Похожие презентации:
The Functional Histology of Respiratory System
1.
The FunctionalHistology of
Respiratory
System
2.
The Respiratory SystemFunction of the respiratory system
1.Replinish blood oxygen levels which is
needed for tissue metabolism.
2.Remove the carbon dioxide from the blood
which produced as a by product of metabolic
activity.
3.To assist the body in maintaining a near
constant PH
3.
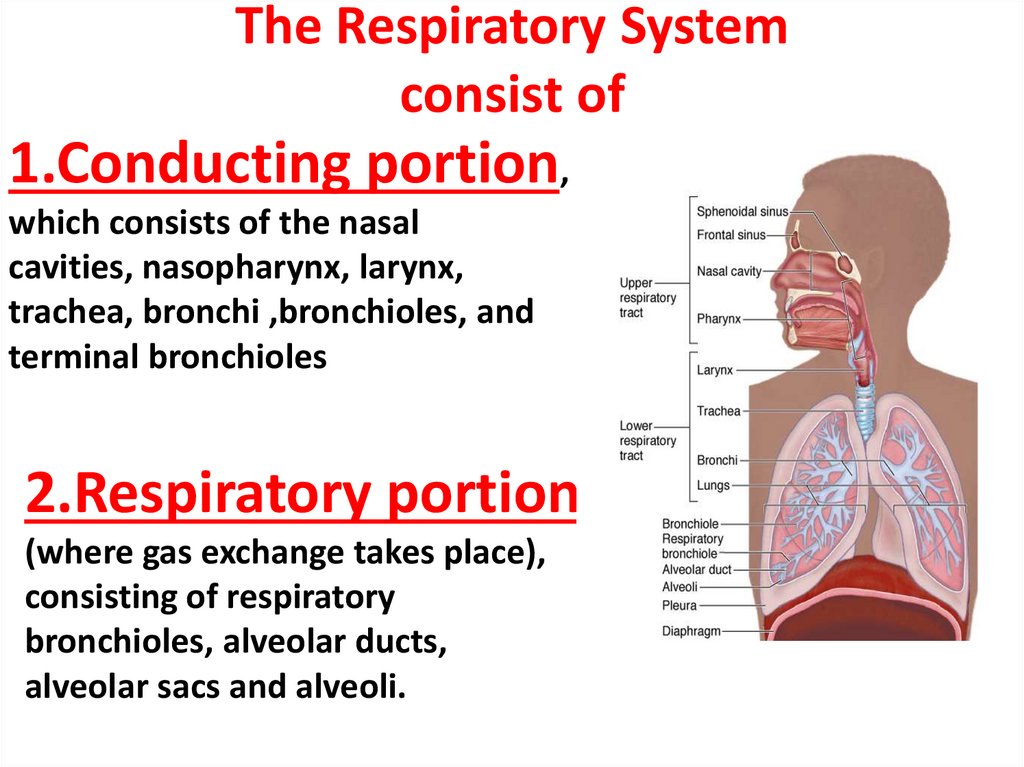
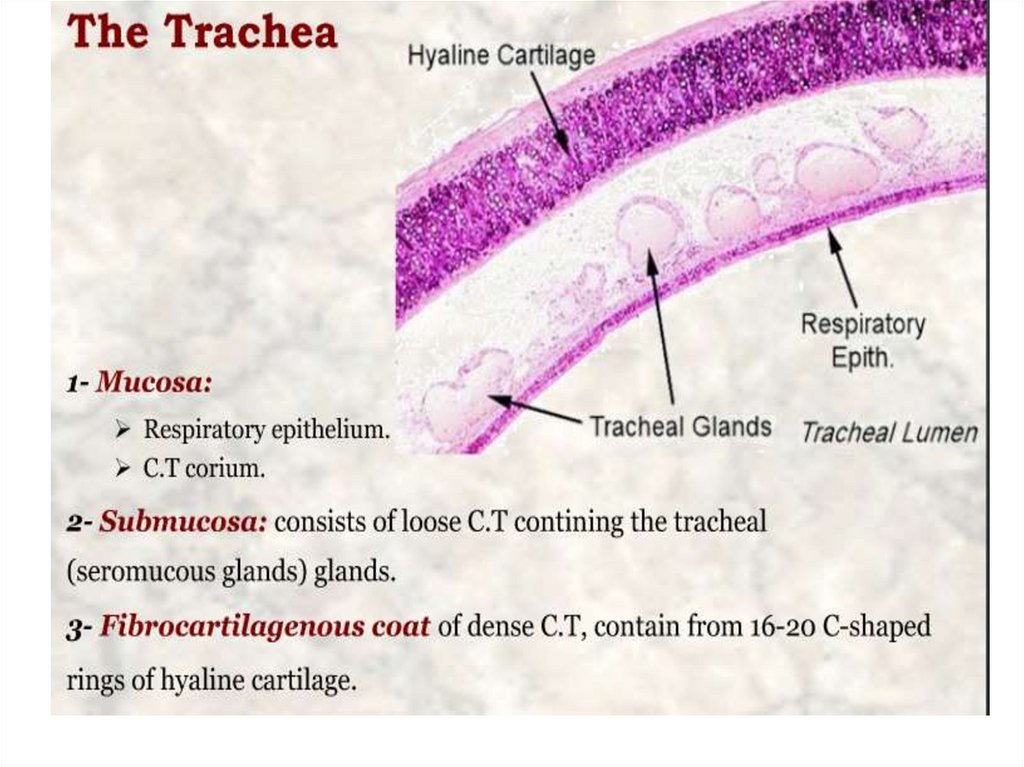
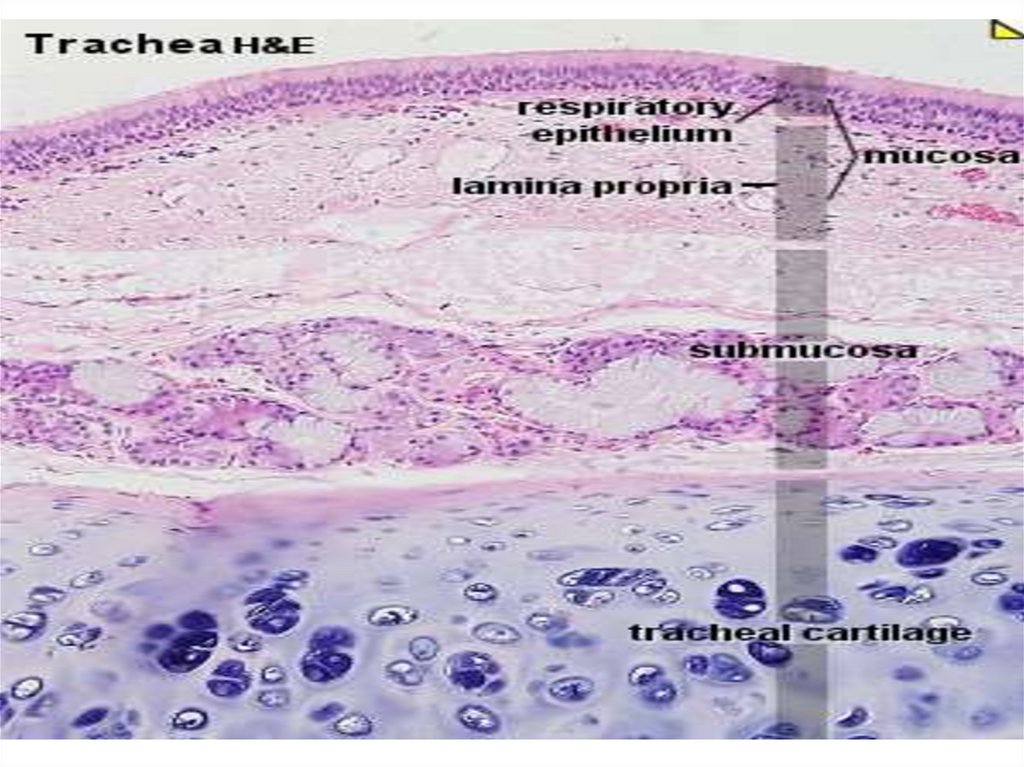
The Respiratory Systemconsist of
1.Conducting portion,
which consists of the nasal
cavities, nasopharynx, larynx,
trachea, bronchi ,bronchioles, and
terminal bronchioles
2.Respiratory portion
(where gas exchange takes place),
consisting of respiratory
bronchioles, alveolar ducts,
alveolar sacs and alveoli.
4.
