Похожие презентации:
Anatomy of bones in childhood
1. Background of the lecture
1.Anatomy of bones in childhood
2.
When do the bones of the child` skeleton arise?
3.
Bones and teeth in Biological age evaluation.
4.
The skeleton examination. The most important semiotics of bone
diseases in children.
The skull
The Neck.
The chest
The spine.
The limbs and tubular bones.
The symptoms of innate displastic/dislocative hip (DDH).
5.
6.
The teeth and teeth formula in children. The semiotics of teeth
diseases.
The features of muscles in children
2.
The Anatomical andphysiological particularities of
bone and muscular systems &
its clinical importance. The Teeth
and teeth formula.
3.
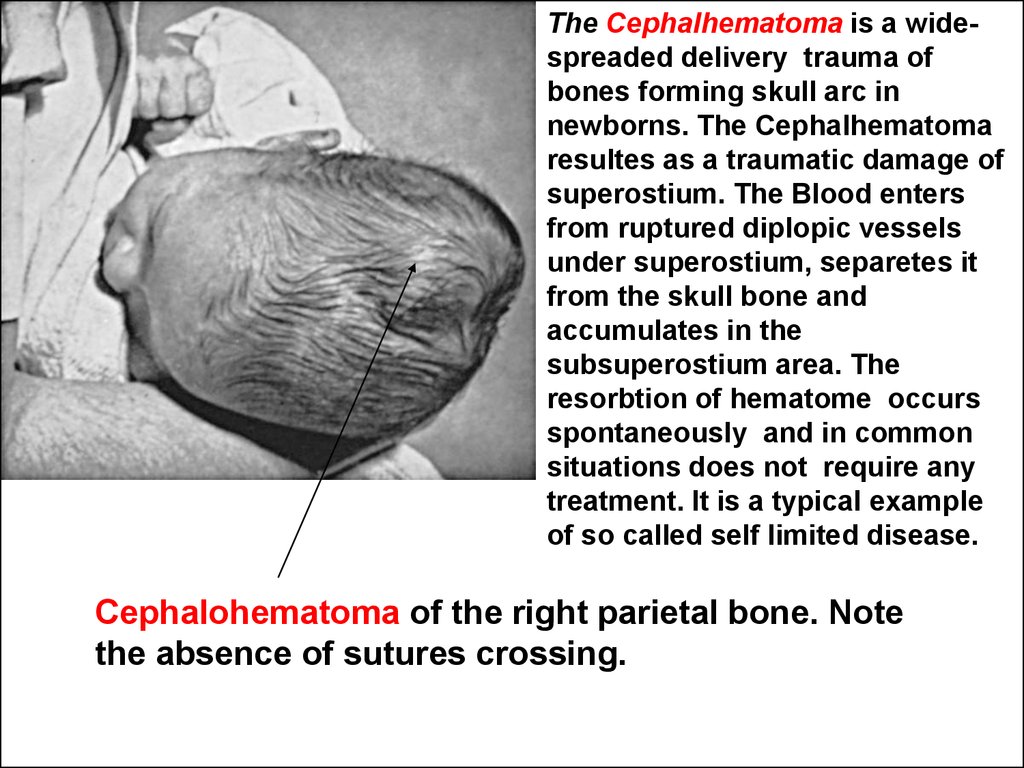
The First kernel of the large bone ossificationappears in a 7-8 weeks aged embryo within its
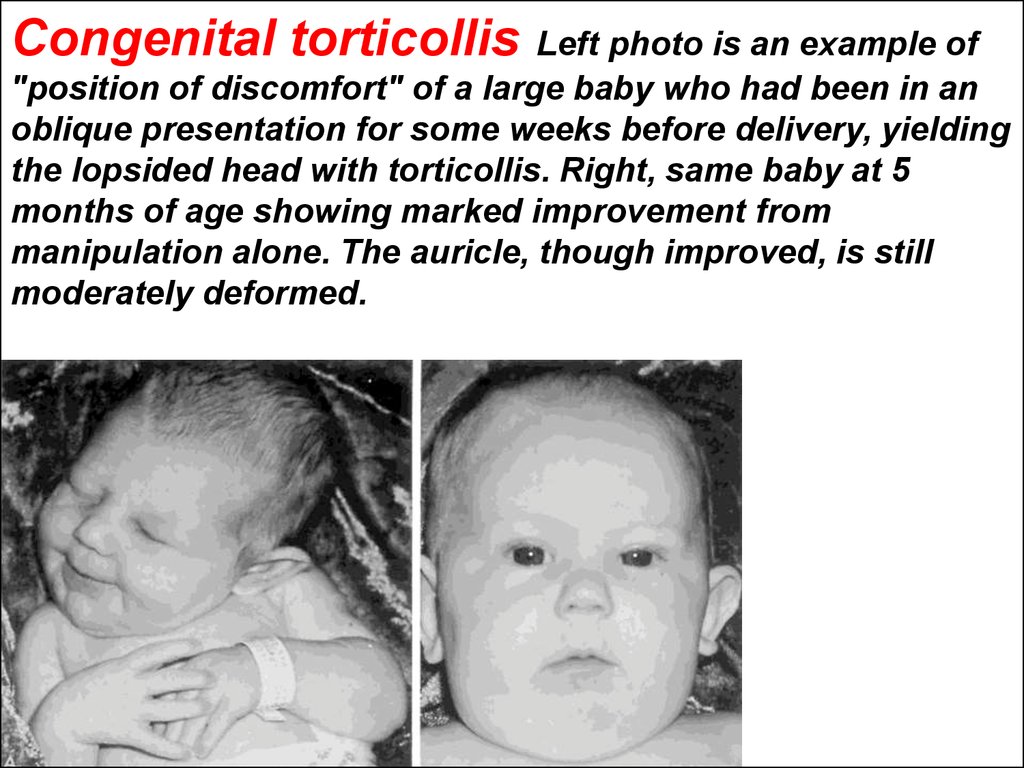
in uteri development. Consequently, at this
time it is possible to consider that bones of
the child skeleton arise.
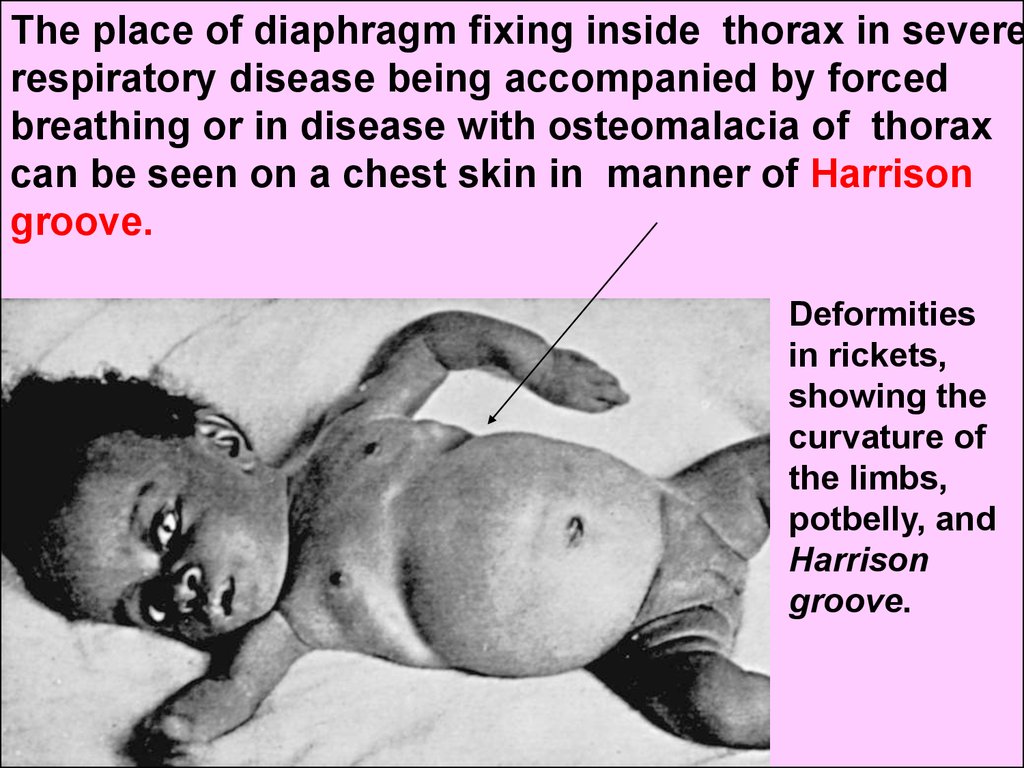
4.
After birth the size of skeleton increases veryintensively according the mass and length growth
of baby body. In this period at list until to 3 years
of age the child skeleton can not be estimated as
stable, firm structure. So called the bone
rebuilding processes are running very intensively.
Alongside with bones growing lengthwise and
width, big importance has a realignment of the
direction of bone beems under gravitation stimulus
influence changing in its direction within childhood.
5.
