Похожие презентации:
Neurology
1.
NeurologyMULTIPLE SCLEROSIS
MOTOR NEURON DISEASE
MOVEMENT DISORDER
2.
Multiple sclerosisCause is unknown
Usually young females
Charcot’s neurologic triad
Dysarthria
Nystagmus
Intension tremor
Specific signs:
Uhthoff’s sign
Lhermitte’s sign
3.
Multiple sclerosisDiagnosis
MRI
Cerebrospinal fluid
Visual evoked potential
Treatment
RRMS
Corticosteroids, cyclophosphamide,
intravenous immunoglobulin
Plasmapheresis
Immunosuppressant: recombinant b-IFN
Progressive MS
Manage symptoms
Physical therapy
Cognitive rehabilitation therapy
4.
5.
6.
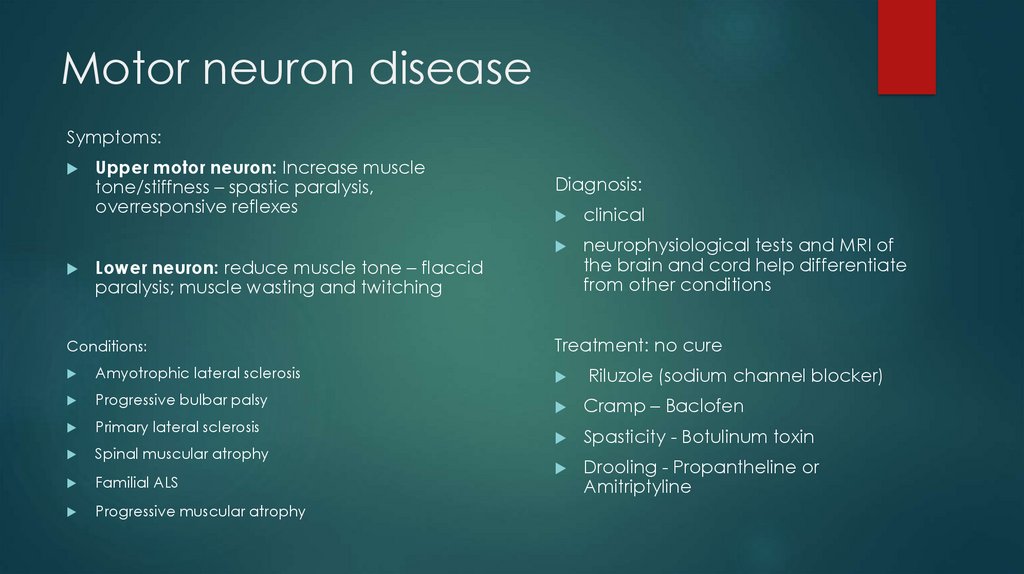
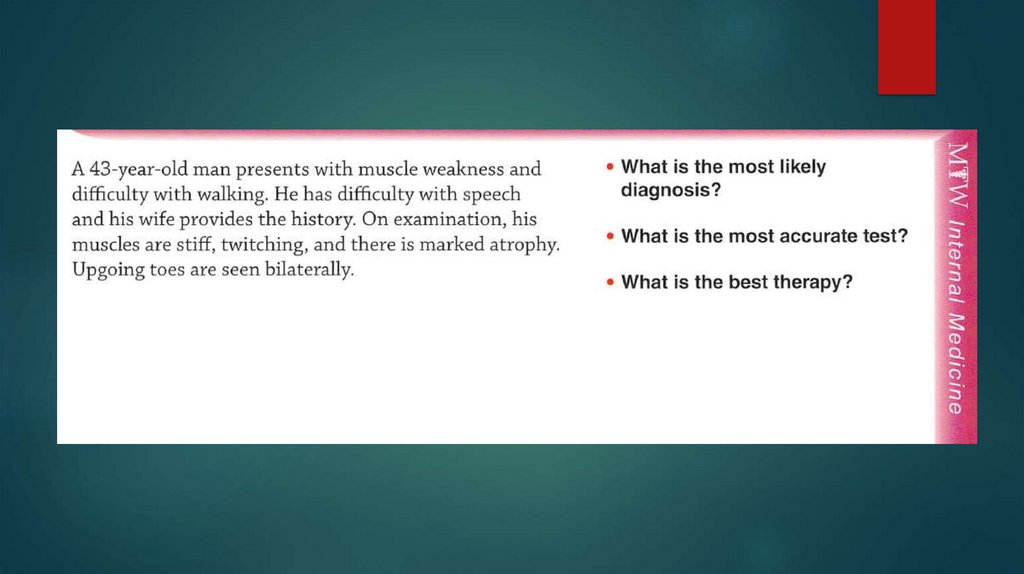
Motor neuron diseaseSymptoms:
Upper motor neuron: Increase muscle
tone/stiffness – spastic paralysis,
overresponsive reflexes
Diagnosis:
clinical
neurophysiological tests and MRI of
the brain and cord help differentiate
from other conditions
Lower neuron: reduce muscle tone – flaccid
paralysis; muscle wasting and twitching
Conditions:
Treatment: no cure
Amyotrophic lateral sclerosis
Progressive bulbar palsy
Cramp – Baclofen
Primary lateral sclerosis
Spasticity - Botulinum toxin
Spinal muscular atrophy
Familial ALS
Drooling - Propantheline or
Amitriptyline
Progressive muscular atrophy
Riluzole (sodium channel blocker)
7.
