Похожие презентации:
Cardiologу
1.
CARDIOLOGYScientia potentia est
2.
PART 1Anatomy of the heart
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
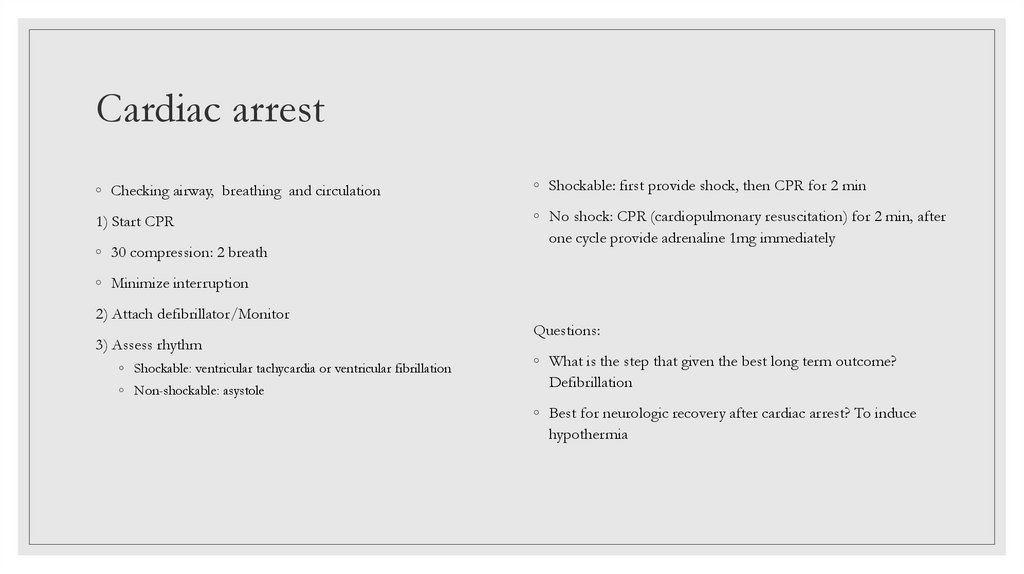
Cardiac arrest◦ Checking airway, breathing and circulation
◦ Shockable: first provide shock, then CPR for 2 min
1) Start CPR
◦ No shock: CPR (cardiopulmonary resuscitation) for 2 min, after
one cycle provide adrenaline 1mg immediately
◦ 30 compression: 2 breath
◦ Minimize interruption
2) Attach defibrillator/Monitor
3) Assess rhythm
◦ Shockable: ventricular tachycardia or ventricular fibrillation
◦ Non-shockable: asystole
Questions:
◦ What is the step that given the best long term outcome?
Defibrillation
◦ Best for neurologic recovery after cardiac arrest? To induce
hypothermia
16.
PART 2Electrically conductive disorders
17.
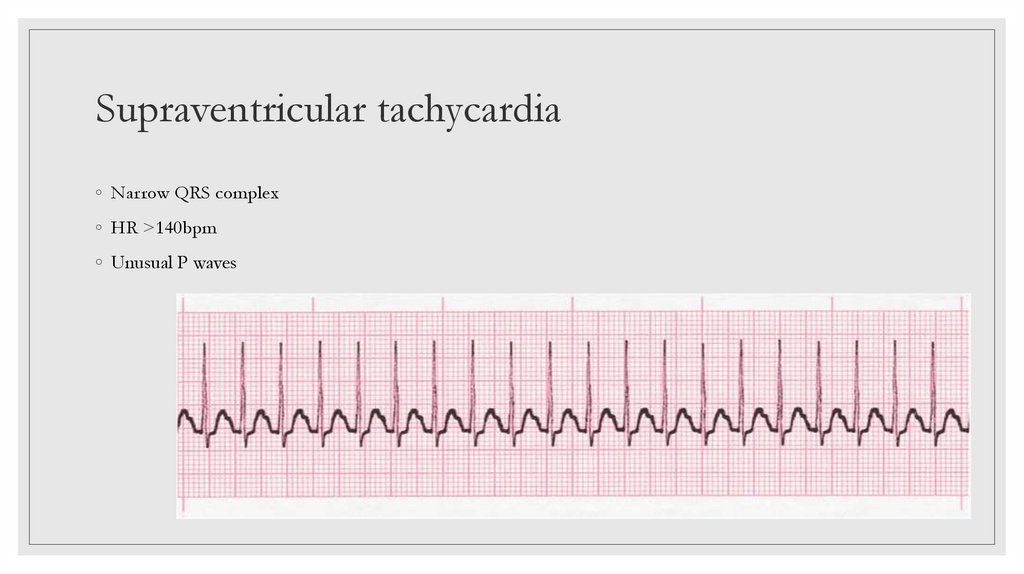
Supraventricular tachycardia◦ Narrow QRS complex
◦ HR >140bpm
◦ Unusual P waves
18.
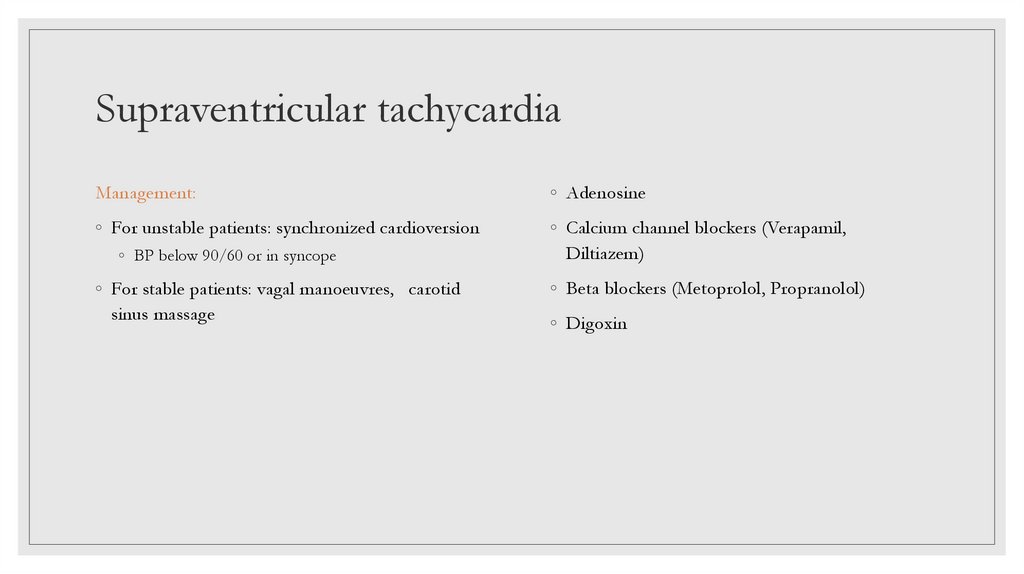
Supraventricular tachycardiaManagement:
◦ Adenosine
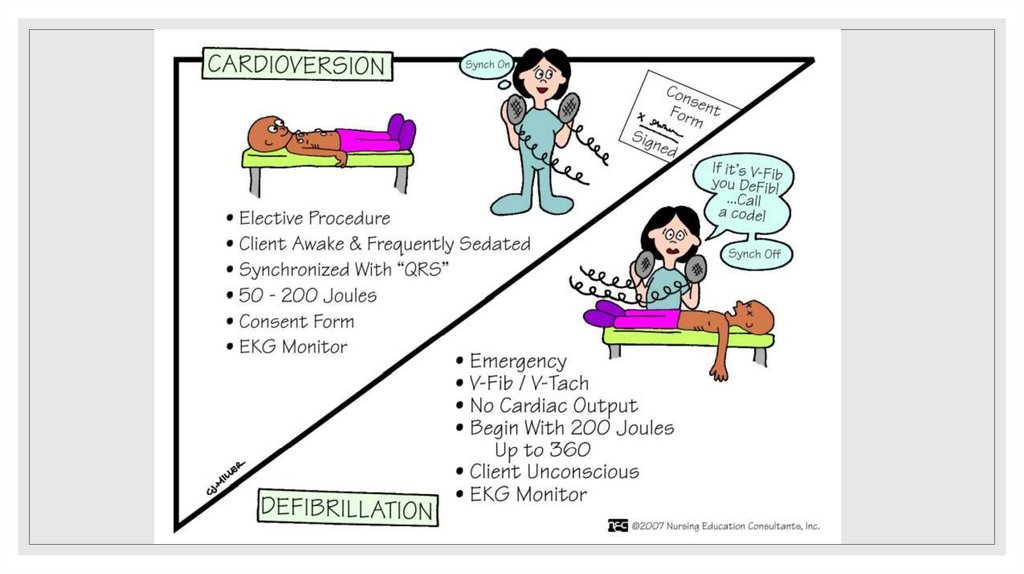
◦ For unstable patients: synchronized cardioversion
◦ Calcium channel blockers (Verapamil,
Diltiazem)
◦ BP below 90/60 or in syncope
◦ For stable patients: vagal manoeuvres, carotid
sinus massage
◦ Beta blockers (Metoprolol, Propranolol)
◦ Digoxin
19.
20.
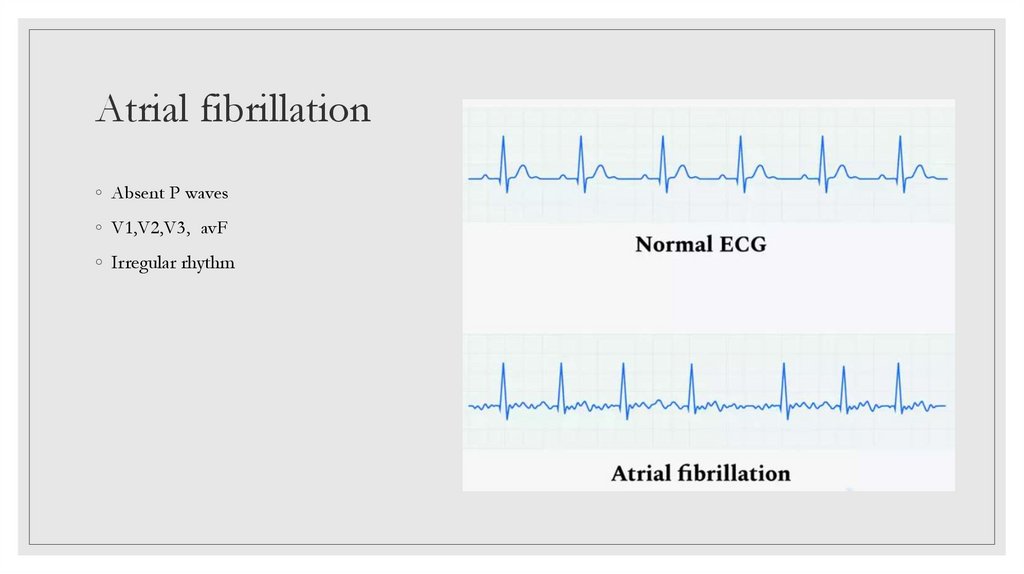
Atrial fibrillation◦ Absent P waves
◦ V1,V2,V3, avF
◦ Irregular rhythm
21.
