Похожие презентации:
Introduction to the Oral Cavity and Periodontal Disease
1. Histology: Introduction to the Oral Cavity and Periodontal Disease
Histology: Introduction to theOral Cavity and Periodontal
Disease
2.
Learning ObjectivesTo recognize the normal structure of the tooth
To recognize the normal structure of the supportive tissues of dentition: gingiva,
periodontial
ligament, cementum and alveolar bone.
To understand the normal mechanisms that anchor a tooth in the jaw
List the symptoms of periodontal disease
Describe the pathophysiology of periodontal disease
Understand the connections between periodontitis and systemic diseases
Identify the three major salivary glands.
Distinguish between a mucous and serous secreting acinus.
To recognize the structure & function of three types of ducts in the salivary glands.
Appreciate the organization of the skeletal muscles of the tongue.
Distinguish among the three types of lingual papillae and the function of each.
Discuss the specific cell types that form the taste buds.
2
3. Oral Cavity
Consists of:• Tongue
• Salivary glands
• Teeth
• Tonsils (will be covered in
lymphatic system)
3
4. Tongue
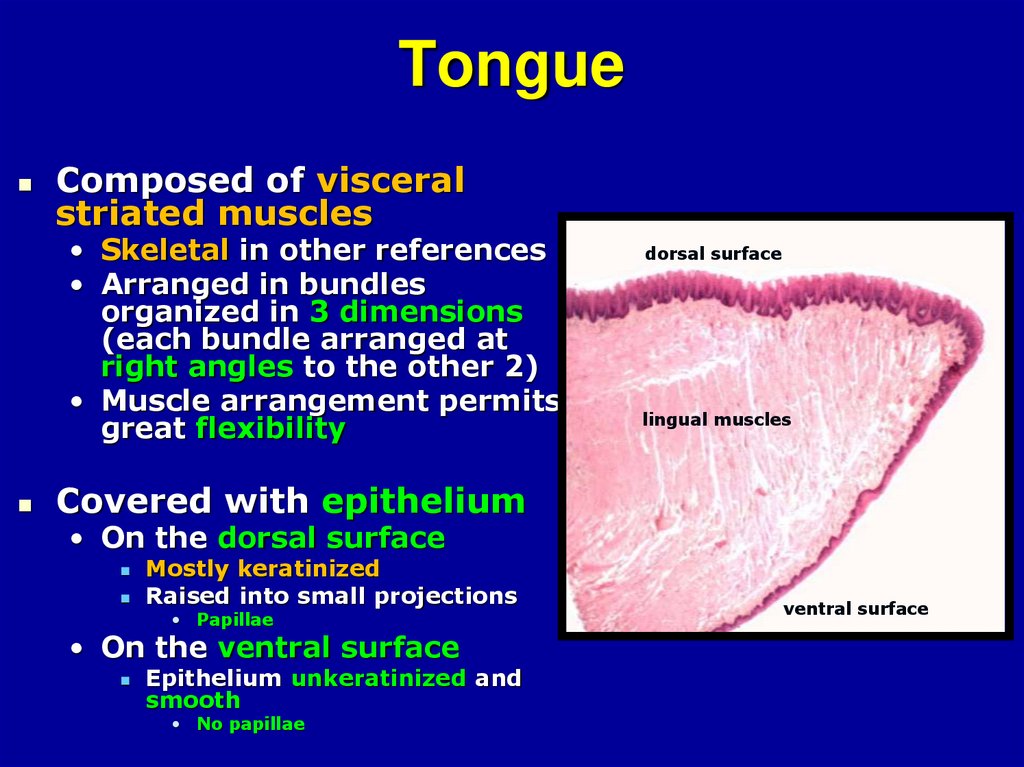
Composed of visceralstriated muscles
• Skeletal in other references
• Arranged in bundles
organized in 3 dimensions
(each bundle arranged at
right angles to the other 2)
• Muscle arrangement permits
great flexibility
dorsal surface
lingual muscles
Covered with epithelium
• On the dorsal surface
Mostly keratinized
Raised into small projections
• Papillae
• On the ventral surface
Epithelium unkeratinized and
smooth
• No papillae
ventral surface
5.
56. Tongue cont.
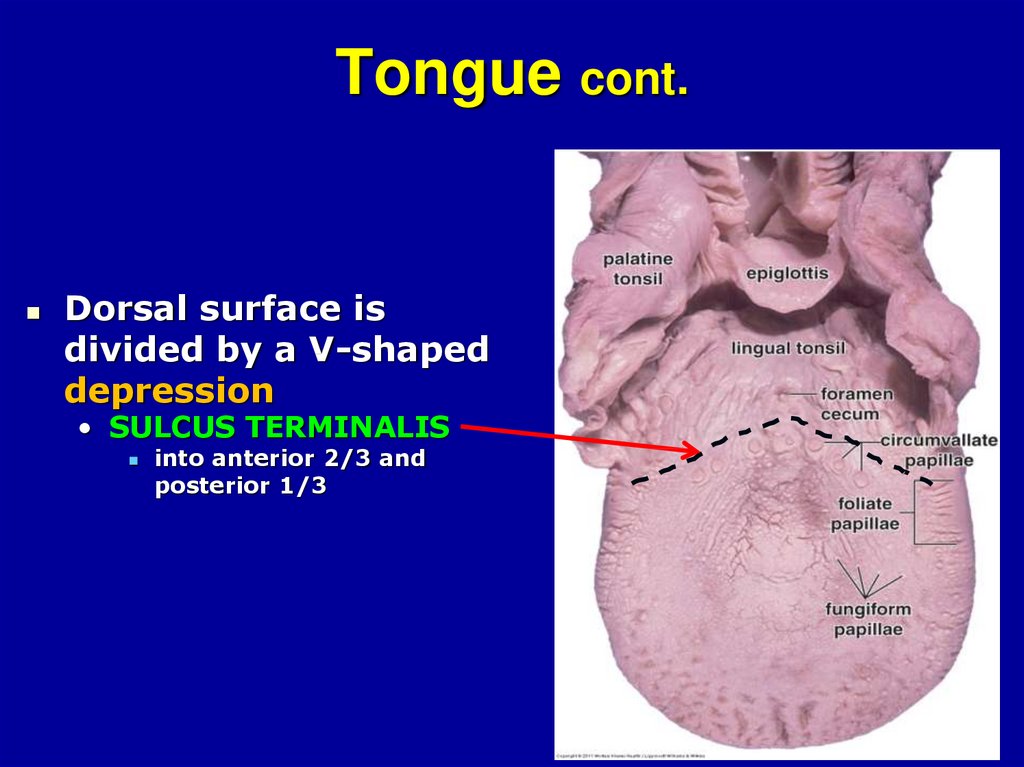
Dorsal surface isdivided by a V-shaped
depression
• SULCUS TERMINALIS
into anterior 2/3 and
posterior 1/3
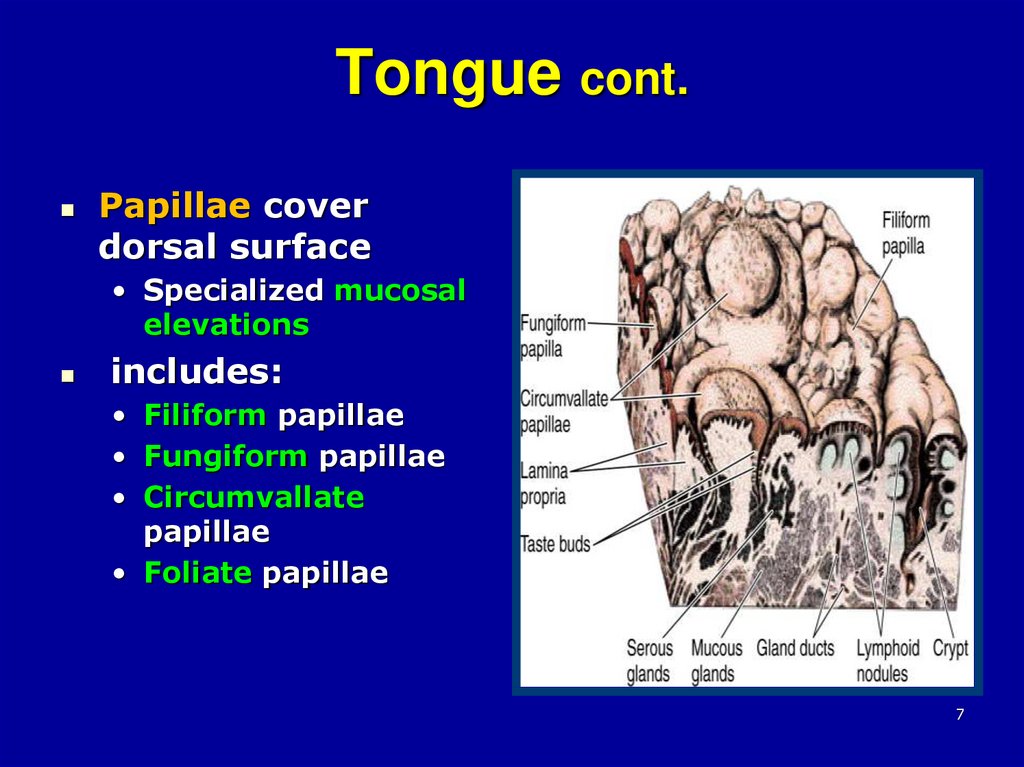
7. Tongue cont.
Papillae coverdorsal surface
• Specialized mucosal
elevations
includes:
• Filiform papillae
• Fungiform papillae
• Circumvallate
papillae
• Foliate papillae
7
8.
