Похожие презентации:
Psoriasis and lichen
1.
Lection 5 Psoriasis and lichenмараках марван якин нажи
Department of Dermatovenerology
1
2.
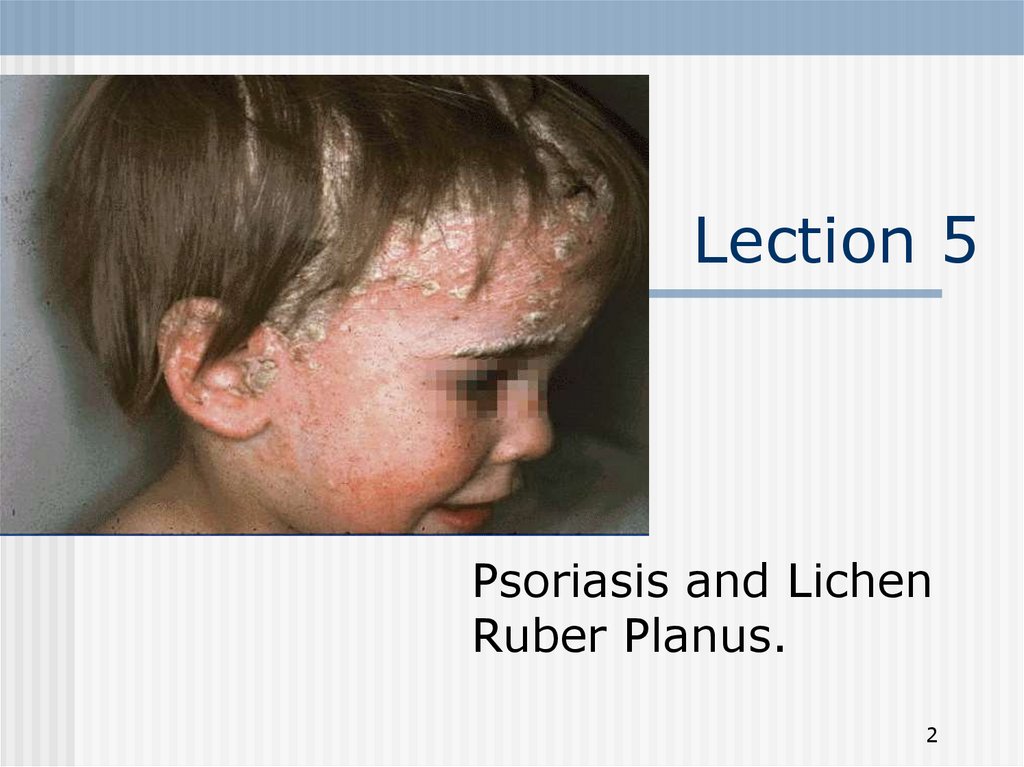
Lection 5Psoriasis and Lichen
Ruber Planus.
2
3.
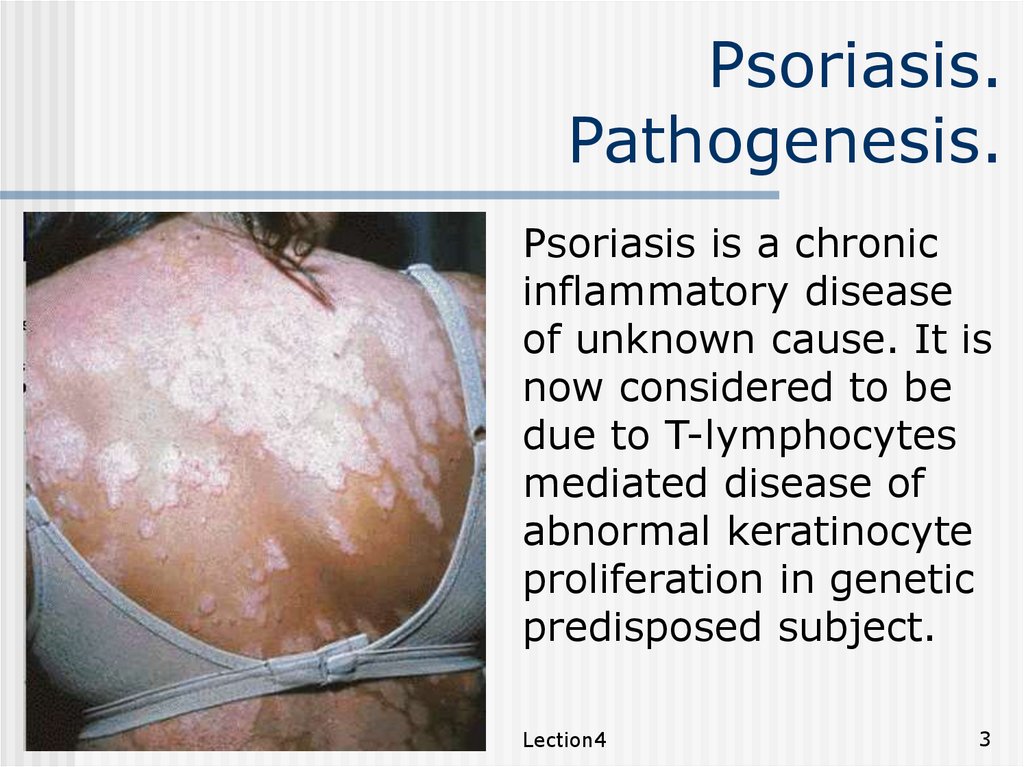
Psoriasis.Pathogenesis.
Psoriasis is a chronic
inflammatory disease
of unknown cause. It is
now considered to be
due to T-lymphocytes
mediated disease of
abnormal keratinocyte
proliferation in genetic
predisposed subject.
Lection4
3
4.
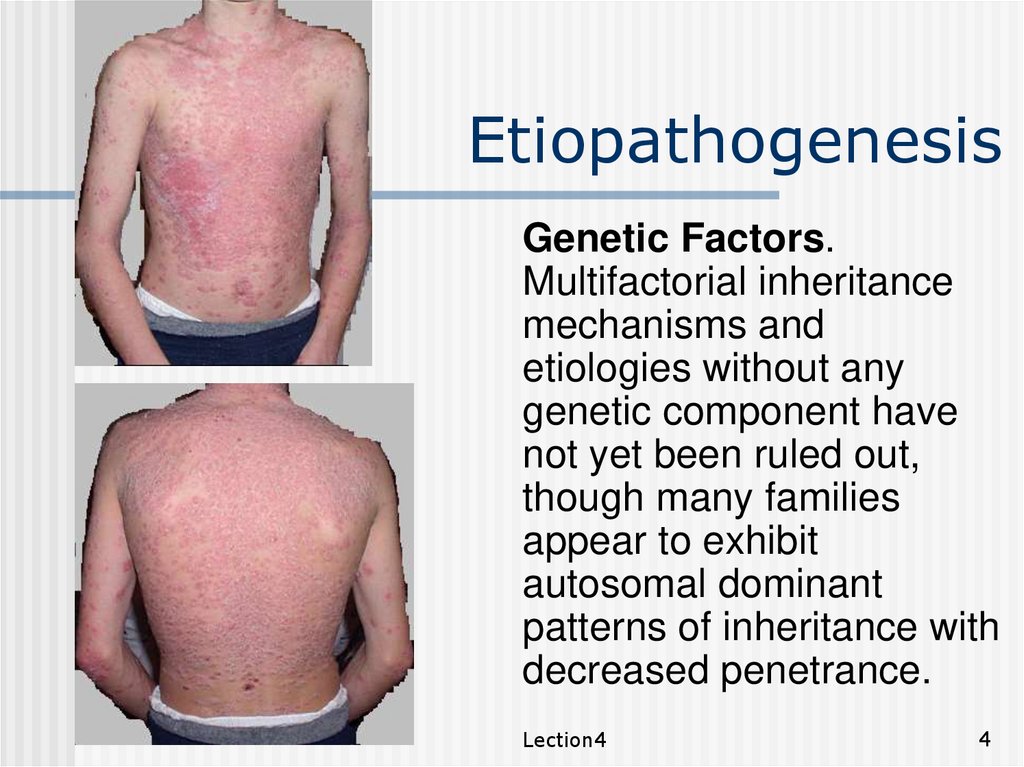
EtiopathogenesisGenetic Factors.
Multifactorial inheritance
mechanisms and
etiologies without any
genetic component have
not yet been ruled out,
though many families
appear to exhibit
autosomal dominant
patterns of inheritance with
decreased penetrance.
Lection4
4
5.
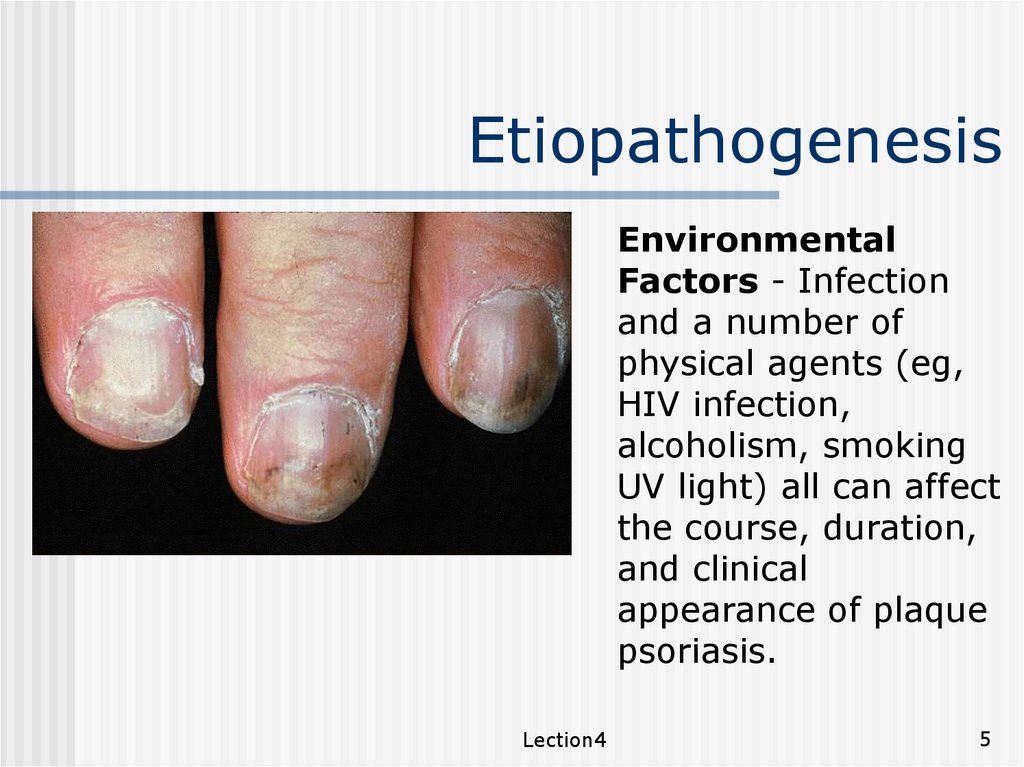
EtiopathogenesisEnvironmental
Factors - Infection
and a number of
physical agents (eg,
HIV infection,
alcoholism, smoking
UV light) all can affect
the course, duration,
and clinical
appearance of plaque
psoriasis.
Lection4
5
6.
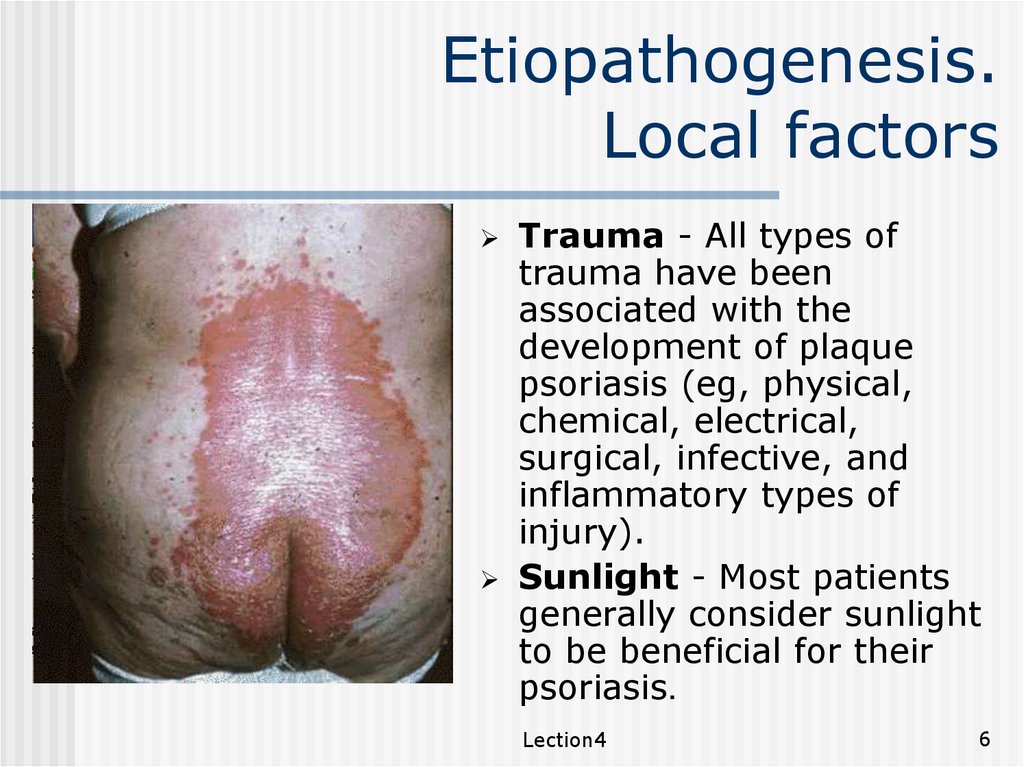
Etiopathogenesis.Local factors
Trauma - All types of
trauma have been
associated with the
development of plaque
psoriasis (eg, physical,
chemical, electrical,
surgical, infective, and
inflammatory types of
injury).