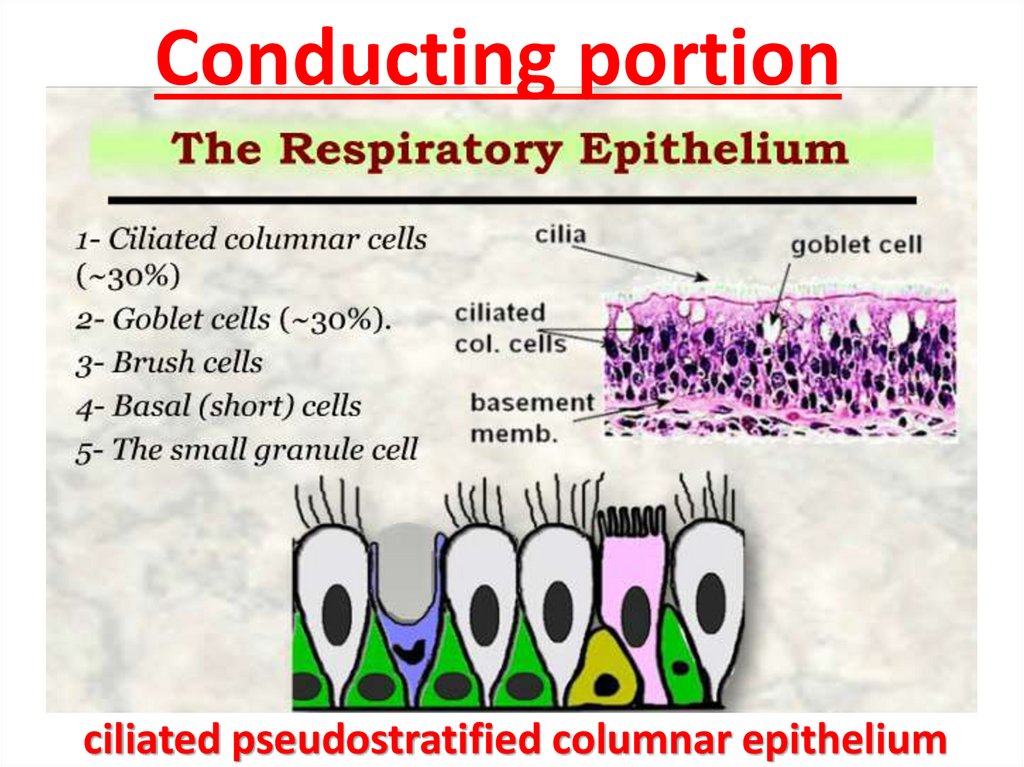
Conducting portionciliated pseudostratified columnar epithelium
5.
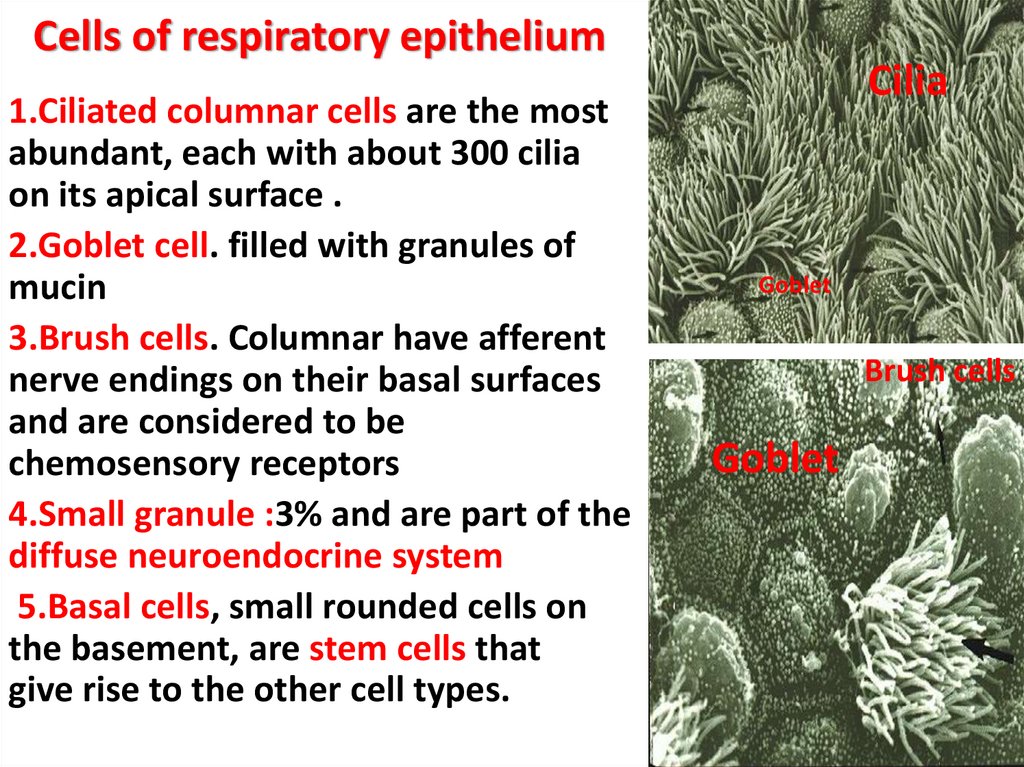
Cells of respiratory epithelium1.Ciliated columnar cells are the most
abundant, each with about 300 cilia
on its apical surface .
2.Goblet cell. filled with granules of
mucin
3.Brush cells. Columnar have afferent
nerve endings on their basal surfaces
and are considered to be
chemosensory receptors
4.Small granule :3% and are part of the
diffuse neuroendocrine system
5.Basal cells, small rounded cells on
the basement, are stem cells that
give rise to the other cell types.
Cilia
Goblet
Brush cells
Goblet
6.
7.
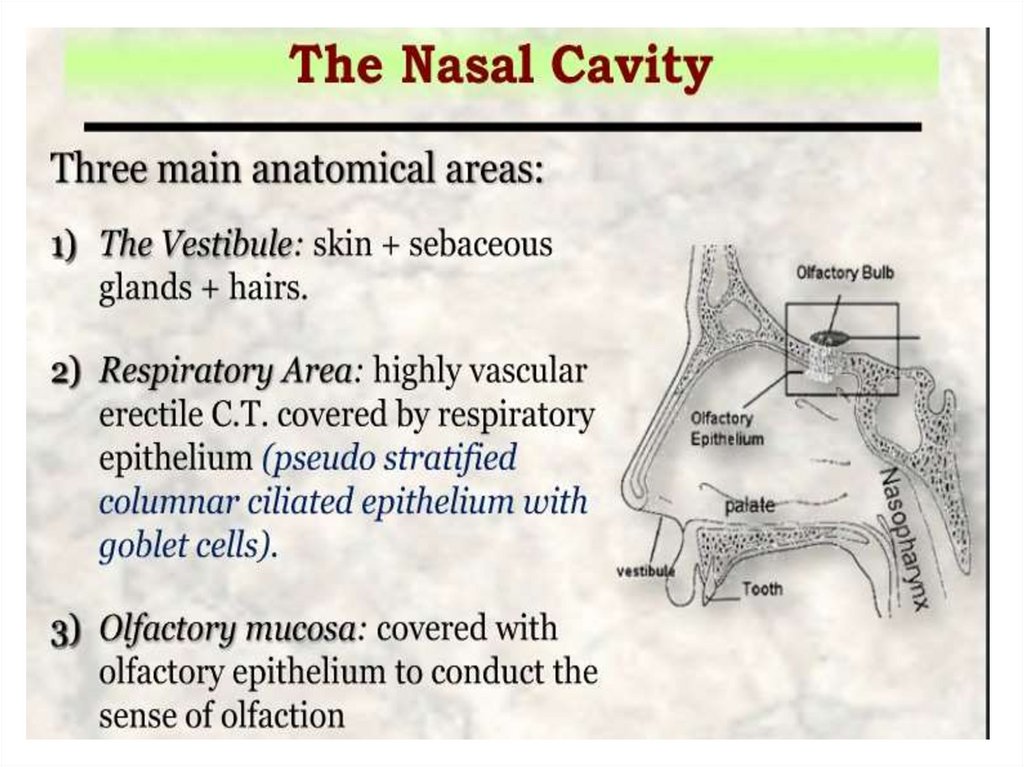
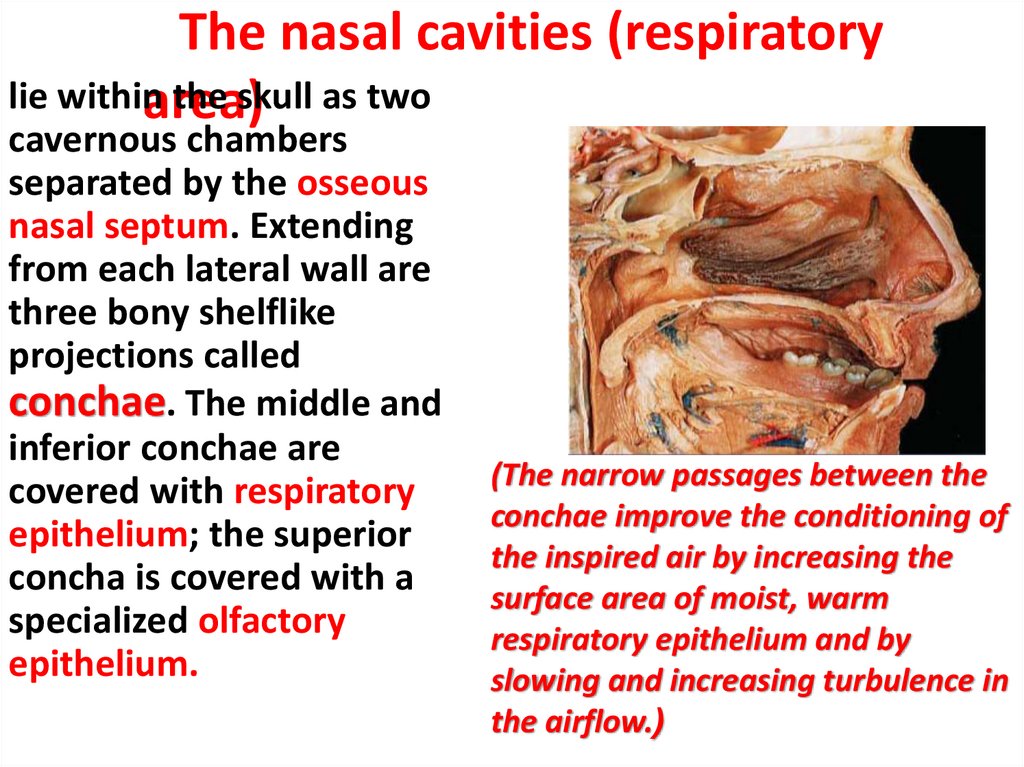
The nasal cavities (respiratorylie within
the skull as two
area)
cavernous chambers
separated by the osseous
nasal septum. Extending
from each lateral wall are
three bony shelflike
projections called
conchae. The middle and
inferior conchae are
covered with respiratory
epithelium; the superior
concha is covered with a
specialized olfactory
epithelium.