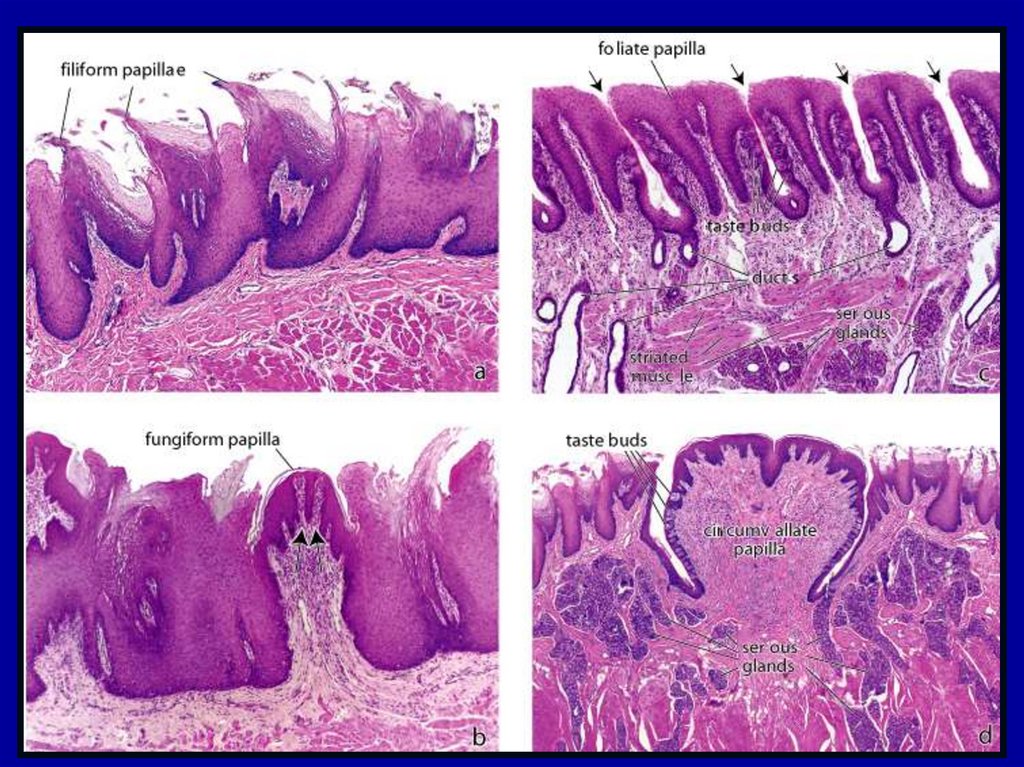
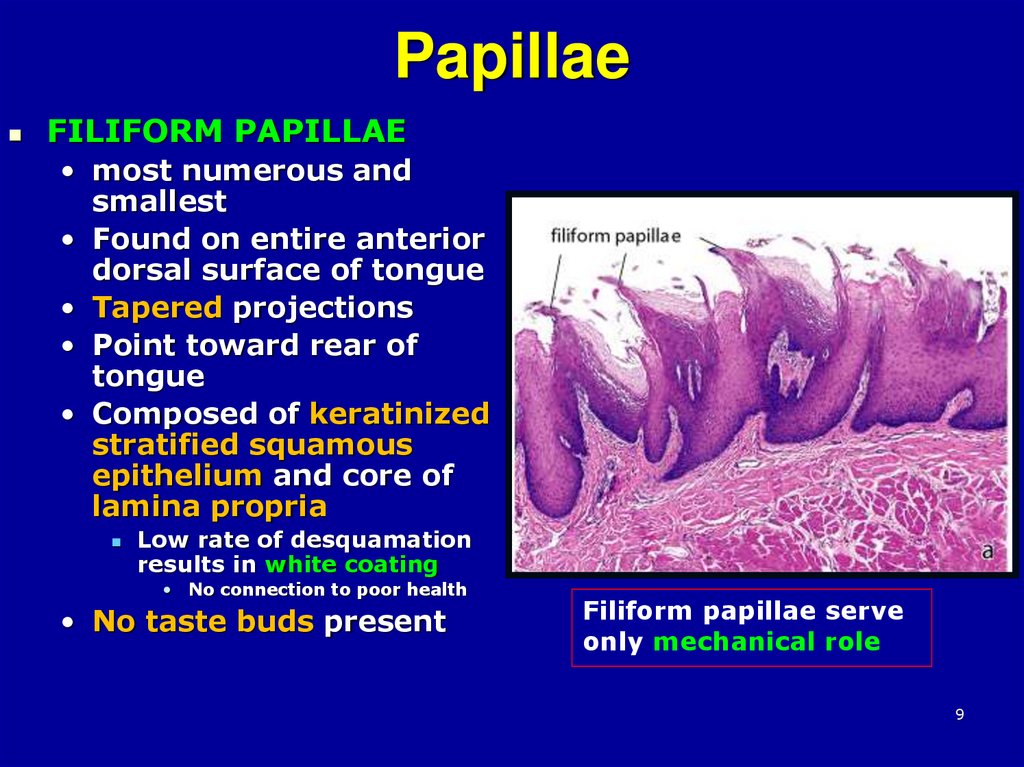
89. Papillae
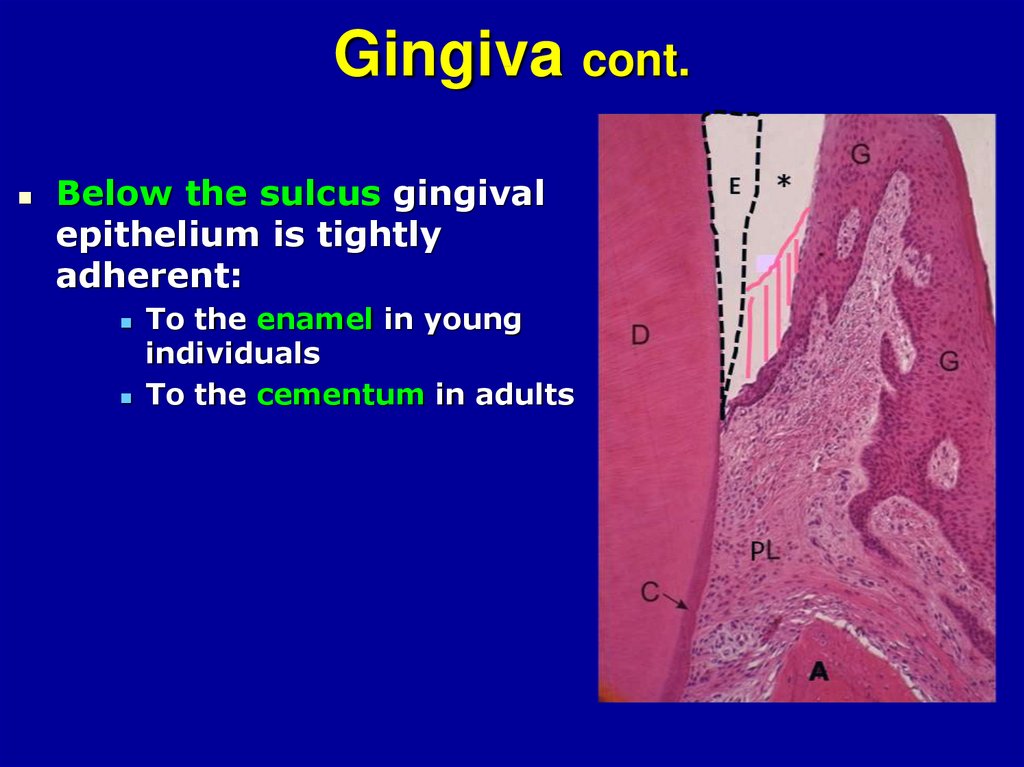
FILIFORM PAPILLAE• most numerous and
smallest
• Found on entire anterior
dorsal surface of tongue
• Tapered projections
• Point toward rear of
tongue
• Composed of keratinized
stratified squamous
epithelium and core of
lamina propria
Low rate of desquamation
results in white coating
• No connection to poor health
• No taste buds present
Filiform papillae serve
only mechanical role
9
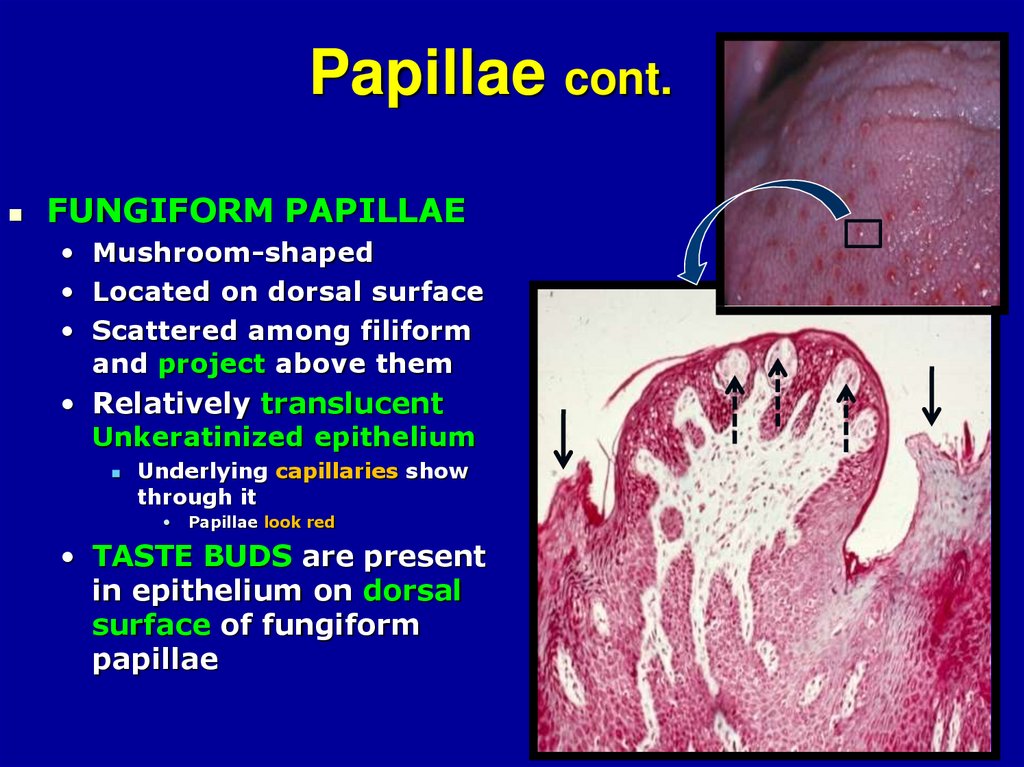
10. Papillae cont.
FUNGIFORM PAPILLAE• Mushroom-shaped
• Located on dorsal surface
• Scattered among filiform
and project above them
• Relatively translucent
Unkeratinized epithelium
Underlying capillaries show
through it
Papillae look red
• TASTE BUDS are present
in epithelium on dorsal
surface of fungiform
papillae
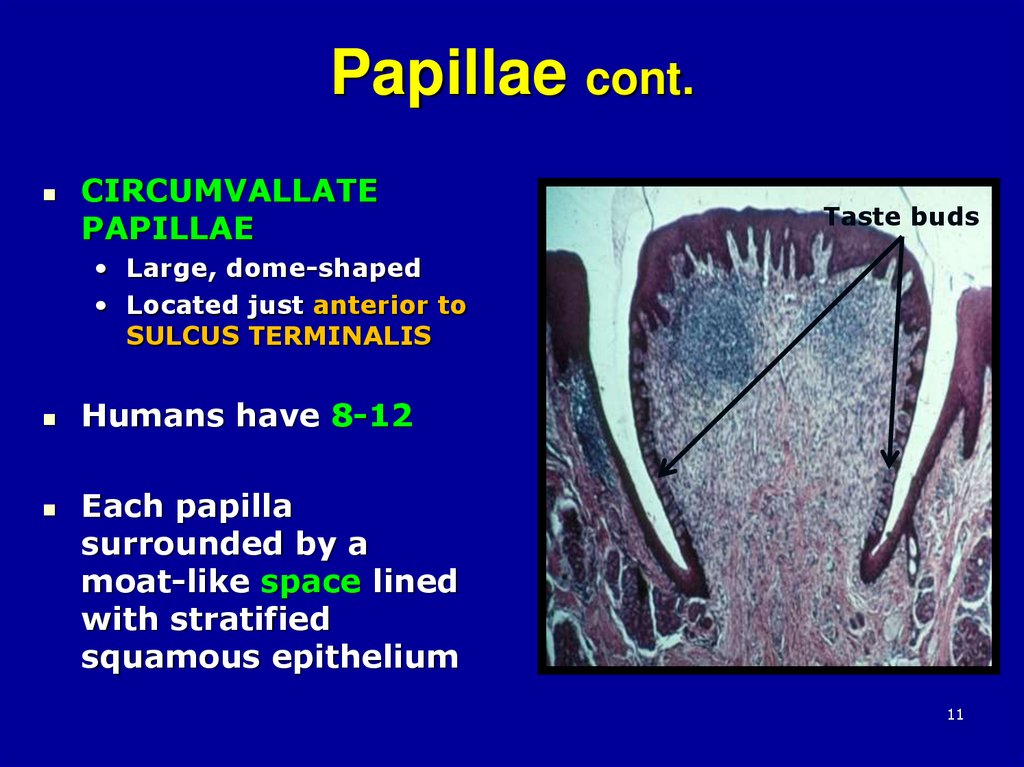
11. Papillae cont.
CIRCUMVALLATEPAPILLAE
Taste buds
• Large, dome-shaped
• Located just anterior to
SULCUS TERMINALIS
Humans have 8-12
Each papilla
surrounded by a
moat-like space lined
with stratified
squamous epithelium
11
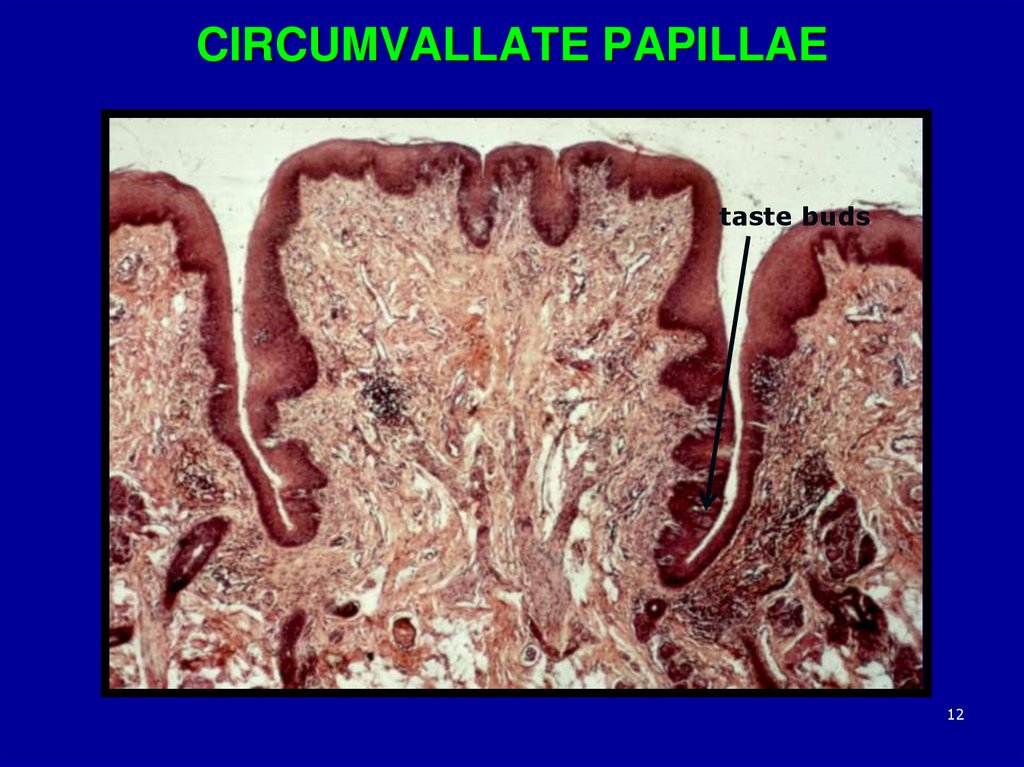
12. CIRCUMVALLATE PAPILLAE
taste buds12
13.
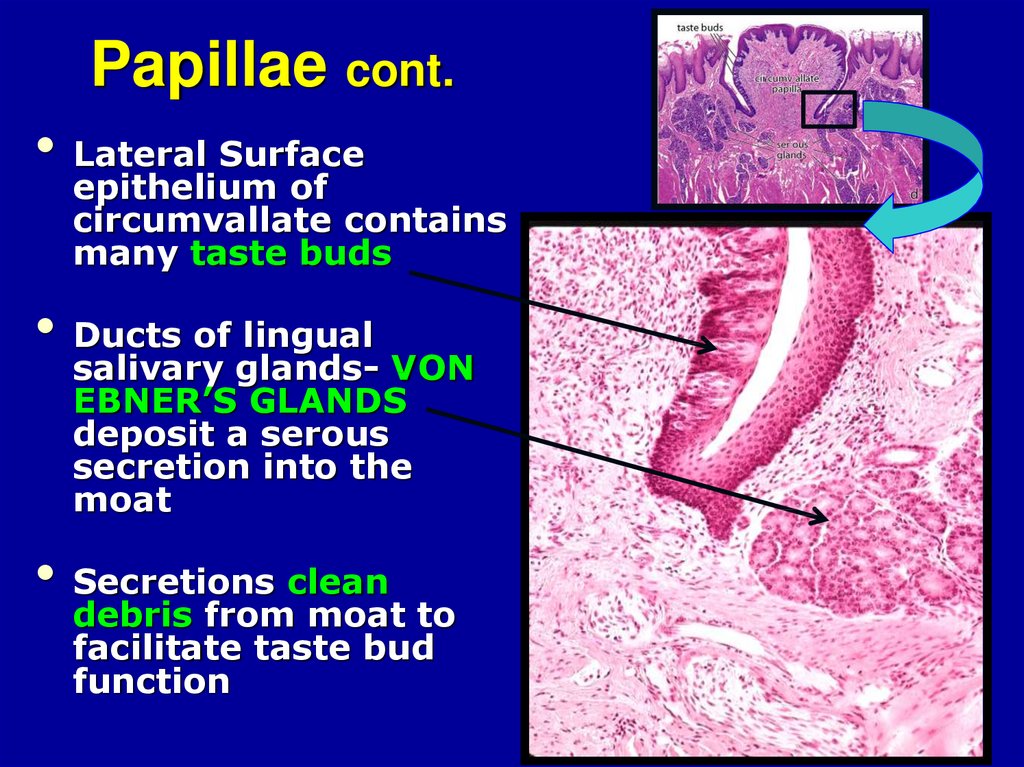
1314. Papillae cont.
• Lateral Surfaceepithelium of
circumvallate contains
many taste buds
• Ducts of lingual
salivary glands- VON
EBNER’S GLANDS
deposit a serous
secretion into the
moat
• Secretions clean
debris from moat to
facilitate taste bud
function
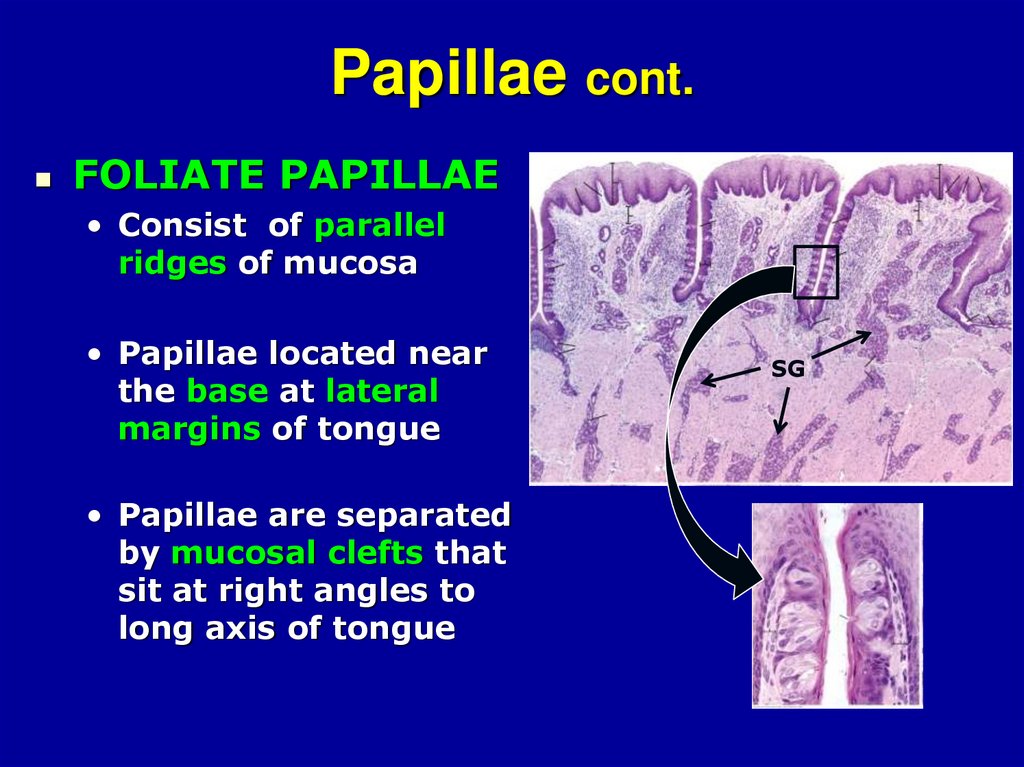
15. Papillae cont.
FOLIATE PAPILLAE• Consist of parallel
ridges of mucosa
• Papillae located near
the base at lateral
margins of tongue
• Papillae are separated
by mucosal clefts that
sit at right angles to
long axis of tongue
SG
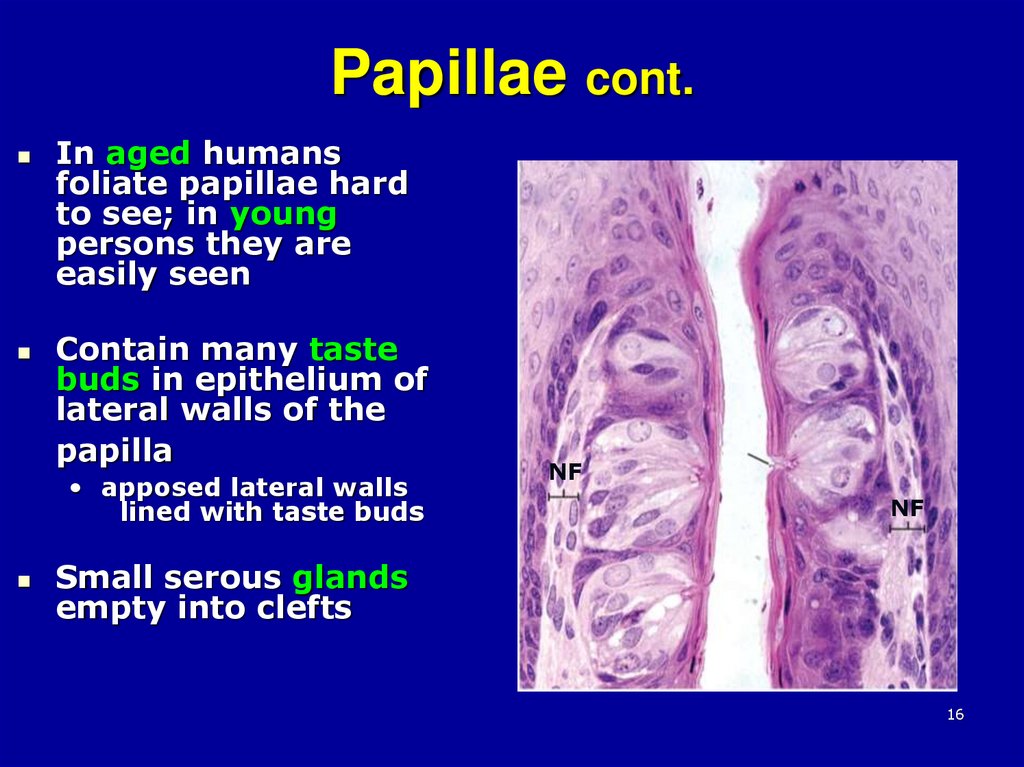
16. Papillae cont.
In aged humansfoliate papillae hard
to see; in young
persons they are
easily seen
Contain many taste
buds in epithelium of
lateral walls of the
papilla
• apposed lateral walls
lined with taste buds
NF
NF
Small serous glands
empty into clefts
16
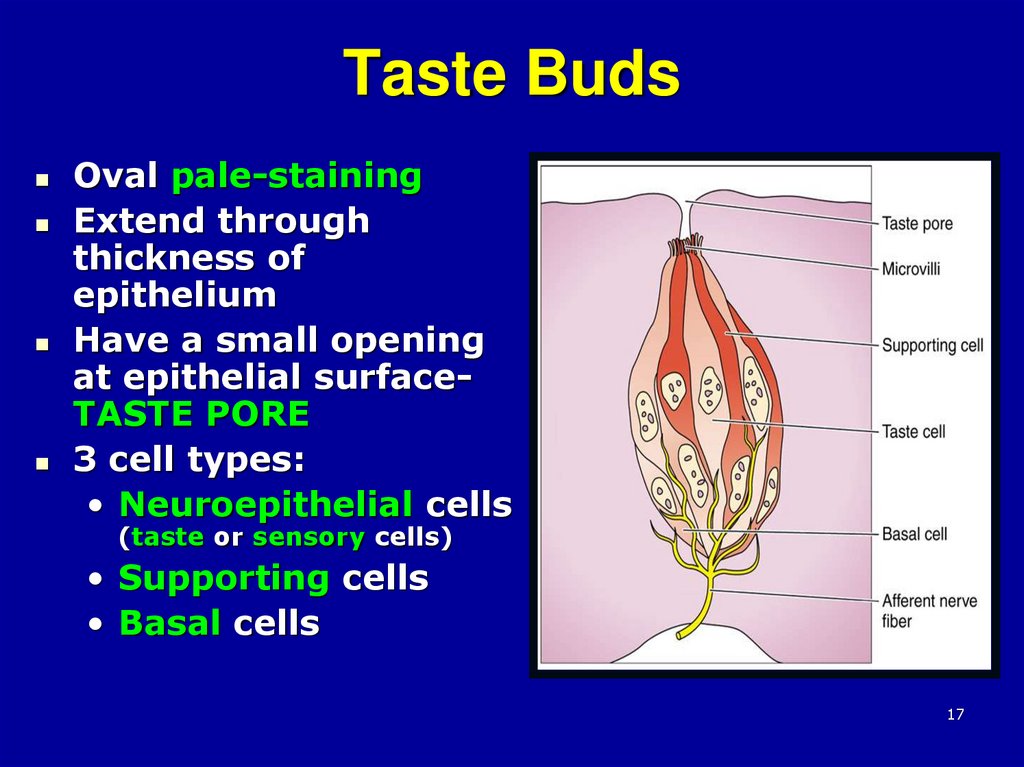
17. Taste Buds
Oval pale-stainingExtend through
thickness of
epithelium
Have a small opening
at epithelial surfaceTASTE PORE
3 cell types:
• Neuroepithelial cells
(taste or sensory cells)