Sunlight - Most patients
generally consider sunlight
to be beneficial for their
psoriasis.
Lection4
6
7.
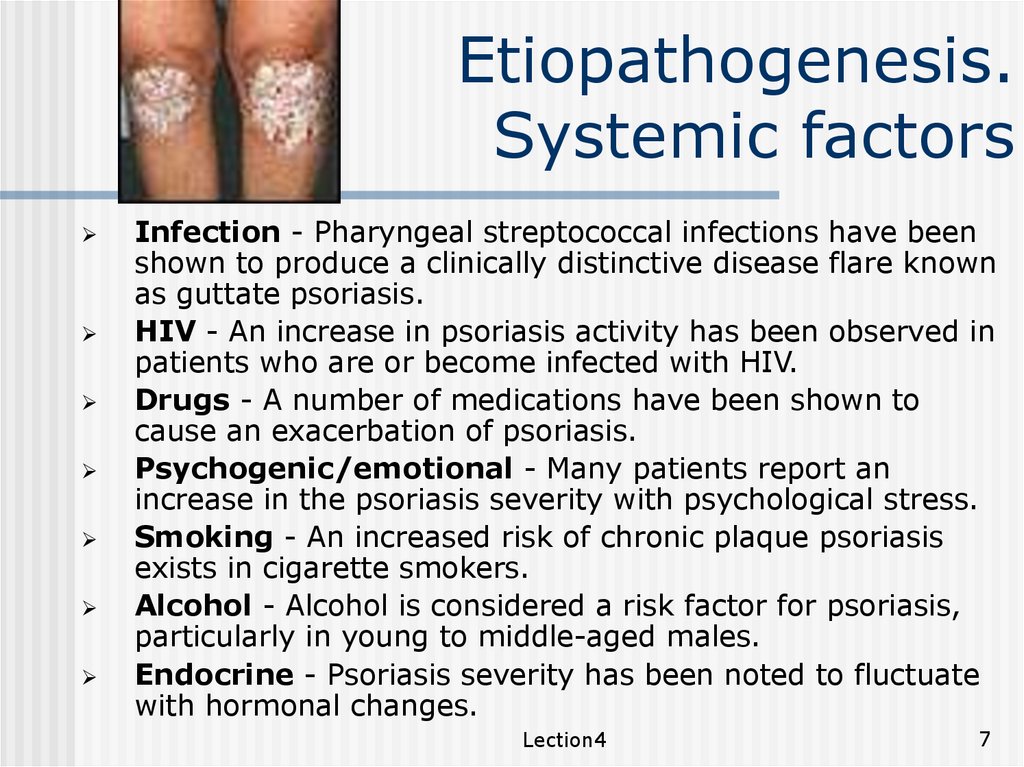
Etiopathogenesis.Systemic factors
Infection - Pharyngeal streptococcal infections have been
shown to produce a clinically distinctive disease flare known
as guttate psoriasis.
HIV - An increase in psoriasis activity has been observed in
patients who are or become infected with HIV.
Drugs - A number of medications have been shown to
cause an exacerbation of psoriasis.
Psychogenic/emotional - Many patients report an
increase in the psoriasis severity with psychological stress.
Smoking - An increased risk of chronic plaque psoriasis
exists in cigarette smokers.
Alcohol - Alcohol is considered a risk factor for psoriasis,
particularly in young to middle-aged males.
Endocrine - Psoriasis severity has been noted to fluctuate
with hormonal changes.
Lection4
7
8.
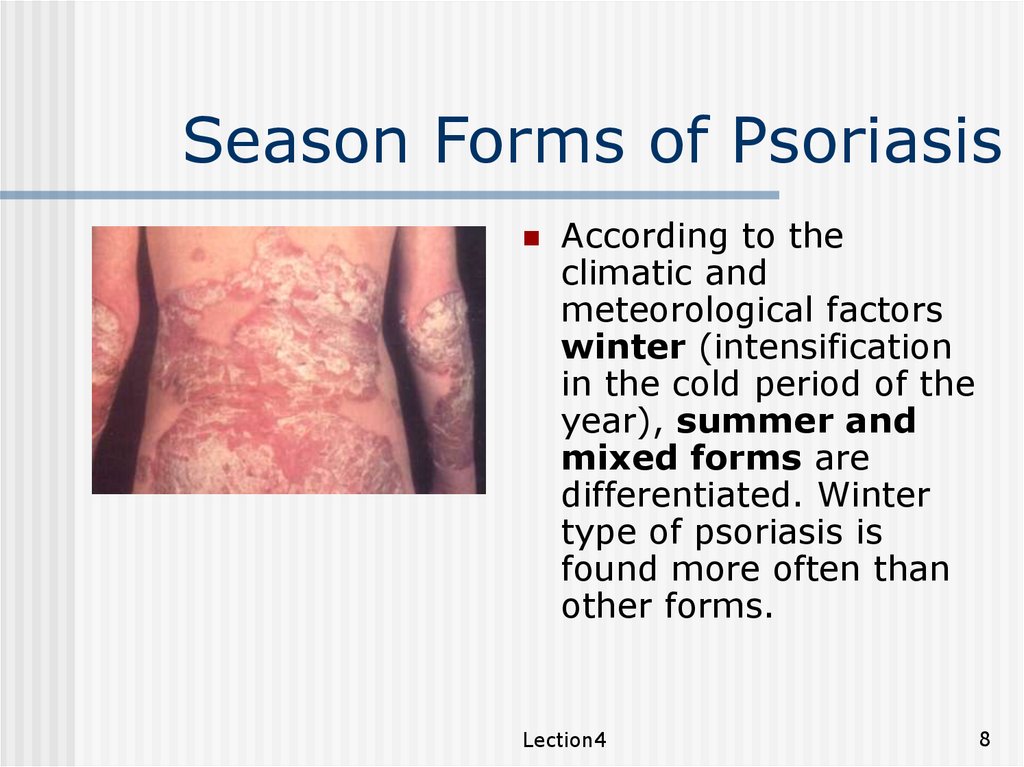
Season Forms of PsoriasisAccording to the
climatic and
meteorological factors
winter (intensification
in the cold period of the
year), summer and
mixed forms are
differentiated. Winter
type of psoriasis is
found more often than
other forms.
Lection4
8
9.
StagesStages. In the progress of clinical development three stages
of inflammatory process are distinguished: progressive,
hospital and regressive.
For the progressive stage characteristic features are
intensive itching, development of new papules, peripheral
growth of old papules, presence of the inflammatory crown
around the papule, Köbner’s phenomenon. (Fig. 6.)
At the hospital stage fresh lesions do not develop, the
peripheral crowns are absent, Köbner’s phenomenon is not
seen.
At the regressive stage the lesions are compressed, get
pale,
the
desquamation
decreases
or
stops,
depigmentation of the crown takes place around the
papule (pseudoatrophied Woron’s crown) and resolution of
the lesions.
Lection4
9
10.
Clinical classificationNon-pustular Psoriasis
Chronic Plague type
Acute Guttate
Inverse, flexural
Erythrodermic
Regional: palms and soles, nails
Sebo-psoriasis
Lection4
10
11.
Clinical classificationPustular Psoriasis
Generalized Pustular psoriasis (von Zumbusch)
Localized pustular psoriasis of palms & soles
Psoriasis with Arthropathy
oligoarticular asymmetrical arthritis, symmetrical
involving small joints of fingers likes rheumatoid
arthritis, classical distal arthropathy involving
distal interphalangeal joints, destructive arthritis
mutilans and psoriatic spondyloarthropathy which
is similar to ankylosing spondylitis.
Lection4
11
12.
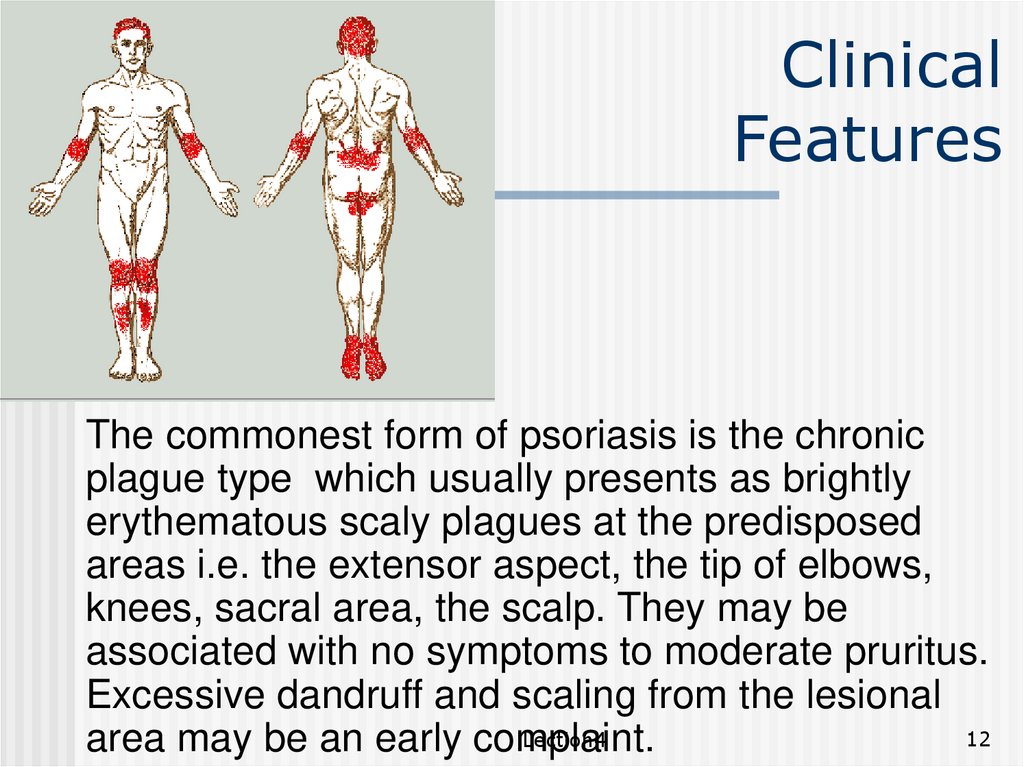
ClinicalFeatures
The commonest form of psoriasis is the chronic
plague type which usually presents as brightly
erythematous scaly plagues at the predisposed
areas i.e. the extensor aspect, the tip of elbows,
knees, sacral area, the scalp. They may be
associated with no symptoms to moderate pruritus.
Excessive dandruff and scaling from the lesional
12
Lection4
area may be an early complaint.
13.
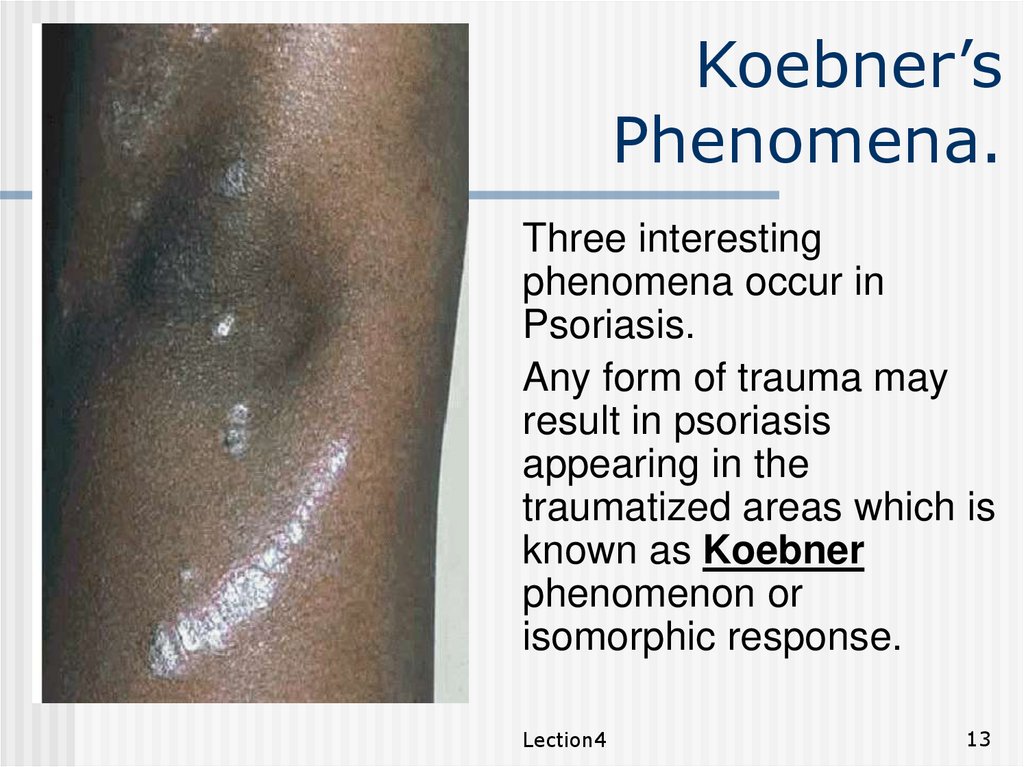
Koebner’sPhenomena.
