Похожие презентации:
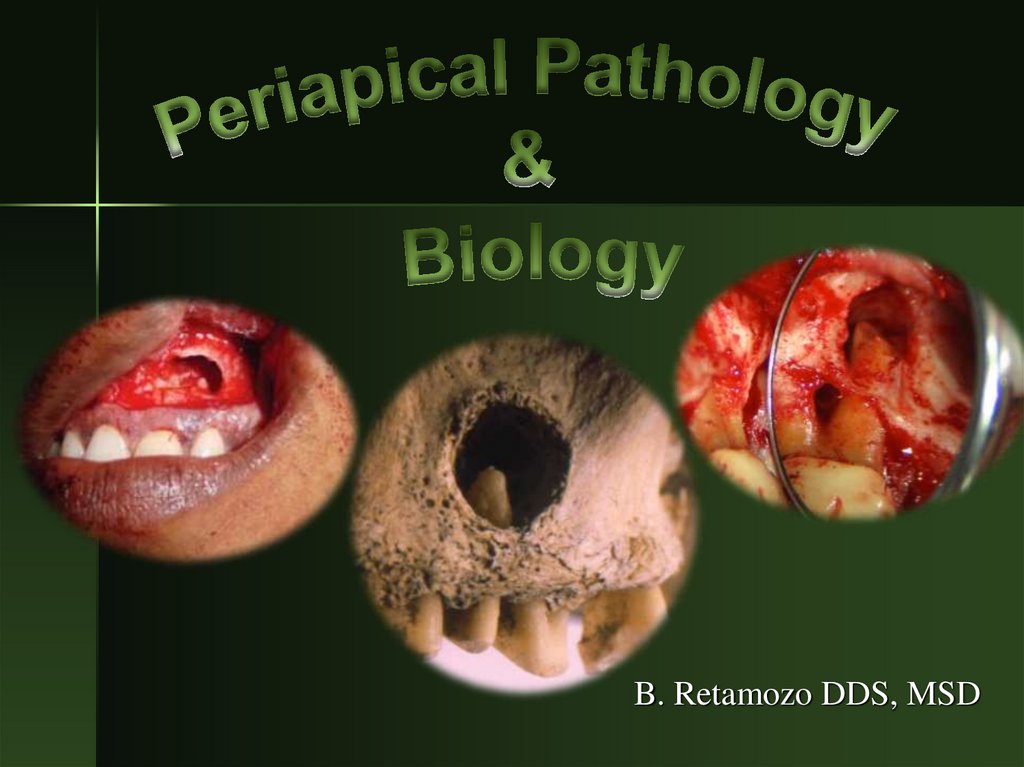
Periapical Pathology
1.
B. Retamozo DDS, MSD2. Pulpitis = Inflammation of the Pulp
Irritant– Direct irritation
– Chemical irritation
Fillings
Erosion
Bleaching
– Thermal changes
Uninsulated large
fillings
Drilling
– Mechanical damage
Trauma
Bruxism
Attrition
Abrasion
Bacterial irritation from
caries
Cracked tooth
Root fractures
Immune response
– Chemical mediators that
initiate inflammation
3. Microbial Irritant
Microbes produce toxinsInitially pulp is infiltrated by chronic
inflammatory cells
– Macrophages, lymphocytes & plasma cells
Secondarily PMNs infiltrate
– Area of liquefaction necrosis
4. The Infectious Process
Sites of established infection
– Main pulp canal space and walls
– Accessory canals and apical delta
– Dentinal tubules
– Cementum surface
– Extraradicular colonizations
Relative importance? – few data, but
the root canal infection is of course paramount
–
Brynolf 1966, Langeland et al. 1977
5. The Infectious Process
Apicalperiodontitis
The Infectious Process
Pulpitis
Necrosis
Canal
infection
Spread to
apex
Increasing infectious load;