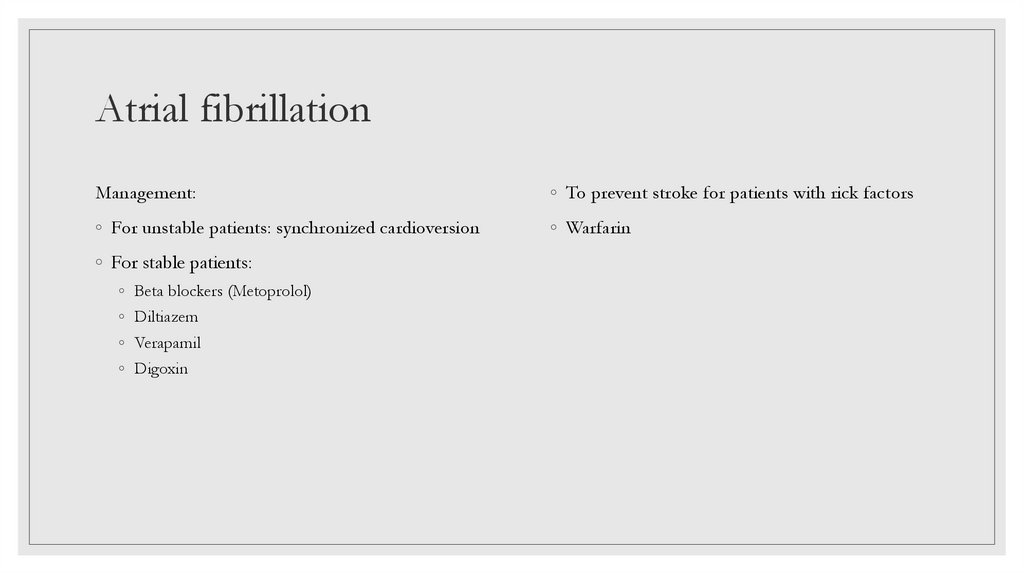
Atrial fibrillationManagement:
◦ To prevent stroke for patients with rick factors
◦ For unstable patients: synchronized cardioversion
◦ Warfarin
◦ For stable patients:
◦ Beta blockers (Metoprolol)
◦ Diltiazem
◦ Verapamil
◦ Digoxin
22.
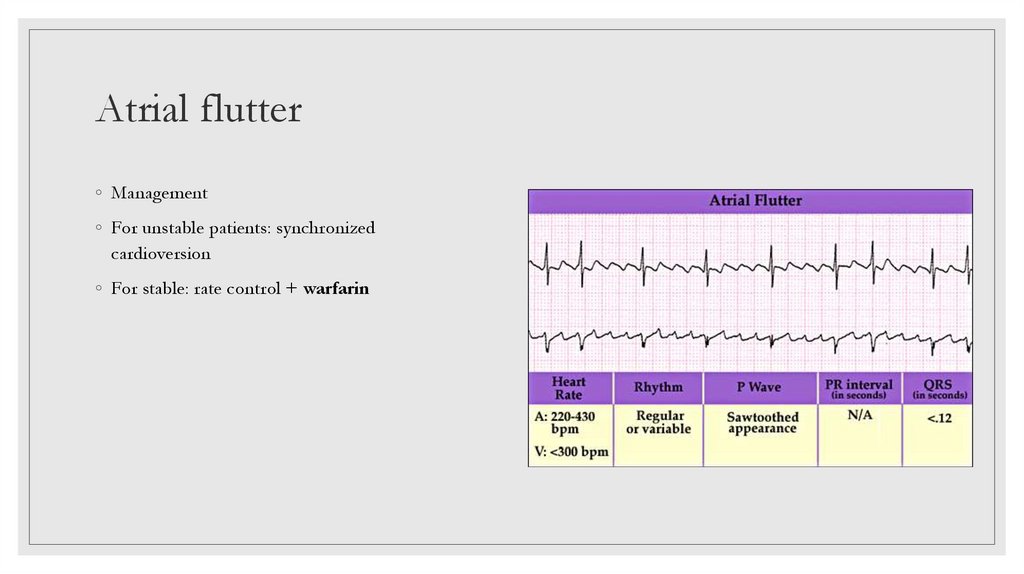
Atrial flutter◦ Management
◦ For unstable patients: synchronized
cardioversion
◦ For stable: rate control + warfarin
23.
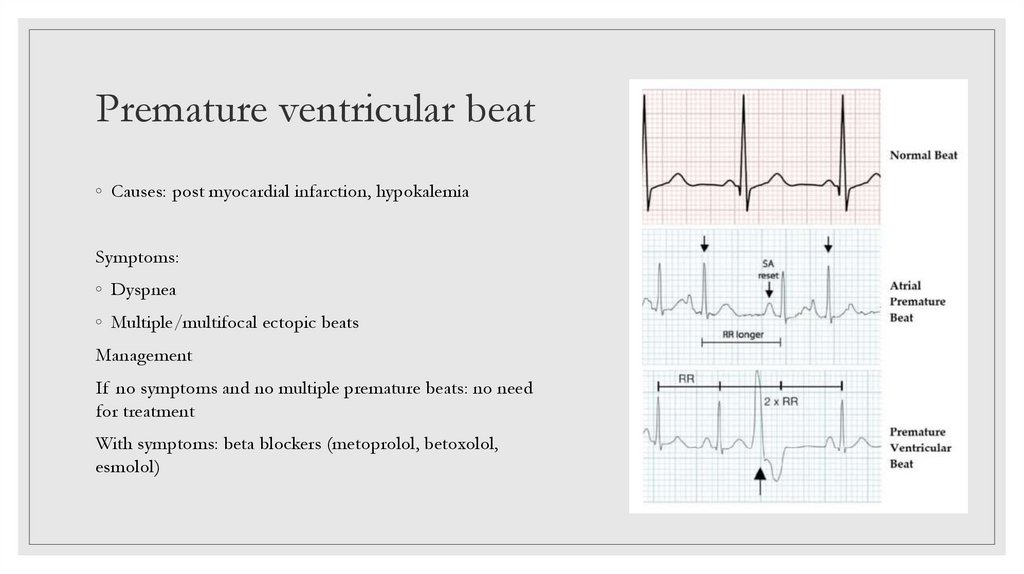
Premature ventricular beat◦ Causes: post myocardial infarction, hypokalemia
Symptoms:
◦ Dyspnea
◦ Multiple/multifocal ectopic beats
Management
If no symptoms and no multiple premature beats: no need
for treatment
With symptoms: beta blockers (metoprolol, betoxolol,
esmolol)
24.
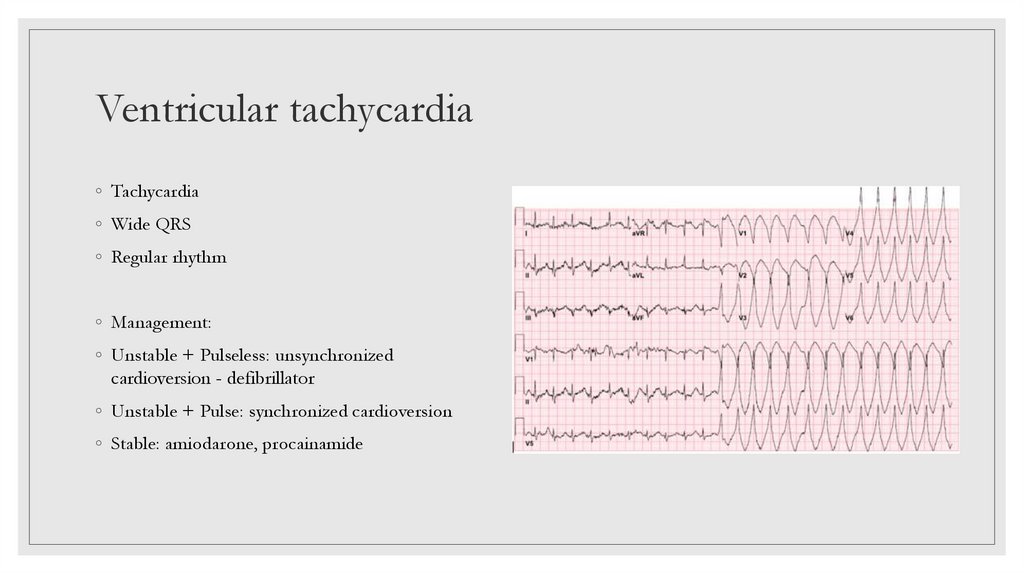
Ventricular tachycardia◦ Tachycardia
◦ Wide QRS
◦ Regular rhythm
◦ Management:
◦ Unstable + Pulseless: unsynchronized
cardioversion - defibrillator
◦ Unstable + Pulse: synchronized cardioversion
◦ Stable: amiodarone, procainamide
25.
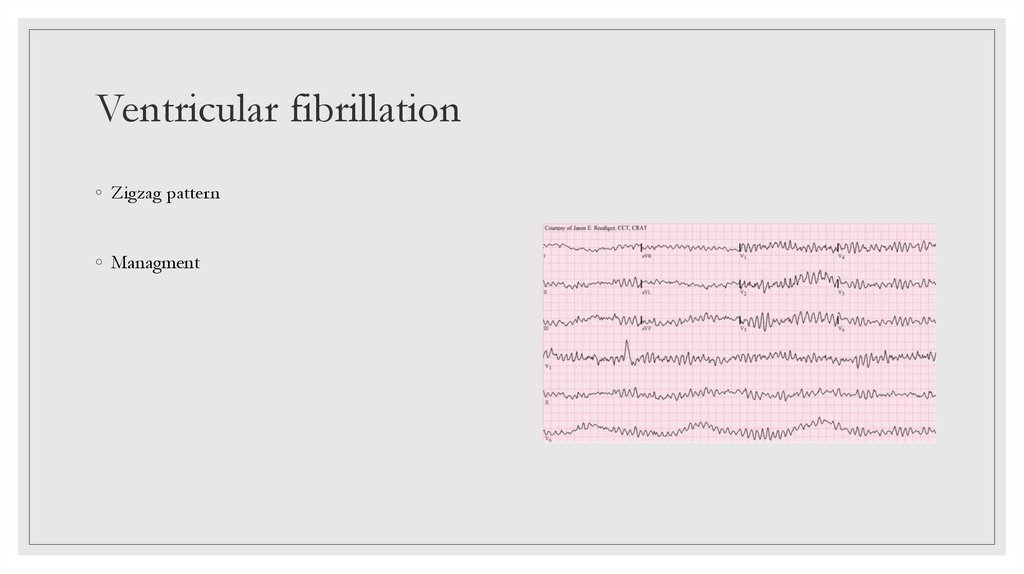
Ventricular fibrillation◦ Zigzag pattern
◦ Managment
26.