Three interesting
phenomena occur in
Psoriasis.
Any form of trauma may
result in psoriasis
appearing in the
traumatized areas which is
known as Koebner
phenomenon or
isomorphic response.
Lection4
13
14.
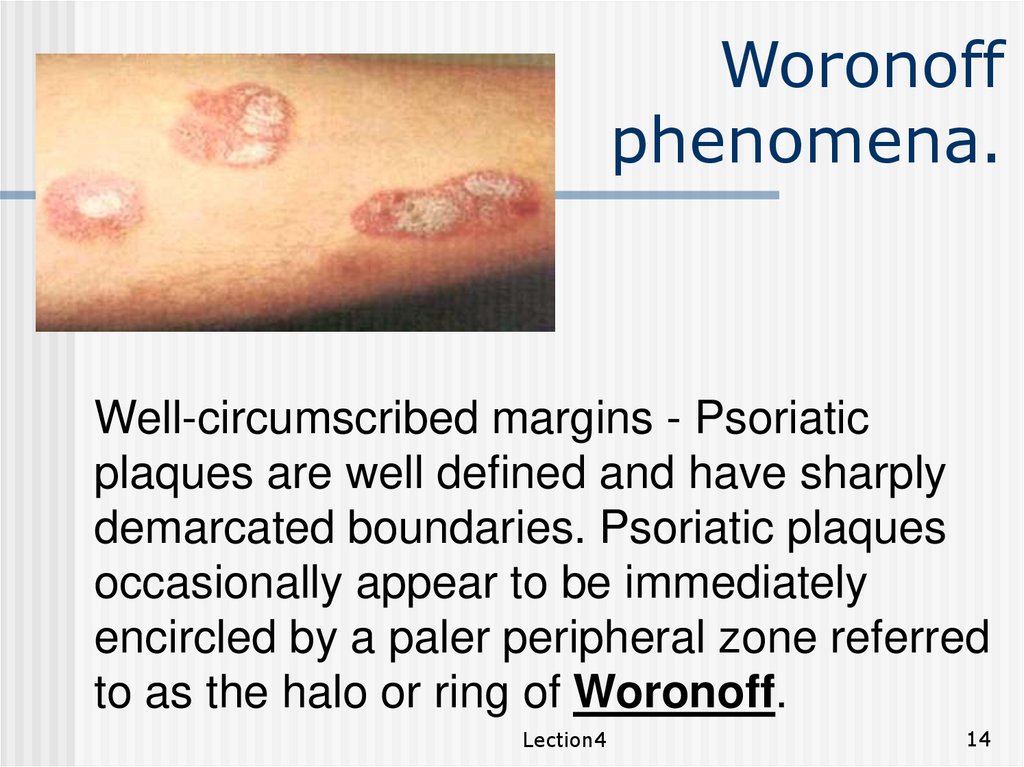
Woronoffphenomena.
Well-circumscribed margins - Psoriatic
plaques are well defined and have sharply
demarcated boundaries. Psoriatic plaques
occasionally appear to be immediately
encircled by a paler peripheral zone referred
to as the halo or ring of Woronoff.
Lection4
14
15.
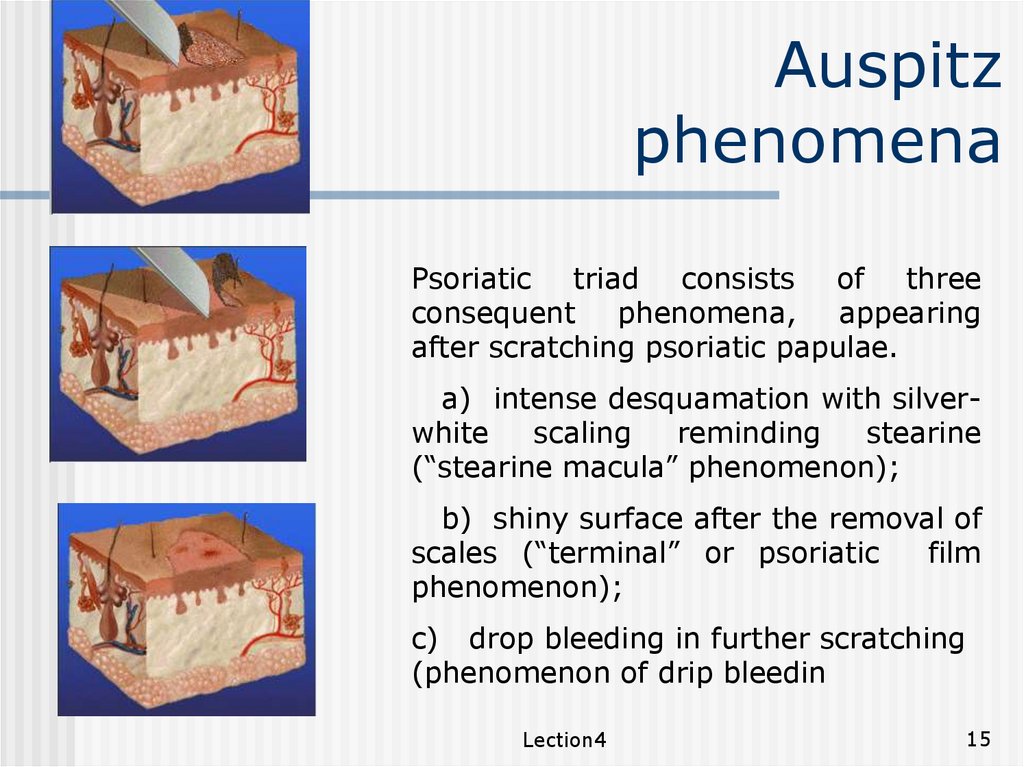
Auspitzphenomena
Psoriatic triad consists of three
consequent phenomena, appearing
after scratching psoriatic papulae.
a) intense desquamation with silverwhite
scaling
reminding
stearine
(“stearine macula” phenomenon);
b) shiny surface after the removal of
scales (“terminal” or psoriatic
film
phenomenon);
c) drop bleeding in further scratching
(phenomenon of drip bleedin
Lection4
15
16.
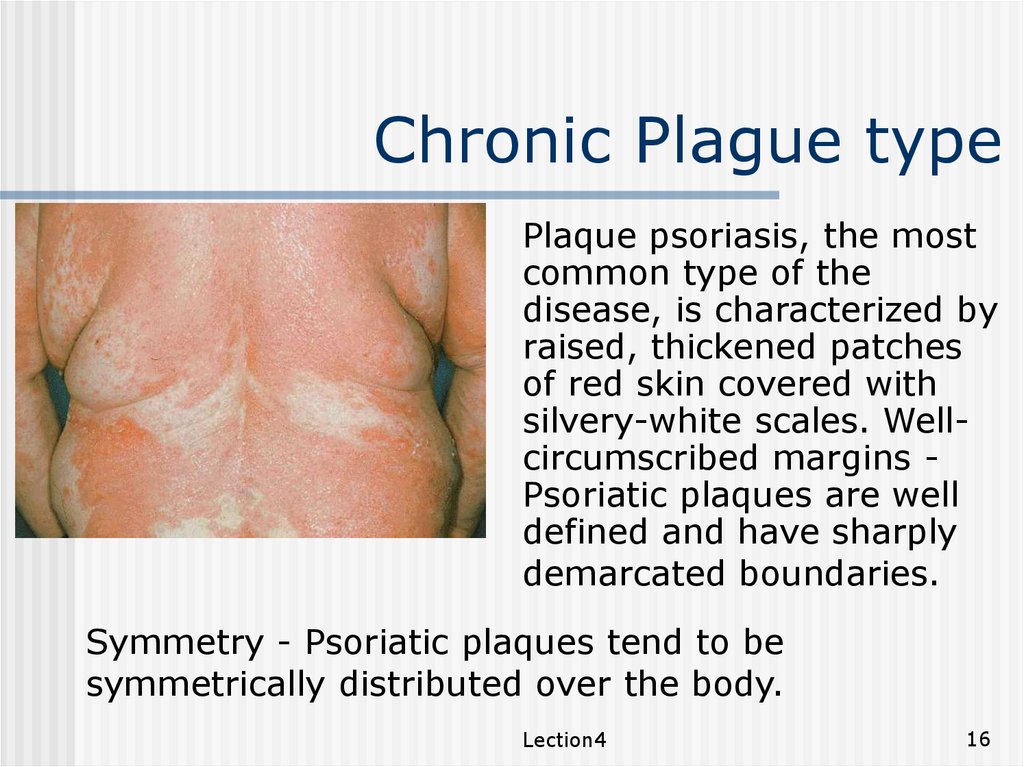
Chronic Plague typePlaque psoriasis, the most
common type of the
disease, is characterized by
raised, thickened patches
of red skin covered with
silvery-white scales. Wellcircumscribed margins Psoriatic plaques are well
defined and have sharply
demarcated boundaries.
Symmetry - Psoriatic plaques tend to be
symmetrically distributed over the body.
Lection4
16
17.
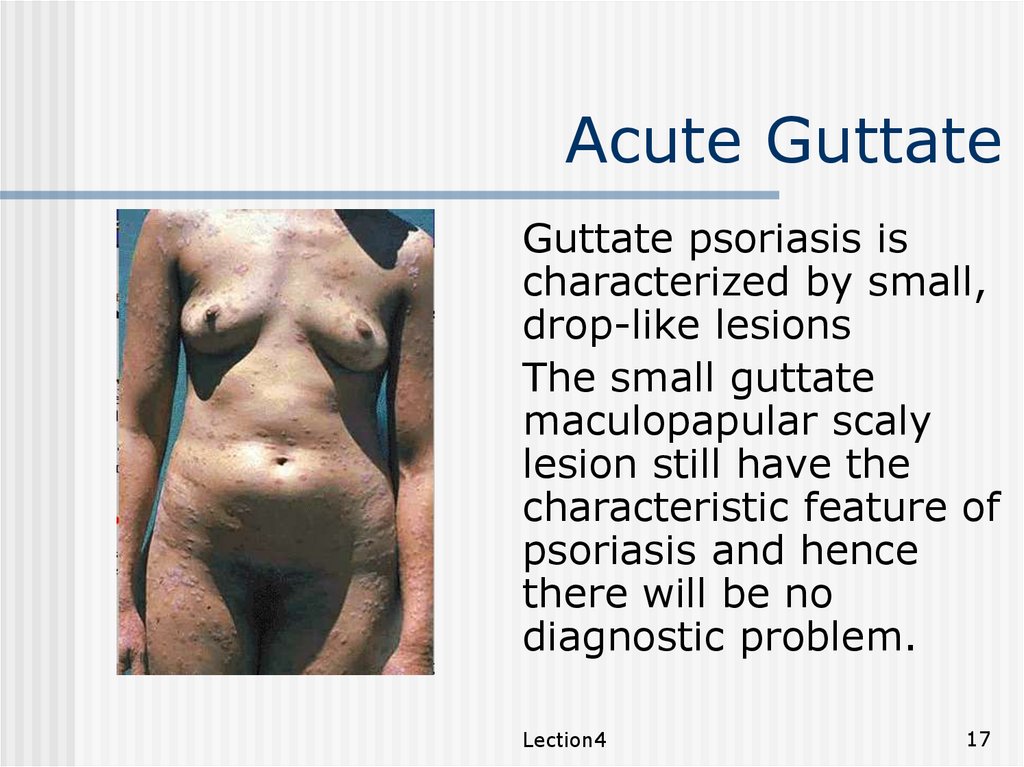
Acute GuttateGuttate psoriasis is
characterized by small,
drop-like lesions
The small guttate
maculopapular scaly
lesion still have the
characteristic feature of
psoriasis and hence
there will be no
diagnostic problem.
Lection4
17
18.