• Supporting cells
• Basal cells
17
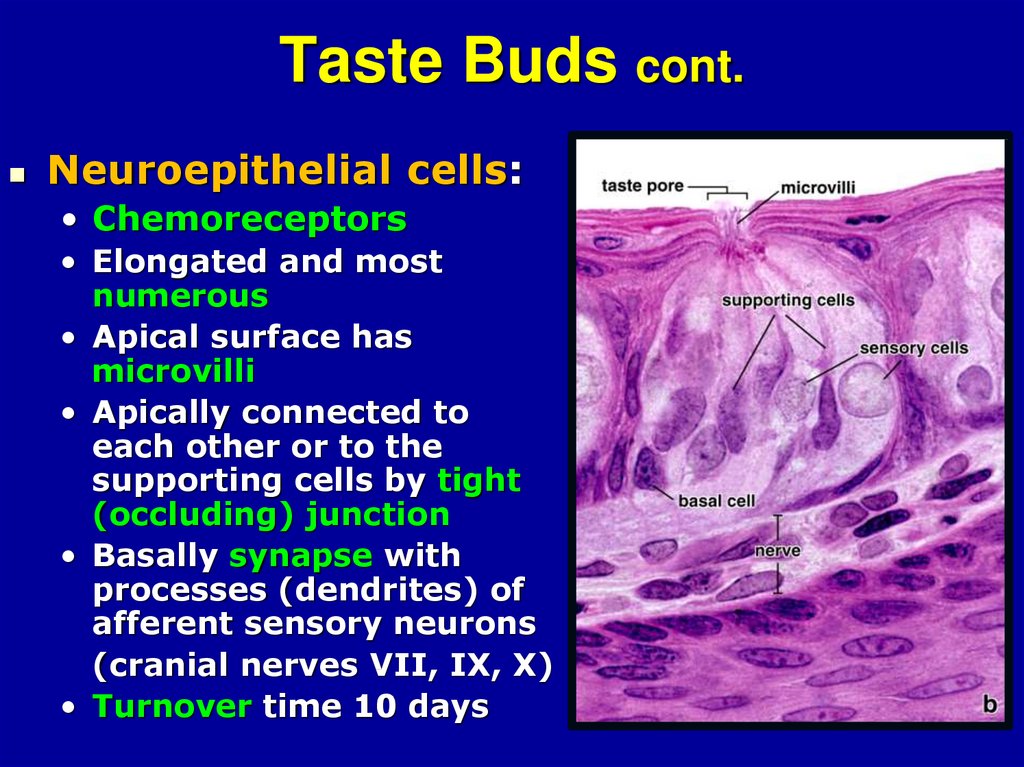
18. Taste Buds cont.
Neuroepithelial cells:• Chemoreceptors
• Elongated and most
numerous
• Apical surface has
microvilli
• Apically connected to
each other or to the
supporting cells by tight
(occluding) junction
• Basally synapse with
processes (dendrites) of
afferent sensory neurons
(cranial nerves VII, IX, X)
• Turnover time 10 days
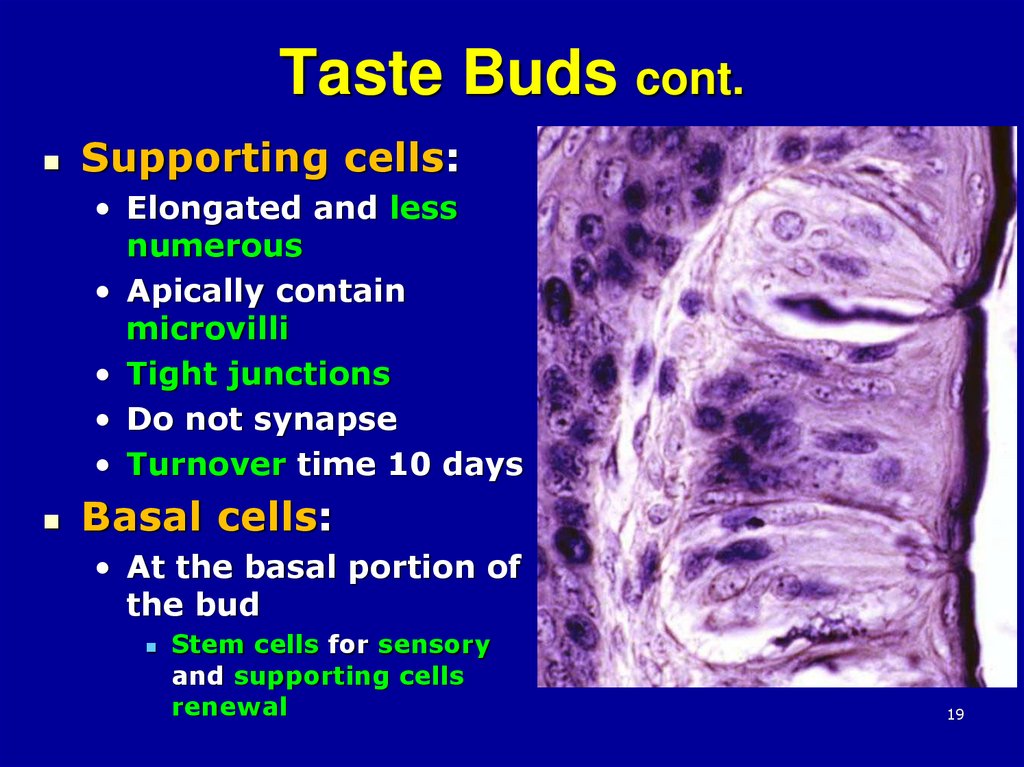
19. Taste Buds cont.
Supporting cells:• Elongated and less
numerous
• Apically contain
microvilli
• Tight junctions
• Do not synapse
• Turnover time 10 days
Basal cells:
• At the basal portion of
the bud
Stem cells for sensory
and supporting cells
renewal
19
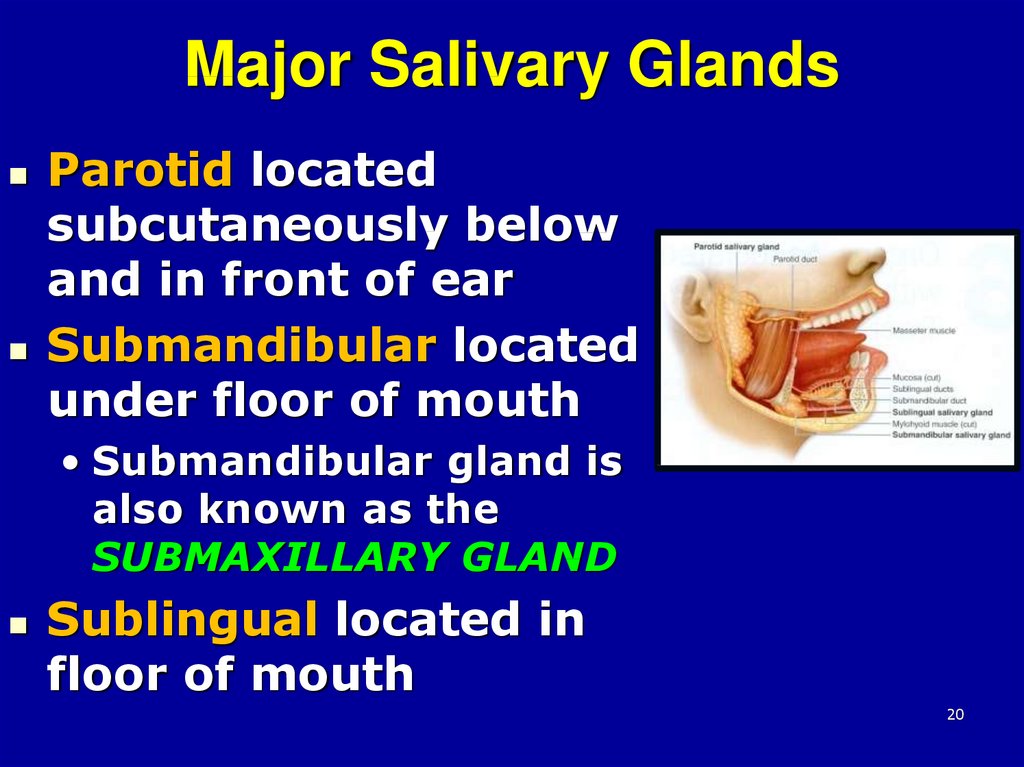
20. Major Salivary Glands
Parotid locatedsubcutaneously below
and in front of ear
Submandibular located
under floor of mouth
• Submandibular gland is
also known as the
SUBMAXILLARY GLAND
Sublingual located in
floor of mouth
20
21. Minor Salivary Glands
Located in the submucosa ofdifferent parts of the oral cavity
• Lingual
• Labial
• Buccal
• Molar
• Palatine glands
21
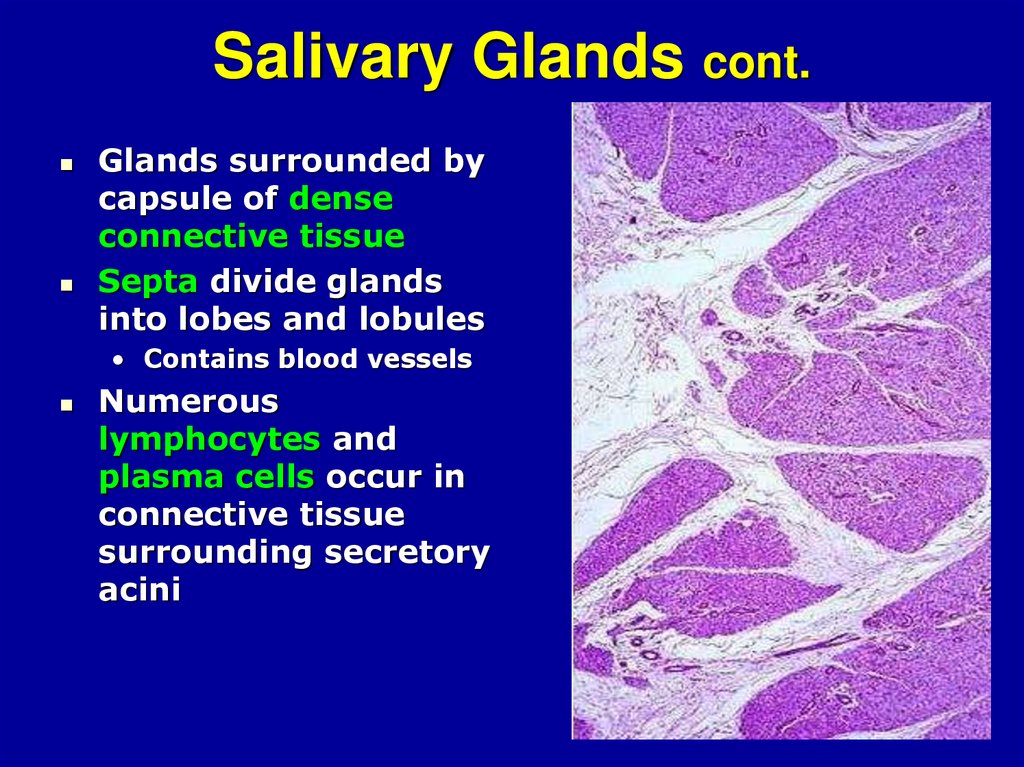
22. Salivary Glands cont.
Glands surrounded bycapsule of dense
connective tissue
Septa divide glands
into lobes and lobules
• Contains blood vessels
Numerous
lymphocytes and
plasma cells occur in
connective tissue
surrounding secretory
acini
22
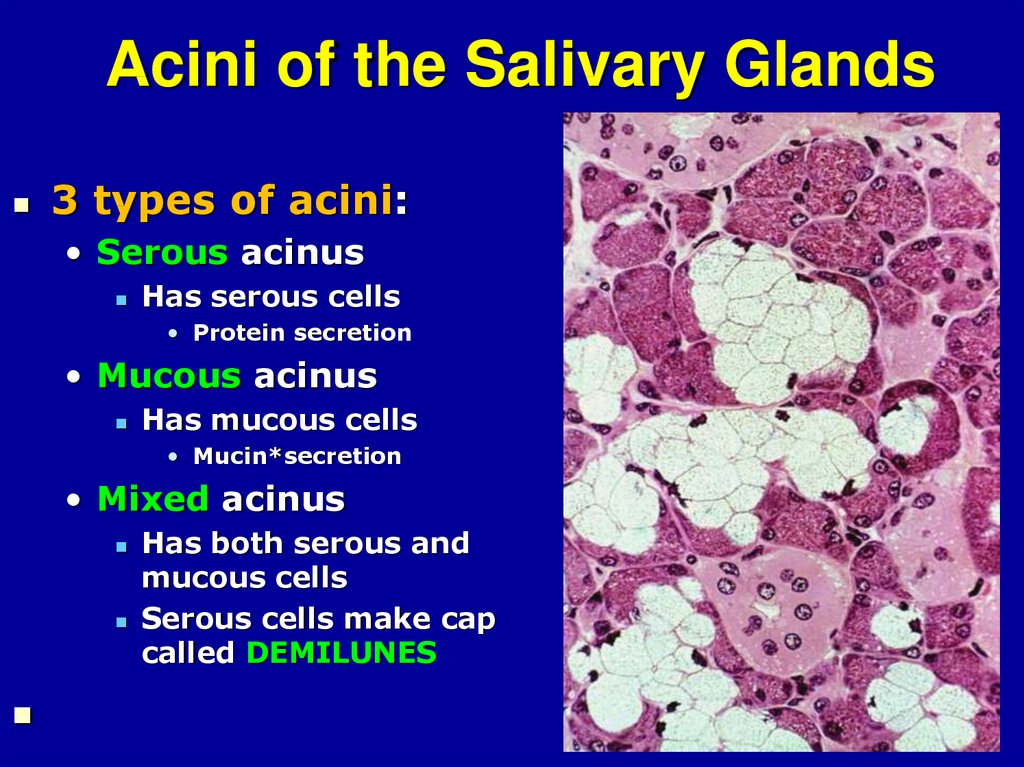
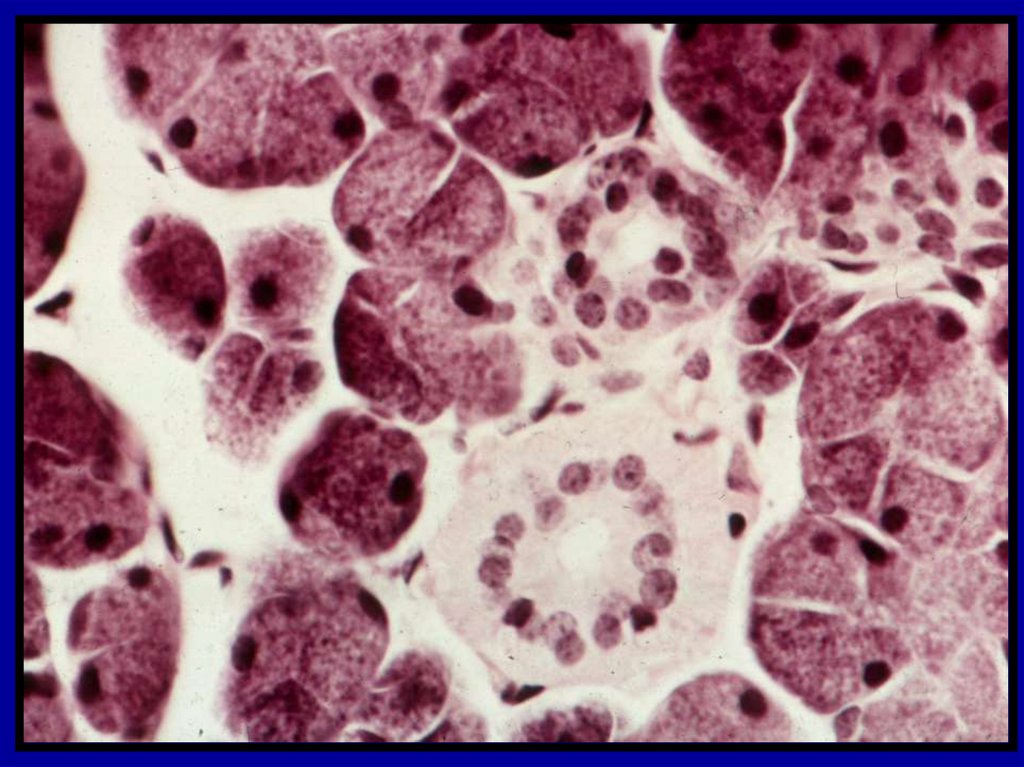
23. Acini of the Salivary Glands
3 types of acini:• Serous acinus
Has serous cells
• Protein secretion
• Mucous acinus
Has mucous cells
• Mucin*secretion
• Mixed acinus
Has both serous and
mucous cells
Serous cells make cap
called DEMILUNES
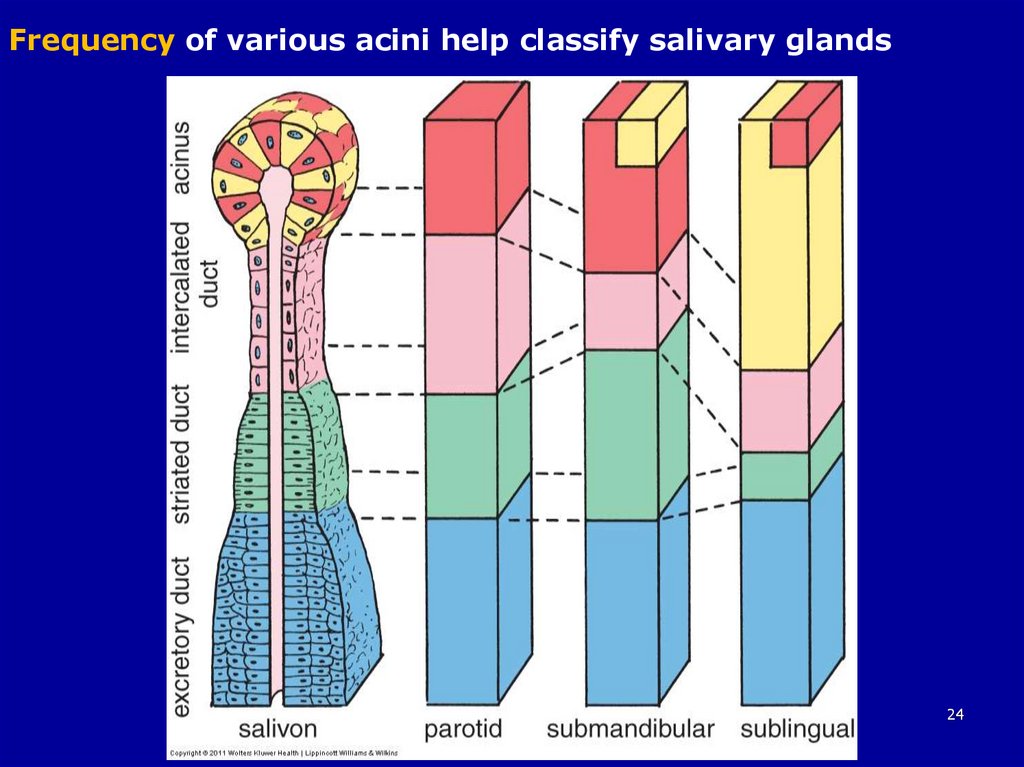
24.