The fetus and newborn have a sponge likebone masses (A). After age of 3-4 years
children have the lamellar built big bones and
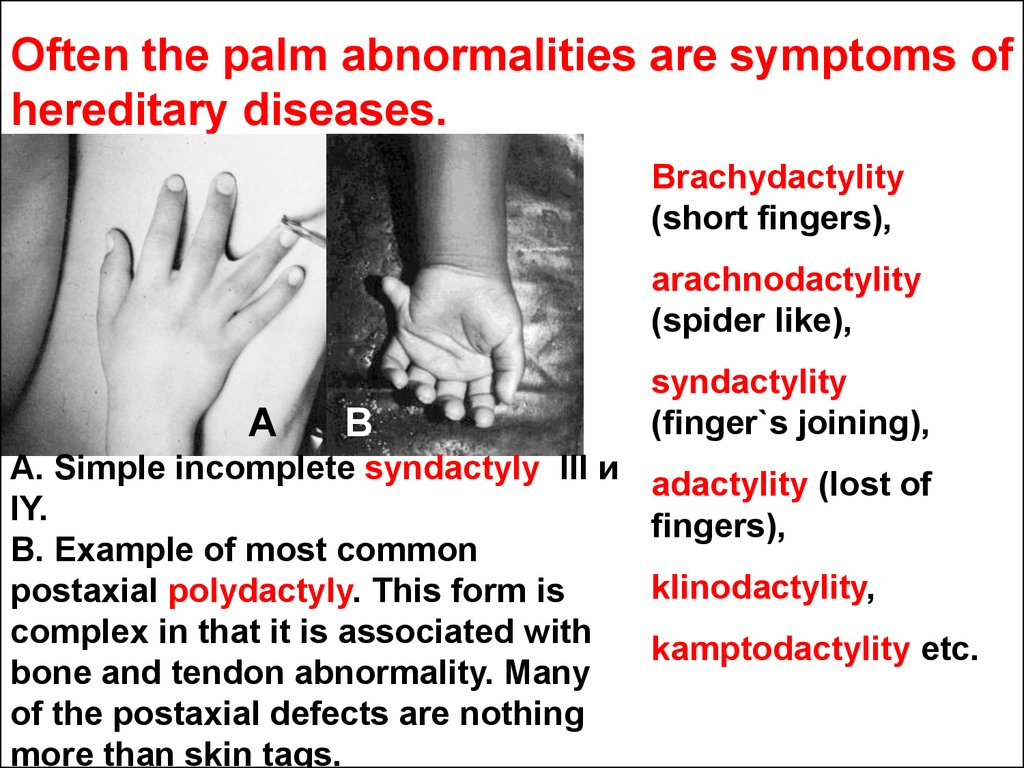
their bone beems are orientated strictly
against earth attraction (gravity, Б). For the
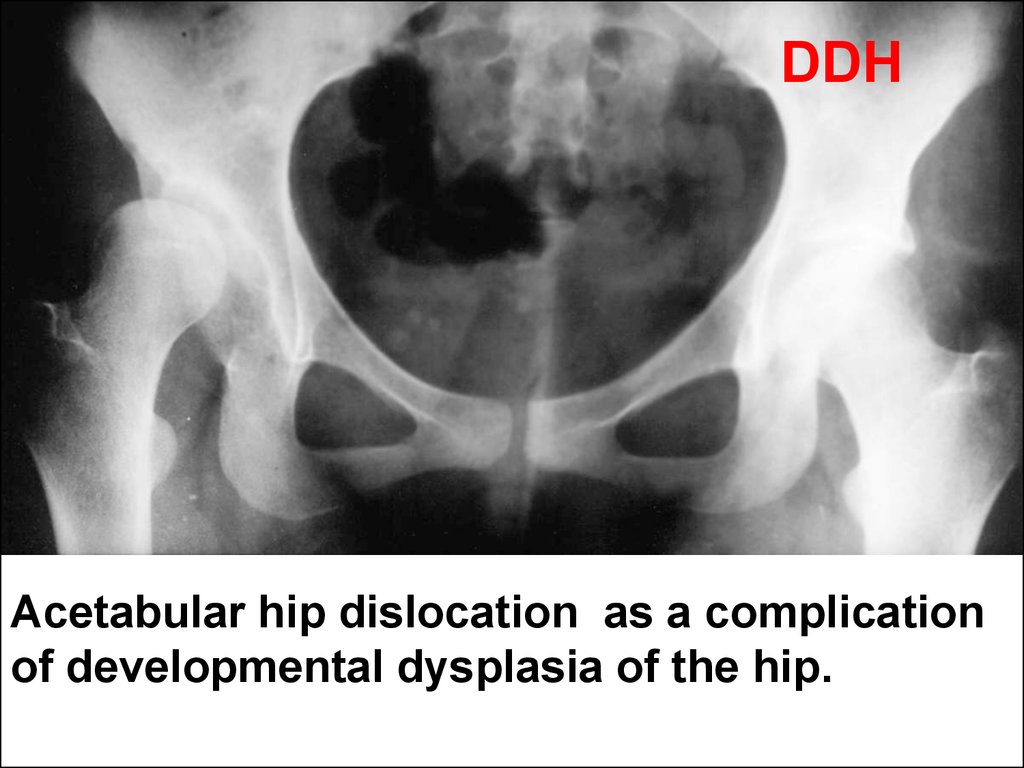
first year of the life about 70% bone tissues
are reutilized and rebuilt.
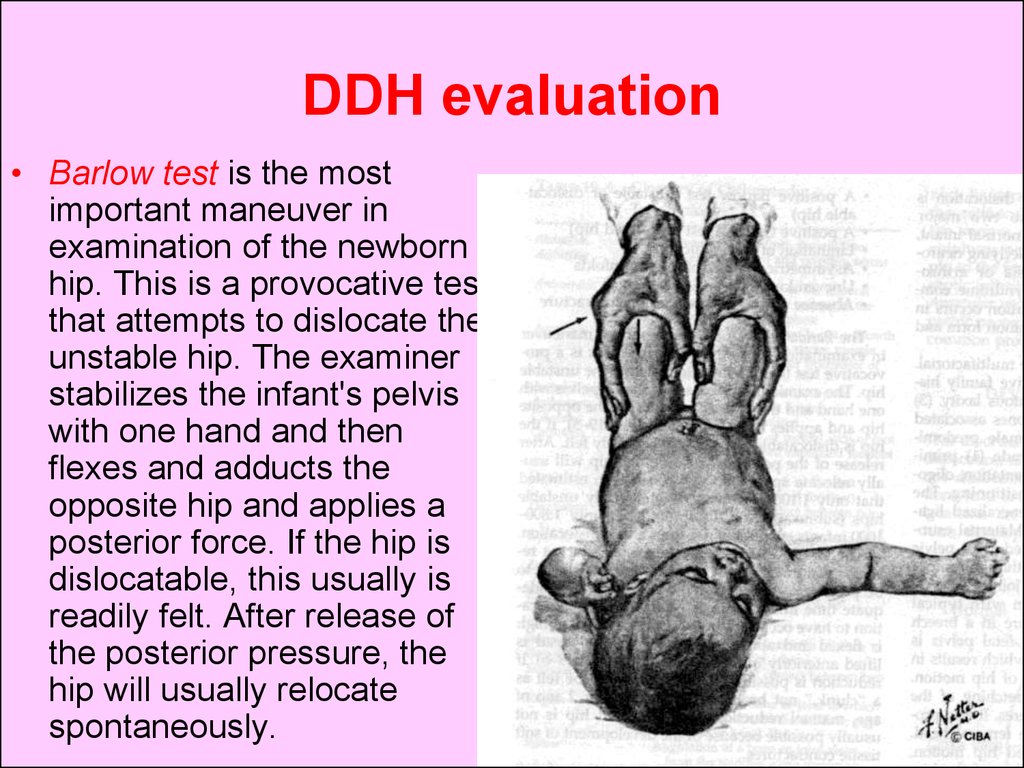
6.
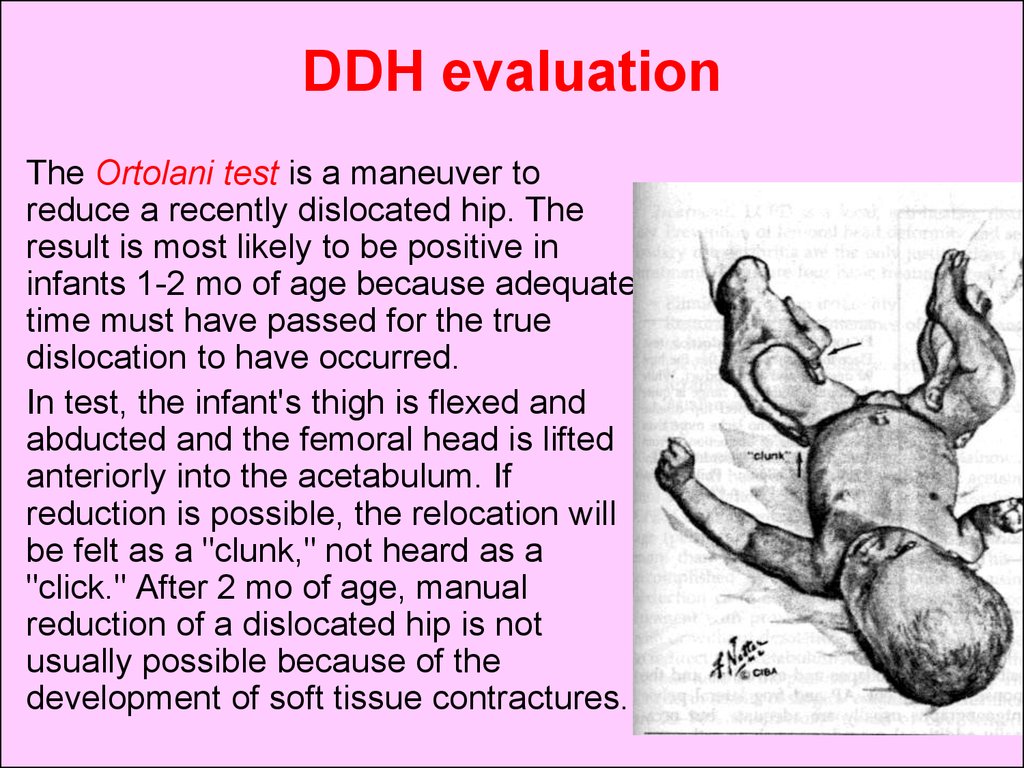
The regeneration and healing processes inchild bones occur in contrast with adult
much sooner. Because of sponge like
construction and special in contrast with
adults chemical composition (pro rata more
significant contents of water and organic
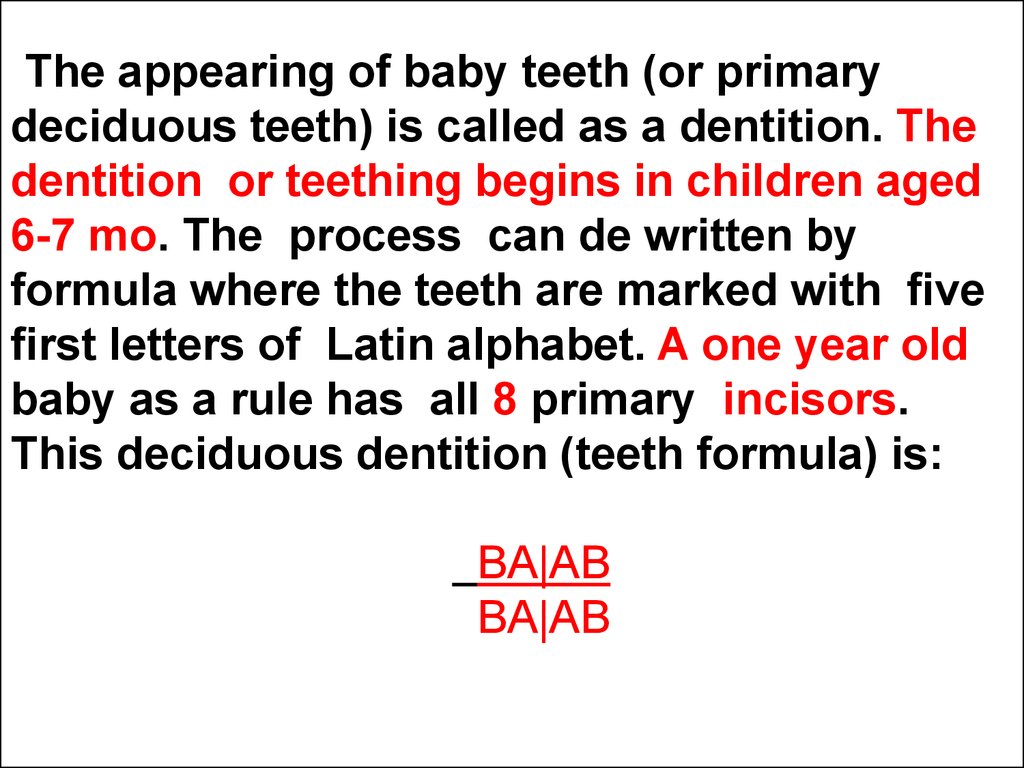
material vs. mineral materials) the children
bones are soft and flexible. That is way
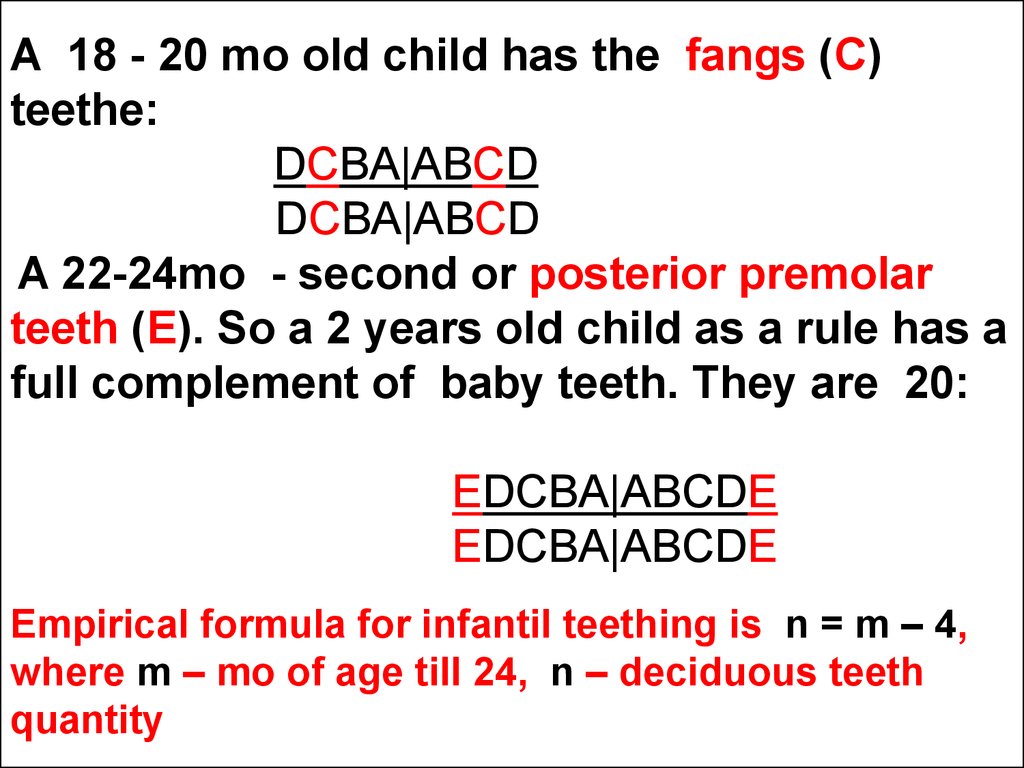
children are less predisposed to fractures