(The narrow passages between the
conchae improve the conditioning of
the inspired air by increasing the
surface area of moist, warm
respiratory epithelium and by
slowing and increasing turbulence in
the airflow.(
8.
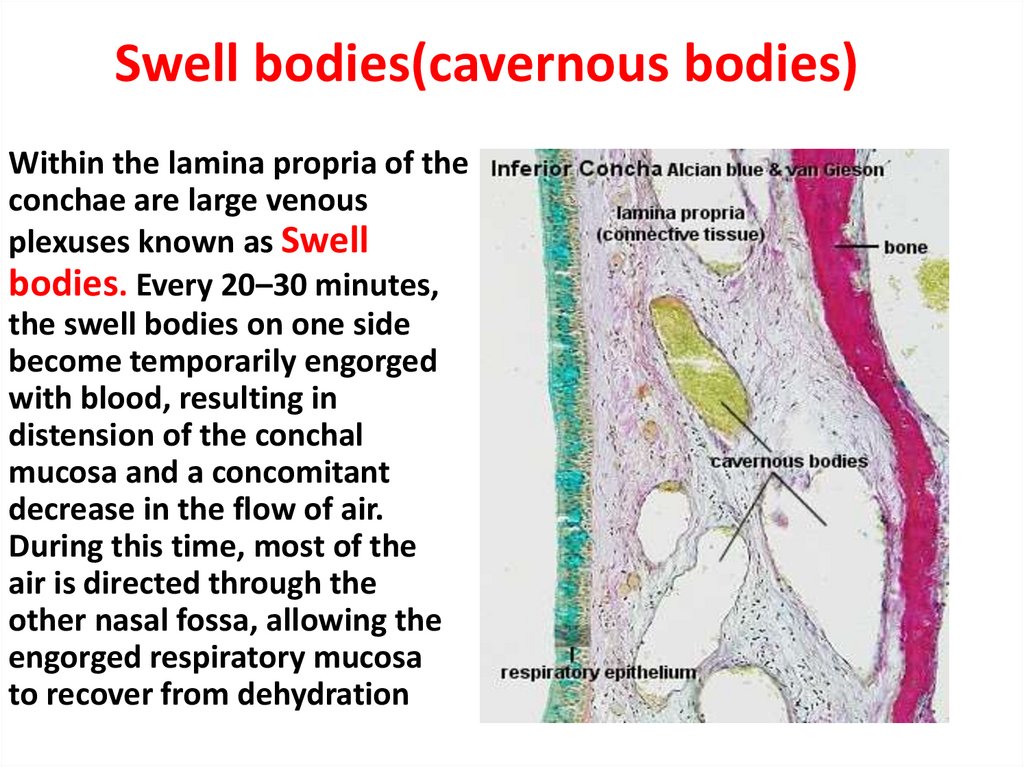
Swell bodies(cavernous bodies)Within the lamina propria of the
conchae are large venous
plexuses known as Swell
bodies. Every 20–30 minutes,
the swell bodies on one side
become temporarily engorged
with blood, resulting in
distension of the conchal
mucosa and a concomitant
decrease in the flow of air.
During this time, most of the
air is directed through the
other nasal fossa, allowing the
engorged respiratory mucosa
to recover from dehydration
9.
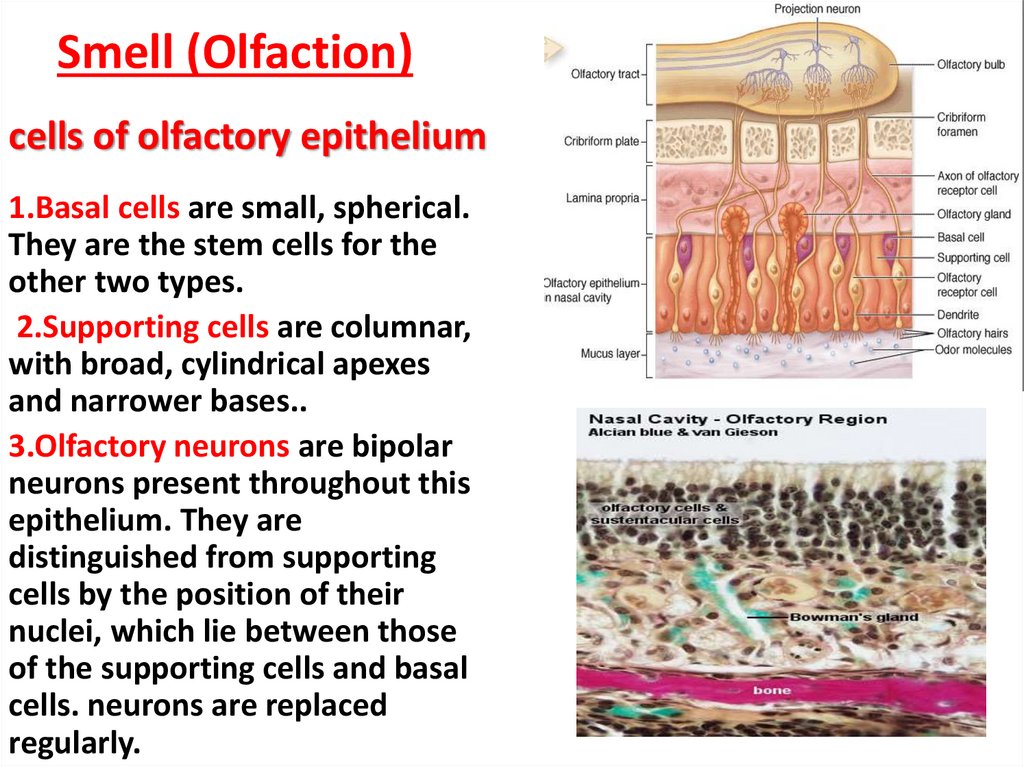
Smell (Olfaction)cells of olfactory epithelium
1.Basal cells are small, spherical.
They are the stem cells for the
other two types.
2.Supporting cells are columnar,
with broad, cylindrical apexes
and narrower bases..
3.Olfactory neurons are bipolar
neurons present throughout this
epithelium. They are
distinguished from supporting
cells by the position of their
nuclei, which lie between those
of the supporting cells and basal
cells. neurons are replaced
regularly.
10.
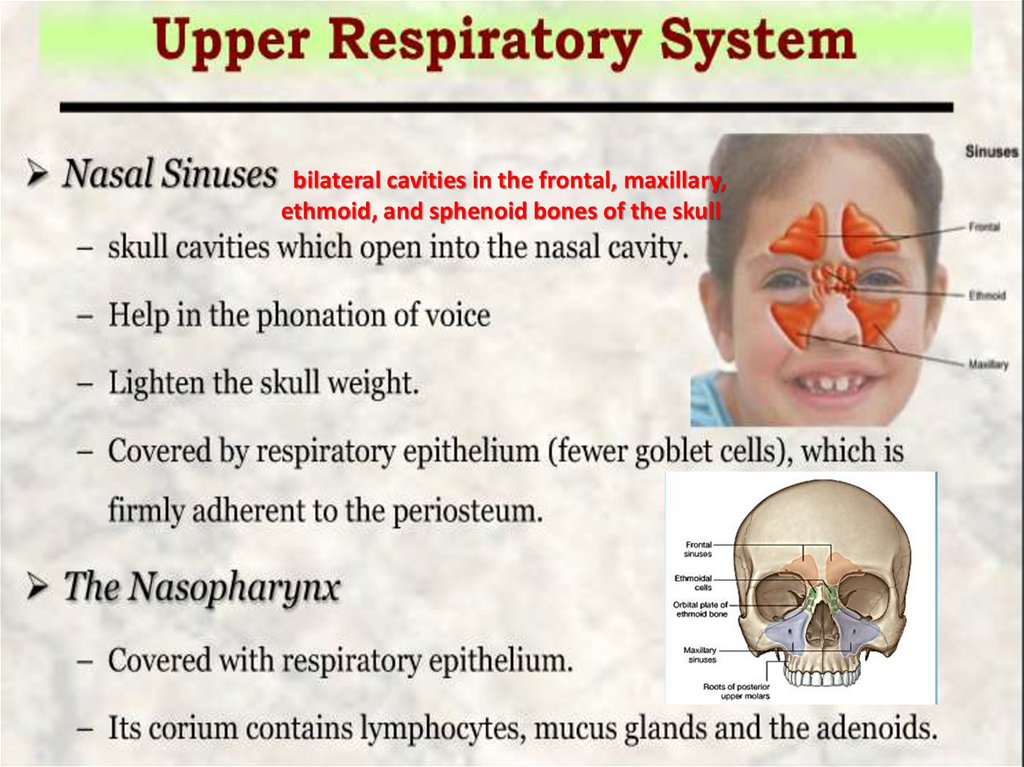
bilateral cavities in the frontal, maxillary,ethmoid, and sphenoid bones of the skull
11.