increasingly difficult to treat
Time
6. The Inflammartory Process
Mast cells– Histamine release
Kinins
– responsible symptoms of acute inflammation
Cellular damage releases Phospholipase A2
– Prostaglandins, thrombaxanes & leukotrienes
Neuropeptides: SP & CGRP
– Recruit inflammatory cells
7. Inflammation => Necrosis
Inflammation => NecrosisPulp can impede spread of infection
Factors
– Virulence of bacteria
– Ability of pulp to release inflammatory factors to
prevent increase in intrapulpal pressure
– Host resistance
– Lymph drainage
Necrosis: coronal => apical
8. More about inflammation..
Inflammation => vascular responseIncreased vascular permeabiltiy
Infiltrate of leukocytes
Decreased lymphatic drainage
Edema =>
Increased local pressure
9. So whats really going on?
Pulp is enclosed within calcified walls– Low compliance system
Circulation slows due to compression of
venous return
– Odontoblasts are altered or destroyed
Increase in tissue pressure
– Compression of venules in area of injury
– Progresses coronal => Apex
10. The sum total of the inflammatory response may cause more damage that the initial irritants alone!
11.
12. Time-Course of Apical Peridontitis
Dynamics of pulpal infection
Bacterial succession and variations in
virulence and pathogenicity
Host factors modulating inflammation
and spread of the infection
Ultimate consequences of root canal
infection
13. Microbes
BaumgartnerMicrobes
Type:
– Dependent on the environment, nutrients, and
competition
Primary infection:
– Obligate anaerobes and Gram Negative bacteria.
Secondary infection:
– Facultative and Gram Positive bacteria. Including E.
Faecalis and candida.
14. Natural Course of the Disease Vs. Pain
Varies in intensity and severity
– Pain sometimes accompanies pulpitis and apical
periodontitis
Unpredictable if untreated
– Pulpitis and acute apical periodontitis dominate as sources
for acute dental pain in children and adults (Zeng et al 1994,
Lygidakis et at 1998)
– which may be debilitating to the patient and lead to absence
from work and involvement of costly health services.
(Ørstavik, 2009)
15. Inflammation of the periapical region
Relationship between pulpal and periapicalpathosis
– Periapical pathology follows pulp pathology
Periapical disease meets a more effective
resistance that pulpal disease
– Repair is more often achieved
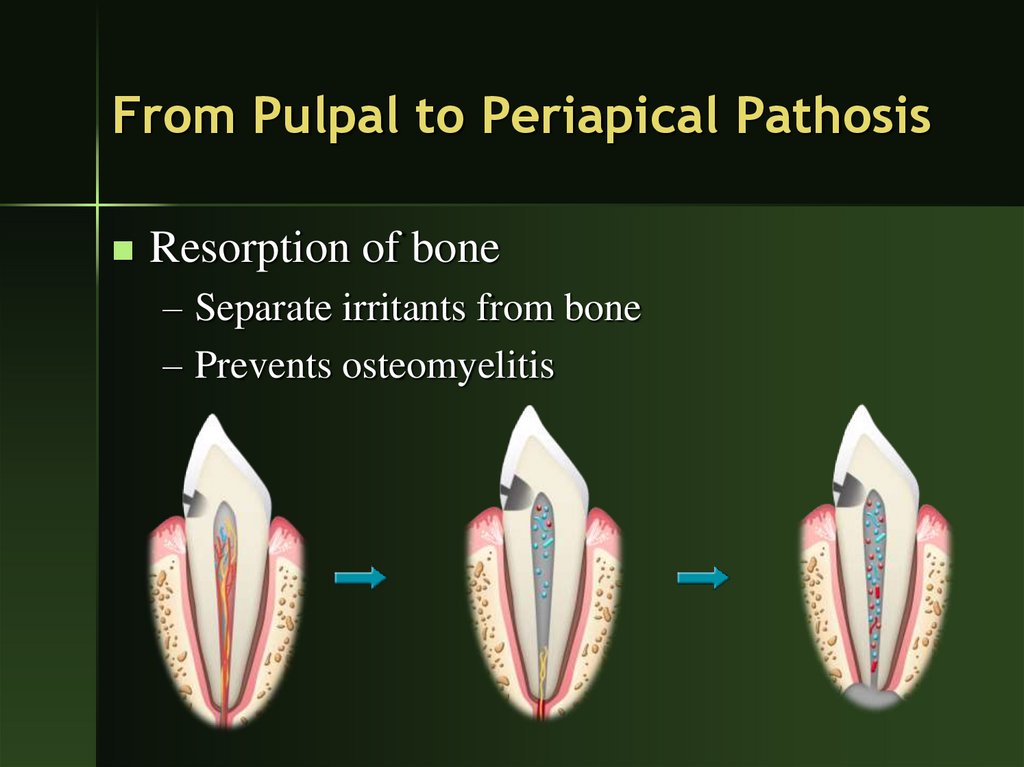
16. From Pulpal to Periapical Pathosis
Resorption of bone– Separate irritants from bone
– Prevents osteomyelitis
17. Periapical Pathosis
Bacterial endotoxins & inflammatorymediators trigger surrounding immune cells
Defense cells
– Prevent spread of infection into bone
Cytokines: interleukins and TNF
– activate surrounding osteoclasts to destroy bone
18. Periapical Pathosis
Bone is replaced by highly vascularizedinflammatory tissue which can much better
eliminate invading microbes than the original
bone tissue could have.
