Похожие презентации:
Filariasis
1. Filariasis
The topic of the lecture:Filariasis
Professor Kutmanova A.Z.
2. History
• Pre-1876– The only known symptom of this disease was elephantiasis
because of its outward appearance.
• 600BC
– Ancient Hindu medical workers referred to elephantiasis in
Sanskrit texts.
• 600- 250BC
– Men affected by elephantiasis were not allowed to become
Buddhist priests.
• 10th- 13th Centuries
– Persian and European physicians have accurate descriptions
of elephantiasis.
• 1876
– Joseph Bancroft discovered the parasite that causes
lymphatic filariasis in an abscess on the arm of a butcher.
3.
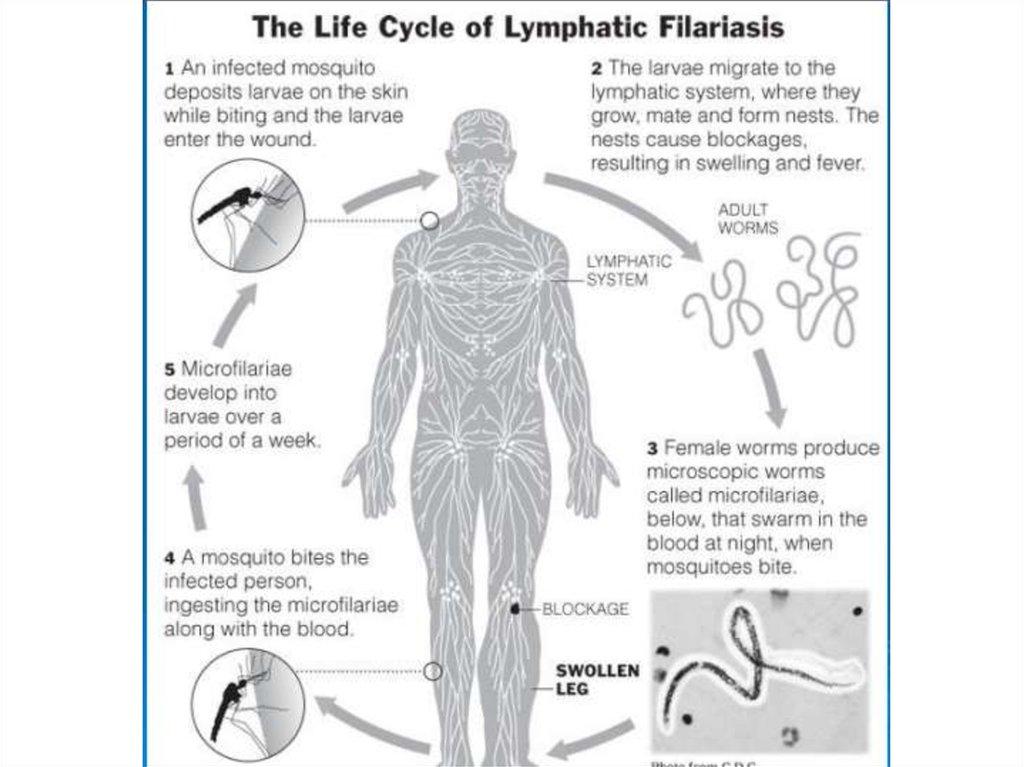
• Lymphatic filariasis, commonly known aselephantiasis, is a neglected tropical disease.
• Infection occurs when filarial parasites are
transmitted to humans through mosquitoes.
• Infection is usually acquired in childhood
causing hidden damage to the lymphatic
system.
• 856 million people in 52 countries worldwide
remain threatened by lymphatic filariasis and
require preventive chemotherapy to stop the
spread of this parasitic infection.
4.
• In 2000 over 120 million people were infected, withabout 40 million disfigured and incapacitated by the
disease.
• Lymphatic filariasis can be eliminated by stopping the
spread of infection through preventive chemotherapy
with safe medicine combinations, repeated annually for
at least 5 years.
• 6.7 billion treatments have been delivered to stop the
spread of infection since 2000.
• 499 million people no longer require preventive
chemotherapy due to successful implementation of WHO
strategies.
• A basic, recommended package of care can alleviate
suffering and prevent further disability among persons
living with disease caused by lymphatic filariasis.
5. What is Lymphatic Filariasis?
• Parasitic disease where wormsenter the blood stream
through numerous mosquito
bites over a number of years.