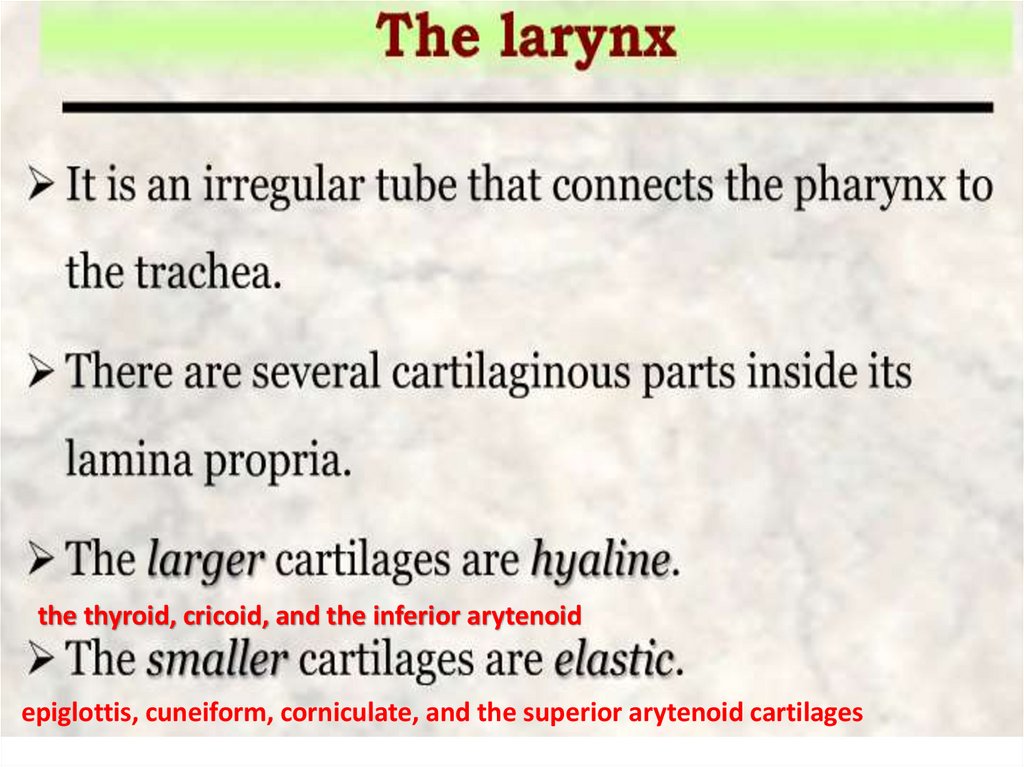
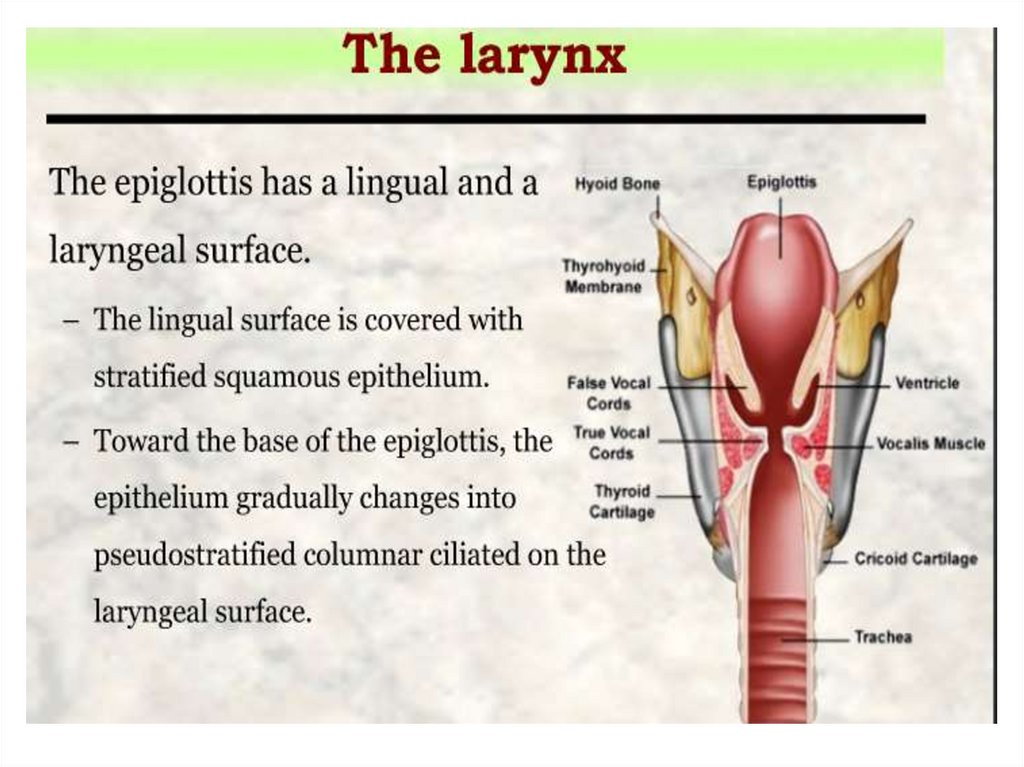
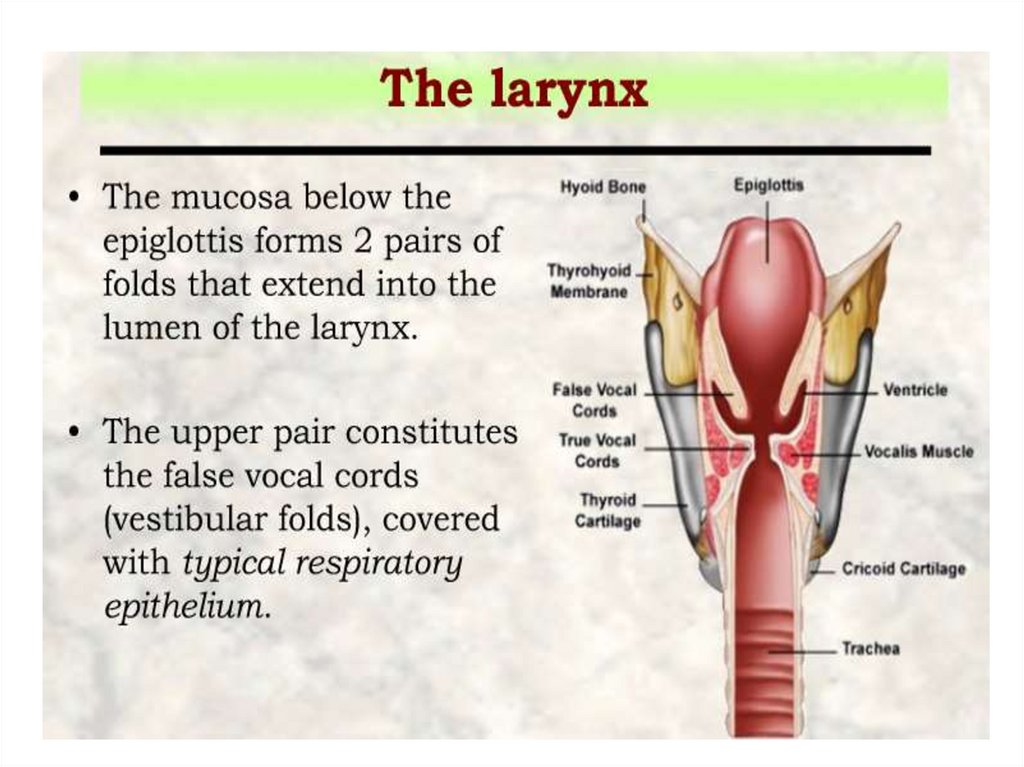
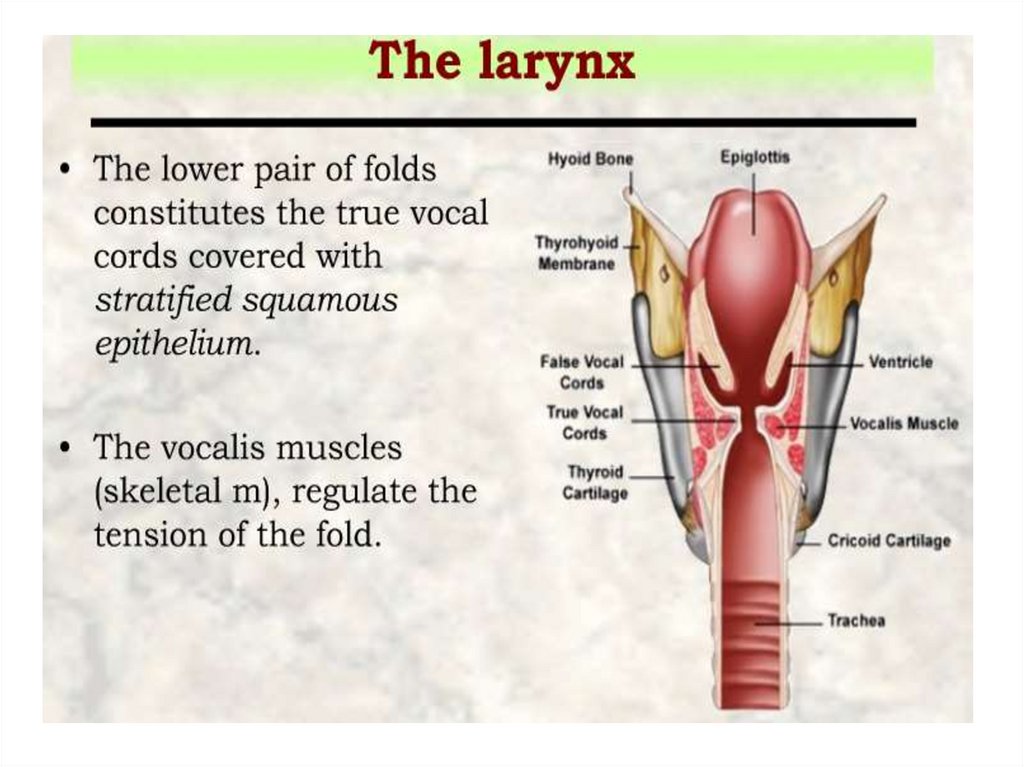
the thyroid, cricoid, and the inferior arytenoidepiglottis, cuneiform, corniculate, and the superior arytenoid cartilages
12.