Motor neuron diseaseSpinal muscular atrophy
Amyotrophic lateral sclerosis
(Gehrig disease)
Most common
Affects lower motor neuron
Affects both upper and lower
motor neurons
Autosomal recessive inheritance
Clinical features: spastic paralysis,
overactive reflexes in lower limbs;
flaccid paralysis, reduced reflexes
in upper limbs; tongue twitching
In the later stage: difficulty
swallowing and breathing
Spinobulbar muscular atrophy
Strikes in adulthood
Affects mostly men
Early symptoms: tremor, lower limb
weakness, tongue twitching
Late symptoms: widespread
muscle weakness and wasting
8.
9.
10.
Movement disordersParkinson’s disease
The classic quintet of PD
1. tremor (at rest)
2. rigidity
3. bradykinesia
4. postural instability
5. gait freezing
≥2 signs = Parkinson disease
11.
Parkinson’s diseaseLevodopa + Carbidopa
Add more dopamine to brain
MAO Inhibiter Type B
Don’t take with: MAO-Binhibitors,
vitamins B6, protein food
Ropinirole
Dopamine agonist
SE: drowsiness
Amantadine
Stimulate dopaminergic activity in
CNS
Anticholinergic
Not for patient’s with Glaucoma
Don’t quit taking suddenly
Increase dopamine by stopping MAO
activity
Foods with Tyramine
COMT Inhibiter
Blocks COMT enzyme
Surgery
Deep brain Stimulation
12.
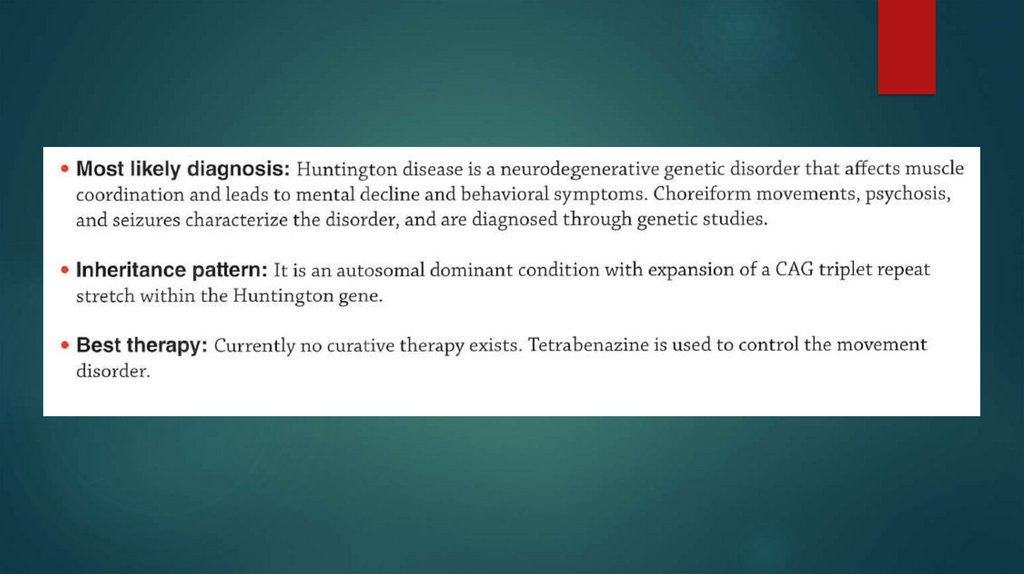
Movement disordersHuntington’s disease
Insidious onset and progression of
chorea
Onset most often between 35 and
55 years
Mental changes—change in
behavior, intellectual deterioration
leading to dementia
Motor symptoms: flicking
movements of arms, lilting gait,
facial grimacing, ataxia, dystonia
DxT chorea + abnormal behavior +
dementia + family
Treatment
There is no cure or specific
treatment
Supportive treatment with agents
such as haloperidol
13.