• Affects 120 million individuals
in over 80 countries in the
tropical regions due to
stagnant water and poor
irrigation systems
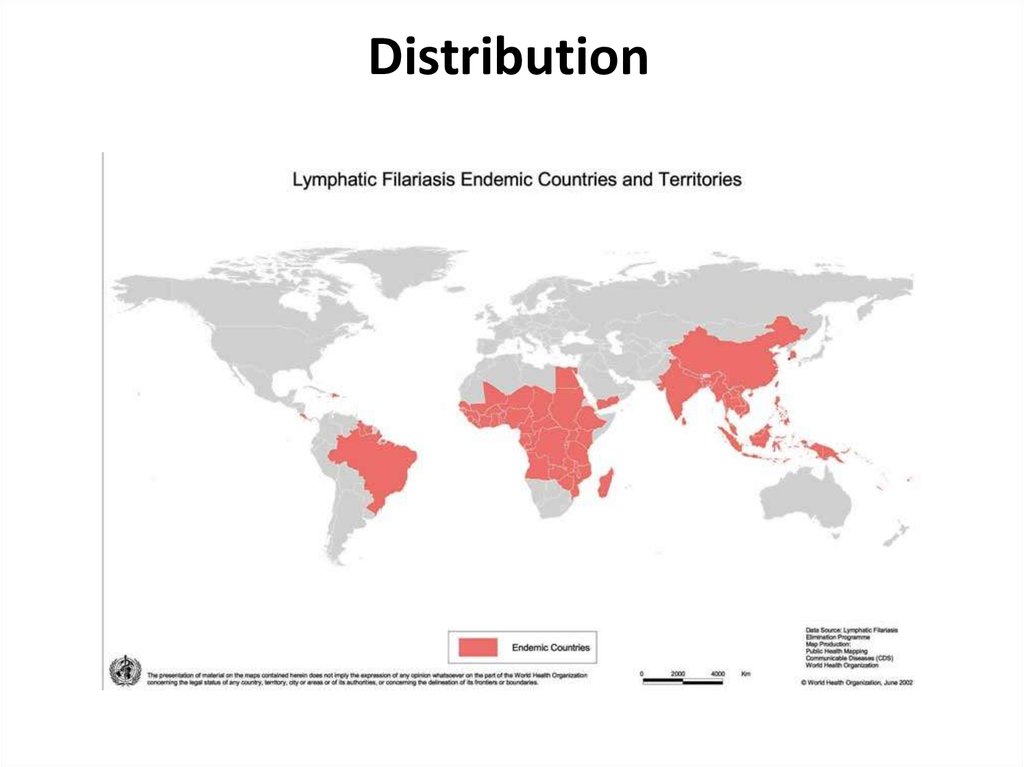
6. Distribution
7. Parasites
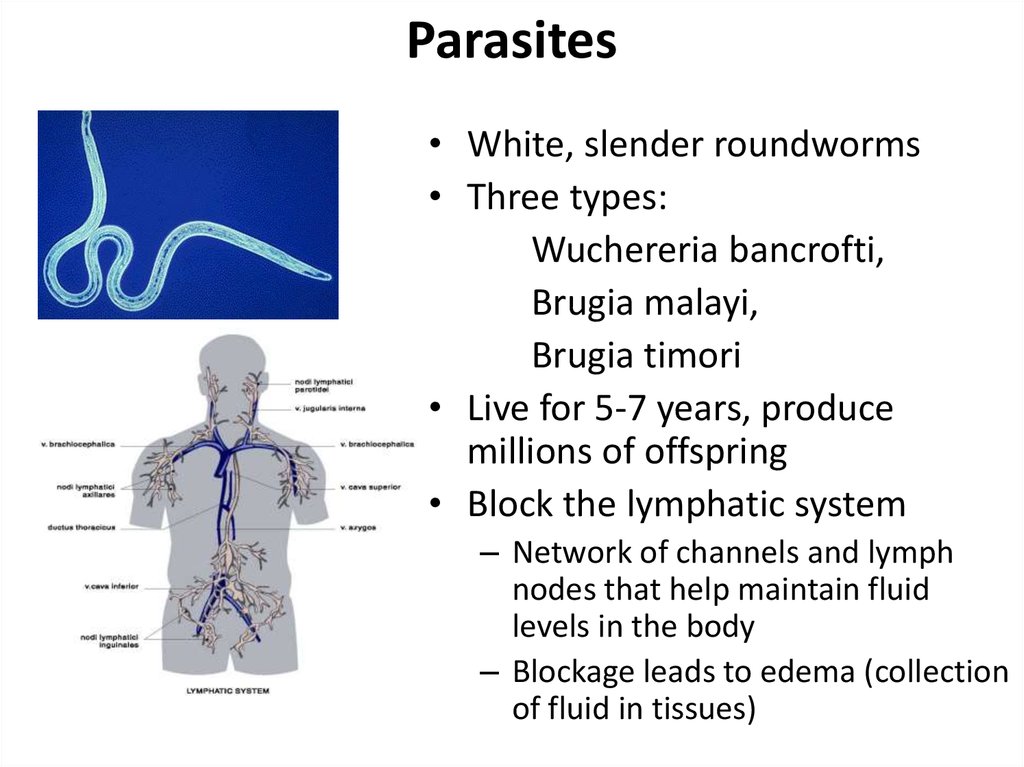
• White, slender roundworms• Three types:
Wuchereria bancrofti,
Brugia malayi,
Brugia timori
• Live for 5-7 years, produce
millions of offspring
• Block the lymphatic system
– Network of channels and lymph
nodes that help maintain fluid
levels in the body
– Blockage leads to edema (collection
of fluid in tissues)
8.