13.
14.
15.
16.
17.
18.
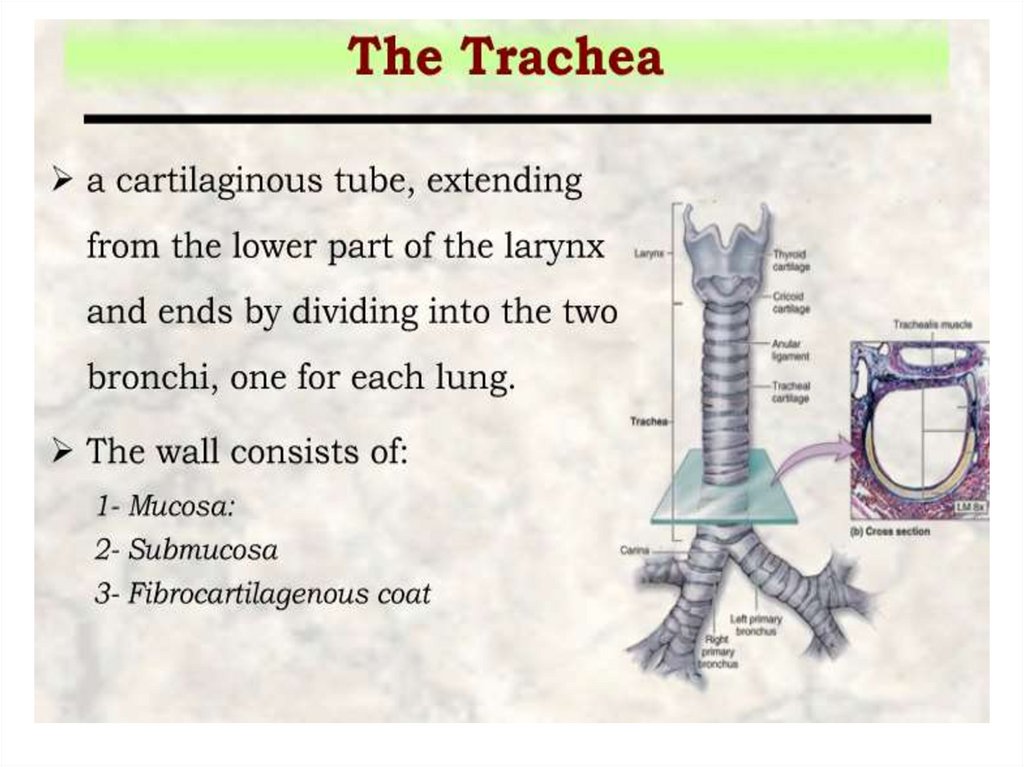
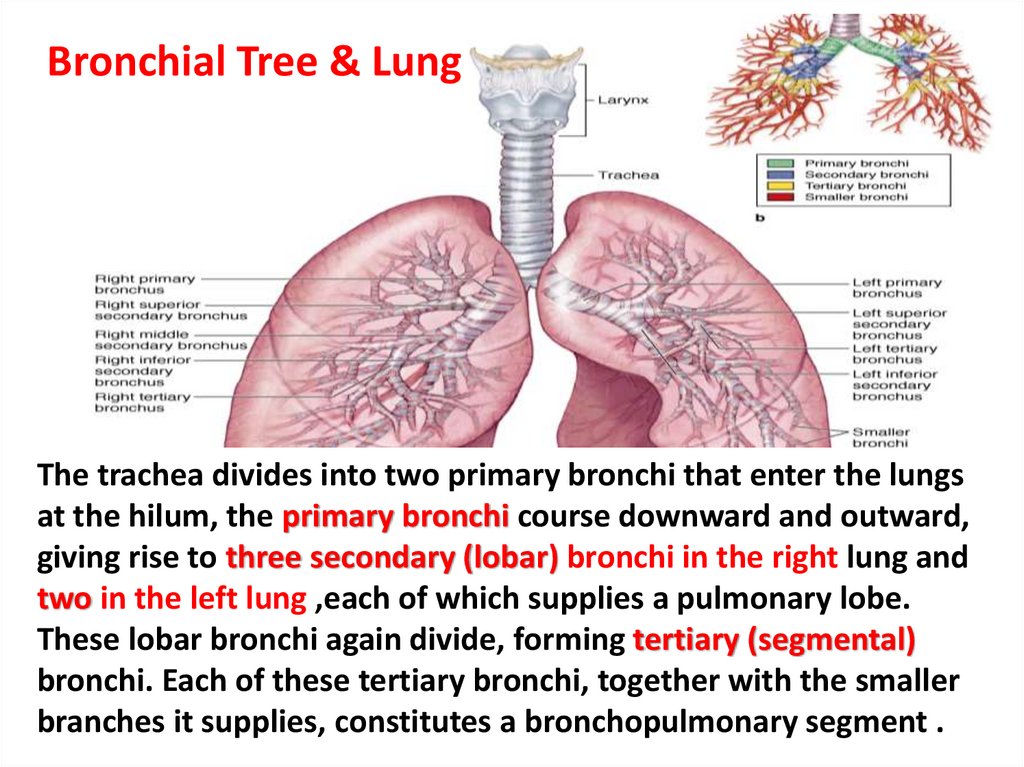
Bronchial Tree & LungThe trachea divides into two primary bronchi that enter the lungs
at the hilum, the primary bronchi course downward and outward,
giving rise to three secondary (lobar) bronchi in the right lung and
two in the left lung ,each of which supplies a pulmonary lobe.
These lobar bronchi again divide, forming tertiary (segmental)
bronchi. Each of these tertiary bronchi, together with the smaller
branches it supplies, constitutes a bronchopulmonary segment .
19.
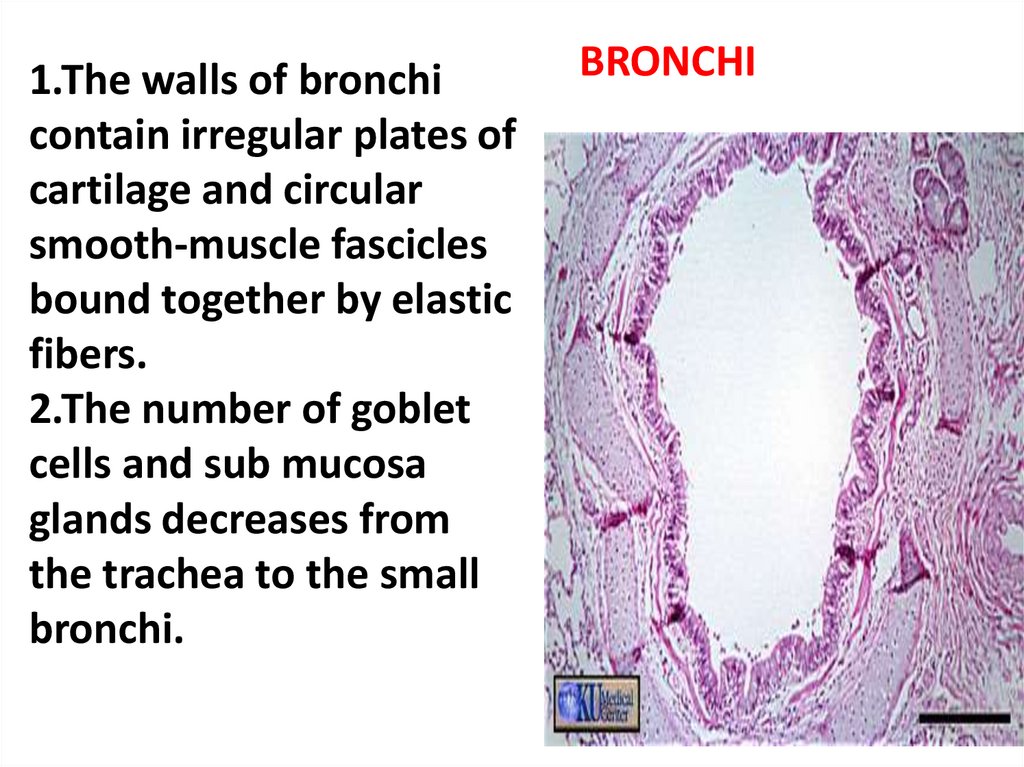
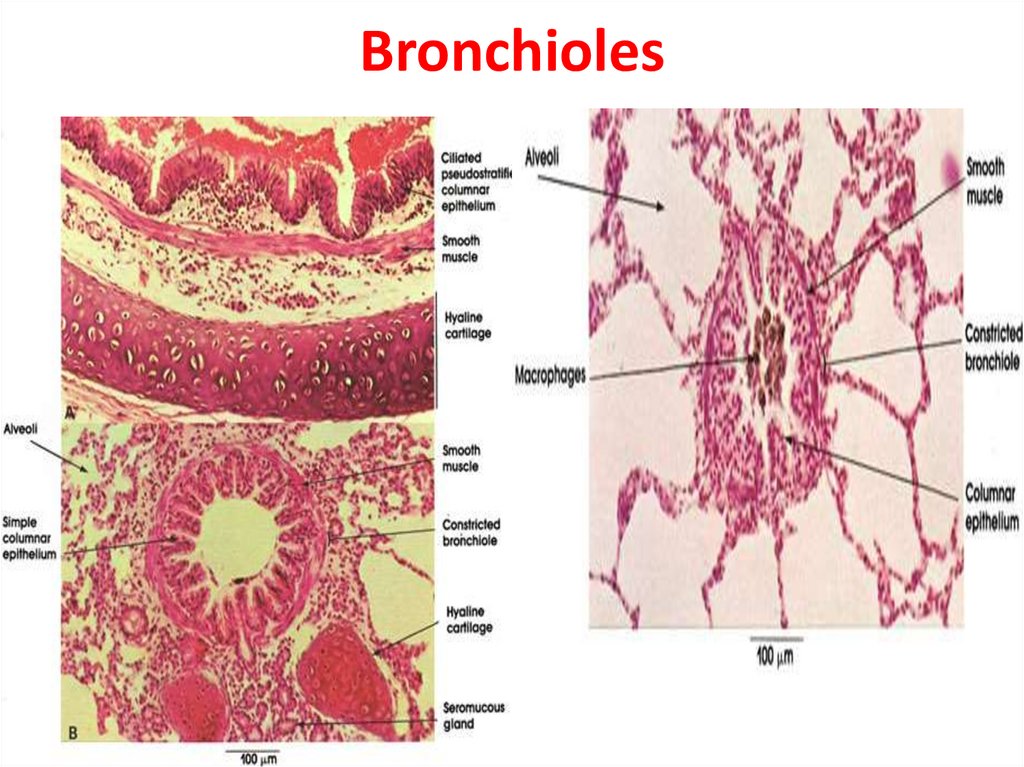
1.The walls of bronchicontain irregular plates of
cartilage and circular
smooth-muscle fascicles
bound together by elastic
fibers.
