Похожие презентации:
Melanocytic and Epidermal Tumors
1. Melanocytic and Epidermal Tumors
Prof. dr. Skaidra ValiukevicieneDepartment Skin and Veneral Disaeses
2. Contents
Melanocytic tumors• Benign
• Malignant melanoma
Epidermal tumors
• Benign
• Carcinomas in situ (precanceroses)
• Skin carcinoma (basal cell carconoma and squamous cell
carcinoma)
3. Benign melanocytic lesions
The first step in analyzing pigmented lesions is to decide if:• Only increased melanin is present: Then one must think of
hyperpigmentation (café-au-lait spot, freckles)
• Increased numbers of melanocytes and/or theirs nests are
present: lentigo, melanocytic nevus (MN) or malignant
melanoma (MM)
4. Ehpelides, sin. Freckles
• Definition. Ephelides is the Greek word and medical term for freckle.Freckles are flat, brown multiple pigmented macules which develop
due to an increase of melanin that produce melanocytes on sunexposed skin after repeated exposure to sunlight.
• Epidemiology. These are particularly common in people with red hair
and a fair complexion. They may appear on children as young as 1 or
2 years of age.
• Clinical findings. Most freckles are generally uniform in color but can
vary somewhat in color -- they may be reddish, yellow, tan, light
brown, brown, or black -- but they are basically slightly darker than the
surrounding skin. They may become darker and more apparent after
sun exposure and lighten in the winter months.
• Diagnostic: Anamnesis and clinical symptoms.
• Therapy: no needed.