19. Periradicular lesions of pulpal origin
Symptomatic apical periodontitisAsymptomatic apical periodontitis
Apical abscess
Symptomatic
Apical Periodontitis
Apical Abcess
20.
Periapical InflammationPeriapical
Abscess
Apical
Periodontitis
Cellulitis
Osteitis
Osteomyelitis
Cavernous sinus
thrombosis
Periapical cyst
21. Symptomatic Apical Periodontitis
Clinical features–
–
–
–
–
Localized
Frequently spontaneous
Intense throbbing pain
Painful to touch
None to minimal swelling
22. Symptomatic Apical Periodontitis
Histology– Inflammation of the PDL with acute and
chronic inflammatory cells
X-ray exam
– no change to slight thickening of
periodontal membrane
Treatment
– RCT or extraction
23. Asymptomatic Apical Periodontitis
Clinical features– Represents a “stand-off” between local
resistance and noxious stimuli
– Indicative of pulpal necrosis
– Common
– Painless
– Slow growing
– May transform into a cyst or granuloma
24. Asymptomatic Apical Periodontitis
Histology– Proliferation of fibroblasts and endothelial
cells
– Lymphocytes, plasma cells and phagocytes
Foam cells and cholesterol clefts
– Epithelial rest of Malassez
X-ray
– Large radiolucency up to 1cm
Treatment => RCTx or extraction
25. Asymptomatic Apical Periodontitis
26.
27. Periapical Abscess
A localized collection of pus in a cavityformed by the disintegration of tissues.
Indicative of pupal death
Type is based on the degree of exudate
formation, severity of pain and the presence
of symptoms
– Symptomatic apical abscess
– Asymptomatic apical abscess
28. Periapical Abscess
Clinical features–
–
–
–
–
–
Rapid onset of extreme pain
Painful to percussion
Not localized – adjacent teeth can be painful
SWELLING present
Sinus tract can form
Potentially life threatening
29. Periapical Abscess
Histology– Resembles and acute apical periodontitis
– Involvement of the adjacent bone and soft tissue
– Pus and tissue necrosis
X-ray
– Widened PDL to large alveolar radiolucency
Treatment
– Rx for antibiotics
– Establish drainage
30. Untreated Apical Abscess
Cellulitis– Infection travels through the facial planes of least resistance
– Fever
Osteomyelitis
– Infection within bone through the medullary spaces
Parulis = “gum boil”
Ludwig’s angina
– Swelling in floor of mouth elevates tongue and blocks
airway
Cavernous sinus thrombosis
– Infection from MX premolars and molars extends into the
cranial vault
31. End-Points of Root Canal Infections
Immediate abscess and sinus tract formation: incidence?
Chronic, stable encapsulation
Chronic cyst formation
Exacerbation of chronic lesion: incidence (5% per year?)
Sinus tract formation: incidence?
20 – 70%
– Any available surface, sinus, nose, mucosa, skin
Spreading oral infection: incidence?
– Submandibular, sublingual, local fascies
– Eyes, brain, mediastinum
32. Spread of infection… The path of least resistance
Buccal plate is the most common route due tothe thin buccal bone
Outside on face
Palate
Neck below mylohyoid
PDL
Pulp canal
Maxillary sinus
Mandibular canal
33.
34.
35.
36.
37.
38.