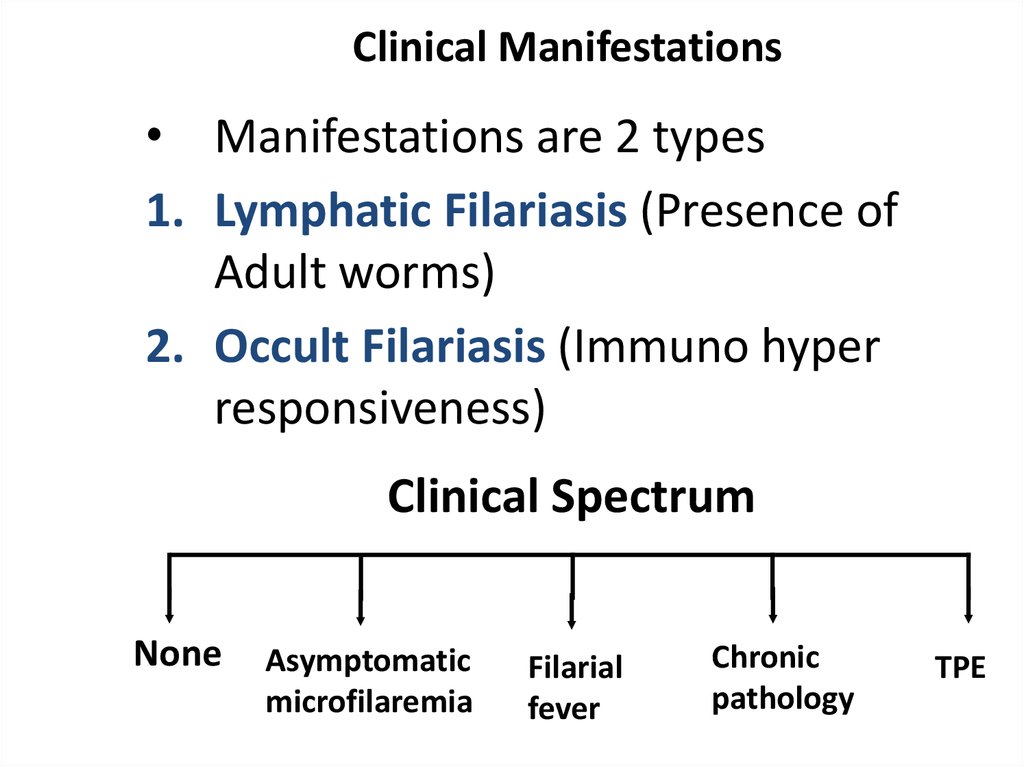
9. Clinical Manifestations
• Manifestations are 2 types1. Lymphatic Filariasis (Presence of
Adult worms)
2. Occult Filariasis (Immuno hyper
responsiveness)
Clinical Spectrum
None
Asymptomatic
microfilaremia
Filarial
fever
Chronic
pathology
TPE
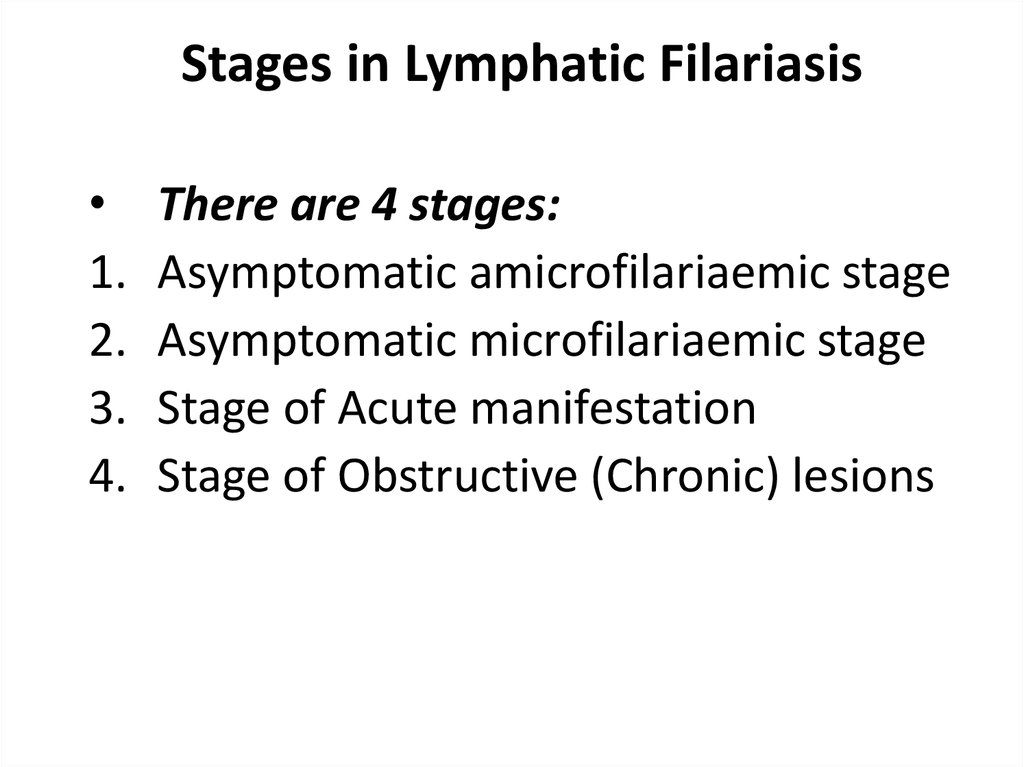
10. Stages in Lymphatic Filariasis
1.
2.
3.
4.