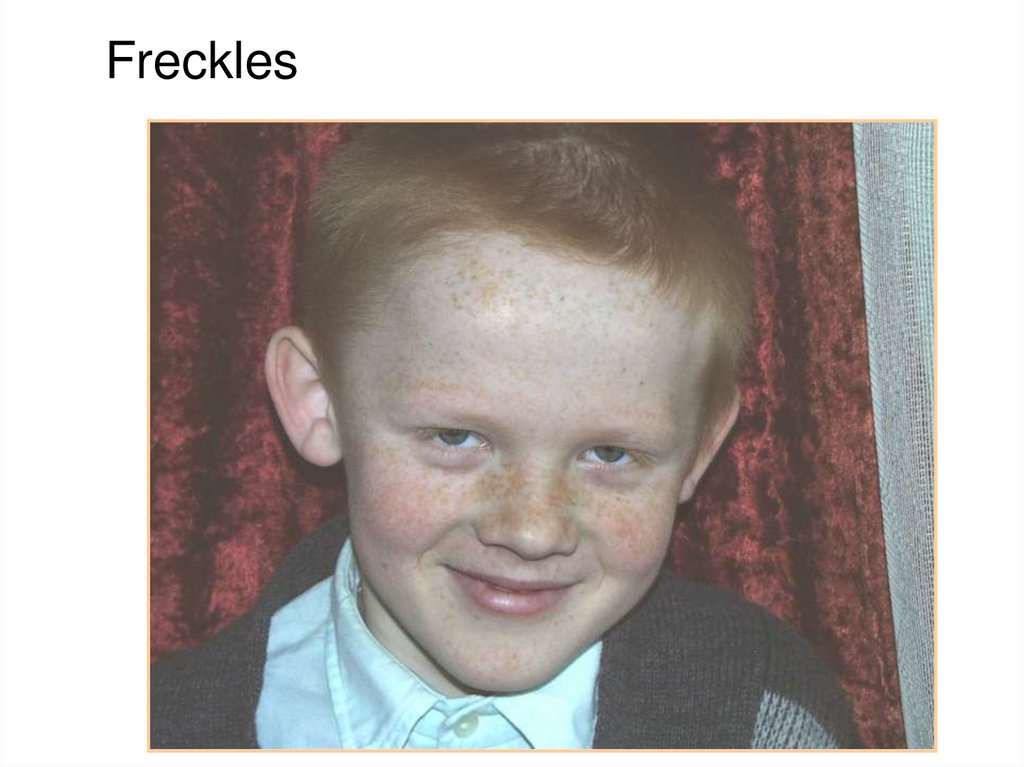
5. Freckles
6. Lentigo simplex
• Definition: localized hyperpigmentation withincrease of melanocytes at the dermoepidermal
junction
• Clinical features: uniformly pigmented tan to
dark brown macules; no relation to sun
exposure (unlike frecles)
• Diagnostic approach: clinical features,
dermatoscopy (DS); a biopsy is not needed
• Dif. Diagnostic: ephelides (frecles) – it are
paler, more irregular and becoming more
prominent in the summer
7. Lentigines
Other clinical types of lentigines:• Solar lentigo (senile or actinic lentigo): common acquired
melanocytic lesion in older adults becoming often after sun
exposure
• Multiple lentigines with or without associated findings
Therapy: no needed
8. Solar Lentigenes
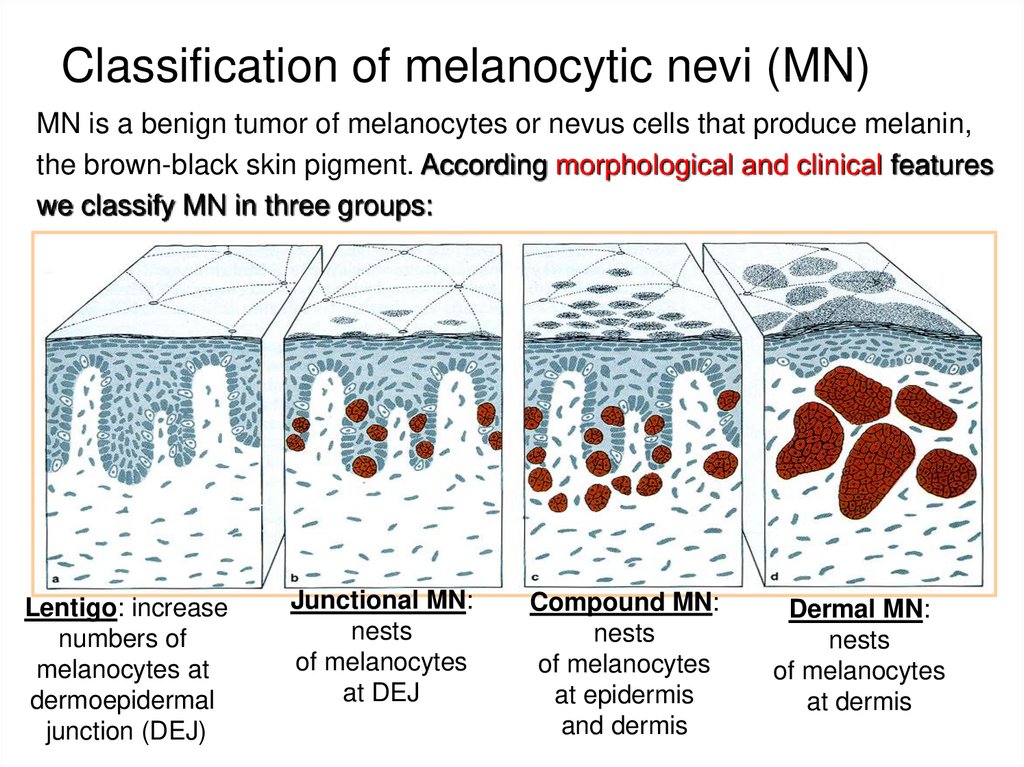
9. Classification of melanocytic nevi (MN)
MN is a benign tumor of melanocytes or nevus cells that produce melanin,the brown-black skin pigment. According morphological and clinical features
we classify MN in three groups:
Lentigo: increase
numbers of
melanocytes at
dermoepidermal
junction (DEJ)
Junctional MN:
nests
of melanocytes
at DEJ
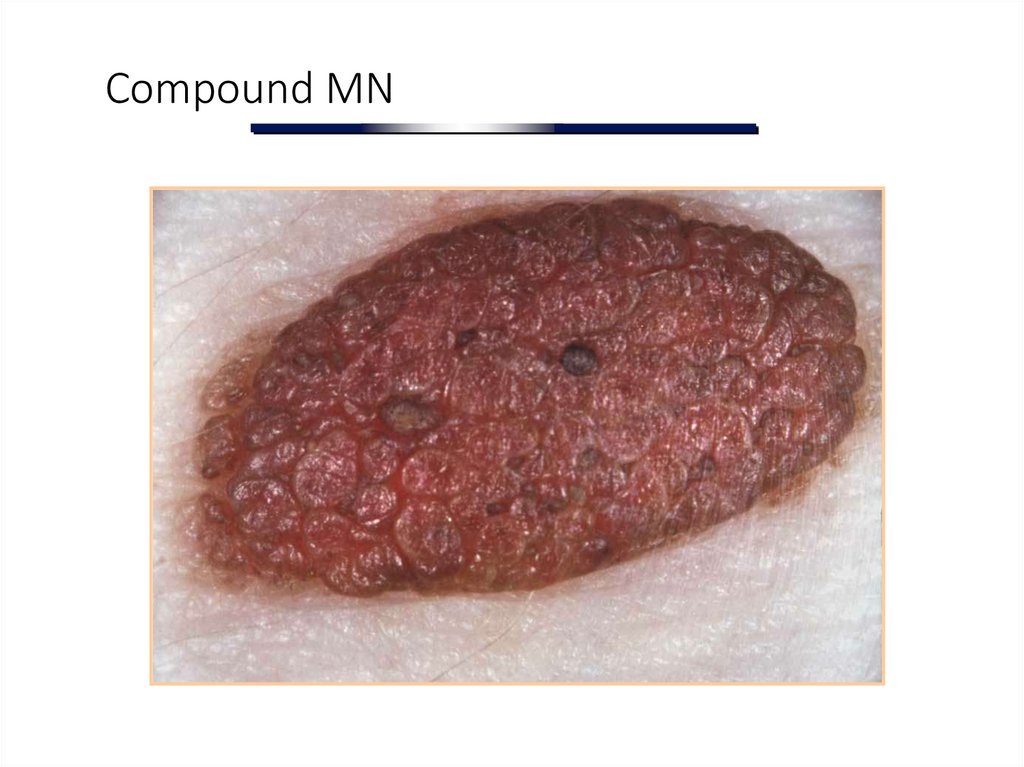
Compound MN:
nests
of melanocytes
at epidermis
and dermis
Dermal MN:
nests
of melanocytes
at dermis
10. Classification of MN
We classify MN according anamnesis and clinicalfeatures in two groups:
• Congenital MN (prevalence 2%)
• Acquired MN (prevalence 98-99%)
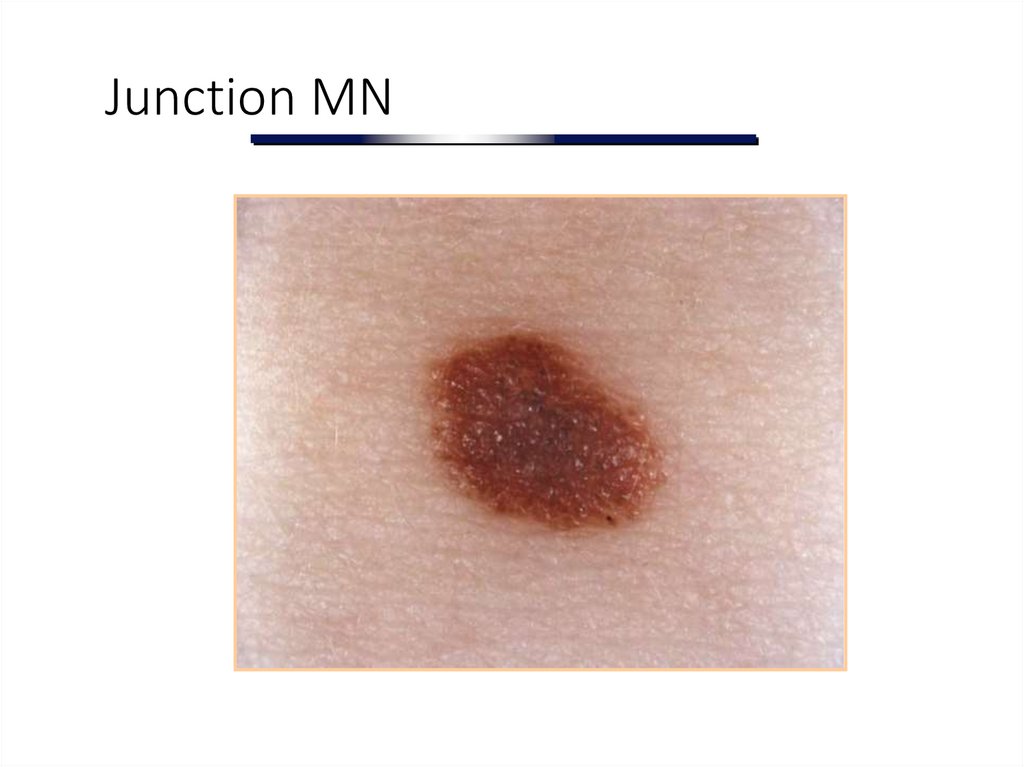
11. Junction MN
12. Compound MN
13.