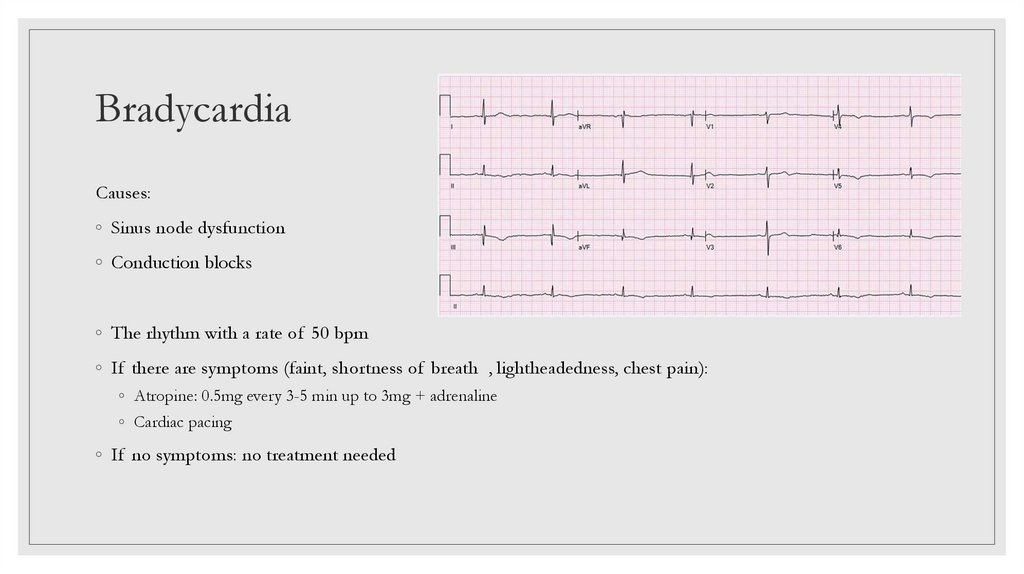
BradycardiaCauses:
◦ Sinus node dysfunction
◦ Conduction blocks
◦ The rhythm with a rate of 50 bpm
◦ If there are symptoms (faint, shortness of breath , lightheadedness, chest pain):
◦ Atropine: 0.5mg every 3-5 min up to 3mg + adrenaline
◦ Cardiac pacing
◦ If no symptoms: no treatment needed
27.
Wolff Parkinson-white syndrome◦ Short PR interval <12 sec
◦ Wide QRS
◦ Delta wave
◦ Management
◦ Unstable patient: cardioversion
◦ Stable: Amiodarone, Procainamide, Esmolol
◦ WPW+SVT: Adenosine
◦ WPW+AF: Amiodarone, Procainamide
◦ Best treatment: Catheter ablation
◦ Newer prescribe: digoxin and verapamile
28.
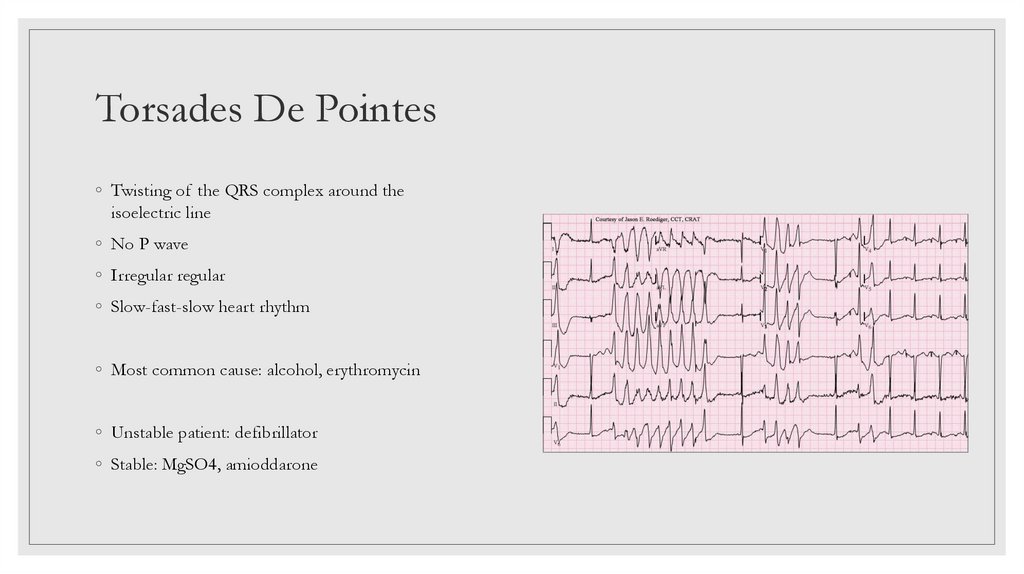
Torsades De Pointes◦ Twisting of the QRS complex around the
isoelectric line
◦ No P wave
◦ Irregular regular
◦ Slow-fast-slow heart rhythm
◦ Most common cause: alcohol, erythromycin
◦ Unstable patient: defibrillator
◦ Stable: MgSO4, amioddarone
29.
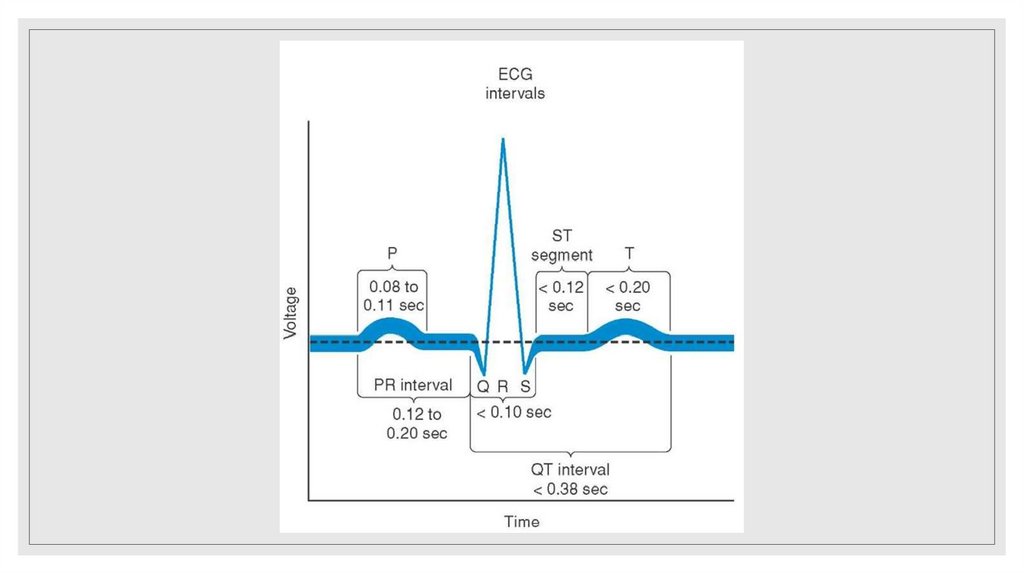
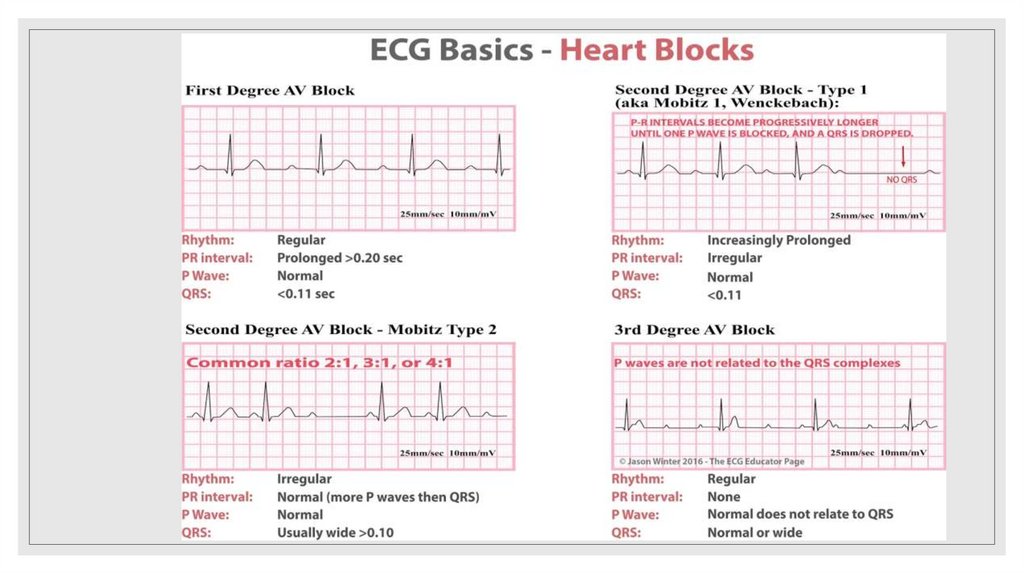
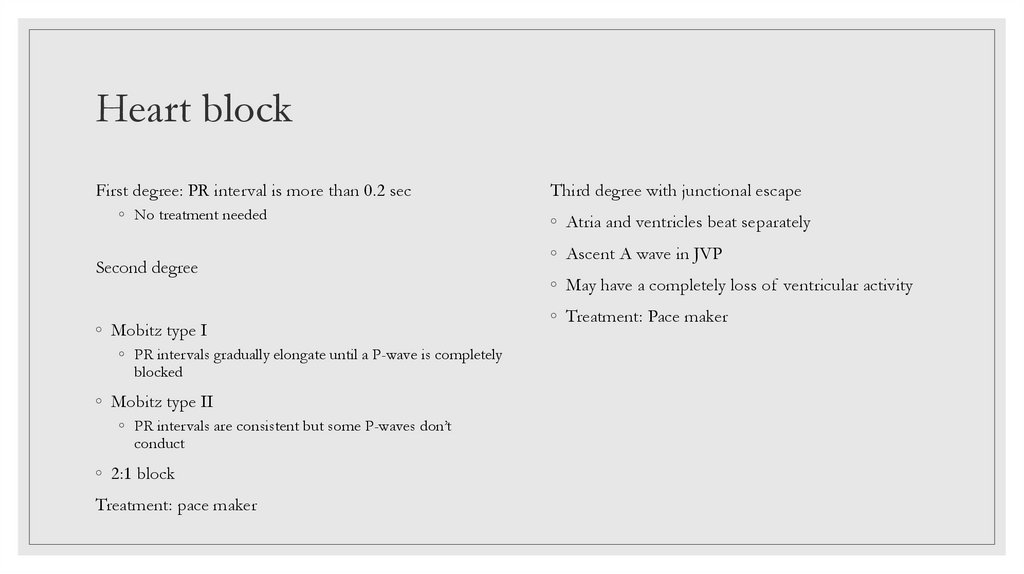
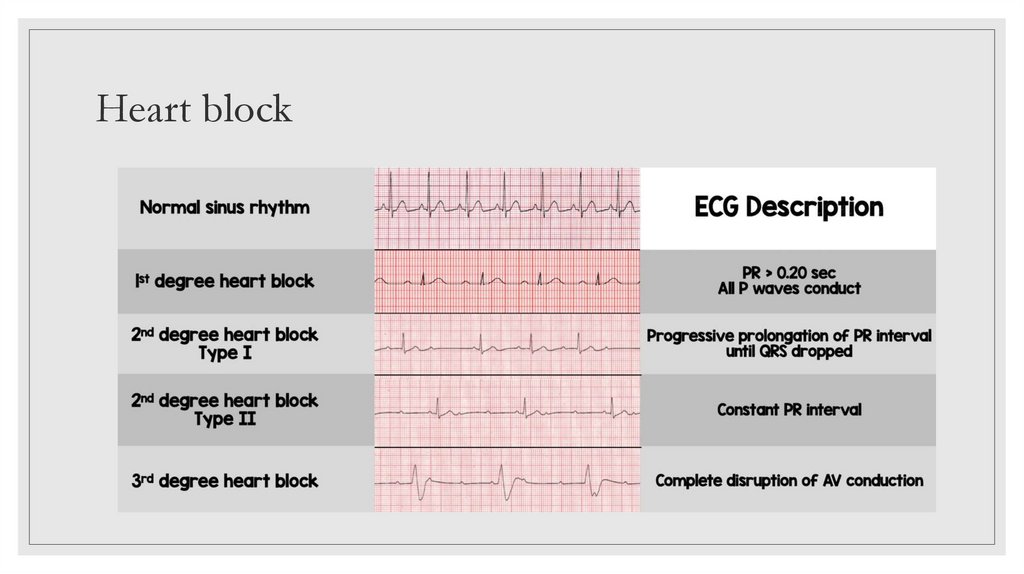
Heart blockFirst degree: PR interval is more than 0.2 sec
◦ No treatment needed
Second degree
◦ Mobitz type I
◦ PR intervals gradually elongate until a P-wave is completely
blocked
◦ Mobitz type II
◦ PR intervals are consistent but some P-waves don’t
conduct
◦ 2:1 block
Treatment: pace maker
Third degree with junctional escape
◦ Atria and ventricles beat separately
◦ Ascent A wave in JVP
◦ May have a completely loss of ventricular activity
◦ Treatment: Pace maker
30.