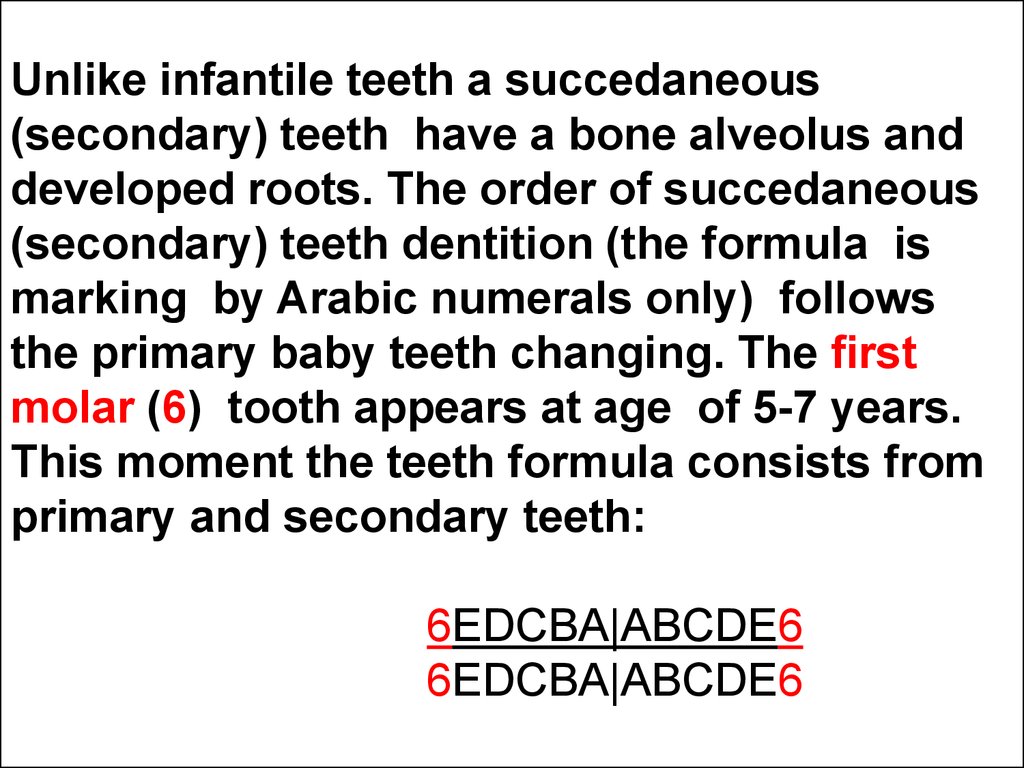
by comparison with adults.
7.
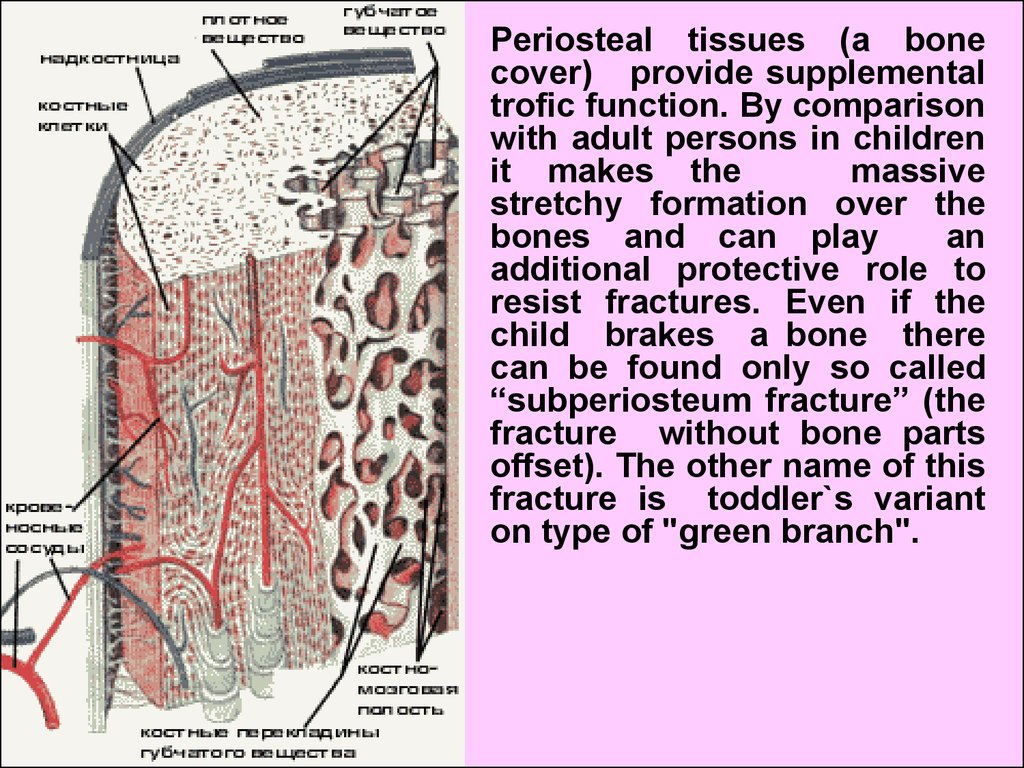
Periosteal tissues (a bonecover) provide supplemental
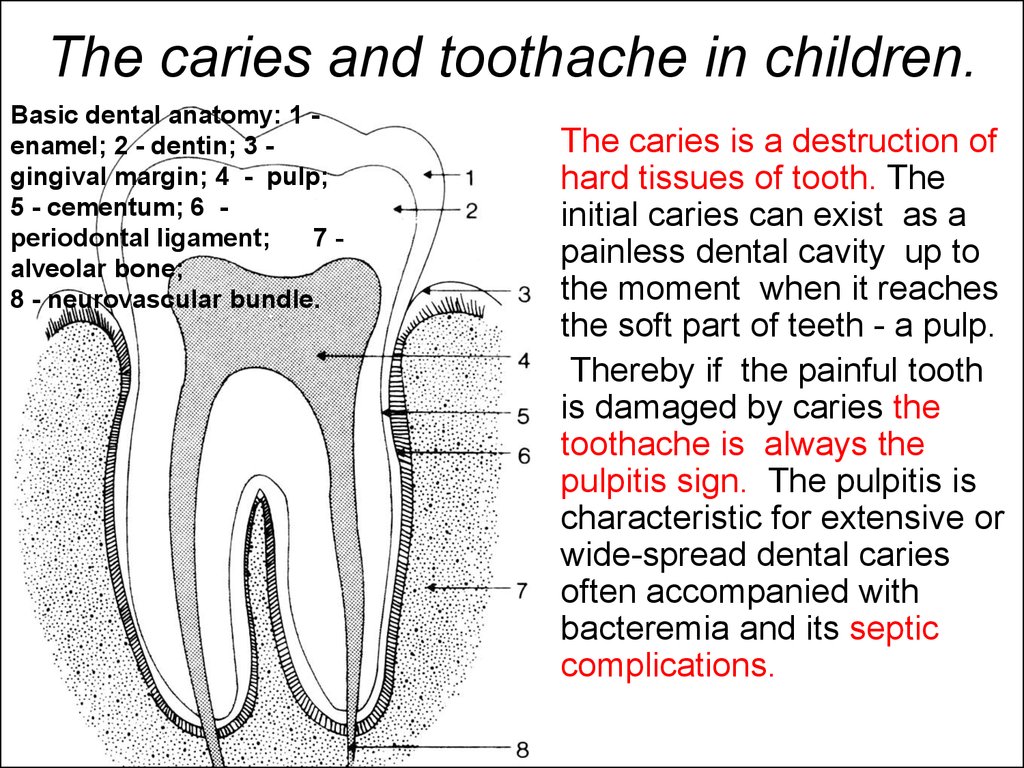
trofic function. By comparison
with adult persons in children
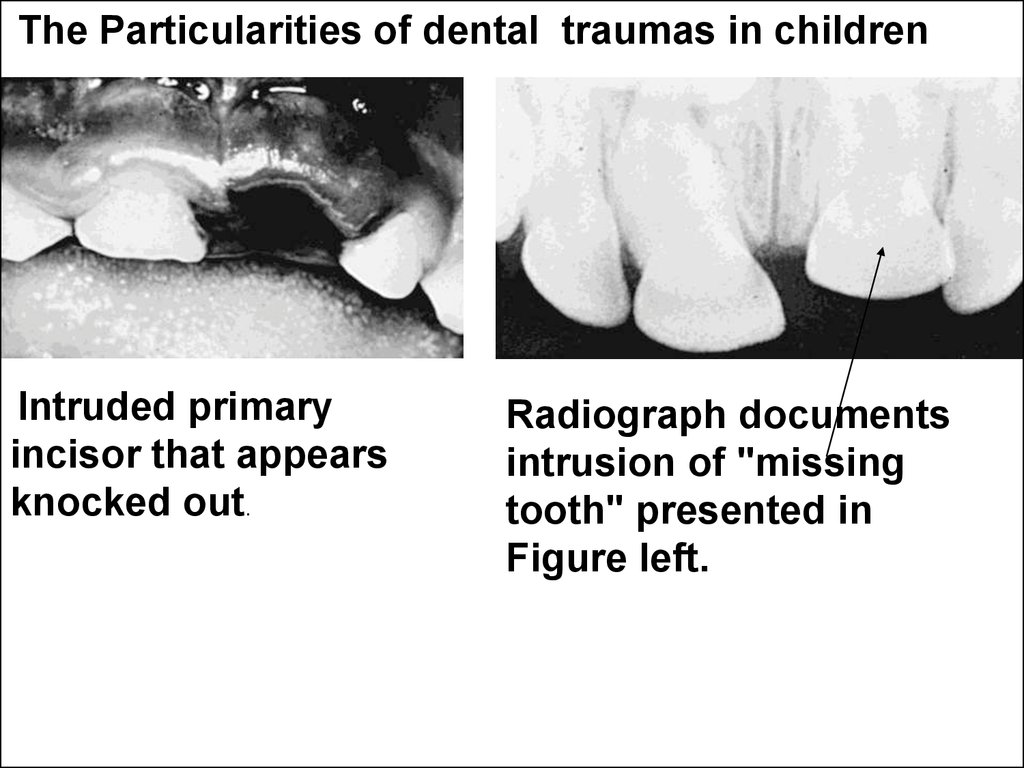
it makes the
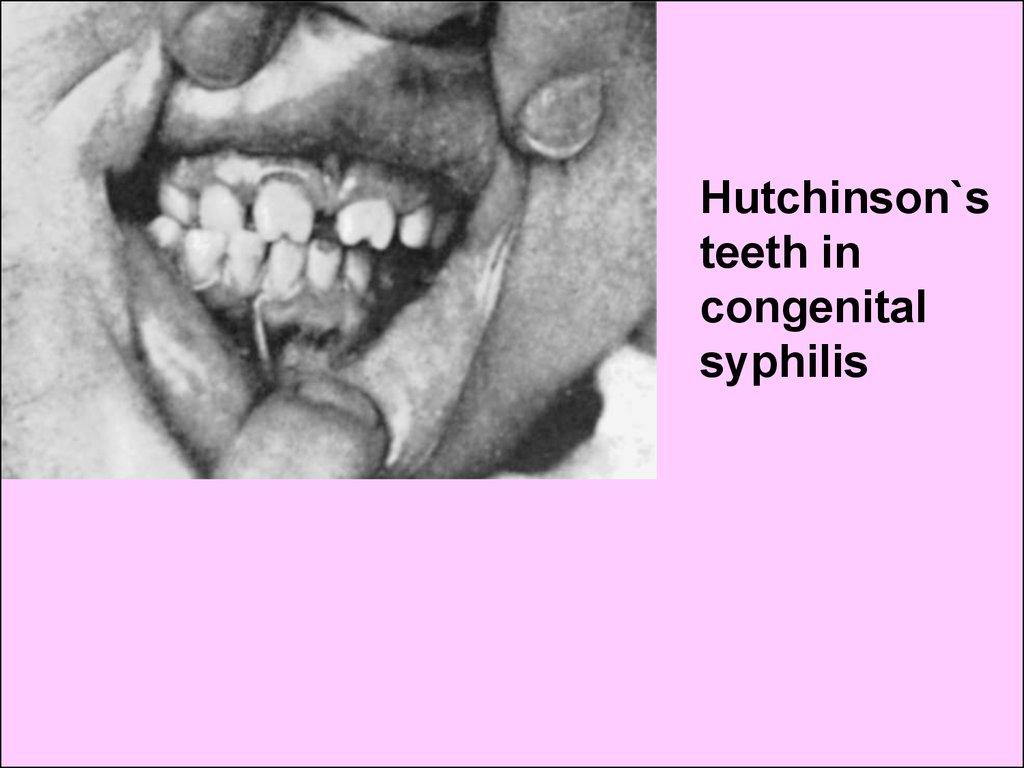
massive
stretchy formation over the
bones and can play
an
additional protective role to
resist fractures. Even if the
child brakes a bone there
can be found only so called
“subperiosteum fracture” (the
fracture without bone parts
offset). The other name of this
fracture is toddler`s variant
on type of "green branch".
8.
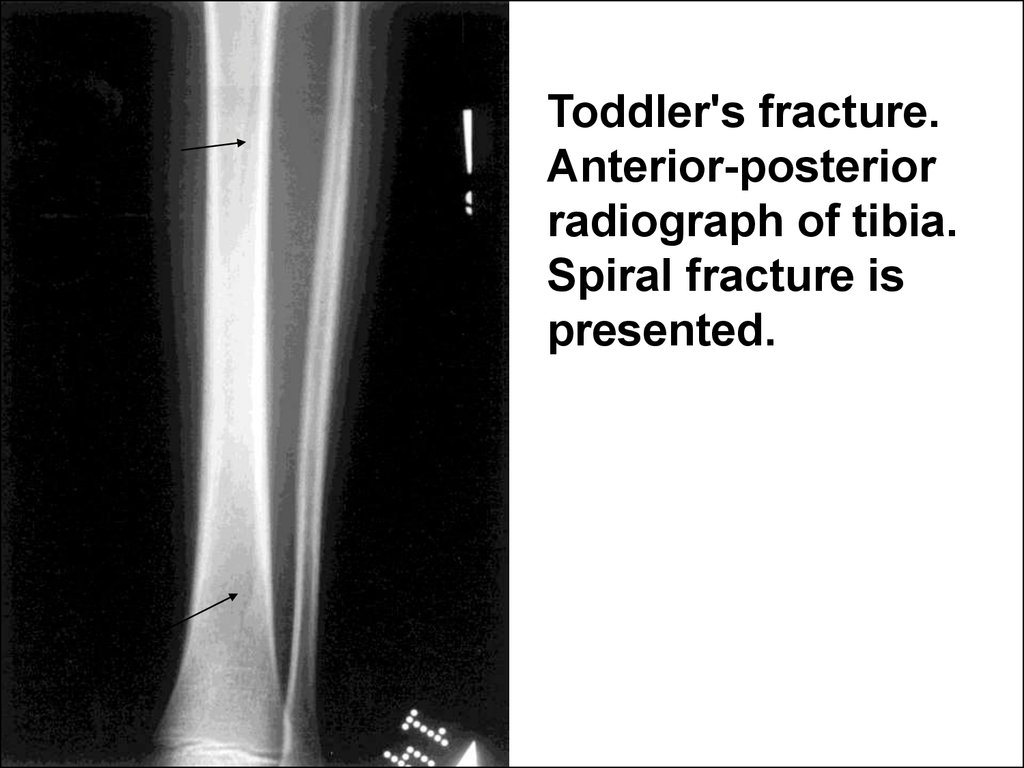
Toddler's fracture.Anterior-posterior
radiograph of tibia.
Spiral fracture is
presented.
9. 3 parameters associated with bone tissue development and biochemicaly same teeth matrix should participate in biological child age estimationon.
