Похожие презентации:
Preneoplastic lesions of female genitals
1. Preneoplastic lesions of female genitals
1. Background diseases – potentiallypremalignant
2. True precancerous diseases
potentially malignant
-
2.
Background diseases includechronic dystrophic processes
without cellular displasia and
cellular atypia, characterized
with proliferation, atrophic
changes, without invasion
3.
True precancerous diseasesinclude lesions, characterized
with dysplasia, atypical
epithelial excrescence, focal
proliferation (without invasion),
cellular atypism.
4. Background processes of vulva :
kraurosis of the vulvaleukoplakia of the vulva
condylomatosis of the vulva
lichen sclerosis
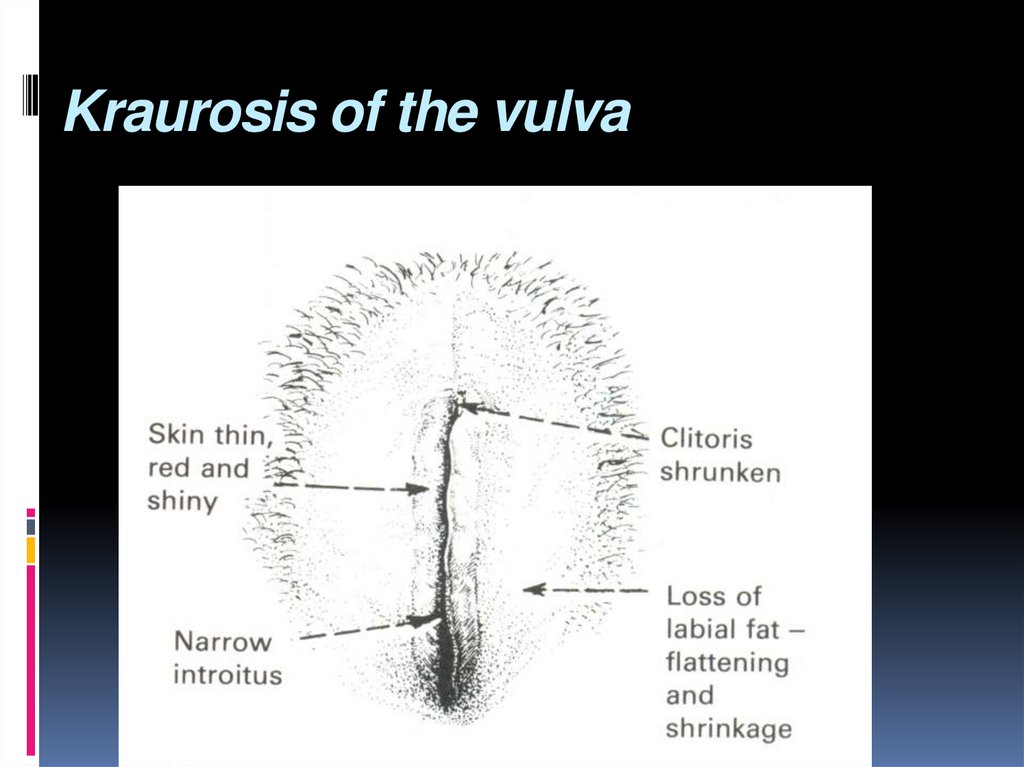
5. Kraurosis of the vulva
6. Craurosis of the vulva
Morphologically characterized withatrophy of papillary and reticular layers
of the skin, destruction of elastic fibers,
and hyalinization of connective tissue.
Fatty tissue of large lips of pudendum
disappears, and sebaceous and
sudoriferous glands atrophy occurs.
7. Craurosis: features
Thinning and fibrosis of the vulvarepidermis
stenosis of the introitus
Vulvar skin becomes dry, brittle, and thinskinned.
8. Craurosis: complaints
vulvar itchingpain
burning
scratches
secondary inflammations
9. Diagnosis
is based on:detailed inspection,
vulvar colposcopy,
evaluation of glycemia,
Pap-smears,
cytological investigations,
biopsy.
10. Craurosis - Treatment
local application of estrogeniccream
or oral estrogen in small doses.