There are 4 stages:
Asymptomatic amicrofilariaemic stage
Asymptomatic microfilariaemic stage
Stage of Acute manifestation
Stage of Obstructive (Chronic) lesions
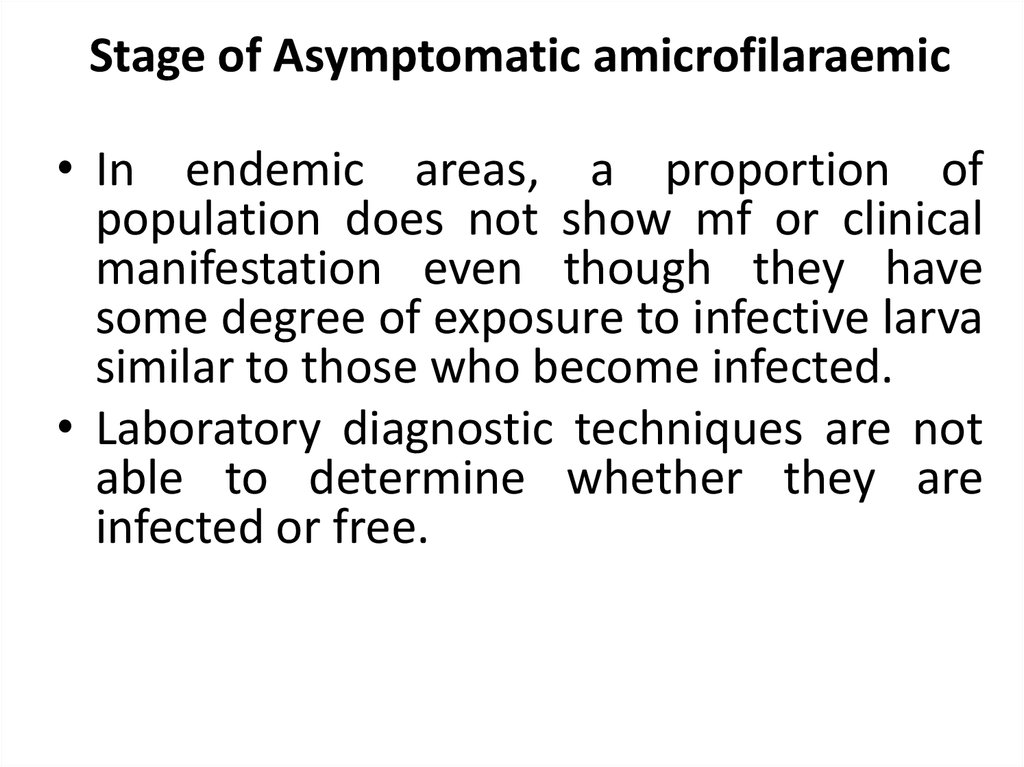
11. Stage of Asymptomatic amicrofilaraemic
• In endemic areas, a proportion ofpopulation does not show mf or clinical
manifestation even though they have
some degree of exposure to infective larva
similar to those who become infected.
• Laboratory diagnostic techniques are not
able to determine whether they are
infected or free.
12. Stage of Asymptomatic Microfilariaemic
• Considerableproportions
are
asymptomatic for months and years,
though
they
have
circulating
microfilariae.
• They are an important source of
infection.
• They can be detected by Night Blood
Survey and other suitable procedures.
13. Stage of Acute Manifestation
During initial months and years, there are
recurrent episodes of Acute inflammation in
the lymph vessel/node of the limb &
scrotum that are related to bacterial &
fungal super infections of the tissue that are
already compromised lymphatic function.
• Clinical manifestations are consisting of:
1. Filarial fever (ADL-DLA)
2. Lymphangitis
3. Lymphadinitis
4. Epididimo orchitis
14. Chronic Manifestation
Chronic (Obstructive) lesions takes 10-15 years.
This is due to the permanent damage to the lymph
vessels caused by the adult worms, the pathological
changes causing dilation of the lymph vessels due to
recurrent inflammatory episodes leading to
endothelial
proliferation
and
inflammatory
granulomnatous reaction around the parasite.
• Initially, it starts with pitting oedema which gives rise
to browny oedema leading to hardening the tissues.
Still late, hyper pigmentation, caratosis, wart like
lesions are developed. Eg. Hydrocele (40-60%),
Elephantiasis of Scrotum, Penis, Leg, Arm, Vulva,
Breast, Chyluria.
15. Leg
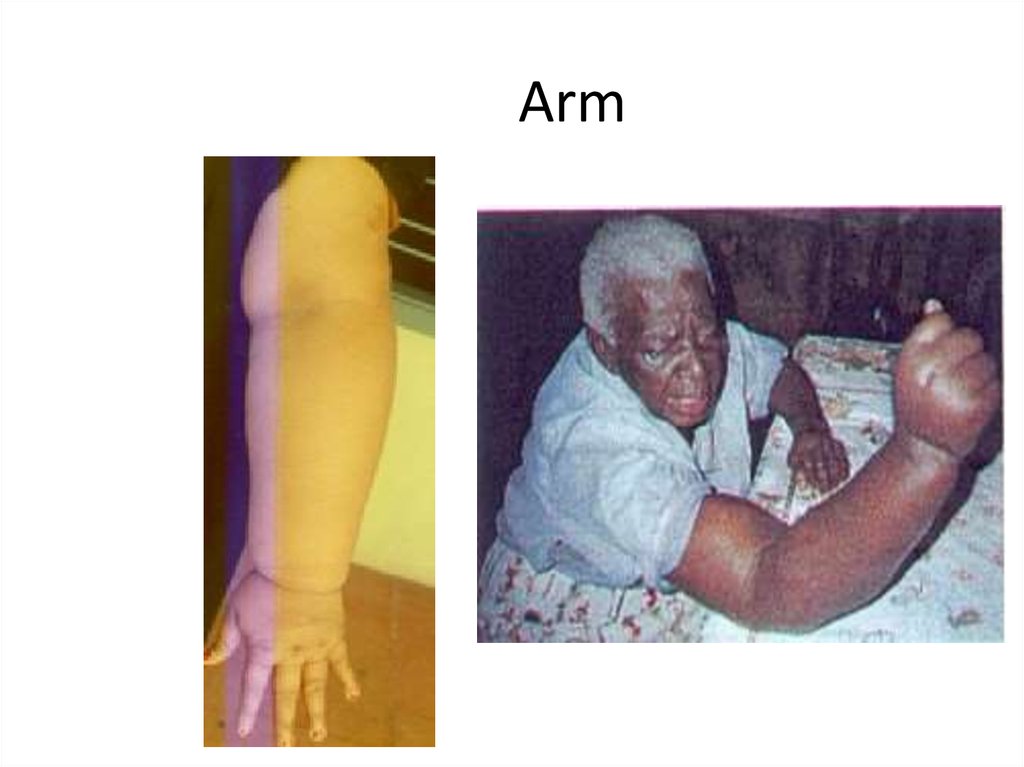
16. Arm
17. Occult Filariasis (TPE)
• Occult or Cryptic filariasis, in classical clinicalmanifestation mf will be absent. Occult
filariasis is believed to be the result of hyper
responsiveness to filarial antigens derived
from mf. Seen more in males.