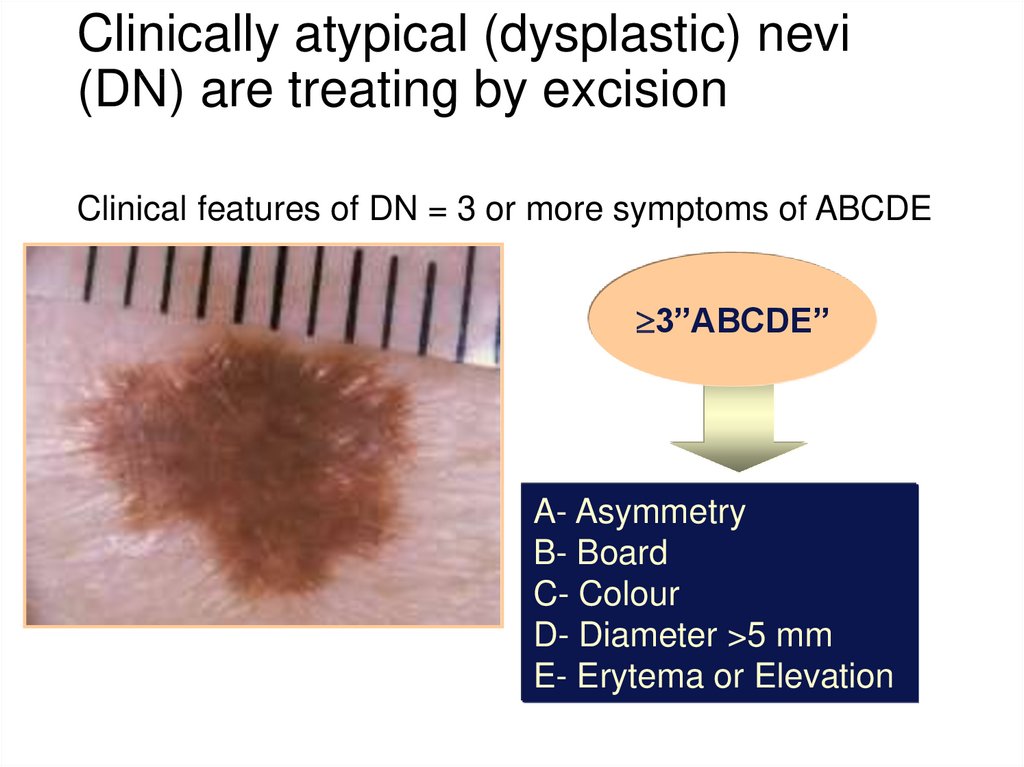
Dermal MN14. Clinically atypical (dysplastic) nevi (DN) are treating by excision
Clinical features of DN = 3 or more symptoms of ABCDE3”ABCDE”
A- Asymmetry
B- Board
C- Colour
D- Diameter >5 mm
E- Erytema or Elevation
15. Congenital MN
• Definition: MN present at birth• Epidemiology: 1-2% of newborns have MN
• Clinical features: small <1.5 cm diameter;
medium: 1,5-20 cm diameter; large: > 20 cm
diameter. Most congenital MN have a
papillomatous surface and contain hair
• Prognosis: risk of developing malignant
melanoma is higher in congenital nevus than in
acquired nevus
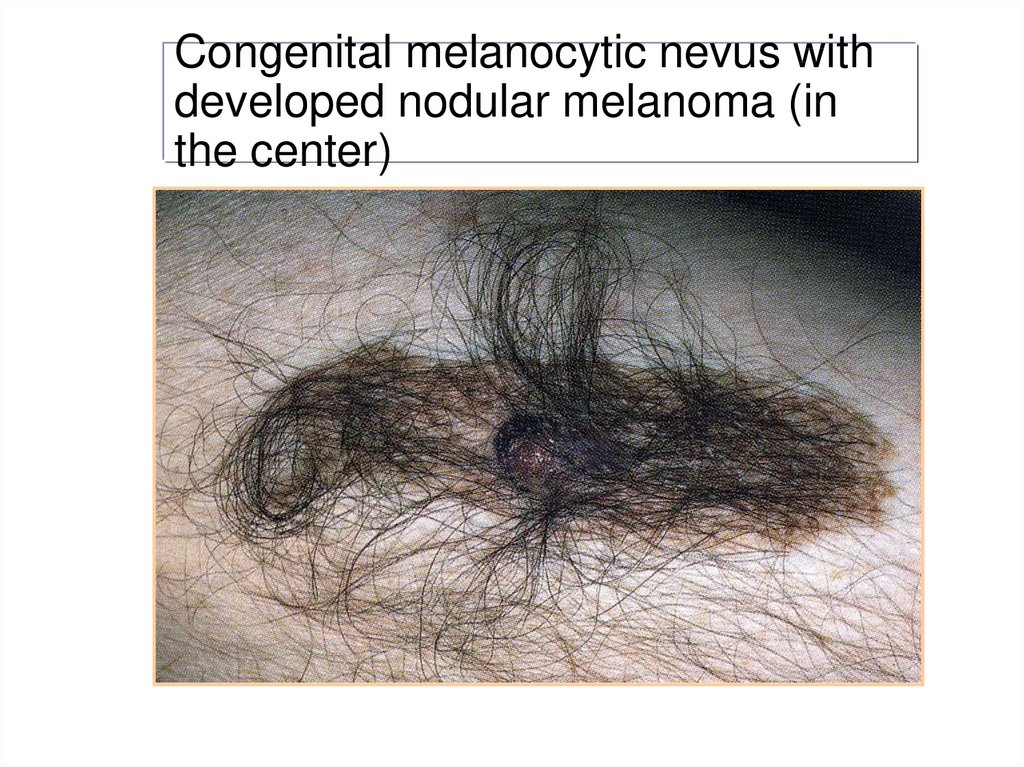
16. Congenital melanocytic nevus with developed nodular melanoma (in the center)
17. Malignant melanoma
18. Malignant melanoma (MM)
• Definition: malignant tumor of melanocytes• Epidemiology: the lifetime risk of MM for white Europeans
increased dramatically, representing doubling of incidence
every 10-15 years.
• The incidence of melanoma:
− <10-25 new melanoma cases per 100,000 inhabitants in
Europe;
− 20-30 per 100,000 in the United States of America;
− 50-60 per 100,000 in Australia
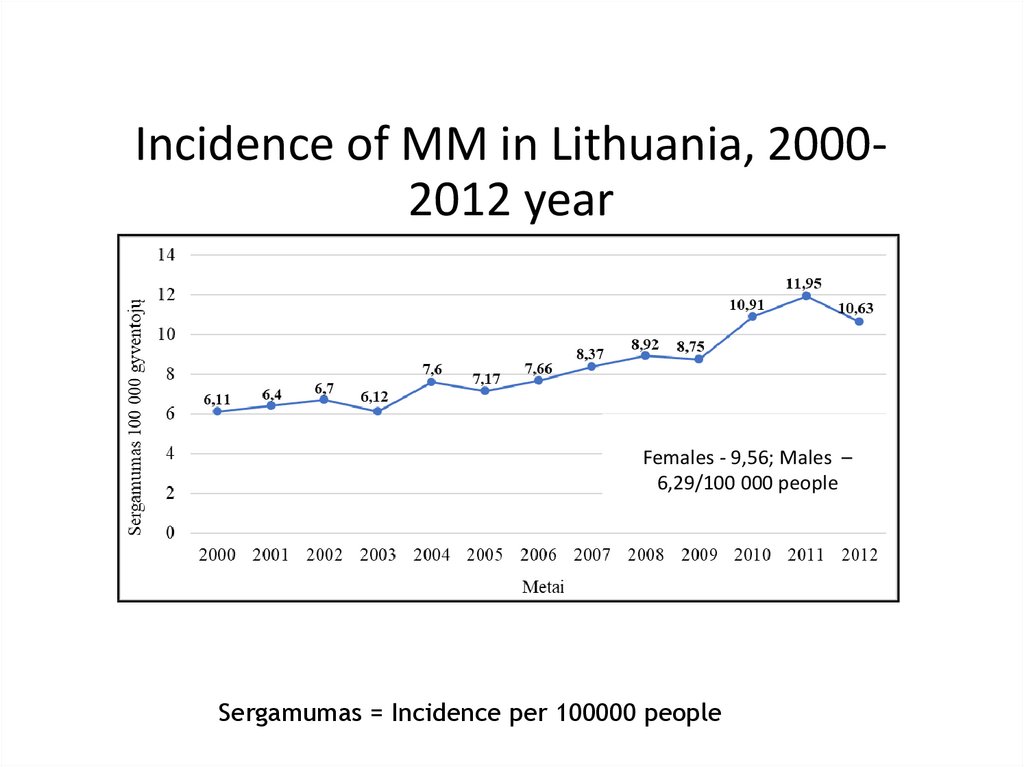
19. Incidence of MM in Lithuania, 2000-2012 year
Incidence of MM in Lithuania, 20002012 yearFemales - 9,56; Males –
6,29/100 000 people
Sergamumas = Incidence per 100000 people
20. Pathogenesis of MM
Risk factors of MM are these:• Genetic predisposition (familial melanoma syndrome
(up to 10%)
• Excessive sun exposure and sunburns <20 years of
age, especially infants
• More than 50 MN on the body
• Presence of atypical (dysplatic) melanocytic nevi.
• In many cases (70 %) melanomas develop de novo.
About 25% melanomas show histological features of
preexisting MN.