Frequency of various acini help classify salivary glands24
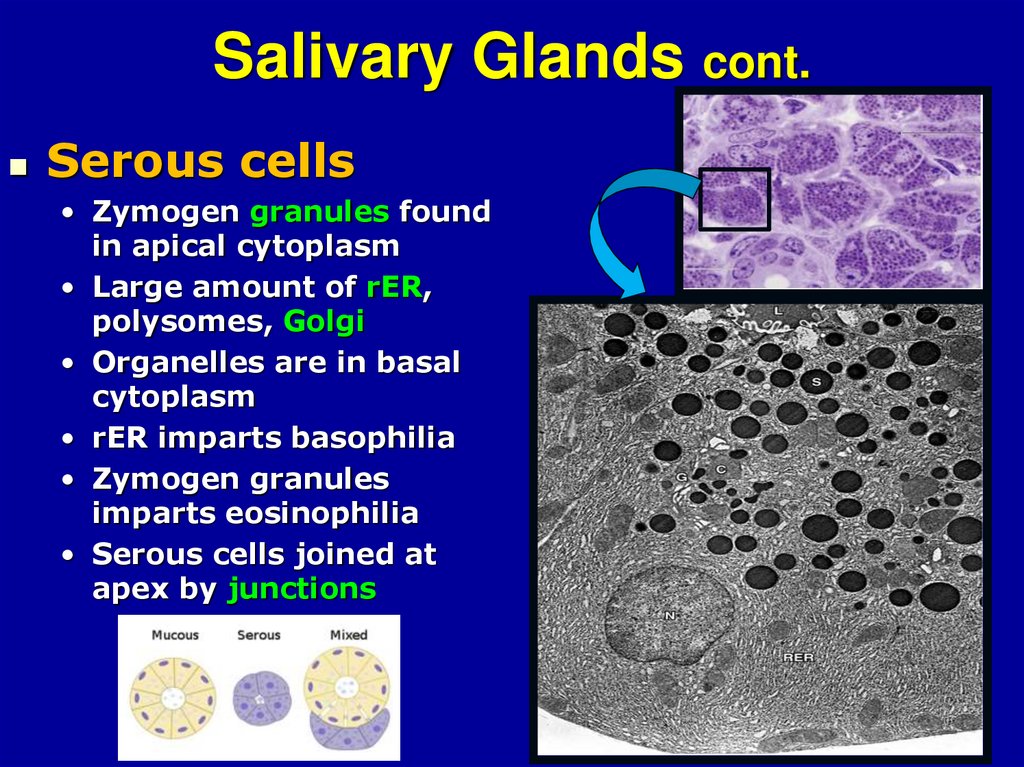
25. Salivary Glands cont.
Serous cells• Zymogen granules found
in apical cytoplasm
• Large amount of rER,
polysomes, Golgi
• Organelles are in basal
cytoplasm
• rER imparts basophilia
• Zymogen granules
imparts eosinophilia
• Serous cells joined at
apex by junctions
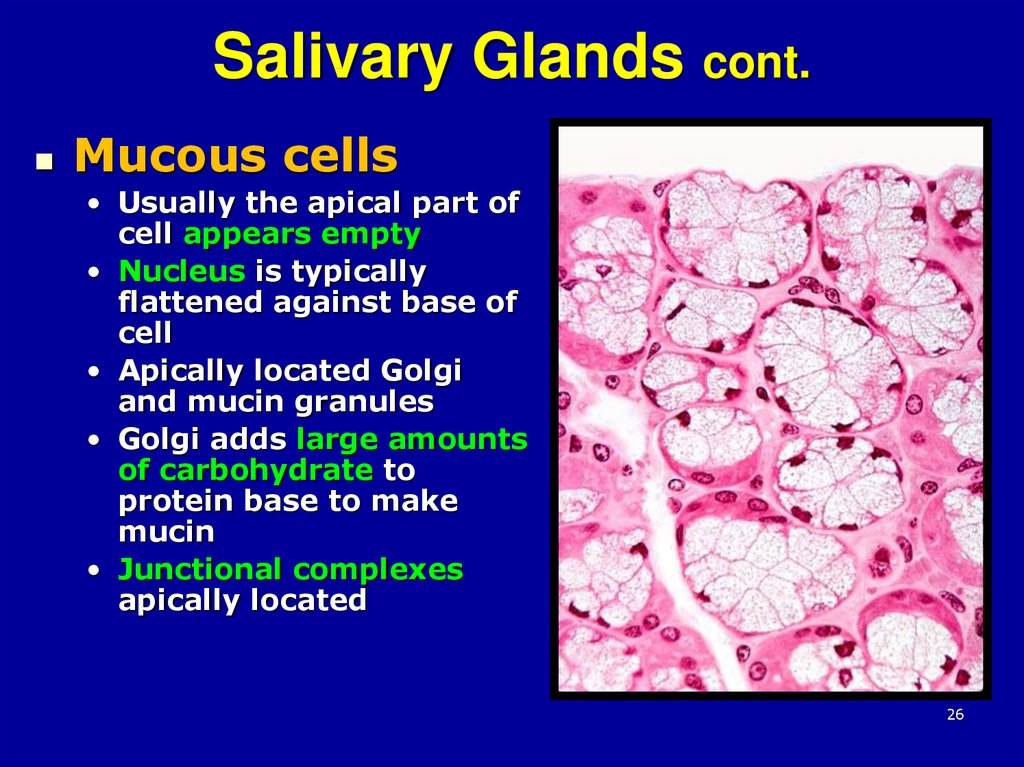
26. Salivary Glands cont.
Mucous cells• Usually the apical part of
cell appears empty
• Nucleus is typically
flattened against base of
cell
• Apically located Golgi
and mucin granules
• Golgi adds large amounts
of carbohydrate to
protein base to make
mucin
• Junctional complexes
apically located
26
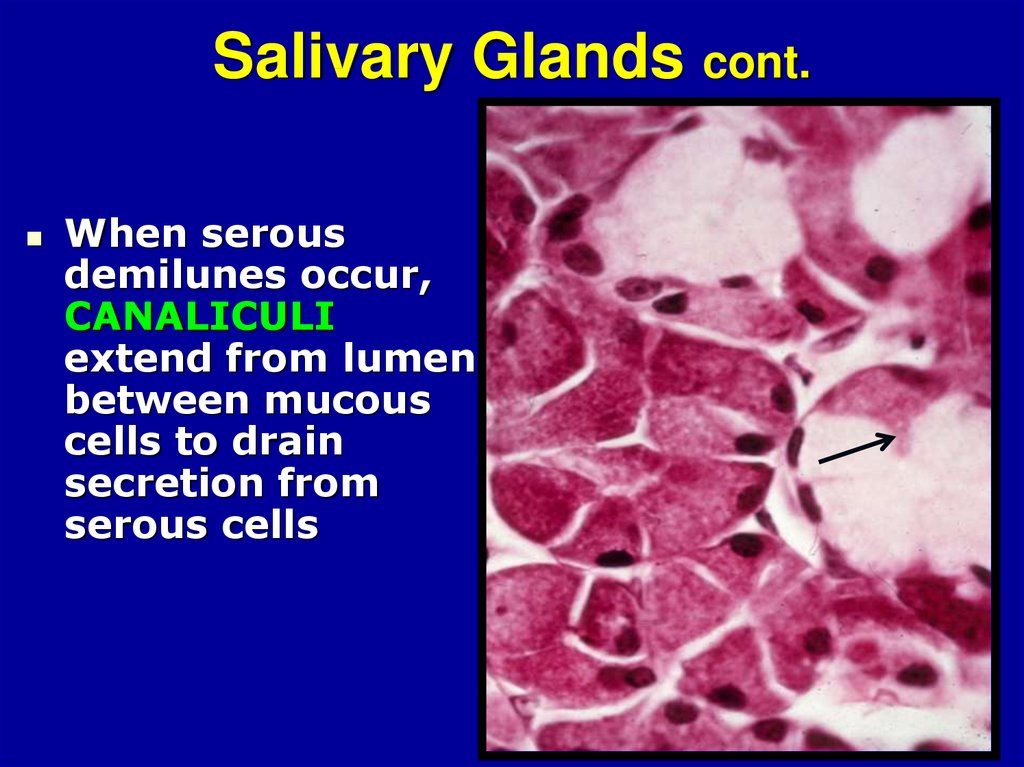
27. Salivary Glands cont.
When serousdemilunes occur,
CANALICULI
extend from lumen
between mucous
cells to drain
secretion from
serous cells
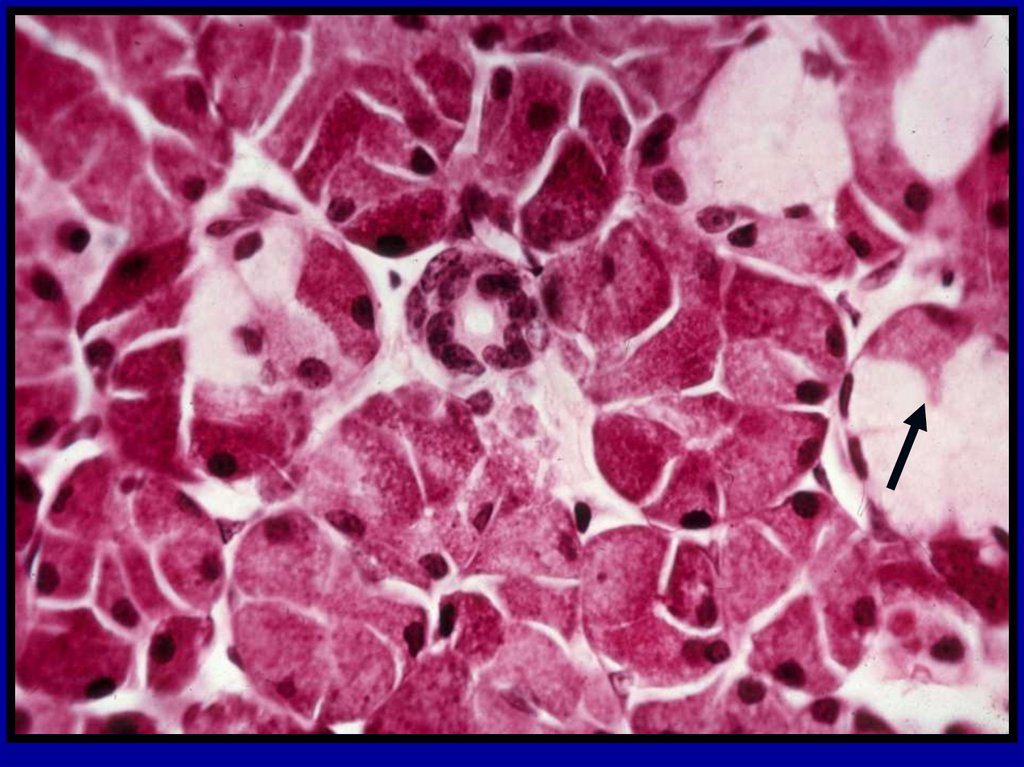
28. Salivary Glands cont.
MYOEPITHELIAL CELLS• Contractile with numerous processes
• Located between basal plasma membrane
of the secretory cells and basal lamina
• Also underlie cells of proximal part of duct
system
• Myoepithelial cells help move secretions to
excretory ducts
• Hard to identify in H&E sections
28
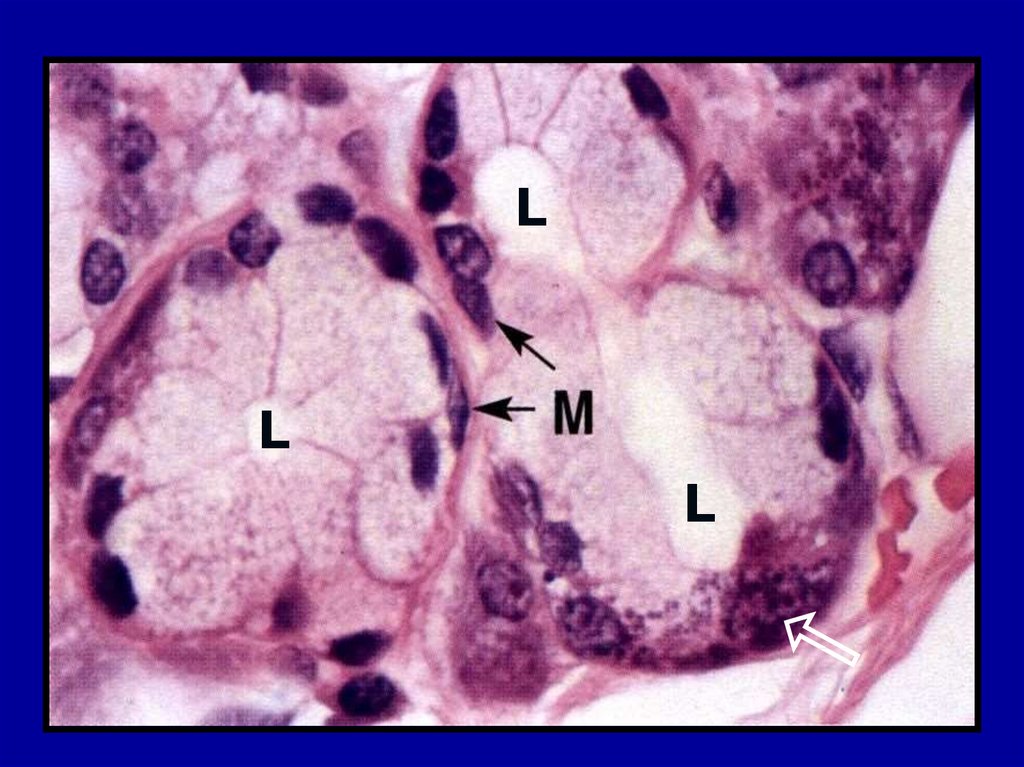
29.
LL
L
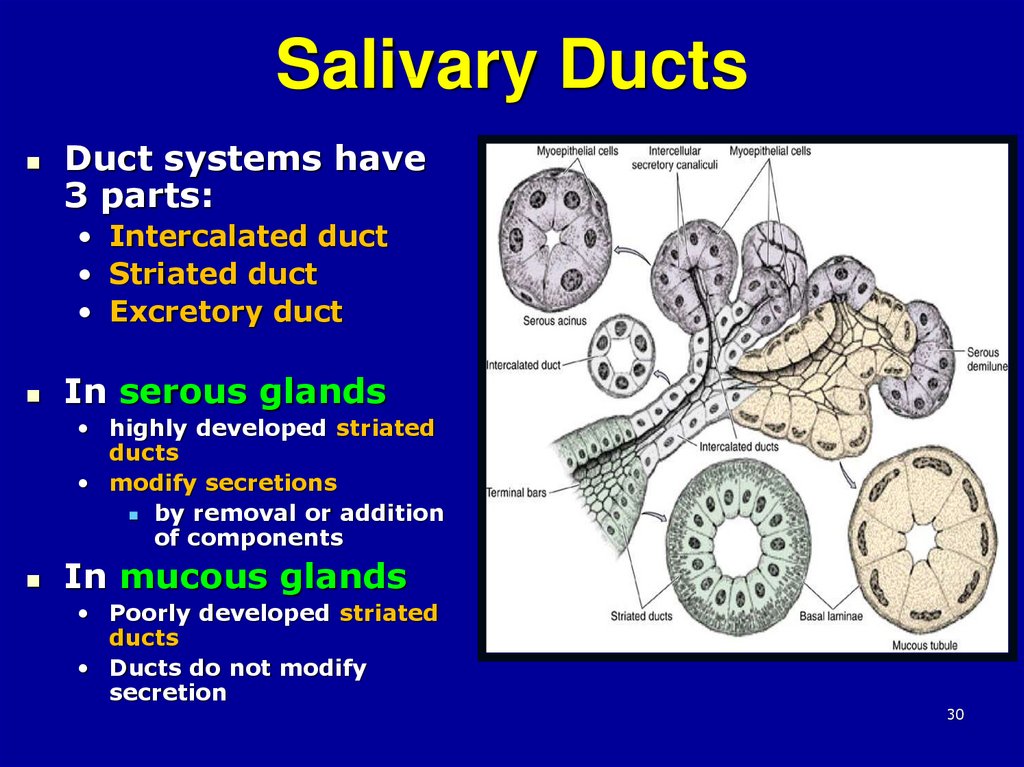
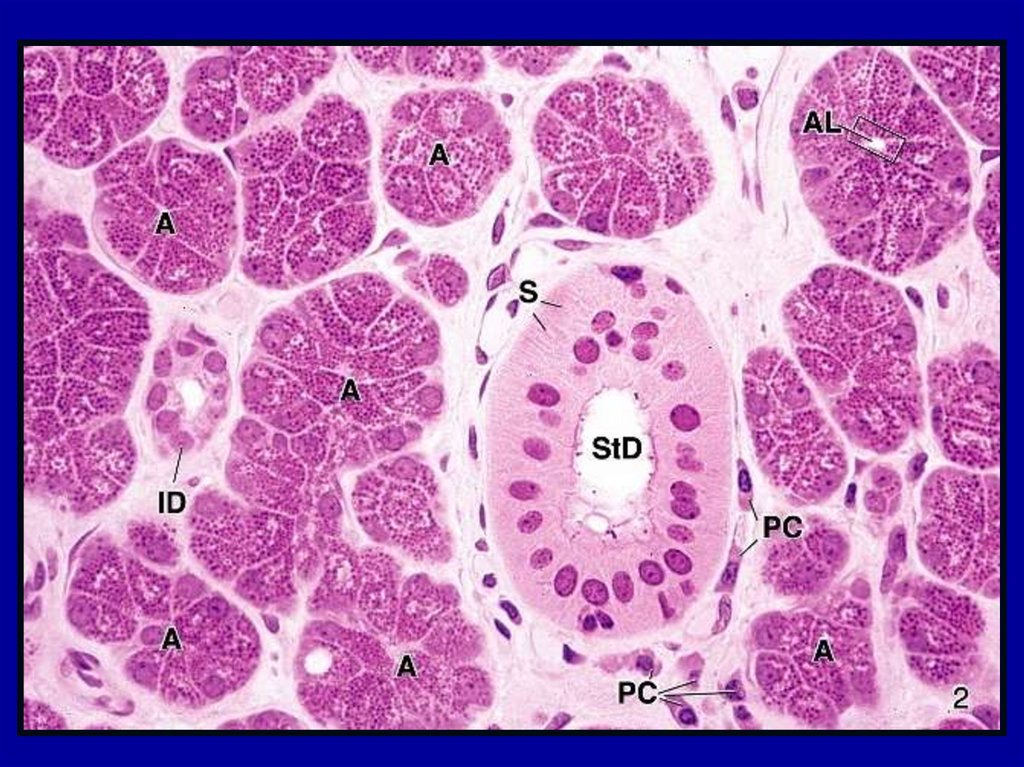
30. Salivary Ducts
Duct systems have3 parts:
• Intercalated duct
• Striated duct
• Excretory duct
In serous glands
• highly developed striated
ducts
• modify secretions
by removal or addition
of components
In mucous glands
• Poorly developed striated
ducts
• Ducts do not modify
secretion
30
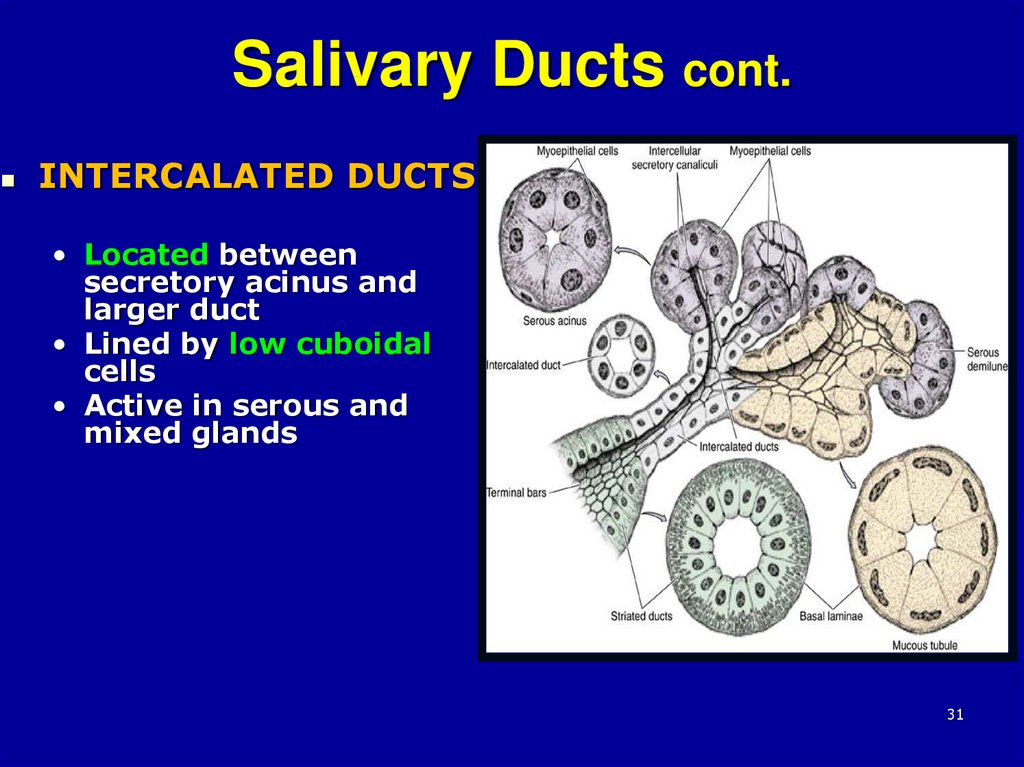
31. Salivary Ducts cont.
INTERCALATED DUCTS• Located between
secretory acinus and
larger duct
• Lined by low cuboidal
cells
• Active in serous and
mixed glands
31
32.
