Похожие презентации:
Pediatric HSV Epithelial Keratitis
1. Pediartic HSV Epithelial Keratitis
2.
3.
Herpes simplex virus (HSV) keratitis is an important cause of ocular morbidity thatcan cause
significant vision loss due to its recurring nature. It is caused by the same 2 closely
related viruses:
herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2).
HSV-1 is the first
member of the human herpes viruses (HHV-1) belonging to the subfamily
Alphaherpesviridae. At
least 80% of the world’s population has been exposed to HSV-1.
Children with HSV keratitis pose a unique challenge to the clinician. The most
serious concern in children is that they are susceptible to amblyopia (lazy eye) from
corneal scarring that may
occur. The virus is transmitted from human to human via secreted fluids and close
contact with
mucosal surfaces or abraded skin. Initial infection is usually asymptomatic and
occurs in children
younger than 5 years old. In cases of HSV-2, it is transmitted as the newborn
passes through an
infected birth canal. Ocular infection may occur directly through droplet spread or
indirectly via
neuronal spread from a nonocular site such as the oral mucosa.
4.
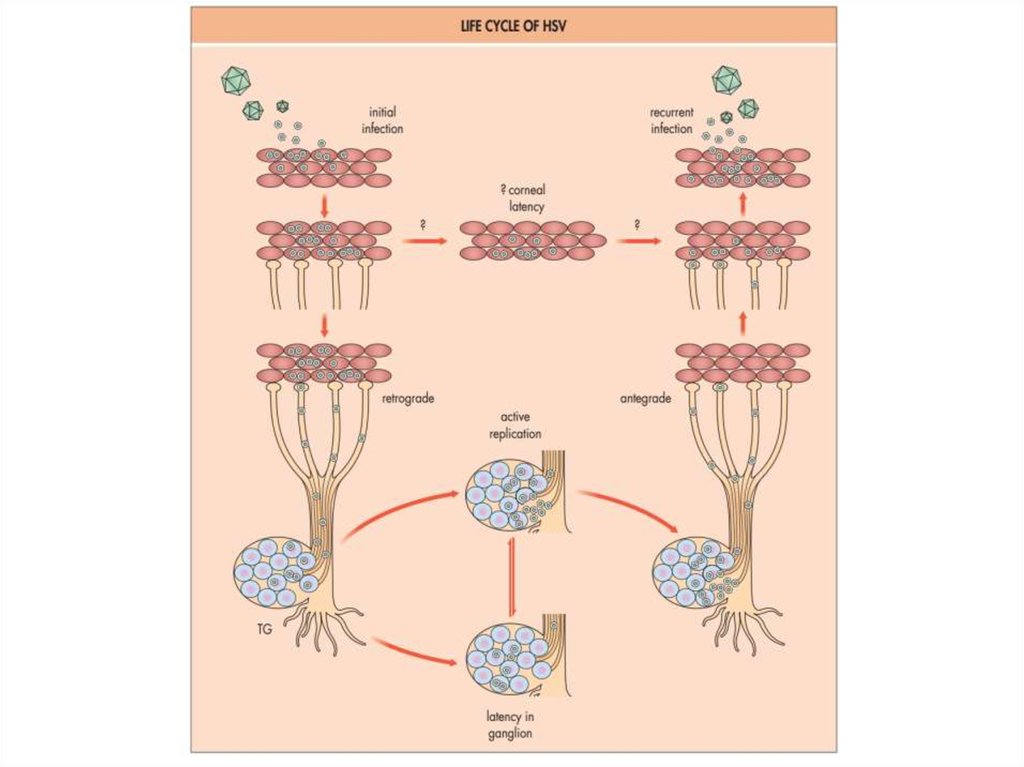
HSV keratitis occurs when the infection reaches the cornealepithelium and stroma of the cornea. Manifestations can include
cutaneous vesicles, blepharitis, conjunctivitis, epithelial keratitis
(corneal dendritic ulcers), and stromal keratitis. Nonspecific
signs of primary herpetic corneal
infection include fever, malaise, and lymphadenopathy. When
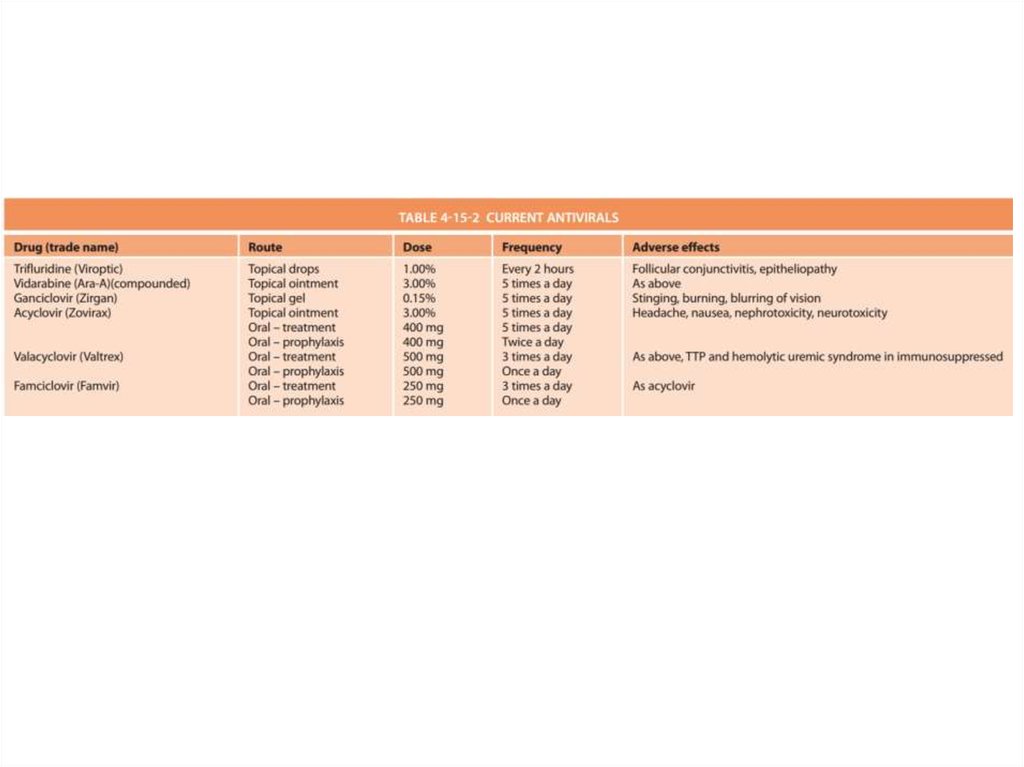
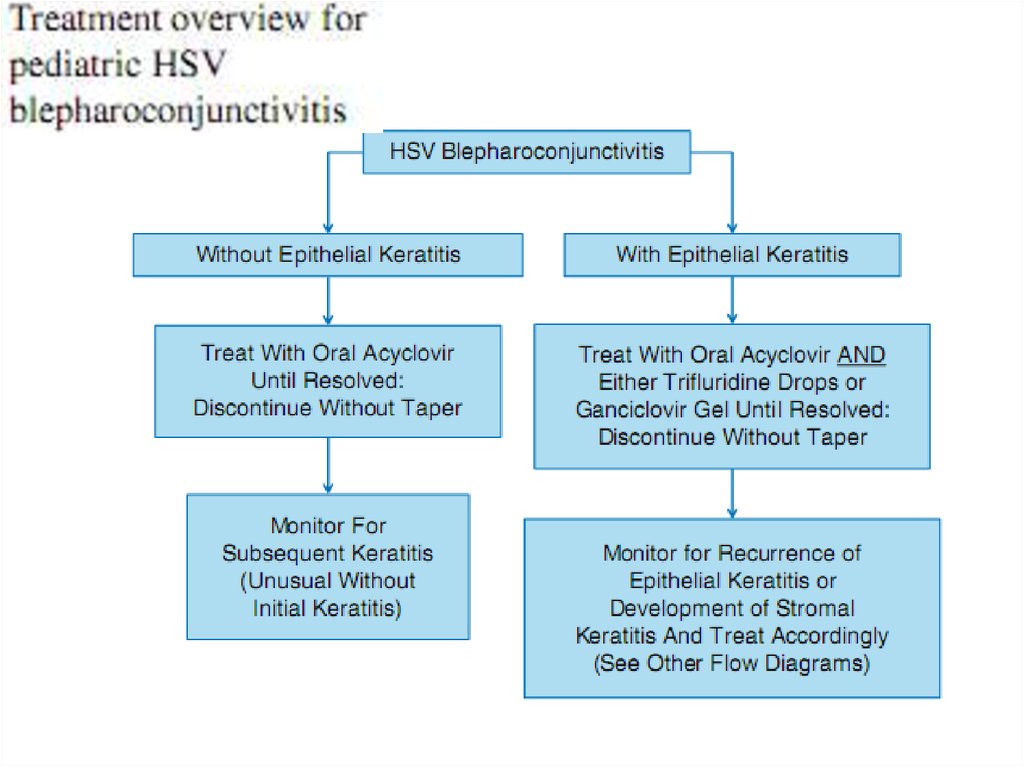
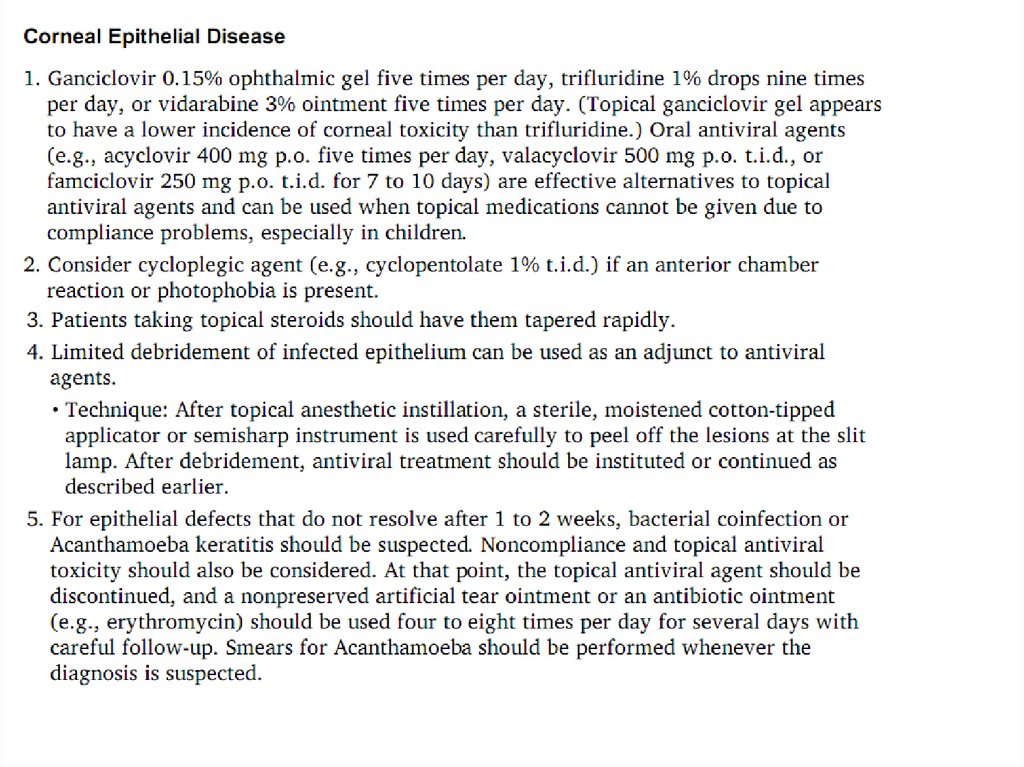
the virus gains access to the central
nervous system, the virus becomes latent in the trigeminal
ganglia (HSV-1 or varicella–zoster
virus [VZV]) or in the spinal ganglia (HSV-2). Recurrent attacks
occur when the virus travels
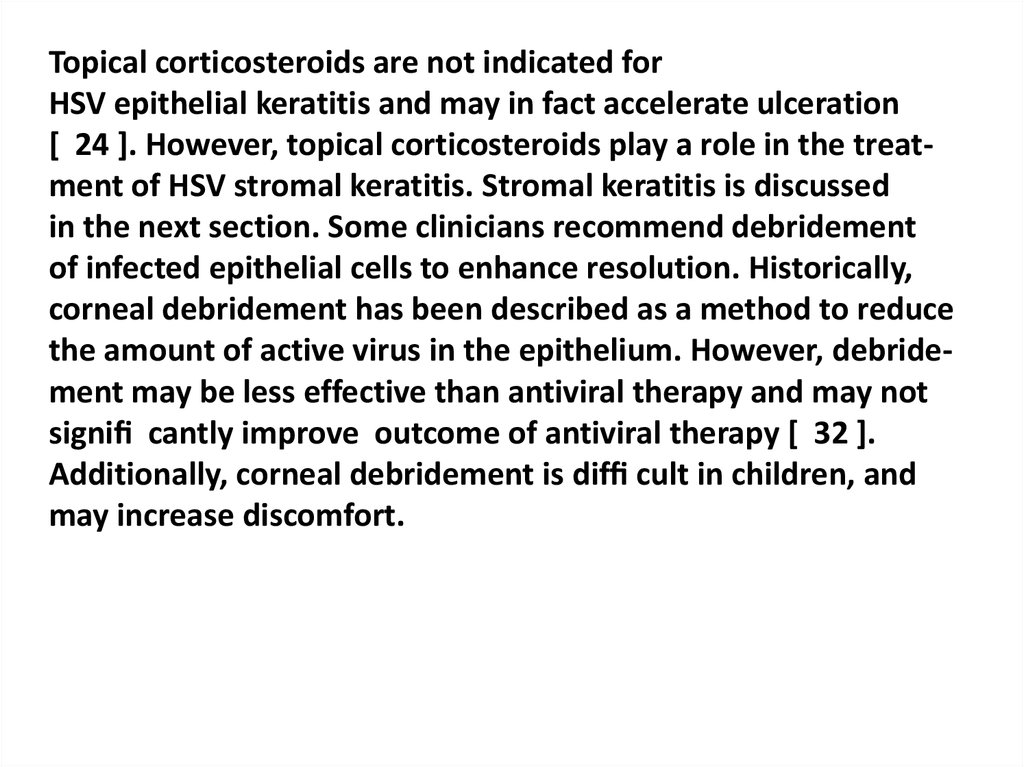
peripherally via sensory nerves to infect target tissues in the
eye. These attacks may be triggered
by any of the following stressors: fever, ultraviolet light