2.The number of goblet
cells and sub mucosa
glands decreases from
the trachea to the small
bronchi.
BRONCHI
20.
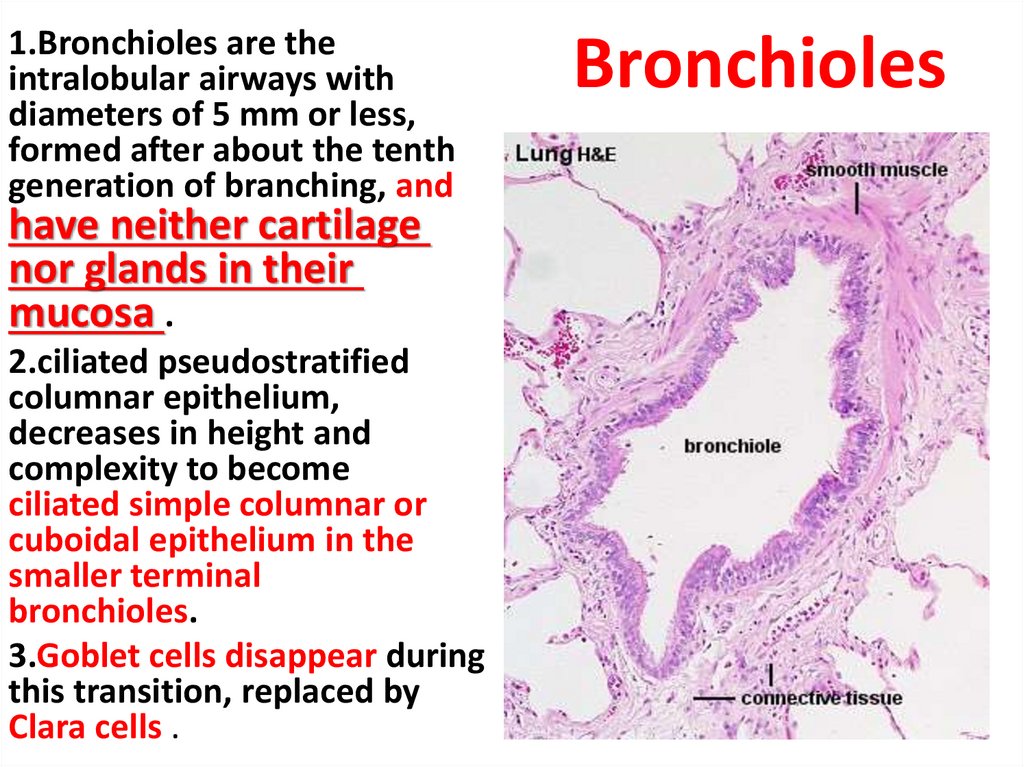
1.Bronchioles are theintralobular airways with
diameters of 5 mm or less,
formed after about the tenth
generation of branching, and
have neither cartilage
nor glands in their
mucosa .
2.ciliated pseudostratified
columnar epithelium,
decreases in height and
complexity to become
ciliated simple columnar or
cuboidal epithelium in the
smaller terminal
bronchioles.
3.Goblet cells disappear during
this transition, replaced by
Clara cells .
Bronchioles
21.
Bronchioles22.
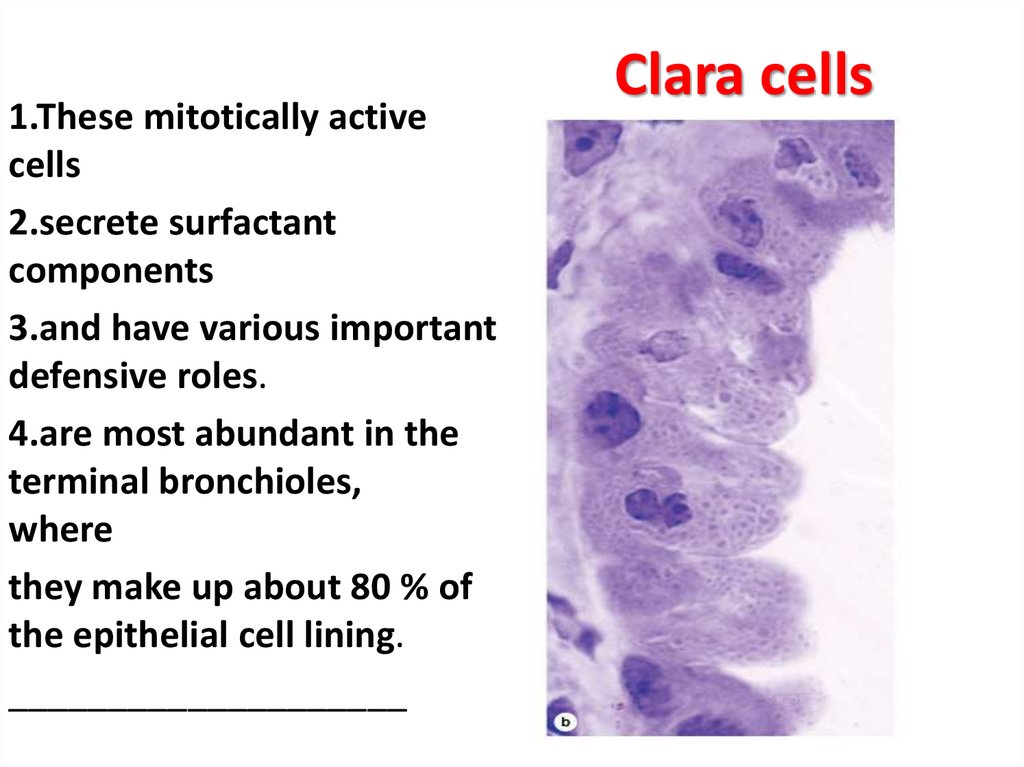
1.These mitotically activecells
2.secrete surfactant
components
3.and have various important
defensive roles.
4.are most abundant in the
terminal bronchioles,
where
they make up about 80 % of
the epithelial cell lining.
____________________
Clara cells
23.