• Patients present with paroxysmal cough and
wheezing, low grade fever, scandy sputum
with occasional haemoptysis, adenopathy
and increased eosinophilia. X-ray shows
diffused nodular mottling and interstial
thickening.
18. Chyluria & Haematuria
Chyluria & Haematuria19. Classification of Lymphoedema
1.
2.
3.
4.
5.
Lymphoedema is classified into 7 stages
on the basis of the presence & absence
of the following:
Oedema
Folds
Knobs
Mossy foot
Disability
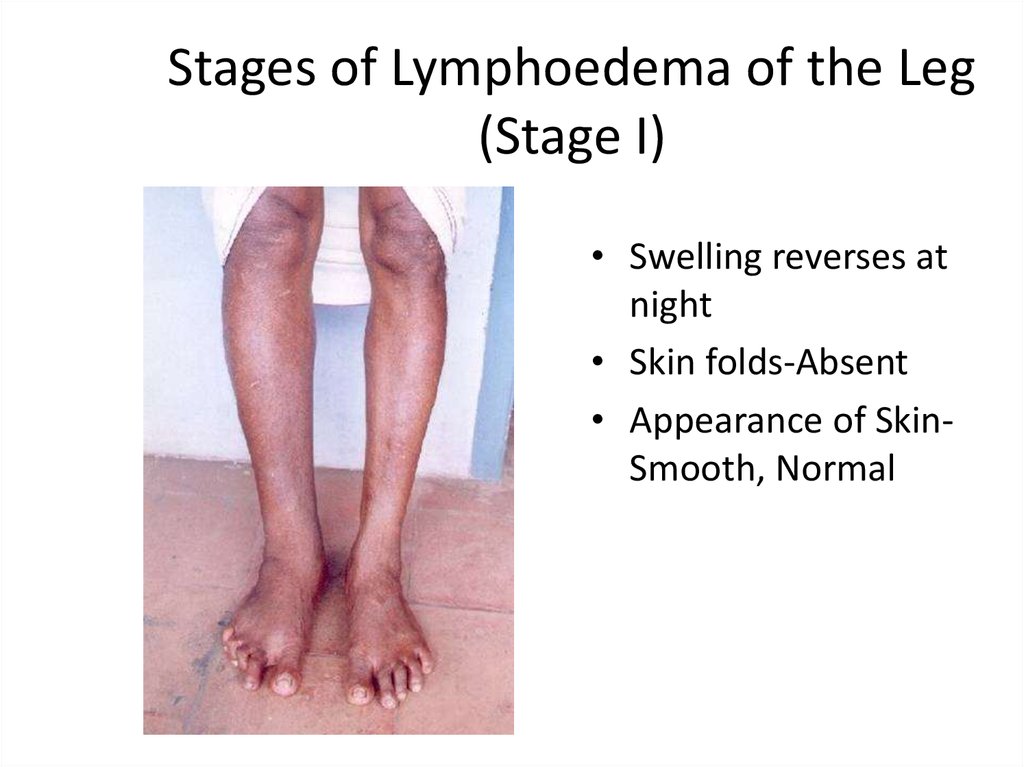
20. Stages of Lymphoedema of the Leg (Stage I)
• Swelling reverses atnight
• Skin folds-Absent
• Appearance of SkinSmooth, Normal
21. Stages of Lymphoedema of the Leg (Stage II)
• Swelling not reversibleat night
• Skin folds-Absent
• Appearance of skinSmooth, Normal