If uneffective/severe pruritus
occurs, a simple vulvectomy is
recommended
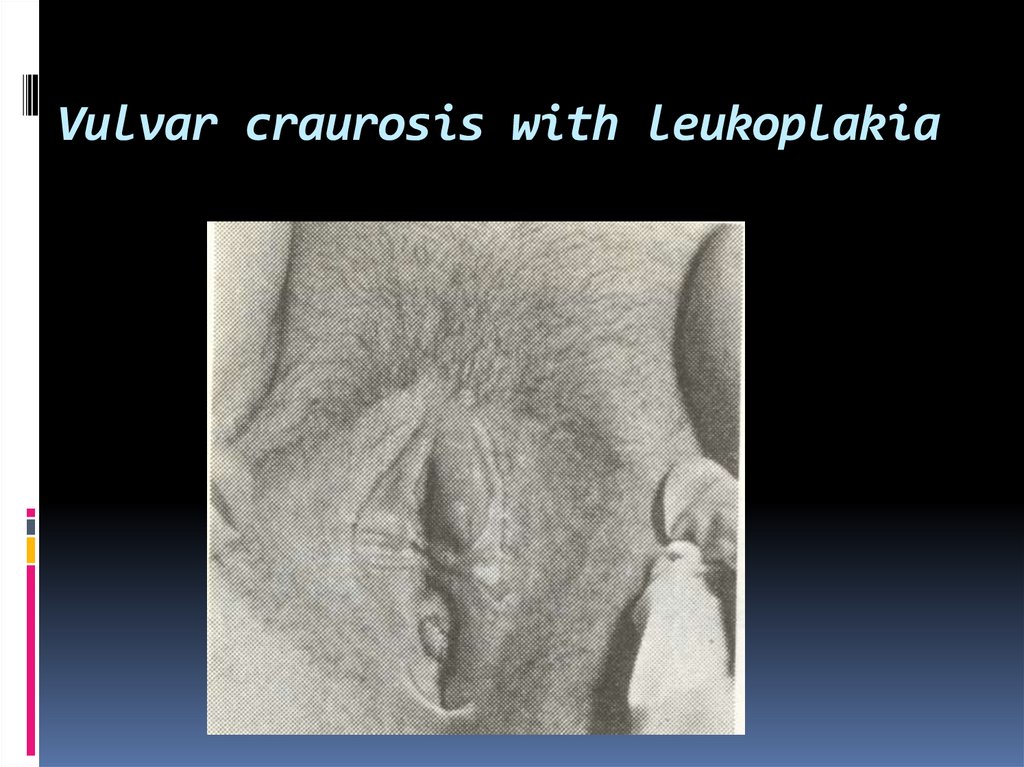
11. Vulvar craurosis with leukoplakia
12. Leukoplakia of the vulva.
Characterized with: proliferation ofstratified epithelium, epithelial
hyperplasia of the rate Malpighii and
hyaline degeneration of the collagen.
Histopathologic variants are:
dermatosis, dermatopathy,
hyperkeratosis.
13. Leukoplakia: Clinical features
The affected area has a thickened, hard andindurated skin consisting of white patches
scattered irregularly, mainly over the labia
majora.
The skin cracks easily due to the increased
keratin on the surface.
Hyperplasia of the epidermis may lead to
carcinoma
Combination of leucoplackia with craurosis is
frequent condition.
14. Leukoplakia of the vulva:complaints
pruritissevere discomfort
discharge
15. Leukoplakia of the vulva:diagnosis&treatment
Leukoplakia of thevulva:diagnosis&treatment
Diagnosis :
detailed inspection,
vulvar colposcopy,
Pap-smears, cytological investigations,
biopsy.
The treatment of leucoplakia is simple
vulvectomy.
16. Vulvar condylomas
It occurs in young, sexuallly active womenCondyloma presents excrescences, covered