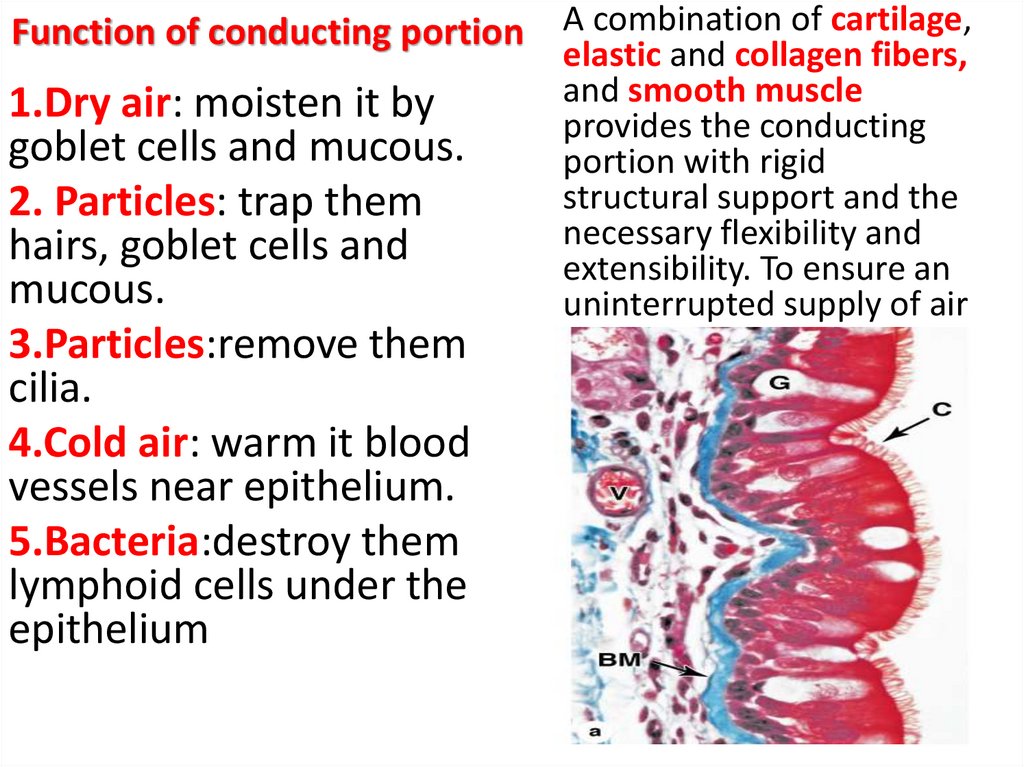
Function of conducting portion A combination of cartilage,1.Dry air: moisten it by
goblet cells and mucous.
2. Particles: trap them
hairs, goblet cells and
mucous.
3.Particles:remove them
cilia.
4.Cold air: warm it blood
vessels near epithelium.
5.Bacteria:destroy them
lymphoid cells under the
epithelium
elastic and collagen fibers,
and smooth muscle
provides the conducting
portion with rigid
structural support and the
necessary flexibility and
extensibility. To ensure an
uninterrupted supply of air
24.
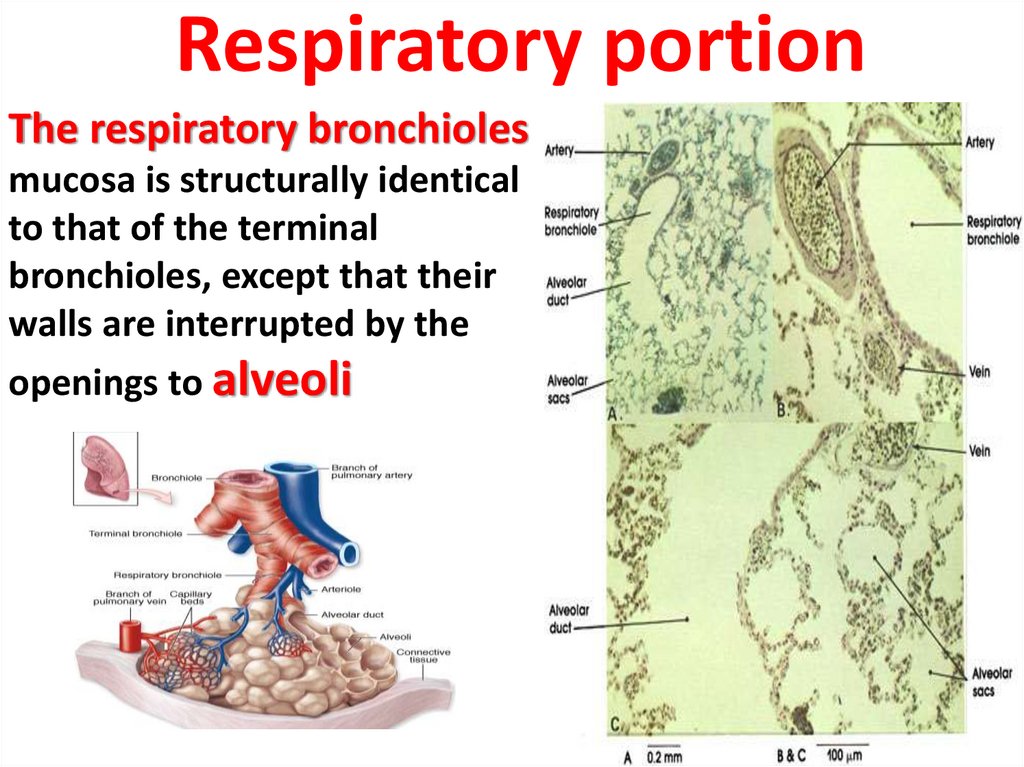
Respiratory portionThe respiratory bronchioles
mucosa is structurally identical
to that of the terminal
bronchioles, except that their
walls are interrupted by the
openings to alveoli
25.
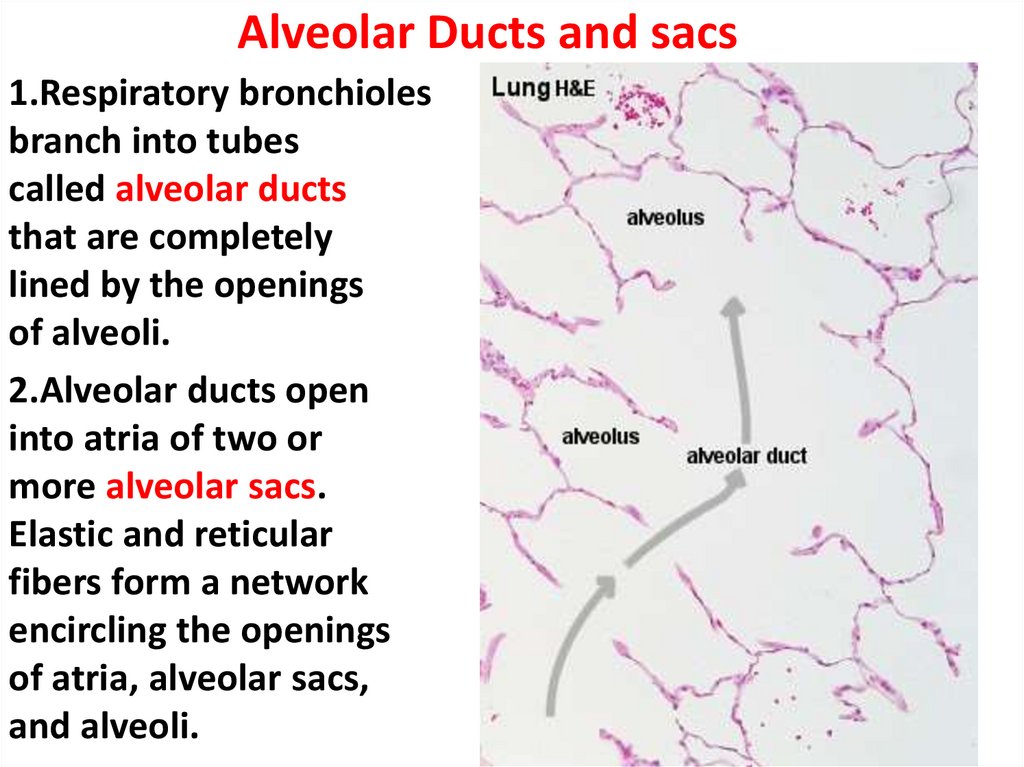
Alveolar Ducts and sacs1.Respiratory bronchioles
branch into tubes
called alveolar ducts
that are completely
lined by the openings
of alveoli.
2.Alveolar ducts open
into atria of two or
more alveolar sacs.
Elastic and reticular
fibers form a network
encircling the openings
of atria, alveolar sacs,
and alveoli.
26.