exposure, trauma, stress, menses, and
immunosuppression.
5.
Recurrent ocular HSV-1 infection and inflammation eventuallycause corneal scarring, thinning, neovascularization, and
stromal keratitis. This disease usually occurs unilaterally, but
bilateral infection, although not frequently seen, usually afflicts a
younger age group and can be
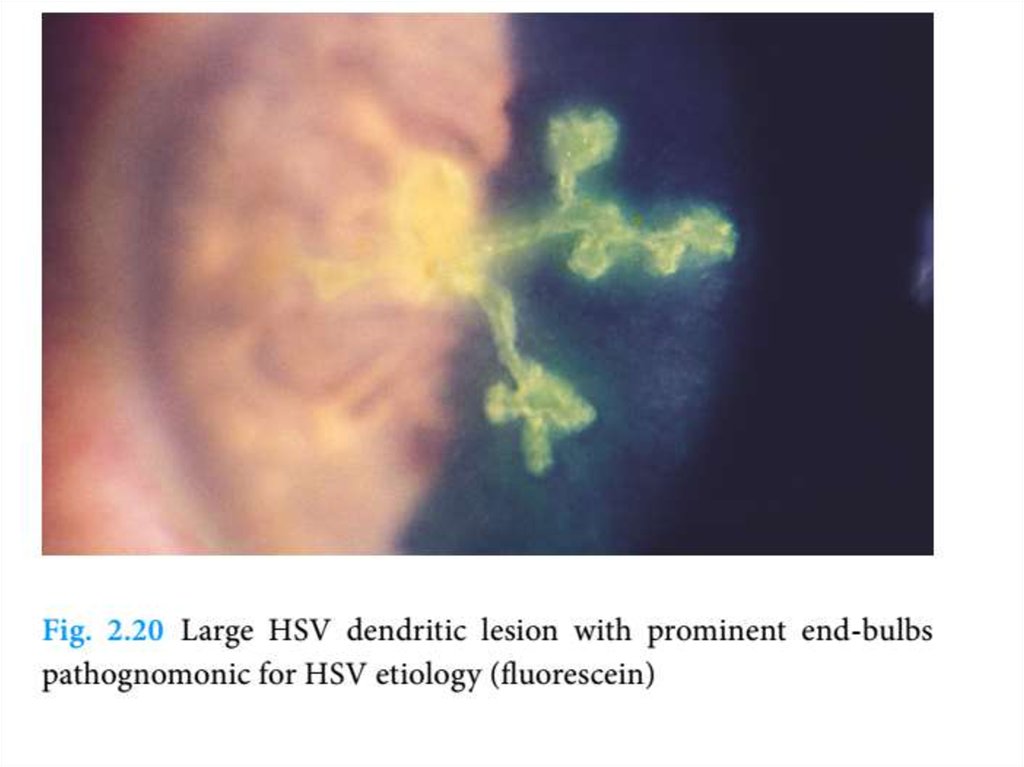
more severe. The corneal dendrites of herpes simplex infections are
epithelial ulcers whose edges
stain brightly with fluorescein and have terminal bulbs (Figure 19-1).
Herpes zoster dendrites
are raised lesions, do not have terminal bulbs, and do not stain well
with fluorescein. Some ophthalmic findings of HSV keratitis are not
directly caused by the viral infection itself, but instead
relate to the immunologic response to the infection, such as chronic
keratouveitis (inflammation
within the anterior chamber of the eye) and disciform and necrotizing
keratitis (cornea is filled
with inflammatory cells and has neovascularization despite an intact
surface).
6.