The Biological age can be evaluated on:• child growth (body length or height),
• terms of bone ossification (ossification centers
appearing),
• terms of dentition (appearing of constant teeth).
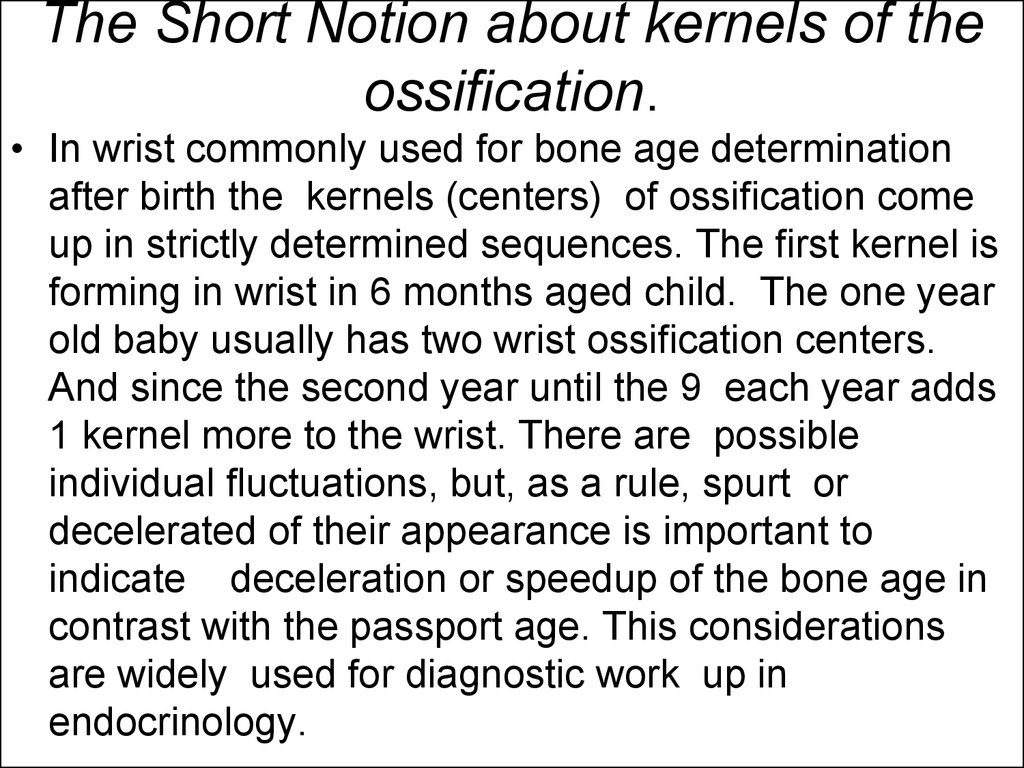
10. The Short Notion about kernels of the ossification.
• In wrist commonly used for bone age determinationafter birth the kernels (centers) of ossification come
up in strictly determined sequences. The first kernel is
forming in wrist in 6 months aged child. The one year
old baby usually has two wrist ossification centers.
And since the second year until the 9 each year adds
1 kernel more to the wrist. There are possible
individual fluctuations, but, as a rule, spurt or
decelerated of their appearance is important to
indicate deceleration or speedup of the bone age in
contrast with the passport age. This considerations
are widely used for diagnostic work up in
endocrinology.