• Light skin (skin types I and II)
21. Biology of MM
Melanomas have two growth phases:• Horizontal (radial phase): melanoma starts with
abnormal junctional melanocytes; expands
laterally for long time; in this phase tumor rarely
metastasize
• Vertical: tumor cells break through the
basement membrane and begin to grow down
into dermis. Once the basement membrane has
been bridged, the melanoma begins to
metastasize
22. Clinical features of MM
We classify melanomas in four clinical and morphologicalsubtypes:
• Superficial spreading melanoma (SSM): most common
type (60%); age peak 40-60 years; horizontal growth phase
and later vertical
• Nodular melanoma (NM): about 20%; age peak 40-60
years; it has vertical growth phase with very short period of
horizontal phase (worst prognosis)
• Lentigo maligna melanoma (LMM): about 10%; it is more
common for older patients (peaks > 60 years); better
prognosis because of very long radial growth phase
• Acral-lentiginous melanoma (ALM): 5%; most common in
dark-skinned people; occurs on areas without hair follicules;
subungual like tinea nigra, digital or on oral mucosa
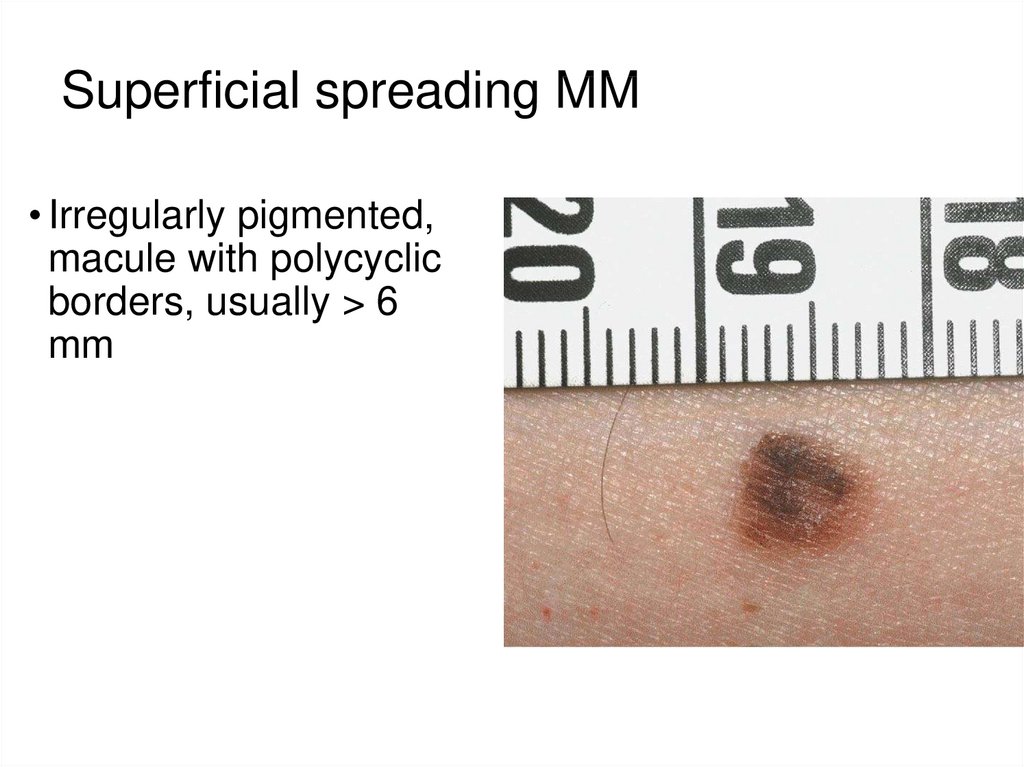
23. Superficial spreading MM
• Irregularly pigmented,macule with polycyclic
borders, usually > 6
mm
24.
Nodular melanoma:dark-brown papule or
nodule, frequently
ulcerated
25.
Lentigo malignamelanoma (LMM):
large irregularly
pigmented macula or
plaque in sun
exposed sites
(face or scalp); its
more common for
older people
26.
entiginous melanoma (ALM) may present asreak in nails like tinea nigra or on oral mucosa
27. Diagnostic of MM
Diagnostic of melanoma consists from such procedures:• Clinical examination (the ABCDE rule, bleeding and
ulceration of preexisting lesion)
• Dermatoscopic examination (irregularly pigment network,
radial streaks, pseudopods, gray-blue areas)
• Ultrasonography 20-50 MHz: can be used for assessment of
tumor thickness (Tu) for surgery planning
• Excisional biopsy. Incisional biopsies should be reserved for
cases of ALM that are too large for excision
• Tumor histology is the most important prognostic parameters
(the tumor thickness (Tp) according Breslow)
• Tumor immunhistochemistry (with marker S100)
• Sentinel lymph node biopsy (when Tu or Tp is >0.8 -1mm)
28. Staging of MM
When the diagnosis of MM has been established, thefollowing tests are performed:
• Chest radiography
• Sonography of regional lymph nodes (LM), abdomen,
pelvis, and retroperitoneum
• In higher risk patients CT or MRI
• In blood antigen of melanoma and melanocytes (S100)
• PET (if during sentinel lymph node biopsy positive
sentinel LM was found)
• Molecular diagnostics: BRAF V600 mutation. Is required
for patients with regional or distant metastasis, in order to
identify patients eligible for treatment with BRAF inhibitors
and MEK inhibitors.
29.
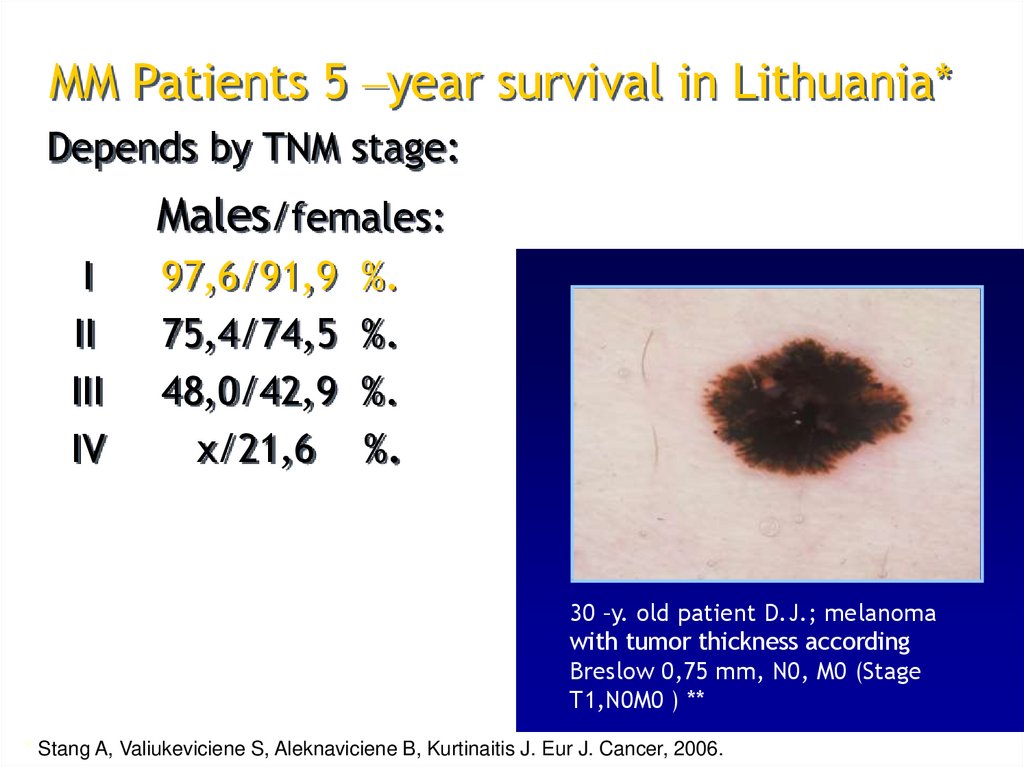
MM Patients 5 –year survival in Lithuania*Depends by TNM stage:
Males/females:
I
II
III
IV
97,6/91,9
75,4/74,5
48,0/42,9
x/21,6
%.
