
6. Serological methods:
- RPHA; - RIHA; - RN; - ELISA;
7. PCR
34.
Treatment1. Obligate hospitalization in a specialized
department;
2. In cases of suspected plague immediate beginning of etiotropic
treatment before etiological confirmation (more favorable
prognosis);
3. Firs-choice drug - streptomycin – 1g × 4 t/d i/m or i/v
till the 5-th day of normal temperature (on an average
7-14 days);
4. At absence of ARF can be taken gentamycin - 0,002 g/kg × 3 t/d
i/m within 10 days;
5. Second-choice drug – doxycycline 0,1 g × 2 t/d i/m or per os
within 10 days;
6. At the resistance - chloramphenicol - 0,5-1 g × 4 t/d
35.
Pathogenetic treatment(depends on the form and severity of the disease)
- Detoxication (dextrose, reopoliglyucin, saline solutions),
- diuretics,
- cardiac glycosides,
- glucocorticoids,
- vitamins;
Symptomatic treatment: antipyretics, analgetics;
NB!!! Surgical treatment (opening buboes) is contraindicated due
to possible dissemination of Yersinia (action of promoted factors);
Patient can be discharged from the department in
4 (bubonic form) - 6 (pneumonic form) weeks from the
moment of recovery at presence of 3 negative results of
bacteriologic investigation of bubo- punctate, sputum,
feces and pharyngeal swab;
36.
Keep calm andcatch good
moments
in life !!!













 Медицина
Медицина