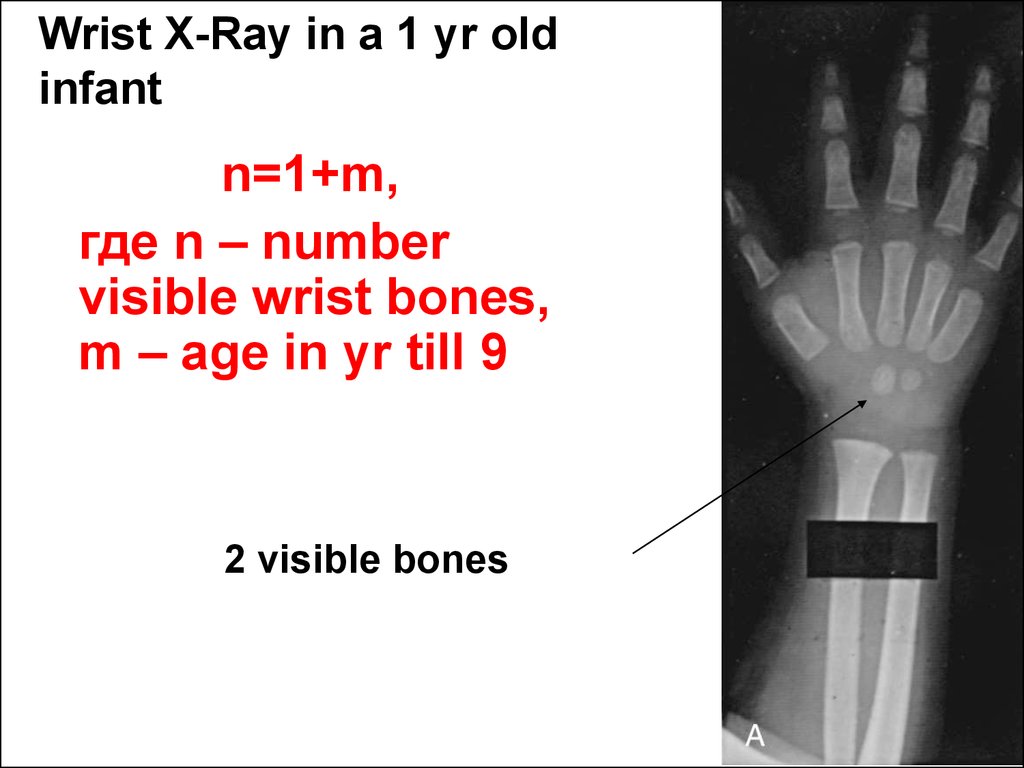
11.
Wrist X-Ray in a 1 yr oldinfant
n=1+m,
где n – number
visible wrist bones,
m – age in yr till 9
2 visible bones
12.
The bone, growth, teeth and passport agecoincidence is indicative for the normal
biological development in a child. If the age
of psychic development also corresponds to
the biological and passport ages you should
consider the child as a harmoniously
developed one. In opposite event the
conclusion about decelerated, accelerated or
disproportional child development has to be
done.
13.
The skeleton examination and themost important semiotics of bone
diseases in children.
14. Estimating the bone system the next clinical approaches are useful:
• Complaints• Additional questioning (case history)
• Objective methods:
visual inspection
palpation
bone percussion sometimes
• Instrumental (mainly X-Ray) investigations.
15.
The most common complaint is thepain. Most often the extremities pain
in children depends on
posttraumatic origin.
16. Complaints
• "Pains of the growing" are typical bed timeaccidental and self limited symptoms in a 4-5
years old children. Their origin is unclear.
The pain in legs could be provoked by
intensively periosteum stretching due to
quick growth and nervous superstimulation.
Often this "Pains" are provoked with
previous high motor activity especially at
evening. The Particularities of care. "Pains of
the growing" should be overcame by careful
inattention from side of the parents. If the
child really require a help the heat
procedures and massage are sufficient.
17. Complaints
• The Flat foot Pains disturb some childrencommonly in shank and appear more often at
evening time after physical load. Do not forget that
in children aged less 2 years the "physiological"
flat foot exists. This phenomenon is better seen
in a child standing on the table or having wet
imprint from the feet. It disappears in tiptoe
position. The guidelines of flat feet prevention
and care are directed on the normal formed arc of
foot shaping in a child. From the infancy the kid
chooses must have an enough hard sole and low
heel. If the foot is shaping flat the insole
supported internal part of foot can be used.
18. Complaints
• The most serious pain symptom whichcould be claimed by the child is a night pain
in bones. This pain often wakes up the
child. Also it accompanies by sensations
of blood pulsations and vascular noises.
This symptom can be provoked by
malignancy of bone (osteosarcoma) or
leukemia (the bone tissues decay occurs
due to leukemic cells infiltration). Also the
bacterial osteomyelitis can be origin of this
pain .
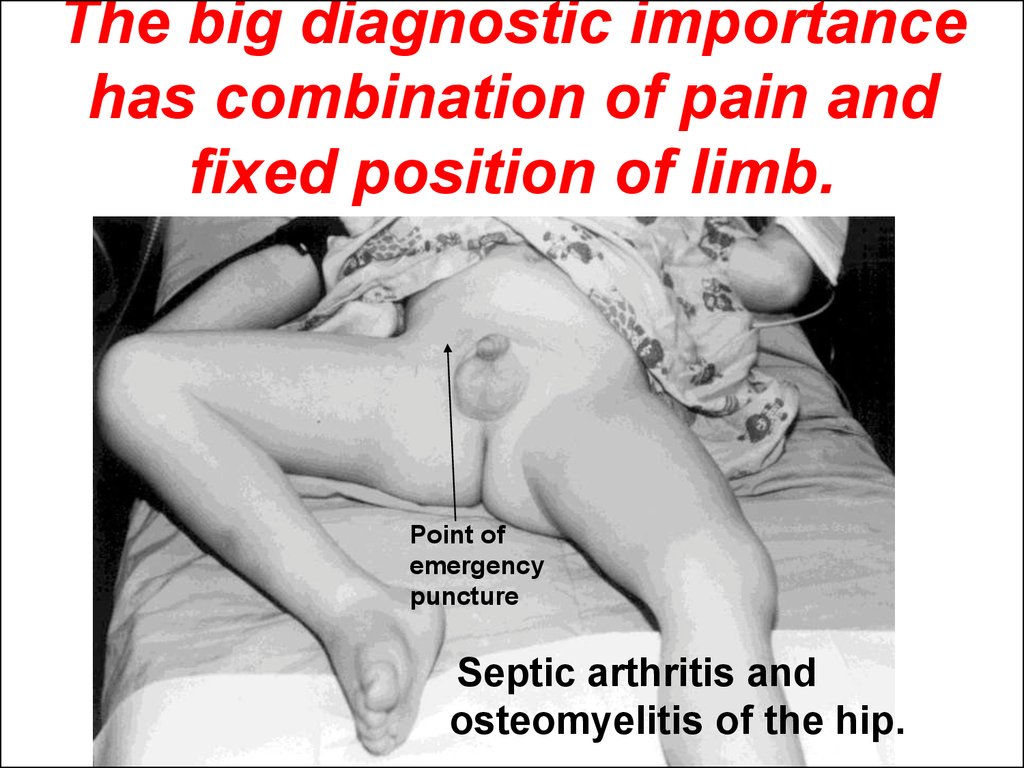
19. The big diagnostic importance has combination of pain and fixed position of limb.
Point ofemergency
puncture
Septic arthritis and
osteomyelitis of the hip.
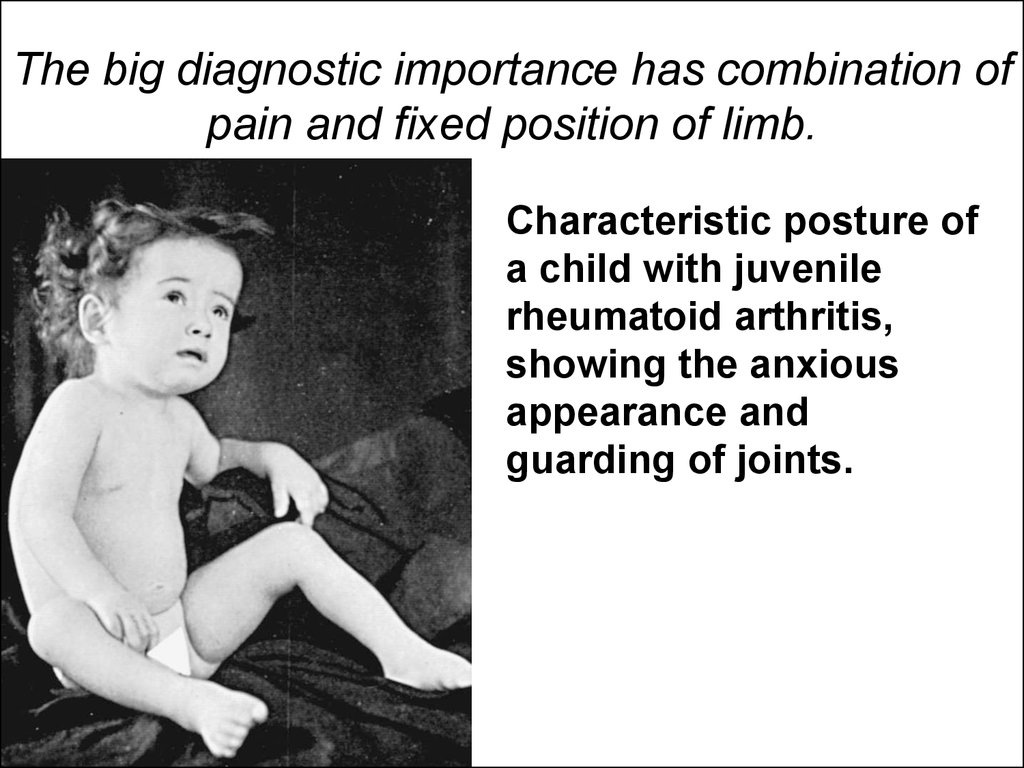
20. The big diagnostic importance has combination of pain and fixed position of limb.
Characteristic posture ofa child with juvenile
rheumatoid arthritis,
showing the anxious
appearance and
guarding of joints.
21. Visual inspection & palpation
Visual inspection & palpation• The Objective investigation of the skeleton
is recommended to conduct from the top
to bottom (from the head vertex to the
feet).
22.
The skull23.
In newborns and early infants the skull has more developedbrain part in contrast with a face skeleton. The brain skull
consists from paired or dabbled bones including frontal
bones and unpaired occipital bone. The opened and formed
by elastic membranes sutures separate one scull bone from
another. This sutures are closing within the infancy period
but lock up completely only in school age. This process is
identified as a synostosis.
There are a fontanels in points of bones joining on. Anterior
fontanel is situated between frontal and temporal bones.