Striated ductIntercalated
duct
33.
3334.
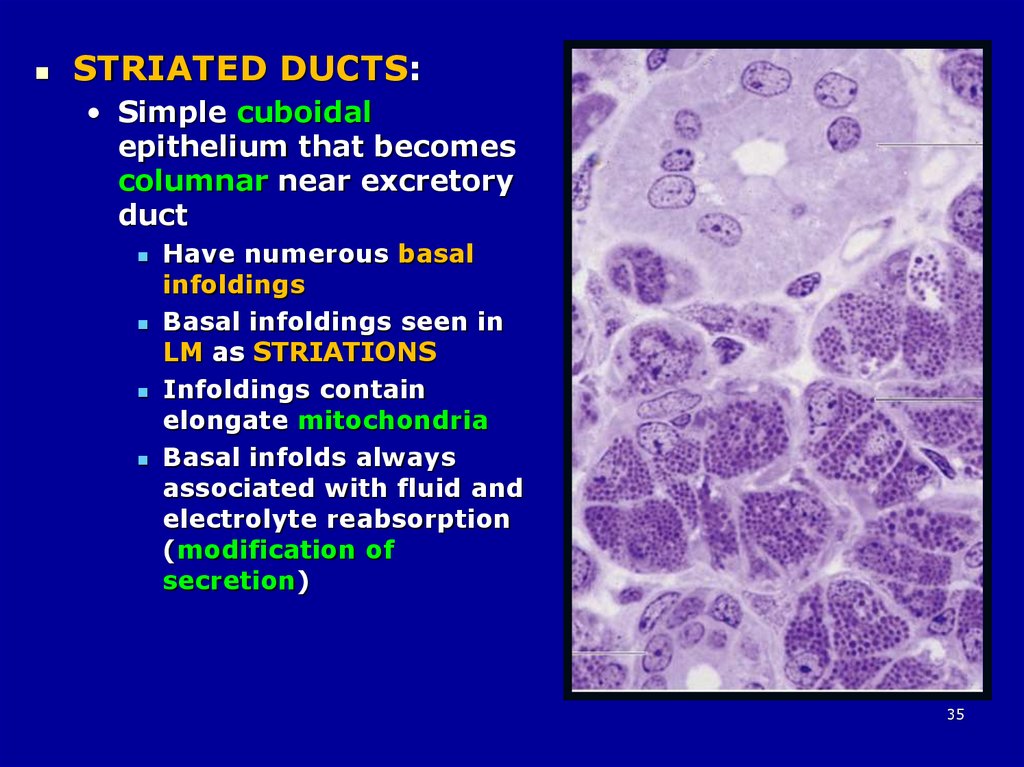
3435.
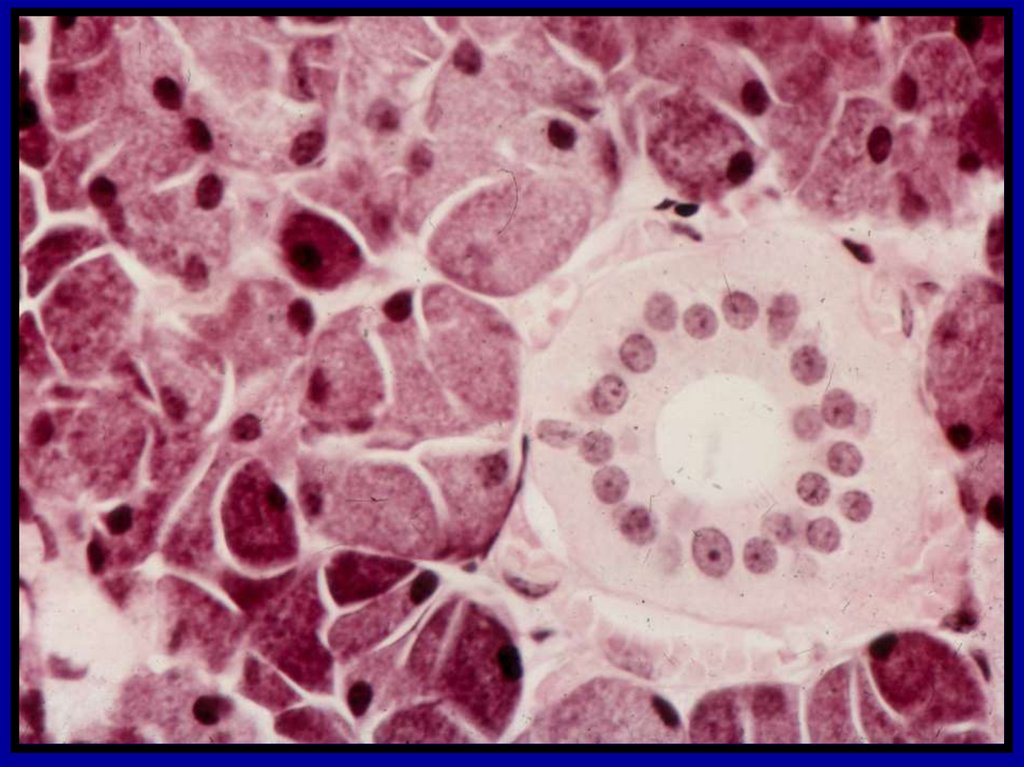
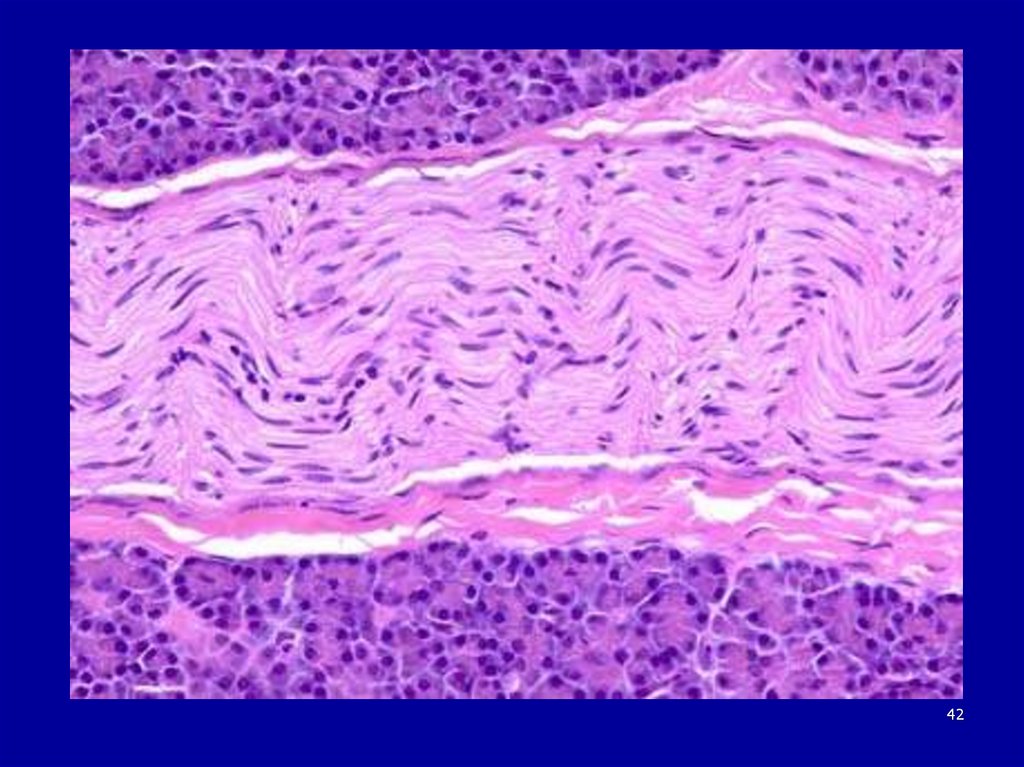
STRIATED DUCTS:• Simple cuboidal
epithelium that becomes
columnar near excretory
duct
Have numerous basal
infoldings
Basal infoldings seen in
LM as STRIATIONS
Infoldings contain
elongate mitochondria
Basal infolds always
associated with fluid and
electrolyte reabsorption
(modification of
secretion)
35
36.
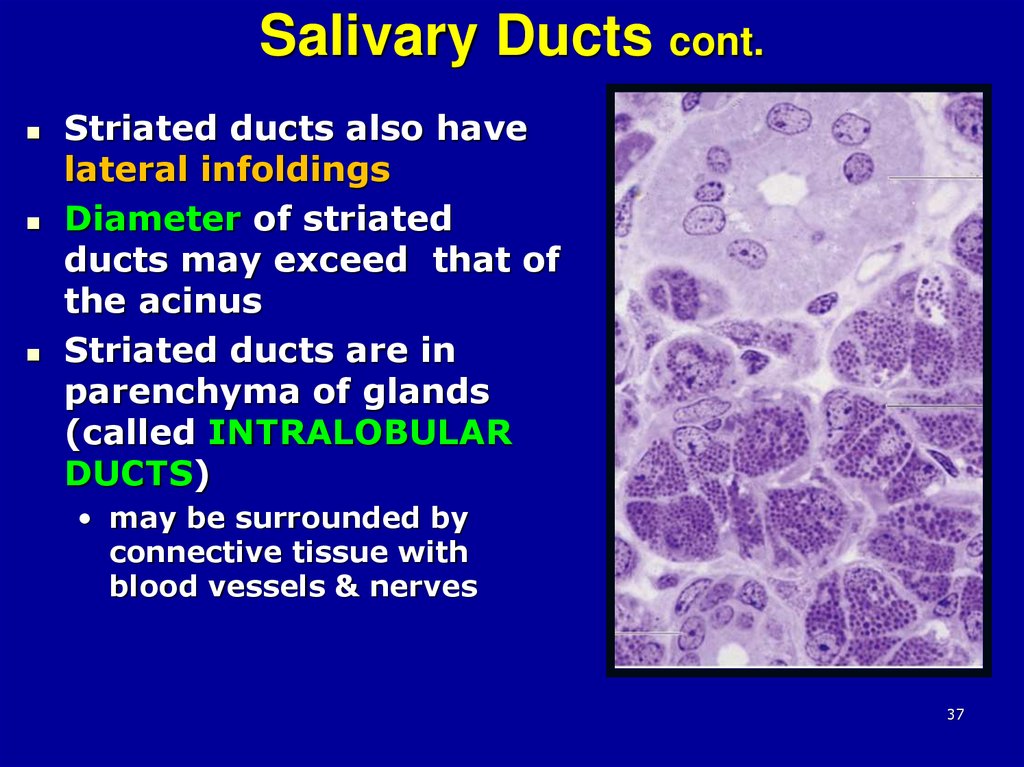
3637. Salivary Ducts cont.
Striated ducts also havelateral infoldings
Diameter of striated
ducts may exceed that of
the acinus
Striated ducts are in
parenchyma of glands
(called INTRALOBULAR
DUCTS)
• may be surrounded by
connective tissue with
blood vessels & nerves
37
38.
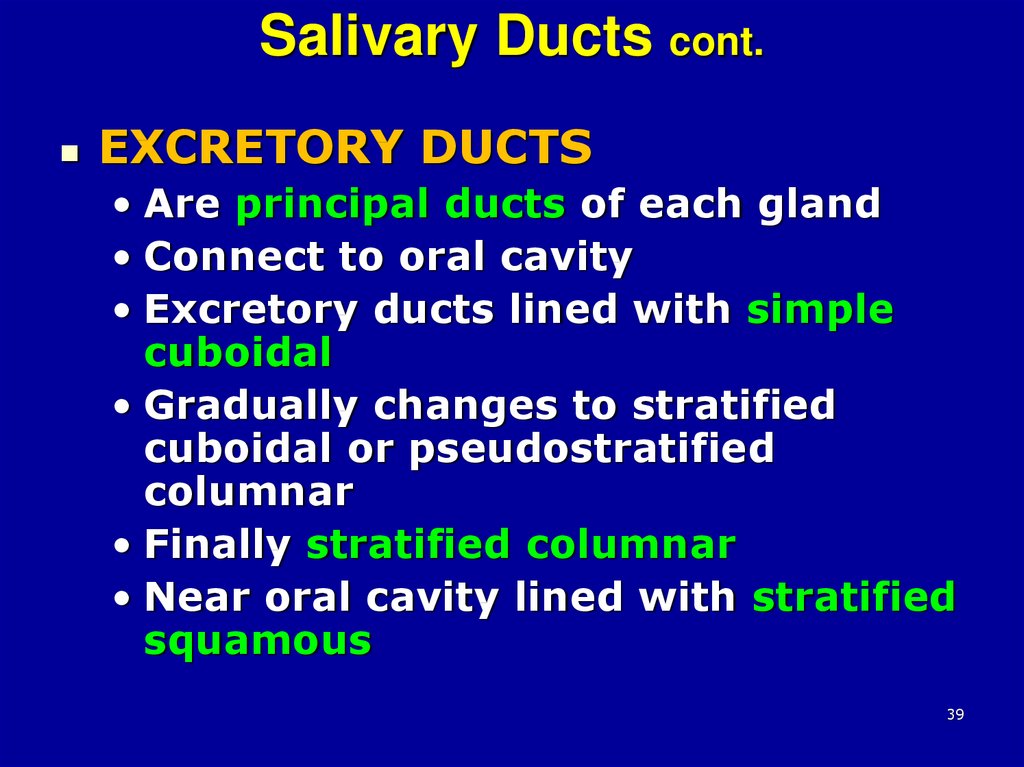
3839. Salivary Ducts cont.
EXCRETORY DUCTS• Are principal ducts of each gland
• Connect to oral cavity
• Excretory ducts lined with simple
cuboidal
• Gradually changes to stratified
cuboidal or pseudostratified
columnar
• Finally stratified columnar
• Near oral cavity lined with stratified
squamous
39
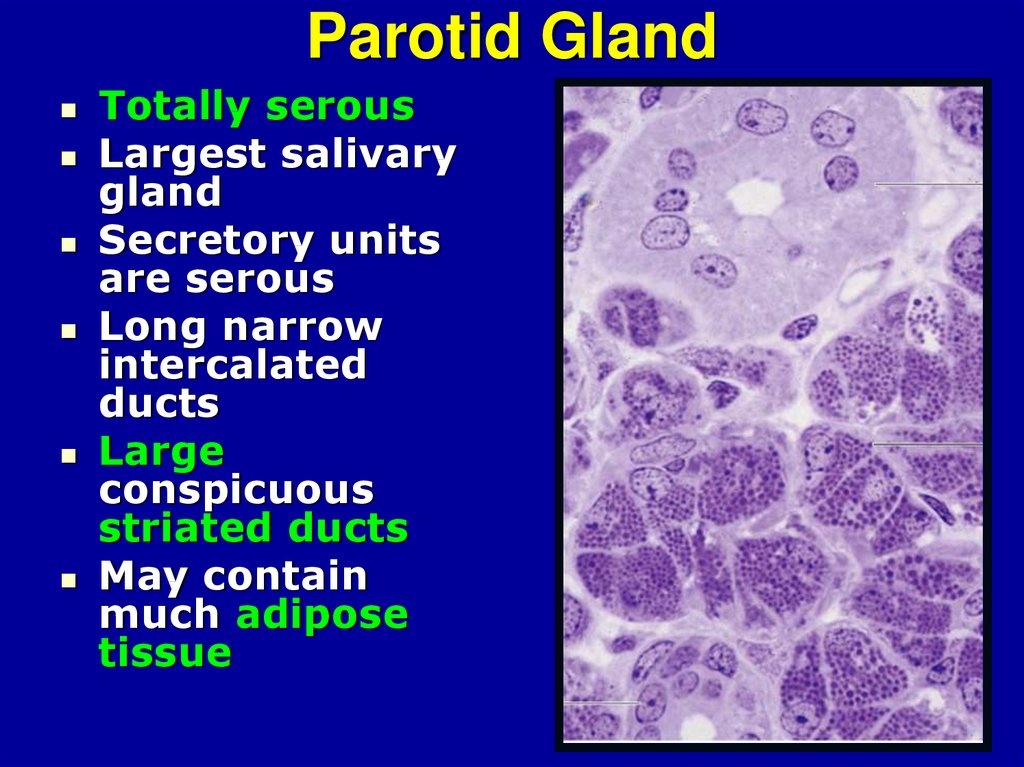
40. Parotid Gland
Totally serousLargest salivary
gland
Secretory units
are serous
Long narrow
intercalated
ducts
Large
conspicuous
striated ducts
May contain
much adipose
tissue
40
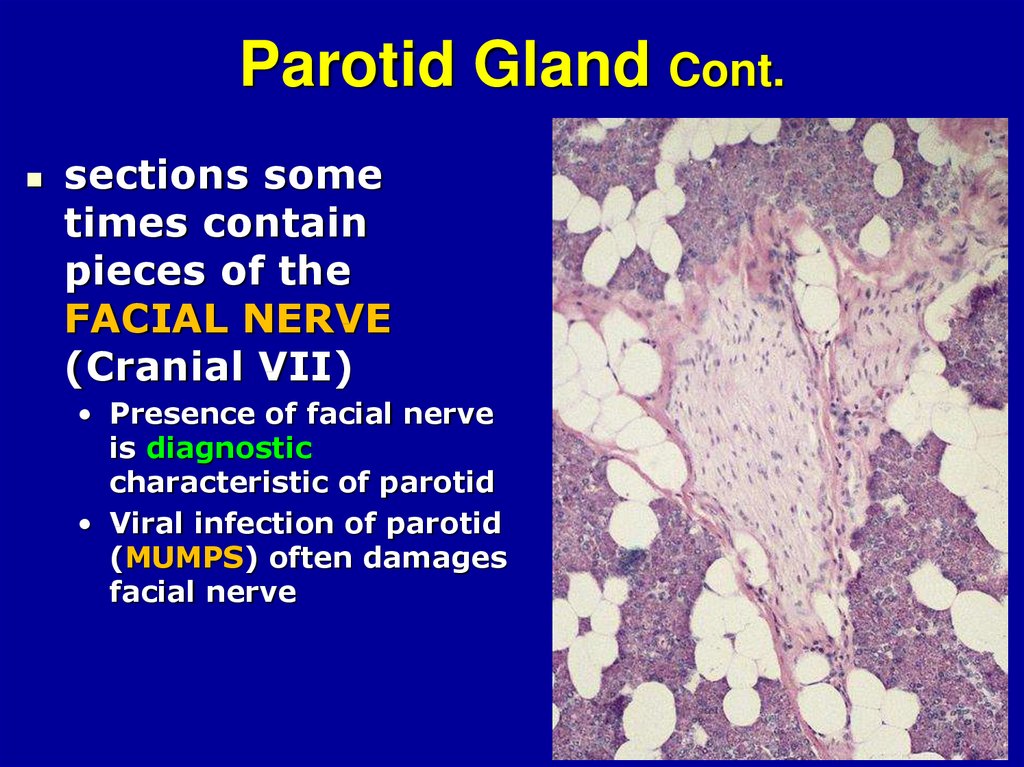
41. Parotid Gland Cont.
sections sometimes contain
pieces of the
FACIAL NERVE
(Cranial VII)
• Presence of facial nerve
is diagnostic
characteristic of parotid
• Viral infection of parotid
(MUMPS) often damages
facial nerve
42.