Heart block31.
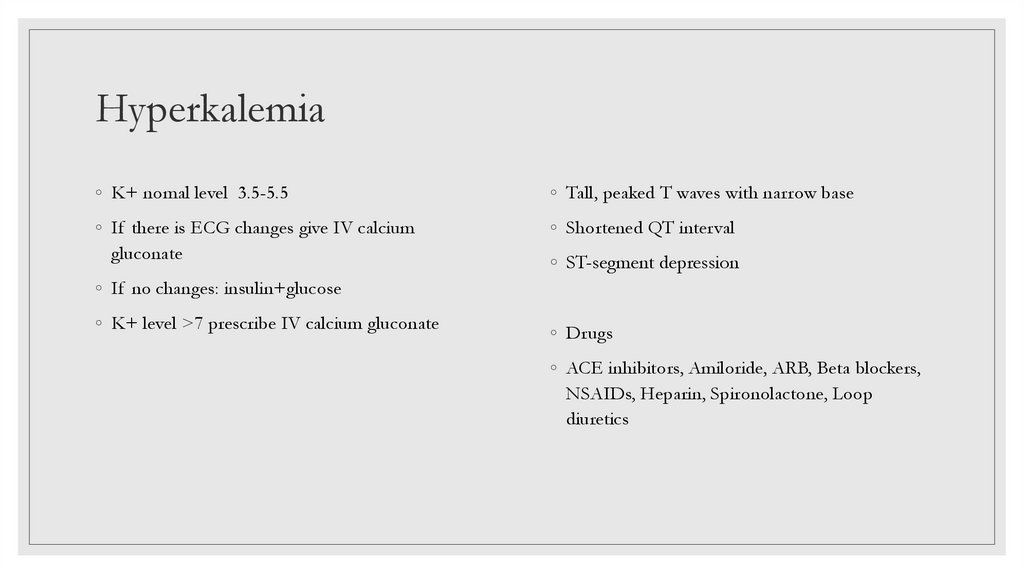
Hyperkalemia◦ K+ nomal level 3.5-5.5
◦ Tall, peaked T waves with narrow base
◦ If there is ECG changes give IV calcium
gluconate
◦ Shortened QT interval
◦ ST-segment depression
◦ If no changes: insulin+glucose
◦ K+ level >7 prescribe IV calcium gluconate
◦ Drugs
◦ ACE inhibitors, Amiloride, ARB, Beta blockers,
NSAIDs, Heparin, Spironolactone, Loop
diuretics
32.
Hypokalemia33.
LBBB◦ M shaped comlex usually in leads in V% and V6
34.
LBBB35.
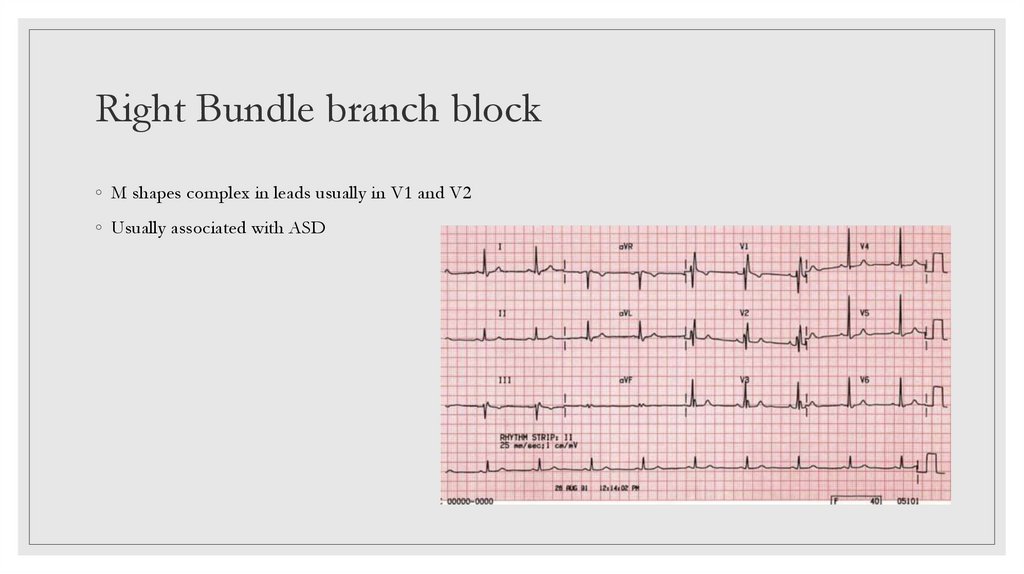
Right Bundle branch block◦ M shapes complex in leads usually in V1 and V2
◦ Usually associated with ASD
36.
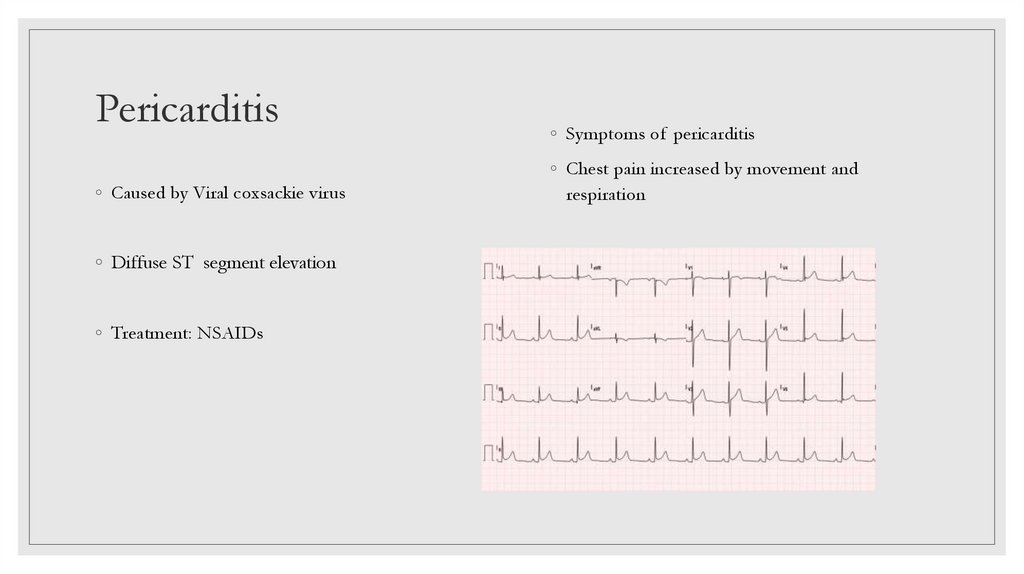
Pericarditis◦ Caused by Viral coxsackie virus
◦ Diffuse ST segment elevation
◦ Treatment: NSAIDs
◦ Symptoms of pericarditis
◦ Chest pain increased by movement and
respiration
37.