HSV keratitis in children may differ from that in adults. The rate ofbilateral involvement in
the largest series of infected children was 10% to 26%, which is
higher than seen in adults. The
Herpetic Eye Disease Study estimated that both epithelial and
stromal keratitis recurred in 18%
of patients during a follow-up period of 18 months. Age, sex,
ethnicity, and nonocular herpes were
not significantly associated with recurrences. However, the Herpetic
Eye Disease Study was limited to patients 12 years or older. In
different series of pediatric herpetic viral keratitis, recurrence
rates ranged from 33% to 80%. Corneal scarring and ulcerations
from recurrent herpetic keratitis
can be visually debilitating and potentially necessitate surgical
intervention with penetrating keratoplasty (corneal transplantation)
or tarsorrhaphy (partial lid closure). The inflammatory response
from herpetic keratitis leads to stromal scarring and opacification
and tends to be more severe
in children than adults. For younger children, especially under age
8, the corneal opacity and
irregular astigmatism induced by the scars lead to visual deprivation
and loss of vision. Even with
antiviral therapy, corneal healing can take up to 1 month and will
require continued ophthalmic
care due to residual corneal scarring and risk of vision loss.
7.
8.
HERPES SIMPLEXVIRUS
PRIMARY HSV INFECTION
Primary HSV ocular infection most commonly manifests as
blepharoconjunctivitis (often with conjunctival ulceration) that heals without
scarring (Fig. 4-15-3). The associated follicular conjunctivitis is often
mistaken for adenoviral conjunctivitis (Fig. 4-15-4); up to a third of
unilateral follicular conjunctivitis may be culture-positive for HSV.13–15
Other features include lid vesicles and conjunctival dendrites. Keratitis
is rare, occurring in only 3–5% of cases, though severe bilateral disease
can occur in atopic or immunocompromised patients.
9.
10.
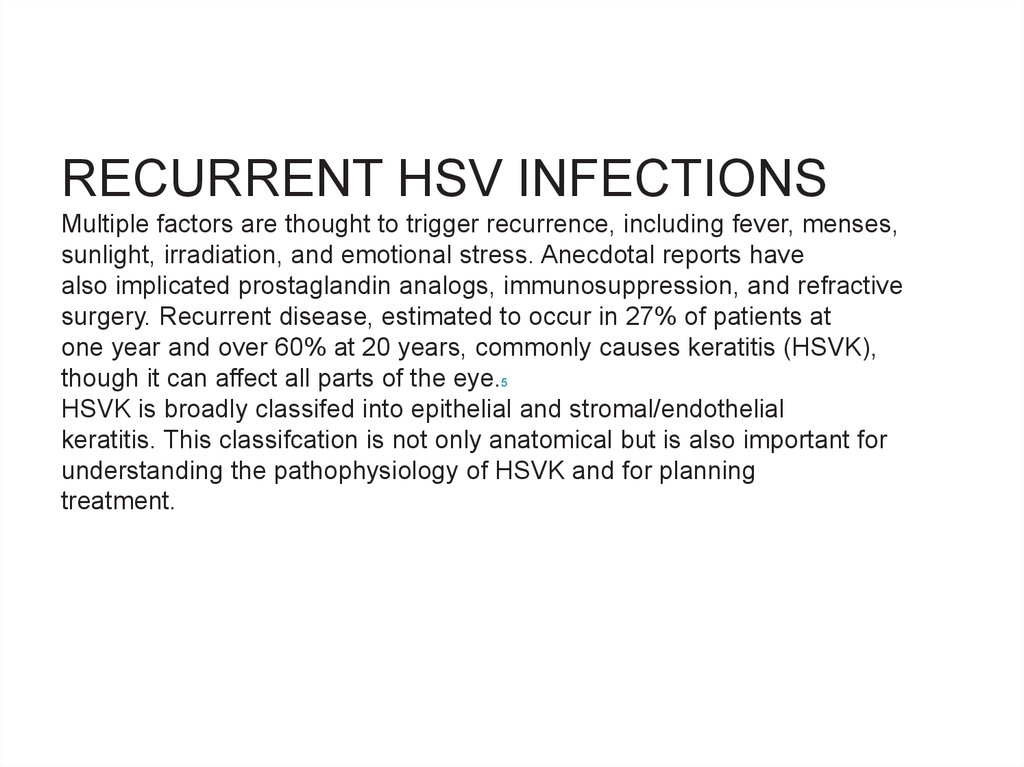
RECURRENT HSV INFECTIONSMultiple factors are thought to trigger recurrence, including fever, menses,
sunlight, irradiation, and emotional stress. Anecdotal reports have
also implicated prostaglandin analogs, immunosuppression, and refractive
surgery. Recurrent disease, estimated to occur in 27% of patients at
one year and over 60% at 20 years, commonly causes keratitis (HSVK),
though it can affect all parts of the eye.5
HSVK is broadly classifed into epithelial and stromal/endothelial
keratitis. This classifcation is not only anatomical but is also important for
understanding the pathophysiology of HSVK and for planning
treatment.
11.
Sunlight, local physical trauma, hormonal changes, andimmunological stress (as by fever) are thought to contribute
to risk of recurrence of non-ocular herpetic disease [ 9 ].
However, with correction for recall bias, the Herpetic Eye
Disease Study (HEDS) Group found that none of these factors were a signi cant cause of recurrent ocular herpes [ 10 ].
However, a history of atopic disease has been associated
with recurrent herpetic eye disease, possibly secondary to
immunologic dysfunction [ 11 – 13 ]. Therefore, the practitioner should inquire about personal and family history of conditions such as asthma, eczema, and seasonal allergies.
12.
Epithelial ulcers may cause sensitivity to light,blurriness, or a foreign body sensation [ 24 ]. In children,
photophobia is easily observed [ 26 ]. Pediatric HSV
keratitis is typically unilateral; however, atopy and an
altered immune system predispose to bilateral disease [ 7 ].
Diagnosis of HSV epithelial keratitis is typically based on
clinical ndings. Figure 11.2 shows a typical HSV
dendrite.
The distinctive appearance and staining pattern of these
ulcers are important diagnostic points.
13.
14.
15.
16.
17.
Fig. 1.17a–d Features of an
HSV dendritic
(branching) fgure, visualized (a)
without staining, (b and c) with
uoresceinsodium, (c and d) in time
sequence, and (d) with rose bengal
dye added. (a) Te fgure consist of
two parts: a central corethat appears
granular (long arrow) and a
surrounding zone (short arrow) (cf.
drawing). (b) Green-stained tear
uid is pooling within the central
core. Te surrounding zone is elevated
(dark). Within this zone, green uid
is pooling between protruding
swollen/rounded cells (dark rounded
dots, arrowhead)
18.