with stratified epithelium, with connectivetissue stroma and vessels inside.
Usually they appear in the area of large and
small lips of pudendum, often plural.
Mostly caused by Human papillomovirus’
infection (HIV)
17. Condilomatosis: Clinical signs&treatment
Condilomatosis: Clinicalsigns&treatment
Signs are:
pain,
itch,
secondary inflammation
Treatment : antibiotic therapy,
surgical removing with subsequent
treatment of underlying diseases.
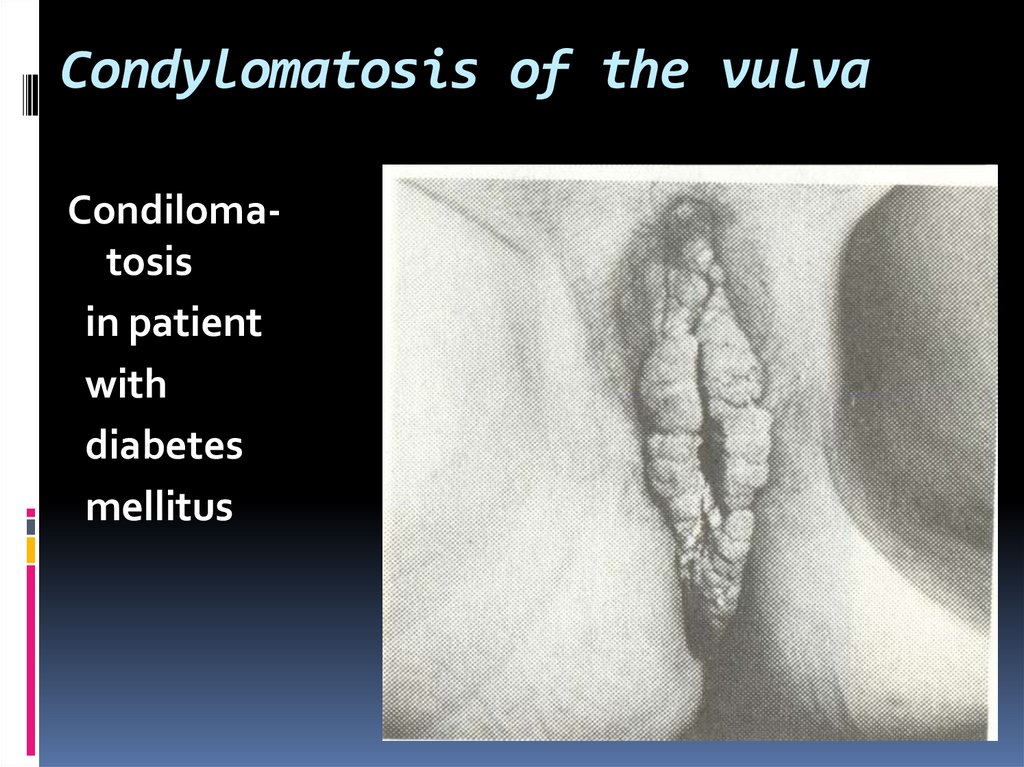
18. Condylomatosis of the vulva
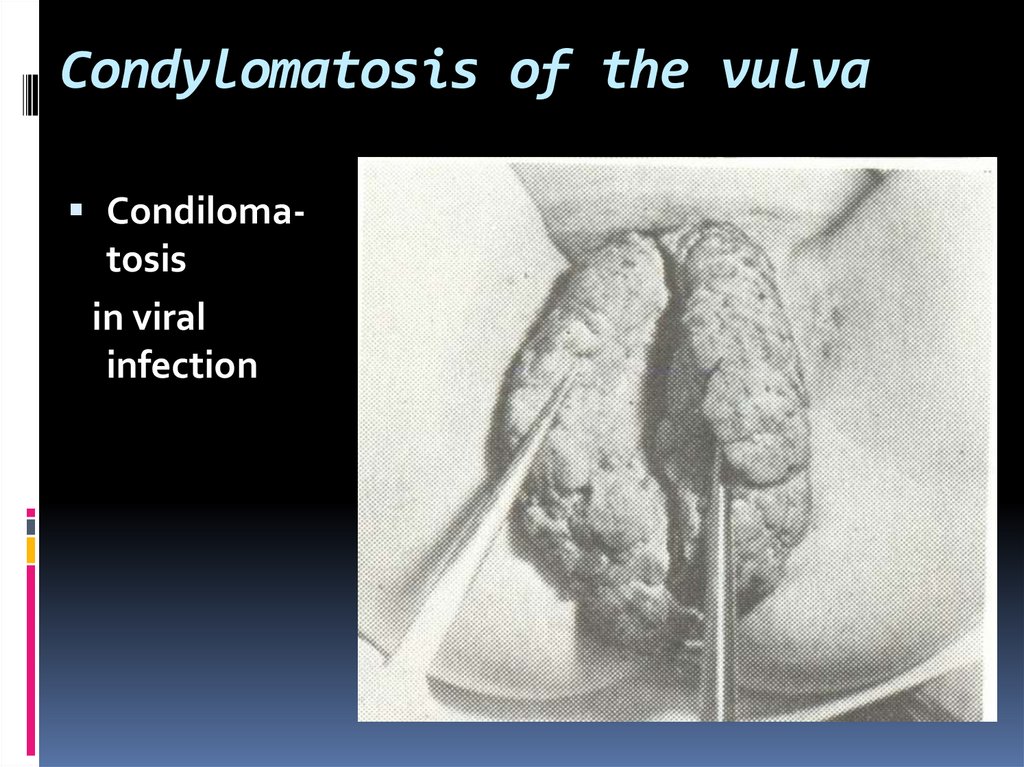
Condilomatosisin viral
infection
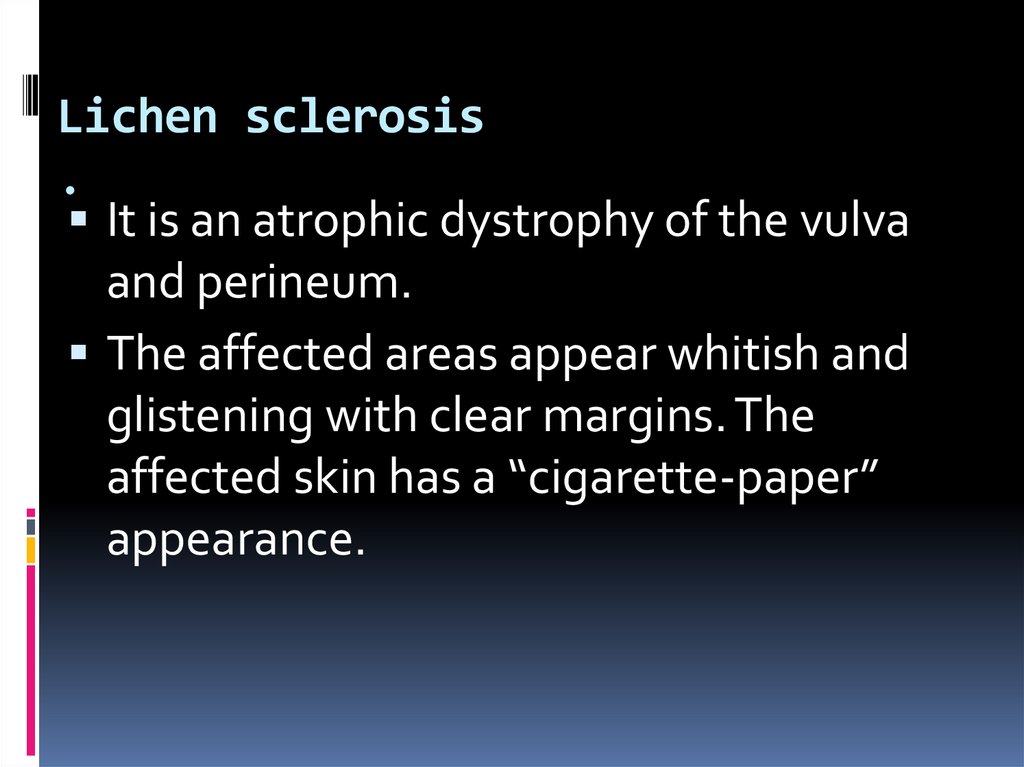
19. Condylomatosis of the vulva
Condilomatosisin patient
with
diabetes
mellitus
20. Condylomatosis of the vulva
Vulvar condilomaswith malignancy
21. Lichen sclerosis .
It is an atrophic dystrophy of the vulvaand perineum.
The affected areas appear whitish and
glistening with clear margins. The
affected skin has a “cigarette-paper”
appearance.
22. (CON)
In acute phase the area may be red andpurple.
In severe case the affected area on the
vulva extends to the anus in a shape of
figure 8 causing involutional adhesion of
labia minora to the labia majora, thus
burying the clitoris and causing shrinkage
of the introitus.