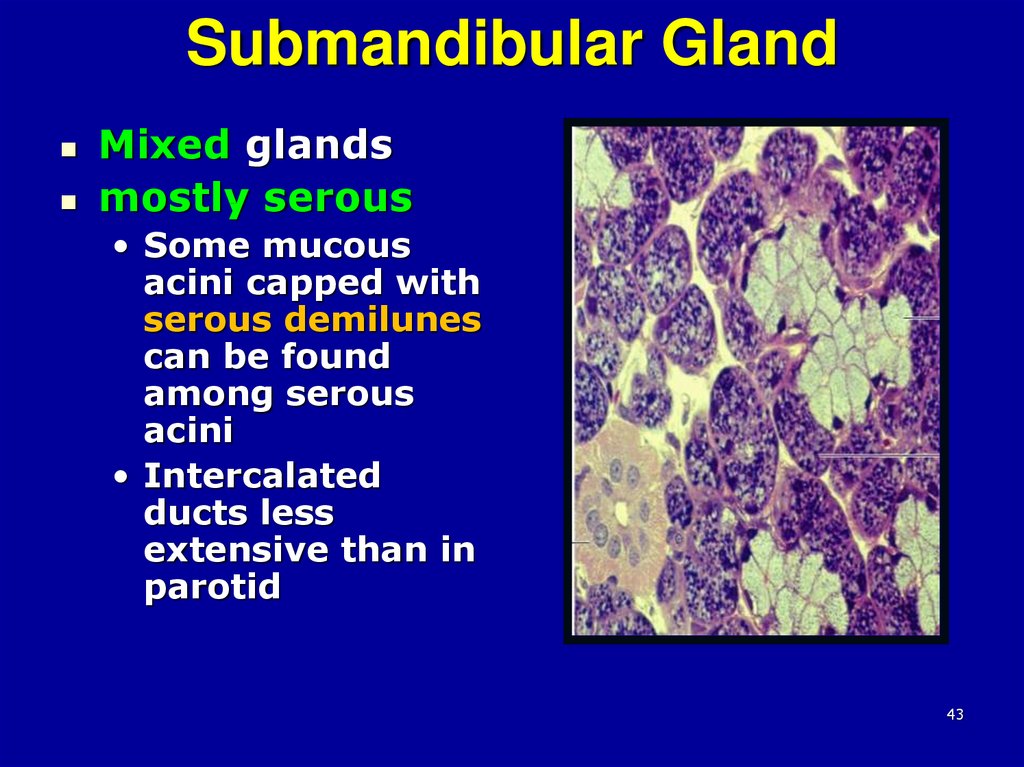
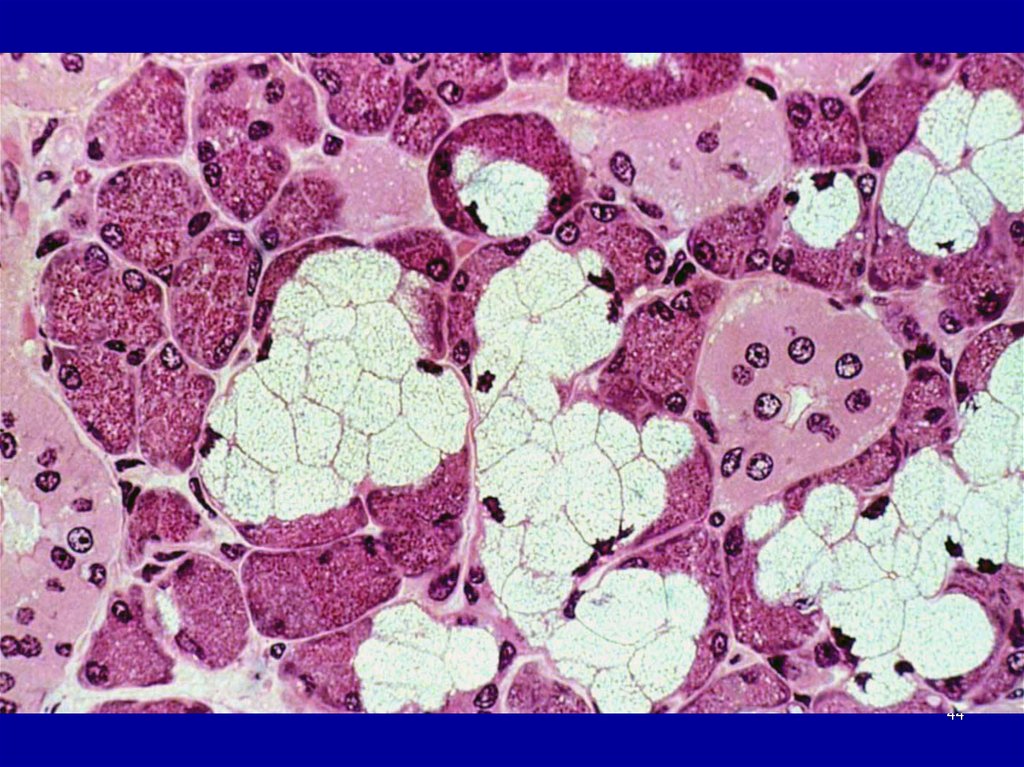
4243. Submandibular Gland
Mixed glandsmostly serous
• Some mucous
acini capped with
serous demilunes
can be found
among serous
acini
• Intercalated
ducts less
extensive than in
parotid
43
44.
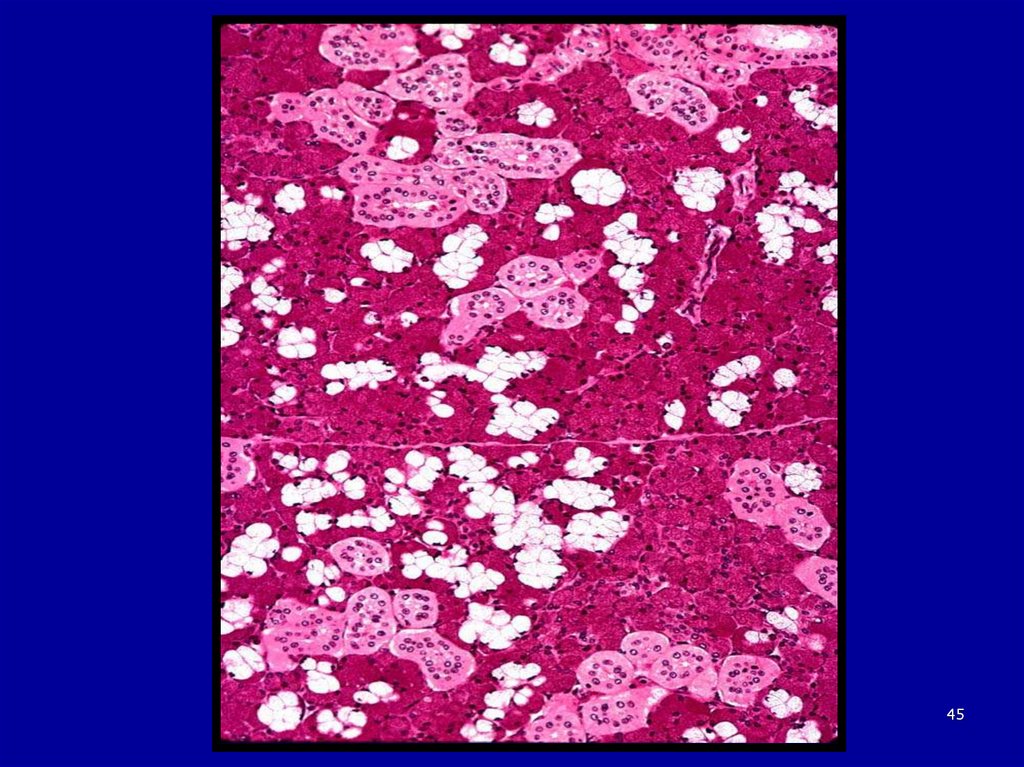
4445.
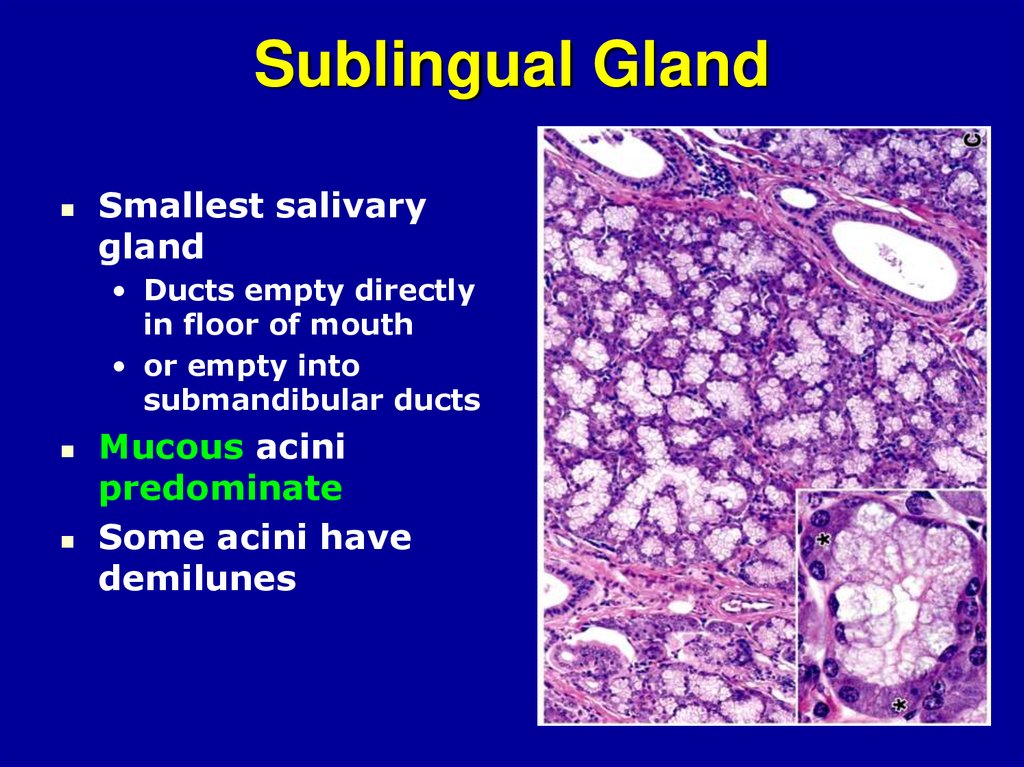
4546. Sublingual Gland
Smallest salivarygland
• Ducts empty directly
in floor of mouth
• or empty into
submandibular ducts
Mucous acini
predominate
Some acini have
demilunes
46
47.
4748. Sublingual Gland Cont.
4849. Teeth
Embedded and attached tomaxilla and mandible
16 permanent teeth in each jaw:
•2
•2
•2
•4
•6
Central incisors
Lateral incisors
Canine
premolar teeth
molar teeth
49
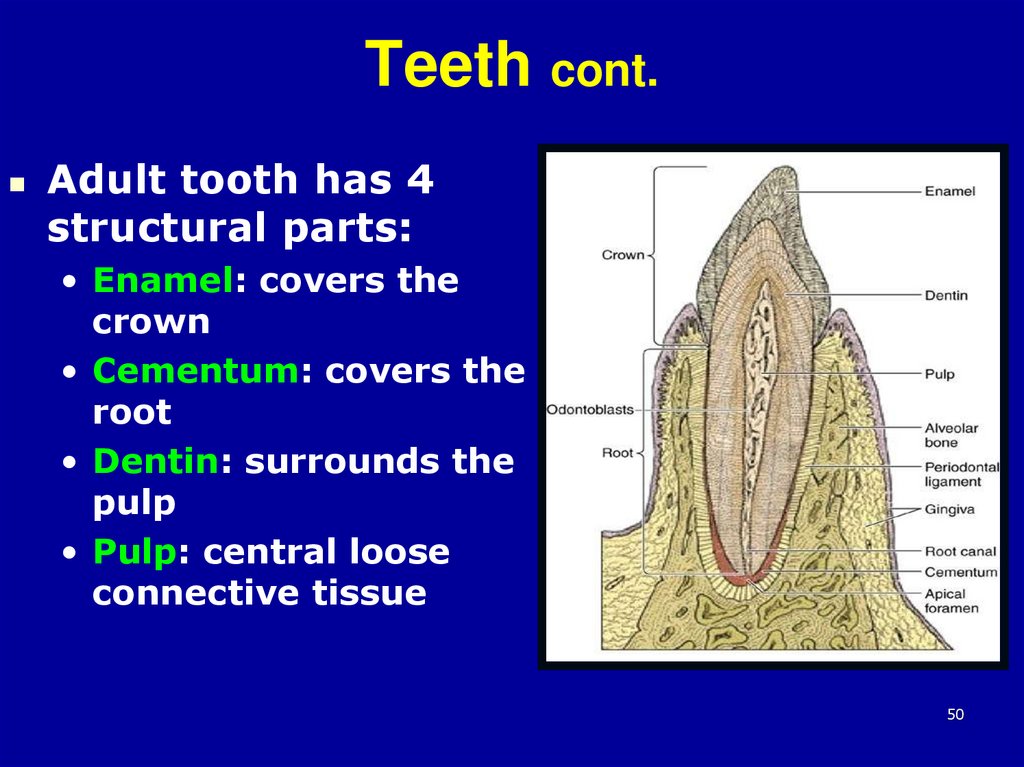
50. Teeth cont.
Adult tooth has 4structural parts:
• Enamel: covers the
crown
• Cementum: covers the
root
• Dentin: surrounds the
pulp
• Pulp: central loose
connective tissue
50
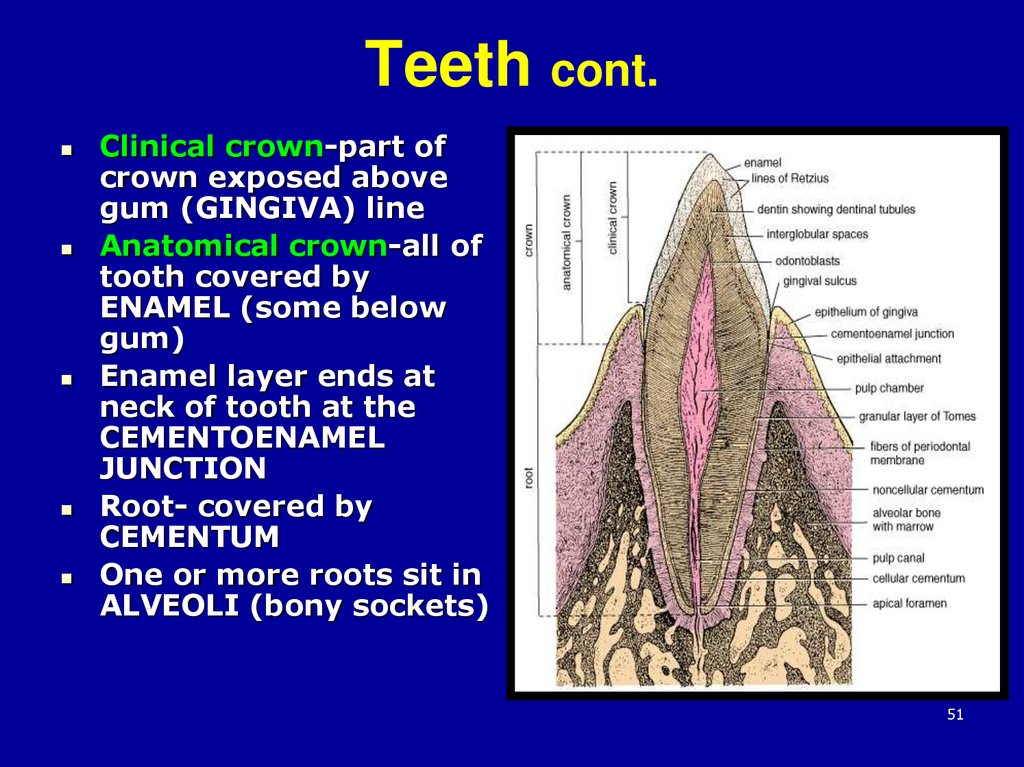
51. Teeth cont.
Clinical crown-part ofcrown exposed above
gum (GINGIVA) line
Anatomical crown-all of
tooth covered by
ENAMEL (some below
gum)
Enamel layer ends at
neck of tooth at the
CEMENTOENAMEL
JUNCTION
Root- covered by
CEMENTUM
One or more roots sit in
ALVEOLI (bony sockets)