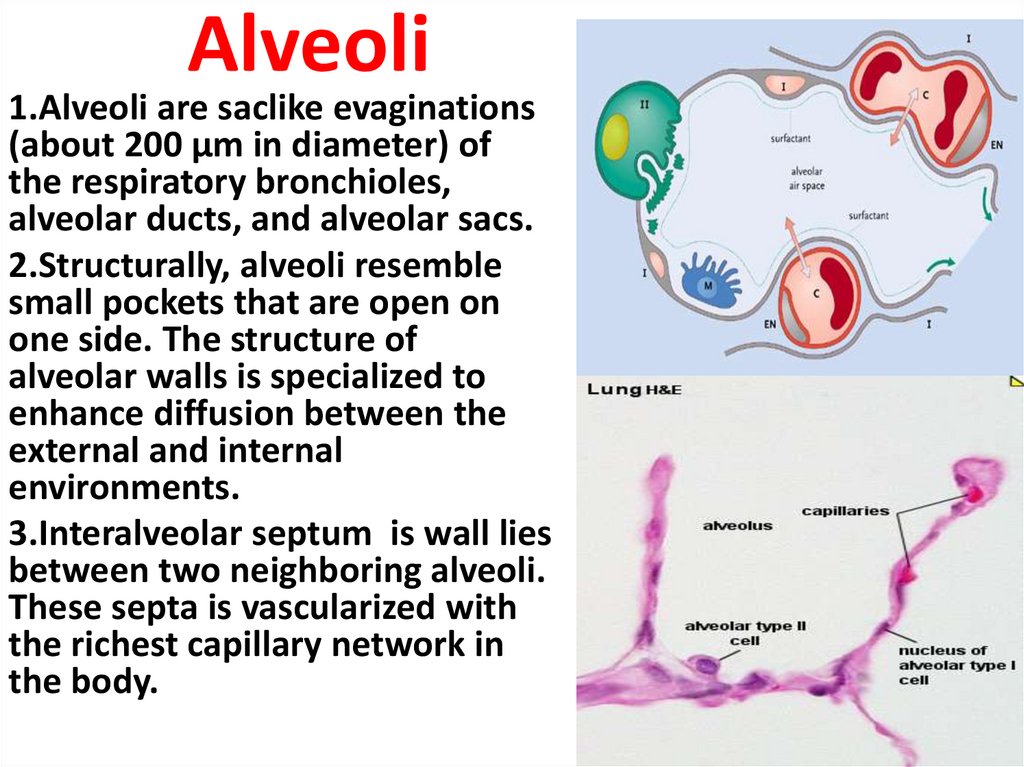
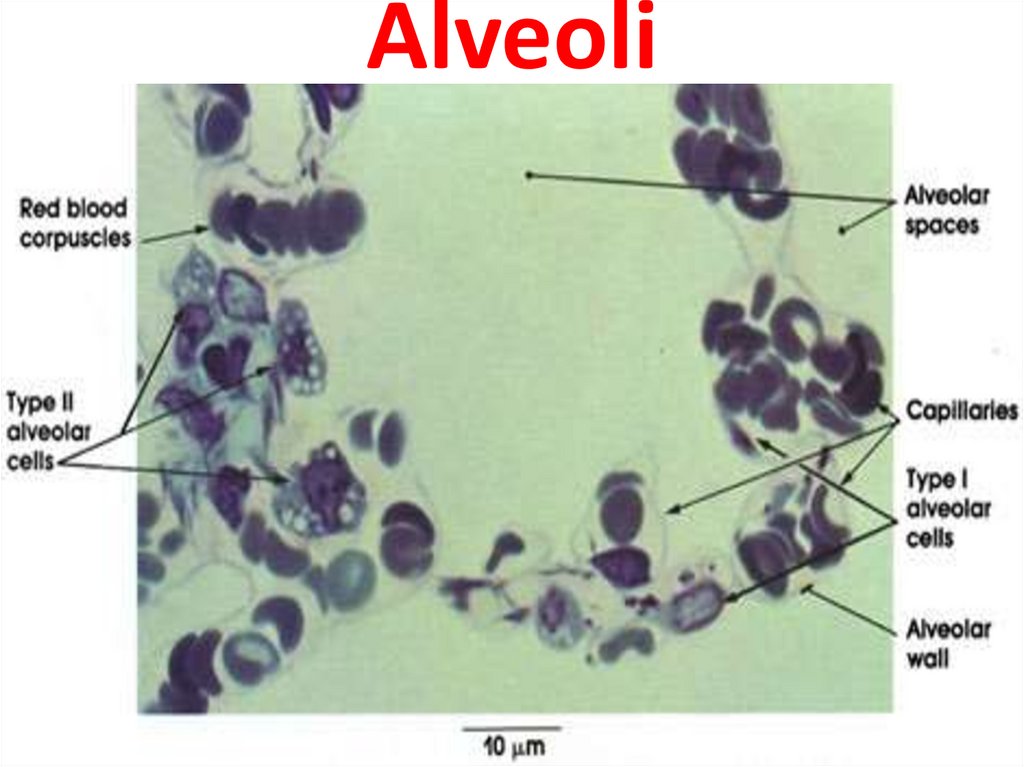
Alveoli1.Alveoli are saclike evaginations
(about 200 µm in diameter) of
the respiratory bronchioles,
alveolar ducts, and alveolar sacs.
2.Structurally, alveoli resemble
small pockets that are open on
one side. The structure of
alveolar walls is specialized to
enhance diffusion between the
external and internal
environments.
3.Interalveolar septum is wall lies
between two neighboring alveoli.
These septa is vascularized with
the richest capillary network in
the body.
27.
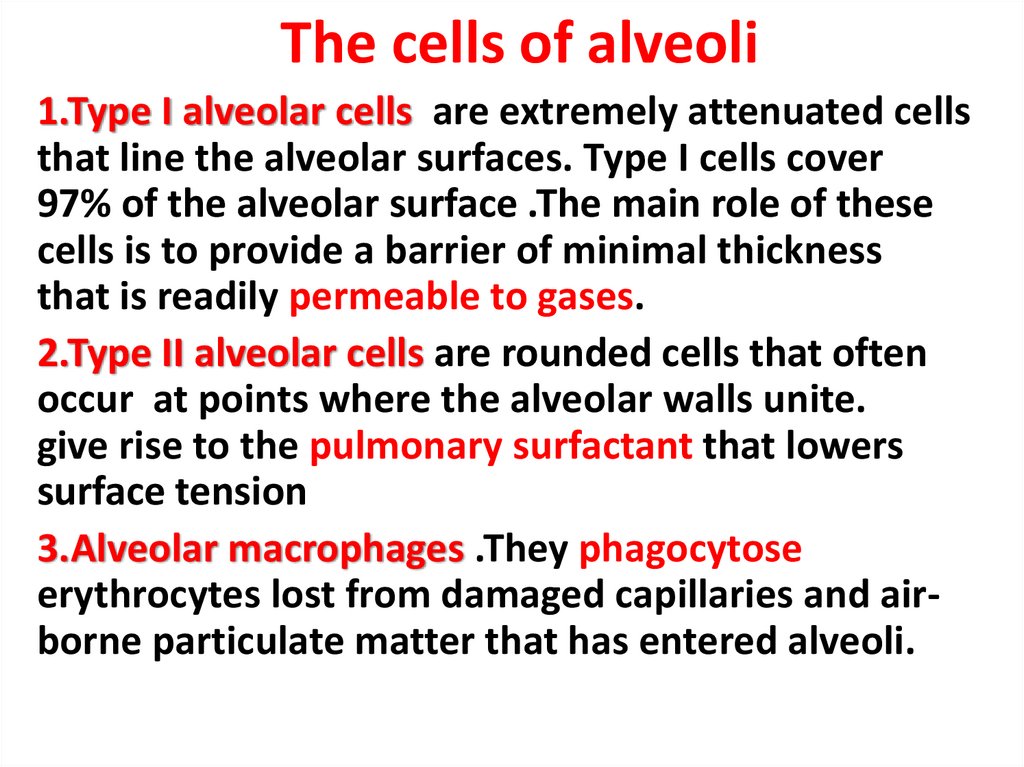
The cells of alveoli1.Type I alveolar cells are extremely attenuated cells
that line the alveolar surfaces. Type I cells cover
97% of the alveolar surface .The main role of these
cells is to provide a barrier of minimal thickness
that is readily permeable to gases.
2.Type II alveolar cells are rounded cells that often
occur at points where the alveolar walls unite.
give rise to the pulmonary surfactant that lowers
surface tension
3.Alveolar macrophages .They phagocytose
erythrocytes lost from damaged capillaries and airborne particulate matter that has entered alveoli.
28.
Alveoli29.
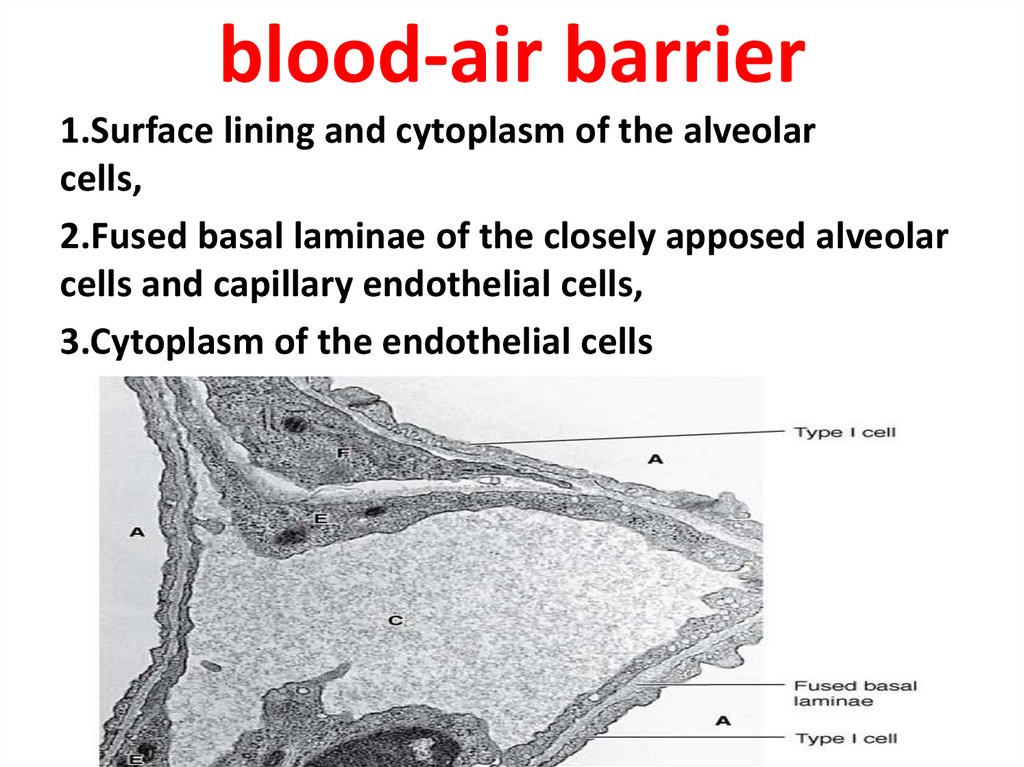
blood-air barrier1.Surface lining and cytoplasm of the alveolar
cells,
2.Fused basal laminae of the closely apposed alveolar
cells and capillary endothelial cells,
3.Cytoplasm of the endothelial cells
 Медицина
Медицина