The condition occurs in postmenopausal
women.
23. Lichen sclerosis: clinical features
The leading symptom is intense itching. Ifsecondary infection occurs, ulceration and
contractures may follow resulting in
dyspareunia and dysuria.
Histologically there is a thin inactive
epithelium and loss of elastic tissue.
Prognosis: areas of dysplasia or
malignancy may develop in this lesion.
24. Lichen sclerosis - Treatment
Oral antihistamines and topical antipruriticLocal application of estrogen cream
topical corticosteroid
In atrophic lesions: androgenic steroids (2%
testosterone propionate ointment twice daily for 3
to 4 weeks.
Oral retinoids or vitamin A analogues have also been
used for this condition.
Surgical therapy for the Lichen sclerosis of the vulva
has also been reported. Cryosurgery, laser ablation,
or simple vulvectomy, though rarely, are the surgical
methods followed.
25. Lichen sclerosis - surgery
Cryosurgery,laser ablation,
simple vulvectomy
26. Simple vulvectomy
linesof incision
the view
after vulvectomy
wound closure
27. TRUE PRECANCEROUS LESIONS OF VULVA
28. Classification:
- Dysplasia –atypical hyperplasia(mild, moderate, severe):
a) without dystrophy
b) with dystrophy
- Paget’s disease of the vulva
- Squamous cell carcinoma of skin
29. True precancerous lesions:
Vulval dysplasia - squamous VINI, II, III
30. Vulvar intraepithelial neoplasm - VIN
VIN is precancerous condition thatcan be either white, dark, or red.
Excess keratin production leads to a
white appearance, whereas excess
melanin production leads to dark
lesions.
31.
Vulvar intraepithelial neoplasia result inabnormal Pap smears.
It is diagnosed on biopsy :
If only the bottom third of the epithelial (skin)
lining has these changes, mild dysplasia or
VIN I is diagnosed;
if the full thickness of the epithelium has
abnormal cells, VIN III, also called vulvar
carcinoma in situ, is diagnosed.
If these vulvar changes are left untreated for
many years, some of them turn into an
invasive cancer in later years.
32.
VIN I refers to mild dysplasiaVIN II equals moderate dysplasia,
VIN III denotes severe dysplasia (also called
carcinoma in situ).
VIN may be focal or affect multiple sites on
the vulva.
Colposcopy with acetic acid may help
delineate areas of VIN and make biopsy
easier.
VIN in younger women is strongly associated
with HPV (particularly types 16 and 18)
33.
VIN may be asymptomatic and can cometo the attention of a patient's health care
provider during an annual examination.
Pruritus, burning, sensation of the vulva
may be present.
Biopsy of any white, red, or dark lesion is
prudent, particularly in the older patient.
Progression from VIN to cancer is
uncommon in younger women, but more
likely in older patients.
34. VIN - diagnosis
acetic acid applicationcolposcopy
and biopsy
35. VIN - treatment
topical 5-fluorouracil,laser vaporization (particularly useful
for with low risk of subsequent
cancer),
simple vulvectomy
radical vulvectomy
36. Radical vulvectomy
37. Paget's disease
Paget's disease of the vulva canproduce lesions that are white or
red.
An eczematoid, erythematous
lesion is most common.
Paget's disease produces pruritus.
38. Paget's disease
This condition is associated withmalignancy of the vulva and other
extraovular locations, such as the
breasts and colon.
Biopsy is mandatory
Treatment is wide local excision,
although, unfortunately, local
recurrence is not uncommon.
39. Vulvar neoplasms:
Squamous cell carcinomas (with HPV, withoutHPV)
Verrucous carcinoma
Melanomas
Basal cell carcinomas
Sarcomas of the vulva: Leiomyosarcomas,
Rhabdomyosarcoma, Malignant fibrous
histiocytoma, Alveolar soft part sarcoma,
Dermatofibrosarcoma protuberans
Paget's disease of the vulva
40.
Treatment depends on the extent of diseaseand anatomic location. Some lateral tumors
are treated with radical wide excision, and
possible ipsilateral inguinal-femoral
lymphadenectomy.
More extensive disease may require bilateral
lymphadenectomy,
and some cases require a modified radical
vulvectomy.