%.
%.
%.
30 –y. old patient D.J.; melanoma
with tumor thickness according
Breslow 0,75 mm, N0, M0 (Stage
T1,N0M0 ) **
* Stang A, Valiukeviciene S, Aleknaviciene B, Kurtinaitis J. Eur J. Cancer, 2006.
30.
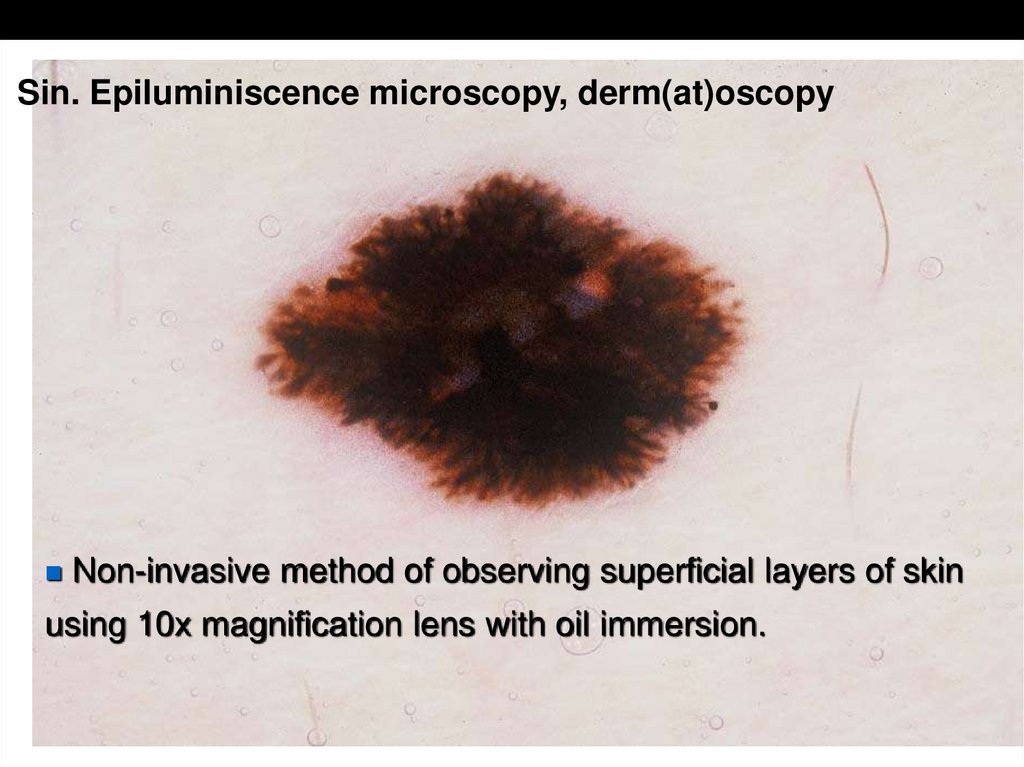
Preoperative diagnostic: DermatoscopySin. Epiluminiscence microscopy, derm(at)oscopy
Non-invasive method of observing superficial layers of skin
using 10x magnification lens with oil immersion.
31.
Hand - help Dermatoscope Heine Delta 1032. Digital dermatoscope
FotoFinder Dermatoscope• Digital camera, PC, optic
lens
• Automatic programme for
evaluation of MM according
Tuebingen researcher group
(Germany) 1.
• Programme consists from 64
parameters of ABCD rule and
other
1
Blum A, Luedtke H, Ellwanger U, Schwabe R, Rassner G,
Garbe C. Digital image analysis for diagnosis of cutaneous
melanoma. Development of a highly effective computer
algorithm based on analysis of 837 melanocytic lesions. Br
J Dermatol 2004;151:1029-1038.
33.
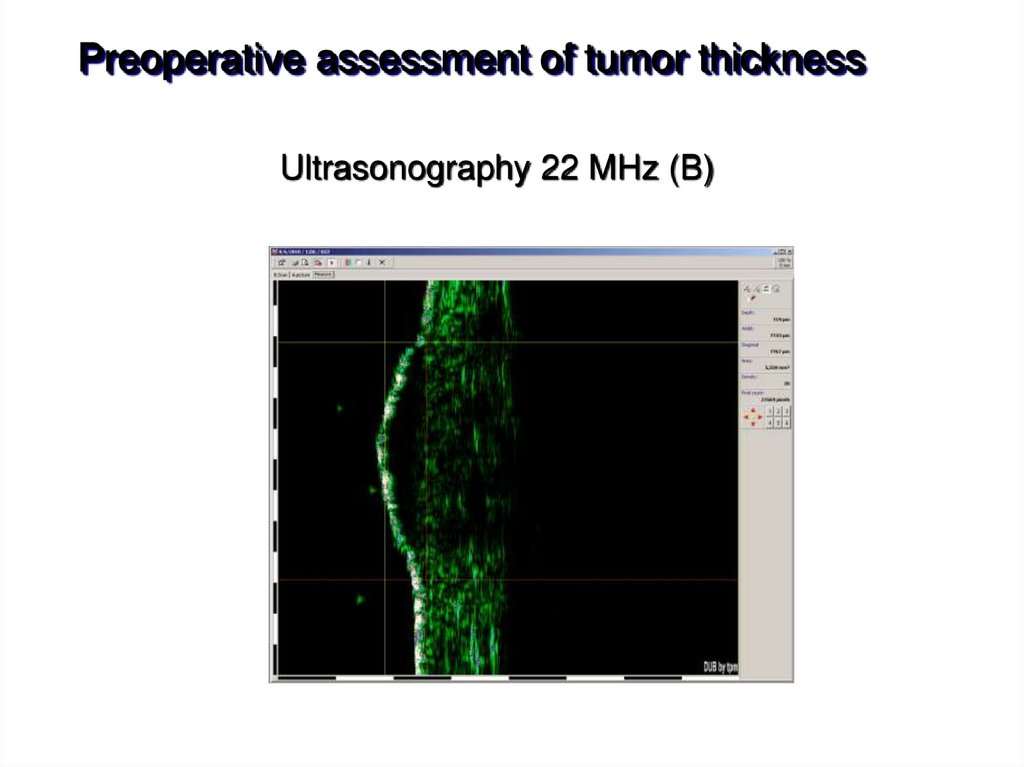
Preoperative assessment of tumor thicknessUltrasonography 22 MHz (B)
34. Ultrasonography for evaluation of regional lymph nodes (LN)
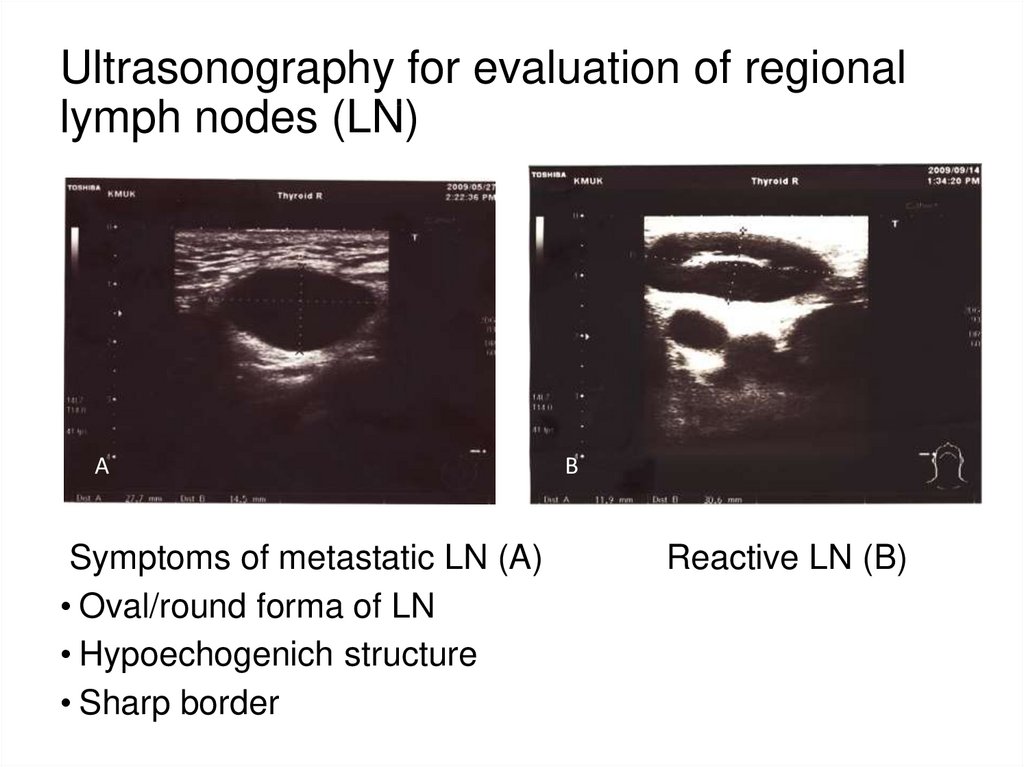
ASymptoms of metastatic LN (A)
• Oval/round forma of LN
• Hypoechogenich structure
• Sharp border
B
Reactive LN (B)
35. Sentinel Lymph Node (SLN) biopsy
• The procedure recommended when melanoma thickness>0.8-1 mm.