Fig. 1.17 (c) Afer a blink,the stained tear uid
appears more brilliantly
green. As in (b), it is
pooling within the
central core
and between the
protruding
swollen/rounded cells
(arrowhead). So far,
there is no uorescein
di usion into the
elevated surrounding
zone. (d) A few minutes
later, the elevated
surrounding zone is
stained brilliantly green
( uorescein di usion).
Rose
bengal dye reveals
patches of surface
debris within the central
core and a few rounded
dots (arrowhead)
19.
20.
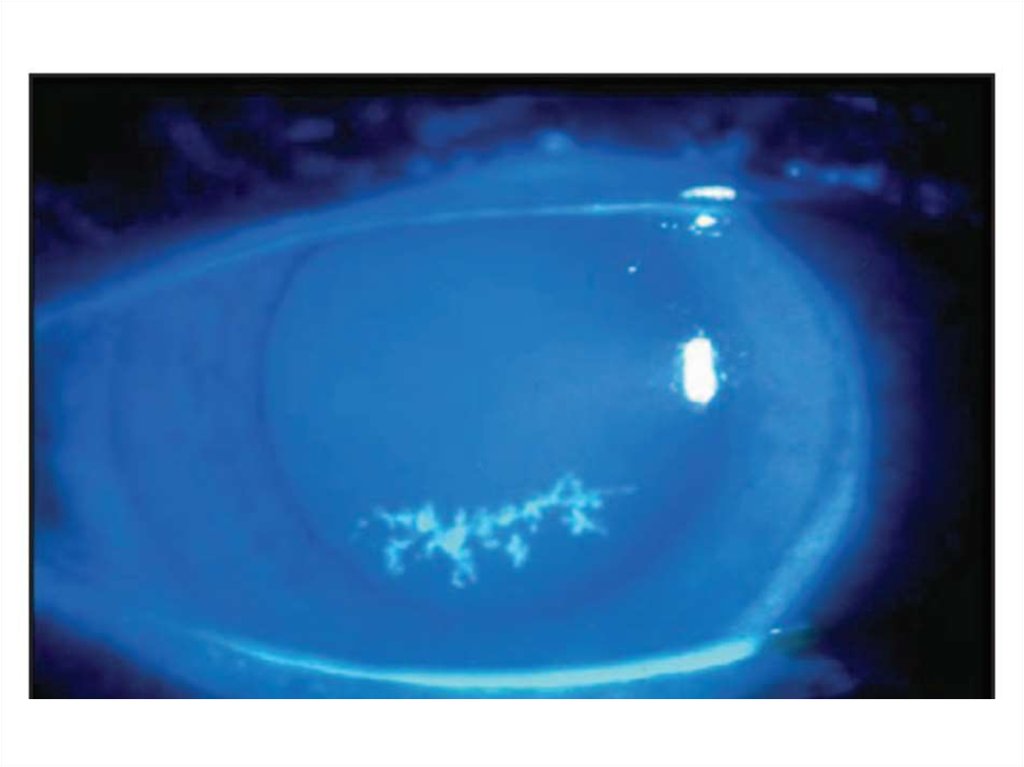
Epithelial herpes simplex keratitis. (A) Stellate lesions; (B) bedof a dendritic ulcer stained with fuorescein;
21.
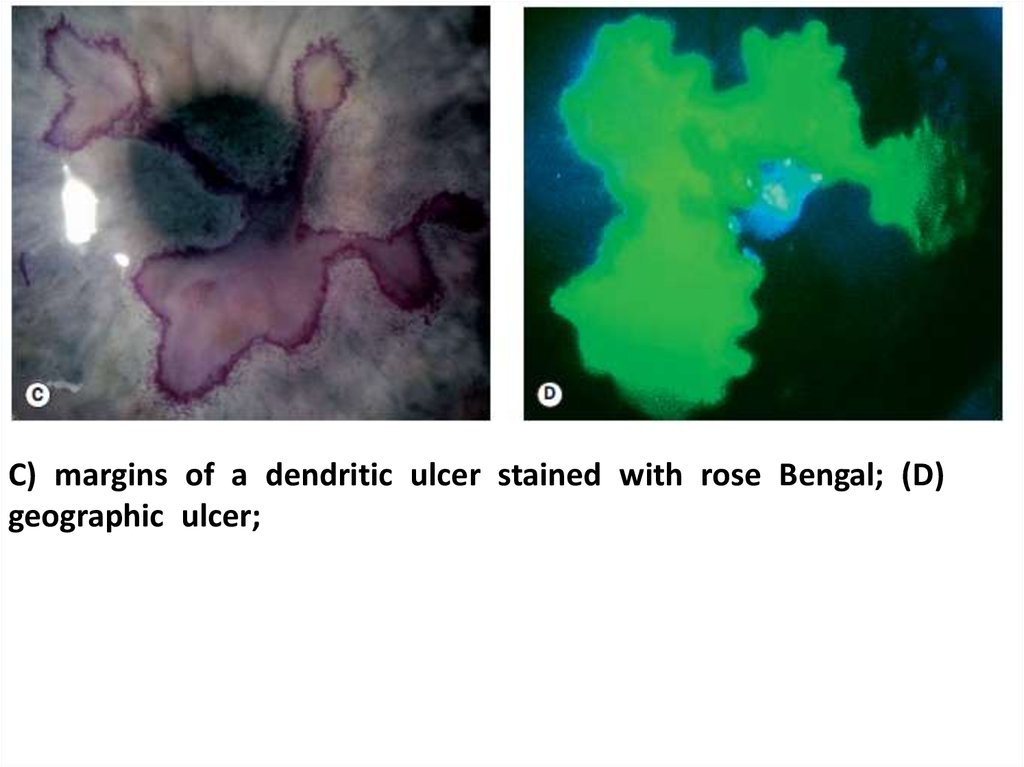
C) margins of a dendritic ulcer stained with rose Bengal; (D)geographic ulcer;
22.
(E) persistent epithelial changes following resolutionof active infection;
(F) residual subepithelial haze
23.
24.
25.
26.
27.
28.
In particular, HSVculture and PCR are commonly available testing methods
that can be utilized to aid in the diagnosis of HSV epithelial
keratitis. Serum antibody testing can identify previous HSV
infection. It is important to note that viral samples for lab
testing should be collected prior to epithelial staining
since rose bengal is toxic to HSV [ 29 ]. Collecting samples
prior to staining will thus reduce false negative test results.