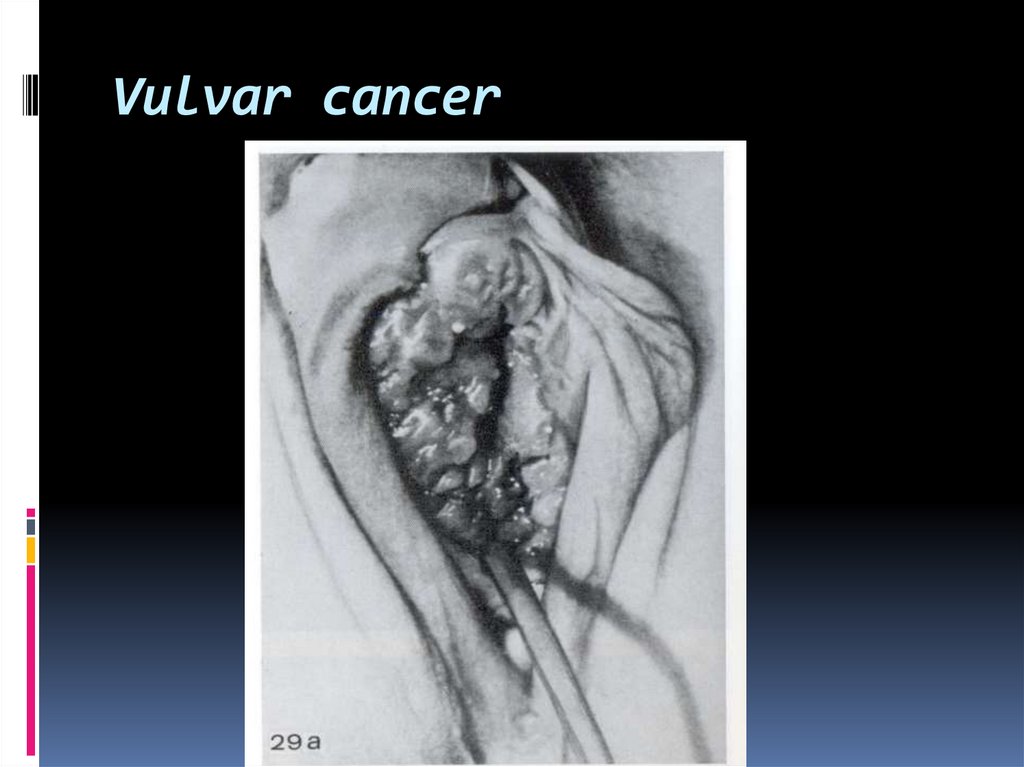
41. Vulvar cancer
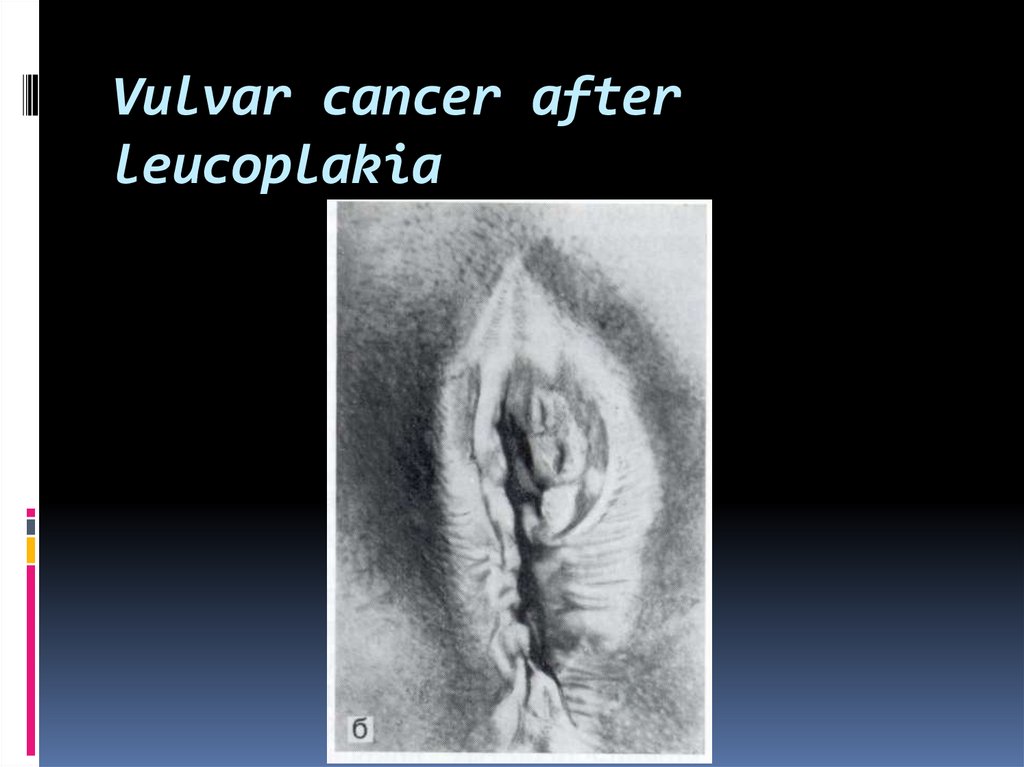
42. Vulvar cancer after leucoplakia
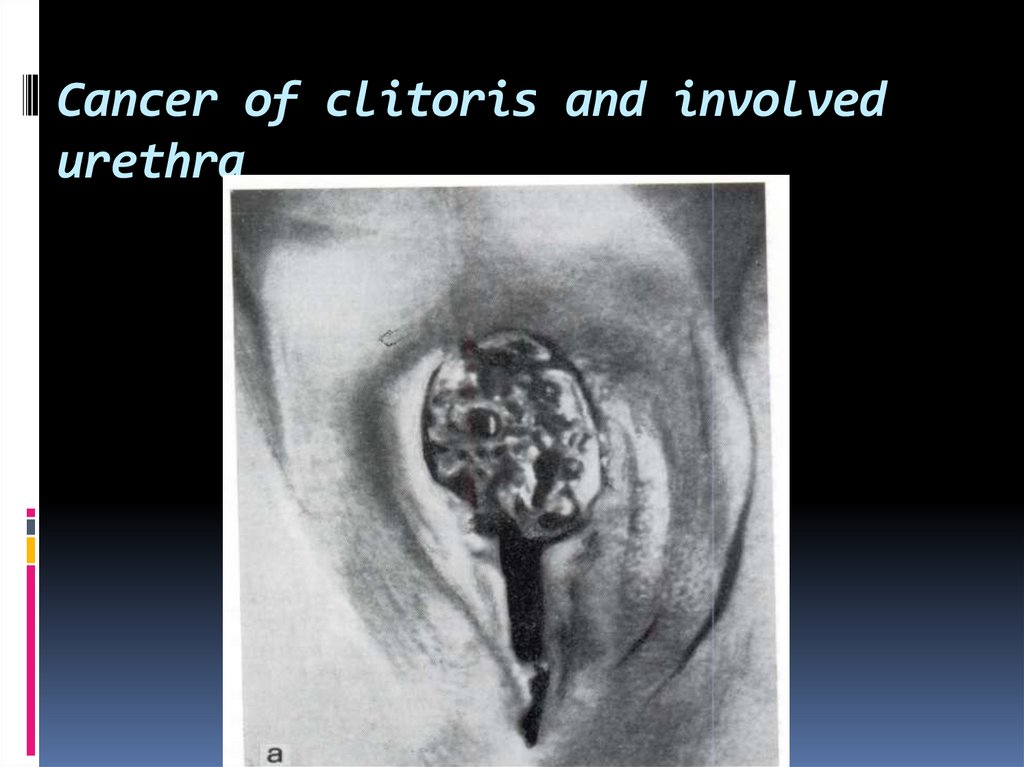
43. Cancer of clitoris and involved urethra