• Used for assessment of micrometastasis in LN and
staging of MM.
• Histological status of SLN is of great prognostic factor.
Negative SLN – 85% 5-year survival; positive SLN - 30%
5-year survival.
• If SLN is positive, regional LN dissection must be perform.
36.
Procedure of SLN biopsy*Kaikaris V (tyrėjas), Valiukevičienė S, Rimdeika R, Gollnick H,
Ulrich J. Medicina 2003; 39(7):621-30.
37. Therapy of primary MM
• Primary tumor excision is “gold” treatment.Margin of safety excision:
Tumor <=1mm thickness – 1cm excision
margin
Tumor >1mm thickness – 2 cm excision
margin
• After tumor and metastasis excision
recommended adjuvant therapy with
interfernon alfa for high risk patients (stage IIB
or higher)
38. Therapy of metastatic MM (stage III)
• If LN metastasis (or SLN micrometastasis) are identified, radicalLN dissection is required. After this operation adjuvant
immunotherapy should be applied
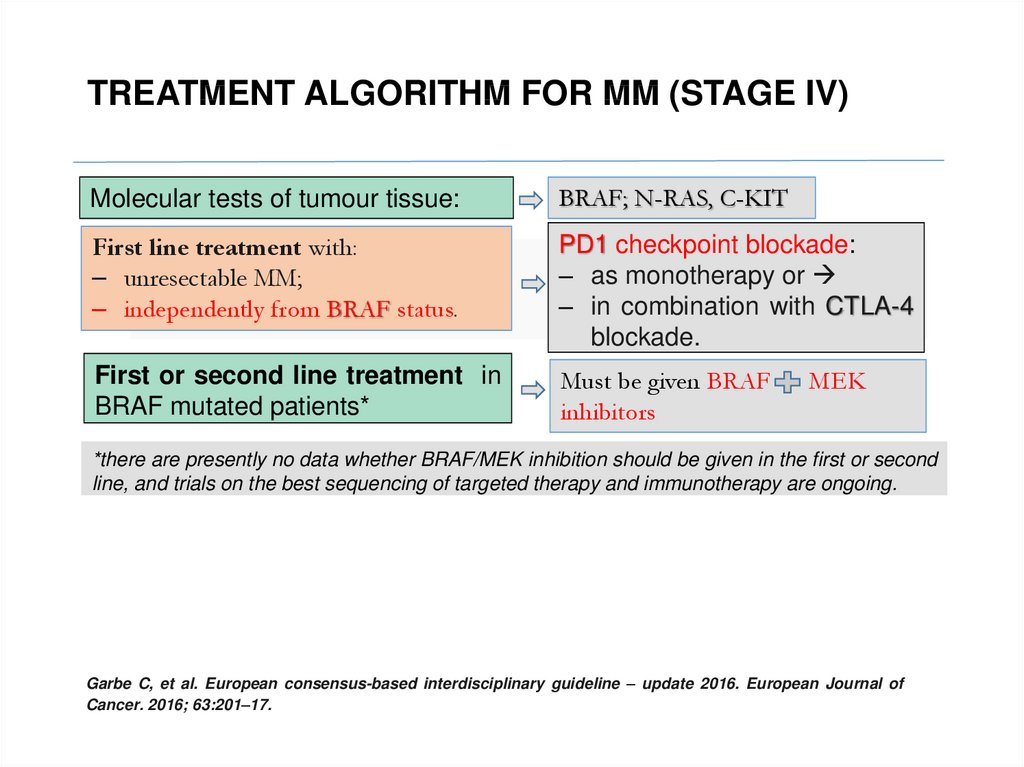
39. TREATMENT ALGORITHM FOR MM (STAGE IV)
Molecular tests of tumour tissue:BRAF; N-RAS, C-KIT
First line treatment with:
‒ unresectable MM;
‒ independently from BRAF status.
PD1 checkpoint blockade:
‒ as monotherapy or
‒ in combination with CTLA-4
blockade.
First or second line treatment in
BRAF mutated patients*
Must be given BRAF
inhibitors
MEK
*there are presently no data whether BRAF/MEK inhibition should be given in the first or second
line, and trials on the best sequencing of targeted therapy and immunotherapy are ongoing.
Garbe C, et al. European consensus-based interdisciplinary guideline – update 2016. European Journal of
Cancer. 2016; 63:201–17.
40. Contents
Melanocytic tumors• Benign
• Malignant melanoma
Epidermal tumors
• Benign
• Carcinoma in situ (precanceroses)
• BCC and SCC
41. Precanceroses (PC)
Ca in situ is a epithelium neoplasm without invasion of thebasement membrane. If left untreated, progression to invasive
squamous cell carcinoma (SCC) may be occur.