51
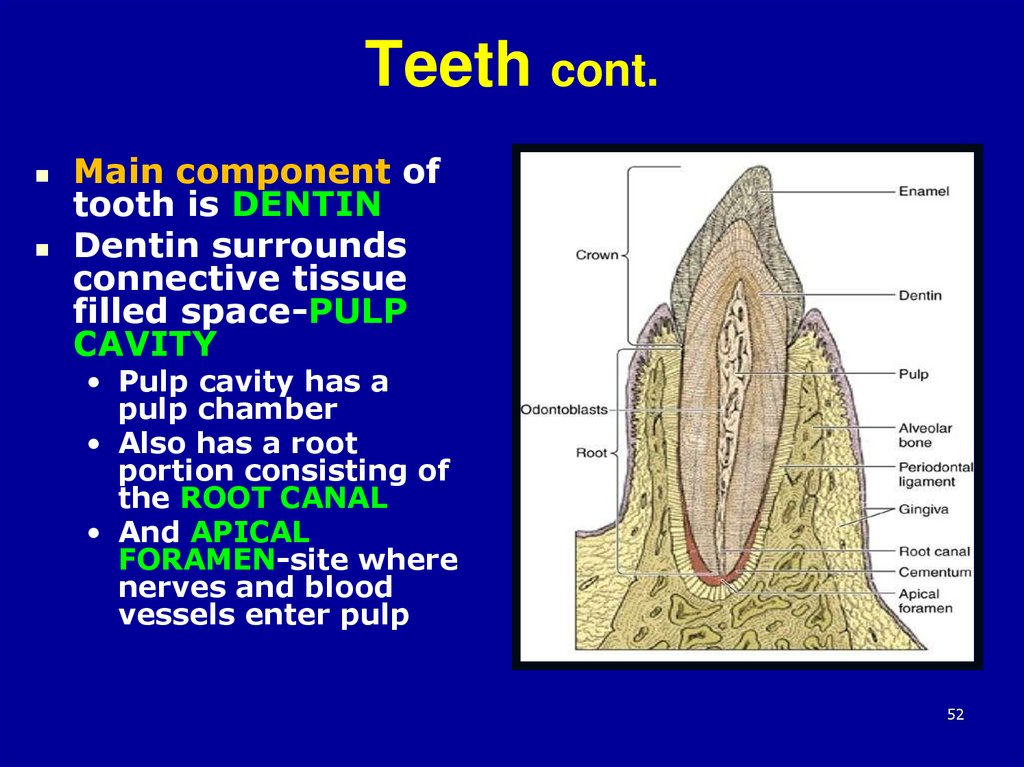
52. Teeth cont.
Main component oftooth is DENTIN
Dentin surrounds
connective tissue
filled space-PULP
CAVITY
• Pulp cavity has a
pulp chamber
• Also has a root
portion consisting of
the ROOT CANAL
• And APICAL
FORAMEN-site where
nerves and blood
vessels enter pulp
52
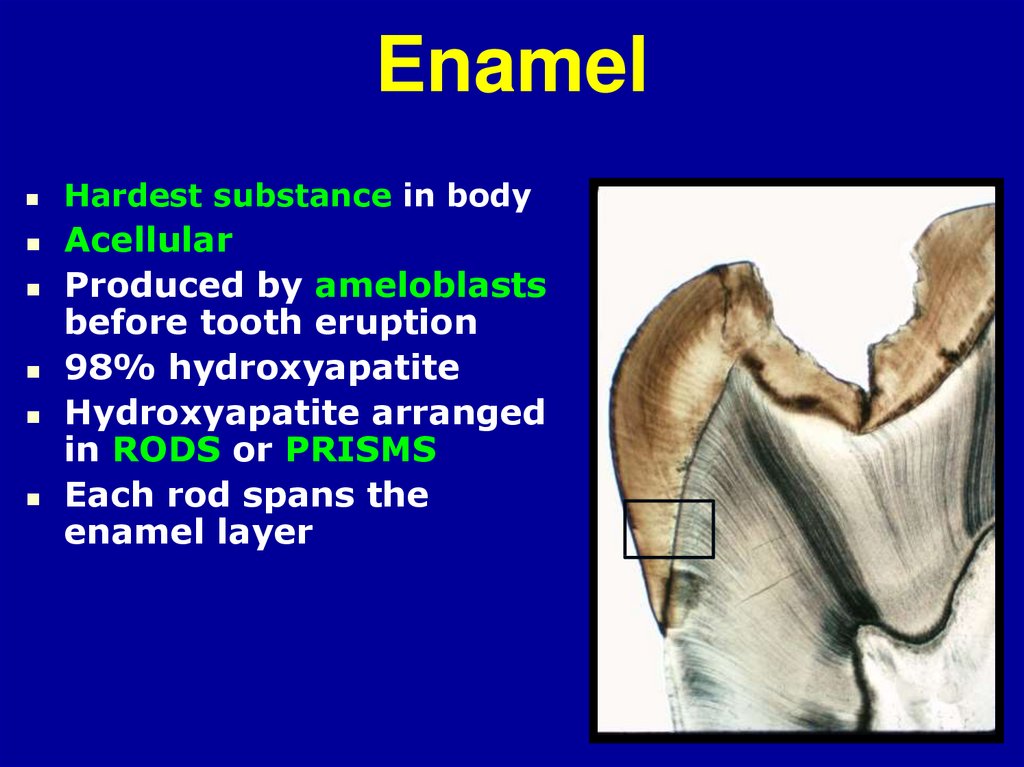
53. Enamel
Hardest substance in bodyAcellular
Produced by ameloblasts
before tooth eruption
98% hydroxyapatite
Hydroxyapatite arranged
in RODS or PRISMS
Each rod spans the
enamel layer
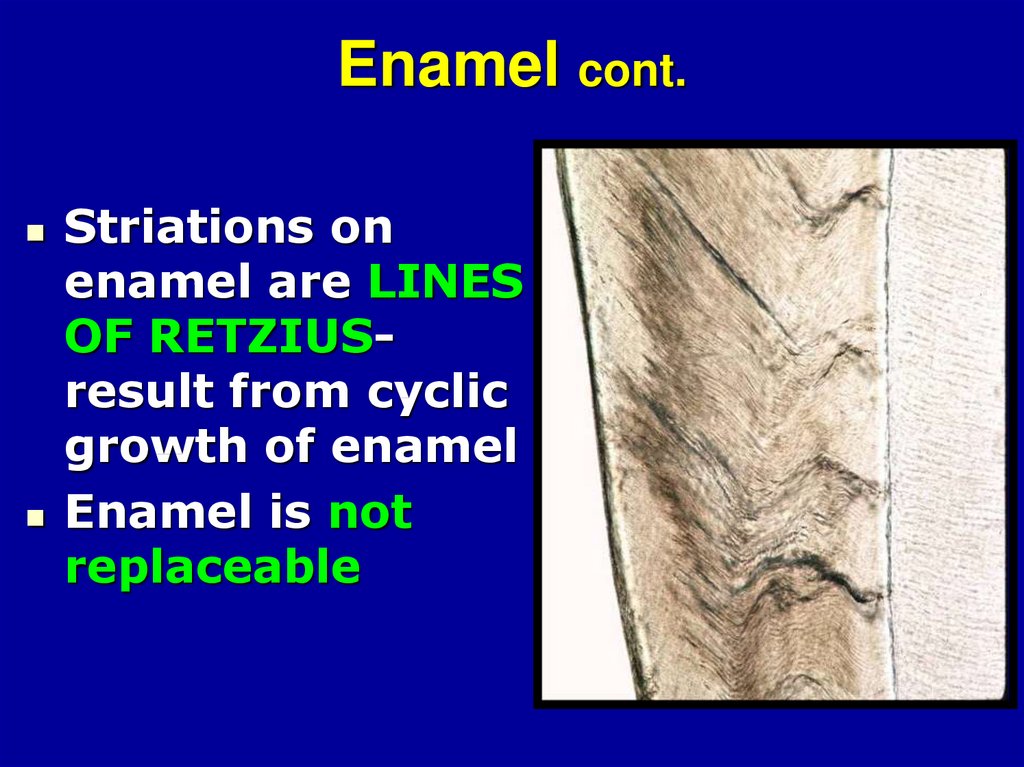
54. Enamel cont.
Striations onenamel are LINES
OF RETZIUSresult from cyclic
growth of enamel
Enamel is not
replaceable
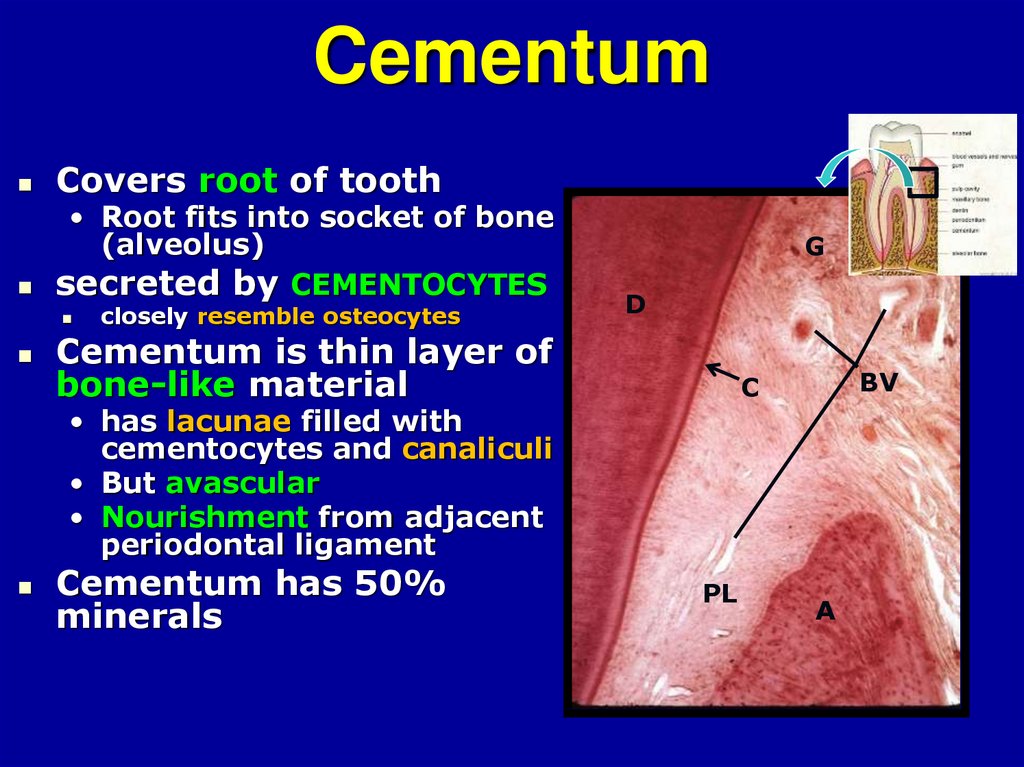
55. Cementum
Covers root of tooth• Root fits into socket of bone
(alveolus)
secreted by CEMENTOCYTES
closely resemble osteocytes
G
D
Cementum is thin layer of
bone-like material
BV
C
• has lacunae filled with
cementocytes and canaliculi
• But avascular
• Nourishment from adjacent
periodontal ligament
Cementum has 50%
minerals
PL
A
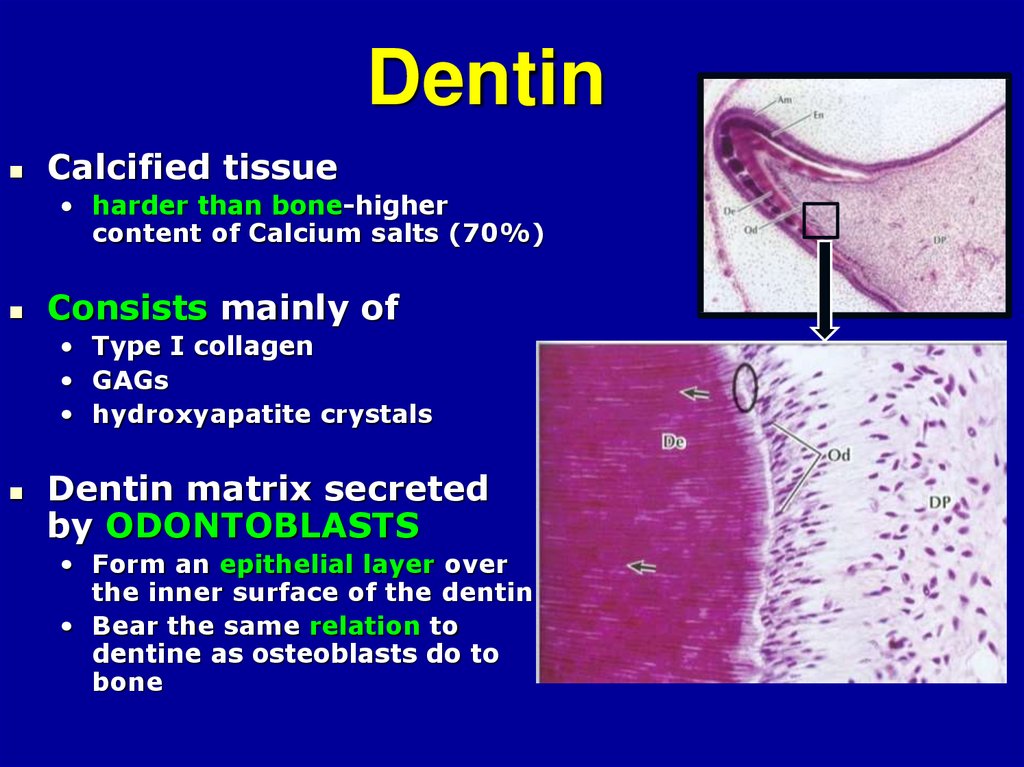
56. Dentin
Calcified tissue• harder than bone-higher
content of Calcium salts (70%)
Consists mainly of
• Type I collagen
• GAGs
• hydroxyapatite crystals
Dentin matrix secreted
by ODONTOBLASTS
• Form an epithelial layer over
the inner surface of the dentin
• Bear the same relation to
dentine as osteoblasts do to
bone
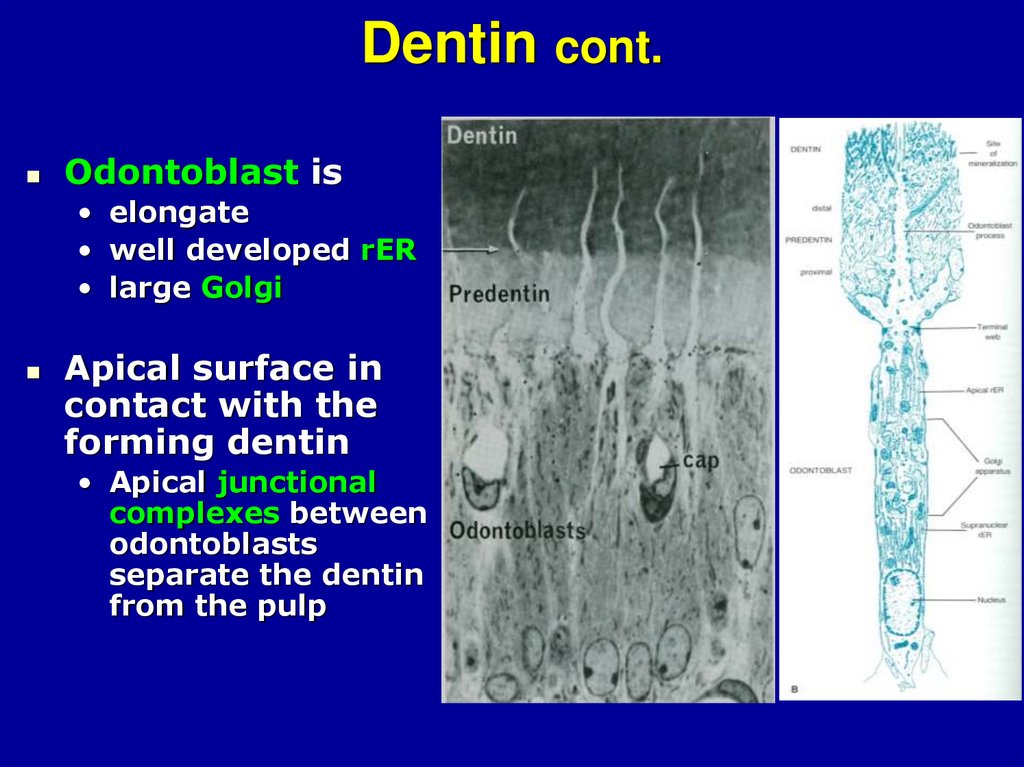
57. Dentin cont.
Odontoblast is• elongate
• well developed rER
• large Golgi
Apical surface in
contact with the
forming dentin
• Apical junctional
complexes between
odontoblasts
separate the dentin
from the pulp
58.
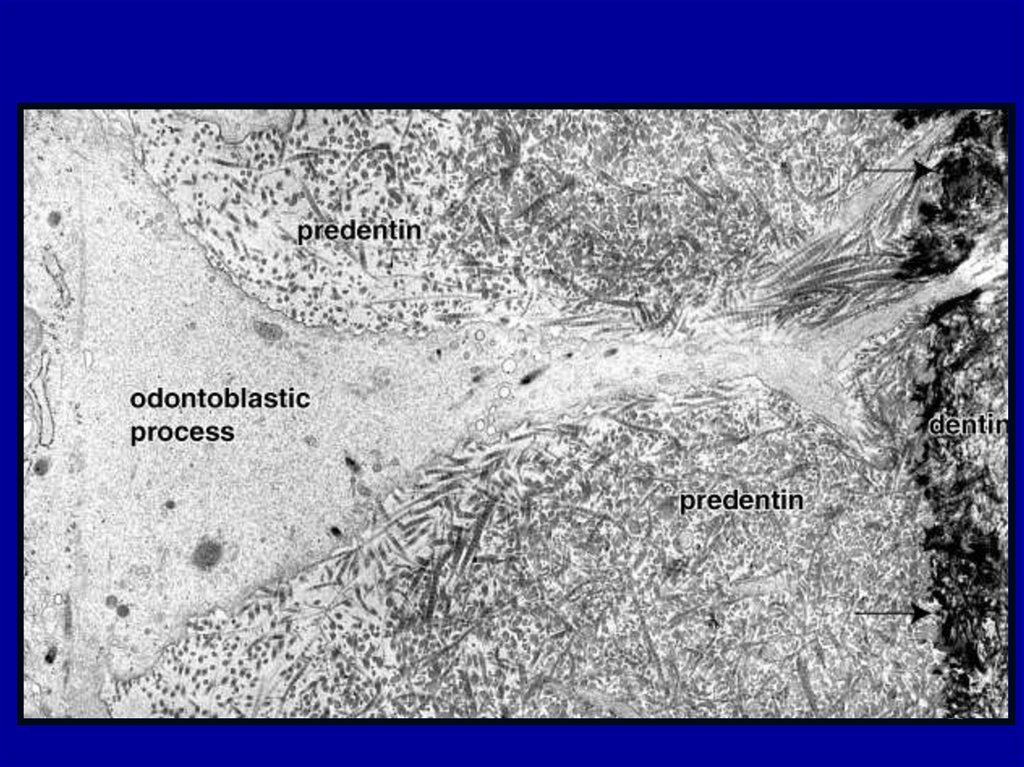
Dentin cont.Odontoblasts have
branched apical
processes that
penetrates
perpendicularly
through the dentin
• Called odontoblast
processes
• Processes become
longer as the
odontoblast is
displaced centrally
during dentin
deposition
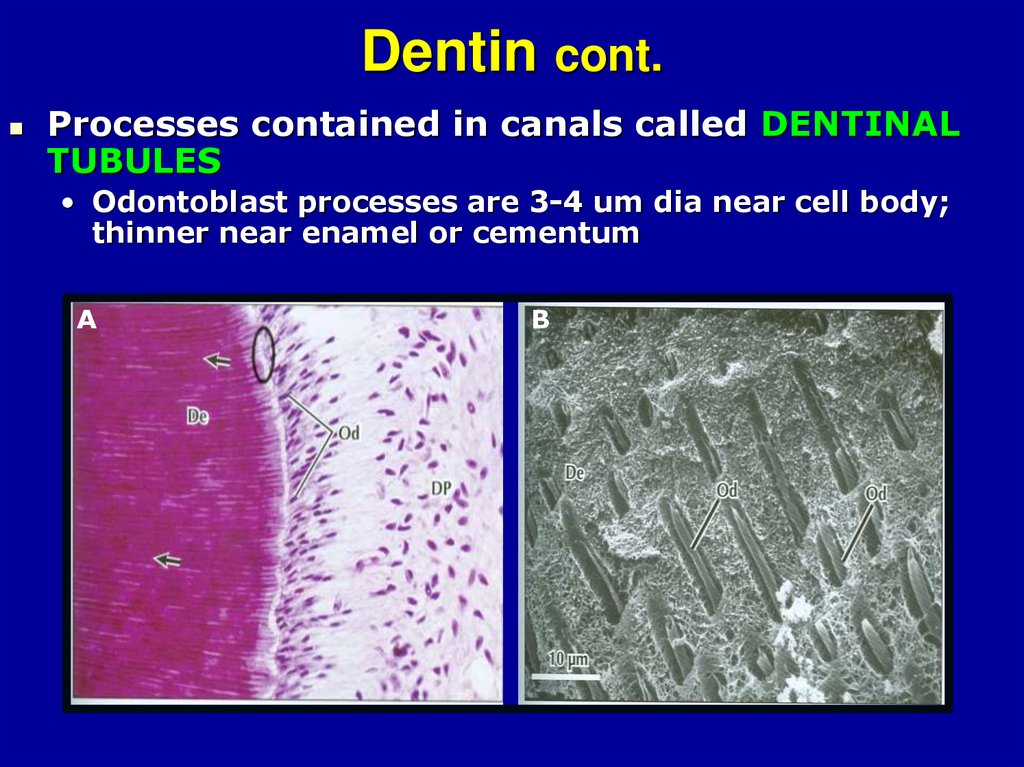
59. Dentin cont.
Processes contained in canals called DENTINALTUBULES
• Odontoblast processes are 3-4 um dia near cell body;
thinner near enamel or cementum
A
B
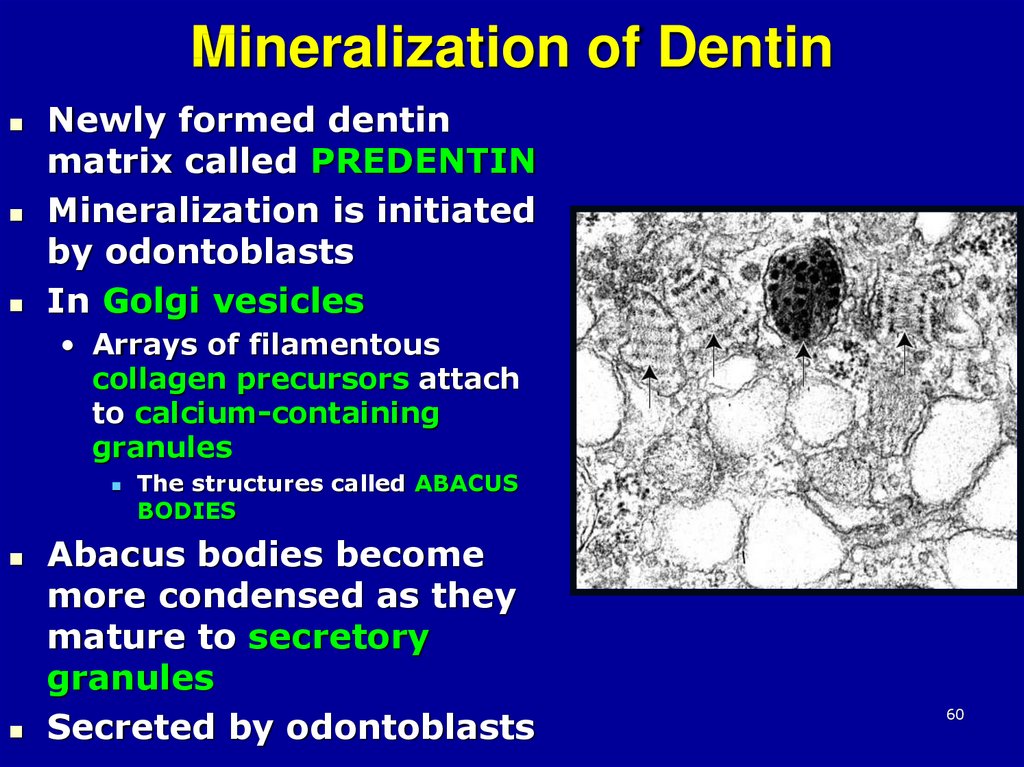
60. Mineralization of Dentin
Newly formed dentinmatrix called PREDENTIN
Mineralization is initiated
by odontoblasts
In Golgi vesicles
• Arrays of filamentous
collagen precursors attach
to calcium-containing
granules
The structures called ABACUS
BODIES
Abacus bodies become
more condensed as they
mature to secretory
granules
Secreted by odontoblasts
60
61.