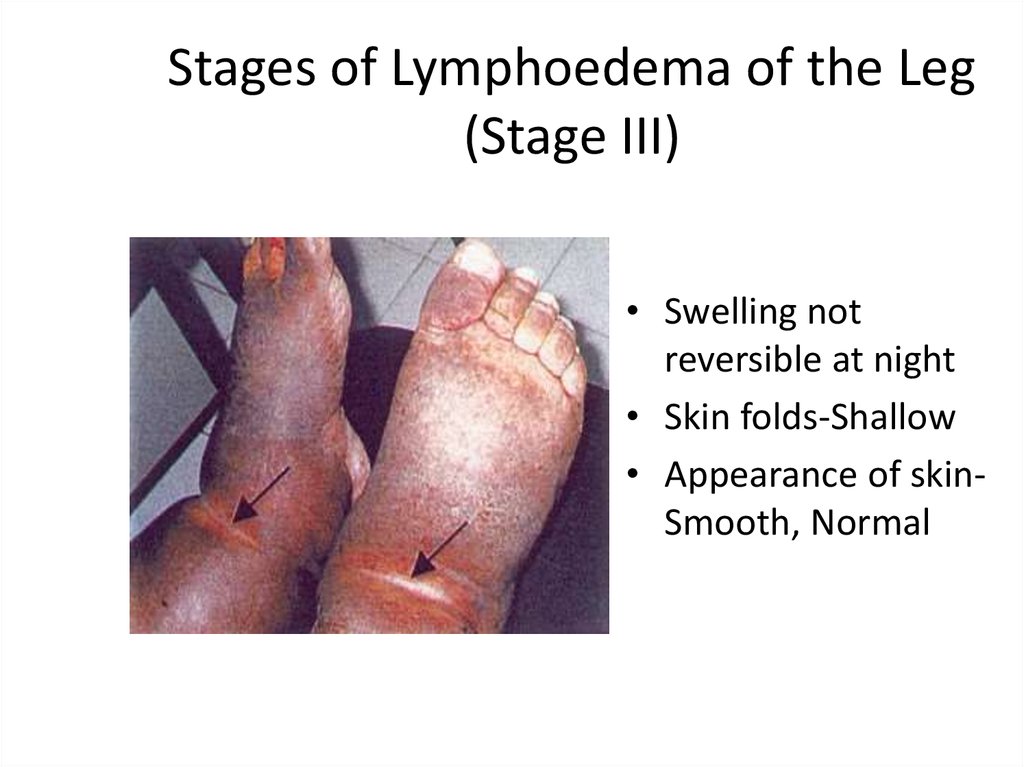
22. Stages of Lymphoedema of the Leg (Stage III)
• Swelling notreversible at night
• Skin folds-Shallow
• Appearance of skinSmooth, Normal
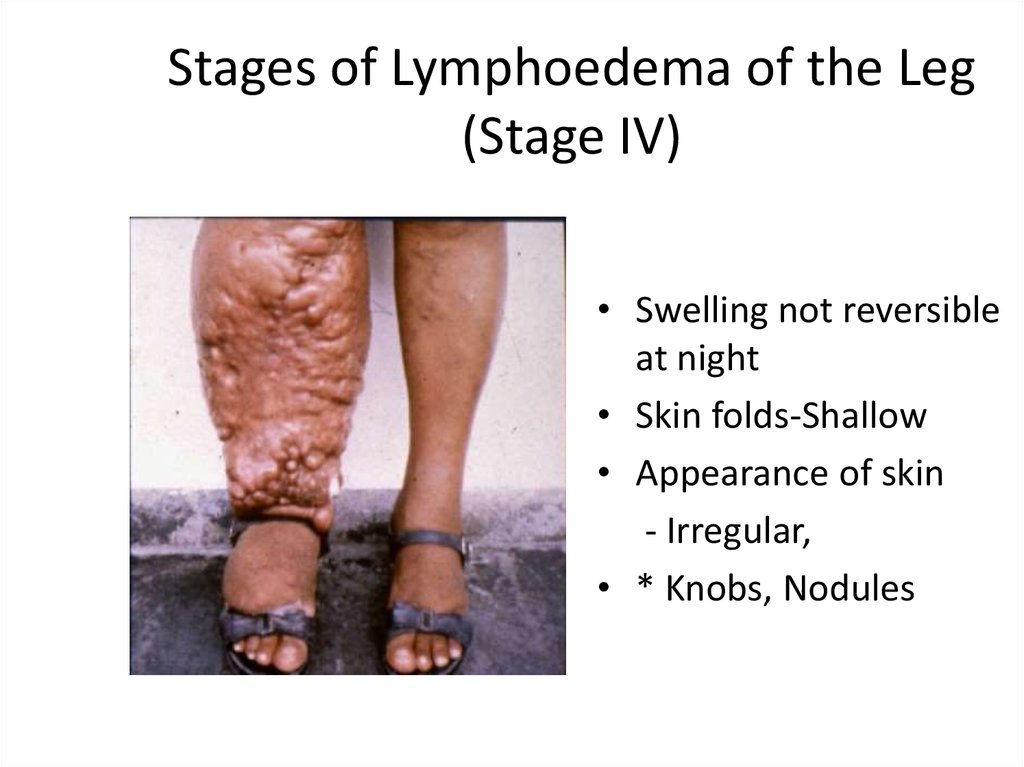
23. Stages of Lymphoedema of the Leg (Stage IV)
• Swelling not reversibleat night
• Skin folds-Shallow
• Appearance of skin
- Irregular,
• * Knobs, Nodules
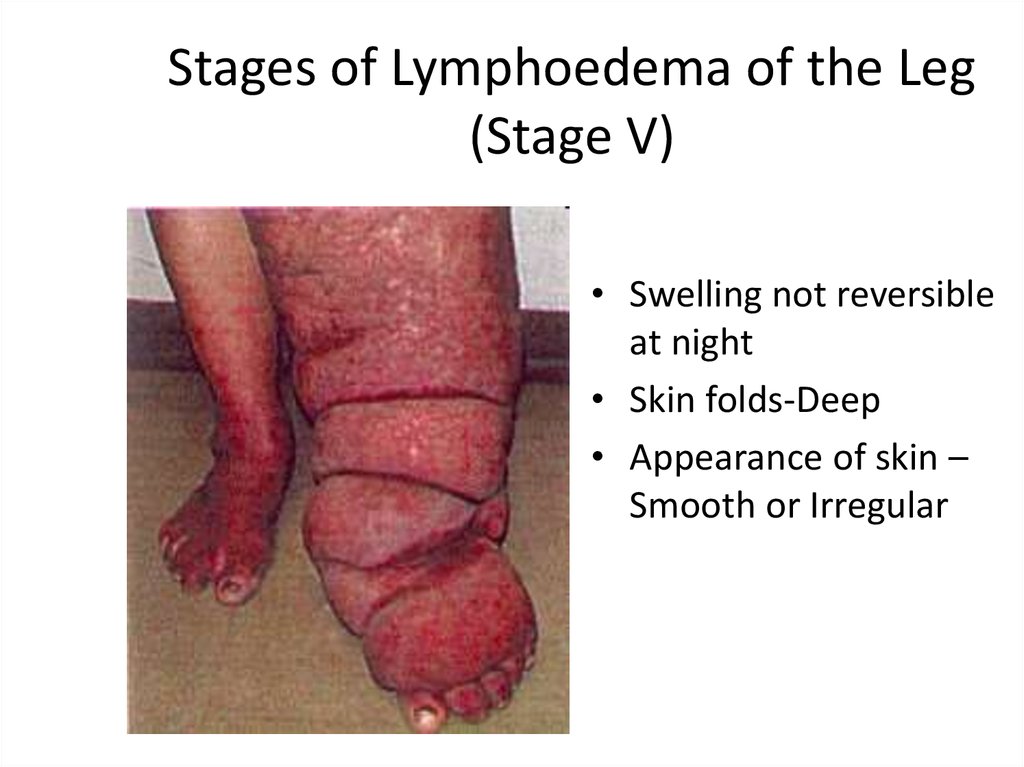
24. Stages of Lymphoedema of the Leg (Stage V)
• Swelling not reversibleat night
• Skin folds-Deep
• Appearance of skin –
Smooth or Irregular
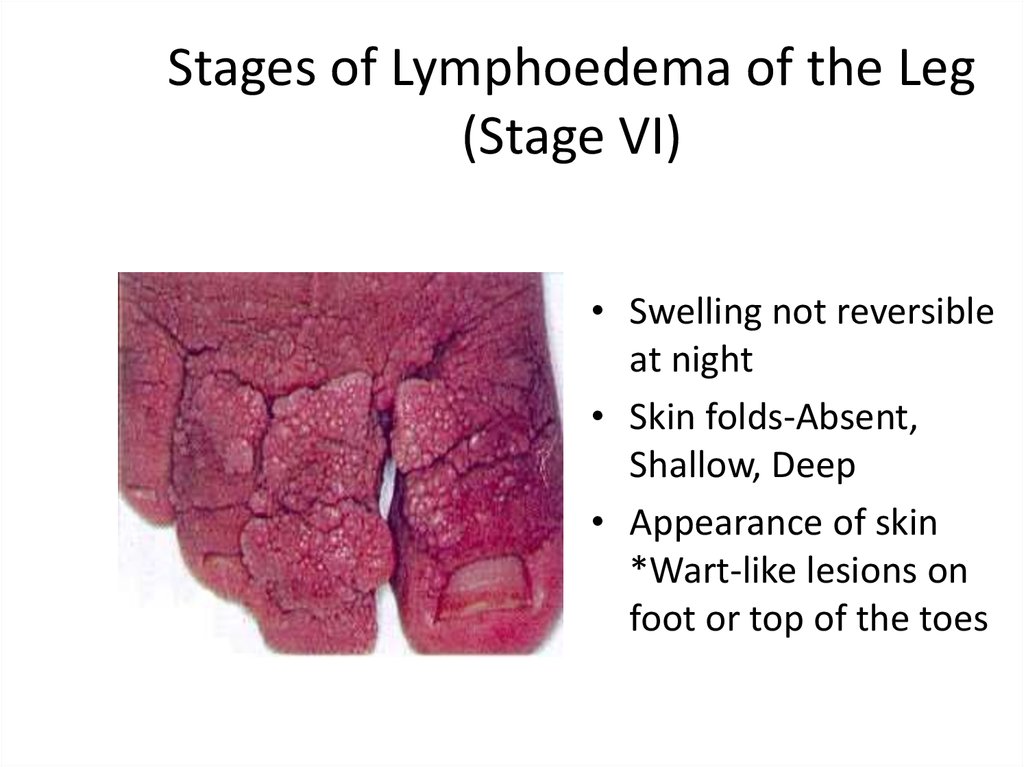
25. Stages of Lymphoedema of the Leg (Stage VI)
• Swelling not reversibleat night
• Skin folds-Absent,
Shallow, Deep
• Appearance of skin
*Wart-like lesions on