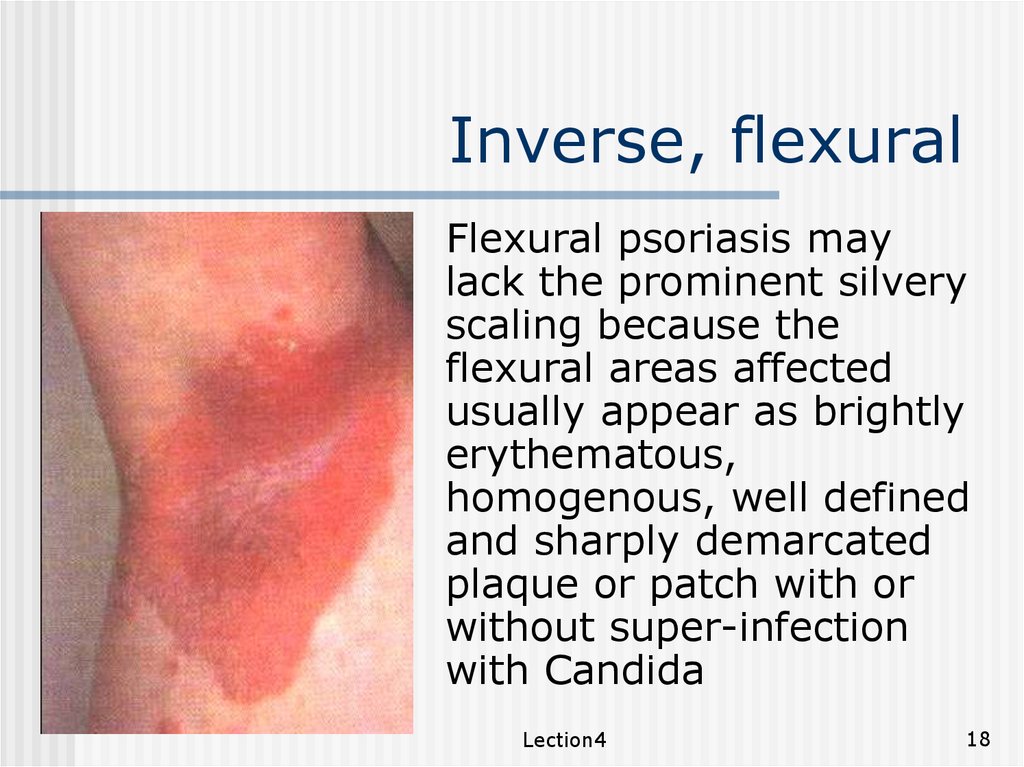
Inverse, flexuralFlexural psoriasis may
lack the prominent silvery
scaling because the
flexural areas affected
usually appear as brightly
erythematous,
homogenous, well defined
and sharply demarcated
plaque or patch with or
without super-infection
with Candida
Lection4
18
19.
Erythrodermicpsoriasis
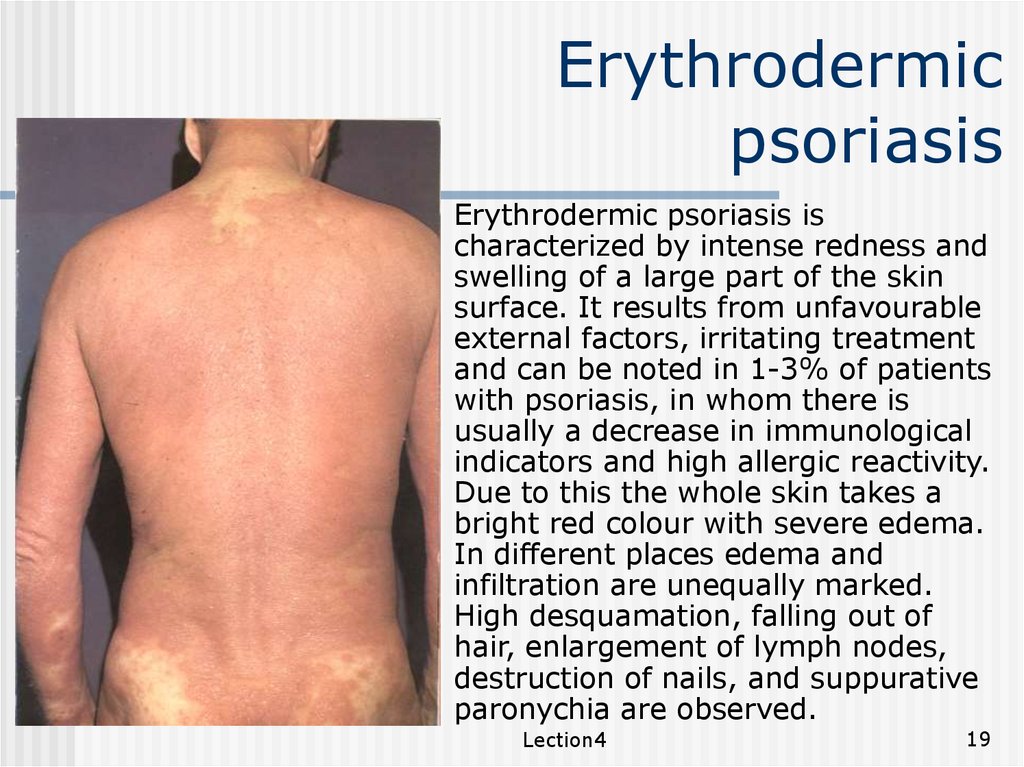
Erythrodermic psoriasis is
characterized by intense redness and
swelling of a large part of the skin
surface. It results from unfavourable
external factors, irritating treatment
and can be noted in 1-3% of patients
with psoriasis, in whom there is
usually a decrease in immunological
indicators and high allergic reactivity.
Due to this the whole skin takes a
bright red colour with severe edema.
In different places edema and
infiltration are unequally marked.
High desquamation, falling out of
hair, enlargement of lymph nodes,
destruction of nails, and suppurative
paronychia are observed.
Lection4
19
20.
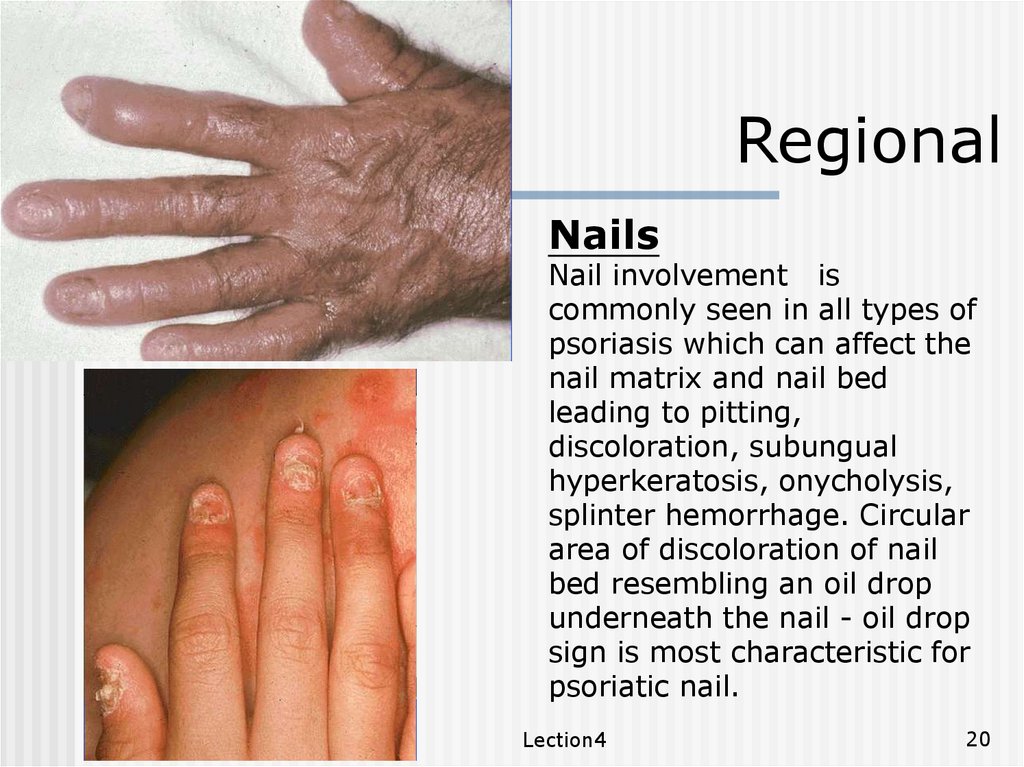
RegionalNails
Nail involvement is
commonly seen in all types of
psoriasis which can affect the
nail matrix and nail bed
leading to pitting,
discoloration, subungual
hyperkeratosis, onycholysis,
splinter hemorrhage. Circular
area of discoloration of nail
bed resembling an oil drop
underneath the nail - oil drop
sign is most characteristic for
psoriatic nail.
Lection4
20
21.
Seborrheicpsoriasis
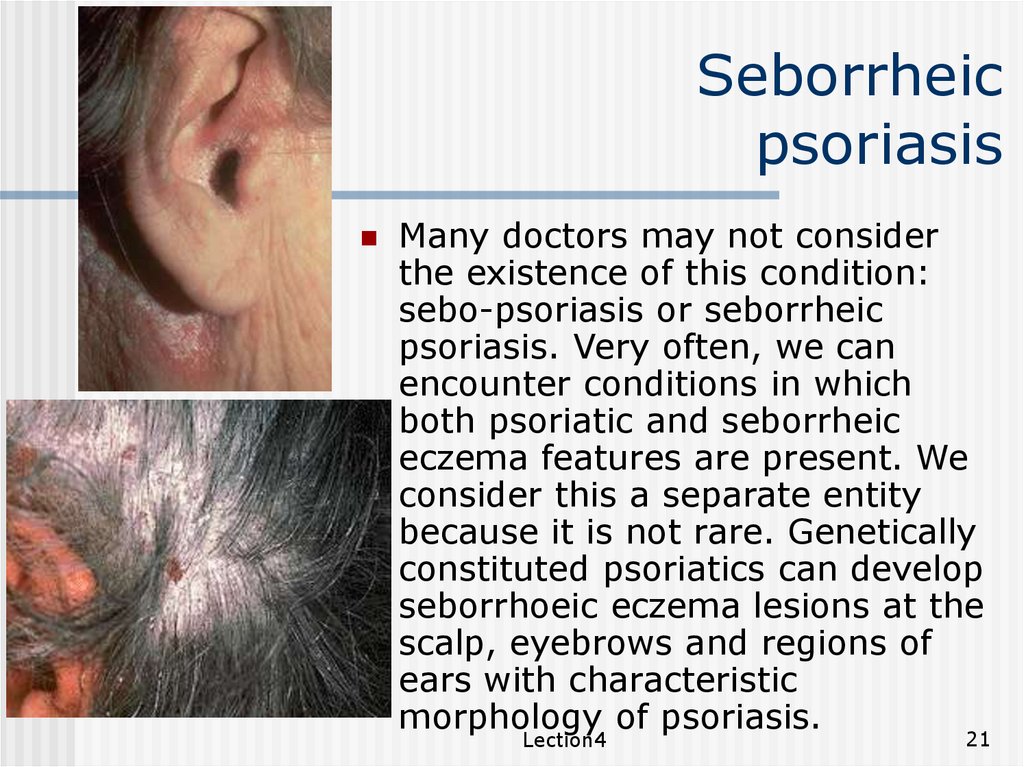
Many doctors may not consider
the existence of this condition:
sebo-psoriasis or seborrheic
psoriasis. Very often, we can
encounter conditions in which
both psoriatic and seborrheic
eczema features are present. We
consider this a separate entity
because it is not rare. Genetically
constituted psoriatics can develop
seborrhoeic eczema lesions at the
scalp, eyebrows and regions of
ears with characteristic
morphology of psoriasis.
Lection4
21
22.
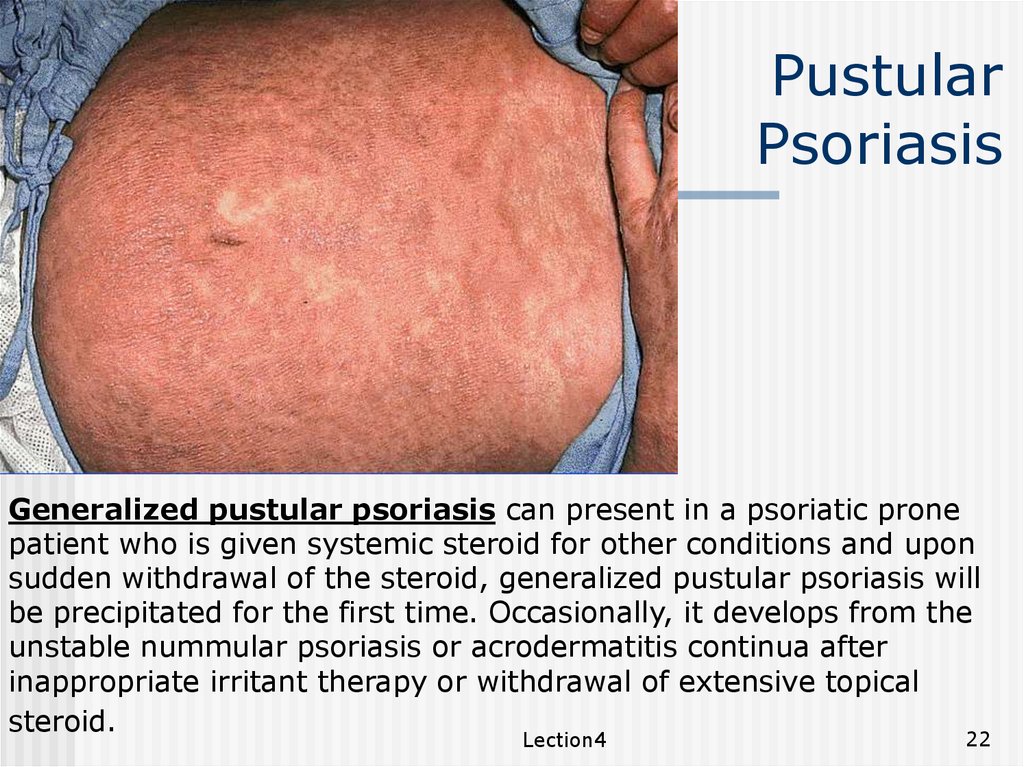
PustularPsoriasis
Generalized pustular psoriasis can present in a psoriatic prone
patient who is given systemic steroid for other conditions and upon
sudden withdrawal of the steroid, generalized pustular psoriasis will
be precipitated for the first time. Occasionally, it develops from the
unstable nummular psoriasis or acrodermatitis continua after
inappropriate irritant therapy or withdrawal of extensive topical
steroid.