Its normal size at birth is 2-3 sm referring to a measurement
perpendicular to the bone edges. Its synostosis occurs in
age between 4 to 18 mo. Posterior fontanel is found between
temporal and occipital bones. It is locked in 75% of full term
newborns. In rest of the children the posterior fontanel
closes by the end of the first month of life.
24.
During the difficult labor the skull bone edges are crawlingone another one. This is a molding. The molding can be
palpated easy on a kid head and it reflects the physiological
phenomena of head adjustment to delivery.
The broadly opened and soft skull sutures are indicative for
hydrocephalus. In opposite event the premature scull sutures
lock happens and skull is getting small. The small head size
reflects microcephalus as a reduction in volume of the whole
brain skull. The circumfiarence of the child head are smaller
than 5-th percentille size. Often children with microcephalus
suffer from mental deficit disorders and spasticity.
The pathological craniosynostosis is the disorder leading to
skull growth partial limitation and various head deformations
happen.
25.
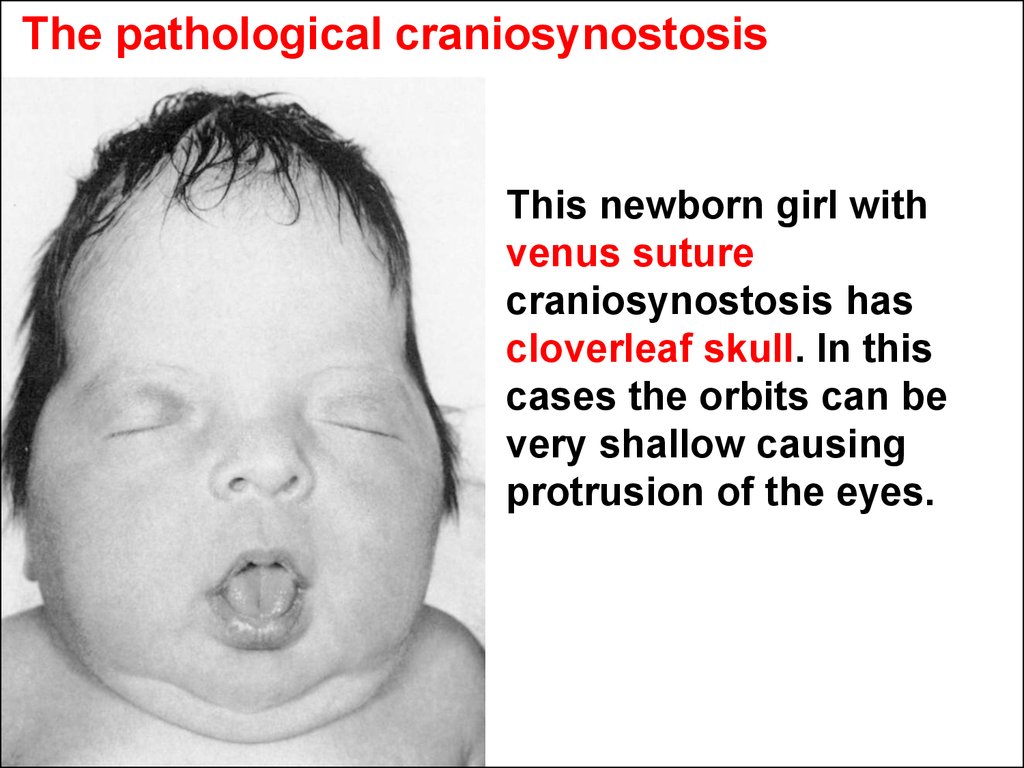
The pathological craniosynostosisThis newborn girl with
venus suture
craniosynostosis has
cloverleaf skull. In this
cases the orbits can be
very shallow causing
protrusion of the eyes.
26.
The pathological craniosynostosisThree-week-old infant with premature sagittal
craniosynostosis.
Lateral view demonstrates the elongated head shape with
tapering in the occipital region. Except for the abnormal
configuration of the head, the child is developmentally
normal for age.
Vertex view reveals the characteristic long, narrow shape of
the calvarium with premature closure of the sagittal suture.
27.
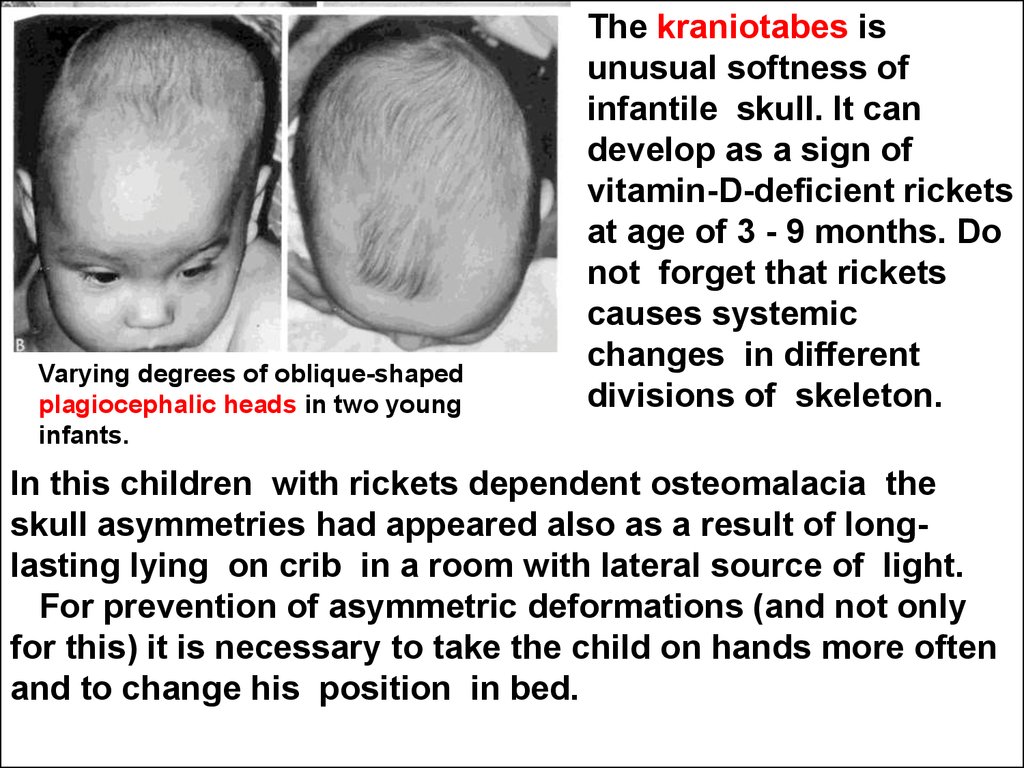
Varying degrees of oblique-shapedplagiocephalic heads in two young
infants.
The kraniotabes is
unusual softness of
infantile skull. It can
develop as a sign of
vitamin-D-deficient rickets
at age of 3 - 9 months. Do
not forget that rickets
causes systemic
changes in different
divisions of skeleton.
In this children with rickets dependent osteomalacia the
skull asymmetries had appeared also as a result of longlasting lying on crib in a room with lateral source of light.
For prevention of asymmetric deformations (and not only
for this) it is necessary to take the child on hands more often
and to change his position in bed.
28.
The Cephalhematoma is a widespreaded delivery trauma ofbones forming skull arc in
newborns. The Cephalhematoma
resultes as a traumatic damage of
superostium. The Blood enters
from ruptured diplopic vessels
under superostium, separetes it
from the skull bone and
accumulates in the
subsuperostium area. The
resorbtion of hematome occurs
spontaneously and in common
situations does not require any
treatment. It is a typical example
of so called self limited disease.
Cephalohematoma of the right parietal bone. Note
the absence of sutures crossing.
29.
The Neck.30.
Congenital torticollisLeft photo is an example of
"position of discomfort" of a large baby who had been in an
oblique presentation for some weeks before delivery, yielding
the lopsided head with torticollis. Right, same baby at 5
months of age showing marked improvement from
manipulation alone. The auricle, though improved, is still
moderately deformed.
31.
The chest32.
In small children the thorax has roundedform and starts to be flat in anterior-posterior
axis in school age. In small children the
breathing mostly is provided by diaphragm.
The ribs for the first year of life are located
horizontally as they were in position of the
maximum inspiration in adults. When the
child begins to walk the diaphragm is
lowered gradually and ribs take a tilt position.
33.
The place of diaphragm fixing inside thorax in severerespiratory disease being accompanied by forced
breathing or in disease with osteomalacia of thorax
can be seen on a chest skin in manner of Harrison
groove.
Deformities
in rickets,
showing the
curvature of
the limbs,
potbelly, and
Harrison
groove.
34.
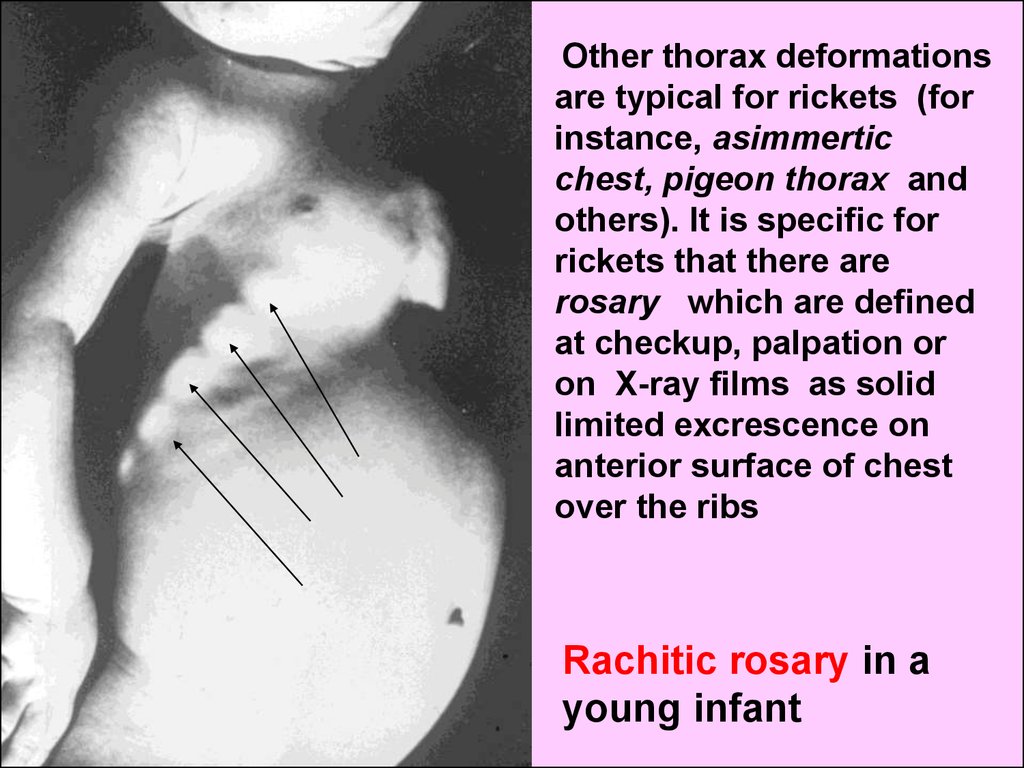
Other thorax deformationsare typical for rickets (for
instance, asimmertic
chest, pigeon thorax and
others). It is specific for
rickets that there are
rosary which are defined
at checkup, palpation or
on X-ray films as solid
limited excrescence on
anterior surface of chest
over the ribs
Rachitic rosary in a
young infant
35. Other thorax deformations
• The insulated thorax deformations most oftenare innate and same of them can be
discovered in child`s relatives.