foot or top of the toes
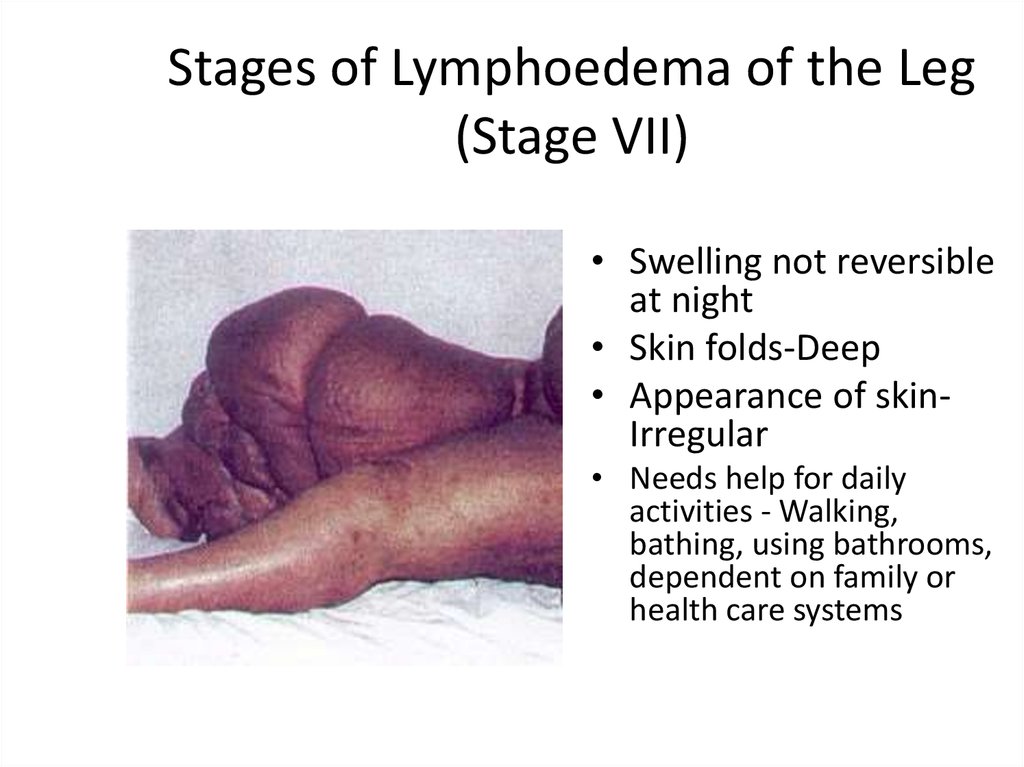
26. Stages of Lymphoedema of the Leg (Stage VII)
• Swelling not reversibleat night
• Skin folds-Deep
• Appearance of skinIrregular
• Needs help for daily
activities - Walking,
bathing, using bathrooms,
dependent on family or
health care systems
27. Social Impact of Disease
• Sexual Disability• Communities frequently shun
those disfigured.
• Inability to work
• Women with visible signs may
never marry or spouses and
families will reject them.
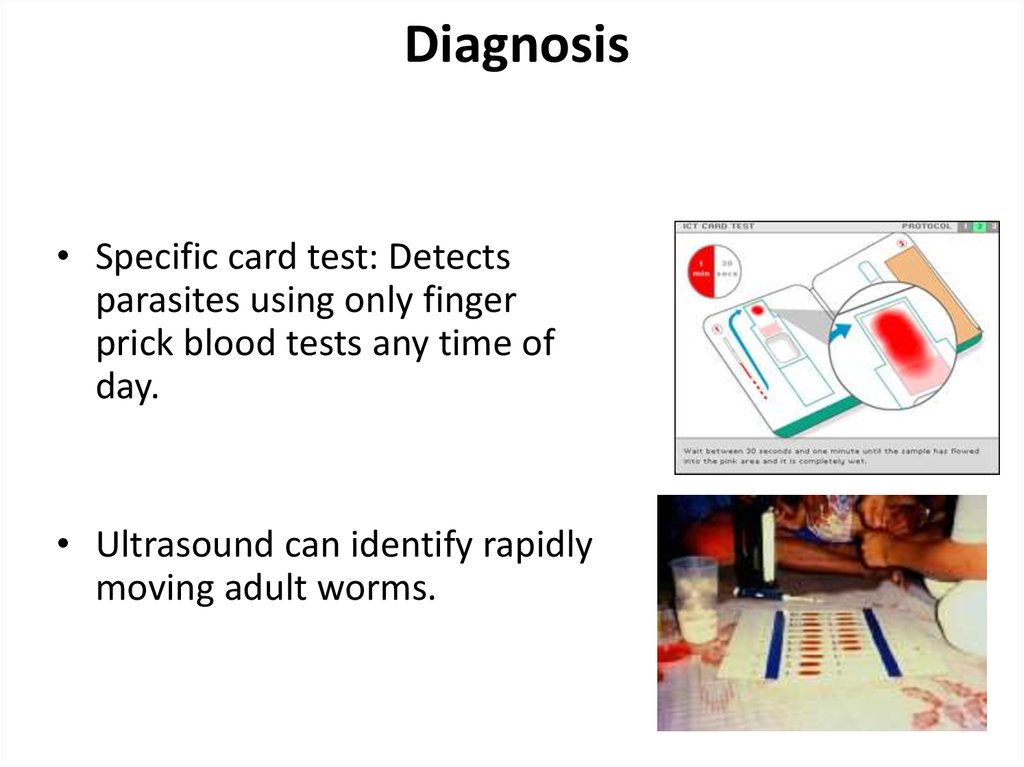
28. Diagnosis
• Specific card test: Detectsparasites using only finger
prick blood tests any time of
day.
• Ultrasound can identify rapidly
moving adult worms.
29. Chemotherapy of Filariasis
Drugs effective against filarial parasites1. Diethyl Carbomazine citrate (DEC) 6mg/Kg/12 days
2. Ivermectin 200µg – 400µg/Kg body weight
3. Albendazole 400mg/twice day /2 weeks. With
combination of DEC & Ivermectin, it enhances the action of
the drugs.
4. Couramin compound
Treatment of microfilaraemic patients may prevent
chronic obstructive disease and may be repeated
every 6 months till mf and/or symptoms
disappears.
30. Treatment and Management of Elephantiasis
• Prevention– Mosquito nets, insect repellents
• Voodoo healing techniques
• Elevate and exercise affected body part
• Skin treatment
– Wash area twice daily
– Antibacterial cream
• CDP (Complex decongestive physiotherapy)
– Lymph drainage, massage, compressive
bandages




 Медицина
Медицина