Lection4
22
23.
PustularPsoriasis
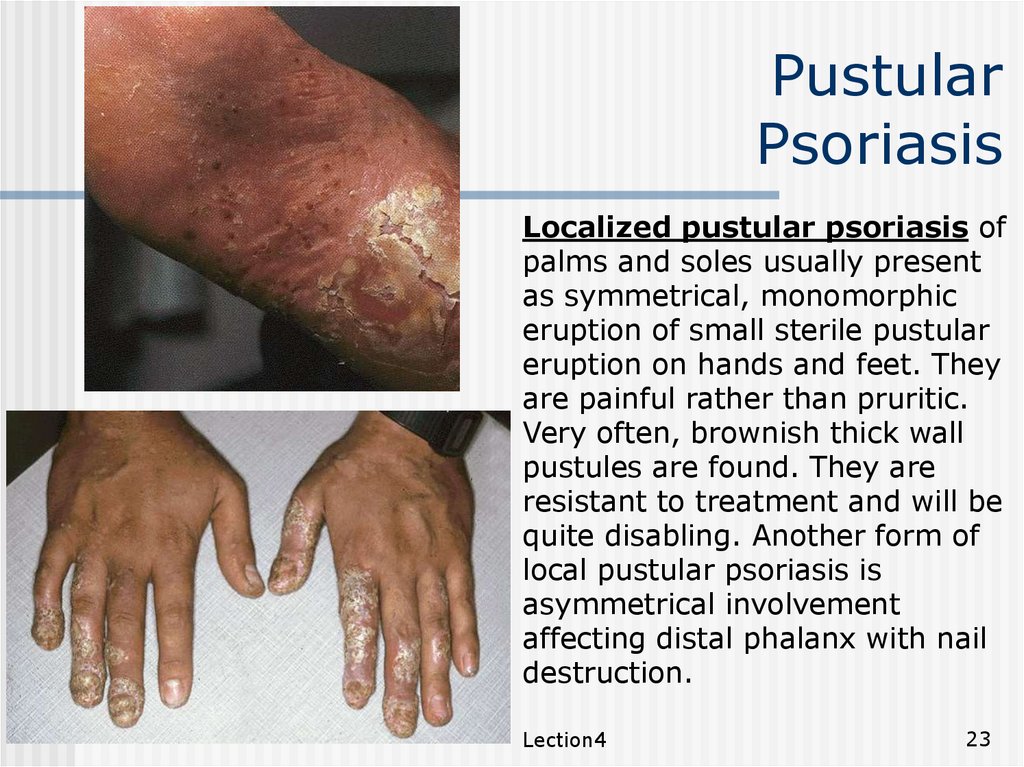
Localized pustular psoriasis of
palms and soles usually present
as symmetrical, monomorphic
eruption of small sterile pustular
eruption on hands and feet. They
are painful rather than pruritic.
Very often, brownish thick wall
pustules are found. They are
resistant to treatment and will be
quite disabling. Another form of
local pustular psoriasis is
asymmetrical involvement
affecting distal phalanx with nail
destruction.
Lection4
23
24.
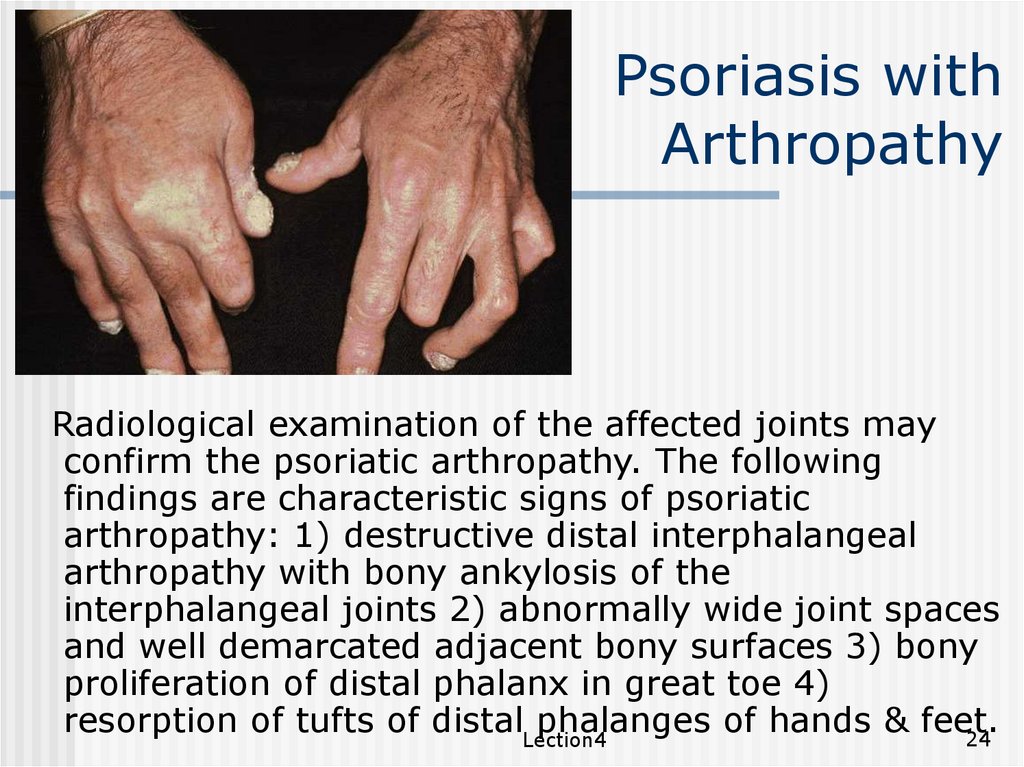
Psoriasis withArthropathy
Radiological examination of the affected joints may
confirm the psoriatic arthropathy. The following
findings are characteristic signs of psoriatic
arthropathy: 1) destructive distal interphalangeal
arthropathy with bony ankylosis of the
interphalangeal joints 2) abnormally wide joint spaces
and well demarcated adjacent bony surfaces 3) bony
proliferation of distal phalanx in great toe 4)
resorption of tufts of distalLection4
phalanges of hands & feet.
24
25.
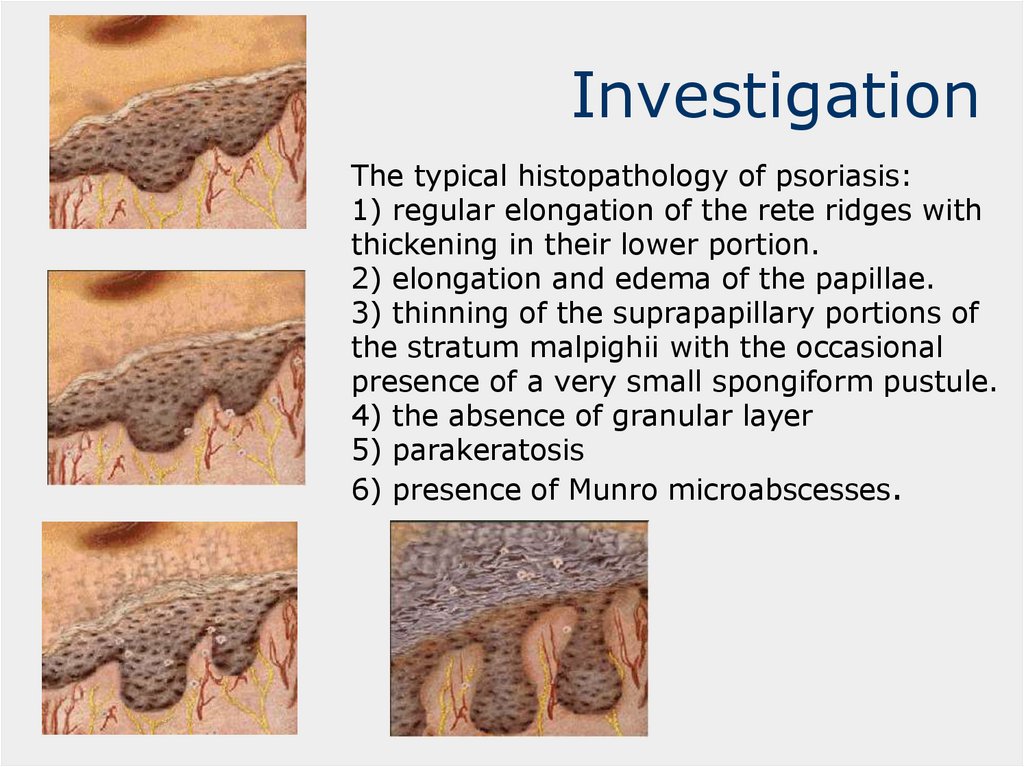
InvestigationThe typical histopathology of psoriasis:
1) regular elongation of the rete ridges with
thickening in their lower portion.
2) elongation and edema of the papillae.
3) thinning of the suprapapillary portions of
the stratum malpighii with the occasional
presence of a very small spongiform pustule.
4) the absence of granular layer
5) parakeratosis
6) presence of Munro microabscesses.
26.
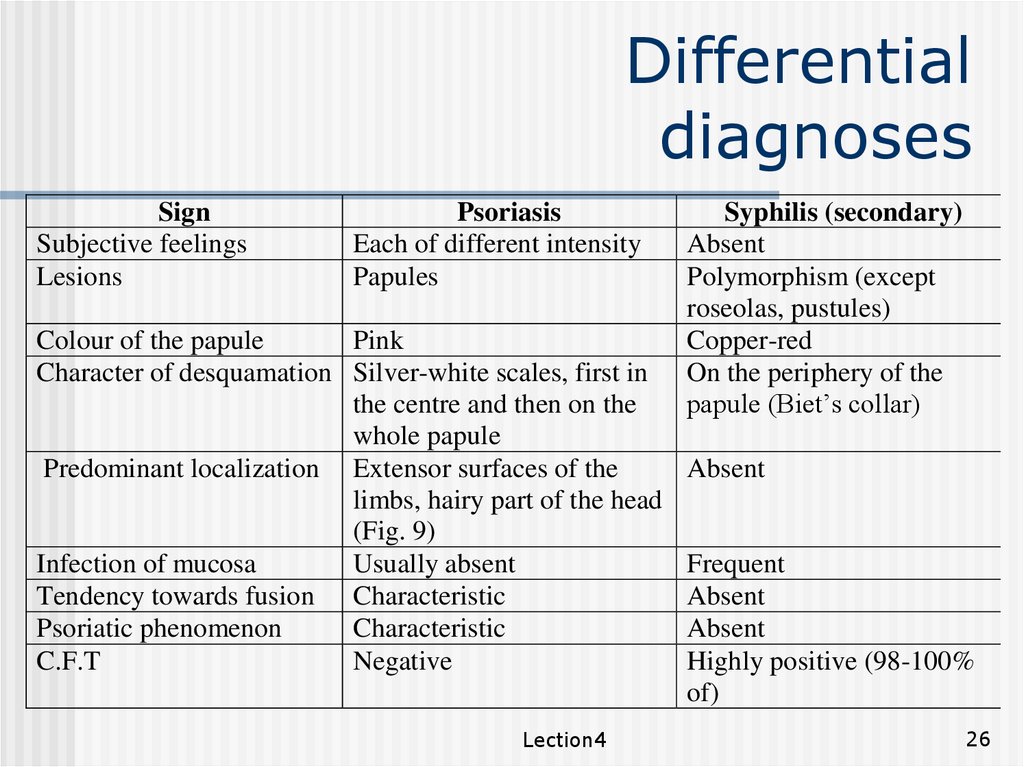
Differentialdiagnoses
Sign
Subjective feelings
Lesions
Psoriasis
Each of different intensity
Papules
Colour of the papule
Pink
Character of desquamation Silver-white scales, first in
the centre and then on the
whole papule
Predominant localization Extensor surfaces of the
limbs, hairy part of the head
(Fig. 9)
Infection of mucosa
Usually absent
Tendency towards fusion Characteristic
Psoriatic phenomenon
Characteristic
C.F.T
Negative
Lection4
Syphilis (secondary)
Absent
Polymorphism (except
roseolas, pustules)
Copper-red
On the periphery of the
papule (Biet’s collar)
Absent
Frequent
Absent
Absent
Highly positive (98-100%
of)
26
27.