More common PC are:
• Actinic keratosis
• Leukoplakia
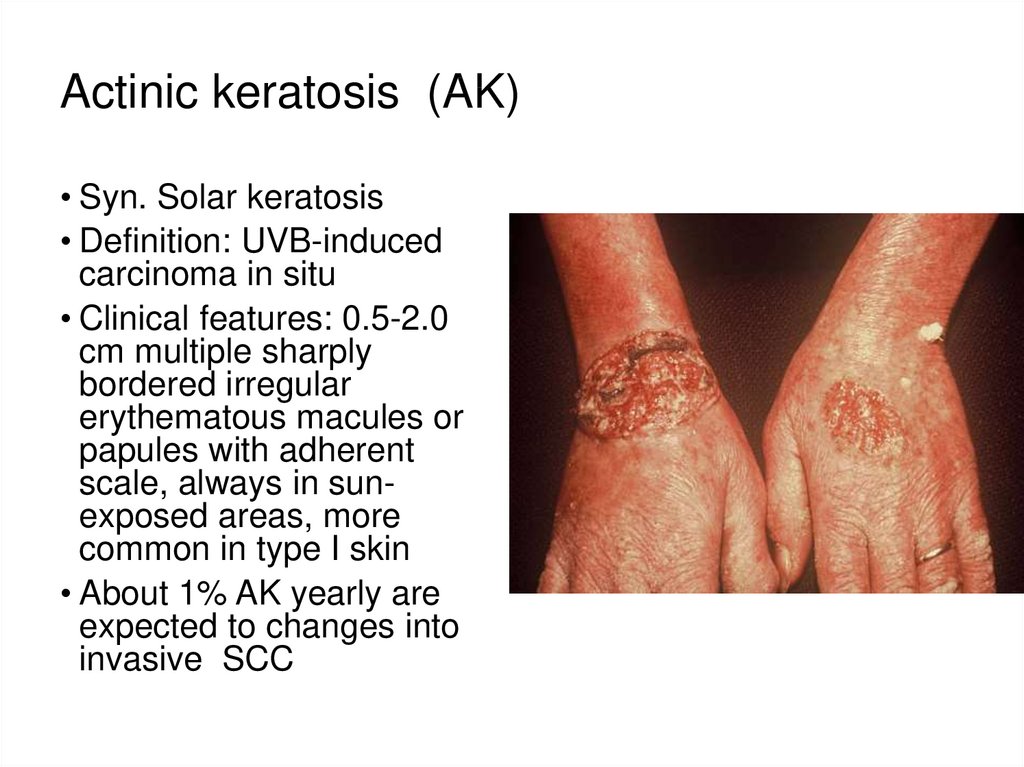
42. Actinic keratosis (AK)
• Syn. Solar keratosis• Definition: UVB-induced
carcinoma in situ
• Clinical features: 0.5-2.0
cm multiple sharply
bordered irregular
erythematous macules or
papules with adherent
scale, always in sunexposed areas, more
common in type I skin
• About 1% AK yearly are
expected to changes into
invasive SCC
43. Leukoplakia
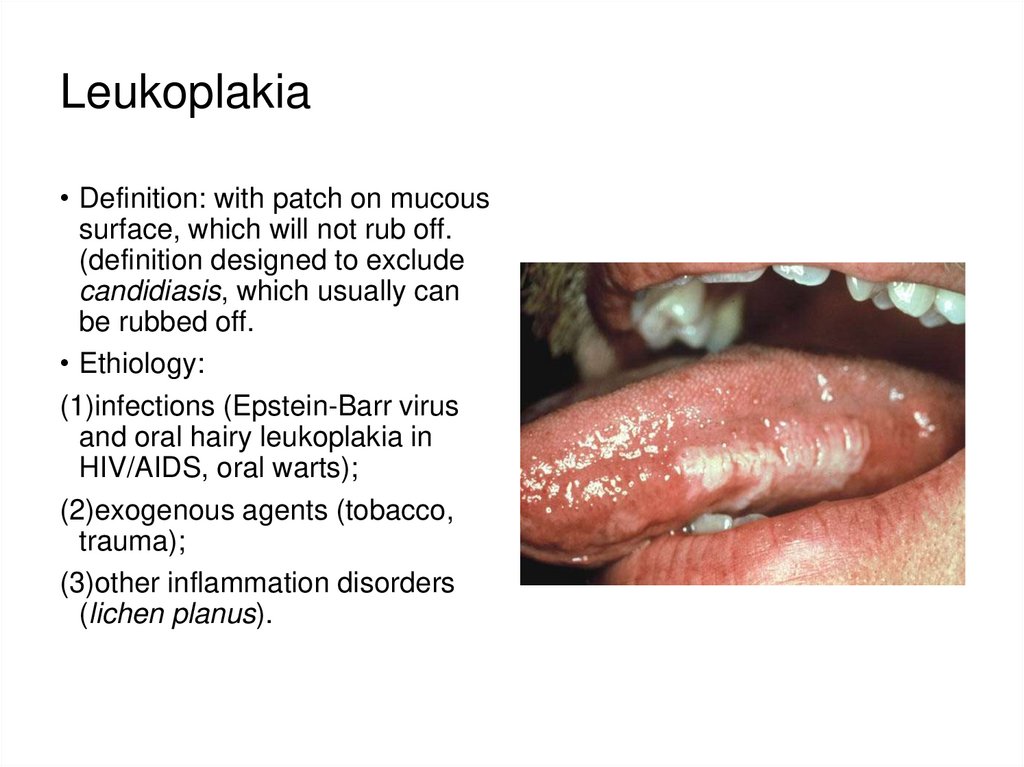
• Definition: with patch on mucoussurface, which will not rub off.
(definition designed to exclude
candidiasis, which usually can
be rubbed off.
• Ethiology:
(1)infections (Epstein-Barr virus
and oral hairy leukoplakia in
HIV/AIDS, oral warts);
(2)exogenous agents (tobacco,
trauma);
(3)other inflammation disorders
(lichen planus).
44. Leukoplakia
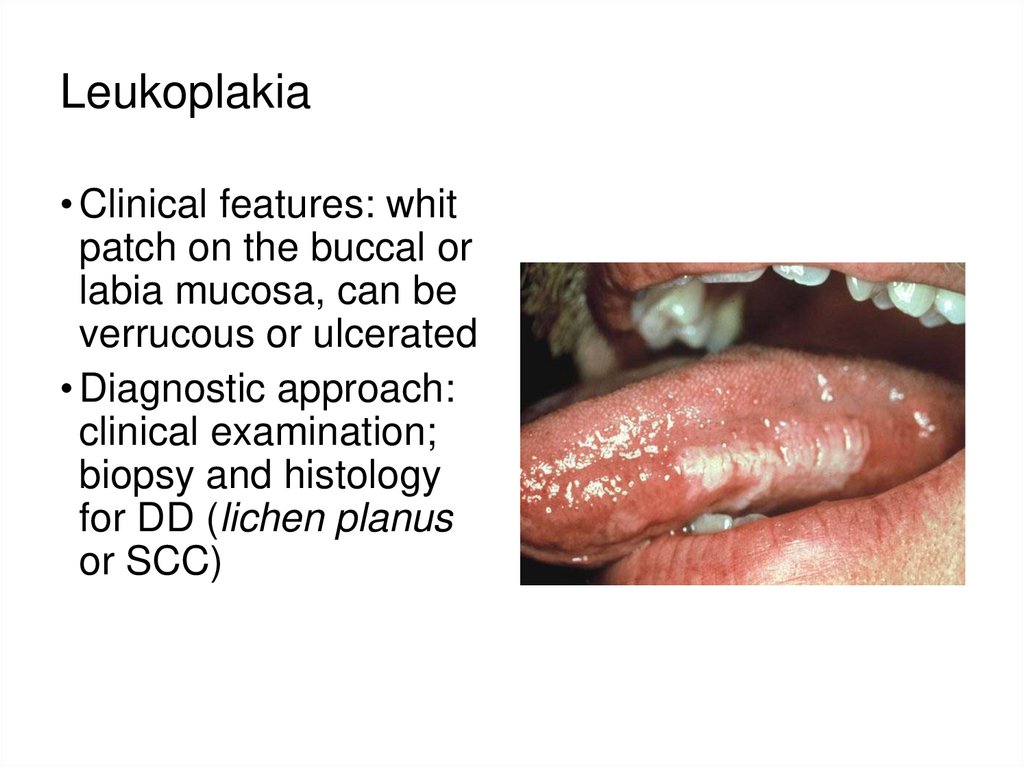
• Clinical features: whitpatch on the buccal or
labia mucosa, can be
verrucous or ulcerated
• Diagnostic approach:
clinical examination;
biopsy and histology
for DD (lichen planus
or SCC)
45. Treatment of Precanceroses
• Elektrodissekation or cautery*• Laser therapy*
• Cryotherapy
• Photodynamic therapy: topical application of
photosensitizes (aminolevullinic acid) followed by
irradiation at a wavelength absorbed by agent.