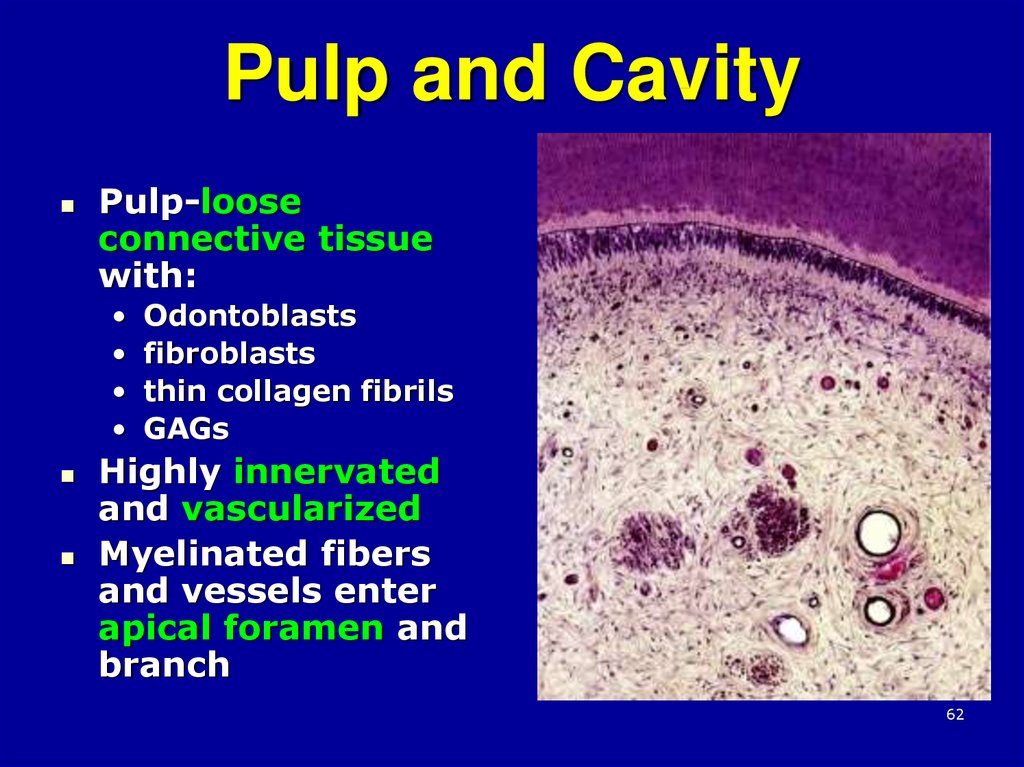
6162. Pulp and Cavity
Pulp-looseconnective tissue
with:
Odontoblasts
fibroblasts
thin collagen fibrils
GAGs
Highly innervated
and vascularized
Myelinated fibers
and vessels enter
apical foramen and
branch
62
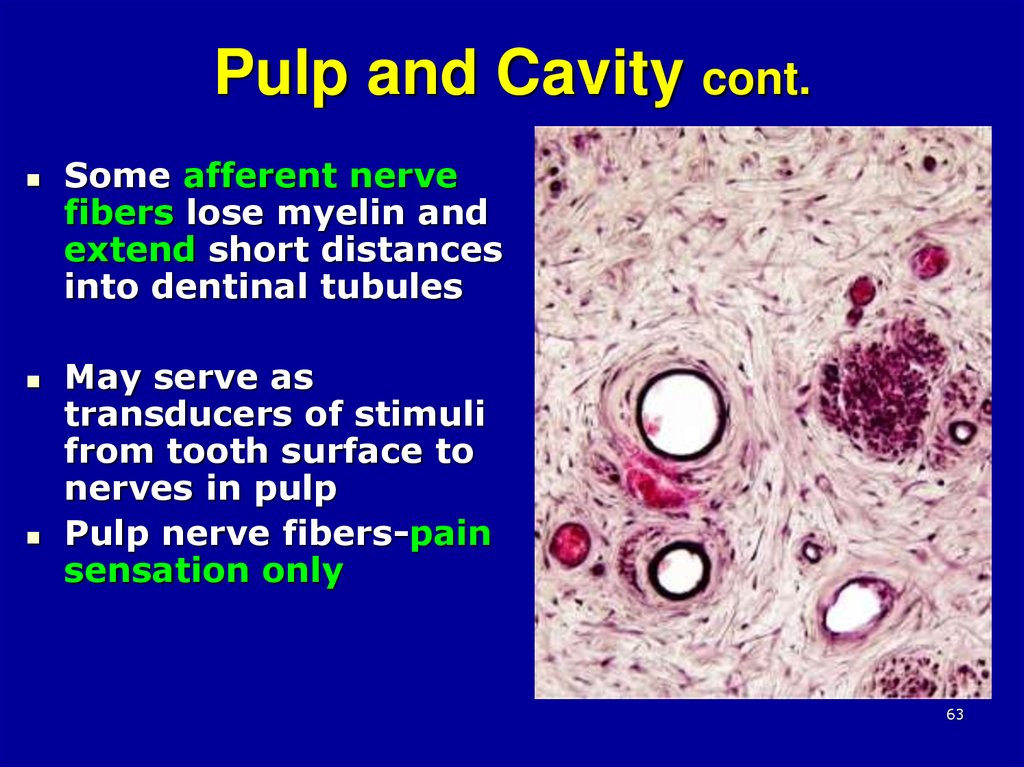
63. Pulp and Cavity cont.
Some afferent nervefibers lose myelin and
extend short distances
into dentinal tubules
May serve as
transducers of stimuli
from tooth surface to
nerves in pulp
Pulp nerve fibers-pain
sensation only
63
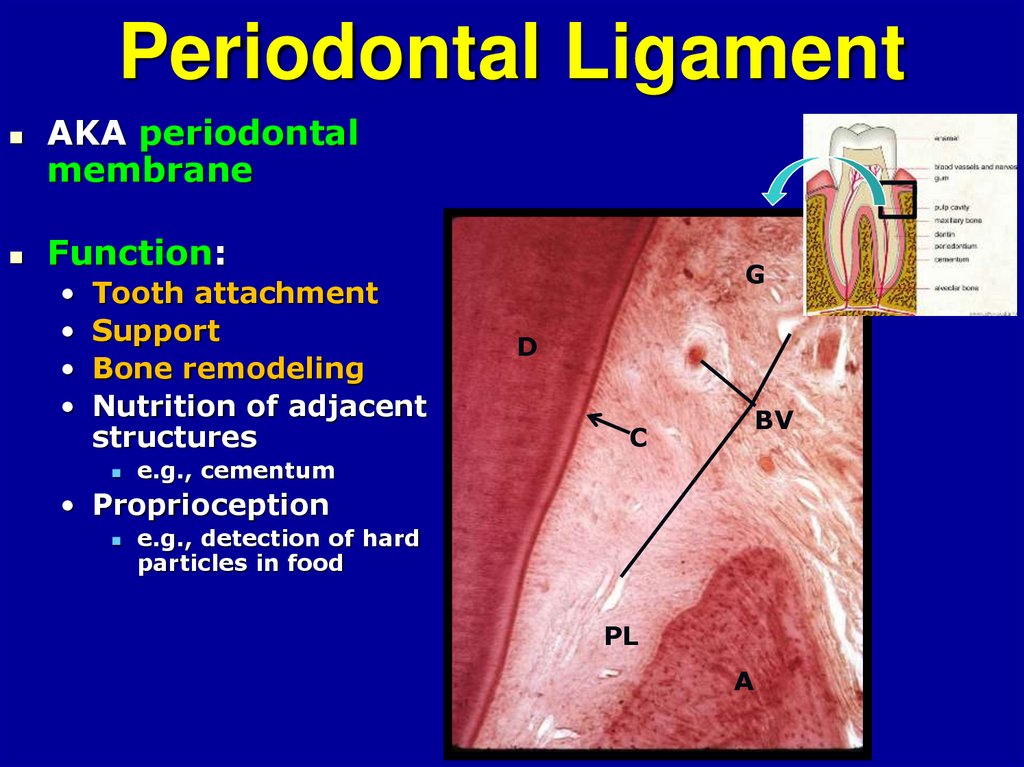
64. Periodontal Ligament
AKA periodontalmembrane
Function:
Tooth attachment
Support
Bone remodeling
Nutrition of adjacent
structures
G
D
BV
C
e.g., cementum
• Proprioception
e.g., detection of hard
particles in food
PL
A
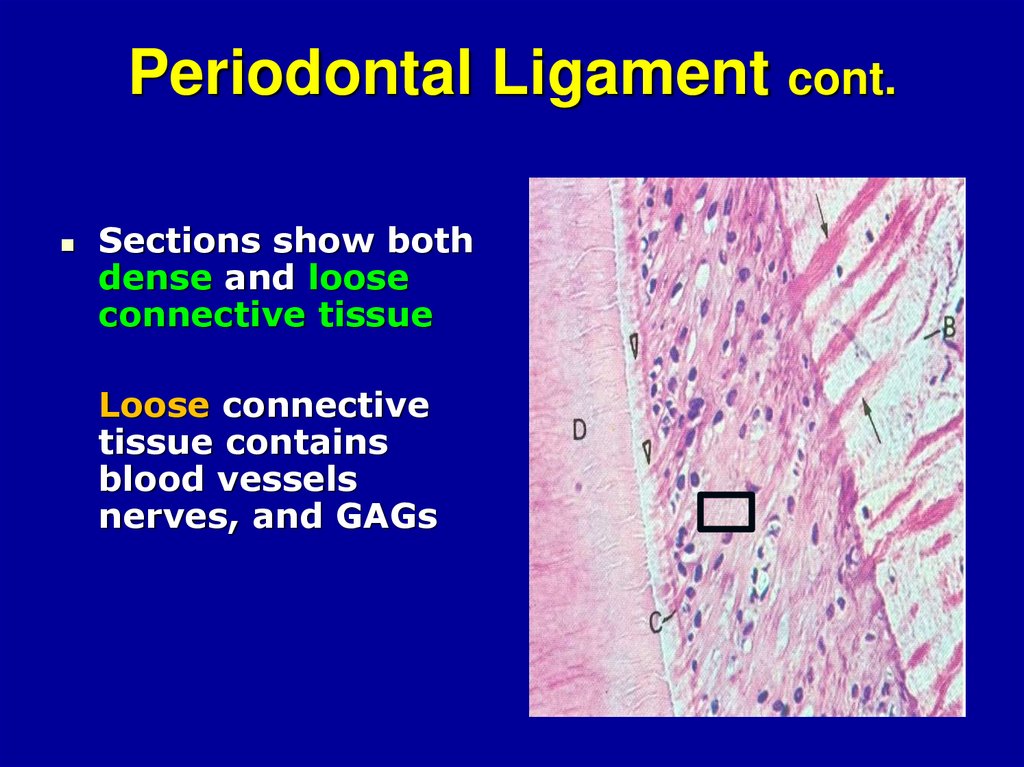
65. Periodontal Ligament cont.
Sections show bothdense and loose
connective tissue
Loose connective
tissue contains
blood vessels
nerves, and GAGs
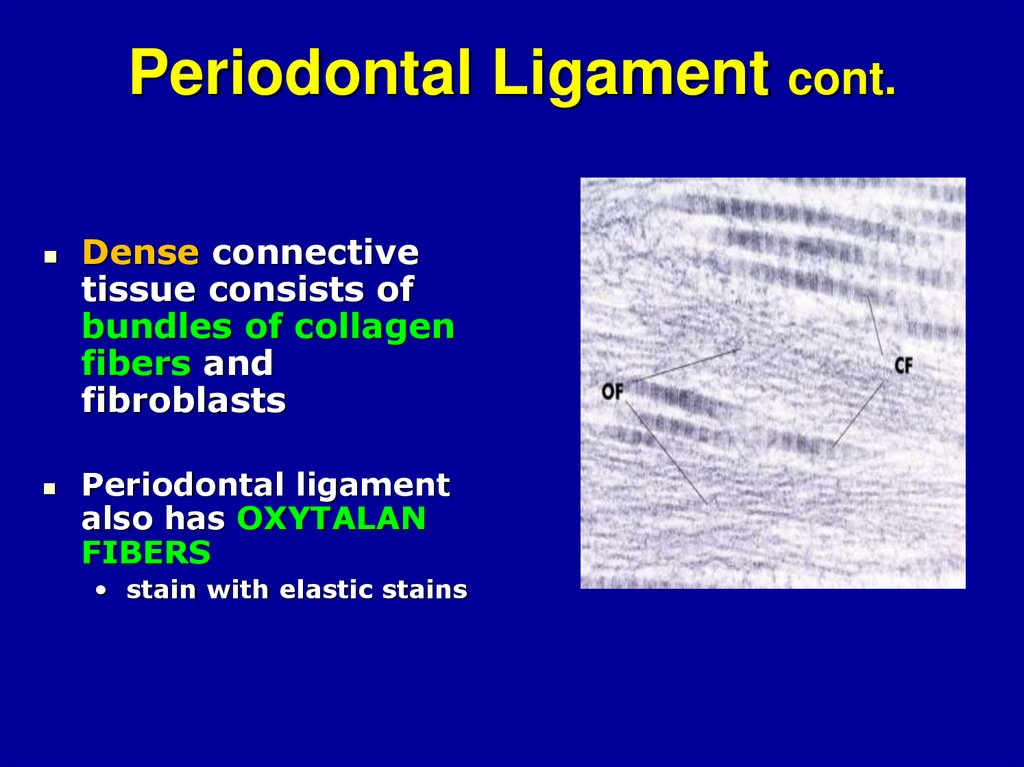
66. Periodontal Ligament cont.
Dense connectivetissue consists of
bundles of collagen
fibers and
fibroblasts
Periodontal ligament
also has OXYTALAN
FIBERS
• stain with elastic stains
67.
Alveolar bonePeriodontal ligament
Collagen fibers are
embedded in the
cementum at one end
and in alveolar bone
at the other
cementum
As Sharpey’s fibers
67
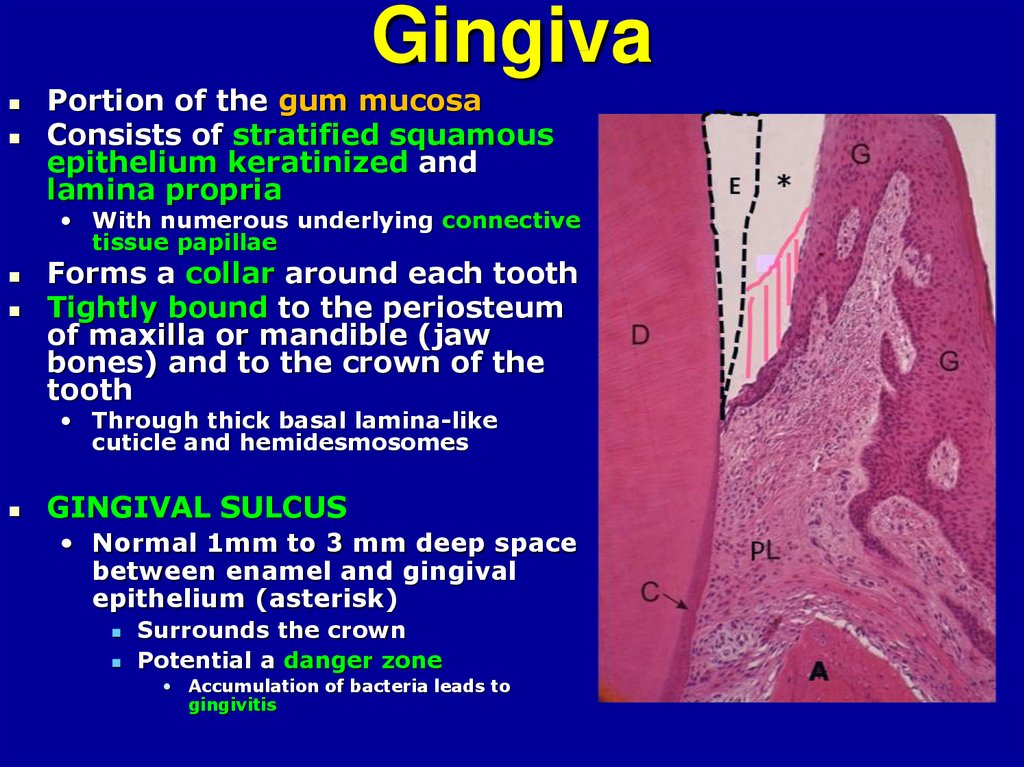
68. Gingiva
Portion of the gum mucosaConsists of stratified squamous
epithelium keratinized and
lamina propria
• With numerous underlying connective
tissue papillae
Forms a collar around each tooth
Tightly bound to the periosteum
of maxilla or mandible (jaw
bones) and to the crown of the
tooth
• Through thick basal lamina-like
cuticle and hemidesmosomes
GINGIVAL SULCUS
• Normal 1mm to 3 mm deep space
between enamel and gingival
epithelium (asterisk)
Surrounds the crown
Potential a danger zone
• Accumulation of bacteria leads to
gingivitis
69. Gingiva cont.
Below the sulcus gingivalepithelium is tightly
adherent:
To the enamel in young
individuals
To the cementum in adults







 Медицина
Медицина