29.
A 5-year-old patient with a history of type I diabetes mellituspresented with 7 days of right eye pain, redness, and irritation. She
was diagnosed with viral conjunctivitis by her primary care physician
but did not improve. Slit-lamp examination with uorescein
revealed a dendritic epithelial defect with terminal bulbs
(Fig. 10.3 ), and she
was subsequently
diagnosed with HSV
epithelial keratitis.
Treatment with
400 mg oral acyclovir
suspension 4 times
daily led to
resolution of the
dendrite with only
minimal corneal
scarring.
30.
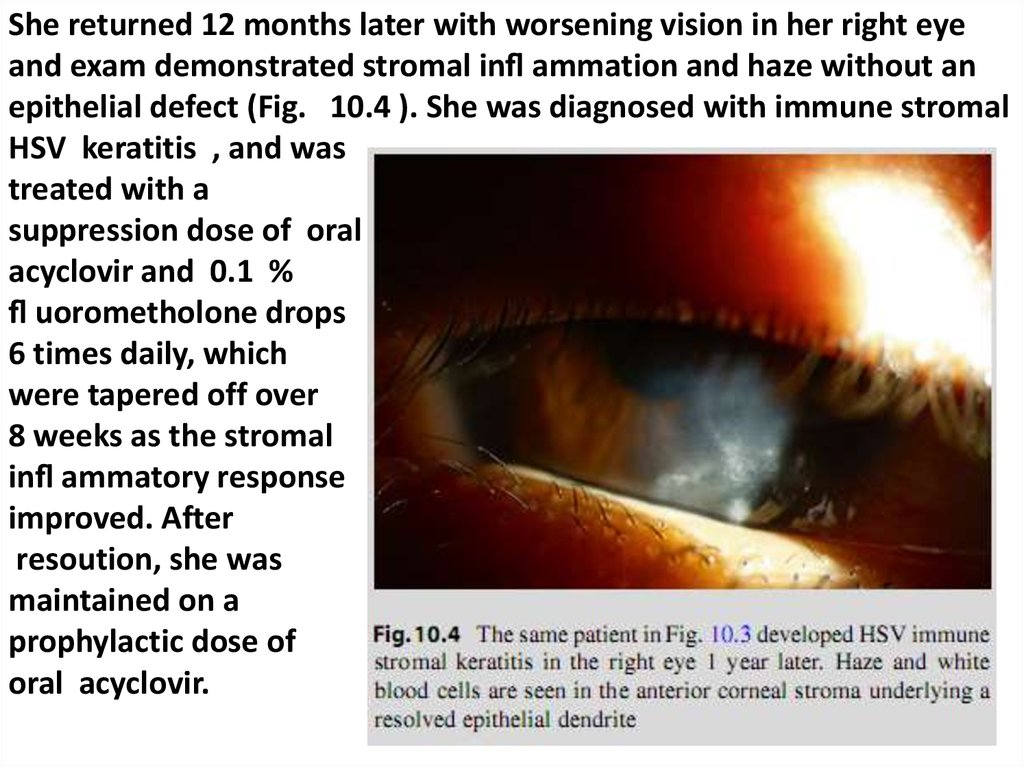
She returned 12 months later with worsening vision in her right eyeand exam demonstrated stromal in ammation and haze without an
epithelial defect (Fig. 10.4 ). She was diagnosed with immune stromal
HSV keratitis , and was
treated with a
suppression dose of oral
acyclovir and 0.1 %
uorometholone drops
6 times daily, which
were tapered off over
8 weeks as the stromal
in ammatory response
improved. After
resoution, she was
maintained on a
prophylactic dose of
oral acyclovir.
31.
Although HSV epithelial disease may resolve in somecases without intervention [ 30 ], medication is utilized to speed
resolution,
reduce corneal scarring, and diminish stromal
in ammation. Since the epithelial ulcers are caused by actively
replicating virus, treatment targets the virus itself. Topical
antiviral drugs (tri uridine drops, vidarabine ointment [not
currently commercially available], or ganciclovir gel) have
been shown to be effective in resolving HSV epithelial keratitis. However, instillation of eye drops in small
children may be dif cult, and tear dilution from crying could
prevent an effective dose. Oral acyclovir thus provides an
important adjunctive treatment for pediatric HSV epithelial
keratitis, and may provide effective treatment without the use
of a topical antiviral [ 21 ]. See Table 11.1 for acyclovir dosage
considerations.
32.
33.
Interestingly, only topical antiviral medication has beenFDA approved for the treatment of HSV keratitis and only
for epithelial keratitis. Evidence-based oral antiviral
treatment protocols have been developed for multiple
forms of ocular HSV disease from retrospective studies as
well as from the prospective studies conducted by the HEDS
Group.
For infectious HSV epithelial keratitis, topical or oral
antivirals are effective. In children, the recommended dose
of oral acyclovir in epithelial keratitis is 12-40 mg/kg/day in
divided doses up to 40 kg, and the adult dose of 400 mg 5
times daily in children greater than 40 kg [2].
34.
35.
Epithelial HSV disease (dendritic ulcer, geographic ulcer)is the result of viral replication, and is treated with a
topical antiviral agent (Table 15.9). Oral antiviral and
topical corticosteroid is not required.
Oral acyclovir did not hasten
healing of epithelial disease when used in combination with
topical treatment.
36.
Topical corticosteroids are not indicated forHSV epithelial keratitis and may in fact accelerate ulceration
[ 24 ]. However, topical corticosteroids play a role in the treatment of HSV stromal keratitis. Stromal keratitis is discussed
in the next section. Some clinicians recommend debridement
of infected epithelial cells to enhance resolution. Historically,
corneal debridement has been described as a method to reduce
the amount of active virus in the epithelium. However, debridement may be less effective than antiviral therapy and may not
signi cantly improve outcome of antiviral therapy [ 32 ].
Additionally, corneal debridement is dif cult in children, and
may increase discomfort.
37.
Unfortunately, as described in the introduction,HSV epithelial keratitis can recur. After an epithelial ulcer resolves, a
faint stromal scar may remain. Recurrent HSV dendritic
ulcers may recur near the scar. Epithelial recurrences increase
the risk of HSV stromal keratitis, an immune-mediated disease process. Recurrence of HSV keratitis is higher in children and is a major management concern [ 21 ]. Thus,
monitoring of children with periodic follow-up examinations
and educating the parents for signs of recurrence are essential.