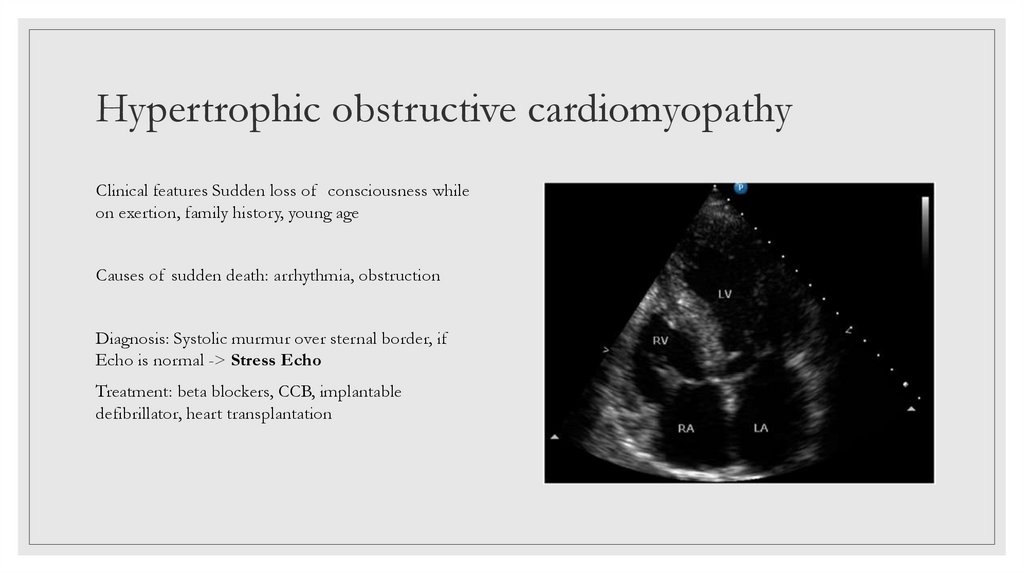
Hypertrophic obstructive cardiomyopathyClinical features Sudden loss of consciousness while
on exertion, family history, young age
Causes of sudden death: arrhythmia, obstruction
Diagnosis: Systolic murmur over sternal border, if
Echo is normal -> Stress Echo
Treatment: beta blockers, CCB, implantable
defibrillator, heart transplantation
38.
PART 339.
Abdominal aorta aneurysm◦ Clinical features:
Treatment
◦ A bulge or swelling in the aorta
◦ Dacron graft after 5 years of AAA
◦ Family history
◦ Endovascular graft
◦ May be asymptomatic, abdominal discomfort,
pulsatile mass
◦ Normal 10-30mm
◦ Emergency situation >30 mm
◦ Rupture of AAA: abdominal pain+ pale+
shocked +/- back pain
40.
Aortic dissection◦ Symptoms: severe, sudden, midline tearing or
rippig sensation
◦ Occlusion of the coronary or kidney arteries
◦ Diagnosis: X-ray and CT scan
41.
Superior vena cava syndrome◦ Caused by: external compression or thrombosis
◦ Malignant mediastinal tumour
◦ Bronchogenic carcinoma
◦ Non-Hodgkin lymphoma
◦ Mediastinal fibrosis
◦ Vascular diseases
◦ Infections
◦ Teratoma, cystic hygroma
◦ Pericarditis, atrial myxoma
◦ Thrombosis due to central vein catheter
◦ Clinical features: dyspnoea, facial swelling, head
fullness, cough, arm swelling, chest pain,
dysphagia, orthopnea, distorted vision,
hoarseness, stridor, pleural effusion
42.
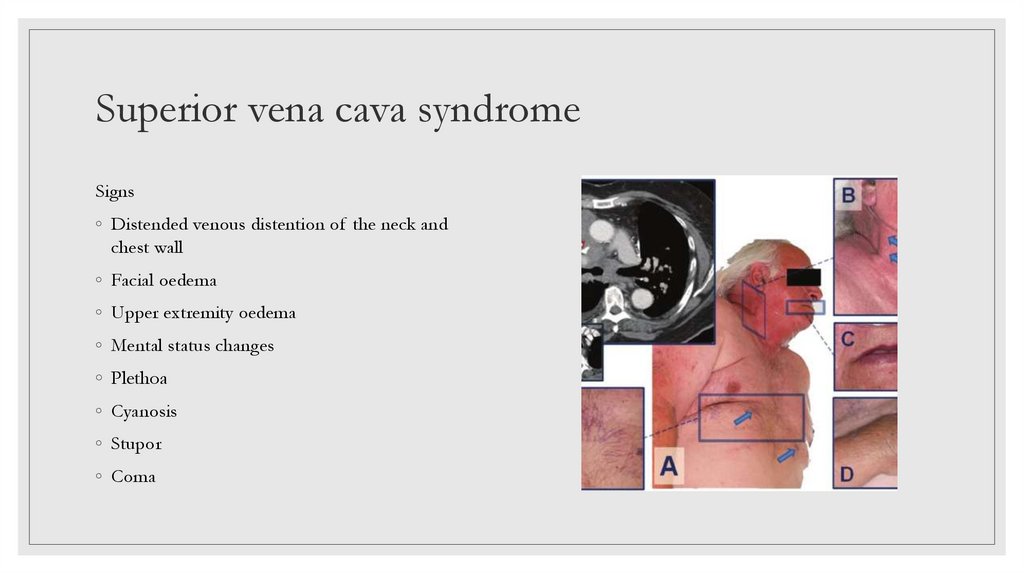
Superior vena cava syndromeSigns
◦ Distended venous distention of the neck and
chest wall
◦ Facial oedema
◦ Upper extremity oedema
◦ Mental status changes
◦ Plethoa
◦ Cyanosis
◦ Stupor
◦ Coma
43.
Superior vena cava syndrome44.
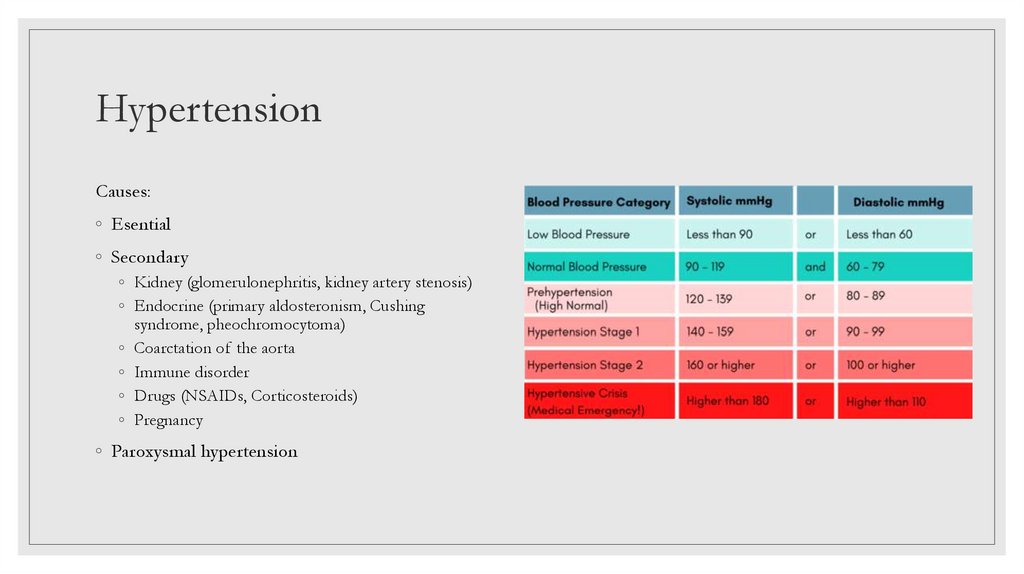
HypertensionCauses:
◦ Esential
◦ Secondary
◦ Kidney (glomerulonephritis, kidney artery stenosis)
◦ Endocrine (primary aldosteronism, Cushing
syndrome, pheochromocytoma)
◦ Coarctation of the aorta
◦ Immune disorder
◦ Drugs (NSAIDs, Corticosteroids)
◦ Pregnancy
◦ Paroxysmal hypertension
45.
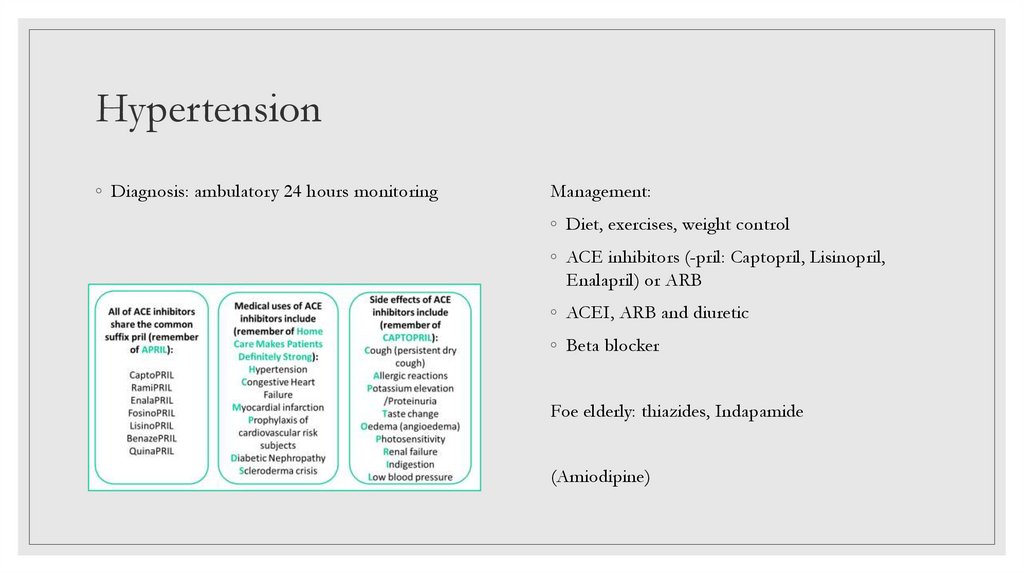
Hypertension◦ Diagnosis: ambulatory 24 hours monitoring
Management:
◦ Diet, exercises, weight control
◦ ACE inhibitors (-pril: Captopril, Lisinopril,
Enalapril) or ARB
◦ ACEI, ARB and diuretic
◦ Beta blocker
Foe elderly: thiazides, Indapamide
(Amiodipine)
46.
Dilated CardiomyopathyMost common causes:
Diagnosis: Echo, x-ray
◦ Alcohol, Coxsackie virus, drugs (doxorubicin,
anthracycline)
Management: ACEI and BB
Clinical features:
◦ Pedal oedema
◦ Orthopnea
◦ Dyspnea
◦ Arrhythmia
47.
PART 448.