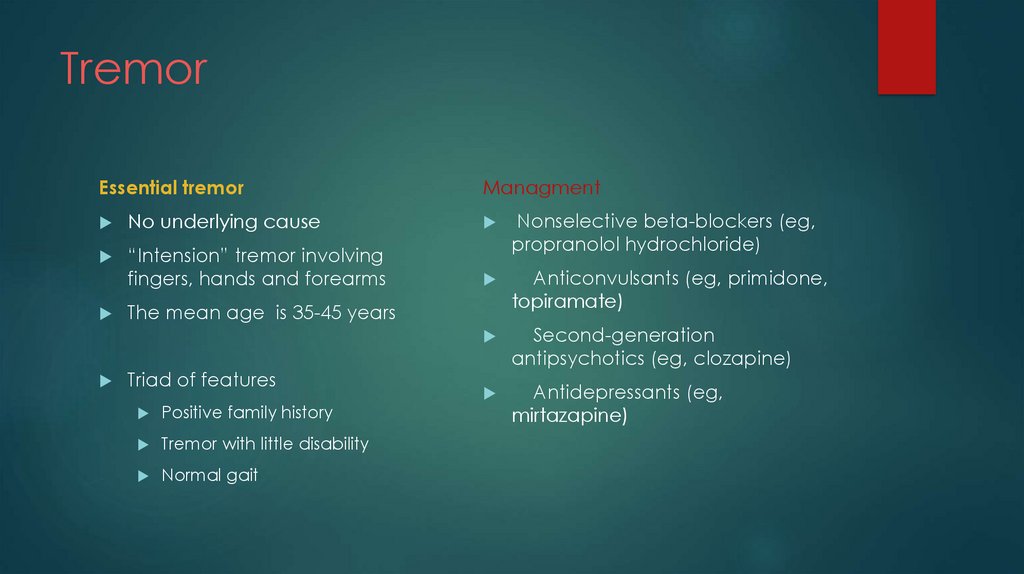
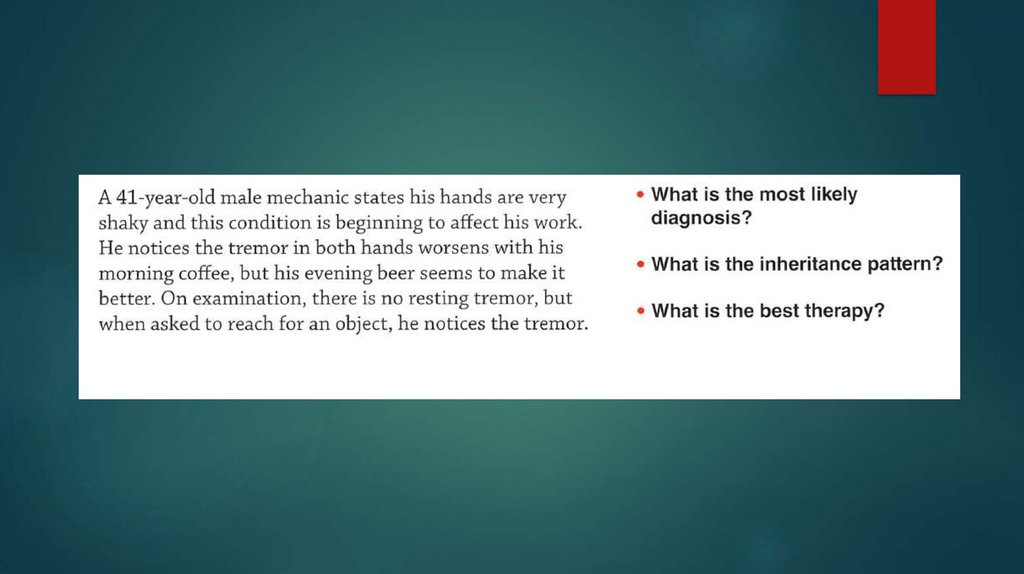
TremorEssential tremor
Managment
No underlying cause
“Intension” tremor involving
fingers, hands and forearms
Nonselective beta-blockers (eg,
propranolol hydrochloride)
Anticonvulsants (eg, primidone,
topiramate)
Second-generation
antipsychotics (eg, clozapine)
Antidepressants (eg,
mirtazapine)
The mean age is 35-45 years
Triad of features
Positive family history
Tremor with little disability
Normal gait













 Медицина
Медицина