38.
39.
40.
41.
HSV stromal keratitis classically involves an immunemediated response to inactive HSV antigen in the cornealstroma [ 6 ]. However, complex presentations with mixed patterns of anterior corneal disease and corneal scarring from
multiple recurrences are possible [ 24 ]. Simple HSV stromal
keratitis may present with single or multifocal sub-epithelial
in ammatory in ltrates.
42.
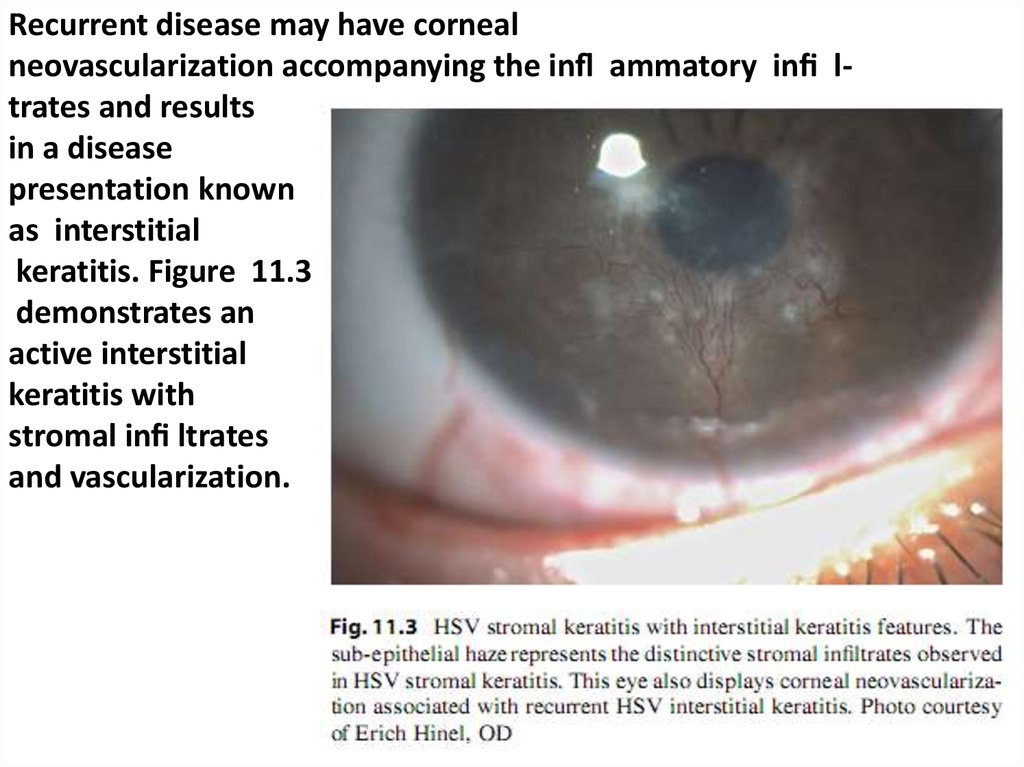
Recurrent disease may have cornealneovascularization accompanying the in ammatory in ltrates and results
in a disease
presentation known
as interstitial
keratitis. Figure 11.3
demonstrates an
active interstitial
keratitis with
stromal in ltrates
and vascularization.
43.
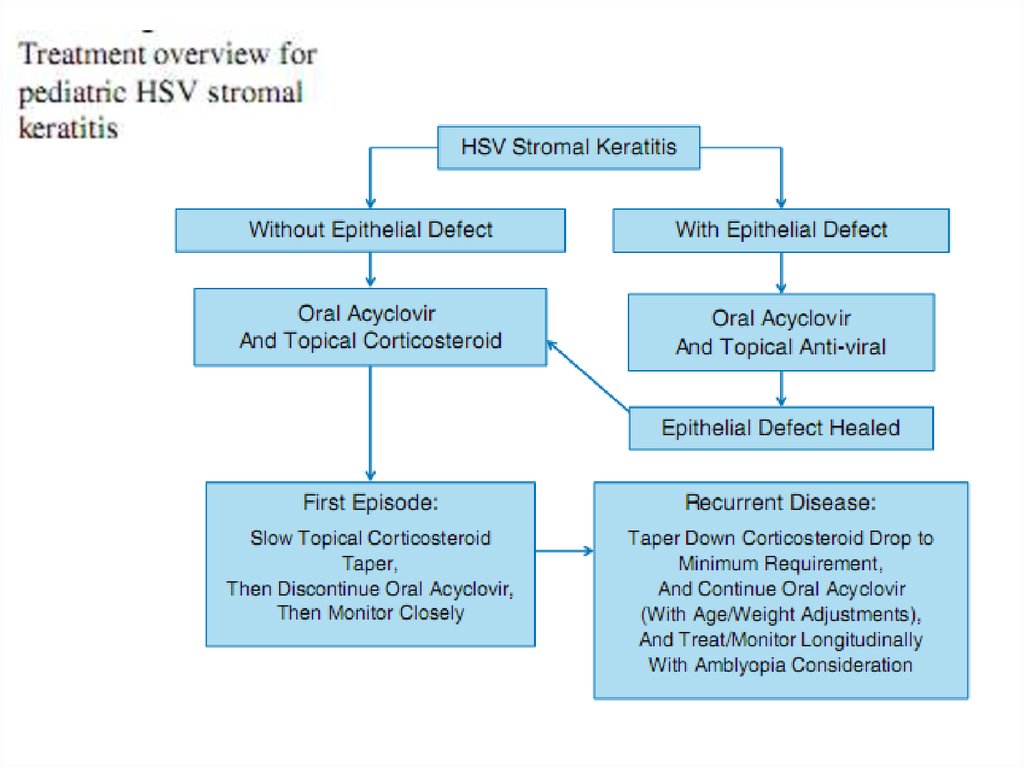
Treatment ofstromal keratitis in children typically involves the use of topical corticosteroids and oral antivirals. The topical corticosteroid is necessary to treat the stromal in ammation, and the
oral antiviral treats any active viral disease in addition to a
putative contribution in preventing recurrence
44.