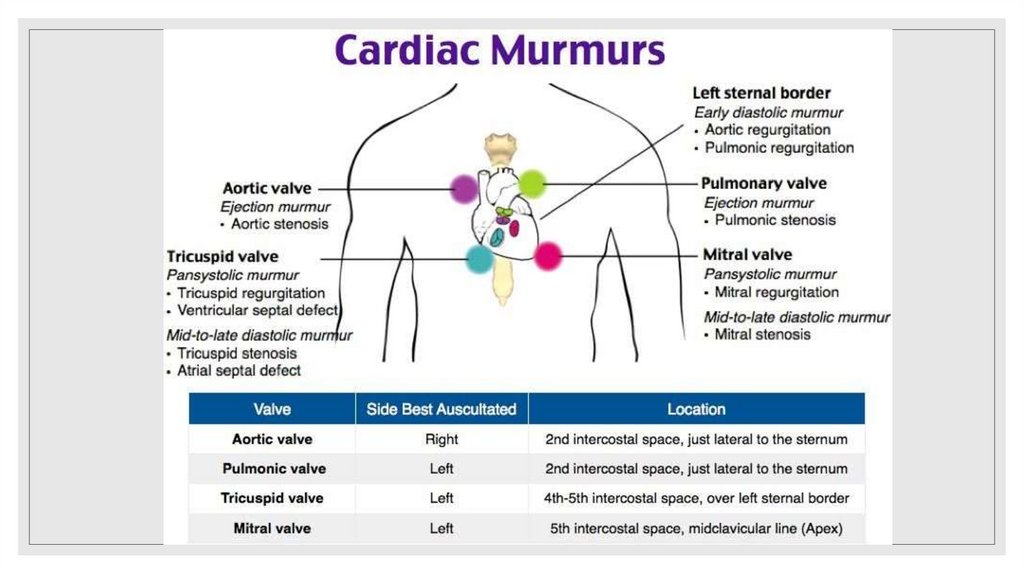
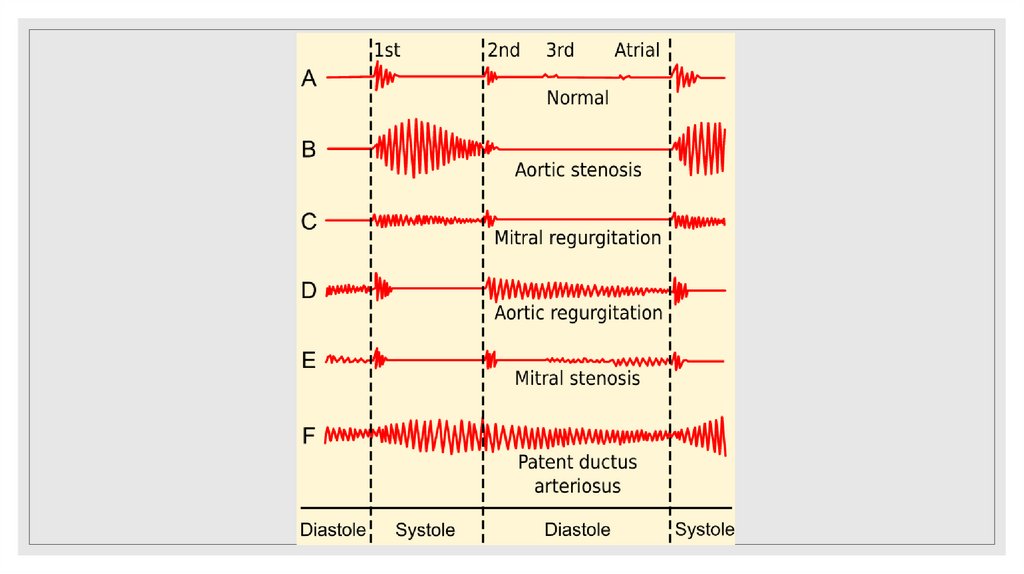
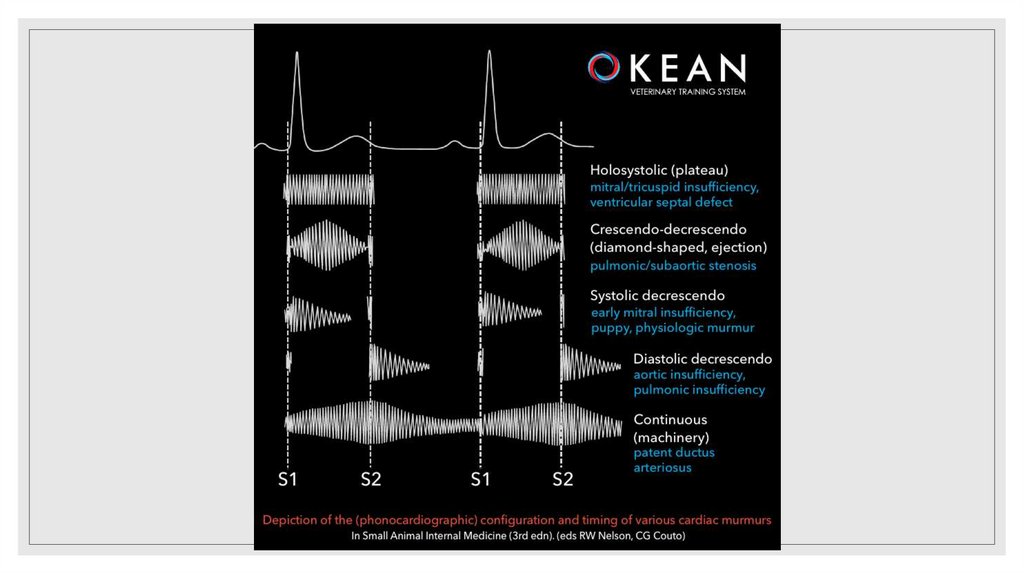
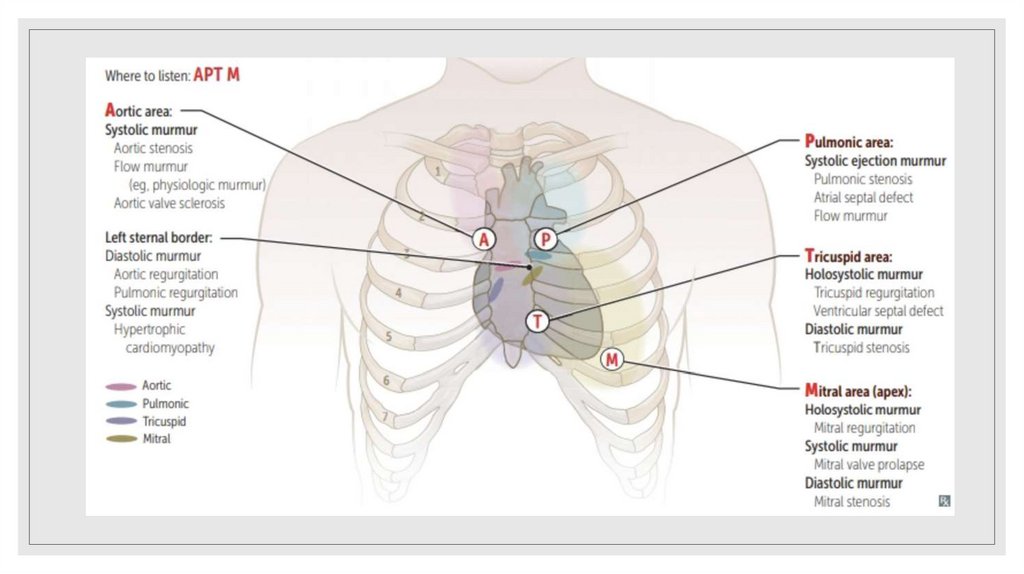
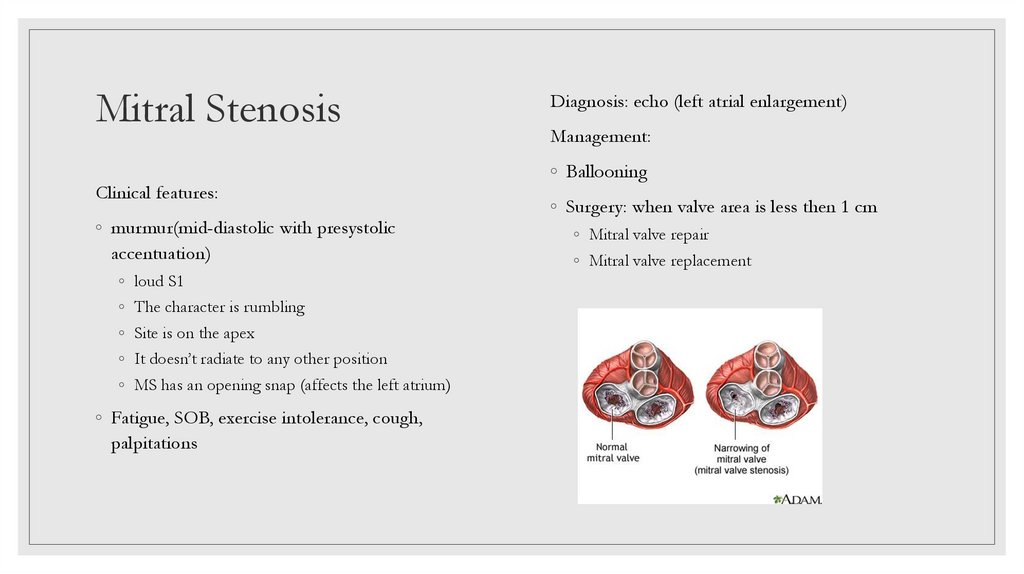
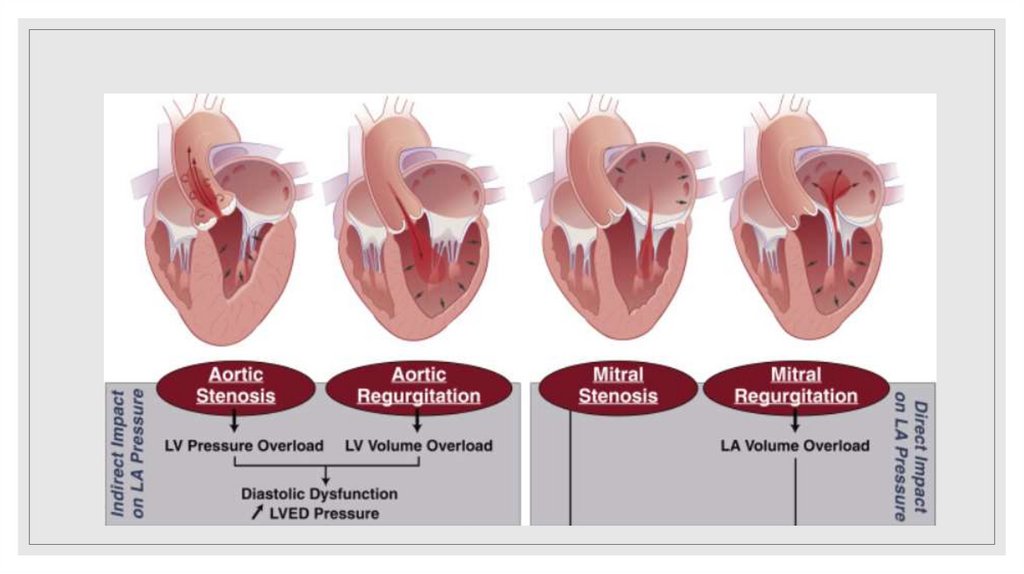
Mitral StenosisClinical features:
◦ murmur(mid-diastolic with presystolic
accentuation)
◦ loud S1
◦ The character is rumbling
◦ Site is on the apex
◦ It doesn’t radiate to any other position
◦ MS has an opening snap (affects the left atrium)
◦ Fatigue, SOB, exercise intolerance, cough,
palpitations
Diagnosis: echo (left atrial enlargement)
Management:
◦ Ballooning
◦ Surgery: when valve area is less then 1 cm
◦ Mitral valve repair
◦ Mitral valve replacement
49.