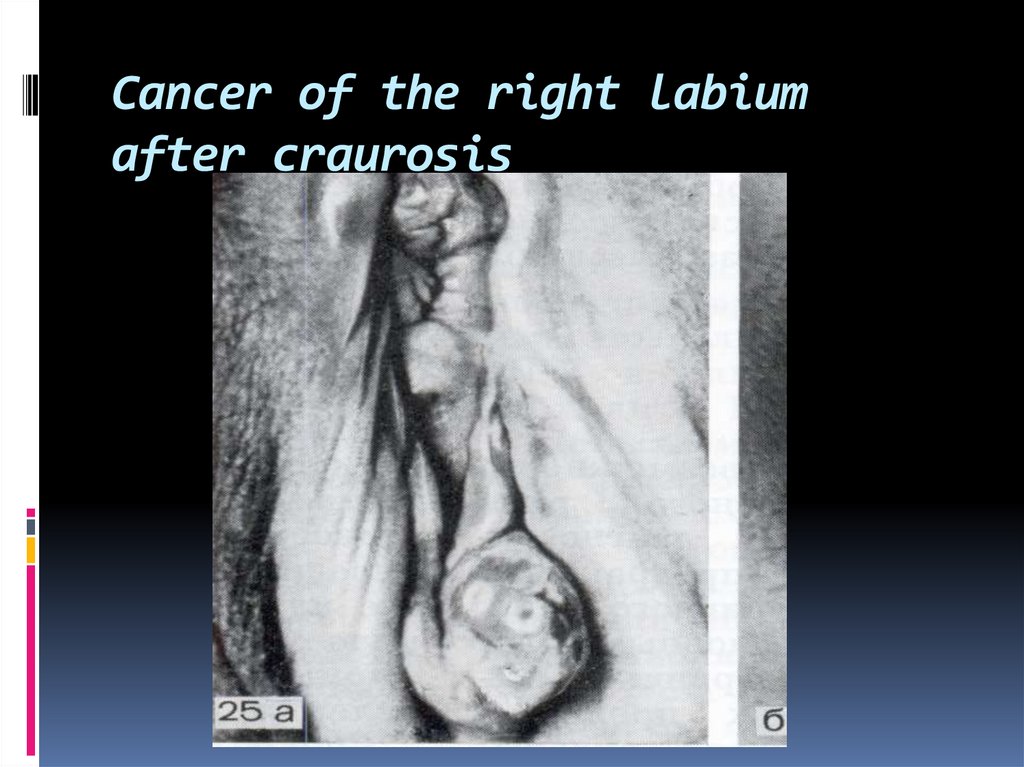
44. Cancer of the right labium after craurosis
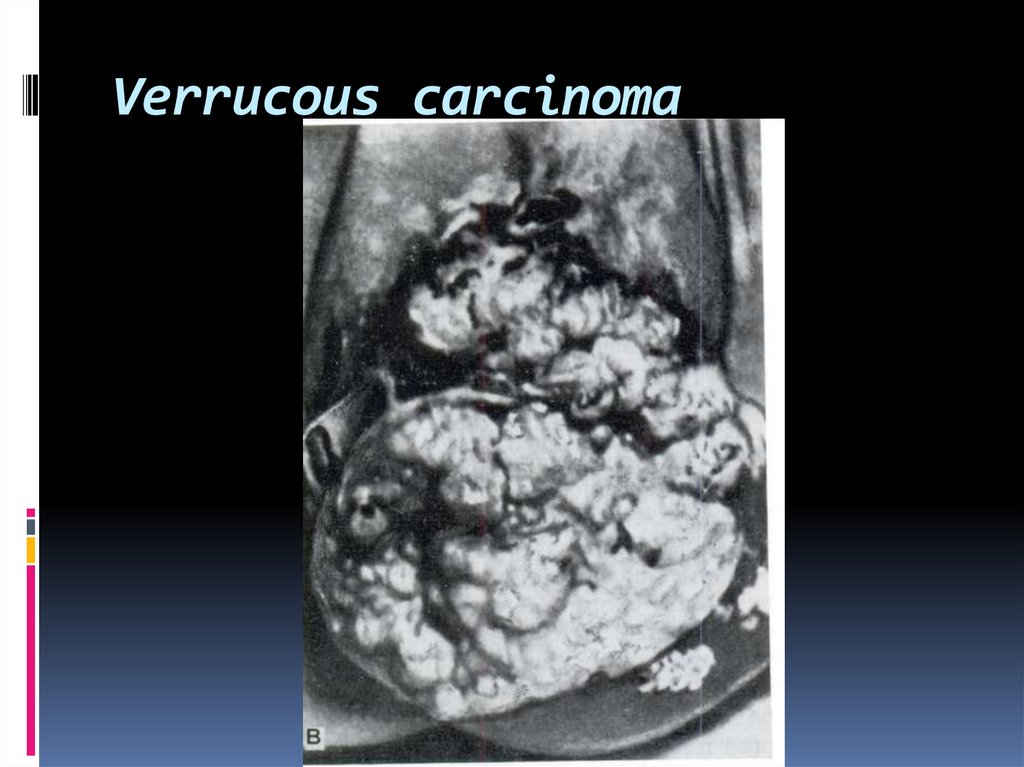
45. Verrucous carcinoma
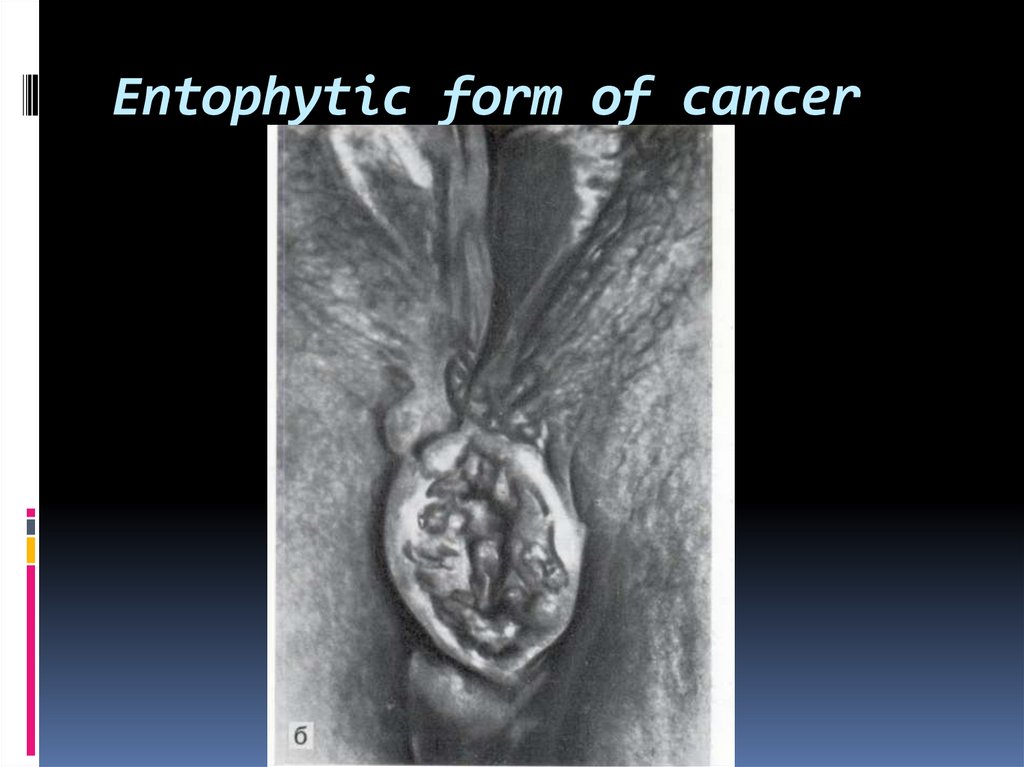