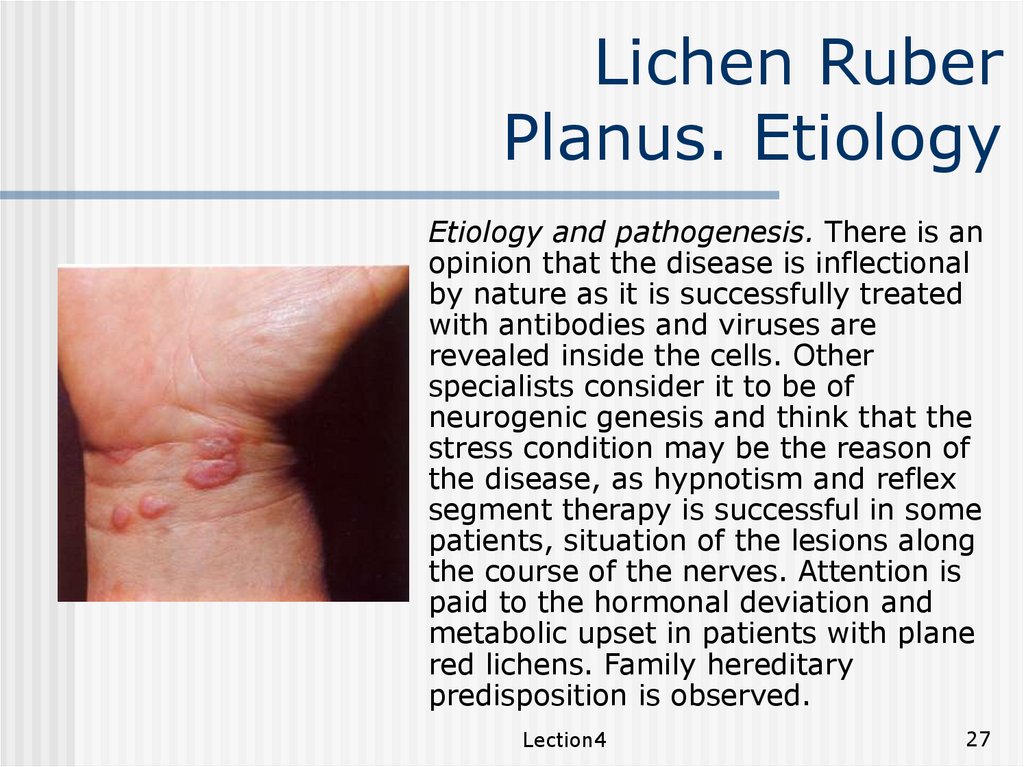
Lichen RuberPlanus. Etiology
Etiology and pathogenesis. There is an
opinion that the disease is inflectional
by nature as it is successfully treated
with antibodies and viruses are
revealed inside the cells. Other
specialists consider it to be of
neurogenic genesis and think that the
stress condition may be the reason of
the disease, as hypnotism and reflex
segment therapy is successful in some
patients, situation of the lesions along
the course of the nerves. Attention is
paid to the hormonal deviation and
metabolic upset in patients with plane
red lichens. Family hereditary
predisposition is observed.
Lection4
27
28.
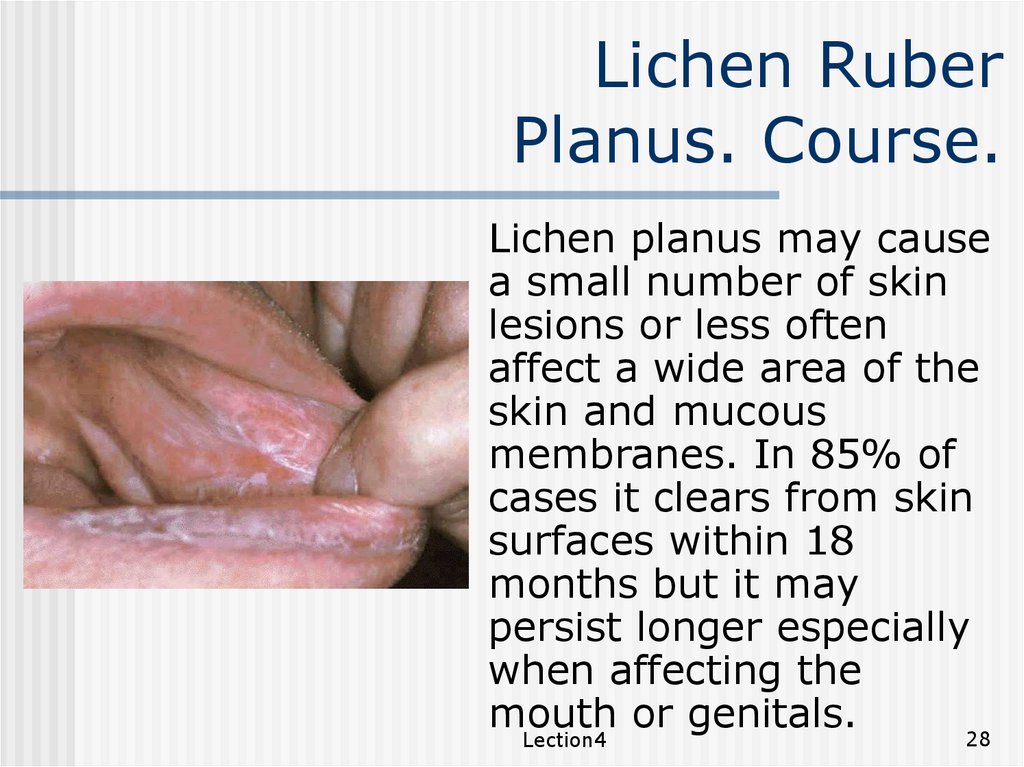
Lichen RuberPlanus. Course.
Lichen planus may cause
a small number of skin
lesions or less often
affect a wide area of the
skin and mucous
membranes. In 85% of
cases it clears from skin
surfaces within 18
months but it may
persist longer especially
when affecting the
mouth
or
genitals.
28
Lection4
29.
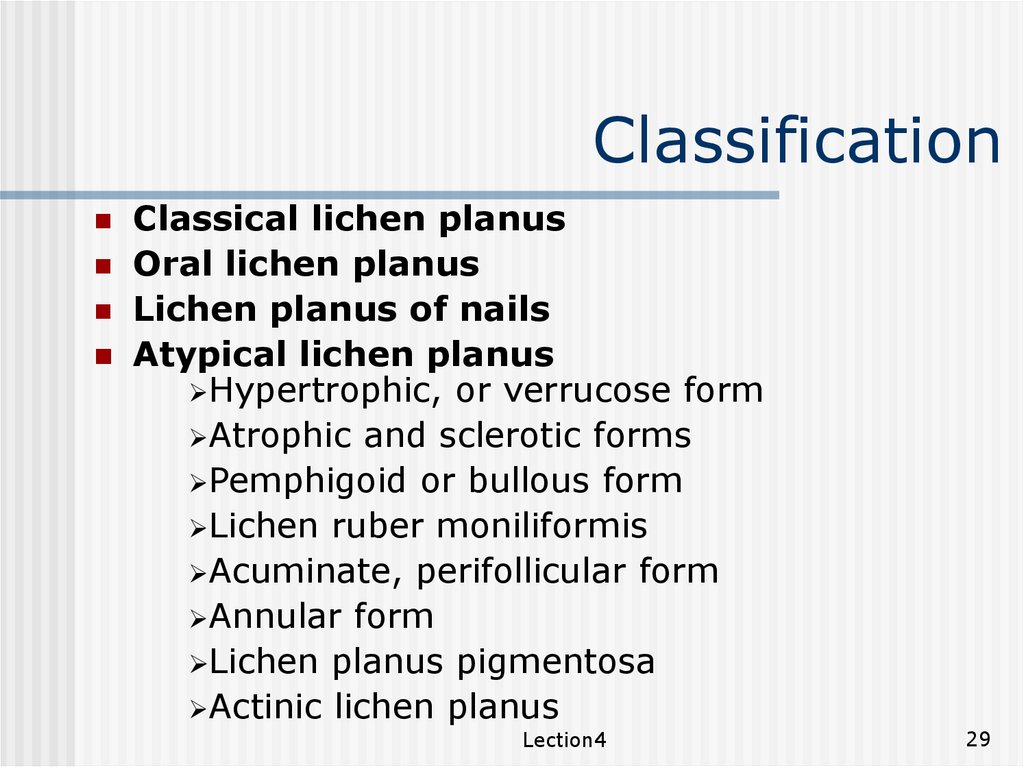
ClassificationClassical lichen planus
Oral lichen planus
Lichen planus of nails
Atypical lichen planus
Hypertrophic, or verrucose form
Atrophic and sclerotic forms
Pemphigoid or bullous form
Lichen ruber moniliformis
Acuminate, perifollicular form
Annular form
Lichen planus pigmentosa
Actinic lichen planus
Lection4
29
30.
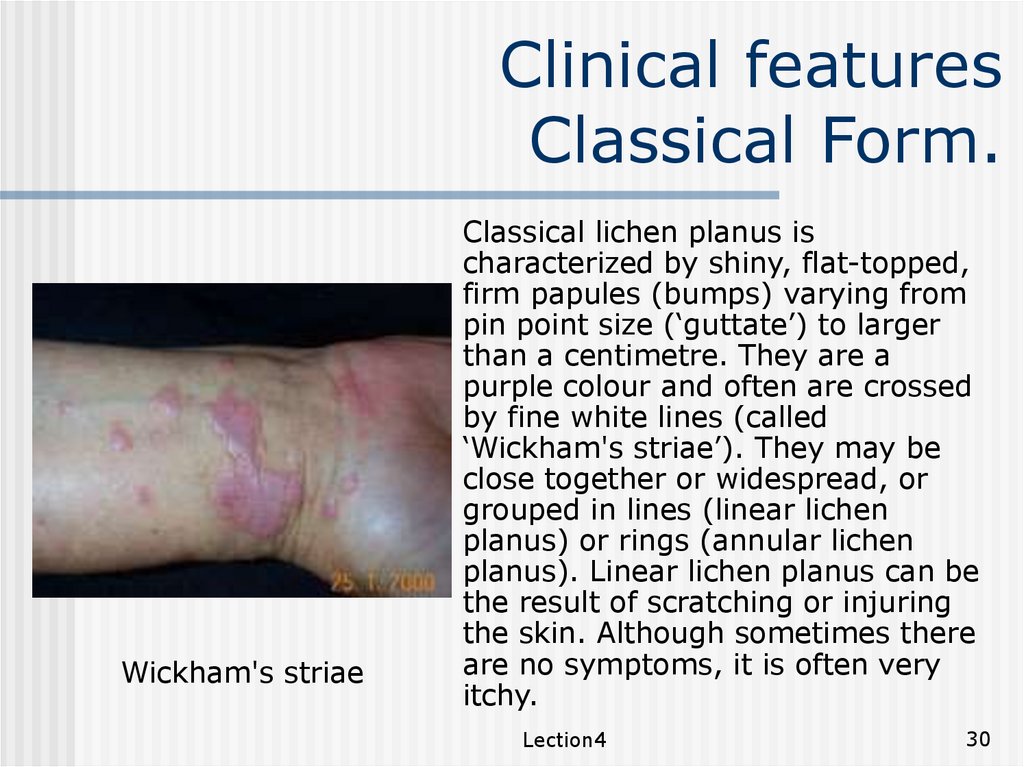
Clinical featuresClassical Form.
Wickham's striae
Classical lichen planus is
characterized by shiny, flat-topped,
firm papules (bumps) varying from
pin point size (‘guttate’) to larger
than a centimetre. They are a
purple colour and often are crossed
by fine white lines (called
‘Wickham's striae’). They may be
close together or widespread, or
grouped in lines (linear lichen
planus) or rings (annular lichen
planus). Linear lichen planus can be
the result of scratching or injuring
the skin. Although sometimes there
are no symptoms, it is often very
itchy.
Lection4
30
31.
Clinical features.Hyperpigmentation.