• The big diagnostic importance in cases of
advanced heart diseases with a cardiomegaly
(big heart size) has a symptom of precordial
bulge. The precordial bulge is formed on
anterior thorax surface on area of the heart
projection.
36.
The spine.37. Spinal curves
• In newborns the spine is direct with a smallprotuberance backwards in the area of rump. There
are not cervical, thorax or pelvic physiological spine
deviations in anterior-posterior direction. They will be
very useful for amortization of the spinal column when
the child walks, jumps.
• After the child lies in prone position and begins to
raise slightly the head upwards the cervical lordosis
(onwards spinal arc) is forming. When the child starts
to sit down the lumbar lordosis and to stand up the
chest kyphosis will appear. The cases of the
exaggerated lordosis and kyphosis (backwards spinal
arc especially in thorax) are defined as hyperlordosis
and hyperkiphosis and are to be treated.
38. The spine deviations aside are never being physiological and are nominated as scoliotic.
• One of the predisposing factors of scoliosis development is aphenomenon of functional human body asymmetry. By other
words the left and right half of human body are seldom
completely alike on size. Under monotonous load deforming
spine the accustomed or functional scoliosis can appear.
• That is way the parents and school teachers have to pay
much attention on children bearing shaping. It means a pose
correction at letter in school, advise do not carry briefcases
etc. The bed in childhood has to have an enough hard better
orthopedic mattress. All motor sports especially swimming as
a rule promote the correct bearing shaping.
• The pathological scoliosis appears as result of preceding
diseases of bones and muscles.
39.
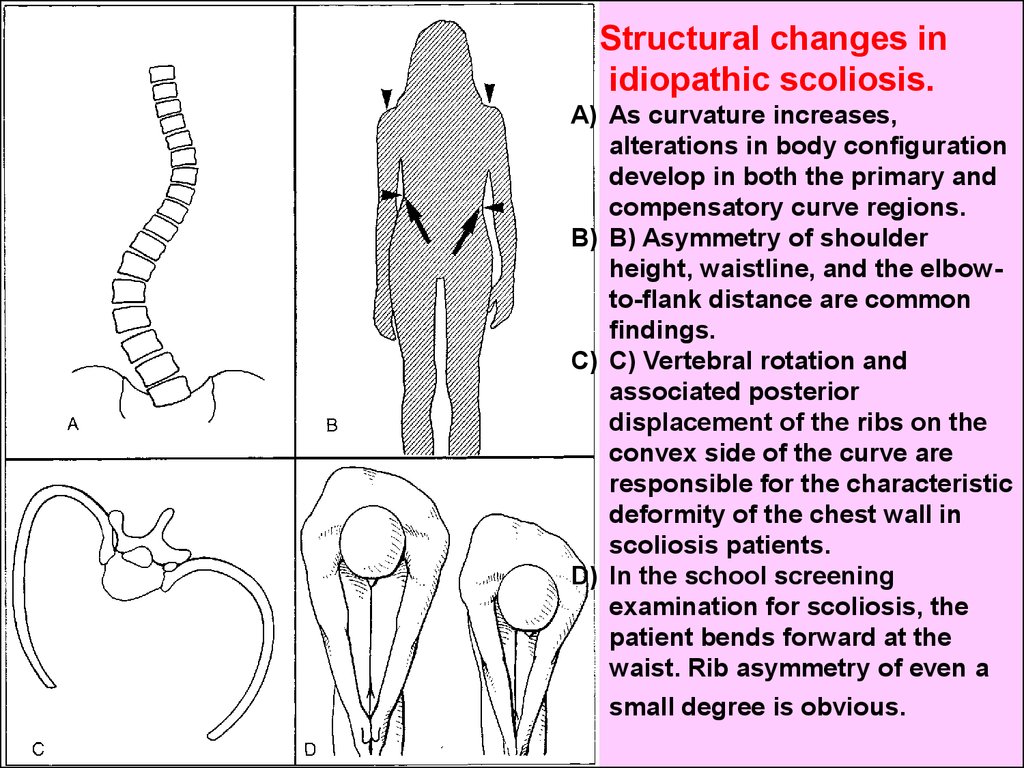
Structural changes inidiopathic scoliosis.
A) As curvature increases,
alterations in body configuration
develop in both the primary and
compensatory curve regions.
B) B) Asymmetry of shoulder
height, waistline, and the elbowto-flank distance are common
findings.
C) C) Vertebral rotation and
associated posterior
displacement of the ribs on the
convex side of the curve are
responsible for the characteristic
deformity of the chest wall in
scoliosis patients.
D) In the school screening
examination for scoliosis, the
patient bends forward at the
waist. Rib asymmetry of even a
small degree is obvious.
40.
The limbs and tubular bones.41.
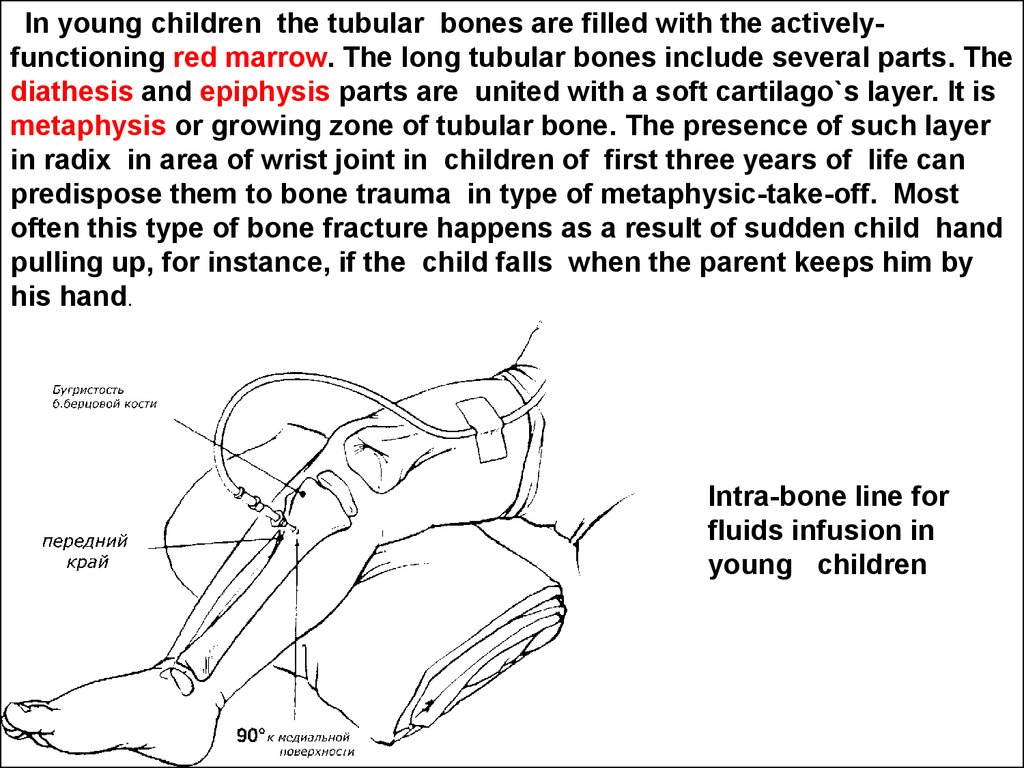
In young children the tubular bones are filled with the activelyfunctioning red marrow. The long tubular bones include several parts. Thediathesis and epiphysis parts are united with a soft cartilago`s layer. It is
metaphysis or growing zone of tubular bone. The presence of such layer
in radix in area of wrist joint in children of first three years of life can
predispose them to bone trauma in type of metaphysic-take-off. Most
often this type of bone fracture happens as a result of sudden child hand
pulling up, for instance, if the child falls when the parent keeps him by
his hand.
Intra-bone line for
fluids infusion in
young children
42. Limb` deformations
• It is known that multiple symmetricdeformations of upper and lower limbs are
characteristic of severe rickets. Especially so
called knock-knee (valgus or X-shaped)
deformity of knees or bowleg like deformity varus angulation (О-shaped or genu varum) are
related with rickets in children.
• However it must be kept in mind that in children
younger 2 yr the first impression is that their
legs are slightly varus – formed, and children
aged 2-7 yr – valgus - formed.
43. Skeleton` deformations
• If the deformations of skeleton areconditioned by anatomical elements lost
(for instance, absence of clavicles, radix or
fibula), or there is an unusual construction
of joints (arthrogriposis) or pathologicaly
repeated bone fractures (osteogenesis
imperfecta) such conditions pertain to
innate hereditary diseases.
44.
Congenital absence of clavicles45.
Often the palm abnormalities are symptoms ofhereditary diseases.
Brachydactylity
(short fingers),
arachnodactylity
(spider like),
А
В
А. Simple incomplete syndactyly III и
IY.
В. Example of most common
postaxial polydactyly. This form is
complex in that it is associated with
bone and tendon abnormality. Many
of the postaxial defects are nothing
more than skin tags.
syndactylity
(finger`s joining),
adactylity (lost of
fingers),
klinodactylity,
kamptodactylity etc.
46.
The symptoms of innatedisplastic/dislocative hip
(DDH) in infants and
children.
47.
DDHAcetabular hip dislocation as a complication
of developmental dysplasia of the hip.
48. DDH evaluation
• Limitation of hipabduction is
indicative of soft
tissue contractures
and may indicate
DDH. Conversely,
hip abduction
contractures may
indicate dysplasia of
the contralateral hip.
49. DDH evaluation
• Barlow test is the mostimportant maneuver in
examination of the newborn
hip. This is a provocative test
that attempts to dislocate the
unstable hip. The examiner
stabilizes the infant's pelvis
with one hand and then
flexes and adducts the
opposite hip and applies a
posterior force. If the hip is
dislocatable, this usually is
readily felt. After release of
the posterior pressure, the
hip will usually relocate
spontaneously.
50. DDH evaluation
The Ortolani test is a maneuver toreduce a recently dislocated hip. The
result is most likely to be positive in
infants 1-2 mo of age because adequate
time must have passed for the true
dislocation to have occurred.
In test, the infant's thigh is flexed and
abducted and the femoral head is lifted
anteriorly into the acetabulum. If
reduction is possible, the relocation will
be felt as a "clunk," not heard as a
"click." After 2 mo of age, manual
reduction of a dislocated hip is not
usually possible because of the
development of soft tissue contractures.
51. DDH evaluation
An asymmetric number of thigh skinfolds and
apparent shortening of an extremity when the
supine infant's feet are placed together on the
examining table with the hips and knees
flexed (positive Galeazzi - Allias sign) is
suggestive of DDH because these findings
indicate proximal displacement of the femoral
head.