The topical corticosteroid may be tapered and the oral antiviraldiscontinued after the rst episode. However, longitudinal
treatment throughout the amblyogenic period may be required
to prevent visually debilitating scarring in the visual axis and
resultant amblyopia. Corticosteroid should be tapered to the
minimum amount necessary to control in ammation.
45.
Valacyclovir may be considered forolder teenage patients with HSV stromal keratitis since it has
been FDA approved for long-term treatment (at the 1 g/day
suppressive therapy dose for genital herpes) [ 33 ]. Valacyclovir
is a pro-drug of acyclovir that has an ester moiety that is
removed by esterases to result in the active acyclovir. As a
pro-drug of acyclovir, valacyclovir has greater bioavailability
and would theoretically be expected to have a similar side
effect pro le. Famciclovir has also been approved for longterm suppressive therapy of genital herpes (at 250 mg twice a
day), so it may also be considered for HSV stromal keratitis
in older teenage patients [ 34 ]. However, famciclovir is not
FDA approved for children.
46.
Epithelial keratitis later followed bystromal keratitis or concomitant epithelial
disease.
In cases with concomitant epithelial
disease, topical treatment is generally added
for the rst 2 weeks.
47.
48.
49.
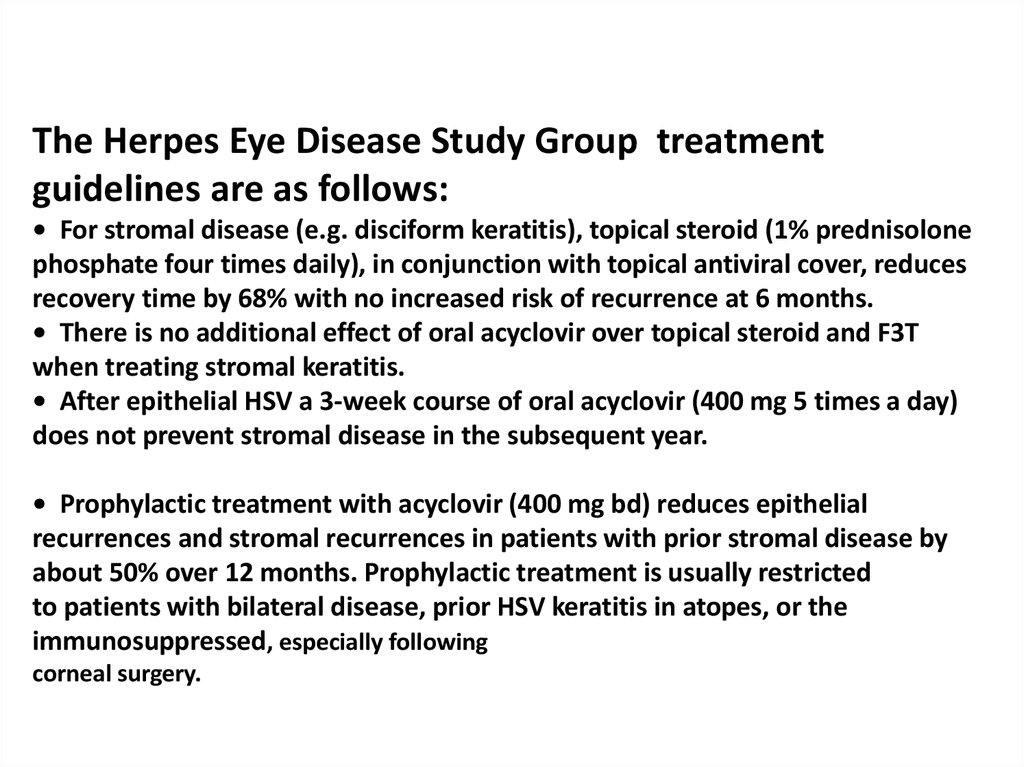
The Herpes Eye Disease Study Group treatmentguidelines are as follows:
• For stromal disease (e.g. disciform keratitis), topical steroid (1% prednisolone
phosphate four times daily), in conjunction with topical antiviral cover, reduces
recovery time by 68% with no increased risk of recurrence at 6 months.
• There is no additional effect of oral acyclovir over topical steroid and F3T
when treating stromal keratitis.
• After epithelial HSV a 3-week course of oral acyclovir (400 mg 5 times a day)
does not prevent stromal disease in the subsequent year.
• Prophylactic treatment with acyclovir (400 mg bd) reduces epithelial
recurrences and stromal recurrences in patients with prior stromal disease by
about 50% over 12 months. Prophylactic treatment is usually restricted
to patients with bilateral disease, prior HSV keratitis in atopes, or the
immunosuppressed, especially following
corneal surgery.
50.
51.
Typical features of a neonatal HSV infection include localizedexternal lesions (skin, eye, and/or mouth), disseminated
herpes affecting internal organs, and central nervous system
infection (encephalitis). An infected infant may display several of these features. Ocular herpes in the newborn typically
appears as periorbital skin vesicles, blepharoconjunctivitis,
keratitis, anterior uveitis, chorioretinitis, and congenital cataracts [ 3 , 39 ]. Importantly, a dilated fundus examination
should be performed in any neonate with suspected HSV
infection. Since herpes infections may resemble other neonatal infections, laboratory tests (e.g., uorescein antibody tests,
herpes culture, or PCR testing) should be performed in all
cases of suspected neonatal herpes [ 28 ]. While awaiting lab
results, the newborn should be empirically treated with intravenous acyclovir.
52.
Overall prognosis of neonatal ocular HSV infectiontreated with intravenous antiviral therapy is generally good.
However, mortality is higher in newborns with disseminated
infection or CNS disease [ 28 ]. Visual outcome is poorer
when corneal herpetic disease causes scarring. Infants must
also be monitored closely for evidence of recurrent disease.
Infants with recurrent HSV keratitis are typically followed
longitudinally by an infectious disease specialist.
Additionally, longitudinal follow-up by a
pediatric ophthalmologist is important due to the risk of amblyopia development associated with recurrent HSV keratitis. If there is
recurrent neonatal ocular HSV infection, higher oral doses of
acyclovir may be necessary.






































 Медицина
Медицина