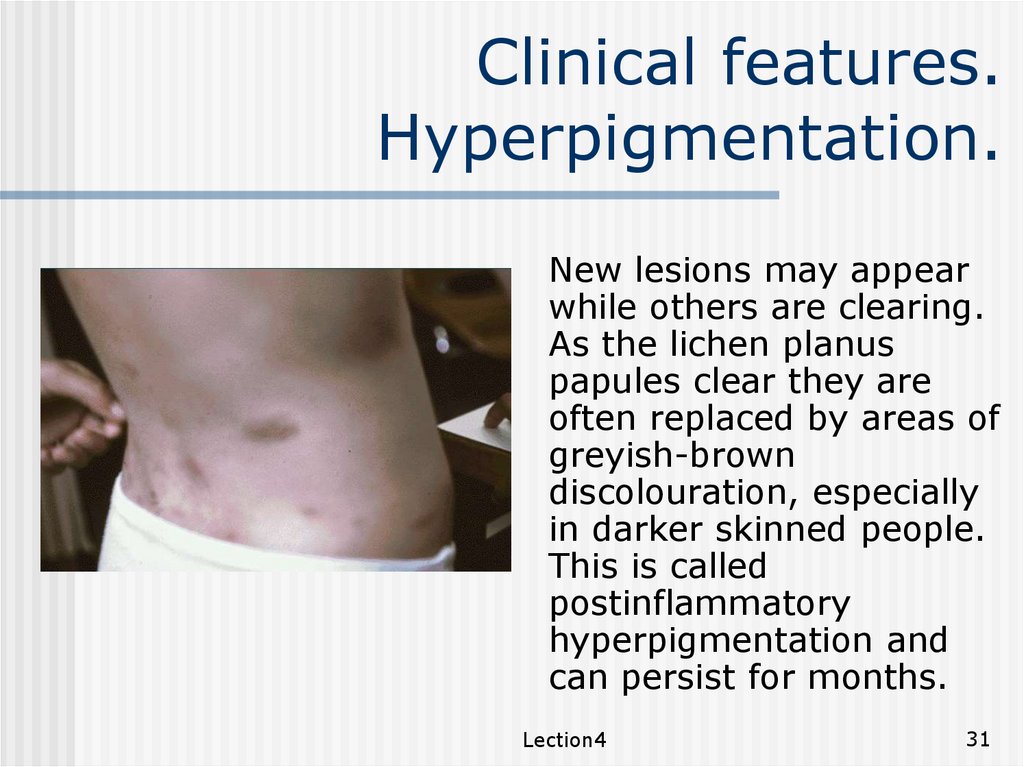
New lesions may appear
while others are clearing.
As the lichen planus
papules clear they are
often replaced by areas of
greyish-brown
discolouration, especially
in darker skinned people.
This is called
postinflammatory
hyperpigmentation and
can persist for months.
Lection4
31
32.
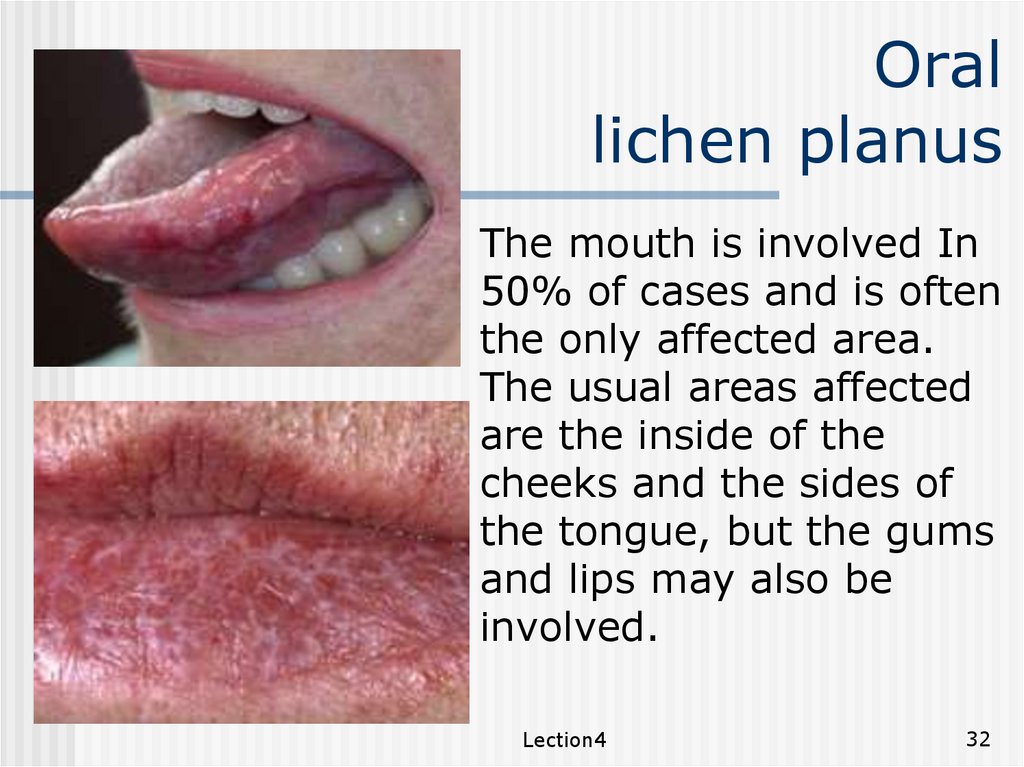
Orallichen planus
The mouth is involved In
50% of cases and is often
the only affected area.
The usual areas affected
are the inside of the
cheeks and the sides of
the tongue, but the gums
and lips may also be
involved.
Lection4
32
33.
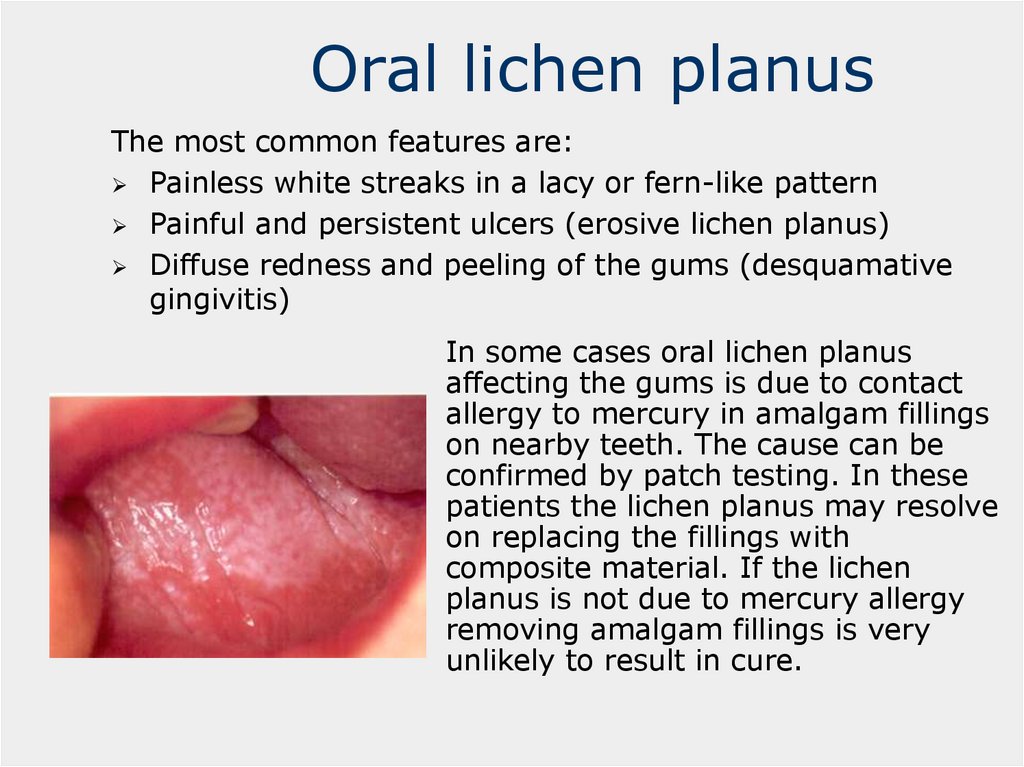
Oral lichen planusThe most common features are:
Painless white streaks in a lacy or fern-like pattern
Painful and persistent ulcers (erosive lichen planus)
Diffuse redness and peeling of the gums (desquamative
gingivitis)
In some cases oral lichen planus
affecting the gums is due to contact
allergy to mercury in amalgam fillings
on nearby teeth. The cause can be
confirmed by patch testing. In these
patients the lichen planus may resolve
on replacing the fillings with
composite material. If the lichen
planus is not due to mercury allergy
removing amalgam fillings is very
unlikely to result in cure.
34.
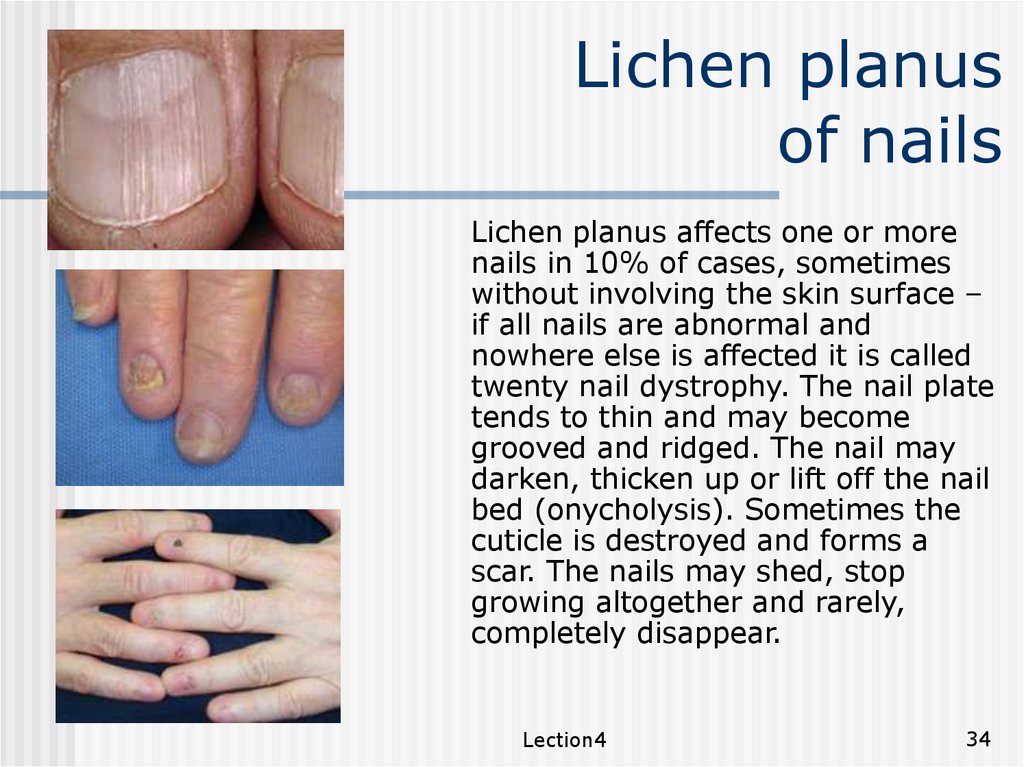
Lichen planusof nails
Lichen planus affects one or more
nails in 10% of cases, sometimes
without involving the skin surface –
if all nails are abnormal and
nowhere else is affected it is called
twenty nail dystrophy. The nail plate
tends to thin and may become
grooved and ridged. The nail may
darken, thicken up or lift off the nail
bed (onycholysis). Sometimes the
cuticle is destroyed and forms a
scar. The nails may shed, stop
growing altogether and rarely,
completely disappear.
Lection4
34
35.
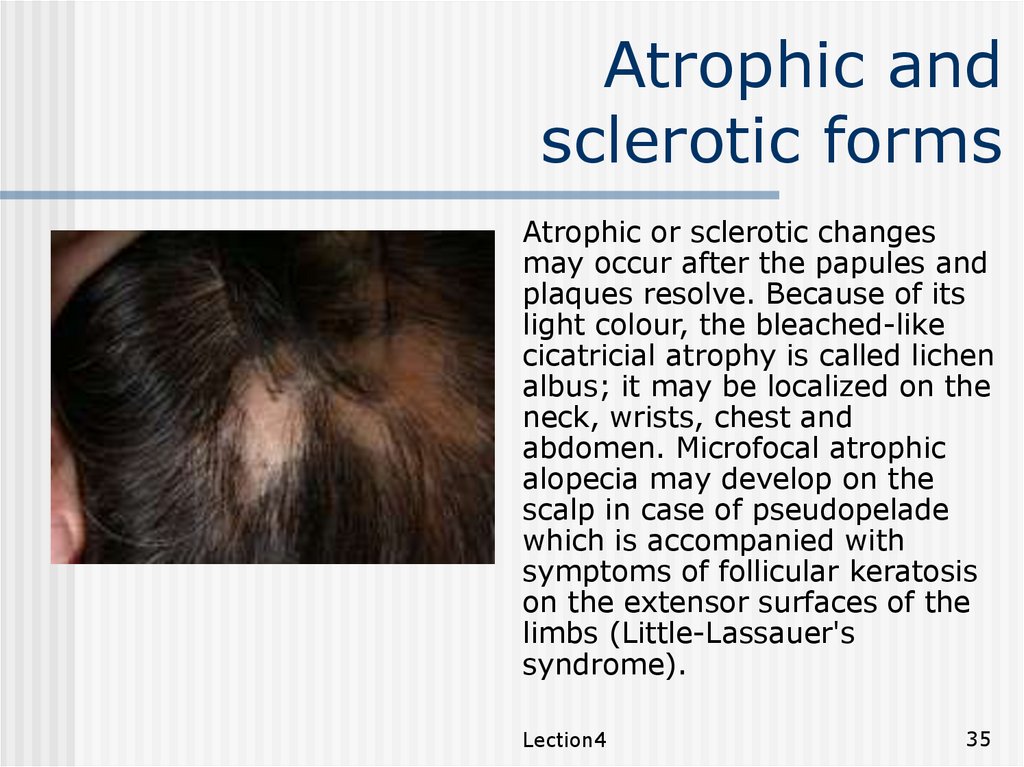
Atrophic andsclerotic forms
Pseudopelade
Atrophic or sclerotic changes
may occur after the papules and
plaques resolve. Because of its
light colour, the bleached-like
cicatricial atrophy is called lichen
albus; it may be localized on the
neck, wrists, chest and
abdomen. Microfocal atrophic
alopecia may develop on the
scalp in case of pseudopelade
which is accompanied with
symptoms of follicular keratosis
on the extensor surfaces of the
limbs (Little-Lassauer's
syndrome).