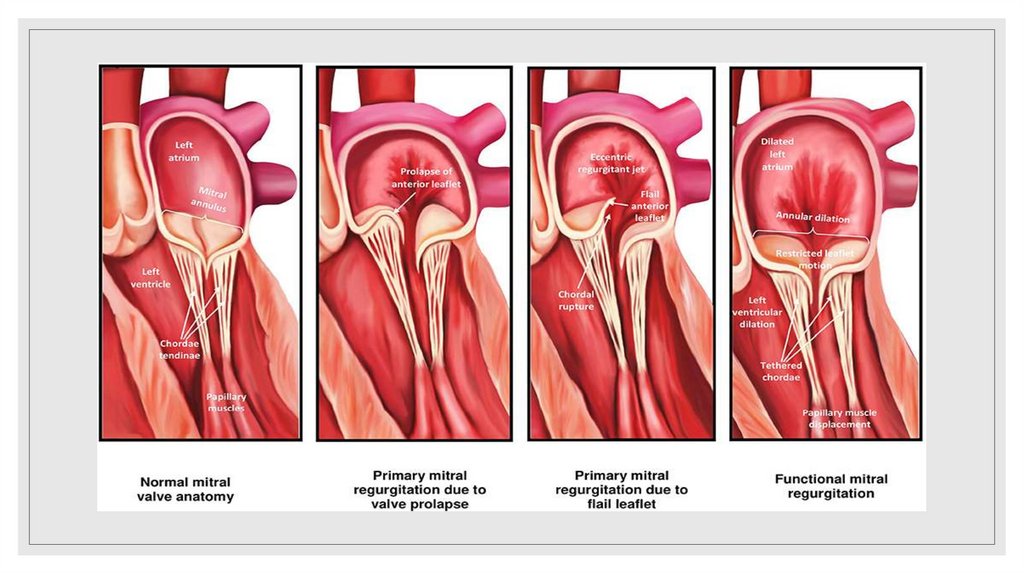
Mitral Regurgitation◦ The most common cause: mitral valve prolapse
Diagnosis: echo (left atrial enlargement)
Clinical features:
Treatment:
◦ History of Rheumatic fever
◦ Diuretics, BB
◦ Murmur
◦ Surgery : repair or replacement
◦ Pan-systolic over the apex and radiates to the axilla
◦ Acute: pulmonary edema, congestive heart failure
◦ Chronic: fatigue, pulmonary congestion/edema
50.
Mitral valve prolapseClinical features:
◦ Young females (with familial connection)
Diagnosis: echo
◦ Atypical chest pain
◦ Palpitations
Treatment: BB
◦ Hyperventilation
◦ Migranes
◦ A mid-systolic click – late systolic murmur
Causes: idiopathic, Marfan Syndrome, Ehlers Danlos
Syndrome
Complication: progression to mitral regurgitation,
certain arrhythmias, infective endocarditis,
thromboembolism
51.
52.
Aortic stenosisClinical features:
◦ Chest pain
◦ Syncope
◦ SOB
◦ Sudden death
◦ Loss of consciousness
◦ Microangiopathic hemolytic anemia
◦ Small or weak pulse
◦ Yang patients: bicuspid aortic valve; rheumatic fever
◦ Elder: calcific aortic valve
◦ Murmur:
◦ Systolic murmur over right 2nd intercostal space, radiating to
carotid
◦ Increased by leaning forward
◦ Crescendo-decrescendo murmur
Diagnosis: Echo (left ventricular hypertrophy)
Treatment:
◦ Valvuloplasty by balloon
◦ Valve replacement surgery
◦ When: patient has severe symptoms, the pressure gradient is
more then 50 mmHg, valve area less then 0.8cm
53.
Aortic regurgitationCauses by:
◦ 80% idiopatic
Clinical features: fatigue, syncope, SOB,
palpitations, widened pulse pressure
◦ Marfan Syndrome
◦ Rheumatic fever
Diagnosis: echo (left ventricular dilatation)
◦ Murmur:
Treatment: replace valve
◦ Early diastolic decrescendo over left 2nd intercostal
space radiating to the apex S2;
◦ Wide fixed
◦ Murmur is increased by leaning forward
AR is associated with: RBBB, atrial septal defect
54.
55.
Constrictive pericarditisCauses: Tb, autoimmune disorders
Diagnosis: CT
Clinical features:
Treatment: Pericardiectomy, Pericardiocentesis
◦ Systemic congestion
◦ Paradoxical increase in JVP distention and
pressure during inspiration (Kussmaul sigh)
◦ Congested Pulsated neck veins
◦ Pulsus paradoxus
Complications:
◦ Cardiac tamponade
◦ Becks triad: hypotension, increased JVP, decreased
heart sound
56.
Infective EndocarditisInfection of the cardiac valves or endometrium
Clinical feature:
Risk factors: known heart disease, history of
endocarditis, abnormal valves, mitral valve
prolapse, calcified aortic valve, congenital cardiac
defects (VSD, PDA)
◦ Fever of unknown region
◦ Cardiac murmur
Classical tetrad:
◦ Embolism
◦ Sighs of infection
◦ Signs of heart disease
◦ Signs of embolism
◦ Immunological phenomenon
57.
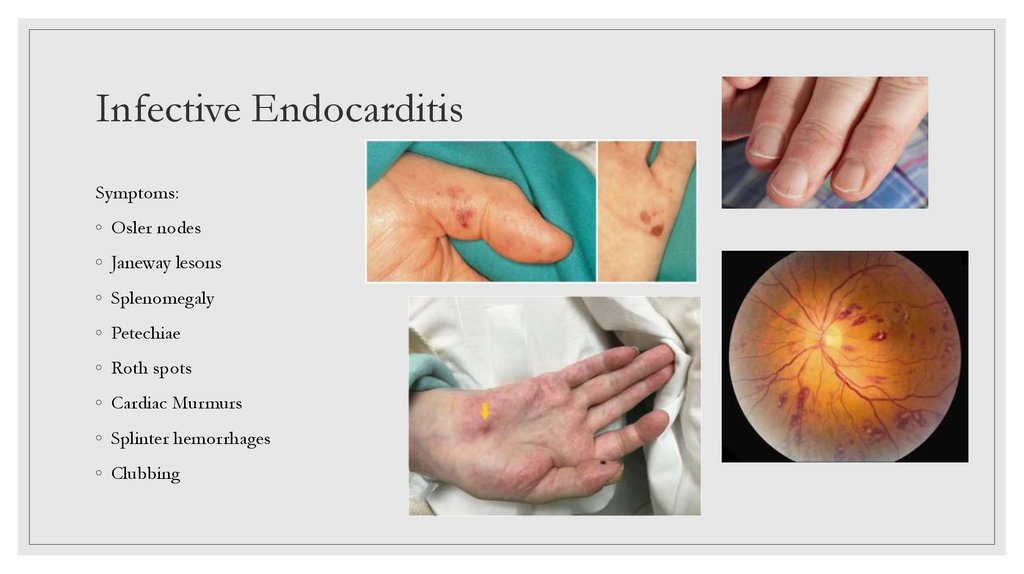
Infective EndocarditisSymptoms:
◦ Osler nodes
◦ Janeway lesons
◦ Splenomegaly
◦ Petechiae
◦ Roth spots
◦ Cardiac Murmurs
◦ Splinter hemorrhages
◦ Clubbing
58.
Infective EndocarditisDiagnosis:
◦ ERS increase, anemia and leucocytosis
◦ In urine: proteinuria and hematuria
◦ Blood culture
◦ Transesophageal echocardiography (to
visualize vegetations)
Treatment: Benzylpenicillin, Flucloxacillin,
gentamicin, vancomycin
59.