46. Entophytic form of cancer
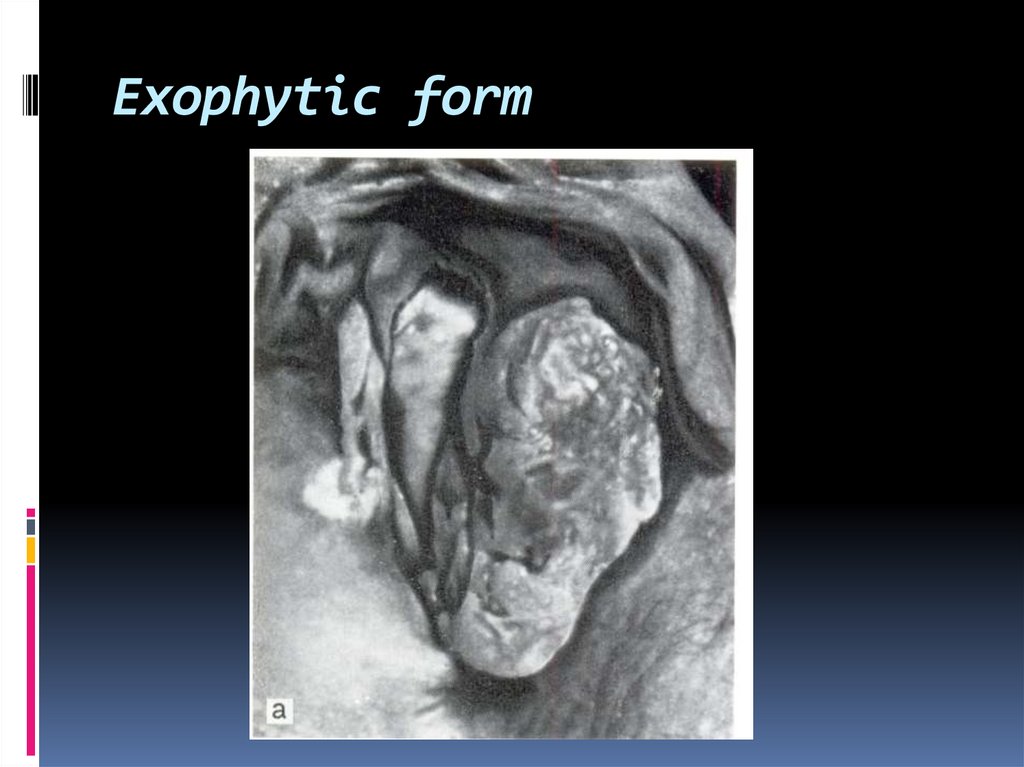
47. Exophytic form
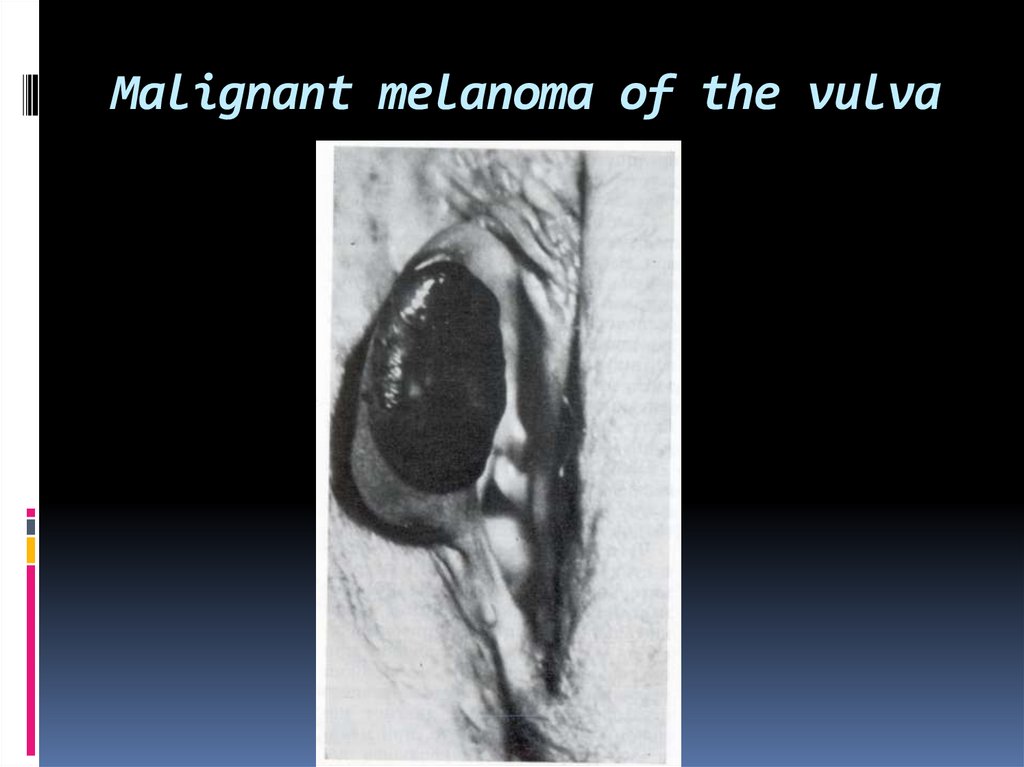
48. Malignant melanoma of the vulva