39. Apical Periodontal Cyst / Granuloma
Clinical features– The most common cyst of the jaws
– May be asymptomatic of become
symptomatic
– Slow continuous enlargement
X-ray
– Well-circumscribed radiolucency
– Associated with apices of teeth
– May cause resorption of teeth and bone
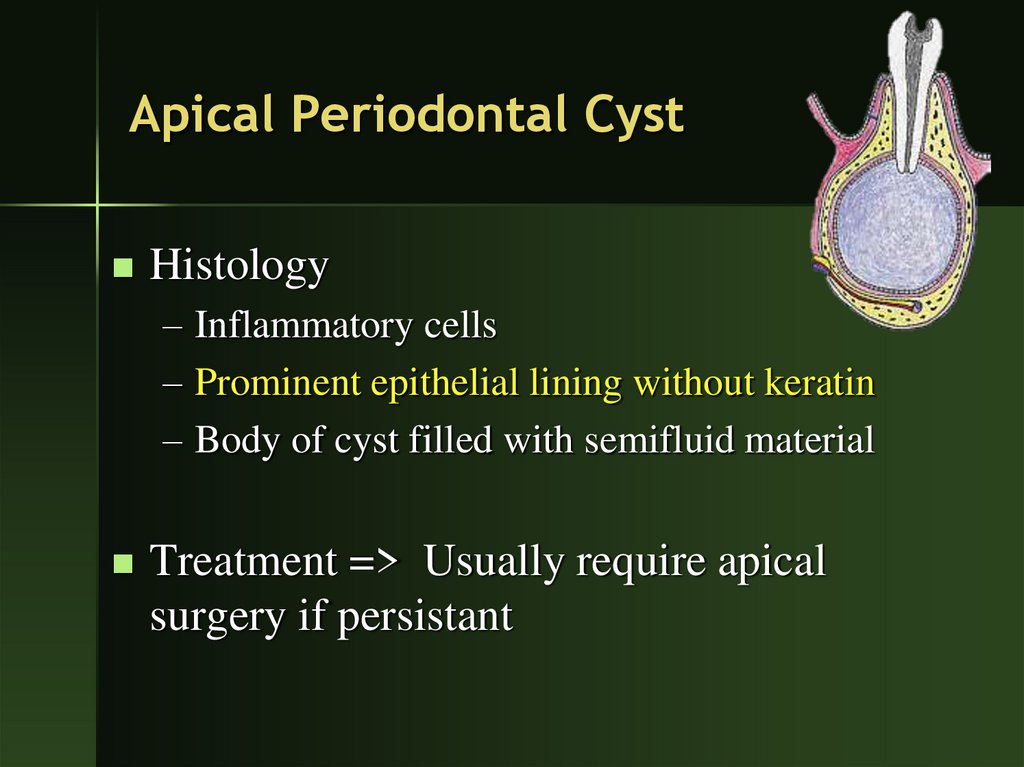
40. Apical Periodontal Cyst
Histology– Inflammatory cells
– Prominent epithelial lining without keratin
– Body of cyst filled with semifluid material
Treatment => Usually require apical
surgery if persistant
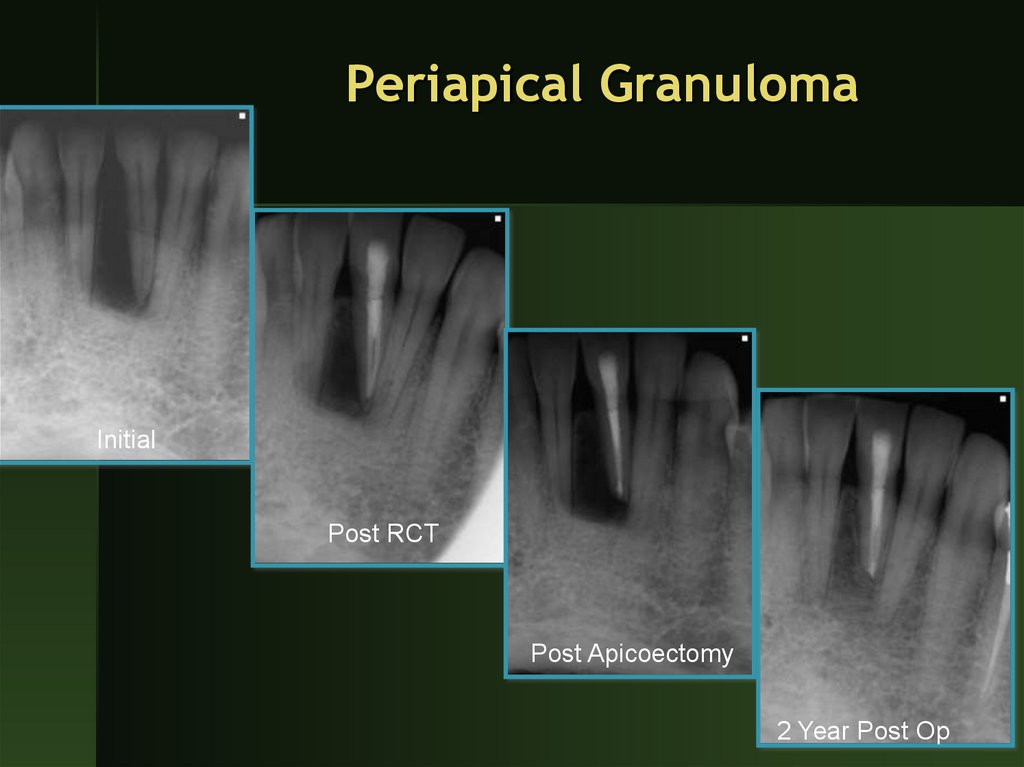
41. Periapical Granuloma
InitialPost RCT
Post Apicoectomy
2 Year Post Op
42. Apical Cyst vs. Granuloma
A cyst is lined by squamous epithelium and containingnecrotic material in the lumen. The cyst wall or capsule
contains dense fibrous connective tissue with slight chronic
inflammation and cholesterin slits surrounded by foreign
body-type giant cells. There are "foam" cells in the epithelial
lining.
A lesion with highly vascular tissue containing macrophages,
fibroblasts, collagen, and immune cells (neutrophils, plasma
cells, T and B cells, lymphocytes, eosinophils
43.
44. Natural Course of the Disease: Conclusions
Unpredictable if untreated
It does not heal
Potentially very painful
Serious complications/sequelae are rare
Filling therapy
Endodontics
Extraction
Pulpitis ->Necrosis->Apical Perio->Acute phases->Local spread->Systemic spread
45. condensing osteitis aka periapical osteosclerosis
Bone sclerosis around apices of tooth with pulpitisOccurs when there is high tissue resistance to low
grade infection
Clinical features
–
–
–
–
Adolescents and young adults