52. DDH evaluation
In older or walking children, complaints of
limping, waddling (bilateral DDH), increased
lumbar lordosis (swayback), toe-walking, and
in-toeing may be associated with an
unrecognized DDH.
In this children the Trendelenburg`s sign
becomes positive. Looking on the trunk from
the back the pelvic movements upwards and
downwards are seen when the child stands up
on well or affected limb alternately.
53.
The teeth and teeth formula inchildren. The semiotics of teeth
diseases.
54.
The teeth are a skin appurtenance becausethey are derived from the embrio ectoderma.
But on their biochemistries and physiologies
the teeth and especially dentin are very
closed to bone tissue. That is way in pediatric
practice traditionally the teeth condition is
used as marker of the bone tissue welfare.
55.
The appearing of baby teeth (or primarydeciduous teeth) is called as a dentition. The
dentition or teething begins in children aged
6-7 mo. The process can de written by
formula where the teeth are marked with five
first letters of Latin alphabet. A one year old
baby as a rule has all 8 primary incisors.
This deciduous dentition (teeth formula) is:
BA|AB
BA|AB
56.
A 12 -15 mo old child as a rule has the first oranterior premolar teeth( D):
D BA|AB D
D BA|AB D
57.
A 18 - 20 mo old child has the fangs (C)teethe:
DCBA|ABCD
DCBA|ABCD
A 22-24mo - second or posterior premolar
teeth (E). So a 2 years old child as a rule has a
full complement of baby teeth. They are 20:
EDCBA|ABCDE
EDCBA|ABCDE
Empirical formula for infantil teething is n = m – 4,
where m – mo of age till 24, n – deciduous teeth
quantity
58.
Unlike infantile teeth a succedaneous(secondary) teeth have a bone alveolus and
developed roots. The order of succedaneous
(secondary) teeth dentition (the formula is
marking by Arabic numerals only) follows
the primary baby teeth changing. The first
molar (6) tooth appears at age of 5-7 years.
This moment the teeth formula consists from
primary and secondary teeth:
6EDCBA|ABCDE6
6EDCBA|ABCDE6
59.
The incisors are changing at age 7-9 years:6EDC21|12CDE6
6EDC21|12CDE6
At age of 10-12 years in children the intensive
secondary teething occurs. The
succedaneous fangs (3) and premolars (4
and 5) change deciduous ones. The second
molars (7) apeare. A little bit later the third
molars (8) appear. This teeth are called “a
teeth of wisdom". .
60. What is the “difficult" teething?
What is the “difficult" teething?Pain, itching, hypersalivation.
Head cold.
Fever.
Diarrhea.
Always a physician has to pay attention to
complicated dentition which a parents as a rule
involve with term "difficult but harmless
teething”.
61. The caries and toothache in children.
Basic dental anatomy: 1 enamel; 2 - dentin; 3 gingival margin; 4 - pulp;5 - cementum; 6 periodontal ligament;
7alveolar bone;
8 - neurovascular bundle.
• The caries is a destruction of
hard tissues of tooth. The
initial caries can exist as a
painless dental cavity up to
the moment when it reaches
the soft part of teeth - a pulp.
• Thereby if the painful tooth
is damaged by caries the
toothache is always the
pulpitis sign. The pulpitis is
characteristic for extensive or
wide-spread dental caries
often accompanied with
bacteremia and its septic
complications.
62.
In smallchildren having
deciduous
teeth with
small amount of
dentin the
dental caries
has some
particularities.
Nursing bottle caries.
63.
The Particularities of dental traumas in childrenIntruded primary
incisor that appears
knocked out.
Radiograph documents
intrusion of "missing
tooth" presented in
Figure left.
64.
Hutchinson`steeth in
congenital
syphilis
65.
The features of muscles inchildren
66. Some features of muscles
• The hystomorfological studies of muscular tissues in young childrenshow the short and thick myocytes containing big amount of cell
nuclei, abundance of interstitium and blood vessels.
• The children skeleton muscles comparatively with such adults contain
less myosin and actine contractive proteins and more water. As a
result the children muscles are very stretchable and are not prone to
ruptures.
• The strength of muscular contractions is lesser then in adults.
• It is considered that intensive blood flow in children muscles
promote quick elimination of acidity forming during muscular load.
This fact explains the high physiological muscular activity in children
which can feel the true muscular joy moving. In any event it is
prohibited to limit children in their motor activity.
• Common muscular mass begins to increase only in teens - from 22 25% from body weight in pre-pubertal children up to 45% in maleteenagers aged 15 years. The muscular mass increasing occurs by
account of each myocyte size increasing. The represented facts
undoubtedly witness that so called "body building" and other athletics
are for children younger 13 meaningless and even harmful.
67. The skeleton muscles clinical investigation
• The complaints most often concern such subjectivesensations of pain in limbs and motion restriction.
This complaints commonly are related with
consequences of traumas which happen in children
very often.
• The spontaneous pain is characteristic for myalgia.
For children it is very typical the muscular pains
related with fever. The mechanism of their origin is
not clear yet.
• The muscle groups clinical survey usually combines
with their palpations. During this procedure it is
necessary to reveal the muscular atrophies,
hypertrophies, contracturas and tenderness.
68.
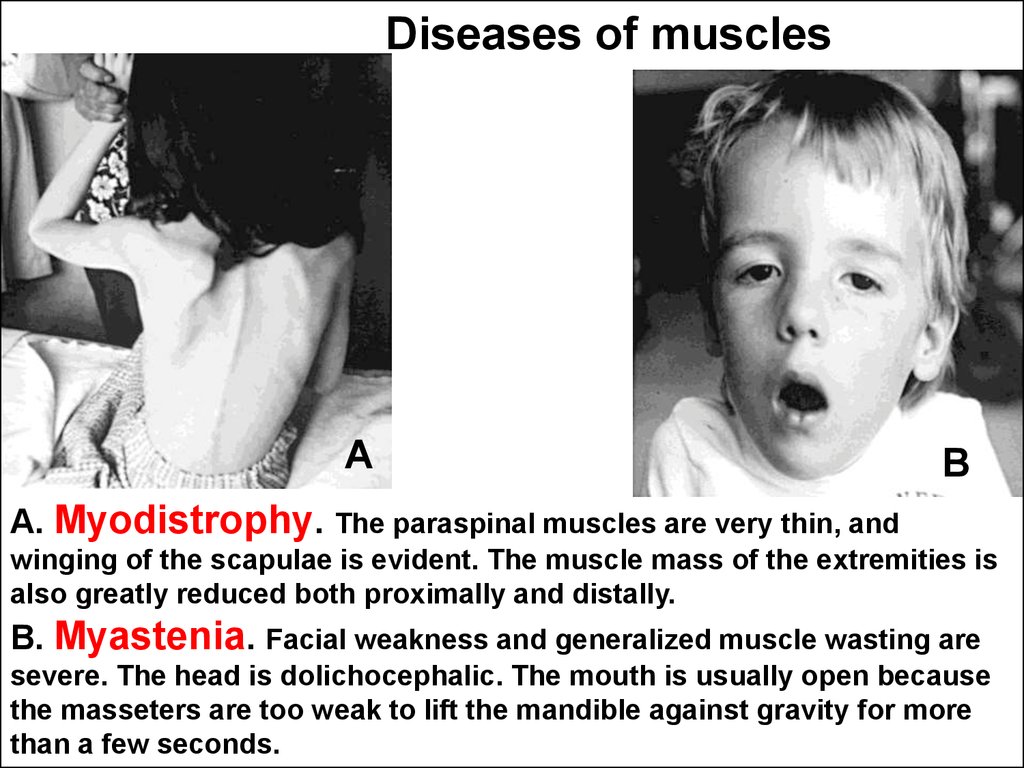
Diseases of musclesА
В
А. Myodistrophy. The paraspinal muscles are very thin, and
winging of the scapulae is evident. The muscle mass of the extremities is
also greatly reduced both proximally and distally.
В. Myastenia. Facial weakness and generalized muscle wasting are
severe. The head is dolichocephalic. The mouth is usually open because
the masseters are too weak to lift the mandible against gravity for more
than a few seconds.
69.
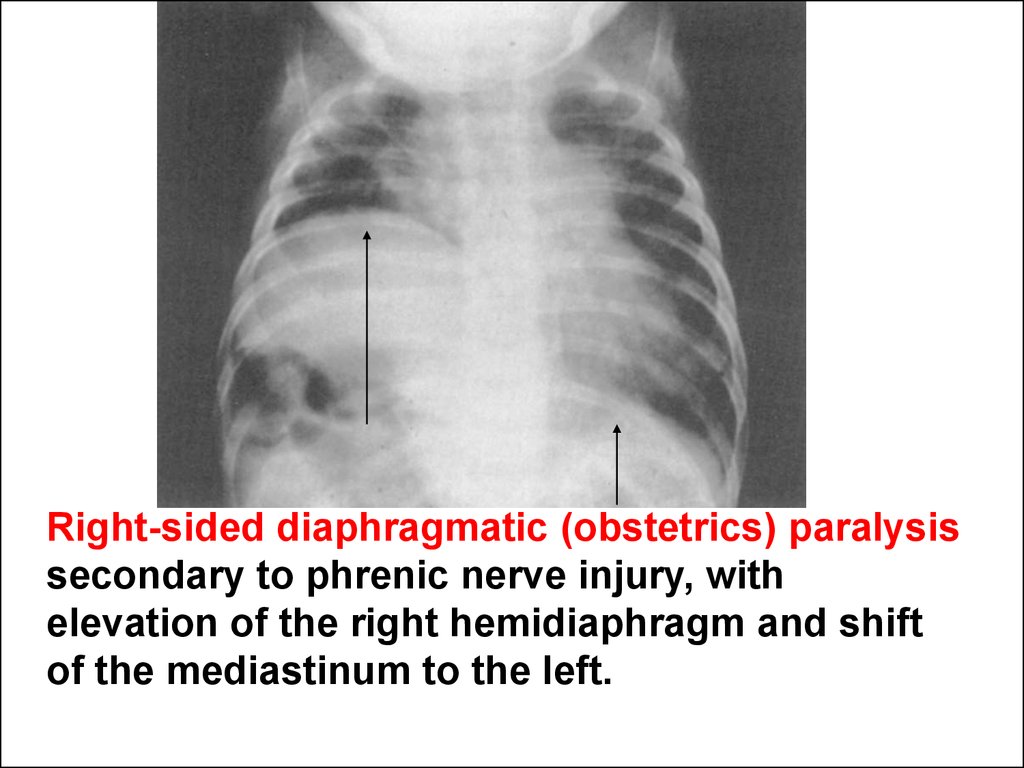
Right-sided diaphragmatic (obstetrics) paralysissecondary to phrenic nerve injury, with
elevation of the right hemidiaphragm and shift
of the mediastinum to the left.
















 Медицина
Медицина