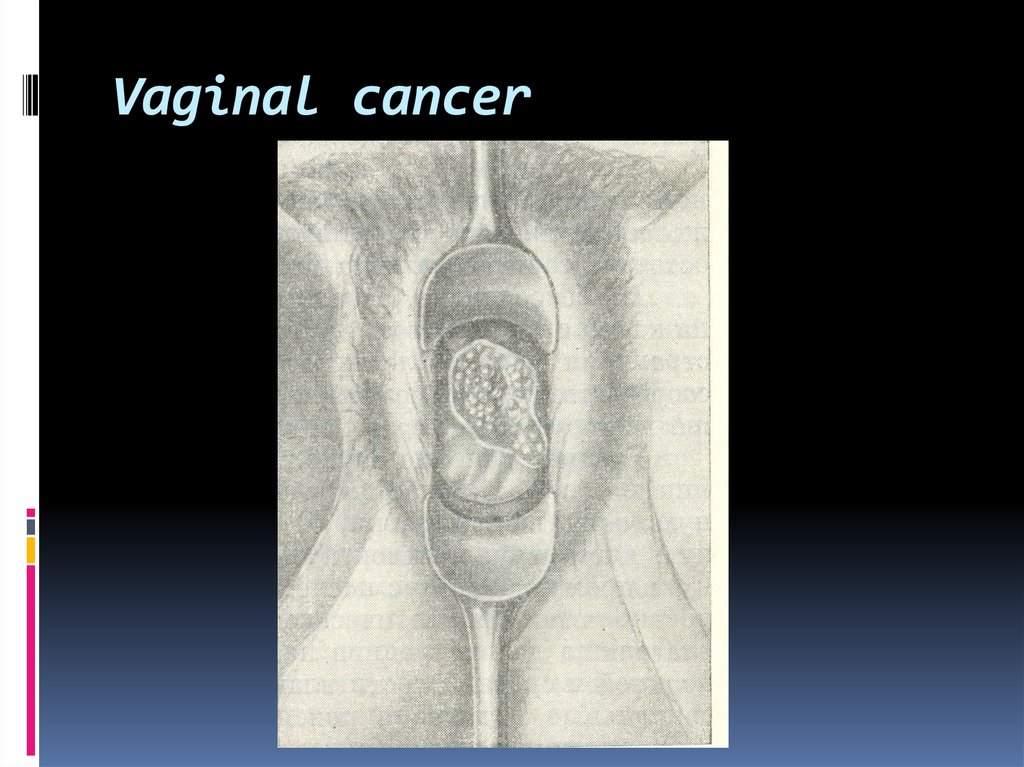
49. Vaginal cancer
50. Vaginal neoplasms
vaginal intraepithelial lesions (VAINs,classified as VAIN 1, 2, or 3, depending
on the thickness of the atypia
invasive vaginal carcinoma