Most common in mandibular first molars
Tooth usually has large carious lesion
No symptoms
46. Condensing Osteitis
Histology– Dense bony trabeculation
X-ray
– Area of radiopaque sclerotic bone with no
radiolucent border
– Entire root outline is visible
– 85% disappear after extraction
47. Condensing Osteitis
Treatment– None
– RCTx
Bone Scar
– The residual area of condensing osteitis that remains
after resolution of inflammation
Differential diagnosis
– Idiopathic osteosclerosis
– Periapical cemental dysplasia
48. Condensing osteitis
49. Osteomyelitis
If the periapical infection and inflammation extendthrough the marrow spaces of the jaw, the result is
osteomyelitis. In this case, you can identify the offending
tooth causing the diffuse and irregular bone destruction.
50.
51. Tooth for Competency II
Plastic Maxillary PremolarBefore the exam
– Mount tooth
– Place your box number in the acrylic of the tooth
– Take 2 initial x-rays
Get nail polish and start check
Access
Clean, shape and obturate one canal
52. Tooth for Competency II
X-rays that must be turned in with tooth– 1 film for total length of root canal
– 1 film with largest working file to working
length
– 1 film with master cone
– 2 final films
Place tooth in ziplock bag with paperwork
and x-rays marked with your box # to your
instructor
53. Final words
All projects must be graded before the endof the competency exam
Remediation of the competency
– Must be done prior to start of break to receive
satisfactory grade
Clinic privileges
– Any molar
Mounted in Endo typodont on the manikin
Access, clean, shape and obturate all canals







































 Медицина
Медицина