• For multiple lesions:
- Topical 5-fluoruracil cream for 10-14 days
- Topical imiquimod 3 x weekly for 6 weeks
• Excision in local anesthesia, especially if thick PC,
resistant to therapy with other treatment methods
* requires local anesthetic
46. Basal cell carcinoma (BCC)
• Definition: low-grade malignant epidermis tumor, locallyaggressive but rare metastatic
• Epidemiology (BCC+SCC): 50/100000. Incidence has doubled
over past decade. Most patients are >50 years of age
• During 1996-2010 year overall BCC incidence rates have
increased from 27.4 to 46.0 cases per 100,000 in Lithuania.
Incidence of BCC during the study period increased faster
among men than among women (by 3.3% and 2.6% per year,
respectively), while the incidence among both sexes in 2010
became almost equal -46.4 among men and 47.4 among
women per 100,000. The head and neck was the most common
site of BCCs for both sexes (31.0 and 32.9 per 100,000 among
men and women, respectively) [R.Jurciukonyte, et al. Br J
Dermatol; 2013].
47. Basal cell carcinoma (BCC)
• Pathogenesis:(1) most BCC arise from epidermal cells differentiated in the
direction of the hair bulb.
(2) the main trigger appears to be UVB
(3) genetic predisposition (genetic mutations in nevoid BCC
syndrome)
48. Basal cell carcinoma (BCC)
• Clinical features: most common on face or trunk (multiple lesions). No mucosal lesions
• Clinical-histological types:
(1)Nodular BCC ( pearly telangiectatic nodule or
papules, often with central ulceration)
(2)Superficial BCC (flat, red-brown patch, often with
scaly and with a pearly border)
(3)Pigmented BCC (pigmented nodule, papule or patch)
(4)Sclerosing BCC (atrophic plaque)
(5)Ulcus terebrans: aggressive BCC invading subcutis
structures, bones, frequently can be fatal.
49. Common types of BCC
Nodular exulcerated BCCSuperficial BCC
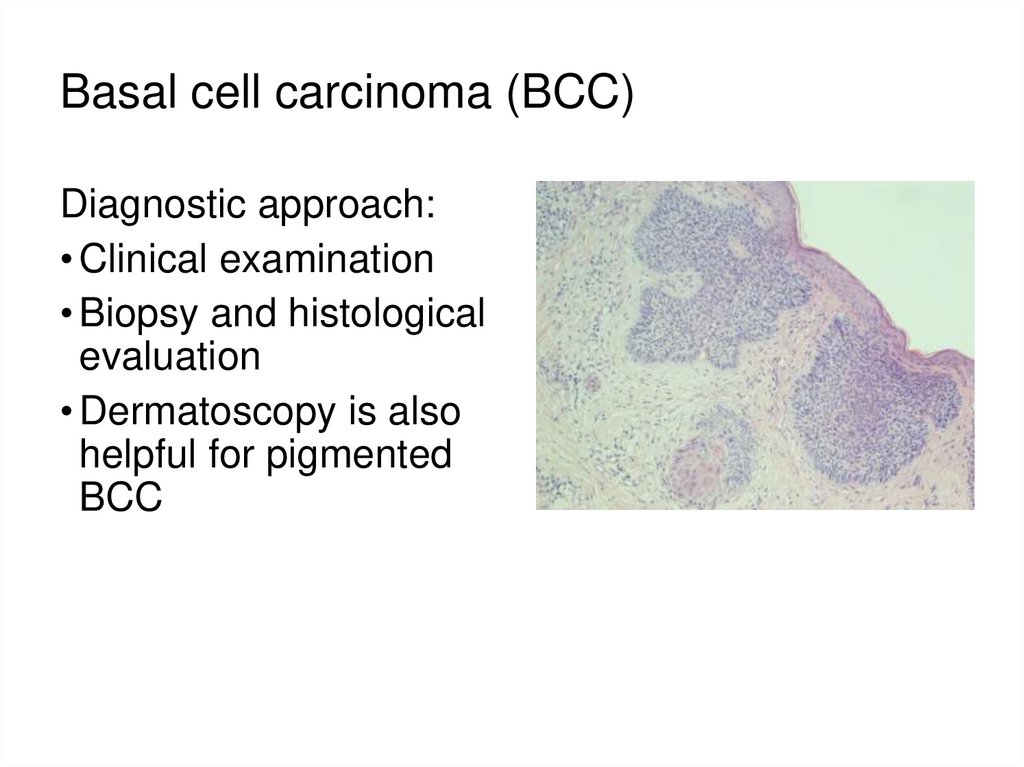
50. Basal cell carcinoma (BCC)
Diagnostic approach:• Clinical examination
• Biopsy and histological
evaluation
• Dermatoscopy is also
helpful for pigmented
BCC
51. Therapy of BCC
Surgical excision with histologic control of margins is the treatment of choice(recurrence rates less than 5%)
Alternatives for superficial BCC or small lesions*:
• Cryosyrgery
• Photodynamic therapy
• Curettage and electrocautery
• Laser ablation
• Topical imiquimod or 5-fluoruracil cream 3x weekly for 6 weeks
• Radiation therapy (multiple lesions or in difficult locations)
Local advanced or metastatic BCC: Hedgehog pathway signaling inhibitor
(vismodegib)
*lack of histologic control and higher recurrence rates
52. Squamous Cell Carcinoma (SCC)
• Definition: malignant epidermal tumor arising fromkeratynocytes, with potential for local spread and metastasis
• Epidemiology (BCC+SCC): 50/100000. Incidence has doubled
over past decade. Most patients are >50 years of age
53. Squamous Cell Carcinoma (SCC)
• Pathogenesis:(1)The main trigger appears to be UVB
(2)HPV (16,18,31,33 and 38 types)
(3)Other: radiation therapy, arsenic or chemical carcincogens;
immunosupression (iatrogenic, HIV/AIDS)
54. Squamous Cell Carcinoma (SCC)
• Clinical features: usually present as hyperceratotic papule orplaque, often with crust or ulceration. Difficult to separate from
precanceroses. Growth rate and risk of metastasis (regional
lymph nodes or visceral) are highly variable
• Diagnostic approach: clinical examination and biopsy
55.
56. Squamous Cell Carcinoma (SCC)
Therapy:• Surgical excision with histologic control of margins is
the treatment of choice (recurrence rates less than 5%)
• All other approaches are less than ideal (cryosyrgery,
photodynamic therapy, laser ablation, radiation therapy)
and used in superficial type of SCC or in in-operable
cases
• Local advanced or metastatic SCC are treated with
radiotherapy or chemotherapeutics (metotrexate or
cisplatin)
57. Literature for studies of Dermatovenereology
E-books:1. Clinical Dermatology (Carol Soutor, Maria K. Hordinsky)
http://accessmedicine.mhmedical.com/book.aspx?bookid=2184
2. Current Diagnosis and Treatment of Sexually Transmitted Diseases
http://accessmedicine.mhmedical.com/book.aspx?bookid=369
Books available in LSMU library:
Martic Rocken et al. Color Atlas of Dermatology, 2012
K. Wolff, R.A Johnson. Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology, 6 Eds.
Color Atlas & Synopsis of Sexually Transmitted Diseases, Third Edition, 2011









 Медицина
Медицина