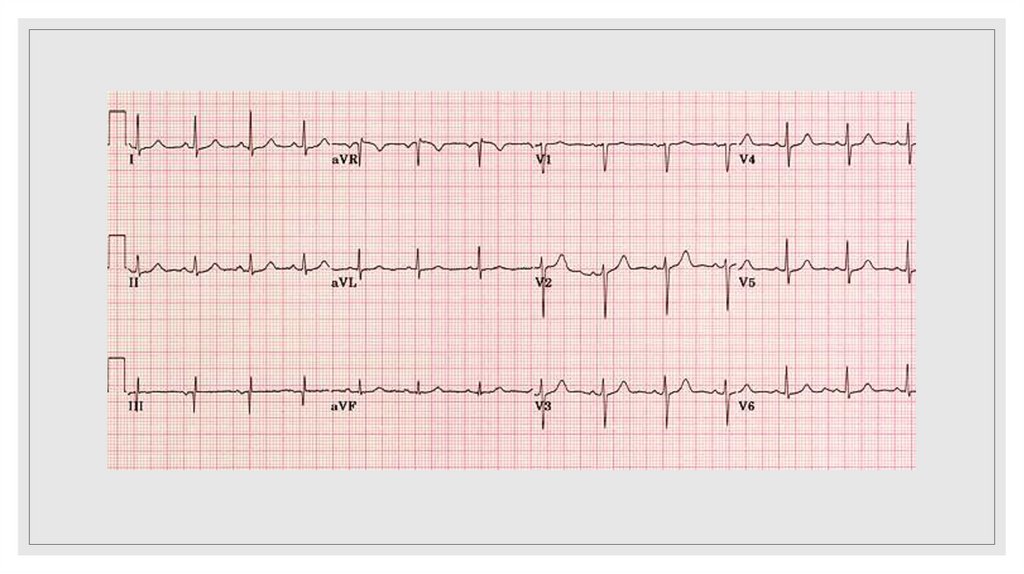
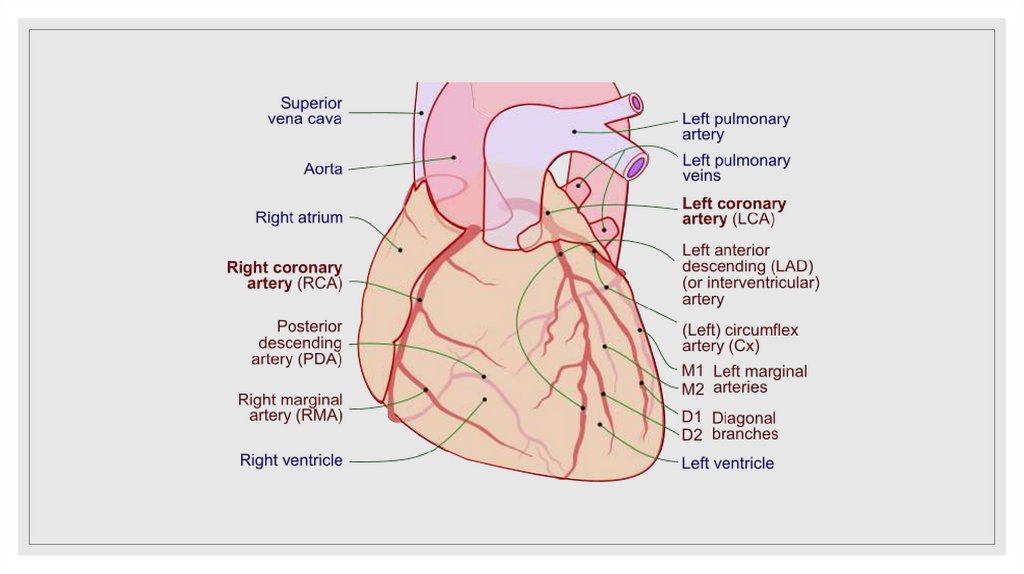
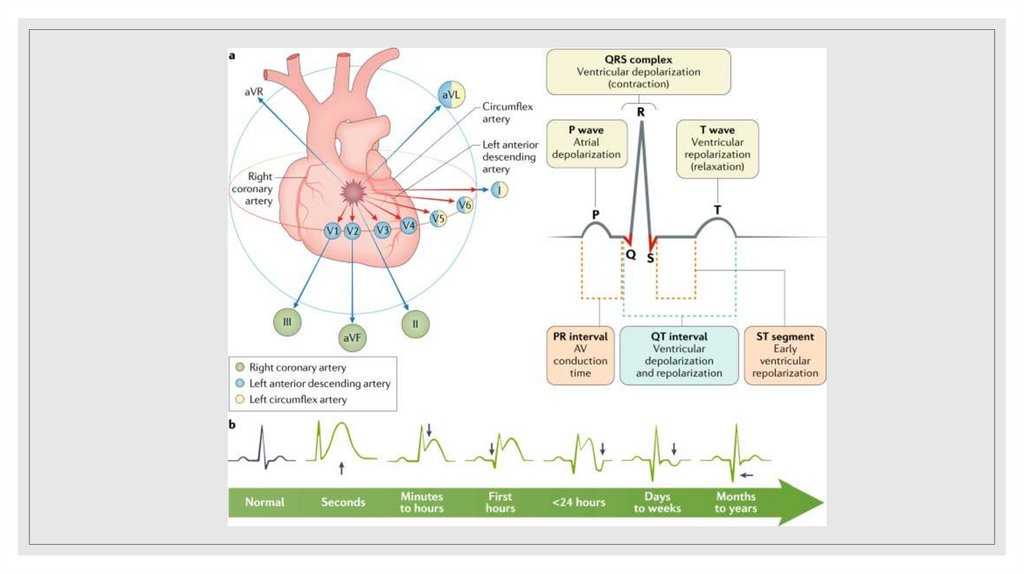
Myocardial infarctionInvestigation:
Criteria of MI:
◦ Typical ECG appearance
◦ ECG: ST segment elevation greater than 1 mm in
two contagious leads in the presence of symptoms
and development of new left bundle branch block
◦ Rise and fall of cardiac enzymes
◦ Cardial Enzymes
◦ History of prolonged ischemic pain
Causes:
◦ Thrombosis with occlusion
◦ Haemorrhage under a plaque
◦ Rupture of a plaque
◦ Coronary artery spasm
◦ Troponin I or T (start rising 3-12 hrs and reached
peak at 24 hours and persist for about 5-14 days)
◦ Creatine Kinase (it peaks at 20-24 hrs and usually
returns to normal after 48hrs)
◦ Coronary angiogram
60.
61.
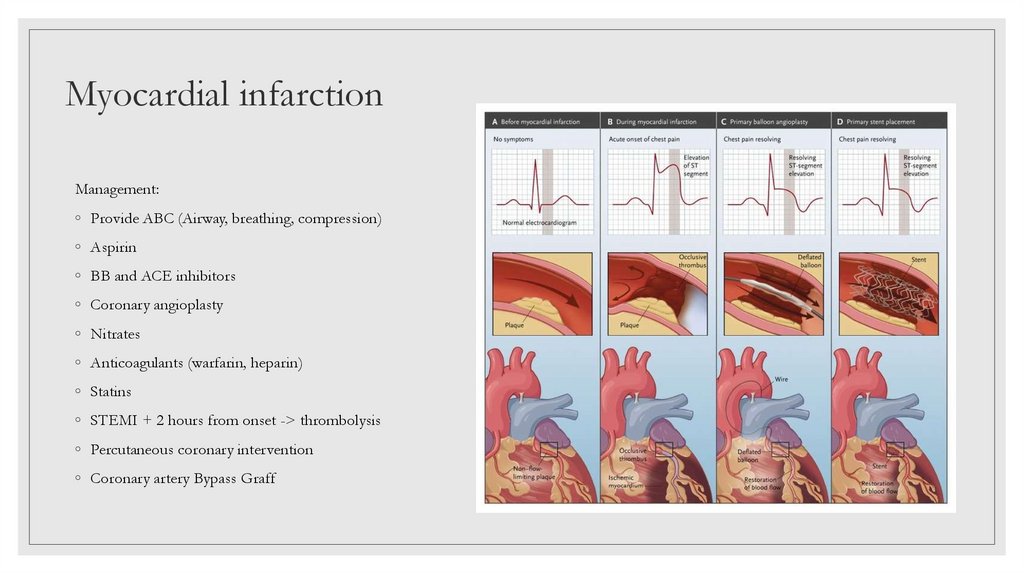
Myocardial infarctionManagement:
◦ Provide ABC (Airway, breathing, compression)
◦ Aspirin
◦ BB and ACE inhibitors
◦ Coronary angioplasty
◦ Nitrates
◦ Anticoagulants (warfarin, heparin)
◦ Statins
◦ STEMI + 2 hours from onset -> thrombolysis
◦ Percutaneous coronary intervention
◦ Coronary artery Bypass Graff
62.
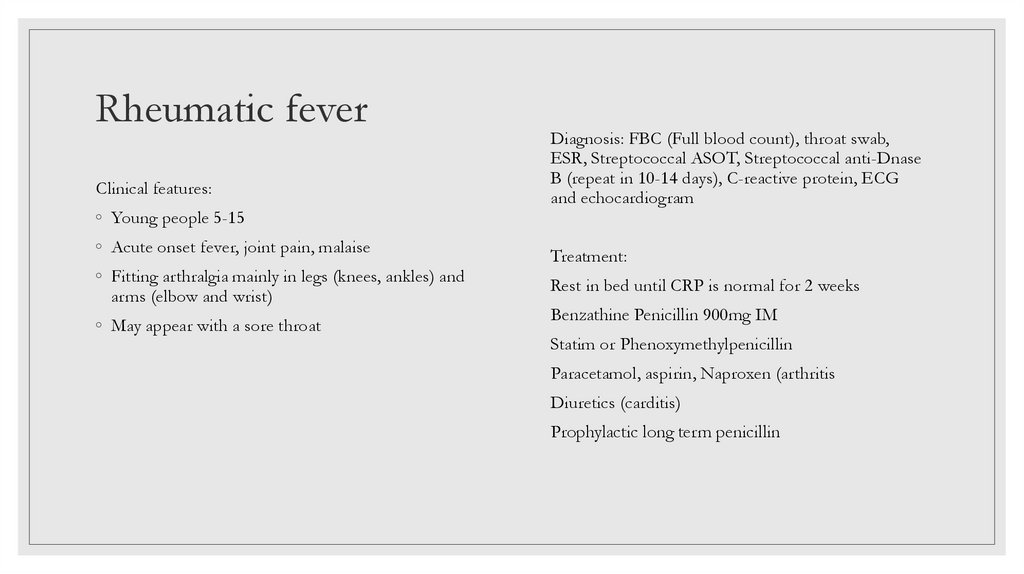
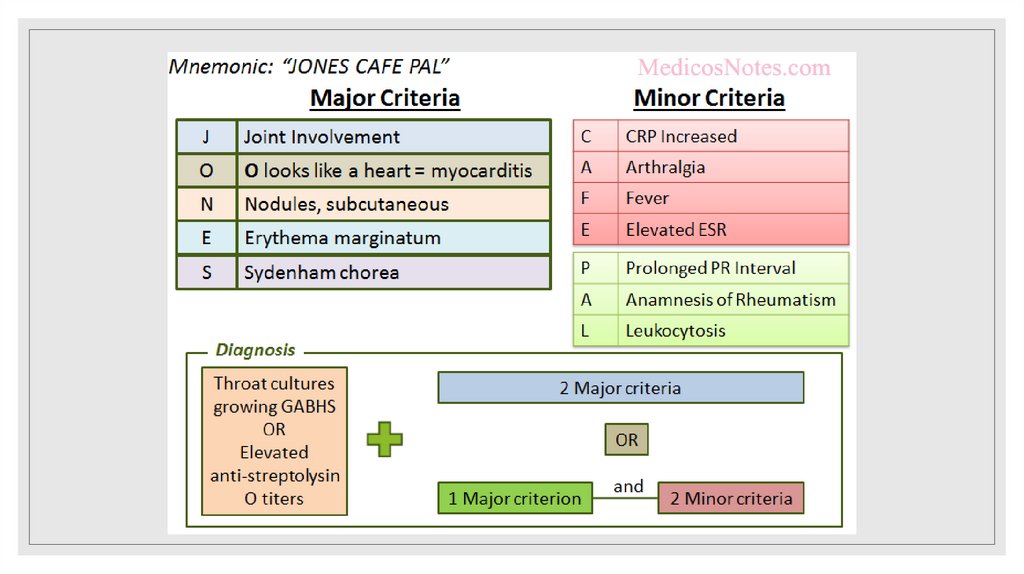
Rheumatic feverClinical features:
◦ Young people 5-15
◦ Acute onset fever, joint pain, malaise
◦ Fitting arthralgia mainly in legs (knees, ankles) and
arms (elbow and wrist)
◦ May appear with a sore throat
Diagnosis: FBC (Full blood count), throat swab,
ESR, Streptococcal ASOT, Streptococcal anti-Dnase
B (repeat in 10-14 days), C-reactive protein, ECG
and echocardiogram
Treatment:
Rest in bed until CRP is normal for 2 weeks
Benzathine Penicillin 900mg IM
Statim or Phenoxymethylpenicillin
Paracetamol, aspirin, Naproxen (arthritis
Diuretics (carditis)
Prophylactic long term penicillin
63.
64.
Rheumatic fevererythema marginatum





 Медицина
Медицина