Lection4
35
36.
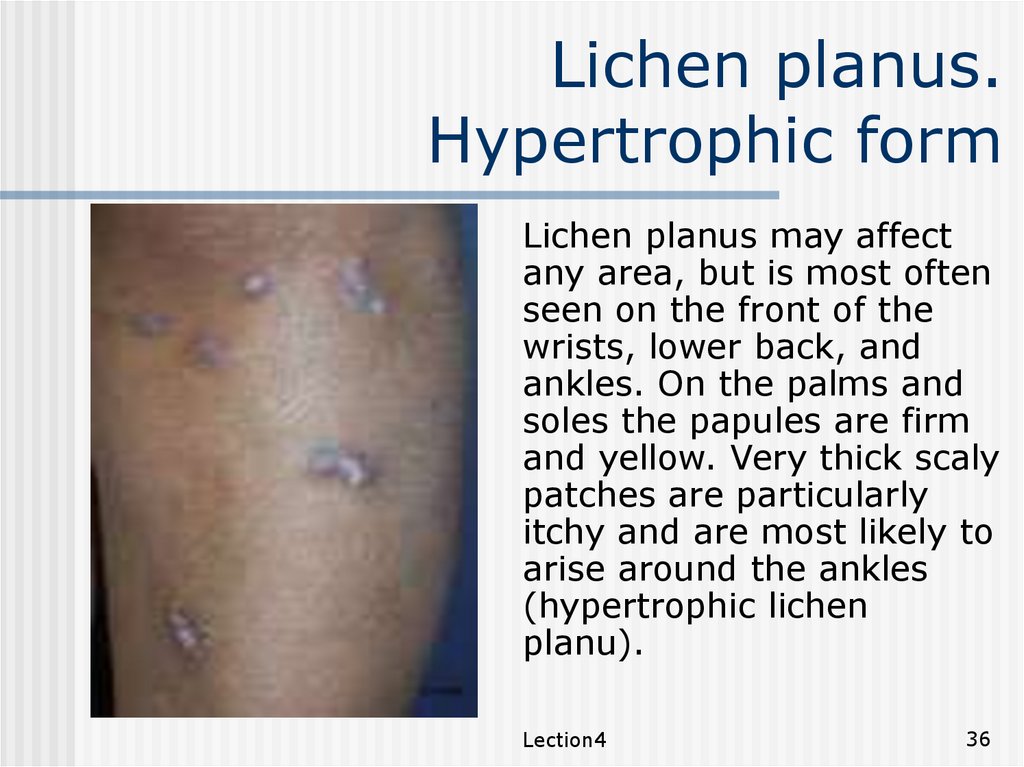
Lichen planus.Hypertrophic form
Lichen planus may affect
any area, but is most often
seen on the front of the
wrists, lower back, and
ankles. On the palms and
soles the papules are firm
and yellow. Very thick scaly
patches are particularly
itchy and are most likely to
arise around the ankles
(hypertrophic lichen
planu).
Lection4
36
37.
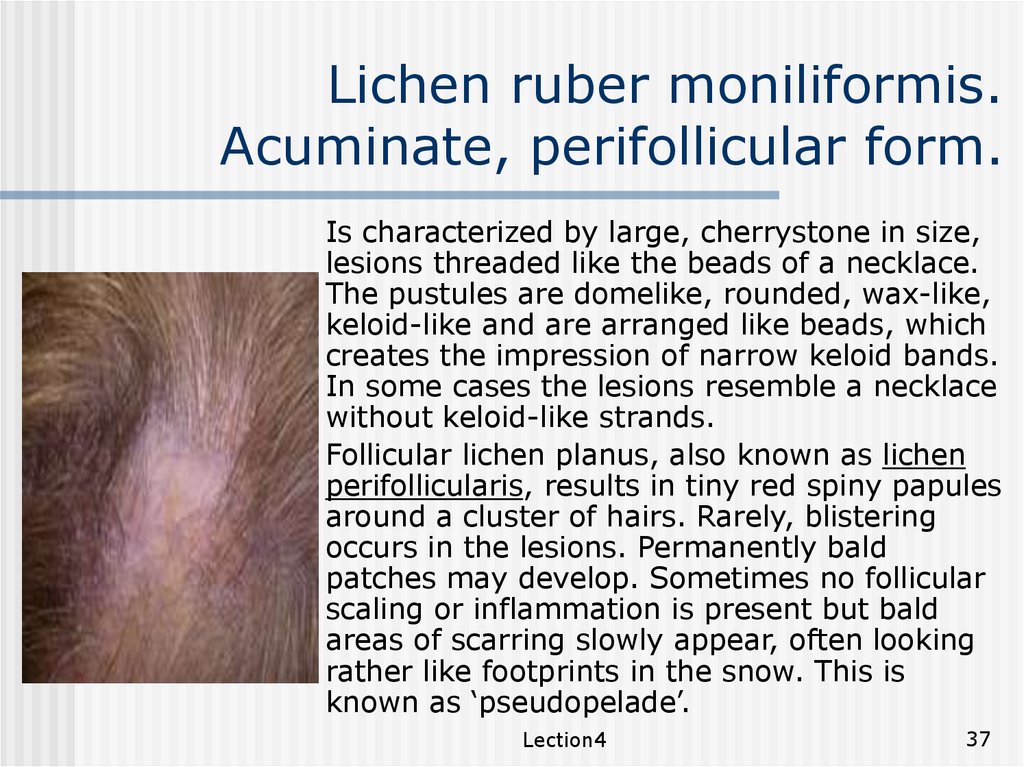
Lichen ruber moniliformis.Acuminate, perifollicular form.
Lichen planopilaris
Is characterized by large, cherrystone in size,
lesions threaded like the beads of a necklace.
The pustules are domelike, rounded, wax-like,
keloid-like and are arranged like beads, which
creates the impression of narrow keloid bands.
In some cases the lesions resemble a necklace
without keloid-like strands.
Follicular lichen planus, also known as lichen
perifollicularis, results in tiny red spiny papules
around a cluster of hairs. Rarely, blistering
occurs in the lesions. Permanently bald
patches may develop. Sometimes no follicular
scaling or inflammation is present but bald
areas of scarring slowly appear, often looking
rather like footprints in the snow. This is
known as ‘pseudopelade’.
Lection4
37
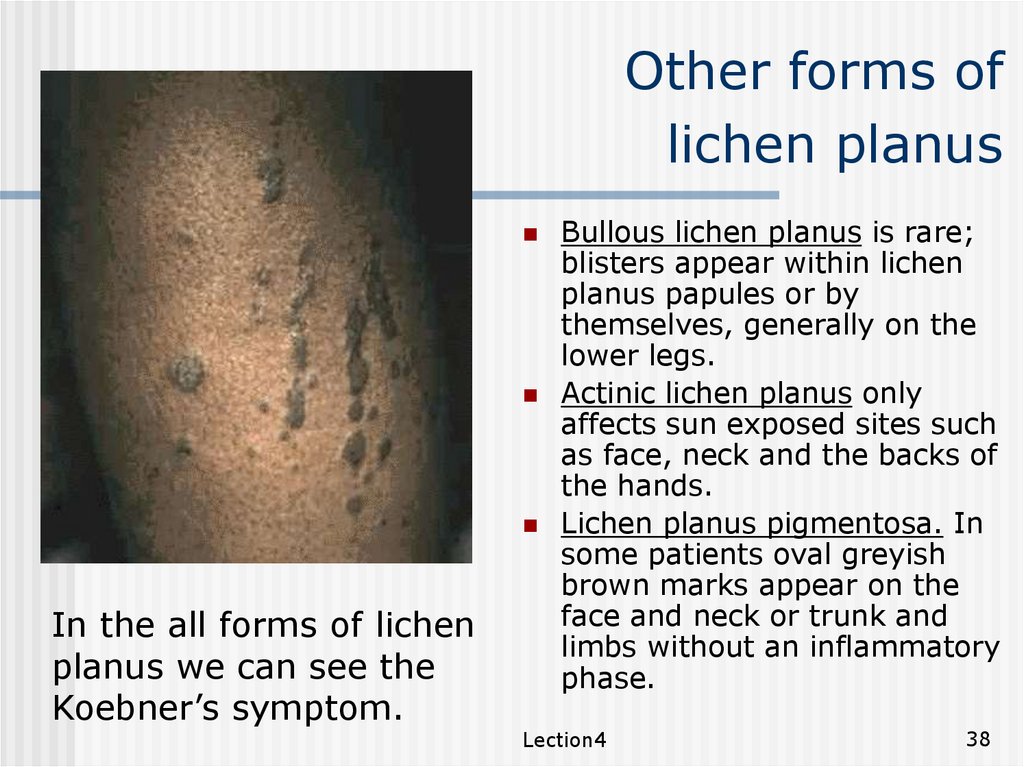
38.
Other forms oflichen planus
In the all forms of lichen
planus we can see the
Koebner’s symptom.
Bullous lichen planus is rare;
blisters appear within lichen
planus papules or by
themselves, generally on the
lower legs.
Actinic lichen planus only
affects sun exposed sites such
as face, neck and the backs of
the hands.
Lichen planus pigmentosa. In
some patients oval greyish
brown marks appear on the
face and neck or trunk and
limbs without an inflammatory
phase.
Lection4
38
39.
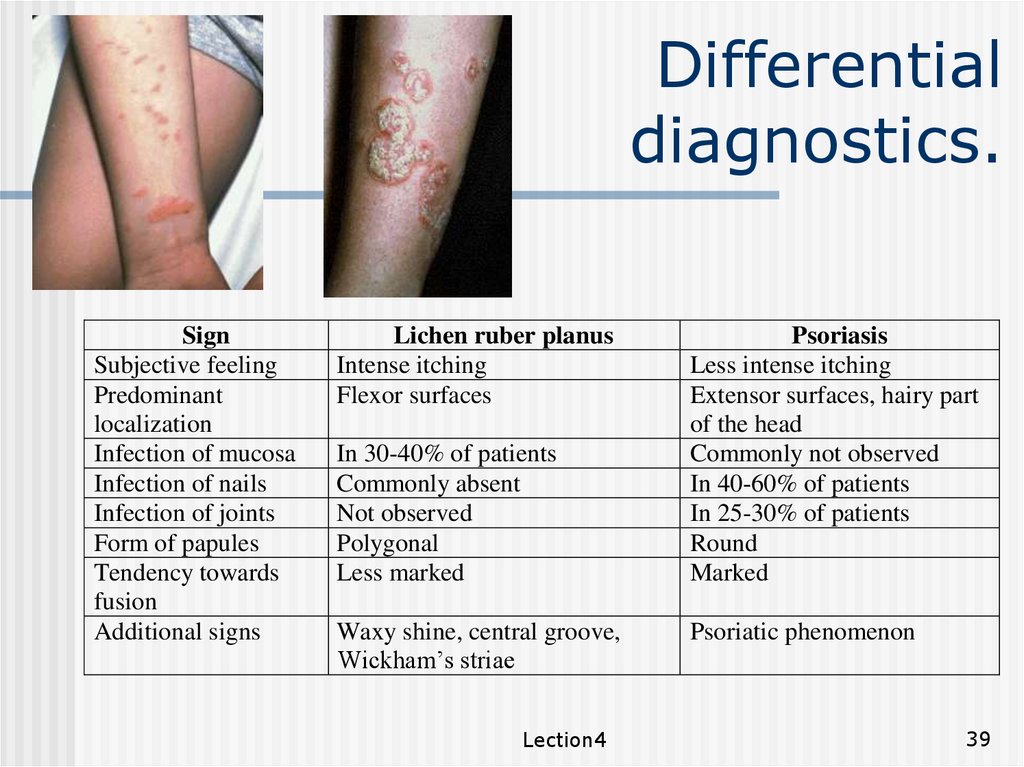
Differentialdiagnostics.
Sign
Subjective feeling
Predominant
localization
Infection of mucosa
Infection of nails
Infection of joints
Form of papules
Tendency towards
fusion
Additional signs
Lichen ruber planus
Intense itching
Flexor surfaces
In 30-40% of patients
Commonly absent
Not observed
Polygonal
Less marked
Waxy shine, central groove,
Wickham’s striae
Lection4
Psoriasis
Less intense itching
Extensor surfaces, hairy part
of the head
Commonly not observed
In 40-60% of patients
In 25-30% of patients
Round
Marked
Psoriatic phenomenon
39
 Медицина
Медицина